#urinary incontinence
Text
shout out to people with bladder and bowel issues this disability pride month.
its so hard to talk about our symptoms without being seen as gross or unsanitary.
you arent gross. you arent dirty. you arent unsanitary. i love you all <3
#disability pride#disability pride month#disabled pride#disabled pride month#neurogenic bladder#urinary incontinence#urinary retention#neurogenic bowel#bowel incontinence#theres so many more i could tag
4K notes
·
View notes
Text
You say you’re supportive and understand of disabled people but are you supportive of people who have urinary or fecal incontinence? Are you supportive of people’s disabilities when it has to deal with something like a biohazard or something unsanitary?
#as someone who has dealt with temporary incontinence it just made me think again bc it just happened again bc of my bladder being inflamed#if my memory serves me correct me— it’s a biohazard if it contains blood#personal#chronic illness#disabled#cripple punk#incontinence#urinary incontinence#fecal incontinence
85 notes
·
View notes
Text
I dunno as someone who actually has problems with my urinary system and wants to read fics where characters experience similar experiences to myself, I hate how the only genres of "character has incontinence/urinary dysfunction" are either kink related, age-regression related, or both.
Like how about people can have urinary incontinence/dysfunction without it being fetishized or infantilized?
#sigh#personal#ableism#medical issues#fandom negative#fetishization#infantilization#urinary incontinence#urinary dysfunction
38 notes
·
View notes
Text
Well, hello hello! We're here, Tumblr! Get the World's Best Adult Incontinence Products with us. We are InControl Diapers - Restoring Freedom and Joy in your life!
#incontinence#health#self help#community#urinary incontinence#urinaryhealth#funny#diapered247#ab/dl diaper#diaper pee#bed wetter#bladder control#bladder holding#urge incontinence#mens health#movember
28 notes
·
View notes
Text
Coping with and Managing Incontinence

Dealing with Incontinence can be an emotional, physical and financial struggle. I wanted to share some things I have learned over the years with others to support my community, spread awareness and educate.
1 in 15 Americans deals with a form of incontinence. Alot of negative feelings can come with the realization or diagnosis of incontinence. First, and most importantly you need to know you are not alone and you have done nothing wrong. Incontinence is sometimes treatable and if not, it is definitely manageable!!!
Most people get toilet trained at an early age and never think of potentially having to deal with issues later like dribbling when they cough or sneeze, getting a sudden urge and not making it, wetting the bed or even not getting the signal that you need to go at all. Often, this comes with embaressment due to the stigma and lack of awareness for these types of problems. Accepting that this is a problem and that it is not your fault is the first step, we need to accept this so we can seek help from our providers, make a plan or find management that works!
Talking to your Doctor
Talking to your health care professional about your problem is very important, but in fact surveys show that only 20% of people living with a form of incontinence report it to a doctor, and most reported cases of incontinence are people who have dealt with it for 7 years or more before mentioning it. Doctors see tons of patients and others with this condition and will not judge you or be cruel. When discussing this with your doctor be prepared to answer some potentially uncomfortable questions, bring a notebook with any questions you may have, keep a bladder diary leading up to the appointment.
Privacy and Independence
Loss of privacy and Independence is one of the hardest things to accept. Going to the bathroom is usally a very private thing. Depending on the type of incontinence and the condition of the person dealing with it sometimes help is neccessary which can feel dehumanizing, can cause a loss of dignity and a feeling of dependence. This is okay and is honestly normal. Waking up with a partner in wet sheets, needing help wiping or changing protection, needing reminders to go or assistance getting there or even needing to use a bedside cammode all means compromising privacy, make sure you communicate with your loved ones or caregivers about how this makes you feel and how you can become more comfortable goes a long way. Some boundaries I asserted to maintain my privacy are:
-When using a bedside cammode I have a lap blanket so I am not exposed, it gets cleaned often so as to keep the environment more normal and sanitary feeling and I can sit there by myself until I need help wiping or transferring back to bed.
-When I need assistance changing my protection not making eye contact during it helped, we make random conversation during it so it is not awkward and if I feel I can help or do it on my own I do.
-Checks or questions about the current condition of my protection are to always happen in private, never in front of company and never assume another person knows. Even if you know another person knows do not ask me in front of others.
Equipment/ Protection
There are alot of things available for now for people with incontinence and what works for you depends totally on your type of incontinence as well as your physical limitations.
Bedside Cammodes- This can be great for someone with urge or functional incontinence. Having one right by the bed or your favorite chair means you dont need as much time to get to the bathroom, it is also easier to get to than to get all the way to a bathroom for someone with physical limitations.
Bed Pans/Bed urinals- This can be handy for someone who knows when they need to go but cannot make it to the bathroom due to injury or being bedridden.
Pads, Underwear, Briefs- Absorbent protection comes in all types of absorbency levels ranging from pads for dribbles to underwear for the occasional light or mild accident to super absorbent underwear or briefs for moderate to severe accidents. Plastic backed briefs or plastic pants/covers can help minimize odor from bowel incontinence as well.
Bed pads/waterproof covers- This can help save furniture and matresses from unavoidable leaks, matress covers also help prevent the smell of urine that builds overtime with long term bedwetting.
Catheters- this is something that should be prescribed by a medical professional if needed, there are various types and sizes and collection systems.
I honestly use most of these things pending my situation. I have no bladder control as I do not get ques to go and I have loss of some bowel control. I use underwear at home on good days when I can manage my protection on my own but I use briefs overnight and for long car rides or outtings. I use a bedside cammode when needed to move my bowels as I struggle to get to the toilet on time due to my own physical limitations. I cath before bed or intercourse to minimize leaking and when I have skin breakdown, bed sores or changes are difficult due to my joint subluxations my dr will put in an indwelling foley catheter.
What you use needs to be comfortable and right for you but it can help you gain back some independence and help minimize the exposure of your condition to people you do not want knowing, if you have an accident without protection everyone sees it, if you have one with protection you just gotta clean up. Honestly finding protection that worked for me gave me my life back.
Traveling With Incontinence
This can be difficult for some people and honestly can deter many people from traveling. Here are some tips ive learned in my experience:
1. Carry a go bag. I keep a bag with extra protection, a spare change of clothes and wipes in my vehichle at all times. So if I am ever blindsided I am prepared.
2. On car rides plan on extra time to stop if you need it.
3. In a car, if comfortable, on long drives (cross country trips a couple of times) I have used external catheters or foleys with a perscription when changes would be difficult.
4. When traveling by plane, protective garments can take up quite a bit of space in luggage and add to the weight. I order supplies to or send some to my destination so it will be there when I arrive and I can have all of my suitcase room.
5. Ask a flight attendant for a seat close to the bathroom, if you ask before boarding and explain you have a medical condition most of the time they are more than willing to accamodate.
6. Handicapped bathrooms and family facilities provide more space and privacy and are usually kept cleaner, this usually makes them safer for catheterization and garment changes.
Hospital Admittance with Incontinence
1. While your incontinence may be documented somewhere on your chart, if it is not what you are currently being seen for more often than not the staff and healthcare providers will have no idea. You should share this information with a nurse or Dr. when you get admitted so they do not find out later when you need assistance and they did not know.
2. If you need help managing your incontinence while inpatient it is your responsibility to let them know that and assert your needs.
3. Bring your own protection. While hospitals do carry briefs and pads what they have may not be what works for you.
4. The curtain around your bed is for you for your privacy, do not be afraid to use it or ask someone to draw it for you during changes (wether independent or assisted) or use of bedside cammodes or urinals.
5. If an accident occurs let staff know strait away, staying in soiled sheets or clothes can cause damge to your skin and infections.
6. If your needs are not being met or you feel you cannot bring them up on your own, ask for a patient advocate.
Skincare
Alot of skin problems can come with Incontinence ranging from chaffing, rashes and infections to bedsores.
1. Change as soon as you can after an accident.
2. Using absorbent protection can help pull the moisture away from your skin.
3. Make sure your skin is completely dry before putting on fresh protection. Pat dry instead of rubbing.
4. Be careful of what you put on your skin. Ointments and barrier creams can be helpful but some things advertised for cleaning those areas can actually be harmful and cause further skin breakdown, if you are unsure, as your doctor or urologist.
I hope this post was helpful. I am kind of wanting to do a series of posts with tips and education on things I have experienced to share with others in support and awareness. Please do not be afraid to reblogg this with some of your own added tips!!!!
#mine#incontinence#disabled#disability#disability awareness#incontinence awareness#itsokaytowear#bladdersmatter#incontinent#urinary incontinence#overactive bladder#bladder control#bladder incontinence#bowel incontinence
183 notes
·
View notes
Text
if youre normal about people with urinary incontinence but not normal about people with bowel incontinence: "DNI" isnt enough i am killing you through psychic attacks
#actually incontinent#actuallyincontinent#urinary incontinence#bowel incontinence#bowel issues#bladder issues#disability#disabled#disabilties#actually disabled
10 notes
·
View notes
Note
hey
i was wondering if you (or any of your followers) have any advice for someone dealing with moderate/severe urinary incontinence for the first time? shit sucks :(
i’m actually navigating what i guess could best be categorized as mild urinary incontinence rn? schrödinger’s incontinence lmao bc mine is due to my involuntary movements making the like, muscle contractions of urination sometimes, it’s a whole thing. anyway what i & my roommates have been discussing is:
- reusable/washable incontinence furniture pad for where i sit on the couch
- waterproof mattress cover
- absorbent underwear (“Thinx for all leaks” is one brand i know of but i think there are a few), although idk how that volume compares to your specific needs - those advertise as up to 100mL
& then ik a lot of folks keep a change of clothes in their car, bag, etc when going out.
from a psychoemotional end i highly highly recommend the article “‘Like, pissing yourself is not a particularly attractive quality, let’s be honest’: Learning to contain through youth, adulthood, disability and sexuality” by Kirsty Liddiard and Jenny Slater — it’s an absolutely life-changing analysis of how the forces demanding we normatively, independently “contain” & manage our bodily fluids are the same forms of biopower that operate to contain people through incarceration and other forms of oppression
i hope some of that is helpful! other folks feel free to add on
44 notes
·
View notes
Note
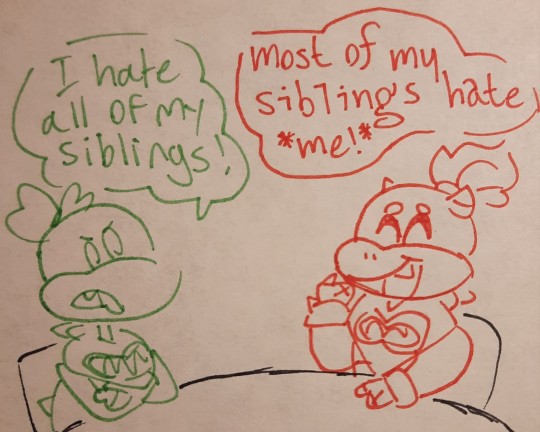
odd question ig but how do thr koopalings react to Ludwig having a accident ?
Odd question indeed... But I can work with it-
Roy: Immediately stops everything he's doing and helps Ludwig. Cleans up the mess, gets Ludwig some different clothes, comforts him, cuddles him, assures him it's not his fault--The whole nine yards. Basically becomes Ludwig's emotional support sibling
Iggy: Isn't too good at comforting people, but will still make sure that Ludwig is okay and attempt to cheer him up
Wendy: Also sucks at comforting people, but still tries to help Ludwig. Will give "death glares" to anyone who even looks in their direction
Morton: Hugs Ludwig and snuggles him until he calms down. Will try to help clean and whatnot--Whatever it takes to make Ludwig not sad
Lemmy: Will most likely give Ludwig some sort of peptalk about how accidents happen, and it's okay. (Lemmy also has accidents a lot, so he just does the same things that Ludwig had done for him in the past)
Jr: Comforts Ludwig as best he can, then will take him to do something fun as a distraction, like watch cartoons or play a game
Most of the Koopalings really like Ludwig and obviously don't want him to be sad. Also, they've all dealt with his bladder issues for like six years--They all know what to do about it by now. Hm... Am I forgetting someone? Oh yeah-
Larry: Runs around, yelling, trying to alert everyone that Ludwig peed himself again and will attempt to get other people to make fun of him. Larry will probably get thrown out of a window after a few seconds of that...
12 notes
·
View notes
Text

Incontinence problems
#disability#disabled#disabilties#incontinence#urinary incontinence#transmasc#furry fandom#furry art#fursona#skunk#comic#relatable
4 notes
·
View notes
Text
I've been afraid to mention it for years but you know what I hc that Sebastian Debeste has urinary incontinence. I think this because I can and it's normal, and also because it's as a result of trauma around fire and smoke, and the old wives tale that if you play in a fire you'll wet the bed.
2 notes
·
View notes
Text
Treatment For Urinary incontinence
Urinary incontinence, the involuntary leakage of urine, can significantly impact a person's quality of life. Treatment options depend on the type and severity of incontinence, as well as underlying causes. Common treatments include:
Lifestyle Modifications: Behavioral changes such as bladder training, scheduled toileting, and fluid management can help improve symptoms.
Pelvic Floor Exercises (Kegels): Strengthening the pelvic floor muscles can support the bladder and improve urinary control.
Medications: Certain medications, such as anticholinergics or beta-3 agonists, can help reduce bladder spasms and increase bladder capacity.
Medical Devices: Devices like pessaries or urethral inserts can help support the bladder and reduce leakage.
Electrical Stimulation: Techniques like sacral neuromodulation or percutaneous tibial nerve stimulation (PTNS) use electrical impulses to improve bladder control.
Interventional Therapies: Botox injections into the bladder or bulking agents around the urethra can help reduce incontinence episodes.
Surgery: In severe cases or when other treatments fail, surgical options like sling procedures or artificial urinary sphincter implantation may be considered.
It's crucial to consult a healthcare professional to determine the most suitable treatment plan based on individual needs and health status.
2 notes
·
View notes
Text

CHUVA DOURADA
Mijo
Xixi
Urina
Piss
4 notes
·
View notes
Text
Does anyone else with UI on here notice it gets worse when it starts to get colder out? Seems to happen every fall/winter. My best guess is it’s because I’m not sweating as much?
8 notes
·
View notes
Text
Don't Let Overactive Bladder Control Your Life
Overactive bladder techniques like sacral neuromodulation or percutaneous tibial nerve stimulation can help le urge to urinate, which can be accompanied by involuntary leakage of urine. OAB can significantly impact a person's quality of life, but treatment options are available. This article will discuss the symptoms, causes, and treatment options for OAB.
Symptoms of Overactive Bladder
The main symptom of OAB is a sudden urge to urinate that is difficult to control. This can occur at any time, including during the night, and can happen even if the bladder is not full. Other symptoms of OAB may include:
Frequent urination (more than eight times a day)
Involuntary leakage of urine (urge incontinence)
The need to urinate immediately
Feelings of urgency or pressure in the lower abdomen
Waking up more than once during the night to urinate (nocturia)
Causes of Overactive Bladder
There are several factors that can contribute to the development of OAB. These may include:
Aging: As we age, the muscles in the bladder can weaken, making it harder to control urination.
Nerve damage: Nerve damage from conditions like multiple sclerosis or diabetes can interfere with the signals between the brain and the bladder, leading to OAB.
Urinary tract infections: Infections in the urinary tract can cause irritation and inflammation, leading to OAB symptoms.
Bladder abnormalities: Conditions like bladder stones or tumors can cause irritation and lead to OAB symptoms.
Treatment Options for Overactive Bladder
There are several treatment options available for OAB. These may include:
Lifestyle changes: Simple changes to your diet and fluid intake can help to reduce the symptoms of OAB.
This can include limiting caffeine and alcohol, drinking plenty of water, and avoiding foods that irritate the bladder, such as spicy food.
Pelvic floor exercises: Strengthening the pelvic floor muscles can help to improve bladder control and reduce OAB symptoms.
Medications: There are several medications available that can help to reduce OAB symptoms. These may include anticholinergic medications or beta-3 agonists.
Nerve stimulation: Techniques like sacral neuromodulation or percutaneous tibial nerve stimulation can help improve bladder control and reduce OAB symptoms.
Surgery: In some cases, surgery may be necessary to treat OAB. This may include procedures like bladder augmentation or urinary diversion.
Conclusion
If you're experiencing signs and symptoms of OAB, it's miles crucial to talk together along with your healthcare company to talk about your remedy options.
Symptoms may include sudden urges to urinate, frequent urination, and involuntary leakage of urine. There are several factors that can contribute to the development of OAB, including aging, nerve damage, and bladder abnormalities. Treatment options may include lifestyle changes, pelvic floor exercises, medications, nerve stimulation, and surgery. If you're experiencing signs and symptoms of OAB, it's miles crucial to talk together along with your healthcare company to talk about your remedy options.
For more information Visit: www.drmayurdalvi.com
#overactive bladder#bladder control#bladder symptoms#urinary incontinence#urinary health#pelvic floor health#bladder problems#bladder health#nerve injury#urinary tract infection#medications#lifestyle changes#nerve stimulation#surgery#healthcare#wellness#treatment options
2 notes
·
View notes
Text
Is Apoquel to blame?
Hubbins took Mandana for a walk last night and because of the ragweed pollen she woke up with some skin issues. I gave her a dose of Apoquel and about an hour or two later she had urinary incontinence (while awake, which was a first).
This is the same thing that happened last time. I gave her Apoquel and then she had a big incontinence accident an hour or two later. Last time she was swollen and drinking a lot of water so the vet suggested thats what caused it but this time the swelling is gone and she’s drinking less water than usual.
I’m not sure about her other symptoms but I’m starting to wonder if the Apoquel and incontinence are connected.
She’s taken Apoquel without incontinence so that’s kind of confusing. She’s also on antibiotics and has never tested positive for a UTI so I don’t think that’s the issue.
#belgian malinois#2 years#service dog in training#sick dog#mystery illness#urinary incontinence#vet#veterinarian#vetblr
7 notes
·
View notes
Text
For those who don't know, I have a younger sister named Maggie, better known as Maggie4ThWin, who also likes drawing the Koopalings, and we decided to do a "cross-over thing," where each of our Koopalings meet, so, here's that...





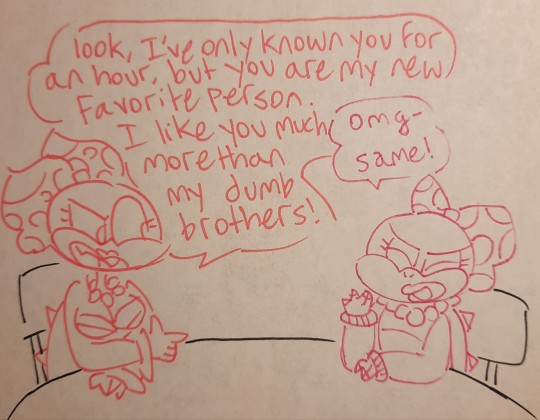
#koopalings#ludwig koopa#roy koopa#lemmy koopa#iggy koopa#morton koopa jr#larry koopa#wendy koopa#bowser jr#urinary incontinence#tiny bladder struggles#Maggie4ThWin
25 notes
·
View notes