#clinical disease
Text
Acetylcholine

Patreon
#studyblr#notes#my notes#medblr#medical notes#pathology#pathology notes#pathophysiology#pathophysiology notes#health and disease#diseases#disorders#human health#human disease#human pathology#human disorders#diseases and disorders#clinical pathology#clinical health#clinical disease#premed#mcat#mcat biology#medical biology#bio#biology#mcat bio#human pathophysiology#note cards#flash cards
8 notes
·
View notes
Text
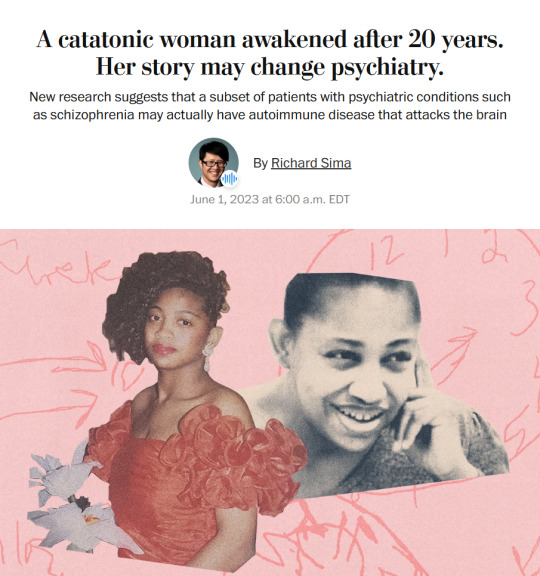
Story from the Washington Post here, non-paywall version here.
Washington Post stop blocking linksharing and shit challenge.
"The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.” ...
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries...
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments [for lupus] — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other people with similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients, the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.” ...
Waking up after two decades
The medical team set to work counteracting April’s rampaging immune system and started April on an intensive immunotherapy treatment for neuropsychiatric lupus...
The regimen is grueling, requiring a month-long break between each of the six rounds to allow the immune system to recover. But April started showing signs of improvement almost immediately...
A joyful reunion
“I’ve always wanted my sister to get back to who she was,” Guy Burrell said.
In 2020, April was deemed mentally competent to discharge herself from the psychiatric hospital where she had lived for nearly two decades, and she moved to a rehabilitation center...
Because of visiting restrictions related to covid, the family’s face-to-face reunion with April was delayed until last year. April’s brother, sister-in-law and their kids were finally able to visit her at a rehabilitation center, and the occasion was tearful and joyous.
“When she came in there, you would’ve thought she was a brand-new person,” Guy Burrell said. “She knew all of us, remembered different stuff from back when she was a child.” ...
The family felt as if they’d witnessed a miracle.
“She was hugging me, she was holding my hand,” Guy Burrell said. “You might as well have thrown a parade because we were so happy, because we hadn’t seen her like that in, like, forever.”
“It was like she came home,” Markx said. “We never thought that was possible.”
...After April’s unexpected recovery, the medical team put out an alert to the hospital system to identify any patients with antibody markers for autoimmune disease. A few months later, Anca Askanase, a rheumatologist and director of the Columbia Lupus Center,who had been on April’s treatment team, approached Markx. “I think we found our girl,” she said.
Bringing back Devine
When Devine Cruz was 9, she began to hear voices. At first, the voices fought with one another. But as she grew older, the voices would talk about her, [and over the years, things got worse].
For more than a decade, the young woman moved in and out of hospitals for treatment. Her symptoms included visual and auditory hallucinations, as well as delusions that prevented her from living a normal life.
Devine was eventually diagnosed with schizoaffective disorder, which can result in symptoms of both schizophrenia and bipolar disorder. She also was diagnosed with intellectual disability.
She was on a laundry list of drugs — two antipsychotic medications, lithium, clonazepam, Ativan and benztropine — that came with a litany of side effects but didn’t resolve all her symptoms...
She also had lupus, which she had been diagnosed with when she was about 14, although doctors had never made a connection between the disease and her mental health...
Last August, the medical team prescribed monthly immunosuppressive infusions of corticosteroids and chemotherapy drugs, a regime similar to what April had been given a few years prior. By October, there were already dramatic signs of improvement.
“She was like ‘Yeah, I gotta go,’” Markx said. “‘Like, I’ve been missing out.’”
After several treatments, Devine began developing awareness that the voices in her head were different from real voices, a sign that she was reconnecting with reality. She finished her sixth and final round of infusions in January.
In March, she was well enough to meet with a reporter. “I feel like I’m already better,” Devine said during a conversation in Markx’s office at the New York State Psychiatric Institute, where she was treated. “I feel myself being a person that I was supposed to be my whole entire life.” ...
Her recovery is remarkable for several reasons, her doctors said. The voices and visions have stopped. And she no longer meets the diagnostic criteria for either schizoaffective disorder or intellectual disability, Markx said...
Today, Devine lives with her mother and is leading a more active and engaged life. She helps her mother cook, goes to the grocery store and navigates public transportation to keep her appointments. She is even babysitting her siblings’ young children — listening to music, taking them to the park or watching “Frozen 2” — responsibilities her family never would have entrusted her with before her recovery.
Expanding the search for more patients
While it is likely that only a subset of people diagnosed with schizophrenia and psychotic disorders have an underlying autoimmune condition, Markx and other doctors believe there are probably many more patients whose psychiatric conditions are caused or exacerbated by autoimmune issues...
The cases of April and Devine also helped inspire the development of the SNF Center for Precision Psychiatry and Mental Health at Columbia, which was named for the Stavros Niarchos Foundation, which awarded it a $75 million grant in April. The goal of the center is to develop new treatments based on specific genetic and autoimmune causes of psychiatric illness, said Joseph Gogos, co-director of the SNF Center.
Markx said he has begun care and treatment on about 40 patients since the SNF Center opened. The SNF Center is working with the New York State Office of Mental Health, which oversees one of the largest public mental health systems in America, to conduct whole genome sequencing and autoimmunity screening on inpatients at long-term facilities.
For “the most disabled, the sickest of the sick, even if we can help just a small fraction of them, by doing these detailed analyses, that’s worth something,” said Thomas Smith, chief medical officer for the New York State Office of Mental Health. “You’re helping save someone’s life, get them out of the hospital, have them live in the community, go home.”
Discussions are underway to extend the search to the 20,000 outpatients in the New York state system as well. Serious psychiatric disorders, like schizophrenia, are more likely to be undertreated in underprivileged groups. And autoimmune disorders like lupus disproportionately affect women and people of color with more severity.
Changing psychiatric care
How many people ultimately will be helped by the research remains a subject of debate in the scientific community. But the research has spurred excitement about the potential to better understand what is going on in the brain during serious mental illness...
Emerging research has implicated inflammation and immunological dysfunction as potential players in a variety of neuropsychiatric conditions, including schizophrenia, depression and autism.
“It opens new treatment possibilities to patients that used to be treated very differently,” said Ludger Tebartz van Elst, a professor of psychiatry and psychotherapy at University Medical Clinic Freiburg in Germany.
In one study, published last year in Molecular Psychiatry, Tebartz van Elst and his colleagues identified 91 psychiatric patients with suspected autoimmune diseases, and reported that immunotherapies benefited the majority of them.
Belinda Lennox, head of the psychiatry department at the University of Oxford, is enrolling patients in clinical trials to test the effectiveness of immunotherapy for autoimmune psychosis patients.
As a result of the research, screenings for immunological markers in psychotic patients are already routine in Germany, where psychiatrists regularly collect samples from cerebrospinal fluid.
Markx is also doing similar screening with his patients. He believes highly sensitive and inexpensive blood tests to detect different antibodies should become part of the standard screening protocol for psychosis.
Also on the horizon: more targeted immunotherapy rather than current “sledgehammer approaches” that suppress the immune system on a broad level, said George Yancopoulos, the co-founder and president of the pharmaceutical company Regeneron.
“I think we’re at the dawn of a new era. This is just the beginning,” said Yancopoulos."
-via The Washington Post, June 1, 2023
#mental illness#schizophrenia#schizoaffective#psychotic disorders#psychology#neurology#autoimmune#autoimmine disease#neuroscience#medical news#medical research#catatonia#immunotherapy#immune system#clinical trials#good news#hope
6K notes
·
View notes
Text
17:12 — JOSHUA
inspired by this clip of shua at the airport today. special mention to @duhnova i've never been the same since she sent it to me <3
"s-shua."
"hm?"
"why're you being so..."
"so what, baby?"
you flash your boyfriend a little pout that makes him laugh. joshua's large hands massage your thighs as he leans forward to press his lips to yours. you nearly melt into him again when he licks into your mouth only for joshua pull away the moment you let your guard down—earning himself another whine in protest.
"you're such a tease," you complain, lightly punching his chest for good measure. "i thought you said you missed me."
he laughs again, that sinful tongue swiping along the plump curve of his bottom lip. you know he doesn't miss the way your eyes catch the movement and it only makes that stupid smirk grow wider.
"i did miss you, sweetheart," he coos and if he thinks he can distract you with the way his hands grip your thighs with just a tinge of possessiveness, he's not wrong. "it just so happens that i also miss the way you react whenever i tease. why? does my baby hate it so much when i do?"
you want to say that yes, you do hate it when he strings you along like this. but part of you is well aware of joshua's penchant for building up your arousal and anticipation. he likes the chase. likes holding the prize over your head to see how desperate you're willing to get just to get his hands on you.
well, in this case: his tongue.
"just want your tongue in me, shua," you mumble, the muscles of your aching cunt clenching around nothing as your boyfriend gazes up at you with a lazy, hooded gaze. "gets me so hot whenever you kiss me like that... please, please, baby. i've been good for you, right? you'll give it to me, right?"
a low laugh reverberates in joshua's chest as he reaches a hand up to tuck your hair behind your ear. when you beg so prettily like that, how can he ever refuse you?
that's how he finds his face smothered between the plush give of your thighs as he slurps at your pussy like he's been dreaming of the entire week. your fingers are tangled in his hair, eyes screwed shut. every breathless moan that slips from your lips rushes straight to his cock, but joshua doesn't have any plans on relieving himself until you've coated his face with release.
"fuck, joshua," you breathe sharply—air whistling down your throat when he slides two fingers inside you. coupled with the sensation of his hot tongue alternating between flicking across your clit and licking long stripes across your soaked folds, you're completely at the mercy of your merciless boyfriend. "s-so good..."
he laughs again—those deep-seated vibrations humming across every nerve ending between your legs. it doesn't help that your boyfriend knows exactly how to drive you insane at any given moment, curling his long fingers as he flattens his tongue across your slit.
your spine immediately straightens at the stimulation and joshua's hands migrate from your legs to twine them with yours—making it much easier for you to rock your hips into his face as he brings you to the apex of pleasure.
"shua," you nearly sob, loving how your fingers fit in the spaces between his, loving how he makes you lose your mind every time, loving him. "'m close."
he parts from your sopping cunt for just a moment to breathe out, "i know, baby. i know," before he dives back into you—tonguing at your entrance until all that's coming out of you are high-pitched keens of his name.
you come undone on your boyfriend's tongue when he squeezes your fingers with his. like a wordless confirmation that he's allowing you to come and the authority he has over you magnifies the sensation a few hundred notches.
joshua helps you ride it out the entire time—peppering your inner thighs with butterfly kisses as he goads you on. my beautiful baby, you look so fucking sexy when you come all over my face. that's it, pretty. let yourself feel it. i promise i'll make you feel even better in a minute.
#seventeen smut#joshua smut#hong jisoo smut#svthub#im clinically insane atp#im so obsessed w shua it's a disease#i'd write more to this but#it will just be a neverending fuckfest tbfh#lovelyhan
759 notes
·
View notes
Text
And on this Valentine’s I almost broke down in tears at a wife’s dedication to her heart surgeon husband whose brain is deteriorating with a rare case of dementia
#I shadowed the doctor for the first time today and almost broke down in tears multiple times listening to her talk about her story#he performed his last heart surgery last October. and ever since he’s been fading away and had to retire. rapid onset but behavior changes#were happening over the last like 6 years#this HEART SURGEON BRAINIAC started chewing tobacco in his 60s beyond his wife’s knowledge. a very common sign of this brain disease#I’m still in clinic but have to ride down to the office and get some chart stuff done now and I’m like?? spiraling about it still#at least love is real. they’ve been married for 45 years and she’s on top of her shit taking caring of him all by herself#and she only has glowing things to say about him#she wants her heart surgeon husband back but he’s fading away#I’ve wanted to be a doctor my whole life but I’m such a crybaby OK I’m going now#happy valentine’s day#p#v day
101 notes
·
View notes
Text


i need to be put down
#delete later#there’s clinically insane and then there is whatever tf i’m going thorough rn#they should put esen/ouyang disease in the dms5#mx parker chan i’m in your walls#send post#he who drowned the world
195 notes
·
View notes
Text
silna and goodsir’s relationship is everything to me. they’re lovers. they’re besties. they’re lesbians. they’re teaching each other about their cultures. one of them is a coloniser who wants to take the other back to england. the other wants all his friends dead. they’re orpheus and eurydice. they’re a tragedy. they could’ve loved each other. their relationship would never have worked. the love was there but it didn’t save anyone. did i mention they’re lesbians.
#no because i cannot stop thinking about them#it’s like a clinical disease#instead of brain there is goodsir and silna#idk their ship name though :(#harry goodsir#henry goodsir#lady silence#silna#the terror#amc the terror#tig talks
175 notes
·
View notes
Text
How come I can help others, but not myself?
How does that even make sense?
Why are people in psychology the most messed up people?
#chronic illness#fibromyalgia#ptsd#adhd#autism#ODD#Borderline personality disorder#chronic pain#chronically ill#fibro problems#autoimmune disease#invisible illness#disability#semi verbal#clinical depression#insominia#ADHD#auditory processing disorder#hard of hearing#rare illness im dealing with on top of it all#oppositional defiant disorder#autism spectrum disorder#cluster b disorders#trauma#OCD-ish#ocd is a part of my autism so its not its own thing but its the same just... yeah
23 notes
·
View notes
Text

[ID: the “wait, it’s all [blank]” meme of one astronaut pointing a gun at the other, edited to read “wait, it’s all celiac?” / “always has been.” with the word celiac in a groovy pink font. end ID]
happy celiac awareness month 💓🖤💓 folks expressed interest in my #Controversial Opinion, so here we go:
as someone who “has” non-celiac gluten intolerance, i don’t believe it exists.
this, as with all of my diagnostic opinions, is built from both health research & sociology, specifically the genealogy of (my) disabilities – how the labels we use & the divides we create between diagnoses are socially constructed. conditions don’t announce themselves as discrete entities; instead, labels are given based on, at best, current medical understandings of symptoms + clinical visualization measures (imaging, bloodwork, genetic testing, etc). conditions that were once considered two separate things may eventually be restructured under the same diagnostic label, & what was once considered one singular disease may be divided into separate categories, in response to new information or the new recognition / respect of existing information.
the issue with this system, though – with access to healthcare which is predicated upon diagnosis, which is itself predicated on checklists of symptoms & clinical visibility – is that we don’t know shit. our bodies are not required to present symptoms in accordance with the ICD 10, & chronic illnesses are very much an “ask four doctors, get five answers” situation.
for example: without any of my symptoms, imaging, or bloodwork changing, i’ve been diagnosed with active ankylosing spondylitis, ankylosing spondylitis that is in remission, fibromyalgia, & spondyloarthropathy. the only difference is the doctors: their belief or lack thereof in my symptoms, their familiarity with current research, & the diagnostic systems they abide by. under the NHS, it was definitionally impossible for me to have ankylosing spondylitis that was not visible on an MRI, therefore i must have been in remission, even as my symptoms were just as debilitating as before & treatable by immunosuppressants.
how this pertains to celiac: as with all chronic illnesses, symptoms of celiac disease are a broad spectrum. some people have severe growth impairment from a young age; others may only have minor skin manifestations. other common symptoms are vague & potentially attributable to any chronic illness, such as fatigue, depression, & gastrointestinal issues. crucially, though, damage to the small intestine is still occurring even in people with celiac who do not flare after consuming gluten.
following this,
the diagnosis of non-celiac gluten intolerance has nothing to do with symptom presentation or severity. it doesn’t even mean there is no clinically visible damage to the small intestine. rather, it just means you didn’t pass the test:
in my case, not only was the (notoriously unreliable) antibody blood test negative, but so were subsequent tests for the genetic markers associated with celiac.
two people with the same exact experiences can get put into two different boxes, solely based on bloodwork – but that’s not how genetics works. it’s pretty much impossible that only those two markers dictate whether or not someone has celiac, or any given disease, because genetics are infinitely more complex than that; equally, plenty of autoimmune disorders can have a genetic component but are not exclusively found in people with that particular marker (ankylosing spondylitis & HLA-B27, for example).
therefore, i firmly believe non-celiac gluten intolerance is celiac disease, just influenced by other genetic factors and/or antibodies we haven’t yet identified.
there are a whole host of issues created by the false divide of celiac vs non-celiac gluten intolerance, certainly including things i’ve never considered, but here are a few examples of what i refer to as diagnostic violence, the physical & social consequences of these forms of categorization:
celiac disease increases people’s risk for small bowel cancer. but if it’s been determined by the medical establishment that according to their criteria, you don’t have celiac disease, then you won’t receive cancer screening.
since a food intolerance is not considered an autoimmune disease, there is no medical evidence of an underlying cause of arthritis, for example, making it that much harder for people to receive diagnosis & treatment for autoimmune symptoms.
diagnostic paperwork & a letter from a doctor is almost always required to receive accommodations, & food-related accommodations are notoriously difficult to obtain at universities which require the purchase of a meal plan without sufficient gluten-free options, for example.
as a response to the dangerous ableism permeating societal attitudes toward gluten-free food, many people (diagnosed) with celiac fall back on communicating the seriousness of their needs at the expense of their undiagnosable peers. “it’s not just an intolerance!” i read over & over – never mind that gluten made me so sick i lost a significant amount of weight, my hair fell out, i had signs of multiple vitamin deficiencies, & i could only keep down liquids.
this is honestly the most blatant example i’ve come across of the complete arbitrariness of diagnostic categories, but it’s far from the only one, & i’d love to hear other folks’ controversial opinions – what physical disabilities do you tell people you have without a diagnosis? do you consider yourself to have that condition, or is this just for expediency of communication? how does your undiagnosability affect your interactions with community formed around that diagnosis?
your experiences are real, your symptoms are serious, & it is not your fault that white supremacy demands a categorizability which all bodies inherently fail. join the club – we’ve got plenty of gluten-free snacks. 💓🖤💓
#celiac#celiac disease#dietary restrictions#gluten intolerance#gluten free#sociology#disability studies#diagnosis is a form of violence#abolish the clinic#mac.txt#image described
79 notes
·
View notes
Text
what do you do when all hope seems to be lost
when the body is tired and exhausted
and your existence has yet to feel accomplished
#writers on tumblr#writerslife#poetry#mental health#mental illness#clinical depression#major depressive disorder#social anxiety#social anxiety disorder#adult adhd#migraine#celiac disease#chronic illness
25 notes
·
View notes
Text
The er is fucking boring.
Somebody ask me about Tim Drake or something.
#I'm convinced my workplace poisoned me so here i am#it speaks#god i don't wanna be here#i hate the hospital i do not wanna be in it#my poor dad spent all day at a cancer clinic with my mom and now he's waiting in the parking lot for me to get seen#i wanna go hooome#i wanna go to sleep#i wanna be with my mom#my conspiracy theory is that I've had exposure to propane and carbon monoxide and my blood disease is making worse#yes i am posting this and hopes of getting attention I'm bored and want a social interaction
8 notes
·
View notes
Text
nothin hits like the validation of a doctor taking a look at you and going "oh this is really bad"
#chronic illness#text#🤭 me when i go to the infectious disease clinic and all the docs go huh this is unusual
7 notes
·
View notes
Text
Hypokalemia Causes
-- gastrointestinal issues
-- periodic paralysis
-- insulin excess
-- renal problems
-- hypothermia
-- aldosterone
-- Cushing's syndrome
-- diuretics
-- insufficient intake
-- alkalosis
-- elevated beta-adrenergic activity
.
Patreon
#studyblr#notes#my notes#medblr#medical notes#pathology#pathology notes#pathophysiology#pathophysiology notes#health and disease#diseases#disorders#human health#human disease#human pathology#human disorders#diseases and disorders#clinical pathology#clinical health#clinical disease#premed#mcat#mcat biology#medical biology#bio#biology#mcat bio#human pathophysiology#note cards#flash cards
10 notes
·
View notes
Photo


#zack sabre jr#kenta#njpw#i have still thinking about this match disease sorry#they really said let's put on one of the horniest clinics you've ever seen <3#zsj#mygifs
144 notes
·
View notes
Text

today was... not the greatest! for a number of reasons which don't bear repeating, but have shlorped me dry of my typical nocturnal zest regardless. so, with that in mind: i'm gonna try and hit the hay sooner rather than later.
send me more shenanigans, ( bingo or otherwise ), and I'll lavish you all with my love in turn on the morrow. mwah mwah, kiss kiss.
#signing off.#ooc.#spontaneous bad feelings would be more surprising if i didn't have clinical 'uppy downy badfeelings' disease but. whatcha gonna do?#itty bitty negativity if you squint.#just a rough one! back at it tomorrow.
5 notes
·
View notes
Text


I luv my mom
#I was pretty nervous ab my neuro clinic internship too and she told me that im def ready to be at a neurodegenerative diseases hospital#These r snippets of a much longer conversation but just the fact that her first & immediate texts are so supportive 🤎🤎
52 notes
·
View notes
Photo

dilf alert
[image ID: a digital sketch page of dracula from monster high: adventures of the ghoul squad, a middle-aged vampire with light purple skin, grey-streaked hair, and square glasses dressed in a collared shirt, a vest, and a cravate. he is shown 1) happily giving a side hug to his daughter draculaura; 2) smiling while holding a book; and 3) adjusting his glasses with a concerned look and saying, “ghouls, please pay attention.” end ID]
#art#monster high#dracula#mh draculaura#mh dracula#digital art#fan art#draculaura#vampire#vampires#monster high adventures of the ghoul squad#I watched all of this in one day and thought it was pretty cute#gotta feed my monster high hyperfixation with more media#esp of draculaura and clawdeen and rochelle <3 faves#I also love seeing wraith and deuce exhibiting clinical idiot teenage boy disease /lh#and obv is there's a vampire dilf I'm right there#a nice contrast to my dracula daily experience lol#some more vampire art to come [eyes emoji]#with id
248 notes
·
View notes