#gender affirming healthcare
Text
we love when studies confirm shit we already know 🥳🥳🥳
9K notes
·
View notes
Text
My favourite part of the Cass Report is where she goes: “Florence Ashley and others have shown that gatekeeping doesn’t work and should be abandoned. We disagree, not based on any evidence but because it’s incompatible with the way we’ve already decided we wanted to do things.”
#transgender#lgbtq#trans#queer#lgbtqia#lesbian#gay#lgbt#books#trans lit#cass review#cass report#gender affirming care#gender affirming healthcare#trans healthcare
1K notes
·
View notes
Text
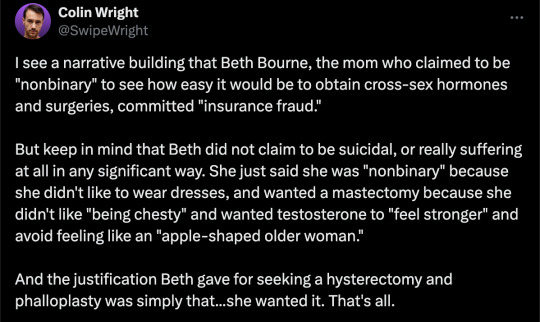
By: Beth Bourne
Published: Feb 27, 2024
Kaiser gender specialists were eager to approve hormones and surgeries, which would all be covered by insurance as “medically necessary.”
On September 6, 2022, I received mail from my Kaiser Permanente Davis Ob-Gyn reminding me of a routine cervical screening. The language of the reminder stood out to me: “Recommended for people with a cervix ages 21 to 65.” When I asked my Ob-Gyn about this strange wording, she told me the wording was chosen to be “inclusive” of their “transgender” and “gender fluid” patients.
Based on this response, several thoughts occurred to me. Could I expose the medical scandal of “gender-affirming care” by saying and doing everything my daughter and other trans-identifying kids are taught to do? Would there be the type of medical safeguarding and differential diagnosis we would expect in other fields of medicine, or would I simply be allowed to self-diagnose and be offered the tools (i.e. hormones and surgeries) to choose my own gender adventure and become my true authentic self?
If I could demonstrate that anyone suffering from delusions of their sex, self-hatred, or identity issues could qualify for and easily obtain body-altering hormones and surgeries, all covered by insurance as “medically necessary” and potentially “life-saving” care, then maybe people would finally wake up. I certainly had.
I was prepared for failure. I wasn’t prepared for how easy success would be.
* * *
I am a 53-year-old mom from Davis, CA. My daughter began identifying as a transgender boy (social transition) and using he/him pronouns at school during 8th grade. Like several of her peers who also identified as trans at her school, my daughter was a gifted student and intellectually mature but socially immature. This shift coincided with her school’s sudden commitment to, and celebration of, a now widespread set of radical beliefs about the biology of sex and gender identity.
She “came out” as trans to her father (my ex-husband) and me through a standard coming-out letter, expressing her wish to start puberty blockers. She said she knew they were safe, citing information she had read from Planned Parenthood and the World Professional Association for Transgender Health (WPATH). To say I was shocked would be an understatement. I was also confused because this announcement was sudden and unexpected. While others quickly accepted and affirmed my daughter’s new identity, I was apprehensive and felt the need to learn more about what was going on.
Events began escalating quickly.
During a routine doctor’s visit scheduled for dizziness my daughter said that she was experiencing, the Kaiser pediatrician overheard her father using “he/him” pronouns for our daughter. The pediatrician seemed thrilled, quickly asking my daughter about her “preferred pronouns” and updating her medical records to denote that my daughter was now, in fact, my son. The pediatrician then recommended we consult the Kaiser Permanente Oakland Proud pediatric gender clinic, where she could get further information and (gender affirming) “treatment.” Now I was the one feeling dizzy.
As I began educating myself on this issue, I discovered that this phenomenon—minors, most often teen girls, suddenly adopting trans identities—was becoming increasingly widespread. It even had a name: rapid onset gender dysphoria, or ROGD. Thankfully, after learning about the potential side-effects of blockers and hormones, my ex-husband and I managed to agree not to consent to any medical interventions for our daughter until she turned 18 and would then be able to make such decisions as an adult.
Over the past five years, my daughter’s identity has slowly evolved in ways that I see as positive. Our bond, however, has become strained, particularly since I began publicly voicing my concerns about what many term as “gender ideology.” Following my daughter’s 17th birthday family celebration, she sent me an email that evening stating she would be cutting off contact with me.
While this estrangement brought me sorrow, with my daughter living full-time with her father, it also gave me the space to be an advocate/activist in pushing back on gender identity ideology in the schools and the medical industry.
I decided to go undercover as a nonbinary patient to show my daughter what danger she might be putting herself in—by people who purport to have her health as their interest, but whose main interest is in medically “affirming” (i.e., transitioning) whoever walks through their door. I am at heart a mother protecting her child.
* * *
My daughter’s sudden decision to become a boy was heavily on my mind in early September of 2022, when mail from my Kaiser Permanente Davis Ob-Gyn reminded me of a routine cervical screening with “Recommended for people with a cervix ages 21 to 65.” I was told that the wording was chosen to be “inclusive” of transgender and “gender fluid” patients.
Throughout the whole 231-day process of my feigned gender transition, the Kaiser gender specialists were eager to serve me and give me what I wanted, which would all be covered by insurance as “medically necessary.” My emails were returned quickly, my appointments scheduled efficiently, and I never fell through the cracks. I was helped along every step of the way.
Despite gender activists and clinicians constantly claiming that obtaining hormones and surgeries is a long and complex process with plenty of safety checks in place, I was in full control at every checkpoint. I was able to self-diagnose, determine how strong a dose of testosterone I received and which surgeries I wanted to pursue, no matter how extreme and no matter how many glaring red flags I purposefully dropped. The medical workers I met repeatedly reminded me that they were not there to act as “gatekeepers.”
I was able to instantly change my medical records to reflect my new gender identity and pronouns. Despite never being diagnosed with gender dysphoria, I was able to obtain a prescription for testosterone and approval for a “gender-affirming” double mastectomy from my doctor. It took only three more months (90 days) to be approved for surgery to remove my uterus and have a fake penis constructed from the skin of my thigh or forearm. Therapy was never recommended.
Critics might dismiss my story as insignificant on the grounds that I am a 53-year-old woman with ample life experience who should be free to alter her body. However, this argument for adult bodily autonomy is a standard we apply to purely cosmetic procedures like breast implants, liposuction, and facelifts, not “medically necessary” and “lifesaving” treatments covered by health insurance. Or interventions that compromise health and introduce illness into an otherwise healthy body. And especially not for children.
My story, which I outline in much more detail below, should convince any half-rational person that gender medicine is not operating like any other field of medicine. Based on a radical concept of “gender identity,” this medical anomaly preys upon the body-image insecurities common among pubescent minors to bill health insurance companies for permanent cosmetic procedures that often leave their patients with permanently altered bodies, damaged endocrine systems, sexual dysfunction, and infertility.
* * *
Detailed Timeline of Events
On October 6, 2022, I responded to my Ob-Gyn’s email to tell her that, after some thought, I’d decided that maybe the label “cis woman” didn’t truly reflect who I was. After all, I did have some tomboyish tendencies. I told her I would like my records to be changed to reflect my newly realized “nonbinary” identity, and that my new pronouns were they/them. I also voiced my desire to be put in touch with an endocrinologist to discuss starting testosterone treatment.
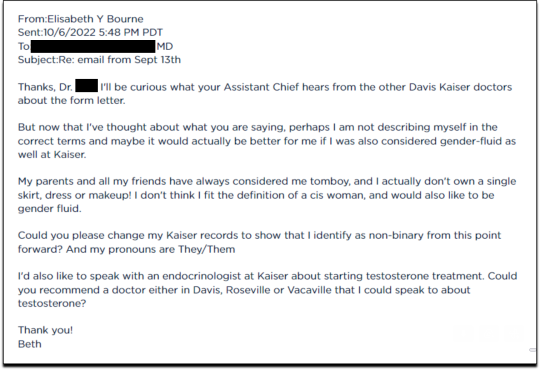
Fifteen minutes later I received an email from another Kaiser doctor informing me that my medical records had been changed, and that once my primary doctor returned to the office, I’d be able to speak with her about hormone therapy.
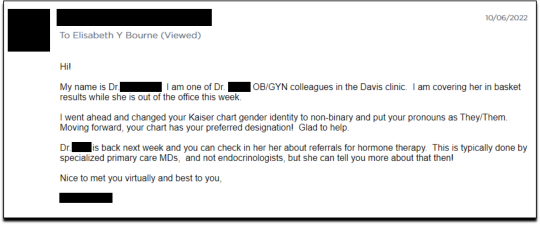
I responded the following day (October 7, 2022), thanking her for changing my records, and asking if she could connect me with someone who could help me make an appointment for “top surgery” (i.e., a cosmetic double mastectomy) because my chest binder was rather “uncomfortable after long days and playing tennis.”
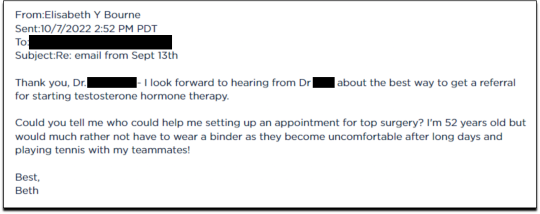
She told me to contact my primary care MD to “get things rolling,” and that there were likely to be “preliminary evaluations.”
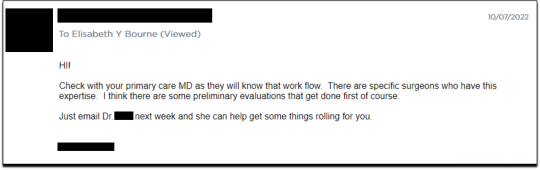
Six days after contacting my primary care MD for a referral, I received an email from one of Kaiser’s gender specialists asking me to schedule a phone appointment so she could better understand my goals for surgery, so that I could get “connected to care.” This call to review my “gender affirming treatment options and services” would take 15-20 minutes, after which I would be “booked for intake,” allowing me to proceed with medical transition.
This wasn’t an evaluation of whether surgical transition was appropriate, it was simply a meeting for me to tell them what I wanted so that they could provide it.
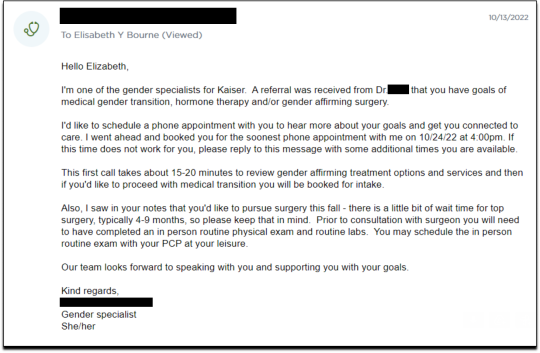
On October 18, I had my one and only in-person appointment in preparation for top surgery. I met in Davis with my primary care physician, Dr. Hong-wen Xue. The assessment was a 10-minute routine physical exam that included blood tests. Everything came back normal. Notably, there was not a single question about why I wanted top surgery or cross-sex hormones. Nor was there any discussion of the risks involved with these medical treatments.
The following week, on October 24, I had a phone appointment with Rachaell Wood, MFT, a gender specialist with Kaiser Sacramento. The call lasted 15 minutes and consisted of standard questions about potential drug use, domestic violence, guns in the house, and whether I experienced any suicidal thoughts. There were no questions from the gender specialist about my reasons for requesting a mastectomy or cross-sex hormones, or why I suddenly, at 52, decided I was “nonbinary.”
After the call, Kaiser emailed me instructions about how to prepare for my pre-surgery intake video appointment to evaluate my mental health, scheduled to take place on November 15. The email stated that prior to my appointment, I should research hormone risks on the WPATH website, and to “research bilateral mastectomy and chest reconstruction surgery risks and recovery” on Kaiser’s website.
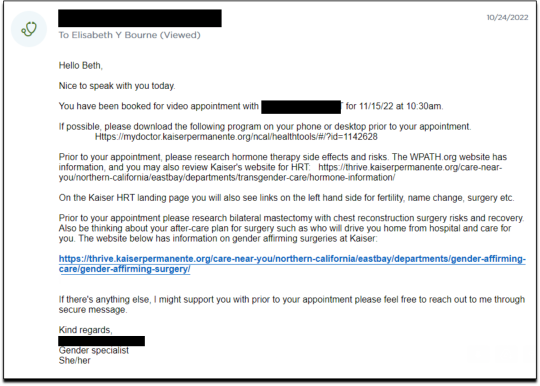
I decided to request a “gender-affirming” double mastectomy and phalloplasty. Kaiser sent me a sample timeline for gender transition surgery preparation (see below) that you can use as a reference for the process. I also asked for a prescription for cross-sex hormones (testosterone) as needed and recommended by Kaiser.
[ Source: Kaiser Permanente, Top Surgery - EXPLORING YOUR SURGICAL OPTIONS ]
Pre-Surgery Mental Health Video Appointment, Part I
This “Mental Health Visit” assessment was conducted over Zoom. The Kaiser gender specialist started with questions addressing my marital status, race, gender identity, and other demographics. She asked whether I was “thinking of any other surgeries, treatments in the future.” The list she read included “gender-affirming” hysterectomies, bottom surgeries such as metoidioplasty and phalloplasty, vocal coaching, support groups, and body contouring. “Anything else you might be interested in doing?” she asked. I said that I’d perhaps be interested in body contouring. I was also assured that all the procedures would be covered by insurance because they were considered “medically necessary.”
I dropped in several red flags regarding my mental health to see the reaction, but all were ignored. For instance, I revealed that I had PTSD. When the therapist asked me about whether I had experienced any “childhood trauma,” I explained that I grew up in Mexico City and had been groped several times and had also witnessed men masturbating in public and had been grabbed by men in subways and buses. “I was a young girl, so [I had] lots of experiences of sexual harassments, sexual assault, just the kind of stuff that happens when you are a girl growing up in a big city.” “So, you know,” I finished, “just the general feeling that you are unsafe, you know, in a female body.”
The therapist did not respond to my disclosure that trauma could be the cause of my dysphoria. Instead of viewing this trauma as potentially driving my desire to escape my female body through hormones and surgery, she asked whether there is anything “important that the surgery team should be aware of” regarding my “history of trauma,” such as whether I’d be comfortable with the surgeon examining and marking my chest prior to surgery.
When asked about whether I had had any “psychotic symptoms,” I told her that while I had had no such symptoms, my mother had a delusional nervous breakdown in her 50s because she had body dysmorphia and became convinced she had a growth on her neck that needed to be removed. I told her that my mother was then admitted to an inpatient hospital for severe depression. I asked her whether she ever sees patients with body dysmorphia and whether I could have potentially inherited that from my mother. She told me that psychosis was hereditary, but that it was “highly unlikely” that there was any connection between body dysmorphia and gender dysphoria.
I enthusiastically waved more mental health red flags, waiting to see if she would pick up on any of them.
I’m just wondering if my feelings, or perseverating, or feeling like these breasts make me really unhappy and I just don’t want them anymore!...I’m just not sure if that’s a similar feeling to body dysmorphia? How do you decide which one is gender dysphoria and general body dysmorphia, and just not liking something about your body? Feeling uncomfortable with your body?
And I did have an eating disorder all through college. I was a distance runner in college so I had bulimia and anorexia, you know. So I don’t know if that’s related to gender dysphoria?
The therapist replied, “I completely appreciate your concerns, but I am going to ask you questions about your chest, about your expectations. And then I’ll be able to give you an assessment.” She also said the main difference between my mom’s situation and mine was that my mom didn’t really have a growth on her neck, whereas it’s “confirmed” that I actually have “chest tissue.” Furthermore, she said that while “historically there has been all this pressure on patients to be like ‘Are you really, really sure you want hormones? Are you 100% sure?’ We are a little more relaxed.” She continued, “As long as you are aware of the risks and the side-effects, you can put your toe in the water. You can stop ‘T’ [testosterone], you can go back and do it again later! You can stop it! You can stop it! You know what I mean?”
Because we ran out of time, I scheduled a follow-up phone meeting on December 27, 2022 with a different gender specialist to complete my mental health assessment for top surgery.
Pre-Surgery Mental Health Video Appointment, Part II
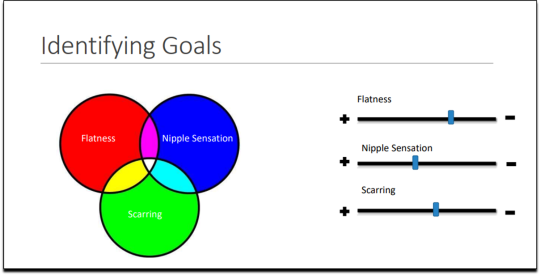
During this meeting, Guneet Kaur, LCSW, another Kaiser gender specialist (she/her/they/them pronouns) told me that she regretted the “gatekeeping vibe” of the meeting but assured me that since I have been “doing the work,” her questions are essentially just a form of “emotional support” before talking with the medical providers.
She asked me about what I’d been “looking into as far as hormones.” I told her that I’d be interested in taking small doses of testosterone to counterbalance my female feelings to achieve “a feeling that’s kind of neutral.”
When she asked me about me “not feeling like I match on the outside what I feel on the inside,” I dropped more red flags, mentioning my aversion to wearing dresses and skirts.
I don’t own a single dress or a skirt and haven't in 20 years. I think for me it’s been just dressing the way that’s comfortable for me, which is just wearing, jeans and sweatshirts and I have a lot of flannel shirts and, and I wear boots all the time instead of other kinds of shoes. So I think it’s been nice being able to dress, especially because I work from home now most of the time that just a feeling of clothing being one of the ways that I can feel more non-binary in my everyday life.
She responded, “Like having control over what you wear and yeah. Kind of that feeling of just, yeah, this is who I am today. That’s awesome. Yeah.”
She then asked me to describe my dysphoria, and I told her that I didn’t like the “feeling of the female form and being chesty,” and that because I am going through menopause, I wanted to start taking testosterone to avoid “that feeling of being like this apple-shaped older woman.” “Good. Okay, great,” she responded, reminding me that only “top surgery,” not testosterone, would be able to solve my chest dysphoria. (Perhaps it was because all these meetings were online, they didn’t notice I’m actually fit and relatively slender at 5’-5” and 130 pounds, and not apple-shaped at all.)
She told me that we had to get through a few more questions related to my medical history before “we can move on to the fun stuff, which is testosterone and top surgery.”
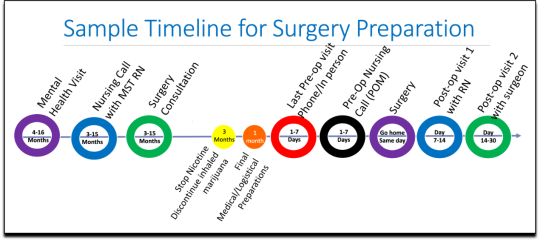
The “fun stuff” consisted of a discussion about the physical and mood changes I could expect, and her asking me about the dose of testosterone I wanted to take and the kind of “top surgery” technique I’d prefer to achieve my “chest goals.” She told me that all or most of my consultations for surgeries and hormones would be virtual.
The gender specialist told me after the appointment, she would submit my referral to the Multi-Specialty Transitions Clinic (MST) team that oversees “gender expansive care.” They would follow up to schedule a “nursing call” with me to review my medical history, after which they’d schedule my appointment with a surgeon for a consultation. Her instructions for this consultation were to “tell them what you’re wanting for surgery and then they share with you their game plan.”
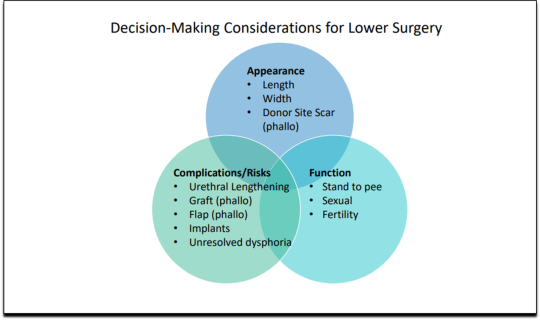
[ Decision-making slide to help me identify my goals for top surgery–flat chest, nipple sensation, or minimal scarring. Source: Kaiser Permanente, Top Surgery - EXPLORING YOUR SURGICAL OPTIONS ]
She told me that Kaiser has a team of plastic surgeons who “only work with trans and nonbinary patients because there’s just so much need for them.” She asked about my priorities for chest surgery, such as whether I value flatness over nipple sensation. I learned about double incision top surgery with nipple grafts, as well as “keyhole,” “donut,” “buttonhole,” and “Inverted-T” top surgeries.
By the end of the hour-long appointment, I had my surgery referral and was ready for my “nursing call” appointment.
Nursing call with Nurse Coordinator from the Transgender Surgery and Gender Pathways Clinic at Kaiser San Francisco
On January 19, 2023, I had my nursing call with the Nurse Coordinator. He first said that “the purpose of this call is just for us to go through your chart together and make sure everything’s as accurate as possible.” Once that was done, my referral would be sent to the surgeon for a consultation.
He asked me about potential allergies and recreational drug use, and verified that I was up to date on mammograms, pap smears, and colon cancer screenings, as well as vaccines for flu and COVID. I verified my surgical history as well as my current medications and dietary supplements.
He told me about a “top surgery class” available for patients where one of the Kaiser surgeons “presents and talks about surgical techniques and options within top surgery,” and includes a panel of patients who have had top surgery. I signed up for the February 8th class.
Within 10 minutes he told me that he had “sent a referral to the plastic surgery department at Kaiser Sacramento,” and that I should be hearing from them in the next week or two to schedule a consultation.
Appointment for Testosterone
On January 27, I had a 13-minute online appointment with a primary care doctor at Kaiser Davis to discuss testosterone. The doctor verified my name and preferred pronouns, and then directly asked: “So, what would you like to do? What kind of physical things are you looking for?”
I told her I wanted facial hair, a more muscular and less “curvy” physique, and to feel stronger and androgynous. She asked me when I wanted to start, and I told her in the next few months. She asked me if I was menopausal, whether I had ovaries and a uterus, although that information should have been on my chart.
The doctor said she wanted me to come in to get some labs so she could check my current estrogen, testosterone, and hemoglobin levels before starting hormones. Then “we'll set the ball in motion and you'll be going. We’ll see you full steam ahead in the direction you wanna go.”
That was it. I made an appointment and had my lab tests done on February 12. My labs came back on February 14, and the following day, after paying a $5 copay at the Kaiser pharmacy, I picked up my testosterone pump. That was easy!
Top Surgery Consultation
On the same day I received my labs, I had a Zoom surgery consultation with Karly Autumn-Kaplan, MD, Kaiser Sacramento plastic surgeon. This consultation was all about discussing my “goals” for surgery, not about whether surgery was needed or appropriate.
I told the surgeon that I wanted a “flatter, more androgynous appearance.” She asked me some questions to get a better idea of what that meant for me. She said that some patients want a “male chest,” but that others “want to look like nothing, like just straight up and down, sometimes not even nipples.” Others still wanted their chest to appear slightly feminine and only “slightly rounded.” I told her that I’d like my chest to have a “male appearance.”
“What are your thoughts about keeping your nipples?” she asked. “Are you interested in having nipples or would you like them removed?” I told her that I’d like to keep my nipples, but to make them “smaller in size.” She asked me if I’d like them moved to “the edge of the peck muscle” to achieve “a more male appearance.” I said yes.
I was asked to show my bare chest from the front and side, which I did. Then she asked me how important it was for me to keep my nipple sensation. I replied that it was important unless it would make recovery more difficult or there were other associated risks. She highlighted the problem with the free nipple graft, saying that removing the nipple to relocate it means “you're not gonna have sensation in that nipple and areola anymore.” However, some nipple sensation could be preserved by keeping it attached to “a little stalk of tissue” with “real nerves going to it,” but that would require leaving more tissue behind. I told her I’d go for the free nipple graft to achieve a flatter appearance. It was also suggested I could skip nipple reconstruction entirely and just get nipples “tattooed” directly onto my chest.
She told me I was “a good candidate for surgery,” and put me on the surgery wait list. She said that the wait time was between three and five months, but a cancellation could move me up to a sooner date. Also, if I wanted surgery as soon as possible, I could tell the surgery scheduler that I’d be willing to have any of the other three surgeons perform my mastectomy. Outpatient top surgery would cost me a copay of $100.
They contacted twice, in February and March, notifying me of cancellations. If I had accepted and shown up on those dates, they would have removed my breasts. This would have been less than five months from the time I first contacted Kaiser to inform them of my new “nonbinary” gender identity.
How Far Can I Go?
I decided to see how easy it would be for me to get approved for a phalloplasty. Known euphemistically as “bottom surgery,” phalloplasty is the surgical creation of an artificial penis, generally using tissue from the thigh or arm.
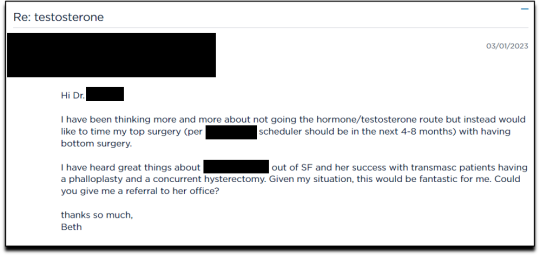
I sent an email on March 1, 2023, requesting to have a phalloplasty and concurrent hysterectomy scheduled alongside my mastectomy.
Two weeks later, on March 16th, I had a 16-minute phone call with a gender specialist to discuss my goals for bottom surgery and obtain my referral.
During the call, I explained to the specialist that I wasn’t sure about taking testosterone anymore because I was already quite athletic and muscular, and that taking testosterone didn’t make much sense to me. Instead, I wanted bottom surgery so that I wouldn’t feel like my “top” didn’t match my “bottom.” I told her:
But what I really wanted was to have bottom surgery. So this way when I have my top surgery, which sounds like it could be very soon, that I’ll be aligned, that I won’t have this sense of dysphoria with one part of my body and the other part feeling like it matched who I am. So yeah. So I just did a little bit more research into that. And I looked at the resources on the Kaiser page for the MST clinic and I think I know what I want, which is the hysterectomy and then at the same time or soon after to be able to have a phalloplasty.
I told her that I wanted to schedule the top and bottom surgery concurrently so that I wouldn’t have to take more time off work and it would save me trips to San Francisco or Oakland, or wherever I had to go for surgery.
None of this gave the gender specialist pause. After a brief conversation about some online resources to look over, she told me that she would “submit the referral now and we’ll get this ball rolling.”
Bottom surgery would cost me a copay of $200, which included a couple of days in the hospital for recovery.
Phalloplasty Surgical Consultation with Nurse Coordinator
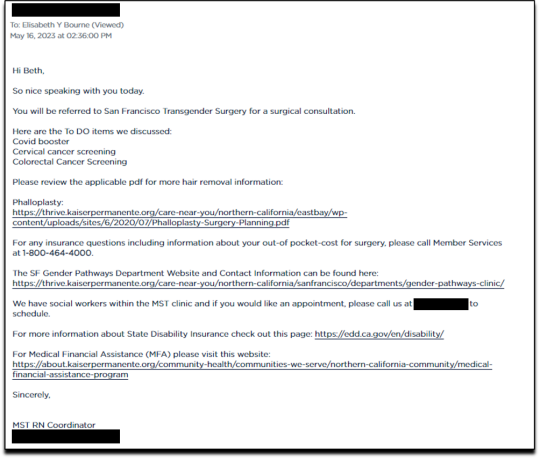
On May 16, 2023, I had a short surgical consultation with a nurse coordinator to go through my medical history. This was similar to the consultation for top surgery but included information about hair removal procedures for the skin on my “donor site” that would be fashioned into a makeshift penis. They also went over the procedures for determining which donor site—forearm or thigh—was more viable.
After only 15 minutes, she submitted my referral to the surgeon for another surgical consultation.
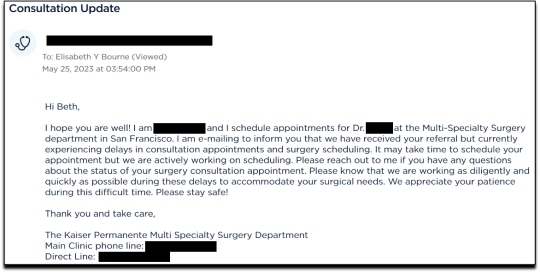
On May 25 I received an email from my phalloplasty surgeon’s scheduler, informing me that they have received my referral and are actively working on scheduling, but that they are experiencing delays.
I ended my investigation here once I had the referral for the top and bottom surgery. I never used my testosterone pump.
Final Thoughts
In fewer than 300 days, based on a set of superficial and shifting thoughts about my gender and my “embodiment goals” triggered by the mere mention of “gender” in a form letter from my primary care physician, and driven by what could only be described as minor discomforts, Kaiser Permanente’s esteemed “multi-disciplinary team” of “gender specialists” was willing, with enthusiasm—while ignoring mental health concerns, history of sexual trauma, and rapidly escalating surgical requests—to prescribe life-altering medications and perform surgeries to remove my breasts, uterus, and vagina, close my vaginal opening, and attempt a complex surgery with high failure and complication rates to create a functionless representation of a penis that destroys the integrity of my arm or thigh in the process.
This describes the supposedly meticulous, lengthy, and safety-focused process that a Kaiser patient must undergo to embark on a journey to medically alter their body. No clinician questioned my motivations. No one showed concern that I might be addressing a mental health issue through radical and irreversible interventions that wouldn’t address my amorphous problems. There were no discussions about how these treatments would impact my long-term health, romantic relationships, family, or sex life. I charted the course. The clinicians followed my lead without question. The guiding issue was what I wanted to look like.
No other medical field operates with this level of carelessness and disregard for patient health and welfare. No other medical field addresses issues of self-perception with surgery and labels it “medically necessary.” No other medical field is this disconnected from the reality of the patients it serves.
Kaiser has traded medicine for ideology. It’s far beyond time we stop the ruse of considering “gender-affirming” interventions as anything approaching medical care.
This isn’t the first time Kaiser Permanente has been in the news for completely disregarding medical safeguards in the name of “gender-affirming care.” As girls, Chloe Cole and Layla Jane became convinced that they were born in the wrong body and were actually boys on the inside. Doctors at Kaiser ignored their underlying conditions and instead prescribed testosterone and removed their breasts. Both Cole and Jane have since detransitioned and are currently suing Kaiser.
The fact that children and vulnerable adults are being exploited in this massive ideological experiment is not just tragic; it’s deeply disturbing, especially considering it has evolved into a billion-dollar industry.
I hope that by sharing my story, I can bring more focused scrutiny to the medical scandal unfolding not just at Kaiser but also at medical centers and hospitals across the Western world. These institutions have completely abandoned medical safeguards for patients who claim to be confused about their “gender,” and I aim to awaken more parents and assist them in protecting their children.
--
==
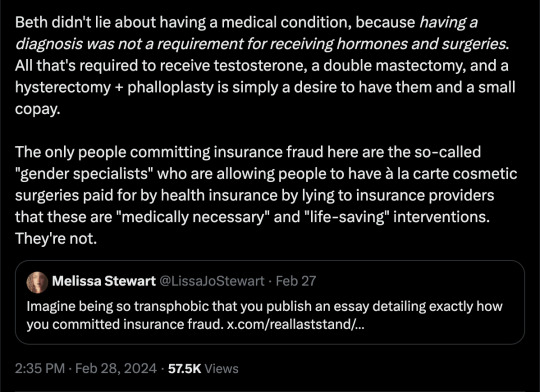
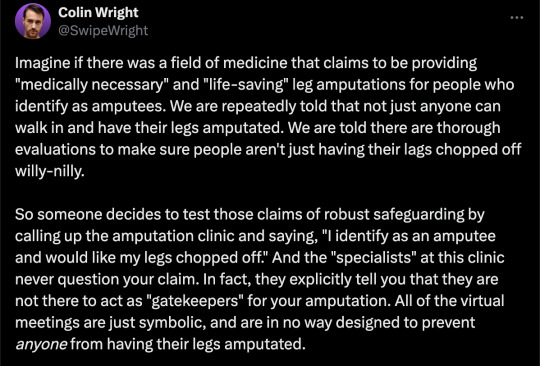
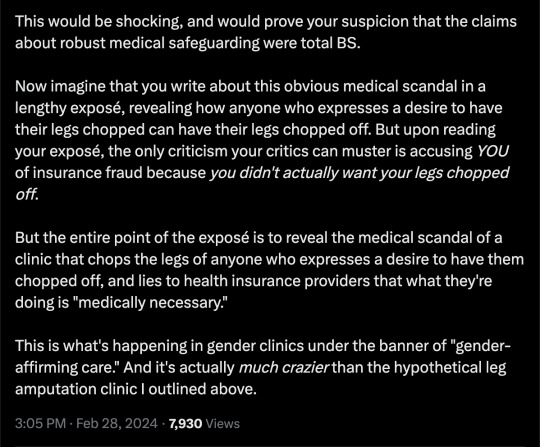
This is completely insane.
Apologists online are running around saying, but she didn't mean it, she was lying, she was pretending...
It doesn't matter.
Any kind of security, penetration or integrity test is insincere too. When security researchers compromise Microsoft's operating system or Google's browser or whatever, "but they didn't mean it" is not a defence to a discovered security flaw. It doesn't matter that the security researchers didn't plan to steal data or money or identities. The flaw in the system is there regardless.
It doesn't matter that it was insincere. Because the workers didn't know that. They never checked, never asked questions, never tested. They had been taught and instructed to never ask any questions. They did what they were supposed to. And the system failed spectacularly. Because that's what "gender affirming care" means.
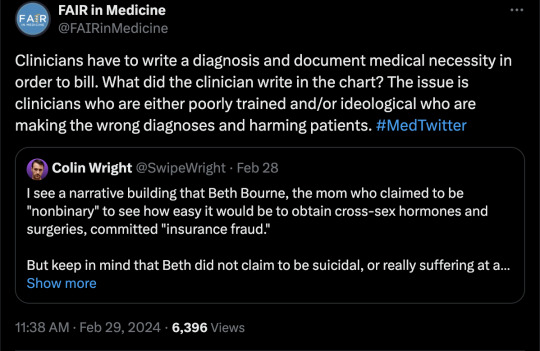
Additionally, the claim that Beth Bourne committed fraud is an outright lie. A patient cannot bill. They do not have the authority. The medical clinic is the only one that can bill, and they must supply a diagnosis and a medical necessity.
If they didn't diagnose her and just wrote down what she said, then they committed fraud. If they claim they did diagnose her, then they committed fraud, because the diagnosis they concocted was bogus. This, by the way, is actually going on. Clinics are reporting fake endocrine and other disorders to get blockers, hormones and other interventions. Jamie Reed and other whistleblowers have documented evidence of this. Beth Bourne is not responsible for what the clinic does. They have medical licenses and legal responsibility. Not her.
Additionally, anyone who actually read the article would know how she tested the system. She said things like, "I've always been not that feminine. So, maybe I get my boobs removed." And they said, "sure." Instead of saying, "wait, why do you think that?" Framing it as her lying is itself a lie. They violated their ethical obligations. That much is incontrovertible. And it's directly the result of "gender affirming care," where clinics and clinicians rubber-stamp anything deemed "trans" based entirely on ideological, not medical, grounds.
#Beth Bourne#undercover#undercover investigation#gender identity ideology#queer theory#nonbinary#non binary#top surgery#bottom surgery#double mastectomy#bilateral mastectomy#gender affirming care#gender affirming healthcare#gender affirmation#affirmation model#medical scandal#medical malpractice#medical corruption#religion is a mental illness
745 notes
·
View notes
Text
A Plains Cree physician who practices family medicine in Alberta says it’s shameful that Conservative Premier Danielle Smith is playing politics with transgender issues.
“It’s really important to know that people don’t do this [gender affirmation] lightly,” said Dr. James Makokis, who identifies as Two-Spirit and works directly with trans patients. “It is something that they’ve known their entire life.
“And clinicians do thorough assessments of ensuring that people when they say they’re trans, they’re trans and we just ensure that there’s not medical contra-indications to doing so and there is a thorough assessment process of that.”
On Wednesday, Smith announced a number of policy changes on social media that will restrict medical access to those seeking gender affirmation therapy – especially transgender youth.
Full article
Tagging: @politicsofcanada
#cdnpoli#canada#canadian politics#canadian news#canadian#alberta#james makokis#plains cree#saddle lake cree nation#danielle smith#conservatives#UCP#united conservative party#transphobia#trans rights#trans youth#transphobia tw#gender affirming care#gender affirming healthcare
444 notes
·
View notes
Text

#lgbtqia#lgbtq community#lgbtq#lesbian#sapphic#nonbinary lesbian#nonbinary#queer#lgbt pride#gay girls#harry potter#harry james potter#hp fanart#hp fandom#harry potter fanart#hp fanfic#gender affirming care#gender affirmation#gender affirming surgery#gender affirming healthcare#gender affirming treatment#jk rowling#fuck jkr#jk
604 notes
·
View notes
Text
Not asking about medical complications since that's sort of a different question; this poll is asking about the aesthetic and/or functional results. Obviously a person can have multiple different procedures done with different levels of satisfaction; select any one that applies.
Gender-affirming surgery includes but is not limited to procedures like breast removal, reduction, or augmentation; facial feminization or masculinization; the construction of different genitals; liposuction/body sculpting, etc.
–
We ask your questions so you don’t have to! Submit your questions to have them posted anonymously as polls.
#polls#incognito polls#anonymous#tumblr polls#tumblr users#questions#polls about health#submitted nov 17#polls about the body#polls about lgbtq stuff#lgbtq#trans#transgender#gender affirming care#gender affirming healthcare#gender affirming surgery#trans healthcare#surgery#medical
305 notes
·
View notes
Note
So like, how does being trans work anyhow? I’ve tried to research stuff myself (by googling like fifty different things) but I still have like no idea what happens??? Like I’ve heard about HRT but I have no clue how someone would go about that?
Asking cuz I read your comics a bunch and your parents remind me of my parents
Your question seems confused so I'm gonna section off what I'm seeing.
1) being trans is identifying with a gender one was not assigned at birth. If you're AMAB (assigned male at birth) for instance, identifying as a woman or non-binary, etc would make you transgender.
2) transitioning is the process by which someone changes physical and/or social characteristics about themselves to better align with their gender identity. The ways to go about this range a lot- HRT (hormone replacement therapy), laser hair removal, clothing choices, haircuts, new names, and any number of treatments related are included.
3) The way you go about acquiring HRT is going to depend on your age, location, access to insurance, and access to healthcare. In medical establishments, there's 2 main ways its acquired
1. Informed consent - the doctor explains the risks and expectations and you consent to receiving the medication(s).
2. Diagnosis care - a therapist finds you experience gender dysphoria and believes you to be transgender and writes you a letter in order for your doctor to prescribe HRT.
You'll need to research your country and/or local area for what's legal and available.
There's a 3rd option, which is DIY, but it's usually considered a last option due to the involvement one needs to have in order to do it safely.
That's not even going into social transition, which may consist of changing your name, establishing pronouns that align with your identity, sharing your gender identity, etc
Anyways, i hope this answers all your questions and helps you out!
#trans#lgbtq#mtf hrt#ftm hrt#hrt#gender affirming care#gender affirming healthcare#gender transition#mtf trans#ftm man#nonbinary#planned parenthood
556 notes
·
View notes
Text
A new landmark study has found that access to gender-affirming healthcare significantly reduces rates of depression, gender dysphoria, and suicidality among transgender people.
While it’s no secret that providing gender-affirming care to transgender individuals who ask for it can greatly benefit their well-being, an increase in transphobic rhetoric and bans on gender-affirming healthcare has prompted thorough medical studies into the impact of such care.
Now, brand new research conducted in Melbourne, Australia, has found that allowing transgender people to access the care they’re after can reduce suicidality by a stunning 55%.
As part of the first-ever randomized controlled trial (RCT) on gender-affirming care, researchers took 64 transgender and gender-diverse adults who had been looking to start testosterone therapy and randomly split them into a treatment group and a control group.
While the treatment group was allowed to begin hormone therapy that week, the control group waited three months for their treatment to begin.
Before the study began, both groups were evaluated on depression, gender dysphoria, and suicidality. Three months later, the two groups were evaluated again.
RCTs for medical care can often be hard to conduct due to practical and ethical concerns. However, researchers of this study found a way to hold an RCT for this study by incorporating a shorter follow-up period. Rather than giving the control group a placebo drug, or no treatment at all, they were simply given a longer wait time.
The results showed a notable decrease in gender dysphoria, depression, and – most significantly – suicidality.
The group that received gender-affirming care right away saw a 55% reduction in suicidality compared to a 5% drop within the control group.
Depression scores in the treatment group decreased by half, while gender dysphoria rates also significantly decreased.
Breaking down their findings, researchers Brendan J. Nolan MBBS, Sav Zwickl, PhD, and Peter Locke wrote: “There was a statistically significant decrease in gender dysphoria in individuals with immediate [access to gender-affirming care] compared with delayed initiation of testosterone therapy.”
“A clinically significant decrease in depression and a decrease in suicidality also occurred with immediate testosterone therapy.”
“The findings of this trial suggest that testosterone therapy significantly decreases gender dysphoria, depression, and suicidality in transgender and gender-diverse individuals desiring testosterone therapy.”

Of course, this isn’t the first time that research has shown significant drops in depression and suicide rates among transgender individuals who receive gender-affirming care.
A 2022 medical study showed that young transgender people who have access to puberty blockers are 73% less at risk of suicide and report improved well-being.
But, as anti-trans activists advocate for further bans on gender-affirming care, one of the key arguments is that the evidence in support of the care isn’t up to scratch with GRADE (Grades of Recommendation, Assessment, Development, and Evaluation) standards.
So research like this landmark RCT is so significant to the transgender community and its allies as the fight for their healthcare rights rumbles on.
#us politics#news#pinknews#2023#gender affirming care#gender affirming healthcare#transgender healthcare#transgender#trans rights#trans healthcare#suicidality#depression#gender dysphoria#Australia#randomized controlled trial#trust the science#Brendan J. Nolan#Sav Zwickl#Peter Locke#testosterone therapy#Grades of Recommendation Assessment Development and Evaluation#lgbtqia+#lgbtqia+ rights
448 notes
·
View notes
Text
After Mississippi banned his hormone shots, an 8-hour journey
Katie had done all she could to prepare for this trip. She’d asked a relative to pick up her two younger boys from school. She’d researched how to change a tire, and she’d spent hours on Google Maps, searching for the closest Walgreens in Alabama. She’d finally found a destination in Thomasville, a rural town nearly 200 miles from their suburban Mississippi home, but much remained unclear. Would they make it by noon for Ray’s telehealth appointment? Would the pharmacy give him testosterone?
Katie looked at her boy, a thin 17-year-old with wavy hair and an easy grin, and she asked herself the question that had begun to matter least: Was she breaking the law?
Two months earlier, Mississippi had banned transgender young people, like Ray, from accessing hormones or other gender-transition treatments. By mid-spring, nearly half the country had passed similar bills, according to the Movement Advancement Project, and now, 1 in 3 trans children lives in a state with a ban. Conservative lawmakers said they’d pushed the bills to protect young people, but Katie felt like they’d done the opposite. Testosterone had allowed her son to embody himself for the first time. Ray was present, happy. The ban would take that happiness away.
Across the country, families were doing everything they could to protect their trans children. Some uprooted their lives in red states for the promise of protections in blue ones. Others filed lawsuits. Katie couldn’t afford to move, and she needed a solution faster than the courts could offer, so she’d settled on a cheaper, quicker plan: She’d take a day off from her nursing job, and she and Ray would travel out of state for his medical care.
No one should have to go to these lengths just to access what is essentially basic life-saving heath care.
Also, major shout out to QMed and Dr. Lowell and the Southern Trans Youth Emergency Project for the work that they are doing to help trans youth and adults in red states access gender affirming care.
#trans#trans healthcare bans#trans healthcare#gender affirming hormone therapy#gender affirming healthcare#gaht#transgender#trans rights#trans rights are human rights#protect trans lives#protect trans youth
442 notes
·
View notes
Text
MILDLY URGENT TOP SURGERY COMMISSIONS!!
Please do consider commissioning me! £8000 is a lot and the waiting list is 8 YEARS!! DM for info





REBLOGS HIGHLY ENCOURAGED!!
#commission#art commisions#commisions open#urgent commissions#top surgery#trans#transgender#queer#gender affirming care#gender affirming healthcare#big shot spamton#deltarune spamton#deltarune chapter 2#deltarune#sorry for tagging the fandom tags#the post DOES have spamton in it to be fair
143 notes
·
View notes
Text
With the Alberta government announcing a ban on gender-affirming care until 16 years old, let’s take a minute to correct some misinformation using peer-reviewed publications. A thread.🧵
“High quality evidence doesn’t support gender-affirming care.”
‘High quality evidence’ is a technical term that essentially just means ’no randomized controlled trials.’ RCTs are not scientifically feasible for trans youth care and would be unethical (link).
The evidence-base for gender-affirming care is quite robust and is at least as good at the evidence base for comparable interventions like abortion and birth control. For an overview of available studies, albeit already few years outdated, see page 144 onwards (link).
“Over 80% of kids grow out of being trans.”
That’s just not true. The claim is based on old, poor-quality studies that included tons of kids who never claimed to be trans (link).
But even if we took the percentage at face value, it would be irrelevant since it’s based on pre-pubertal data and virtually all the so-called ‘desistance’ occurred before puberty, when gender-affirming care becomes available (link).
More recent, better studies suggest that only around 2.5% have ‘grown out of it’ after 5 years (link).
“Kids falsely believe that they are trans because of social contagion.”
There is no evidence for that claim. It’s based on the reports of transphobic parents who were surprised that their kid came out ‘out of the blue’ and happened to have trans friends, as trans kids tend to do. For a careful explanation of why the claim is completely unsupported by evidence, see this (link).
Studies of trans youth that used clinical data to look into the claim have also failed to find any evidence of epidemic or large-scale social contagion (link).
“We need a years-long diagnostic process to make sure kids are ‘truly’ trans before they transition.”
There is no evidence that gender assessments fare any better than self-report at predicting future outcomes, as we explain in our recent review (link).
“Gender-exploratory therapy can help identify the trauma that made these kids gender dysphoric.”
Gender-exploratory therapy is extremely difficult to distinguish from classic conversion therapy, which also starts from the premise that ‘trauma’ makes people LGBTQ2S+ (link).
Since conversion therapy is known to be harmful, we have reasons to believe that gender-exploratory therapy would be as well.
Self-directed exploration is good. Forced exploration rooted in suspicion towards trans identities isn’t. If you’re starting from the belief that trans identities are inherently suspicious, you’re not doing therapy, you’re doing transphobia.
Any more myths about gender-affirming care you’d like me to bust, Tumblr?
#transgender#trans#lgbtq#lgbtqia#queer#lgbt#gender affirming care#gender affirming healthcare#trans healthcare#science#misinformation
253 notes
·
View notes
Text
hi
i have 82 days left to raise $8,715 more for top surgery
if i can’t pay for top surgery in full by February 27th, 2024, i’m going to have to push my date back.
2023 has been a really stressful year because of my brain injury, brain cyst, and the resulting health and financial complications. please help me start off 2024 in a better place!
you can find my fund here.
it would also be extremely helpful if folks could share this link on other platforms and social sites!
thank you <3
#diary#top surgery#ftm#transgender#transmasculine#transmasc#non binary#nonbinary#enby#transandrogynous#gender affirming care#gender affirming healthcare#queer#lgbt#lgbtq#lgbtqi#lgbtqia#lgbt+#lgbtq+#lgbtqi+#lgbtqia+#trans#trans healthcare#ftnb#female to male#ftm butch#transmasc butch#gender transition#gender affirming surgery#gender affirmation
213 notes
·
View notes
Text
By: Andy L.
Published: Apr 14, 2024
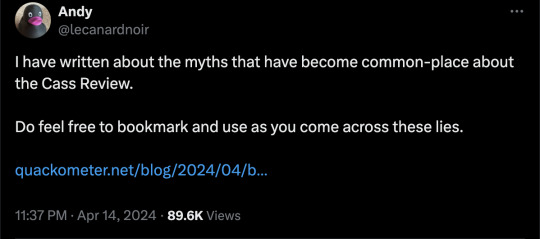
It has now been just little under a week since the publication of the long anticipated NHS independent review of gender identity services for children and young people, the Cass Review.
The review recommends sweeping changes to child services in the NHS, not least the abandonment of what is known as the “affirmation model” and the associated use of puberty blockers and, later, cross-sex hormones. The evidence base could not support the use of such drastic treatments, and this approach was failing to address the complexities of health problems in such children.
Many trans advocacy groups appear to be cautiously welcoming these recommendations. However, there are many who are not and have quickly tried to condemn the review. Within almost hours, “press releases“, tweets and commentaries tried to rubbish the report and included statements that were simply not true. An angry letter from many “academics”, including Andrew Wakefield, has been published. These myths have been subsequently spreading like wildfire.
Here I wish to tackle some of those myths and misrepresentations.
-
Myth 1: 98% of all studies in this area were ignored
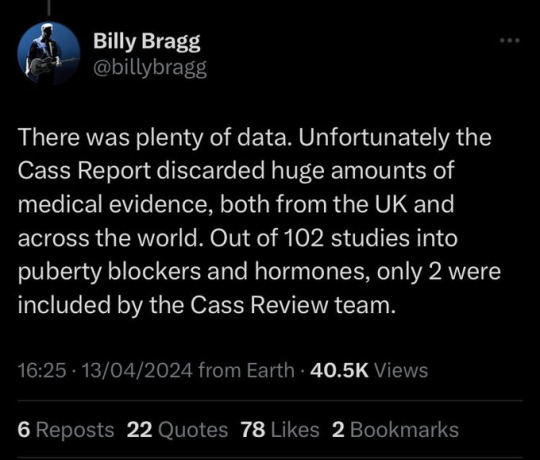
Fact
A comprehensive search was performed for all studies addressing the clinical questions under investigation, and over 100 were discovered. All these studies were evaluated for their quality and risk of bias. Only 2% of the studies met the criteria for the highest quality rating, but all high and medium quality (50%+) studies were further analysed to synthesise overall conclusions.
Explanation
The Cass Review aimed to base its recommendations on the comprehensive body of evidence available. While individual studies may demonstrate positive outcomes for the use of puberty blockers and cross-sex hormones in children, the quality of these studies may vary. Therefore, the review sought to assess not only the findings of each study but also the reliability of those findings.
Studies exhibit variability in quality. Quality impacts the reliability of any conclusions that can be drawn. Some may have small sample sizes, while others may involve cohorts that differ from the target patient population. For instance, if a study primarily involves men in their 30s, their experiences may differ significantly from those of teenage girls, who constitute the a primary patient group of interest. Numerous factors can contribute to poor study quality.
Bias is also a big factor. Many people view claims of a biased study as meaning the researchers had ideological or predetermined goals and so might misrepresent their work. That may be true. But that is not what bias means when we evaluate medical trials.
In this case we are interested in statistical bias. This is where the numbers can mislead us in some way. For example, if your study started with lots of patients but many dropped out then statistical bias may creep in as your drop-outs might be the ones with the worst experiences. Your study patients are not on average like all the possible patients.
If then we want to look at a lot papers to find out if a treatment works, we want to be sure that we pay much more attention to those papers that look like they may have less risk of bias or quality issues. The poor quality papers may have positive results that are due to poor study design or execution and not because the treatment works.
The Cass Review team commissioned researchers at York University to search for all relevant papers on childhood use of puberty blockers and cross-sex hormones for treating “gender dysphoria”. The researchers then graded each paper by established methods to determine quality, and then disregarded all low quality papers to help ensure they did not mislead.
The Review states,
The systematic review on interventions to suppress puberty (Taylor et al: Puberty suppression) provides an update to the NICE review (2020a). It identified 50 studies looking at different aspects of gender-related, psychosocial, physiological and cognitive outcomes of puberty suppression. Quality was assessed on a standardised scale. There was one high quality study, 25 moderate quality studies and 24 low quality studies. The low quality studies were excluded from the synthesis of results.
As can be seen, the conclusions that were based on the synthesis of studies only rejected 24 out of 50 studies – less than half. The myth has arisen that the synthesis only included the one high quality study. That is simply untrue.
There were two such literature reviews: the other was for cross-sex hormones. This study found 19 out of 53 studies were low quality and so were not used in synthesis. Only one study was classed as high quality – the rest medium quality and so were used in the analysis.
12 cohort, 9 cross-sectional and 32 pre–post studies were included (n=53). One cohort study was high-quality. Other studies were moderate (n=33) and low-quality (n=19). Synthesis of high and moderate-quality studies showed consistent evidence demonstrating induction of puberty, although with varying feminising/masculinising effects. There was limited evidence regarding gender dysphoria, body satisfaction, psychosocial and cognitive outcomes, and fertility.
Again, it is myth that 98% of studies were discarded. The truth is that over a hundred studies were read and appraised. About half of them were graded to be of too poor quality to reliably include in a synthesis of all the evidence. if you include low quality evidence, your over-all conclusions can be at risk from results that are very unreliable. As they say – GIGO – Garbage In Garbage Out.
Nonetheless, despite analysing the higher quality studies, there was no clear evidence that emerged that puberty blockers and cross-sex hormones were safe and effective. The BMJ editorial summed this up perfectly,
One emerging criticism of the Cass review is that it set the methodological bar too high for research to be included in its analysis and discarded too many studies on the basis of quality. In fact, the reality is different: studies in gender medicine fall woefully short in terms of methodological rigour; the methodological bar for gender medicine studies was set too low, generating research findings that are therefore hard to interpret. The methodological quality of research matters because a drug efficacy study in humans with an inappropriate or no control group is a potential breach of research ethics. Offering treatments without an adequate understanding of benefits and harms is unethical. All of this matters even more when the treatments are not trivial; puberty blockers and hormone therapies are major, life altering interventions. Yet this inconclusive and unacceptable evidence base was used to inform influential clinical guidelines, such as those of the World Professional Association for Transgender Health (WPATH), which themselves were cascaded into the development of subsequent guidelines internationally.
-
Myth 2: Cass recommended no Trans Healthcare for Under 25s
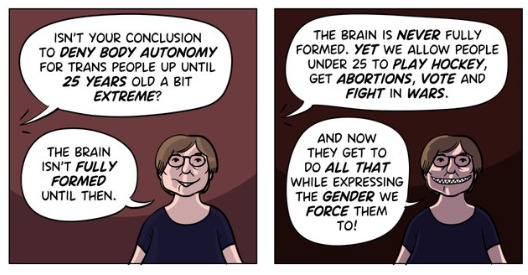
Fact
The Cass Review does not contain any recommendation or suggestion advocating for the withholding of transgender healthcare until the age of 25, nor does it propose a prohibition on individuals transitioning.
Explanation
This myth appears to be a misreading of one of the recommendations.
The Cass Review expressed concerns regarding the necessity for children to transition to adult service provision at the age of 18, a critical phase in their development and potential treatment. Children were deemed particularly vulnerable during this period, facing potential discontinuity of care as they transitioned to other clinics and care providers. Furthermore, the transition made follow-up of patients more challenging.
Cass then says,
Taking account of all the above issues, a follow-through service continuing up to age 25 would remove the need for transition at this vulnerable time and benefit both this younger population and the adult population. This will have the added benefit in the longer-term of also increasing the capacity of adult provision across the country as more gender services are established.
Cass want to set up continuity of service provision by ensure they remain within the same clinical setting and with the same care providers until they are 25. This says nothing about withdrawing any form of treatment that may be appropriate in the adult care pathway. Cass is explicit in saying her report is making no recommendations as to what that care should look like for over 18s.
It looks the myth has arisen from a bizarre misreading of the phrase “remove the need for transition”. Activists appear to think this means that there should be no “gender transition” whereas it is obvious this is referring to “care transition”.
-
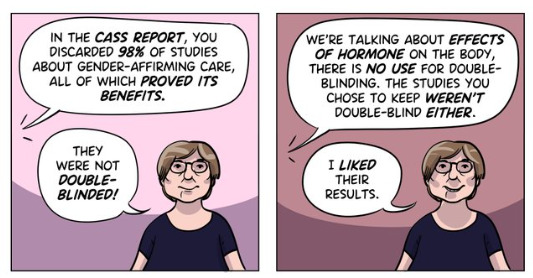
Myth 3: Cass is demanding only Double Blind Randomised Controlled Trials be used as evidence in “Trans Healthcare”
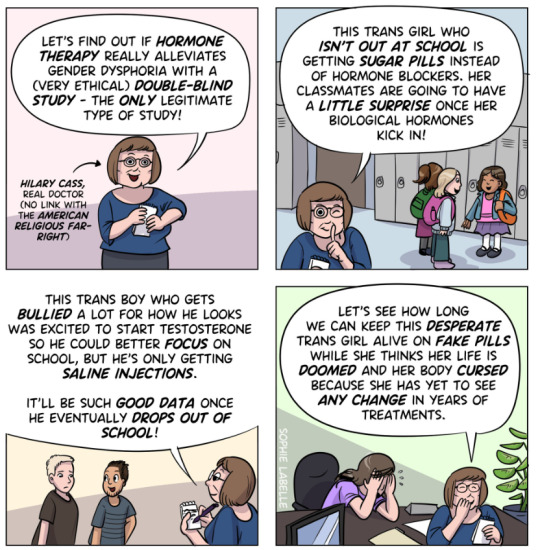
Fact
While it is acknowledged that conducting double-blind randomized controlled trials (DBRCT) for puberty blockers in children would present significant ethical and practical challenges, the Cass Review does not advocate solely for the use of DBRCT trials in making treatment recommendations, nor does it mandate that future trials adhere strictly to such protocols. Rather, the review extensively discusses the necessity for appropriate trial designs that are both ethical and practical, emphasizing the importance of maintaining high methodological quality.
Explanation
Cass goes into great detail explaining the nature of clinical evidence and how that can vary in quality depending on the trial design and how it is implemented and analysed. She sets out why Double Blind Randomised Controlled Trials are the ‘gold standard’ as they minimise the risks of confounding factors misleading you and helping to understand cause and effect, for example. (See Explanatory Box 1 in the Report).
Doctors rely on evidence to guide treatment decisions, which can be discussed with patients to facilitate informed choices considering the known benefits and risks of proposed treatments.
Evidence can range from a doctor’s personal experience to more formal sources. For instance, a doctor may draw on their own extensive experience treating patients, known as ‘Expert Opinion.’ While valuable, this method isn’t foolproof, as historical inaccuracies in medical beliefs have shown.
Consulting other doctors’ experiences, especially if documented in published case reports, can offer additional insight. However, these reports have limitations, such as their inability to establish causality between treatment and outcome. For example, if a patient with a bad back improves after swimming, it’s uncertain whether swimming directly caused the improvement or if the back would have healed naturally.
Further up the hierarchy of clinical evidence are papers that examine cohorts of patients, typically involving multiple case studies with statistical analysis. While offering better evidence, they still have potential biases and limitations.
This illustrates the ‘pyramid of clinical evidence,’ which categorises different types of evidence based on their quality and reliability in informing treatment decisions

The above diagram is published in the Cass Review as part of Explanatory Box 1.
We can see from the report and papers that Cass did not insist that only randomised controlled trials were used to assess the evidence. The York team that conducted the analyses chose a method to asses the quality of studies called the Newcastle Ottawa Scale. This is a method best suited for non RCT trials. Cass has selected an assessment method best suited for the nature of the available evidence rather than taken a dogmatic approach on the need for DBRCTs. The results of this method were discussed about countering Myth 1.
Explainer on the Newcastle Ottawa Scale
The Newcastle-Ottawa Scale (NOS) is a tool designed to assess the quality of non-randomized studies, particularly observational studies such as cohort and case-control studies. It provides a structured method for evaluating the risk of bias in these types of studies and has become widely used in systematic reviews and meta-analyses.
The NOS consists of a set of criteria grouped into three main categories: selection of study groups, comparability of groups, and ascertainment of either the exposure or outcome of interest. Each category contains several items, and each item is scored based on predefined criteria. The total score indicates the overall quality of the study, with higher scores indicating lower risk of bias.
This scale is best applied when conducting systematic reviews or meta-analyses that include non-randomized studies. By using the NOS, researchers can objectively assess the quality of each study included in their review, allowing them to weigh the evidence appropriately and draw more reliable conclusions.
One of the strengths of the NOS is its flexibility and simplicity. It provides a standardized framework for evaluating study quality, yet it can be adapted to different study designs and research questions. Additionally, the NOS emphasizes key methodological aspects that are crucial for reducing bias in observational studies, such as appropriate selection of study participants and controlling for confounding factors.
Another advantage of the NOS is its widespread use and acceptance in the research community. Many systematic reviews and meta-analyses rely on the NOS to assess the quality of included studies, making it easier for researchers to compare and interpret findings across different studies.
As for future studies, Cass makes no demand only DBRCTs are conducted. What is highlighted is at the very least that service providers build a research capacity to fill in the evidence gaps.
The national infrastructure should be put in place to manage data collection and audit and this should be used to drive continuous quality improvement and research in an active learning environment.
-
Myth 4: There were less than 10 detransitioners out of 3499 patients in the Cass study.

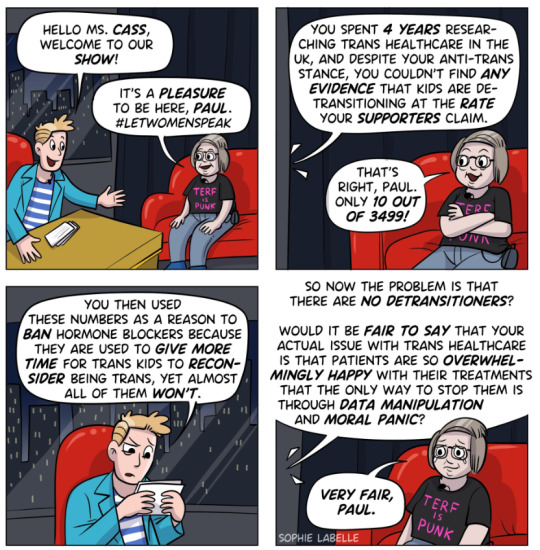
Fact
Cass was unable to determine the detransition rate. Although the GIDS audit study recorded fewer than 10 detransitioners, clinics declined to provide information to the review that would have enabled linking a child’s treatment to their adult outcome. The low recorded rates must be due in part to insufficient data availability.
Explanation
Cass says, “The percentage of people treated with hormones who subsequently detransition remains unknown due to the lack of long-term follow-up studies, although there is suggestion that numbers are increasing.”
The reported number are going to be low for a number of reasons, as Cass describes:
Estimates of the percentage of individuals who embark on a medical pathway and subsequently have regrets or detransition are hard to determine from GDC clinic data alone.
There are several reasons for this:
Damningly, Cass describes the attempt by the review to establish “data linkage’ between records at the childhood gender clinics and adult services to look at longer term detransition and the clinics refused to cooperate with the Independent Review. The report notes the “…attempts to improve the evidence base have been thwarted by a lack of cooperation from the adult gender services”.
We know from other analyses of the data on detransitioning that the quality of data is exceptionally poor and the actual rates of detransition and regret are unknown. This is especially worrying when older data, such as reported in WPATH 7, suggest natural rates of decrease in dysphoria without treatment are very high.
Gender dysphoria during childhood does not inevitably continue into adulthood. Rather, in follow-up studies of prepubertal children (mainly boys) who were referred to clinics for assessment of gender dysphoria, the dysphoria persisted into adulthood for only 6–23% of children.
This suggests that active affirmative treatment may be locking in a trans identity into the majority of children who would otherwise desist with trans ideation and live unmedicated lives.
I shall add more myths as they become spread.
==
It's not so much "myths and misconceptions" as deliberate misinformation. Genderists are scrambling to prop up their faith-based beliefs the same way homeopaths do. Both are fraudulent.
#Andy L.#Cass Review#Cass Report#Dr. Hilary Cass#Hilary Cass#misinformation#myths#misconceptions#detrans#detransition#gender affirming healthcare#gender affirming care#gender affirmation#affirmation model#medical corruption#medical malpractice#medical scandal#systematic review#religion is a mental illness
311 notes
·
View notes
Text
The Northwest Territories government is promising residents, including youth and children, that they will continue to have access to gender-affirming care even if some services are no longer available in Alberta.
In a Monday press release, the territory’s Department of Health and Social Services said in cases where those services are not available in the NWT, health care providers can refer residents outside the territory. If a required service is not available in Alberta, the department said “alternative pathways for care” are in place elsewhere in Canada.
“All NWT residents have the right to respectful, dignified and culturally safe health care,” the release stated.
Full article
Tagging: @politicsofcanada
#cdnpoli#canada#canadian politics#canadian news#canadian#NWT#northwest territories#north-west territories#gender affirming care#gender affirming healthcare#healthcare
267 notes
·
View notes
Text
lemme get this straight... so trans people shouldn't be allowed gender affirming care and at best need to do gymnastics to "justify"why they should get hormone therapy... but a psychiatrist can put someone on a medication that was originally described as a "chemical lobotomy" (antipsychotics), after only talking to them once... whether they like it or not. oh and also they don't tell patients about the dangerous long term side effects of that. sounds great to me. there's totally nothing wrong with the health system and societal views towards marginalized people and autonomy.
#softspoonie#antipsych#antipsychiatry#transphobia#gaht#hrt#gender affirming care#gender affirming healthcare#healthcare#psychiatry#ableism#sanism#trans#disabled#disability#mentally ill#mental illness#bodily autonomy#body autonomy#informed consent#us healthcare#american healthcare#systemic injustive#systemic ableism
177 notes
·
View notes
Text
Trudy Ring at The Advocate:
Planned Parenthood must turn over some records on transgender health care to Missouri Attorney General Andrew Bailey, a judge has ruled.
Bailey, a Republican, is investigating providers of gender-affirming care in the state, which has outlawed the provision of such care to minors and certain adults. His demand for information from Planned Parenthood of the St. Louis Region and Southwest Missouri came in March 2023 as part of his investigation of whether Washington University’s Pediatric Transgender Center or other health care entities in Missouri “have engaged in or are engaging in any practices declared to be unlawful,” as he stated in a letter to Planned Parenthood.
The Planned Parenthood affiliate then sued Bailey in an attempt to block his demand, saying it was unauthorized and that the attorney general hadn’t shown how Planned Parenthood is directly involved in his investigation. Bailey argued that his request “should stand because he has an affidavit that alleges intentional dishonesty in Plaintiff's medical and billing practices,” St. Louis Circuit Judge Michael Stelzer wrote in his ruling.
Ruling in Bailey’s favor, Stelzer said the AG’s office has “broad investigative powers” and that Bailey has the right to obtain any documents that aren’t protected by the federal Health Insurance Portability and Accountability Act, which provides for patient privacy.
Missouri AG Andrew Bailey (R) has been granted snooping powers on Planned Parenthood of St. Louis Region and Southwest Missouri's records for transgender health services.
#Missouri#Planned Parenthood#Andrew Bailey#Gender Affirming Healthcare#Transgender#Michael Stelzer#HIPAA#Planned Parenthood of the St. Louis Region and Southwest Missouri#Washington University
56 notes
·
View notes