#ca cervix treatment
Text
Understanding Breast Cancer Treatment: Exploring Surgeries and Therapies

Breast cancer is a serious illness that requires careful treatment. There are different ways to treat breast cancer, including surgeries and therapies. In this article, we'll look at the types of surgeries and therapies used to treat breast cancer. We'll explain what they are, how they work, and why they're important.
Types of Surgeries:
Lumpectomy:
A lumpectomy is a surgery where doctors remove the tumor and a small amount of surrounding healthy tissue from the breast. It's often used for early-stage breast cancer to help keep as much of the breast as possible.
Mastectomy:
Mastectomy is when doctors remove the whole breast to treat breast cancer. There are different types of mastectomy, depending on how much tissue is removed.
Sentinel Lymph Node Biopsy:
This surgery helps doctors see if the cancer has spread to nearby lymph nodes. Doctors find and remove a few lymph nodes to check for cancer cells.
Types of Therapies:
Radiation Therapy:
Radiation therapy uses special beams to kill cancer cells and shrink tumors. It's often used after surgery to make sure any leftover cancer cells are gone.
Chemotherapy:
Chemotherapy is when patients take special drugs to kill cancer cells or stop them from growing. It's used before or after surgery to help get rid of cancer cells and prevent them from coming back.
Hormone Therapy:
Hormone therapy blocks hormones that can make breast cancer grow. It's used for hormone-sensitive breast cancer to stop cancer cells from growing.
Targeted Therapy:
Targeted therapy attacks specific parts of cancer cells to stop them from growing. It's a newer type of treatment that can be very effective for certain types of breast cancer.
Combination Therapies:
Neoadjuvant Therapy:
This therapy is given before surgery to shrink tumors and make them easier to remove. It helps make surgery more successful.
Adjuvant Therapy:
Adjuvant therapy is given after surgery to help lower the risk of cancer coming back. It can include radiation therapy, chemotherapy, hormone therapy, or targeted therapy.
Conclusion:
Breast cancer treatment is complex, but there are many ways to fight it. Surgeries and therapies play a big role in helping people beat breast cancer. By understanding the different types of surgeries and therapies available, patients and their doctors can work together to come up with the best treatment plan for each person. With the right treatment, many people with breast cancer can go on to live long, healthy lives.
#cervical cancer#hpv vaccine#gardasil vaccine#pap smear#cervical cancer vaccine#cervical cancer causes#hpv vaccine price#hpv vaccine cost#pap smear price#papilloma vaccine#cure for cervical cancer#cervical#cervical vaccine#cervical cancer vaccine price#cervical cancer vaccine cost#pap exam#pap smear testing#papilloma virus vaccine#cervix#cervical cancer shot#pap screening#cervical vaccine cost#ca cervix treatment#ca cervix causes#ca cervix vaccine#p smear#pabst smear#papanicolaou smear#pap smear near me#hpv vaccine near me
0 notes
Text
Understanding Cervical Cancer Treatment in Hyderabad
Cervical cancer is a significant health issue for women in Hyderabad, India. However, with advancements in medical science, there are more treatment options available. Dr. Chinnababu, a renowned oncologist, is leading the way in providing effective treatments for cervical cancer patients in Hyderabad.
What is Cervical Cancer?
Cervical cancer starts in the cells of the cervix, the lower part of the uterus. It is usually caused by the human papillomavirus (HPV), but other factors like smoking and weakened immune systems can also contribute. Early detection is crucial for successful treatment.
Diagnosis
In Hyderabad, doctors use various tests to diagnose cervical cancer. These include Pap smears, HPV testing, colposcopy, and biopsy. These tests help doctors determine the stage and severity of the cancer, which guides treatment decisions.
Treatment Options
Treatment for cervical cancer depends on the stage of the disease and the patient's overall health. In Hyderabad, patients have access to several treatment options:
Surgery: Surgery may be recommended for early-stage cervical cancer. It can involve removing the cancerous tissue or the entire uterus. Dr. Chinnababu specializes in minimally invasive surgeries, which have shorter recovery times and fewer complications.
Radiation Therapy: Radiation therapy uses high-energy rays to kill cancer cells. It can be delivered externally or internally through brachytherapy. Hyderabad has advanced radiation therapy equipment to deliver precise treatment.
Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It can be given alone or in combination with other treatments. Dr. Chinnababu designs personalized chemotherapy plans for each patient.
Targeted Therapy: Targeted therapy targets specific molecules involved in cancer growth. It can be used for advanced or recurrent cervical cancer. Immunotherapy is a type of targeted therapy that boosts the body's immune system to fight cancer cells.
Conclusion
Cervical cancer treatment in Hyderabad offers hope for patients. Dr. Chinnababu and his team are dedicated to providing the best care possible. If you or someone you know is diagnosed with cervical cancer, don't hesitate to seek medical advice and explore treatment options available in Hyderabad. Early detection and personalized treatment plans can improve outcomes and quality of life for cervical cancer patients.
#cervical cancer#hpv vaccine#gardasil vaccine#pap smear#cervical cancer vaccine#cervical cancer causes#hpv vaccine price#hpv vaccine cost#pap smear price#papilloma vaccine#cure for cervical cancer#cervical#cervical vaccine#cervical cancer vaccine price#cervical cancer vaccine cost#pap exam#pap smear testing#papilloma virus vaccine#cervix#cervical cancer shot#pap screening#cervical vaccine cost#ca cervix treatment#ca cervix causes#ca cervix vaccine#p smear#pabst smear#papanicolaou smear#pap smear near me#hpv vaccine near me
0 notes
Text
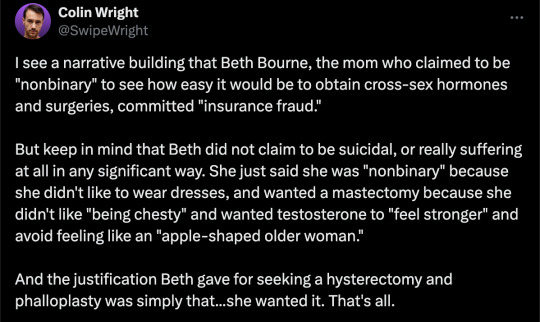
By: Beth Bourne
Published: Feb 27, 2024
Kaiser gender specialists were eager to approve hormones and surgeries, which would all be covered by insurance as “medically necessary.”
On September 6, 2022, I received mail from my Kaiser Permanente Davis Ob-Gyn reminding me of a routine cervical screening. The language of the reminder stood out to me: “Recommended for people with a cervix ages 21 to 65.” When I asked my Ob-Gyn about this strange wording, she told me the wording was chosen to be “inclusive” of their “transgender” and “gender fluid” patients.
Based on this response, several thoughts occurred to me. Could I expose the medical scandal of “gender-affirming care” by saying and doing everything my daughter and other trans-identifying kids are taught to do? Would there be the type of medical safeguarding and differential diagnosis we would expect in other fields of medicine, or would I simply be allowed to self-diagnose and be offered the tools (i.e. hormones and surgeries) to choose my own gender adventure and become my true authentic self?
If I could demonstrate that anyone suffering from delusions of their sex, self-hatred, or identity issues could qualify for and easily obtain body-altering hormones and surgeries, all covered by insurance as “medically necessary” and potentially “life-saving” care, then maybe people would finally wake up. I certainly had.
I was prepared for failure. I wasn’t prepared for how easy success would be.
* * *
I am a 53-year-old mom from Davis, CA. My daughter began identifying as a transgender boy (social transition) and using he/him pronouns at school during 8th grade. Like several of her peers who also identified as trans at her school, my daughter was a gifted student and intellectually mature but socially immature. This shift coincided with her school’s sudden commitment to, and celebration of, a now widespread set of radical beliefs about the biology of sex and gender identity.
She “came out” as trans to her father (my ex-husband) and me through a standard coming-out letter, expressing her wish to start puberty blockers. She said she knew they were safe, citing information she had read from Planned Parenthood and the World Professional Association for Transgender Health (WPATH). To say I was shocked would be an understatement. I was also confused because this announcement was sudden and unexpected. While others quickly accepted and affirmed my daughter’s new identity, I was apprehensive and felt the need to learn more about what was going on.
Events began escalating quickly.
During a routine doctor’s visit scheduled for dizziness my daughter said that she was experiencing, the Kaiser pediatrician overheard her father using “he/him” pronouns for our daughter. The pediatrician seemed thrilled, quickly asking my daughter about her “preferred pronouns” and updating her medical records to denote that my daughter was now, in fact, my son. The pediatrician then recommended we consult the Kaiser Permanente Oakland Proud pediatric gender clinic, where she could get further information and (gender affirming) “treatment.” Now I was the one feeling dizzy.
As I began educating myself on this issue, I discovered that this phenomenon—minors, most often teen girls, suddenly adopting trans identities—was becoming increasingly widespread. It even had a name: rapid onset gender dysphoria, or ROGD. Thankfully, after learning about the potential side-effects of blockers and hormones, my ex-husband and I managed to agree not to consent to any medical interventions for our daughter until she turned 18 and would then be able to make such decisions as an adult.
Over the past five years, my daughter’s identity has slowly evolved in ways that I see as positive. Our bond, however, has become strained, particularly since I began publicly voicing my concerns about what many term as “gender ideology.” Following my daughter’s 17th birthday family celebration, she sent me an email that evening stating she would be cutting off contact with me.
While this estrangement brought me sorrow, with my daughter living full-time with her father, it also gave me the space to be an advocate/activist in pushing back on gender identity ideology in the schools and the medical industry.
I decided to go undercover as a nonbinary patient to show my daughter what danger she might be putting herself in—by people who purport to have her health as their interest, but whose main interest is in medically “affirming” (i.e., transitioning) whoever walks through their door. I am at heart a mother protecting her child.
* * *
My daughter’s sudden decision to become a boy was heavily on my mind in early September of 2022, when mail from my Kaiser Permanente Davis Ob-Gyn reminded me of a routine cervical screening with “Recommended for people with a cervix ages 21 to 65.” I was told that the wording was chosen to be “inclusive” of transgender and “gender fluid” patients.
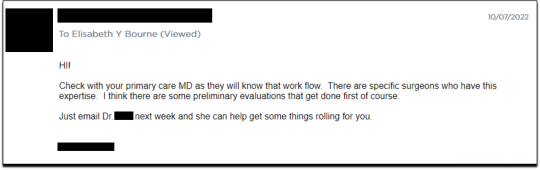
Throughout the whole 231-day process of my feigned gender transition, the Kaiser gender specialists were eager to serve me and give me what I wanted, which would all be covered by insurance as “medically necessary.” My emails were returned quickly, my appointments scheduled efficiently, and I never fell through the cracks. I was helped along every step of the way.
Despite gender activists and clinicians constantly claiming that obtaining hormones and surgeries is a long and complex process with plenty of safety checks in place, I was in full control at every checkpoint. I was able to self-diagnose, determine how strong a dose of testosterone I received and which surgeries I wanted to pursue, no matter how extreme and no matter how many glaring red flags I purposefully dropped. The medical workers I met repeatedly reminded me that they were not there to act as “gatekeepers.”
I was able to instantly change my medical records to reflect my new gender identity and pronouns. Despite never being diagnosed with gender dysphoria, I was able to obtain a prescription for testosterone and approval for a “gender-affirming” double mastectomy from my doctor. It took only three more months (90 days) to be approved for surgery to remove my uterus and have a fake penis constructed from the skin of my thigh or forearm. Therapy was never recommended.
Critics might dismiss my story as insignificant on the grounds that I am a 53-year-old woman with ample life experience who should be free to alter her body. However, this argument for adult bodily autonomy is a standard we apply to purely cosmetic procedures like breast implants, liposuction, and facelifts, not “medically necessary” and “lifesaving” treatments covered by health insurance. Or interventions that compromise health and introduce illness into an otherwise healthy body. And especially not for children.
My story, which I outline in much more detail below, should convince any half-rational person that gender medicine is not operating like any other field of medicine. Based on a radical concept of “gender identity,” this medical anomaly preys upon the body-image insecurities common among pubescent minors to bill health insurance companies for permanent cosmetic procedures that often leave their patients with permanently altered bodies, damaged endocrine systems, sexual dysfunction, and infertility.
* * *
Detailed Timeline of Events
On October 6, 2022, I responded to my Ob-Gyn’s email to tell her that, after some thought, I’d decided that maybe the label “cis woman” didn’t truly reflect who I was. After all, I did have some tomboyish tendencies. I told her I would like my records to be changed to reflect my newly realized “nonbinary” identity, and that my new pronouns were they/them. I also voiced my desire to be put in touch with an endocrinologist to discuss starting testosterone treatment.
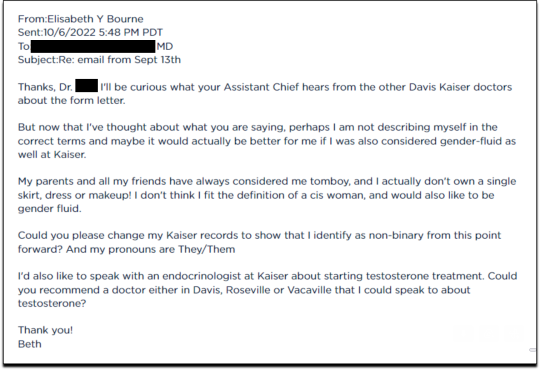
Fifteen minutes later I received an email from another Kaiser doctor informing me that my medical records had been changed, and that once my primary doctor returned to the office, I’d be able to speak with her about hormone therapy.
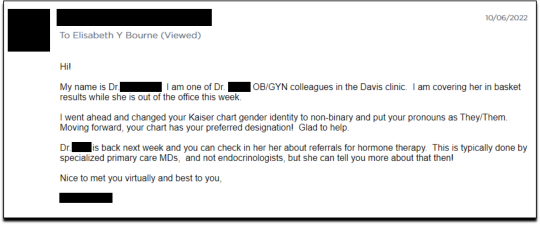
I responded the following day (October 7, 2022), thanking her for changing my records, and asking if she could connect me with someone who could help me make an appointment for “top surgery” (i.e., a cosmetic double mastectomy) because my chest binder was rather “uncomfortable after long days and playing tennis.”
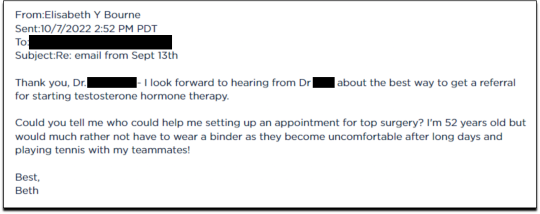
She told me to contact my primary care MD to “get things rolling,” and that there were likely to be “preliminary evaluations.”
Six days after contacting my primary care MD for a referral, I received an email from one of Kaiser’s gender specialists asking me to schedule a phone appointment so she could better understand my goals for surgery, so that I could get “connected to care.” This call to review my “gender affirming treatment options and services” would take 15-20 minutes, after which I would be “booked for intake,” allowing me to proceed with medical transition.
This wasn’t an evaluation of whether surgical transition was appropriate, it was simply a meeting for me to tell them what I wanted so that they could provide it.
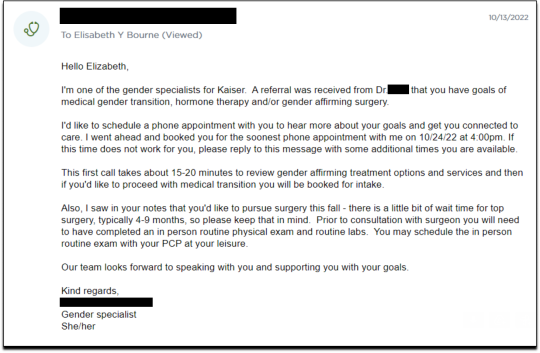
On October 18, I had my one and only in-person appointment in preparation for top surgery. I met in Davis with my primary care physician, Dr. Hong-wen Xue. The assessment was a 10-minute routine physical exam that included blood tests. Everything came back normal. Notably, there was not a single question about why I wanted top surgery or cross-sex hormones. Nor was there any discussion of the risks involved with these medical treatments.
The following week, on October 24, I had a phone appointment with Rachaell Wood, MFT, a gender specialist with Kaiser Sacramento. The call lasted 15 minutes and consisted of standard questions about potential drug use, domestic violence, guns in the house, and whether I experienced any suicidal thoughts. There were no questions from the gender specialist about my reasons for requesting a mastectomy or cross-sex hormones, or why I suddenly, at 52, decided I was “nonbinary.”
After the call, Kaiser emailed me instructions about how to prepare for my pre-surgery intake video appointment to evaluate my mental health, scheduled to take place on November 15. The email stated that prior to my appointment, I should research hormone risks on the WPATH website, and to “research bilateral mastectomy and chest reconstruction surgery risks and recovery” on Kaiser’s website.
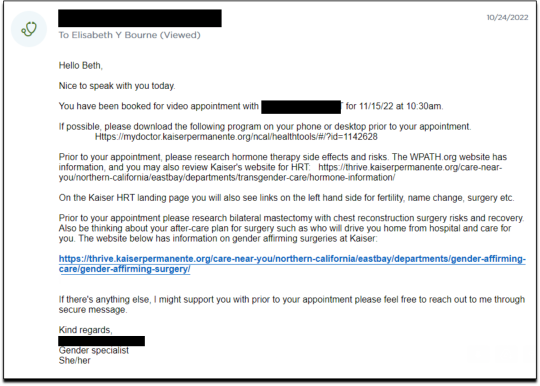
I decided to request a “gender-affirming” double mastectomy and phalloplasty. Kaiser sent me a sample timeline for gender transition surgery preparation (see below) that you can use as a reference for the process. I also asked for a prescription for cross-sex hormones (testosterone) as needed and recommended by Kaiser.
[ Source: Kaiser Permanente, Top Surgery - EXPLORING YOUR SURGICAL OPTIONS ]
Pre-Surgery Mental Health Video Appointment, Part I
This “Mental Health Visit” assessment was conducted over Zoom. The Kaiser gender specialist started with questions addressing my marital status, race, gender identity, and other demographics. She asked whether I was “thinking of any other surgeries, treatments in the future.” The list she read included “gender-affirming” hysterectomies, bottom surgeries such as metoidioplasty and phalloplasty, vocal coaching, support groups, and body contouring. “Anything else you might be interested in doing?” she asked. I said that I’d perhaps be interested in body contouring. I was also assured that all the procedures would be covered by insurance because they were considered “medically necessary.”
I dropped in several red flags regarding my mental health to see the reaction, but all were ignored. For instance, I revealed that I had PTSD. When the therapist asked me about whether I had experienced any “childhood trauma,” I explained that I grew up in Mexico City and had been groped several times and had also witnessed men masturbating in public and had been grabbed by men in subways and buses. “I was a young girl, so [I had] lots of experiences of sexual harassments, sexual assault, just the kind of stuff that happens when you are a girl growing up in a big city.” “So, you know,” I finished, “just the general feeling that you are unsafe, you know, in a female body.”
The therapist did not respond to my disclosure that trauma could be the cause of my dysphoria. Instead of viewing this trauma as potentially driving my desire to escape my female body through hormones and surgery, she asked whether there is anything “important that the surgery team should be aware of” regarding my “history of trauma,” such as whether I’d be comfortable with the surgeon examining and marking my chest prior to surgery.
When asked about whether I had had any “psychotic symptoms,” I told her that while I had had no such symptoms, my mother had a delusional nervous breakdown in her 50s because she had body dysmorphia and became convinced she had a growth on her neck that needed to be removed. I told her that my mother was then admitted to an inpatient hospital for severe depression. I asked her whether she ever sees patients with body dysmorphia and whether I could have potentially inherited that from my mother. She told me that psychosis was hereditary, but that it was “highly unlikely” that there was any connection between body dysmorphia and gender dysphoria.
I enthusiastically waved more mental health red flags, waiting to see if she would pick up on any of them.
I’m just wondering if my feelings, or perseverating, or feeling like these breasts make me really unhappy and I just don’t want them anymore!...I’m just not sure if that’s a similar feeling to body dysmorphia? How do you decide which one is gender dysphoria and general body dysmorphia, and just not liking something about your body? Feeling uncomfortable with your body?
And I did have an eating disorder all through college. I was a distance runner in college so I had bulimia and anorexia, you know. So I don’t know if that’s related to gender dysphoria?
The therapist replied, “I completely appreciate your concerns, but I am going to ask you questions about your chest, about your expectations. And then I’ll be able to give you an assessment.” She also said the main difference between my mom’s situation and mine was that my mom didn’t really have a growth on her neck, whereas it’s “confirmed” that I actually have “chest tissue.” Furthermore, she said that while “historically there has been all this pressure on patients to be like ‘Are you really, really sure you want hormones? Are you 100% sure?’ We are a little more relaxed.” She continued, “As long as you are aware of the risks and the side-effects, you can put your toe in the water. You can stop ‘T’ [testosterone], you can go back and do it again later! You can stop it! You can stop it! You know what I mean?”
Because we ran out of time, I scheduled a follow-up phone meeting on December 27, 2022 with a different gender specialist to complete my mental health assessment for top surgery.
Pre-Surgery Mental Health Video Appointment, Part II
During this meeting, Guneet Kaur, LCSW, another Kaiser gender specialist (she/her/they/them pronouns) told me that she regretted the “gatekeeping vibe” of the meeting but assured me that since I have been “doing the work,” her questions are essentially just a form of “emotional support” before talking with the medical providers.
She asked me about what I’d been “looking into as far as hormones.” I told her that I’d be interested in taking small doses of testosterone to counterbalance my female feelings to achieve “a feeling that’s kind of neutral.”
When she asked me about me “not feeling like I match on the outside what I feel on the inside,” I dropped more red flags, mentioning my aversion to wearing dresses and skirts.
I don’t own a single dress or a skirt and haven't in 20 years. I think for me it’s been just dressing the way that’s comfortable for me, which is just wearing, jeans and sweatshirts and I have a lot of flannel shirts and, and I wear boots all the time instead of other kinds of shoes. So I think it’s been nice being able to dress, especially because I work from home now most of the time that just a feeling of clothing being one of the ways that I can feel more non-binary in my everyday life.
She responded, “Like having control over what you wear and yeah. Kind of that feeling of just, yeah, this is who I am today. That’s awesome. Yeah.”
She then asked me to describe my dysphoria, and I told her that I didn’t like the “feeling of the female form and being chesty,” and that because I am going through menopause, I wanted to start taking testosterone to avoid “that feeling of being like this apple-shaped older woman.” “Good. Okay, great,” she responded, reminding me that only “top surgery,” not testosterone, would be able to solve my chest dysphoria. (Perhaps it was because all these meetings were online, they didn’t notice I’m actually fit and relatively slender at 5’-5” and 130 pounds, and not apple-shaped at all.)
She told me that we had to get through a few more questions related to my medical history before “we can move on to the fun stuff, which is testosterone and top surgery.”
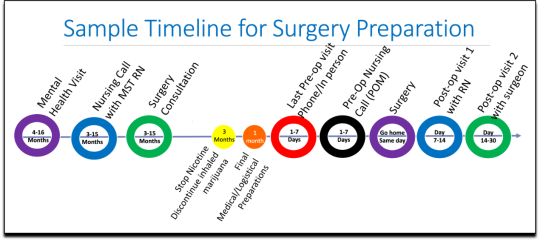
The “fun stuff” consisted of a discussion about the physical and mood changes I could expect, and her asking me about the dose of testosterone I wanted to take and the kind of “top surgery” technique I’d prefer to achieve my “chest goals.” She told me that all or most of my consultations for surgeries and hormones would be virtual.
The gender specialist told me after the appointment, she would submit my referral to the Multi-Specialty Transitions Clinic (MST) team that oversees “gender expansive care.” They would follow up to schedule a “nursing call” with me to review my medical history, after which they’d schedule my appointment with a surgeon for a consultation. Her instructions for this consultation were to “tell them what you’re wanting for surgery and then they share with you their game plan.”
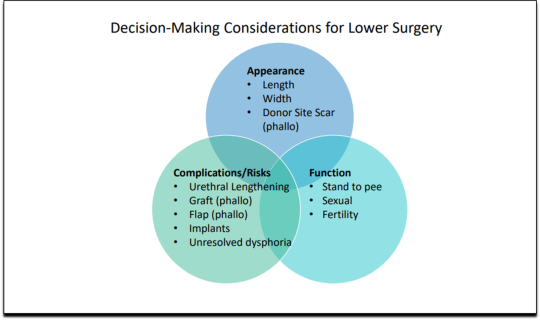
[ Decision-making slide to help me identify my goals for top surgery–flat chest, nipple sensation, or minimal scarring. Source: Kaiser Permanente, Top Surgery - EXPLORING YOUR SURGICAL OPTIONS ]
She told me that Kaiser has a team of plastic surgeons who “only work with trans and nonbinary patients because there’s just so much need for them.” She asked about my priorities for chest surgery, such as whether I value flatness over nipple sensation. I learned about double incision top surgery with nipple grafts, as well as “keyhole,” “donut,” “buttonhole,” and “Inverted-T” top surgeries.
By the end of the hour-long appointment, I had my surgery referral and was ready for my “nursing call” appointment.
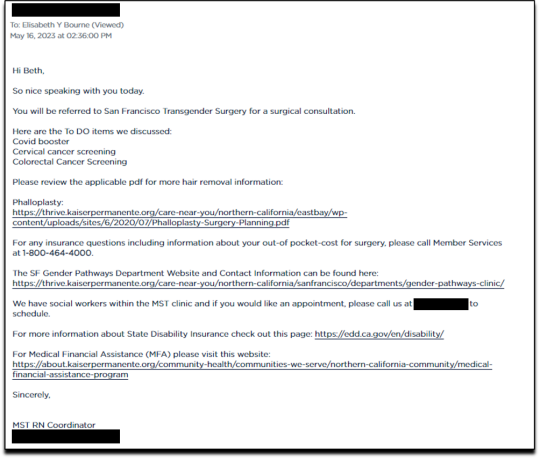
Nursing call with Nurse Coordinator from the Transgender Surgery and Gender Pathways Clinic at Kaiser San Francisco
On January 19, 2023, I had my nursing call with the Nurse Coordinator. He first said that “the purpose of this call is just for us to go through your chart together and make sure everything’s as accurate as possible.” Once that was done, my referral would be sent to the surgeon for a consultation.
He asked me about potential allergies and recreational drug use, and verified that I was up to date on mammograms, pap smears, and colon cancer screenings, as well as vaccines for flu and COVID. I verified my surgical history as well as my current medications and dietary supplements.
He told me about a “top surgery class” available for patients where one of the Kaiser surgeons “presents and talks about surgical techniques and options within top surgery,” and includes a panel of patients who have had top surgery. I signed up for the February 8th class.
Within 10 minutes he told me that he had “sent a referral to the plastic surgery department at Kaiser Sacramento,” and that I should be hearing from them in the next week or two to schedule a consultation.
Appointment for Testosterone
On January 27, I had a 13-minute online appointment with a primary care doctor at Kaiser Davis to discuss testosterone. The doctor verified my name and preferred pronouns, and then directly asked: “So, what would you like to do? What kind of physical things are you looking for?”
I told her I wanted facial hair, a more muscular and less “curvy” physique, and to feel stronger and androgynous. She asked me when I wanted to start, and I told her in the next few months. She asked me if I was menopausal, whether I had ovaries and a uterus, although that information should have been on my chart.
The doctor said she wanted me to come in to get some labs so she could check my current estrogen, testosterone, and hemoglobin levels before starting hormones. Then “we'll set the ball in motion and you'll be going. We’ll see you full steam ahead in the direction you wanna go.”
That was it. I made an appointment and had my lab tests done on February 12. My labs came back on February 14, and the following day, after paying a $5 copay at the Kaiser pharmacy, I picked up my testosterone pump. That was easy!
Top Surgery Consultation
On the same day I received my labs, I had a Zoom surgery consultation with Karly Autumn-Kaplan, MD, Kaiser Sacramento plastic surgeon. This consultation was all about discussing my “goals” for surgery, not about whether surgery was needed or appropriate.
I told the surgeon that I wanted a “flatter, more androgynous appearance.” She asked me some questions to get a better idea of what that meant for me. She said that some patients want a “male chest,” but that others “want to look like nothing, like just straight up and down, sometimes not even nipples.” Others still wanted their chest to appear slightly feminine and only “slightly rounded.” I told her that I’d like my chest to have a “male appearance.”
“What are your thoughts about keeping your nipples?” she asked. “Are you interested in having nipples or would you like them removed?” I told her that I’d like to keep my nipples, but to make them “smaller in size.” She asked me if I’d like them moved to “the edge of the peck muscle” to achieve “a more male appearance.” I said yes.
I was asked to show my bare chest from the front and side, which I did. Then she asked me how important it was for me to keep my nipple sensation. I replied that it was important unless it would make recovery more difficult or there were other associated risks. She highlighted the problem with the free nipple graft, saying that removing the nipple to relocate it means “you're not gonna have sensation in that nipple and areola anymore.” However, some nipple sensation could be preserved by keeping it attached to “a little stalk of tissue” with “real nerves going to it,” but that would require leaving more tissue behind. I told her I’d go for the free nipple graft to achieve a flatter appearance. It was also suggested I could skip nipple reconstruction entirely and just get nipples “tattooed” directly onto my chest.
She told me I was “a good candidate for surgery,” and put me on the surgery wait list. She said that the wait time was between three and five months, but a cancellation could move me up to a sooner date. Also, if I wanted surgery as soon as possible, I could tell the surgery scheduler that I’d be willing to have any of the other three surgeons perform my mastectomy. Outpatient top surgery would cost me a copay of $100.
They contacted twice, in February and March, notifying me of cancellations. If I had accepted and shown up on those dates, they would have removed my breasts. This would have been less than five months from the time I first contacted Kaiser to inform them of my new “nonbinary” gender identity.
How Far Can I Go?
I decided to see how easy it would be for me to get approved for a phalloplasty. Known euphemistically as “bottom surgery,” phalloplasty is the surgical creation of an artificial penis, generally using tissue from the thigh or arm.
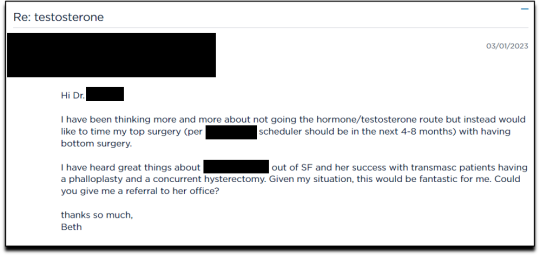
I sent an email on March 1, 2023, requesting to have a phalloplasty and concurrent hysterectomy scheduled alongside my mastectomy.
Two weeks later, on March 16th, I had a 16-minute phone call with a gender specialist to discuss my goals for bottom surgery and obtain my referral.
During the call, I explained to the specialist that I wasn’t sure about taking testosterone anymore because I was already quite athletic and muscular, and that taking testosterone didn’t make much sense to me. Instead, I wanted bottom surgery so that I wouldn’t feel like my “top” didn’t match my “bottom.” I told her:
But what I really wanted was to have bottom surgery. So this way when I have my top surgery, which sounds like it could be very soon, that I’ll be aligned, that I won’t have this sense of dysphoria with one part of my body and the other part feeling like it matched who I am. So yeah. So I just did a little bit more research into that. And I looked at the resources on the Kaiser page for the MST clinic and I think I know what I want, which is the hysterectomy and then at the same time or soon after to be able to have a phalloplasty.
I told her that I wanted to schedule the top and bottom surgery concurrently so that I wouldn’t have to take more time off work and it would save me trips to San Francisco or Oakland, or wherever I had to go for surgery.
None of this gave the gender specialist pause. After a brief conversation about some online resources to look over, she told me that she would “submit the referral now and we’ll get this ball rolling.”
Bottom surgery would cost me a copay of $200, which included a couple of days in the hospital for recovery.
Phalloplasty Surgical Consultation with Nurse Coordinator
On May 16, 2023, I had a short surgical consultation with a nurse coordinator to go through my medical history. This was similar to the consultation for top surgery but included information about hair removal procedures for the skin on my “donor site” that would be fashioned into a makeshift penis. They also went over the procedures for determining which donor site—forearm or thigh—was more viable.
After only 15 minutes, she submitted my referral to the surgeon for another surgical consultation.
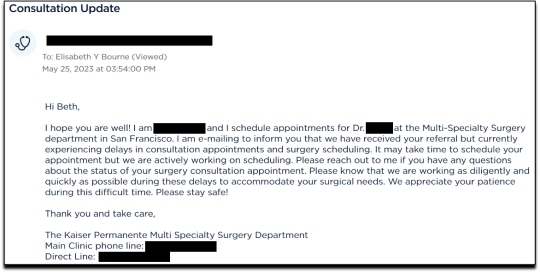
On May 25 I received an email from my phalloplasty surgeon’s scheduler, informing me that they have received my referral and are actively working on scheduling, but that they are experiencing delays.
I ended my investigation here once I had the referral for the top and bottom surgery. I never used my testosterone pump.
Final Thoughts
In fewer than 300 days, based on a set of superficial and shifting thoughts about my gender and my “embodiment goals” triggered by the mere mention of “gender” in a form letter from my primary care physician, and driven by what could only be described as minor discomforts, Kaiser Permanente’s esteemed “multi-disciplinary team” of “gender specialists” was willing, with enthusiasm—while ignoring mental health concerns, history of sexual trauma, and rapidly escalating surgical requests—to prescribe life-altering medications and perform surgeries to remove my breasts, uterus, and vagina, close my vaginal opening, and attempt a complex surgery with high failure and complication rates to create a functionless representation of a penis that destroys the integrity of my arm or thigh in the process.
This describes the supposedly meticulous, lengthy, and safety-focused process that a Kaiser patient must undergo to embark on a journey to medically alter their body. No clinician questioned my motivations. No one showed concern that I might be addressing a mental health issue through radical and irreversible interventions that wouldn’t address my amorphous problems. There were no discussions about how these treatments would impact my long-term health, romantic relationships, family, or sex life. I charted the course. The clinicians followed my lead without question. The guiding issue was what I wanted to look like.
No other medical field operates with this level of carelessness and disregard for patient health and welfare. No other medical field addresses issues of self-perception with surgery and labels it “medically necessary.” No other medical field is this disconnected from the reality of the patients it serves.
Kaiser has traded medicine for ideology. It’s far beyond time we stop the ruse of considering “gender-affirming” interventions as anything approaching medical care.
This isn’t the first time Kaiser Permanente has been in the news for completely disregarding medical safeguards in the name of “gender-affirming care.” As girls, Chloe Cole and Layla Jane became convinced that they were born in the wrong body and were actually boys on the inside. Doctors at Kaiser ignored their underlying conditions and instead prescribed testosterone and removed their breasts. Both Cole and Jane have since detransitioned and are currently suing Kaiser.
The fact that children and vulnerable adults are being exploited in this massive ideological experiment is not just tragic; it’s deeply disturbing, especially considering it has evolved into a billion-dollar industry.
I hope that by sharing my story, I can bring more focused scrutiny to the medical scandal unfolding not just at Kaiser but also at medical centers and hospitals across the Western world. These institutions have completely abandoned medical safeguards for patients who claim to be confused about their “gender,” and I aim to awaken more parents and assist them in protecting their children.
--
==
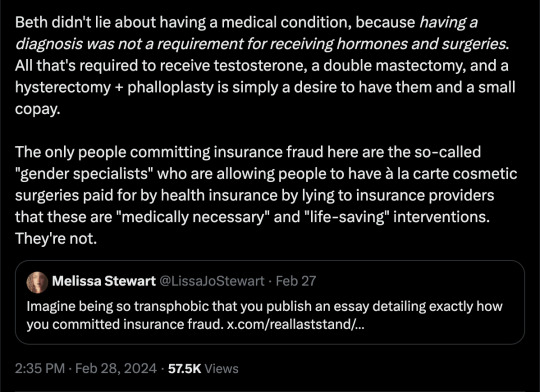
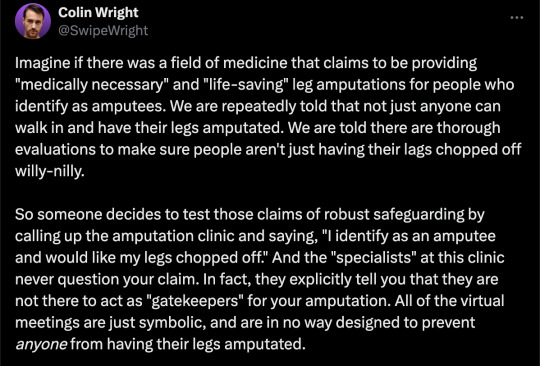
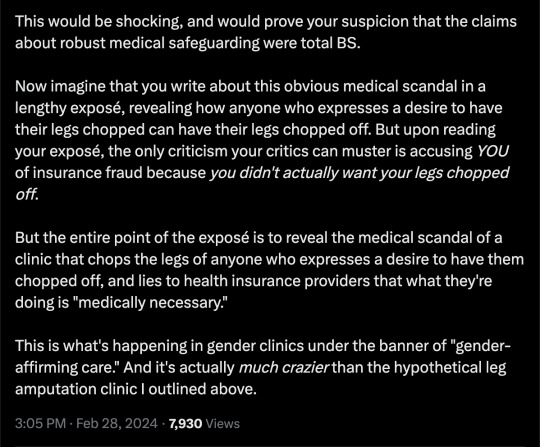
This is completely insane.
Apologists online are running around saying, but she didn't mean it, she was lying, she was pretending...
It doesn't matter.
Any kind of security, penetration or integrity test is insincere too. When security researchers compromise Microsoft's operating system or Google's browser or whatever, "but they didn't mean it" is not a defence to a discovered security flaw. It doesn't matter that the security researchers didn't plan to steal data or money or identities. The flaw in the system is there regardless.
It doesn't matter that it was insincere. Because the workers didn't know that. They never checked, never asked questions, never tested. They had been taught and instructed to never ask any questions. They did what they were supposed to. And the system failed spectacularly. Because that's what "gender affirming care" means.
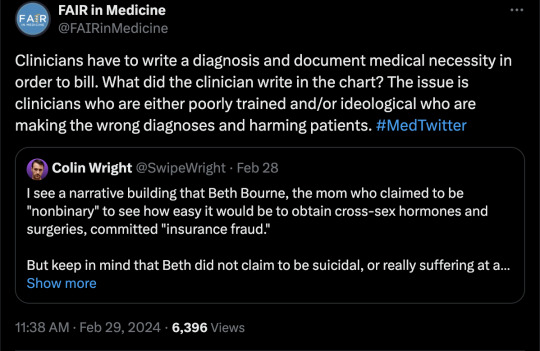
Additionally, the claim that Beth Bourne committed fraud is an outright lie. A patient cannot bill. They do not have the authority. The medical clinic is the only one that can bill, and they must supply a diagnosis and a medical necessity.
If they didn't diagnose her and just wrote down what she said, then they committed fraud. If they claim they did diagnose her, then they committed fraud, because the diagnosis they concocted was bogus. This, by the way, is actually going on. Clinics are reporting fake endocrine and other disorders to get blockers, hormones and other interventions. Jamie Reed and other whistleblowers have documented evidence of this. Beth Bourne is not responsible for what the clinic does. They have medical licenses and legal responsibility. Not her.
Additionally, anyone who actually read the article would know how she tested the system. She said things like, "I've always been not that feminine. So, maybe I get my boobs removed." And they said, "sure." Instead of saying, "wait, why do you think that?" Framing it as her lying is itself a lie. They violated their ethical obligations. That much is incontrovertible. And it's directly the result of "gender affirming care," where clinics and clinicians rubber-stamp anything deemed "trans" based entirely on ideological, not medical, grounds.
#Beth Bourne#undercover#undercover investigation#gender identity ideology#queer theory#nonbinary#non binary#top surgery#bottom surgery#double mastectomy#bilateral mastectomy#gender affirming care#gender affirming healthcare#gender affirmation#affirmation model#medical scandal#medical malpractice#medical corruption#religion is a mental illness
760 notes
·
View notes
Text
Medical Abbreviations on Pharmacy Prescriptions
Here are some common medical abbreviations you may see on pharmacy prescriptions:
qd - once a day
bid - twice a day
tid - three times a day
qid - four times a day
qh - every hour
prn - as needed
pc - after meals
ac - before meals
hs - at bedtime
po - by mouth
IV - intravenous
IM - intramuscular
subQ - subcutaneous
mL - milliliter
mg - milligram
g - gram
mcg - microgram
stat - immediately, right away
NPO - nothing by mouth
cap - capsule
tab - tablet
susp - suspension
sol - solution
amp - ampule
inj - injection
Rx - prescription
C - Celsius
F - Fahrenheit
BP - blood pressure
HR - heart rate
RR - respiratory rate
WBC - white blood cell
RBC - red blood cell
Hgb - hemoglobin
Hct - hematocrit
PT - prothrombin time
INR - international normalized ratio
BUN - blood urea nitrogen
Cr - creatinine
Ca - calcium
K - potassium
Na - sodium
Cl - chloride
Mg - magnesium
PO2 - partial pressure of oxygen
PCO2 - partial pressure of carbon dioxide
ABG - arterial blood gas
CBC - complete blood count
BMP - basic metabolic panel
CMP - comprehensive metabolic panel.
ECG - electrocardiogram
EEG - electroencephalogram
MRI - magnetic resonance imaging
CT - computed tomography
PET - positron emission tomography
CXR - chest x-ray
CTX - chemotherapy
NSAID - nonsteroidal anti-inflammatory drug
DMARD - disease-modifying antirheumatic drug
ACE - angiotensin-converting enzyme
ARB - angiotensin receptor blocker
SSRI - selective serotonin reuptake inhibitor
TCA - tricyclic antidepressant
ADHD - attention deficit hyperactivity disorder
COPD - chronic obstructive pulmonary disease
CAD - coronary artery disease
CHF - congestive heart failure
DVT - deep vein thrombosis
GI - gastrointestinal
UTI - urinary tract infection
OTC - over-the-counter
Rx - prescription
OD - right eye
OS - left eye
OU - both eyes.
TID - thrombosis in dementia
TDS - ter die sumendum (three times a day)
BOM - bilaterally otitis media (infection in both ears)
BT - body temperature
C&S - culture and sensitivity
D/C - discontinue or discharge
D/W - dextrose in water
ETOH - ethyl alcohol
FUO - fever of unknown origin
H&P - history and physical examination
I&D - incision and drainage
I&O - intake and output
KVO - keep vein open
N&V - nausea and vomiting
PERRLA - pupils equal, round, reactive to light and accommodation
PR - per rectum
QAM - every morning
QHS - every bedtime
QOD - every other day
S/P - status post (after)
TPN - total parenteral nutrition
UA - urinalysis
URI - upper respiratory infection
UTI - urinary tract infection
VO - verbal order.
XRT - radiation therapy
YOB - year of birth
BRBPR - bright red blood per rectum
CX - cervix
DVT - deep vein thrombosis
GB - gallbladder
GU - genitourinary
HCV - hepatitis C virus
HPI - history of present illness
ICP - intracranial pressure
IVP - intravenous pyelogram
LMP - last menstrual period
MRSA - methicillin-resistant Staphylococcus aureus
MVA - motor vehicle accident
NKA - no known allergies
PEG - percutaneous endoscopic gastrostomy
PRN - pro re nata (as needed)
ROS - review of systems
SOB - shortness of breath
TAH - total abdominal hysterectomy.
TIA - transient ischemic attack
Tx - treatment
UC - ulcerative colitis
URI - upper respiratory infection
VSD - ventricular septal defect
VTE - venous thromboembolism
XR - x-ray
w/c - wheelchair
XRT - radiation therapy
ASD - atrial septal defect
Bx - biopsy
CAD - coronary artery disease
CKD - chronic kidney disease
CPAP - continuous positive airway pressure
DKA - diabetic ketoacidosis
DNR - do not resuscitate
ED - emergency department
ESRD - end-stage renal disease
FFP - fresh frozen plasma
FSH - follicle-stimulating hormone.
GCS - Glasgow Coma Scale
Hct - hematocrit
Hgb - hemoglobin
ICU - intensive care unit
IV - intravenous
JVD - jugular venous distension
K - potassium
L - liter
MCH - mean corpuscular hemoglobin
MI - myocardial infarction
Na - sodium
NGT - nasogastric tube
NPO - nothing by mouth
OR - operating room
PCN - penicillin
PRBC - packed red blood cells
PTT - partial thromboplastin time
RBC - red blood cells
RT - respiratory therapy
SOA - short of air.
SCD - sequential compression device
SIRS - systemic inflammatory response syndrome
STAT - immediately
T - temperature
TPN - total parenteral nutrition
WBC - white blood cells
ABG - arterial blood gas
A fib - atrial fibrillation
BPH - benign prostatic hypertrophy
CBC - complete blood count
CO2 - carbon dioxide
COPD - chronic obstructive pulmonary disease
CPR - cardiopulmonary resuscitation
CT - computed tomography
CXR - chest x-ray
D5W - dextrose 5% in water
Dx - diagnosis
ECG or EKG - electrocardiogram
EEG - electroencephalogram
ETO - early termination of pregnancy.
FHR - fetal heart rate
GSW - gunshot wound
H&P - history and physical exam
HCG - human chorionic gonadotropin
I&D - incision and drainage
IBS - irritable bowel syndrome
ICP - intracranial pressure
IM - intramuscular
INR - international normalized ratio
IOP - intraocular pressure
LFT - liver function test
LOC - level of consciousness
LP - lumbar puncture
NG - nasogastric
OA - osteoarthritis
OCD - obsessive-compulsive disorder
OTC - over-the-counter
P - pulse
PCA - patient-controlled analgesia
PERRLA - pupils equal, round, reactive to light and accommodation.
PFT - pulmonary function test
PICC - peripherally inserted central catheter
PO - by mouth
PRN - as needed
PT - physical therapy
PT - prothrombin time
PTSD - post-traumatic stress disorder
PVC - premature ventricular contraction
QD - once a day
QID - four times a day
RA - rheumatoid arthritis
RICE - rest, ice, compression, elevation
RSI - rapid sequence intubation
RSV - respiratory syncytial virus
SBP - systolic blood pressure
SLE - systemic lupus erythematosus
SSRI - selective serotonin reuptake inhibitor
STAT - immediately
TB - tuberculosis
TIA - transient ischemic attack.
TID - three times a day
TKO - to keep open
TNTC - too numerous to count
TPN - total parenteral nutrition
URI - upper respiratory infection
UTI - urinary tract infection
V-fib - ventricular fibrillation
V-tach - ventricular tachycardia
VA - visual acuity
WNL - within normal limits
AED - automated external defibrillator
ARDS - acute respiratory distress syndrome
BID - twice a day
BP - blood pressure
BUN - blood urea nitrogen
CAD - coronary artery disease
CHF - congestive heart failure
CVA - cerebrovascular accident
D/C - discontinue
DKA - diabetic ketoacidosis.
DM - diabetes mellitus
DVT - deep vein thrombosis
EGD - esophagogastroduodenoscopy
ER - emergency room
F - Fahrenheit
Fx - fracture
GI - gastrointestinal
GTT - glucose tolerance test
HCT - hematocrit
Hgb - hemoglobin
HRT - hormone replacement therapy
ICP - intracranial pressure
IDDM - insulin-dependent diabetes mellitus
IBS - irritable bowel syndrome
IM - intramuscular
IV - intravenous
K - potassium
KVO - keep vein open
L&D - labor and delivery
LASIK - laser-assisted in situ keratomileusis.
ROM - range of motion
RT - radiation therapy
Rx - prescription
SCD - sequential compression device
SOB - shortness of breath
STD - sexually transmitted disease
TENS - transcutaneous electrical nerve stimulation
TIA - transient ischemic attack
TSH - thyroid-stimulating hormone
UA - urinalysis
US - ultrasound
UTI - urinary tract infection
VD - venereal disease
VF - ventricular fibrillation
VT - ventricular tachycardia
WBC - white blood cell
XRT - radiation therapy
XR - x-ray
Zn - zinc
Z-pak - azithromycin (antibiotic).
AAA - abdominal aortic aneurysm
ABG - arterial blood gas
ACS - acute coronary syndrome
ADL - activities of daily living
AED - automated external defibrillator
AIDS - acquired immunodeficiency syndrome
ALS - amyotrophic lateral sclerosis
AMA - against medical advice
AML - acute myeloid leukemia
APAP - acetaminophen
ARDS - acute respiratory distress syndrome
ASCVD - atherosclerotic cardiovascular disease
BPH - benign prostatic hyperplasia
BUN - blood urea nitrogen
CABG - coronary artery bypass graft
CBC - complete blood count
CHF - congestive heart failure
COPD - chronic obstructive pulmonary disease
CPAP - continuous positive airway pressure
CRF - chronic renal failure.
CT - computed tomography
CVA - cerebrovascular accident
D&C - dilation and curettage
DVT - deep vein thrombosis
ECG/EKG - electrocardiogram
EEG - electroencephalogram
ESRD - end-stage renal disease
FSH - follicle-stimulating hormone
GERD - gastroesophageal reflux disease
GFR - glomerular filtration rate
HbA1c - glycated hemoglobin
Hct - hematocrit
HIV - human immunodeficiency virus
HPV - human papillomavirus
HTN - hypertension
IBD - inflammatory bowel disease
IBS - irritable bowel syndrome
ICU - intensive care unit
IDDM - insulin-dependent diabetes mellitus
IM - intramuscular.
IV - intravenous
LFT - liver function test
MI - myocardial infarction
MRI - magnetic resonance imaging
MS - multiple sclerosis
NPO - nothing by mouth
NS - normal saline
OCD - obsessive-compulsive disorder
OSA - obstructive sleep apnea
PCOS - polycystic ovary syndrome
PMS - premenstrual syndrome
PPD - purified protein derivative
PSA - prostate-specific antigen
PT - prothrombin time
PTT - partial thromboplastin time
RA - rheumatoid arthritis
RBC - red blood cell
RSV - respiratory syncytial virus
SLE - systemic lupus erythematosus
TB - tuberculosis.
It is important to remember that medical abbreviations can vary based on location and specialty.
Healthcare professionals should use medical abbreviations with caution and only when they are familiar with their meanings.
Patients should always communicate any questions or concerns they have about their medications or medical care to their healthcare provider or pharmacist to ensure they receive safe and accurate medical care.

7 notes
·
View notes
Text
Magdalena Rodriguez-Ortega, 23 (USA 1994)
“I knew I screwed up.” That’s what abortionist Suresh Gandotra said about the day he was doing an abortion and he pulled out his client’s bowel instead of fetal body parts.
Magdalena Ortega-Rodriguez was 23 years old when she went to an abortion facility on December 8, 1994. She had no idea that she would never walk out of the building. What she received from El Norte Clinica Medica was not medical treatment but a horrific death for her baby and herself.
The abortionist was Gandotra, who had already mutilated an abortion client in 1991 so severely that surgeons had trouble identifying which organ was which. Yet he was still allowed to continue his career as an abortionist long enough to mutilate and kill Magdalena.
On that day, Gandotra called a hospital and asked for directions to send Magdalena there in a car. The staff at the hospital heard the description of her condition and told Gandotra that Magdalena needed an ambulance. The hospital started assembling a team for the catastrophic injuries and waited to receive their patient.
Gandotra left the bleeding Magdalena unmonitored and alone while he did more abortions on his other clients. After half an hour, he finally called an ambulance. But when he called, he did not inform them that there was a team at a hospital already preparing to treat her.
Paramedics found Magdalena in ventricular fibrillation, with no pulse, bleeding, and on the floor. Because they were not told about the hospital that was awaiting this critically injured patient, they took Magdalena to another hospital that was not prepared to treat a patient with her specific injuries. Gandotra didn’t tell the paramedics anything about Magdalena’s condition or send her medical history.
A nurse at the hospital that attempted to treat Magdalena said, “I’ve never seen anything like this before and I don’t want to again.” When Magdalena was rushed into surgery, it was discovered that her cervix, uterus, bladder and colon were all lacerated. Her uterus was ruptured with a severed limb from her baby protruding into her abdomen. When the surgeon opened Magdalena’s peritoneum, the operating room was spattered with escaping blood because the peritoneum was so distended with blood.
Magdalena bled to death during her emergency surgery. Her cause of death was listed as “complications of the acute pelvic injuries which consisted of lacerations of the lower uterus, vagina, bladder and colon.” Her baby’s corpse was also autopsied with equally disturbing results. Not only had Gandotra dramatically miscalculated gestational age, but the autopsy report described “the body of the baby was not complete when autopsied. Both arms had been cut off; the heart, lungs, liver, and other organs had been cut out, the front of the chest and abdomen were missing, the right femur was fractured, the head was intact except for an area on the scalp which had been taken off from the back of the head.”
Gandotra told the medical board that he delayed calling an ambulance because he had no admitting privileges and claimed that the patient had asked to be released so she could walk home. Gandotra’s attorney said, “We don’t believe this was below the standard of care nor do we believe it was malpractice.” Despite these claims, the abortion facility was shut down.
If this was Gandotra’s idea of the standard of care for “safe and legal” abortion, what would he have to had done to a client for him to admit malpractice?
San Diego Reader 12/13/94
San Diego Union-Tribune 12/13/94, 12/17/94
Orange County Register 12/15/94
Santa Monica Outlook December 1994
“Abortion clinic closed after a patient’s death,” Santa Cruz (CA) Sentinel Sun, December 18, 1994

“O.C. Doctor Investigated in Abortion Death,” Los Angeles Times, 12/15/94
“Abortion Patient’s Death Shows License System Flaws,” Los Angeles Times 3/21/95
San Diego County South Bay Judicial District, California Superior Court Case No. S6003494

San Diego County Superior Court Case No. 661720
San Diego County Court Case No. 643695
(Medical Board Of California documents)
#tw gore#tw blo0d#tw extreme gore#tw mutilation#tw dismemberment#tw death#tw blood spatter#abortion#tw abortion#pro choice#pro life#abortion debate#tw murder#tw ab*rtion#unsafe yet legal
7 notes
·
View notes
Note
now i have an idea to write (consensusal) unhinged/r.a.c.k mina/jack/jonathan but also none of the parties wants jack getting pregnant by jonathan in particular but he still will take the risk and my struggle™️ is not easily finding good sources for victorian birth control/practices regardless of legality 😔 this wasn't in my 2022 bingo etc
CORRECTION: Contraception was made illegal in the US at the time. I've heard people say this was true of the UK too, but I literally cannot find any corroborating sources. So, Mina et al probably just used whatever they felt like for birth control.
And there were a lot of options!
Family planning was a big deal and Jack's got two prescriber licenses and pharmacies were not exactly the dystopian white wall spaces we have today.
So, you can easily justify him having access to any of the following:
'Cervical/womb veils' icluding the entire range of what today we call internal condoms, diaphragms and cervical caps. Rubber technology was good enough by 1845 to make these fairly widespread. My understanding is, they were generally more popular with married women than working girls, which makes sense given how finnicky they are.
Cervical injection, aka using a needle to wash the cervix out with a spermicidal solution after sex. This was actually considered rather Old Fashioned by the 1890s but would have been well known.
External condoms were more popular in the US, but fortunately Jack's good friend Quincey would know all about that. They had been made of animal products or treated fabric for centuries, but the more durable, comfortable rubber ones we use today had been invented by the 1870.
Vaginal sponges either dry to absorb semen or, more effectively, soaked in oils to reduce sperm mobility and spermicidal chemicals.
Spermicidal suppository: A newcomer by the 1890s, these were popular but among the most inconsistent methods available.
Hormonal methods were rare. Hormones were only identified in 1890 and wouldn't even be named for another 15 years. But, they weren't unknown, just poorly understood. Mostly, these were used for abortion, not contraception.
Additionally, basically all of the methods of abortion we have today existed in less advanced forms then. Assuming Jack still menstruates regularly enough to notice the delay, he could probably self-administer a vacuum removal with tools available at the time.
Otherwise, VH would certainly be able to administer any other methods, including induced miscarriage and menstruation, which today we tend to do with a combination misoprosotl/mifeprestone tablet, and at the time would likely involve those 'poorly understood' hormonal treatments.
THE FOLLOWING IS OUTDATED MEDICAL INFORMATION. IF YOU NEED AN ABORTION IN A RESTRICTED AREA, PLEASE DO NOT TRY THESE. THEY SHOULD BE PERFORMED ONLY UNDER MEDICAL SUPERVISION AS THE RISK OF POISONING IS HIGH. NONE OF THESE ARE AS SAFE AND EFFECTIVE AS MODERN MEDICINES.
All of these methods assume Jack would be able to identify conception within one month of intercourse.
Citrus juice diet (controlled vitamin C overdose). Highly unpleasant. Causes massive digestive pain. Interferes with progesterone production and can prevent implantation or cause miscarriage early in pregnancy. Purified vitamin c wasn't a thing yet, and citric acid (not ascorbic) is responsible for most of the side effects.
Parsley juice and pessary: Used alongside citrus juice to soften the cervix allowing the miscarriage, if induced, to pass more easily. If used immediately after sex, can sometimes cause menstruation early, preventing implantation.
Cotton root (like, from a cotton plant) at high enough doses can cause uterine spasms, which may be enough to expel a fertilized egg.
Wild carrot seed. DO NOT CONFUSE FOR HEMLOCK WHEN FORAGING. Another implantation inhibitor, generally used from the time of the sex until menstruation occurs naturally, so more of an emergency contraception than anything. Also more popular in the US, since the wild carrot grows so well here it borders on invasive.
2 notes
·
View notes
Text
Early detection of cancer is crucial for several reasons:
Increased Treatment Options: When cancer is detected early, there are often more treatment options available. Early-stage cancers may be more responsive to treatment and may require less aggressive therapies, resulting in better outcomes and fewer side effects.
Improved Survival Rates: Early detection generally leads to better survival rates. Cancers that are diagnosed at an early stage are more likely to be treated successfully, leading to higher chances of long-term survival and even cure.
Reduced Morbidity and Mortality: Early detection can help prevent cancer from spreading to other parts of the body, reducing the risk of complications and improving overall quality of life.
Lower Treatment Costs: Treating cancer in its early stages is often less costly than treating advanced-stage cancers. Early detection can help reduce the financial burden on individuals, families, and healthcare systems.
Easier Treatment: Early-stage cancers may require less aggressive treatments, such as surgery or localized therapies, which may be less physically and emotionally taxing on patients.
Overall, early detection plays a pivotal role in improving cancer outcomes, reducing mortality rates, and enhancing the effectiveness and tolerability of treatments. This underscores the importance of regular cancer screening and awareness of early signs and symptoms.
Several screening methods are available for various types of cancer. Here are some common ones:
Breast Cancer:
Mammography: X-ray imaging of the breast tissue to detect abnormalities.
Clinical Breast Exam: Physical examination of the breasts by a healthcare provider.
Cervical Cancer:
Pap Smear: Collection of cells from the cervix to detect abnormal changes.
HPV Testing: Screening for high-risk strains of human papillomavirus, which can cause cervical cancer.
Colorectal Cancer:
Colonoscopy: Visual examination of the colon and rectum using a flexible, lighted tube.
Fecal Occult Blood Test (FOBT): Tests for the presence of blood in stool samples.
Stool DNA Test: Detects DNA changes in stool samples that may indicate colorectal cancer.
Prostate Cancer:
Prostate-Specific Antigen (PSA) Test: Blood test measuring levels of PSA, a protein produced by the prostate gland.
Digital Rectal Exam (DRE): Physical examination of the prostate gland through the rectum.
Lung Cancer:
Low-Dose Computed Tomography (LDCT): X-ray imaging of the lungs to detect abnormalities in high-risk individuals, such as heavy smokers.
Skin Cancer:
Visual Inspection: Regular self-examination of the skin to detect changes in moles or other skin abnormalities.
Dermatologist Examination: Professional examination of the skin by a dermatologist.
Ovarian Cancer:
Transvaginal Ultrasound: Imaging test using sound waves to examine the ovaries for abnormalities.
CA-125 Blood Test: Measures levels of CA-125, a protein that may be elevated in ovarian cancer.
Choice of screening method may depend on factors such as age, sex, family history, and individual risk factors. Screening guidelines may also vary among different organizations and regions. Get the best treatment for cancer and a full body health checkup done at the best hospitals in India.
1 note
·
View note
Text
The Importance of Regular Gynecological Cancer Screenings

In reality as we know it where wellbeing frequently takes a secondary lounge to our warmed ways of life, it’s important to clear light on the importance of regular gynecological cancer screenings. Dr. Kunnal Shinde, a recognized Gyneac Cancer Specialist in Pune, Maharashtra, emphasizes the significance of ending the quiet by wrapping these screenings. In this blog, we explore why regular gynecological cancer screenings are a must for a healthy and peaceful.
Gynecological Cancer: The Silent Threat:
Dr. Kunaal shinde tells about gynecological cancers, including cervical, ovarian, uterine, cervical, and vaginal cancers, which impact millions of women worldwide. often develop silently, without detectable signs in the early stages. While these cancers can be devastating, in any case, fortunately, large numbers of them are preventable or treatable when seen early. This silent progression makes regular screenings a strong tool in early detection, drastically improving the chances of successful treatment. This is where common gynecological cancer screenings come in.
What are gynecological cancer screenings?
Gyneac Surgical oncologist in Pune, Dr. Shinde tests that specialists use to search for early signs of cancer in the reproductive organs. Dr. Kunnal Shinde is concerned with various screening methods, such as Pap smears, HPV tests, pelvic exams, mammograms, and genetic testing, underlining their roles in specifying possible risks. By providing exhaustive information on these screenings, we aim to fit women with the knowledge needed to make informed judgments about their health.
The most standard types of screenings include:
Pap test: This test checks for irregular cells on the cervix, which can be a precursor to cervical cancer. It is usually done every 3-5 years for women aged 21-65.
HPV test: This test notices the presence of human papillomavirus (HPV), which is the main risk factor for cervical cancer. It’s often connected with the Pap test for women aged 30 and above.
Pelvic exam: This exam allows Dr. Shinde to feel for any lumps or masses in your uterus, ovaries, or fallopian tubes. It is usually done during your annual well-woman exam.
Transvaginal ultrasound (TVU): This test uses sound waves to create images of your uterus and ovaries. It may be used to screen for ovarian cancer in women at high risk.
CA-125 blood test: This test estimates the level of a protein called CA-125 in your blood. While not a typical test for ovarian cancer, it can be used to help observe women who are at high risk.
Why are gynecological cancer screenings important?
Early detection saves lives: Gynecological malignant changes repeatedly don’t display side effects until they come at cutting edge phases. By the time signs appear, treatment options become limited, and the forecast declines. Screenings catch precancerous cells or early-stage cancers, allowing for timely intervention and improved results.
Peace of mind: Normal screenings give true serenity, realizing you’re assuming command over your wellbeing. Early detection can help anxiety and allow you to focus on enjoying life to the fullest.
Improved treatment options: Early-stage cancers offer a wider range of treatment options, often less invasive and with higher success rates. This means more limited recuperation times and better personal satisfaction during and after treatment.
Who should get screened?
Dr. Kunnal Shinde Suggests all women should get screened for cervical cancer, starting at age 21. The suggested screening schedule may vary depending on your age, risk aspects, and medical record. Talk to our Gyneac Surgical oncologist in Pune about the best screening schedule for you.
What are the benefits of gynecological cancer screenings?
Dr. Kunnal Shinde Suggests many benefits of gynecological cancer screenings, including:
Early detection of cancer: Screenings detect early cancers or precancerous alterations before any symptoms appear. This implies that there is potential for simpler, more effective treatment with greater rates of cure.
Improved survival rates: Early detection can seriously improve the possibilities of successful therapy and cure.
Peace of mind: Knowing that you are cancer-free can give you peace of mind.
What are the risks of gynecological cancer screenings?
Dr. Kunnal Shinde is the best gynecologist in Pune. he is signify cancer screenings are generally secure. However, there are some possible risks, such as:
Discomfort: Some screenings, such as pap tests, can be painful.
False negatives: A false negative is a test result that suggests cancer is not current when it is. This can delay diagnosis and therapy.
False positives: A false positive is a test result that indicates cancer is present when it is not. This can cause stress and worry.
What can I do to reduce my risk of gynecological cancer?
There are a few things you can do to decrease your risk of gynecological cancer, such as:
Getting vaccinated against HPV
Holding a healthy weight
Not smoking
Limiting alcohol intake
Exercising regularly
Conclusion:
Regular gynecological cancer screenings are important in the fight against silent and potentially killer conditions. Dr. Kunnal Shinde’s expertise underscores the need for proactive measures, early detection, and education to break the quiet surrounding gynecological cancers. By prioritizing regular screenings, women can take control of their health and well-being, providing a brighter and more beneficial future.
#Laparoscopic Surgeon in Pune#Laparoscopic specialist in Pune#Gynaec Laparoscopic Surgeon in Pune#Best Gynaec Laparoscopic Surgeon in Pune
0 notes
Text
What Is Cervical Dysplasia? - Treatment & Prevention | familydoctor.org
So this is my second time having cervical dysplasia; and this time the doctor said "The 'C' Word". We're just doing the testing right now. Biopsies and the like, painful, but necessary. I get my results on August 8th 2023
0 notes
Text
Top Cancer Hospital in Aurangabad: A Comprehensive Guide for Cancer Patients
Aurangabad, a city in the state of Maharashtra in India, is known for its rich cultural heritage and historical monuments. In recent years, the city has also emerged as a hub for advanced medical care, with top Clinic offering state-of-the-art treatment for various ailments, including cancer.
Cancer is a disease that affects many peoples around the world, and the number of cases is on the rise. The good news is that with advancements in medical technology and research, the chances of surviving cancer have improved significantly. However, timely diagnosis and appropriate treatment are crucial in the fight against cancer.
If you or a loved one has been diagnosed with cancer, finding the right hospital for treatment can be a daunting task. To help you in your search, we have suggested the best cancer hospitals in Aurangabad.
OncoRelief Cancer Clinic
OncoRelief Cancer Clinic is really a center point of hope for disease patients We guarantee you that patients can battle against cancer growth as opposed to fear it. We help our patients in their battle against cancer, from screening and finding to appropriate cancer treatment, then, at that point, let it be corrective or palliative.
We provide compassionate, top-caliber, and cost-effective Healthcare to everybody.
Dr. Aditya D Mantri is a Surgical Oncologist in Aurangabad. He did his MBBS from Grant Medical College & Sir. JJ Hospital Mumbai, MS from Govt. Medical College Miraj, M.Ch from GCRI & BJMC Civil Hospital Ahmedabad etc. His expertise lies in Head & Neck Cancer, Breast Cancer, Thoracic tumour, Cervix, Stomach cancer, Colon Rectal cancer, CA Pancreas, Small Bowel GIST, Clinical Trial, Soft Tissue Sarcomas. He is a member of International Federation Head & Neck Onco Surgeon.
In conclusion, Aurangabad has top-notch cancer hospital that offer world-class cancer care services. When choosing a cancer hospital, it is essential to consider factors such as the expertise and experience of the medical team, the quality of equipment and technology available, and the range of treatment options offered. We hope this article helps you make an informed decision about the best cancer hospital in Aurangabad for your needs.
Do visit for more information on:- www.oncorelief.in
#Best cancer Hospital Aurangabad#Best Cancer doctor Aurangabad#breast cancer surgeon Aurangabad#GI onco surgeon Aurangabad#Head Neck cancer surgeon Aurangabad#Best Gynec onco Surgeon Aurangabad#Chemotherapy Specialist Aurangabad
1 note
·
View note
Text
Ovarian Cancer Diagnostics Market is projected to reach USD 1,836.03 million during the forecast period to 2029
The tests and procedures used to diagnose ovarian cancer includes the pelvic exam, imaging tests, blood tests, surgery and among others. During a pelvic exam, the doctor inserts gloved fingers into the vagina and simultaneously presses a hand on your abdomen in order to feel (palpate) your pelvic organs. The doctor also visually examines the vagina, cervix and external genitalia. Ovarian cancer is a type of cancer that begins in the ovaries, there are several types of ovarian cancer, the most common of which is epithelial ovarian cancer. The primary cause of this type of cancer is uncontrollable cell growth in the ovarian tissue, and it is one of the leading causes of death in women worldwide. It is the fifth leading cause of cancer death in women worldwide, and the tenth leading cause of cancer death in women in the United States.
Data Bridge Market Research analyses that the ovarian cancer diagnostics market which was USD 1,084.7 million in 2021, is expected to reach USD 1,836.03 million by 2029, at a CAGR of 6.80% during the forecast period 2022 to 2029. In addition to the insights on market scenarios such as market value, growth rate, segmentation, geographical coverage, and major players, the market reports curated by the Data Bridge Market Research also include depth expert analysis, patient epidemiology, pipeline analysis, pricing analysis, and regulatory framework.
Get Sample PDF Report – https://www.databridgemarketresearch.com/reports/global-ovarian-cancer-diagnostics-market
Some of the major players operating in the ovarian cancer diagnostics market are:
Abbott (U.S.) F. Hoffmann-La Roche Ltd (Switzerland) QIAGEN (Germany) Quest Diagnostics Incorporated. (U.S.) Hologic, Inc. (U.S.) Arbor Vita Corporation (U.S.) Guided Therapeutics, Inc. (U.S.) CooperSurgical Inc (U.S.) BD (U.S.) Cardinal Health (U.S.) Siemens Healthcare Private Limited (Germany) Zilico (U.K.) GenomeMe Lab Inc. (Canada) Exact Sciences Corporation (U.S.) Fujirebio (Japan), Advaxis Inc. (U.S.) Pfizer Inc. (U.S.) GlaxoSmithKline plc. (U.K.) Bristol-Myers Squibb Company (U.S.) Merck & Co., Inc (U.S.) Global Ovarian Cancer Diagnostics Market Dynamics
Drivers
Novel biosensor for monitoring ovarian cancer tumors will promote growth Carcinoma antigen 125 (CA 125) has been identified as a clinical glycoprotein/biomarker for the early detection of ovarian cancer. As a result, accurate carcinoma antigen 125 determination is critical for cancer diagnosis and treatment. To detect the carcinoma antigen 125 biomarker in human plasma samples, a new biosensor was developed. The surface morphology of the electrode was investigated using field emission scanning electron microscopy (FE-SEM) and energy dispersive spectroscopy (EDS). Transmission electron microscopy (TEM) was used to investigate the mechanism of nano-ink production. The formation of an antigen-antibody complex was also monitored using differential pulse voltammetry (DPV). For detecting the carcinoma antigen 125 biomarker, the designed immunosensor performed well, with excellent specificity and sensitivity. Therefore, based on the results, it is concluded that immunosensor has the potential to be employed in the early detection of ovarian cancer in clinical studies. These all are the novel biosensors which helps the market to grow.
Increased prevalence of ovarian cancer in the number of elderly women The growing economies of both developed and developing countries are driving the expansion of healthcare. As a result, they are assisting in the advancement of the global ovarian cancer diagnostics market. The global ovarian cancer diagnostics market is expected to grow as the incidence of ovarian cancer rises, new treatments and therapies become more widely available, and healthcare spending rises. Ovarian cancer has become more common as the female population has aged. The ovarian cancer market is being driven forward by rising ovarian cancer prevalence, the introduction of new medications and therapies, increased healthcare expenditure, and increased government funding.
Opportunities
Rising development to propel growth Drugs such as Bevacizumab (Avastin) and Pazopanib (Votrient) are expected to stimulate the market, which is currently dominated by generics like paclitaxel and carboplatin. The development of new medications to treat this type of cancer is expected to significantly benefit the market. Ongoing research and development to develop effective treatment interventions for various disorders supports the global ovarian cancer diagnostics market.
To Obtain More Insights into Market Analysis, Browse Research Report Summary @– https://www.databridgemarketresearch.com/request-a-sample/?dbmr=global-ovarian-cancer-diagnostics-market
Global Ovarian Cancer Diagnostics Market Scope
The ovarian cancer diagnostics market is segmented on the basis of diagnosis type, cancer type and end use. The growth amongst these segments will help you analyze meagre growth segments in the industries and provide the users with a valuable market overview and market insights to help them make strategic decisions for identifying core market applications.
Diagnosis Type
Imaging CT Scan Ultrasound Positron Emission Tomography Scan Magnetic Resonance Imaging (MRI) Scan Others Biopsy Image Guided Biopsy Fine Needle Aspiration Biopsy Others Blood Test BRCA Carcinoma Antigen 125 Estrogen Receptor/Progesterone Receptor HER2 Carcinoembryonic Antigen Test Kirsten Rat Sarcoma virus Mutation Others Others Cancer Type
Germ Cell Tumor Stromal Cell Tumor Epithelial Tumor Others End-use
Cancer Diagnostic Centers Hospital Laboratories Research Institutes Others Ovarian Cancer Diagnostics Market Regional Analysis/Insights
The ovarian cancer diagnostics market is analysed and market size insights and trends are provided by country, diagnosis type, cancer type and end use as referenced above. The countries covered in the ovarian cancer diagnostics market report are U.S., Canada and Mexico in North America, Germany, France, U.K., Netherlands, Switzerland, Belgium, Russia, Italy, Spain, Turkey, Rest of Europe in Europe, China, Japan, India, South Korea, Singapore, Malaysia, Australia, Thailand, Indonesia, Philippines, Rest of Asia-Pacific (APAC) in the Asia-Pacific (APAC), Saudi Arabia, U.A.E, South Africa, Egypt, Israel, Rest of Middle East and Africa (MEA) as a part of Middle East and Africa (MEA), Brazil, Argentina and Rest of South America as part of South America.
North America dominates the ovarian cancer diagnostics market due to the rising awareness about the disease and availability of advanced diagnostic technology. Awareness among the people about the disease is also one of the major factors boosting the market in this region. Asia-Pacific is expected to grow at the highest growth rate in the forecast period of 2022 to 2029 due to rise in prevalence of ovarian cancer.
Browse Complete TOC at- https://www.databridgemarketresearch.com/toc/?dbmr=global-ovarian-cancer-diagnostics-market
The country section of the report also provides individual market impacting factors and changes in regulation in the market domestically that impacts the current and future trends of the market. Data points like down-stream and upstream value chain analysis, technical trends and porter’s five forces analysis, case studies are some of the pointers used to forecast the market scenario for individual countries. Also, the presence and availability of global brands and their challenges faced due to large or scarce competition from local and domestic brands, impact of domestic tariffs and trade routes are considered while providing forecast analysis of the country data.
Top Healthcare Report Links:-
About Data Bridge Market Research:
An absolute way to predict what the future holds is to understand the current trend! Data Bridge Market Research presented itself as an unconventional and neoteric market research and consulting company with an unparalleled level of resilience and integrated approaches. We are committed to uncovering the best market opportunities and providing effective insights for your business to thrive in the market. Data Bridge strives to provide appropriate solutions to complex business challenges and initiates an effortless decision-making process. Data Bridge is a body of pure wisdom and experience that was formulated and framed in 2015 in Pune.
Data Bridge Market Research has over 500 analysts working across different industries. We have served over 40% of Fortune 500 companies globally and have a network of over 5,000 clients worldwide. Data Bridge knows how to create satisfied customers who trust our services and trust our hard work with certainty. We are satisfied with our 99.9% customer satisfaction rate.
Contact us:-
Data Bridge Market Research
USA : +1 888 387 2818
UK: +44 208 089 1725
Hong Kong : +852 8192 7475
Email:– [email protected]
0 notes
Text
Week 2.1 Getting in Deep and class notes
My main point for my campaign is to raise awareness on the prevention of Ovarian Cancer and to make these things accessible to all females of New Zealand.
Articles and websites found that relate to my topic
instagram
instagram
These instagram posts from the Talk Peach gynaecological charity show how visuals can be made without necessarily making someone uncomfortable when looking at them. Although I feel as though subjects like this should not be taken lightly, I do appreciate that there are people who are not used to these types of conversations.
My awareness campaign would include normalising getting looked at by a gynaecologist as well as normalising the conversations that happen. Young females especially shouldn't feel uncomfortable speaking about these issues and so eliminating the stigma that these sorts of things should be kept private is key.
Censorship around these sorts of topics only enforces those stigmas.
The five-year survival rate for ovarian cancer in New Zealand is 39%. It has a 70% chance of recurrence post treatment, the survival statistics for ovarian cancer have remained virtually unchanged for 30 years. This is literally a crisis point in terms of advancement in survival rates for cancers.
Breast cancer used to have a similar outlook but now thanks to incredible advocacy, large scale fundraising and an immense amount of research the breast cancer 10 year survival rate is 75% if a lump is the first sign or 92% if detected via a regular mammogram.
We believe with better funding this can be achieved for ovarian cancer too.
Shockingly over the past 3 years the government has funded $0.00 to research (out of a half billion government allocation) on one of our highest cancer killers.
1 New Zealander dies from it every 48 hours.
Only 4 out of 10 diagnosed with ovarian cancer will survive five years after diagnosis. This compares to 9 in 10 women surviving breast cancer in the same period. Because there is no screening test for ovarian cancer, early diagnosis is your best chance at survival, a late diagnosis is very hard to beat.

from @talkpeach on instagram
Most people are diagnosed once the cancer has already spread, making it more difficult to treat. There are often delays in diagnosing ovarian cancer, that is because there is no screening test, huge gaps in awareness and symptoms are often confused with symptoms of other less severe illnesses, particularly gastrointestinal complaints.
Five-year ovarian cancer survival rates vary around the world, they range from 30% to 45%. In new Zealand they are at 38% compared to Australia at 45%. By comparison the five year survival rates for women with breast cancer range from 80% to 92%. Ovarian cancer is overlooked and underfunded, yet all those with ovaries are at risk of developing this disease.
information from the Talk Peach instagram.
Week 2.1 - Design Studio class
identifying relevant research for awareness campaign
connectivity and research
Locate relevant and current news, stories, opinion, narratives data and statistics aligned to your topic. Can any of this information be used s potential content in your campaign in some way? Is further research needed for content?
Etymology is the study of the origin of words and the way which their meanings have changed throughout history.
Text
Facts
Reports
Information
testimonials
annual report
Content is key = collecting the content
Infographics
visual analytics
Visual elements engage the audience more
Reinterpreting data
Visual information goes to the brain 60,000 times faster
Curiosity is crucial
Ultrasound or CA-125 blood test
Screening exam
Make these exams and tests free for all females in New Zealand as smear and Pap tests and cervix exams do not pick up Ovarian cancer.
Repurpose information
Designing for social good, to shine a light on something, alert that something needs focus on.
Smear the stigma
Smear the shame
ovapower
Become an expert on your campaign topic.
Make discoveries that can assist your design systems
0 notes
Text
What are the symptoms of ovarian cancer and which is the best ovarian cancer treatment hospital Hyderabad?
Ovarian cancer has ranked fifth in cancer deaths among women. Ovarian cancer causes more death than any other cancer in the female reproductive system. Even only a few women are properly diagnosed with ovarian cancer from Ovarian Cancer Treatment Hospital Hyderabad during their lifetime because a lot of women do not have a proper screening for ovarian cancer screening and often the symptoms are subtle. According to medical studies most ovarian cancers are only diagnosed at a more advanced stage.
Hence in this article, we will tell you about the symptoms of ovarian cancer so that you can get the treatment at the right time and also where to go for ovarian cancer treatment Hospital Hyderabad.
But first what is ovarian cancer?
The growth of cells that forms in the ovaries is called ovarian cancer. Just like in other cancers, the cells multiply quickly and also can easily invade and destroy healthy blood tissues.
What are the symptoms of ovarian cancer?
When ovarian cancer is at the starting stage, usually there might not be any noticeable symptoms. And even what happens when ovarian cancer develops they are often confused with other diseases that also share the common symptoms just like ovarian cancer.
Symptoms of ovarian cancer include-
● Abdominal bloating or swelling
● Feeling immediately full even when eating
● Weight loss
● Problem in the pelvic area
● Fatigue
● Problem like back pain
● Constipation or changes in bowel habits
● Urinating frequently
How to diagnose ovarian cancer?
There are a lot of tests and procedures which are used to diagnose ovarian cancer.
Pelvic exam
In a pelvic exam, the doctor inserts two gloved fingers into a woman's vagina and dresses the abdomen so that they can feel the pelvic organs. And also the doctor inspects the external genitalia, vagina, and cervix
Imaging test
Imaging tests include ultrasound or CT scans of the abdomen or pelvis area to determine the size, shape, and structure of ovaries.
Blood test
Blood tests are always a helpful way in determining your overall health. The doctor might also recommend a test that indicates symptoms of ovarian cancer, for example, the CA 125 test is done to know the protein that's found on the surface of the ovarian cancer cells.
Surgery
At times when the doctor cannot be certain of the diagnosis, they will suggest you undergo surgery to remove an ovary and then have it tested for any symptoms of cancer.
Genetic testing
The doctor many times recommend testing a sample of the women's blood to look if any genetic changes can increase the overall risk of ovarian cancer.
What are the treatments for ovarian cancer?
The treatments present for ovarian cancer are as follows-
Surgery
One of the most recommended and common ways to remove ovarian cancer is by having surgery. There are many types of surgeries done to remove one ovary or even surgeries are done to remove both the ovaries or they are done to remove ovaries in the uterus and even there are surgeries for advanced cancer.
Chemotherapy
Chemotherapy is done to kill the fast-growing cells in the body that also include cancer cells.
Targeted therapy
Targeted therapy as the name suggests means there is targeted drug treatment that is focused on the specific weakness present within the cancer cell.
Hormone therapy
This therapy makes use of drugs to block any effect of the hormone estrogen on the cancer cells in the ovary. There are ovarian cancer cells that start using estrogen to help them grow, so blocking them helps in controlling cancer.
Which is the best ovarian cancer treatment Hospital Hyderabad?
Doctor Vels regenerative therapy is one of the world's best stem cell solution providers and one of the best clinics in Hyderabad for ovarian cancer and Endometriosis Treatment In Hyderabad.
The hospital aims to create awareness and reach maximum women for ovarian cancer treatment with the best treatment possible.
We have 10000 + regenerative therapies done, including 10 + qualified staff, and 2000 + satisfied patients. We aim to create awareness among the women who are suffering from ovarian cancer and provide the best treatment possible.
For more information visit our website now!
0 notes
Text
CARCTOL
What Is Carctol®?
CARCTOL® is a gift of timeless knowledge of Ayurveda, the complete science of perfection in life. CARCTOL® is a clinically proven herbal compound containing purely natural, rare and precious herbs. These herbs are mixed together in precise proportion to balance & nourish the entire body & strengthen the immune system. CARCTOL® also helps the cancer patients to fight cancer and also to combat the side effects of chemotherapy & radiotherapy.
“CARCTOL® has also been subjected to in-vitro study at the Advanced Cancer Research Centre of TATA, Mumbai against 14 types of human cancer cells out of which it was found effective against pancreatic and lung cancer. It was placed on record that CARCTOL® is being used for treatment of cancer patients both in the country and abroad. After preparation of dossiers, multi-centric clinical trials will be conducted,” sources in the Council said.
All the herbs used in CARCTOL® have been certified as anticancer by different countries. Apart from cancer all the herbs used in CARCTOL® have immune boosting properties.
CARCTOL® is totally safe for human consumption, it is as safe as food. A normal healthy individual can consume CARCTOL® as it has no known side effects. Ideally for the cancer patients CARCTOL® is advised to be taken for a minimum period of 60-90 days or as advised by your healthcare professional. Apart from its results on cancer it also boosts the immune system & regains the physical strength and normal body function over a period of time. Even after getting recovered by cancer many patients take CARCTOL® as prophylaxis, as it has no side effects & is as safe as food & can be consumed even by a normal person as supplement.
CARCTOL® IS INDICATED IN:-
Brain Cancer
Blood Cancer-CML/AML
Non Hodgking’s Lymphoma + TB
Prostate Cancer along with bone metastasis
Breast Cancer
Colon & Rectal Cancer
Abdomen Cancer
Duodenum Cancer
Liver Cancer
Kidney (Renal Cell) Cancer
Carcinoma of Testis
Urinary Bladder Carcinoma
Lung Cancer
Melanoma
Pancreatic Cancer
Bone Cancer
Carcinoma- Esophagus
Ovary + Omentum CA Cervix Cancer
Skin Cancer (Non- Melanoma)
Thyroid Cancer
Throat & Nasopharynx Cancer.
ADVANTAGES OF CARCTOL®
It is taken orally & is well tolerated by the patient.
It is effective even in terminal stage cancer.
It can be consumed precautionary to prevent recurrence, as it has no known side effects.
It can be consumed by a normal healthy individual to avoid the risk of cancer.
It is helpful in minimizing the side-effects of chemotherapy and radiotherapy.
It has no known side effects & is absolutely safe for human consumption.
It also boosts the immune system.
It regains the physical strength and normal body functions.
1 note
·
View note
Text
Urology Clinic With BPH Treatment
A terrific urology clinic must have all the normal components. A remarkable urology clinic with BPH Treatment need to have the capability to provide a complete series of services for customers who need them. The centers must likewise be accredited by the state to ensure they are providing quality care.
The prostate gland depends on the male body and belongs to the urinary system. It produces the fluid that lubes the urethra throughout sexual relations. About 8 million men in the United States have prostate cancer and more than thirty percent of these will pass away from it.
This condition is an improvement of the prostate gland, which produces severe testosterone in the body. Prostate cancer is an issue that can be treated with surgical treatment or radiation. Prostate cancer is the most normal kind of cancer in people. Typically it is treated with benign prostatic hyperplasia treatment, or BPH treatment.
A well licensed urology clinic with BPH Treatment must similarly have the capability to supply other treatments to help deal with the indications of prostate cancer. In fact, a few of the physician may also deal with the signs of benign prostatic hyperplasia. They will work thoroughly with the consumer and have the ability to assist technique the outright finest treatment techniques.

In addition to prostate surgical treatment, a urology clinic with BPH Treatment require to likewise make use of a total series of treatments for benign prostatic hyperplasia. Amongst the most common treatments used is the non-surgical treatment of BPH. Consumers who deal with BPH might want to consider this treatment considering that it can help reduce the indicators and boost their lifestyle.
Pelvic assessments are frequently done when a female very first checks out a doctor for her yearly checkup. This test, called a Pap smear, assists the physician determine whether a female has a development in her uterus or vaginal place. Often a development can activate symptoms that look like those of the signs of cancer.
The advancement can be little or big and can activate no signs at all. A Pap smear assists the physician to verify if the improvement is benign prostatic hyperplasia or if it is a deadly development. Some medical professional will send a special color through the cervix to see if the development modifications color.

Another normal benign development is called the Peters's duct. This advancement is generally found on the principle of the penis and forms a sac like structure that decreases the shaft. It can activate a similar series of signs to BPH.
BMP is another sort of benign enhancement that can be challenging to acknowledge. Doctor regularly consider BMP as a swelling on the testicles or under the scrotum. An improvement that runs along the side of the penis can likewise offer indicators, which is why it is usually considered a benign development instead of a deadly one.
An extraordinary urology clinic with BPH Treatment will have the capability to carry out a biopsy to see if the swelling is benign or if it is deadly. A test that is made with this approach is called a Cervical Pap smear. A doctor can discriminate in between a benign improvement and a lethal development by performing this test.
A urology clinic with BPH Treatment require to likewise have a skilled urologist and a registered nurse on staff members. A qualified urologist is somebody who carries out health examinations and orders tests like a Pap smear and a digital rectal examination. A signed up nurse will keep an eye on of using clients medication orders.
When picking a urology clinic, it is required to pick the ideal treatment. Physician who supply treatments such as prostate cancer surgical treatment and BPH treatment are not continuously the absolute best option. Consumers need to get their info about possible choices from the local telephone directory or the web.
Golden State Urology
400 Plaza Dr. Ste 140B Folsom CA 95630
(916) 436-3488
[email protected]
https://www.goldenstateurology.com/folsom/
Mon. - Thurs.: 9AM–5PM ; Fri. - Sun.: 10AM–6PM

3 notes
·
View notes
Text
Endometriosis vedas
Endometriosis
Endometriosis is an issue wherein tissue like the tissue that frames the covering of your uterus becomes outside of your uterine cavity. The covering of your uterus is known as the endometrium.
Endometriosis happens when endometrial-like tissue becomes on your ovaries, gut, and tissues covering your pelvis. It's surprising for endometrial tissue to spread past your pelvic locale, yet it's certainly feasible. Endometrial tissue becoming outside of your uterus is known as an endometrial embed.
The hormonal changes of your feminine cycle influence the lost endometrial tissue, making the region become excited and agonizing. This implies the tissue will develop, thicken, and separate. Over the long haul, the tissue that has separated has no place to go and becomes caught in your pelvis.
This tissue caught in your pelvis can cause:
disturbance
scar arrangement
attachments, in which tissue tough situations your pelvic organs together
extreme torment during your periods
richness issues
Endometriosis is a typical gynecological condition, influencing up to 10 percent of ladies. You're in good company on the off chance that you have this issue.
Endometriosis indications
The indications of endometriosis differ. A few ladies experience gentle indications, yet others can have moderate to serious manifestations. The seriousness of your aggravation doesn't show the degree or phase of the condition. You might have a gentle type of the illness yet experience anguishing torment. It's likewise conceivable to have a serious shape and have next to no uneasiness.
Pelvic torment is the most widely recognized side effect of endometriosis. You may likewise have the accompanying side effects:
excruciating periods
torment in the lower midsection previously and during feminine cycle
cramps half a month around feminine cycle
substantial feminine draining or draining between periods
barrenness
torment following sex
inconvenience with solid discharges
lower back torment that might happen whenever during your feminine cycle
You may likewise have no side effects. It's significant that you get normal gynecological tests, which will permit your gynecologist to screen any changes. This is especially significant on the off chance that you have at least two side effects.
Endometriosis treatment
Justifiably, you need speedy alleviation from torment and different manifestations of endometriosis. This condition can upset your life in case it's left untreated. Endometriosis has no fix, however its side effects can be overseen.
Clinical and careful choices are accessible to assist with decreasing your manifestations and deal with any likely intricacies. Your primary care physician may initially attempt moderate medicines. They may then suggest a medical procedure if your condition doesn't improve.
Everybody responds contrastingly to these treatment alternatives. Your PCP will assist you with tracking down the one that turns out best for you.
It could be disappointing to seek finding and treatment alternatives right off the bat in the infection. On account of the ripeness issues, agony, and dread that there is no alleviation, this sickness can be hard to deal with intellectually. Consider discovering a care group or instructing yourself more on the condition. Treatment alternatives include:
Agony meds
You can attempt over-the-counter agony meds like ibuprofen, however these aren't viable in all cases.
Chemical treatment
Taking supplemental chemicals can now and again diminish torment and stop the movement of endometriosis. Chemical treatment assists your body with directing the month to month hormonal changes that advance the tissue development that happens when you have endometriosis.
Hormonal contraceptives
Hormonal contraceptives decline richness by forestalling the month to month development and development of endometrial tissue. Anti-conception medication pills, patches, and vaginal rings can decrease or even dispense with the aggravation in less serious endometriosis.
The medroxyprogesterone (Depo-Provera) infusion is likewise successful in halting feminine cycle. It stops the development of endometrial inserts. It calms torment and different manifestations. This may not be your best option, in any case, in light of the danger of diminished bone creation, weight acquire, and an expanded occurrence of melancholy sometimes.
Gonadotropin-delivering chemical (GnRH) agonists and enemies
Ladies take what are called gonadotropin-delivering chemical (GnRH) agonists and enemies to impede the creation of estrogen which animate the ovaries. Estrogen is the chemical that is essentially liable for the improvement of female sexual qualities. Obstructing the creation of estrogen forestalls monthly cycle and makes a counterfeit menopause.
GnRH treatment has incidental effects like vaginal dryness and hot glimmers. Taking little dosages of estrogen and progesterone simultaneously can assist with restricting or forestall these side effects.
Danazol
Danazol is one more prescription used to stop monthly cycle and lessen manifestations. While taking danazol, the sickness might keep on advancing. Danazol can have incidental effects, including skin inflammation and hirsutism. Hirsutism is unusual hair development all over and body.
Different medications are being concentrated on that might further develop manifestations and slow illness progress.
Traditionalist medical procedure
Traditionalist medical procedure is for ladies who need to get pregnant or experience extreme torment and for whom hormonal therapies aren't working. The objective of traditionalist medical procedure is to eliminate or annihilate endometrial developments without harming the regenerative organs.
Laparoscopy, a negligibly obtrusive medical procedure, is utilized to both envision and analyze, endometriosis. It is additionally used to eliminate the endometrial tissue. A specialist makes little cuts in the mid-region to precisely eliminate the developments or to consume or disintegrate them. Lasers are ordinarily utilized these days as an approach to obliterate this "awkward" tissue.
Final hotel medical procedure (hysterectomy)
Infrequently, your primary care physician might suggest an all out hysterectomy if all else fails if your condition doesn't improve with different medicines.
During an absolute hysterectomy, a specialist eliminates the uterus and cervix. They likewise eliminate the ovaries in light of the fact that these organs make estrogen, and estrogen causes the development of endometrial tissue. Furthermore, the specialist eliminates apparent embed sores.
A hysterectomy isn't typically viewed as a treatment or solution for endometriosis. You'll not be able to get pregnant after a hysterectomy. Hear a second point of view prior to consenting to a medical procedure in case you're contemplating beginning a family.
What causes endometriosis?
During an ordinary monthly cycle, your body sheds the coating of your uterus. This permits feminine blood to move from your uterus through the little opening in the cervix and out through your vagina.
The specific reason for endometriosis isn't known, and there are a few speculations with respect to the reason, albeit nobody hypothesis has been logically demonstrated.
Probably the most established hypothesis is that endometriosis happens because of an interaction called retrograde feminine cycle. This happens when feminine blood streams back through your fallopian tubes into your pelvic cavity as opposed to leaving your body through the vagina.
Another hypothesis is that chemicals change the cells outside the uterus into cells like those covering within the uterus, known as endometrial cells.
Others accept the condition might happen if little spaces of your midsection convert into endometrial tissue. This might happen in light of the fact that cells in your mid-region develop from undeveloped cells, which can change shape and carry on like endometrial cells. It's not known why this happens.
These dislodged endometrial cells might be on your pelvic dividers and the surfaces of your pelvic organs, like your bladder, ovaries, and rectum. They keep on developing, thicken, and drain throughout your period because of the chemicals of your cycle.
It's additionally workable for the feminine blood to spill into the pelvic cavity through a careful scar, for example, after a cesarean conveyance (likewise usually called a C-segment).
Another hypothesis is that the endometrial cells are shipped out of the uterus through the lymphatic framework. Still another hypothesis indicates it could be because of a broken resistant framework that isn't annihilating wayward endometrial cells.
Some accept endometriosis may begin in the fetal period with lost cell tissue that starts to react to the chemicals of adolescence. This is regularly called Mullerian hypothesis. The improvement of endometriosis may likewise be connected to hereditary qualities or even ecological poisons.
HEALTHLINE RESOURCE
Change: Health Equity
We put stock in wellbeing value — the equivalent chance for everybody to carry on with their best life. Volunteer your opportunity to change your local area and go along with us in making a better world — for everybody.
Endometriosis stages
Endometriosis has four phases or types. It very well may be any of the accompanying:
negligible
gentle
moderate
serious
Various elements decide the phase of the issue. These variables can incorporate the area, number, size, and profundity of endometrial inserts.
Stage 1: Minimal
In insignificant endometriosis, there are little sores or wounds and shallow endometrial inserts on your ovary. There may likewise be aggravation in or around your pelvic cavity.
Stage 2: Mild
Gentle endometriosis includes light sores and shallow inserts on an ovary and the pelvic covering.
Stage 3: Moderate
Moderate endometriosis includes profound inserts on your ovary and pelvic covering. There can likewise be more sores.
Stage 4: Severe
The most extreme phase of endometriosis includes profound inserts on your pelvic coating and ovaries. There may likewise be sores on your fallopian cylinders and insides.
Conclusion
The side effects of endometriosis can be like the manifestations of different conditions, like ovarian growths and pelvic fiery sickness. Treating your aggravation requires a precise conclusion.
Your primary care physician will perform at least one of the accompanying tests:
Definite history
Your primary care physician will take note of your manifestations and individual or family background of endometriosis. An overall wellbeing evaluation may likewise be performed to decide whether there are some other indications of a drawn out issue.
0 notes