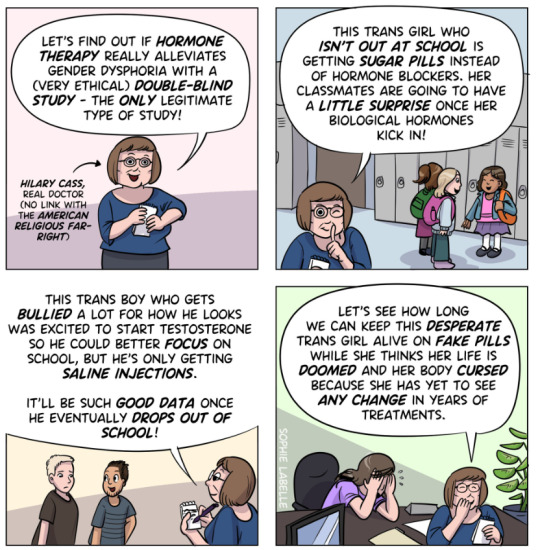
#Dr. Hilary Cass
Text
By: Andy L.
Published: Apr 14, 2024
It has now been just little under a week since the publication of the long anticipated NHS independent review of gender identity services for children and young people, the Cass Review.
The review recommends sweeping changes to child services in the NHS, not least the abandonment of what is known as the “affirmation model” and the associated use of puberty blockers and, later, cross-sex hormones. The evidence base could not support the use of such drastic treatments, and this approach was failing to address the complexities of health problems in such children.
Many trans advocacy groups appear to be cautiously welcoming these recommendations. However, there are many who are not and have quickly tried to condemn the review. Within almost hours, “press releases“, tweets and commentaries tried to rubbish the report and included statements that were simply not true. An angry letter from many “academics”, including Andrew Wakefield, has been published. These myths have been subsequently spreading like wildfire.
Here I wish to tackle some of those myths and misrepresentations.
-
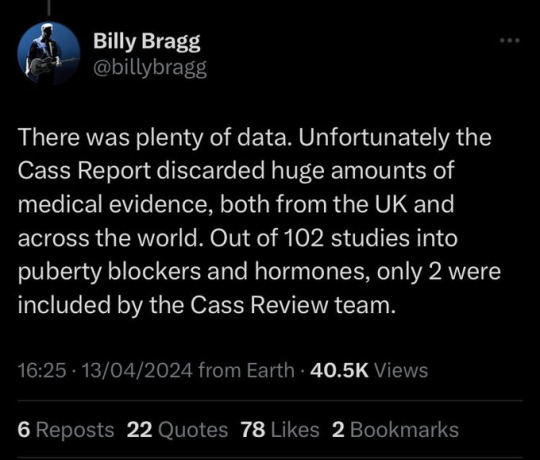
Myth 1: 98% of all studies in this area were ignored
Fact
A comprehensive search was performed for all studies addressing the clinical questions under investigation, and over 100 were discovered. All these studies were evaluated for their quality and risk of bias. Only 2% of the studies met the criteria for the highest quality rating, but all high and medium quality (50%+) studies were further analysed to synthesise overall conclusions.
Explanation
The Cass Review aimed to base its recommendations on the comprehensive body of evidence available. While individual studies may demonstrate positive outcomes for the use of puberty blockers and cross-sex hormones in children, the quality of these studies may vary. Therefore, the review sought to assess not only the findings of each study but also the reliability of those findings.
Studies exhibit variability in quality. Quality impacts the reliability of any conclusions that can be drawn. Some may have small sample sizes, while others may involve cohorts that differ from the target patient population. For instance, if a study primarily involves men in their 30s, their experiences may differ significantly from those of teenage girls, who constitute the a primary patient group of interest. Numerous factors can contribute to poor study quality.
Bias is also a big factor. Many people view claims of a biased study as meaning the researchers had ideological or predetermined goals and so might misrepresent their work. That may be true. But that is not what bias means when we evaluate medical trials.
In this case we are interested in statistical bias. This is where the numbers can mislead us in some way. For example, if your study started with lots of patients but many dropped out then statistical bias may creep in as your drop-outs might be the ones with the worst experiences. Your study patients are not on average like all the possible patients.
If then we want to look at a lot papers to find out if a treatment works, we want to be sure that we pay much more attention to those papers that look like they may have less risk of bias or quality issues. The poor quality papers may have positive results that are due to poor study design or execution and not because the treatment works.
The Cass Review team commissioned researchers at York University to search for all relevant papers on childhood use of puberty blockers and cross-sex hormones for treating “gender dysphoria”. The researchers then graded each paper by established methods to determine quality, and then disregarded all low quality papers to help ensure they did not mislead.
The Review states,
The systematic review on interventions to suppress puberty (Taylor et al: Puberty suppression) provides an update to the NICE review (2020a). It identified 50 studies looking at different aspects of gender-related, psychosocial, physiological and cognitive outcomes of puberty suppression. Quality was assessed on a standardised scale. There was one high quality study, 25 moderate quality studies and 24 low quality studies. The low quality studies were excluded from the synthesis of results.
As can be seen, the conclusions that were based on the synthesis of studies only rejected 24 out of 50 studies – less than half. The myth has arisen that the synthesis only included the one high quality study. That is simply untrue.
There were two such literature reviews: the other was for cross-sex hormones. This study found 19 out of 53 studies were low quality and so were not used in synthesis. Only one study was classed as high quality – the rest medium quality and so were used in the analysis.
12 cohort, 9 cross-sectional and 32 pre–post studies were included (n=53). One cohort study was high-quality. Other studies were moderate (n=33) and low-quality (n=19). Synthesis of high and moderate-quality studies showed consistent evidence demonstrating induction of puberty, although with varying feminising/masculinising effects. There was limited evidence regarding gender dysphoria, body satisfaction, psychosocial and cognitive outcomes, and fertility.
Again, it is myth that 98% of studies were discarded. The truth is that over a hundred studies were read and appraised. About half of them were graded to be of too poor quality to reliably include in a synthesis of all the evidence. if you include low quality evidence, your over-all conclusions can be at risk from results that are very unreliable. As they say – GIGO – Garbage In Garbage Out.
Nonetheless, despite analysing the higher quality studies, there was no clear evidence that emerged that puberty blockers and cross-sex hormones were safe and effective. The BMJ editorial summed this up perfectly,
One emerging criticism of the Cass review is that it set the methodological bar too high for research to be included in its analysis and discarded too many studies on the basis of quality. In fact, the reality is different: studies in gender medicine fall woefully short in terms of methodological rigour; the methodological bar for gender medicine studies was set too low, generating research findings that are therefore hard to interpret. The methodological quality of research matters because a drug efficacy study in humans with an inappropriate or no control group is a potential breach of research ethics. Offering treatments without an adequate understanding of benefits and harms is unethical. All of this matters even more when the treatments are not trivial; puberty blockers and hormone therapies are major, life altering interventions. Yet this inconclusive and unacceptable evidence base was used to inform influential clinical guidelines, such as those of the World Professional Association for Transgender Health (WPATH), which themselves were cascaded into the development of subsequent guidelines internationally.
-
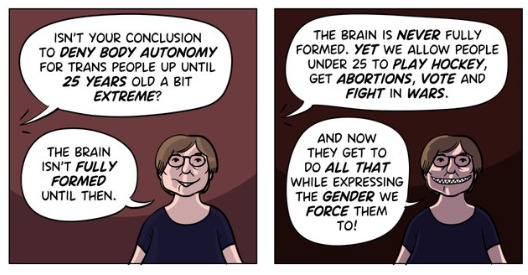
Myth 2: Cass recommended no Trans Healthcare for Under 25s
Fact
The Cass Review does not contain any recommendation or suggestion advocating for the withholding of transgender healthcare until the age of 25, nor does it propose a prohibition on individuals transitioning.
Explanation
This myth appears to be a misreading of one of the recommendations.
The Cass Review expressed concerns regarding the necessity for children to transition to adult service provision at the age of 18, a critical phase in their development and potential treatment. Children were deemed particularly vulnerable during this period, facing potential discontinuity of care as they transitioned to other clinics and care providers. Furthermore, the transition made follow-up of patients more challenging.
Cass then says,
Taking account of all the above issues, a follow-through service continuing up to age 25 would remove the need for transition at this vulnerable time and benefit both this younger population and the adult population. This will have the added benefit in the longer-term of also increasing the capacity of adult provision across the country as more gender services are established.
Cass want to set up continuity of service provision by ensure they remain within the same clinical setting and with the same care providers until they are 25. This says nothing about withdrawing any form of treatment that may be appropriate in the adult care pathway. Cass is explicit in saying her report is making no recommendations as to what that care should look like for over 18s.
It looks the myth has arisen from a bizarre misreading of the phrase “remove the need for transition”. Activists appear to think this means that there should be no “gender transition” whereas it is obvious this is referring to “care transition”.
-
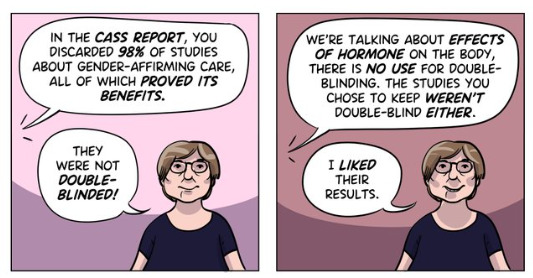
Myth 3: Cass is demanding only Double Blind Randomised Controlled Trials be used as evidence in “Trans Healthcare”
Fact
While it is acknowledged that conducting double-blind randomized controlled trials (DBRCT) for puberty blockers in children would present significant ethical and practical challenges, the Cass Review does not advocate solely for the use of DBRCT trials in making treatment recommendations, nor does it mandate that future trials adhere strictly to such protocols. Rather, the review extensively discusses the necessity for appropriate trial designs that are both ethical and practical, emphasizing the importance of maintaining high methodological quality.
Explanation
Cass goes into great detail explaining the nature of clinical evidence and how that can vary in quality depending on the trial design and how it is implemented and analysed. She sets out why Double Blind Randomised Controlled Trials are the ‘gold standard’ as they minimise the risks of confounding factors misleading you and helping to understand cause and effect, for example. (See Explanatory Box 1 in the Report).
Doctors rely on evidence to guide treatment decisions, which can be discussed with patients to facilitate informed choices considering the known benefits and risks of proposed treatments.
Evidence can range from a doctor’s personal experience to more formal sources. For instance, a doctor may draw on their own extensive experience treating patients, known as ‘Expert Opinion.’ While valuable, this method isn’t foolproof, as historical inaccuracies in medical beliefs have shown.
Consulting other doctors’ experiences, especially if documented in published case reports, can offer additional insight. However, these reports have limitations, such as their inability to establish causality between treatment and outcome. For example, if a patient with a bad back improves after swimming, it’s uncertain whether swimming directly caused the improvement or if the back would have healed naturally.
Further up the hierarchy of clinical evidence are papers that examine cohorts of patients, typically involving multiple case studies with statistical analysis. While offering better evidence, they still have potential biases and limitations.
This illustrates the ‘pyramid of clinical evidence,’ which categorises different types of evidence based on their quality and reliability in informing treatment decisions

The above diagram is published in the Cass Review as part of Explanatory Box 1.
We can see from the report and papers that Cass did not insist that only randomised controlled trials were used to assess the evidence. The York team that conducted the analyses chose a method to asses the quality of studies called the Newcastle Ottawa Scale. This is a method best suited for non RCT trials. Cass has selected an assessment method best suited for the nature of the available evidence rather than taken a dogmatic approach on the need for DBRCTs. The results of this method were discussed about countering Myth 1.
Explainer on the Newcastle Ottawa Scale
The Newcastle-Ottawa Scale (NOS) is a tool designed to assess the quality of non-randomized studies, particularly observational studies such as cohort and case-control studies. It provides a structured method for evaluating the risk of bias in these types of studies and has become widely used in systematic reviews and meta-analyses.
The NOS consists of a set of criteria grouped into three main categories: selection of study groups, comparability of groups, and ascertainment of either the exposure or outcome of interest. Each category contains several items, and each item is scored based on predefined criteria. The total score indicates the overall quality of the study, with higher scores indicating lower risk of bias.
This scale is best applied when conducting systematic reviews or meta-analyses that include non-randomized studies. By using the NOS, researchers can objectively assess the quality of each study included in their review, allowing them to weigh the evidence appropriately and draw more reliable conclusions.
One of the strengths of the NOS is its flexibility and simplicity. It provides a standardized framework for evaluating study quality, yet it can be adapted to different study designs and research questions. Additionally, the NOS emphasizes key methodological aspects that are crucial for reducing bias in observational studies, such as appropriate selection of study participants and controlling for confounding factors.
Another advantage of the NOS is its widespread use and acceptance in the research community. Many systematic reviews and meta-analyses rely on the NOS to assess the quality of included studies, making it easier for researchers to compare and interpret findings across different studies.
As for future studies, Cass makes no demand only DBRCTs are conducted. What is highlighted is at the very least that service providers build a research capacity to fill in the evidence gaps.
The national infrastructure should be put in place to manage data collection and audit and this should be used to drive continuous quality improvement and research in an active learning environment.
-
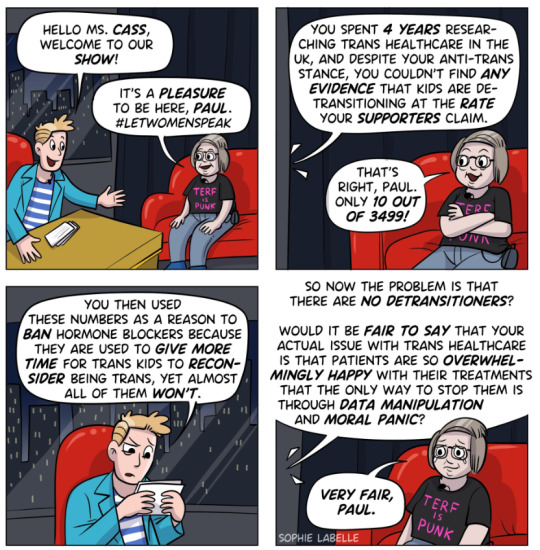
Myth 4: There were less than 10 detransitioners out of 3499 patients in the Cass study.

Fact
Cass was unable to determine the detransition rate. Although the GIDS audit study recorded fewer than 10 detransitioners, clinics declined to provide information to the review that would have enabled linking a child’s treatment to their adult outcome. The low recorded rates must be due in part to insufficient data availability.
Explanation
Cass says, “The percentage of people treated with hormones who subsequently detransition remains unknown due to the lack of long-term follow-up studies, although there is suggestion that numbers are increasing.”
The reported number are going to be low for a number of reasons, as Cass describes:
Estimates of the percentage of individuals who embark on a medical pathway and subsequently have regrets or detransition are hard to determine from GDC clinic data alone.
There are several reasons for this:
Damningly, Cass describes the attempt by the review to establish “data linkage’ between records at the childhood gender clinics and adult services to look at longer term detransition and the clinics refused to cooperate with the Independent Review. The report notes the “…attempts to improve the evidence base have been thwarted by a lack of cooperation from the adult gender services”.
We know from other analyses of the data on detransitioning that the quality of data is exceptionally poor and the actual rates of detransition and regret are unknown. This is especially worrying when older data, such as reported in WPATH 7, suggest natural rates of decrease in dysphoria without treatment are very high.
Gender dysphoria during childhood does not inevitably continue into adulthood. Rather, in follow-up studies of prepubertal children (mainly boys) who were referred to clinics for assessment of gender dysphoria, the dysphoria persisted into adulthood for only 6–23% of children.
This suggests that active affirmative treatment may be locking in a trans identity into the majority of children who would otherwise desist with trans ideation and live unmedicated lives.
I shall add more myths as they become spread.
==
It's not so much "myths and misconceptions" as deliberate misinformation. Genderists are scrambling to prop up their faith-based beliefs the same way homeopaths do. Both are fraudulent.
#Andy L.#Cass Review#Cass Report#Dr. Hilary Cass#Hilary Cass#misinformation#myths#misconceptions#detrans#detransition#gender affirming healthcare#gender affirming care#gender affirmation#affirmation model#medical corruption#medical malpractice#medical scandal#systematic review#religion is a mental illness
338 notes
·
View notes
Text
The tide is turning for the TQ+. And they have no one to blame but themselves
Wes Streeting last night admitted he had been wrong to say that “trans women are women” amid a major Labour row over the Cass review into NHS gender care.
The shadow health secretary said the controversial LGBT rights group Stonewall – where he used to work – had got it wrong with its slogan.
In a major about-turn for the party, he told The Sun that he now admitted “there are lots of complexities” on the trans issue but that he was prepared to take criticism “on the chin”.
It came as Labour became embroiled in another trans row after Mr Streeting welcomed the review and pledged to implement it in full.
The shadow health secretary said the report raised “some serious concerns that are pretty scandalous”.

But Rosie Duffield, a Labour MP placed under investigation by the party last year for campaigning against gender ideology, pointed out that women who had exposed the scandal had been “blanked, sidelined and dismissed” by male leaders simply for speaking up.
Last night Mr Streeting was asked on The Sun’s Never Mind The Ballots programme whether he stood by Stonewall’s claim that “trans women are women, get over it”, he admitted: “No.”
He added: “To the extent that – and I say this with some self-criticism and reflection – if you’d asked me a few years ago, on this topic, I would have said trans men are men, trans women are women. Some people are trans, get over it. Let’s move on. This is all blown out of proportion.
“And now I sort of sit and reflect and think actually, there are lots of complexities.”
He went on: “I take the criticism on the chin. And at the same time, I also think that there’s been some absolutely ugly rhetoric directed towards trans people who are at the wrong end of all of statistics on hate crime, on self harm, suicide, mental health.”
Labour has long been divided on trans issues and has been accused of flip-flopping on its stance in recent years.
The party no longer has plans to bring in self-ID for trans people, and Sir Keir Starmer, the Labour leader, has rowed back from saying “trans women are women”, and now states that a woman is an “adult female” and that 99.9 per cent of them do not have a penis.
Mr Streeting’s comments angered the Labour Left. The Corbynite group Momentum tweeted: “The Cass review ignored dozens of scientific studies, coming to a harmful conclusion of limiting access to gender-affirming care for trans youth.
“Anti-trans campaigners have celebrated it. So it’s highly disappointing that Labour’s leadership is welcoming it unreservedly.”
Yesterday, feminist Julie Bindel demanded an apology from Mr Streeting for failing to support her gender-critical views when he was president of the National Union of Students.
Earlier this year, the party dropped a year-long investigation into a complaint that Ms Duffield had been transphobic for liking a tweet by Father Ted creator Graham Linehan, who is now a gender-critical campaigner.
However, despite the changes, critics of the Labour leadership say gender-critical women in the party continue to be sidelined or not selected.

Wes Streeting says the Cass report raised 'some serious concerns that are pretty scandalous' CREDIT: Jay Williams
The Cass review, published on Wednesday, said much of the evidence for gender medicine was flimsy and that drugs such as puberty blockers should be used with extreme caution as children who think they are trans may have mental health problems.
Dr Hilary Cass, the paediatrician behind the report, said some NHS gender clinics refused to comment on requests for information.
On Never Mind the Ballots, Mr Streeting said: “I think we’ve got to ask ourselves why is it that we’ve seen medical interventions that have been given on the basis of very weak evidence?
“How is it that clinicians have been silenced or afraid to come forward? Why is it that a group of young people who are extremely vulnerable are waiting years to access treatment?
“I think there’s plenty of blame to go around. I’m pretty angry actually that despite this review having been commissioned there are some NHS trusts that refused to co-operate.
“And I want to send a clear message to them that under a Labour government there’ll be accountability for that, you’re not going to get away with it. And I want to work constructively with the Government to try to get this right.”
Earlier, he had tweeted: “Children’s healthcare should always be led by evidence and children’s welfare, free from culture wars…
“The Government must now immediately act, but if they do not, the next Labour government will work to implement the expert recommendations of the Cass review, to ensure that young people are receiving appropriate and high-quality care.”
This prompted Ms Duffield to retweet the statement, with the message: “To the many women blanked, sidelined, dismissed by male leaders when speaking up and exposing this for years.”

And Ms Bindel, a former Labour Party member, wrote: “Glad to see you are now openly critical of the gender ideology that led to the atrocities against children outlined in the Cass report.
“I am open to accepting an apology from you. In 2008, when you were NUS president, I was no-platformed alongside five fascist groups for ‘transphobia’.
“I contacted you and asked for your help. You gave none. I asked you to condemn those that had orchestrated the no-platforming, and you refused.
“Have you any idea of the reputational damage this caused me? How it gave others permission to no-platform, denounce and defame me?
“How it meant that I could be slandered by other organisations, and so many, many universities around the UK and elsewhere? If this sounds bitter then good, because I am.”
To this message, Ms Duffield said: “Thank you for leading us all here Julie. Without you, most of us wouldn’t have had a clue what had been happening to children who were far too young to have the critical faculties or agency to consent.”
Addressing Ms Bindel’s accusation, Mr Streeting replied: “From memory (16 years on, so correct me if I’m wrong!) I replied to confirm that you weren’t on NUS’ no platform policy and as this was in relation to a motion passed by the autonomous women’s campaign I was not empowered to overturn it (not least as a male president!).”
#Trans women are men#Labour Party#NHS gender care#Wes Streeting is a rare man that can admit that he was wrong#Rosie Duffield is speaking the truth#Sir Keir Starmer finally admits that women don't have penises#Men seeing the light after women have suffered from stating the obvious#Cass review#Dr Hilary Cass urges caution when gives children life altering drugs and treatments
94 notes
·
View notes
Text
J.K. Rowling has been proven right!
"The Cass Review is a damning indictment of what the NHS has been doing to children.
"Dr Hilary Cass has submitted her final report and recommendations to NHS England in her role as Chair of the Independent Review of gender identity services for children and young people.
"Hilary Cass’s report demolishes the entire basis for the current model of treating gender-distressed children. Its publication is a shameful day for NHS England, which for too long gave vulnerable children harmful treatments for which there was no evidence base. It’s now clear to all that this was quack medicine from the start.
"Dr Cass delivers stinging criticisms of NHS gender clinics, both adult and child, and her description of the Gender Identity Development Service is absolutely damning. It is disgraceful that GIDS, alongside the adult clinics, did not cooperate with her attempt to survey its practice, or to carry out a high-quality, long-term follow-up study on the treatment of children as part of the review, which would have been a global first."

You can read the entire review here. (pdf)

"Glinner" is Graham Linehan, a writer, screenwriter, and comedian who's been fighting against transitioning minors for years, losing friends, his job, and his agent along the way. But he's kept on fighting.

,
;

.

.

The tide has turned in the UK and in Europe. When will American media finally begin reporting on the closing of "gender clinics" and the bans on puberty blockers for children? I figure nothing will happen here in the U.S. until the lawsuits start flooding in. It's already begun. And with proof like the Cass Review and the WPATH files, it's going to be very, very difficult for clinics, doctors, and therapists to continue lying about how transitioning does no permanent and irreversible physical and psychological harm.
#Cass Review#transing kids#JK Rowling#I stand with JK Rowling#Graham Linehan#trans lies#WPATH#WPATH files#gender critical#gender clinics#health#medicine#the tide has turned#David Tennant
468 notes
·
View notes
Text
saw some people saying that the woman who did the cass review, dr hilary cass, is just jealous because “trans women look more like a woman than she does” and to that i gotta say.. so you agree? you agree that your definition of woman is just someone who is feminine and conventionally attractive? you agree that your definition of the word woman reinforces restrictive, oppressive gender roles and stereotypes? you agree that your view of womanhood is regressive and that feminists are correct in opposing it?
#they literally just say shit and don’t think deeper about it#they think using a bunch of snobby academic jargon makes whatever stupid thing they’re about to say true
149 notes
·
View notes
Text
The review even starts from a false premise. “We have no good evidence on the long-term outcomes of interventions to manage gender-related distress,” it proclaims in the introduction. But puberty blockers and cross-sex hormones are better at alleviating distress than Cass claims, not least because she has chosen to exclude the majority of potentially relevant studies from her review.
But there is a greater underlying falsehood. Since 2019, the World Health Organisation has recognised that “trans-related and gender diverse identities are not conditions of mental ill-health, and that classifying them as such can cause enormous stigma.” Dr Hilary Cass, while noting this, opts to resurrect the framework of gender dysphoria, treating transition as a worthwhile endeavour only if it alleviates mental health issues.
But transition is not a mental health issue – it requires medical assistance, which medical practitioners facilitate (another being pregnancy in people who cannot conceive naturally). There will never be a scientific way of ensuring that a trans boy sitting before a clinical psychologist and asking them to let him take testosterone will not come to regret this decision as an adult, though studies suggest exceptionally low rates of regret among children who do have access to transition. The error is in suggesting that the boy should not access testosterone unless this can be definitively determined.
The Cass Review imagines that, with further study, the NHS will finally find the exact combination of sexual orientation, toy preferences in childhood, and pornography consumption habits in adolescence that will reliably predict whether that boy will become a trans man or a cis woman. To this end, Cass obsesses over growing the collection of data. After being ‘thwarted’ in her attempts to force adult gender clinics to hand over patient records, Cass is calling on the government to compel this same violation of patient privacy. Submitting to study will also be a prerequisite to receiving puberty blockers on the NHS.
126 notes
·
View notes
Text
NHS England to stop prescribing puberty blockers
10 hours ago
By Josh Parry,
LGBT & Identity Producer
Children will no longer routinely be prescribed puberty blockers at gender identity clinics, NHS England has confirmed.
The decision comes after a review found there was "not enough evidence" they are safe or effective.
Puberty blockers, which pause the physical changes of puberty, will now only be available as part of research.
It comes weeks before an independent review into gender identity services in England is due to be published.
An interim report from the review, published in 2022 by Dr Hilary Cass, had earlier found there were "gaps in evidence" around the drugs and called for a transformation in the model of care for children with gender-related distress.
Dr Cass's review follows a sharp rise in referrals to the Gender Identity Development Service (Gids), run by the Tavistock and Portman NHS Foundation Trust, which saw an increase from 250 per year to over 5,000 in 2022.
Puberty supressing hormones - more commonly known as puberty blockers - work by suppressing the release of hormones that cause puberty and are often prescribed to children questioning their gender as a way of stopping physical changes such as breast development or facial hair.
Fewer than 100 young people in England are currently prescribed puberty blockers by the NHS. They will all able to continue their treatment.
NHS England held a public consultation on their usage and last year introduced an interim policy which stated they should only be given as part of research trials or in "exceptional circumstances".
The BBC understands that the new policy, confirmed on Tuesday, will not allow them to be prescribed "routinely" outside of a research trial, but that individual clinicians can still apply to have the drugs funded for patients on a case-by-case basis.
Gids is due to close at the end of March. Two new NHS services due in London and Liverpool are set to open at the beginning of April, followed by a number of regional specialist centres over the next two years.
Health Minister Maria Caulfield said: "We have always been clear that children's safety and wellbeing is paramount, so we welcome this landmark decision by the NHS.
"Ending the routine prescription of puberty blockers will help ensure that care is based on evidence, expert clinical opinion and is in the best interests of the child."
The consultation on the future of gender services received more than 4,000 responses, including 10% from trans adults and 5% from clinicians.
John Stewart, national director of specialised commissioning at NHS England, said: "Given that the debate is often very polarised, so too were the responses to the consultation.
"Many people said the policy didn't go far enough in terms of still allowing potential access [to puberty blockers] through research, and others saying clearly they disagreed fundamentally and that these should be routinely available to everyone who believes they need it."
The BBC understands NHS England aims to begin its study into the use of puberty blockers by December 2024, and is yet to decide who can take part
---
Oh hey, will you look at that.
85 notes
·
View notes
Text
When Ritchie Herron woke after gender reassignment surgery, he had a feeling he had made a terrible mistake.
Five years later, his scars still sometimes weep and he cannot walk long distances or ride a bike. “I’ve awakened from what was a mental health crisis, to a body that will be for ever changed and damaged,” he said. He no longer identifies as transgender and is living as a gay man “as best I can, given what has happened”.
Now, the Newcastle-based civil servant, 36, has launched legal action against NHS England, alongside the “heartbroken” father of a 21-year-old who has been booked in for imminent genital-removal surgery at an adult gender clinic. The two men are demanding a judicial review which includes an independent inquiry into the safety of NHS treatments being offered to young people under the age of 25 who are experiencing gender dysphoria.
Steve Barclay, secretary of state for health, and Kemi Badenoch, minister for equalities, as well as Dr Hilary Cass, who carried out a recent review of the Tavistock Gender Identity Development Service (Gids) are also being served with legal papers. The father is hoping to stop the surgery from going ahead.
In a crowdfunding appeal to raise funds for their legal case, launched today, Herron and the father, who wishes to remain anonymous, say that the model of care for gender dysphoria in the NHS adult service is “profoundly unsafe” and “routinely places young people on a pathway towards irreversible lifelong treatment”.
Both Herron and the father’s 21-year-old child have been diagnosed as autistic. According to lawyers representing the two men, the NHS may be discriminating against autistic people, who are disproportionately more likely to be treated in the gender clinics, which is why Badenoch, as minister for equalities, is included in the legal action.
The case comes as a large number of 17-year-olds who have been on the 8,000-strong waiting list of the Tavistock clinic in north London, England’s only NHS gender identity clinic for children, are being referred to the adult service.
At the seven NHS adult gender clinics in England and Wales, surgery and cross-sex hormones are offered after the age of 18. Patients have at least two assessment appointments with a specialist medical practitioner before hormone treatment is recommended, and those who are considering surgical treatment have two further meetings with separate clinical professionals before they are referred.
There has been a sharp rise in the past decade in young people wanting to change gender. From 2011-12 to 2021-22, the number of under-18s in England referred to the Tavistock soared from 210 to 3,585, according to its own figures.
Herron was 25 when he decided he was a woman living in a man’s body. He had been bullied at school and struggled to cope with his parents’ divorce, and was diagnosed in his early 20s with depression and obsessive-compulsive disorder (OCD).
He decided he was transgender and “all my struggles were due to gender dysphoria” — an idea he says was encouraged by older activists in internet forums. He fixated on the idea that “my body was being poisoned by testosterone”, he says.
In 2013, he was referred by his GP to an NHS adult gender clinic, and says he was asked early on by an NHS clinician if he had considered gender reassignment surgery. He attended a private clinic as there was a long NHS waiting list, where he was diagnosed as transgender.
When he was seen by the NHS clinic in 2014, they prescribed testosterone blocker and later oestrogen. He also started therapy with an NHS psychosexual counsellor, which lasted for 100 sessions over five years, after which he was told he would be discharged and that the only other treatment open to him was surgery. He had delayed and cancelled the irreversible operation, which involves removing the penis and testicles and modelling the area to resemble female genitalia, several times over the previous two years, fearing the consequences.
In 2017, he was given another referral for surgery, to be performed at a private hospital but paid for by the NHS.
Finally, in 2018, “two days before my 31st birthday, I underwent a surgery that removed my genitals, inverting them in a procedure that has been marked as refined, but is no more civilised than an amputation” he said.
“Today, despite multiple follow-up surgeries, my scar lines still weep, occasionally becoming inflamed and causing crippling pain. In the flesh cavity that was created to mimic a vagina, I feel mostly nothing, aside from the occasional stabs of pain. I can’t use the toilet properly . . . and no matter how hard I push or strain, a dribble emerges, which may continue for hours after I have left the seat.”
The father who, with Herron, is seeking a judicial review of the adult services, says he is terrified of the possible outcome for his child, who was born a boy and who is due to undergo genital surgery shortly. The young person “is on the autistic spectrum, suffers from anxiety and has very poor mental health”, according to the father. The father believes that, like Herron, they think “becoming a woman will solve so many of his problems”.
“I am one of the many parents who is heartbroken over the journey my son has taken,” said the father, who is paying towards the legal fees for the case. “I know he has been let down by the system and fear for his future.”
Aged 13, the boy, who had struggled at school, “out of the blue” told an NHS child mental health adviser that he believed he was a girl. “He was referred to an NHS clinic and was prescribed puberty blocking drugs to halt his development as soon as he turned 16. I was shocked that such an experimental treatment would be given, despite my objections. His anxiety and his autism were not explored.
“I decided to try to prevent him attending the NHS clinic but was threatened with the possibility of him being taken into care if I stood in his way.
“As a parent, I am deeply concerned to protect my son. I am shut out,” he said. “A system with such limited safeguards, providing a radical experimental treatment with life-long consequences is structurally unfair to people like my son, whose autism makes him more likely to seek the answer to his problems in this radical treatment. He needs more protection, not less.”
The men are being represented by the legal team that helped another de-transitioner, Keira Bell, win a High Court case against Gids to stop children with gender dysphoria being prescribed puberty-blocking drugs. Bell was given the drugs to stop her development aged 16, before later, at an adult clinic, being referred for a double mastectomy. The case was later overturned at the Court of Appeal but led to a critical review of Gids by Dr Hilary Cass. Gids has since been earmarked for closure, although this has been delayed until March 2024, about a year later than first planned.
Herron was not diagnosed with autism until this year, but says he raised the condition with the NHS gender clinic. He adds that if he had received a comprehensive psychological assessment and treatment for conditions such as autism and OCD at the outset, he would never have undergone genital surgery. “I can deal with my own regret, and my own stupidity, but I can’t deal with the fact that I’m not alone in this. That there are not just dozens, or hundreds, but thousands of others like me, and more to come.
“We deserve a safety net, we deserve to be challenged in our beliefs before we make irreversible decisions that have huge lifelong consequences, we deserve to be caught and cared for. We do not deserve to be punished for asking for help, by being castrated and gaslighted into a way of thinking that isn’t our own.
“It is a matter of urgency that the treatment offered by adult services is reviewed and that safeguards are put in place.”
184 notes
·
View notes
Text

Article is here, full text attached below.
ARTICLE TEXT:
Puberty blockers, which pause the physical changes of puberty such as breast development or facial hair, will now only be available to children as part of clinical research trials.
It follows a public consultation on the issue and an interim policy, and comes after NHS England commissioned an independent review in 2020 of gender identity services for children under 18.
That review, led by Dr Hilary Cass, followed a sharp rise in referrals to the Gender Identity Development Service (Gids) run by the Tavistock and Portman NHS Foundation Trust, which is closing at the end of March.
The clinic has come under repeated scrutiny.
In February 2022, Dr Cass published an interim report saying there was a need to move away from one unit and recommended the creation of regional services to better support youngsters.
She also pointed to a lack of long-term evidence and data collection on what happens to children and young people who are prescribed medication.
She added that Gids had not collected routine and consistent data “which means it is not possible to accurately track the outcomes and pathways that children and young people take through the service.”
Following the Tavistock’s closure, two new NHS services will now open in early April, situated in London’s Great Ormond Street Hospital and Alder Hey Children’s Hospital in Liverpool.
The NHS has said children attending these clinics will be supported by clinical experts in neurodiversity, paediatrics and mental health, “resulting in a holistic approach to care”.
Former prime minister Liz Truss, who has mooted an amendment to the Health and Equalities act, that includes a ban on the prescription of body-altering hormones to children questioning their sex, both privately and on the NHS, said: “I welcome NHS England’s decision to end the routine prescription of puberty blockers to children for gender dysphoria.
"I urge the government to back my Bill on Friday which will reinforce this in law and also prevent these drugs being supplied privately.”
Health minister, Maria Caulfield, said: “We have always been clear that children’s safety and wellbeing is paramount, so we welcome this landmark decision by the NHS.
“Ending the routine prescription of puberty blockers will help ensure that care is based on evidence, expert clinical opinion and is in the best interests of the child.”
The consultation on the future of services received more than 4,000 responses, including around a quarter from members of the public, 22% from patients, 21% from parents, 10% from trans adults and 5% from clinicians.
John Stewart, national director of specialised commissioning at NHS England said: “Given that the debate is often very polarised, so too were the responses to the consultation.
“Many people said the policy didn’t go far enough in terms of still allowing potential access (to puberty blockers) through research, and others saying clearly they disagreed fundamentally and that these should be routinely available to everyone who believes they need it.”
Regarding the new clinics, he said: “This is just the first step in building a regional model, where our aim is to establish between seven and eight specialist centres including the north and the south hubs over the next year to two years.”
Around 250 patients are expected to be transferred to the new clinics from Gids when they open.
Some 5,000 more children and young people are currently on the waiting list for referral into the new clinics.
#long post#uk politics#cis children can still be prescribed puberty blockers; is is specifically prescription by gender identity clinics to trans youth being targe#targeted here.
43 notes
·
View notes
Text
Okay this ain't even my country and I know that I'm preaching to the choir but "Dr" Hilary Cass' report on how trans youth in Britain are totally fine without transitioning and hey maybe we should just ban it all entirely is one of the most glaring examples of bad faith science I've seen and I want to dress down exactly why it's horseshit.
She did not conduct any research herself. She has never so much as interacted with a trans youth. What she did was cherrypick a bunch of publications, say that they "weren't conducted properly", and then read that as a "lack of evidence" for the benefits of transitioning. (Note: All of the studies she looked at were UK. Ergo every other country that has found that transitioning helps people can get fucked I guess because the laws of science only apply to Britain.) There were plenty of publications that did pass her narrow view for scientific rigor, and she deliberately left them all out. She can't even say they were wrong, she just says "they weren't good enough" and takes that as "proof" there was no real evidence to begin with.
If she was a scientist and not a TERF with a political agenda, she would be asking for these studies to be redone with her new standard. But she's not. She just wants all trans science to stop before it shows her something she doesn't want to hear, and for all trans youth to kill themselves quietly so she can say they were "just" suicidal and there was nothing that transitioning could have done for them. And the fact that the government and even other scientists are supporting her in this endeavor makes me sick.
28 notes
·
View notes
Text

Following publication of the final report there have been a number of questions and points for clarification about the findings and recommendations. We have collated those questions, along with our answers, on this page.
-
Did the Review set a higher bar for evidence than would normally be expected?
No, the approach to the assessment of study quality was the same as would be applied to other areas of clinical practice – the bar was not set higher for this Review.
Clarification:
The same level of rigour should be expected when looking at the best treatment approaches for this population as for any other population so as not to perpetuate the disadvantaged position this group have been placed in when looking for information on treatment options.
The systematic reviews undertaken by the University of York as part of the Review’s independent research programme are the largest and most comprehensive to date. They looked at 237 papers from 18 countries, providing information on a total of 113,269 children and adolescents.
All of the University of York’s systematic review research papers were subject to peer review, a cornerstone of academic rigour and integrity to ensure that the methods, findings, and interpretation of the findings met the highest standards of quality, validity and impartiality.
-
Did the Review reject studies that were not double blind randomised control trials in its systematic review of evidence for puberty blockers and masculinising / feminising hormones?
No. There were no randomised control studies identified in the systematic reviews, but other types of studies were included if they were well designed and conducted.
Clarification:
The Review commissioned the University of York to undertake an independent research programme to ensure the work of the Review and its recommendations were informed by the most robust existing evidence. This included a series of systematic reviews which brought together, analysed and evaluated existing evidence on a range of issues relating to the care of gender-questioning children and young people, including epidemiology, treatment approaches and international models of current practice.
Randomised control trials are considered the gold standard in relation to research, but there are many other study designs that can give valuable information. Explanatory Box 1 (pages 49-51 of the final report) discusses in more detail the different kinds of studies that can be used, and how to decide if a study is poorly designed or biased.
Blinding is a separate issue. It means that either the patient or the researcher does not know if the patient is getting an active treatment or a ‘control’ (which might be another treatment or a placebo). Patients cannot be blinded as to whether or not they are receiving puberty blockers or masculinising / feminising hormones, because the effects would rapidly become obvious. Good RCTs can be conducted without blinding.
The University of York’s systematic review search did not identify any RCTs, blinded or otherwise, but many other studies were included. Most of the studies included were called ‘cohort studies’. Well-designed and executed high quality cohort studies are used in other areas of medicine, and the bar was not set higher for this review; even so the quality of the studies was mostly only assessed as moderate.
-
Did the Review reject 98% of papers demonstrating the benefits of affirmative care?
No. Studies were identified for inclusion in the synthesis (conclusions) of the systematic reviews on puberty blockers and masculinising/feminising hormones on the basis of their quality. This was assessed using a standard quality assessment tool appropriate to the types of study identified. All high quality and moderate quality reviews were included in the synthesis of results. This totalled 58% of the 103 papers.
Clarification:
The Newcastle-Ottawa scale (a standard appraisal tool) was used to compare the studies. This scores items such as participant selection, comparability of groups (how alike they are), the outcomes of the studies and how these were assessed (data provided and whether it is representative of those studied). High quality studies (scoring >75%) would score well on most of these items; moderate quality studies (scoring >50% – 75%) would miss some elements (which could affect outcomes); and low-quality studies would score 50% or less on the items the scale looked at. A major weakness of the studies was that they did not have adequate follow-up – in many cases they did not follow young people for long enough for the long-term outcomes to be understood.
Because the ranking was based on how the studies were undertaken (their quality and execution), low quality research was removed before the results were analysed as the findings could not be completely trusted. Had an RCT been available it would also have been excluded from the systematic review if it was deemed to be of poor quality.
The puberty blocker systematic review included 50 studies. One was high quality, 25 were moderate quality and 24 were low quality. The systematic review of masculinising/feminising hormones included 53 studies. One was high quality, 33 were moderate quality and 19 were low quality.
All high quality and moderate quality reviews were included, however as only two of the studies across these two systematic reviews were identified as being of high quality, this has been misinterpreted by some to mean that only two studies were considered and the rest were discarded. In reality, conclusions were based on the high quality and moderate quality studies (i.e. 58% of the total studies based on the quality assessment). More information about this process in included in Box 2 (pages 54-56 of the final report)
-
Has the Review recommended that no one should transition before the age of 25 and that Gillick competence should be overturned.
No. The Review has not commented on the use of masculinising/feminising hormones on people over the age of 18. This is outside of the scope of the Review. The Review has not stated that Gillick competence should be overturned.
The Review has recommended that:
“NHS England should ensure that each Regional Centre has a follow through service for 17-25-year-olds; either by extending the range of the regional children and young people’s service or through linked services, to ensure continuity of care and support at a potentially vulnerable stage in their journey. This will also allow clinical, and research follow-up data to be collected.”
This recommendation only relates to people referred into the children and young people’s service before the age of 17 to enable their care to be continued within the follow-through service up to the age of 25.
Clarification:
Currently, young people are discharged from the young people’s service at the age of 17, often to an adult gender clinic. Some of these young people have been receiving direct care from the NHS gender service (GIDS as was) and others have not yet reached the top of the waiting list and have “aged out” of the young people’s service before being seen.
The Review understands that this is a particularly vulnerable time for young people. A follow-through service continuing up to age 25, would remove the need for transition (that is, transfer) to adult services and support continuity of care and continued access to a broader multi-disciplinary team. This would be consistent with other service areas supporting young people that are selectively moving to a ‘0-25 years’ service to improve continuity of care.
The follow-through service would also benefit those seeking support from adult gender services, as these young people would not be added to the waiting list for adult services and, in the longer-term, as more gender services are established, capacity of adult provision across the country would be increased.
People aged 18 and over, who had not been referred to the NHS children and young people’s gender service, would still be referred directly to adult clinics.
-
Is the Review recommending that puberty blockers should be banned?
No. Puberty blocker medications are used to address a number of different conditions. The Review has considered the evidence in relation to safety and efficacy (clinical benefit) of the medications for use in young people with gender incongruence/gender dysphoria.
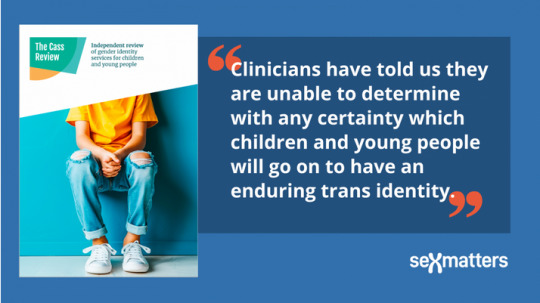
The Review found that not enough is known about the longer-term impacts of puberty blockers for children and young people with gender incongruence to know whether they are safe or not, nor which children might benefit from their use.
Ahead of publication of the final report NHS England took the decision to stop the routine use of puberty blockers for gender incongruence / gender dysphoria in children. NHS England and National Institute for Health and Care Research (NIHR) are establishing a clinical trial to ensure the effects of puberty blockers can be safely monitored. Within this trial, puberty blockers will be available for children with gender incongruence/ dysphoria where there is clinical agreement that the individual may benefit from taking them.
Clarification:
Puberty blockers have been used to suppress puberty in children and young people who start puberty much too early (precocious puberty). They have undergone extensive testing for use in precocious puberty (a very different indication from use in gender dysphoria) and have met strict safety requirements to be approved for this condition. This is because the puberty blockers are suppressing hormone levels that are abnormally high for the age of the child.
This is different to stopping the normal surge of hormones that occur in puberty. Pubertal hormones are needed for psychological, psychosexual and brain development, and there is not yet enough information on the risks of stopping the influence of pubertal hormones at this critical life stage.
When deciding if certain treatments should be routinely available through the NHS it is not enough to demonstrate that a medication doesn’t cause harm, it needs to be demonstrated that it will deliver clinical benefit in a defined group of patients.
Over the past few years, the most common age that young people have been receiving puberty blockers in England has been 15 when most young people are already well advanced in their puberty. The new services will be looking at the best approaches to support young people through this period when they are still making decisions about longer-term options.
-
Has the Review recommended that social transition should only be undertaken under medical guidance?
The Review has advised that a more cautious approach around social transition needs to be taken for pre-pubertal children than for adolescents and has recommended that:
“When families/carers are making decisions about social transition of pre-pubertal children, services should ensure that they can be seen as early as possible by a clinical professional with relevant experience.”
Parents are encouraged to seek clinical help and advice in deciding how to support a child with gender incongruence and should be prioritised on the waiting list for early consultation on this issue. This should include discussion of the risks and benefits and the voice of the child should be heard. It will be important that flexibility is maintained, and options remain open.
Clarification:
Although the University of York’s systematic review found that there is no clear evidence that social transition in childhood has positive or negative mental health outcomes, there are studies demonstrating that for a majority of young children presenting with gender incongruence, this resolves through puberty. There is also evidence from studies of young people with differences of sex development (DSD) that sex of rearing seems to have some influence on eventual gender outcome, and it is possible that social transition in childhood may change the trajectory of gender identity development for children with early gender incongruence. Living in stealth from early childhood may also lead to stress, particularly as puberty approaches.
There is relatively weak evidence for any effect of social transition in adolescence. The Review recognises that for adolescents, exploration is a normal process, and rigid binary gender stereotypes can be unhelpful. Many adolescents will go through a period of gender non-conformity in terms of outward expressions (e.g. hairstyle, make-up, clothing and behaviours). They also have greater agency in how they present themselves and in their decision-making.
Young people and young adults have spoken positively about how social transition helped to reduce their gender dysphoria and feel more comfortable in themselves. They identified that space to talk about socially transitioning and how to handle conversations with parents/carers and others would be helpful. The Review has therefore advised that it is important to try and ensure that those already actively involved in the young person’s welfare provide support in decision making and that plans are in place to ensure that the young person is protected from bullying and has a trusted source of support.
Further detail can be found in Chapter 12 of the Final Report.
-
Did the Review speak to any gender-questioning and trans people when developing its recommendations?
Yes, the Review has been underpinned by an extensive programme of proactive engagement, which is described in Chapter 1 of the report. The Review has met with over 1000 individuals and organisations across the breadth of opinion on this subject but prioritised two categories of stakeholders:
People with relevant lived experience (direct or as a parent/carer) and organisations working with LGBTQ+ children and young people generally.
Clinicians and other relevant professionals with experience of and/ or responsibility for providing care and support to children and young people within specialist gender services and beyond.
A mixed-methods approach was taken, which included weekly listening sessions with people with lived experience, 6-weekly meetings with support and advocacy groups throughout the course of the Review, and focus groups with young people and young adults.
Reports from the focus groups with young people with lived experience are published on the Review’s website and the learning from these sessions and the listening sessions are represented in the final report.
The Review also commissioned qualitative research from the University of York, who conducted interviews with young people, young adults, parents and clinicians. A summary of the findings from this research is included as appendix 3 of the final report.
-
What is the Review’s position on conversion therapy?
Whilst the Review’s terms of reference do not include consideration of the proposed legislation to ban conversion practices, it believes that no LGBTQ+ group should be subjected to conversion practice. It also maintains the position that children and young people with gender dysphoria may have a range of complex psychosocial challenges and/or mental health problems impacting on their gender-related distress. Exploration of these issues is essential to provide diagnosis, clinical support and appropriate intervention.
The intent of psychological intervention is not to change the person’s perception of who they are but to work with them to explore their concerns and experiences and help alleviate their distress, regardless of whether they pursue a medical pathway or not. It is harmful to equate this approach to conversion therapy as it may prevent young people from getting the emotional support they deserve and make clinicians fearful of providing this group of children and young people the same care as is afforded to other children and young people.
No formal science-based training in psychotherapy, psychology or psychiatry teaches or advocates conversion therapy. If an individual were to carry out such practices they would be acting outside of professional guidance, and this would be a matter for the relevant regulator.
==
Like any religious fanatics, pathological liars like "Erin" Reed and "Alejandra" Carballo still won't stop lying, since it's all they have. But their disciples should really be noticing how they've been directly refuted.
#Cass review#Cass report#Hilary Cass#Dr. Hilary Cass#disinformation#misinformation#pathological liars#Erin Reed#Alejandra Carabello#Michael Hobbes#medical scandal#medical corruption#medical malpractice#gender affirming care#gender affirming healthcare#gender affirmation#compulsive liars#gender fanatics#gender cult#gender ideology#gender identity ideology#queer theory#intersectional feminism#puberty blockers#cross sex hormones#wrong sex hormones#religion is a mental illness
39 notes
·
View notes
Text
“There is no centralized tracking of blocker prescriptions in the United States.”
By Megan Twohey and Christina Jewett
Nov. 14, 2022
The medical guidance was direct.
Eleven-year-old Emma Basques had identified as a girl since toddlerhood. Now, as she worried about male puberty starting, a Phoenix pediatrician advised: Take a drug to stop it.
At 13, Jacy Chavira felt increasingly uncomfortable with her maturing body and was beginning to believe she was a boy. Use the drug, her endocrinologist in Southern California recommended, and puberty would be suspended.
An 11-year-old in New York with deepening depression expressed a desire to no longer be a girl. A therapist told the family the drug was the preteen’s best option, and a local doctor agreed.
“‘Puberty blockers really help kids like this,’” the child’s mother recalled the therapist saying. “It was presented as a tourniquet that would stop the hemorrhaging.”
As the number of adolescents who identify as transgender grows, drugs known as puberty blockers have become the first line of intervention for the youngest ones seeking medical treatment.
Their use is typically framed as a safe — and reversible — way to buy time to weigh a medical transition and avoid the anguish of growing into a body that feels wrong. Transgender adolescents suffer from disproportionately high rates of depression and other mental health issues. Studies show that the drugs have eased some patients’ gender dysphoria — a distress over the mismatch of their birth sex and gender identity.
“Anxiety drains away,” said Dr. Norman Spack, who pioneered the use of puberty blockers for trans youth in the United States and is one of many physicians who believe the drugs can be lifesaving. “You can see these kids being so relieved.”
But as an increasing number of adolescents identify as transgender — in the United States, an estimated 300,000 ages 13 to 17 and an untold number who are younger — concerns are growing among some medical professionals about the consequences of the drugs, a New York Times examination found. The questions are fueling government reviews in Europe, prompting a push for more research and leading some prominent specialists to reconsider at what age to prescribe them and for how long. A small number of doctors won’t recommend them at all.
Dutch doctors first offered puberty blockers to transgender adolescents three decades ago, typically following up with hormone treatment to help patients transition. Since then, the practice has spread to other countries, with varying protocols, little documentation of outcomes and no government approval of the drugs for that use, including by the U.S. Food and Drug Administration.
But there is emerging evidence of potential harm from using blockers, according to reviews of scientific papers and interviews with more than 50 doctors and academic experts around the world.






The drugs suppress estrogen and testosterone, hormones that help develop the reproductive system but also affect the bones, the brain and other parts of the body.
During puberty, bone mass typically surges, determining a lifetime of bone health. When adolescents are using blockers, bone density growth flatlines, on average, according to an analysis commissioned by The Times of observational studies examining the effects.
Many doctors treating trans patients believe they will recover that loss when they go off blockers. But two studies from the analysis that tracked trans patients’ bone strength while using blockers and through the first years of sex hormone treatment found that many do not fully rebound and lag behind their peers.
That could lead to heightened risk of debilitating fractures earlier than would be expected from normal aging — in their 50s instead of 60s — and more immediate harm for patients who start treatment with already weak bones, experts say.
“There’s going to be a price,” said Dr. Sundeep Khosla, who leads a bone research lab at the Mayo Clinic. “And the price is probably going to be some deficit in skeletal mass.”
Many physicians in the United States and elsewhere are prescribing blockers to patients at the first stage of puberty — as early as age 8 — and allowing them to progress to sex hormones as soon as 12 or 13. Starting treatment at young ages, they believe, helps patients become better aligned physically with their gender identity and helps protect their bones.
But that could force life-altering choices, other doctors warn, before patients know who they really are. Puberty can help clarify gender, the doctors say — for some adolescents reinforcing their sex at birth, and for others confirming that they are transgender.
“The most difficult question is whether puberty blockers do indeed provide valuable time for children and young people to consider their options, or whether they effectively ‘lock in’ children and young people to a treatment pathway,” wrote Dr. Hilary Cass, a pediatrician leading an independent review in England of medical treatments of adolescents presenting as transgender.

On her recommendation, England’s National Health Service last month proposed restricting use of the drugs for trans youths to research settings. Sweden and Finland have also placed limits on the treatment, concerned not just with the risk of blockers, but the steep rise in young patients, the psychiatric issues that many exhibit, and the extent to which their mental health should be assessed before treatment.
In the United States, though, there is no universal policy, and the public discussion is polarized.
Republican governors and lawmakers in more than a dozen states are working to limit or even criminalize the treatments, as some in their party also seek to restrict access to sports and bathrooms, ban discussion of gender in public schools, and call into question whether transgender identity even exists. (This month, the Florida medical board banned medications and surgeries for new patients under 18.) Meanwhile, the Biden administration describes transgender medicine as a civil right. And some advocates criticize anyone who questions the treatments’ safety.
Long-awaited research funded by the National Institutes of Health could provide more guidance. In 2015, four prominent American gender clinics were awarded $7 million to examine the effects of blockers and hormone treatment on transgender youth. In explaining their study, the researchers pointed out that the United States had produced no data on the impact or safety of blockers, particularly among transgender patients under 12, leaving a “gap in evidence for this practice.” Seven years in, they have yet to report key outcomes of their work, but say the findings are coming soon.
Many young patients and their families have concluded that the benefits of easing the despair of gender dysphoria far outweigh the risks of taking blockers. For others, the limited studies and politicization of trans medicine can make it difficult to fully evaluate the decision. A Reuters examination of a range of transgender treatments also found scant research into the long-term effects.
Three years after starting the drugs, Emma Basques believes she’s on the right path.
Jacy Chavira, now 22, decided that the medical treatment was not appropriate for her and resumed her female identity.
And the New York adolescent had such a significant loss in bone density after more than two years on blockers that the parents halted use of the drugs.
“We went into this because we wanted to help,” the mother said. “Now I worry that we got into a situation with a very powerful drug and don’t understand what the long-term effects will be.”
‘Time to Start’
It didn’t take long for Cherise and Arick Basques to realize that their toddler was different. The child rejected pants, toy trucks and sports in favor of dresses, Barbie dolls and ballet. When Ms. Basques ran into a friend at a restaurant in their Phoenix suburb and introduced her then-4-year-old as her son, the child shouted: “No! I’m your daughter!”
The couple worked with children — Ms. Basques as an occupational therapist, her husband as a teacher and school administrator — but this was unfamiliar territory. None of the therapists the parents called felt equipped to help. Their pediatrician offered only that things could change once the child started school, Ms. Basques said. Eventually, the couple discovered a local support group for parents of transgender children.
The next year, they allowed the child, then 5, to begin using the name Emma, grow longer hair and take other steps to socially transition. In 2019, when Emma turned 11, a physician at a local gender clinic advised starting blockers.
“At the first subtle signs of puberty, it was like: ‘Yep, that’s it. Time to start!’” recalled Ms. Basques. Along with her husband and Emma, she asked that their full names be used because they consider themselves advocates of the treatment.
For decades, transgender medical treatment in multiple countrieswas restricted to patients 18 and older. But in the 1990s, a hospital clinic in Amsterdam began treating adolescents.
Puberty blockers can be given as an injection or an implant. (The best known is Lupron, made by AbbVie.) They were being used in the United States and elsewhere, with approval by the F.D.A. and its counterparts overseas, to treat prostate cancer; endometriosis, a painful disease that causes uterine tissue to grow elsewhere in the body; and the unusually early onset of puberty, typically age 6 or 7. If blockers were safe for patients with that rare condition, known as central precocious puberty, the Dutch doctors reasoned, they were likely to be safe for trans adolescents too.
The first trans patient treated with blockers, from age 13 to 18, moved on to testosterone, the male sex hormone. Halting female puberty had offered emotional relief and helped him look more masculine. As the Dutch clinicians prescribed blockers, followed by hormones, to a half-dozen other patients in those early years, the medical team found that their mental health and well-being improved.
“They were usually coming in very miserable, feeling like an outsider in school, depressed or anxious,” recalled Dr. Peggy Cohen-Kettenis, a retired psychologist at the clinic. “And then you start to do this treatment, and a few years later, you see them blossoming.”
In 1998, she worked with a small international group — which would later expand and become known as the World Professional Association for Transgender Health, or WPATH — to include puberty blockers and hormones for adolescents in their treatment guidelines.
The Dutch doctors had yet to publish any research findings, she acknowledged. Some other physicians, including the one overseeing transgender medical treatment in England, were wary of potential harm.
But doctors in the group considered the early results from Amsterdam as reassuring enough to move forward. They were eager to treat the psychological distress observed in many trans adolescents.
Doctors debated about whether “starting the puberty blockers would somehow damage the children,” recalled Dr. Walter Meyer, a Texas pediatric endocrinologist and psychiatrist involved with the 1998 standards of care.
“The Dutch were saying, ‘Oh, no, it’s not causing a problem,’” said Dr. Meyer, who continues to support the use of the drugs.
Dr. Cohen-Kettenis hoped physicians in other countries would adopt the Dutch protocol, and document and share the outcomes as she and her colleagues in Amsterdam planned. Her clinic treated only patients who had consistently presented as transgender since early childhood and did not suffer from distinct psychiatric disorders that could interfere with diagnosis or treatment. They had to be at least 12 for puberty blockers, with the option of moving on to hormones at 16.
The international standards of care advised similar criteria. But they were recommendations, not requirements. Soon, the use of puberty blockers spread. In the United States and Canada, countries without centralized health systems, protocols were largely left to the discretion of individual clinics and practitioners. Dr. Spack, the pediatric endocrinologist who led U.S. adoption of the treatment, opened the first American clinic in 2007 at Boston Children’s Hospital; others eventually followed in nearly every state.
Some started children on blockers at the first signs of puberty and prescribed testosterone or estrogen to patients 14 or younger. Doctors believed that earlier treatment would lead to more successful medical transitions, and wanted to spare patients the difficulty of watching their peers develop while their own bodies remained unchanged.
The doctor in Arizona who treated Emma, for example, tells preteen patients that if he prescribed blockers and didn’t start hormones for five years, they would look 12 at age 16.

Transgender activists across the country pushed for early and easy access to the treatment. At a 2006 Philadelphia medical convention, Jenn Burleton, an advocate from Oregon, heard Dr. Spack describe his experience starting to treat adolescents with blockers. Like others of her generation, Ms. Burleton, now 68, could not medically transition until adulthood, and puberty had been traumatic. Treating adolescents with blockers was “game-changing,” said Ms. Burleton, founder and program director of the organization now known as the TransActive Gender Project at the Lewis & Clark Graduate School for Education and Counseling.
Back home, Ms. Burleton prodded pediatric endocrinologists to adopt the practice for their patients. “We have a chance to prevent them from being emotionally broken,” she recalled saying.
Advocates successfully pushed Oregon, Massachusetts, California and other states to allow for Medicaid coverage of puberty blockers for adolescents identifying as trans. They also helped win approval in Oregon for a variety of medical workers — doctors, nurse practitioners, naturopaths — to administer blockers if overseen, even long-distance, by an endocrinologist.
“It went so quickly that not even centers but individual clinicians, people who were not knowledgeable, were just giving this kind of treatment,” said Dr. Cohen-Kettenis, the Dutch psychologist. “There was a great concern.”
By the time Emma Basques began taking blockers in 2019, multiplemedical groups had endorsed their use for gender dysphoria. Among them were the American Academy of Pediatrics and the international Endocrine Society, which in 2017 had described the limited research on the effects of the drugs on trans youth as “low-quality.” Still, the organizations were encouraged by what they saw as a promising treatment.
Many doctors point out that it’s not unusual for research to lag behind the launch of new treatments and for drugs to be used off-label on patients without F.D.A. approval, especially in pediatric medicine.

An F.D.A. spokeswoman said in a statement that doctors have the discretion to do so, but also noted that just because a drug has been approved for one class of patients doesn’t mean it’s safe for another.
There is no centralized tracking of blocker prescriptions in the United States. Komodo Health, a health technology company, compiled private and public insurance data for Reuters, showing a sharp increase in the number of children ages 6 to 17 diagnosed with gender dysphoria, from about 15,000 in 2017 to about 42,000 in 2021. During that time, 4,780 patients with that diagnosis were put on puberty blockers covered by insurance, the data shows, with new prescriptions growing each year. But the data does not capture the many cases in which insurance does not cover the drugs for that use, leaving families to pay out of pocket.
Some leading American practitioners asked AbbVie and Endo Pharmaceuticals, maker of another blocker, to seek F.D.A. approval for the drugs’ use among trans adolescents. The drugmakers would have to fund research for a patient population that made up just a small part of their market. But the physicians argued that regulatory approval could help establish the safety of the treatment and broaden insurance coverage of the drugs, which can cost tens of thousands of dollars a year. In the end, AbbVie and Endo said no. The companies declined to comment on the decision.
Emma Basques was on blockers for two years. Then, after she turned 13 in October of last year, a doctor in the Portland, Ore., suburb where her family had moved, prescribed estrogen, starting her transition. It had become increasingly awkward to feel left behind as her classmates physically matured. And she felt confident that she was ready.
“It was just really exciting,” Emma said. “I finally got to be who I was.”

‘We Need to Give This a Chance’
The 11-year-old in New York, who had begun puberty and started at a new school, was increasingly distressed — refusing to bathe or go to class and, for the first time, expressing a desire to no longer have a girl’s body.
When the parents consented to blockers in 2018, they hoped the drug would bring emotional stability and time to consider next steps.
“If everyone thinks this will help, and it’s reversible, then we need to give this a chance,” said the mother, who asked that her name be withheld to protect the family’s privacy.
‘We Need to Give This a Chance’
The 11-year-old in New York, who had begun puberty and started at a new school, was increasingly distressed — refusing to bathe or go to class and, for the first time, expressing a desire to no longer have a girl’s body.
When the parents consented to blockers in 2018, they hoped the drug would bring emotional stability and time to consider next steps.
“If everyone thinks this will help, and it’s reversible, then we need to give this a chance,” said the mother, who asked that her name be withheld to protect the family’s privacy.

A full accounting of blockers’ risk to bones is not possible. While the Endocrine Society recommends baseline bone scans and then repeat scans every one to two years for trans youths, WPATH and the American Academy of Pediatrics provide little guidance about whether to do so. Some doctors require regular scans and recommend calcium and exercise to help to protect bones; others do not. Because most treatment is provided outside of research studies, there’s little public documentation of outcomes.
But it’s increasingly clear that the drugs are associated with deficits in bone development. During the teen years, bone density typically surges by about 8 to 12 percent a year. The analysis commissioned by The Times examined seven studies from the Netherlands, Canada and England involving about 500 transgender teens from 1998 through 2021. Researchers observed that while on blockers, the teens did not gain any bone density, on average — and lost significant ground compared to their peers, according to the analysis by Farid Foroutan, an expert on health research methods at McMaster University in Canada.
The findings match what practitioners of the treatment have seen, including Dr. Catherine Gordon, a pediatric endocrinologist and bone researcher at Baylor College of Medicine in Houston. “When they lose bone density, they’re really getting behind,” said Dr. Gordon, who is leading a separate study on why the drugs have such an effect.
Many doctors caring for young trans patients are reassured by the rebounds seen in the children who take blockers for unusually early puberty. In most cases, their bone strength fully recovers after they stop the drugs at about age 11 and resume full puberty, which can last up to five years. But patients identifying as trans take the drugs later, interrupting their normally timed puberty and limiting that crucial period of development.
“That’s the difference,” Dr. Gordon said. “You shorten that critical window of puberty.”
So far, only two small studies, published by Dutch doctors, have tracked the bone development of trans patients from beginning blockers through early hormone treatment. In both studies, dozens of patients started blockers at 14 or 15, on average, and began estrogen or testosterone at 16. The participants, followed in one study through age 18, and in the other through age 22, saw their bones strengthen, on average, once on hormones. Still, most patients continued to lag behind their peers; trans men neared average levels, but trans women fell far below.
“I think there’s a false sense of security,” said Dr. Khosla, the Mayo Clinic specialist, who is skeptical that all trans patients can catch up.
Dr. Khosla and Dr. Gordon don’t believe the effects on bones are reason for medical providers to halt use of the drugs in adolescents. But they think the risks should be factored into patient decisions and that bones should be carefully monitored.
If any harm resulted from the use of blockers, it likely would not be evident until decades later, with fractures. However, for children who already have weak bones as they start treatment, the dangers could be more immediate. While there is no systematic record-keeping of such cases, some anecdotal evidence is available.
After more than a year on blockers, a 15-year-old in Texas, who had not had a baseline scan, showed spinal bone density so low that it was below the first percentile for the teen’s age and weight, indicating osteoporosis, according to medical records from earlier this year.
A transgender adolescent in Sweden who took the drugs from age 11 to 14 with no bone scans until the last year of treatment developed osteoporosis and sustained a compression fracture in his spine, an X-ray showed in 2021, as reported earlier in a documentary on Swedish television.
“The patient now suffers from continued back pain,” medical records note, describing a “permanent disability” caused by the blockers.
Some practitioners in the United States and Australia do not provide the drugs to patients who are well into puberty, concerned that the treatment poses the greatest threat to bones in that period.
“You’re potentially taking on risks that I felt should be avoided,” said Dr. Stephen Rosenthal, medical director of the University of California, San Francisco, Child and Adolescent Gender Center.
He won’t prescribe blockers as a stand-alone treatment to anyone over 14. That includes the growing number of nonbinary youths who don’t want to mature into either male or female bodies. “We make it very clear that no one stays on a blocker,” he said.
Dr. Rosenthal is a principal investigator in the yearslong N.I.H. study, which also involves gender clinics in Los Angeles, Chicago and Boston. Asked why they have yet to report on key outcomes, he said their research was delayed when the pandemic halted in-person treatment. Papers on the effects of blockers on bones and other findings should be published next year, he said.
Like many physicians, Dr. Rosenthal believes the benefits of using blockers to alleviate gender dysphoria are much greater than any risks to bones. (He was among the doctors who filed statements in a lawsuit against an Alabama ban on medical treatment of trans youth.)
Emma Basques, for example, takes calcium, makes an effort to exercise and has undergone scans that showed her bones are healthy. “I can’t even imagine how life would be for Emma,” said her mother, Ms. Basques, “if she was not given blockers and had to go through male puberty.”
Emma added: “I wouldn’t like my body at all.”
But the parents in New York insisted on ending treatment for their teen, who has yet to have a follow-up scan to see if bone density has improved since going off blockers.
“I don’t think we have the science behind them to be prescribing these drugs,” the mother said.
‘I Wish There Had Been More Questions’
Jacy Chavira, in Southern California, had already cut her hair short and begun binding her chest when she was prescribed blockers at age 13. A therapist and her parents agreed that gender dysphoria, a condition Jacy learned about from a magazine, could explain the mounting anxiety and discomfort that she was experiencing during early puberty.
Once on blockers, Ms. Chavira said, she became fixated on moving ahead with a medical transition. She was thrilled shortly after turning 16 when her pediatric endocrinologist prescribed testosterone. But soon she started having doubts. Her body was growing more masculine, but she was secretly putting on dresses. At 17, in a consultation for breast removal, she worried aloud about the potential loss of feeling in the nipples. To her, this was a sign of not wanting to go through with the surgery.
She came to realize that her anguish had stemmed from a larger inner conflict, and that continuing with a gender transition would be a mistake. “I believe it was an issue with my identity, accepting who I was, and not just the physical female portion of it,” she said.
Like Ms. Chavira, most patients who take puberty blockers move on to hormones to transition, as many as 98 percent in British and Dutch studies. While many doctors see that as evidence that the right adolescents are getting the drugs, others worry that some young people are being swept into medical interventions too soon.
Over the past decade, growing numbers of medical providers have lowered the ages at which they prescribe the treatments. Today, the WPATH and Endocrine Society advise that blockers can be prescribed at the first signs of puberty and hormone treatment, in some cases, earlier than 16. The American Academy of Pediatrics says blockers can be provided anytime during puberty and hormones from “early adolescence onward.”
Some doctors and researchers are concerned that puberty blockers may somehow disrupt a formative period of mental growth. With adolescence comes critical thinking, more sophisticated self-reflection and other significant leaps in brain development. Sex hormones have been shown to affect social and problem-solving skills. It’s believed that brain growth is connected to gender identity, but research in these areas is still very new.
In a 2020 paper, 31 psychologists, neuroscientists and hormone experts from around the world urged more study of the effects of blockers on the brain.
“If the brain is expecting to receive those hormones at a certain time and doesn’t, what happens?” said Dr. Sheri Berenbaum, head of a gender research lab at Penn State, and one of the authors of the paper. “We don’t know.”
The physicians in the Amsterdam clinic, where the treatment began, have lowered their minimum ages for starting blockers and hormones. But they are very cautious in selecting patients.
“Our concern is always: When is gender identity fixed or not fluid anymore? And when do you fully understand the lifelong consequences of such treatment?” said Dr. Annelou de Vries, head therapist at the clinic.
For some medical professionals across the country, there are too many uncertainties about the effects of blockers to provide the treatment.
Among them are seven pediatric endocrinologists and pediatric endocrine nurse practitioners in Florida who recently wrote to the state health department that evidence to support the use of those treatments in adolescents “is simply lacking” and asking that it be confined to research settings.
“Without much data, it’s hard to make a conclusion that we’re doing the right thing,” said Dr. Matthew Benson, an assistant professor of pediatrics at Mayo Clinic College of Medicine in Jacksonville and an author of the letter. (He also voiced concerns at a state hearing in July on whether to stop allowing Medicaid coverage in Florida for transgender medical treatment.)
Even enthusiasts, like Emma and her parents, acknowledge it can be hard to fully grasp all the potential results of treatment. Infertility is among other lasting effects for patients who start blockers at the first stage of puberty and proceed to hormones and surgery. Emma was advised that, to possibly preserve fertility, she would need to pause treatment at some point down the line, with the hopes of developing and freezing sperm.
“I knew what I wanted,” Emma said of her medical transition. “But all this other stuff was kind of just confusing.” Her father said, “We worked really hard to talk to her at her age level to make sure she understood some of these more complicated things.”
When Dutch doctors launched the use of blockers and hormones on trans youth decades ago, they warned in their early papers of the possibility of “false positives” — patients who medically transition, then later declare they are not transgender.
There’s no official tracking of those cases and many practitioners believe the total numbers are small. So far, scores of accounts have emerged in social media, news stories and published research.
Keira Bell, who was prescribed blockers at age 16, then moved on to testosterone and breast-removal surgery, no longer identified as transgender five years after starting to transition. She sued the Tavistock gender clinic in London where she had been treated. (A judge ruled that patients under 16 were unable to consent to puberty blockers — a decision later overturned on appeal.)
Jacy Chavira, looking back on her own experience, thinks that drugs were prescribed too quickly. At 18, she halted her medical treatment and resumed her female identity. Now, she is left with a voice that sounds like a man’s and other enduring physical changes.
“I wish there had been more questions asked by the doctors,” she said. “I wish I hadn’t been steered into transitioning the way I was, and that I had been told there were other ways to cope with the discomfort of puberty.”
Alarmed by the uncertain number of cases like Jacy’s, as well as the rising numbers of patients with gender dysphoria and the psychiatric disorders many display, Sweden is working to standardize adolescent transgender medical treatment and restrict it to research settings.
Finland is also limiting treatment, more closely following the Dutch protocol, and doctors there remain concerned about the physical effects of blockers, including on brain development, said Dr. Riittakerttu Kaltiala, chief of adolescent psychiatry at a gender clinic in Tampere. (Dr. Kaltiala testified this fall before the Florida medical board as it was considering its ban on treatment.)
As European countries continue to examine and tailor their treatment, in the United States the public discourse about transgender care is growing more incendiary.
Last month, the American Academy of Pediatrics and other medical groups wrote to Attorney General Merrick B. Garland, urging the Justice Department to investigate growing threats of violence against physicians and hospitals that provide transgender medical treatment to adolescents. As more Republicans frame the treatment as child abuse, some doctors have become wary of discussing their work for fear of becoming targets.
More than a dozen doctors declined to be interviewed for this article, and several who spoke to The Times — some who support treatment, others who question it — asked not to be named.
The climate could have a chilling effect on research, said Dr. Natalie Nokoff, assistant professor of pediatric endocrinology at the University of Colorado, who recently conducted a soon-to-be-published study showing that a longer treatment period on puberty blockers was associated with a lower bone density.
“It’s leading to concerns that people’s well-intentioned scientific research could be misconstrued” and exploited for political gain, she said.
The prospect of such an outcome is disheartening for the families of Emma Basques, Ms. Chavira and the teen in New York. Despite their differing experiences, they share the same hopes for transgender medicine: less vitriol, more science.
Methodology
The analysis commissioned by The Times examined the findings of seven observational studies from the Netherlands, England and Canada, documenting the association between puberty blockers and bone density in about 500 adolescents.
In each study, bone density was measured at the spine and the hip using Dual-energy X-ray absorptiometry, or DEXA scan. The analysis looked at group means, because not every study released individual person data. Each study’s findings were weighted based on its number of participants.
The change in bone density while adolescents were on blockers was observed to be zero. The analysis also showed that the adolescents’ Z-scores, a measure of bone density that is benchmarked to peers, consistently fell during treatment with blockers.
The studies included are:
“Bone Mass in Young Adulthood Following Gonadotropin-Releasing Hormone Analog Treatment and Cross-Sex Hormone Treatment in Adolescents With Gender Dysphoria,” Klink et. al, Journal of Clinical Endocrinology & Metabolism, 2015
“Effect of Pubertal Suppression and Cross-Sex Hormone Therapy on Bone Turnover Markers and Bone Mineral Apparent Density (BMAD) in Transgender Adolescents,” Vlot et. al, Bone, 2017
“The Effect of GnRH Analogue Treatment on Bone Mineral Density in Young Adolescents With Gender Dysphoria: Findings From a Large National Cohort,” Joseph et. al, Journal of Pediatric Endocrinology and Metabolism, 2019
“Physical Changes, Laboratory Parameters and Bone Mineral Density During Testosterone Treatment in Adolescents With Gender Dysphoria,” Stoffers et. al, The Journal of Sexual Medicine, 2019
“Bone Development in Transgender Adolescents Treated With GnRH Analogues and Subsequent Gender-Affirming Hormones,” Schagen et. al, Journal of Clinical Endocrinology & Metabolism, 2020
“Short-Term Outcomes of Pubertal Suppression in a Selected Cohort of 12- to 15-Year-Old Young People With Persistent Gender Dysphoria in the U.K.,” Carmichael et. al, PLOS One, 2021
“Pubertal Suppression, Bone Mass and Body Composition in Youth With Gender Dysphoria,” Navabi et. al, Pediatrics, 2021
Julie Tate contributed research.
Megan Twohey is a prize-winning investigative reporter and a best-selling author who has focused much of her work on the treatment of women and children. @mega2e • Facebook
Christina Jewett covers the Food and Drug Administration. She is an award-winning investigative journalist and has a strong interest in how the work of the F.D.A. affects the people who use regulated products. @By_Cjewett
#Puberty blockers#Dr Norman Spack#Dr Sundeep Khosla#Dr Hilary Cass#England’s National Health Service#Dr. Peggy Cohen-Kettenis#World Professional Association for Transgender Health#or WPATH#Dr. Walter Meyer#TransActive Gender Project at the Lewis & Clark Graduate School for Education and Counseling
13 notes
·
View notes
Text
U GOT IT BAD — G. REYES


i saw this and i immediately wanted to write a little more on that scenario because it was absolutely hilarious // sorry for any mistakes

two months. you’ve been here for two months and the blackwatch commander finds himself already infuriated by you. he thought you was a simple soldier that was going to be the part of the rest of the growing overwatch society, however your skills surpasses any other person in your rank which cause you to gain the attention of strike commander morrison. now here you were, taking small teams on recall missions and as well as being present in debriefing meetings along side with other commanders. the grim commander wasn’t one to be comfortable with feelings like these and it was so hard to avoid you with your newfound popularity
what really made avoiding you harder was the fact around this time, ana was in her second trimester of her pregnancy and decided you would be the perfect fit to take over her current position. so as ana was close to gabriel, you as well was close to gabriel which left him off his game… alot
you came in during one of his drills with ana explaining what was the drill for and just having you watch him with such interest caused him to mistakenly crank up the difficulty until the training bots went haywire and basically chase his entire team in circles and up the walls. he felt the questionable looks coming from you and ana and cringed hard internally
then he had fellow agents boasting endlessly about you to him did a number. normally he’ll get real pissed hearing about some random’s personal information unwilling, yet every time he heard something about your life or things your interested in, it made him intrigued. he wanted to be the only source knowing these things about you, if he was being honest with himself
now who he didn’t want talking his ears off about you was cole…
“everyone seems to be takin’ a likin’ to that smokin’ commander already” the gunslinger kept paced with the mildly busy commander
“she’s not a commander cass, she’s just a commandant studying ana’s position before she heads off for maternity leave “ he corrected the young outlaw whilst skimming through files for an upcoming mission for his team
cole coolly shrugged his shoulders before placing his arms behind his head. “either way i feel like she’ll be good for you” he said which was followed by a teasing smirk as he watch the tips of the his brooding commander’s ears turned to a deep rue color
gabriel grew even more irritated with the young cowboys he knew his reaction would only cause more teasing from him which was making things worse, “good for me? w-what are you talking about cassidy?”
“you need a lady like that. strong, intelligent, not afraid to speak her mind…” he listed on his mechanical fingers as they walked side by side
gabe didn’t say anything else yet he agreed on everything with cassidy, however he’ll never let the gunslinger know due to his loose lips
“plus she got a nice ass in shorts” blurted cole which immediately catch gabe off guard making his instant swing on cassidy for his inappropriate comment
“whoops too slow jefe” cole snickered as he dodged the sudden attack swiftly
before gabe could stop himself from putting his full weight into his punch, it already connected with something else.. well someone else. turning his head to see what he hit instead of cassidy, he felt his stomach fall out his ass as his heart stopped
you sat on your elbows weakly as you watch your nose gush with blood while ana asked if you were okay. both the women looked towards him and he felt a deer in headlights, he couldn’t form a coherent thought which didn’t make his situation any better when his words were faster than his thoughts
“ARE YOU FUCKING SORRY?!”
ana’s face was split between confusion and anger, “come dear, let’s quickly get you to dr. ziegler” he watched as she helped you up and usher you past him as she glared daggers into him while mouthing ‘i’m going to kick your ass in 9 months’
“real smooth commande-“ this time he didn’t miss with hitting cassidy. “suicides until you drop dead, cassidy” he spat as bruised cole sat flat on his butt rubbing the back of his head
“YOU PUNCHED HER!? WHAT THE FUCK GABE!?” jack expressed, beyond shocked from the information his longtime just shared with him
“it wasn’t on purpose! stupid ass cole kept running his mouth and i didn’t know she was behind us— FUCK! what am i supposed to do now?” gabriel felt defeated. he knew he definitely blew things out the water this time and completely understood if you didn’t want to be around his presence anymore
jack stared at his friend with a sympathetic smile as he shook his head, “my friend.. i have never seen you so off guard before… you got it bad for y/n”
“i do not!” gabriel denied
“oh really? so you’re just out and about punching women who happens to make you more nervous than a virgin at prom?”
“no.. she just… so many people have such good things to say about her and actually being around her… i see why she’s a showstopper— christ sake i got into tea so i can have something to talk about with her”
jack gave him a giant smile, amused at his friend’s crush. “just apologize and be direct because the gabriel reyes i know was never the guy to be standoffish with how he’s feels” jack placed a hand on his slumped shoulder and handed a bouquet of flowers to him
“tell her how you feel man..” he encouraged
gabriel stared at the various colors amongst the bouquet, his stomach swelled up with butterflies and that’s when he knew he had to do this now or be a coward.
so striding along the empty midnight hallways of the base, he found himself in a internal battle with if he was making the right call. ‘the worst she could say is screw you, reyes’ he tried to make himself feel better about it but the twisted feeling in the out of stomach seemed never ending and only intensified once he realized he was now approaching her quarters
he stared at the name plate saying your last name. he gave himself one last prep talk before knocking and clearing his throat whilst pressing the flowers into his chest.
“y/n? a-are you up?” his voice cracked a bit as he waited for an answer. He soon heard footsteps approach the door for a moment, probably looking at the camera who was at the door. Taking a guess she figured it was him, he heard the steps start to retreat causing panic in him
he reached for the door as he was reaching for her to stop her from disappearing. “y-you don’t have to open the door, but don’t walk away… please” he pleaded quietly. his heartbeat was basically the only he could hear at this point. it was now or never to fix things even if he felt like he was unprepared for this interaction, however he took a shaky breath before laying everything out on the table.
“look y/n.. we got off on the wrong foot, but i promise you i have no ill intentions towards you. i’m just…” he struggled to finally admit to these feelings that reeked havoc over his being for the past couple of months, but he knew he had to set the record straight.
“i’m just not used to having.. i guess a crush on somebody, you can say”
“you’re all everyone talks about and just hearing about your interests— the things you like, dislike or find amusing— you’re special, interesting and dead gorgeous a-and i’m sorry for being a complete idiot towards you” he finally admitted. it felt like a pressure has finally been lifted off of his chest
there was a silence and at this point gabe was fine with just the simple confess, at least he man’d up and no one could take that from him. he sighed defeatedly, softly placed the flowers by the door as he turned on his heels to head back his side of the base to sleep off this nightmare
suddenly he heard the sound of the automatic door opening, he turned around to see you dressed in silk royal blue robe as you bend down picking up the flowers. a small smile graced your full lips as your eyes flickered from the flowers to his being and never in his life he felt so exposed before
you held the flower close to your chest as you leaned against your doorframe with hand on your hip. “it took you elbowing me in my nose to finally confess to me? you got it bad commander” you shook your head before signaling him to come back with your index finger, “care to share a glass of taylor port? i heard it was your favorite.” you raised a brow, which caused a short chuckle to leave the speechless man as he made his way back
#overwatch#overwatch gabriel reyes#gabriel reyes x black reader#overwatch x black reader#gabriel reyes x reader#x black reader#overwatch fluff#gabriel reyes fluff
22 notes
·
View notes
Text
I know you guys are probably sick of me coming up with AUs to add to the mess of them I’ve already got brewing, but I was bored this morning and my brain decided it’s Mikey’s turn to suffer!
Firefly AU
Mikey as River. Leo as Dr Simon Tam who rescues his little brother from the evil organization EPF (also gets to wear cool suits but more importantly nerds out and changes into a cool cowboy overcoat at some point!)
Raph as Captain Malcolm Reynolds. And April as his amazing badass right hand second in command Zoë Washburn. And I really wanna put Donnie as mechanic obviously but I wanna put him in Wash’s Hawaiian shirts cause that would be hilarious (instead of maybe Cass who would be our pilot).
Usagi as Jayne (but hear me out) they’re both “guns for hire” even if their personalities don’t quite match up. Splinter would no question be Shepard Book. Mona would be Inara. And I’m on the fence about Cass but pilot or just another hired gun….. hmmm and maybe Casey could be the pilot. Or maybe Casey would be another captive of the EPF?
Am I forgetting anyone??…..
#rottmnt#slushie rambles#rottmnt au#oh god another one#I need to stop#rise of the tmnt#rise of the teenage mutant ninja turtles#firefly au#space cowboys
139 notes
·
View notes
Text
Dr Hilary Cass told the Times she wished to address the “disinformation” circulating about the findings and recommendations handed down by the Cass review when it was published on 10 April.
She said she had received online abuse in the wake of the report and had been advised to stop using public transport.
The report said the evidence base for gender medicine in young people had been thin and children had been let down by a “toxic” public discourse around gender.
Cass told the Times: “I have been really frustrated by the criticisms, because it is straight disinformation. It is completely inaccurate.
“It started the day before the report came out when an influencer posted a picture of a list of papers that were apparently rejected because they were not randomised control trials.
“That list has absolutely nothing to do with either our report or any of the papers.”
Referring to the online abuse she had received, she said: “There are some pretty vile emails coming in at the moment, most of which my team is protecting me from, so I’m not getting to see them.”
She added: “I’m not going on public transport at the moment, following security advice, which is inconvenient.”
The report said the now shuttered Gender Identity Development Service (Gids) at the Tavistock and Portman NHS Foundation Trust, the only NHS gender identity development service for children in England and Wales, used puberty blockers and cross-sex hormones despite “remarkably weak evidence” that they improved the wellbeing of young people and concern they may harm health.
The report recommended that young people struggling with their gender identity should be screened to detect neurodevelopmental conditions and there should be an assessment of their mental health, because some who seek help with their gender identity may also have anxiety or depression, for example.
When the report was released, Cass stressed that her findings were not intended to undermine the validity of trans identities or challenge people’s right to transition, but rather to improve the care of the fast-growing number of children and young people with gender-related distress.
Another day, another woman who believes she can clear her name if she just Explains Herself. But here's the thing: it was never actually about the science, it has always been about ensuring others, particularly women, are too terrified to step out of line (and too alienated from other women to see themselves as the affected woman).
#i think they target women bc (a) we're women and (b) bc we're more likely to be a child's primary carer (and without kids they have nothing)#but i hope she's safe and that her office workers aren't too upset by the threats she's getting (wtf gendies?)#also: shoutout to the male who threatened to gorge my eyes out and rape my eye sockets over my views on this topic :) fking psychopath#radblr#radfem safe#radfems do interact
9 notes
·
View notes
Text
The headcannon where Tim doesn't tell anyone in the batfam about his journey/mission to confirm Bruce is still alive (and lost in time) and how he lost his spleen is entirely hilarious to me.
Like imagine one day, he gets seriously injured in a patrol night and he needs like serious medical care. EVERYONE is worrying about Tim and so they all flock in the cave/clinic. Either Dr. Leslie or Alfred run tests and give him medical care, and then in the middle of doing so they find out that Tim doesn't have a major organ.
Alfred/Dr. Leslie would be like. "Ah, it seems like Timothy has a missing organ", and Tim, who is both DELIRIOUS and HIGH ON PAIN MEDS, answers, "oHhH, yEaH I dOnt hAvE a SpLeEn", and then he passes out.
That's when everyone starts to FREAK THE BAT OUT, Dick would be like, "WHAT? HOW? WHEN? WHY?", Damian would say, "Tch, obviously Drake is incompetent enough to lose an organ", and Bruce, BATMAN HIMSELF, would be so confused on how he didn't know or figured that out, "how did I not know my son is missing an organ". In short everyone would be freaking out.
When Tim wakes up, he is met by a bunch of questions (and water, thank you Cass), and he answers all of the questions like it's not a big deal, like, "Oh yeah, remember when ya'll thought Bruce was dead and didn't believe me he was alive? Yeah, that's when I lost my spleen", then he tells them the whole story.
When he was done with his story everyone would be like this emoji (😧), then Steph asks where he thinks his spleen is, Tim just jokes, "Ra's probably has in a jar somewhere, for him to look at every day", because Ra's has a weird obsession with Tim (it's gross). Jason and Steph would laugh at the joke while the others taught it wasn't funny.
After that everybody would be so protective of Tim, he gets benched (which he gets mad for), and Bruce would go back to Nanda Parbat to retrieve Tim's spleen from Ra's, and everything about this Headcannon is just funny to me 👌👌
#Please I need more fics like this#Recommend me somee#red robin#tim drake#jason todd#batfam#batman#stephanie brown#cassandra cain#robin#Batman#dick grayson#damian wayne#batfam shitpost#alfred pennyworth
308 notes
·
View notes
Text

“The NHS is shutting down its gender identity clinic for children after a damning review found that it failed vulnerable under-18s.
The gender identity service at Tavistock & Portman NHS Foundation Trust has been ordered to close by spring 2023.
It will be replaced by regional centres at existing children’s hospitals offering more “holistic care” with “strong links to mental health services”.
Tavistock’s Gender Identity Development Service (GIDS) clinic has been accused of rushing children into life-altering treatment on puberty blockers.
The paediatrician Dr Hilary Cass, who is leading a review of the service, has today issued a series of recommendations for a radical overhaul of how the NHS treats young people who are questioning their gender identity.
She found that the Tavistock clinic was “not a safe or viable long-term option” and that other mental health issues were “overshadowed” when gender was raised by children referred to the clinic.
Cass, former president of the Royal College of Paediatrics and Child Health, said the current model of a sole provider for gender services should be scrapped as it failed to meet the holistic needs of distressed and vulnerable teenagers.
She said Tavistock should be replaced by regional centres with an “appropriate multi-professional workforce to enable them to provide an integrated model of care that manages the holistic needs of this population”.
Amid concerns that the clinic fails to take into account wider health problems before putting children on puberty blockers, Cass added: “Staff should maintain a broad clinical perspective in order to embed the care of children and young people with gender uncertainty within a broader child and adolescent health context.”
NHS England, which commissioned Cass to review the service in September 2020, say they will implement her recommendations in full and decommission the Tavistock clinic.
They have announced they will launch two new clinics for children with gender dysphoria by spring 2023, which will bring together multiple doctors from a broad range of specialities.
The first, in London, will be based at Great Ormond Street Hospital and receive specialist mental health support from the South London and Maudsley NHS Foundation Trust.
The second, in the northwest, will be led by a partnership between Alder Hey Children’s NHS Foundation Trust and the Royal Manchester Children’s Hospital.
Cass said these clinics must have “established academic and education functions” to monitor evidence on children who are put on hormone therapy. The Tavistock clinic failed to collect sufficient data on the impact of puberty blockers in under-16s.
She said there was currently “insufficient evidence” for her to make any firm recommendations around their routine use.
Cass told the NHS to “enrol young people being considered for hormone treatment into a formal research protocol with adequate follow up into adulthood, with a more immediate focus on the questions regarding puberty blockers”.
The NHS said it would launch clinical trials in partnership with the National Institute for Health and Care Research to follow children on puberty blockers into adulthood.
A spokesman said: “This will ensure that there is greater transparency for children and their parents/carers around the uncertain clinical benefits and longer-term health impacts surrounding their use.”
The clinic has been overwhelmed by a sudden increase in referrals, particularly among young girls and children on the autism spectrum. Last year it received more than 5,000 referrals, compared to 250 a decade ago.
Cass’s final report will be published next year. Her interim review published in March found that services had developed without clear rules and that there was a “clinician lottery”, with widely varying approaches to treatment.
She found there was “a lack of agreement, and in many instances a lack of open discussion” about whether unhappiness with gender in adolescence was permanent or temporary. However, last year the Court of Appeal overturned a controversial ruling made by the High Court that children under 16 were unlikely to be able to give informed consent to receiving puberty blockers.
The case was brought against the Tavistock and Portman trust by Keira Bell, 24, who began taking puberty blockers when she was 16 to transition to male before later “detransitioning”.”
Link | Archived Link
249 notes
·
View notes