#nontreatable
Text
Boonk Gang Fucking Bitch on Instagram
Ninfetinha linda mandou nude e caiu na Net
leather doll femdom
Namorada caiu na net delirando de prazer na pica grossa desse cara
Ronaldo e Ana Dando leitinho na boca dela
Ava Little like to suck and get nailed from behind
Teen babe eating her perv stepmoms pussy
Reverse anal cowgirl with pretty TS Sol and boyfriend Kai
First anal penetration gay and group young gays rough sex Slim Twink
Chinese Bodybuilder Show
#unmannishly#uglis#peronial#nontreatable#upbring#bridlewise#Copeognatha#heavy-seeming#latcher#Oconee#dunging#austin#Seychelles#harps#subtiliate#half-consumed#tetracadactylity#aswim#time-bent#ingluviitis
0 notes
Text
Big natural boobed amateur housewife fucked in her kitchen
Extremely hairy babe in a FFM threesome
Beautiful Latin nude webcam show
La maman de salope veut la bite
Busty wife anal fucks husband in bondage
Hot and wicked ebony babe gets fat chocolate dick in ass
Yahaira y Coto, pobre foquita
Beautiful gal has passionate sex under shower
Beautiful Girls With Hot Boobs From Snapchat
swathi naidu exposing and compilation
#unpoeticalness#peacekeeping#preresponsibility#wilkin#Tamera#Pattani#intrapsychic#heaven-clear#retests#severalties#hoisting#disembargoed#tracts#romanced#histopathologist#feasibly#dickinson#reinterpreting#freshener#nontreated
1 note
·
View note
Note
An actual question which is pretty popular in the Splatoon fandom, how do you think lings wash themselves? Keep themselves clean. Canonically it is stated that water affects them.
Well I actually think I got a pretty good idea of this one !
I've made a little illustrated guide which pretty much summarizes it all, but here is my thought process beneath it anyways. (Long post buckle up)
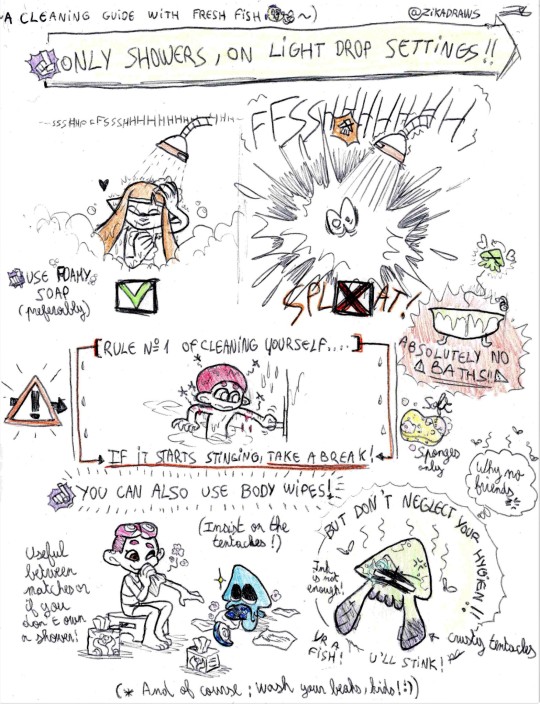
So, while it's true that in my mind their ink is already taking care of most of their dirt, one can only swim into their own body fluids before it starts to reek. Especially while being a(n ink)fish. Besides, enemy ink inevitably creates irritations if not properly cleaned off at least once or twice a day. (Off The Hook advises to clean your tentacles thoroughly after a match canonically.)
Now about the water issue, the main thing to keep in mind is that it's mentioned it dissolves Inkfish, sure, but only if they are submerged in it (because ink is less dense that water). So I think that they can take water drops, although it's also mentioned (in a game dev interview) that their skin actually breaks really easily.
But they CAN clean themselves nevertheless ; they just have to follow a few rules.
-----------
Absolutely NO BATHS.
Showers only, but put on the lightest drop setting, to the point the water feels more like drizzle (the type of rain they endure the best), just enough to get them moist and allow them to get themselves clean.
(There are specially designed shower heads on the marketplace for that, although it's the norm to have a shower with multiple options. It's recommended to always test the shower when looking for a new place, and use a portable spawner for the first times to be extra secure. Also, check your water pressure before going for a shower.)
Be gentle with your skin and tentacles while cleaning. Use foamy soaps, preferably, and soft sponges. If you're too rough, you might break the skin.
Only run the water to get yourself moisturized, then to wash the soaps. Not any more than needed.
At any time, if it starts to sting, or you feel weak, cut the water and take a break. Listen to your body.
If you don't have the time to take a shower, if you're not feeling like it or simply don't have a shower, there are always specialized body wipes available anywhere in stores. Fitting different kinds of skins & tentacles, with various perfumes, they are ideal to be used between Turf Wars or for a quick groom on the go. You can even clean yourself integraly this way if you wish, but please if you must do that in public, do so in Swim Form. Be decent.
(However, keep in mind the body wipes may be somewhat cheap and required to be at least recyclable, and also a huge market/job source, they still represent a budget, and important waste. Avoid resorting to these only. Water is in most places paid for by the community.)
In any way, do not neglect your hygiene. Else you may develop irritations, itching, dry & crusty tentacles (especially in choppy tentacuts), infections if nontreated injuries, and of course bad odor, which gets pretty bad as you count as a fish. All of these can get you mocked of and ostracized, as Freshness comes from having your turf and yourself figured out and taken well care of (we like to show that off), and unlike you may think- YOUR PEERS NOTICE.
And, of course, always brush your beak and scrub your tongue at least twice a day. Bad hygiene within the beak is the least tolerable, squiddos <3
-----------
And so yeah, those are their golden rules when it comes to hygiene. As you can see, I might have gotten a little overboard with it, but I wanted to make it feel like a legit cleaning guide, as I suspect that's something that is taught thoroughly to young Inkfish.
They have various illustrated child books/notices about cleaning safety, and probably have at least one mandatory class about that when they're in elementary school or younger. Being fresh 'n shiny is pretty important, and they are taught to take care of their turf/living space and of themselves, because they need that so they can then properly show off. So they are taught how to do it properly and safely early on, and they're not kidding about that.
I mean in a social system where the store managers can straight up refuse to serve you if you're deemed not fresh enough, you've got to be a little serious when it comes to your personal figure.
Alright, I hope you enjoyed my explanation ! I had a lot of with it~ :))
(Also before I go, I just wanna add a filter I made of this same guide, to make it look like a poorly taken scientific report picture like in a Sunken Scroll, 'cause I thought it was Sunken Scroll material. Enjoy.)
(Thanks for asking, bye 🎵 =:> =:> =:>)
#answered ask#splatoon#splatoon 2#splatoon 3#splatoon headcanons#splatoon headcanon#splatoon theory#splatoon hc#inkling#octoling#and yeah lol that was#captain 3#anyway#long post#scanner#cute
1K notes
·
View notes
Link
#DeeLusby#smallcell#resistantbees#naturalarrangementofhoneycombs#Varroaresistance#breedingselection#workwithnucs#4point9#inevitablecrisis#hiverecord#unlimitedbroodnest#ownexperiencesinVarroaresistance#treatmentfreebeekeeping
0 notes
Text
Where to Buy Decking Wood

Whether you’re a do-it-yourselfer or building your deck as part of a home remodel project, there are many factors to consider. One of them is the material you’ll use for your new deck, which should be chosen based on the type of deck you want to have as well as your budget and aesthetic preferences. For a better overview about deck woods, look here for more info here today.
Choosing the right wood is an important decision, as it will affect your deck’s longevity, maintenance needs, and overall cost. Depending on the wood you choose, you may need to apply a sealer or stain every few years. Alternatively, you might opt for composite boards, which are made from recycled materials and come in a variety of colors and styles.
Aside from looking at the material itself, you should also pay attention to where it came from. Often, woods for outdoor use are sourced from unsustainable sources. Check for Forest Stewardship Council (FSC) certification, which ensures that the wood was harvested responsibly and does not harm the environment.
Softwoods, such as cedar and redwood, are popular choices because they are naturally resistant to rot and insects. However, these species will need to be treated with a preservative or stain every couple of years to extend their lifespan and maintain their vibrant color.
For a more natural look, try using a combination of both hardwood and softwood. Both contain oils that resist decay and insects, but hardwoods tend to require more frequent treatment than softwoods do, including staining or applying a wood preservative.
Imported lumber, such as ipe or cumaru, can be a more expensive choice but are extremely durable. If you plan to spend a lot of time on your deck, these exotic woods can be a good option.
Modified wood, like Kebony, takes sustainable softwoods and adds a non-toxic liquid that changes the wood cell structure to make it more dense, similar to tropical hardwoods such as mahogany and teak. This gives it better dimensional stability and makes it more resistant to termite damage.
In addition, modified wood can be a great option for homeowners who have kids and pets because it contains no harmful chemicals and is safe to play on. It comes in both clear and character grades, so you can select the look that suits your family’s preferences.
Pressure-treated lumber is another popular option, as it can be readily found and is easy to work with. It’s permeated with chemicals that deter insects and inhibit mold and mildew. But it’s important to wear protective gear while working with it, as the chemicals can be toxic if inhaled.
Aside from being easy to find and cut, pressure-treated lumber can be relatively inexpensive. But the chemicals that are applied to it can be expensive, so you may end up spending more on maintenance than you would with a higher-quality, nontreated deck.
As with all types of materials, wood’s longevity will depend on how much care you take of it. You’ll want to make sure that you can get at least 10 years out of it before replacing your deck. The best way to do that is by ensuring that you have a high-quality, UV-inhibiting penetrating oil on hand that will help preserve its beautiful color and keep it in good condition. Check out this related post to get more enlightened on the topic: https://en.wikipedia.org/wiki/Deck_(building).
0 notes
Text
Eating tomato sauce while lounging on furniture makes upholstery
Eating tomato sauce while lounging on furniture makes upholstery vulnerable to red sauce stains. Tomato sauce permeates upholstery and eventually dries, leaving furniture blemished with crusty, red stains. Like all food stains, tomato sauce is best removed when fresh. The longer the red sauce lingers on furniture, the more difficult upholstery becomes to restore. Promptly remove red tomato sauce from upholstery using basic, convenient techniques.Not easy but you need to try. Blot spills immediately with a clean, 28/410 trigger sprayer white cloth, and then clean the spot as quickly as you can. The more time that elapses, the more difficult it will be to remove stains.Scrape as much of the excess as possible with a spatula. Apply a wet spotter and work into the fabric.
Rinse thoroughly with water and launder. If laundering must wait, and there is any stain remaining, apply an enzyme presoak paste and let it work awhile, keeping the paste moist. Thoroughly rinse area to remove all traces of enzyme presoak paste. Allow to dry and launder as soon as possible.For the wooden type, wiping these surfaces with a damp cloth is sufficient to remove the spill. Nontreated surfaces should be wiped immediately with a cloth dipped in warm sudsy water, rinsed with a clean damp cloth, wiped dry, and polished or waxed as usual.Easy StepsUpholstery1. Mix one tablespoon of liquid hand dishwashing detergent with two cups of cool water.2. Using a clean white cloth, sponge the stain with the detergent solution.3. Blot until the liquid is absorbed.4. Repeat Steps 2 and 3 until the stain disappears.5. Sponge with cold water and blot dry.More Steps if the easier steps wont work in upholstery cleaningBlot up excess red sauce off the upholstery's surface using paper towels. Do not rub the sauce stain, as this smears it.Add cool water to a spray bottle. Douse the remaining sauce stain with the water.
Let the sauce-stained upholstery soak for one minute.Blot the moistened stain with fresh paper towels. Lift as much red sauce from the upholstery as possible.Prepare a detergent solution if stubborn red sauce remains in the upholstery. Fill a cleaning pail with 2 cups of cold water, and then stir in 1 tablespoon of bleach-free liquid dishwashing detergent.Dampen a cloth with the solution. Using the moist cloth, tamp the remaining red sauce stain until it disappears completely.Moisten another cloth with cool water. Blot the previously stained area, thoroughly rinsing the upholstery.Blot the damp upholstery with a towel. Absorb as much moisture as possibleSeek pros assistance if still persist, check out Auckland Upholstery Cleaning for reliable assistance needed
0 notes
Text
The RNA Verteporfin readers YTHDC1 silences retrotransposons along with guards Puede ser cellular id
2009 occasions greater than that will in the gasoline phase. For the time being, whilst response there was a time Forty minimum as well as comparable humidity has been 70%, your concentration of HONO and p-NP created upon alpha-Fe2O3 a new surface area had been about Three or more.55 and a pair of.1951 times more than those who work in your gasoline stage, along with the generate of p-NP had been Three.74% and a couple of.99%, respectively. Surfaces impact performed a respected position within photochemical result of HNO3 as well as benzene on alpha-Fe2O3 surface. (C) This year Elsevier N.Sixth is v. Almost all protection under the law set aside.A couple of studies ended up executed to discover exactly how application of the particular cytokinin benzyladenine (BA) affected blooming inside Doritaenopsis along with Phalaenopsis orchid identical dwellings. From the first test, two vegetative orchid clones developing throughout 15-cm cooking pots were transferred from the 28 diplomas C techniques in which restricted blooming to a 23 diplomas Chemical techniques regarding blossom induction (day 0). A foliar apply (0.Only two D michael(-2)) made up of BA at #Link# Hundred, Two hundred, or even 500 milligrams M(-1) as well as Twenty five, Fifty, or even A hundred milligram D(-1) everyone of BA and also gibberellins The(4) + A(6) (BA+GA) was applied to days and nights Zero, Seven, and 14. Vegetation treated with BA by yourself in Two hundred as well as 400 milligrams M(-1) a visible inflorescence 3-9 days and nights earlier coupled with an average associated with 0 #Link# .7-3.A few far more inflorescences along with 3-8 more plants per place as compared to nontreated crops. The use of BA+GA did not have any effect on inflorescence number and also overall bloom amount at the costs screened. In the second experiment, three orchid identical dwellings obtained one particular foliar bottle of spray of BA in 2 hundred milligrams D(-1) from six to eight time details in accordance with time of shift through Twenty nine diplomas C in order to Twenty-three levels D (-1, Zero, +1, +2, +4, or even +6 several weeks). Another number of #Link# plant life acquired the BA request from week Zero but has been preserved from Twenty nine certifications C. Inflorescence range was greatest in all of the about three orchid identical dwellings when crops had been addressed with BA 7 days as soon as the temperature exchange. Vegetation that have been painted using BA and also maintained at 30 diplomas H did not trigger inflorescences. The particular promotion involving its heyday by the application of BA points too cytokinins at the very least partially get a grip on inflorescence initiation regarding Doritaenopsis along with Phalaenopsis, however its marketing is actually depending and BA program can't entirely alternative to a good inductive low temperature.Your mammalian goal associated with rapamycin (mTOR) signa ling community handles cell growth, expansion as well as mobile emergency. Deregulated account activation on this pathway is a kind of occasion in varied man ailments like cancers, cardiac hypertrophy, vascular restenosis and nephrotic hypertrophy. Though mTOR chemical, rapamycin, has become trusted in order to prevent the aberrant signaling on account of mTOR account activation that will plays a major position in hyperproliferative conditions, in some instances rapamycin doesn't attenuate the mobile or portable expansion as well as emergency.
0 notes
Text
Pseudomeningocele Together with Orbital Expansion being a Side-effect regarding Fronto-Orbital Development along with Trametinibg in Craniosynostosis
09). These information advise the inflamation related walkway mediated simply by mast mobile service can be involved in shared tablet fibrosis after upsetting injury.Any growth-chamber research has been performed to determine precisely how foliar illness or injuring affects light beer Only two phylloplane yeasts (Rhodotorula glutinis and also Cryptococcus laurentii) to be able to colonize simply leaves of high fescue (Festuca arundinacea). Yeasts were utilized separately and collectively onto healthy simply leaves, leaves infected with Rhizoctonia solani (unhealthy), and also mechanically hurt (hurt) simply leaves. In most Three #Link# trial offers, the actual foliage disruption treatment method considerably #Link# afflicted the actual abundance associated with fungus on the phylloplane regarding taller fescue. Candida large quantity for the unhealthy as well as hurt results in was drastically more than around the nontreated, healthy foliage. By 50 percent in the Three or more studies, the thrush kinds employed furthermore had a substantial relation to thrush plethora. Normally, Ur. glutinis had been a lot more considerable compared to Chemical. laurentii when used individually, and not considerably higher than the whole fungus colony-forming devices from the co-inoculated remedy. If the Only two yeasts had been co-inoculated onto the simply leaves, Third. glutinis comprised 89.7%, 75.4%, and 67.6% with the retrieved thrush colony-forming devices on wholesome, unhealthy, and hurt simply leaves, professionally. Each of our info advise that these kinds of A couple of varieties of yeasts will differentially colonize affected foliage muscle using illness as well as wounds favoring numbers of R. glutinis above D. laurentii.Your phylogenetic relationships from the main lineages in the arachnid get #Link# Pseudoscorpiones are usually looked at initially using molecular sequence files through a couple of nuclear ribosomal family genes then one mitochondrial protein-encoding gene. The info ended up reviewed using a vibrant homology strategy with the brand-new plan POY /.4 below parsimony because optimality criterion. Your data display monophyly of Pseudoscorpiones as well as many of the superfamilies (Feaelloidea, Chthonioidea, Cheiridioidea as well as Sternophoroidea), although not for Neobisiodea or perhaps Garypoidea. Cheliferoidea wasn't monophyletic both because of the situation involving Neochelanops, that assembled with some garypoids. In all the examines, Feaelloidea constituted your sister group to any or all additional pseudoscorpions; Chthonioidea is the cousin party on the leftover family members, which usually make up the gang locheirata sensu Harvey-a clade including pseudoscorpions together with venom glands within the pedipalpal fingers. This particular phylogenetic design shows that venom glands advanced one time in this particular buy associated with arachnids. (C) 08 Elsevier Inc. Just about all privileges set-aside.pi-Conjugated phosphasilenes having a selection of aryl substituents about the silicon atom are already synthesized through a 1,A single,3,Several,Five,A few,7,7-octaethyl-s-hydrindacen-4-yl (Eind) class. X-ray structural analysis exhibits your remarkably coplanar pi-framework stabilized through the perpendicularly fixed Eind teams. Your solid pi-pi* absorptions have been noticed, demonstrating the actual off shoot of pi-conjugation over the bones. The particular DFT data suggest that this LUMO necessitates the large info of the 3p pi*(Si- P)-2p(private investigator)1 .(co2 pi-electron system) conjugation. The particular electrochemical properties with the phosphasilens may also be presented.
0 notes
Text
One more thing between Jaskier and Geralt and then I gotta go to bed because this show has had me up for 22 hours:
We realize that had Yenn not said anything about seeing Jaskier in Oxenfurt, Geralt would’ve never gone to get our Bard out of that jail, right? And we realized that Geralt only went to Oxenfurt because Yenn absconded with Ciri and Geralt knew Jaskier had information about Yenn.
No, what’s up Jaskier? Where’s your lute Jaskier? Why are you in prison Jaskier? Nope, Geralt is only about was Jaskier can do for him. Heck, he doesn’t even ask Yarpin for two horses, nope, I guess the Bard can walk. (Although to be fair, does Joey even want to ride a horse? I can’t speak for him, but I’m terrified of horses.)
Then he drags poor Jaskier on this adventure, gets him mixed up in this danger that could’ve killed him and only Yenn acknowledges his existence after they get back through the portal. Like I realized you’re a responsible Dad now, Geralt, but my goodness, be a better friend already!
#witcher spoilers#jaskier#geralt#is this friendship?#I have concerns#esp. if they don't sort this before they get to the events of Baptism of Fire#it is my fav#but also Jaskier follows Geralt everywhere#and they never explain why#and it's a crapfest#that book drives me nuts#and so does Geralt's nontreatment of Jaskier#but also Jask baby#have a little self respect#because you're awesome#and more people should treat you that way
37 notes
·
View notes
Text
Take advantage of valentine's day flower sales. You can use the dried, pressed, or plucked flowers as decor, ingredients(if you're using them for anything you'll be ingesting, applying to your skin, or burning, only use food safe nontreated flowers), offerings, etc. Remember to look up the meanings of the flowers before you use them.
1K notes
·
View notes
Link
Medicine’s Fundamentalists
The randomized control trial controversy: Why one size doesn’t fit all and why we need observational studies, case histories, and even anecdotes if we are to have personalized medicine
BY NORMAN DOIDGE
AUGUST 14, 2020
If the study was not randomized, we would suggest that you stop reading it and go on to the next article.
—Quote from Evidence-Based Medicine: How to Practice and Teach EBM
Why is it we increasingly hear that we can only know that a new treatment is useful if we have a large randomized control trial, or “RCT,” that has positive results? Why is it so commonly said that individual case histories are “mere anecdotes” and count for nothing, even if a patient, who has had a chronic disease, suddenly gets better with a new treatment after all others failed for years—an assertion that seems, to many people, to run counter to common sense?
Indeed, some version of the statement, “only randomized control trials are useful” has become boilerplate during the COVID-19 crisis. It is uttered as though it is self-evidently the mainstream medical position. When other kinds of studies come out, we are told they are “flawed,” or “fatally flawed,” if not RCTs (especially if the commentator doesn’t like the result; if they like the result, not so often). The implication is that the RCT is the sole reliable methodological machine that can uncover truths in medicine, or expose untruths. But if this is so self-evident, why then, do major medical journals continue to publish other study designs, and often praise them as good studies, and why do medical schools teach other methods?
They do because, as extraordinary an invention as the RCT is, RCTs are not superior in all situations, and are inferior in many. The assertion that “only the RCTs matter” is not the mainstream position in practice, and if it ever was, it is fading fast, because, increasingly, the limits of RCTs are being more clearly understood. Here is Thomas R. Frieden, M.D., former head of the CDC, writing in the New England Journal of Medicine, in 2017, in an article on the kind of thinking about evidence that normally goes into public health policy now:
Although randomized, controlled trials (RCTs) have long been presumed to be the ideal source for data on the effects of treatment, other methods of obtaining evidence for decisive action are receiving increased interest, prompting new approaches to leverage the strengths and overcome the limitations of different data sources. In this article, I describe the use of RCTs and alternative (and sometimes superior) data sources from the vantage point of public health, illustrate key limitations of RCTs, and suggest ways to improve the use of multiple data sources for health decision making. … Despite their strengths, RCTs have substantial limitations.
That, in fact, is the “mainstream” position now, and it is a case where the mainstream position makes very good sense. The head of the CDC is about as “mainstream” as it gets.
The idea that “only RCTs can decide,” is still the defining attitude, though, of what I shall describe as the RCT fundamentalist. By fundamentalist I here mean someone evincing an unwavering attachment to a set of beliefs and a kind of literal mindedness that lacks nuance—and that, in this case, sees the RCT as the sole source of objective truth in medicine (as fundamentalists often see their own core belief). Like many a fundamentalist, this often involves posing as a purveyor of the authoritative position, but in fact their position may not be. As well, the core belief is repeated, like a catechism, at times ad nauseum, and contrasting beliefs are treated like heresies. What the RCT fundamentalist is peddling is not a scientific attitude, but rather forcing a tool, the RCT, which was designed for a particular kind of problem to become the only tool we use. In this case, RCT is best understood as standing not for Randomized Control Trials, but rather “Rigidly Constrained Thinking” (a phrase coined by the statistician David Streiner in the 1990s).
Studies ask questions. Understanding the question, and its context, is always essential in determining what kind of study, or tool, to use to answer those questions. In the “RCT controversy,” to coin a phrase, neither side is dismissive of the virtues of the RCT; but one side, the fundamentalists, are dismissive of the virtues of other studies, for reasons to be explained. The RCT fundamentalist is the classic case of the person who has a hammer, and thinks that everything must therefore be a nail. The nonfundamentalist position is that RCTs are a precious addition to the researcher’s toolkit, but just because you have a wonderful new hammer doesn’t mean you should throw out your electric drill, screwdriver, or saw.
So let’s begin with a quick review of the rationale for the “randomized” control trial, and their very real strengths, as originally understood. It’s best illustrated by what happens without randomization.
Say you want to assess the impact of a drug or other treatment on an illness. Before the invention of RCTs, scientists might take a group of people with the illness, and give them the drug, and then find another group of people, with the same illness, say, at another hospital, who didn’t get the drug, and then compare the outcome, and observe which group did better. These are called “observational studies,” and they come in different versions.
But scientists soon realized that these results would only be meaningful if those two groups were well matched in terms of illness severity and on a number of other factors that affect the unfolding of the illness.
If the two groups were different, it would be impossible to tell if the group that did better did so because of the medication, or perhaps because of something about that group that gave it an advantage and better outcome. For instance, we know that age is a huge risk factor for COVID-19 death, probably because the immune system declines as we age, and the elderly often already have other illnesses to contend with, even before COVID-19 afflicts them. Say one group was, on average, 60 years old, and all the members got the drug, and the other group was on average 75 years old, and they were the ones that didn’t get the drug. Say that when results were analyzed and compared, they showed the younger group had a higher survival rate.
A naive researcher might think that he or she was measuring “the power of the medication to protect patients from COVID-19 death” but may actually have also been measuring the relative role of youth, in protecting the patients. Scientists soon concluded there was a flaw in that design, because we do not know, with any reasonable degree of confidence, whether the better outcomes were due to age or the medication.
Age, here, is considered a “confounding factor.” It is called a confounding factor, because it causes confusion, because age can also influence the outcome of the study in the group as a whole. Other confounding factors we know about in COVID-19 now include how advanced the illness is at the time of the study, diabetes, obesity, heart disease, and probably the person’s vitamin D levels. But there could easily be, and probably are, many other confounding factors we don’t know, as of yet. There are even potential confounding factors that we suspect play a role, but are not quite certain about: the person’s general physical fitness, the ventilation in their home, and so on.
This is where randomization is helpful. In a randomized control trial, one takes a sufficiently large group of patients and randomly assigns them to either the treatment group, or the nontreatment (“placebo” or sugar pill) control group, for instance. Efforts are made to make sure that apart from the treatment, everything else remains the same in the lives of the two groups. It is hoped that by randomly assigning this large number of patients to either the treatment or nontreatment condition, that each of the confounding factors will have an equal chance of appearing in both groups—the factors we know, such as age, but also mysterious ones we don’t yet understand. While observational studies can, with some effort, match at least some confounding factors we do understand in a “group matched design” (and, for instance, make sure both groups are the same age, or disease severity), what they can’t do is match confounding factors we don’t understand. It is here, that RCTs are generally thought to have an advantage.
With such a good technique as RCTs, one might wonder, why do we ever bother with observational studies?
There are a number of situations in medicine in which observational studies are obviously superior to randomized control trials (RCTs), such as when we want to identify the risk factors for an illness. If we suspected that using crack cocaine was bad for the developing brains of children, it would not be acceptable to do an RCT (which would take a large group of kids, and randomly prescribe half of them crack cocaine and the other half a placebo and then see which group did better on tests of brain function). We would instead follow kids who had previously taken crack, and those who never had, in an observational study, and see which group did better. All studies ask questions, and exist in a context, and the moral context is relevant to the choice of the tool you use to answer the question. That is Hippocrates 101: Do no harm.
Now, you might say that a study of risk factors is very different from the study of a treatment. But it is not that different. There can be very similar moral and even methodological issues.
In the 1980s, quite suddenly, clinicians became aware that infants were dying, in large numbers, in their cribs, for reasons that couldn’t be explained, and a new disorder was discovered, sudden infant death syndrome, or SIDS, or “crib death.” Some people wondered if parents were murdering their children, or if it was infectious, and many theories abounded. A large observational study was done in New Zealand that observed and compared factors in the lives of the infants who died and those who didn’t. The study showed that the infants who died were frequently put to sleep on their tummies. It was “just” an observation. But on that basis alone, it was suggested that having infants sleep on their backs might be helpful, and that parents should avoid putting their infants on their fronts in their cribs. Lo and behold, the rates of infant death radically diminished—not completely, but radically. No sane caring person said: “We should really do an RCT, rule out confounding factors, and settle this with greater certainty, once and for all: All we have to do is randomly assign half the kids to be put to bed on their tummies and the other half on their backs.” That would have been unconscionable. The evidence provided by the observational study was good enough.
Again, all studies have a context and are a means to answering questions. The pressing question with SIDS was not: How can we have absolute certainty about all the causes of SIDS? It was: How can we save infant lives, as soon as possible? In this case, the observational study answered it well.
The SIDS story is a case where we can see how close, in moral terms, a study of risk factors and a study of a new treatment can be in a case where the treatment might be lifesaving. Putting children on their tummies is a risk factorfor SIDS. Putting them on their backs is a treatment for it. The moral issue of not harming research subjects by subjecting them to a likely risk is clear.
Similarly, withholding the most promising treatment we have for a lethal illness is also a moral matter. That is precisely the position taken by the French researchers who thought that hydroxychloroquine plus azithromycin was the most promising treatment known for seriously ill COVID-19 patients, and who argued that doing an RCT (which meant withholding the drug from half the patients) was unconscionable. RCT fundamentalists called their study “flawed” and “sloppy,” implying it had a weak methodology. The French researchers responded, in effect saying, we are physicians first; these people are coming to us to help them survive a lethal illness, not to be research subjects. We can’t randomize them and say to half, sorry, this isn’t your lucky day today, you are in the nontreatment group.
There are other advantages to observational studies in assessing new treatments. They are generally lower in cost than RCTs, and can often be started more quickly, and published more rapidly, which helps when information is needed urgently, as in a novel pandemic when little is understood about the illness. (RCTs, in part because of the moral issues, take longer to get ethics approval.) Observational studies are also easier to conduct at a time when patients are dying in high numbers, and hospital staff is overwhelmed, trying to keep people alive. They can involve looking back in time, to make use of observations in the medical chart. In such cases, it is crucial that the initial observations about how patients responded to the medications and treatments that the staff had on hand is documented, in as systematic as way as is possible, because there might be clues and nuggets as to what worked.
Exclusion Criteria: Do RCTs Study Real-World Patients?
But there are also problems at the conceptual heart of the RCT. Often the RCT design sees “confounding factors” not simply as something that has to be balanced between the treatment and no-treatment groups by randomization, but eliminated at the outset. For a variety of reasons, includinga wish to make interpretation of final results more certain, they aggressively eliminate known confounding factors before the study starts, by not letting patients with certain confounding factors get into the study in the first place. They do this by often having a lot of what are called “exclusion criteria,” i.e., reasons to exclude or disqualify people from entering the study.
Thus, RCTs for depression typically study patients who only have depression and no other mental disorders, which might be confounding factors. So, they usually study people who are depressed but who are not also alcoholic, not on illicit drugs, and who don’t have personality disorders. They also tend to exclude people who are actively suicidal (because if they are, they might not complete the expensive study, and some people think it is unethical to give a placebo to a person in acute risk of killing themselves). There are many other reasons given for different exclusions, such as a known allergy to a medication in the study.
But here’s the problem. These exclusions often add up until many, maybe even most, real-world depressives get excluded from such a study. So, the study sample is not representative of real-world patients. Yet this undermines the whole purpose of a research study “sample” in the first place, which is to test a small number of people (which is economical to do), and then extrapolate from them on to the rest of the population. As well, many studies of depression and drugs end up looking at people who are about as depressed as a college student who just got a B+ and not an A on a term paper. This is why many medications (or short-term therapies) end up doing well in short-term studies, but the patients relapse.
If you are a drug company (which pay for most of these studies) and you’re testing your new drug, exclusion criteria can be made to work in favor of making your drug appear more powerful than it really is, if sicker patients are eliminated. (This is a good trick, especially if your goal of making money from the drug is your first priority.)
This isn’t a matter of conjecture. This question of whether RCTs, in general, are made up of representative samples has been studied. An important review of RCTs found that 71.2% were not representative of what patients are actually like in real-world clinical practice, and many of the patients studied were less sick than real-world patients. That, combined with the fact that many of the so-called finest RCTs, in the most respected and cited journals, can’t be replicated 35% of the time when their raw data is turned over to another group that is asked to reconfirm the findings, shows that in practice they are far from perfect. That finding—that something as simple as the reanalysis of the numbers and measurements in the study can’t be replicated—doesn’t even begin to deal with other potential problems in the studies: Did the author ask the right questions, collect appropriate data, have reliable tests, diagnose patients properly, use the proper medication dose, for long enough, and were their enough patients in it? And did they, as do so many RCTs, exclude the most typical and the sickest patients?
Note, other study designs also have exclusion criteria, but they often are less problematic than in RCTs for reasons to be explained below.
The Gold Standard and the Hierarchy of Evidence
So, why is it we also hear that “RCTs are the gold standard,” and the highest form of evidence in the “hierarchy of evidence,” with observational studies beneath them, and case histories, at the bottom, and anecdotes beneath contempt?
There are several main reasons.
The first you just learned. It had been believed that RCTs were a completely reliable way to study a treatment given to a small sample of people in a population, see how they did, and then one could extrapolate those findings to the larger population. But that was just an assumption, and now that we have learned the patients studied are too often atypical, we have to be very careful about generalizing from an RCT. This embarrassment is a fairly recent finding that has yet to be taken fully into account by those who say RCTs are the gold standard.
The second reason has to do with the fundamentalists relying on outdated science, which argued that RCTs are more reliable in their quantitative estimates of how effective treatments are because they randomize and rule out confounding factors.
But a scientist who wanted to know if RCTs, as a group, were universally better and more reliable than observational studies at truth-finding would actually study the question scientifically, and not just assert it. And, in the 1980s, Chalmers and others did just that, examining studies from the 1960s and 1970s. They found that in the cases where both RCTs and observational studies had been done on the same treatment, the observational studies yielded positive results 56% of the time, whereas blinded RCTs did so only 30% of the time. It thus seemed that observational studies probably exaggerated how effective new treatments were.
Three other reviews of comparisons of observational and RCT study outcomes showed this same difference, and so researchers concluded that RCTs really were likely better at detecting an investigator’s bias for the treatment being studied, and hence more reliable. Since many scientific studies of drugs were paid for by drug companies that manufactured those drugs, it was not a surprise that the studies would have biases. These reviews formed much of the basis for RCT fundamentalism.
Just because an RCT is performed and published is no reason to assume it doesn’t exaggerate efficacy.
Share→︎TwitterFacebookEmailPrintLinkCopied link
But here’s the problem: These were reviews of studies that were done in the 1960s and 1970s. Once the observational study researchers became aware of the problem, they upped their game, and improved safeguards.
In 2000, new reviews comparing the results from hundreds of RCTs and observational studies in medicine that had been conducted in the 1990s were conducted by scientists from Yale and Iowa College of Medicine. They found that the tendency of observational studies to suggest better results in treatments had now disappeared. They now got similar results to RCTs. This was an important finding, but it has not been sufficiently integrated into the medical curriculum.
There is another reason we hear about RCTs. As RCTs became the type of study favored by regulatory bodies to test new drugs, they rose to prominence, and drug companies upped their game and learned many ingenious ways to make RCTs exaggerate the effectiveness of the drugs they are testing.
Entire books have been written on this subject, an excellent one being Ben Goldacre’s Bad Pharma: How Drug Companies Mislead Doctors and Harm Patients.Since, to bring a drug to market requires only two RCTs showing the drug works, these techniques include doing many studies but not publishing the ones that don’t show good results. But there are sneakier techniques than making whole studies with negative outcomes go missing. There are ways to publish studies but hide embarrassing data; publish the good data in well-known journals and the negative findings in obscure journals; not study short-term side effects; almost never study, or ask about, long-term side effects; or play with measuring scales, so that patients appear to achieve statistically meaningful benefits which make no clinical difference. If you do a study that gives you a bad outcome on your key measure, don’t report that, just find some small outcome that was in your favor and retroactively change the goal of the study, to report that benefit and that alone. Make researchers and subjects sign gag clauses and nondisclosures. Have the drug companies ghostwrite the papers, make up the tables, and get academics, who never see the raw data sign them. This is routine.
The list goes on, and those tricks have often been used, successfully, to gain approval for drugs. Becoming very familiar with these ruses can save lives, because in a pandemic, new drugs will earn Big Pharma billions because the illness is so widespread, and they have a large playbook to draw from. Once two RCTs are selected from the many done to take the drug forward, the propaganda campaign begins, and as Goldacre shows, drug companies spend twice as much on marketing as they do on research. So, to repeat, just because an RCT is performed and published is no reason to assume it doesn’t exaggerate efficacy.
One group of studies, though, that don’t often play by these corrupt rules are RCTs done on already generic drugs, because they are off-patent, and there is really very little money to be made in them. In these cases, when a drug company has a generic rival to what might be a big money maker, there are ways of making that generic look bad. If the generic takes four weeks to work, test your drug against it, in a three-week study (the placebo effect for your drug won’t have worn off yet). If a vitamin is threatening your drug, test your drug against it, but use the cheapest version, in a dose that is too low. It’s an RCT, that’s all that matters.
Despite all this, advocates of RCTs still teach that, all else being equal, RCTs are always more reliable, and teach this by cherry-picking well-known cases where RCTs were superior to observational studies, and ignore cases where observational studies have been superior, or at least the better tool for the situation. They take the blunt position that “RCTs are better than observational studies,” and not, the more reasonable, accurate, and moderate, “All else being equal, in many, but not all situations, RCTs are better than observational studies.”
The phrase, “all else being equal,” is crucial, because so often all else is not equal. Simply repeating “RCTs are the gold standard of evidence-based medicine” implies to the naive listener that if it is an RCT then it must be a good study, and reliable, and replicable. It leaves out that most studies have many steps in them, and even if they have a randomization component, they can be badly designed in a step or two, and then lead to misinformation. Then there is the very uncomfortable fact that, so often, RCTs can’t even be replicated, and so often contradict each other, as anyone who has followed RCTs done on their own medical condition often sadly finds out. A lot of this turns out to be because they have many steps, and because Big Pharma is so adept now at gaming the system. Like gold, they turn out to be valuable but also malleable. A lot of the problem is that patients differ far more than these studies concede, and these complexities are not well addressed in the study design.
The Hierarchy-of-Evidence Notion Does Harm, Even to RCTs
One of the peculiar things about current evidence-based medicine’s love affair with its “hierarchy of evidence” is that it is still proceeding along, ignoring the implications of the scientifically documented replication crisis. True, the fact there is a replication crisis is now widely taught, and known about, but to the fundamentalists, it is as though that “crisis” doesn’t require that they reexamine basic assumptions. The replication crisis is compartmentalized off from business as usual and replaced with RCT hubris.
The irony is that the beauty of the RCT is that it’s a technique designed to neutralize the effects of confounding factors that we don’t understand on a study’s outcome, and thus it begins in epistemological humility. The RCT, as a discovery, is one of humanity’s wonderful epistemological achievements, a kind of statistical Socrates, which finds that wisdom begins with the idea, “whatever I do not know, I do not even suppose I know” (Apology, 21d).
But that beautiful idea, captured by a fundamentalist movement, has been turned on its head. The way the RCT fundamentalist demeans other study designs is to judge all those designs by the very real strengths of RCTs. This exaggeration is implicit in the tiresome language they use to discuss them: The RCTs are the “gold standard,” i.e., against which all else is measured, and the true source of value. Can these other designs equal the RCT in eliminating confounders? No. So, they are inferior. This works, as long as one pretends there are no epistemological limitations on RCTs. The problem with that attitude is, it virtually guarantees that the RCT design will not be improved, alas, because improved RCTs would benefit everyone. In fact, RCTs would be most quickly improved if the fundamentalists thought more carefully about the benefits of other studies, and tried to incorporate them, or work alongside them in a more sophisticated way. That is another way of saying we need the “all available evidence” approach.
The Case History and Anecdotes
Also disturbing, and, odd, actually, is the belittling of the case history as a mode of making discoveries, or what it has to offer science as a form of evidence. In neurology, for instance, it was the individual cases, such as the case of Phineas Gage, that taught us about the frontal lobes, and the case of H.M., that taught us about the role of memory, two of the most important discoveries ever made in brain science.
Here’s how the belittlement goes. “Case histories are anecdotes, and the plural of anecdote is not data, it is just lots of anecdotes.”
First of all, case histories are not anecdotes. An anecdote, in a medical text, is usually several sentences, at most a paragraph, stripped of many essential details, usually to make a single point, such as “a 50-year-old woman presented with X disease, and was treated with Y medication, for 10 days, and Figure 7 shows her before and after X-rays, and the dramatic improvement.” In that sense, an anecdote is actually the opposite of a case history, which depends on a multiplicity of concrete, vivid details.
A case history (particularly in classic neurology or psychiatry) can run for many pages. It is so elaborated because it understands, as the Canadian physician William Osler pointed out: “The good physician treats the disease; the great physician treats the patient who has the disease.” And who that patient is—their strengths, weaknesses, their other illnesses, other medications, emotional supports, diet, exercise habits, bad habits, genetics, previous treatment histories, all factor into the result. To practice good medicine, you must take it all into account, understanding that the patient is not any one of these details, but a whole who is more than the sum of the parts. Thus, true patient-centered medicine necessarily aspires toward a holistic approach. So, a case history is a concrete portrait of a real person, not an anecdote; and it is vivid, and the furthest thing possible from an abstract data set.
A typical RCT describes several data points about hundreds of patients. A typical case history describes perhaps hundreds of data points about a single patient. It’s not inferior, it’s different. The case history is, in fact, a technology, albeit an old one, set in language (another invention, we forget) and its structure (what is included in the case history, such as descriptions of the patient’s symptoms, objective signs, their subjective experiences, detailed life history, what makes the illness better, what worse, etc.) was developed over centuries.
Even anecdotes have their place. We often hear methodologists say, when a physician claims he or she gave a patient a particular medication, or supplement, or treatments, and they got better, “that that proves nothing. It is just an anecdote.” The problem is in the word “just.” Something doesn’t become meaningless, or a nonevent because a scientist adds the word “just” before it. That word really says nothing about the anecdote and a lot about the speaker’s preference for large number sets.
But anecdotes are very meaningful, too, and not just when lives are changed by a new treatment for the first time. This dismissive indifference to anecdotes turns out to be very convenient, for instance, for drug companies. If you are a physician, and you give a patient who had perfectly good balance an antibiotic, like gentamicin, and she suddenly loses all sense of balance because it injured her balance apparatus, the drug maker can say that is “just” an anecdote. It doesn’t count. And in fact, it is a fairly rare event. But it is by just such anecdotes that we learn of side effects, in part because (as I said above) most RCTs for new drugs don’t ask about those kinds of things, because they don’t want to hear the answer.
If we are to be honest, evidence-based medicine is, in large part, still aspirational. It is an ideal.
That’s why the approach I take—and I think most trained physicians with any amount of experience and investment in their patients’ well-being also take—might be called the all-available-evidence approach. This means, one has to get to know each of the study designs, their strengths, and their weaknesses, and then put it all together with what one is seeing, with one’s own eyes, and hearing from the particular patient who is seeking your care. There are no shortcuts.
One of the implications of this approach in the current COVID-19 situation is that we cannot simply, as so many are insisting, rely only on the long-awaited RCTs to decide how to treat COVID-19. That is because physicians in the end don’t treat illnesses, they treat patients with illnesses, and these patients differ.
The RCTs that are on the way may recommend, in the end, one medication as “best” for COVID-19. What does that mean? That it is best for everyone? No, just that in a large group, it helped more people than other approaches.
That information—which medication is best for most people, is very useful if you are in charge of public health for a poor country and can only afford one medication. Then you want the one that will help most people.
But if you are ordering for a community that has sufficient funds for a variety of medications, you are interested in a different question: What do I need on hand to cover as many sick people as possible, and not just those who benefit from medication X which helps most, but not all people? Even if a medication helps, say, only 10% of people, those will be lives saved, and it should be on hand. A medication that helped so few might not even have been studied, but if the others failed, it should be tried.
A physician on the frontline wants, and needs, access to those medications. He or she asks, “What if my patient is allergic to the medication that helps most people? Then, what others might I try?” Or, “What if the recommended medication is one that interacts negatively with a medication that my patient needs to stay alive for their non-COVID-19 condition?”
There are so many different combinations and permutations of such problems—and hardly any of them are ever studied—that only the physician who knows the patient has even a chance of making an informed decision. They are the kinds of things that arise on physician chat lines, that ask questions to 1,000 online peers like, “I have a patient with heart disease, on A, B, and C meds, and kidney disease on D, who was allergic to the COVID-19 med E. Has anyone tried med F, and if so, given their kidney function, should I halve the dose?”
Evidence-based medicine hasn’t studied some of the most basic treatments with RCTs or observational studies, never mind these kinds of individual complexities. So, the most prudent option is to allow the professional who knows the patient to have as much flexibility as possible and access to as many medications as possible. If we are to be honest, evidence-based medicine is, in large part, still aspirational. It is an ideal. Clinicians need latitude, and patients assume they have it. But now the RCT fundamentalists are using the absence of RCTs for some drugs to restrict access to them. They have gone too far. This is epistemological hubris, at the expense of lives, and brings to mind the old adage, “Absence of evidence is not evidence of absence.” As long as we’ve not got the best studies for all conceivable permutations, medicine will remain both an art and a science.
So, does conceding as much and giving the clinician latitude mean I don’t believe in science?
“Believe,” you say?
That is not a scientific word. Science is a tool. I don’t worship tools. Rather, I try to find the right one for the job. Or, for a complex task, which is usually the case in medicine—especially since we are all different, and all complex—the right ones, plural.
#medicine#fav#print this off later#family medicine#internal medicine#philosophy#science#covid-19#sars-cov-2#covid-19 vaccine
3 notes
·
View notes
Text
Tarantula Care basics:
I've gotten tired of typing out "beginner tips" when people ask for them in Facebook groups, so I'm posting this as a resource to anyone who wants to get a tarantula but needs a place to start with researching. Please research elsewhere as well and be aware that there are many people who are successful at keeping tarantulas that may disagree on certain husbandry topics. This information is based off of the research I've done and how I care for my tarantulas. I may not be an expert with decades of experience, but I am a science minded individual who did a lot of research before getting my first tarantula and who has continued to learn each day I keep these beautiful animals as pets.
Temperatures-
No heat lamp, no heat pad. Fine at normal room temperature. If you're not cold neither is your tarantula. If your house is kinda cold get a space heater for the room you keep your tarantula in. Between 60-80F is fine for most tarantulas. Slightly below or slightly higher won't likely hurt them. If your house regularly goes below 60F then consider getting a space heater.
Enclosures-
Don't buy an enclosure until you know the size of the tarantula youre getting. You could be investing in a huge tank when all you're going to need for the next 5 years is a Tupperware or critter keeper. Give your tarantula at least 2x their legspan in all demensions of the enclosure. So a 2in. legspan tarantula needs at least a 4x4in enclosure minimum. Too large an enclosure may mean you struggle to find your tarantula or that your tarantula has a higher risk of falling and getting hurt. You can be generous with space without going overboard. For example a 3wx4Lx2h in. display case is a bit large for a 3/4 in. sling however it's much more appropriate than putting a tiny sling in a huge enclosure. Small slings are often kept in 4oz or 6oz deli cups and that is completely fine for a few months. Remember that you don't have to spend big bucks on glass enclosures. Often acrylic and plastic is more ideal for providing proper ventilation anyways. Explore stores like the Container Store for ideas. You can use anything from display cases to clear shoe boxes. Invest in a drill and get some 1/16th inch drill bits (that's what i use on sling enclosures, you can use a larger bit for bigger spiders).
You should know whether or not your tarantula is terrestrial (lives on or near the ground), arboreal (lives in trees), or fossorial (lives primarily underground). I won't discuss fossorials in depth in this post because I don't have any first hand experience, however the biggest difference between fossorial and terrestrial is you need to give them A LOT of substrate. Get them a tall enclosure and fill it most of the way with substrate. Most "beginner species" aren't fossorials so it's unlikely you'll be getting one soon unless you get an Aphomapelma seemanni. Tom Moran has a husbandry video on Aphonopelma seemanni if that's the species you're interested in getting.
Terrestrials should have at least enough substrate to burrow if they choose, so at least one leg span if possible. Do not give a terrestrial more than 2x their legspan between the surface of the substrate and the lid of their enclosure. They have very fragile abdomens and can die if they fall from even small heights. A terrestrial enclosure should be wider/longer than it is high.
Arboreals need an enclosure that is taller than it is wide. I like the AMAC boxes sold at the Container Store for slings, however other options include clear pill jars, plastic jars, and file boxes. Be creative. There are also glass exoterra enclosures that people like, however I personally don't like them because they don't give you enough cross ventilation and tarantulas can get their feet caught on the mesh/screen lids. I prefer something with cross ventilation (something where i can add a bunch of holes in the sides). Arboreals don't need that much substrate. Just provide enough to cover the bottom of the enclosure, help keep anything that you may place on the bottom of the enclosure in place, and absorb moisture.
Water and moisture-
You'll see some care sheets say that certain genera and species such as "Theraposa stirmi" (which I would not recommend for a beginner) need "high humidity". What they really need is wet substrate. "High humidity" species need their substrate to be soaked down more frequently or more generously. Many "beginner" terrestrial species are arid species (they live in drier climates). Nearly all Brachypelma, Grammostola, and Aphomapelma can be kept in the same type of enclosures. Give them dry substrate and a water dish, and overflow the dish a little when you fill it. Do not put rocks or a sponge in the dish. Tarantulas cannot drink from a sponge and rocks and gravel simply provide more surface area for mold to grow.
Small slings do not necessarily need a water dish. While they are small tarantulas lack the waxy curticle on their exoskeletons that keeps water in. Because they lack the cuticle they can get moisture from their substrate. Keep generally all terrestrial slings an moderately damp substrate and watch for mold growth.
Substrate-
There are a number of popular options including ecoearth (or another brand of coconut fiber substrate) and organic potting soil. Some people mix vermiculite in with their substrate but vermiculite shouldn't be used alone as a substrate. If you use potting soil ensure it's only soil and doesn't have added fertilizer or chemicals. Topsoil is heavy so doesnt need to be packed down. If you choose ecoearth or coconut fiber, it comes often in dense bricks. Add water to these bricks and pull them apart. You may need to do this ahead of time so you can let the coconut fiber dry off before you assemble the enclosure. Coconut fiber is loose and fluffy when you put it in the enclosure. Pat it down firmly with your hands otherwise the tarantula won't like walking on the substrate. Coconut fiber, topsoil, or specially designed tarantula substrates are all acceptable. Substrates NOT to use: sand, aquarium gravel, woodchips, mulch, pure vermiculite. The goal with a substrate is to provide a maxtrix that the tarantula won't mind walking on that will hold moisture and hold the shape of their burrows.
Tank accessories-
Hides- The most important accessory besides a water dish (which I recommend for all tarantulas besides tiny slings) for a terrestrial tarantula is a hide. This can be a plastic hide bought from a pet store, a piece of corkbark, flat or curved driftwood, a broken flower pot, or half a cup. Be creative. They can be as cheap as you want. Just be sure there aren't any super sharp edges. In a pinch you can make a hide from a plastic soda bottle. Cut out a portion of it and CAREFULLY use a lighter to curve the piece of plastic and melt the edges so that's theyre not sharp. I have used this technique a number of times. These hides then should be partially buried so that they are dark inside, but the opening is visible so they tarantula can use it as a starter burrow. Cork bark is very popular for hides and can be bought from a pet store or online. A variety of other hides can also be bought from pet stores. Anything that's half a cylinder and open on both sides will function well as a hide for your tarantula. A hide can be skipped with super small slings but should be provided once the enclosure is large enough. For slings I've used short parts of powdered drink tubes that I bury with one end exposed on the surface. You'd be amazed what junk you can cut up and use in an enclosure.
Tall anchor points- for arboreal tarantulas they need something that reaches close to the top of their enclosure so they have something that they can climb and use to anchor webbing. This can be a piece of corkbark on end, a pcv pipe, a log, silk plants, or anything! Corkbark and silk plants are the popular choices but you can use a 2x4 (nontreated wood) and paint sticks if you feel so inclined.
Low anchor points- all tarantulas can web, although some will do so more than others. A number of species, especially the popular "green bottle blue" are heavy webbers and should be provided with some anchor points even though they're terrestrial (even though some may argue sort of otherwise). These anchor points can simply be fake plants or something. Protip: fishtank plants are cheaper than terrarium plants and work just as well. Even cheaper are silk plants from craft stores. Just rinse and pat dry any tank accessories to remove dust from the store just in case. All tarantulas can benefit from some anchor points in their enclosures. Also adding a silk plant or two looks nice.
Food-
A tarantula can be fed practically any sort of feeder insect from meal worms to roaches to crickets. Meal worms, superworms, and dubia roaches will burrow if you let them, so before offering them to your tarantula you should pinch the feeder's head so that it is disabled but not entirely dead. Crickets are fine but can bite, so don't leave them unattended with a tarantula. Red runners (B. lateralis) are good but beware that they can infest your home if they escape, so use caution. Hornworms can make an occasional nutrional treat, however only use store bought worms. If hornworms have eaten tomato plants it can make them toxic to anything that eats them. On that note: NEVER feed wild caught prey of any kind. Wild caught feeders may carry parasites such as nematodes that can be passed to your tarantula and may eventually kill them. Purchase feeders from a pet store, online supplier, local breeders (some people will breed colonies of feeders), or from vendors at an expo.
Feed your tarantula a prey item around the size of their abdomen once every week or two if they will eat. If you don't have larger prey items you can feed them a couple at once. If they stop eating do not be alarmed, they might just be full, or they may be in premolt. Some species can fast for up to a year, so you tarantula is not going to die from self inflicted starvation. If it wants to eat it will. If it's not eating then remove the prey and try again in a week or two. If your tarantula is really fat, perhaps just wait to try feeding until it gets skinnier or molts.
Molting-
Tarantulas have an exoskeleton which does not grow with them. Because of that, like all arthropods they will molt, where they shed their old exoskeleton. They will likely stop eating. Premolt, or the period where they may stop eating and perhaps become more elusive or even close themselve off in their burrow, may last anywhere from a week to months, to a year in severe cases. Sometimes they will get duller in color during premolt, their abdomens may get black and shiny, and they may lose hair on their abdomens. If they refuse food and/or seal off the entrance to their burrrow, then leave them be, continue to fill their water dish, and wait to offer food again until they start wandering around their enclosure again.
When a tarantula molts it usually flips over on it's back. DO NOT TOUCH IT. They are very fragile during and after a molt. A molt can take anywhere from half an hour to 8 hours depending on the size of the tarantula. Do not intervene, just make sure they have water and leave them alone. After they have left their old exoskeleton they will be very vulnerable. The new exoskeleton is very soft and takes awhile to harden. Wait 1-2 weeks before you feed them. Best to go on the side of caution and wait 2 weeks if you're in doubt. What's important here is you wait until their new fangs have fully hardened and turned shiny and dark black. After 2 weeks it should be safe to feed. Remember, your tarantula is fine going awhile without eating, waiting an extra week or two isn't neglectful. Just keep its water dish filled and it will be ok.
Useful tools-
Feeding tongs: a must have. They can be purchased at a pet store or online. You'll need them for feeding and for removing things from the enclosure.
Paintbrush or makeup brush: a soft and clean paintbrush or makeup brush can be used to gently touch the back legs of a tarantula and coax it where you need it to go.
Plastic straw: just rinse and save one after a trip to a fast food place. Used for the same use as the paintbrush, but more useful if you have a tarantula that tries to bite (a plastic straw will not hurt their fangs if they bite it)
Wooden chopsticks: I don't see this on many lists but I've found chopsticks can be useful for pushing prey around if they're "playing dead" or for cleaning an enclosure (once again the wood is safer for fangs than metal tongs, however still attempt to avoid having your tarantula bite the chopsticks).
Plastic spoon: i guess it doesnt have to be plastic but thats what i use. Just keep one around. Its good for packing down substrate in enclosures that are too small to reach your hands into, and for digging starter burrows when assembling an enclosure.
Spray bottle: get a clean plastic water bottle for filling water dishes, misting, and wetting substrate. You can buy an empty spray bottle with an adjustable stream from Walmart for a dollar or two. Look near the household cleaning supplies.
Catch cups: collect a variety of clear or translucent plastic cups and bowls that you can poke air holes in. Always have a few catch cups and some flat pieces of cardboard that can cover them around when you open an enclosure. Should a tarantula escape, wait for it to stop moving, place the cup over it, and gently slide cardboard underneath. I bought a pack of clear solo cups a year ago and those are what I most commonly use. Empty containers from shredded cheese work well too and keep those lids in case you want to use them as sling enclosures later on.
Pocket knife: not everyone does this, but I have one old pocket knife that is my feeder insect knife. Sometimes you need to cut mealworms in half for smaller slings, that is the knife I use. Afterwards I wipe the blade off and close it and keep it with the rest of my tarantula tools.
You will discover what tools you find work for you after you have been caring for a tarantula for awhile. At the bare minimum get feeding tongs, a plastic straw, and some catch cups.
Conclusions, disclaimers, and further reading:
This guide is from my personal experience and research, however my opinions may vary from those of other keepers and hobbyists. This advice is based off of the care I provide for my tarantulas however you may find different care works better for you. I highly recommend you read through Tom Moran's beginner guides https://tomsbigspiders.com/beginner-guides/
Browse the forums on arachnoboards. There are many good youtube channels out there as well but some are more informative than others. I highly recommend Tom Moran for husbandry information. He may not be the most exciting and attention grabbing channel, but he has the most comprehensive and well phrased husbandry information than any other single person I've come across.
Each individual species is different and you should research the care and temperment of your particular species, but I encourage you not to trust traditional "care sheets" as many are misleading. I recommend using Tom Moran's content as a resource and asking questions on arachnoboards and other forums if you have further questions. Good luck and welcome to the hobby!
#invertebrate#spider#tarantula#exotic pets#theraphosidae#care sheet#tarantulas#information#long post#beginner guide#arboreal#terrestrial
46 notes
·
View notes
Text
Review: Testosterone Replacement Therapy. Through 2018 Updates, should we Still Consider it a Prostate Cancer Risk Factor?- Juniper Publishers
Introduction
Testosterone Replacement Therapy (TRT) usage has great benefits on men’s health and do improve more the symptoms that could occur in those who are complaining of hypogonadism or andropause. However, it is classically known the oncological risks that may be caused due to its usage on the prostate, that’s why it was used with cautious. Recently many articles appeared in the last few years refuting this and evidencing the concept that there is no harm of their usage with those who are at risk of prostate cancer or even have treated prostate cancer. In this short review, it is aimed to review the literature that support this evidence published in 2018 on the PubMed.
Discussion
The decrease of the serum Testosterone levels causes what is known as hypogonadism which is manifested by decrease in libido, erectile dysfunction, fatigue and depression. This condition has a counted prevalence in men above the age of 50 years old. On the other side prostate cancer incidence starts to sharpen up after this age also and that’s why most of the screening programmes recommends starting the screening for men without family history at the age of 50 years old. As a historical knowledge it is known that Testosterone fuels the prostate cancer, this originally comes from 1941 when Dr Charles Huggins found that castration resulted in regression of the metastatic PCa and the debate is on since then [1].
Is it important to use it?
Restoring testosterone levels to within the normal range by using testosterone replacement therapy can improve many of the effects of hypogonadism. Most importantly, this also include beneficial effects on mood, energy levels and patients’ sense of well-being, sexual function, lean body mass and muscle strength, erythropoiesis and bone mineral density in addition to its use to improve other clinical symptoms of the metabolic syndrome, which presents as visceral obesity, hypertension, diabetes mellitus, and dyslipidaemia and are considered to be a potential risk for cardiovascular disease and cerebral apoplexy [2].
Recent Evidence of its Safety on the Prostate
Looking for the recent evidences and literature supporting that there is no correlation between the TRT and the prostate cancer which is challenging the classic opinion, Walsh TJ et al. [3] identified 56,833 men who initiated testosterone treatment for low testosterone levels and they were followed up for 3 years with PSA compared to non-treated group and a total of 1,439 prostate cancers were diagnosed; 848 were diagnosed among untreated and 591 among testosterone-treated men which was not a big statistical difference. So, they concluded that there is no much increase in the risk of prostate cancer development in those who are treated with testosterone in compared to nontreated group. However, the main pitfall of this study its short duration and it was recommended to have the same study for longer time up to 10 years.
A review by Torres et al. [4] summarized some evidences from the literature by different studies that compared patient who have a sort of treated prostate cancer and normal person and it was concluded at the end of the review that there are a lot of reassuring data that TRT doesn’t have a direct risk in causing PCa but yet there is still a small number that have a prostate cancer under TRT so a larger number studies and longer duration of follow up is recommended. Finally, a 2015 retrospective review of 98 hypogonadal men treated with TRT after radiation therapy for PCa and followed for about 40 months, they showed a rise in the levels of serum testosterone but there was no significant increase in mean PSA [5].
Conclusion
To our knowledge in 2018 there was limited published evidence on this subject. However, the new data keeping with the flow of the new evidence that there is conservative safety in TRT usage as regard its prostate cancer potential risk.
For more about Juniper Publishers please click on: https://twitter.com/Juniper_publish
For more about Journal of Thyroid Research please click on: https://juniperpublishers.com/jetr/index.php
#Testosterone#Homeostasis#hormones#Endocrine Signaling#Juniper Video Articles#Juniper Publishers Plagiarism policy
0 notes
Text
Recipe for success and practical tips for small cell and treatment free bees
To succeed, we must have a good concept. We are fortunate that we can rely on the experiences of many beekeepers who have already paved the way for us.
Fortunatelly we were able now to establish a new concept, through the help of experienced small cell beekeepers, how you can start sucessfully with small cell hives where other hives are nearby. The problem radicates in migration and reinfection by Varroa mites.
--> new concept
In the 90s Erik had a brilliant idea. At that time, there were already some beekeepers around the world, who had managed to breed resistant bees. He wrote to his colleagues about his experience, and asked them to describe theirs. The underlying idea was that if they all had done it, or had partially succeeded in breeding bees that fought back against the disease by themselves, there must be, in all these different forms of management, some truth. Back then the Internet was not yet as widespread as it is today, these beekeepers had little contact with each other - thus they had all achieved it in their own way. Erik said - if we make a summary of all the different experiences, we would have some very useful guidelines to get to our main aim, resistant bees. This summary of experience has existed since 2004.
Dee Lusby has 25 years of experience in dealing with disease-resistant, small cell bees without any treatment, so in addition with Erik’s study success is very likely.
I am now trying to form a concept from these sources that will include the most important points, from which we can develop a very good starting point.
- First, we should accustom our bees to small cells - reduction of distance between frames or thickness of frames to 32mm
- Then we should consider the natural arrangement of the combs.
- At the beginning we should work only with nucs until 80% of the bees can survive on their own. This means that we wait until a colony has nearly filled the box, and then instead of supering it, we make a nuc with the queen. We take 3 or 4 sealed brood combs, the queen, honey and pollen, and put all of them in a different box or nuc, and place it in the same yard, but orienting the entrance in a different direction. This means that the parent colony has a breeding break, because they raise a new queen and the nuc as well, since all the flying bees return to the parent colony. So we have created in both an advantage in terms of Varroa reproduction. If this whole thing is made very strong, with plenty of bees, lots of capped brood and a lot of food, we will be soon able to repeat the same process. Thus we are able to quickly build a nice collection of small cell colonies.
- Manage all the colonies in the apiary the same way (do not mix large and small cell colonies)
- Spread the colonies out in the apiary, have them as far away from each other as possible, to avoid drifting.
- Only place 6-12 colonies in each apiary to begin with. If you loose all colonies in an apiary due to domino effects, you won’t lose all of them.
- Plan for more than one small apiary (placed”together”), as isolated as possible from other bees.
- The best colonies are placed in the center apiary, the worse are placed further away. The new queens bred are mated in the center of these project apiaries, or in the center apiary.
-Also try to make sure that apiaries that may spread mites heavily aren’t placed close to your project apiaries.
- Use no chemical whatsoever in the project .
- Mite populations have to be kept low to hinder re-infestation of other colonies this is possible by other means, for example by removing all capped brood in two stages, with for example 9 days in between. Remember this is not done to keep good a producing colony alive, but to hinder re-infestation of the other colonies.
- Make sure, or as sure as possible, that you have a healthy microfauna in your colonies, or try to improve it, by for example get a nontreated colony from somewhere to mix in these bees and combs with your bees.
- Use combs which are drawn on wax foundation made from as chemical free wax as possible
- Try to leave as much honey as possible for winter food. After all that’s what the bees ”expect” for winter food.
- if problems appear in the first autumn, we can use powdered sugar to help. Also if there is strong re-infection by mites from other hives we can apply this same type of treatment.
- Teach the bees to build no more than 10% drone brood on any comb. This means cut out a small corner on each foundation sheet, where the bees will then rear their drone brood, and then in every inspection of the hives , cull step by step, any combs that have more than 10% drone brood.
- Ensure Accurate recording of each hive in every inspection
- no migration of hives
In the beginning, if we just start with nucs, the problem of the varroa mite is kept to a minimum.
I have to add what is happening in the nucs then.
Since we form the nucs with 3 to 4 sealed brood combs, we soon have a lot of young emerged bees.
A 4.9 mm Langstroth comb has 8600 cells (a 5.44 mm has only 7000 cells) and if we assume that a brood comb has 2/3 brood cells, we come at 3 frames of brood to 17,000 bees (with 4 frames of brood 23,000).
As the nuc is situated on the same apiary, all the foraging bees return to the mother hive and the egg laying of the queen will be drastically reduced.
And such a number of young bees, that also do not have to complete much brood care, have the consequence that they eliminate the Varroa mites very successful from the newly infected cells. The correlations between the number of bees, lifespan of bees, hygienic behavior and cell size, we present in our lecture.
We must not forget to give these nucs enough food, pollen and honey, as the most important is the strength of the hive. Or rather, the number of bees for the necessary work.
And that is simply in small cell bees much larger for two reasons.
For one thing, the brood nest is more compact due to the smaller cell size and also spacing of the honeycomb is reduced. Thus, fewer bees are necessary for brood care. On the other hand the lifespan of small cell bees is much larger than that of the large cell bees, which understandably has a decisive contribution that an excess of bees is available for the work to be performed in the hive.
Through this great number of bees the hygienic behavior is stimulated.
Now we see the distinct advantage of working with nucs at the beginning of our shifting to small cells.
Because as we know each hive HAS TO GO through one (or more) crises until it can defend itself on its own against the diseases.
And with this approach, we make it much easier for our bees.
The crisis will run less serious.
When we are frequently looking through our hives, it will enable us to become familiar with the habits of the bees and to study how they defend themselves against these diseases.
Some say that frequent opening of the hives should be avoided. Of course, this is right when our visit causes stress in the colonies. Since we arranged the natural order of the combs, we have seen an incredible peace in our hives. When we open them, the bees go down, they behave completely passively and continue to work normally. Thus, you can explore your hives as often as you want, and the most important issue is that WE, the beekeepers, will learn to recognise signs of crisis in the hive in the very first stage and we must also learn to respond to it properly.
We will then see how the bees defend themselves against the Varroa mites and chew out the infected cells.
Then we'll have to watch how they build the small cells and also to intervene constantly to help them. The small-cell foundations are drawn best near to, or in, the brood nest. Heavy nectar flow is also problematic and our timing has to be adapted, so that they will not have to build too much comb during slow nectar flow times.
If I cannot do all of these points, is it worth just starting with the small cells?
On the one hand it is quite clear that it will be much easier if we can change all these points.
But on the other hand, there is no reason, I think, to continue with the over-sized cells. This gives even more problems, as can be seen with the present disastrous situation of the bees.
If you do all the possible changes in the hives (small cells, comb arrangement, 10% drones etc., etc.) you will get the bees in a decidedly better, healthier condition.
You will see that they will defend themselves against the Varroa mite by hygienic behavior and that is something that very few beekeepers have achieved so far. But if reinvasion comes, you can treat with powdered sugar to help your bees. If you use it once per month, 200g per box of bees, you will always be able to see what is happening on the bottom board. To have complete success, you will need to have many hives and the others remain simply overwhelmed.
Read the full article
0 notes
Text
Moderate to severe osteoarthritis pain and its impact in USA
New Post has been published on https://depression-md.com/moderate-to-severe-osteoarthritis-pain-and-its-impact-in-usa/
Moderate to severe osteoarthritis pain and its impact in USA

Introduction
Chronic pain impacts approximately 100 million individuals in the United States (US), accounting for an estimated $560 to $635 billion per year (2010 dollars) in direct and indirect healthcare costs, including lost workplace productivity.1 Osteoarthritis (OA) is one of the most common causes of chronic pain and a leading cause of disability in the US,2–4 impacting activities of daily living.5 OA, the most common form of arthritis, is a joint disorder characterized by swelling, stiffness, inflammation, and pain that negatively impacts both physical and mental health in more than 32.5 million adults in the US.4,6–9 OA is associated with substantial economic and societal burdens resulting from functional impairment, decreased health-related quality of life (HRQoL), increased healthcare resource utilization (HCRU) and costs.8,10–19
Given the heterogeneity of patients with OA, development of new therapies to treat OA pain often requires targeting patient subgroups such as those with different levels of pain severity. For example, therapies targeting moderate-to-severe OA pain require a thorough understanding of the burden of illness and unmet need in this population. Establishing a new treatment’s positioning among available treatment options for OA will be critical to the population it serves and will provide value to payers and healthcare providers.
The humanistic and economic burden of OA has been investigated, to some extent, by disease and pain severity levels.19–25 Of 7 publications representing 6 unique studies, one study examined OA patients using claims and electronic health record (EHR) data,22 and the remaining studies were based on patient and/or healthcare provider surveys. Two of the 6 studies focused on disease or OA severity,20,21 and 4 stratified OA patients by pain severity19,22–25 even though two studies did not specify the pain as OA-specific.19,22
In those studies, pain severity was assessed using several measures including:
Numeric rating scales (NRS)
NRS; generic 0–10
Western Ontario and McMaster Universities Arthritis Index or WOMAC 3.126
Visual analog scales (VAS)
VAS; generic 0–100
Short-Form McGill Pain Questionnaire VAS (SF-MPQ-VAS)27,28
Likert scale
Pain Interference with Activities (PIA) scale derived from the 12-item Short Form Health Survey (SF-12v2) developed for the Medical Outcomes Study.29
While all of these measures are well-accepted,30 the recall periods in the studies varied from 48 hours to 7 days to 4 weeks. When specified, cut points for pain severity were generally similar: 0–3 representing no/mild, 4–6 for moderate, 7–10 for severe, and 4–10 for moderate-to-severe pain.
All of the published studies compared cohorts of no/mild pain with increasing severity cohorts. Four of the 6 studies examined differences between no/mild, moderate, and severe patients (1 study vs a non-OA cohort),20–22,24,25 and 2 compared no/mild vs moderate-to-severe pain.19,23 For most outcomes examined, increasing burden was observed with increasing OA and/or pain severity.
None of the studies exclusively investigated the burden of patients with symptomatic OA pain in a nationally representative sample that included treated and nontreated patients. This study provides a comprehensive, holistic view of the clinical and economic burden of OA by pain severity, in symptomatic patients only, from the patient perspective using a geographically representative national sample in a real-world setting. Clinical and economic burdens were examined in patients with moderate-to-severe OA pain vs mild OA pain, with a focus on patient demographics, comorbidities, HRQoL, pain medication use (including satisfaction and adherence), and HCRU.
Patients and Methods
Data Source and Population
Data were from the OA-specific module of the Kantar 2019 (January through December) US National Health and Wellness Survey (NHWS), a cross-sectional, nationally representative observational survey of general health.31 Respondents were identified primarily through opt-in online survey panels, with stratified random sampling within the panel to ensure representativeness for age and gender. Adults ≥18 years with self-reported physician-diagnosed OA and experiencing OA pain were included in the study. Respondents were excluded if they reported cancer pain, no OA pain, or that the only joint affected by OA was the back, shoulder, or neck.
Patients were stratified into OA pain severity cohorts based on responses to the SF-MPQ-VAS that assesses pain severity over the past week.28,32 Severity strata were based on scores of 1–34 for mild pain, 35–74 for moderate pain, and ≥75 for severe pain. Patients with scores of 0 (no OA pain) were excluded, and the moderate-to-severe cohort consisted of the combination of those with moderate and severe pain scores.
Outcomes
Demographic and Clinical Characteristics
All outcomes were self-reported including patient demographics (age, gender, race/ethnicity, employment status, and income level) and clinical characteristics of OA (affected joint or body region; duration of OA in years; frequency of OA pain in days, weeks, and months). Other clinical characteristics collected were comorbidities including sleep difficulties, depression and anxiety, and the Charlson Comorbidity Index (CCI).33 Information on body mass index (BMI), exercise, alcohol use, and smoking status was also captured and stratified by OA pain severity.
Health-Related Quality of Life (HRQoL)
HRQoL was measured using several validated instruments. Domains of HRQoL were evaluated using the Medical Outcomes Study (MOS) 36-item Short Form version 2 (SF-36v2) consisting of 36 items that assess general health and wellbeing over the past 4 weeks and includes 8 domain scores: physical functioning, role physical, bodily pain, general health, vitality, social function, role emotional, and mental health.34 Two summary scores, the mental component summary (MCS) and physical component summary (PCS), were also calculated. Scores range from 0 to 100 with higher scores indicating better HRQoL. The Short Form 6-dimension (SF-6D) health state utility score was calculated from the SF-36v2.35
The 5-level EQ-5D version (EQ-5D-5L) was used to assess general health status. The EQ-5D-5L consists of 5 questions that encompass mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.36–38 Each dimension has 5 scoring levels (no problems, slight problems, moderate problems, severe problems, and extreme problems) that enable calculation of health state utilities, which range from 0 (death) to 1 (perfect health).
Work Productivity
Work productivity was assessed using the validated 6-item Work Productivity and Activity Impairment General Health V2.0 questionnaire (WPAI-GH), which has a 7-day recall period. The WPAI-GH includes 4 subscales: absenteeism (absence from work), presenteeism (lost productivity while at work), overall work impairment (based on absenteeism and presenteeism), and overall activity impairment. All subscales are scored from 0% to 100%, with higher scores indicative of greater work or activity impairment.39,40 While the regular activities subscale was evaluated in all respondents, the work productivity subscales were evaluated only among employed respondents.
Medication Use for OA Pain
Current use of over the counter (OTC) pain medications to treat respondents’ OA pain was captured for ibuprofen, acetaminophen, naproxen, and acetylsalicylic acid. Information on the type of OA pain medication prescribed and the number of pain medications received was collected. Prescription medication duration was measured as the length of time, in months, that respondents reported using pain medication, and medication frequency was assessed as the maximum number of days any prescription pain medication was taken during the previous month. Medication adherence was assessed using the simple version of the Medication Adherence Rating Scale (MARS),41 for which respondents provided an estimate of how much, as a percentage, of their prescribed pain medication they had taken in the last 4 weeks. Respondents’ satisfaction with their current medication was measured using the stand-alone question “How satisfied are you with these prescription medication(s)?”, using a Likert scale of 1–7 (1 = extremely dissatisfied, 7 = extremely satisfied).
Healthcare Resource Utilization (HCRU)
Respondents were asked about their use of aids for OA including cold compresses, heat packs/patches, knee wraps, medical devices (eg, transcutaneous electrical nerve stimulation [TENS]), and braces. Respondents were also asked about their HCRU in the 6 months prior to the survey for categories of any outpatient visits, OA-related emergency room or urgent care visits, and OA-related hospitalizations.
Statistical Analyses
Total population and cohorts were analyzed using descriptive statistics; categorical variables were summarized as counts and proportions of the total study population and by subgroups as appropriate, and continuous variables were summarized as means and standard deviations. To represent the demographic composition of the US population, the data were weighted by gender, age and race/ethnicity.31 For pair-wise comparisons of categorical variables, first-order Rao-Scott chi-square tests were employed. For mean differences between continuous variables, t-tests were used. Statistical significance was defined as P<0.05. All analyses were performed using Statistical Analysis System (SAS) version 9.4 or higher (SAS Institute, Cary, NC, USA).
Results
Among 74,994 NHWS participants in 2019, 8607 (11.5%) self-reported a physician diagnosis of OA, of whom 5836 reported experiencing OA pain and were included in the analysis (Figure 1). These respondents were stratified into cohorts of mild (n=2038) and moderate-to-severe (n=3798) OA pain. Mean SF-MPQ-VAS was 19.7 (range 1–34) for mild OA pain respondents and 60.0 (range 35–100) for moderate-to-severe OA pain respondents.

Figure 1 Study population attrition.
Abbreviations: NHWS, National Health and Wellness Survey; OA, osteoarthritis.
Significant differences were observed between the two OA pain cohorts with respect to gender, age, race and ethnicity, and employment (P<0.0001) (Table 1). The moderate-to-severe cohort was younger (61.9 vs 64.3 years), had higher proportions of females (69.4% vs 57.3%), non-Hispanic Blacks (7.9% vs 4.0%), and Hispanics (4.0% vs 2.8%) compared to the mild OA pain cohort. More moderate-to-severe OA pain respondents were of working age (<65 years old), yet fewer were employed (29.5% vs 35.5%), and a greater proportion were on long-term disability leave (12.4% vs 3.8%) compared to mild OA pain respondents. Fewer moderate-to-severe respondents reported an income ≥$75,000 compared with mild OA pain (26.4% vs 42.1%).

Table 1 Demographic Characteristics
Statistically significant differences were observed between cohorts with respect to comorbidities, weight, and lifestyle preferences (P<0.0001) (Table 2). Mean CCI (0.68 vs 0.45) and CCI scores >1 were reported in a higher proportion of those with moderate-to-severe OA pain relative to mild (37.8% vs 23.9%), and these respondents also had a higher self-reported diagnosis of sleep disturbance (16.4% vs 7.8%), insomnia (25.3% vs 12.2%), depression (41.6% vs 23.6%), and general anxiety disorder (19.1% vs 10.2%) compared with mild OA pain. As indicated by the BMI, obesity was more prevalent among those with moderate-to-severe OA pain, and a higher proportion of these respondents also reported not having exercised for at least 20 minutes in the past month (53.5% vs 36.6%) (P<0.0001). Smoking status was significantly different between severity levels (P<0.0001); a higher proportion of respondents with moderate-to-severe OA pain reported a history of smoking (current or former) relative to respondents with mild OA pain (54.0% vs 48.6%).
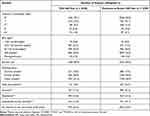
Table 2 Clinical Characteristics
Significant differences were also observed for OA type, length of OA, and OA pain frequency (P<0.01) (Table 3). Higher proportions of patients with moderate-to-severe OA pain had OA of the knee, finger, hip, spine, hand, shoulder, and neck, although these categories were not mutually exclusive. The majority of OA pain patients had more than 1 joint affected, with higher proportions in the moderate-to-severe cohort (89.5% vs 79.2%), including mean number of joints affected (4.8 vs 3.4) compared with mild OA. Significantly more patients with moderate-to-severe OA pain reported their arthritis as a result of injury compared with mild OA pain (36.1% vs 31.6%). Among these patients, median age of moderate-to-severe OA respondents was younger than those with mild OA pain (60.6 vs 62.0 years) (P<0.05, data not shown). Additionally, higher proportions of the respondents with moderate-to-severe OA pain had OA for more than a decade (58.6% vs 54.1%) and experienced daily OA pain compared with respondents with mild OA pain (80.9% vs 48.8%).

Table 3 Osteoarthritis Characteristics
Scores on all SF-36v2 domains were significantly lower (worse HRQoL) in those with moderate-to-severe OA pain compared with mild OA pain (P<0.0001) (Figure 2A). Similarly, both the MCS (46.7 vs 52.3) and PCS (37.5 vs 46.5) scores on the SF-36v2 were significantly lower with moderate-to-severe OA pain vs mild OA pain (both P<0.0001) (Figure 2B). The health state utilities derived from the SF-6D and EQ-5D-5L also showed significantly poorer health status in the moderate-to-severe OA pain respondents compared with mild OA (mean SF-6D: 0.62 vs 0.72; mean EQ-5D-5L: 0.68 vs 0.80; both P<0.0001) (Figure 2C).

Figure 2 Health-related quality of life. (A) General health and well-being assessed on SF-36v2 domains. (B) Mental Component Summary (MCS) and Physical Component Summary (PCS) scores of the SF-36v2. (C) SF-6D and EQ-5D-5L health index scores.
Abbreviations: SF-6D, Short Form 6-dimension; SF-36v2, 36-item Short Form version 2.
Note: *P<0.0001 vs mild OA pain.
Among employed respondents, the percentage of lost work productivity was significantly higher in those with moderate-to-severe OA pain due to both absenteeism and presenteeism, with presenteeism resulting in greater work impairment (both P<0.0001) (Figure 3). Additionally, total work impairment (35.9% vs 15.1%) and overall activity impairment (49.8% vs 23.6%) were significantly higher in the moderate-to-severe OA pain cohort compared with mild OA pain (both P<0.0001) (Figure 3).
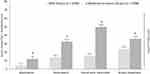
Figure 3 Impaired work and productivity assessed on the Work Productivity and Impairment Questionnaire for General Health (WPAI-GH)a.
Abbreviation: OA, osteoarthritis.
Notes: aWork productivity subscales evaluated only for responders who were employed; overall activity impairment evaluated among all responders. *P<0.0001 vs mild OA pain.
Respondents with moderate-to-severe OA pain took significantly more OTC acetaminophen (26.5% vs 23.0%) for their OA pain than those with mild OA pain (P<0.01) (Figure 4). In contrast, use of ibuprofen was higher in mild OA pain respondents compared with moderate-to-severe (24.9% vs 21.4%) as was use of acetylsalicylic acid (6.3% vs 4.5%) (both P<0.01). Additionally, use of an aid for OA, such as cold compresses, knee wraps, heat packs, patches, or braces was significantly higher for moderate-to-severe OA pain than mild OA pain (8.9% vs 7.1%, P<0.05).

Figure 4 Current use of over-the-counter pain medications reported by OA patientsa.
Abbreviations: OA, osteoarthritis; OTC, over the counter.
Notes: aData are for OTC medications taken by ≥5% of either respondent group. *P<0.01, mild vs moderate to severe OA pain.
Nonsteroidal anti-inflammatory drugs (NSAIDs) and non-tramadol opioids were the most prescribed pain medications in both cohorts (Table 4). However, a significantly higher proportion of moderate-to-severe OA pain respondents were prescribed OA pain medications overall (41.0% vs 17.0%), including cyclooxygenase-2 (COX-2) inhibitors (2.1% vs 1.2%), NSAIDs (18.3% vs 7.9%), tramadol (8.7% vs 3.3%), non-tramadol opioids (18.2% vs 5.3%), and steroids (2.5% vs 0.9%) compared with mild OA pain (all P<0.05) (Table 4).

Table 4 Current Use of Select Prescription Pain Medications Reported by OA Patients
Moderate-to-severe OA pain respondents had higher adherence, ie, took more of their prescription pain medications (75.9%) than those with mild OA pain (64.1%) during the last month (P<0.001). Moderate-to-severe OA respondents reported significantly lower overall satisfaction with their prescription pain medication compared with mild OA pain respondents (4.9 vs 5.3, P<0.0001) (Figure 5) and were significantly less satisfied with their prescription pain medication across classes (all P<0.05). On average, moderate-to-severe OA pain respondents scores were in the “somewhat satisfied” to “neither dissatisfied nor satisfied” range. For mild OA pain respondents, scores were higher and ranged between “somewhat satisfied” and “extremely satisfied”.

Figure 5 Satisfaction with currently prescribed OA medicationa.
Abbreviations: NSAID, nonsteroidal anti-inflammatory drug; OA, osteoarthritis; SNRI, serotonin-norepinephrine reuptake inhibitor.
Notes: aAll drugs that were statistically significant (P<0.05). *P<0.05, **P<0.0001, mild vs moderate to severe OA pain.
Overall, higher proportions of those with moderate-to-severe OA reported HCRU visits in the past 6 months across all resource categories than respondents with mild OA pain including outpatient visits (95.8% vs 94.3%, P<0.05), emergency room visits (18.9% vs 11.5%, P<0.0001), and hospitalizations (10.8% vs 8.1%, P<0.01) (Figure 6).

Figure 6 Respondent-reported healthcare resource utilization in the past 6 months.
Abbreviation: OA, osteoarthritis.
Notes: *P<0.05, **P<0.01, ***P<0.0001, mild vs moderate-to-severe OA pain.
Discussion
This study provides a holistic approach to the burden of OA pain from the respondents’ perspective based on a nationally representative survey. Unique aspects of this study are that respondents who reported no OA pain in the last week were excluded from the analysis, and that the data set represents a population subsequent to the updated CDC guidelines for opioid use42 and therefore may be more aligned with current practice. In contrast, previous studies were conducted using data sets that antedate the CDC guidelines, and either stratified their populations by disease severity rather than pain severity,20,21 or consisted of both symptomatic and asymptomatic patients, eg, the mild pain cohorts included OA patients with pain scores of zero (no pain).19,22–25 Among those studies, two did not confirm that the pain was specifically related to OA due to inherent limitations of the data source.19,22 Exclusion of patients with a zero pain score likely encompasses a more homogenous population with mild pain relative to the other studies. However, this cannot be confirmed since differentiation between no pain and mild OA pain patients in the mild cohorts was not reported.
Utilizing a robust sample size and23 multiple OA types, nearly one-third (35%) of respondents reported their OA pain severity level as mild, while nearly two-thirds (65%) reported moderate-to-severe OA pain. Collapsing the moderate and severe groups in the studies that reported 3 pain categories allowed us to compare results for a more severe population that is likely the target for several novel agents under investigation for OA pain43–47 and resulted in moderate-to-severe OA pain proportions that varied from 42% in Wei et al22 to 65% in the current study. In previous studies, no/mild OA pain ranged from 45% to 58% in patients that were not stratified by medication use.19,22–25 The lower proportions of mild and greater moderate-to-severe OA pain reported in this study are likely due to exclusion of respondents reporting no OA pain.
While moderate-to-severe OA pain respondents were significantly more likely to be female and of working age (<65 years), they were also less likely to be employed and have an income ≥$75,000. These trends in employment and income were reported in both Zhao et al19 and Nalamachu et al.25 Similarly, the significantly greater prevalence of clinical comorbidities in moderate-to-severe respondents is consistent with those two studies; however, depression and insomnia were 2- to 4-fold greater, respectively, in the mild OA pain cohort in our study. Although these differences likely reflect the mild cohort definition, they may also be due to use of self-report in the current study relative to diagnostic coding in administrative claims or a physician-reported diagnosis in the medical chart at the time of the visit for OA.
Duration of OA was generally longer, and pain was more frequent, among those with moderate-to-severe OA pain compared with mild OA pain. Similarly, obesity (BMI≥30) appeared to be more prevalent in the moderate-to-severe pain respondents, consistent with 3 of the other pain severity studies.19,21,24,25
Moderate-to-severe OA pain respondents reported significantly poorer HRQoL compared with mild OA pain across all measures of HRQoL, with calculated health state utility values similar to those observed by Jackson et al23 in their non-opioid cohort. As observed for HRQoL, moderate-to-severe OA pain respondents reported a significantly greater impact on daily activities including work productivity compared to the mild OA cohort. Similar to our study, significantly greater impact on daily activities and work productivity was observed in moderate-to-severe patients reported by Jackson et al.23
This study also evaluated both OTC and prescription pain medication use specific to OA by pain severity level. Among the OTC medications, significantly greater use of acetaminophen was observed in moderate-to-severe OA respondents, and in contrast, significantly greater use of ibuprofen and acetylsalicylic acid was observed in mild OA respondents. These observations are generally consistent with the greater recommended use of acetaminophen and less recommended use of ibuprofen with increasing OA pain severity reported by Nalamachu et al.24 While the current study showed less usage of naproxen with increasing OA pain severity, this could potentially result from less recommended use as suggested in the study by Nalamachu et al.24
Overall, prescription pain medication was significantly greater in moderate-to-severe OA pain patients, compared with mild OA, driven by significantly greater use of most classes of pain medications including COX-2 inhibitors, NSAIDs, steroids, anti-depressants, tramadol, and non-tramadol opioids. The overall low rates of prescription medication use among those with moderate-to-severe OA pain observed in our study compared to a recent study24 is likely attributable to differences in data sources; the NHWS captures both treated and non-treated respondents, and medication use is respondent-reported rather than physician-reported.
Interestingly, significantly greater adherence to pain medication was observed in moderate-to-severe OA pain respondents. This greater adherence may potentially be attributed to higher pain scores that provides a more constant reminder or awareness of their disease. Not unexpectedly, the higher rate of adherence observed in moderate-to-severe OA pain coincided with more respondents taking their prescription pain medications over a longer duration and at a higher frequency compared with mild OA pain. The greater duration of pain medication may also be reflective of disease progression where moderate-to-severe OA pain respondents experienced OA and OA-related pain for longer periods of time.
Among those taking prescription pain medication, treatment satisfaction was significantly lower in moderate-to-severe OA respondents compared with the mild OA pain cohort, possibly because OA pain medications are symptomatic treatments, and have no impact on disease progression. Those with moderate-to-severe OA were characterized by more comorbid conditions and poorer HRQoL compared with mild OA and may have had more advanced disease. The relationship between satisfaction with treatment and OA progression warrants further investigation.
Significantly greater HCRU across all categories in the prior 6 months was observed in moderate-to-severe OA respondents compared with mild OA. While similar trends in resource utilization were generally observed in the other studies,19,22,25 heterogeneity in measurement and definitions precludes meaningful comparisons.
Strengths of this study include our ability to examine the impact of OA pain severity on a wide variety of outcomes using a robust and nationally representative sample size. However, as with any study, there are limitations, including the large sample, which could result in inferring statistical significance solely based on sample size. The study was based on patients’ agreement to participate, and their perceptions may differ from those who refused to participate, introducing selection bias, and impacting generalizability. Additional selection bias may result from the fact that persons not seeking help from healthcare professionals for their symptomatic OA will not be captured in this analysis. The NHWS is broadly representative of the corresponding national adult population; however, as with other patient-reported surveys, it likely underrepresents people without access to or proficiency with internet use, as well as frail older adults, institutionalized patients, and those with severe comorbidities and disabilities. The survey relies on self-reported data where recall bias may be present, especially recall beyond 7 days. Further, clinician assessments like OA categorization and Kellgren-Lawrence grade were not captured. Finally, multiple joints may be affected, complicating the respondent’s ability to classify their OA pain as mild, moderate, or severe.
Due to the cross-sectional nature of the study, any relationships should be considered associative rather than causal. Using general health rather than disease-specific measures may minimize the true impact of OA pain on patient outcomes. The survey did not capture information on prior medication use, which may be important when considering OA pain treatment patterns. From an analytic standpoint, univariate analysis identified differences between cohorts without adjustment for variables such as BMI, comorbid conditions, and age, that may have influenced outcomes. Despite these limitations, findings were consistent with other studies that assessed OA populations. Expanding this research to provide national estimates of the burden and to further apply these findings for the design of international studies of OA pain and its impact is warranted for a greater understanding of OA pain severity across populations.
Conclusion
This study confirms that moderate-to-severe OA pain has a significantly greater multidimensional impact compared with mild OA pain, including lower HRQoL, reduced work productivity, and a greater medication burden. In addition, despite greater adherence rates, moderate-to-severe OA pain respondents were less satisfied with their current pain medication. Higher OA pain severity was also associated with more HCRU, including outpatient visits, emergency room visits, and hospitalizations. Understanding this burden of OA pain with its clinical and economic implications in real-world settings may inform decision-making by stakeholders to ensure more effective pain management. Further studies that include prospective longitudinal assessment of these burdens associated with OA pain are warranted.
Consent and Ethical Considerations
All respondents provided informed consent.
Acknowledgments
The study was sponsored by Pfizer and Eli Lilly and Company. Pfizer and Eli Lilly and Company collaborated on study design and interpretation of results. Editorial support was provided by Alesia Sadosky of Apperture LLC and was funded by Pfizer and Eli Lilly and Company. The data that support the findings of this study are available on request from the corresponding author, ST.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, agreed to the submitted journal, and agree to be accountable for all aspects of the work.
Disclosure
The findings of this manuscript have been presented at the ISPOR 2020 Virtual Annual Meeting; May 18–20, 2020 and at PAINWeek 2020 Virtual Meeting; September 11–13, 2020. The following authors are employees of Pfizer with stock and/or stock options: PS, ST, CB, DM, and BE. RR is an employee and stockholder of Eli Lilly and Company. AS was financially compensated for providing editorial support in the drafting of this manuscript. The authors report no other conflicts of interest in this work.
References
1. Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715–724. doi:10.1016/j.jpain.2012.03.009
2. Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an internet-based survey. J Pain. 2010;11(11):1230–1239. doi:10.1016/j.jpain.2010.07.002
3. Centers for Disease Control and Prevention. Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation–United States, 2010–2012. MMWR Morb Mortal Wkly Rep. 2013;62(44):869–873.
4. United States Bone and Joint Initiative. Osteoarthritis. The Burden of Musculoskeletal Diseases in the United States (BMUS). Rosemont, IL; 2018: Available from: https://www.boneandjointburden.org/fourth-edition. Accessed January14, 2020.
5. Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthritis Cartilage. 2013;21(9):1145–1153. doi:10.1016/j.joca.2013.03.018
6. Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105:185–199. doi:10.1093/bmb/lds038
7. Deshpande BR, Katz JN, Solomon DH, et al. Number of persons with symptomatic knee osteoarthritis in the US: impact of race and ethnicity, age, sex, and obesity. Arthritis Care Res (Hoboken). 2016;68(12):1743–1750. doi:10.1002/acr.22897
8. Osteoarthritis Research Society International (OARSI). Osteoarthritis: a serious disease, submitted to the U.S. Food and Drug Administration; 2016. Available from: https://oarsi.org/sites/default/files/docs/2016/oarsi_white_paper_oa_serious_disease_121416_1.pdf. Accessed January14, 2021.
9. Centers for Disease Control and Prevention (CDC). Osteoarthritis (OA); 2020. Available from: https://www.cdc.gov/arthritis/basics/osteoarthritis.htm. Accessed January14, 2021.
10. Bitton R. The economic burden of osteoarthritis. Am J Manag Care. 2009;15(8 Suppl):S230–235.
11. Kotlarz H, Gunnarsson CL, Fang H, Rizzo JA. Osteoarthritis and absenteeism costs: evidence from US National Survey Data. J Occup Environ Med. 2010;52(3):263–268. doi:10.1097/JOM.0b013e3181cf00aa
12. Gore M, Tai KS, Sadosky A, Leslie D, Stacey BR. Clinical comorbidities, treatment patterns, and healthcare costs of patients with osteoarthritis in usual care: a database analysis. J Med Econ. 2011;14(4):497–507. doi:10.3111/13696998.2011.594347
13. Berger A, Bozic K, Stacey B, Edelsberg J, Sadosky A, Oster G. Patterns of pharmacotherapy and health care utilization and costs prior to total hip or total knee replacement in patients with osteoarthritis. Arthritis Rheum. 2011;63(8):2268–2275. doi:10.1002/art.30417
14. DiBonaventura M, Gupta S, McDonald M, Sadosky A. Evaluating the health and economic impact of osteoarthritis pain in the workforce: results from the National Health and Wellness Survey. BMC Musculoskelet Disord. 2011;12:83. doi:10.1186/1471-2474-12-83
15. Gore M, Tai KS, Sadosky A, Leslie D, Stacey BR. Use and costs of prescription medications and alternative treatments in patients with osteoarthritis and chronic low back pain in community-based settings. Pain Pract. 2012;12(7):550–560. doi:10.1111/j.1533-2500.2012.00532.x
16. Murphy L, Helmick CG. The impact of osteoarthritis in the United States: a population-health perspective. Am J Nurs. 2012;112(3 Suppl 1):S13–19. doi:10.1097/01.NAJ.0000412646.80054.21
17. Xie F, Kovic B, Jin X, He X, Wang M, Silvestre C. Economic and humanistic burden of osteoarthritis: a systematic review of large sample studies. Pharmacoeconomics. 2016;34(11):1087–1100. doi:10.1007/s40273-016-0424-x
18. Wang SX, Ganguli AX, Bodhani A, Medema JK, Reichmann WM, Macaulay D. Healthcare resource utilization and costs by age and joint location among osteoarthritis patients in a privately insured population. J Med Econ. 2017;20(12):1299–1306. doi:10.1080/13696998.2017.1377717
19. Zhao X, Shah D, Gandhi K, et al. Clinical, humanistic, and economic burden of osteoarthritis among noninstitutionalized adults in the United States. Osteoarthritis Cartilage. 2019;27(11):1618–1626. doi:10.1016/j.joca.2019.07.002
20. Sadosky A, Bushmakin A, Cappelleri JC, Lionberger DR. Relationship between patient-reported disease severity in osteoarthritis and self-reported pain, function, and work productivity. Arthritis Res Ther. 2010;12:R162. doi:10.1186/ar3121
21. DiBonaventura M, Gupta S, McDonald M, Sadosky A, Pettit D, Silverman S. Impact of self-rated osteoarthritis severity in an employed population: cross-sectional analysis of data from the national health and wellness survey. Health Qual Life Outcomes. 2012;10:30. doi:10.1186/1477-7525-10-30
22. Wei W, Gandhi K, Blauer-Peterson C, Johnson J. Impact of pain severity and opioid use on health care resource utilization and costs among patients with knee and hip osteoarthritis. J Manag Care Spec Pharm. 2019;25(9):957–965. doi:10.18553/jmcp.2019.25.9.957
23. Jackson J, Iyer R, Mellor J, Wei W. The burden of pain associated with osteoarthritis in the hip or knee from the patient’s perspective: a multinational cross-sectional study. Adv Ther. 2020;37(9):3985–3999. doi:10.1007/s12325-020-01445-4
24. Nalamachu SR, Robinson RL, Viktrup L, et al. Multimodal treatment patterns for osteoarthritis and their relationship to patient-reported pain severity: a cross-sectional survey in the United States. J Pain Res. 2020;13:3415–3425. doi:10.2147/JPR.S285124
25. Nalamachu S, Robinson RL, Viktrup L, et al. Pain severity and healthcare resource utilization in patients with osteoarthritis in the United States. Postgrad Med. 2021;133(1):10–19. doi:10.1080/00325481.2020.1841988
26. Bellamy N. Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC); 2021. Available from: http://www.auscan.org/womac/index.htm. Accessed January14, 2021.
27. Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975;1(3):277–299. doi:10.1016/0304-3959(75)90044-5
28. Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30:191–197. doi:10.1016/0304-3959(87)91074-8
29. Ware JE, Kosinski M, Turner-Bowker D, Sundaram M, Gandek B, Maruish ME. User’s Manual for the SF-12v2 Health Survey Second Edition. Lincoln, RI: QualityMetric Incorporated; 2009.
30. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S240–252.
31. Kantar Health. National Health and Wellness Survey. Patient-reported healthcare insights; 2019. Available from: https://www.kantarhealth.com/docs/datasheets/kh-national-health-and-wellness-survey.pdf. Accessed January28, 2021.
32. Boonstra AM, Schiphorst Preuper HR, Balk GA, Stewart RE. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain. 2014;155(12):2545–2550. doi:10.1016/j.pain.2014.09.014
33. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
34. Maruish M, Maruish M, Kosinski M, et al. User’s Manual for the SF36v2 Health Survey. 3rd Ed. Lincoln, RI: QualityMetric Incorporated; 2011.
35. Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21(2):271–292. doi:10.1016/S0167-6296(01)00130-8
36. The EuroQol Group. EQ-5D-5L user guide; 2021. Available from: https://euroqol.org/publications/user-guides/. Accessed June11, 2017.
37. Conner-Spady BL, Marshall DA, Bohm E, et al. Reliability and validity of the EQ-5D-5L compared to the EQ-5D-3L in patients with osteoarthritis referred for hip and knee replacement. Qual Life Res. 2015;24(7):1775–1784. doi:10.1007/s11136-014-0910-6
38. Bilbao A, Garcia-Perez L, Arenaza JC, et al. Psychometric properties of the EQ-5D-5L in patients with hip or knee osteoarthritis: reliability, validity and responsiveness. Qual Life Res. 2018;27(11):2897–2908. doi:10.1007/s11136-018-1929-x
39. Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4:353–365. doi:10.2165/00019053-199304050-00006
40. Reilly MC. Work productivity and activity impairment questionnaire: specific health problem V2.0 (WPAI:SHP); 2010. Available from: http://www.reillyassociates.net/WPAI_SHP.html. Accessed January14, 2021.
41. Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophr Res. 2000;42(3):241–247. doi:10.1016/S0920-9964(99)00130-9
42. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain–United States, 2016. JAMA. 2016;315(15):1624–1645. doi:10.1001/jama.2016.1464
43. Dakin P, DiMartino SJ, Gao H, et al. The efficacy, tolerability, and joint safety of fasinumab in osteoarthritis pain: a phase IIb/III double-blind, placebo-controlled, randomized clinical trial. Arthritis Rheumatol. 2019;71(11):1824–1834. doi:10.1002/art.41012
44. Berenbaum F, Blanco FJ, Guermazi A, et al. Subcutaneous tanezumab for osteoarthritis of the hip or knee: efficacy and safety results from a 24-week randomised phase III study with a 24-week follow-up period. Ann Rheum Dis. 2020;79(6):800–810. doi:10.1136/annrheumdis-2019-216296
45. Schnitzer TJ, Easton R, Pang S, et al. Effect of tanezumab on joint pain, physical function, and patient global assessment of osteoarthritis among patients with osteoarthritis of the hip or knee: a randomized clinical trial. JAMA. 2019;322(1):37–48. doi:10.1001/jama.2019.8044
46. Krupka E, Jiang GL, Jan C. Efficacy and safety of intra-articular injection of tropomyosin receptor kinase A inhibitor in painful knee osteoarthritis: a randomized, double-blind and placebo-controlled study. Osteoarthritis Cartilage. 2019;27(11):1599–1607. doi:10.1016/j.joca.2019.05.028
47. Stevens RM, Ervin J, Nezzer J, et al. Randomized, double-blind, placebo-controlled trial of intraarticular trans-capsaicin for pain associated with osteoarthritis of the knee. Arthritis Rheumatol. 2019;71(9):1524–1533. doi:10.1002/art.40894
Source link
0 notes
Text
Hawaii’s Pushing Decision to Allow Assisted Suicide: A Brief History In Hawaii’s Legal Battle In Promoting “Our Care, Our Choice Act"
By Caitlin Vera, Loyola University New Orleans Class of 2021
October 2, 2020

As the battle for human rights ever persist, the still relatively new concept of assisted suicide or “doctor-prescribed suicide” continues to make its way to hospitals. A 2018 survey by the American Institute of Public Opinion uncovered that a majority of Americans (72%) are in favor of physician-assisted suicide [2]. It is now possible in 9 states to receive this procedure. This count includes Montana that has no specific law forbidding it. Hawaii, New Jersey, Colorado, California, Maine, Oregon, Vermont, and Washington are the latest to join the growing list. Examining the history of Hawaii’s move to allow assisted suicide shows just how quickly these lawmakers change their opinions. As 2020,There have been two new bills introduced in an effort to expand right of terminally ill patients as well as amendments to the 2018 “Our Care, Our Choice Act”. The bills include 2proposals for reimbursement for the patients that have enacted the “Our Care, Our Choice Act,”regardless of medical insurance coverage [3]. As well as a bill to waive the patient’s waiting period from twenty days to fifteen days for those who are not expected to survive the mandatory waiting period. As for the amendments, there are additional medical staff (I.E., mental health nurse practitioners) to have the ability to conduct mental health screenings of patients using the “Our Care, Our Choice Act” [4].
None of these bills or amendments have been passed as the beginning of the SARS-COV-2 pandemic have delayed this process and called for a recess regarding these changes. As of January 1, 2019 Hawaii has become the seventh state of legalize assisted suicide. The house bill has put into effect the “Our Care, Our Choice Act” which allows competent, terminally ill Hawaii residents to have request a doctor prescribe a lethal dose of medication. The bill states that this would allow for “the person to die in a peaceful, humane, and dignified manner.” The Act would allow for another option in the patient’s care which would permit them to make the decision to voluntarily stop eating/drinking (VSED) or opt to stop any life-sustaining medical measures [5]. In order for a patient to be able to enact the “Our Care, Our Choice Act,” the following criteria must be met [5]:(1)
Confirmation by two health care providers of the patient’s diagnoses, prognosis, and medical decision-making capacity, and the voluntariness of the patient’s request; 3(2)Determination by a counselor that the patient is capable, and does not appear to be suffering from undertreatment or nontreatment of depression or other condition which may interfere with the patient's ability to make an informed decision;(3)Two oral requests from the patient, separated by not less than twenty days; one singed written request that is witnessed by two people, one of whom must be unrelated to the patient and one singed final attestation; and(4)An additional waiting period between the written request and the writing of the prescription 4Page 1 & 2 from the “Our Choice, Our Care Act” [ House Bill NO. 2731, House of Representatives Twenty-ninth legislature, 2018 State of Hawaii [2]]As of 2018In reviewing the proposed bills for 2017, the House of Representatives for the state of Hawaii has taken a firm stance in not passing any of the five bills presented to them regarding assisted suicide. This becomes that last year in using “Medical Aid in Dying” and “Voluntary Assisted Dying” as house bill, as a new focus on “Our Care, Our Choice Act” is taking focus for assisted suicide activist groups.
________________________________________________________________
(1) Patient's Rights Council,
(2) Emanuel, E. (November 1994). "History of Euthanasia Debates in the United States and Britain". Annals of Internal Medicine. 121 (10): 793–802. doi:10.7326/0003-4819-121-10-19941115000010. PMID7944057. S2CID20754659.
(3) “Hawaii.” Patients Rights Council, www.patientsrightscouncil.org/site/hawaii/
(4) “Hawaii.” Death With Dignity, 30 June 2020, www.deathwithdignity.org/states/hawaii/.
(5)A Bill for an Act. health.hawaii.gov/opppd/files/2018/11/OCOC-Act2.pdf.Caitlin Vera is a senior criminology and justice major at Lo
0 notes