#early onset child psychosis
Text
looking back on my childhood objectively and with the insight of knowing what my schizoaffective psychosis symptoms are, i realize that most people weren’t just constantly terrified of everything growing up. they didn’t develop multiple UTIs from holding their pee at night because they thought someone was waiting in the bathroom to kill them. they didn’t calculate all the ways they could hide in their room if someone broke into the house and went over these steps in their heads for hours every night. they didn’t lose sleep over the feeling of bugs crawling around inside their bodies. they didn’t have this terror in their lives before they even hit double digits and by the gods am i sad for young me that he had to deal with it
#i had really early onset symptoms (they really started becoming bad around age 6) but i was dismissed as being over imaginative#i was on antipsychotics by age 12#i turn 21 this year and i just wish child me had been able to experience the freedom of childhood#schizoaffective#schizophrenia#psychosis#ghost.txt#lemme know if i need to tag any triggers for this post btw
21 notes
·
View notes
Text
on the topic of the aero aesthetic my feelings on it r a little funny bc i was actually a little shocked to find out thats the windows customization other 2000s old web ppl consider The y2k PC thing bc.if i recall correctly it wasnt just my family that went through this the whole country had a kind of technology rush during the 2000s, so from kindergarten to fifth grade i had already experienced windows 98 to windows 7 which makes my brain see "old computer" n think of our ancient 98 PC, so while other ppl think "y2k computer aesthetic" n think of aero i think that n think of that peculiar green n gray color scheme.its just funny aero feels a little too modern for me bc of all that i need my computer set to the opaque options or its just wrong
#analiceoriginal.txt#god i loved that thing i remember.i think it was my uncle? who drove over w a computer n i rushed to the car to see what he bought#n i was all WHATS THAT WHATS THAT IS THAT A COMPUTER#my aunt installed some emulated atari games n would call me over to play them n i was obsessed w the forest n robber ones#the one w that rly weird dragon sprite n the castle fascinated but also scared me#i also loveeed that version of paint w the spray can that would leak downwards i thought it was so stylish#'werent you guys poor how the hell did get that many computers' thats a great question baby.#sadly i dont know the answer to that i was busy having child issues like having to eat my carrots n having early onset psychosis to ask#any adults abt it
2 notes
·
View notes
Text
[“Kraepelin worked at a time when “therapeutic pessimism” characterized psychiatry in Germany and elsewhere. Overcrowding had destroyed institutions’ potential for the “moral cure” of a structured environment and close physicians’ care, and such pessimism rose from the profession’s lack of other solutions, prescriptions, or cures. Kraepelin’s classification filled this diagnostic gap in late-nineteenth-century medicine. In the absence of knowledge about origins or possibilities of treatment, Kraepelin directed his efforts away from subjective clinical experience, instead simply delineating onset, course, and outcome of psychiatric diseases. Since Kraepelin sought simply to classify and observe disease, his system did not lead to meaningful therapeutic results. This vacuum led to “the predominance of prevention and neutralization,” contemporary scholar Michael Shepherd writes. In this pessimistic framework and always with a strong allegiance to the German Fatherland, Kraepelin viewed forms of mental illness as social disorders from which the German body politic should be protected. Criminal behavior, for example, arose from “a congenitally inferior predisposition.” This emphasis on the prevention and neutralization of psychiatric diseases helped to set the stage for sterilization and euthanasia. Supt. Powell in Georgia, as we have seen, was also working on the same ideological stage set.
Kraepelin’s diagnostic system would prove a pivotal moment in psychiatry’s modernity, and versions of it have persisted into the twenty-first century. In 1921, the American Medico-Psychological Association (AMPA) became the American Psychiatric Association (APA) that we know today. After 1921, the American Journal of Insanity became known as the American Journal of Psychiatry. In 1918, the AMPA published a Statistical Manual for the Use of Hospitals for Mental Diseases with the Bureau of Statistics of the National Committee for Mental Health. In 1952, the Statistical Manual’s categories would provide one model for the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders. The first two DSMs were highly infected by Freudian psychoanalysis, which prevailed in U.S. psychiatry from the 1930s to the early 1970s. DSM-III marked a return to the biomedical model on which subsequent editions have elaborated, including DSM-5.”
[…] …in 1910, responding to what they understood as American psychiatry’s best practices, Georgia doctors reshaped their understanding of patient behaviors according to Kraepelin’s categories. The differences were profound. For example, the 1888 annual report by Supt. Powell had noted “Cause or Supposed Cause of Insanity” (with “whites” and “coloreds” listed separately). This list willy-nilly mixed the effects of diseases (syph ilis, epilepsy, attacks of fevers) and other conditions (such as “idiocy,” “menstrual derangement,” old age) with responses to life events (disappointed affections, failure in business, death of a child, fall from a house, financial trouble, eating peach kernels) and habits thought to be mentally unhygienic (masturbation, excessive use of alcohol, overstudy, religious excitement, taking opium).23 The 1909 report looked almost the same. But with a nod to Atlanta’s most famous beverage, it did include one incident of “excessive use of Coca Cola.” By only one year later, in 1910, the table of “Causes or Supposed Causes of Insanity” was dropped, leaving only the table “Forms of Psychosis,” with descriptions of each diagnostic category.
That year, these understandings of psychiatric categories informed the Milledgeville interview protocol experienced by Stork Hardly. Questions regarding affect or mood that might signal manic-depressive psychosis became: “Are you happy or sad?” To detect dementia praecox, with its delusions, hallucinations, and disordered thoughts, the questions included: “Ever hear noises or voices?”; “Ever see strange things you cannot account for?”; and, in some cases, “Do you ever talk to God?” and “Does God ever talk to you?” As we will see in the interviews, the doctor starts off with “Are you sad or happy?” and goes on to clarify his answer with “Why?” and queries on, for example, whether a patient cries. One suspects that no one else of authority in these Georgia patients’ lives had ever paid quite so much attention to whether or not they were happy. It is not so clear that the doctors cared either, except to diagnose them (when they did).”]
mab segrest, from administrations of lunacy: a story of racism and psychiatry at the milledgeville asylum
41 notes
·
View notes
Text
Chapter 3 of Schizophrenia, Third Edition: Child and adolescent schizophrenia
Although it's rare before the age of 10, childhood and adolescent schizophrenia does happen. Things like clinical severity, impact on development, and poor prognosis calls for a need of early detection, prompt diagnosis, and effective treatment. Childhood/adolescent onset schizophrenia is associated with poor premorbid functioning and early developmental delays, which is particularly striking for people with onset before adolescence. Similar impairments have been reported in adult-onset cases but are more common in child/adolescent-onset cases. These premorbid impairments may be a risk, or a precursor to psychosis. Diagnoses like anxiety, depression, ADHD, and autism may precede the diagnosis of schizophrenia in children and adolescents.
People who develop schizophrenia typically go through a prodromal phase characterized by a marked decline in functioning. Things like social withdrawal, decline in school performance, and uncharacteristic and odd behavior begin on average a year before the onset of psychotic symptoms. In retrospect things like non-specific behavioral changes were frequently early negative symptoms well before positive symptoms showed. Prodromal symptoms may also include odd ideas, eccentric interests, changes in affect, unusual experiences, and bizarre perceptual experiences. While these are characteristic of schizotypal personality disorder, in a schizophrenic prodrome there is usually a progression to a more severe dysfunction.
Child and adolescent-onset schizophrenia is characteristically chronic, with only a minority of cases making a full recovery. If full recovery does occur it is most likely in the first three months, and Hollis (1999) found that 12% of cases of schizophrenia only reached full remission. A Maudsley study found that those who were psychotic after 6 months have a 15% chance of full remission, while over half of cases who made a full recovery had active psychotic symptoms for less than 3 months. This indicates that observation past 6 months adds little new information, and the course over the first 6 months is the best predictor of remission.
A number of long-term follow-up studies of child and adolescent-onset schizophrenia all describe a chronic, unremitting long-term course with severely impaired functioning in adult life. Roughly one-fifth of cases in most studies have a good outcome while at the other extreme one-third are severely impaired. After the first few years of the illness there is little evidence of further progressive decline. Third, child and adolescent-onset schizophrenia has a worse outcome than adult-onset schizophrenia and affective psychoses. Social functioning is also very impaired in early onset schizophrenia. These findings confirm childhood schizophrenia is at an extreme end of a continuum of severity.
Cognitive symptoms of schizophrenia are increasingly being acknowledged as core features of the disorder. The degree of cognitive impairment is greater in child and adolescent-onset than adult-onset cases, which raises several questions. Are cognitive deficits specific or general - are some areas more affected? Which deficits precede psychosis and could be causal, and which are consequences of psychosis? Is it specific to schizophrenia or is it common between other developmental and psychotic disorders? Are cognitive impairments progressive or static after the onset of psychosis?
In summary of the findings: sensorimoter skills, associative memory, and simple language abilities are preserved in children with schizophrenia. Bigger decifits include tasks that require sustained and focused attention, flexible switching of cognitive set, high-information processing speed, and suppression of prepotent responses. These cognitive processes are executive functions, necessary for organizing goal-directed behavior.
Assessing a child or adolescent with schizophrenia should include detailed history, mental state and physical examination, and laboratory tests. Usually physical exams include a full blood count and biochemistry, including liver and thyroid function and a drug screen. Progressive structural brain changes indicate value in getting an MRI. Antipsychotics stay a cornerstone of treatment of schizophrenia but treatment should take a multimodal approach including pharmacotherapy, family and individual counselling, education about the illness, and provision to meet social/educational needs.
#nerdpost#graypost#psychology#psychosis#schizophrenia#long post#book: schizophrenia third edition#childhood schizophrenia#adolescent schizophrenia#early onset schizophrenia
5 notes
·
View notes
Text
Ok I think I just have a major anxiety disorder but when I was a child like 9 and younger as soon as I was able to conceptualize death I became obsessed with it in a bad way. I couldn’t stop thinking about it, having visions of deaths of strangers and family members to the point of panic, sitting for long periods of time unable to stop conceptualizing the firsthand experience of death (to the point of panic. Again), avoiding anything that could somehow bring me to the face of death even in small or silly ways.
Looking back, it definitely wasn’t just death I was afraid of to the point of obsession. It was anything fear inducing. But death was usually involved. I remember being very young and losing my goddamn mind over the thought of major storms like tornadoes coming to CA and crying and panicking until my parents screamed at me to shut the fuck up because I couldn’t stop visualizing it and feeling the emotions as if they were really happening. Same thing with death in general but I have always had the problem of these hypothetical disasters of any and every kind hitting me and being sucked into a whirlpool of panic and “fantastical” terror
My parents certainly were not equipped to deal with a mentally ill child (hypocrite cunts cough cough) and just went banana gorilla black parents on me instead of trying to help but. Goddamn was I going through it in my own mind. And that’s not even touching on the (very) early onset psychosis. ://
3 notes
·
View notes
Text
The indicators of inflammation in adolescent depression vary between males and females.

Recent research conducted by the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) at King’s College London has uncovered a connection between depression and the risk of depression, and specific inflammatory proteins in both boys and girls.
Inflammation triggers the release of proteins called cytokines into the bloodstream. While prior studies have shown that higher cytokine levels are linked to depression in adults, little was known about this relationship during adolescence.
The researchers delved into sex-specific distinctions in the association between inflammatory proteins and depression. Published in the Journal of Affective Disorders, the study revealed that different cytokines played a role in the risk and severity of depression in boys as opposed to girls. This investigation was part of the IDEA (Identifying Depression Early in Adolescence) project, supported by MQ Mental Health Research.
To assess inflammation, the team measured cytokine levels in the blood of 75 adolescent boys and 75 adolescent girls (aged 14-16) from Brazil. These 150 participants were divided equally into three groups: those at low risk of depression without current depression, those at high risk of depression without current depression, and those currently experiencing major depressive disorder (MDD).
The results indicated notable sex-specific differences in the specific inflammatory proteins associated with adolescent depression. Elevated levels of the cytokine interleukin-2 (IL-2) were linked to an increased risk and severity of depressive symptoms in boys but not in girls. Conversely, higher levels of IL-6 were connected to the severity of depression in girls but not boys. In boys, IL-2 levels were higher in the high-risk group compared to the low-risk group, and even higher in the group diagnosed with depression. This suggests that in boys, IL-2 levels in the blood could serve as an indicator for the onset of future depression.
Dr. Zuzanna Zajkowska, Postdoctoral Researcher at King’s IoPPN and the study’s first author, commented,
“This is the first study to show differences between boys and girls in the patterns of inflammation that are linked to the risk and development of adolescent depression. We found that the severity of depressive symptoms was associated with increased levels of the cytokine interleukin-2 in boys, but interleukin-6 in girls. We know more adolescent girls develop depression than boys and that the disorder takes a different course depending on sex so we hope that our findings will enable us to better understand why there are these differences and ultimately help develop more targeted treatments for different biological sexes.”
The adolescents were recruited from public schools in Brazil, and the risk of depression was assessed using a composite risk score based on 11 sociodemographic variables developed as part of the IDEA project. They completed various questionnaires regarding their emotional well-being, relationships, experiences, and mood, as well as underwent clinical assessments with a child and adolescent psychiatrist.
Senior author Professor Valeria Mondelli, Clinical Professor of Psychoneuroimmunology at King’s IoPPN, and theme-lead for Psychosis and Mood Disorders at the NIHR Maudsley BRC, emphasized,
“Our findings suggest that inflammation and biological sex may have combined contribution to the risk for depression. We know that adolescence is a key time when many mental disorders first develop and by identifying which inflammatory proteins are linked to depression and how this is different between boys and girls we hope that our findings can pave the way to understanding what happens at this critical time in life. Our research highlights the importance of considering the combined impact of biology, psychology, and social factors to understand the mechanisms underlying depression.”
This study is part of the Identifying Depression Early in Adolescence (IDEA) project led by Professor Valeria Mondelli at King’s IoPPN and funded by MQ Mental Health Research. The IDEA project aims to investigate how cultural, social, genetic, and environmental factors contribute to the development of depression in individuals aged 10-24 across various countries including the UK, Brazil, Nigeria, Nepal, New Zealand, and the USA. The study received support from the charity MQ Mental Health Research, UK Medical Research Council, and the Academy of Medical Sciences. Professor Valeria Mondelli is supported by the National Institute for Health and Care Research (NIHR) Maudsley Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London, as well as the Medical Research Council.
Remember, if you need further guidance or support, don’t hesitate to reach out to your mental health professional or contact us for assistance.
#health#medicine#pain management#mental health#back pain#apdss#chiropractic#neckpain#neurostar#depressionhelp
0 notes
Text
#JamesDonaldson On #MentalHealth – Watching For Signs Of #Psychosis In #Teens

Catching #kids early and supporting them before they're in crisis can delay #mentalhealthdisorders and reduce impairment
Photo by Andrea Piacquadio on Pexels.com
Writer: Juliann Garey
Clinical Experts: Tiziano Colibazzi, MD , Christoph Correll, MD
What You'll Learn
- What is psychosis?
- What are prodromal symptoms?
- What symptoms should I look for in my teen?
- How is early psychosis in teens treated?
- Quick Read
- Full Article
- What are “prodromal” symptoms?
- First step if you feel your child is at risk: An evaluation
- Lifestyle and #mentalhealth options
- Treatment for prodromal psychotic symptoms
Psychosis is a condition in which a person loses touch with reality. If a teen has psychosis, they might hear or see things that aren’t there. Psychosis is often a symptom of an illness called schizophrenia. It shows up in the late teen or early adult years.
But some teens show early warning signs of psychosis. If doctors can catch these early signs, they may be able to delay the full-blown illness and minimize its symptoms. Since psychotic symptoms cause problems in everything from #school to friendships to family, acting fast can help teens a lot.
Early signs of psychosis are called “prodromal” symptoms. They include things like not wanting to see friends, feeling like people want to hurt them, not showering, and seeing or hearing things that aren’t there. To a #parent, the change in their teen would probably be very noticeable.
The good news is that in the early stages, psychosis in teens can be treated by making pretty simple changes in their habits. These include reducing stress, making sure they have good sleep habits and getting treatment for other problems like anxiety.
If you’re worried your teen might be having these symptoms, the first step is to take them to their regular doctor. Their doctor will rule out drug use, which can also cause these symptoms. Then, they will send the teen to be examined by a psychiatrist. It’s hard for #doctors to know which teens will go on to develop serious psychotic illnesses — not all will. But getting your teen to a professional who can watch their symptoms may be the most important step a parent can take.
There are fewer more frightening or challenging psychiatric conditions for a family to face than psychosis, an extreme mental state in which impaired thinking and emotions cause a person to lose contact with reality. This could mean hearing or seeing things that aren’t there (hallucinations), or believing things that aren’t true (delusions).
The illness most often associated with #psychosis, #schizophrenia, usually doesn’t show up until very late #adolescence or early #adulthood. Recently, however, experts in the field have been working to identify high-risk kids who show symptoms that could serve as early warning signs of psychosis, and several academic centers have been set up to focus on this crucial period when it may be possible to change the trajectory of mental illness.
Not all the kids who are identified with what experts call “prodromal” symptoms will progress, or “convert” to full-blown psychotic illness. But early intervention has been shown to improve outcomes for those who do. And since psychotic symptoms cause disruption across a teenager’s life, from school to friendships to family, researchers are hoping quick action can prevent impairment and prolong typical functioning.
What’s more, some of the approaches that show promise in delaying onset of psychosis or mitigating symptoms include fairly simple lifestyle changes like #stress reduction and sleep hygiene, and managing co-occurring disorders like #anxiety. The key: identifying at-risk kids earlier when these low-impact measures are still effective.
What are “prodromal” symptoms?
Prodromal symptoms are “attenuated” or weak symptoms of psychosis. Moreover, “they are a warning sign,” says Christoph Correll, MD, the medical director of the Recognition and Prevention Program (RAP) at Zucker Hillside Hospital in Queens, NY, which specializes in diagnosing and treating early symptoms of #mentalillness in #teenagers and young adults. “These signs can happen in people who don’t go on to develop psychosis—but if we follow these people who are in the risk state based on these watered-down versions, one third will probably go on to develop psychosis. That’s a lot more than in the general population.”
Prodromal symptoms occur on a spectrum from very, very mild to severe and can include:
- Withdrawing from friends and family/feeling suspicious of others
- Changes in sleeping or eating patterns
- Less concern with appearance, clothes or hygiene
- Difficulty organizing thoughts or speech
- Loss of usual interest in activities or of motivation and energy
- Development of unusual ideas or behaviors
- Unusual perceptions, such as visions or hearing voices (or even seeing shadows)
- Feeling like things are unreal
- Change in personality
- Feelings of grandiosity (belief he has a superpower, etc)
In some cases, these symptoms represent the early stages of a disorder, and will eventually convert. In others, the symptoms actually fade or remain mild. Tiziano Colibazzi, MD, is a #psychiatrist at Columbia Presbyterian’s COPE clinic (Center for Prevention and Evaluation), which was established to research and treat prodromal symptoms. “We can identify a group of people that are at clinically high risk,” says Dr. Colibazzi. “What we can’t do is narrow that group down further to identify the 30 percent who will convert.”
First step if you feel your child is at risk: An evaluation
The right treatment for prodromal symptoms depends entirely on how severe they are when they are diagnosed. The first step is a proper and complete diagnosis by a #mentalhealthprofessional with experience in assessing psychotic illness.
If you see marked changes in motivation, thinking, and/or behavior in your child, the first place to start is with her pediatrician to rule out a medical illness. #Substanceuse also needs to be ruled out as the cause of any #behavior changes in #adolescents. After that, you’re going to want to have your child evaluated by a qualified #psychiatrist or #psychologist. This in itself might be a multi-step process.
“You can’t just look at the kid once and get a bit of a history and then know what’s going on, ” says Dr. Correll. “Kids develop; symptoms develop. And the trajectory—how things change, get better or worse, what other symptoms add on to it—will be highly informative in telling us something about the prognosis, what we expect to happen.”
One aid to predicting the evolution and severity of symptoms, notes Dr. Colibazzi, is the patient’s ability to doubt his symptoms. If your child retains the self-awareness to know that it’s his mind that is playing tricks on him, it’s an indication that symptoms are still in the very early stages. As symptoms become more severe, the patient’s beliefs (whether paranoid, grandiose or hallucinatory) become increasingly difficult to challenge.
#James Donaldson notes:Welcome to the “next chapter” of my life… being a voice and an advocate for #mentalhealthawarenessandsuicideprevention, especially pertaining to our younger generation of students and student-athletes.Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.Having gone through a recent bout of #depression and #suicidalthoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. #http://bit.ly/JamesMentalHealthArticleFind out more about the work I do on my 501c3 non-profit foundationwebsite www.yourgiftoflife.org Order your copy of James Donaldson's latest book,#CelebratingYourGiftofLife: From The Verge of Suicide to a Life of Purpose and Joy
www.celebratingyourgiftoflife.com
Lifestyle and #mentalhealth options
Psychotic symptoms and illnesses have been shown to vary quite a bit depending on the environment—the health of our bodies, our interpersonal relationships, our mindsets. As with any illness, but particularly important in at-risk #youth, healthy living is key. Regardless of the severity of prodromal symptoms, Dr. Correll says that your child’s outcome can be improved by making sure your kid sticks to a routine that includes:
- Eating well
- Getting regular exercise
- Adhering to a regular sleep schedule
- Reducing stress as much as possible
- Staying away from drugs—particularly marijuana, which can interact with prodromal symptoms and increase the risk for psychosis significantly
Also, don’t forget to address depression and #anxiety. According to Dr. Correll, “#adults who eventually developed #schizophrenia identified a three to five year period during which they experienced depression or anxiety before developing the prodromal symptoms of psychosis and then developed full-blown psychosis.” “So treating the #depression early,” he says, “might actually interrupt the progression from depression to psychosis in some #patients.”
Treatment for prodromal #psychotic symptoms
Dr. Correll recommends trying several approaches. Mild symptoms call for more low-key treatments including:
- Psycho-education: teaching both the kid and the family more about the symptoms and the illness.
- Therapy, particularly #cognitivebehavioraltherapy: “#CBT can be good to change one’s thinking patterns,” says Correll, “and also to address developing #self-esteem. We have to be careful that kids with a psychiatric diagnosis don’t self-stigmatize and get into a hopeless or negative mode where they feel they can’t achieve.”
- Lifestyle adjustments: Assessing whether the current school environment is best for the child. Perhaps a therapeutic social group to help the #child cope.
- Reducing #Stress: #Stress is often a trigger for symptoms, so reducing stress in these kids’ lives is crucial and may prevent or delay conversion to psychotic illness.
Understanding prodromal symptoms and monitoring kids who are at high risk for psychotic illness means that #parents can do more for their kids than wait for symptoms to get worse or merely hope for the best. Early monitoring and intervention can give high-risk #kids an advantage, which researchers hope will eventually change the odds when it comes to #psychotic illness.
“The duration of untreated #psychosis does actually seem to affect the course of the illness,” Dr. Colibazzi says. The longer the illness goes untreated, the greater the chance that it will cause serious disruption in all areas of the #patient’s life. “So it is reasonable to think that just following someone very closely and treating them very early, as soon as they develop symptoms, would be helpful.”
Photo by Andrea Piacquadio on Pexels.com
Read the full article
0 notes
Text
Understanding and Facing Addiction at the Student Level
In this episode of Real Talk, KJK Student Defense Attorneys Susan Stone and Kristina Supler are joined by Philip van Guilder, a Director of Greenhouse Treatment Center’s Community Affairs. They discuss mental health and addiction issues in students. The conversation includes the unexpected patterns of addiction and mental health issues prevalent is students today how to identify and address the symptoms of addictive behavior, and what every parent needs to know about the treatment and prevention of mental health and addiction issues.
Links Mentioned In the Show:
KJK Student Defense
Show Notes:
(01:37) From personally going through addiction to becoming a mental health evangelist
(02:44) The stigma against mental health and addiction issues versus the Greenhouse Treatment Center: how they can help children and adults in 28 days
(03:17) What makes the Greenhouse Treatment Center different from most other kinds of hospitals
(04:57) Why parents now need to monitor their children for addiction issues as early as the 7th grade
(06:30) Marijuana and the serious damage it can do to a child’s developing brain, including psychosis
(07:40) Why children can get access to drugs from the comfort of their own home
(08:58) The warning signs of addictive behavior in children that every parent should be aware of
(09:36) One way in which parents and college faculty can curb the onset of addiction issues in students
(11:17) The severe and sometimes fatal consequences of overindulgence in alcohol and drugs in college students
(12:34) The science behind why compulsive addictive behavior takes place
(15:02) The battle of alcohol addiction and sobriety from a first-hand perspective
(16:26) Mind vs. Body: Sticking to the path of sobriety
(17:57) The ongoing stigma against those with mental health issues
(19:44) The best approach to addressing a simultaneous mental health and addiction challenge in college students
(22:19) Can someone just have a naturally addictive personality?
(24:12) The prevalence of alcohol inhalation and why it’s a symptom of addiction
(25:38) The relationship between alcohol/drug disorders and eating orders in patients
(26:45) The easy steps parents can take to protect their kids and their friends from mental health and/or addiction issues
Transcript:
Kristina Supler: So here at Real Talk, we're committed to educating our listeners about substance abuse and safety measures that parents and students should know about. On a past episode of Real Talk, we were pleased to have on as a guest, Dr. Beth Weinstock of the Birdie Light organization, whose mission is really to spread information about test strips.
And we're so pleased to have our guests today.
Susan Stone: We are going to talk to Philip van Guilder, Guilder. I'm sorry. Do you pronounce it? Guilder? Phil Philip.
Philip Van Guilder: I do. Yes.
Susan Stone: I, I have my tongue twisted today, Kristina. And he is a self-described mental health evangelist at the Greenhouse Treatment Center. And I wanna add a father of five, uh, Philip, without speaking out of turn, you indicated in our pre-chat that you had some addiction issues. And so did your children and for our listeners out there who are mainly parents of high school and college age students, I think your insight is gonna be invaluable. And just add on our last podcast with podcast with Dr. Weinstock so could, before we begin, can you tell us what is a mental health evangelist?
I, I saw that and I'm like, are you religious? Where are you coming from?
Philip Van Guilder: No, no, it has nothing to do with spirituality. Uh, actually the, the evangelist is a, it pulls me away from the marketing aspects. I, what I'm trying to do and what I do for the greenhouse is make us as transparent to the outside community as possible and make the outside community as transparent to the personnel here as possible.
So we can maximize all the resources available and, and we can normalize the stigma of, of mental health issues and, and addiction so that it encourages people to, uh, just to normalize it so that people can get help and, and not feel any sort of a stigma. So I kind of wear my recovery on my sleeve.
I mean, if you were to meet me on the street, we were having coffee bumped into each other within about two or three minutes somehow or another, I would word it that you would know. I was a person in long term recovery.
Kristina Supler: Philip, you are at Greenhouse Treatment Center, which is a part of the American Addiction Center.
Tell us, what's give us some insight into the population that you work with on a daily basis. And what do you do?
Susan Stone: Tell us what I, I wanna learn about you.
Philip Van Guilder: Okay, thank you. So, so our population is 18 and above, and there are people who primary, uh, diagnosis is substance use. What, what I do, as I said, I reach out to the community.
We wanna know what resources are out there. When you come to treatment, whether you're, uh, going to treatment as it, a young adult, or whether you're going to treatment as a, as a child, whatever age you're going to treatment. The 28 days today, which is about what most people can, can, uh, expect to get from their insurance.
That's the first step. Uh, we're a hospital. Uh, most hospitals you go to when you go to the hospital, you get medicine, you get a cast, you you're injuries are, are stitched up. And when you leave, you're, you're virtually on your way to, to recovery.
This hospital is different. What we do here is we give you information and, and when you leave, what you do with that information determines whether or not you're gonna get well, we don't.
And so this is just the first step of your recovery process. So when, so for us, it's important for us to connect with the community because we expect to take the patient, the client from the 28 days and send them to someone else for the next level of care, which is a, um, perhaps partial partial hospitalization, which is the same as all day programming, but not in a hospital setting or intensive outpatient, I O P, which is, number of hours each day, allowing them to work, but continuing their recovery journey or, or even perhaps, uh, as complete step down to continuing care where they show up for a group, uh, once a week or once a month for continuing care.
Susan Stone: It's such a long process to recovery. I really, I admire anybody who has the courage to go through it. You talked about working with students 18 and above. Tell us what insights do you have today on young adults battling with addiction, anything different, new,
Kristina Supler: or what's the most prevalent form of addiction you're seeing.
Susan Stone: Oh, great question, Kristina.
Philip Van Guilder: yeah, that, that is a good question. Yeah. What, what we're seeing today is it starts much younger. So by the time we see an 18 year old, they've been involved in, in some of the statistics, I can show, go back to the seventh and eighth grade and it was, and, and, and with alcohol
Susan Stone: or drugs, seventh or eighth grade,
Philip Van Guilder: Both and with non-prescribed medications and, and, and I, some statistics as recently as 2020, just from this area, we're, we're in, we're just would be the same as any area.
30% of 10th graders, 30% of 10th graders either found it, not dangerous to use marijuana. And yet we know the THC content of marijuana today is so high, that, that it can be very destructive in young developing minds and 30%. So fully, a third of 10th graders believe it's safe to use marijuana.
Susan Stone: Well, if it's legal in some states, how would parents dispel that belief?
Kristina Supler: Well, I will say in a past episode, we had on Dr. Jill Grimes and who's written a book for college audiences and she is a big believer that it is essential that parents educate their children. That marijuana is harmful no matter what anyone thinks, if it's legalized or not, it does things to developing brains and students need to be aware of the negative impact on brain develop.
Philip Van Guilder: Yeah. I mean, there's, there's no doubt about that. So, so let's go back 30, 40 years ago when the THC was three to 4% and, people, perhaps college age experimented with it, maybe they even used it frequently, but it's still three to 4% today. We see pure, uh, marijuana. 18 to 20% and in a developing brain, we're seeing cases of psychosis in 16 year olds, first time use, and we're talking some serious damage.
And we know that well, first of all, , and it is not to, it's not to beat up on young people, but. If a little is good, a lot is better. So there is no moderation when we're looking see another thing I've got here. One in five eighth graders believe that it's that's 20, 20% to almost 21% of eight graders.
Believe it's okay to use non-prescribed medications because of the way it makes you feel. not just marijuana, but we're talking about people that walk up to the medicine cabinet and grab some, uh, mood altering medication and think it's safe to use a non-prescribed medication.
Susan Stone: It's right in the home.
Philip Van Guilder: That, that they get out of the medicine cabinet because their parents are taking it on a prescribed basis for the right reasons and they believe it's okay. And it's safe. They believe it's safe, not just okay, but safe to use it because it's after all it's a prescribed medication. Prescribed for someone else.
Kristina Supler: Sure. Well, and also, I think we'd be remiss not to mention that with marijuana in this day and age, there's also all the risks. As in that we don't know what marijuana or, or other street drugs could be laced with.
Susan Stone: Right. And I, I was thinking one of the questions I wanted you to opine about is. How, if you're in college and you're drinking or occasionally using recreational drugs, how would a student know if what they're doing is within that normal college range versus heading to addiction?
What is the line between, okay. You're just having fun in college, a recreational user recreational user, between or. You need to get help. Is it grade slipping, loss of friendships? What are your thoughts?
Philip Van Guilder: so I don't wanna be vague about this, but let's, let's go back to what we mean by addictive behavior. When it's compulsive, when I have no choice, but to use.
When it's no longer a matter of it was socially fun, but when I have to use in order to feel normal. So what is it like for any, for everybody it's that day when you wake up and you say, you know, I can't face the day without a drink or I can't face the day without first lighting up a blunt or I can't face the day without getting a rig and loading it.
That's the day when it's gone too far. In fact, one of the newest organizations that we've seen start off in the last, I would say, I want to, and I'm guessing at this, maybe the last four or five years is young people in recovery on college campuses. We're starting to see a real big push for that because they're not learning how to use in college. They're bringing the addiction to college with them.
And so a number of places and, and there's a number of campuses around the country. Arizona was one of the first universities in Tempe was one of the first universities to have a young people on campus. I'm not trying to promote them, but they're just, I just remember meeting some folks that had come out to, to, to bring that template to other campuses around the DFW area.
And, and it seemed like people were gravitating towards it because they realized they had a problem. Now that's, I don't know, that's just taken off, but I know that today, when I'm talking to a young person, that's worried about going to school. Like I'm, I'm about a young 18 year old yesterday in a meet last night in a meeting.
And he said, he's starting on campus. So small. And I was able to direct him to a young people's group on the local university campus. So it was kind of nice to see him. Know that there's a safe place for him to go. He's been struggling since January of this year. It was kind of nice.
Susan Stone: Do you think it's gotta be very lonely to be a college student today in a fraternity or on a sports team and have to say I don't drink.
I don't, I'm an addict. Yeah. I, I can't imagine the shame, but you know, Kristina, we've had a lot of friends tell us, they're now sober curious. Mm-hmm , you know,
Kristina Supler: A question I had for you, Philip, Susan and I working with students across the country day in and day out. We, every day we're hearing terms like blackout, brown out, gray out and, and.
Binge drinking has, has really seems been, been normalized.
Susan Stone: We've seen deaths.
Kristina Supler: Yeah, actually we've had a couple different cases with a death component and it's an absolute tragedy. What are your thoughts on why. Students are indulging, whether it's alcohol or drugs to such extremes now. Do you think it's the influence of social media?
Is it the pandemic in mental health? Or, I mean, working with populations at Greenhouse, do you have any insights?
Susan Stone: Yeah, I was gonna say, Kristina, you know, we dealt with that one case where students drink whole bottles of alcohol. And I, I have to tell you, I don't remember that. Did you have that at college?
Kristina Supler: I mean, it certainly seems that in the news, there's more reports about fraternity hazing in, in student let's just say excess. And I don't know if it's because it's going on with greater frequency or just the media and other professionals are trying to bring more awareness so that students can be safe. But Philip, what are your thoughts?
Philip Van Guilder: I really, I don't think someone says, uh, this is the weekend I wanna binge. You get there with that compulsive addictive behavior.
It there's it's if you're truly let's use alcohol, let me separate that from other other drugs. Let's just use alcohol. We know that medically there's a craving component that comes people that are, that, that are alcoholics typically. If we look at the medical, uh, component, it says that we're not able to process or metabolize alcohol at the same rate of non-alcoholic is. Whereas a non-alcoholic can process about one ounce per hour.
We can't, we're missing certain components, genetically that keep us, or prevent us from being able to do that. So if we drink more than one ounce per hour, and what happens because we, we retain the alcohol in our system longer because we can't metabolize it. We can't discharge it. It kicks off the craving.
So the more we drink, the more we crave that's
Kristina Supler: oh, that's interesting.
Philip Van Guilder: That's medical thing, whereas you might drink one ounce per hour. By the time you get to the second or third one, you're going, uh, oh, I got a buzz. I'm sitting here thinking man, I need to have some more. I don't have a buzz. Like I want the buzz. You considered something that makes you uncomfortable and I considered something that's necessary.
Susan Stone: So that's why all of a sudden they're craving, craving, craving these students. And then all of a sudden blackout.
Philip Van Guilder: Yeah. Yeah, because the more they drink, the more they crave, I mean, at midnight, Joe and Charlie, talk about this two wonderful people that are in recovery that, that are both passed now, but that, that have the thing they took about at midnight.
After I've been drinking all night long. And I pass out in, the the parking lot of a, of a bar and I get run over by a car and you come over to help me. And the first thing I say is, when you say, what can I do to help you? And I say, oh my God, get me a drink. Like I still haven't had enough. That for me, the cravings kicked off at two o'clock in the morning.
My craving, my desire for alcohol is so much greater than it was when I started. Cuz I didn't have a craving until I put alcohol in my body. That initiated the craving. Hmm. The more, the more I crave
Susan Stone: I'm sorry, gotta ask. I'm so sorry. I didn't mean to interrupt. Um, oh, but does the craving ever go away or do you just learn to live with the learn to manage it?
Philip Van Guilder: Yeah. So, so that goes to the second component. It's the obsession of the mind coupled with the allergy of the body. If I don't put the alcohol on my body, I cannot kick off the craving. And what happens is after some period of time, I go, well, you know, I haven't had a drink in three weeks. Uh, I'm probably not that bad.
It I'm just gonna have one. And so I played this game that says I'm just gonna have one because it's been a while since I've kicked off the craving. The moment I put the alcohol in my body, I kick off the craving. I'm back in this cycle again. And I wake up once again in a, in, in the next day. I can't tell you what happened the night before.
And, and once again, I'm gonna swear off alcohol forever.
Kristina Supler: so with a long, let's just say, for example, a long stint of sobriety from, from any substance alcohol or drug drugs, if an individual has been sober for let's just say five years, does it get easier as time passes or do you still really have to be focused and dedicated to sobriety?
Philip Van Guilder: Right. So I, I wouldn't speak for others each journey's individual, but for the people that I've been around, the people that I hang out with, I'm sober coming up on just about 19 years. As I said to you earlier, I met a young man at a meeting last night. I go to meetings frequently. Mm-hmm , uh, two or three times a week.
Cuz I have a disease that tells me I don't have a disease. So for me, the easiest thing for me to do, cuz I used to spend all my time thinking about drinking. If I didn't, if I wasn't thinking about it, I was drinking. Today it's a few hours. I spend a few moments each morning, starting my day. A little prayer meditation, trying to connect with the power greater than myself and, and do meetings and do service work, carry the message to others.
But the only time I think about drinking is I go to a meeting that I am meeting a newcomer that's talking about drinking. I don't think about it. But that's my disease. so my disease is sitting there on my shoulder. Disease's telling you,
Kristina Supler: you don't have a disease. I've never, I don't that way.
Susan Stone: Interesting.
See, that's an incredible thought that the difference between your disease and let's say, God forbid someone with cancer is someone with cancer doesn't say I don't have cancer. But someone with alcoholism says, I don't have it. That's incredible. I wanna shift gears a little bit because Kristina and I work with students with mental health challenges, other mental health challenges.
And we know you do too. As you call yourself a mental health evangelist. And we see you've done a lot of work with the stigma associated with mental health issues. We've come a long way, our society as a whole de-stigmatizing mental health issues. But I'd like to know from your perspective, what do you think today remains as a stigma? If anything, or do you think it, the stigma's gone?
Philip Van Guilder: Oh, uh, no, the stigma's there. Until you have a loved one, that's struggling. It'll you said it, let's talk about substance use or we'll talk about mental health, even mental health issues. We're still the bottom feeders of diseases. I mean, if you tell somebody you got cancer, they're out there having a parade to raise money, to help you with your treatment.
You tell somebody that you've got a mental health issue or you're a, you're an alcoholic and they're gonna change seats so that they don't catch it. we're talking about it openly now. But that doesn't take it away because until it's actually a part of your family, or until you have a neighbor or until you have a loved one or until, you know, someone on a personal level until that happens, it's just a, a terrible thing that, that, that happens to other people.
And I don't wanna be around them because they're mentally not right.
Kristina Supler: Sure. Or, or it's a theoretical issue. That's, you know, a lack of discipline that right. Wouldn't happen in my family. My kids wouldn't succumb to that. So let me ask you on this topic of mental health and substance abuse, how much more difficult if at all, is it to, to treat substance abuse when there's other mental health issues present? Or is it sort of the same approach to treatments regardless of anxiety, depression and other comorbidities?
Susan Stone: That's a good question. And also we know a lot of students with mental health issues have to take medications like Ritalin. Or Adderall or they can't function and learn. But if there's also an addiction issue, I also always wondered, oh my gosh, that's really complicated.
Philip Van Guilder: This is a tough one because we, we have to stabilize the mental health component before you can treat the addiction.
What comes first? I mean, oftentimes the addiction was their solution for their perceived problem. It's really tough, but you gotta do 'em. They both have to be done together. But you can't treat the, the addiction. If you're not treating the mental health component and, and you can, and, and it's gotta be done in conjunction with one another.
If they're acute before you can treat the addiction, you have to help them get stabilized because you can't begin to pay attention. Remember I told you we're transferring knowledge to an individual. If the individual can't sit still and can't regulate, we can't transfer that knowledge. So now we've gotta find a place for them to go where they can be stabilized.
So, so that they can be okay in their own skin. It mean when you see certain people with certain mental health issues, they're climbing out of their skin. The last thing is they your solution, right? We can't take away your solution because you just you're already climbing outta your own skin.
Susan Stone: Yeah. You know, it's so interesting because Kristina and I will often have to have students get ready for their interview or for a hearing.
And we will notice that if there's a student and they have not taken their, let's say medication for whatever issue that's going on. It is very hard for us to work with those students because they're literally, they can't focus and they're fidgeting.
Philip Van Guilder: Yeah. I mean, what a dilemma. And then if it's addictive behavior, let's just say we, so let's say that they're, they're, they're normal.
They're regulated. And then let's say we've got 'em to where they're not. The alcohol or the, the drug component is manageable. Suddenly their sex addiction takes off. Mm. Or,
Kristina Supler: or we get this so interesting that you bring that up because we, we see that in, in so many of our cases where the addiction is perhaps a coping mechanism for other underlying mental health issues.
And sometimes one, addiction just sort of trades out for another. And so let me ask you, is it true that there is such thing as an addictive personality? Someone who's just naturally, whether it's baseball cards, coffee, substances, they, if they do something once they just really like it and they're all in and everything is to excess.
Philip Van Guilder: Well, I, I don't think, I, I think I'd leave that to the medical community, but, but I would say this, I think it's possible to have addicted behavior as opposed to addicted personality. Going to what you were saying, I mean, now we get the sex addiction under control. We get the, the alcohol addiction into control that we are regulated and suddenly we're sitting at the casino gambling.
Or we're or we're online shopping with Amazon, whatever it is.
Kristina Supler: Or overeating
Susan Stone: or overeating or food or over exercising or over, over, over, but over. Yeah. Is it, is it it's actually an addictive personality or is it a sign of just some other emotional need to fill a space or a void?
Philip Van Guilder: Uh, once again, I think I have to go to defer to the medical community as the causation.
Susan Stone: You know, we're gonna have to explore this more in our podcast, Kristina, and I wanna switch gears because I was reading a little bit about you to get ready. And I noticed that you also talk about eating disorders and I'm 56. And when I went to college, I knew many, many, many students who suffered from bulimia or anorexia.
And as also a mother who has raised and is raising daughters. I don't see the eating disorders as being as prevalent. And in fact, I see a lot more body positivity, uh, but I see more cutting mm-hmm a different type of, uh, form of control or relieving of mental health issues. And I just wanna know what your thoughts are on the topic of eating disorders versus cutting versus trichotillomania, which is the hair pulling hair.
Philip Van Guilder: They're all symptomatic and, and indicative of someone that's ill. And eating disorders probably. And I've gotta be careful for all my friends in the eating disorder community that I love all the professionals, uh, because I I'm around so many experts and I don't perceive myself to be an expert.
But I'm someone that's passionate about it because I see it as a very common trait. I remember at one point about 10 years ago, one of the big things going on, you were talking about college and it was mostly college. It was, it was sororites. So it was mostly the female side.
But there was this, uh, ability to inhale alcohol and women were, uh, using these and, uh, there was using like, humidifiers. And they would adjust alcohol that way to, to, to minimize the amount of weight they put on by consuming alcohol.
So they could get the effect of being's drunk it's they could get the effect of being drunk, but they wouldn't add weight. Yeah. Do you, so, and there's a, there's a name for it and I can't remember now, but we had a real rash of that I'm gonna say this about 10 years ago. Where we, that was the big thing on college campuses especially for sororities. They would have these parties where they would inhale through these misters alcohol.
So they wouldn't gain weight. Very prevalent.
Susan Stone: Hm. So what are you seeing now? That's coming in in terms of eating disorders in your centers.
Philip Van Guilder: Especially here at the greenhouse, we're, we're screening for it because it's, if, if you've got an alcohol or a drug disorder, you're very high on the spectrum of of possibilities of the eating disorder.
And, and in fact, we see quite a bit of that, uh, So it I'm getting the problem here. It says I should dial in. I'm not sure if that's correct. No, you're okay. Okay. So, all right, I'm sorry. I just got a warning and I I's sure, like NASA we're like about to do a launch. That's
Susan Stone: what makes this a real podcast?
Philip is that I start with the tongue twister, you get a tech warning and that's what makes our listeners know that is not scripted or canned and that we're being authentic here. That's
Philip Van Guilder: right. Oh, I love it. That's great.
Kristina Supler: Last question, Phillip, what is the best piece of advice that you can offer for our parent listeners out there in terms of what they should talk to their students about before heading off to college in the fall, or
Susan Stone: even on summer break right now?
Kristina Supler: Yeah, actually that you're so right. Susan.
Philip Van Guilder: Every parent, whether you see any sort of behavior, not statistically, your child is either connected with addictive behavior doing it themselves, or they know someone that is. But, but you've gotta start talking to 'em about resources, about no shame and ask, just talking about it, just being open about it.
We never talked about it and, uh, I remember, um, Uh, and this is part of my background many years ago. The way I got involved with eating disorders is I was on the board of directors of a ballet company in California. And I would listen to the artistic director line, the young people up, and we're talking young 12, 13, 14 year old students.
And she would call him, she would say, you're all fat. And I would ask friends of mine. I, I, it didn't seem to me that that was appropriate. And I would say to people that, that, that doesn't seem like a very nice way to treat young people. That's what I thought. That's just not a nice thing to say. And they would say yes, but you understand she's a balanchine.
She loves slender dancers. And I would go, oh, okay. Not realizing how much damage was being done by these statements by this adult, to these 12 and 13 and 14 year olds. That goes on today. We allow kids to make fun of other kids based on their body the, the visibility, and, and instead of being body beautiful.
It's like every advertisement today is still around slender body types. It's rare that we see a commercial with real people. And so I, I guess going back to your question, what are for adults, let's just talk about it. Let's just have a discussion about it. Let's just make it safe for people to come to us and chat with us about things they don't understand.
Susan Stone: Well, and we are so lucky that you came here to chat with us on Real Talk with Susan and Kristina. Because that's what the goal of our podcast is. We
Kristina Supler: always want to encourage parents to have open dialogue with their students about any topic, drugs, sex, alcohol, disabilities, stress management. Our goal is just to promote wellness for the student population.
So we're so pleased that you were able to. Today. Thank you.
Philip Van Guilder: Thank you. Thank you both very much. It was a pleasure to be here, right? Excited to be with you guys and exciting for what you're doing. Thank you.
Check out our Real Talk podcast! We talk about everything from consent, Title IX and #MeToo to mental health, autism, bullying and hazing, social media pitfalls, academic integrity, special education, student discipline and misconduct, navigating police encounters and staying out of trouble.
0 notes
Text
Days of Childhood
~::~ 10 Years Ago ~::~
Summary: 5+1, Visitation Day. Yancy palling around with his family. All taking place within the same week.
A/N: Bim and Yan are currently 21, making Yancy and Kay 22, and Illinois and Arthur 23. Meaning that here they are 11, 12, and 13 respectively.
5. Arthur- Bugs Alive:
“Come on, hurry up,” Arthur called out, his notebook clutched to his chest as he ran off, Yancy was struggling to keep up with all the rocks and tree roots.
The two boys were running around the spooky woods surrounding the Manor. No wild animals, except for insects and rats, could be found. Normally people who entered the woods became lost and died. Dark took great pains to hide the skeletons that could be found within the unhallowed woods.
Yancy only caught up when the young Author had stopped at a fallen tree that was covered in mushrooms and other fungi, moss covering the rotting wood in sickly patches. He looked giddy and excited, holding a large jar along with his notebook.
In later retellings, Yancy would admit to this being a huge red flag.
“There you are slowpoke,” Arthur shoved the jar into Yancy’s hands. “I need some bugs so I can study them for my stories.”
Unsuspecting, Yancy smiled, “Can I look at them too?”
The young author shrugged, “Sure, whatever.”
“Did you hear?” Arthur started, smiling mischievously, cracking his notebook open. “Dark gave me a nickname, like the kind his network have.”
“I thought we weren’t allowed to join,” Yancy reminded in confusion.
“Well I’ve got one, that means I’m better than Illy,” with a couple quick words, the entire tree trunk violently flipped over, exposing dozens of types of teaming insects out in the open. “No one else here has one but me.”
Yancy frowned at the snide look on his older adopted brother’s face, “Bim goes by Junior.”
“He doesn’t count,” Arthur snapped angrily, and ripped the jar away and started scooping up insects, uncaring if they crawled over his hands to get away from him. “Wil gave him that.
“So what’s your nickname then?” Yancy asked.
“Dark calls me “his little Author” neat huh?” Arthur smiled proudly as he screwed the cap on and smiled at the jar.
“Yeah,” Yancy leaned in to look at the bugs. “So where are you going to hide them? Dark’ll get mad if you bring them into the house.”
Arthur wrote another couple of words and his bat appeared at his feet, a smile on his face, “What do yah mean, Yanc?”
Yancy scurried back with his hands as Arthur brought the bat onto the jar, crushing many insects as others frantically tried to escape. The young author crushed one trying to flee, bringing up his notebook and making sure they all froze in place. “Where do you think you’re going?”
Sick to his stomach, Yancy tried to scoop up some of the insects, the little crawlers freed from Arthur’s powers when they touched his hand, and he flung them into the safety of the bushes.
“Hey, they’re mine!” Arthur shouted. “Don’t throw them away.”
“Run little bugs,” Yancy scooped up some beetles and a worm and threw them into the bushes.
With a couple flourishes of his wrist, an equal number of bugs that Yancy had saved, exploded. “I can kill them faster than you can take them.”
Yancy stuck out his tongue, scooping up another beetle, “You can’t stop me!
Their game continued, Yancy running back to the Manor with a bloody nose and Arthur more than a bit scratched up.
4. Illinois- Heroes and Villains:
Inside the Manor there were two young boys running around the house, one as, and the other who was in a kid’s brown fedora that tended to fall over his eyes was 13.
“Stop running,” Illinois yelled at Yancy. “You’re the hero, you’re supposed to chase me.”
“Youse always play the villain, I’s want a turn,” Yancy yelled back at him and tripped over the rug, crashing hard on the ground.
“Oww,” Yancy grumbled as Illinois jumped onto him and started tying up his feet.
“Gotcha!” Illinois cheered, “now it’s . . .”
The older boy paused for a bit, “You okay.”
“Yeah it just hurts,” he complained.
“Oh,” Illinois stopped and finished tying him up, grabbing a blanket that had been left on the couch. “You can be the villain for a little bit long if you want.”
“Youse gonna ta drag me ta jail?” Yancy asked, smiling and giggling when Illinois rolled him onto the blanket.
Illinois grabbed the blanket and began dragging it towards, “You’re going to jail for stealing a candy bar!”
“No!” Yancy yelled overdramatically.
Illinois picked up a corner of the blanket and began dragging him towards the nearest closet. They passed Dark who was outside his office and looking at them, unimpressed.
“You two aren’t playing that game again are you?” He asked.
Illinois adjusted his hat so it wasn’t over his eyes, “Yes?”
Dark groaned, “Play that outside, you’re going to break something.”
“OK, Dad,” both Yancy and Illinois agreed and Illinois began dragging Yancy and the blanket towards the door.
Because both of them were turned away they missed the scared look on Dark’s face at the title they’d give him. Fear that quickly gave way to a colder mask. “It’s Dark.”
Both the boys frowned,, correcting themselves before Illinois finished dragging Yancy onto the back patio and then carried him down the stairs to the lawn where he grabbed a couple croquet pins and made a little small fence around him. Both boys unaware that Dark was watching them from the balcony
“There,” Illinois said proudly, hands resting on his hips. “I won.”
“Yeah, yeah,” Yancy complained. “Whatever. Untie me already.”
Illinois tapped his chin, “Nah, untie yourself.”
“Noisy!” Yancy yelled. “Get back here!”
Then Yancy noticed a danger sticking out of the ground. Quickly Yancy rolled over and grabbed the knife and began cutting himself free.
“Hey!” Illinois began racing for the patio stairwell door as Yancy finished cutting himself free. Since the knots were tied by a thirteen-year-old and Illinois hadn’t actually meant to keep him trapped indefinitely, it didn’t take long.
However, now Yancy was chasing Illinois around with a knife in his hand as the boys ran up the stairs. Dark quickly snatched the knife out of his hand the first chance he got.
“Dark, he cheated!” Illinois called out.
The Entity was just sipping from his coffee cup as the two boys raced around him. “You’re the villain now, get away from him.”
Yancy and Illinois kept running around the backyard until they got exhausted and Dark brought them inside for a nap and a snack.
3. Kay- The King of the Squirrels:
Kay was arranging some of the stuffed animals he owned into a pile. The young boy had a red blanket tied around his neck. Dark and King were in a bit of an arms race. King always asked for a pet, every birthday, Christmas, and Thursday. Dark, sick and tired of always saying a two-letter word over and over again bet he could find any stuffed animal and if he was ever unable to, Kay could have that animal as a pet.
It was bet Dark had yet to lose, which led to an arms race of Kay finding different names for animals, and a very extensive stuffed animal collection.
Yancy jumped out of the pile, and raised a stuffed platypus above his head, “Found it!”
“Uh, they don’t hunt squirrels,” Kay reminded him.
“What do they eat then?” Yancy asked, trying to get out of the pile without knocking the whole thing over.
“Bugs, worms,” Kay shrugged and grabbed a leopard plushie. “Here, cats can eat squirrels.”
“But I’s like the platty-pus,” Yancy complained.
“Bring them both,” Kay shrugged, and Yancy took the leopard and held both of them in his arms in a warm hug.
Out of all of his siblings, Yancy liked spending time with Illy, but he always thought Kay was the nicest. The boys ran outside, to where Kay had hidden some of his favorite stuffed animals, his squirrels, up into a tree towards the edge of the tree line into the creepy forest. Wil had magicked them all up a treehouse. Dark had been less than impressed, only agreeing to keep the kids’ new “wooden death trap” when Wil demonstrated its sturdiness by getting up and jumping up and down on the thing and not fall through the wood.
King usually spent all his time up in the treehouse. And Yancy waited at the bottom until he could throw the toys up and climb up.
The afternoon was spent peacefully playing with the stuffed animals.
2. Bim- Starlight, Starbright:
Yancy and Bim were out on the front lawn, sneaking out late at night to catch fireflies. Normally Dark let them stay up late all summer collecting bugs and sleeping in the backyard. But for the last few days he’d been keeping them all inside, constantly watching them any time they went near the backyard. He promised them that whatever was lurking around the area would be gone soon and they could go back to enjoying the stars and bugs.
And if Yancy heard Dark screaming and fighting something in what he was pretty sure was a dead, haunted forest, the young boy was too nervous to talk about it with anyone else.
Bim jumped, his glasses almost falling off his face. He caught another firefly in his hands, cupping his hands around it, “Yes!”
Yancy was catching another firefly and carefully putting it in a jar where there were already a dozen fireflies buzzing around inside. After the fiasco with Arthur, he kept a tight grip on the insect jar, even though Bim had never ruthlessly tortured insects before.
The two boys kept putting little lightning bugs into their jar until Bim was finally satisfied. “Yeah, look at them,” Bim cheered. “Aren’t they cool, their little butts glow.”
“Yeah, ain’t they something,” Yancy agreed, before noticing that the fireflies were disappearing from their backyard, as if they were being chased. “I’s think Dark’s comin’ we should get inside.”
Bim frowned, “I didn’t even get my wish.”
“We’ll make it inside, come on,” Yancy began running inside, both boys missing the slowly gathering black mist that was in the treeline as the two boys raced inside and up into Bim’s bedroom. Only then did they giggle a little bit in the darkness, the only light was from the little bugs in their jar.
“Let me make the first one,” Bim reached for the jar.
“No, you’ll let them all go,” Yancy reminded, holding the jar away from him. “Come on, I’s never get the first one.”
He pouted, folding his arms like Wil tended to do, “Come on.”
Yancy moved over to Bim’s window and began to open it as Bim swiped the jar and grabbed one of the bugs, pinning it to his hand with his almost invisible aura. Yancy lunged for the jar to close it, but two glowing bugs escaped through the window. “Hey!”
“I want to be just like Daddy when I grown up,” Bim wished, blowing gently on the insect and allowing it to fly off.
Yancy was carefully getting another lightning bug on his own finger so he could make his own wish: “I’s wanna be a good person.”
Bim scoffed at that, but only ordered, “Give me another bug, I’ve got more wishes to make.”
Glaring at him, Yancy fought over the fireflies until they were all gone and Bim closed the window, all their troubles safely locked out of Manor.
1. Yan- Teddy Bear Picnic:
Yancy was sitting out in the back lawn with Yan, a little table between them and as many chairs as the little table could fit with a teddy on each chair. Each bear had on a bow tie and a frilly hat and a full tea party in front of them.
Yan was in a nice little red dress while Yancy was in a bow tie,
Two of the bears belonged to Yan and Yancy respectively, and the other three were politely and quietly “borrowed” from Kay’s collection.
Yan kicked her feet a little bit as she poured tea for the bear next to her.
“Why do you always give tea to her first?” Yancy complained.
“Because Ms. Talia is a lady,” Yan said.
“Youse been sittings’ there pouring her tea fer ferever,” Yancy reminded.
Then suddenly the whole table jolted, Yan and Yancy froze and leaned away from the table, Yan gasping in horror as her hard work was mostly tossed to the floor.
“Rawr! Rawr!” Artie began growling excitedly as he moved underneath the same tablecloth.
“Artie!” Yan got up and stomped her feet angrily. “You wrecked my tea party!”
“I’m not Artie,” Arthur said. “I’m a sea monster.”
“There’s no sea monsters at tea parties,” Yancy reminded sharply.
Arthur frowned, “Then you’re having a lousy tea party.”
“No,” Yan spat. “I don’t want sea monsters at my tea party!”
The young author frowned, before growing a bit and running off with the table cloth.
A chase ensued on the back lawn, the two kids chasing their older brother until they could rip the cloth away and slowly start rebuilding their little tea party. With Artie the sea monster in sea monster jail until the end of the tea party.
+1. Dark and Wil- Bruised Egos and Bloodied Knuckles:
It began simply enough. Arthur had brought a rat into the house, and Kay had been excited. A secret little pet to hide from Dark for a while.
Kay named him Pretzel.
The poor creature barely lasted an hour. It was in debate for the rest of Arthur’s existence on what had happened to the rodent. Whether he was jealous of the rat spending more time with Kay, or he simply got bored of it.
Either way when Kay snuck off to check on Pretzel, the rat was gone with only a couple specks of blood on the floor of its cage.
He angrily went to confront Arthur, who was watching a show with Wil and the other kids. Arthur feigned ignorance and Yancy jumped Arthur for killing another creature, trying to separate him from his notebook and hold him down.
The fight resulted in Arthur getting a black eye, Kay getting some scratches to the face, and Yancy getting one of the last of his baby teeth getting literally kicked out of his skull.
Wil was trying to separate the three boys with his aura, and looked relieved when Dark ran in and grabbed Arthur, the two porting over to the young boy’s room.
With Arthur gone Kay finally stopped fighting and just started crying, Yancy crying a bit at how upset he was.
Yancy was given a lollipop as Kay spoke through his tears. “He killed my rat, he killed Pretzel.”
“There, there,” Wilford waved another lollipop into his hand and did a little magic trick. “You’ll see Pretzel again. He didn’t die.”
“Wil!” Dark walked in, looking unhappy. “Don’t make it worse.”
“Kaylor if you wanted another rat toy I could have given it to you,” Dark reprimanded, summoning up a little rat plushie in his hands and holding it out to the boy. “You shouldn’t be fighting with Arthur over a rat.”
Kay glared at the toy and pushed it away, “I don’t want a toy, I want Pretzel.”
Dark took a deep, audible breath, and handed Yancy the toy instead. “We can’t have a pet, and this is why. Be lucky you got as long as you did with the thing.”
“Pretzel,” Yancy corrected.
Rolling his eyes, Dark corrected, “Pretzel, fine. Be lucky you got any time with Pretzel. No one in the house can control themselves, and any other pet will not last. Hopefully Pretzel escaped on his own.”
Dark picked Yancy up with his aura, setting the boys side-by-side as he talked to them. “Just imagine that Pretzel escaped and is living with the other rats. If that makes you feel better.”
Kay nodded and Dark smiled as he dried Kay’s eyes, “I’m sorry we can’t have the pet you want, and maybe one day you’ll get to actually own a pet.”
Giving a small smile, Dark smiled back and smooth out Kay’s slight curly hair.
Then he turned to Yancy, “As for you.”
“What?” Yancy argued back.
“What were you thinking?” Dark demanded.
“Artie killed Pretzel an’ might use his book ta hurt Kay,” Yancy accused.
“How do you know he killed it?” Dark quizzed.
“Because he smashed a jar a bugs an’ he hit me,” Yancy answered as Dark just stoically stared at him.
When Yancy finished, Dark summoned up his favorite candy bar and held it up in front of the young boy.
“Listen to me, Yancy, you need to always protect your siblings, even if sometimes you have to protect them from each other.” Dark had the softest look in his eyes that Yancy had ever seen. When Yancy reached for the candy bar, Dark’s looked hardened and he pulled it away.
“This isn’t a free license to beat up on your brother, do you understand me?” Dark demanded.
“Yes,” Yancy replied earnestly.
Dark smiled and gave him the candy bar. Turning back to Will he said, “Well hopefully Arthur’s calmed down a bit. Can’t leave him in his room all day.”
Dark ripped open a portal in the Void and walked through it, leaving Wil to take the kids back to the living room where then TV was waiting for them.
#Superhero AU#Masks and Maladies#Visitation Day#5+1 things#senseless killing of insects#Markiplier#Darkstache#ahwm Yancy#kid!Yancy#the Author#kid!Author#ahwm Illinois#kid!Illinois#King of the Squirrels#kid!King#Bim Trimmer#kid!Bim#Yandereplier#kid!Yan#early onset child psychosis#domestic fluff#mostly fluff#Dark has problems with his emotions#he’s doing his best#justice for Pretzel the rat
18 notes
·
View notes
Text
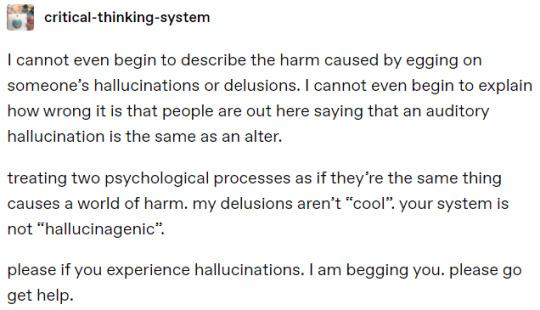
@critical-thinking-system
Just another reminder that while not all hallucinations are inherently headmates, actual DID specialists believe that certain voices in these cases are parts of dissociative systems. Just bullet pointing the most relevant details. But please, if you can, read the entire article. It's very informative.
The complex and multi-faceted relationship between dissociation and psychosis has been the subject of study in the dissociative disorders field for over thirty years
...
A key finding in this literature is the fact that Schneiderian first-rank symptoms of schizophrenia, including auditory hallucinations, are more common in dissociative identity disorder (DID) than they are in schizophrenia (Kluft, 1987; Ross, 1997, 2004). There are only a few qualitative differences between the voices in DID and those in schizophrenia (Dorahy et al., 2009; Honig et al., 1998; Ross, 1997, 2004): there are more often child voices and the onset of the voices is usually at an earlier age in DID than in schizophrenia, for instance.
...
The decision to begin a trial of psychotherapy for psychosis using techniques from the DID literature, which we will describe below, need not hinge on the diagnosis, or a decision as to whether the Schneiderian symptoms are “psychotic” or “dissociative.” We believe that, irrespective of diagnosis, patients presenting with hallucinatory voices that comment on one’s thoughts or actions or that have a conversation with other hallucinated voices, can often be treated effectively with psychotherapy. On the other hand, voices that are merely mumbling, repeating single phrases, or are incomprehensible, are unlikely to engage in psychotherapy.
...
The authors believe that in many of the cases that do not respond well to standard interventions, including medication, unresolved internal conflicts and traumatic issues could explain the maintenance of symptoms. The internal system of the person has organized itself into dissociated parts that hold thoughts, feelings, memories, and impulses that were intolerable for the individual. Some of these dissociated aspects of self are often angry and often converse with each other and with the part of self in executive control.
...
A key aspect of the work with hostile parts of the personality and voices is to listen and understand their function and the meaning behind their disruptive behaviors. The less we listen and the more the voices are ignored, the more they tend to scream or escalate their behaviors in a desperate attempt to be heard. If both clinician and patient understand this, we have the basic ground on which to begin building a good alliance with the whole system of parts and voices.
...
The work with the dissociative system might be more cognitive than emotional in the beginning, since dissociative clients will not be ready to feel emotions in early phases of treatment.
There are definitely many cases of voices that are not headmates. The ones mentioned that won't respond to psychotherapy, which are just mumbling, repeating single phrases or on incomprehensible.
But literal DID specialists are saying "hallucingenic" systems exist, and that they believe people experiencing complex and intelligent hallucinations are dissociative systems. And they're actively recommending the same exact methods used in treating persecutor alters be used for treating persecutory voices in people with psychotic disorders.
I've seen a lot of discourse over the term hallucingenic. In fact, from what I understand, the coiners were basically harassed into deleting their post (and possibly their account) because people claimed it was harmful misinformation. So I want to set the record straight and say that not only are hallucingenic systems valid, but that they have the backing of actual professional DID researchers who believe that treating certain hallucinations similar to alters is beneficial to the system.
#syscourse#psychiatry#psychology#mental health#therapy#plural#plurality#plural system#endogenic system#endogenic#actually plural#system stuff#multiplicity#hallucingenic#science#discourse#system#actuallyplural#pluralgang
76 notes
·
View notes
Note
Spencer got a spoon as a special friend first because it had some nice indents on the handle (it was also from Diana's house and she always gave that to him while he was teething as traditionally spoons could be given to babies and Diana liked to use some old-fashioned methods). But around age 3 the spoon got lost/got thrown out and Spencer just cried and cried for days and no one could figure it out what was the problem because he couldn't explain it and never referred to it as spoon 1/2?

HFHDJDJDKSDK
The intensity of the Nikola fantasy leads Hotch to take Spencer to a child psychologist with concerns about early onset psychosis, because of Diana. The doctor tells him nothing is wrong, Spencer is just weird
51 notes
·
View notes
Note
And I hate to do this- So on that thread, not that he's as bad, why do you think Michael is redeemable? (and also Frank) Especially by his main victim? :? I hope that isn't as bad or as judgmental as I think it sounds... - Sleepy (its like 5am here :3 living up to my name i see)
So, these I gave a short and a long answer for under cut, but forgot I’m on mobile and can’t do that. I can tag it “long post” but uhhh, sorry about this. Anyway, thats why Frank comes in two chunks. I wrote it expecting to be able to use a read more. :’-] also ya fine. And I hope you’re in bed 🤣 now. Okay so. Here’s my reasons:
For Michael, to start, Halloween is complicated af. You have to know what timeline people are talking about, because there are like 8+ and Michael has been written as a wildly different character by wildly different content creators, and I would not feel the same ways towards them all. They’re not the same character. When I talk about Michael, unless I’m going on about a specific other film, I mean either H20 canon, or DbD canon, which are in line with each other when it comes to characterization. (This also includes Halloween’s 1 & 2 in the H20 line, and Halloween 1 at least in DbD). In those timelines, Michael has like at best 2% agency and choice in his own life and what he becomes. That’s why I am sympathetic. I still root for Laurie to nail his ass to the wall of course, and everything he has done to hurt someone isn’t okay just because his life is unfair & awful & out of his control, but I still find him a very tragic character. He was canonically suffering violent psychosis his parents refused him treatment for, isolated with a monster as his doctor & only human contact for 15 years from age 6 on, overdosed on medications that when OD’d worsen psychosis symptoms and can cause permanent brain damage, and stuck like that until escaping briefly when he turned 21.
In Halloween canon, Michael tells his parents he hears voices telling him to do bad things like hurt people, but they tell him he is imagining stuff, and ignore his attempts to get help. The voices say they will be quiet, which is what he desperately wants, if he kills his sister Judith. So he does, at age six. Scientifically speaking, that’s literally too young to really have a complete grasp on death and mortality itself, let alone complex ethics. He immediately goes to his parents after doing the deed, so they can do whatever they need to do. Instead of getting him help, he is sentenced to 15 years in a 1960s American sanitorium (hell), until he turns 21 and can be tried for murder as an adult (fucking ridiculous and unfair?? Tried as an adult is for like, upper teens who commit heinous murders. How tf you justify trying a six year old literally too young to really understand murder as an adult for murdering someone??). They give him to Dr. Sam Loomis, a fucking horrible person, who says he spends 8 years trying to help Michael (a fkn lie), but canonically by only a few months of meeting the kid is thoroughly convinced he is evil, the devil or a demon in human form, faking his psychosis and side effect symptoms (trauma induced mutism from killing his sister, onset of catatonia/motion loss symptoms, etc, all of which are common with his disorder & trauma), desperate to kill again, and an evil mastermind doing the devil’s work, and says so. Spends four hours every day accusing Michael as a six year old child on, of planning to do horrible things and faking his illness and being a demon and not a human, and Loomis, from age 6 to 21, is this kid’s only human contact. And the staff knew it and how wrong and disturbed Loomis was, but did nothing. So from age 6 to 21—barring one or two visits from his mom & Laurie before his dad beat 4 year old Laurie for saying Michael’s, who he hated after Judith’s death, name—until she trauma blocked out having had a brother or sister at all, and then both parents died in a car crash—his only human contact in complete isolation was an adult man who told him for four hours a day he was an evil lying demon faking his symptoms and plotting murder and not a human and promised he would kill Michael and stop him, from childhood on, and that was it. He was never given an understanding of what was medically wrong with him, or that anything was at all. He was threatened and abused and kept overdosed on drugs for 15 years since early childhood, and his only understanding of the world taught in that absolute isolation, was that he was a demon who wanted to get out and kill again. And the violent psychosis, telling him if he killed both sisters, they would go away and leave him in peace with no more constant noise. With no normal understanding of the world or people or life like he was owed ever given to him, no understanding at all of what you were going through or were aside from the promise drilled into your head you were a monster who wanted to kill every day for 15 years while drugged up? Like, I’m a firm believe people are responsible for their own actions, but in a case as extreme as that, honestly, how else was that ever going to even be able to end? You forget, as a child. Who you used to be. That’s beyond grooming even, it’s being grown in a lab for the sole purpose of someday walking out, taking a large kitchen knife, and killing Laurie Strode. And it’s tragic. It’s unfair. Halloween is a tragedy, not a horror film. It didn’t have to be that way. He wanted help. He asked for help. Loomis is directly and pretty much solely responsible for the lives lost in 1978. You know he won’t even call Michael “him”? The only human he contact he had since age six on called him “it.” And no one stopped any of that. And even then. Even then, even with all that. With the drugs, and the lab grown killer, and all of it? Michael is pretty much the single least sadistic slasher killer there /is/.
Everyone he kills in Halloween? He kills fast. It’s actually kind of boring if you’re expecting a scary slasher, because there’s no chase until Laurie. He just appears, runs you through, and you die. Very fast. And if there is any emotion expressed towards the act of killing or aftermath, it’s not pleasure or hate or happiness, it’s curiosity, because literally everything is something he wasn’t allowed to experience growing up and just has no practical experience with yet. And on top of all that, he also just doesn’t kill people he doesn’t have to. He kills one man for clothes, kills Annie to re-do Judith’s murder since it didn’t work the first time and he needs both sisters for the voices to stop, and he kills Bob and Lynda becuase they stumble onto where he is & are a threat to success. (This + Judith 15 years prior is all the deaths in Halloween period, btw). Michael routinely only kills his target, and anyone who is a threat to success. Literally doesn’t even jump out to kill Bob or attack until Bob opens the door to the closet he was hiding in, and he has been seen. Walks past a security guard and lets him go in H20 becuase he doesn’t see him, steals keys from a mom with her 4 year old kid and doesn’t even hurt them because they don’t see him really either, steals a knife from an old lady making a sandwich who is one foot away but looking the other direction, so he lets her go. Even with all the possible stakes against him, really, Michael is like, the least cruel and most sympathetic and merciful version of that lab grown killer possible, which can only be a testament to the person he was initially/still somehow has managed to keep faint traces of alive inside.
As for Laurie finding him redeemable, answer is threefold I guess, and I’ll start with the most important. 1: in Halloween canon, Laurie cares for Michael and is incredibly sad about what he turned into and wishes he could be different (once she remembers who he is). That’s established canon, not a choice of mine. In Halloween 2, she tries to talk him down before shooting him, and he hesitates when she says his name and lowers his weapon for a moment. In H20, she talks about him a lot & even asks her boyfriend (a psychologist) if he thinks something so traumatic can happen to someone that they can never recover, bc even though she hasn’t seen him in 20 years, he’s still on her heart. She hesitates to kill him once she has him helpless in the finale, and when he reaches out for her hand, she almost cries and starts to reach back because it’s what she has truly wanted for so long. 2: Michael & Laurie are siblings, and that’s a very important relationship to me. Obviously, there’s lines where you cross, it’s fkn over, but it is special, and I’m weak for it. They were both cheated of the good family life they could have had, and I like characters I care for getting recovery and rehabilitation, and I would like them to be able to recover and have whatever fragments of the lives they wanted which are still possible. And then 3: Laurie is his victim, but they’re also both victims of Loomis, and the system, and her parents, and if she does /wish/ for him to be okay and things to be like they were, which was canon before me, so she does, then I think them finding happiness and her relief and new hope in regained family and him redemption and rehabilitation through the quite literally only person he has /ever/ known who treated him well or like even a human at all & is still living, that’s so good. It’s sweet, and it makes sense. I like broken people putting the pieces together and finding ways to be okay. None of the shit that happened to either of them was okay, and Michael sure did fucking do it, but it’s about as “it’s complicated” as literally possible, and Laurie wants him to be her brother again, and Michael deserves a chance to experience personhood enough to want anything like that again too, and I think it’s sweet. To be able to find happiness and peace and a new life in that rubble. It shouldn’t be possible, because Halloween is a tragedy that never gets a happy ending, no matter how many timelines they create or versions they tell, but I wish it could have one. It needs one. At least one, among all the fated tragedies for those two cruelly cursed siblings. They both had their lives stolen. Michael by Loomis, and Laurie by Michael. And I want them to find those stolen lives again. And if they can do it together, that’s a very odd and unusual set of circumstances for that kind of thing, but it’s a very complete way to tell the story. He tried to kill her, but if she asked him to stop and he stopped, if he himself chose to change on his own, when it really, really mattered—decided that it was what he wanted more than all the things he was before, and she decided that was enough, and they could both have a future as family? I like that. It’s a happy ending stolen back.
Long Frank Answer, in case you /have/ read ILM & thus short answer did not answer your question: So. Again, for me, I always talk about Frank as in the version of him I myself write, and I wrote ILM before the archives retcon, and also just ignore them because they’re usually dumb and blatantly contradict well established and longstanding canon. Even then, I usually don’t like Frank though—didn’t like him when I started writing ILM. But Frank has very little established canon character. All there is for sure is he was a foster kid that went through some bad stuff, he met Julie and changed his mind about desperately trying to be homed somewhere other than with Clive bc he liked Julie a lot, he met Susie and Joey, they became a gang chilling in Ormond’s abandoned lodge, then tried to rob a store Joey was fired from, were surprised by a cleaner who grabbed Julie, and Frank impulse stabbed him, freaked, and ordered the others to finish it with him and be in it together. Then before they’d even really finished burying the body, they got snagged. That leaves a whole lot of personality and thoughts and motivations and future choices and person wildly undetermined. Writing, sometimes characters just do their own thing completely out of my control, and I have to adapt. Frank chose not to kill Meg at the end of Tenacity, Adrenaline, & Grit, which surprised me, because he’d been nothing but a dipshit asshole bastard till one minute ago, but I knew it was because he recognized what she’d tried to do at great pain to herself because she wouldn’t bow down and die, and he connected/empathized or sympathized on some level. He also couldn’t go through with killing Quentin immediately after being helped by him in Distortion/Iron Maiden. Neither was like, planned. It’s just who the character was. I was frustrated. I did not want to like or feel sympathy for Frank at all. Then in The Lost, Jeff just fkn hijacked the whole plot and added 20 pages not in the outline because he wanted to be kind to Frank & it’s not like I can stop characters when they do whatever they do. And while writing it, I got to know that the version of Frank Morrison in the world I was writing—which is always the version I refer to/think of him as & write now myself—was not somebody past saving. He’s a piece of shit and he’s done fucked up and inexcusable stuff, and he pays for it. In many ways, Frank gets away with a lot over the course of ILM, but it’s always because characters choose on their own to forgive him, not because they or he doesn’t think it was fucked. And Frank suffers—a lot—for his choices, and has to live through appropriate and large amounts of regret and remorse about stuff he did before the end. He gets the chance to make better choices several times, and mostly he doesn’t. He continues to fuck up. But right near the end, he makes a couple good decisions when it’s down to the wire, sees where his bad choices got him and what he has to live with, and then he does live with it. He almost dies, and then ends up falling on Jeff’s mercy, which he knows he doesn’t deserve and doesn’t expect to get, for a last chance to make it, and because Jeff is an ungodly kind and forgiving soul, he makes it.
Frank isn’t a good person, and he does a lot of stuff that isn’t remotely okay or justified or excused, but he /is/ a kid—the upper end of it, but he’s not a full grown adult. He has every reason to believe nothing of himself or others, a fucked up childhood and life which isn’t his fault, and the Entity got all four Legion kids before they’d even had time to process the one and only violent crime they did (which was unplanned), and it is historically running a PHD in psychological warfare vs everyone. Absolutely none of that excuses or justifies him, but it is an explanation for some of it that is not as bad as say, doing that shit for fun or cruelty or hate or what have you, which makes him a bad person, but one with a lot more humanity left than say, Kenneth. Who is at -100 or something. If he’s still got a lot of humanity left, that means he could be redeemed, and he eventually chooses that path for himself and hits the appropriate “I did something horrible. Fuck. It was really bad. I should not have done it.” “I am really sorry I did this. I feel awful. I’m sorry.” “I cant change it, but I can try to do better and make whatever reparations I can.” “I want to be better, and I am going to try.” necessary stages of actually trying to improve. So, I like him. He did a lot of really awful shit that wasn’t okay, but he was never without sympathetic elements. He does love his friends and his girlfriend, he is a good boyfriend to Julie and selfless towards her and his crew (overall anyway—has even risked death for them very willingly, even the one who was fighting with/kinda hated him), will keep his word in deals and has some semblance of both sympathy and honor, feels guilt, is a kid, did not choose this life but was rather catapulted into it and too weak to climb out once he landed in the mud. All of that together makes him someone I feel sympathy towards and find quite redeemable, so long as he will decide he wants that, which, in ILM, he does. If you just meant Frank in general then idk how to answer because there’s not much established Frank period it’s kinda a shell like all original dead by daylight characters, and I have no thoughts on it by itself because it’s not a whole person, and so I really only think of Frank as ILM verse Frank now.
#ask#sleepy#hope this is coherant. I love answering but I’m also on vacation trip rn so I’m not proofreading & u get what u get 🤣 adds flavor#in living memory (fic)#in living memory#spoilers#ILM spoilers#Halloween#dead by daylight#long post#Michel is not the villain of Halloween: he and Laurie are both the victims & it’s a fkn Greek tragedy#they both deserved so much more than the lives they were thrown into#: (#sad now just thinkin bout it
12 notes
·
View notes
Text
Iris Publishers - Current Trends in Clinical & Medical Sciences (CTCMS)
Suicides and Suicide attempts among Child and Adolescent Psychiatric Inpatients in Iran
Authored by Saeed Shoja Shafti

The WHO report “Preventing suicide: a global imperative” published in 2014 estimates that over 800,000 people die by suicide, and more than 20 million attempts suicide each year. This implies that every 40 seconds, a person dies by suicide somewhere on the globe, and every 1.5 seconds, someone will attempt to take his/her own life. However, those numbers are underreported, as not all countries in the world report suicide mortality to the WHO Globally, suicides account for 52 percent of all violent deaths in men and 71 percent of all violent deaths in women. In high-income countries, 79 percent of violent deaths in both males and females are caused by suicide. Suicide occurs in all regions of the world and throughout the life span, and it accounts for 1.4 percent of all deaths worldwide, by that, ranking as the 15th leading cause of death [1]. Suicide is rare in childhood and early adolescence and becomes more frequent with increasing age. The latest mean worldwide annual rates of suicide per 100 000 were 0.5 for females and 0.9 for males among 5-14-year-olds, and 12.0 for females and 14.2 for males among 15-24-year-olds, respectively. In most countries, males outnumber females in youth suicide statistics. Although the rates vary between countries, suicide is one of the commonest causes of death among young people. Due to the growing risk for suicide with increasing age, adolescents are the main target of suicide prevention. Reportedly, less than half of young people who have committed suicide had received psychiatric care, and thus broad prevention strategies are needed in healthcare and social services. Primary care clinicians are key professionals in recognizing youth at risk for suicide [2]. In ten years follow up of eighty-eight subjects with adolescent-onset psychotic disorders, mainly schizophrenia and affective disorders, 4.5% of subjects had died from suicide while another 25% of the subjects had attempted suicide [3].
In the context of suicide, there is a growing body of evidence showing that exposure to early-life maltreatment can affect molecular mechanisms involved in the regulation of behavior through methylation and histone modification, supposed to induce behavioral deviations during the early development, and possibly later in life, affect genes involved in crucial neural processes. This mechanism is called epigenetics. Childhood abuse and other detrimental environmental factors seem to target the epigenetic regulation of genes involved in the synthesis of neurotrophic factors and neurotransmission [4]. On the other hand, some scholars believe that People with first episode psychosis (FEP) are at increased risk of premature death, suicide [5]. According to the findings of a study, the rate of attempted suicide among young people undergoing treatment for first episode psychosis was around 12%. Of these 72.6% attempted suicide on one occasion. 85.3% of attempts occurred when patients were treated as outpatients and were in regular contact with the service. 77.6%of suicide attempts tended to be impulsive triggered by interpersonal conflict or distress due to psychotic symptoms. Two thirds involved self-poisoning, usually by overdose of prescribed medications. All inpatient suicide attempts were by hanging or strangulation [6].
So, Individuals with a first episode of psychotic illness are known to be at high risk of suicide, yet little is understood about the timing of risk in this critical period. Suicide risk was highest in the first month of treatment, decreasing rapidly over the next 6 months and declining slightly thereafter [7]. In this regard, longer duration of untreated psychosis, greater symptoms of depression, and positive symptoms of psychosis were found to increase the odds of experiencing suicidal ideation in first episode psychosis [8]. While according to some studies depressive symptoms during the index psychotic episode and comorbidity with stimulant abuse at baseline were relevant predictive factors for suicidal behavior during the first years of first affective and non-affective psychotic episodes [9], more depressive symptoms, higher insight, and negative beliefs about psychosis increase the risk for suicidality in FEP [10].
Impulsive behavior such as self-harm, as well as having a family history of severe mental disorder or substance use, have been stated as important risk factors for suicide in FEP [11,12]. Furthermore, low levels of cholesterol have been described in suicide behavior including among those individuals who have an increased tendency for impulsivity [13,14]. While, as a kind of psychological explanation, some scholars believe that young men in the early stages of their treatment are seeking to find meaning for frightening, intrusive experiences with origins which often precede psychosis, and these experiences invade personal identity, interactions and recovery [15], some suggests that personality characters, specifically, passive-dependent traits can be a predictor of first suicide attempts FEP [16].
On the other hand, no general agreement regarding higher prevalence of suicide in FEP is so far achievable. For example, while researchers like Nordentoft et al. [17], Bornheimer LA [8], Fedyszyn et al. [7], and Cohen et al. [18] have stated that FEP is a particularly high-risk period for suicide, with a risk as high as 10-60% during the first year of treatment, other scholars like Preti et al. [19], Pompili et al. [20], Crumlish et al. [21], and Addington et al. [22] have expected a lower risk or stated that suicide rates are difficult to measure in FEP patients, even in carefully defined samples. In the present study, suicides and suicide attempts among child and adolescent psychiatric in-patients, during the last five years, in Razi psychiatric hospital, as the largest national psychiatric hospital in Iran and region, has been evaluated to assess the general profile of suicidal behavior among native child and adolescent psychiatric inpatients, and comparing first admission with recurrent admission patients.
Methods
Child and adolescent section of the Razi psychiatric hospital was the field of the present assessment. For valuation, all inpatients with suicidal behavior (successful suicide and attempted suicide, in total), during the last sixty months, had been included in the current retrospective study.
Statistical analyses
Difference of suicidal behavior between first admission and recurrent admission patients, had been analyzed by ‘comparison of proportions’. Statistical significance as well, had been defined as p value ≤0.05. MedCalc Statistical Software version 15.2 was used as statistical software tool for analysis.
Results
As said by the results, among 748 child and adolescent psychiatric patients hospitalized in razi psychiatric hospital, during a sixty months period (2013-2018), 14 suicide attempts, without any successful one, had been recorded by the security board of hospital (Table 1). Six of suicide subjects were male and 8 of them were female, with no significant difference about quantity (Table 2). The most frequent mental illness was bipolar I disorder (50%), which was significantly more prevalent among female patients (z=2.72, p<0.007, CI 95%:0.19, 1.23), followed by conduct disorder (42.85%), and substance abuse disorder (7.14%). In this regard, no significant difference was evident among psychiatric disorders (Table 3). Moreover, no significant difference was evident between the first admission and recurrent admission child and adolescent inpatients, totally (p<0.44) and separately (Table 3). The annual incidences of suicidal behavior in both groups were comparable, and they were around 0.21% and 0.16%, in first admission and recurrent admission psychiatric inpatients, respectively (Table 1). Table 1: Comparing suicidal behavior between first admission and recurrent admission child and adolescents psychiatric patients in Razi psychiatric hospital thru 2013-2018.
To read more about this article: https://irispublishers.com/ctcms/fulltext/suicides-and-suicide-attempts-among-child-and-adolescent-psychiatric-inpatients-in-iran.ID.000502.php
Indexing List of Iris Publishers: https://medium.com/@irispublishers/what-is-the-indexing-list-of-iris-publishers-4ace353e4eee
Iris publishers google scholar citations: https://scholar.google.co.in/scholar?hl=en&as_sdt=0%2C5&q=irispublishers&btnG=
#Iris Publishers#Iris Publishers LLC#Medical Science Journals#Open access journal of Current Trends in Clinical & Medical Sciences#Clinical Science#Clinical sciences Open access journals
2 notes
·
View notes
Text
One frustrating thing about the extreme focus on “recovery” is that with developmental trauma & extremely early-onset illnesses, there is just nothing to recover, no “who was I before the accident,” just this burnt slate that has always looked something like this— maybe better somedays, maybe worse some days, but not in a linear way, and never better enough that anyone would consider a return to that state to be “recovery.” I’m tasked with this order to form something out of these ashes that makes sense, “build on what you once had,” and I swear that must be why why it’s so insurmountable. Frankly I’m tired of trying to make sense. No recovery is possible if there is nothing to recover. Going back to the good ol’ days is going back to multi-source child abuse, indoctrination, and untreated and unacknowledged psychosis. Why am I still focused on it?
... But what would be better than that? What’s my alternative? If I don’t work on “recovering” what do I work on?
1 note
·
View note
Text
14 is too young for a schizophrenia onset. it’s rare for someone younger than 13 to be diagnosed and women tend to have a latter onset and azula doesn’t really show symptoms of early onset schizophrenia hence why, despite how the comics portray her, I am very reluctant to go in that direction. azula clearly has an episode of psychosis but in the context of the show I wouldn’t say it lasts longer than a couple of days max so it’s perfectly possible that it’s an isolated episode brought on by trauma and stress especially cause at no point in the rest of the show does she show signs of any sort of mental illness. she has trouble relating to others and is a perfectionist which can be explained by low empathy and her upbringing as a gifted child.
#ch; azula#( ;; behind the writing pen )#mental illness cw#actively ignoring the comics cause it doesn't feel like enough research went into it#give her a couple more years before a mental illness actually manifests#as something that is there 24/7#I'd rather have it become serious at around 20 since that's closer to average onset#imo she may develop ppd but during the course of the show she's struggling with low empathy and a psychosis episode#I also feel like there's maybe a bigger history of paranoia in the family#her dad and grandfather and great grandfather all have some problems with grandiose delusions#just trying to do actual research cause diagnosing a 14 year old with an actual mental disorder is……… I don't like it#so yeah if you're expecting an azula who gets out of sozin's comet with a fully formed mental disorder you need someone else#she's 14 and stressed!
4 notes
·
View notes
Text

Klaus was never adopted by Reggie au thoughts n ideas:
He was born in Rüdesheim am Rhein in Germany
His full name is Klaus Wolfgang Alscher
Altho his birth mother didn’t trust Reginald, she still gave Klaus up for adoption in the traditional sense, handing him over to the state
As a toddler his various foster parents struggled to cope with him, Klaus was always crying, or having tantrums, or screaming at seemingly nothing. He was a constantly upset baby for reasons that no one could figure out
Eventually as Klaus grew older and learned how to talk he would babble about scary men and dead people, much to the horror of his foster parents
No one quite knew what to do with the fact that this child was apparently having quite violent hallucinations
Eventually he was diagnosed with extremely early onset psychosis and schizophrenia and became a bit of a case study as the youngest patient the doctors had ever seen
He was put on antipsychotics which helped a little, but he was still having “hallucinations” and vivid nightmares unless he was put on the highest dose and a veritable cocktail of tablets, something which doctors were relatively reluctant to give a child
Eventually as a teenager he was adopted by the foster parents he’d been staying with for a few years, Finn and Barbara Herrmann
Spent a lot of time in therapy
Struggled at school and to hold down a job, but got some part time work in a local cafe and worked shifts between therapy and doctors appointments, and lived with his adoptive parents
One day went into a mystic shop owned by a woman called Ronja because fuck it he’d tried everything else, and she instantly started talking about him being a gateway to the spiritual world and his powers with the dead. Klaus didn’t want to believe her, but he had to admit that every single hallucination he’d ever had, was about dead people. She gave him some books to read, and a few weeks later he was back asking for more info
After a few experiments with Ronja involving graveyards, oujji boards, and tarots he started to come round to the idea. He quit his job at the cafe and began working with Ronja in her shop
Slowly started decreasing his meds, although still took them to an extent because at this point he’d been on them his entire life and was scared of what he would do without them
Eventually in March 2019 he was contacted by the ghost of a man named Sir Reginald Hargreeves, an absolute bastard who insisted Klaus go to America and pass on messaged to the umbrella academy there, Klaus wanted to ignore him on principle of him being an ass, but Ronja encouraged him to go
Grabbing Vanya’s book for research he hopped on a plane and set off to try and get Reggie’s ghost off his ass
7 notes
·
View notes