#psychological disorders
Text
Happy Disability Pride Month!
In honor of the shift from LGBTQ Pride Month to Disability Pride Month, I’m going to bring awareness to some underrepresented and underinformed disabilities as a queer and disabled artist/writer. These are all disorders that I have come across among friends and acquaintances. Every disorder I discuss must have a clinical diagnosis in order to be treated. You should only be self-diagnosing if you plan on going to a doctor to confirm your speculations. Do not self-diagnose if you are not willing to confirm with a medical professional. This post is not to diagnose you.
Big Trigger Warning: Discussions of psychological disorders like E/Ds, depression, and personality disorders.
Dysautonomia
Any disorder relating to the autonomic (involuntary) nervous system
POTS
I have this! It is a nervous system disorder that affects heart rate and blood pressure because your nervous system does not allow your muscles to properly circulate blood, especially through the legs. Some symptoms include elevated heart rate, chest pain, low or high blood pressure, fatigue, changes in body temperature, and dizziness or fainting. POTS is more common in AFAB people than AMAB.
Amyloidosis
Amyloidosis is a disorder that occurs when a protein known as amyloid builds up in the organs. Amyloidosis is closely related to dysautonomia and chronic pain syndromes such as Ehlers-Danlos Syndrome because of the comorbid symptoms. These symptoms include edema, purpura around the eyes, skin that bruises easily, and fatigue.
Frey’s Syndrome
A neurological disorder closely related to dysautonomia that causes excessive sweating while eating. There are very few solutions to this disorder and even fewer of them are known to work.
Mitochondrial Syndrome
Mitochondrial diseases occur when there are genetic mutations and deformations to the mitochondria in cells that directly influence how the organelle produces energy. People with mitochondrial diseases can have poor growth, muscle weakness, seizures, visual and / or hearing problems, learning disabilities, and may develop kidney, liver, or heart disease.
Autonomic Dysreflexia
Autonomic dysreflexia is a disorder that causes abnormal overreactions of the autonomic nervous system. Symptoms include elevated heart rate, excessive sweating, and high blood pressure.
Chronic Pain
Any disorder relating to long-lasting pain surrounding any part of the body.
Patellofemoral Pain Syndrome
I have this one too! Patellofemoral pain syndrome is a chronic pain syndrome in which muscles in the lower extremities are too weak to support patellar (kneecap) movement. Thus, the patella (kneecap) will not track right. this causes lots of issues with walking.
Scoliosis
I also have this one! Scoliosis is defined as a physical disorder in which the spine is not a straight vertical line. There is either an “S” or “J” curve in the spine, compressing it and causing sharp or aching back pain.
Temporomandibular Joint Dysfunction
TMJ causes pain and tenderness in jaw joints and surrounding muscles and ligaments. Symptoms of TMJ include jaw stiffness, limited movement and locking of the jaw, ringing in ears, and dizziness.
Myofascial Pain Syndrome
This is a chronic muscular pain disorder. Typically, this pain is confined to one specific area, such as the neck or shoulders.
Fibromyalgia
A chronic disorder that causes pain and tenderness throughout the body, as well as fatigue. People with fibromyalgia can also have depression, anxiety, and trouble with memory and concentration.
Ehlers-Danlos Syndrome
EDS is a group of disorders that affect connective tissues that support the skin, bones, blood vessels, organs, and other tissues. Symptoms of EDS include stretchy, translucent skin, loose joints, and chronic pain.
Arthritis
Arthritis is defined as inflammation in one or more joints causing stiffness and pain. There are many different kinds of arthritis, each with different causes. These causes can include wear over time, infections, and underlying diseases.
Neurological Disorders
Any disorder relating to the brain and how it functions.
Seizure Disorders
Epilepsy
Epilepsy is a disorder of the brain characterized by repeated seizures. People with epilepsy can experience multiple kinds of seizures and can experience symptoms such as confusion, staring spells, stiff muscles, and loss of consciousness.
Cerebrovascular Diseases
Functional Neurological Disorder
Functional Neurological Disorder is essentially a stroke mimic. It can replicate the symptoms of a stroke, such as limb weakness, numbness, and speech disturbance.
Migraines
Lots of people have migraines and I am no exception. Migraines are caused by excessive blood flow to the brain. Migraines affect more than 10% of people worldwide and are 3 times more likely to affect AFAB people than AMAB people.
Psychological Disorders
Any disorders affecting mood, thinking, and behavior. I will not be discussing my mental disorders on the internet. Most people are familiar with what these are and what they look like, so I will instead be providing statistics for each one.
Anxiety Disorders
Generalized Anxiety Disorder (GAD) affects 6.8 million adults. Only 43.2% of those adults are receiving treatment. AFAB are twice as likely to be affected (Anxiety Disorders Association of America).
Panic disorder (PD) affects 6 million adults. AFAB are twice as likely to be affected (Anxiety Disorders Association of America) .
Obsessive-Compulsive Disorder (OCD) affects 2.5 million adults. AFAB are 3x more likely to be affected (Anxiety Disorders Association of America) .
Post-Traumatic Stress Disorder (PTSD) affects 7.7 million adults. AFAB are 5x more likely to be affected (Anxiety Disorders Association of America) .
Depression
Approximately 280 million people in the world have depression. AFAB are twice as likely to develop depression (World Health Organization).
Bipolar Disorder
4.4% of US adults experience bipolar disorder in their lives (National Institute of Health).
Personality Disorders
It is estimated that 9% of US adults have at least one personality disorder (American Psychiatric Association).
Eating Disorders (TW)
Eating Disorders affect 9% of the population worldwide (National Association of Anorexia Nervosa and Associated Disorders).
BIPOC are significantly less likely than white people to be asked by a doctor about eating disorder symptoms (National Association of Anorexia Nervosa and Associated Disorders).
Black teenagers are 50% more likely than white teenagers to exhibit bulimic behaviors (National Association of Anorexia Nervosa and Associated Disorders).
Rates of body dissatisfaction were higher among transgender and nonbinary youth (90%) compared to cisgender youth (80%) (National Association of Anorexia Nervosa and Associated Disorders).
#disability pride month#disability awareness#disability#dysautonomia#pots#chronic pain#neurological disorder#psychological disorders
15 notes
·
View notes
Text
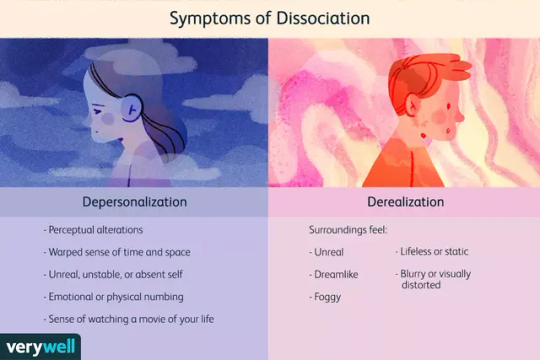
Image created by Theresa Chiechi (I think)
4 notes
·
View notes
Text
Having a psychologically induced physical disability be like “sorry I can’t walk right now I’m sad.” And it’s completely unexaggerated and literal.
I’ve been in therapy for ten years, and have been inpatient, iop, and partial hospitals. I was taught unresolved trauma and stress can cause like. Stomach and heart issues, migraines.
No one ever told me whatever the actual duck THIS is could happen. Like yeah, my new normal is that crying and panic attacks and triggers make me jerk around involuntarily until I’m catatonic. Is that. How does. PLEASE TELL ME I’M NOT CASE 0 FOR THIS??? MY DOCTORS ARE SO CONFUSED BUT APPARENTLY ACCORDING TO PSYCHOLOGY PROFESSIONALS ‘YEAH, PSYCH DISORDERS CAN CAUSE THIS.’ While also seeming confused. I am baffled myself. Like huh???
#mental illness#physically disabled#psychological disorders#mobility aid user#what even#involuntary movement disorder#neurodivergent#young disabled#anxiety#depression#medical trauma#psychological trauma#chronic fatigue#mobility issues#tw psych ward#catatonia
3 notes
·
View notes
Text

#studyblr#notes#medblr#medical notes#med notes#psychology#psychology notes#psych#psych notes#psychiatry#psychiatry notes#neurology#neurology notes#neuro#neuro notes#alertness#alert state#brainstem#brain stem#psychological disorders#diseases and disorders
8 notes
·
View notes
Text
By: Jason L. Riley
Published: Dec 12, 2023
A decade ago, New York City launched a campaign to combat teen pregnancy. It featured ads on buses and subway cars that read: “If you finish high school, get a job, and get married before having children, you have a 98% chance of not being in poverty.”
That advice, more popularly known as the “success sequence,” is often credited to research done by Brookings Institution scholars Isabel Sawhill and Ron Haskins, though others have made similar observations. In his recent book, “Agency,” Ian Rowe of the American Enterprise Institute writes that the message “has attracted many admirers because of the simplicity of the three steps that young people, even if born into disadvantaged circumstances or raised by a young single parent, can themselves control and take in their lives.”
The effort nevertheless faced significant backlash from detractors who accused then-Mayor Michael Bloomberg of stigmatizing teen pregnancy and pushing a “moralistic, conservative agenda to revitalize marriage,” Mr. Rowe writes. Mr. Bloomberg’s successor, Bill de Blasio, ultimately abandoned the effort. Public moralizing has since fallen further out of favor and been replaced by a kind of self-congratulatory nonjudgmentalism. In today’s New York, you’re likely to see ads for free syringes and directions to “safe” injections sites for junkies, even as drug overdoses have reached record levels.
We could use more of that moralizing from public officials, whether the issue is solo parenting, substance abuse or crime. The success sequence works to keep people not only off the dole but also out of trouble with the law. High-school graduates and children raised by both parents are much less likely to end up in jail. “Virtually every major social pathology,” political scientist Stephen Baskerville writes, “has been linked to fatherless children: violent crime, drug and alcohol abuse, truancy, unwed pregnancy, suicide, and psychological disorders—all correlating more strongly with fatherlessness than with any other single factor, surpassing even race and poverty.”
America’s crime debate tends to focus on so-called root causes, such as joblessness. But it’s worth remembering that the sharpest increase in violent crime began in the 1960s, a decade that saw low unemployment, strong economic growth and a doubling of black household incomes. As notable, labor-force participation rates of young black men fell during the 1980s and ’90s, one of the longest periods of sustained economic growth in U.S. history.
A new academic paper from the Institute for Family Studies doesn’t deny that economic conditions play a role in criminal behavior. And co-authors Rafael Mangual, Brad Wilcox, Joseph Price and Seth Cannon write that “changes in law-enforcement and the prosecution of criminals have also had a hand in the recent uptick in violent crime in American cities.” The paper’s main argument, however, is that family instability may be the biggest factor of all and that it’s not receiving the attention it deserves.
“Cities are safer when two-parent families are dominant and more crime-ridden when family instability is common,” the authors write. Nationwide, the total crime rate is about 48% higher in cities “that have above the median share of single-parent families, compared to cities that have fewer single-parent families.” Even when controlling for variables such as race, income and educational attainment, “the association between family structure and total crime rates, as well as violent crime rates, in cities across the United States remains statistically significant.”
Having a father around, the authors note, is about more than an additional paycheck. Fathers teach their sons responsibility, self-control, how to carry themselves, how to treat women. They tend to be more effective disciplinarians, and their involvement in childrearing is linked to positive outcomes in the academic development of their children, “especially in mathematics and verbal skills.” That finding “has been established for both sons and daughters but, unsurprisingly, it is especially pronounced among boys. The presence of married fathers is also protective against school suspensions and expulsions, as well as the risk of dropping out of high school.”
Between 1960 and 2019, the percentage of babies in the U.S. born to unwed mothers grew from 5% to almost 50%. “Shifts from the late-1960s to the 1990s away from stable families have left some cities, and especially some neighborhoods, vulnerable to higher rates of crime, especially violent crime,” the study concludes. “We need to realign material and cultural incentives in our cities to favor marriage and stable families, not undercut them.”
We all know single mothers—some of us even may be related to them—who heroically beat these odds and raised children that have gone on to lead productive lives. The public-policy goal should be to reduce the number of people who will have to face those odds. And that means calling out behavior that is objectively harmful to people and society in general.
--
Study: Stronger Families, Safer Streets: Exploring Links Between Family Structure and Crime
Executive Summary
This Institute for Family Studies report finds that strong families are associated with less crime in cities across the United States, as well in neighborhoods across Chicago. Specifically, our analyses indicate that the total crime rate in cities with high levels of single parenthood are 48% higher than those with low levels of single parenthood. When it comes to violent crime and homicide, cities with high levels of single parenthood have 118% higher rates of violence and 255% higher rates of homicide. And in Chicago, our analysis of census tract data from the city shows that tracts with high levels of single-parent-headed households face 137% higher total crime rates, 226% higher violent crime rates, and 436% higher homicide rates, compared to tracts with low levels of single parenthood. We also find that poverty, education, and race are linked to city and census-tract level trends in crime. In general, in cities across America, and on the streets of Chicago, this report finds that public safety is greater in communities where the twoparent family is the dominant norm.
==
Not everything needs to be normalized or destigmatized.
The problem with the discussion around addressing social issues is that many people only want to do the politically virtuous thing, not the harder, more politically difficult thing. They want to shout, "defund the police!" But they don't want to do anything that would actually facilitate a reduction in the need for police.
What this tells us is that they don't really care about actually solving it, they just want to be seen to care about it. Indeed, if it was resolved, it would be politically inconvenient, as they'd no longer be able to posture around it.
#Jason L. Riley#fatherlessness#success sequence#crime#violent crime#homicide#crime rate#teen pregnancy#drug abuse#alcohol abuse#truancy#suicide#psychological disorders#social pathology#law enforcement#religion is a mental illness
6 notes
·
View notes
Text
New vocabulary word: Schadenfreude
Definition: the experience of pleasure, joy, or self-satisfaction that comes from learning of or witnessing the troubles, failures, or humiliation of another.
It is a borrowed word from German, with no direct translation, that originated in the 18th century. Schadenfreude has been detected in children as young as 24 months and may be an important social emotion establishing "inequity aversion".
"To envy is human, to savor schadenfrude is devilish." -Arthur Schopenhauer
2 notes
·
View notes
Text
Three friends who can never be best friends
Life and pain go hand in hand and normally so does happiness, I mean we have two hands. Sometimes it’s like we like to play favorites and become best friends with one of them. If we do it consciously or subconsciously I guess is based on life experiences and choices we make. In my case I became best friends with the wrong one. I feel one needs to become friends with both of them to have a…
View On WordPress
#battling bad thoughts#Borderline personality disorder#Comfort#Comfort zone#experiences#Fear#feelings#Future#Happiness#inner calm#journey#Life#Living with BPD#Mental Health#Mindful#negativity#Open minded#pain#psychological disorders#reflection#self exploration#Self worth#Though#thoughts#writing
0 notes
Text
Erectile Dysfunction: What You Need to Know
"It's shocking what erectile dysfunction can indicate.
What is Erectile Dysfunction?
Erectile dysfunction is a condition where a man has trouble getting or keeping an erection. It can happen to people of all ages, not just older men. Some experts believe that lifestyle factors like stress and lack of physical activity can contribute to this problem.
Causes of Erectile Dysfunction
Erectile dysfunction can be caused by many things. It’s a complex…

View On WordPress
#a healthier lifestyle#Address psychological issues#Atherosclerosis#Burnout#Causes#Certain medications#complex issue#Constant stress#Diagnosis and Treatment#Eat a balanced diet#Erectile Dysfunction#Improper lifestyle#Myths About Erectile Dysfunction Drugs#Other health conditions#Overwork#Psychological disorders#psychological factors#Quit smoking#Quit smoking and limit alcohol consumption#Seek Help#Stay physically active#the body
0 notes
Text
The importance of mental health and its impact on activity and life
#mental health#health#mental health awareness#mental health tips#how to improve mental health#improve mental health#psychological health#world mental health day#mental health education#[ health#mental health crisis#health psychologist#health psychology#mental health matters#mental health problems#health tips#improving mental health tips#mental health awareness month#healthy habits#psychological disorders#mental health terminology#child mental health
1 note
·
View note
Text
Mental Health Disorders: the Real Struggles Faced by Individuals
I would like to engage in a conversation about a matter that holds great importance to me – mental health disorders. You have probably encountered numerous discussions on this topic, but do you truly comprehend the lived experience? It extends beyond mere feelings of sadness or worry; it entails intricate complexities and formidable obstacles.
Unraveling Mental Health Disorders
First and…

View On WordPress
#anxiety#Bipolar disorder#depression#emotional wellness#Health#healthcare accessibility#Mental disorder#mental disorders#Mental Health#mental health advocacy#mental health apps#mental health care#mental health education#mental health stigma#mental health support#mental health treatment#mental illness#mental illness awareness#psychological disorders#Schizophrenia#teletherapy#therapy#workplace mental health
0 notes
Text
I talk to many people who say things like "oh I have trauma but I don't have PTSD", but then when I talk to them a little more I realize that they most likely do, they just can't recognize it as such due to how lacking PTSD awareness is, even beyond the whole "it's not just a veteran's disorder" thing.
The main reason they think they don't have PTSD usually has to do with flashbacks and nightmares, either they have one but not the other or have neither. But here's the thing, those are only two symptoms out of the 23-odd recognized symptoms. Flashbacks and nightmares are two of the five symptoms under Criterion B (Intrusion), which you only need one of for a diagnosis. The other three symptoms are unwanted upsetting memories, emotional distress after being reminded of trauma and physical reactivity after being reminded of trauma (i.e. shaking, sweating, heart racing, feeling sick, nauseous or faint, etc). Therefore you can have both flashbacks and nightmares, one but not the other, or neither and still have PTSD.
In fact, a lot of the reasons people give me for why they don't think they have PTSD are literally a part of the diagnostic criteria.
"Oh, I can barely remember most parts of my trauma anyway." Criterion D (Negative Alterations in Cognition and Mood) includes inability to recall key features of the trauma.
"Oh but I don't get upset about my trauma that often because I avoid thinking of it or being around things that remind me of it most of the time." Criterion C (Avoidance) includes avoiding trauma-related thoughts or feelings and avoiding trauma-related external reminders, and you literally cannot get diagnosed if you don't have at least one of those two symptoms.
"Oh I just have trouble getting to sleep or staying asleep, but I don't have nightmares." Criterion E (Alterations in Arousal and Reactivity) includes difficulting sleeping outside of nightmares.
"But I didn't have many/any trauma symptoms until a long time after the trauma happened." There's literally an entire specification for that.
Really it just shows how despite being one of the most well-known mental illnesses, people really don't know much about PTSD. If you have trauma, I ask you to at least look at the criteria before you decide you don't have PTSD. Hell, even if you don't have trauma, look at the criteria anyway because there are so many symptoms in there that just are not talked about.
PTSD awareness is not just about flashbacks and nightmares.
#ptsd#post traumatic stress disorder#cptsd#complex post traumatic stress disorder#complex ptsd#trauma#actually ptsd#actually cptsd#mental illness#mental health#mental health awareness#ptsd awareness#cptsd awareness#neurodivergent#ptsd thoughts#awareness#important#mentally ill#actually mentally ill#psychology
47K notes
·
View notes
Text

#aspd thoughts#aspd feels#aspd things#actually aspd#aspd traits#psychology#life quote#quotes#mental health#quoteoftheday#bipolar#bipolar girl#bipolar disorder#dark humor#dark#art
26K notes
·
View notes
Photo

New Post has been published on https://www.knewtoday.net/understanding-the-complex-emotions-experienced-by-individuals-with-schizophrenia/
Understanding the Complex Emotions Experienced by Individuals with Schizophrenia

Schizophrenia is a mental disorder that profoundly affects the thoughts, emotions, and behaviors of individuals who experience it. Beyond the commonly known symptoms such as hallucinations and delusions, the emotional landscape of schizophrenia is equally complex and nuanced. Exploring the feelings and emotional experiences of individuals with schizophrenia is crucial for developing a comprehensive understanding of the disorder and providing effective support and treatment.
In this article, we delve into the multifaceted emotions that individuals with schizophrenia may encounter. By shedding light on these emotional experiences, we aim to increase awareness, reduce stigma, and promote empathy toward those living with schizophrenia.
Understanding the emotional dimension of schizophrenia goes beyond recognizing its impact on daily life; it also encompasses the inner world of individuals with the disorder. Through an exploration of the various emotional states they experience, we can gain insight into their struggles, resilience, and unique perspectives.
We will examine the common emotional manifestations of schizophrenia, including the challenges individuals face in processing and expressing emotions. Additionally, we will explore the impact of social isolation, anxiety, and depression, which often coexist with schizophrenia, further complicating the emotional well-being of affected individuals.
By recognizing and validating the emotions experienced by those with schizophrenia, we can foster a more compassionate and inclusive society. Moreover, understanding the emotional underpinnings of the disorder can contribute to the development of tailored interventions that address the specific emotional needs of individuals with schizophrenia.
While the specific experiences and symptoms can vary among individuals, here are some details about the feelings that individuals with schizophrenia may commonly experience:
Delusions: People with schizophrenia often have persistent false beliefs, known as delusions. These delusions can be paranoid in nature, leading the individual to believe that others are plotting against them or that they are being watched or controlled by external forces.
Hallucinations: Schizophrenia may involve hallucinations, which are sensory experiences that are not based on reality. Auditory hallucinations, such as hearing voices or sounds, are the most common. These voices may be critical, commanding, or conversational. Visual hallucinations and other sensory distortions can also occur.
Disorganized thinking: Individuals with schizophrenia may experience disorganized thinking, which can make it difficult for them to process information, follow a conversation, or express their thoughts coherently. Their speech may become disorganized, fragmented, or tangential, making it challenging for others to understand them.
Emotional difficulties: Schizophrenia can significantly impact a person’s emotional experiences. Some individuals may exhibit a flattened or blunted affect, where their emotional expression becomes limited, and they may appear emotionally unresponsive. Others may experience heightened emotions or inappropriate emotional responses to situations.
Social withdrawal: Many individuals with schizophrenia experience social withdrawal or isolation due to their symptoms. They may struggle with communication, experience paranoia or anxiety in social situations, or fear judgment or persecution by others.
Anxiety and depression: Schizophrenia often co-occurs with other mental health conditions, such as anxiety disorders or depression. These comorbid conditions can intensify feelings of distress, hopelessness, and fear, further impacting the emotional well-being of individuals with schizophrenia.
Lack of insight: A characteristic feature of schizophrenia is a reduced ability to recognize or acknowledge that one’s thoughts, perceptions, or experiences are abnormal. This lack of insight, known as anosognosia, can make it challenging for individuals to understand the impact of their symptoms and seek appropriate treatment.
It’s important to note that the experiences and feelings of individuals with schizophrenia can vary widely. Some individuals may have periods of stability where their symptoms are manageable, while others may experience more severe and persistent symptoms. Treatment for schizophrenia often involves a combination of medication, therapy, and support from healthcare professionals and loved ones.
Delusions
Delusions are a prominent symptom of schizophrenia and involve persistent false beliefs that are not based on reality. These beliefs are held strongly by individuals with schizophrenia, despite evidence or logic to the contrary. Here are some details about delusions:
Types of Delusions: Delusions can take various forms, but some common types include:
a. Persecutory delusions: These involve a belief that one is being harmed, harassed, or conspired against by others. The individual may think they are being followed, spied on, or that people are plotting to harm them.
b. Grandiose delusions: These delusions involve inflated beliefs about one’s own importance, power, knowledge, or identity. Individuals may believe they have special abilities, are famous, or have a special connection to a deity or prominent figure.
c. Referential delusions: This type of delusion involves the belief that neutral events or objects have a specific and personal meaning or significance. For example, a person may believe that certain gestures or words are directed at them personally.
d. Somatic delusions: Somatic delusions involve false beliefs about one’s body or bodily functions. Individuals may believe they have a severe illness or that their body is changing or being controlled by external forces.e. Erotomanic delusions: These delusions involve a belief that someone, usually of higher social status, is in love with the individual, even when there is no evidence to support such a relationship.
Impact on daily life: Delusions can significantly impact a person’s thoughts, emotions, and behaviors. They may cause distress, anxiety, and paranoia, leading individuals to alter their behaviors and routines to protect themselves from perceived threats. Delusions can also strain relationships, as individuals may become suspicious or confrontational toward others based on their false beliefs.
Lack of insight: One of the distinguishing features of delusions in schizophrenia is the reduced ability to recognize that the beliefs are not based in reality. This lack of insight, known as anosognosia, can make it challenging for individuals to accept or seek treatment for their delusions.
Treatment: Delusions in schizophrenia are typically addressed through a combination of medication, therapy, and support. Antipsychotic medications can help reduce the intensity and frequency of delusions. Cognitive-behavioral therapy (CBT) can also be beneficial in helping individuals challenge and modify their distorted beliefs. Additionally, support from healthcare professionals, family, and friends is crucial in providing a supportive and understanding environment for individuals with delusions.
It’s important to approach individuals with delusions with empathy, understanding, and respect. Engaging in open and non-judgmental communication can help build trust and support their well-being.
Hallucinations
Hallucinations are a common symptom experienced by individuals with schizophrenia. They involve perceiving sensory stimuli that are not actually present in the external environment. Here are some details about hallucinations:
Types of hallucinations: The most common type of hallucination in schizophrenia is auditory hallucinations, which involve hearing voices or sounds. These voices can be experienced as coming from inside the person’s head or as if they are external and distinct individuals. Other types of hallucinations that can occur include visual hallucinations (seeing things that are not there), tactile hallucinations (feeling sensations on the body in the absence of stimuli), olfactory hallucinations (smelling odors that are not present), and gustatory hallucinations (tasting things that are not there).
Characteristics of auditory hallucinations: Auditory hallucinations in schizophrenia often involve hearing voices that can be critical, commanding, conversational, or even narrating the person’s actions. The content of the voices can vary greatly, and individuals may perceive them as distinct personalities or entities. The experience of auditory hallucinations can be distressing and disruptive to daily life.
Impact on daily functioning: Hallucinations can have a significant impact on a person’s thoughts, emotions, and behaviors. They can be intrusive, making it difficult to concentrate, engage in conversations, or perform tasks. Individuals may struggle with distinguishing between hallucinations and reality, leading to confusion and disorientation. Hallucinations can also contribute to social withdrawal and isolation, as individuals may fear judgment or feel uncomfortable in social settings.
Emotional response: Hallucinations can evoke strong emotional responses in individuals with schizophrenia. The content of the hallucinations, especially auditory ones, can influence the person’s mood and feelings. The voices may be critical, hostile, or distressing, leading to increased anxiety, fear, or sadness. On the other hand, some individuals may have hallucinations that are more neutral or even comforting, providing a sense of companionship or support.
Treatment: The treatment of hallucinations in schizophrenia typically involves a combination of medication and therapy. Antipsychotic medications can help reduce the intensity and frequency of hallucinations. Therapy approaches such as cognitive-behavioral therapy (CBT) or specialized interventions like voice dialogue techniques can assist individuals in coping with and managing their hallucinations.
Coping strategies: Individuals with hallucinations may find certain coping strategies helpful in managing their experiences. These may include distracting themselves with engaging activities, practicing relaxation techniques, using grounding exercises to stay connected to reality, and seeking support from healthcare professionals or support groups.
Understanding and supporting individuals with hallucinations require empathy, patience, and non-judgmental attitudes. Creating a safe and supportive environment can help individuals navigate their hallucinatory experiences and improve their overall well-being.
Disorganized Thinking
Disorganized thinking, also known as formal thought disorder, is a common symptom of schizophrenia. It refers to difficulties in organizing and expressing thoughts in a coherent and logical manner. Here are some details about disorganized thinking:
Fragmented and tangential speech: Disorganized thinking often manifests in the way individuals speak. Their speech may be disorganized, fragmented, and difficult to follow. They may jump between unrelated topics or provide irrelevant or nonsensical answers to questions. This tangential speech pattern can make it challenging for others to understand their intended message.
Loose associations: Another characteristic of disorganized thinking is loose associations or “word salad.” This occurs when individuals make connections between words or ideas that appear unrelated or lack logical coherence. Their speech may include rapid shifts in topic or connections based on sounds, rhymes, or personal associations rather than logical connections.
Incoherence and neologisms: In severe cases, individuals with disorganized thinking may exhibit incoherent speech that is difficult to decipher. They may create new words (neologisms) or use words in unusual or idiosyncratic ways that are not understood by others.
Impaired concentration and attention: Disorganized thinking can lead to difficulties in concentrating and maintaining attention. Individuals may get easily distracted, have trouble following conversations or instructions, and struggle to focus on tasks or activities.
Disrupted thought processes: Disorganized thinking reflects a disruption in the normal thought processes that underlie logical reasoning and coherent communication. The underlying cognitive impairments can affect various aspects of thinking, including problem-solving, decision-making, and abstract reasoning.
Impact on daily functioning: Disorganized thinking can significantly impact an individual’s ability to communicate effectively, engage in meaningful conversations, and carry out tasks that require logical thought processes. It may also affect their social interactions, as others may find it challenging to understand and connect with individuals exhibiting disorganized thinking.
Treatment: Treatment for disorganized thinking in schizophrenia typically involves a combination of antipsychotic medication and therapy. Antipsychotic medications help reduce the severity of disorganized thinking and other symptoms of schizophrenia. Cognitive-behavioral therapy (CBT) and other psychosocial interventions can also be beneficial in improving communication skills, enhancing problem-solving abilities, and providing support for individuals with disorganized thinking.
Supportive environment: Creating a supportive and understanding environment is crucial for individuals with disorganized thinking. Patience, active listening, and providing structure and clarity in communication can help individuals feel validated and heard. Encouraging and assisting with the development of organizational and planning skills can also be beneficial.
Understanding the challenges associated with disorganized thinking can contribute to improved communication and support for individuals with schizophrenia. By promoting empathy and offering appropriate interventions, we can help individuals navigate their disorganized thinking and enhance their overall functioning.
Emotional Difficulties
Emotional difficulties are common among individuals with schizophrenia. These difficulties can arise due to the impact of the disorder itself as well as the challenges associated with living with schizophrenia. Here are some details about emotional difficulties in schizophrenia:
Flattened affect: Some individuals with schizophrenia may exhibit a flattened or blunted affect, meaning they display limited emotional expression. Their range of emotions may appear diminished or muted compared to what is typically observed in others. They may have difficulty experiencing and expressing a wide range of emotions, which can affect their interactions and social relationships.
Heightened emotions: On the other hand, some individuals with schizophrenia may experience heightened emotions. They may display intense emotional responses that are disproportionate to the situation at hand. These emotional responses may be unpredictable and contribute to difficulties in regulating and managing emotions effectively.
Inappropriate emotional responses: Individuals with schizophrenia may also exhibit inappropriate emotional responses, where their emotional reactions do not align with the context or social norms. For example, they may laugh or cry in situations that are not typically considered humorous or sad, respectively. These responses can be confusing or disconcerting to others and may further impact social interactions.
Emotional volatility: Schizophrenia can be associated with emotional volatility, where individuals may experience rapid shifts in their emotional states. They may move from one emotional extreme to another quickly, making it challenging to maintain emotional stability and regulate their emotions effectively.
Emotional withdrawal and isolation: The symptoms of schizophrenia, including emotional difficulties, can contribute to social withdrawal and isolation. Individuals may feel overwhelmed by their emotional experiences, have difficulty understanding or expressing their emotions, or fear judgment or rejection from others. As a result, they may choose to isolate themselves, which can further impact their emotional well-being.
Co-occurring anxiety and depression: Schizophrenia often coexists with other mental health conditions, such as anxiety disorders and depression. These comorbid conditions can intensify emotional difficulties and contribute to increased levels of distress, hopelessness, and impaired functioning.
Impact on quality of life: Emotional difficulties in schizophrenia can significantly impact an individual’s quality of life. They may struggle with forming and maintaining relationships, experience challenges in daily functioning, and have difficulty coping with stress or life changes. Emotional difficulties can also contribute to a reduced sense of well-being and overall life satisfaction.
Treatment and support: Treatment for emotional difficulties in schizophrenia typically involves a comprehensive approach. This may include a combination of medication, therapy (such as cognitive-behavioral therapy or supportive therapy), and psychosocial interventions. Supportive environments, peer support, and psychoeducation can also play a crucial role in helping individuals manage their emotions and improve their overall emotional well-being.
Understanding and addressing the emotional difficulties experienced by individuals with schizophrenia is essential for providing effective support and treatment. By promoting emotional regulation skills, fostering social connections, and addressing comorbid conditions, we can enhance the emotional well-being and quality of life of individuals living with schizophrenia.
Social Withdrawal
Social withdrawal is a common phenomenon observed in individuals with schizophrenia. It refers to the tendency to isolate oneself from social interactions and to withdraw from social relationships. Here are some details about social withdrawal in schizophrenia:
Avoidance of social situations: Individuals with schizophrenia often avoid or limit their participation in social activities, gatherings, and interactions. They may prefer to spend extended periods alone and avoid contact with others. This withdrawal can occur gradually or be more abrupt, depending on the individual and the course of their illness.
Impact on relationships: Social withdrawal can strain existing relationships and make it challenging to form new ones. Individuals may have difficulty maintaining friendships, romantic relationships, and family connections. The withdrawal may lead to a sense of loneliness and isolation, both for the individual and their loved ones.
Fear and paranoia: Social withdrawal can be driven by fears and paranoid thoughts that others are judging, criticizing, or plotting against the individual. They may have a heightened sense of suspicion and mistrust towards others, leading them to withdraw to protect themselves from perceived threats.
Negative symptoms of schizophrenia: Social withdrawal is often associated with negative symptoms of schizophrenia, such as reduced motivation, decreased emotional expression, and diminished social drive. These symptoms can contribute to a lack of interest or pleasure in social interactions and result in withdrawal from social situations.
Cognitive impairments: Cognitive impairments associated with schizophrenia, such as difficulties with attention, memory, and processing information, can make social interactions challenging. Individuals may find it hard to follow conversations, understand social cues, or engage in complex social exchanges, leading them to withdraw to avoid potential embarrassment or frustration.
Stigma and self-esteem: Stigma surrounding mental illness, including schizophrenia, can lead individuals to internalize negative beliefs and develop low self-esteem. They may feel ashamed or embarrassed about their condition, leading to social withdrawal as a way to protect themselves from potential judgment or rejection.
Impact on recovery and functioning: Social withdrawal can hinder the recovery process for individuals with schizophrenia. Social support and engagement in meaningful social interactions are important for maintaining motivation, fostering a sense of belonging, and enhancing overall well-being. Withdrawal from social connections can impede functional recovery and hinder engagement in treatment and rehabilitation efforts.
Treatment and support: Addressing social withdrawal in schizophrenia involves a multidimensional approach. It may include individual therapy, social skills training, cognitive remediation, and peer support interventions. Encouraging gradual exposure to social situations, providing education about the illness, and fostering a supportive and inclusive environment can also contribute to reducing social withdrawal and promoting social integration.
Understanding the reasons behind social withdrawal in schizophrenia is crucial for providing appropriate support and interventions. By promoting social inclusion, reducing stigma, and offering opportunities for social engagement, individuals with schizophrenia can have improved social functioning and a better quality of life.
Lack of Insight
Lack of insight, also known as anosognosia, is a common feature of schizophrenia. It refers to a person’s inability to recognize or fully understand their own mental health condition. Here are some details about the lack of insight in schizophrenia:
Lack of awareness: Individuals with schizophrenia may have limited awareness or denial of their symptoms, illness, or the need for treatment. They may fail to recognize that they have a mental health condition or may underestimate the severity and impact of their symptoms on their daily functioning.
Factors contributing to lack of insight: Lack of insight in schizophrenia can be influenced by various factors, including the underlying neurobiological changes associated with the disorder, cognitive impairments, and the presence of delusions or hallucinations that reinforce a distorted perception of reality. Additionally, fear, stigma, and societal attitudes toward mental illness can also contribute to a person’s lack of insight.
Implications for treatment adherence: Lack of insight can significantly impact treatment adherence. Individuals may resist or refuse treatment recommendations, including medication, therapy, or other interventions, as they do not perceive the need for it. This can impede their recovery and potentially lead to worsening symptoms, increased risk of relapse, and functional impairment.
Impact on personal and social functioning: Lack of insight can have significant consequences on an individual’s personal and social functioning. They may struggle to recognize when they need help or support, leading to delayed or inadequate intervention. Lack of insight can also hinder their ability to make informed decisions about their treatment, employment, and relationships.
Family and caregiver challenges: Lack of insight can place a burden on family members and caregivers. They may experience frustration, confusion, and distress when attempting to help and support someone who lacks awareness of their illness. It can be challenging for them to navigate situations where the individual refuses treatment or fails to recognize the need for professional help.
Strategies for addressing lack of insight: Addressing lack of insight requires a compassionate and patient approach. Building trust, establishing a therapeutic alliance, and providing psychoeducation about schizophrenia and its symptoms can help increase insight over time. Involving family members and caregivers in treatment discussions can also be beneficial, as they can provide support, offer different perspectives, and help reinforce the importance of treatment.
Legal implications: Lack of insight can have legal implications, particularly in situations where the individual poses a risk to themselves or others. In some cases, involuntary hospitalization or legal interventions may be necessary to ensure the person’s safety and well-being.
Addressing the lack of insight in schizophrenia is an ongoing process that requires a collaborative effort between healthcare professionals, individuals with schizophrenia, their families, and caregivers. By providing education, and support, and fostering a trusting therapeutic relationship, individuals with schizophrenia may gradually gain insight into their condition and the importance of treatment.
#Anxiety#Depression#Emotional experiences#Empathy#Mental health#Psychiatric conditions#Psychological disorders#Schizophrenia#Social isolation#Stigma
0 notes
Text
Factitious Disorder
-- a disorder where someone deceives others by appearing sick, by purposely getting sick, or by self-injury
-- can also happen when family members or caregivers falsely present others as being ill, injured, or impaired
-- symptoms can range from mild (slight exaggeration of symptoms) to severe
-- patient may make-up symptoms or tamper with medical tests
-- not the same as inventing medical problems for a practical benefit
-- challenging to identify
-- hard to treat
#studyblr#notes#medblr#medical notes#med notes#psychology#psychology notes#psych#psych notes#psychiatry#psychiatry notes#factitious disorder#tw self-injury#tw#psychological disorders#psychiatric disorders
5 notes
·
View notes
Text
Rare Mental Disorders: Conditions Beyond the Mainstream
youtube
#mental disorders#mental health#mental disorder#rare mental disorders#weird mental disorders#most rare mental disorders#mental illness#disorders#rare psychological disorders#top 10 rare mental disorders#bizarre mental disorders#scary mental disorders#probability comparison: mental disorder#psychological disorders#brain disorders#rare disorders#rare mental disorders test#rarest mental disorders#10 rare mental disorders to learn about#health#mental heath support#mental heath issues#Youtube
0 notes
Text
Story from the Washington Post here, non-paywall version here.
Washington Post stop blocking linksharing and shit challenge.
"The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.” ...
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries...
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments [for lupus] — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other people with similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients, the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.” ...
Waking up after two decades
The medical team set to work counteracting April’s rampaging immune system and started April on an intensive immunotherapy treatment for neuropsychiatric lupus...
The regimen is grueling, requiring a month-long break between each of the six rounds to allow the immune system to recover. But April started showing signs of improvement almost immediately...
A joyful reunion
“I’ve always wanted my sister to get back to who she was,” Guy Burrell said.
In 2020, April was deemed mentally competent to discharge herself from the psychiatric hospital where she had lived for nearly two decades, and she moved to a rehabilitation center...
Because of visiting restrictions related to covid, the family’s face-to-face reunion with April was delayed until last year. April’s brother, sister-in-law and their kids were finally able to visit her at a rehabilitation center, and the occasion was tearful and joyous.
“When she came in there, you would’ve thought she was a brand-new person,” Guy Burrell said. “She knew all of us, remembered different stuff from back when she was a child.” ...
The family felt as if they’d witnessed a miracle.
“She was hugging me, she was holding my hand,” Guy Burrell said. “You might as well have thrown a parade because we were so happy, because we hadn’t seen her like that in, like, forever.”
“It was like she came home,” Markx said. “We never thought that was possible.”
...After April’s unexpected recovery, the medical team put out an alert to the hospital system to identify any patients with antibody markers for autoimmune disease. A few months later, Anca Askanase, a rheumatologist and director of the Columbia Lupus Center,who had been on April’s treatment team, approached Markx. “I think we found our girl,” she said.
Bringing back Devine
When Devine Cruz was 9, she began to hear voices. At first, the voices fought with one another. But as she grew older, the voices would talk about her, [and over the years, things got worse].
For more than a decade, the young woman moved in and out of hospitals for treatment. Her symptoms included visual and auditory hallucinations, as well as delusions that prevented her from living a normal life.
Devine was eventually diagnosed with schizoaffective disorder, which can result in symptoms of both schizophrenia and bipolar disorder. She also was diagnosed with intellectual disability.
She was on a laundry list of drugs — two antipsychotic medications, lithium, clonazepam, Ativan and benztropine — that came with a litany of side effects but didn’t resolve all her symptoms...
She also had lupus, which she had been diagnosed with when she was about 14, although doctors had never made a connection between the disease and her mental health...
Last August, the medical team prescribed monthly immunosuppressive infusions of corticosteroids and chemotherapy drugs, a regime similar to what April had been given a few years prior. By October, there were already dramatic signs of improvement.
“She was like ‘Yeah, I gotta go,’” Markx said. “‘Like, I’ve been missing out.’”
After several treatments, Devine began developing awareness that the voices in her head were different from real voices, a sign that she was reconnecting with reality. She finished her sixth and final round of infusions in January.
In March, she was well enough to meet with a reporter. “I feel like I’m already better,” Devine said during a conversation in Markx’s office at the New York State Psychiatric Institute, where she was treated. “I feel myself being a person that I was supposed to be my whole entire life.” ...
Her recovery is remarkable for several reasons, her doctors said. The voices and visions have stopped. And she no longer meets the diagnostic criteria for either schizoaffective disorder or intellectual disability, Markx said...
Today, Devine lives with her mother and is leading a more active and engaged life. She helps her mother cook, goes to the grocery store and navigates public transportation to keep her appointments. She is even babysitting her siblings’ young children — listening to music, taking them to the park or watching “Frozen 2” — responsibilities her family never would have entrusted her with before her recovery.
Expanding the search for more patients
While it is likely that only a subset of people diagnosed with schizophrenia and psychotic disorders have an underlying autoimmune condition, Markx and other doctors believe there are probably many more patients whose psychiatric conditions are caused or exacerbated by autoimmune issues...
The cases of April and Devine also helped inspire the development of the SNF Center for Precision Psychiatry and Mental Health at Columbia, which was named for the Stavros Niarchos Foundation, which awarded it a $75 million grant in April. The goal of the center is to develop new treatments based on specific genetic and autoimmune causes of psychiatric illness, said Joseph Gogos, co-director of the SNF Center.
Markx said he has begun care and treatment on about 40 patients since the SNF Center opened. The SNF Center is working with the New York State Office of Mental Health, which oversees one of the largest public mental health systems in America, to conduct whole genome sequencing and autoimmunity screening on inpatients at long-term facilities.
For “the most disabled, the sickest of the sick, even if we can help just a small fraction of them, by doing these detailed analyses, that’s worth something,” said Thomas Smith, chief medical officer for the New York State Office of Mental Health. “You’re helping save someone’s life, get them out of the hospital, have them live in the community, go home.”
Discussions are underway to extend the search to the 20,000 outpatients in the New York state system as well. Serious psychiatric disorders, like schizophrenia, are more likely to be undertreated in underprivileged groups. And autoimmune disorders like lupus disproportionately affect women and people of color with more severity.
Changing psychiatric care
How many people ultimately will be helped by the research remains a subject of debate in the scientific community. But the research has spurred excitement about the potential to better understand what is going on in the brain during serious mental illness...
Emerging research has implicated inflammation and immunological dysfunction as potential players in a variety of neuropsychiatric conditions, including schizophrenia, depression and autism.
“It opens new treatment possibilities to patients that used to be treated very differently,” said Ludger Tebartz van Elst, a professor of psychiatry and psychotherapy at University Medical Clinic Freiburg in Germany.
In one study, published last year in Molecular Psychiatry, Tebartz van Elst and his colleagues identified 91 psychiatric patients with suspected autoimmune diseases, and reported that immunotherapies benefited the majority of them.
Belinda Lennox, head of the psychiatry department at the University of Oxford, is enrolling patients in clinical trials to test the effectiveness of immunotherapy for autoimmune psychosis patients.
As a result of the research, screenings for immunological markers in psychotic patients are already routine in Germany, where psychiatrists regularly collect samples from cerebrospinal fluid.
Markx is also doing similar screening with his patients. He believes highly sensitive and inexpensive blood tests to detect different antibodies should become part of the standard screening protocol for psychosis.
Also on the horizon: more targeted immunotherapy rather than current “sledgehammer approaches” that suppress the immune system on a broad level, said George Yancopoulos, the co-founder and president of the pharmaceutical company Regeneron.
“I think we’re at the dawn of a new era. This is just the beginning,” said Yancopoulos."
-via The Washington Post, June 1, 2023
#mental illness#schizophrenia#schizoaffective#psychotic disorders#psychology#neurology#autoimmune#autoimmine disease#neuroscience#medical news#medical research#catatonia#immunotherapy#immune system#clinical trials#good news#hope
6K notes
·
View notes