#brain disorder
Text
Here's a quick shout-out to all the disabled and chronically ill with neurological conditions. No matter how your disorder and your symptoms might affect you, know that you are worthy of good things in life.
You are worthy of love.
You are worthy of respect.
You are worthy of compassion.
Speaking from personal experience, life with a brain condition sucks ASS, because our brain is responsible for basically everything we do. The fact that all of us are still pushing through every second of the day is admirable, and you are allowed to celebrate that part of your existence no matter how invisible your efforts might be to those around you (or even to yourself).
And even though life might never be fully "okay" for some of us, because chronic conditions can sadly be a lifelong battle after all, I'm glad that we are here. Cheers to the small victories and joys of life, whatever they might be!
#that includes neurodivergencies btw#if your brain is fucked welcome to the club#brain condition#brain disorder#chronically ill#chronic illness#recovery#lgbtq+#mentally ill#mental illness#depression#personality disorder#bpd#autistic#adhd#autism#iih#idiopathic intracranial hypertension#migraine#tic disorder#pans#pandas#tourrettes#functional neurological disorder#epilepsy#seizures#neurological problems#neurological disorders#positivity#chronic headaches
10 notes
·
View notes
Text

#ocd#brain disorder#amazing#facts#mental disorder#healed#suicide#wow#life saving#crazy#weird#true#real
3 notes
·
View notes
Text
Lupine Publishers | Airway Management of Penetrating Facial Trauma from an Impaled Screwdriver: A Case Report

Abstract
Airway management of a patient with penetrating facial trauma is often anticipated to be difficult. However, due to the variation in presentation of penetrating facial trauma, there are no consensus guidelines established for securing the airway. We present a case of penetrating facial trauma with an impaled screwdriver, describe the anatomical significance of the embedded foreign object, and suggest an approach to airway management. Ultimately, a skilled provider must use his or her clinical judgement and have a clear understanding of anatomy to best approach these unique scenarios.
Introduction
Penetrating facial trauma can present without a compromised airway, but some cases present major challenges with disruption of airway anatomy. Hemorrhage and soft tissue edema may lead to airway obstruction. Nasal bleeding can obscure the airway and the laryngeal and/or tracheal swelling can displace the epiglottis, arytenoid cartilages, and vocal cords, making for difficult visualization and increasing the risk of airway compromise. Other major concerns in these airways are the other potentially unknown injuries to the cervicofacial vasculature, teeth, cervical spine, and brain tissue [1]. Bag-mask ventilation and endotracheal intubation are predicted to be challenging in a patient with maxillofacial trauma. Effective pre-oxygenation prolongs the time that the patient can tolerate apnea, which can be crucial for intubation of an anticipated difficult airway in these patients. Oral endotracheal intubation with rapid-sequence induction and in-line stabilization of the neck is the gold standard in general trauma patients [2]. However, there is no current consensus amongst the anesthesia community on airway management of penetrating maxillofacial injuries and much variability exists [2-5]. Here, we present a case of an impaled foreign body to the face and our approach to airway management of this patient. Written consent was obtained from the patient and a Health Information Portability and Accountability Act (HIPAA) authorization form was completed. This manuscript adheres to the applicable Case Report (CARE) guidelines for case reports.
Case Description
A middle-aged male with an unknown past medical history presented with an impaled screwdriver within the left maxilla immediately adjacent to the nose. The patient was agitated, confused, and intoxicated. No loss of consciousness or other bodily injuries were noted. A computerized tomography scan performed in the emergency room showed the screwdriver to be penetrating through the maxilla and entering the clivus with the tip in the prepontine cistern. The patient was transported directly to the operating room with a cervical spine collar in place for emergent intubation and control of nasal hemorrhage. He was breathing spontaneously, and the physical examination revealed multiple midface fractures, significant bloody secretions from the oronasopharynx, and a Mallampati class IV airway. The location of the screwdriver prohibited bag-mask ventilation, so the patient was pre-oxygenated with a nasal cannula at 10 L-min-1 of oxygen. He was then premedicated with midazolam and fentanyl prior to any intubation attempts. The oropharynx was gently suctioned, and 4% lidocaine hurricane spray was administered. Because of the anticipated difficult airway, an awake fiberoptic intubation was performed. The image from the bronchoscope was significantly obscured by bloody secretions from the injury.
In addition, the patient was unable to cooperate for the awake fiberoptic intubation, as he was intoxicated and confused. Hence, the procedure was abandoned. A second effort was then attempted using a C-MAC® video laryngoscope (Karl Storz, Tuttlingen, Germany) with a size 3 blade. In-line stabilization was performed by the anesthesia team, preventing extension or flexion of the cervical spine during the intubation attempt. A small dose of propofol was given, but no paralytic was administered, and the patient was maintained on spontaneous respiration. Direct visualization of the cords with a Grade 1 view was obtained on the video laryngoscope screen, without significant secretions blocking the view. A size 8.0 endotracheal tube was passed a traumatically through the cords, the cuff was inflated, and the endotracheal tube was secured (Figure 1). There were no desaturation episodes and oxygen saturation were maintained above 95% throughout the procedure. Appropriate placement was confirmed by bilateral chest rise, equal and bilateral breath sounds, and positive end-tidal CO2 on capnography. Following intubation, the surgical team packed the nose to control the bleeding. The nasal ala and the vestibular lacerations were repaired, and the patient was transferred to interventional radiology for angiography and embolization of the bleeding vessels. Intraoperative fluoroscopy and angiography of the cerebral vessels revealed the final point of contact of the screwdriver to be the posterior face of the clivus, but without any significant cervical or intracranial vascular abnormalities (Figures 2&3). The left sphenopalatine and descending palatine branches of the left maxillary artery were successfully embolized and the patient returned to the operating room for the removal of the screwdriver. The patient eventually underwent definitive surgical management of his facial fractures and was discharged home without complications.
Discussion
This patient had a screwdriver penetrating the clivus, a bony depression of the cranium that is occupied by the pons (Figure 2). The clivus is an important landmark because the basilar artery lies posterior to it; lateral to the clivus are the foramina lacerum bilaterally, from where the internal carotid arteries enter into the middle cranial fossa to form the Circle of Willis. Injury to any of these structures would likely have caused neurological injury or life-threatening bleeding. From the initial scan in the emergency room, it was unclear whether the screwdriver perforated any of the major blood vessel of the brain. The surgery team did not want to remove or move the screwdriver due to the risk of neurological injury. Thus, four vessel angiographies of the brain were performed to assess the integrity of blood vessels, and only when it was confirmed that no vessels were involved, was the screwdriver removed. In penetrating facial trauma, oropharyngeal anatomy could be distorted by edema or blocked by hemorrhage, which could prevent a proper mask fit and seal or effective air transfer to the lungs [2]. Facemask ventilation was impossible in this case due to the proximity of the screwdriver to the nose. Another concern at the time of intubation was that the tip of the screwdriver was known to be in the clivus, which meant any movement of the screwdriver by a mask pushing on it may result in vascular or brain damage. An aggravated patient who has impending hypoxemia combined with the risk of aspiration or cervical-spine injury could lead to the life-threatening “can’t intubate, can’t ventilate” scenario, especially if there is administration of a paralytic before securing the airway. In this case, we fitted a nasal cannula with high flow oxygen for pre-oxygenation to maximize oxygenation and held paralytics to allow the patient to breathe spontaneously during any intubation attempts as mask ventilation was difficult in this patient.
This patient also had significant bleeding into the oropharynx from the transection of the left sphenopalatine and descending palatine branches of the left maxillary artery, which branches from the left external carotid artery (Figure 3). Bleeding in the airway can contribute to difficult intubation and mask ventilation. A rapidly expanding hematoma causing airway obstruction must also be considered [6]. Even though awake fiberoptic intubation is the standard for traumatic airway injury and has been successfully performed in other instances of penetrating facial injury [5], it was unsuccessful in this case because the patient had active hemorrhage from an arterial transection that significantly obscured visualization of the airway anatomy. Furthermore, the patient was intoxicated and uncooperative with the fiberoptic intubation and every attempt with the bronchoscope only worsened his agitation. In emergency situations such as this, specialized experience plays a major role. The American Society of Anesthesiologists has a difficult airway algorithm, which has been adopted for trauma. As a part of the algorithm, if awake intubation is not possible and if the patient has a recognized difficult airway, then the next step in management suggests proceeding with surgical or percutaneous surgical access of the airway [7] Fortunately, while preparing for surgical airway access in this patient, the attempt with the C-MAC® video laryngoscope was successful. The camera attached below the video laryngoscope blade was not blurred by blood, and successful endotracheal intubation was achieved while the patient was still breathing spontaneously. In addition, extreme caution was undertaken to avoid overextension of the neck or bucking, as the slightest movement could worsen a cervical spine injury or damage the basilar or internal carotid artery (Figure 3).
Conclusion
In conclusion, there is no unified approach for airway management in penetrating facial trauma. An appropriately skilled provider is needed to manage these airways and anticipate difficulties such as the inability to mask ventilate, severe hemorrhage, or obscured airway view. An anesthesiologist should be comfortable basing his or her decision-making process on the clinical scenario rather than relying on a preset algorithm. Finally, a full understanding of anatomy is required to consider the significance of other potentially unknown injuries to sensibly apply basic and advanced airway management techniques.
for more information about Global Journal of Anesthesia & Pain Medicine archive page click on below link
https://lupinepublishers.com/anesthesia-pain-medicine-journal/archive.php
for more information about lupine publishers page click on below link
https://lupinepublishers.com/index.php
4 notes
·
View notes
Text
i used to be so good at writing strong, thoroughly-researched, thoroughly-edited essays.
as a kid in hs, my teacher literally came up to me, holding my 40 page essay on the intersection of the European witch hunts and capitalism/exploitation/gender roles (it was supposed to be 7 pages...whoops) and went like "this is literally a master's-degree level thesis. what are you doing?? you could literally use this as your final dissertation in a master's program, what the fuck."
NOW??? NOW?? you'd think I'd be oh so skilled. but alas. i can barely piece together two ideas. adhd skill-regression is so so real. im SOBBING
#this is just me ranting sorry#im very tired and hungry#and i want to sleep but brain go brrrrr#well i used to be nice and smart and now im neither of those or however the song goes#pretty sure he was exaggerating cause looking back. it was good. but some of the wording was a lil wonky#adhd#actually adhd#executive dysfunction#actually neurodiverse#adhd paralysis#adult adhd#attention deficit hyperactivity disorder#adhd hacks#academia#neurodivergent#adhd skill regression#confessions of a burnt out gifted kid#<< i guess#former gifted kid#burnt out gifted kid#gifted kid burnout#realizing i sound rly pretentious here sorry -- formal speech patterns i picked up as an autistic child and never put down again haha
41K notes
·
View notes
Text

#autism#actually autistic#autistic brain#autistic adult#autism spectrum disorder#autistic culture#autistic characters#autistic experiences#being autistic
108K notes
·
View notes
Text
seeing people my age talk about how scared they are of memory loss, which they only associate with old age, is so surreal to see as a 24 year old who has actively experienced memory loss for a long time now
there are causes for memory loss besides dementia and alzheimer’s, i hope y’all know that. dissociative disorders, trauma, brain injuries, thyroid problems, even just stress and lack of sleep can fuck up your ability to store, process, and access memory. and that’s just a few of the many causes i can think of off the top of my head right now.
please stop treating disabled people like some scary “other” that you might become only in the distant, decades-away future. we are your age, too. you may become one of us sooner than you know. stop acting like memory loss marks the end of a life, when so many of us have so much living left to do!
#diary#memory loss#memory disorder#dementia#alzheimers#dissociative disorder#dissociative amnesia#dissociation#dissociative identity disorder#trauma#brain injury#memory#amnesia#actually dissociative#complex dissociative disorder#osddid#osdd system#dissociative system#other specified dissociative disorder#did system
20K notes
·
View notes
Text
The Emotional Terrain of Caregiving
Betys’s show today features the remarkable Elliot Sisters—Natalie, JJ, and Emilie. Natalie is the Founder of Sisterhood of Care, LLC, JJ is the eldest, and Emilie is a hands-on caregiver for their mother battling Parkinson’s Disease. In the interview, we discussed the importance of understanding family dynamics in caregiving, emphasizing how recognizing each member’s strengths contributes to a…

View On WordPress
#Betsy Wurzel#Brain Disease#Brain Disorder#Caregiving#Families Grieving#Heros#Natalie Elliot#Parkinson Disease#Veterans
0 notes
Text
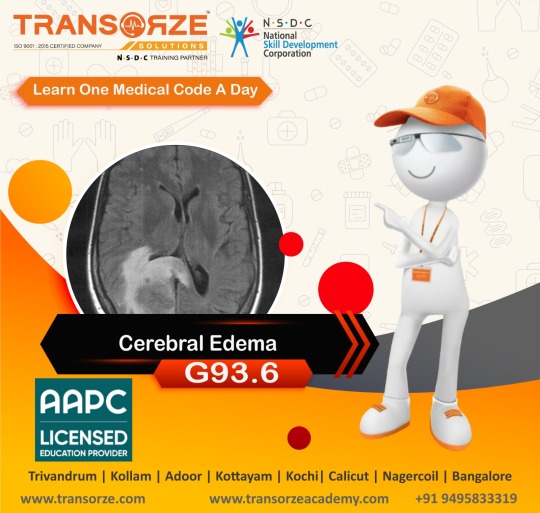
ICD-10 code G93. 6 for Cerebral edema is a medical classification as listed by WHO under the range - Diseases of the nervous system.
For more details:
🌐 www.transorze.com
☎️ 9495833319
#medical coding#icd 10#cerebral edema#health#brain disorder#nervous system#hospitals#medical sector#transorze calicut#transorze dubai#transorzesolutions
1 note
·
View note
Text
#lmao#for anyone who's curious the process went:#send ask to aita official#blog blows up#someone realizes its a chexer fic#i follow them bc they seem cool#i join their rvb server#their encouragement pushes me to finish the Actual Fic i was working on#i expand the fic to be more of a whole au after it comes out much better than expected#the next fic in the au that i work on has to do with a character's brain injury#this leads me to do research into brain injuries#''......huh. this sounds. a lot like the neurological symptoms that my doctors have been saying is just part of my anxiety disorder''#think on that for a while#go to the ER for unrelated reasons#remember my theory#bring it up to the doctor#Doctor Immediate Concern#doctors orders a ct scan#''eeyup! that there's some atrophying and a chiari malformation! y'ever had a head injury''#(i had had several)#''well! shit! time to refer you to neurosurgery :) see if we cant do somethin about all that memory loss and severe pain and shit''#and now we are here#it also lead me to research osddid systems for the first fic#and now my therapist is having me tested for osdd because i did not know that those symptoms were not a thing everyone experiences#so like. thanks for helping me meet friends who could encourage me to engage with the things i like + learn more about myself#^ ^ <3#im actually not gonna say ''ok last update fr this time'' bc idfk maybe something WOULD be funny to post on here
6K notes
·
View notes
Text
As someone who is somewhat of a “veteran” of the online ND community, I’m disappointed in the lack of positivity and love for lesser known diverse cognitive conditions, and the opposing abundance of posts about “cures” or outdated criteria or treatments for those conditions. So, without further ado, I want to say hello to anyone with any of the disorders I’m listing, and give them the love and support that hardly anyone else in our community has… Shoutout to:
People with Down syndrome
People with Fragile X
People with William’s syndrome
People with dyslexia
People with dyspraxia
People with dyscalculia
People with dysgraphia
People with Prader-Willi syndrome
People with PANS or PANDAS
People with aphasia
People with a TBI (traumatic brain injury)
People with chronic/early onset mental illnesses
People with cerebral palsy
People with FASD or were otherwise disabled via other substances in utero
And many, many more I may have forgotten to list (but still support and love, I will add more to my list)
You are all beautiful and wonderful, and you all deserve so more love, appreciation, acceptance and support. You are just as neurodiverse as the rest of us, and your voices deserve to be heard and amplified.
I love you all ❤️
#autism#autistic#actually autistic#neurodivergent#actually neurodiverse#audhd#sensory processing disorder#down syndrome#fragile x#fragile x syndrome#williams syndrome#dyslexia#dyspraxia#dyscalculia#prader willi#aphasia#tbi#traumatic brain injury#chronically ill#chronic mental illness#cerebral palsy#fasd#neurodivergent love#dysgraphia#pans#pandas
8K notes
·
View notes
Text

They should publish books in this format.
FYI: There are apps and plug-ins of this Bionic Reading for Google Play, Chrome, Microsoft Edge (Internet Explorer), Firefox, iOS (Apple) and on WEB
#bionic reading#bionicreading#adhd#living with adhd#adhd things#adhd brain#adhd tips#adhd warrior#helpful#brain fog#living with chronic illness#living with fibro#spoonie witch#life hacks#life hacks for adhd#life hacks for spoonies#chronic fatigue#adhd stuff#attention deficit disorder (add)#add#attention deficit#attention deficit hyperactivity disorder#spectrum#dyslexia#dyslexic#neurodivergent#neurodivergency#focusing problems
17K notes
·
View notes
Note
I wish my father was dead. All he does is yell and scream and I don't have the money to move out even with my job because I'm a full time student who works part time and most of the money I make goes toward medical bills. He has verbally abused me ever since I was 2. I am terrified of him. It's worse because he's a cop and thinks he does nothing wrong. I try to tell him how I feel and he just yells more. He has an incurable and rare brain disorder that causes him pain but I dont care. I'm glad he's in pain because he deserves it. I wish the disease would just kill him. He hates that I'm queer and I so far up trump's ass you wouldn't believe it. I'm a transplant patient and he cares more about him comfort than my health. I hate being at home because he's retired now so he's always home ready to yell at me no matter how hard I try to please him. I wish he'd fucking die.
Hey there,
This sounds like a really difficult to be in.
You mentioned that your father has an incurable and rare brain disorder that causes him pain, I am not sure what he has been diagnosed with and nor am I a doctor, but is it possible that part of his brain disorder is him not having full control over his temper? Even if this is the case though, I know that this doesn’t change anything in regards to you feeling terrified of him, but if this is the case (in regards to his brain disorder) then it may help you to put into perspective that he doesn’t really mean what he is saying? Just a thought!
Being a transplant patient and having to live with an abusive father for whatever reason is never easy and especially as you cannot move out due to most of your finances going towards medical bills. But do you have any close friends you could possibly sleep over at or another family member when your father is being particular abusive (more so than he often is) so that you can have some respite from him? Having a break may be really helpful and will also enable you to look after yourself a bit as well and recharge your batteries.
Although I know personally how easy it is to wish for another person’s death, there are more practical things that you can be doing with your time, for example one idea may be to find some things you can do after work and when you are not busy studying to help keep you out of the house for a bit longer – like joining some kind of group perhaps.
I really hope that this has helped a bit and please do let us know if we can help to support you in any other way!
I’m thinking of you and hope that you are going well!
Take care,
Lauren
#mha-lauren#advice#advice blog#mental health advice#anonymous#wanting father to be dead#brain disorder#incurable and rare#abusive#transplant patient#full time student#working part time
0 notes
Text
#its always october in my brain#dissociation#shifting#shiftblr#shifting community#desired reality#dr#dreamer#maladaptive daydreaming#maladapting daydreaming disorder
5K notes
·
View notes
Text
If you have speech issues due to brain fog or psychosis or schizophrenia spectrum or intellectual disability or aphasia or whatever reason love you forever. We are not stupid, we are not freaks, we are disabled (if you identify that way) and deserve to be normalized. Speak "strange" forever
-schizophrenic with somewhat constant disorganized speech and writing
#i didnt correct this post even though i normally do because i want to let people know some grammar#issues are not the end of the world or cause a lack of legitamacy#disorganized speech#brain fog#actuallypsychotic#actually schizophrenic#pseriouslyschizospectrum#aphasia#disordered speech#not tagging id because i dont wanna soeak over actually id people in the tag but you are thr most important
6K notes
·
View notes
Link
Taking care of a loved one with dementia poses several challenges for caregivers and family members. Dementia is a progressive brain disorder that interferes with how a person communicates. It can also cause mood swings and change a person’s behavior and personality. It makes it all the more challenging to communicate and provide elder care.
0 notes
Text
What are they desperatley trying to tell you
In today’s episode 18 of the Truth, Lies, & Alzheimer’s show, Lisa goes into depth about how effective communication is key to working with Alzheimer’s disease and dementia sufferers. Probably the most difficult challenge for family members and caregivers to overcome is the ability to understand what people who are living with dementia are trying to tell them, especially when they can no longer…

View On WordPress
#Alzheimers#Brain Disorder#caregiver#Dementia#Dementia Advocate#Depression#Lisa Skinner#Truth Lies and Alzheimers
0 notes