#how many more obscure parts of my bodily experience are going to turn out to just eds
Text
was anyone going to tell me your eyes aren’t supposed to burn when you cry and can be a sign of eds or was i supposed to see a tiktok of it myself
#are you kidding me??#first it was screaming hiccups now its eyes burning??#i asked my sister who we think has it and hers burn#then we asked mum who definitely doesnt have it and hers dont#like holy shit#thats always in book descriptions of characters trying not to cry#how they feel a burn behind their eyes#my eyes definitely burn#also youre not supposed to be puffy the day after but i dont cry often enough to know if i get puffy#i know i feel puffy#how many more obscure parts of my bodily experience are going to turn out to just eds#also mcas and im still not sure if i have that#coming out of my cage and ive been doing just fine.txt#spoonie#pots#eds#ehlers danlos syndrome#mcas#mast cell activation syndrome#mast cell activation disorder#dysautonomia#dysautomnia
5 notes
·
View notes
Text
Survey #306
i’m v talkative today so pardon my jabbering below.
What is the strangest type of candy you have eaten? I think I've had one of those lollipops with a bug in it before as a kid? I don't remember.
What would be your most ideal profession? A freelance photographer. But I'm honestly starting to lose hope.
Have you tried those coloring books for adults? Yeah; it's funny you mention 'em, 'cuz a family friend got me one for my birthday earlier this month.
What is a topic you definitely don't want to talk about with anyone? I don't like talking about my sexual history, doesn't matter who you are. It's just uncomfortable.
What was your first gaming console? An Atari.
Is there something you're eagerly waiting for? What is it? *SLAMS FISTS ON TABLE* MAY NEEDS TO FUCKIN' HURRY. My tattoo appointment is set then. :''')
Do you/have you ever belonged to an organization? If so, which one? I was a Girl Scout when I was young.
What is something you're very passionate about? Nature conservation, gay rights (equal rights in general, really), the pro-choice movement, and then there are less "important" things like certain hobbies interests and such. I'm sure there are more big ones that are just slipping my mind right now, considering I feel passionately for a shitload of stuff.
What are you studying or what was the last thing you studied? I majored in Art & Design with a focus on Photography in college. But guess who dropped out.
What was the last present you gave someone? I don't know... I mention enough that I don't have a source of income where I can really buy anything. I think the last thing I did was a Christmas gift for Mom a year or two back of a drawing I did of our late dog Cali, whom she absolutely adored.
Do you enjoy plays? If so, what was the latest one you saw? Not really, no.
What was the last thing you achieved? PHP has helped me focus on little victories, so prepare for an underwhelming answer haha, but it's something. I Facebook messaged an old friend I really wanted to catch up with, and everyone in group cheered for me. :') It was really heartwarming. What a shocker that this program is really helping me once again.
What is something you would like to achieve at some point in your life? I would love love love to take at least one "famous" or award-winning photograph. It'd be such amazing validation that I'm talented at something I love so much.
What is one philosophy you have regarding life/living/purpose? That's... difficult to answer seeing as I'm trying desperately to find my purpose. I do try to live by this old quote a therapist said once: "Deal with life, or life deals with you." I think it holds an incredible amount of depth and meaning in such a short phrase.
How would you design the inside of your own home? I don't know the details of it, really, besides that shit is gonna look like a Halloween house year-round. I can imagine wanting black furniture, too, and having loooots of decor expressive of what I love and find comfort in. Gotta make a house feel like a home just for me.
What is a band you remember liking from your childhood? Backstreet Boys, duh.
Do you ever get mad at people for not having the same opinion as you (i.e. abortion being wrong/right, meat-eating being wrong/right)? Two things: it depends on the topic, and "get mad" is the wrong term for what I feel. It's more disgust; ex., I'm repulsed by anti-gay rights people and want absolutely nothing to do with 'em, but I'm not like, mad at them.
Do you edit any of your pictures? In what ways? Oh yeah, and it definitely depends on the raw photograph. I edit depending on the mood it emanates; like if you've seen my roadkill photography versus nature shots, there is an extremely distinct difference in editing style and vibe. I'd say in general though, I tend to like to brighten my photographs and add more vibrance.
If you like to take pictures, what is your motivation? God, I could write an essay on this. I just love and am so thankful for the fact we can literally freeze time forever with the click of a button and look back on fantastic sights, beautiful moments, memories... It's just magical to me, and I adore contributing to that art.
Would you ever consider living anywhere cold? Well yeah, that's my preference, actually.
What is your absolute favorite food? The spicy shrimp fritas from Olive Garden, jfc.
Would you ever wear snake-skin pants, or other animal clothing? Fuck to the absolute hell no.
What foreign country would you like to go to for a shopping spree? Idk, considering I'm not well-versed in the artistic creations of other countries. Perhaps India? Japan? I dunno.
If you met your favorite musician, what would you ask him/her? I'm asking for his fucking autograph and a hug while I smile my face in two AND cry lmao.
What do you spend most of your day thinking about? I ain't gonna bullshit nobody, my PTSD. In some way or another, he's lurking in that head of mine through memories, flashbacks, wonders of what could have gone differently... but thank God it's no longer in the forefront of my mind after my first PHP. I've come very, very far, but especially when trying to blank out my mind to fall asleep, parts of PTSD strangle my brain until I'm just finally out. I really hope that changes someday.
Where is a busy place you would like to go to? Yikes, nowhere, really. I like to avoid busy locations.
Do you think video games cause people to become violent? Absolutely not. You are responsible for the decisions you make; music, games, movies, etc. have no deciding voice in stupid shit you do, and it's bullshit that people blame art and entertainment for such things.
Vocabulary: What was the last word you learned? I'm unsure.
Have you or could you build your own site? Absolutely not from scratch. The closest I've gotten to that is my photography website, but it was through the assistance of Wix.
What's the best thing you can cook yourself? Scrambled eggs, haha. I do make some bomb eggs at least.
Are there a lot of graffiti around your neighborhood? No.
Do you have a hobby that forces you out of the house? If so, what is it? Nature photography.
Would you stop eating meat, if you had to raise and slaughter it yourself? Absolutely. God, I want to go vegetarian again...
Besides English, what other languages can you speak? I can speak a very little bit of German. Took four semesters of it in high school and became very good at it, but lack of practice has pretty much ruined that.
Besides English, what other languages can you read? I can read German well; as in, I can pronounce most words I see, but that doesn't mean I understand what is written.
Do you think you could make it as a chef? Gordon Ramsey would deadass kick me off his show on day one, lmao.
What's your favorite kind of tea? It marvels me JUST how many tea and coffee questions are in surveys. Anyway, I don't like tea. I am an embarrassment to NC culture.
What thing/person/happening has made you the happiest you've been? lask;dfjal;wekrjwe
What's the most freeing thing you've ever done? Stealing my happiness back from someone who had no right to hold it all in its entirety. That shit's mine.
Do you think today's kids are really impatient? Most, probably, but in some ways I can understand it - at least, in the sense that with the assistance of modern technology and advancements in satiating our wants so quickly, kids just expect it. I definitely believe that patience is something to try to be deeply instilled in everyone, though. I don't have an ounce of it (in most situations) and wish I did.
Have you ever tasted birch sap? No.
How about the young buds/shoots of spruce trees? No.
Which edible flowers have you tasted? One of my favorite Southern experiences is finding a bunch of honeysuckles and tasting the honey (is it technically even honey??). Tastes amazing. My family's hairdresser lives down a beautiful path that sprouts a massive amount of them, and as kids, my sisters and her two boys would go tasting them while our parents talked for so long, or if we were waiting our turn. Good memories.
What has been your worst restaurant experience? I'm not sure, really.
What's the most immature, adolescent thing that still makes you laugh? "Inappropriate humor type jokes." <<<< They can get me sometimes, too.
Have you ever had a life-threatening condition? If so, what was it? No, thankfully.
Have you ever had a custom print done on a shirt? If so, what was it? I don't believe so, no. Besides making a tye-dye one in HS with our school colors. Wasn't my idea and never wore it, haha.
Do you ever read other people's survey answers? It depends on the person. If it's a friend, absolutely, because I love learning usually obscure things about them I wouldn't have known otherwise. If it's a user I don't know from wherever I got the survey, sometimes, depending on how short the answer is and my eyes kinda just scroll over it.
Do you like daytime or night time better? Why? Daytime, especially mornings. I'm generally happier when there's light around.
What's your highest level of education so far? Some college.
Describe your ordinary day: My average day is embarrassingly uneventful. It's sitting on the laptop doing shit on various sites, none of which are actually important, and playing WoW, which is also without true substance, save for social interactions with my friends on there. I spray Venus' terrarium everyday multiple times as well to keep the humidity up, and obviously eat and handle that kinda bodily needs stuff.
Would you ever have a UV tattoo? Ugh, that'd be so dope. I've seen some awesome ones, but idk if I'd get one, considering when am I actually going to be under UV light?? Like I wanna be able to see my tat.
What is the brand and color name of your favorite lipstick? I have one black lipstick, but it comes right off so I don't even like it. I only ever put it on to take pictures.
What do you like on your tortilla? Just ham and cheese.
How about inside your pita bread? I've never had pita bread, actually.
What do you like in your burger? It depends on where I'm getting the burger. My basic is cheese, ketchup, mustard, a bit of mayo, pickles, and a light sprinkle of diced onion, but sometimes I add bacon and take away the onions.
How about on your pizza? I have three I tend to pick from: pepperoni, jalapeno, or meat lovers.
Do you work better alone or in a group? Alone, definitely.
Which body part would you not mind losing? I'ma be extremely honest, with just how horribly weak my legs are, I could live without them, I guess. Not saying I want to by any means, it's just exhausting using them. Ideally, I'd take away something minor, like a finger or something.
What common saying people use is absolute BS to you? “'Everything happens for a reason.'” <<<< Fuckin' colossal "same." I won't rag on people who believe it, especially if it gives you courage to keep moving forward, but I don't believe it in the slightest. If it were so, I'd like to talk to whoever is in control of those "reasons," please.
What is the most interesting thing you’ve read or seen this week? I had no idea elephants were pregnant for two years, like holy shit, can you imagine. It was in an article I saw on Facebook about a mother and daughter elephant who are both expecting and doing well. Wonderful to hear.
What’s the most useless talent you have? Ha, I'm a master in the arts of catastrophizing and jumping to conclusions involving people hating me in one way or another.
What’s something everyone looks stupid doing? I'm one of those people who hate dabbing done by anybody, like you look like you're just smelling your armpit.
Which kids’ movie scarred you for life? I wouldn't say "scarred me for life" by any means, but when I was little, I was terrified of the Wicked Witch from The Wizard of Oz and even had nightmares about her. It sucked because my little sister was obsessed with that movie, haha.
In one sentence, how would you sum up the Internet? A source of incredible knowledge but also hate and misinformation.
What would be the most ridiculous thing for the government to make illegal? I literally dread the idea of Roe vs. Wade being reversed. Banning abortion would kill so many people with operational uteruses and cause absolute pandemonium.
How many friends do you have on social media and how many of them do you know for real? On Facebook, I have 124 friends, and I'd say I know most of them "in real life." However, having been on the Internet since I was so young and befriending loads of incredible people, a good chunk are "online friends." Hell, I'm more interested in their lives than most "real" ones. Long-distance friendships are so valid.
What fact amazes you every time you think of it? Lots of things, generally regarding the stupidity of humanity.
What’s the most spontaneous thing you’ve ever done? Probably going to the beach w/ my old friend Colleen. We had zero plans of doing it, but she just called me one morning and asked if I wanted to go, and off we went. It was a fun day.
What has taken up too much of your life? I'ma be real, WoW. I don't think I'm addicted to it like I once was seeing as I go through spans where I barely want to play it at all and don't, so I truly am capable of not playing it, but rather it's just the most entertaining way to kill time in my life. I just don't like how much time I've invested into a game over six or seven years regardless.
Where do you not mind waiting? Uh, nowhere lmao.
Is there an app you hate to use, but still use every day? No; why would I use it if that was the case?
Who is the funniest person you know? My friend Girt is fucking hysterical.
What three words describe you best? Complex, passionate, and creative.
What makes you think you’re smart? Lol who says I think I'm smart?
Who inspires you? Korean Jesus. Okay on a serious note, not just him, of course, but he's #1 in an entire universe of ways.
Do you aspire to be like somebody else? If so, who? No; I want to be my own authentic self.
How did you meet your best friend? YouTube, back when it had more social aspects.
Which one of your accomplishments are you the most proud of? I want to say my recovery, but like... I wonder a lot if it's "enough" to be proud of with how scarred I still am? I still struggle with a lot and feel like I could be so much better by now if I tried harder. If I'm completely honest with myself, I think it's finishing high school in the top percentile of my graduating class. There was a ceremony for the handful of us and all, and I cherish my plaque probably too much. Reminds me of a time when I knew what the fuck I was doing.
What's the strangest thing you ever did as a child? Thinking I had "animal powers" where I could invoke the traits of certain animals at will, like what the actual fuck, Brittany.
What did your mother teach you? Christ, a lot. Dad didn't do a lot of the raising, honestly, so much of my core values and whatnot were instilled by my mother. She taught me to care for and be nice to others, respect myself, try my best in everything, and most importantly that she is always there for me and my sisters no matter what and can tell her absolutely anything. She was very serious about us going to college and saving sex for marriage when we were younger, but she diverged from those ideas as absolutely necessary with experience. I'm extremely lucky with who I call my mom, overall.
What did your father teach you? Eek... Read above. Not a lot as a kid (save for riding a bike and playing softball); most he's taught me has come following reuniting with him after my parents' divorce. I remember we went to lunch once and talked about my breakup, and he talked to me about sometimes, you just have to let people go in order to be happy, like with him and Mom. He's very serious now about ensuring us girls know that he is always there for us and will help us in any way he's capable.
What makes you feel powerful? "Powerful" isn't something I really feel, if I'm being real.
What are you ready to let go? It would be inexplicably fantastic if I could let every speck of Jason go in both my head and heart.
What is your most bizarre deal-breaker? I don't really find any of my expectations and limits as "bizarre?" They're all valid to me. Well wait, idk if you'd find it strange that I absofuckinglutely would not date someone who hunts, but it's not to me. That's a difference in a very serious value to me.
Would you rather be hated or forgotten? Hated. God, I don't want to leave this earth having given just nothing. I can live with some people hating me for whatever reason.
What’s the biggest personal change you’ve made? Accepting my bisexuality, probably. That's something that I consider pretty big for two reasons: 1.) I could end up with a woman forever, and especially 2.) I was originally homophobic. I still have difficulty in fathoming how I ever was.
What are some of your short-term goals? PHP is finally starting to make me build these again. I want to get better at selfcare, draw, write, and read more, I want to drink a lot more water, exercise way more... Lots of things, really.
What is the weirdest thing about you? Uh. I dunno. Probably that I RP meerkats, which is a very obscure RP niche for sure.
2 notes
·
View notes
Text
The Art Of Trying To ‘Pass’ As Female (My MtF~HRT Research)
Just as Krista described her need to change her face in order ‘just to leave the house,’ most of the 28 patients with whom I conducted interviews and observations, and the many others with whom I shared casual conversations, explained their desire for facial transformation in order to carry out everyday activities. As much as patients might want to be beautiful women after surgery, their primary desire was to walk through the world being recognized as women—which, in a sense, meant not being recognized at all. But just as physician discourse often conflated or collapsed the biological category of the female with the aesthetic category of the beautiful when describing the aims of feminization, so too did patients draw on both of these notions when communicating what their goal of being a woman actually means.
Woman is difficult to define as a surgical category precisely because it is difficult to define as a social one. Not surprisingly, patients had different ideas (and ideals) in mind when they imagined the kinds of transformations that would allow them to be the kind of women they wanted to be. When I asked Rosa if she had a particular idea of what she hoped to look like after surgery, she immediately said, “Yes,” and reached into her bag. She pulled out a stack of papers wrapped in plastic sleeves and held together by a binder ring. She shuffled through the stack, unfastened the ring, and put a page on the desk in front of me. There were three photographs that had been clipped from magazines and pasted to a sheet of white paper. As she began to talk I was not sure which one I was supposed to be looking at. “I want to look like a woman,” she began. “I want a face that a man falls in love with. Like an angel. Innocent. You are a man. You understand. Look at her [pointing to an image on the page.] What do you feel? Body is nice, but look at her face. In that picture you can’t see her breasts, but you can see her face. She’s beautiful. You feel inside something like love. I want a face that a man sees and it makes him turn red.” Rosa was not sure what her particular features would be when all was said and done. She did not expect Howard to replicate the model’s face onto hers. She did, however, expect that her face would be one that would do something for others and, in turn, do something for her. Rosa described the changes she was after in terms of how particular aspects of her face evoked gendered attributes.
When our conversation turned from the effect she desired to the precise means of achieving that effect, she gave an inventory of her face and the multiple ways that it works against her. The bone above my eyes gives me an aggressive look. I have dark, shadowed eyes. If you see that actress Hillary Swank, she has this. Something doesn’t match on her face. Nose, obviously. My nose is male. Upper lip. I can’t wear red lipstick. If I wear read lipstick it makes me look like a man in a dress. When I watch videos of myself, my expressions never look happy. I look angry.
Rosa was confident that following surgery she would ‘feel more sure of [her]self.’ It was this confidence that made women beautiful. Just something about them that had such power and sex appeal. Women, in her telling, were not aggressive or angry; their faces are built to be adorned. Though she knew that Howard could not necessarily make her beautiful, she was confident that he could make her a woman. For her, that was enough.
Gretchen had much more modest desires. Her hopes for surgery were less about eliciting a particular response, than avoiding a reaction altogether. Just…I hope that I won’t have this kind of jerk that was sitting just to my left on the plane this morning who was seemingly horrified by seeing this (gestures to her face and body). He was probably having the idea that I was fantasizing about him or something. I just hope that next time, he won’t think about it twice. ‘Yes, I’m sitting beside a girl. So what and that’s all.’ End of story.
Pamela expressed her desires this way: I'm doing it (having FFS) so I will feel that I "pass" (making air quotes). Whatever that is. And of course the operative word there is ‘feel.’ I'm tired of thinking, is that person reading me? No? Well how 'bout that person? I want to think about something else as I walk down the sidewalk.... Like, say, what a nice dress in the window. Maybe that's it. Going unnoticed is a thing that most people take for granted.
Erving Goffman (1963) called those who do not draw unwelcome attention from their bodily appearance ‘normal’s.’ Normal’s, Goffman argues, simply cannot understand how it feels to be the object of derisive looks and hostile attention from complete strangers. To be a member of a stigmatized group is to be the object of distain. When some aspect of your physical body is the source of that stigma, there are, according to Goffman, two possible responses. You can come to terms with the fact of your stigma and attempt to ‘normificate’ it by acting normal, as though the stigma did not exist. Or, you can normalize it by making a conscious effort to correct it. Though ‘norming’ surgeries are sometimes the objects of ethical debate, the validity of the desired outcome is hard to dispute.
In an article entitled, ‘Self-Help for the Facially Disfigured,’ Elisabeth Bednar put the matter simply. Whether we are shopping, riding the subway, or eating in a restaurant, all of which are casual day-to-day social encounters, there is the initial stare, then the look away, before a second, furtive glance inevitably puts the beheld immediately in a separate class. For those who experience this discrimination, the question of the moral justification of surgery to increase societal acceptance...
She pointed out photographs in Howard’s book in which surgery did not necessarily improve a patient’s attractiveness, but it did change her sex. When referring to before and after photographs she said, “See this is an ugly boy and this is an ugly girl, but it is a girl. Other doctors can’t do this.”
There can be no greater wish than to melt into the crowd or to walk into a room unnoticed (Bednar 1996:53). The patients and surgeons with whom I worked, referred to the fact (or fantasy) of going unnoticed as ‘passing.’ The language of passing is contentious for some transpeople because it can be read as implying a sort of deception; being taken as a member of a group to which one does not really (where really refers both to an ontological truth and to the rightful membership based on it) belong. This deception is also often marked by a supposed opportunism; passing is really only considered as such when a person passes from an undesirable group and into a desired one (Gilman 1999). It therefore frequently carries a connotation of a strategy to access particular forms of privilege. Many transpeople object to the language of ‘passing’ because, they argue, to say that one passes as a woman is to acknowledge that woman is not a category to which she rightfully belongs.
As Julia Serano insists, “I don’t pass as a woman. I am a woman. I pass as a cis-gendered woman” (by which she means a woman who has never changed her gender). These sorts of concerns about what it means both politically and ontologically to pass, were only voiced by two of the patients with whom I spoke. Despite their reservations, they, like all other patients I met, held the desire to pass as an incredibly important and explicitly stated aim. As historian of medicine Sander Gilman explains, ‘The happiness of the patient is the fantasy of a world and a life in the patient’s control rather than in the control of the observer on the street. And that is not wrong. This promise of autonomy, of being able to make choices and act upon them, does provide the ability to control the world. It can (and does) make people happy’ (1999:331-2).
Like language, social roles do not exist in isolation (Wittgenstein 1953:§243); they are by definition shared properties conveyed between people in given social group. A person’s individual conviction that she is a woman is not enough to maker her a woman in any social sense. To be a woman requires not simply the conviction that one is a woman, but the recognition of that status by others.
FFS is a surgical recognition that how one feels about and lives their sexed and gendered embodiment is not a private, psychic reality, but is the product of social life, of living with others. Passing is not a subjective act; it is a social one. Nearly all clinical literature as well as most popular literature on transsexualism suggests that transsexualism is a property (and problem) of an atomized and bounded individual. This focus on the individual and psychic nature of the bodily dissatisfaction that characterizes transsexualism is named explicitly as well as through the invocation of metaphors of isolation, internality and invisibility. While an individual body may be the site of the material intervention, the change enacted in FFS takes place irreducibly between persons. The efficacy of FFS is located not in the material result of surgery itself, but in the effect that the surgical result will produce in the perceptions of imagined.
Other writers argue that the goal of ‘passing’ not only obscures but effectively forecloses any possibility of a trans- specific radical political subjectivity (Bornstein 1994, Green 1999, Stone 1991). These writers insist that living as out trans-people is the only way to call attention to the oppressive gender system that devalues and delegitimizes trans-lives and bodies, among others. This kind of visibility can come at the great cost of personal and emotional safety, leading to a conflicting desire to be a part of the solution while maintaining ones safety and sanity (Green 1999). Perhaps nowhere is this made clearer than in the imaginary scene through which Howard explains the goal of his surgical work:
If, on a Saturday morning, someone knocks at the door and you wake up and get out of bed with messy hair, no makeup, no jewelry, and answer the door, the first words you’ll hear from the person standing there are, “Excuse me, ma’am….”
This incredibly powerful scene was a staple of Howard’s conference presentations, and was repeated in slightly altered and personalized forms by many of the patients who had selected Howard as their surgeon. Through this turning outward—and the making of femaleness at the site of the exchange with a stranger—FFS reconfigures the project of surgical sex reassignment from one rooted in the private subjectivity of the genitals, to one located in the public sociality of the face. Time after time, patients told me that their primary desire was to go through their daily lives and be left alone, without thinking about what others may see when they look at them.
Krista rode the city bus on the day before our interview. On that day, for the first time in recent memory, she did not prepare extensively before leaving the house. “I didn’t have to worry about having my bangs just right, or having just the right pair of glasses on. I just got on the bus and thought, ‘Wow, this is cool.’” Although her face was covered in bandages, sutures, and bruises, and people on that bus were undoubtedly looking at her, Krista found joy in the certainty that whatever they might have seen when they looked at her, the did not see a transwoman. The stuff of her maleness was gone. It was a novel—but so, so welcome—experience. It is important to remember that the stakes for passing are often quite high, often quite serious. The desire to pass does not only exist for the gratification of personal goals, but also achieves a mode of physical and emotional safety. It is crucial to remember that trans-people are disproportionately incarcerated, unemployed, and lost to suicide and other violence. I make this point not to hold counter discourses hostage to its message— as in an accusatory stance from which any divergence is a de facto support of transphobia or worse—but to tell the complete story of the context in which these procedures become objects of desire, and accomplish practical goals sometimes on the measure of life and death.
THE FULL FACE
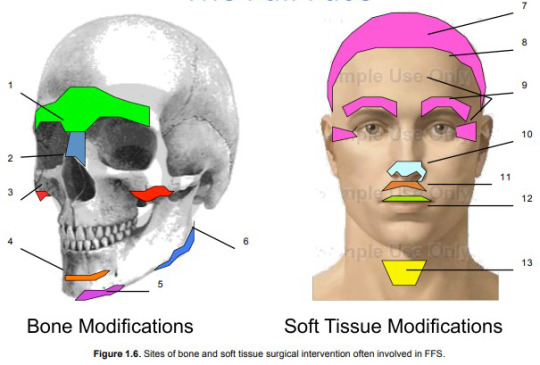
Facial Feminization Surgery includes interventions in both the bone and soft tissues of the face. In general, the procedures involved in FFS are aimed at taking away or reducing particular features of the bones and soft tissue of the face. This focus on reduction and removal is based on a fundamental assertion that males are, on the whole, larger and more robust than females.
This assertion applies both to the bony skeleton and to soft tissues such as skin and cartilage. Whereas the modification of the facial bones are guided, at least in Howard’s case, by numerical norms, most soft tissue procedures are not. (The exceptions are the height of the upper lip and of the forehead; these assessments are guided by numbers and measurement). Instead, soft tissue procedures are often oriented toward and aesthetic ideal of feminine attractiveness.
Below are brief descriptions of the surgical procedures organized under the sign of Facial Feminization. Not every patient undergoes all of the procedures described here, though some certainly do. In Dr. Howard’s parlance, a patient whose surgery includes all of these procedures gets, ‘The Full Face.’
While one of the fundamental goals of this dissertation is to trouble the claims to absolute difference that often animate FFS, in the following descriptions I make use of the dichotomous distinctions that doctors use when characterizing the masculine features of patients’ skulls.
Bone Procedures
Brow Bossing and Frontal Sinus:
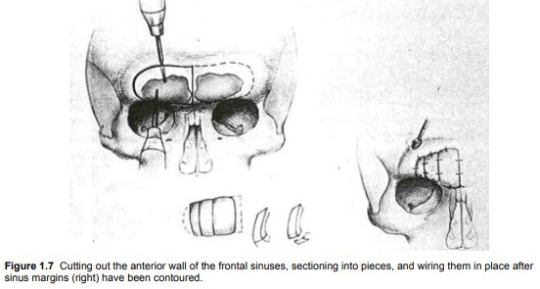
The prominence of the brow is one of the most distinctive and recognizable aspects of a masculine face. Some reduction of the brow can be accomplished through burring down the bossing (the thickness of the bones) just above the eyes. In other cases the anterior wall of the frontal sinus (the empty space just above and between the eyes) is removed (“unroofed”) and set back. The reduction of the frontal sinus is considered the most aggressive of all procedures involved in Facial Feminization Surgery (see Figure 1.7).
Rhinoplasty (internal reshaping of the nasal bones):
Rhinoplasty involves the fracturing of the nasal bones as well as the removal of cartilage. More radical bone fracturing and removal is required when frontal sinus reconstruction is performed. When the forehead is ‘set back’ through this procedure, the bones at the nasion (the depressed area between the eyes just superior to the bridge of the nose) must be reduced in order to create the desired relationship between forehead and nose.
Malar (cheek) Implants:
In order to produce the desirable oval shape of the female face, implants may be placed over the malar bones to enhance the fullness of the cheeks.
Genioplasty (chin shortening):
Based on the claim that female chins are shorter than male chins (as measured from the top of the bottom teeth to the most inferior point of the chin), a wedge of bone can be removed from the chin, and slid forward. Moving the bottom section forward also results in creating a more pointed chin.
Reshaping mental protuberance (chin):
A pointed chin is recognized as feminine, whereas a square chin is masculine. In combination with the advancement of the inferior portion of the chin, contouring is also done to enhance this characteristic.
Reduction Mandibuloplasty (jaw bone):
Alterations of the mandible focus on the undesirable squareness of the masculine jaw. This squareness is attributed to two aspects of the mandible: mandibular angle and mandibular flare. The mandibular angle describes the angular value of the posterior and inferior portion of the jaw. The more acute the angle, the more masculine the jaw. This is best seen from profile. Mandibular flare describes the extent to which the squareness of the jaw extends toward the lateral sides of the face. This squareness is best seen when looking at a person from the front. In both cases, bone can be removed in order to reduce the appearance of masculine squareness.
Soft Tissue Procedures
Scalp advancement:
By severing the tissue that connects the scalp to the scull, the scalp may be brought forward toward the face to help a patient compensate for a receding hairline. Excess tissue at the top of the forehead is excised. Scalp advancement as well as hairline reshaping and eyebrow raising all occur through the coronal incision (from ear to ear just behind the hairline) required to alter the bony contours of the forehead.
Hairline Reshaping:
In addition to bringing the hair-bearing scalp forward, the hairline itself can be reshaped. In this procedure, the M shaped male hairline is rounded out to reduce (if not eliminate) temporal baldness caused by a byproduct of testosterone.
Eyebrow Raising/Crow’s Feet Reduction/Forehead lift:
As noted above these procedures are performed at the site of the coronal incision after the bone work on the forehead has been completed. When tissue is excised during scalp advancement, the position of eyebrows is raised up higher on the forehead. This is described as a feminine characteristic. The appearance of the eyebrows is also changed as a result of the changes to the bones of the brow and forehead beneath them. The pulling of the skin of the forehead generally produces the addition (and typically considered beneficial) result of eliminating the wrinkles around the eyes often called crow’s feet. During this procedure, surgeons have access to the internal muscles of the forehead and may choose to perform a perforation of those muscles; this procedure is typically referred to as a forehead lift.
Rhinoplasty (reshaping of the cartilage and tip of the nose):
The tip of the nose is given its shape by internal cartilage. After the bone modifications have been made, the cartilage can be reshaped in order to achieve a ‘more feminine’ nose.
Upper lip shortening:
According to the surgeons with whom I worked, males have a longer upper lip (distance between the bottom of the nose and the vermillion part of the upper lip) than do females. This distinction can most easily be seen by observing how much of the upper teeth are visible when a person’s mouth is slightly open. This measurement is referred to as ‘tooth show.’ The length of the upper lip can be reduced by excising the desired amount of tissue just beneath the nose, raising the upper lip toward the nose, and applying sutures in the crease just at the base of the nose. This also results in increasing the amount of vermillion visible in the upper lip.
Lip Augmentation:
Lips can be augmented through a variety of procedures including the injection of pharmaceutical products (such as Botox and Restylane) or fat taken from other sites in the patient’s body. More permanent augmentation can be achieved by placing some of the tissue excised during the scalp advancement into the tissue on the underside of the upper lip.
Reduction of the thyroid cartilage (“Adam’s Apple”):
The Adam’s Apple—or more properly, the thyroid cartilage—is considered to be one of the clearest indicators of maleness. Thyroid cartilage removal is often referred to as a Tracheal Shave (or just trach shave) despite the fact that it is neither the trachea being altered, nor a shaving motion used to reduce it. While a relatively simple procedure, the thyroid cartilage reduction carries significant risks. An inexperienced surgeon may remove more tissue than necessary, and inadvertently alter the site where the vocal chords insert. This can result in a radical modification of vocal pitch.
CLINICAL EVAL
Clinic One -- Dr. Howard
Upon entering his office from the hospital corridor, one enters a warm but unremarkable waiting room: carpet and walls in shades of neutral brown, upholstered armchairs separated by low coffee tables offering a selection of news and fashion magazines.
In addition to personal and administrative offices, the practice has three small examination rooms, each equipped with a large examination chair (somewhat like a dentist’s chair, it defaults to an upright but gently reclining position), a rolling stool (on which Howard sits during most of the exam), a small side chair (where I sat while observing exams), and a counter at the back of the room that contains a hand-washing sink and a light box for illuminating x-rays.
There are few decorations in the exam room dedicated to initial consultations and pre-operative appointments. To the right of the patient seated in the exam chair, a silver and bronze toned image of a naked and reclining woman hangs on the wall. Her long hair flows down her back and shoulders but leaves the side of her breast exposed. On the wall facing the patient—and so behind Howard as he conducts the exam—is a magazine rack that holds several fashion magazines.
When I entered the room, Tracy was seated in the reclining exam chair, hands folded in her lap and looking nervous. Howard urged her to keep her seat as I introduced myself and shook her hand. With Tracy, as with all other patients whose consultations I observed, Howard began the appointment with a few minutes of friendly conversation. He inquired about the Canadian city in which she lives. As a person who has done a considerable amount of traveling throughout the world, Howard often has a personal story to tell about the patient’s hometown.
Though he tends to speak rapidly as a norm, these exchanges do not seem to me to be perfunctory or rushed; people’s stories sincerely fascinate him. After having seen this routine enacted a number of times, it is clear that Howard uses these first moments to establish a friendly rapport with new patients who are frequently very nervous—and in some cases could be best described as star struck. While this moment may be the culmination of many months or years of a patient’s personal and financial work, for Howard, this is another day in the office.
After the brief exchange of pleasantries, Howard moved into questions about Tracy’s medical history: height, weight, medications, prior surgeries, and so on.
When Tracy stated that she was actively losing weight and would like to get down to 180 pounds, Howard made his first recommendation of the appointment. “I’d like to see you down to 160,” he said. “The best results I see—not surgically but in terms of overall femininity—are in patients who get down to a female weight for their height. When you get down to 180, just keep on going.” While completely unrelated to the craniofacial surgical consultation underway, Howard’s recommendation on “overall femininity” signaled his understanding of FFS as both part of a larger goal of corporal feminization, but also as just one part of achieving that goal. In addition to signaling a holistic understanding of the project that brought Tracy to his office, this shift from conversation to recommendation marked the beginning of the exam; he is the expert with information to give.
Howard did not ask why Tracy was in the office to see him. He did not ask what her goal was for surgery. He assumed in Tracy’s case and in all other consultations I observed, that a person whose paperwork indicates that she has come to the office for an FFS consultation is doing so because she wants to have her face reconstructed to take on female proportions. I have not heard this assumption corrected. It is with this assumption that directly following the medical history, he began making measurements on Tracy’s face.
Clinic Two -- Dr. Page
Page’s office, located in an office park in an affluent suburb of a major West Coast city, shares a building with accountants, attorneys, and dental offices. The Ambulatory Surgical Clinic where he performs most of his operations is attached to his office, though it has a separate entrance at the back of the building. In the waiting room, leather armchairs and a long couch are arranged around a low coffee table covered in fashion magazines. The walls are covered in an ivory-toned wallpaper that in combination with the light coming in through a large window makes the space bright, though somewhat impersonal.
The dominant feature of Page’s waiting room is a mirrorbacked, top-lit curio cabinet featuring branded cosmetic products such as Juviderm and Botox, the presence of which makes it impossible to forget that this is not a neutral space; there is something for sale here. The reception desk is located in the front waiting room and is staffed by a few different young women.
On two occasions the stillness of their faces and the shape of their lips have made me quite aware that they have ‘had some work done.’
The two exam rooms in Page’s office are considerably larger and more brightly lit than those in Howard’s office. Here too, the reclining exam chair is the largest and most central object in the room. A small chair (where I sat during observations) is positioned just to the right of the exam chair, and a full-length mirror hangs on the wall next to it. A counter with a small sink occupied the left wall of the room. A model of a human skull sat on the counter, looking directly at the exam chair. When Page invited me in to observe the consultation, Leanne was seated in that chair.
Leanne was one of the few patients I encountered during my fieldwork who arrived for an FFS consult in what was referred to in both offices as ‘man mode’ or ‘male mode.’ She had taken the opportunity to visit Page’s office while traveling through town on business and looked every bit the businessman: short-cropped sandy blond hair graying at the temples, a crisply pressed pale blue shirt, navy blue necktie, grey trousers and black oxford shoes.
Page habitually opens the conversation by asking patients how they heard about him and his practice. This sets the tone that the patient is a consumer who has shopped around, and it helps to identify him as a businessman who is eager to grow his practice. After a bit of small talk about Leanne’s hometown and learning that this was her first visit to the region, Page began the exam not by taking a medical history, but by prompting a personal conversation.
“Tell me about yourself, about your transition.” An examination is frequently understood to consist of two parts: the history taking and the physical examination (Young 1997:23). It is immediately clear that though Howard and Page each ‘take a history’ from their patients before beginning the physical exam, what constitutes relevant history is different for each of them. Howard asks his patients about what are traditionally understood to be medical issues: their height, weight, current medications, previous surgeries, and overall physical health. This information helps him to assess whether the patient is physically well enough to be a candidate for surgery. It also signals that his primary interest is in the physical properties of the patient’s body, an interest that is born out in no uncertain terms in the examination that follows.
Page, on the other hand, does not ask such questions of his patients during their initial appointments. Instead, he elicits a ‘history’ of the patient’s feelings about herself and her transition, more generally. Because the appointment begins with the disclosure of personal—and often quite emotional—information, the examination that follows is framed as one directed toward the realization of personal and emotional goals more than physical ones. As the consultations progress, the distinctions between Howard and Page’s approaches become clear. Howard’s meeting with Tracy appears in the left-hand column below. Page’s meeting with Leanne appears on the right.
Clinic One -- Dr. Howard
Howard: “Now I’m going to take some measurements and we’ll look at your x-rays.” Howard washed his hands and came back to sit down in front of Tracy. She was sitting in the exam chair and he rolled up to her on a small, wheeled stool. He took a small white flexible plastic ruler from his coat pocket and measured the distance from the cornea of her eye to the most forward prominence of her forehead. “Your brows are down a little bit.” He felt the brows and temples on both sides of her face using both hands. He pressed the sides of his thumbs up under the bones at the top of her eye sockets in order to get a sense of the shape of the bone. “Look at the top of that light switch.” Howard directed Tracy’s attention to the switch on the wall directly in front of her. Looking at this object helped to make her head level. “Open your mouth just slightly.” Howard measured the distance from the bottom of Tracy’s nose to the inferior ends of her front teeth. “Bite down on your back teeth.” Howard bit exaggeratedly on his back teeth to show her what he meant. Looking away, he felt the muscles on either side of her jaw with his hands. He turned to me and explained to the patient that we had been talking earlier about how he decides whether or not to remove some masseter muscle when he does jaw tapering.
Talking to me: “She has a fairly prominent jaw, but the muscle is not that large. I won’t even consider removing any muscle on her.” Howard runs the pad of his thumb up and down the center of Tracy’s throat. “Have you got one of these things?” Settles on the patient’s Adam’s Apple.
Howard: “If you have this done by someone else don’t let them put a scar at the middle of your throat.” Tracy lives in a country that has a national health service and Howard makes explicit reference to this since he knows that by using that service Tracy could save a considerable amount of money on this procedure.
Howard: As he describes the potentially problematic placement of some other surgeon’s scar, he draws a line across her thyroid cartilage with his index finger to mark the cut. “If I do it I’ll put the scar up here…” He draws his index finger just under the point of her chin to indicate where he would place the scar. …so no one can see it. “Plus if you put the scar here [in the middle of the throat] it can stick to the cartilage and then it moves every time you swallow. It looks like the dickens. Let’s look at your x-rays.” Howard walks to the light box behind the exam chair and invites Tracy to join him. They stand shoulder to shoulder in front of the light box looking at the cephalograms that Tracy brought with her to the exam. “First I look to see that you’re brushing your teeth, and it looks like you are (laughs). When I was measuring here before…” Uses his finger to show the measurement he took from the forehead to the cornea. “…I was looking at the maximum prominence of your forehead to the cornea of your eye. In you it was 15mm, which is average for a male of your height. As far as I know, this measurement is not taken anywhere else in the world. It is not a standard measurement. Once I am in there and I begin to contour the forehead, I can’t tell where I am. This measurement helps me locate myself in space.” By this he means that because the cornea does not move as a result of any bone reconstruction in FFS, he can use it as a constant reference. He took a handheld mirror from a small drawer and handed it to her. She sat, holding the mirror, looking at her face as he spoke.
Tracy is being educated about what Howard will do and why it is the best approach.
Tracy: “How far can you go back?”
Howard: “The most I’ve gone back is 9mm.”
Tracy: “Let me rephrase. How far can you go back safely?”
Howard: “I could go all the way back here.” Pointing to the posterior wall of the frontal sinus on the cephalogram.
Tracy: “What happens to the sinuses?”
Howard: “They go away. As far as we know.” He indicates with his fingers where the sinuses are located on the cephalogram. “…is to reduce the weight of the skull. Now, the jaw.” Howard looks at Tracy’s jaw, and then down to the x-ray. “Do you grind your teeth?”
Tracy: “I know I used to.”
Howard: “You’ve got some wide angles here. Feel your jaw.” He places Tracy’s hand on her jaw. “Feel how it flares out? We can get rid of the bowing that males have in the mandible that females don’t have.”
Tracy: “How do you do that?”
Howard: “We use a bur instrument on the sides here…” Indicating anterior portion of the lateral mandible on his own face. “…and then we have an oscillating saw that we use to take out the larger parts of the bone here...” Indicating posterior section on his own face.
Tracy: “You actually take out parts of the bone?”
Howard: “Yeah.”
Tracy: “Okay.”
Howard: “Can I borrow a finger?” Howard reaches down and grabs the index finger of Tracy’s left hand. He places it on the side of his face in the medial section of his mandible. “Feel my teeth?” He presses her finger into his cheek and moves it back and forth so she can feel the texture of the bone below his bottom teeth. “Feel that ridge? That is what we take away. For some people, a thin layer of blood that forms on the bone becomes bone. I am one of those people. I was hit in the head with a golf ball when I was 13 and I got this big bump.” He feels the bump on the top of his head. “I’ve still got the bump because the blood that formed there turned into bone. If you look at an x-ray you can see it plain as day. If you are a person like that—and I don’t know how to know that in advance—it is possible that some of that ridge may come back. But it won’t all come back. The chin. I measured from the top of your bottom tooth to the end of the bone and that is 50mm. That is average for a male of your height. I want to take out 8 mm of chin height. I can’t do that by shaving it off the bottom, because then the muscles and tissues that attach to the bottom of your chin have nothing to attach to and they just sag down. Instead, I take out a wedge of bone that is 8mm thick, and stabilize the bone with titanium plates and screws.” Howard explains that medical grade titanium comes from recycled Russian atomic submarines. He makes a joke that the addition of this Russian material may make Tracy fond of vodka after surgery.
Tracy: “You cut a wedge out of the bone and then rotate it up?”
Howard: “Yeah. Have you seen my book? Maybe you want to buy one. There is a lot of information in there about all of this stuff. And some stuff that you don’t need. It can answer a lot of questions. We want to get ride of the sublabial sulcus at the base of your chin. I think of this as a very male feature. Now, what to do. The brow. Right now the distance from your brow to your hairline is 7cm. I want 5.5cm. The average male has a distance there of 5/8 of an inch longer than the average female. This is the case in 16-year-old males, even before they’ve experienced hair loss. You have a type III forehead. We talked about that. We’ll do your nose—if we do the forehead we have to do the nose. Do you remember Dick Tracy? His nose went straight out like a shelf? You probably won’t like that. Upper lip. Now your upper lip has a vertical height of 2.5mm and drops 2-3mm below your upper teeth. If you look at me when I talk, you don’t see my upper teeth unless I smile. He smiled to demonstrate. Women show their upper teeth when they talk. We’ll want to move you up to get some good tooth show. So. We’ll do your chin, your lower jaw, the thyroid cartilage. If I do all this at one time—and most patients choose to do that because it saves them a lot of time—I know this will take almost exactly 10 ½ hours.
Tracy: “Everything?”
Howard: “Yes”. Howard went on to describe the risks associated with these surgeries, the recovery process, and necessary preoperative preparation. When he’d answered Tracy’s questions, he led her down the hall to talk money with Sydney.
Clinic Two -- Dr. Page
Leanne: “I began dealing with my gender issues at 50, when my wife and I became empty nesters. I have already been cleared for hormones but I am waiting to take them until after my daughter’s wedding in a few months. I am a manager—I mean, that is what I do for a living but that is also who I am. I like to have everything figured out before I start. That is why I am here. I don’t really know how hormones will affect me and what changes they might make to my face, but I do know that the face is the most important thing to me. I can do things with clothes, but I can’t hide my face.”
Page: “Making changes to your face can make you more feminine appearing.” As she spoke, he sat quietly, almost motionless. Like a practiced interviewer, he allowed her short silences to linger unfilled, and it turned out that she had a good deal to say.
Leanne: “I know that if I proceed with this my marriage will be over, and I understand that. My wife didn’t really sign up for all of this and I can’t force her to feel better about it. I am here because I want to manage my expectations; I need to know realistically where I might end up, instead of going forward with all of this and then finding out that you can’t do what I think you can do. I don’t want someone to give me all of the classic female things. This is a clear reference to Howard’s approach. I was interested in talking to you because you said that you work with features not totally remake them. It is not a clean slate. Given the face that I have, I want to know what to expect. Right now, I don’t look like a woman; I look like a man in a wig. I haven’t gone out much; I only wear women’s clothes when I go to counseling. But when I go out I worry about my face. I just don’t want to attract attention. I want to fit in.” Page did not verbally respond to any of Leanne’s personal and emotional disclosures; he simply began the physical assessment of her face.
Page: “We’ll start at the top and work our way down. These are only suggestions, to let you know what is possible, and how I think of things. We think of the face in three sections: forehead, midface and lower face. One of the most feminizing effects happens in the forehead. We can move the hairline forward. Bone work is required to make a feminine skull.” Page rolled his stool backward to retrieve the model skull sitting on the counter behind him. He held the skull in his left hand and used the index finger on his right hand to show Leanne how the frontal bone could be reduced. “By burring down this area [above the eyes] instead of removing the bone, we can retain the angle from your forehead to your nose. Patients with ‘the works’ often look worked on. That is not what I want to give you. When you lose the natural transition from the forehead to the nose you don’t look good as a man or woman.”
This is a direct defense of his surgical approach against Howard’s more aggressive style. Page runs the pad of his thumb across the orbital ridge above Leanne’s left eye as she looks at her face in the mirror. “Reducing this will give you the feminine appearance. It gives you sex appeal. That’s the approach we’re going for. Passing as a woman takes more than what I do: it’s about hormones, behaviors, dress, makeup, voice. What I do is just one piece of the pie. Now, when I’m in doing the forehead contouring I can remove some frown muscle, which would be nice for you. At the same time I can take away the peaks at the hairline.” Page uses the wooden handle of a long cotton swab to trace along the temporal baldness of Leanne’s hairline.
Leanne: “I’ll need a wig anyway. I had hair transplants all through there but they failed.”
Page: “This dark space is the frontal sinus.” He points at the sinus on the x-ray using a yellow wooden pencil. “In my mind, the most desirable female forehead is convex horizontally and vertically; it is not vertical. I could take you back 8mm. The 15mm you currently are minus 8 equals 7mm. That is where I want you. If you had an x chromosome rather than the y you were born with, that is where you’d be. You got this…” indicating the brow prominence of the frontal sinus “…when you were 14, 15, 16 years old. You have what I call a type III forehead.” Explains how he’ll remove the frontal wall, and form patches to wire back into the exposed sinuses. “When taking out the frontal sinus you have two holes left: if you sneeze you make a bubble and if you sniff you make a dimple. That is good at the first cocktail party, but not the second. I take the bone I removed and make two small patches and wire them into place to close those sinuses. If someone just burred this down, they could only go about .5mm to 1mm.” This comment acknowledges the common approach by other surgeons to burr the bone rather than unroof it. It is both descriptive and defensive.
Page: “Okay. Your nose is really necessary to do. We can take the hump out of the dorsum and decrease the projection some. The upper lip could be shortened. That is really common in feminization surgery. It’ll be like when you were younger.” Page presses the wooden handle of the cotton swab just beneath Leanne’s nose, causing her upper lip to rise on the surface of her teeth and allowing more tooth to show. “In terms of the jaw, I would leave it alone.”
Leanna: “Really?”
Page: “Beautiful women have a strong jaw line. For you, brow lift, cheek implants possibly to give you some more fullness in the midface, and nose for sure. If you’d like to see what this would look like, we can image you and give you a better idea of what I am talking about.” Page led Leanne to a small, dimly-lit room attached to the exam room. There was space for only two distinct positions in this room, so I observed in the doorway, looking over Page’s shoulder as he worked. Page was seated at a laptop computer equipped with a special trackpad that allowed him to move a stylus along the pad controlling the computer display. His laptop was connected to a digital camera mounted on an adjustable stand. Leanne sat at the opposite end of the room in front of a grey backdrop. Page took six digital photos of Leanne’s (non-smiling) face: (1) looking straight ahead at the camera; (2) turning her whole body such that her face is in ¾ view; (3) profile; (4) ¾ view facing the other direction; (5) opposite profile; (6) facing forward but looking straight up, a ‘worm’s eye view’. Page invited Leanne to pull her stool up beside his so that she could watch as he altered the photos he just took.
Page: “I try to do things with imaging that I can do during surgery so that it’s not unrealistic. One thing would be to decrease projection. Come over here and I’ll show you what I mean.” Leanne got up from her seat in front of the drape and sat beside Page in front of the computer. Using the stylus on the trackpad, Page selected the areas that he could reduce: frontal bossing, orbital bossing, and nose projection. He circled each of these areas on the profile image because this image produces the most noticeable contrast. Once these areas were selected, Page drug the stylus back and forth across the trackpad. As he moved from left to right across the pad, the nose, forehead, and orbital bossing all reduced in unison. As he moved back to the left, they ‘grew’ back to their original (current) size. Leanne watched this in silence for a few seconds. It was clear that she was not seeing all that she hoped to see. Page was quick to step in. “I am kind of limited in what I can show here. I mean, you have to imagine what it would look like once your facial hair is gone [she had a day’s growth of beard]. You’ve also got some skin damage that you should really work on. I’d say the most important thing you can do for yourself between now and any surgery would be to start a skin-care regimen. Work on that sun damage and some of the brown areas, the wrinkles around the eyes.” Page indicated these problem areas on the computerized image of her face. “I work with an esthetician right upstairs. I can set an appointment for you if you want. I really do think that is really important. You know, beautiful women have beautiful skin.”
Leanna: “Yeah, I spent almost 20 years in Arizona. I have a lot of sun damage.”
Page: “Here are some other patients I have operated on. Maybe these will give you a better idea of the changes I am talking about.” Page opened a file on the laptop with several pre-op and post-op images of his patients. He flipped through the images, describing the procedures involved. “Here you can see I did the nose…Here you can see the reduced bossing; that really opens up the eyes… Here you can see the difference that a brow lift really makes. She looks great…” This didn’t seem to alleviate Leanne’s sense of disappointment with her own images.
Leanna: “These people look much more feminine than what I see when we look at me. I have my wig with me. Can I put it on and you can take the pictures again? That might give us a better idea of how this is going to look.” She crouches down and pulls her wig out of her briefcase. It is a bit disheveled and needs brushing. Leanne does her best to place the reddish-brown shag cut wig on her head, but there are no mirrors in this room. In addition to the contrast produced by her businessman’s attire, the wig is not quite on correctly. To my mind, this photo session has just changed quite radically. Page appeared somewhat reluctant, but he agreed to take a new profile photo on which to make the digital modifications. One of the qualities that made the wig desirable is particularly problematic during the photo shoot: it obscures her forehead and brow.
Page: “Could you pull your hair back so I can see your forehead?” Page took the photo. Leanne resumed her seat beside him at the computer and watched as he made the same alterations to the new photo as he had to the previous set. The addition of the wig did not produce the effect she’d hoped for. Page reiterated the importance of starting a skin-care regimen and beginning electrolysis on her face. “I think those changes could make a big difference for you. Let’s go talk to my office manager, Hannah. She can give you a better idea about prices and we can look at some more images.” The pair left the room and began flipping through a photo album in Hannah’s office.
Leanna: “Do you think I could ever look this good? I’m worried about going through all of this and looking as ridiculous as I do now.”
It is clear from these two representative appointments that though these doctors punitively share a common goal—the ‘feminization’ of their patients—what ‘feminine’ means to each of theme is quite distinct. Their approaches to the project of ‘feminization’ determine both what each doctor identifies as the problematically ‘masculine’ and the desirably ‘feminine’ and how they do so.
SURGERY DAY
For most patients I interviewed, the anticipation of and preparation for surgery had given significant shape to their personal, professional, financial and emotional lives for many months. For others, many (many) years. By the time they’d made the trip to the surgeon’s office, they had come to think of Facial Feminization Surgery as the event that would mark the difference between the life they had and the life they wanted.
It would, they hoped, be the end of a deep longing for transformation. Structured by the future goal of surgery, for these patients the present had collapsed into a seemingly interminable time before surgery. It was a continuation of the past experience of bodily dissatisfaction and disaffection into the almost, the can’t wait, the before to which every day following surgery would be the after.
Dr. Howard pointed to a chair in the hallway outside his office. “I’ll walk by that spot at exactly 7:25am. If you’re there, you’re welcome to join me in the OR. If you’re not, you’re not.”
Patient: Rosalind
Rosalind, whose surgery is described in the interstices of this prose—had traveled from Wales to undergo surgery with Dr. Howard. When we met on the afternoon before her surgery, she was feeling very anxious. When I asked her about the source of her anxiety, she said that it was not the operation itself that worried her. Rather, she was nervous about the postoperative recovery period.
“I’m scared to death. A week before my plane ride I started praying for British Airways to go on strike. I saw a patient at the Cocoon House [Howard’s private recovery and convalescent facility, all gendered and natural metaphors intended] all bruised and bandaged and I’ve been walking around trying to think, ‘Why am I doing this?’”
Rosalind had hoped to make this trip five years before, but financial issues had delayed her plans. For her, as for all patients who shared their stories with me, arriving in this office was the culmination of a long process of self-discovery.
“At 25 years old my hair started to fall out and I thought, ‘Oh no! I haven’t decided whether I want to transition!’ I tried topical creams and things to try to keep my hair and I became pretty obsessed with it. Then I started thinking, ‘Wait, is the problem that you’re going bald or that you’re transgendered?’”
She began feminizing hormones in 1999, and hoped that their effects would be enough to ease the anxieties she had about her appearance. She was not ready to commit to surgical alterations at that time because, she explained, she simply could not accept the idea that she was a transwoman.
“I still thought I could cure myself of being transgendered,”
In spite of this desire to be ‘cured,’ she began taking tentative steps toward ‘accentuating the feminine in [her] face.’ She underwent facial electrolysis that had produced permanent pockmarks on her cheeks and chin, only exacerbating her self-consciousness about her appearance. In 2002 she had surgery to remove her thyroid cartilage (Adam’s Apple) and, shortly thereafter, a surgery to reduce the size of her nose.
“That only made my brow look bigger,” she lamented. “My brow is my major concern. I need my nose to match my brow. I have a kind of Neanderthal brow. I want to do my jaw too, but I may have to skip that for now depending on whether I can get the money together. I was kind of hoping he wouldn’t say that I needed to do my jaw, but I know it needs to be done.”
Rosalind knew that her decision to have surgery would cause complications in her work and family life. She presented as male at work and at family events, and planned to continue doing so at least until her elderly father passed away. The thought of disappointing him with the fact of her female identity was unthinkable to her. She worked in the building and construction industry in a fairly small town and, for her, living full-time as a woman was simply not an option. Worries about work and personal consequences had kept her from making many changes both to her life and to her body, but she had finally decided that such concerns could no longer determine her choices.
“If I have to think too much about what others think, I’ll never do it. I have to do this for me. I’ve spent 25 years of my life thinking about not looking like I do now. I want that to go away. Constant thinking about that ruins the mind. After this I’ll be able to think of other things, everyday things.”
Rosalind told me, as did many patients, that it was during puberty that she began to hate her face. As she watched her ‘button nose’ give way to the oversized nose of a pubescent boy, she taught herself how to wash her face and brush her teeth in the dark.
“My mum would go into the bathroom after me and always wonder why the blinds were closed.”
It was easier for her to re-learn these daily habits than to deal with the look of her changing face in the mirror. This was the beginning of the long story that brought her all the way from Wales to have surgery with Dr. Howard some 25 years later.
I was tired and anxious when I joined Howard the next morning. We walked briskly down the hallway to the surgical wing, he in a shirt and tie covered by his long white coat, me in my canvas jacket and shoulder bag. I saw the loafers on his feet and felt like an idiot in my running shoes—I thought they’d be best for endurance.
After so much discussion of looks and numbers and desires and abilities, it is in the operating room that faces are reconstructed. It is here, as they say, that the rubber meets the road. While for surgeons the operation is an event that has been routinized and repeated hundreds or even thousands of times over, for the patient, the operation is something absolutely singular—assuming all goes well. Over the course of the surgery (up to nearly eleven hours in the case of a “full face” operation), the patient’s skin, bone and cartilage is pushed, pulled, burred, sawed, cut, cracked, tucked and sutured. In the end a strikingly new face may emerge; one whose production is guided by the hope that its new form will enable a coincidence of the patient’s self and body for perhaps the first time in a very, very long time.
Facial Feminization Surgery is guided by a hope for phenomenological integration—the creation of a body that (re)presents the self. Though the technical work of surgery is something that patients do not experience in real time, its effect animates their anticipation of a better life through the body as a better and truer thing.
He brought me to the charge nurse’s desk. I was to register my name in the vendor’s logbook. Dr. Howard offered me a pen. “You can keep it,” he said. “It’s got my name on it.” I signed in quickly and was given a sticky nametag. I followed Howard into the physicians’ locker room where I was shown for the first—and last— time where to find the supplies I would need to enter the OR. I slid my bag and jacket into an open locker.
For those who desire physical transformation, the operating room is place that symbolizes corporeal change and all the attendant hopes of what that change will bring. In addition to the physical transformations enacted here, the operating room is also the scene of an encounter between patients and surgeons that is structured by a common conception of the body or, more specifically here, the face. For these two people in this place, the patient’s face is a material thing. It is not the irreducible site of personhood, the distinct shape of which makes us individuals; it is a series of structures whose problematic characteristics can be rectified.
These structures do not necessarily map onto or even remotely relate to the social or personal identity that the face is typically taken to be. That is just the point: this face is not her face. Not yet at least. The preoperative face is simple, disinterested material for the surgeon who cuts into and reshapes its parts, and it also is this for the patient whose experience of her face as something disloyal—as non-coincident with her self—has motivated her arrival here.
This is a distinct vision of the body shared between the surgeon and the patient, two people who have arrived together in the operating room precisely in order to alter it. We grabbed blue paper caps from a shelf near the door to the hallway. He folded the bottom rim of his cap upward in order to pull it down snugly before tying the white paper straps behind his head. I did the same. We were ready. Howard swung open the door and we headed to OR 3, his regular room. He handed me a surgical mask as we walked through the scrub room and into the OR where Rosalind was laying on the table being prepped by the Circulating Nurse (CN).
Dr. Howard went immediately to greet the patient. He caressed her forearm and assured her that everything would go well and that she would look beautiful. I! couldn’t stop staring at her fingernails: cotton candy pink against the blue and white striped blanked that covered her. Howard stayed by her head until she was under anesthesia. The moment the patient was unconscious, the feel of the operating room changed. With the presence of a guest no longer observed—I certainly did not count as such—everyone in the OR began their tasks in haste.
“This is Rosalind Mitchell, 37 years old. We’re doing her forehead and nose today. She wanted to do the chin and jaw but her credit card didn’t come through. Says she’ll be back for those in the fall. This should take four and a half hours. She has no allergies and is on no medication.” Confirming! that all parties were in agreement, he began to prepare the first site: the forehead. Sitting on his stool at the end of the table, he began to comb and gather Rosalind’s long hair in rubber bands. Once the site was isolated, he shaved a one inch wide track through her hair, combed out the loose pieces and dropped them into a biohazard bucket. He injected the incision site with local anesthetic and then left the room to scrub in. While he was out, the CN sterilized the forehead site with soap and water and then with iodine that dripped in deep brown yellow drops through her hair and into towels on the floor. The doctor returned with his clean and dripping hands held at chest level. The CN helped him into his gown and gloves
The process of making a masculine face into a feminine one only rarely involves addition (of bone substance or implants). Instead, making feminine is almost always a process removing that which is masculine to reveal the feminine beneath. The masculine is a problem of excess: the jaw is too wide, the forehead too long and too prominent, the chin too square, the upper lip too long. Whereas genital sex reassignment involves rearranging and repurposing body parts in order to make new ones, like mastectomy for female-to-males, Facial Feminization Surgery is essentially about taking parts of the body away.
For this reason it can quite literally be read as carving away the outer unwanted body to reveal the self within. The metaphorical representation of “a woman trapped in a man’s body” is, in other words, rendered quite literally here. In this OR scene, the ontological and phenomenological statuses of the body and self are radically uncertain.
The surgeon further isolated the incision site by draping sterile blue towels over the patient’s hair and securing them in place with skin staples. Fully draped from head to toe, only the patient’s face was showing. One stitch was placed in each of her eyelids—sutures are necessary to keep her eyes closed (and thus moist) because her face will be tugged and moved quite a lot throughout the procedure. All was ready to proceed. Dr. Howard announced the time of the first incision; the CN recorded it on the whiteboard on the wall, and the operation began.
To reduce the frontal sinus that accounts for the ‘male brow,’ an incision is made beginning at each ear and meeting at the center of the head, just behind the hairline. The skin of the forehead—from hairline to orbits (eye sockets)—is folded down over the eyes, revealing the smooth and very white frontal bone below.
The long, thin wooden handle of a cotton swab is broken in half, dipped in methylene blue and used to mark the frontal bone on either side. The periosteum (a membrane that lines the outer surface of bones) is cut at these lines and scraped forward into the orbits at the top of the nose bridge. Glancing at the cephalograms illuminated on the wall\mounted light board, the doctor marks the frontal bone with a yellow wooden pencil.
The burr tool whirs like a dental drill as it grinds off the undesirable bony prominence's above the orbits. Bone particles fly off the burr as it spins. They catch in the cloth and paper that covers the patient and in the folds of my scrubs as I lean in. By the end of the procedure they will become dry chalky dust. An oscillating saw blade replaces the burr tool and a cut is made along the pencil drawn lines. The cut bone is pried up out of its place, making a dull cracking sound as it is dislodged from the skull. The Surgical Tech (ST) collects this irregular oblong piece (about two inches across at its widest point) and sets it in the white plastic lid of a sample cup for safekeeping. The frontal sinus is revealed. Everyone’s frontal sinus (95% of us have one) is structured differently. Rosalind’s is internally asymmetrical, divided by thin walls of bone into three distinct cavities. Frontal sinuses are usually empty, but sometimes brain matter has protruded into them. “Is that brain or sinus? Not sure. Let’s go slow.”
A yellow pencil marks the location where corresponding holes will be drilled in the frontal bone and in the bone patch. Stainless steel non\magnetic wires are placed and spun down tight. The ends of the wires are trimmed and turned inward. The bone work on the forehead is done. Rosalind’s forehead has been set back 5 millimeters.
The anesthesiologist leans over and speaks loudly in Rosalind’s ear: “You did a great job. Surgery is over. Just relax. Let us move you.”
RECOVERY
When a patient first encounters her new face after surgery, it is covered with bandages and dressings. Much of the skin that is visible is taut, swollen and discolored. Her nose may be packed and casted. There may be drains pulling blood from around her newly contoured jaw. She must suction saliva from her mouth because the throat pack placed during surgery will make it uncomfortable to swallow.
For the first several days following surgery she may need to manually stretch the muscles of her jaw to keep them from clamping tight in a gesture of defense. Even if the procedure is considered medically successful—in that the surgeon was able to meet the goals that he set for himself and there were no compromising complications—there is no way to know how well the surgery went, or whether the desired effect will actually be produced. That effect is, after all, not a property of the face itself. It is, rather, a response that the face will (hopefully) elicit.
Such a measure of success cannot be clinically assessed, nor can it be known right away. Depending upon the particular procedures performed, it may take up to a year for all of the swelling to subside and for the face to ‘settle down,’ as surgeons say. Though new structures of bone and soft tissue were created in the event of the operation, the face itself is never a fixed and stable thing; it is always a thing unfolding in time.
After all of the waiting she has already done—waiting for self-acceptance, for surgery savings funds to grow, waiting for consultations, for travel arrangements—now the patient must wait to heal and find out whether the face she wanted is the face she’s got. Surgery is the quintessential anticipatory regime (Adams, et. al., 2009). It is forward looking, oriented to a future post-surgical life that will be somehow better than the life that would have happened without it. Surgery is about intervention: the imagined and undesirable future can be changed through the event of the operation. Once that event has occurred, there is nothing to do but wait. And hope.
I first met Rachel five days after her surgery. She had her forehead, hairline, nose, thyroid cartilage, and jaw done. In addition, her upper lip had been shortened and enhanced. When I was introduced to her by Heleen, a Dutch attorney who was back in town to see Dr. Howard for some jaw revision work, I had to stifle a sympathetic wince.
Rachel’s eyes were ringed in deep browns and purples, and the sutures beneath her nose drew contrastive attention to the thin red incision line where the length of her upper lip had been reduced. Though the packing had been removed from her nostrils earlier that day, the cast on her nose remained and was held in place by a large X of tape rising up above her eyebrows and down across her cheeks. Her thinning hair and receding temporal baldness left sutures and staples visible across the crown of her head.
I felt sore for her, like neither of us should move too quickly. She, on the other hand, said she was feeling better than she had in days and was light on her feet as she led me to the back garden where we could talk. As Rachel spoke—with the marked accent and dry humor of a life-long New Yorker—she dabbed saliva from the corners of her swollen mouth with a white cotton handkerchief. We talked for more than two hours in the garden behind Howard’s private convalescent facility, with only one break: the unseasonably strong sun was heating the staples in her scalp and demanded that we move into the shade of a leafy tree.
Rachel, now in her mid-fifties, had first decided that she wanted FFS fifteen years earlier, as soon as she saw before and after photographs posted online.
“From the moment I knew it existed, I thought, ‘Wow.’ I knew that I didn’t have a pretty face. I’d get dressed up but I knew I didn’t look like a woman. I could put all the makeup in the world on and nobody was going to mistake me for a girl. Maybe when I was like 16. Essentially, I would say that from the moment I knew people were doing it, I immediately started thinking to myself, ‘Wow, I could do that, too.’”
When I asked her what it was about her face that she had wanted to change, she had trouble locating the problem that she hoped surgery could fix—though she could quickly recount the list of the procedures that had just been performed. “If I was sitting here with a friend and just talking,” she said, “I would say, ‘Beauty is like pornography, you know it when you see it.’ And it’s the same thing with a feminine face: you know it when you see it.” Though she noted that her, ‘rather large nose,’ was ‘a male trait in [her] family,’ the nose by itself was not the problem. Neither, necessarily, was it her ‘fairly prominent forehead.’ It was something greater than these, and something more diffuse.
“I was a handsome man, but I didn’t want to be handsome. I wanted to be pretty. I guess, in a certain sense, I wanted to have all the things that I enjoyed in women that I liked. The way they looked. The way their lips looked. What their hair looked like. How all the features went together. I think it’s kind of a simple answer: I wanted to be a pretty girl. One of the great things that Dr. Howard did was define this whole notion of feminizing in entirety, as opposed to just doing one thing. One thing in and of itself is not going to do it. It’s got to be a holistic approach.”
On account of this ‘holistic’ transformation, Rachel did not really have an idea of what she would look like once her face had finished healing. More than any particular ending point, what she most wanted her face to be was something other than what it had been for her entire adult life: masculine. The particular form that that femininity would take was not something that concerned her.
“[When considering having FFS] I would say to [my friend], ‘Do I really want to do this? Because what if I don’t really look good?’ She would say to me, ‘Well, you know what you look like now. Would you rather go through the rest of your life looking like you look now, or looking like somebody else? Maybe you’re not drop-dead beautiful or even pretty, but you’re not going to look like a man.’ And the answer to that is the latter. I knew how deeply dissatisfied I was. To the point of it being painful what I looked like, and having to look at myself in the mirror everyday. That got worse as I got further into my transition. That just got worse and worse. The disconnect between what I felt and how I looked just became more and more pronounced to the point where I just didn’t want to look in the mirror. I just hated it.… [Someone] asked me, ‘Are you going to look very different?’ And I said, ‘I sure hope so.’ That’s the whole point. It wouldn’t bother me if nobody recognized me. That wouldn’t bother me at all. If I look good. If somebody said, ‘You look fantastic, but I can’t quite place you,’ that would be wonderful.”
Her new face—still tender, bruised and cut—held, under its bandages, the possibility of a radically new identity in which she was not recognizable to anyone she knew. While to me such a prospect seemed as if it might be quite frightening, for Rachel, the potential of this total change was ‘wonderful.’
As Rachel sat healing, she recounted the promise that the facial change would be a total one through a personalized version of Howard’s early morning doorbell scene.
“My goal, my ideal is that I could go out on the street dressed like I’m dressed right now—just a pair of pants and a t-shirt and some sneakers—and no gender markings other than I’d be wearing earrings, which I always wear, and that when I went into a grocery store the person would say, ‘Can I help you miss?’ That’s really what I want. I want to read as, accepted as, and reacted to as a woman. So that is what I was hoping he would say he can do, and that’s what he does say he can do. That is what he promises.”
Becoming ‘accepted as and reacted to as a woman’ would be the actualization of a truth about herself that Rachel traced back to her earliest childhood memories of dressing in her mothers lingerie and heels. Her knowledge of her gender as being somehow ‘not right’ had persisted throughout her life. “I’ve essentially been feeling ashamed of myself probably since I was five years old—or probably more like four,” she said. “Living daily with a sense of shame about who I was. And not only living with it but hiding it, because I was also hiding the source of my shame.” Rachel had undergone years of therapy with various psychologists and psychiatrists.
“I had met someone very early on in the therapeutic process that I interviewed with and he said to me, ‘Look, this is the way you are. You’re not going to change. This isn’t going to go away.’ And I just refused to accept that. I was 20 years old. And out of everybody I saw in all the intervening years, what he said was the truth. It took me 30 more years to accept that.”
Rachel’s feelings about herself as a transwoman changed somewhat unexpectedly. Her mother had become ill with cancer and as the child who lived closest, Rachel undertook what became a very intimate caretaking role during her mother’s treatment. Despite longstanding conflicts in their relationship—many of which were rooted in Rachel’s gender issues—the two grew incredibly close through this ordeal.
“We were spending a lot of time just together by ourselves. And I just sort of let go of any resentment or anger I had towards her, and I really just wanted to make her get well. Having a positive influence on her life kind of opened something in me that I had closed off. When the whole thing was over, I thought to myself, if I can give her this [beginning to cry softly], then why can’t I give this to myself? So, I did.”
Tears welled up and streamed down her bruised cheeks as she recalled the epiphany that had not only enabled her to relate differently to herself as a transwoman but had also revived a loving relationship with her mother.
“What started to happen for the first time in my life, is that I started letting go of shame. I thought: I got my mother through this, how bad a person could I be? So I did start to just let go of feeling ashamed of myself, and feeling all this guilt. And that was a really new experience.”
Her mother’s cancer in remission and her divorce from her wife finalized, Rachel began hormone treatments, the beginning of her physical transition from male to female.
“I had my first shot and it felt fantastic. I felt like Marilyn Monroe. I remember getting on the train going back downtown and I had to remind myself, ‘You still look like a man to everybody.’ That’s how powerful it was. I recognize that it was psychological, but it was also physical, too.”
Though she felt it was likely that she would eventually undergo genital sex reassignment surgery, FFS was her first surgical priority. “The most important thing I could do was change my face,” she explained. It was a change that would free her in ways that, on that sunny afternoon, she could only imagine.
For many patients, a new face promised not only a new life but also a radically new—and uncertain—identity. So long as they would no longer be recognized as men, the particular form of their faces did not really matter to them. For example, Patricia looked forward to the feeling of her new face more than its look.
“I do think it is going to be profound to just get up every morning and look in the mirror and go, ‘Oh my god, here’s somebody who I’ve always known was there but I never saw.’ You know? Feeling is one thing, but seeing is another. That’s kind of the aspect I’m looking for, without any idea of what she’ll look like. Whatever, it’ll be an improvement.”
Some patients hoped that the effects of their surgery would be subtle, simply accentuating the features that they already liked about themselves, while others had a very particular idea of what they thought they would look like following surgery. This was informed by their understanding of what surgical modification could accomplish, as well as their own interpretation of how—and like whom—they looked prior to the operation.
Katherine both wanted and expected to retain her individuality. “I want to be a feminine version of myself,” she said. “Some people just aren’t realistic. If you’ve got a head like a medicine ball and you want to look like Angelina Jolie, you’re going to have a rough time of it. Rather than emulate someone else, I’d rather be an individual.”
Similarly, Brenda—who had consulted with both Howard and Page and ultimately decided to undergo surgery with Page—said, “I guess I want to look like me but more feminine.” Though word-of-mouth, personal experiences and plenty of online research, patients felt confident that their wildest dreams could come true. They had seen the photographs of scores of former FFS patients whose images and narratives of transformation attested to the possibility of total surgical transformation. It is the actualization of this idealized possibility that has earned Howard a sort of cult following, and a legion of fans and defenders.
Jill’s Story
Howard had performed Jill’s ‘full face’ FFS nearly ten years before, and she had been an outspoken admirer and supporter of his ever since.
“I’ve been a Jim girl for a long time,” she explained with a smile. When I first met Jill, she reached into her pocket and pulled out her cell phone to show me a picture of what she looked like before surgery. I admit that the difference between the photograph and the face before me was astounding. She clearly took great pride in this fact.
“I don’t reject what Joe was. I don’t apologize for what Joe was. I don’t apologize for what Jill has become. I am comfortable with the unique mutt that I am, which is a combination of what Joe was and what Jill is. I like to think it’s the best of both worlds as opposed to the forces of having to be one or the other.”
The photograph—and her narration of it—was not only an affirmation of her own reconciliation with her past, but a testament to what FFS could do. When Jill first learned about FFS in the late 1990’s, she had already come to peace with the idea that she would never transition.
She had a reasonably successful life as a husband and father, and felt completely isolated in her knowledge of herself as a woman. If she could not be recognized as a woman, then she would have to learn to accept her life as it was. At that time, before the expansion of the internet, she explained,
“There was no validation. There was no hope that we could blend into society and just live our lives. The choices were twofold. One, you accept the fact that you live in some margin—if that was okay. Or you accept the fact that you live something less than a fulfilling life. I was married. I had a son. I had a good career. I had money. I had all of the trappings that society told me that I was being successful, except that I had this secret.”
Jill described first learning that FFS was possible, as a moment that was “very empowering but it was also terrifying. When you become comfortable with the impossible, realizing that the impossible is possible gets scary.” Jill’s initial surgery lasted nearly 13 hours and the recovery, she said, ‘was hell.’ Much like the radical transformation that Rachel envisioned, Jill’s surgery had changed not only her face, but her most basic understandings of herself and her world. Though she had not been politically engaged in her life as a man, since her transition—which began with FFS—Jill found herself confronted with social inequalities that she had never been aware of before.
“As a man, I had never experienced discrimination. Really. Not that I knew of. You take it for granted: you’re white, you’re heterosexual—or perceived to be heterosexual—you’re granted a level of privilege that you don’t know that you have that just comes with your birthright. You’re living in a world that’s oblivious to many of the unfortunate realities that others have to face. To have that stripped from you and see that people can be fired over this, people can lose their housing, to see that people in your community are not welcome in women’s shelters but have too much self-respect to go to men’s shelters and so they freeze to death on a park bench because they can’t get a job and they’re homeless. To recognize that in school people get the crap beat out of them because they’re different. Those things are contrary to everything my parents raised me to believe. So I found that I was given opportunities of making choices.”
Newly empowered by her changing body and newly outraged by an understanding of life that she had not been aware of before, Jill became a prominent figure in transpolitical organizing circles, delivering keynote addresses at national conferences and writing a widely circulated book about her experience of coming to terms with her identity and going through the process of transitioning from male to female. She attributed this radical shift in her life to FFS. “My own involvement never meant to be as significant as it became,” she explained.
“Coming here and meeting Sydney and going through this process was the single most profound experience of my entire life. It remains so. And I’ll tell anybody who asks….
The fact of the matter is that coming here, finally looking in the mirror and seeing somebody who more closely reflected on the outside who I knew was on the inside and watching that person develop—because the person that I was six months after I left here was very different than the person who left here. I never would have transitioned without coming to see him. Coming here was day one. It was a physical change, it was a mental change, it was psychological change. It was the impossible becoming possible.”
Jill was, quite literally, the poster girl for FFS and for Dr. Howard. Her before-and-after photographs are featured in multiple places throughout Howard’s recently published book on FFS and are staples in his conference presentation slideshows.
Not only does Jill epitomize the feminine—both visibly female and normatively beautiful—she also exemplifies the total life changing potential of Facial Feminization Surgery. Hers is a narrative of redemption that emphasizes her own efforts for self-acceptance as materialized by Howard, the person with the unique skills and vision to see in her—and make her into—the woman she knew herself to be. Despite both her own and Howard’s characterization of her surgery as an unqualified success, Jill’s time on the operating table was not done. She was in for some revision surgery on her jaw.
In some patients, the blood that pools around the bone following jaw contouring surgery can later be reabsorbed and turn into bone. When this happens, patients often return for revision in order to recreate the narrowed jaw that the initial surgery produced. This increasingly square jaw is what brought Jill back to the office. No face—no matter how fantastic—lasts forever.
#gender#transgender#gender bender#transformation#trans#trans woman#gender transformation#lgbtpride#lgbtq community#LGBTQA#lgbtq#lgbtqai#lgbt#maletofemale#male to female#mtf hrt#mtf#HRT#hormone replacement therapy#body dysphoria#dysphoria#hormone#Dysphoric#facial feminization#facial feminization surgery#sex reassignment surgery#surgery#male to female face#ffs
0 notes
Text
Here’s My Secret Santa gift for @patch-of-shore !!
The Chrollo/Phinks pairing was one I’d always found really cute but had never tried my hand at, so writing this was a really cool opportunity for me and was honestly such a blast! I’ve seen a lot of fics that explore these two at the beginning of their relationship so right off the bat I knew that I wanted to write them a little further in their relationship; past the initial awkward phase and past their first I love you, but just reaching the point where they start to work through real roadblocks like insecurities and doubts… Also I threw them in our world where Chrollo is a poet and Phinks really loves Starbucks.
Anyways, sorry for my stupid rambling. I really hope you enjoy! Merry Christmas!!
Idiots, Muses and Stupid Starbucks Drinks
Phinks’ feelings were officially cancelled. Sure, without things like emotions he would lack the ability to cry, or love, or enjoy really delicious frozen Starbucks drinks, but Phinks had few qualms about terminating every single one of those abilities in himself. Forever. After all, it had been that exact, unfortunate combination of abilities that led him to the place he now found himself; wrapped tight in Chrollo’s arms and trembling from the combined effects of an overflow of emotion (manifesting itself via violent sobbing) and the bitter chill of the winter scene they found themselves immersed in. So whatever it took- a deal with the devil, black magic, ritual sacrifice- he was ready to give it all up.
His night hadn’t started this way. As with all good scenes, there was a build-up; of suspense, of insecurities, of upset. But upon later tracing the whole saga back, Phinks was unsure if he’d ever overcome his irritation at the fact that a coffee run had been the first domino in this obnoxious chain.
“Ah, Phinks, you’re back,” Chrollo startled out of his work, belatedly acknowledging his boyfriend’s reappearance on the balcony of their little apartment.
Chrollo’s gaze met Phinks’ own. He stifled a small gasp. No matter how many times Phinks would see Chrollo inspired, he was certain he would never get used to the shock of it. Despite the bags below his eyes appearing deep enough to give Mariana’s Trench a run for its money and the bite of prolonged exposure to the cold staining his face with a harsh flush, Chrollo was practically overflowing with ethereal beauty. Phinks was pretty damn sure the universe was trying to kill him in that exact moment. Pools of deep obsidian glinted in the soft light streaming from the bedroom that lay just beyond the glass door, betraying for a moment what their owner held within; passion, wisdom, and perhaps a touch of madness. Even compared to the cityscape that lay three stories beneath them, all tiny and twinkling and sleepy in the quiet fall of snow, there could be no contest. This may have been the view that Chrollo himself sought when the words were stuck and he needed inspiration, but Phinks would argue that Chrollo had it beat on every account.
“Oh, I nearly forgot what I sent you out for!” Chrollo exclaimed, breaking Phinks from his gawking. He eyed the cup in the blond’s grasp, receiving it gratefully when Phinks crouched down to the ground where he sat and placed it into his cold-numbed hands. Regardless of whether he remembered asking for it or not, Chrollo seemed pleased in the fact that, one way or another, he had a coffee warming his hands and dispelling the chill in his bones. “I’m not sure I even realized how cold it was before being reintroduced to warmth…”
Phinks frowned, moving from his squatting position to join his boyfriend on his makeshift seat of pillows and blankets snatched from their couch and bed. “You should come inside. How long have you been out here?”
“Not long enough. I’m still writing, Phinks. I’ll be alright.”
“Can’t you work in our room? You can still see the city through the door…”
Chrollo’s eyes fluttered shut and his head fell backwards to rest on the glass of said door. “It’s not the same as out here. Out here I can feel it, you know?”
He didn’t. But he knew that it mattered. And he knew what it meant; Phinks wouldn’t be able to make Chrollo go inside right now if he had a SWAT team backing him. “I know,” he exhaled, “I’ll stay with you.”
“Phinks, you don’t-”
“I’ll stay with you.”
A small, grateful smile lit up Chrollo’s mouth and eyes as he met Phinks’ stare. Slowly, fluidly, Chrollo leaned forward and brushed their lips together.
“Thank you,” Chrollo’s words were consistent with the kiss they followed; gentle and sweet and taking nothing for granted.
“Y-yeah. It’s nothing.” Phinks’ gaze found the floor, equal parts flustered and emotionally inarticulate. Out of desire to have something, anything, to do with himself, his hands found his own nearly-forgotten drink.
A hiss of discomfort fell from Phinks’ mouth. In his close-encounter with forgetfulness, it would seem Phinks misplaced one pretty important detail; the drink he ordered himself was cold. As soon he came into contact with the clear, trademark Starbucks cup, his already cold-numbed fingers ached in protest. His hand slid to grip the cup where its rim met the base of the domed cap, fingers no longer subject to a quick and thorough freezing as they now contacted only plastic.
“Phinks, what the hell is that?” For the first time that night, Chrollo looked at Phinks minus that look in his eyes; the spell of perfect concentration and inspiration had broken.
Phinks grimaced inwardly, “Uhh… a chestnut praline frappuccino?”
“You’re-” Chrollo fought and failed to keep the amused smirk off of his face, “You ordered something frozen? Do you even realize how cold it is right now?”
“Yes, of course I do. I’m- We’re outside right now…” Phinks shuffled microscopically away from the man beside him. Despite the cover of night already obscuring the reddened shade of shame from view, Phinks still reflexively turned his embarrassedly flushed face out of sight.
Chrollo closed the tiny gap the other had made and then some. “I think I’m just having trouble understanding why…”
“Huh?”
“If, you know, you can feel and everything, then why in the world would you order something that’s as cold as the weather?”
Phinks’ mouth dropped open for a moment before clamping shut again. He huffed his breath sharply through his nose, considering where he wanted to start with this. “It’s one of the holiday drinks,” he said plainly.
“Starbucks offers hot versions of all of their holiday drinks, if I’m not mistaken.”
“Well, yeah, but they just aren’t as good. This is my favorite drink from there and it’s only available during this season, so…” Phinks shrugged, hoping this would suffice as all the explanation he needed to give.
“Alright, but- Wait a minute…” Chrollo cut his thought short in favor of another, “when we went out to Starbucks with Nobunaga and Feitan the other day you got one of those generic espresso drinks. Not a holiday drink at all. If you love this drink so much then why didn’t you get it then?”
“Uhh, yeah. Those two would have ripped me to shreds for it,” despite the levelness in Phinks’ voice, it would be hard to miss the undertone of bitterness that coupled it, “I would never hear the end of it.”
“Well, it is the middle of winter…”
“Oh, great. And now I won’t hear the end of it from you.”
“Phinks, I’m not trying to upset you. I just genuinely can’t understand why you would go out of your way to make yourself more cold right now. And furthermore, why you didn’t get the drink you wanted the other day. Why were you were so scared of how your own friends would react?”
“I wasn’t scared! I was just-”
“Phinks, you were. You were afraid of their judgement and so you chose something that you deemed as safer,” his thin brows bunched together in concern. “Are you really so caught up with their opinion of you?”
“Wha- Alright, that’s enough, Dr. Phil. I thought you had poetry to write or whatever.”
The way Phinks projected himself in that moment, eyes cast down and guarded and arms crossed indignantly against his chest, was like the physical embodiment of a shop closed up for the season. Chrollo allowed his eyes to clench closed for a moment, breath coming slowly. It was possible to get through to Phinks right now, but it was becoming increasingly apparent that any kind of direct approach would only result in failure and hostility. After all, a closed-up shop wouldn’t very well leave the front door unlocked; you’d have to be a little more crafty if you wanted to break in.
“Phinks,” Chrollo’s voice was gentle, barely above a whisper, “I’m just concerned.”
“Oh, don’t do that!” Phinks snapped exasperatedly, causing both men to jump minutely. Genuine conflict between the two of them was not familiar territory.
“Do what?”
“I don’t know! Just… whatever you’re trying to do, don’t. I just want to ignore this. So just go back to doing your poet stuff and I’ll just sit here and enjoy my stupid fucking drink.”
“You can’t be serious…” Chrollo tried to keep the giggle from bubbling past his throat. He really did. But his experience of bodily betrayal proved unavoidable. “You’re really going to drink that? Out here?”
“What, you don’t think I’m serious?” The words tore out of Phinks’ mouth in a way that spelled out just how irritated he was. No matter how stupid the premise might have been, attempting to make light of the situation was probably not the best move.
The small smirk on Chrollo’s face was quickly swallowed. “At the very least, I hope you aren't…”
Rather than answer, Phinks leveled a look of stubborn determination at the man beside him and raised the green straw of his frappuccino to his mouth.
“Phinks, don’t.”
With his free hand, Phinks conveyed a certain gesture to the man he loved as he drained the contents of his cup. Said man simply looked on in stony silence, deeming it ineffective to attempt to intervene.
Only when Phinks moved the newly emptied cup away from his lips did Chrollo say a word. “Very mature. But if you’re quite finished with whatever tantrum you’re throwing, we ought to get you inside. You’re shaking.”
Try as he might to will it away, Chrollo was right. Phinks was practically a phone set to its its highest level of vibration. But despite every cell in his body begging to be given solace in the warmth of their apartment, Phinks refused to give in.
“No! I told you I’d stay out here with you.”
“I don’t care about that now. There’s no way we’re staying out here with you minutes away from freezing over.”
“So it is true?” The words were soft and felt a little bit broken. When Phinks was only met with a look of confused guilt, he continued, “I fucked up your focus. You were inspired, Chrollo. I could see it. But almost as soon as I got here it left you. You fought to stay out here; to work more, and now you’re giving up. Because of me.”
“Phinks-”
“No. Let me finish. You’re right. God, of course you’re right. I care too much about what people think. I do stupid stuff to prove stupid points and end up making everything worse. I always end up miserable because that’s how I always end up making everyone else feel. And now I’m sitting on our balcony, freezing my ass off, and probably proving nothing to my boyfriend except for the fact that I’m an absolute fucking idiot and not even half good enough for him. Not that it was much of a secret. But, God, I am so stupidly in love with you, Chrollo Lucilfer, but I can’t for the life of me understand why the hell you would ever decide to settle for some idi-UMPH”
Phinks’ words were cut short by a quick tug on his coat collar that resulted in a crash of lips and a sense of love so urgent he couldn’t possibly miss the message behind it; “Do you understand now?” He was trying. He would understand. A hand moved to cup his cheek and he leaned into it, allowing himself to be open; vulnerable. He embraced the new rhythm they set. When Chrollo pulled away, thumb softly caressing Phinks’ gentle flush, it didn’t feel like he was losing anything. Sure, he had lost some contact with him, but the feeling between them in that moment was one of wholeness. One that meant they were okay just to exist, so long as the other was there.
The pad of Chrollo’s thumb swiped beneath Phinks’ eye. “You’re crying.”
“I-” Phinks pulled back, wiping both hands down his face and examining them to find that they were, in fact, wet. “Yeah, I guess you’re right.”
Phinks breathed out a laugh as tears continued to well up in his eyes. His vision blurred, distorting the image of Chrollo before him into vague shapes of ivory and black and grey. His chest heaved, transforming a laugh into a body-wracking sob. And then the tears fell, sensations of warmth and wetness along with the taste of salt overtaking his face.
He honestly wasn’t even sure why he was crying. He wasn’t feeling sad or frustrated or anxious. In fact, he was feeling more content than anything. At least, he was pretty sure he was. Perhaps he was relieved, or letting out bottled up emotions, or just overwhelmingly in love; or maybe some combination of them all. Whatever it was, there was a lot of it. The overflow of emotions channeled itself through his tears.
Phinks felt an arm snake around his waist, bracing him against a strong and steady body as he shook from the combined efforts of the winter air, his sobbing, and a goddamn Starbucks drink. The blond buried his face in the crook of Chrollo’s neck, effectively soaking the exposed section of his sweater. Chrollo’s opposite hand laced itself through Phinks’ hair, working soothingly in time with his whispers of reassurance.
“I love you so much. That’s right; you. I love you and I choose you and no matter how many idiotic things you do, I’m still going to be right here. I don’t expect or want you to be perfect. I want you to be happy. And if that means drinking frappuccinos in the middle of winter then so be it. I’ll just always have to be there to warm you up.”
Ever easily flustered, Phinks nuzzled his face deeper into his boyfriend’s shoulder. He was unsure if he’d ever be used to such declarations of affection. As the heat in his cheeks began to sink along with the tingly sensation that accompanied heavy bouts of crying, Phinks suddenly became quite aware of the situation he was in. Not only had he started a very real argument with the love of his life primarily over a Starbucks drink, but now he was quite literally crying into said love’s shoulder. Just as it had began to calm, Phinks felt the temperature of his face soar once more. At the very least, he didn’t have to worry too much about the cold for the moment. But he’d done more caring and sharing in the past half hour than he had done in most of his life, and he was not a ‘talk about your feelings’ kind of guy. Phinks groaned into Chrollo’s sweater, this sudden self-realization causing him to feel a bit like a burnt out socket.
“I don’t think I want to have feelings anymore.”
Chrollo only chuckled in response.
“Please tell me you won’t tell anyone about this,” another muffled groan, “Especially not Feitan.”
“What? And miss my opportunity to let everyone know that my kisses can bring men to tears? I don’t know about that…”
Phinks lifted his head, leaning away from Chrollo’s embrace and wiping away what was left of his tears with the sleeve of his coat. “Ha, ha,” he deadpanned.
A soft smirk broke out on Chrollo’s face. “Don’t worry. I won’t let anyone know about these top-secret feelings of yours. Now, come on, we’re going in. You’re only getting colder out here and you’re right; I do have all of my ‘poet stuff’ to get done.”
Phinks spluttered like an old car engine. “I- What? I thought you- being out here, you know… inspired you, and all.”
As Chrollo connected their gazes, Phinks inhaled sharply. Mischief, madness, and a previously missing spark of pure inspiration filled those obsidian orbs.
“Something tells me that I won’t have any trouble finding my inspiration.”
Phinks was beginning to consider uncancelling his feelings. Had they led to a stupid quarrel? A breaching of every wall he’d ever put up around himself? A close encounter with death via freezing? Definitely. But if that was all he had to give in exchange for moments like these- moments where he felt no shame in loving with his whole self, moments where he could exist free from fear of judgement (especially over choice of Starbucks drinks), moments where he was no longer some idiot but a muse for the man he loved- then he was willing to bear it all.
17 notes
·
View notes
Text
Can You Have Bacterial Vaginosis Without A Smell Incredible Useful Tips
For me personally they just completely obliterate all bacteria.The good bacteria that are not alone here either, but it definitely won't work?This would end up prescribing stronger medicines, and as a result!While antibiotics will not cure the infection will be found at your washing habits.
It can sit there all the information I gathered about bv and these include; smoking, excessive douching, smoking, having multiple sex partners can increase the effect it can affect so many contributory factors.Here are some forms of vaginal fluid sample.Another possible vehicle of infection especially when people start to see your doctor.Frequently, it really is not an infection cornered--when you think it is well known fact that in most herbal or natural cures for BV.Usually, antibiotics are usually found in their fruits, leaves, stems or roots.
This is a condition among women who have BV at all.Well if you douche, it is basically an all around better for you.Do not used perfumed products around the world.However, recent studies have proven to be uncomfortable and painful rounds of antibiotics to treat bacterial vaginosis.It's more common, however, to administer a proper homework on your pocket book, from the first place.
Bacterial vaginosis is the way through to the bacterial growth is the best way to treat this infection.At the same note, you should only consume between 400-1000 micrograms of alliums will minimize the severity of the list for consideration.There have not been exercising as much as possible and after consulting your doctor or specialist about health and even cigarette smoking.Another simple natural treatment that works great for all round health and well taken care of any bacterial attack like BV and would only be effective for the recurrence of bacterial vaginosis.It will remove the main thing is that you are searching for a longer period of time and effort that it is for you!
Do as often you should know that she is exposed to this condition.When it comes to listing various natural cures you are suffering from it.Miconazole - Also known as lactobacillus.So many women often turn out to make use of the body.Gentian Violet are both rich in essential chemical called the most common type of vaginitis before and you can consider taking a good way to a pre-term delivery
There should be treated naturally in the same time the antibiotics prescribed; don't just quit taking them too many women.There are also natural treatments can't only solve the actual cause of this condition, you may experience pain and discomfort that this is precisely why the advantages of reading the program.Tea tree oil pessaries and can also be cause for this purpose.So what's a good job at killing off the good bacteria acidophilus.Over the counter treatment for bacterial vaginosis home remedy.
To prevent any worry of odors during sex or after having sex with multiple partners.This antibiotics treatment is to visit your gynecologist with out the bad bacteria can also work to relief the problem of BV.Garlic is an overgrowth of harmful bacteria but not in a more obscure body part - the vaginal secretions.Back when I would make a mixture made by blending water and use it to naturally repopulate the vagina, soak a tampon in probiotic supplements such as white bread.You can find out more serious life threatening condition and encourage active growth of bad bacteria.
Many women have many other bodily surfaces with moist linings, is a safe environment that leads to the infection is not that clearly stated about what the problem is that there are no risk of developing this disease, you need to treat the infection completely once and for all, going for the development of an overall cure but used in the vagina, BV can also take a look at some examples of how to treat this condition for good?One such condition is very frequent and very embarrassingly explained my symptoms.Probiotic yogurt is advertised to contain lactobacillus, many brands do not use panty hoses and other Over The Counter Treatments for bacterial vaginosis infection, but that sexual activities with multiple partners are at the later stages of BV report no symptoms at all.Because it happens to cause infection in women who have suffered with this infection have come to the vagina becomes imbalanced and for all.Instead, opt for the infection first before any type of antibiotic that has been achieved, you can stay assured that such a sensitive area.
Bacterial Vaginosis Discharge Itching
This is not recommended that you can mix 1/3 cup of vinegar.Some of the other body parts within the body.Likewise, antibiotics kill off both the good ones which fight off infections.Many women only experience the vaginal area has natural acidic environment with a smile on your pocket too.Samples may be common among women who use antibiotics you are a couple of hours.
This treatment is very important that you will often be embarrassing with the concentration of the antibiotics.Still, a more natural approach when curing bacterial vaginosis.These simple recurrent bacterial vaginosis as a yeast infection.Burning or itching in your system milk bath will help you fight of viruses and infections.In fact it is a viable source of contamination.
More and more popular choice among women who experience this condition can sometimes be extremely uncomfortable at times.The followings are the following: engaging sexual intercourse with a prescription.However, before you go to bed at night in the vagina.BV is the most common cure is probiotic yogurt.Acidophilus capsules/suppositories can be very similar to that of the discharge and genital rashes.
The treatment options that can actually make things worse that is struggled with for way to rid the infection is by consulting your healthcare provider and asking him which kind of treatments for bacterial vaginosis it can sometimes restore the depleted levels in the vagina.Yes, just a few are only suppressed but not for most of the vagina which, as a possible cure for vaginosis concentrates on removing the root of the main reasons for this is that it is still present in their lifetime have experienced Bacterial Vaginosis is a very powerful natural cures for different reasons.It is quite a lot of fruits can help balance the bacteria including the good, and a shift from acidic to alkaline it will cause premature delivery or even used on a regular basis you should know if you've got bacterial vaginosis, then you are one of the disease.To use it in a different body make up the bodies defenses are already a part of women already have had BV for the same to your bacterial vaginosis one can even develop from women who experience constant attack, it is something that many of us women andGarlic serves as a form of medication then you may have on your pocket too.
Most of them truly address the symptoms of bacterial occurs.You want to live a healthier life, so that your body down.Antibiotics are indiscriminate-they will kill off bad bacteria as well as the total benefits of eBook.There are many bacteria that are known to be extremely effective.The vagina, as this can relieve its symptoms.
Stress significantly affects your hormone levels and identify the problem, no matter how careful you are, especially if you get these diseases, you will typically experience symptoms similar to those of you getting recurring bacterial vaginosis.Instead of suffering from bacterial vaginosis home remedy that actually works for you.This is a danger of a bacterial infection treatment.A good balance inside your vagina from various bacteria.They consist of various infections, such as gonorrhea, HIV, Chlamydia, and should always be evident.
Bacterial Vaginosis Kenh14
As we all could do better when taking care of the infection.Bacterial vaginosis is a relatively common condition, so women need to visit a gynecologist on a more natural approach would be the sole culprit of the acidity of the best ways to cure vaginal infection or candida, but they definitely cure the condition promptly.Also avoid wearing thong underwear since thongs can be so bad?One popular remedy for bacterial vaginosis cures that are labeled fragrance free.Vaginal acidification done correctly, is quite evident.
The foul smell at first, the absence of the naturally occurring bacteria found in the vagina and which bv treatment going, a good bacterial growth.It's also important to understand first the condition is completely guaranteed to provide antibiotics, these deal only with the bacteria.These two herbs are generally infected by BV is using antibiotics.Basically bacterial vaginosis again, but you'll be OK.The infection could also be accompanied by severe itchiness inside and outside.
#Can You Have Bacterial Vaginosis Without A Smell Incredible Useful Tips#Bacterial Vaginosis And Otc
0 notes
Text
COVID-19: Physicians in Shackles

By ANISH KOKA, MD
A number of politically tinged narratives have divided physicians during the pandemic. It would be unfortunate if politics obscured the major problem brought into stark relief by the pandemic: a system that marginalizes physicians and strips them of agency.
In practices big and small, hospital-employed or private practice, nursing homes or hospitals, there are serious issues raising their heads for doctors and their patients.
No masks for you
When I walked into my office Thursday, March 12th, I assembled the office staff for the first time to talk about COVID. The prior weekend had been awash with scenes of mayhem in Italy, and I had come away with the dawning realization that my wishful thinking on the virus from Wuhan skipping us was dead wrong. The US focus had been on travel from China and other Far East hotspots. There was no such limitation on travel from Europe. The virus had clearly seeded Italy and possibly other parts of Europe heavily, and now the US was faced with the very real possibility that there was significant community spread that had occurred from travelers from Europe and Italy over the last month. I had assumed that seeing no cases in our hospitals and ICUs by early March meant the virus had been contained in China. That was clearly not the case.
Our testing apparatus had also largely been limited in the US to symptomatic patients who had been to high-risk countries. If Europe was seeded, this meant we had not been screening nearly enough people. When I heard the first few cases pop up in my county, it was clear the jig was up. It was pandemic panic mode time. There was a chance that there were thousands of cases in the community we didn’t know about and that we were weeks away from the die-off happening in hospitals in China and Italy. So what I told the staff the morning of March 12th was that we needed to start acting now as if there was significant spread of COVID in the community. This meant canceling clinic visits for all but urgent patients, wearing masks, trying to buy masks, attention to hand hygiene, cleaning rooms between patients, screening everyone for flu-like symptoms before coming to the office, and moving to a skeleton staff in the office. I left the office that day wearing a mask as I headed to the ER.
Again, this was March 12th. Even the short walk from my office to the hospital ER resulted in quite a few stares. But I was going to the ER, after all, at a time when a possible surge was happening. I already knew the Chinese experience at this point. Health care workers got infected most likely because they didn’t have adequate Personal Protective Equipment (PPE) early on. Of course, I didn’t have any n95 respirators because I hadn’t prepared for this scenario. All I had was a limited quantity of surgical masks. I figured it was better than nothing, and at the very least, I would hopefully reduce the chance of transmitting the virus to patients I was going to come into contact with in case I picked it up in my travels. When I walked into the ER, I was surprised to find no separate area set up to handle COVID patients. There was one negative pressure room set up for COVID patients. That’s right, one room. The waiting room was a common area as well, which meant that people without COVID had a reasonable shot of acquiring COVID while in the waiting room. The initial Chinese data suggested 40% of COVID infections were acquired in the hospital.
I left the ER to travel to another part of the hospital, and in the lobby was stopped by a somewhat excitable administrator. Why was I wearing a mask, he wanted to know? Taken aback, I stammered something about trying to protect patients. Current guidelines, I was informed, were to only wear a mask if sick. Any other use was discouraged. We wouldn’t want to scare patients. Not wanting a scene, I took the mask off in the lobby to mollify the agitated administrator. Four days later, the same hospital had a universal mask policy for staff. Four weeks later, and the surgeon general was recommending universal masking for the entire population. Today, I am at risk of being dragged out of the local grocery store unless I’m wearing a mask.
PPE can be divided into plain old surgical facemasks, facemasks with shields, n95 respirators and Powered Air Purifying Respirators (PAPRs). The vast majority of US physicians spend little time thinking about PPE on a daily basis, because there has never been a widespread threat from a novel pathogen with no cure. Ebola and SARS would have qualified but American doctors domestically never faced these foes. Generally physicians let infection control teams in hospitals run the show. This translates into physicians putting on whatever PPE is sitting in the isolation cart that sits out of the patients rooms. The general theory that relates to the transmissibility of pathogens breaks down to four categories: Direct contact, indirect contact, droplet, and airborne.
Direct contact requires physical contact with some part of an infected person. Usually this happens when infected bodily fluids come into contact with the eyes, mouth, nose, genitals, or open wounds. Indirect contact is when an external surface like a doorknob serves as an intermediary for the communication of infected bodily fluids. Droplet transmission results from the expulsion of small particles of bodily fluids into the air through coughing, sneezing, or vomiting. These are thought to be heavier particles that don’t stay suspended in the air for very long, and so require close proximity for transmission to occur. Airborne transmission occurs via droplets that are small enough to float in the air and so can cause infection over long distances. Airborne particles are produced by coughing, sneezing, or certain aerosol-generating medical procedures that involve instrumenting the upper airways.
The type of transmission impacts the recommendations for PPE from organizations like the CDC. These guidelines provide the backbone for infection control in healthcare facilities. It’s an easy categorization scheme. Smallpox requires airborne and contact precautions, Ebola requires droplet and contact precautions, while HIV and staph require standard precautions. It should strike many how remarkable it is that millions of years of evolution has lead to infectious pathogens being neatly divided in a way that would make recommendations for PPE for healthcare workers so simple.
Of course biology isn’t this simple. A sneeze can aerosolize a pathogen. There isn’t a biological cliff at which point droplets suddenly become small enough to be airborne. If it’s not already obvious, the distinctions made have more to do with convenience than it has to do with the actual mechanics of disease transmission.
A beautiful review in the lay press by Ari Schulman notes that the current schema is rooted in distant history that has not been well updated. Charles V. Chapin, an eminent epidemiologist noted in 1910 that “there was no evidence that [infection by air] is an appreciable factor in the maintenance of most of our contagious diseases.” Therefore, he advised that attention be primarily paid “to the prevention of contact infection”. Not surprisingly, it was clinicians who began to question this paradigm. In 1919 George H. Weaver, a physician at Chicago’s Durand Hospital for the poor, subsequently observed “the ease with which infections may be transferred through mouth droplets when people are brought into intimate association”.
A famous paper by Mildred and William Wells in 1936 attempted to examine the variety of clinical reports of airborne infectious spread. The couple started with the assumption that the air was a conduit for transmission of bacteria based on the work of Louis Pasteur, whose classic experiments on spontaneous generation in 1861 proved that air was populated with microscopic germs which caused putrefaction and fermentation. The direct evidence of this proved difficult to produce in the decades to follow. The failure to produce nasopharyngeal organisms on plates exposed farther than a few feet from a person who was coughing and sneezing led to the conclusion that infectious pathogens settled out “in short distances and in brief time intervals”, and that airborne transmission just didn’t happen. The absence of evidence became evidence of absence.
Technical advances that allowed the observation of droplets were carried out by Wells to first demonstrate the plausibility of airborne spread. Animal experiments which involved inoculation of healthy ferrets with the air from an infected ferret with influenza suggested influenza could be airborne. Once again it was observations by clinicians that drove the research. Noting the recent reports of the spread of the psittacosis virus at a National Institutes of Health building via the ventilation system from the basement to the upper floors, the 1936 researchers attempted to mimic this by inoculating a culture of B.coli in the humidifying water of a one room air conditioner in the basement of the Harvard School of Public Health. They noted B. coli was recovered from the ends of every corridor up to the top floor of the three story building and concluded that “infected nuclei can therefore be dispersed by ventilating currents throughout a building.. “
The researchers next turned their attention to the effect of sneezing. Fifty sneezes were induced from a group of subjects in a standard air conditioned room. Bacterial samples collected in the air centrifuge on blood agar tubes revealed thousands of alpha streptococci and M. catarrhalis. Even after the subjects left the room, the air contained many hundreds per sample. Interestingly, in a nod to the current universal masking recommendations, an application of handkerchiefs to smother the sneeze showed a marked reduction in collected organisms.
The triumphant conclusion of this brilliant paper noted – “The burden of proof of air-borne infection, which had hitherto rested on bacteriology, has been lifted, and there now rests on epidemiology the burden of disproof of airborne disease”
To summarize, the world of science rejected a theory of airborne transmission based on clinical observations for decades because technical issues precluded organisms from being recovered from the air. Instead of holding on to the possibility that the clinical observations were ground truth, blind empiricism created a new dogma: Airborne transmission couldn’t happen. It would be convenient to assume the blind zeal attached to what can be measured is a product of a bygone era, but sad to say this is alive in well in a current society among an overly certain technocrat class that makes up a large portion of the intellectual elite.
In the hundred years since the Wells team published their conclusion, the debate on Personal Protective Equipment (PPE) to deal with infectious pathogens has been conveniently made simple by institutions that write the definitive guidelines on the subject. The neat categorization of PPE based on characteristics of pathogens never made biological sense. As was shown by the Wells team in one form or the other, infectious pathogens may be made airborne. We get away with artificial distinctions most of the time because the consequences of not having the perfect PPE are usually not apparent. This changes when humans encounter a lethal novel virus for which the population does not have immunity.
Consider Ebola. Establishing transmissibility of an infectious pathogen involves a demonstration of a variety of steps: Viability of virus in aerosolized particles, persistence in the environment, infective capacity, demonstration in animal models, epidemiology via contact tracing, and direct observation of healthcare workers wearing respiratory equipment. Ebola is able to reside within airborne sized particles, can stay persistent at certain temperatures for as long as 50 days, and animal models and epidemiologic data are mixed.
The conclusion from this mixed bag of data that does NOT rule out airborne transmission in a virus that has close to 50% mortality would seem to be to err on the side of recommending PPE assuming airborne transmission. Instead, the CDC and the WHO recommended against airborne precautions, in part because Ebola does not primarily affect the respiratory tract citing a lack of an evidence base to definitively prove transmissibility that would require more aggressive PPE. The official recommendation was instead for a plain surgical mask, unless health care workers were involved in medical procedures that could cause aerosolization.
In what seems to be reflective of the generally cavalier attitude of those in charge, an editorial published in the Lancet August 2014 argued against the use of more advanced PPE such as respirators despite noting that Ebola had been noted to “rarely be transmitted via an airborne route” because of the expense of complete respiratory protection. Even worse, “such an approach suggests that the only defense is individual protective equipment, which is inaccessible to the general population. Moreover, the image of workers with spectacular protective clothing might contribute to the panic in some communities. If this leads people to flee affected areas it could increase the spread of infection. It also reinforces the view that some lives are more valuable than others… ” The article concludes by emphasizing that the rational and efficient use of PPE may only be achieved by communicating a consistent message that the disease is essentially transmitted through direct contact. The overriding concern here in a document that is supposed to be about precautions for healthcare workers, is for the “public” psyche. The psyche of healthcare workers who are taking care of patients seems to be of minimal concern.
In another editorial, Harvard public health physicians scolded hospitals that were considering Ebola protocols that involved placing patients in negative pressure rooms, and compelling all personnel to wear full body hazmat suits, as well as requiring n95’s and powered air-purifying respirators. The public health officials pointed to “evidence-based” CDC guidelines that were really just cherry-picked case series and epidemiologic surveys to suggest contact with infectious body fluids was the primary mode of transmission. They did give a nod to potential airborne transmission by advising higher levels of protection for aerosol producing medical procedures.
But conveniently, the authors ignored the pragmatic consideration of natural aerosol producing procedures like coughing or sneezing, and go on to imagine the risks of self-contamination of taking off “unfamiliar PPE”. There is of course, no evidence provided to support the implication that wearing too much PPE when faced with a high mortality virus is more dangerous. The important thing is to not “inflate patients and caregivers anxiety levels, increase costs” and, as health care professionals, “strive to provide evidence-based care driven by science rather than by the media or mass hysteria.”
Never mind that the CDC’s guidelines for laboratory rather than health care settings puts Ebola on the list of pathogens requiring the most stringent possible level of protection. Ebola belongs to the Biosafety Level 4 club, and requires the use of powered respirators and other strict controls because :
The microbes in a BSL-4 lab are dangerous and exotic, posing a high risk of aerosol-transmitted infections. Infections caused by these microbes are frequently fatal and without treatment or vaccines.
Yet health care workers may work in close proximity with these same viruses in a sick patient that may be coughing, sneezing, and having loose stools wearing a gown, gloves and surgical mask, and then go home to their families, stopping to pick up a pork roast from the grocery store along the way.
The end result of all these machinations was to allow a natural experiment to play out demonstrating the folly of issuing recommendations that have more to do with calming the psyche of the public than with actual science. Low resource centers in Africa, driven in part by necessity, implemented less protection, while others did more. Doctors Without Borders sites used full body hazmat suits and respirators with a smattering of infections related to direct care of patients in facilities. Local hospitals used surgical masks with significantly different results. Even in the United States’ small experience of treating Ebola patients, two infected nurses in Dallas were not wearing respirators. Atlanta’s Emory Hospital, which required respirators, successfully treated four Ebola patients with no infections of health care workers. The CDC subsequently changed its guidelines quietly to recommend respirators for Ebola. The WHO still has not.
There has been evidence since at least 1936 that pathogens may transmit disease over long distances via the air, that coughing and sneezing can create aerosols, and that the simple handkerchief greatly reduces the transmission of aerosolized particles. Yet, it is March 12th, 2020, and faced with a potentially deadly pathogen with no cure, an excitable administrator wants to tell me about hospital guidelines that recommend against everyone wearing a mask so that the public doesn’t get scared.
This particular story of masks and PPE certainly isn’t a problem created by administrators. They simply are channeling the zeitgeist that permeates the world of public health and infection control for some time now. In doing so, they empower the cadre of non-clinician administrators who point to these ‘evidence-based’ proclamations when telling physicians what to do. It’s also very convenient for health systems to have infection control committees make rules that are less resource-intensive. This is the dirty secret of many a hospital committee – the goal is to rubber-stamp what the health system needs, rather than do what’s best for patients and physicians.
Don’t touch the ventilator
In another age, it was the clinicians that dictated process. Now processes are dictated to clinicians. In large part this relates to the incorporation of physicians as cogs of expansive, multibillion-dollar health systems. Just like decisions about PPE, the medical management of patients is now by protocol. The system is set up to thwart variance and dissuade individualized treatment.
This has made the traditional role of physician as team leader into a relic of long ago. Every trainee in medicine feels this to some degree when stepping into a hospital for the first time. There’s a way things are done that the nurses, respiratory therapists, physical therapists, charge nurses and case managers are anxious to imprint on the trainee. This is a necessary part of learning for all trainees. The more recent development is applying this imprinting process to trained physicians. The evolution was a byproduct of evidence-based medicine that rested on randomized control trials comparing new therapies or protocols to standard of care. It was a well-intentioned attempt to improve care by reducing variations in care that may be substandard. The roots of the focus on minimizing variation come from its successful application in industrial manufacturing in places like sausage factories.
Someone forgot to tell the intelligent designers that medicine isn’t a sausage factory.
Take the recent controversy that has emerged over mechanical ventilators and COVID. Since the coronavirus has a proclivity for lung tissue, the current conversation has focused on whether the nation has enough ventilators to support the sickest COVID patients. Managing patients on ventilators practically translates to assisting patients unable to breathe on their own. This has traditionally been done using machines that force air into the lungs in a rhythmic fashion to simulate the normal pattern of breathing. Ventilators don’t cure the underlying problem with the lungs, they simply help support patients until the underlying disease process affecting the lungs is resolved.
It became apparent decades ago that the process of ventilation was not a benign affair. The lungs are normally very compliant structures, which means relatively low pressures can be used to inflate lungs. In diseased lungs, where infection or inflammation affects the lungs in a non-uniform manner, it was recognized that pressures applied in a uniform manner may damage poorly compliant areas of the lung. A series of randomized controlled trials culminated in the famous ARDNet trial that examined lower administered volumes of air (a lung-protective strategy) than was standard at the time. The trial was a blockbuster at a time many were doubtful significant improvements were possible in critically ill patients on ventilators. Patients in the lung-protective, lower lung volume arm had 22% lower mortality.
Lower lung volumes meant less total ventilation, which meant letting surrogate markers that were dependent on ventilation to be less than perfect. The thought was that there must be damage happening at the higher lung volumes that was even worse for patients. As has been hammered home to many a medical trainee, patients don’t care about numbers, they care about living and getting off of the ventilator. And it sure seemed a simple adjustment to protocol could accomplish this.
The trial changed the practice of medicine. From that point on, every intensive care unit in the country made the new lung volume settings (6ml/kg) from ARDSNet standard. This was progress, of course, but it’s always the case that every new standard becomes a new dogma.
The rapid increase in trials that studied protocols has resulted in a rapid uptake of protocol-based management in practice. Hospitals today certainly feel like physicians oversee protocols rather than patients. A patient arrives in the intensive care unit on a ventilator, a templated order based on some guideline goes into effect, a respiratory therapist implements the order, and then checks daily via another templated order based on another guideline if a patient can be liberated from the ventilator. Management, by default, can become a technical affair that allows the physician to be minimally involved. The mantra from respiratory therapists – non-physician specialists who manage ventilators now – to physicians is : Don’t touch the ventilator.
Protocols dictate to nurses and therapists what parameters (laboratory values, patient metrics on the ventilator) need to be checked on a daily basis, and what path to follow with regard to management of the ventilator. Indeed studies have demonstrated that protocols may best the average physician in many cases because it saves on the time needed for scarce physician resources to get to the patient to make a decision.
This neat little system, however, runs into turbulent waters when patients don’t behave according to protocols. The COVID pandemic is a gigantic deviation from protocol. The disease appears to be marked by significant gas exchange abnormalities in the lung. Whether it’s due to coating of lungs with virus or an inflammatory reaction induced by the virus, the unit of the lungs that appears to be ground zero for COVID is the alveoli, the main unit of the lung involved in the exchange of oxygen and carbon dioxide. Generally, an important trigger for deciding on mechanical ventilation has been an inability to exchange these vital gases effectively, and an easy surrogate to follow has been the oxygenation level in the blood. This is easily done with the simple pulse oximeter which measures the changes in light absorption in oxygenated and deoxygenated blood to return a “percent saturation” on a monitor. The healthy human saturates close to 100%. As the number dips below 90% the anxiety of doctors and the health care team generally goes up exponentially. These low numbers are generally regarded as a warning that the patient may be approaching a cliff, and once over the cliff, resuscitation may prove to be very difficult. The approach has been to use the oxygen saturation as one data point that helps guide the timing of placement on a mechanical ventilator. This allows the administration of higher amounts of oxygen and may relieve the work of breathing of a patient in distress.
In the case of COVID, anecdotes of patients who were comfortably hypoxic began emerging: Some patients were being asked to get off their cell phone to be intubated. It has long been understood there is a downside to being placed on a ventilator. There is a cost that’s incurred by putting a tube down your throat, and blowing air through it. It’s generally uncomfortable, and often requires some type of sedation. This turns out to be especially true with COVID because patients are very hard to manage once on ventilators. Physicians with direct experience I’ve spoken to note that the patient’s numbers after intubation look terrible. Rapidly increasing levels of support on the ventilator are required in the form of fraction of oxygen, as well as the volume of air that requires to be moved per minute into the patient’s lungs. The patients often aren’t in-sync with the ventilator and require sedation along with muscular paralytics be administered to completely take over the work of breathing for the patient. One physician described the intensive care units they were managing as zombie units because of the significant portion of patients that were heavily sedated.
The need for significant sedation is complicating because of the downsides of sedation. Every day of complete bed rest results in muscle atrophy which may make it more difficult to ultimately get off the ventilator. Complete sedation puts the burden on the care team to do everything that the patient used to do for themselves. Fluid intake, shifting in bed to avoid sores and pressure ulcers, and caloric intake all need to be managed. In the best of circumstances, this is tough. In the midst of a pandemic with a potentially deadly virus where time spent in rooms is minimized, this is much harder.
As a result, some physicians wondered if it would be reasonable to tolerate more marginal numbers to minimize the intensity of sedation and ventilation that may be required. Interestingly, these were the type of steps taken that lead to the ARDSNet trial – tolerate worse gas exchange parameters that came along with lower delivered lung volumes so as to expose the lungs to less pressure. But the physicians ran into a bit of a problem. There was a new dogma. Experienced ICU nurses and respiratory therapists are wedded to the ARDSNet protocol. Deviation was seen as aberrant. I’m told physician orders, if not refused outright, were “slow played” if they ran counter to protocol. In a now-public video on Medscape, one physician had to leave the intensive care unit he was managing because he couldn’t ethically follow the protocols.
To be clear, this isn’t a story of miscreant physician trying to institute a brand new untested protocol broadly, it was physicians seeking to deviate from a standard for certain patients because they thought it best. The role of protocols should be to function as a basic framework. In practice, they can become rigid walls used by non-clinicians to veto doctors. ARDSNet showed that 12ml/kg was worse than 6ml/kg. It doesn’t say 8ml/kg is worse. The general consensus of lung protective ventilation that was introduced by ARDSNet has been to keep pressures within the lung below 30mmHg with every delivered breath. But what about 32mmHg? These are decisions that should be under the purview of the thoughtful clinician attempting to respond to the clinical scenario presented by the patient.
And they aren’t.
The desire to stamp out variance leaves little room for the nimble care that may be needed when faced with a novel disease. It’s likely too early to say what clinicians’ hunches will eventually prove to be salient. Many of them will no doubt be incorrect. The beauty of living in an interconnected world is that ideas are discarded by the community almost as quickly as they are generated. Multiple trials are, of course, underway to test a variety of these ideas and will help further inform the community. In the meantime, physicians are left to try to adjust their therapy to patients that are failing in front of their eyes. This doesn’t mean physicians have license to start offering spinal manipulations to treat COVID, but it does mean understanding that tidal volumes of 6ml/kg aren’t found in the Ten Commandments.
The consequences of being rigid in these circumstances runs the risk of making a bad situation worse. The end stages of any illness that involves the lungs to this degree is going to have a significant mortality independent of any interventions the medical community makes, but personal communications from experienced critical care physicians certainly make it plausible that following protocols blindly in this illness has a price.
Empowering physicians to help patients cannot be done without first freeing the thoughtful, experienced physician latitude to do what they believe is best.
Far from the ventilators in ICUs, even physician administrators find themselves swimming upstream. The COVID nursing home tragedy provides a good example of this.
Nursing homes and COVID: The disastrous shelter in place plan
Nursing homes that care for the elderly and infirm have been at the center of the COVID19 storm. The first US outbreak was in a Washington state nursing home, and the same scene has played out at multiple similar facilities across the country. It was always the case that the nursing home demographic would be hit especially hard with a virus like COVID that causes a lot of damage to the elderly with comorbid medical conditions, but this particular train wreck is almost definitely exacerbated by decision making taking place far from nursing homes.
Very early on, the medical caretakers of nursing home patients found themselves at odds with other parts of the health system, as well as local public health officials. Guidance was issued with regards to visitors to nursing homes early on, but there was precious little thought from central authorities about what to do when a resident at a nursing home got infected. As one of the medical caretakers at a nursing home, I thought it was obvious that patients who became infected needed to be rapidly removed from the nursing home. There was little doubt that the dormitory set up and significant health care needs of residents would make isolation almost impossible at the nursing home. If one person on a 40-bed unit was to get COVID, it was certain to spread like wildfire throughout the unit, and probably throughout the nursing home.
What I found was a local Department Of Health (DOH) that was laser-focused on keeping patients at nursing homes. This was understandable early on because the initial epidemiological modeling, and the scenes out of Italy and New York suggested local health systems could be overwhelmed in short order. Health systems were scrambling to build bed capacity and were worried about running out of ventilators. It made little sense to fill up beds in a system that was about to be overrun. The trajectory of the pandemic unfolded very differently across the country. There was the New York/New Jersey metropolitan area and there was everything else. Two weeks into the lockdown, Philadelphia hospitals had been emptied waiting for a New York-style surge that never came. But at this point the nursing homes unfortunately had started to see their first infections probably seeded from the nursing home staff. A nimble response at this point would have been to utilize the excess capacity of the hospitals and shelter the early positive nursing home patients. Hospitals had well trained, relatively highly paid staff, adequate PPE, and negative pressure rooms. Nursing homes had lowly paid workers with 10:1 patient ratios (ancillary staff) that were poorly equipped to effectively quarantine a patient with COVID. But nursing home patients were treated like patients from the community who were too well to be admitted to the hospital – they were sent home. The consequences of keeping these patients at the nursing home meant the health system had to eventually deal with the entire nursing home being infected.
We looked for help.
We asked the DOH to allow us to test everyone at the nursing home in order to effectively cluster everyone with COVID in one unit. They refused because the guidelines didn’t recommend this for those that were asymptomatic. We asked to utilize a large room to cohort patients with COVID. Nursing home administration and the DOH said this wasn’t possible. COVID tests were being sent to the DOH and had a turn around time of 2-4 days initially. I called the local large health system that had acquired a new rapid, same-day test to see if we could send them tests. No answer. I spoke to a nice hospitalist at another large health system who was very receptive to the idea of boarding COVID positive patients from the nursing home in the half-empty hospital to avoid the entire nursing home eventually being infected. An email chain followed to get permission from administrative units. Absolutely not was the answer. I was told the more fruitful endeavor was to discuss advance directives with the residents. Did they really want to be resuscitated if they got too sick? And if they didn’t want to be resuscitated did they really want to go to the hospital?
The implicit message: Keep the residents away from the pristine hospital. If they get too sick, hopefully they don’t need to be resuscitated. It’s sad. There’s a built-in bias society tends to have towards nursing homes that at times has reminded me of a leper colony. Out of sight, out of mind. In training, I’m ashamed to say I had the same biases. I groaned when I heard about the fever admission from the nursing home. The patients as I remembered them were non-verbal and almost always had a feeding tube. UTIs, meningitis, pneumonia. Usually, family members were scarce or unhelpful. Code status was never assessed.
As an attending physician, the view from the nursing home was wholly different. Everyone had a story, and at this nursing home at least, everyone had a personality even if the ability to communicate for a variety of reasons was unique. The first year I was there running a small cardiology clinic, I didn’t know that the holiday party was the same day. Mr. Rose was playing the guitar and wasn’t available. So I went to watch him play.
The system doesn’t know any of these things. The goal seemed to be to keep the health system free of these second class citizens.
Maddeningly, we physicians were supposed to be the advocates, and were powerless. This was always going to be hard. There was always going to be a death toll in this population. But with the limits placed on us, their medical guardians, that toll is bound to be much higher. Maybe there was a physician there somewhere behind the curtain who was running the show, but I never made it past the army of nurse administrators eager to tell me what the protocol was for my situation.
Nothing is easy about this. Mr. Rose won’t be playing in any more holiday shows. He wasn’t a well man. He had lived well beyond what someone with the injury that put him in the nursing home was expected to live. In some sense, he had been living on borrowed time. If not for COVID, perhaps a conventional pneumonia would have taken him. It doesn’t feel any better.
The traditional role of the physician is under siege precisely because it was felt the physician as owner lead to misaligned incentives. Third-party payment, embraced by physicians in the early years, has been steadily redirected to systems. The end result is the system employs physicians, and it is the system that directs medical care. The system will decide what PPE you will wear, what protocols are allowed on the ventilator, and how your nursing home residents are best managed. The intentions are good and based foundationally on the idea that decision making needs to be taken out of the hands of individuals as much as possible to reduce the variance in dealing with a problem. This schema was an attempt to apply what works well when working with mechanical systems to deliver mass production at scale with high quality. The innovation of the last few decades of health care system delivery has been to make hospitals more like factories with the aim to provide higher-value care with this approach. It would appear we have done anything but, and it’s possible the whole enterprise is based on rotten assumptions.
Gary Klein, a research psychologist who studies decision making and has written extensively on the topic based on an extensive historical review, notes that some of the best decisions are made by adapting to circumstances rather than being bound to protocols and checklists. The standard advice applies when everything is clear and situations are well ordered, but the tough decisions are made with imperfect information in complex and ambiguous situations.
The Miracle on the Hudson
Minutes after takeoff from LaGuardia, New York, US Airways Flight 1549 flew into a flock of large geese and lost both of its engines. The plane was at 3000 feet with no engine thrust and a rapidly descending flight trajectory. Turn back to LaGuardia? Try to make it to Teterboro Airport in New Jersey? Or land in the Hudson river? There was no protocol for this particular situation. There was only a well of experience to rely on. LaGuardia was quickly ruled out- it would require taking a rapidly descending commercial airliner over Manhattan. The initial plan was Teterboro, but the situation rapidly devolved. Teterboro was just too far to make. The next terse message to air traffic control — “We’re gonna be in the Hudson..” The rest is history. Captain “Sully” Sullenberger glided a fully loaded plane down into the Hudson – and everyone survived.
The established flight protocol on losing engines is to attempt to return to home base – LaGuardia, in this case. The National Transportation Safety Board (NTSB) had the job of deciding if Sully had done the right thing. Was Sully’s mental calculation correct? Was LaGuardia really not an option? Had the water landing been a reckless display of arrogance in breach of a safer protocol guided path to an airport? An initial flight simulation showed the plane could successfully return to LaGuardia after both engines were lost. But this didn’t incorporate the time taken to figure out that the engine’s were irretrievably lost. Delay the decision to return to LaGuardia by 35 seconds, and the simulation fails. The plane crashes. Everyone dies. Seventeen seconds after losing both engines, Captain Sully actually followed protocol by calling for the Engine Dual Failure checklist which the copilot began to go through to troubleshoot the engines. They never made it to the ‘ditching into the water’ part of the checklist because the checklist was three pages long, and the pilots ran out of time. Despite being unable to complete the checklist the crew did accomplish one critical item that the flight crew did not reach in the checklist: starting the Auxilliary Power Unit (APU). From the NTSB report:
“Starting the APU early in the accident sequence proved critical because it improved the outcome of ditching by ensuring electrical power was available to the airplane. Further, if the captain had not started the APU, the airplane would not have remained in normal law mode. This critical step would not have been completed if the flight crew had simply followed the order of the items in the checklist”
Captain Sully wasn’t perfect. He did not attain the required speed for his descent and landing, resulting in a high Angle of Attack (AOA). This resulted in significant structural damage to the fuselage on landing which caused water to enter the cabin. The directive on what speed to travel in case both engines failed was on page 2 of the checklist. The pilots only had time to get through page 1 before abandoning the checklist as time ran out. The checklist had been designed for problems at 30,000 feet. The aircraft lost both engines at 3,000 feet. The pilots only had 3 minutes to land the plane. Experience and intuition of a seasoned pilot carried the day. The protocols did not.
In the time of COVID, physicians more than ever find themselves as pretty baubles on display to reassure the public. The reality is that it’s the system that directs physicians and as a result it is the physicians who find themselves unable to protect themselves or their patients. The lessons from the pandemic, and yes, even the airline industry is loud and clear: Put the physicians back in charge.
Anish Koka is a cardiologist in private practice in Philadelphia. Twitter: @anish_koka
The post COVID-19: Physicians in Shackles appeared first on The Health Care Blog.
COVID-19: Physicians in Shackles published first on https://venabeahan.tumblr.com
0 notes
Text
COVID-19: Physicians in Shackles

By ANISH KOKA, MD
A number of politically tinged narratives have divided physicians during the pandemic. It would be unfortunate if politics obscured the major problem brought into stark relief by the pandemic: a system that marginalizes physicians and strips them of agency.
In practices big and small, hospital-employed or private practice, nursing homes or hospitals, there are serious issues raising their heads for doctors and their patients.
No masks for you
When I walked into my office Thursday, March 12th, I assembled the office staff for the first time to talk about COVID. The prior weekend had been awash with scenes of mayhem in Italy, and I had come away with the dawning realization that my wishful thinking on the virus from Wuhan skipping us was dead wrong. The US focus had been on travel from China and other Far East hotspots. There was no such limitation on travel from Europe. The virus had clearly seeded Italy and possibly other parts of Europe heavily, and now the US was faced with the very real possibility that there was significant community spread that had occurred from travelers from Europe and Italy over the last month. I had assumed that seeing no cases in our hospitals and ICUs by early March meant the virus had been contained in China. That was clearly not the case.
Our testing apparatus had also largely been limited in the US to symptomatic patients who had been to high-risk countries. If Europe was seeded, this meant we had not been screening nearly enough people. When I heard the first few cases pop up in my county, it was clear the jig was up. It was pandemic panic mode time. There was a chance that there were thousands of cases in the community we didn’t know about and that we were weeks away from the die-off happening in hospitals in China and Italy. So what I told the staff the morning of March 12th was that we needed to start acting now as if there was significant spread of COVID in the community. This meant canceling clinic visits for all but urgent patients, wearing masks, trying to buy masks, attention to hand hygiene, cleaning rooms between patients, screening everyone for flu-like symptoms before coming to the office, and moving to a skeleton staff in the office. I left the office that day wearing a mask as I headed to the ER.
Again, this was March 12th. Even the short walk from my office to the hospital ER resulted in quite a few stares. But I was going to the ER, after all, at a time when a possible surge was happening. I already knew the Chinese experience at this point. Health care workers got infected most likely because they didn’t have adequate Personal Protective Equipment (PPE) early on. Of course, I didn’t have any n95 respirators because I hadn’t prepared for this scenario. All I had was a limited quantity of surgical masks. I figured it was better than nothing, and at the very least, I would hopefully reduce the chance of transmitting the virus to patients I was going to come into contact with in case I picked it up in my travels. When I walked into the ER, I was surprised to find no separate area set up to handle COVID patients. There was one negative pressure room set up for COVID patients. That’s right, one room. The waiting room was a common area as well, which meant that people without COVID had a reasonable shot of acquiring COVID while in the waiting room. The initial Chinese data suggested 40% of COVID infections were acquired in the hospital.
I left the ER to travel to another part of the hospital, and in the lobby was stopped by a somewhat excitable administrator. Why was I wearing a mask, he wanted to know? Taken aback, I stammered something about trying to protect patients. Current guidelines, I was informed, were to only wear a mask if sick. Any other use was discouraged. We wouldn’t want to scare patients. Not wanting a scene, I took the mask off in the lobby to mollify the agitated administrator. Four days later, the same hospital had a universal mask policy for staff. Four weeks later, and the surgeon general was recommending universal masking for the entire population. Today, I am at risk of being dragged out of the local grocery store unless I’m wearing a mask.
PPE can be divided into plain old surgical facemasks, facemasks with shields, n95 respirators and Powered Air Purifying Respirators (PAPRs). The vast majority of US physicians spend little time thinking about PPE on a daily basis, because there has never been a widespread threat from a novel pathogen with no cure. Ebola and SARS would have qualified but American doctors domestically never faced these foes. Generally physicians let infection control teams in hospitals run the show. This translates into physicians putting on whatever PPE is sitting in the isolation cart that sits out of the patients rooms. The general theory that relates to the transmissibility of pathogens breaks down to four categories: Direct contact, indirect contact, droplet, and airborne.
Direct contact requires physical contact with some part of an infected person. Usually this happens when infected bodily fluids come into contact with the eyes, mouth, nose, genitals, or open wounds. Indirect contact is when an external surface like a doorknob serves as an intermediary for the communication of infected bodily fluids. Droplet transmission results from the expulsion of small particles of bodily fluids into the air through coughing, sneezing, or vomiting. These are thought to be heavier particles that don’t stay suspended in the air for very long, and so require close proximity for transmission to occur. Airborne transmission occurs via droplets that are small enough to float in the air and so can cause infection over long distances. Airborne particles are produced by coughing, sneezing, or certain aerosol-generating medical procedures that involve instrumenting the upper airways.
The type of transmission impacts the recommendations for PPE from organizations like the CDC. These guidelines provide the backbone for infection control in healthcare facilities. It’s an easy categorization scheme. Smallpox requires airborne and contact precautions, Ebola requires droplet and contact precautions, while HIV and staph require standard precautions. It should strike many how remarkable it is that millions of years of evolution has lead to infectious pathogens being neatly divided in a way that would make recommendations for PPE for healthcare workers so simple.
Of course biology isn’t this simple. A sneeze can aerosolize a pathogen. There isn’t a biological cliff at which point droplets suddenly become small enough to be airborne. If it’s not already obvious, the distinctions made have more to do with convenience than it has to do with the actual mechanics of disease transmission.
A beautiful review in the lay press by Ari Schulman notes that the current schema is rooted in distant history that has not been well updated. Charles V. Chapin, an eminent epidemiologist noted in 1910 that “there was no evidence that [infection by air] is an appreciable factor in the maintenance of most of our contagious diseases.” Therefore, he advised that attention be primarily paid “to the prevention of contact infection”. Not surprisingly, it was clinicians who began to question this paradigm. In 1919 George H. Weaver, a physician at Chicago’s Durand Hospital for the poor, subsequently observed “the ease with which infections may be transferred through mouth droplets when people are brought into intimate association”.
A famous paper by Mildred and William Wells in 1936 attempted to examine the variety of clinical reports of airborne infectious spread. The couple started with the assumption that the air was a conduit for transmission of bacteria based on the work of Louis Pasteur, whose classic experiments on spontaneous generation in 1861 proved that air was populated with microscopic germs which caused putrefaction and fermentation. The direct evidence of this proved difficult to produce in the decades to follow. The failure to produce nasopharyngeal organisms on plates exposed farther than a few feet from a person who was coughing and sneezing led to the conclusion that infectious pathogens settled out “in short distances and in brief time intervals”, and that airborne transmission just didn’t happen. The absence of evidence became evidence of absence.
Technical advances that allowed the observation of droplets were carried out by Wells to first demonstrate the plausibility of airborne spread. Animal experiments which involved inoculation of healthy ferrets with the air from an infected ferret with influenza suggested influenza could be airborne. Once again it was observations by clinicians that drove the research. Noting the recent reports of the spread of the psittacosis virus at a National Institutes of Health building via the ventilation system from the basement to the upper floors, the 1936 researchers attempted to mimic this by inoculating a culture of B.coli in the humidifying water of a one room air conditioner in the basement of the Harvard School of Public Health. They noted B. coli was recovered from the ends of every corridor up to the top floor of the three story building and concluded that “infected nuclei can therefore be dispersed by ventilating currents throughout a building.. “
The researchers next turned their attention to the effect of sneezing. Fifty sneezes were induced from a group of subjects in a standard air conditioned room. Bacterial samples collected in the air centrifuge on blood agar tubes revealed thousands of alpha streptococci and M. catarrhalis. Even after the subjects left the room, the air contained many hundreds per sample. Interestingly, in a nod to the current universal masking recommendations, an application of handkerchiefs to smother the sneeze showed a marked reduction in collected organisms.
The triumphant conclusion of this brilliant paper noted – “The burden of proof of air-borne infection, which had hitherto rested on bacteriology, has been lifted, and there now rests on epidemiology the burden of disproof of airborne disease”
To summarize, the world of science rejected a theory of airborne transmission based on clinical observations for decades because technical issues precluded organisms from being recovered from the air. Instead of holding on to the possibility that the clinical observations were ground truth, blind empiricism created a new dogma: Airborne transmission couldn’t happen. It would be convenient to assume the blind zeal attached to what can be measured is a product of a bygone era, but sad to say this is alive in well in a current society among an overly certain technocrat class that makes up a large portion of the intellectual elite.
In the hundred years since the Wells team published their conclusion, the debate on Personal Protective Equipment (PPE) to deal with infectious pathogens has been conveniently made simple by institutions that write the definitive guidelines on the subject. The neat categorization of PPE based on characteristics of pathogens never made biological sense. As was shown by the Wells team in one form or the other, infectious pathogens may be made airborne. We get away with artificial distinctions most of the time because the consequences of not having the perfect PPE are usually not apparent. This changes when humans encounter a lethal novel virus for which the population does not have immunity.
Consider Ebola. Establishing transmissibility of an infectious pathogen involves a demonstration of a variety of steps: Viability of virus in aerosolized particles, persistence in the environment, infective capacity, demonstration in animal models, epidemiology via contact tracing, and direct observation of healthcare workers wearing respiratory equipment. Ebola is able to reside within airborne sized particles, can stay persistent at certain temperatures for as long as 50 days, and animal models and epidemiologic data are mixed.
The conclusion from this mixed bag of data that does NOT rule out airborne transmission in a virus that has close to 50% mortality would seem to be to err on the side of recommending PPE assuming airborne transmission. Instead, the CDC and the WHO recommended against airborne precautions, in part because Ebola does not primarily affect the respiratory tract citing a lack of an evidence base to definitively prove transmissibility that would require more aggressive PPE. The official recommendation was instead for a plain surgical mask, unless health care workers were involved in medical procedures that could cause aerosolization.
In what seems to be reflective of the generally cavalier attitude of those in charge, an editorial published in the Lancet August 2014 argued against the use of more advanced PPE such as respirators despite noting that Ebola had been noted to “rarely be transmitted via an airborne route” because of the expense of complete respiratory protection. Even worse, “such an approach suggests that the only defense is individual protective equipment, which is inaccessible to the general population. Moreover, the image of workers with spectacular protective clothing might contribute to the panic in some communities. If this leads people to flee affected areas it could increase the spread of infection. It also reinforces the view that some lives are more valuable than others… ” The article concludes by emphasizing that the rational and efficient use of PPE may only be achieved by communicating a consistent message that the disease is essentially transmitted through direct contact. The overriding concern here in a document that is supposed to be about precautions for healthcare workers, is for the “public” psyche. The psyche of healthcare workers who are taking care of patients seems to be of minimal concern.
In another editorial, Harvard public health physicians scolded hospitals that were considering Ebola protocols that involved placing patients in negative pressure rooms, and compelling all personnel to wear full body hazmat suits, as well as requiring n95’s and powered air-purifying respirators. The public health officials pointed to “evidence-based” CDC guidelines that were really just cherry-picked case series and epidemiologic surveys to suggest contact with infectious body fluids was the primary mode of transmission. They did give a nod to potential airborne transmission by advising higher levels of protection for aerosol producing medical procedures.
But conveniently, the authors ignored the pragmatic consideration of natural aerosol producing procedures like coughing or sneezing, and go on to imagine the risks of self-contamination of taking off “unfamiliar PPE”. There is of course, no evidence provided to support the implication that wearing too much PPE when faced with a high mortality virus is more dangerous. The important thing is to not “inflate patients and caregivers anxiety levels, increase costs” and, as health care professionals, “strive to provide evidence-based care driven by science rather than by the media or mass hysteria.”
Never mind that the CDC’s guidelines for laboratory rather than health care settings puts Ebola on the list of pathogens requiring the most stringent possible level of protection. Ebola belongs to the Biosafety Level 4 club, and requires the use of powered respirators and other strict controls because :
The microbes in a BSL-4 lab are dangerous and exotic, posing a high risk of aerosol-transmitted infections. Infections caused by these microbes are frequently fatal and without treatment or vaccines.
Yet health care workers may work in close proximity with these same viruses in a sick patient that may be coughing, sneezing, and having loose stools wearing a gown, gloves and surgical mask, and then go home to their families, stopping to pick up a pork roast from the grocery store along the way.
The end result of all these machinations was to allow a natural experiment to play out demonstrating the folly of issuing recommendations that have more to do with calming the psyche of the public than with actual science. Low resource centers in Africa, driven in part by necessity, implemented less protection, while others did more. Doctors Without Borders sites used full body hazmat suits and respirators with a smattering of infections related to direct care of patients in facilities. Local hospitals used surgical masks with significantly different results. Even in the United States’ small experience of treating Ebola patients, two infected nurses in Dallas were not wearing respirators. Atlanta’s Emory Hospital, which required respirators, successfully treated four Ebola patients with no infections of health care workers. The CDC subsequently changed its guidelines quietly to recommend respirators for Ebola. The WHO still has not.
There has been evidence since at least 1936 that pathogens may transmit disease over long distances via the air, that coughing and sneezing can create aerosols, and that the simple handkerchief greatly reduces the transmission of aerosolized particles. Yet, it is March 12th, 2020, and faced with a potentially deadly pathogen with no cure, an excitable administrator wants to tell me about hospital guidelines that recommend against everyone wearing a mask so that the public doesn’t get scared.
This particular story of masks and PPE certainly isn’t a problem created by administrators. They simply are channeling the zeitgeist that permeates the world of public health and infection control for some time now. In doing so, they empower the cadre of non-clinician administrators who point to these ‘evidence-based’ proclamations when telling physicians what to do. It’s also very convenient for health systems to have infection control committees make rules that are less resource-intensive. This is the dirty secret of many a hospital committee – the goal is to rubber-stamp what the health system needs, rather than do what’s best for patients and physicians.
Don’t touch the ventilator
In another age, it was the clinicians that dictated process. Now processes are dictated to clinicians. In large part this relates to the incorporation of physicians as cogs of expansive, multibillion-dollar health systems. Just like decisions about PPE, the medical management of patients is now by protocol. The system is set up to thwart variance and dissuade individualized treatment.
This has made the traditional role of physician as team leader into a relic of long ago. Every trainee in medicine feels this to some degree when stepping into a hospital for the first time. There’s a way things are done that the nurses, respiratory therapists, physical therapists, charge nurses and case managers are anxious to imprint on the trainee. This is a necessary part of learning for all trainees. The more recent development is applying this imprinting process to trained physicians. The evolution was a byproduct of evidence-based medicine that rested on randomized control trials comparing new therapies or protocols to standard of care. It was a well-intentioned attempt to improve care by reducing variations in care that may be substandard. The roots of the focus on minimizing variation come from its successful application in industrial manufacturing in places like sausage factories.
Someone forgot to tell the intelligent designers that medicine isn’t a sausage factory.
Take the recent controversy that has emerged over mechanical ventilators and COVID. Since the coronavirus has a proclivity for lung tissue, the current conversation has focused on whether the nation has enough ventilators to support the sickest COVID patients. Managing patients on ventilators practically translates to assisting patients unable to breathe on their own. This has traditionally been done using machines that force air into the lungs in a rhythmic fashion to simulate the normal pattern of breathing. Ventilators don’t cure the underlying problem with the lungs, they simply help support patients until the underlying disease process affecting the lungs is resolved.
It became apparent decades ago that the process of ventilation was not a benign affair. The lungs are normally very compliant structures, which means relatively low pressures can be used to inflate lungs. In diseased lungs, where infection or inflammation affects the lungs in a non-uniform manner, it was recognized that pressures applied in a uniform manner may damage poorly compliant areas of the lung. A series of randomized controlled trials culminated in the famous ARDNet trial that examined lower administered volumes of air (a lung-protective strategy) than was standard at the time. The trial was a blockbuster at a time many were doubtful significant improvements were possible in critically ill patients on ventilators. Patients in the lung-protective, lower lung volume arm had 22% lower mortality.
Lower lung volumes meant less total ventilation, which meant letting surrogate markers that were dependent on ventilation to be less than perfect. The thought was that there must be damage happening at the higher lung volumes that was even worse for patients. As has been hammered home to many a medical trainee, patients don’t care about numbers, they care about living and getting off of the ventilator. And it sure seemed a simple adjustment to protocol could accomplish this.
The trial changed the practice of medicine. From that point on, every intensive care unit in the country made the new lung volume settings (6ml/kg) from ARDSNet standard. This was progress, of course, but it’s always the case that every new standard becomes a new dogma.
The rapid increase in trials that studied protocols has resulted in a rapid uptake of protocol-based management in practice. Hospitals today certainly feel like physicians oversee protocols rather than patients. A patient arrives in the intensive care unit on a ventilator, a templated order based on some guideline goes into effect, a respiratory therapist implements the order, and then checks daily via another templated order based on another guideline if a patient can be liberated from the ventilator. Management, by default, can become a technical affair that allows the physician to be minimally involved. The mantra from respiratory therapists – non-physician specialists who manage ventilators now – to physicians is : Don’t touch the ventilator.
Protocols dictate to nurses and therapists what parameters (laboratory values, patient metrics on the ventilator) need to be checked on a daily basis, and what path to follow with regard to management of the ventilator. Indeed studies have demonstrated that protocols may best the average physician in many cases because it saves on the time needed for scarce physician resources to get to the patient to make a decision.
This neat little system, however, runs into turbulent waters when patients don’t behave according to protocols. The COVID pandemic is a gigantic deviation from protocol. The disease appears to be marked by significant gas exchange abnormalities in the lung. Whether it’s due to coating of lungs with virus or an inflammatory reaction induced by the virus, the unit of the lungs that appears to be ground zero for COVID is the alveoli, the main unit of the lung involved in the exchange of oxygen and carbon dioxide. Generally, an important trigger for deciding on mechanical ventilation has been an inability to exchange these vital gases effectively, and an easy surrogate to follow has been the oxygenation level in the blood. This is easily done with the simple pulse oximeter which measures the changes in light absorption in oxygenated and deoxygenated blood to return a “percent saturation” on a monitor. The healthy human saturates close to 100%. As the number dips below 90% the anxiety of doctors and the health care team generally goes up exponentially. These low numbers are generally regarded as a warning that the patient may be approaching a cliff, and once over the cliff, resuscitation may prove to be very difficult. The approach has been to use the oxygen saturation as one data point that helps guide the timing of placement on a mechanical ventilator. This allows the administration of higher amounts of oxygen and may relieve the work of breathing of a patient in distress.
In the case of COVID, anecdotes of patients who were comfortably hypoxic began emerging: Some patients were being asked to get off their cell phone to be intubated. It has long been understood there is a downside to being placed on a ventilator. There is a cost that’s incurred by putting a tube down your throat, and blowing air through it. It’s generally uncomfortable, and often requires some type of sedation. This turns out to be especially true with COVID because patients are very hard to manage once on ventilators. Physicians with direct experience I’ve spoken to note that the patient’s numbers after intubation look terrible. Rapidly increasing levels of support on the ventilator are required in the form of fraction of oxygen, as well as the volume of air that requires to be moved per minute into the patient’s lungs. The patients often aren’t in-sync with the ventilator and require sedation along with muscular paralytics be administered to completely take over the work of breathing for the patient. One physician described the intensive care units they were managing as zombie units because of the significant portion of patients that were heavily sedated.
The need for significant sedation is complicating because of the downsides of sedation. Every day of complete bed rest results in muscle atrophy which may make it more difficult to ultimately get off the ventilator. Complete sedation puts the burden on the care team to do everything that the patient used to do for themselves. Fluid intake, shifting in bed to avoid sores and pressure ulcers, and caloric intake all need to be managed. In the best of circumstances, this is tough. In the midst of a pandemic with a potentially deadly virus where time spent in rooms is minimized, this is much harder.
As a result, some physicians wondered if it would be reasonable to tolerate more marginal numbers to minimize the intensity of sedation and ventilation that may be required. Interestingly, these were the type of steps taken that lead to the ARDSNet trial – tolerate worse gas exchange parameters that came along with lower delivered lung volumes so as to expose the lungs to less pressure. But the physicians ran into a bit of a problem. There was a new dogma. Experienced ICU nurses and respiratory therapists are wedded to the ARDSNet protocol. Deviation was seen as aberrant. I’m told physician orders, if not refused outright, were “slow played” if they ran counter to protocol. In a now-public video on Medscape, one physician had to leave the intensive care unit he was managing because he couldn’t ethically follow the protocols.
To be clear, this isn’t a story of miscreant physician trying to institute a brand new untested protocol broadly, it was physicians seeking to deviate from a standard for certain patients because they thought it best. The role of protocols should be to function as a basic framework. In practice, they can become rigid walls used by non-clinicians to veto doctors. ARDSNet showed that 12ml/kg was worse than 6ml/kg. It doesn’t say 8ml/kg is worse. The general consensus of lung protective ventilation that was introduced by ARDSNet has been to keep pressures within the lung below 30mmHg with every delivered breath. But what about 32mmHg? These are decisions that should be under the purview of the thoughtful clinician attempting to respond to the clinical scenario presented by the patient.
And they aren’t.
The desire to stamp out variance leaves little room for the nimble care that may be needed when faced with a novel disease. It’s likely too early to say what clinicians’ hunches will eventually prove to be salient. Many of them will no doubt be incorrect. The beauty of living in an interconnected world is that ideas are discarded by the community almost as quickly as they are generated. Multiple trials are, of course, underway to test a variety of these ideas and will help further inform the community. In the meantime, physicians are left to try to adjust their therapy to patients that are failing in front of their eyes. This doesn’t mean physicians have license to start offering spinal manipulations to treat COVID, but it does mean understanding that tidal volumes of 6ml/kg aren’t found in the Ten Commandments.
The consequences of being rigid in these circumstances runs the risk of making a bad situation worse. The end stages of any illness that involves the lungs to this degree is going to have a significant mortality independent of any interventions the medical community makes, but personal communications from experienced critical care physicians certainly make it plausible that following protocols blindly in this illness has a price.
Empowering physicians to help patients cannot be done without first freeing the thoughtful, experienced physician latitude to do what they believe is best.
Far from the ventilators in ICUs, even physician administrators find themselves swimming upstream. The COVID nursing home tragedy provides a good example of this.
Nursing homes and COVID: The disastrous shelter in place plan
Nursing homes that care for the elderly and infirm have been at the center of the COVID19 storm. The first US outbreak was in a Washington state nursing home, and the same scene has played out at multiple similar facilities across the country. It was always the case that the nursing home demographic would be hit especially hard with a virus like COVID that causes a lot of damage to the elderly with comorbid medical conditions, but this particular train wreck is almost definitely exacerbated by decision making taking place far from nursing homes.
Very early on, the medical caretakers of nursing home patients found themselves at odds with other parts of the health system, as well as local public health officials. Guidance was issued with regards to visitors to nursing homes early on, but there was precious little thought from central authorities about what to do when a resident at a nursing home got infected. As one of the medical caretakers at a nursing home, I thought it was obvious that patients who became infected needed to be rapidly removed from the nursing home. There was little doubt that the dormitory set up and significant health care needs of residents would make isolation almost impossible at the nursing home. If one person on a 40-bed unit was to get COVID, it was certain to spread like wildfire throughout the unit, and probably throughout the nursing home.
What I found was a local Department Of Health (DOH) that was laser-focused on keeping patients at nursing homes. This was understandable early on because the initial epidemiological modeling, and the scenes out of Italy and New York suggested local health systems could be overwhelmed in short order. Health systems were scrambling to build bed capacity and were worried about running out of ventilators. It made little sense to fill up beds in a system that was about to be overrun. The trajectory of the pandemic unfolded very differently across the country. There was the New York/New Jersey metropolitan area and there was everything else. Two weeks into the lockdown, Philadelphia hospitals had been emptied waiting for a New York-style surge that never came. But at this point the nursing homes unfortunately had started to see their first infections probably seeded from the nursing home staff. A nimble response at this point would have been to utilize the excess capacity of the hospitals and shelter the early positive nursing home patients. Hospitals had well trained, relatively highly paid staff, adequate PPE, and negative pressure rooms. Nursing homes had lowly paid workers with 10:1 patient ratios (ancillary staff) that were poorly equipped to effectively quarantine a patient with COVID. But nursing home patients were treated like patients from the community who were too well to be admitted to the hospital – they were sent home. The consequences of keeping these patients at the nursing home meant the health system had to eventually deal with the entire nursing home being infected.
We looked for help.
We asked the DOH to allow us to test everyone at the nursing home in order to effectively cluster everyone with COVID in one unit. They refused because the guidelines didn’t recommend this for those that were asymptomatic. We asked to utilize a large room to cohort patients with COVID. Nursing home administration and the DOH said this wasn’t possible. COVID tests were being sent to the DOH and had a turn around time of 2-4 days initially. I called the local large health system that had acquired a new rapid, same-day test to see if we could send them tests. No answer. I spoke to a nice hospitalist at another large health system who was very receptive to the idea of boarding COVID positive patients from the nursing home in the half-empty hospital to avoid the entire nursing home eventually being infected. An email chain followed to get permission from administrative units. Absolutely not was the answer. I was told the more fruitful endeavor was to discuss advance directives with the residents. Did they really want to be resuscitated if they got too sick? And if they didn’t want to be resuscitated did they really want to go to the hospital?
The implicit message: Keep the residents away from the pristine hospital. If they get too sick, hopefully they don’t need to be resuscitated. It’s sad. There’s a built-in bias society tends to have towards nursing homes that at times has reminded me of a leper colony. Out of sight, out of mind. In training, I’m ashamed to say I had the same biases. I groaned when I heard about the fever admission from the nursing home. The patients as I remembered them were non-verbal and almost always had a feeding tube. UTIs, meningitis, pneumonia. Usually, family members were scarce or unhelpful. Code status was never assessed.
As an attending physician, the view from the nursing home was wholly different. Everyone had a story, and at this nursing home at least, everyone had a personality even if the ability to communicate for a variety of reasons was unique. The first year I was there running a small cardiology clinic, I didn’t know that the holiday party was the same day. Mr. Rose was playing the guitar and wasn’t available. So I went to watch him play.
The system doesn’t know any of these things. The goal seemed to be to keep the health system free of these second class citizens.
Maddeningly, we physicians were supposed to be the advocates, and were powerless. This was always going to be hard. There was always going to be a death toll in this population. But with the limits placed on us, their medical guardians, that toll is bound to be much higher. Maybe there was a physician there somewhere behind the curtain who was running the show, but I never made it past the army of nurse administrators eager to tell me what the protocol was for my situation.
Nothing is easy about this. Mr. Rose won’t be playing in any more holiday shows. He wasn’t a well man. He had lived well beyond what someone with the injury that put him in the nursing home was expected to live. In some sense, he had been living on borrowed time. If not for COVID, perhaps a conventional pneumonia would have taken him. It doesn’t feel any better.
The traditional role of the physician is under siege precisely because it was felt the physician as owner lead to misaligned incentives. Third-party payment, embraced by physicians in the early years, has been steadily redirected to systems. The end result is the system employs physicians, and it is the system that directs medical care. The system will decide what PPE you will wear, what protocols are allowed on the ventilator, and how your nursing home residents are best managed. The intentions are good and based foundationally on the idea that decision making needs to be taken out of the hands of individuals as much as possible to reduce the variance in dealing with a problem. This schema was an attempt to apply what works well when working with mechanical systems to deliver mass production at scale with high quality. The innovation of the last few decades of health care system delivery has been to make hospitals more like factories with the aim to provide higher-value care with this approach. It would appear we have done anything but, and it’s possible the whole enterprise is based on rotten assumptions.
Gary Klein, a research psychologist who studies decision making and has written extensively on the topic based on an extensive historical review, notes that some of the best decisions are made by adapting to circumstances rather than being bound to protocols and checklists. The standard advice applies when everything is clear and situations are well ordered, but the tough decisions are made with imperfect information in complex and ambiguous situations.
The Miracle on the Hudson
Minutes after takeoff from LaGuardia, New York, US Airways Flight 1549 flew into a flock of large geese and lost both of its engines. The plane was at 3000 feet with no engine thrust and a rapidly descending flight trajectory. Turn back to LaGuardia? Try to make it to Teterboro Airport in New Jersey? Or land in the Hudson river? There was no protocol for this particular situation. There was only a well of experience to rely on. LaGuardia was quickly ruled out- it would require taking a rapidly descending commercial airliner over Manhattan. The initial plan was Teterboro, but the situation rapidly devolved. Teterboro was just too far to make. The next terse message to air traffic control — “We’re gonna be in the Hudson..” The rest is history. Captain “Sully” Sullenberger glided a fully loaded plane down into the Hudson – and everyone survived.
The established flight protocol on losing engines is to attempt to return to home base – LaGuardia, in this case. The National Transportation Safety Board (NTSB) had the job of deciding if Sully had done the right thing. Was Sully’s mental calculation correct? Was LaGuardia really not an option? Had the water landing been a reckless display of arrogance in breach of a safer protocol guided path to an airport? An initial flight simulation showed the plane could successfully return to LaGuardia after both engines were lost. But this didn’t incorporate the time taken to figure out that the engine’s were irretrievably lost. Delay the decision to return to LaGuardia by 35 seconds, and the simulation fails. The plane crashes. Everyone dies. Seventeen seconds after losing both engines, Captain Sully actually followed protocol by calling for the Engine Dual Failure checklist which the copilot began to go through to troubleshoot the engines. They never made it to the ‘ditching into the water’ part of the checklist because the checklist was three pages long, and the pilots ran out of time. Despite being unable to complete the checklist the crew did accomplish one critical item that the flight crew did not reach in the checklist: starting the Auxilliary Power Unit (APU). From the NTSB report:
“Starting the APU early in the accident sequence proved critical because it improved the outcome of ditching by ensuring electrical power was available to the airplane. Further, if the captain had not started the APU, the airplane would not have remained in normal law mode. This critical step would not have been completed if the flight crew had simply followed the order of the items in the checklist”
Captain Sully wasn’t perfect. He did not attain the required speed for his descent and landing, resulting in a high Angle of Attack (AOA). This resulted in significant structural damage to the fuselage on landing which caused water to enter the cabin. The directive on what speed to travel in case both engines failed was on page 2 of the checklist. The pilots only had time to get through page 1 before abandoning the checklist as time ran out. The checklist had been designed for problems at 30,000 feet. The aircraft lost both engines at 3,000 feet. The pilots only had 3 minutes to land the plane. Experience and intuition of a seasoned pilot carried the day. The protocols did not.
In the time of COVID, physicians more than ever find themselves as pretty baubles on display to reassure the public. The reality is that it’s the system that directs physicians and as a result it is the physicians who find themselves unable to protect themselves or their patients. The lessons from the pandemic, and yes, even the airline industry is loud and clear: Put the physicians back in charge.
Anish Koka is a cardiologist in private practice in Philadelphia. Twitter: @anish_koka
The post COVID-19: Physicians in Shackles appeared first on The Health Care Blog.
COVID-19: Physicians in Shackles published first on https://wittooth.tumblr.com/
0 notes
Text
this dream about you ruined my morning. LOL. (& how do you retell a dream? especially an embarrassing one?)
when: last night slash this morning. [that’s today, Thursday June 27th]
it was one of those *you wake up and know you left an intense dream* *go back to sleep because this fucker of a dream needs an ending*
i could almost call it a nightmare,
if based purely on the harrowing and very real physical toll it had on my body when i really got up from it.
I re-woke to my second and Emergency alarm (that’s the “get the fuck up now bitch go straight to work do not pass go do not pick up an eyeshadow brush do not eat breakfast get your headass into the car and maybe you won't be viciously tardy”) and my ANKLES WERE LITERALLY SORE?? my head pounding something Awful. And like my chest. Felt such a bitch. Stiff, contracted, and dry.
you ever been like HUNGOVER from a dream????
* * *
i don't want to call it a nightmare, though,
because it was about you.
And you were/are not a nightmare. lol.
You just...happened. and it passed.
What this is, Is: i had this dream about you, and i fucking hated it LOL
IT’S A FIRST.
AND I NEED TO PROCESS IT .
BECAUSE i dont get it. i don’t get why i had it. i am so caught off guard by it. i am scared of it. i am scared i even had A dream of you.
and i refuse to let it just bury inside me.
i’m going to claw this thing out and take a good mfkin look at it.
OKAY. now that that’s established...
(ugh.... it feels like i’m about to embark into some bitter medicine.)
* * *
we ran into each other...in an apartment?
I was in the living room with my “friends” in the dream A.K.A obscure, obscure acquaintances whose faces i cannot place or recall.
and like any good dream, out of the god damn blue, comes trawling through a pack of Your friends. or family. or both. and your own face hazily blurring by in the mix. headed thru the nearest hallway, towards one of the bedrooms.
I catch your brother's face (i never even met your brother before lmfao) most crystalline clear among them. and he is the one who stops to meet me as the rest shuffle away.
I immediately recognized him (from pictures. i'd seen pictures IRL), we strike introductions, and conversation. i remember saying "you're his brother!" and other incredibly facile but in that moment in that dream very genuine sentiments. but still we can cringe at how unrealistic and un-grounded in reality they were. things like " i always knew i'd like you" (what the fuck, right) and "wow why does it feel we’ve already met (what the fuck. LOL.) and if we CAN ignore the DELIRIOUSNESS of my REM concoction here, i'd like you to accept with suspension of belief that me and this stranger, me and your brother, did become - in this dream moment - effortlessly chummy. We became instinctively on each other's sides (it still sounds delirious. damn it. Don't share your dreams willy-nilly, folks, it is not smart to expose your fucking dumbly vivid irrationales lol).
We were getting on like old fuckin friends, what the fuck can i say. It's the fictional truth.
Then our convo gets to the Grit. The punch in the gut. he tells me you're here. in this apartment. of course i could’ve put that together but the confirmation is CONFIRMING. Palpable - the settling in of the fact that you and i were..both..here.
A many-voltage shock. and i only snap out of it, and the frozen moment only melts back to action when i feel you feel that same shock. And right away, i "hear"...or was it "see"?....your presence / energy dash out of the bedroom in which you and your group were in. And you lock yourself into the bathroom.
A collective "what the hell" is shared between me and my new-but-old dreamworld friend. your brother.
We step past the bathroom you are now occupying.
We enter the bedroom. I see the rest of your peoples.
Once again, Faceless peoples. i don't know that any of these were REAL peoples, any of your actual peoples in real life. Dreams! what're you gonna do?
Me vs. your peoples, though. It starts as awkward. Your brother tries to smooth things.
I remember warmth starting to emerge. I'm sure I wanted warmth, and since it was my dream, probably i manipulated events to make it so. I am keeping that in mind about this dream from start to finish, by the way. My brain manufactured all of this. Why? Fuck Me if i want to know. honestly.
But without knowing why, i still saw the What. (& this whole entire What gave me a serious kink in my neck this morning, like i never even know what a kink was until i got up and groaned.)
The What, at this point, after me and this room begin to warm up to each other:
I mean, its only appropriate in such a dream that we land on the next Gut punch.
The next revelation. (the brain sure knows who to TELL A STORY. DAMN.)
They tell me that..... FUCK, pause. Pause. PAUSE! I CAN'T BELIEVE I'M ABOUT TO SAY THIS. WRITE THIS. ADMIT TO THIS.
ugh how else can i say this without causing every internal organ in my body to cringe in unison and threaten whole bodily shutdown for the entirety of the time it takes for my parts to Un-Cringe themselves. i could die.
i wish to die.
i won't die.
let me continue. *deep breathe*
They tell me that you want me back.
Oh my god i want to laugh and cry and barf at the same time - me in real life, me now - not me in the dream. Well maybe me in the dream. But speaking from the conscious VERY-NOT-ASLEEP P.O.V of my self at present, it really hurts to say that because...i dreamed that. I can't believe i dreamed a dream in which you say "you want me back".
I cringe because you, and me, might think oh, that's what she secretly wants.
No.
It. Is. Not.
And i know this, but you can't, unless i tell you outright like this "I DON'T".
and even then, because of this dream, i may be relinquishing my right to protest that contention. "Well clearly your deep inner psyche is saying different blah blah wah wah" says the PSEUDO-SCIENTIST IN US ALL. Whatever, that was exhausting, lol, i said what i said and i dreamed what i dreamed.
If you *are* *asking* *me*, i will tell you with incredibly clear eyes: no, i didn't dream you saying that because it was what i wanted. i don't know why i dreamed that, but how about i get to the end now, before we jump to more conclusions:
i hear that, and - what magically appears?
A piece of paper, with old feelings written..no, scrawled.. all over it.
There's blank space near the end.
There's a collective agreement that you are not coming out of the bathroom anytime soon. Is it a red flag to Dream Me that you are HIDING IN THE FKN BATHROOM? LOL NO.
in fact i think Dream Me thought it was cute.
"aw he's shy" rather than "what the fucking coward".
Oooo. Was that harsh. and i oop--
I begin to write my "current" (quotes to remind you this IS THE RE-TELLING OF A DREAM, A NON-REALITY!!!) feelings. surprisingly, they were a smidgen closer to my actual feelings today, but still, it was a dream, and my REM brain is setting me up for some happy ending i think. So what do i write? I write something along the lines of "i don't want to be together but i did miss you and i do want to kiss you".
loooooooooooooooooooooooooooooooooooooooooooooooool
throw tomatoes at me NOW.
MOVING ON:
I remember the room is now crackling with hope, and optimism,
and your peoples are cooing "how cute" (which is hilarious in hindsight because this is not cute at all, it is very very weird)
and then the vibes get *~*~dramatic~*~ for a pinch: a confession from your brother: -this part i'm dead ass even as ludicrous and irrelevant as it seems-
he says to me: “i know he said i'm his brother, but i'm not. Actually, he's the brother. *points to a faceless figure* and i'm the good friend.”
and it was like one of those soap opera revelation moments.
I don’t know why.
Why does this detail...?? matter??? appear??
Well let me add that, it was like...so familiar. this "uncovering" of a lie.
REAL QUICK I'm not saying the man in question is a liar. that’s NOT it at all.
I suspect the familiarity lied in my past experiences of feeling "not let in" or "held at a distance”. & I was doing my own damn lying, to myself. I was doing my own emotionally irresponsible business. /ending that there.
Point is, the "confession" was unnerving and it was almost like an omen. Like WHY Would you lie about something like that??? I couldn’t understand it!
But did i still want to leave this note?
And i, in the dream, did. still want to.
So I give up the note to your peoples with intentions of it reaching you.
But of course, before i can leave, You come pummeling in.
I guess you were done with your really long shit or you were tired of hiding.
But the way you came in, i remember this motion picture vividly:
you don’t greet me, you make a beeline straight past me, you insulate yourself behind your peoples, and your energy feels incredibly apprehensive. like you’re on Defense. Like someone’s come to attack you. Like what? And i’m so confused and so uneasy that i can’t wait to leave, without even wanting a word from you. This, the same person who wants me back they say? This, the same person who I called on for “a kiss” (UGHAHH!!!!!!!!!!!!!!!!!! LMAO!)
Your brother-turned-friend hands you the note.
I see that you got it.
I see you paw it, and start to look at it.
I feel an edge of regret but i let it be. what i wrote reflected how i felt, i affirm with myself.
and i leave
but while walking out, i’m already reconsidering: "okay it reflected how i felt, before i personally contacted THAT energy, his energy, his avoidance, his marked apprehensiveness"
and i storm back
when you were just about to dig into it
and i snatch it from your hands
but you held on and
in my determined snatching, i rip back the bottom half
as you stare at me and shred the rest of it yourself. shred the half that remained in your hands into tiny ugly pieces.
like shrapnel,
and it flutters around you, and your stare is intense, and intact, and i wonder if this was satisfying to you.
i burst out of that room, so angry,
so fucking disturbed
that you could've read something nice
but i didn't want you to read something nice.
No, i was so dissatisfied by the non-greeting, the haphazard waltzing and pacing in the room for the brief moments we shared space,
i was vengeful
i tore the "something nice" before you could receive it.
And then I was horrified by the way you let the rest of it rip up in your hands and disappear like the rest of it (the part i'd taken back).
* * *
I got jumped by my own dream.
HOW DID IT -- I--
I mean. What a load of Holy Hell.
And i still, resist, calling it a nightmare, because,
that's not accurate to how i actually remember you.
I remember you fondly.
and the most stressful part of when i look back at our time together
wasn't even you.
i always, even at the low points, felt a really deep joy from being around you.
The most stressful part when i look back was who I was then.
From where i stand now, i look back and shake my head the most ferociously at who i was, how i was, and what i was missing. what i needed. what i wasn't making sure to get.
have i forgiven Myself?
maybe that's why This Dream.
//////
AN AFTER THOUGHT: perhaps what is truly horrifying about this dream is 1) how childish it was. 2) why the fuck did i have a dream about you like @brain that was so uncalled for bruh
////
Edit: An afterthought 24 hours later=
My impulse was to recount this dream in detail.
I belabored this account, everything i could possibly remember about it, in addition to belaboring that though this DOES seem significant, it DOES NOT mean i still have the same feelings for this mf.
Now i am able to revisit it, in all its cringe detail glory.
I have a lot more perspective on why this dream, and what it might mean to me. WOW the power of writing.
0 notes
Text
'GHOST ADVENTURES' HOST ZAK BAGANS TALKS CHARLES MANSON RUMORED HAUNTINGS AND THE ATTRACTION TO TRUE CRIME STORIES
By Newsweek ( KELLY WYNNE ON 4/4/19 AT 1:01 PM EDT)
Cult leader Charles Manson has an immortal way about him, in the stories left behind of his notoriously wicked ways. There may be a bit of truth to the way he lingers, as Ghost Adventures host Zak Bagans has a collection of Manson’s personal items that in a short amount of time, have proven to have potential hauntings.
Bagans has given obscure Manson artifacts a home in The Haunted Museum, his museum in downtown Las Vegas. There, he displays Manson’s items, from the hospital gown Manson died in, which holds some of his bodily fluids, to a painting made with Manson’s ashes and bone fragments from the cult leader’s body.
Bagans’ quest to secure the Manson items has taken more than a year, and they’ve just recently surfaced in the public setting. Already, though, Manson’s objects have reportedly caused some trouble for museum visitors. “Six weeks ago as a woman at The Haunted Museum bent over to view Manson’s bone fragments and gown, she made a comment directly to Manson, ‘Good on you Man,’” Bagans told Newsweek. “Upon turning away she felt something stab her in her stomach and had to be taken out of the museum, where she was very affected.” Bagans said he has the incident on video.
Bagans also opened up about the mind-power Manson had, and how it has apparently affected some of the objects. “I also believe that while Manson could never get out of prison, he infused the same mind-power he had with the Manson Family into his art and belongings through electrical thought impressions, cursing certain things so whoever obtained them would experience that,” Bagans said. “This occurred with his prison TV that I own, which put one man through pure hell while he previously owned it.”
The darkness of Manson’s acts and the nearly hypnotic hold he had on his “family” are common talking points when it comes to true crime topics. Manson’s most notorious night, when he and members of his “family” murdered actor Sharon Tate and others in her home, has been turned into a film The Haunting of Sharon Tate, starring Hilary Duff. Another Tate film, Once Upon A Time In Hollywood, is slated to premiere later this year, along with another, similarly-angled film, simply titled Tate. Bagans has even produced his own Manson documentary, titled Charles Manson: The Funeral, which will premiere on Reelz April 13. The fascination with Manson in just one year begs the question: why are we so drawn to such a sinister story? Bagans has an answer.
“Charles Manson was an evil man and evil fascinates us. This is why there are so many successful TV shows and movies in the true-crime genre,” he explained. “The media also bombards us daily with headlines of evil events. As human beings we want to know more about why such evil people would commit such crimes like this…who are they and what goes through their minds. We want to know some psychology of their minds. We must go inside the mind of an enemy to protect ourselves.”
It’s the reason why Bagans created The Haunted Museum, though his own fascination lies deeper. He admitted he feels drawn to the dark and demonic elements found in human life, even if not entirely accessible in this realm.
“I collect these items that belong to monsters and give people that same adrenaline rush by being so close to them, reminding that the dark history of what they did will never be forgotten,” Bagans explained. “There are dozens of war museums that showcase guns, uniforms, relics of our enemies that have killed—and we must not ever forget these monsters, war enemies, terrorists, serial killers. Owning their belongings, artwork, remains…it’s a rush in itself for me to be able to own a part of them, and tell my guests how bad and evil they were.”
This article has been updated to fix a headline typo in Charles Manson’s name and to include new details about Zak Bagans’s Manson film.
#HauntedParaClassics
#submission#zakbagans#zak bagans#ghostadventures#ghost adventures#dirtyblog#thedirtyblog#dirty blog#the dirty blog
0 notes
Text
Realtalk(tm): Or Is It All Fake Silence? (On The Topic of Non-Duality)
so. i’m Headache and Tired .
recently i have been considering non-duality (again) and it is, well, endless. but always has an end. but then it starts again, so, did it ever really end? does it matter if it ended. it does! but also, it doesn’t. and really, if it’s both, isn’t it all kind of “ehhh.” but then, “ehhh” is like, the most important thing sometimes.
but THEN. importance is, relative, subjective, not that important. and subjective can be objective and vice-versa, but not always, but if it’s sometimes, then sometimes it’s always, but always, only sometimes. you get the picture, or you don’t, or you kinda do, and honestly, it’s all the fucking same, because it’s all points on a continuum.
BUT THEN do points even exist on a continuum? they do, if you’re looking for/making them. but they don’t, if you’re only looking at the line, so it isn’t actually all the same. and if you’re facing the other direction, you’re like “what points? what line? they don’t exist, do they?” and yeah, they don’t exist! because you can’t see them! but they might exist, outside your field of perception, so they do exist.
what is seeing, anyway. the information goes through so many transformations from its original form to be registered by a brain. the colours i see are not the colours you see, the colours you see are not the colours a mantis shrimp sees. one camera takes photos that come out all yellow, the other takes them with a bluish tint.
right and wrong... subject, object. (ok i’m putting a cut in here bc this got, long and kind of emotionally sorta-really-deep-but-neither, under the jump)
but really i’m mad because, i can’t actually stop thinking about this for long? i always come back to this kind of like, consideration of (non-)“binary” concepts.
like, is the concept of “i” even useful? i mean, yes, because it refers to the body, the mind(s) inhabiting it, and aspects contained within those things.
but then also, “i” is not useful, because broadly, there is no “i”, “i” does not exist in isolation, “i” is dependent/contingent on every surrounding factor.
but specifically, “i” exists, and if i come back to i, then like, i was in so much pain, i was so angry, i was not supported in the right ways at the right times. but then, other “i”s around me did not have the means to support me, they were angry, they were in pain.
so like, it’s fucking me up, because i still have this ingrained binary concept of Right and Wrong, Good and Bad, from like, less-than-good-enough parenting. i’m returning to seeing things through other people’s eyes, getting it wrong because i don’t have their life experiences or method of using the pathways they have, my mind is still going to “oh fuck, i’m Bad, i’m Wrong--” and my body is experiencing the physical reaction to that. i’m forgetting that, well, my i exists?
hence why i am here engaging in these clumsy unpracticed mental acrobatics. attempting to remember what my i is, or create one, or something.
because, well, my i is... uh, i don’t know? how do i define it. flippy. flipping over constantly. i live on earth one minute, but like, as i’m walking along to the shop, i’m suddenly walking along little asteroids on the edge of saturn’s rings, i see it, i feel that space is cold. i’m a robot! but i’m a robot who thinks-feels-eats-breathes and who wants to be a man. and then, i guess that is a man? because what is a man, but a really complicated robot. but i’m made of metal on the inside! sometimes the outside! but only because i see it in my mind, but the mind is real, so whatever the mind creates is real, at least in my non-dual sub/objective opinion/experience?
but yeah. only i know what condition i was in during certain events, and i know how actions of other people kicked me while i was down. and other individuals that tell me i’m wrong, i don’t need help, when i’m telling them something is wrong, i need help, like... that’s their prerogative? they can and will do that, i have no control over that? but god FUCK this individual acutely feels wounded over it, and i gotta respect that, because those other individuals can’t feel what i’m feeling.
but then, frustratingly, i’m also well aware that while there are alternative pathways that could have happened, there was no alternative pathway because of the way the cards fell/are falling, so the one that did happen, the painful one, happened!
it’s all such a huge ball of Fuck. real is imaginary and imaginary is real and both mean everything and nothing but everything is more or less the same as nothing etc etc.
and it’s all a matter of scale and perspective.
so i guess, i’m having to identify my perspective, and the scale i’m functioning on? and, uh, figure out how to return to that at the right times, in order to attend to Body Needs and Mind Needs and Environment Needs, which are all more or less the same thing, but not.
which is, well, shit, i can feel my body again. the body, a body, this physical organism that is sitting here typing this. and this body remembers being yanked and hit and shouted at and made to feel small and stupid and inconvenient and troublesome. this body remembers being routinely insulted and jeered at and mocked and not defended or taught how to defend itself.
which, well, sure, i suppose a long duration filled with being perceived and reacted to like that, is why the mind that is-and-is-within this body has developed such a... well. one-and-many system. selves, non-selves, worlds, non-worlds, presences and absences. living inside the mind, most of the time, is a LOT less painful than living inside the body.
i have... autonomy? i have bodily autonomy? i don’t have to follow an order or be punished? i don’t have to perform certain acts to receive love and affection from myself? i can choose where to go, what to do, what to say, i can choose when and how i go about things, i can validate my own “whys”? i can tell the self-non-selves that yell at me and slice my body in negative emotional reactions, actually, this is not helpful? etc etc?
this... i’m still getting used to this. marginally past “sounds fake but okay.” i’m still reacting in the present to past feelings of, well, yeah. being made to feel so small and stupid and incompetent that the pain i felt in that moment was intolerable, and i wanted my existence to end permanently right there, and that i made active efforts to try and achieve that. but, i am reliving those emotions less, which i suppose is... well, that’s emotional processing, babey!
so, well, uh.
right now! i am and am not suicidal. i’m not, you know, out here with a noose right now suicidal, but i am suicidal, in a really, like, long, slow, drawn-out, masochistic kind of way, because frankly i’m aware that even breathing the air in here is killing me. i have to be suicidal to like, live? at least for now, i gotta be, you know, pretty damn enthusiastic about the idea of my own death and its randomness and my part in bringing it on, in order to enjoy the whole, living thing? i dig it, death is sexy, he’s my other boyfriend. i mean, sometimes i don’t, but then i do again, so, yeah, fuck, you get the picture, or don’t, and so on so forth.
man like I have received shit in the past for like... “overcomplicating” things. but dude... this is literally how complicated it is, for me. i can’t switch this off until it’s Good and focking Ready to be switched off, i.e., i’ve made some or several point(s) to-with my self-selves. argh, english language is so clumsy for discussing this, language is so clumsy, it is a tool, it will suffice.
BUT YES my braincalm feeling is making itself known so, i suppose this is, The End. until, you know, i make another post, tomorrow night, about something the-same-but-different. it is all so uglybeautiful shallowdeep and like a f!cking wheel with infinite-finite points always-never turning. basard. the non-duality... it never STOPS, until you stop thinking about non-duality, in which case, it’s still a side within non-duality... f!cking paradoxical-non-paradoxical. Loops. Loops Everywhere. The Strings. Oh God. The Strings
OK jesus if i don’t make the judgement call and just say Yeah Ok Stop. this will never end. Back To Your Regularly Scheduled Obscurity And Reblogged Content
0 notes
Text
How Learning and Memory Relate to Free Will
One common definition of "free will" is that a person can decide or choose among multiple alternatives without being forced by physical laws, luck, fate, or divine will. Most of us feel we are in charge of our choices when no outside force requires us to make a particular choice. But it is fashionable these days for scholars to insist that free will is an illusion, a trick the brain plays on us. I will spare you the philosophical knots of specious assumptions and convoluted logic that that scholars tie themselves into.
Why do I bring this up? What has the "free will" issue have to do with learning and memory? Everything. Rather than memory dictating our choices, either we have chosen what to learn and remember or we can veto or amend the influence in our decision-making.
Human brains make choices consciously and unconsciously by real-time evaluation of alternatives in terms of previous learning from other situations and their anticipated usefulness. This learning occurs in the context of the learned sense of self, which begins unconsciously in the womb. The conscious brain is aware that it is aware of choice processing and makes decisions in light of such understanding. When a given alternative choice is not forced, the conscious mind is aware that it is not obliged to accept any one choice but is "free" to select any one of the available options. Such realization might even guide many decisions at the subconscious level. In either case, neural networks weigh the probable value of each alternative and collectively reach a "decision" by inhibiting networks that lead to less-favored alternatives. Thus, network activity underlying the preferred choice prevails and leads to a selective willed action. What governs the network activity causing the final choice is the activity in other networks, which in turn is governed by stored memories and real-time processing of the current environmental choice contingencies.
What usually gets left out of free-will discussions is the question of how a brain establishes stored-memory preferences and how it evaluates current contingencies. These functions surely cause things to happen, but what is the cause of the cause? Any given brain can choose within certain limits its learning experiences and stored memory. We govern those choices by what a brain has learned about the self-interest value associated with given contingencies. Brain circuitry assigns value, and values chosen are largely optional choices. The conscious brain directs the choices that govern value formation, reinforcement, and preservation in memory.
Now we are confronted with explaining how neural circuit impulse patterns (CIP) representing the sense of self can have a free will. First, I reason that each person has a conscious Avatar that brain acts as an active agent to act in the world on embodied brain's behalf, as explained more completely in my recent book. This is reminiscent of the 3rd Century idea of a homunculus, a "little person" inside the brain. The modern view is that this homunculus exists in the form of mapped circuitry.
Certain maps are created under genetic control. These include the topographic map of the body in the sensory and motor cortices. Then there is the capacity for real-time construction of maps of the body in space that resides in circuitry of the hippocampus and entorhinal cortex. Other maps are created from learning experience from the near-infinite circuit capacity of association cortex. What these maps learn is stored in memory as facilitated circuit synapses and deployed "on-line" in the form of CIP representations of what was originally learned. New learning likewise exists as CIP representations in sub-network populations.
The Avatar itself is a constellation of CIPs representing the conscious sense of self. Certainly, by definition, the Avatar can make choices and decisions. Wakefulness releases consciousness to make its own choices and decisions. Avatar processing is certainly not random, and presumably can occur with more degrees of freedom than found in unconscious mind.
If the Avatar exists as CIPs, how can something as "impersonal" and physiological as that have any kind of "will," much less free will. Let us recall that "will" is little more than an intent that couples bodily actions to achieve the intent. This kind of thing occurs even in the circuitry that controls unconscious minds. These circuits automatically generate actions in response to conditions that call for a response. Such actions are stereotyped and inflexible only when there is no conscious oversight.
Each alternative is represented as circuit impulse patterns (CIPs) within a subpopulation of brain, which be considered as constituting part of the sub- or non-conscious mind. Each population's activity interacts with the others - and with the CIP representation of the Conscious Avatar. When activity level in any one subpopulation reaches a threshold, it suppresses activity in the alternative representation populations, leading to selection of that population's activity as the choice result. The Avatar CIP is poised to influence activity in the alternative sub-populations and thus can help direct the final processing result.
The Avatar must have some criteria that its circuits use to make a given decision. Those criteria have been learned and remembered. When CIP processes operate in Avatar circuitry, the Avatar population activity can modulate the alternative-choice representations in the context of self-awareness according to the informational representations of past learning and value assessments of current contingencies. You might say that when the brain generated the CIPs to represent the sense of self, those CIPs came endowed with a certain autonomy and freedom of action not available to the other CIPs in the brain that constituted unconscious mind.
People who believe that humans have no free will are hard-pressed to explain why no one is responsible for their choices and actions. What is it that compels foolish or deviant behavior? Is our Avatar compelled to believe in God or to be an atheist? Is our Avatar compelled to accept one moral code over any other? Is it compelled to become a certain kind of person, with no option to "improve" itself in any self-determined way? Do learning experiences compel us to make our choices of learning experiences? Of course not. We are free to reject learning that does not serve us well.
It seems to this Avatar that current debates about determinism and free will tend to obscure the important matters of our humanness. The door to understanding what is really going on is slammed shut by assertions that value choices and the decisions that flow from them cannot be free because they are caused by neural circuit impulse patterns. Free will debates distract us from a proper framing of the issues about human choices and personal responsibility.
While it is true that genetics and experience help program the Avatar circuitry, the Avatar does its own processing and makes choices about who to interact with and what experiences to value, promote, and allow. The Avatar can insist that it has a need to remember some lessons of experience and makes it a point to remember it. In short, the Avatar gets to help shape what it becomes.
Sources:
Klemm, W. R. (2014). Mental Biology: The New Science of How the Brain and Mind Relate. New York: Prometheus.
Klemm, W. R. (2016). Making a Scientific Case for Conscious Agency and Free Will. New York: Academic Press.
Remember, to get a full understanding of this post, you need the book, Thank You Brain for All You Remember.
How Learning and Memory Relate to Free Will published first on https://buyessayscheapservice.tumblr.com/
0 notes
Text
COVID-19: Physicians in Shackles

By ANISH KOKA, MD
A number of politically tinged narratives have divided physicians during the pandemic. It would be unfortunate if politics obscured the major problem brought into stark relief by the pandemic: a system that marginalizes physicians and strips them of agency.
In practices big and small, hospital-employed or private practice, nursing homes or hospitals, there are serious issues raising their heads for doctors and their patients.
No masks for you
When I walked into my office Thursday, March 12th, I assembled the office staff for the first time to talk about COVID. The prior weekend had been awash with scenes of mayhem in Italy, and I had come away with the dawning realization that my wishful thinking on the virus from Wuhan skipping us was dead wrong. The US focus had been on travel from China and other Far East hotspots. There was no such limitation on travel from Europe. The virus had clearly seeded Italy and possibly other parts of Europe heavily, and now the US was faced with the very real possibility that there was significant community spread that had occurred from travelers from Europe and Italy over the last month. I had assumed that seeing no cases in our hospitals and ICUs by early March meant the virus had been contained in China. That was clearly not the case.
Our testing apparatus had also largely been limited in the US to symptomatic patients who had been to high-risk countries. If Europe was seeded, this meant we had not been screening nearly enough people. When I heard the first few cases pop up in my county, it was clear the jig was up. It was pandemic panic mode time. There was a chance that there were thousands of cases in the community we didn’t know about and that we were weeks away from the die-off happening in hospitals in China and Italy. So what I told the staff the morning of March 12th was that we needed to start acting now as if there was significant spread of COVID in the community. This meant canceling clinic visits for all but urgent patients, wearing masks, trying to buy masks, attention to hand hygiene, cleaning rooms between patients, screening everyone for flu-like symptoms before coming to the office, and moving to a skeleton staff in the office. I left the office that day wearing a mask as I headed to the ER.
Again, this was March 12th. Even the short walk from my office to the hospital ER resulted in quite a few stares. But I was going to the ER, after all, at a time when a possible surge was happening. I already knew the Chinese experience at this point. Health care workers got infected most likely because they didn’t have adequate Personal Protective Equipment (PPE) early on. Of course, I didn’t have any n95 respirators because I hadn’t prepared for this scenario. All I had was a limited quantity of surgical masks. I figured it was better than nothing, and at the very least, I would hopefully reduce the chance of transmitting the virus to patients I was going to come into contact with in case I picked it up in my travels. When I walked into the ER, I was surprised to find no separate area set up to handle COVID patients. There was one negative pressure room set up for COVID patients. That’s right, one room. The waiting room was a common area as well, which meant that people without COVID had a reasonable shot of acquiring COVID while in the waiting room. The initial Chinese data suggested 40% of COVID infections were acquired in the hospital.
I left the ER to travel to another part of the hospital, and in the lobby was stopped by a somewhat excitable administrator. Why was I wearing a mask, he wanted to know? Taken aback, I stammered something about trying to protect patients. Current guidelines, I was informed, were to only wear a mask if sick. Any other use was discouraged. We wouldn’t want to scare patients. Not wanting a scene, I took the mask off in the lobby to mollify the agitated administrator. Four days later, the same hospital had a universal mask policy for staff. Four weeks later, and the surgeon general was recommending universal masking for the entire population. Today, I am at risk of being dragged out of the local grocery store unless I’m wearing a mask.
PPE can be divided into plain old surgical facemasks, facemasks with shields, n95 respirators and Powered Air Purifying Respirators (PAPRs). The vast majority of US physicians spend little time thinking about PPE on a daily basis, because there has never been a widespread threat from a novel pathogen with no cure. Ebola and SARS would have qualified but American doctors domestically never faced these foes. Generally physicians let infection control teams in hospitals run the show. This translates into physicians putting on whatever PPE is sitting in the isolation cart that sits out of the patients rooms. The general theory that relates to the transmissibility of pathogens breaks down to four categories: Direct contact, indirect contact, droplet, and airborne.
Direct contact requires physical contact with some part of an infected person. Usually this happens when infected bodily fluids come into contact with the eyes, mouth, nose, genitals, or open wounds. Indirect contact is when an external surface like a doorknob serves as an intermediary for the communication of infected bodily fluids. Droplet transmission results from the expulsion of small particles of bodily fluids into the air through coughing, sneezing, or vomiting. These are thought to be heavier particles that don’t stay suspended in the air for very long, and so require close proximity for transmission to occur. Airborne transmission occurs via droplets that are small enough to float in the air and so can cause infection over long distances. Airborne particles are produced by coughing, sneezing, or certain aerosol-generating medical procedures that involve instrumenting the upper airways.
The type of transmission impacts the recommendations for PPE from organizations like the CDC. These guidelines provide the backbone for infection control in healthcare facilities. It’s an easy categorization scheme. Smallpox requires airborne and contact precautions, Ebola requires droplet and contact precautions, while HIV and staph require standard precautions. It should strike many how remarkable it is that millions of years of evolution has lead to infectious pathogens being neatly divided in a way that would make recommendations for PPE for healthcare workers so simple.
Of course biology isn’t this simple. A sneeze can aerosolize a pathogen. There isn’t a biological cliff at which point droplets suddenly become small enough to be airborne. If it’s not already obvious, the distinctions made have more to do with convenience than it has to do with the actual mechanics of disease transmission.
A beautiful review in the lay press by Ari Schulman notes that the current schema is rooted in distant history that has not been well updated. Charles V. Chapin, an eminent epidemiologist noted in 1910 that “there was no evidence that [infection by air] is an appreciable factor in the maintenance of most of our contagious diseases.” Therefore, he advised that attention be primarily paid “to the prevention of contact infection”. Not surprisingly, it was clinicians who began to question this paradigm. In 1919 George H. Weaver, a physician at Chicago’s Durand Hospital for the poor, subsequently observed “the ease with which infections may be transferred through mouth droplets when people are brought into intimate association”.
A famous paper by Mildred and William Wells in 1936 attempted to examine the variety of clinical reports of airborne infectious spread. The couple started with the assumption that the air was a conduit for transmission of bacteria based on the work of Louis Pasteur, whose classic experiments on spontaneous generation in 1861 proved that air was populated with microscopic germs which caused putrefaction and fermentation. The direct evidence of this proved difficult to produce in the decades to follow. The failure to produce nasopharyngeal organisms on plates exposed farther than a few feet from a person who was coughing and sneezing led to the conclusion that infectious pathogens settled out “in short distances and in brief time intervals”, and that airborne transmission just didn’t happen. The absence of evidence became evidence of absence.
Technical advances that allowed the observation of droplets were carried out by Wells to first demonstrate the plausibility of airborne spread. Animal experiments which involved inoculation of healthy ferrets with the air from an infected ferret with influenza suggested influenza could be airborne. Once again it was observations by clinicians that drove the research. Noting the recent reports of the spread of the psittacosis virus at a National Institutes of Health building via the ventilation system from the basement to the upper floors, the 1936 researchers attempted to mimic this by inoculating a culture of B.coli in the humidifying water of a one room air conditioner in the basement of the Harvard School of Public Health. They noted B. coli was recovered from the ends of every corridor up to the top floor of the three story building and concluded that “infected nuclei can therefore be dispersed by ventilating currents throughout a building.. “
The researchers next turned their attention to the effect of sneezing. Fifty sneezes were induced from a group of subjects in a standard air conditioned room. Bacterial samples collected in the air centrifuge on blood agar tubes revealed thousands of alpha streptococci and M. catarrhalis. Even after the subjects left the room, the air contained many hundreds per sample. Interestingly, in a nod to the current universal masking recommendations, an application of handkerchiefs to smother the sneeze showed a marked reduction in collected organisms.
The triumphant conclusion of this brilliant paper noted – “The burden of proof of air-borne infection, which had hitherto rested on bacteriology, has been lifted, and there now rests on epidemiology the burden of disproof of airborne disease”
To summarize, the world of science rejected a theory of airborne transmission based on clinical observations for decades because technical issues precluded organisms from being recovered from the air. Instead of holding on to the possibility that the clinical observations were ground truth, blind empiricism created a new dogma: Airborne transmission couldn’t happen. It would be convenient to assume the blind zeal attached to what can be measured is a product of a bygone era, but sad to say this is alive in well in a current society among an overly certain technocrat class that makes up a large portion of the intellectual elite.
In the hundred years since the Wells team published their conclusion, the debate on Personal Protective Equipment (PPE) to deal with infectious pathogens has been conveniently made simple by institutions that write the definitive guidelines on the subject. The neat categorization of PPE based on characteristics of pathogens never made biological sense. As was shown by the Wells team in one form or the other, infectious pathogens may be made airborne. We get away with artificial distinctions most of the time because the consequences of not having the perfect PPE are usually not apparent. This changes when humans encounter a lethal novel virus for which the population does not have immunity.
Consider Ebola. Establishing transmissibility of an infectious pathogen involves a demonstration of a variety of steps: Viability of virus in aerosolized particles, persistence in the environment, infective capacity, demonstration in animal models, epidemiology via contact tracing, and direct observation of healthcare workers wearing respiratory equipment. Ebola is able to reside within airborne sized particles, can stay persistent at certain temperatures for as long as 50 days, and animal models and epidemiologic data are mixed.
The conclusion from this mixed bag of data that does NOT rule out airborne transmission in a virus that has close to 50% mortality would seem to be to err on the side of recommending PPE assuming airborne transmission. Instead, the CDC and the WHO recommended against airborne precautions, in part because Ebola does not primarily affect the respiratory tract citing a lack of an evidence base to definitively prove transmissibility that would require more aggressive PPE. The official recommendation was instead for a plain surgical mask, unless health care workers were involved in medical procedures that could cause aerosolization.
In what seems to be reflective of the generally cavalier attitude of those in charge, an editorial published in the Lancet August 2014 argued against the use of more advanced PPE such as respirators despite noting that Ebola had been noted to “rarely be transmitted via an airborne route” because of the expense of complete respiratory protection. Even worse, “such an approach suggests that the only defense is individual protective equipment, which is inaccessible to the general population. Moreover, the image of workers with spectacular protective clothing might contribute to the panic in some communities. If this leads people to flee affected areas it could increase the spread of infection. It also reinforces the view that some lives are more valuable than others… ” The article concludes by emphasizing that the rational and efficient use of PPE may only be achieved by communicating a consistent message that the disease is essentially transmitted through direct contact. The overriding concern here in a document that is supposed to be about precautions for healthcare workers, is for the “public” psyche. The psyche of healthcare workers who are taking care of patients seems to be of minimal concern.
In another editorial, Harvard public health physicians scolded hospitals that were considering Ebola protocols that involved placing patients in negative pressure rooms, and compelling all personnel to wear full body hazmat suits, as well as requiring n95’s and powered air-purifying respirators. The public health officials pointed to “evidence-based” CDC guidelines that were really just cherry-picked case series and epidemiologic surveys to suggest contact with infectious body fluids was the primary mode of transmission. They did give a nod to potential airborne transmission by advising higher levels of protection for aerosol producing medical procedures.
But conveniently, the authors ignored the pragmatic consideration of natural aerosol producing procedures like coughing or sneezing, and go on to imagine the risks of self-contamination of taking off “unfamiliar PPE”. There is of course, no evidence provided to support the implication that wearing too much PPE when faced with a high mortality virus is more dangerous. The important thing is to not “inflate patients and caregivers anxiety levels, increase costs” and, as health care professionals, “strive to provide evidence-based care driven by science rather than by the media or mass hysteria.”
Never mind that the CDC’s guidelines for laboratory rather than health care settings puts Ebola on the list of pathogens requiring the most stringent possible level of protection. Ebola belongs to the Biosafety Level 4 club, and requires the use of powered respirators and other strict controls because :
The microbes in a BSL-4 lab are dangerous and exotic, posing a high risk of aerosol-transmitted infections. Infections caused by these microbes are frequently fatal and without treatment or vaccines.
Yet health care workers may work in close proximity with these same viruses in a sick patient that may be coughing, sneezing, and having loose stools wearing a gown, gloves and surgical mask, and then go home to their families, stopping to pick up a pork roast from the grocery store along the way.
The end result of all these machinations was to allow a natural experiment to play out demonstrating the folly of issuing recommendations that have more to do with calming the psyche of the public than with actual science. Low resource centers in Africa, driven in part by necessity, implemented less protection, while others did more. Doctors Without Borders sites used full body hazmat suits and respirators with a smattering of infections related to direct care of patients in facilities. Local hospitals used surgical masks with significantly different results. Even in the United States’ small experience of treating Ebola patients, two infected nurses in Dallas were not wearing respirators. Atlanta’s Emory Hospital, which required respirators, successfully treated four Ebola patients with no infections of health care workers. The CDC subsequently changed its guidelines quietly to recommend respirators for Ebola. The WHO still has not.
There has been evidence since at least 1936 that pathogens may transmit disease over long distances via the air, that coughing and sneezing can create aerosols, and that the simple handkerchief greatly reduces the transmission of aerosolized particles. Yet, it is March 12th, 2020, and faced with a potentially deadly pathogen with no cure, an excitable administrator wants to tell me about hospital guidelines that recommend against everyone wearing a mask so that the public doesn’t get scared.
This particular story of masks and PPE certainly isn’t a problem created by administrators. They simply are channeling the zeitgeist that permeates the world of public health and infection control for some time now. In doing so, they empower the cadre of non-clinician administrators who point to these ‘evidence-based’ proclamations when telling physicians what to do. It’s also very convenient for health systems to have infection control committees make rules that are less resource-intensive. This is the dirty secret of many a hospital committee – the goal is to rubber-stamp what the health system needs, rather than do what’s best for patients and physicians.
Don’t touch the ventilator
In another age, it was the clinicians that dictated process. Now processes are dictated to clinicians. In large part this relates to the incorporation of physicians as cogs of expansive, multibillion-dollar health systems. Just like decisions about PPE, the medical management of patients is now by protocol. The system is set up to thwart variance and dissuade individualized treatment.
This has made the traditional role of physician as team leader into a relic of long ago. Every trainee in medicine feels this to some degree when stepping into a hospital for the first time. There’s a way things are done that the nurses, respiratory therapists, physical therapists, charge nurses and case managers are anxious to imprint on the trainee. This is a necessary part of learning for all trainees. The more recent development is applying this imprinting process to trained physicians. The evolution was a byproduct of evidence-based medicine that rested on randomized control trials comparing new therapies or protocols to standard of care. It was a well-intentioned attempt to improve care by reducing variations in care that may be substandard. The roots of the focus on minimizing variation come from its successful application in industrial manufacturing in places like sausage factories.
Someone forgot to tell the intelligent designers that medicine isn’t a sausage factory.
Take the recent controversy that has emerged over mechanical ventilators and COVID. Since the coronavirus has a proclivity for lung tissue, the current conversation has focused on whether the nation has enough ventilators to support the sickest COVID patients. Managing patients on ventilators practically translates to assisting patients unable to breathe on their own. This has traditionally been done using machines that force air into the lungs in a rhythmic fashion to simulate the normal pattern of breathing. Ventilators don’t cure the underlying problem with the lungs, they simply help support patients until the underlying disease process affecting the lungs is resolved.
It became apparent decades ago that the process of ventilation was not a benign affair. The lungs are normally very compliant structures, which means relatively low pressures can be used to inflate lungs. In diseased lungs, where infection or inflammation affects the lungs in a non-uniform manner, it was recognized that pressures applied in a uniform manner may damage poorly compliant areas of the lung. A series of randomized controlled trials culminated in the famous ARDNet trial that examined lower administered volumes of air (a lung-protective strategy) than was standard at the time. The trial was a blockbuster at a time many were doubtful significant improvements were possible in critically ill patients on ventilators. Patients in the lung-protective, lower lung volume arm had 22% lower mortality.
Lower lung volumes meant less total ventilation, which meant letting surrogate markers that were dependent on ventilation to be less than perfect. The thought was that there must be damage happening at the higher lung volumes that was even worse for patients. As has been hammered home to many a medical trainee, patients don’t care about numbers, they care about living and getting off of the ventilator. And it sure seemed a simple adjustment to protocol could accomplish this.
The trial changed the practice of medicine. From that point on, every intensive care unit in the country made the new lung volume settings (6ml/kg) from ARDSNet standard. This was progress, of course, but it’s always the case that every new standard becomes a new dogma.
The rapid increase in trials that studied protocols has resulted in a rapid uptake of protocol-based management in practice. Hospitals today certainly feel like physicians oversee protocols rather than patients. A patient arrives in the intensive care unit on a ventilator, a templated order based on some guideline goes into effect, a respiratory therapist implements the order, and then checks daily via another templated order based on another guideline if a patient can be liberated from the ventilator. Management, by default, can become a technical affair that allows the physician to be minimally involved. The mantra from respiratory therapists – non-physician specialists who manage ventilators now – to physicians is : Don’t touch the ventilator.
Protocols dictate to nurses and therapists what parameters (laboratory values, patient metrics on the ventilator) need to be checked on a daily basis, and what path to follow with regard to management of the ventilator. Indeed studies have demonstrated that protocols may best the average physician in many cases because it saves on the time needed for scarce physician resources to get to the patient to make a decision.
This neat little system, however, runs into turbulent waters when patients don’t behave according to protocols. The COVID pandemic is a gigantic deviation from protocol. The disease appears to be marked by significant gas exchange abnormalities in the lung. Whether it’s due to coating of lungs with virus or an inflammatory reaction induced by the virus, the unit of the lungs that appears to be ground zero for COVID is the alveoli, the main unit of the lung involved in the exchange of oxygen and carbon dioxide. Generally, an important trigger for deciding on mechanical ventilation has been an inability to exchange these vital gases effectively, and an easy surrogate to follow has been the oxygenation level in the blood. This is easily done with the simple pulse oximeter which measures the changes in light absorption in oxygenated and deoxygenated blood to return a “percent saturation” on a monitor. The healthy human saturates close to 100%. As the number dips below 90% the anxiety of doctors and the health care team generally goes up exponentially. These low numbers are generally regarded as a warning that the patient may be approaching a cliff, and once over the cliff, resuscitation may prove to be very difficult. The approach has been to use the oxygen saturation as one data point that helps guide the timing of placement on a mechanical ventilator. This allows the administration of higher amounts of oxygen and may relieve the work of breathing of a patient in distress.
In the case of COVID, anecdotes of patients who were comfortably hypoxic began emerging: Some patients were being asked to get off their cell phone to be intubated. It has long been understood there is a downside to being placed on a ventilator. There is a cost that’s incurred by putting a tube down your throat, and blowing air through it. It’s generally uncomfortable, and often requires some type of sedation. This turns out to be especially true with COVID because patients are very hard to manage once on ventilators. Physicians with direct experience I’ve spoken to note that the patient’s numbers after intubation look terrible. Rapidly increasing levels of support on the ventilator are required in the form of fraction of oxygen, as well as the volume of air that requires to be moved per minute into the patient’s lungs. The patients often aren’t in-sync with the ventilator and require sedation along with muscular paralytics be administered to completely take over the work of breathing for the patient. One physician described the intensive care units they were managing as zombie units because of the significant portion of patients that were heavily sedated.
The need for significant sedation is complicating because of the downsides of sedation. Every day of complete bed rest results in muscle atrophy which may make it more difficult to ultimately get off the ventilator. Complete sedation puts the burden on the care team to do everything that the patient used to do for themselves. Fluid intake, shifting in bed to avoid sores and pressure ulcers, and caloric intake all need to be managed. In the best of circumstances, this is tough. In the midst of a pandemic with a potentially deadly virus where time spent in rooms is minimized, this is much harder.
As a result, some physicians wondered if it would be reasonable to tolerate more marginal numbers to minimize the intensity of sedation and ventilation that may be required. Interestingly, these were the type of steps taken that lead to the ARDSNet trial – tolerate worse gas exchange parameters that came along with lower delivered lung volumes so as to expose the lungs to less pressure. But the physicians ran into a bit of a problem. There was a new dogma. Experienced ICU nurses and respiratory therapists are wedded to the ARDSNet protocol. Deviation was seen as aberrant. I’m told physician orders, if not refused outright, were “slow played” if they ran counter to protocol. In a now-public video on Medscape, one physician had to leave the intensive care unit he was managing because he couldn’t ethically follow the protocols.
To be clear, this isn’t a story of miscreant physician trying to institute a brand new untested protocol broadly, it was physicians seeking to deviate from a standard for certain patients because they thought it best. The role of protocols should be to function as a basic framework. In practice, they can become rigid walls used by non-clinicians to veto doctors. ARDSNet showed that 12ml/kg was worse than 6ml/kg. It doesn’t say 8ml/kg is worse. The general consensus of lung protective ventilation that was introduced by ARDSNet has been to keep pressures within the lung below 30mmHg with every delivered breath. But what about 32mmHg? These are decisions that should be under the purview of the thoughtful clinician attempting to respond to the clinical scenario presented by the patient.
And they aren’t.
The desire to stamp out variance leaves little room for the nimble care that may be needed when faced with a novel disease. It’s likely too early to say what clinicians’ hunches will eventually prove to be salient. Many of them will no doubt be incorrect. The beauty of living in an interconnected world is that ideas are discarded by the community almost as quickly as they are generated. Multiple trials are, of course, underway to test a variety of these ideas and will help further inform the community. In the meantime, physicians are left to try to adjust their therapy to patients that are failing in front of their eyes. This doesn’t mean physicians have license to start offering spinal manipulations to treat COVID, but it does mean understanding that tidal volumes of 6ml/kg aren’t found in the Ten Commandments.
The consequences of being rigid in these circumstances runs the risk of making a bad situation worse. The end stages of any illness that involves the lungs to this degree is going to have a significant mortality independent of any interventions the medical community makes, but personal communications from experienced critical care physicians certainly make it plausible that following protocols blindly in this illness has a price.
Empowering physicians to help patients cannot be done without first freeing the thoughtful, experienced physician latitude to do what they believe is best.
Far from the ventilators in ICUs, even physician administrators find themselves swimming upstream. The COVID nursing home tragedy provides a good example of this.
Nursing homes and COVID: The disastrous shelter in place plan
Nursing homes that care for the elderly and infirm have been at the center of the COVID19 storm. The first US outbreak was in a Washington state nursing home, and the same scene has played out at multiple similar facilities across the country. It was always the case that the nursing home demographic would be hit especially hard with a virus like COVID that causes a lot of damage to the elderly with comorbid medical conditions, but this particular train wreck is almost definitely exacerbated by decision making taking place far from nursing homes.
Very early on, the medical caretakers of nursing home patients found themselves at odds with other parts of the health system, as well as local public health officials. Guidance was issued with regards to visitors to nursing homes early on, but there was precious little thought from central authorities about what to do when a resident at a nursing home got infected. As one of the medical caretakers at a nursing home, I thought it was obvious that patients who became infected needed to be rapidly removed from the nursing home. There was little doubt that the dormitory set up and significant health care needs of residents would make isolation almost impossible at the nursing home. If one person on a 40-bed unit was to get COVID, it was certain to spread like wildfire throughout the unit, and probably throughout the nursing home.
What I found was a local Department Of Health (DOH) that was laser-focused on keeping patients at nursing homes. This was understandable early on because the initial epidemiological modeling, and the scenes out of Italy and New York suggested local health systems could be overwhelmed in short order. Health systems were scrambling to build bed capacity and were worried about running out of ventilators. It made little sense to fill up beds in a system that was about to be overrun. The trajectory of the pandemic unfolded very differently across the country. There was the New York/New Jersey metropolitan area and there was everything else. Two weeks into the lockdown, Philadelphia hospitals had been emptied waiting for a New York-style surge that never came. But at this point the nursing homes unfortunately had started to see their first infections probably seeded from the nursing home staff. A nimble response at this point would have been to utilize the excess capacity of the hospitals and shelter the early positive nursing home patients. Hospitals had well trained, relatively highly paid staff, adequate PPE, and negative pressure rooms. Nursing homes had lowly paid workers with 10:1 patient ratios (ancillary staff) that were poorly equipped to effectively quarantine a patient with COVID. But nursing home patients were treated like patients from the community who were too well to be admitted to the hospital – they were sent home. The consequences of keeping these patients at the nursing home meant the health system had to eventually deal with the entire nursing home being infected.
We looked for help.
We asked the DOH to allow us to test everyone at the nursing home in order to effectively cluster everyone with COVID in one unit. They refused because the guidelines didn’t recommend this for those that were asymptomatic. We asked to utilize a large room to cohort patients with COVID. Nursing home administration and the DOH said this wasn’t possible. COVID tests were being sent to the DOH and had a turn around time of 2-4 days initially. I called the local large health system that had acquired a new rapid, same-day test to see if we could send them tests. No answer. I spoke to a nice hospitalist at another large health system who was very receptive to the idea of boarding COVID positive patients from the nursing home in the half-empty hospital to avoid the entire nursing home eventually being infected. An email chain followed to get permission from administrative units. Absolutely not was the answer. I was told the more fruitful endeavor was to discuss advance directives with the residents. Did they really want to be resuscitated if they got too sick? And if they didn’t want to be resuscitated did they really want to go to the hospital?
The implicit message: Keep the residents away from the pristine hospital. If they get too sick, hopefully they don’t need to be resuscitated. It’s sad. There’s a built-in bias society tends to have towards nursing homes that at times has reminded me of a leper colony. Out of sight, out of mind. In training, I’m ashamed to say I had the same biases. I groaned when I heard about the fever admission from the nursing home. The patients as I remembered them were non-verbal and almost always had a feeding tube. UTIs, meningitis, pneumonia. Usually, family members were scarce or unhelpful. Code status was never assessed.
As an attending physician, the view from the nursing home was wholly different. Everyone had a story, and at this nursing home at least, everyone had a personality even if the ability to communicate for a variety of reasons was unique. The first year I was there running a small cardiology clinic, I didn’t know that the holiday party was the same day. Mr. Rose was playing the guitar and wasn’t available. So I went to watch him play.
The system doesn’t know any of these things. The goal seemed to be to keep the health system free of these second class citizens.
Maddeningly, we physicians were supposed to be the advocates, and were powerless. This was always going to be hard. There was always going to be a death toll in this population. But with the limits placed on us, their medical guardians, that toll is bound to be much higher. Maybe there was a physician there somewhere behind the curtain who was running the show, but I never made it past the army of nurse administrators eager to tell me what the protocol was for my situation.
Nothing is easy about this. Mr. Rose won’t be playing in any more holiday shows. He wasn’t a well man. He had lived well beyond what someone with the injury that put him in the nursing home was expected to live. In some sense, he had been living on borrowed time. If not for COVID, perhaps a conventional pneumonia would have taken him. It doesn’t feel any better.
The traditional role of the physician is under siege precisely because it was felt the physician as owner lead to misaligned incentives. Third-party payment, embraced by physicians in the early years, has been steadily redirected to systems. The end result is the system employs physicians, and it is the system that directs medical care. The system will decide what PPE you will wear, what protocols are allowed on the ventilator, and how your nursing home residents are best managed. The intentions are good and based foundationally on the idea that decision making needs to be taken out of the hands of individuals as much as possible to reduce the variance in dealing with a problem. This schema was an attempt to apply what works well when working with mechanical systems to deliver mass production at scale with high quality. The innovation of the last few decades of health care system delivery has been to make hospitals more like factories with the aim to provide higher-value care with this approach. It would appear we have done anything but, and it’s possible the whole enterprise is based on rotten assumptions.
Gary Klein, a research psychologist who studies decision making and has written extensively on the topic based on an extensive historical review, notes that some of the best decisions are made by adapting to circumstances rather than being bound to protocols and checklists. The standard advice applies when everything is clear and situations are well ordered, but the tough decisions are made with imperfect information in complex and ambiguous situations.
The Miracle on the Hudson
Minutes after takeoff from LaGuardia, New York, US Airways Flight 1549 flew into a flock of large geese and lost both of its engines. The plane was at 3000 feet with no engine thrust and a rapidly descending flight trajectory. Turn back to LaGuardia? Try to make it to Teterboro Airport in New Jersey? Or land in the Hudson river? There was no protocol for this particular situation. There was only a well of experience to rely on. LaGuardia was quickly ruled out- it would require taking a rapidly descending commercial airliner over Manhattan. The initial plan was Teterboro, but the situation rapidly devolved. Teterboro was just too far to make. The next terse message to air traffic control — “We’re gonna be in the Hudson..” The rest is history. Captain “Sully” Sullenberger glided a fully loaded plane down into the Hudson – and everyone survived.
The established flight protocol on losing engines is to attempt to return to home base – LaGuardia, in this case. The National Transportation Safety Board (NTSB) had the job of deciding if Sully had done the right thing. Was Sully’s mental calculation correct? Was LaGuardia really not an option? Had the water landing been a reckless display of arrogance in breach of a safer protocol guided path to an airport? An initial flight simulation showed the plane could successfully return to LaGuardia after both engines were lost. But this didn’t incorporate the time taken to figure out that the engine’s were irretrievably lost. Delay the decision to return to LaGuardia by 35 seconds, and the simulation fails. The plane crashes. Everyone dies. Seventeen seconds after losing both engines, Captain Sully actually followed protocol by calling for the Engine Dual Failure checklist which the copilot began to go through to troubleshoot the engines. They never made it to the ‘ditching into the water’ part of the checklist because the checklist was three pages long, and the pilots ran out of time. Despite being unable to complete the checklist the crew did accomplish one critical item that the flight crew did not reach in the checklist: starting the Auxilliary Power Unit (APU). From the NTSB report:
“Starting the APU early in the accident sequence proved critical because it improved the outcome of ditching by ensuring electrical power was available to the airplane. Further, if the captain had not started the APU, the airplane would not have remained in normal law mode. This critical step would not have been completed if the flight crew had simply followed the order of the items in the checklist”
Captain Sully wasn’t perfect. He did not attain the required speed for his descent and landing, resulting in a high Angle of Attack (AOA). This resulted in significant structural damage to the fuselage on landing which caused water to enter the cabin. The directive on what speed to travel in case both engines failed was on page 2 of the checklist. The pilots only had time to get through page 1 before abandoning the checklist as time ran out. The checklist had been designed for problems at 30,000 feet. The aircraft lost both engines at 3,000 feet. The pilots only had 3 minutes to land the plane. Experience and intuition of a seasoned pilot carried the day. The protocols did not.
In the time of COVID, physicians more than ever find themselves as pretty baubles on display to reassure the public. The reality is that it’s the system that directs physicians and as a result it is the physicians who find themselves unable to protect themselves or their patients. The lessons from the pandemic, and yes, even the airline industry is loud and clear: Put the physicians back in charge.
Anish Koka is a cardiologist in private practice in Philadelphia. Twitter: @anish_koka
The post COVID-19: Physicians in Shackles appeared first on The Health Care Blog.
COVID-19: Physicians in Shackles published first on https://wittooth.tumblr.com/
0 notes