#human pathophysiology
Text
Acetylcholine

Patreon
#studyblr#notes#my notes#medblr#medical notes#pathology#pathology notes#pathophysiology#pathophysiology notes#health and disease#diseases#disorders#human health#human disease#human pathology#human disorders#diseases and disorders#clinical pathology#clinical health#clinical disease#premed#mcat#mcat biology#medical biology#bio#biology#mcat bio#human pathophysiology#note cards#flash cards
8 notes
·
View notes
Note
genuinely not trying to dunk on molly but when ppl say will and molly were so compatible they loved dogs i just think of molly feeding them canned food from china and not even knowing it could harm the dogs, i feel like this is significant because this was what led to dolarhyde being undetected and her attack which led to her estrangement from will, even her common values w will she did not actually share at all there's a meta here
ngl this is pretty clearly dunking on molly. But let’s refute. I personally haven’t seen many metas/posts about the compatibility between will and molly, so I can’t really contest what they say. However, will and her were as compatible as will led her to believe, as much as he would let. He lied to her about his past, which made it so she couldn’t know all of him and couldn’t connect to parts she couldn’t see. Not a fault of molly’s at all
Having looked back on the script for that episode, no credible veterinarian would ever say “was it canned food from china”. It’s unprofessional and xenophobic. Also, a vet in an emergency situation isn’t going to use scare tactics. They just need to know what went in so they can take care of it. Yes, molly was feeding the dogs canned food because will was out of town so he couldn’t make them food. and I can guarantee will is rational enough to say “hey, these brands are okay” and molly isn’t stupid. And they are very well off, so they would need to buy “cheap dog food from china”. If we want to talk about the dialogue in that scene, we have to admit to ourselves fuller is a misogynist who can’t write women, so ofc he made her say “is it bad to be made in china”. It also neglects how SOME but not ALL food has shown problems, but dog food made in the US has also had toxicity issues! And (I can’t remember if this was in show or just in script) the vet says “pet food safety isn't regulated the same way as human food” which is just false. There is high regulation in pet food, and pet food is made to be human grade and safe for human consumption (and has been for decades). Dogs are more likely to be poisoned by xylitol or chocolate from your candy or get pancreatitis from your table scraps than die from “dog food from china”.
But let’s humor for a second it was the cheap dog food molly bought. The concern and toxic component is melamine, which is added to food to fraudulently increase the protein content. it’s nontoxic (ish) by itself and only becomes a problem when combined with cyanuric acid that forms a crystal and leads to renal toxicosis and failure. Some gi biomes have bacteria that can convert melamine to cyanuric acid, but not all, making it more toxic for these patients. It also wasn’t solely a dog food thing, it happened in human children, too. All that aside, most melamine toxicosis cases are chronic, aka molly would have had to feed the dogs for a while, building up these crystals, and slowly killing the kidneys. This wouldn’t happen suddenly to all the dogs at once. Early signs of toxicosis are very detectable symptoms (vomiting, polyuria, polydipsia, lethargy) and these are signs molly would have noticed and done something about. ALSO if it was melamine the veterinarian was worried about, she wouldn’t use activated charcoal as her treatment (as she states in script, again, don’t remember if this was said in the show). Activated charcoal only works for something currently in the stomach, and that isn’t the pathophysiology for melamine. To treat melamine toxicity, you need iv fluids and supportive care. So what we can take from the veterinarian interaction is 1) fuller doesn’t know how medical professional talk to clients and 2) he doesn’t even understand the toxin he mentioned so it feels xenophobic as fuck to even bring that up.
And no, her canon (fuck you fuller) ignorance to the danger of canned dog food isn’t the cause of dolarhyde being undetected and attacking her. Even if she was feeding them dog food with melamine, Will literally figures out and says that dolarhyde poisons the dogs in the family to get rid of the “alarm system”, so he can attack and not have the family alerted. It didn’t matter what dog food molly fed them, dolarhyde intentionally poisoned them. Even if she fed them food will handmade, dolarhyde would have still poisoned them. And she was a good owner who brought all 7 (probably) puking dogs to the vet as soon as she could. molly had nothing to do with dolarhyde attacking her. dolarhyde had something to do with dolarhyde attacking her (and hannibal ofc). At least give her some credit for, you know, surviving
And no, her getting attacked was not the cause of will estranging himself from her. He never really loved her and used her as a fill in for a man he outright rejected. He was having an emotional affair with Hannibal and not giving a shit about molly. That was nothing molly could control.
And we really can’t thoroughly discuss her values because we barely see her onscreen. Her screentime is a plot motivator, we aren’t privy to who she is as a person. She loves her son, lost her first husband, and loves will. That’s kind of it. Oh, yeah, she also takes her son fishing without Fisherman Husband because he chose to estrange himself.
#you caught me in a mood anon love and light#sorry i know my answer makes me sound like a real jackass but it was worded very rude#like molly did nothing to deserve what happened to her#she was a good person who cared about her family#anonymous#the curious clown
78 notes
·
View notes
Text
i've been collecting resources and studies about myalgic encephalomyelitis for upcoming doctors appointments, and since there's a lot of misinformation about ME out there i thought i'd make a post with links and information that might be helpful for other ME patients, or just generally educational!
for anyone who doesn't know, myalgic encephalomyelitis is a debilitating multi system chronic illness. it's most characteristic symptom is post exertional malaise/symptom exacerbation (meaning symptoms getting significantly worse after exertion with prolonged recovery periods - see the diagnostic criteria linked below for more explanation). it has previously been called chronic fatigue syndrome, a name associated with claims of it being a psychosomatic condition rather than a medical one despite evidence to the contrary (here's a page with some information about the history of ME, and see the pathology section further down for evidence of ME being a physical disease). ME is also often comorbid with conditions like POTS (or other forms of orthostatic intolerance and dysautonomia), MCAS, and Small Fibre Neuropathy, and it's not uncommon for people who have long covid to develop ME. but yea! here's some links to resources i've gathered.
general resources/overviews:
Chronic Fatigue Syndrome Myalgic Encephalomyelitis Primer For Clinical Practitioners 2014 Edition
Diagnosis and Management of Myalgic Encephalomyelitis - ME Action
Initiating Care of a Patient With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)
Medical considerations when treating urgently ill patients with underlying myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)
Caring for the Patient with Severe or Very Severe Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
Three Cases of Severe ME/CFS in Adults
diagnostics:
Myalgic Encephalomyelitis: International Consensus Criteria <- just the criteria
Myalgic encephalomyelitis: International Consensus Criteria <- criteria with explanation of how and why it was developed
TESTING RECOMMENDATIONS FOR SUSPECTED ME/CFS US ME/CFS Clinician Coalition
there are multiple ME severity scales, and exact definitions of what constitutes mild/moderate/severe/very severe vary a bit, but here is one: M.E. Disability Scale, another one is the ME/CFS Disability Rating Scale from ME Association, however the pdf on their website costs so i also have a pdf that i made with the text
pathology:
Brainstem volume changes in myalgic encephalomyelitis/chronic fatigue syndrome and long COVID patients
Decreased oxygen extraction during cardiopulmonary exercise test in patients with chronic fatigue syndrome
Developing a blood cell-based diagnostic test for myalgic encephalomyelitis/chronic fatigue syndrome using peripheral blood mononuclear cells
Human Herpesvirus-6 Reactivation, Mitochondrial Fragmentation, and the Coordination of Antiviral and Metabolic Phenotypes in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
Mitochondrial complex activity in permeabilised cells of chronic fatigue syndrome patients using two cell types
Muscle sodium content in patients with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
Redox imbalance links COVID-19 and myalgic encephalomyelitis/chronic fatigue syndrome
The use of oxygen as a possible screening biomarker for the diagnosis of chronic fatigue
Tissue specific signature of HHV-6 infection in ME/CFS
treatment (both helpful and harmful):
ME/CFS TREATMENT RECOMMENDATIONS US ME/CFS Clinician Coalition
Low-dose naltrexone in the treatment of myalgic encephalomyelitis/chronic fatigue syndrome (ME/ CFS)
Potential Therapeutic Benefit of Low Dose Naltrexone in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Role of Transient Receptor Potential Melastatin 3 Ion Channels in Pathophysiology and Treatment
Back to the Future? Immunoglobulin Therapy for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
Evidence Against Exercise for people with PEM/PESE in Long COVID and ME/CFS
PACE trial claims for recovery in myalgic encephalomyelitis/chronic fatigue syndrome – true or false? It’s time for an independent review of the methodology and results
Treatment harms to patients with ME/CFS
#more than okay to reblog!#🐛#myalgic encephalomyelitis#me/cfs#chronic fatigue syndrome#chronic illness#disability#actually disabled#long covid
139 notes
·
View notes
Text
Some extracts:
---
These assessments highlighted the many key flaws that were endemic in the research, including the confounding of unblinded trials by reliance on solely subjective outcome measures, such as patients’ self-ratings about their health status on questionnaires. This combination of study design features meant that findings were impacted by an unknowable level of bias. Moreover, when tracking treatment outcomes with objective measures—such as physical endurance tests, actometer data, records of workplace participation, or analyses of dependence on social benefits—the research generally showed minimal or null effects for both GET and CBT.
---
This reality also helps explain, once again, the staying power of old ideas. Short-term and low-cost interventions such as GET and CBT are attractive not because of their evidence base, which has been exposed as flimsy and unconvincing, but rather because of their seemingly plausible and easily replicated approach to a very complex scientific and public health issue. The converse is clear as well when critics frame research into the biology and pathophysiology of ME/CFS or long COVID as unnecessarily expensive. If you’re reluctant to spend significant resources addressing a new problem, ignoring its potential significance is an understandable strategy.
---
Although paradigms are bound to shift when new knowledge contradicts prior beliefs, the resistance phase can be highly troublesome. This is especially the case when purportedly effective treatments arising out of poor-quality science carry a risk to human welfare. In the current context, psycho-behavioral approaches to treatment have been shown to be not only flawed but likely harmful by triggering the serious relapses that characterize PEM. Ongoing resistance to the paradigm shift only ensures that patients will continue to be offered inadequate and possibly dangerous therapies. Recent reports from patient support groups suggest that many health care services across England are not yet aligned with the new ME/CFS guideline, still offering treatments that are now disfavored.
---
22 notes
·
View notes
Text
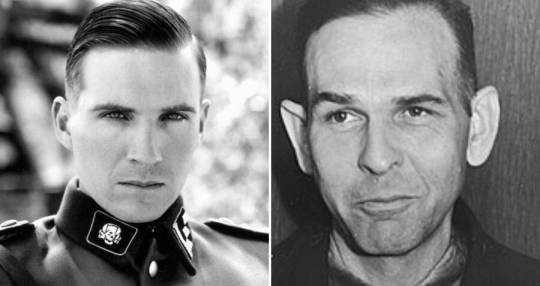

Amon Leopold Goeth is an SS Hauptsturmführer and commandant of the nazi concentration camp in Plaszow. A war criminal, he personally killed at least half a thousand prisoners.
On the left, there is Amon Goeth, played by Ralph Fiennes in "Shindler's list." On the right, there is actual Amon Goeth.
This is how people perceive nazism. At first, it seems to them a very attractive, liberating idea, it gives them a feeling of power and satisfaction. Why do people fall for nazism? Because it has many names, people need time and a lot of blood spilt to realise what it is. In the Middle Ages, it was called Christianity. Nowadays, its name is "From the river to the sea" and "русские вперед". Nazism gives you the feeling that you have the right to kill other people because of their ethnicity or religion. Nazism gives you the feeling that rape and mass murder are justifiable. Nazism violates the main law of the Universe itself, "Thou shalt not kill." "You shall not covet your neighbour's wife, or his manservant or maidservant, or his ox or donkey, or anything that belongs to your neighbour" - these are the words from the Bible. Ironically, in some russian translation, there was a phrase translated like, "Thou shalt not kill your neighbour." Nazism blooms when people are embittered and dream of making their neighbour feel bad just because "I feel bad, so they must suffer even more." Or even "I am happy and my neighbour is also happy, but I don't want my neighbour to be happy, I want to be happy while they're not." This is the physiology of nazism and the pathophysiology of humanity's development.
Russia invaded Ukraine, and Palestine invaded Israel because "I feel bad so my neighbour must suffer even more than me."
But in the end, everyone sees the true face of nazism. When the Insanity virus goes away, and people see the consequences of their actions, they see that nazism has their own faces, that it's not an abstract but a very concrete and material thing. It scares them so much so that they either live in shock and disgust or gaslight themselves that they didn't do anything wrong, that it wasn't their fault, for the rest of their lives. There are maniacs, of course, too, who genuinely enjoy killing, raping, torturing others - but the main body of nazism are "people who just believe in what is right".
God, please, save us and our close ones from nazism. God, please, save us from the neighbours who "believe in what is right" and who "just follow orders". And lead us not into temptation, but deliver us from evil.
#just some thoughts#genocide of ukrainians#russia is a nazi state#russia is a terrorist state#russia finances hamas#stop russian aggression#antisemitism#nazism
7 notes
·
View notes
Text
A very informative text of neurosurgeon and historian of science Pr. Alexander Brawanski on the Edwin Smith Papyrus and more generally on ancient Egyptian medicine - II
"Treatment concepts, magic, and science
The ancient physicians had a specific and rather sophisticated pathophysiological concept of (internal) diseases [33], which unfortunately complies with little of the actual inner workings of the body as we understand them today. They assumed some type of circulatory system, which included the heart and in which bad substances could accumulate and circulate. Furthermore, an elaborated materia medica was available with sophisticated application methods. Some of the applied drugs were effective [34–36]. This knowledge was acquired over the centuries by trial and error and finally led to the high esteem of the medical profession in the ancient world [37]. Part of this knowledge has survived in several larger medical papyri and many fragments [18], a textual corpus of which the ESP constitutes only a minor fraction.
As has often been observed by students, the anatomical descriptions in the ESP are clear, descriptive, and sometimes unique. One of the classics is the comparison of the surface of the (injured) brain to molten copper (case 6). However, the general anatomical knowledge was limited; sometimes it is nicknamed “kitchen” or slaughterhouse anatomy [38] because much of the information seems to be derived from the slaughterhouse indeed. An example is the uterus, which is represented hieroglyphically as the uterus bicornutus, which is not present in human beings. In this context, the question is unresolved as to whether at the time of the ESP the embalmers’ knowledge was used by physicians and whether they were two strictly separated professions. According to Ghalioungui, there were individuals bearing the title of physician who very likely could have been embalmers as well [25]. In the later period of Egyptian history, the Egyptian title for physician could mean both. Some information that is presented in the ESP related to spinal injuries does suggest, however, that there must have been an exchange of information between these groups [7]. Otherwise, some descriptions of spinal injuries in the ESP could not be described in such detail.
Besides all this, the ancient Egyptian physicians firmly believed in supernatural forces such as demons, undead persons (Widergänger), and divine influences as causes of illnesses and consequently treated them by magicical rituals. The less obvious the cause of a disease, the more common was magic [39, 40]! Magic and practical medicine were not different or contradictory to physicians. This differentiation is artificial and was introduced by modern medical historians [41]. The ancients often used magical spells to enhance the effectivity of medical applications, and often magic alone. Thus, there is a significant number of magical spells in other important medical papyri [42]. All this is not so necessary in the ESP, as the causes of the wounds and the injuries are well known, thus showing the “rational” approach, which exemplifies the strength of these ancient societies: The collection of information and facts and the classification of this information. This complies with the “organizational principle” that ruled these societies and without which they could not exist or survive. The ancient Egyptians had available lists of birds, countries, and even objects of daily life [43]. They used them for reference and education. The major intent of these lists was to classify and thus structure the world in order to cope with it. Knowledge meant power. Therefore, the knowledge of the physicians often was called “secret” and was not available to everyone, provided he could read at all.
This classification principle is perfectly exemplified in the ESP. The single cases are arranged from the top to bottom of the body. This may seem natural per se, but this structural principle again had a religious background. We know of litanies of Gliedervergottung (deification of members of the body) [44, 45] that have the same order. Here we come to another important point, namely that medicine was deeply rooted in the divine realm. The relevant documents were stored in the temples; education as well as treatment took place there. Some of the physicians may have been priests as well, and a specific type of priest also could magically treat patients [46] to some extent. All this explains why magic was a firm component of medical practice. Specifically in prescriptions with magic components, patients were often addressed as and equated with the god Horus, who was helped by his mother Isis.
In this context, we come to the major driving force of ancient Egyptian thought. All (official) activities had to follow one major principle that traverses all ancient Egyptian behavior: the universal order of the world—“Maat”—which kept the world running. It had to be preserved by all means because it was threatened every day. This fact sets Egyptian medicine in the proper position and environment in this society. According to Egyptian belief, ancient “objects” with a long tradition underpinned the validity of this concept. Thus, we can find the statement in medical texts “that the text is a copy of an ancient papyrus found in a chest by chance” [47] and thus must be qualitatively good, because otherwise it would have perished. Ancient Egyptian society wanted stability and no abrupt changes. This can be seen very well in ancient Egyptian art, which did not change in its basic principles throughout the existence of ancient Egypt. Once a reasonable solution to a problem was achieved, it was preserved, and one did not necessarily look for other solutions. This complies well with the ESP, which was copied around 1600 BCE, but stems from a much older document according to the language of this papyrus [1].
This does not mean that there was no progress at all or that no variety of approaches existed. In the medical literature, there are significant variants in the selection and applications of drugs [40]. Even foreign treatments were accepted in the medical canon [42, 48, 49]. However, over time there was little obvious significant change. Due to this general attitude of ancient Egyptian society and due to the close connection of medicine to the divine, science in the modern sense was not possible and possibly not even thought of. One did not experiment with religious issues and endanger the general world order. The ancient Greeks were the first to question the divine influence on diseases in the seventh century BCE. Obviously this society was open to these questions [50]. However, even at the time when Hippocrates was active, the Asclepiads still recommended treatment in the temples and help from the gods [51].
The individual patient
Now the fate of the individual patient should be examined in reference to the cases described in the ESP.
One of the major issues seems to have been to establish a proper prognosis that determined the further procedures. This may sound astonishing at first. However, it is understandable when we regard this from the viewpoint of a major organization. This was nothing other than triage, which makes even more sense in the context of limited treatment options (see below). The verdict/prognosis was written in red in the ESP, which underlines its importance. This method is not unusual as we can still find this approach in ancient Greek medicine (1,000 years later). Here the major issue was also determining the prognosis [52]. Actually, the authority and credibility of an ancient Greek physician depended to a large extent on establishing a fast and proper prognosis [53].
It is important to note that the Egyptian physicians did not give a single disease name in the ESP, but an enumeration of symptoms. This is a relevant fact, as a “single-word” diagnosis usually implies a coherent pathophysiological concept that each physician understands. Thus, for modern physicians the concept of diabetes includes various aspects that do not have to be enumerated each time. However, a loose collection of symptoms rather constitutes a syndrome, in the best medical sense, which does not necessarily imply an understanding of the underlying pathophysiology. We would for instance summarize some of the injuries in the ESP (e.g., cases 18–20) as cranial base fractures. To any modern physician, this term would mean a specific injury with variable severity depending on the location and strength of the impact. Thus, a physician would rather summarize the single cases under one heading. Similarly, the last case (case 48) in the ESP deals with lower back pain. Several symptoms are enumerated. From a modern point of view, this could indicate several diagnoses, such as a tumor, a slipped disc, or a simple joint problem. The ancient Egyptian physician gave a “syndromatic” description from which a final modern diagnosis can hardly be developed, as relevant information is missing. Thus, often a definitive modern diagnosis cannot be made simply because of the lack of specific information in the ESP. This is not a denigration of the ancient Egyptian medical art, which was quite sophisticated despite their limited knowledge, but we have to know what we can take for granted.
In addition, we have to be clear that the treatment options in the ESP are very limited. Most of them are supportive in the best sense, but hardly any of them are curative. One exception may be the readjustment of a dislocated jaw (case 25). The same holds true to some extent for the relocation of a broken collarbone (cases 34–35). Here, the outer contour is readjusted; however, the fracture is still there with all its implications for malfunctioning of the adjacent joint (shoulder). Besides this, some treatment suggestions are clearly detrimental to the patient. In case 28, an injury of the esophagus is obviously described. The physician recommended a closure of the superficial wound without further inspection of the deeper layers of the injury. This patient would definitely die from the sequelae of a mediastinitis, which is still a severe disease today. One may muse about the fact that the physician recommended a superficial closure of the wound in this case. Clearly the outflow of water should be mended. The guiding principle was obviously the restoration of the integrity of the outer aspects of the body. This corresponds well to the practice of mummification. Again the outer appearance of the mummy was important for the afterlife, but not so much the internal organs, which were removed during mummification and put in canopic jars separately.
Thus, the fate of the patient was actually determined by the seriousness of the injury, the severity of the following infection, and the physical strength of the patient to cope with these. The main intent of the ancient Egyptian physician was to establish a prognosis. We must be clear about the fact that a negative prognosis meant that the patient was left alone. What this may have looked like is described more fully in the Hippocratic Epidemics. I quote Epidemics 7,32 in reference to the ESP, case 22: “On a Macedonian: …he was struck over the left temple, a superficial wound. He fainted after the hit and fell. On the third day he was speechless. He tossed about. Fever was not very intense…. He heard nothing and was not conscious, nor was he still. Moisture was around his forehead and beneath the nose to the chin. He died on the fifth day” [54]. It is interesting to note that these observations, which are of importance to the physician, are not mentioned in the ESP. This is simply due to the fact that “bad” things could and should not be written down. The Egyptians believed in the supernatural strength of their script; it was not understood as a mere transporter of information. Describing bad events would disturb Maat, the general word order.
Conclusion
What is the best way to approach the ESP? It is rooted in a complex environment, which has to be taken into account in order to appreciate this document fully. Magic definitely was an elementary part of ancient Egyptian medical practice and was applied at various occasions. This approach to cope with problems does not limit the overall achievements of this ancient society. Does the ESP contain science? That depends on the definition and is difficult to grasp [55]. If one applies the “modern” idea of science representing the objective truth, the answer would be no. However, respecting the specific principles to define natural events and mechanisms, which each of these ancient societies used, I would say—in a basic sense—“yes.” However, a simple “close reading” of the ESP, including one to apply modern concepts and diagnoses [56], will most likely not do justice to this unique document."

Professor Alexander Brawanski, University Hospital Regensburg, Germany
5 notes
·
View notes
Text
15 questions, 15 tags
i was tagged by my dear @unclewaynemunson :)) thank you lovely!
(also please excuse my lengthy answers, i get really excited and write a lot lmfao- and some of the answers vaguely mention shitty parenting, not in depth but it is brought up if anyone gets uncomfy by that! (questions 2 & 3 specifically :p)
1. Are you named after anyone? nope! my Government Name™️ is amethyst, like the stone, but my ma just thought it was cool :p i prefer aj or ham, though! i do say that aj stands for apple juice, so i guess i could be named after apple juice :pp
2. When was the last time you cried? friday! i heard really sad news regarding how my younger brothers are being parented by my biodad and it! hurt to realize he's not breaking his cycle :,)
3. Do you have kids? nope! but i do treat my oldest younger brother(the 18yo i write about a lot) like he's my son bc we had some Rough Moments™️ as kids where i was like the parent
4. Do you use sarcasm a lot? yes! but a lot of people don't realize it #thankyouautism
5. What's the first thing you notice about people? oooo,,,,,, it really depends? i really stare at people's lips bc i have auditory processing issues,, and apparently i recognize people based on their mouths?? but im inclined to say eyes because i like them? idk,,, lips or eyes!
6. What's your eye color? i have centralized heterochromia! (like a big portion of people tbh, but i still think it's neat) so my eyes are like,, hazel? but not green hazel, they're grey! on the outside part at least, and the inside is like a golden brown :p
7. Scary movies or happy endings? this is hard!! i really fucking love scary movies,, all of my favorite movies are scary! but i'm a sucker for a happy ending,,, i think,,,, i may have to go scary though!
8. Any special talents? idk if it's a talent but i can macrame necklaces? and i know spanish(fairly fluently, i'm really shy with it though), and am learning asl, which i think is pretty talented?? i also can decorate a cake?(pretty basically, but i know how to do some shitty roses and write!)
9. Where were you born? chicago! (indiana tho, it's like 15 minutes away from where i was born)
10. What are your hobbies? writing, drawing, watching tv, engaging with my local bdsm & queer community!! and getting tattoos and piercings<333 (i have 27 tattoos and like,,, 17? 18 piercings? idk anymore)
11. Do you have any pets? yes! i have one cat, my sweet lady Miss Rizz! i had a cat named flamer who recently had to take his forever sleep, and i miss him dearly. <3 (i'm writing a fic vaguely surrounding this idea that hopefully will be done this weekend!)
12. What sports do you play/have you played? none :)))))) unless you count,,, fishing?
13. How tall are you? i'm 5'8! which is around 173cm for my non american buddies :,)))))
14. Favorite subject in school? languages! i took four years of spanish, one of asl, and i adored my english classes! also, art and painting! and anatomy & physiology, and pathophysiology :) i'm a big human body nerd lmao (also i'm aware i shouldve chosen one but i have too many favorites to choose just one!)
15. Dream job? good question! i'm not sure, honestly. i always say being a piercer, but i tend to get bored rather quickly of jobs and i change a lot, hence why i know how to decorate cakes but also can tell you which alarm companies have a better monitoring service, and can also make a mean ass from-scratch smash burger. i think that when i went to college(i dropped out) my dream job was being a pathologist, and i honestly think that i might still want to do that? but owning a queer run/servicing primarily queer people piercing studio sounds really fucking enticing. i could go on a whole thing about body affirming piercing and the effect it has on queer people, and how we have modern day american piercing thanks to our queer predecessors, but that's nerdy and not what the question asked! so, final answer: either a pathologist, or an owner of a queer piercing shop :p
thank you so much for reading if you did!
i'm gonna tag @cheatghost @punkharringtxn @someforeignband @courtjestermunson @corrodedcorpses @riality-check @rhaenyyras @legitcookie @princessstevemunson @sidekick-hero @babygirlharrington @fagsculinity @harmonictechnicality @strawberryspence and anyone else who wants to do this! you can tag me <3
#get to know ham#pls excuse my lengthiness i cant help it#also if you wanna talk more ab anything i listed feel free to dm me!
22 notes
·
View notes
Text
1.22.23
I have not failed. I’ve just found 10,000 ways that won’t work.” -Thomas Edison
I’m two weeks into my first semester of nursing school. I’m taking two classes right now- Fundamentals of Nursing, and Pathophysiology. Fundamentals is the class that currently consumes most of my time. There are three components that make up this course: didactic, lab, and clinical. Didactic is a term that’s new to me, it’s a fancier way of saying “lecture.” I’m not sure why they call it didactic instead of lecture; but the very essence of nursing school is being unlike anything you’ve ever experienced before. More on that later. The lab portion of this class provides you an opportunity to learn and practice foundational nursing skills on a mannequin prior to attending clinical in a hospital or long term care facility and performing them for the first time on actual patients (under the direct supervision of an an RN of course). With each skill you learn, you have a couple of days to practice before you have to perform what is called a “return demo”. This is a timed and pass/fail graded demonstration of whatever skill you are learning that you perform in front of your clinical instructor. Did I mention it was timed? The clinical portion is the part where you actual go to a clinical site- a LTC facility or a hospital. That’s the extent of knowledge I have on that currently. I will update as time goes on and I get some experience under my belt. I also mentioned pathophysiology. For me, this is a fully online class and a real thorn in my side to work into my schedule, as the assignments are lengthy and time consuming, and my first exam in both classes happen to fall on the same day.
So obviously, a lot has transpired over the last two weeks. I passed my first return dem last week, but my nerves were evident. I was ecstatic about my first win in nursing school. However, I also had my first loss. I failed my first quiz. I could come up with a million excuses but the fact remains; I was ill prepared. I have always been an exceptional student in any class I’ve ever taken, really. This was my first real fail, I took it hard. I beat myself up, cried, and even had talk of quitting. In that moment (actually a little bit later when I talked to my therapist) was when I realized sure on paper I got an F, but that doesn’t have to be the end story. I have an opportunity to turn this around. I can change gears, try some different study tactics. I’m human, and I’m juggling a lot. Going to nursing school, being a mom and juggling a job is a lot on my plate and quite frankly, the hardest thing I’ve ever taken on. So it’s okay to miss the mark. It’s one quiz. So now I’m changing gears and readying myself for that A next time. I’m not a failure because I failed one quiz. I would be though, if I stopped now. My earlier threats were empty. I don’t wave my white flag that easily. Now I have a return demo and another quiz to ready myself for.
Enjoy some pictures from my first couple of weeks in nursing school.




2 notes
·
View notes
Text
At some point I am so going to end up writing metas on how status conditions are treated in humans and different common injuries from battles. After pathophysiology lectures on fluid balances and then rescue tonight I’ve got thoughts on how things like burn heal would escalate healing to quicker times than real world but have their limits (ex cant replace fluids lost).
2 notes
·
View notes
Text
JUST THREE MORE EXAMS TO GO
It's technicaly four but I haven't touched Physical Chemistry II because of the amount of Pathophysiology so I'm going to that exam as a tourist tomorrow and then I can retake it two weeks later when I'll be ready so three exams. But it's closer to two exams actually because I passed everything difficult in Human Physiology II and only left a few small tests for the final which won't take me more than a day or two to prepare
#they're extra far apart though#whoever created a system where finals are from mid june to mid july should die#i hate it#my last exam is on 14th july i think i will die until then#i haven't seen any faoi performances i haven't read a page of a book that isn't uni related in weeks this is pure torture
3 notes
·
View notes
Text
Contracture

Patreon
#studyblr#notes#my notes#medblr#medical notes#pathology#pathology notes#pathophysiology#pathophysiology notes#health and disease#diseases#disorders#human health#human disease#human pathology#human disorders#diseases and disorders#clinical pathology#clinical health#clinical disease#premed#mcat#mcat biology#medical biology#bio#biology#mcat bio#human pathophysiology
0 notes
Text
Study M.Sc Nursing in Karnataka
MSc Nursing is a postgraduate level program aimed at those who have a passion for service. The course intends to provide a deep knowledge in the training on wellness, disease and illness. In India the duration of the course is two years with internship. Those who wish to join the course should have a BSc Nursing qualification with at least 50% marks. Aspirants with a flair for nursing career could opt for a post graduation from(College name, place) where the students would be assured of getting a quality education that meets the demands of the nursing sector.

The candidates could find out top nursing colleges in karnataka with the help of My Mathews Eduportal which is the best educational consultants in kerala. The best college would be recommended by My Mathews admission guidance and career guidance team. The candidates studied in the best colleges will be selected by the top hospitals at the time of employment and recruiting. If the admission consultant is no genuine, the candidates would be cheated. If the admission is obtained by My mathews admission guidance and career guidance team, then no need for you to regret ever.
Moreover, the student could choose specializations as per their wish and skills. The various specializations for MSc Nursing provided by the universities in India are Gynecology and obstetrics nursing, medical and surgical nursing, pediatric nursing, psychiatric nursing, neuroscience and mental health nursing, critical care nursing, oncological nursing, nephrological nursing, neonatal infant and newborn nursing and so on.
Regarding the curriculum, in the first year of study, the topics such as genetics, nursing as a profession, epidemiology, philosophy and theories of nursing, economic and political aspects of health care delivery, nursing process approach, bio-psycho pathology, scope for nursing practice, psychological aspects of human relations, basis of current nursing practice and patient care delivery system, trends in nursing, teaching learning process, meaning of education, developments and trends in nursing education, continuing education in nursing, instructional media and A.V aids, overview of nursing, curriculum development, administration of nursing curriculum, guidance and counseling, teacher education for nursing profession, development of standards, accreditation in nursing education programs, administration of nursing curriculum, research design, research approaches, sampling, analysis and interpretation of data, reporting and utilization results, organization and presentation of data, measures of variability, measures of central tendency, causes-pathophysiology-investigation-clinical features and management of problems of gastrointestinal system, management of problems of endocrine system, problems of the brain and neurological system, causes-pathophysiology-investigation-clinical features and management of problems of muscle-skeletal system, causes-pathophysiology-investigation-clinical features and management of problems of urogenital system and management of problems of the cardiorespiratory system are introduced to the students. During the second year of study the students need to study introduction to management, legal and ethical issues in the nursing management, material management, management information system, roles and functions of the nurse manager in controlling, roles and functions of the nurse manager in directing, organizational behavior, organization of nursing and health delivery system, roles and function of the nurse manager in planning. Management of patients with vascular problems, assessment of normal and abnormal cardiac function, review of anatomy and physiology of cardiovascular system, prevention and control measures of cardiothoracic & vascular disorder, planning and organization of critical care units, advance nursing procedures, geriatric nursing, clinical features and management of problems of infectious conditions, immune system compromising conditions and blood and blood-forming organs as part of theory. The practical session include clinical nursing, thesis viva, nursing education, and management.
The admission to the course vary from college to college. There will be an entrance test and admission is based on the cut-off scores secured by the test followed by a counselling session. The students after completing the course could be able to work both in the private and private organizations, nursing homes, military hospital, medicine industry, medical colleges and universities, healthcare centres, content writing and much more.The various job responsibilities suitable for the aspirants are Nursing Supervisor, Ward Nurse, Tutor(Psychiatric Nursing), Paramedic Nurse, Occupational Health Nurse, Nursing Tutor, Nursing in-charge, Nursing Executive, Dietician, Medical Advisor, Clinical Instructor, Anesthetist, Assistant Nursing Superintendent and the like wit eye-catching salary.
The compensation packages vary from hospital to hospital, country to country, as per skills, experience and other factors. In India, the annual salary for the jobseekers are about 2 lakhs per annum. Nursing professors could get a salary of 536400/- per year. However, the salary packages for the job seekers abroad are double or triple than that in India. In the US, the remuneration of MSc Nurse is $48480 and that of nursing professor ranges from $78417and $142840 in the year. The salary of Nursing Manager in Australia ranges from $69000 and $118000 and that of nursing practitioner it is $77000 to $111000.Canada has a huge demand for nurses with PG and the salary is about 58 lac annually. In the Ireland, Nursing professor at an entry level with an experience of 1-3 years is 32134 euro. However, nursing professor with an experience of about 8 years has a salary of 54080 euro annually in the Ireland. Nursing lecturer salary at entry level in the UK is about 39126 per year.
My Mathews is there in the field of admission counselling for more than two decade and are the best admission guidance providers who guide students to pursue higher studies in the best colleges and top colleges across the country. Our admission team of guidance and career guidance would definitely help you in getting admission in the best and top colleges for securing a nursing degree.
#best nursing colleges in karnataka#top nursing colleges in bangalore#nursing colleges in india#best nursing colleges
2 notes
·
View notes
Text
Empowering Healthcare: The Role and Benefits of an Allied Health Assistant Course
In the dynamic landscape of healthcare, allied health professionals play a pivotal role in supporting patient care, rehabilitation, and therapeutic interventions. Among the pathways to entering this rewarding field is through an Allied Health Assistant course. In this comprehensive guide, we'll explore the significance of Allied Health Assistants, the curriculum of the course, career prospects, and the impact they have on the healthcare industry.
Understanding Allied Health Assistants
Allied Health Assistants (AHAs) are integral members of multidisciplinary healthcare teams, working alongside allied health professionals such as physiotherapists, occupational therapists, speech pathologists, and podiatrists. They provide essential support in delivering therapeutic interventions, implementing treatment plans, assisting with patient exercises, and maintaining clinical documentation. AHAs often work in diverse healthcare settings, including hospitals, rehabilitation centers, community clinics, aged care facilities, and schools.
Importance of Allied Health Assistant Course
An Allied Health Assistant course serves as a foundational training program that equips individuals with the knowledge, skills, and practical experience necessary to excel in their roles as AHAs. The course covers a range of topics relevant to allied health practice, including:
Anatomy and Physiology: Understanding the human body's structure, function, and systems, including musculoskeletal, cardiovascular, respiratory, neurological, and sensory systems.
Therapeutic Techniques: Learning evidence-based therapeutic techniques and interventions, such as mobility exercises, rehabilitation exercises, therapeutic activities, and sensory stimulation techniques.
Communication Skills: Developing effective communication skills for interacting with patients, families, and healthcare teams, including active listening, empathy, cultural sensitivity, and professional documentation.
Clinical Procedures: Assisting with clinical procedures, treatment modalities, equipment setup, patient positioning, and infection control measures in compliance with healthcare standards.
Patient Care and Support: Providing direct patient care and support, including assistance with activities of daily living (ADLs), mobility support, personal hygiene, and emotional support.
Professionalism and Ethics: Understanding ethical principles, confidentiality requirements, professional boundaries, and legal responsibilities in allied health practice.
Health Promotion and Education: Promoting health literacy, conducting health assessments, delivering health education sessions, and empowering patients to manage their health and wellbeing.
Curriculum Overview of Allied Health Assistant Course
The curriculum of an Allied Health Assistant course is designed to provide comprehensive training and practical experience aligned with industry standards and best practices. Key components of the curriculum typically include:
Theoretical Foundations: Foundational knowledge in anatomy, physiology, pathophysiology, and medical terminology relevant to allied health practice.
Clinical Skills Development: Hands-on training in therapeutic techniques, patient care procedures, equipment handling, and safety protocols in simulated and clinical settings.
Interdisciplinary Collaboration: Understanding the roles and responsibilities of allied health professionals, effective teamwork, communication strategies, and collaborative care approaches.
Professional Development: Ethical considerations, legal requirements, professional conduct, continuing education, and career pathways in allied health.
Practical Placements: Structured clinical placements or work-integrated learning experiences in healthcare facilities, allowing students to apply their knowledge and skills under supervision, gain real-world experience, and build professional networks.
Specialized Areas: Optional modules or electives in specialized areas of allied health practice, such as aged care, disability support, mental health, pediatric care, or rehabilitation.
Career Prospects for Allied Health Assistants
Upon successful completion of an Allied Health Assistant course, graduates are well-positioned to pursue diverse career pathways within allied health settings. Some common job roles and career opportunities for AHAs include:
Physiotherapy Assistant: Assisting physiotherapists in delivering exercise programs, mobility assessments, therapeutic interventions, and patient education sessions for individuals with musculoskeletal injuries, neurological conditions, or chronic pain.
Occupational Therapy Assistant: Supporting occupational therapists in facilitating activities of daily living (ADLs), functional assessments, assistive technology use, home modifications, and vocational rehabilitation for clients with disabilities or injuries.
Speech Pathology Assistant: Collaborating with speech pathologists in conducting communication assessments, speech therapy sessions, language interventions, swallowing assessments, and augmentative communication support for clients with speech and language disorders.
Podiatry Assistant: Assisting podiatrists in foot care, orthotic fittings, wound management, diabetic foot assessments, gait analysis, and footwear advice for clients with foot-related conditions or injuries.
Aged Care Assistant: Providing personal care, mobility support, social engagement, and therapeutic activities for elderly clients in aged care facilities, supporting their independence, wellbeing, and quality of life.
Rehabilitation Assistant: Supporting rehabilitation teams in delivering rehabilitation programs, mobility training, functional assessments, home exercise plans, and community reintegration for clients recovering from injuries, surgeries, or illnesses.
Community Support Worker: Collaborating with community health teams, disability support services, and mental health programs to deliver person-centered care, community inclusion support, lifestyle interventions, and psychosocial support for clients in community settings.
Impact of Allied Health Assistants on Healthcare
The role of Allied Health Assistants has a significant impact on the healthcare industry, contributing to:
Improved Patient Outcomes: AHAs play a vital role in facilitating therapeutic interventions, promoting functional independence, enhancing quality of life, and achieving optimal health outcomes for patients across diverse populations and age groups.
Efficient Healthcare Delivery: By assisting allied health professionals with clinical procedures, treatment plans, and patient support, AHAs contribute to efficient healthcare delivery, reduced waiting times, and increased patient access to allied health services.
Multidisciplinary Collaboration: AHAs enhance interdisciplinary collaboration and teamwork within healthcare teams, fostering effective communication, continuity of care, and coordinated care plans for patients with complex needs.
Patient-Centered Care: AHAs prioritize patient-centered care, respecting individual preferences, cultural diversity, and holistic wellbeing while promoting autonomy, self-management, and active participation in healthcare decisions.
Workforce Support: AHAs alleviate the workload of allied health professionals, allowing them to focus on advanced assessments, specialized interventions, and clinical decision-making, thereby enhancing overall workforce capacity and job satisfaction.
Innovation and Adaptation: AHAs contribute to innovation and adaptation within allied health practice, implementing new technologies, evidence-based interventions, and best practice guidelines to improve service delivery and outcomes.
Conclusion
An Allied Health Assistant course serves as a gateway to a fulfilling and impactful career in healthcare, empowering individuals to make a meaningful difference in the lives of patients and communities. With a comprehensive curriculum, hands-on training, and diverse career pathways, AHAs play an essential role in delivering high-quality, patient-centered care, promoting health and wellbeing, and advancing the goals of allied health practice. As integral members of healthcare teams, AHAs contribute to a dynamic, collaborative, and resilient healthcare ecosystem focused on enhancing health outcomes and quality of life for individuals across the lifespan.
0 notes
Text
From Bench to Bedside: Translating Nephrology Research into Clinical Practice
Introduction
The journey from bench to bedside represents a pivotal bridge in the field of nephrology, where groundbreaking research findings are translated into tangible clinical applications, improving patient outcomes and shaping the landscape of renal care. This article explores the intricate process of translating nephrology research from bench to bedside and the profound impact it has on clinical practice.
Innovations in Renal Research
At the forefront of nephrology research, scientists and clinicians are engaged in a perpetual quest to unravel the mysteries of kidney function and disease. From elucidating the genetic and molecular mechanisms underlying renal disorders to pioneering novel therapeutic strategies, research endeavors in nephrology span a diverse array of disciplines, including genetics, cellular biology, pharmacology, and bioengineering.
Cutting-edge advancements in renal research have yielded transformative insights into the pathophysiology of kidney diseases, paving the way for innovative diagnostic tools, therapeutic interventions, and personalized treatment approaches. By harnessing the power of basic science and translational research, nephrology researchers strive to address unmet clinical needs, optimize treatment outcomes, and improve the quality of life for patients with kidney diseases.
Translational Research Paradigms
Translating nephrology research from bench to bedside involves a multifaceted and iterative process that bridges the gap between scientific discovery and clinical application. Translational research paradigms encompass a continuum of activities, including preclinical studies, clinical trials, and implementation science, aimed at evaluating the safety, efficacy, and feasibility of novel interventions in real-world clinical settings.
Preclinical studies, conducted in laboratory models and animal systems, provide crucial insights into the mechanisms of action and therapeutic potential of novel interventions for kidney diseases. These findings serve as the foundation for subsequent clinical trials, where the safety and efficacy of experimental treatments are evaluated in human subjects.
Clinical Trials and Evidence-Based Medicine
Clinical trials represent the cornerstone of evidence-based medicine in nephrology, providing rigorous scientific evidence to guide clinical practice and inform treatment decisions. Randomized controlled trials (RCTs), observational studies, and systematic reviews play a pivotal role in evaluating the effectiveness, safety, and comparative effectiveness of interventions for kidney diseases.
Moreover, collaborative research consortia and multicenter trials foster synergies among investigators, clinicians, and patients, accelerating the pace of discovery and enhancing the generalizability of research findings. By adhering to rigorous methodological standards and ethical principles, clinical trials ensure the integrity and validity of research findings, ultimately guiding clinical practice and improving patient care.
Implementation Science and Quality Improvement
Translating nephrology research into clinical practice requires not only scientific rigor but also a commitment to implementation science and quality improvement initiatives. Implementation science focuses on bridging the gap between research evidence and clinical practice, identifying barriers and facilitators to the adoption of evidence-based interventions, and implementing strategies to promote their uptake and sustainability in real-world settings.
Quality improvement initiatives, such as clinical practice guidelines, performance metrics, and continuous quality monitoring, aim to optimize the delivery of renal care, enhance patient outcomes, and reduce practice variations. By leveraging principles of implementation science and quality improvement, nephrology researchers and clinicians can ensure that evidence-based interventions are effectively translated into clinical practice, ultimately improving the quality and efficiency of renal care delivery.
Conclusion
In conclusion, the translation of nephrology research from bench to bedside represents a dynamic and iterative process that drives innovation, improves patient outcomes, and shapes the landscape of renal care. By embracing translational research paradigms, conducting rigorous clinical trials, and implementing evidence-based interventions, nephrology researchers and clinicians can bridge the gap between scientific discovery and clinical practice, ultimately advancing the field of nephrology and improving the lives of patients with kidney diseases.
1 note
·
View note
Link
0 notes
Photo

Introduction to Human Disease: Pathophysiology for Health Professionals, Sixth Edition provides a broad overview of the most common and important human diseases for students pursuing careers in the health professions. Comprehensive yet accessible, it addresses the aspects of disease epidemiology, diagnosis, and treatment that are essential to clinical practice. The Sixth Edition of this popular
0 notes