#dsm 5 tr
Text
Diagnostic Criteria Examples Masterpost
This is a series of posts that I'm hoping eventually covers all the disorders in the DSM-5-TR.
**This will be periodically updated as more posts are made. Please come back to the original post to see these updates**
NEURODEVELOPMENTAL DISORDERS
Intellectual Developmental Disorder (Intellectual Disability)
Global Develolmental Delay
Unspecified Intellectual Developmental Disorder (Intellectual Disability)
Language Disorder
Speech Sound Disorder
Childhood-Onset Fluency Disorder (Stuttering)
Social (Pragmatic) Communication Disorder
Unspecified Communication Disorder
Autism Spectrum Disorder (Levels System)
Attention-Deficit/Hyperactivity Disorder
Other Specified Attention-Deficit/Hyperactivity Disorder
Unspecified Attention-Deficit/Hyperactivity Disorder
Specific Learning Disorder
Developmental Coordination Disorder
Stereotypic Movement Disorder
Tourette's Disorder [Tourette Syndrome]
Persistent (Chronic) Motor or Vocal Tic Disorder
Provisional Tic Disorder
Other Specified Tic Disorder
Unspecified Tic Disorder
Other Specified Neurodevelopmental Disorder
Unspecified Neurodevelopmental Disorder
SCHIZOPHRENIA SPECTRUM AND OTHER PSYCHOTIC DISORDERS
Delusional Disorder
Brief Psychotic Disorder
Schizophreniform Disorder
Schizophrenia
Schizoaffective Disorder
Substance/Medication-Induced Psychotic Disorder
Psychotic Disorder Due to Another Medical Condition
Catatonia Associated With Another Mental Disorder (Catatonia Specifier)
Catatonic Disorder Due to Another Medical Condition
Unspecified Catatonia
Other Specified Schizophrenia Spectrum and Other Psychotic Disorder
Unspecified Schizophrenia Spectrum and Other Psychotic Disorder
BIPOLAR AND RELATED DISORDERS
Bipolar I Disorder [Includes criteria for manic episodes and major depressive episodes]
Bipolar II Disorder [Includes criteria for hypomanic episodes and major depressive episodes]
Cyclothymic Disorder
Substance/Medication-Induced Bipolar and Related Disorder
Bipolar and Related Disorder Due to Another Medical Condition
Other Specified Bipolar and Related Disorder
Unspecified Bipolar and Related Disorder
Unspecified Mood Disorder
Specifiers for Bipolar and Related Disorders
DEPRESSIVE DISORDERS
Disruptive Mood Dysregulation Disorder
Major Depressive Disorder
Persistent Depressive Disorder
Premenstrual Dysphoric Disorder
Substance/Medication-Induced Depressive Disorder
Depressive Disorder Due to Another Medical Condition
Other Specified Depressive Disorder
Unspecified Depressive Disorder
Specifiers for Depressive Disorders
ANXIETY DISORDERS
Separation Anxiety Disorder
Selective Mutism
Specific Phobia
Social Anxiety Disorder
Panic Disorder
Panic Attack Specifier
Agoraphobia
Generalized Anxiety Disorder
Substance/Medication-Induced Anxiety Disorder
Anxiety Disorder Due to Another Medical Condition
Other Specified Anxiety Disorder
Unspecified Anxiety Disorder
OBSESSIVE-COMPULSIVE AND RELATED DISORDERS
Obsessive-Compulsive Disorder
Body Dysmorphic Disorder
Hoarding Disorder
Trichotillomania (Hair-Pulling Disorder)
Excoriation (Skin-Picking) Disorder [Also called Dermatillomania]
Substance/Medication-Induced Obsessive-Compulsive and Related Disorder
Obsessive-Compulsive and Related Disorder Due to Another Medical Condition
Other Specified Obsessive-Compulsive and Related Disorder
Unspecified Obsessive-Compulsive and Related Disorder
TRAUMA- AND STRESSOR-RELATED DISORDERS
Reactive Attachment Disorder
Disinhibited Social Engagement Disorder
Posttraumatic Stress Disorder
Acute Stress Disorder
Adjustment Disorders
Prolonged Grief Disorder
Other Specified Trauma- and Stressor-Related Disorder
Unspecified Trauma- and Stressor-Related Disorder
DISSOCIATIVE DISORDERS
Dissociative Identity Disorder
Dissociative Amnesia
Depersonalization/Derealization Disorder
Other Specified Dissociative Disorder
Unspecified Dissociative Disorder
SOMATIC SYMPTOM AND RELATED DISORDERS
Somatic Symptom Disorder
Illness Anxiety Disorder [Hypochondria]
Functional Neurological Symptom Disorder (Conversion Disorder)
Psychological Factors Affecting Other Medical Conditions
Factitious Disorder Imposed on Self
Factitious Disorder Imposed on Another
Other Specified Somatic Symptom and Related Disorder
Unspecified Somatic Symptom and Related Disorder
FEEDING AND EATING DISORDERS
Pica
Rumination Disorder
Avoidant/Restrictive Food Intake Disorder
Anorexia Nervosa
Bulimia Nervosa
Binge-Eating Disorder
Other Specified Feeding or Eating Disorder
Unspecified Feeding or Eating Disorder
ELIMINATION DISORDERS
Enuresis
Encopresis
Other Specified Elimination Disorder
Unspecified Elimination Disorder
SLEEP-WAKE DISORDERS
Insomnia Disorder
Hypersomnolence Disorder
Narcolepsy
Obstructive Sleep Apnea Hypopnea
Central Sleep Apnea
Sleep-Related Hypoventilation
Circadian Rhythm Sleep-Wake Disorders
Non-Rapid Eye Movement Sleep Arousal Disorders [Sleepwalking and Sleep/Night Terrors]
Nightmare Disorder
Rapid Eye Movement Sleep Behavior Disorder
Restless Legs Syndrome
Substance/Medication-Induced Sleep Disorder
Other Specified Insomnia Disorder
Unspecified Insomnia Disorder
Other Specified Hypersomnolence Disorder
Unspecified Hypersomnolence Disorder
Other Specified Sleep-Wake Disorder
Unspecified Sleep-Wake Disorder
SEXUAL DYSFUNCTIONS
Delayed Ejaculation
Erectile Disorder [Erectile Dysfunction]
Female Orgasmic Disorder
Female Sexual Interest/Arousal Disorder
Genito-Pelvic Pain/Penetration Disorder
Male Hypoactive Sexual Desire Disorder
Premature (Early) Ejaculation
Substance/Medication-Induced Sexual Dysfunction
Other Specified Sexual Dysfunction
Unspecified Sexual Dysfunction
GENDER DYSPHORIA
Gender Dysphoria
Other Specified Gender Dysphoria
Unspecified Gender Dysphoria
DISRUPTIVE, IMPULSE-CONTROL, AND CONDUCT DISORDERS
Oppositional Defiant Disorder
Intermittent Explosive Disorder
Conduct Disorder
Pyromania
Kleptomania
Other Specified Disruptive, Impulse-Control, and Conduct Disorder
Unspecified Disruptive, Impulse-Control, and Conduct Disorder
SUBSTANCE-RELATED AND ADDICTIVE DISORDERS
Alcohol Use Disorder
Alcohol Intoxication
Alcohol Withdrawal
Unspecified Alcohol-Related Disorder
Caffeine Intoxication
Caffeine Withdrawal
Unspecified Caffeine-Related Disorder
Cannabis Use Disorder
Cannabis Intoxication
Cannabis Withdrawal
Unspecified Cannabis-Related Disorder
Phencyclidine Use Disorder
Other Hallucinogen Use Disorder
Phencyclidine Intoxication
Other Hallucination Intoxication
Hallucinogen Persisting Perception Disorder
Unspecified Phencyclidine-Related Disorder
Unspecified Hallucinogen-Related Disorder
Inhalant Use Disorder
Inhalant Intoxication
Unspecified Inhalant-Related Disorder
Opioid Use Disorder
Opioid Intoxication
Opioid Withdrawal
Unspecified Opioid-Related Disorder
Sedative, Hypnotic, or Anxiolytic Use Disorder
Sedative, Hypnotic, or Anxiolytic Intoxication
Sedative, Hypnotic, or Anxiolytic Withdrawal
Unspecified Sedative-, Hypnotic-, or Anxiolytic-Related Disorder
Stimulant Use Disorder
Stimulant Intoxication
Stimulant Withdrawal
Unspecified Stimulant-Related Disorder
Tobacco Use Disorder
Tobacco Withdrawal
Unspecified Tobacco-Related Disorder
Other (or Unknown) Substance Use Disorder
Other (or Unknown) Substance Intoxication
Other (or Unknown) Substance Withdrawal
Unspecified Other (or Unknown) Substance-Related Disorder
Gambling Disorder
NEUROCOGNITIVE DISORDERS
Delirium
Other Specified Delirium
Unspecified Delirium
Major Neurocognitive Disorder
Minor Neurocognitive Disorder
Major or Mild Neurocognitive Disorder Due to Alzheimer's Disease
Mild or Major Frontotemporal Neurocognitive Disorder
Mild or Major Neurocognitive Disorder With Lewy Bodies
Major or Mild Vascular Neurocognitive Disorder
Major or Mild Neurocognitive Disorder Due to Traumatic Brain Injury
Substance/Medication-Induced Major or Mild Neurocognitive Disorder
Major or Mild Neurocognitive Disorder Due to HIV Infection
Major or Mild Neurocognitive Disorder Due to Prion Disease
Major or Mild Neurocognitive Disorder Due to Parkinson's Disease
Major or Mild Neurocognitive Disorder Due to Huntington's Disease
Major or Mild Neurocognitive Disorder Due to Another Medical Condition
Major or Mild Neurocognitive Disorder Due to Multiple Etiologies
Unspecified Neurocognitive Disorder
PERSONALITY DISORDERS
General Personality Disorder
Paranoid Personality Disorder
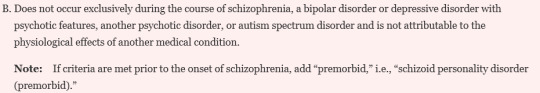
Schizoid Personality Disorder
Schizotypal Personality Disorder
Antisocial Personality Disorder
Borderline Personality Disorder
Histrionic Personality Disorder
Narcissistic Personality Disorder
Avoidant Personality Disorder
Dependent Personality Disorder
Obsessive-Compulsive Personality Disorder [Anankastic Personality Disorder]
Personality Change Due to Another Medical Condition
Other Specified Personality Disorder
Unspecified Personality Disorder
PARAPHILIC DISORDERS
Voyeuristic Disorder
Exhibitionistic Disorder
Frotteuristic Disorder
Sexual Masochism Disorder
Sexual Sadism Disorder
Pedophilic Disorder
Fetishistic Disorder
Transvestic Disorder
Other Specified Paraphilic Disorder
Unspecified Paraphilic Disorder
OTHER MENTAL DISORDERS AND ADDITIONAL CODES
Other Specified Mental Disorder Due to Another Medical Condition
Unspecified Mental Disorder Due to Another Medical Condition
Other Specified Mental Disorder
Unspecified Mental Disorder
MEDICATION-INDUCED MOVEMENT DISORDERS AND OTHER ADVERSE EFFECTS OF MEDICATION
Medication-Induced Parkinsonism
Neuroleptic Malignant Syndrome
Medication-Induced Acute Dystonia
Medication-Induced Acute Akathisia
Tardive Dyskinesia
Tardive Dystonia [and] Tardive Akathisia
Medication-Induced Postural Tremor
Other Medication-Induced Movement Disorder
Antidepressant Discontinuation Syndrome
Other Adverse Effect of Medication
61 notes
·
View notes
Text
I think we need to focus less on the arbitrary division that's been created with PDs when it comes to clusters. The DSM itself notes that the grouping of PDs into clusters is only for research purposes. This is what the DSM-5-TR says in the PD section:
"It should be noted that this clustering system, although useful in some research and educational situations, has serious limitations and has not been consistently validated. For instance, two or more disorders from different clusters, or traits from several of them, can often co-occur and vary in intensity and pervasiveness."
The PDs within each cluster have similarities, yes, but they're not dissimilar from the PDs in other clusters. SzPD has a lot in common with StPD but also with NPD and BPD and OCPD and AvPD - none of which are in the same cluster A. There is no significant meaning behind cluster groupings, don't treat them like there is.
102 notes
·
View notes
Text
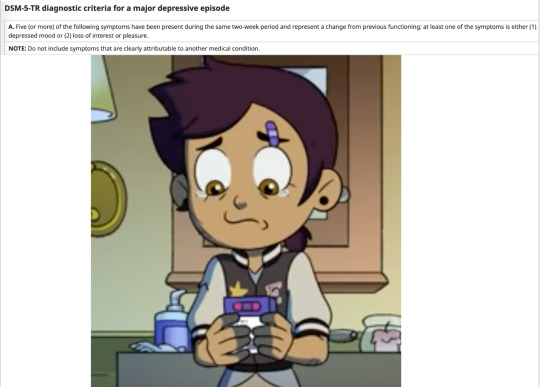






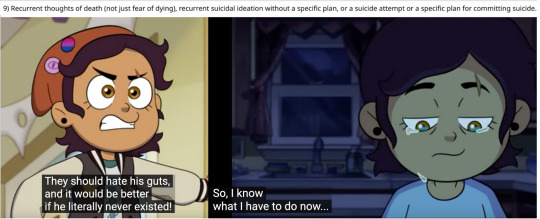

Luz Noceda in S3E1 + DSM-5-TR criteria for a Major Depressive Episode
(I know 9 is a bit of a stretch but the subtext is strong)
#the owl house#tw suicide mention#luz noceda#camila noceda#amity blight#dsm#dsm 5#dsm 5 tr#depression#major depressive episode
12 notes
·
View notes
Text
Not to mention the fact that ASD is supposed to be a spectrum disorder. That's what it's supposed to be. And any and all spectrum disorders need to include that not all symptoms might be present/disabling. The recent change in the DSM-V-TR listing of ASD necessitated that all symptoms be present, which by design makes it not a spectrum disorder.
We can talk about why they did this, namely the large increase in self-awareness and diagnosis due to increased resources that have challenged the status quo in terms of the dominant neurotype, but I want to talk about the specific wording they used, and why this isn't the change they're looking for.
By doing this, they're essentially moving back to the DSM-IV, which listed Aspergers as a separate disorder from Autism due to relative lack of impairment, except this time we don't have Aspergers as a diagnosis. They're specifically and intentionally leaving out a body of people who are struggling and significantly disabled and in need of resources because they don't like what the numbers are saying they're doing to that population.
To specify the changes made, there is still the 2 of 4 required for the diagnostic section of repetitive behaviors. But the section for social defects, specifically the one that is often underscored in minorities and women due to masking and compensation, now requires all three, which makes even less sense than changing the criteria for repetitive behavior due to the discriminatory factors and the fact that they started out by saying they would use the TR to make it MORE inclusive and account for those who are divergent in their presentation due to other factors or variables.
The only way I can see to fix this while maintaining the changes made is to bring back the Aspergers profile in the DSM, likely under another name because there's little use in keeping a name that is after someone specifically discriminatory. The irony.
And all this because they couldn't handle the fact that our society is far more diverse than they thought or wanted. I remember being so excited at the update. Ridiculous.
#autism#actually autistic#dsm 5#dsm 5 tr#psychiatry#psychology#im actually really mad about this#the previous post just reminded me#autistic pride#systematic oppression#what the fuck yall#they really said fuck the poor and marginalized
9 notes
·
View notes
Note
Hello Tistje !!! Do you think or What do you think about Mark Zuckerberg is or can be lightly Autistic ?? Considering on a post you did about Elon Musk on your personal blog !! 
It's a bit hard to say, as we only know him from his public life, but I would be very surprised if Mark Zuckerberg were autistic. If you asked me to bet on a DSM-code, I would put my money on one of the personality disorders or just eccentricity and talent of doing business.
4 notes
·
View notes
Text
Btw, it's been a while, but if anybody was looking to criticize the dsm, there's been a text revision, so look for that newest edition
0 notes
Text
"Comorbid sleep disorders in ADHD are associated with daytime impairments in cognition (e.g., inattention). Many individuals with ADHD report daytime sleepiness that may meet criteria for hypersomnolence disorder. One quarter to one-half of individuals with ADHD report sleep difficulties; studies have shown an association of ADHD with insomnia, circadian rhythm sleep-wake disorder, sleep-disordered breathing, and restless legs syndrome."
American Psychiatric Association. (2022). Neurodevelopmental disorders. In Diagnostic and statistical manual of mental disorders (5th ed., text rev.).
24 notes
·
View notes
Text
So the newly proposed model of personality disorders is fascinating. The criteria has changed a bit so for example with aspd the violent or aggressive behaviors are considered a "varient" as opposed to part of the disorder itself.
It says "specify if with psychopathic features." This is big. This is a shift away from perceiving aspd people as criminals and inmates only. It's interesting.
62 notes
·
View notes
Text
DSM-V TR - Gender Dysphoria.PDF 2022
If anyone wants a PDF here it is
#transgender#trans#trans rights#dsm v tr#dsm#gender dysphoria#Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR)#Diagnostic and Statistical Manual of Mental Disorders
5 notes
·
View notes
Text
What the DSM-5-TR 2022 Says about Factitious disorder and malingering
“Individuals who feign dissociative identity disorder usually do not report the subtle symptoms of intrusion characteristic of the disorder; instead they tend to overreport media-based symptoms of the disorder, such as dramatic dissociative amnesia and melodramatic switching behaviors, while underreporting less-publicized comorbid symptoms, such as depression. Individuals who feign dissociative identity disorder tend to be relatively undisturbed by or may even seem to enjoy “having” the disorder, or may ask clinicians to “find” traumatic memories. In contrast, most individuals with genuine dissociative identity disorder are ashamed of and overwhelmed by their symptoms, deny the diagnosis, underreport their symptoms, and display minimization and avoidance of their trauma history.
Individuals who feign the symptoms of dissociative identity disorder usually create limited, stereotyped alternate identities, with feigned amnesia related only to the events for which gain is sought, with apparent switching behaviors and amnesia only displayed while being observed. They may present an “all-good” identity and an “all-bad” identity in hopes of gaining exculpation for a crime.”
Now that’s a whole lot. Take what you want from the DSM-5, and leave what is not helpful. I honestly don’t know how people studying psychology and living with this disorder feel about the current version of the DSM-5 in the description of DID, which is not here, this is taken as a small section following comparisons of DID to other disorders it gets misdiagnosed for. I have to explain my own feelings and experience here, and then I’ll talk about the other things I have picked up on from the community.
When I had first begun noticing my symptoms, they were pointed out to me. I assumed someone was joking, or bullying me as they usually did, and disregarded all they had said. I don’t even remember what they pointed out, only that I felt exposed and like they were teasing, conflicting emotions at the same time. As I aged, my stories I would tell family were often inconsistent. I would act loving to one sibling, then talk shit to the other, then I would completely forget about them being there in the house. Gaps of memory loss repeated, and they were extremely minor things to major areas of my life where I hadn’t acted out in any way, but I still was not present for any of it. An example was when I went to Disney in Florida with my dad and brother. I have evidence I was there, but the only memory I had was wondering how long my dad would be out tonight. Drinking. Not knowing was always scary to me. When I talked about it (memory loss) with professionals, it was common to experience some childhood memory loss as you get closer to your twenties. I knew I had some awful shit happen to me, as pain had continued all the way until I was about 17, but I didn’t know the extent of any of it. I still do not know. I do not want to know, I never asked to know, and anything that comes close to reminding me of it, I run. I did not know I had DID. I did not know I had anything at all, except that I was depressed. My family treated mental health as an inconvenience, as I was the only one vocal about it.
My ‘identities’ I had at the time, I assumed to be just artistic expression of characters I enjoyed. I only know of 2. First was visual hallucinations of Castiel, only appearing when I was in danger of being hurt. He was briefly in my life, a matter of 7 months, but Sherlock Holmes (now well, well integrated) I often laughed at the idea of being him. For nearly 2 years! It wasn’t simply, ah yes Mr. Holmes. But-- the attitudes, the small grains of details, the pleasant sensations of dopamine, dull driven towards isolation, and the heavy weight of depression when I hadn’t had my own personal version of a ‘high.’ How does a high schooler experience any of that? I didn’t question it, and I didn’t look anything up as to what was going on. I didn’t have control over it, and I had begun missing classes for reasons unknown. Friends retreated as my behavior got more closed-off, I engaged mostly in communities where RP was extraordinarily popular, and my home life was so unstable, I am glad I don’t know how many times I was injured by loved ones. But when I had another tragic event happen, and he had split, I was in danger, and I had put myself in danger, but had never told a soul.
These aren’t qualities you want.
When I got to college, I didn’t understand who the hell I was supposed to be. Literally. I know people say that a lot, but it was beyond looking in the mirror, confused, it was ‘I’m going to be fucking sick.’ I didn’t understand why I would own so many feminine things, why did I like white frilly bedding? Since when? None of it made any sense, a few months later I cut my hair, stopped wearing more feminine clothes, used different pronouns because I’ll be damned to be forced to be a woman. Gender dysphoria was not enough of a description for what was happening. When I heard things, I saw things, all so unexplainable, it would happen when I was on the verge of not recovering from attempts. They had distracted me long enough to get me out of the situation, and after the self hatred I had would be all consuming. These kinds of things are what it’s like for someone w/ DID. We do not have strict rules, no real answers as to what is and isn’t possible, people with DID are trying to survive reality.
I am not trying to make this long post as a way of saying, you have to had have a miserable life to really have DID. No, because I have known people that were so successful, but so fucking depressed, and happened to have people among them internally. More so, if you are trying to research DID, and come across accounts like ours, where we are open about who we are and what we look like, what we enjoy...... etc..... Please be cautious. I say I have it, it does not mean I was proud of it, or currently want it. It’s not cruel to them to say I wish I did not, because they know if I did not then the severity of trauma wouldn’t exist. We’re comfortable in acceptance as we have gone beyond denial. If you look at my archive, this blog is new. It was made 2022. I do not have any other social accounts where I came out as a system because of how afraid I was of myself, even though I’ve known for so long now, there was no pride in it. Only fear. Never confessing to anyone. Only confusion, rage, and amnesia. Reasons why people on here engage in discourse is because they feel the need to protect others from getting them involved in a space where it’s actually not safe at all. We’re traumatised people that have come together to try live, and unless someone in the group has some form of therapy to offer, it’s often a mess of voices and vents. The smaller communities don’t have this happen too often, because even three accounts could be 20 different people with 20 different opinions. Some far more. People fight every day over what DID is and what has to happen for it, but don’t dare try to address how we need to be trying to get ourselves in a safer place over finding someone else who maybe had the Same Kind of Trauma.
I also love to be told why I am wrong, and if you’re comfortable with it, I’d love to have a discussion where I won’t talk over you or fight you on any of it. I enjoy learning deeply, but only these types of topics... Sometimes personal knowledge is more valuable to me.
#long post#isaac#system discourse#did system#system stuff#dsm-5-tr#quen#I think why I am so scared now is because i'm getting a new psy evaluation and im scared somehow I have done this to myself when the years#of evidence exist#so yes not a good idea to read the DSM-5 to prepare#but i look at the whole picture of it this time#this post is not a good example....
3 notes
·
View notes
Text
note to everyone who’s interested in the DSM-V-TR:
you can get a free PDF copy at z-lib via the following link or you can visit z-lib(dot)org, click on books, and type in the title you’re looking for
17 notes
·
View notes
Text
Core schizoid traits and criteria
From the Psychodynamic Diagnostic Manual (2006):
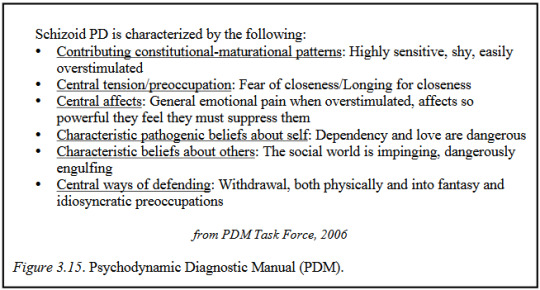
From the DSM-IV-TR (2000) and the ICD-10 (2019):

Guntrip's core traits (1969):
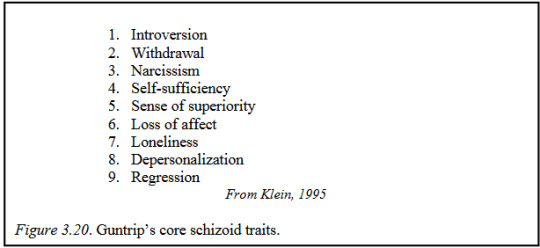
In the SWAP-200 personality assessment:

From the DSM-5-TR (2022):

The ICD-11 (2022) doesn't have a specific schizoid diagnosis, but it's detachment trait domain in its personality disorder traits section is similar to SzPD:
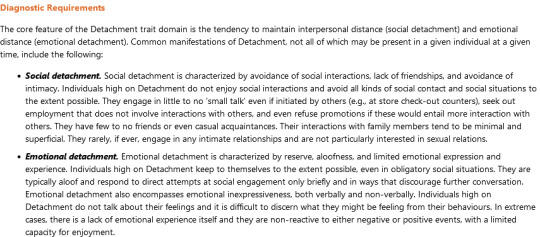
From Zachary Wheeler, Treatment of Schizoid Personality [dissertation] (2013); the DSM-5-TR (2022), & the ICD-11 (2022).
#szpd#szpd info#pd info#pdm#dsm-iv-tr#dsm iv tr#icd 10#icd-10#dsm-5-tr#dsm 5 tr#icd 11#icd-11#harry guntrip#zachary wheeler#swap-200#swap 200#described in alt text#described#dogpost#long post#diagnostic criteria
73 notes
·
View notes
Text
Random psychology disorder (somewhat) explained #1 (Trichotillomania/Hair-Pulling Disorder)
Diagnostic Criteria
A. Recurrent pulling out of one’s hair, resulting in hair loss.
B. Repeated attempts to decrease or stop hair pulling.
C. The hair pulling causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
D. The hair pulling or hair loss is not attributable to another medical condition (e.g., a dermatological condition).
E. The hair pulling is not better explained by the symptoms of another mental disorder (e.g., attempts to improve a perceived defect or flaw in appearance in body dysmorphic disorder).
Diagnostic Features
The essential feature of trichotillomania (hair-pulling disorder) is the recurrent pulling out of one’s own hair (Criterion A).
Hair pulling may occur from any region of the body in which hair grows; the most common sites are the scalp, eyebrows, and eyelids, while less common sites are axillary, facial, pubic, and perirectal regions.
Hair-pulling sites may vary over time.
Hair pulling may occur in brief episodes scattered throughout the day or during less frequent but more sustained periods that can continue for hours, and such hair pulling may endure for months or years.
Criterion A requires that hair pulling lead to hair loss, although individuals with this disorder may pull hair in a widely distributed pattern (i.e., pulling single hairs from all over a site) such that hair loss may not be clearly visible.
In addition, individuals may attempt to conceal or camouflage hair loss (e.g., by using makeup, scarves, or wigs).
Individuals with trichotillmania have made repeated attempts to decrease or stop hair pulling (Criterion B).
Criterion C indicates that hair pulling causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
The term distress includes negative affects that may be experienced by individuals with hair pulling, such as feelings a loss of control, embarrassment, and shame.
Significant impairment may occur in several different areas of functioning (e.g., social, occupational, academic, and leisure), in part because of avoidance of work, school, or other public situations.
Associated Features
Hair pulling may be accompanied by a range of behaviors or rituals involving hair.
Thus, individuals may search for a particular kind of hair to pull (e.g., hairs with specific texture or color), may try to pull out hair in a specific way (e.g., so that the root comes out intact), or may visually examine or tactilely or orally manipulate the hair after it has been pulled (e.g., rolling the hair between the fingers, pulling the strand between the teeth, biting the hair into pieces, or swallowing the hair).
Hair pulling may also be preceded or accompanied by various emotional states; it may be triggered by feelings of anxiety or boredom, may be preceded by an increasing sense of tension (either immediately before pulling out the hair or when attempting to resist the urge to pull), or may lead to gratification, pleasure, or a sense of relief when the hair is pulled out.
Hair-pulling behavior may involve varying degrees of conscious awareness, with some individuals displaying more focused attention on the hair pulling (with preceding tension and subsequent relief), and other individuals displaying more automatic behavior (in which the hair pulling seems to occur without full awareness).
Many individuals report a mix of both behavioral styles.
Some individuals experience an “itch-like” or tingling sensation in the scalp that is alleviated by the act of hair pulling.
Pain does not usually accompany hair pulling.
Patterns of hair loss are highly variable.
Areas of complete alopecia, as well as areas of thinned hair density, are common.
When the scalp is involved, there may be a predilection for pulling out hair in the crown or parietal regions.
There may be a pattern of nearly complete baldness except for a narrow perimeter around the outer margins of the scalp, particularly at the nape of the neck (“tonsure trichotillmania”).
Eyebrows and eyelashes may be completely absent.
Hair pulling does not usually occur in the presence of other individuals, except immediate family members.
Some individuals have urges to pull hair from other individuals and may sometimes try to find opportunities to do so surreptitiously.
Some individuals may pull hairs from pets, dolls, and other fibrous materials (e.g., sweaters or carpets).
Some individuals may deny their hair pulling to others.
The majority of individuals with trichotillmania also have one or more other body-focused repetitive behaviors, including skin picking, nail biting, and lip chewing.
Differential Diagnosis
Normative hair removal/manipulation. Trichotillmania should not be diagnosed when hair removal is performed solely for cosmetic reasons (i.e., to improve physical appearance).
Many individuals twist and play with their hair, but this behavior does not usually qualify for a diagnosis of trichotillmania.
Some individuals may bite rather than pull hair; again, this does not qualify for a diagnosis of trichotillmania.
Other obsessive-compulsive and related disorders. Individuals with OCD and symmetry concerns may pull out hairs as part of their symmetry rituals, and individuals with body dysmorphic disorder may remove body hair that they perceive as ugly, asymmetrical, or abnormal; in such cases a diagnosis of trichotillmania is not given.
Stereotypic movement disorder. Stereotypic movement disorder can sometimes involve hair-pulling behavior.
For example, a child with intellectual developmental disorder (intellectual disability) or autism spectrum disorder may engage in stereotypic head banging, hand or arm biting, and hair pulling when frustrated or angry, and sometimes when excited.
This behavior, if impairing, would be diagnosed as stereotypic movement disorder (co-occurring with intellectual developmental disorder or autism spectrum disorder) rather than trichotillmania.
Psychotic disorder. Individuals with a psychotic disorder may remove hair in response to a delusion or hallucination.
Trichotillmania is not diagnosed in such cases.
Another medical condition. Trichotillmania is not diagnosed if the hair pulling or hair loss is attributed to another medical condition (e.g., inflammation of the skin or other dermatological conditions).
Other causes of noncicatricial (nonscarring) alopecia (e.g., alopecia areata, androgenic alopecia, telogen effluvium) or cicatricial (scarring) (e.g., chronic discoid lupus erythematosus, lichen planopilaris, central centrifugal cicatricial alopecia, pseudopelade, folliculitis decalvans, dissecting folliculitis, acne keloidalis nuchae) should be considered in individuals with hair loss who deny hair pulling.
Skin biopsy or dermoscopy can be used to differentiate individuals with trichotillmania from those with dermatological disorders.
Substance-related disorders. Hair-pulling symptoms may be exacerbated by certain substances-for example, stimulants-but it is less likely that substances are the primary cause of persistent hair pulling.
Comorbidity
Trichotillmania is often accompanied by other mental disorders, most commonly major depressive disorder and excoriation (skin-picking) disorder.
Repetitive body-focused symptoms other than hair pulling or skin picking (e.g., nail biting) occur in the majority of individuals with trichotillmania and may deserve an additional diagnosis or other specified obsessive-compulsive and related disorder (i.e., other body-focused repetitive behavior disorder).
#taken straight from the DSM-5-TR#trichotillomania#hair-pulling disorder#dsm 5#psychology#obsessive-compulsive spectrum#kill me#this took way too long#I honestly just want to talk about psychology#obsessive compulsive spectrum#obsessive compulsive behavior#can you tell that my special interest is psychology?#mental illness#mental health#mentalheathawareness#mental heath support#long post#long ramble#special interest
0 notes
Text
youtube
I don't have a lot to say here except question. everything. even and especially yr government and medical system. harm is systemic.
#DSM-5-TR#Youtube#harmreductioheroes#harmreduction#HRH-Advocate#HRH-KnowYrRights#HRH-ResearchChallenge
0 notes
Text
DSM-5-TR Panel Members Received $14M in Undisclosed Industry Funding
Kelli Whitlock Burton, January 10, 2024
About 60% of US physicians who served as panel and task force members for the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) received more than $14 million in publicly undisclosed industry funding, a new study shows.
Most payments were for food and beverages, travel, and consulting fees. But more than one third of contributors received compensation for services other than consulting, such as serving on a pharmaceutical company's speakers bureau, which medical ethicists say is particularly problematic.
Often referred to as the bible of psychiatric disorders, the DSM-5-TR was released in 2022 by the American Psychiatric Association (APA) and includes changes that were made online since the DSM-5 was first published in 2013.
…However, having industry funding did not preclude contributors' participation, and investigators note that none of the disclosures were published in the manual or shared publicly.
0 notes
Text
I wonder how long it’ll take for extremely toxic stan behaviour to be classified as an actual mental illness
0 notes