#Then seronegative RA
Text
Personal update
Hey guys, I finally have some answers about what's wrong with me and why I'm in pain. Turns out I have fibromyalgia AND either seronegative RA, undifferentiated inflammatory arthritis, or possibly NR-AxSpa if my MRI comes back positive for damage.
Feels bad man.
Feels real bad. Wasn't expecting multiple diagnoses for some reason. But knowing I have both makes me feel kind of justified in my pain in a way, like even a doctor will admit I'm in serious pain every day. It's weird and feels wrong to be treated with respect and care, and to have an answer. I feel... Kinda sick tbh. I was already in a flare.
Update lol: it's actually all three. Seronegative RA, Fibro, and Inflammatory Spondyloarthritis. Go team! Fuck this meat prison
#Kinda wanna barf#kinda wanna cry#Kinda wanna die /j#I want to crawl into a hole and hide to be honest I'm not ready to be this sick and I know I'm sooooo early on I want to fucking BARF omfg#Literally sick to my stomach at the thought of any of those much less fibro plus another one.#Fibro is what I first expected#Then AS/AxSpa#Then seronegative RA#I fucking diagnosed myself dude#This is mad weird.
17 notes
·
View notes
Text
i amb. watching house. i dont believe this man has ever been to medical school
#did u know if RF is negative that means RA is Un Possible... rf is totally super sensitive AND super specific to RA. definitely. for sure#theres no such thing as other more specific blood tests. anti ccp? i dont know her.. inflammation markers? whatre those...#and definitely no such thing as seronegative. no sir. bad bones are ALWAYS found in ur blood. ur blood would NEVER lie about bad bones#did i watch this episode lst night. yes. am i still yelling about how im smarter than him every time i remember it. also yes#i love 2 feel superior
5 notes
·
View notes
Text
I was like why am I shivering violently when I am not cold and then remembered that I have consistently forgotten to eat and have not slept more than like 4 hours a night for the past week. anyways here’s a really cool infographic on autoimmune diseases
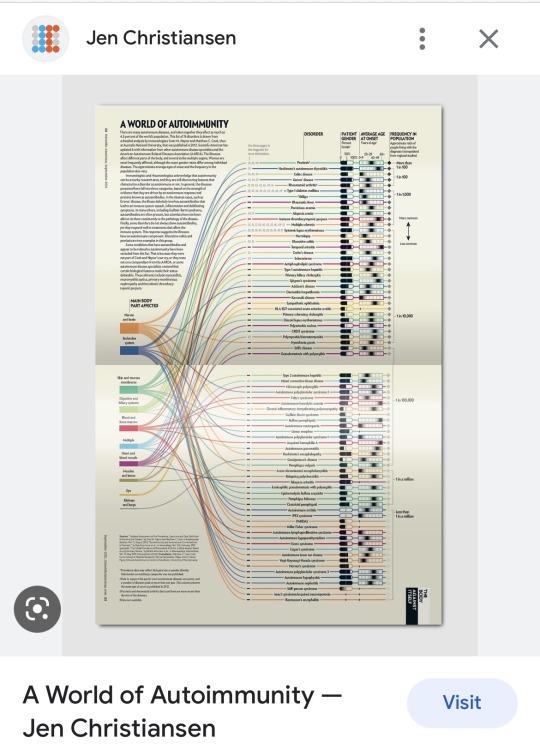
#not even kidding I want this on my wall#also ra under muscles and bones? i mean. i guess? do the joints count for that?#I’m pretty sure there’s more autoimmune diseases that target the joints than that?#ReA/psioriatic I guess. maybe you could count jRA as just RA but iirc they’re different enough to get separate names#unlike seronegative/seropostive RA.#also tbf I don’t think most autoimmune stuff counts ReA bc it’s temporary but who knows. who care. i dropped out of premed for a reason.#tired. will read the article this is from tomorrow.
2 notes
·
View notes
Text
Positive and Negative
I sometimes believe RA patients are divided into two camps. There are those with seropositive disease and there are those with seronegative disease. Those with seropositive disease are treated earlier in their disease. So early that initially hydroxychloroquine might be enough to calm their disease.
In order to be diagnosed with RA, seronegative patients must have more severe disease. Once they…
View On WordPress
#Blogging 101#medrol#Meloxicam#methotrexate#postaday#RA attitude#Rheumatoid arthritis#seronegative#seropositive#zerotohero
4 notes
·
View notes
Text
Well... Welcome me into "I'm in constant excruciating pain but my labs are normal" club :_)
#well not all of them - still waiting for one antibodies screening result#probably next week#but I doubt they'll find anything#literally EVERYTHING is fine with me BUT my anemia#which I already know I have#the irony of receiving clear results on the day I'm having one of the worst pains yet too...#aah.#gonna go to Kyiv and try to get an examination there and hopefully it's just still seronegative RA and not me being a medicam mystery
0 notes
Text
oh wait if ive. if ive had uncontrolled PCOS and HS this whole time........that explains the CRP levels a bit huh.... ..
#sick shit#same w an RA relapse which is fr happening#ram mom is seronegative so itd make sense i am too#(ram mom is bio mom and also only mom its just her title)#and we've established a while ago enthycitis type is. hard#anyway i should see an endo#my tsh was DUMMY low last time anyway#i feel better on a lower levo dose thooo
1 note
·
View note
Note
could you tell us about question 7 in the ask game? Also 1 if that's ok.
Hi! Yeah, of course! No problem at all =D
Question #7: What's a struggle you wish more people talked about?
Oh, there's honestly so much. I wish more people talked about the struggles and importance of accessible household items, I think. I don't think people talk enough about how accessibility is really important when considering buying certain things.
For instance, I struggle to open the handle at the house my family and I live in. We bought our new house a few years ago, and we couldn't change the handle. My parents have been intending to change it, but they haven't.
We are also currently looking to get a new vehicle, which means we have to check how accessible it is for me. How hard it is getting in, how much leg room I have, where the handles are, and how easy it is to handle/drive.
Accessibility is about more than ramps and wheelchair accessible vehicles. Even though I don't 'look disabled' (whatever that means), I still have to consider accessibility wherever I go and anytime I'm looking at something new.
It could simply be the difference between squeezing a tacky glue bottle vs. squeezing an Elmer's glue bottle, which is a struggle I have dealt with. Tacky glue bottles are CONSIDERABLY harder for me to use due to wrist strength than Elmer's glue is.
It's as simple as needing someone else's help to put on a fitted sheet, or having glass containers that are hard to open. I don't 'look disabled', but I am. And because I deal with wrist pain and my disability affects my wrists, it leads to issues with wrist strength.
So while there are many struggles I'd like to hear about more, I think that is my choice.
Question #1: What disability/ies do you have? (and are they mental, physical, or both?)
I have one diagnosed disability. I believe I have some undiagnosed ones (autism, ADHD, anxiety, depression, c-PTSD and/or PTSD, either celiac or non-celiac gluten sensitivity, and hyperthyroidism).
But for the sake of accuracy, I am only going to explain my diagnosed disability =)
I don't think I have gone into full on detail of what my disability is, even on my main blog. I honestly can't remember.
I have an autoimmune disease called RF (rheumatoid factor) negative polyarticular juvenile idiopathic arthritis. Because I am 20, this would (I think) be referred to as juvenile-onset arthritis, but again, for the sake of accuracy, I am going to give the diagnosis I have on my medical record. By 'juvenile' it means that it is diagnosed/occurs when someone is 16-17 or younger.
Polyarticular means 5 or more. This means that at least five joints in my body are affected by my arthritis. In my case, I have arthritis in every single joint in my body.
It affects my neck, jaw, spine, collarbones, ribs, shoulders, elbows, wrists, fingers, hips, knees, ankles, toes, etc. All of it. Pretty much my entire skeleton is affected. I mostly tend to have problems with my knees, jaw, and wrists. But they are all affected. Because of my disability, I do deal with chronic pain. I struggle when walking sometimes, though I often push myself due to familial expectations, and the fact that I don't like 'complaining'. I also can't stand for long periods of time because of my disability.
My disability is physical. It is mobility related. My disability is categorized as a physical disability, an autoimmune disease, a chronic illness, a musculoskeletal condition, a connective tissue disorder, and a mobility impairment, which is honestly a mouthful XD
I think my arthritis has affected other parts of my body that don't inherently have to do with my joints (potential livedo reticularis on my legs, watery eyes, etc.), though because those aren't confirmed, I just went with what the condition is said to cause (the other issues might be caused by RA, which I am technically not diagnosed with [though I feel like I might have seronegative RA, which would just end up being the more adult type of the JIA I have])
Thank you for the questions!
#physical disability#cripple punk#cripplepunk#crip punk#cpunk#physically disabled#physical disabilities#juvenile idiopathic arthritis#juvenile arthritis#arthritis#auto immune disease#autoimmune#invisible disability#disabilities#ask game#chronically ill#chronic illness#chronic pain
9 notes
·
View notes
Note
do you have any resources for figuring out the source of chronic joint pain? ive done some searching myself but its hard to find anything that isnt just talking about rheumatoid arthritis
unfortunately i don’t have like one source i can direct you towards but hopefully some of this is a helpful starting point!
afaik the most common causes of joint pain are rheumatological (rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, lupus/SLE, Sjögren’s, fibromyalgia), secondary to inflammatory bowel disease (Crohn’s or ulcerative colitis), Lyme disease, or due to hypermobility such as EDS. this list (link) from the Mayo Clinic includes rarer causes
my general diagnosis research advice, in no particular order, is:
if you developed symptoms before 18, refer to both adult and juvenile information
look at actual diagnostic criteria, not just summaries. often symptoms are weighted differently according to frequency
focus on any distinctive (common) differences between conditions because often there’s a lot of overlap
if a condition seems to overlap with some aspects of your experience but not others, look into those specific differences - information may be outdated or oversimplified. for example, recent studies show AS is equally common regardless of gender but articles will still say it’s more common in men, people can have seronegative RA (negative blood test for rheumatoid factor), etc
read sites geared towards doctors, such as continuing education sites, for more detailed and accurate information
search PubMed and skim for any recent breakthroughs in diagnosing/classifying a certain condition
search tumblr and other social media platforms to get an idea of what symptoms people who have a certain condition/diagnosis actually experience
keep in mind that if you’ve narrowed options down to something treated by the same medications (for example: RA, AS, psoriatic arthritis, and IBD can all be treated by Humira), then which particular diagnosis you receive isn’t that important
i highly recommend checking out DermNet New Zealand (link) if you experience any dermatological symptoms (skin, nails, hair) - they have click/hovertext definitions of terms, very thorough lists of potential diagnoses for symptoms, acknowledgments that differences in prevalence could be due to bias, and usually include example images of what conditions look like on non-white skin
best of luck to you and i hope you get some answers soon 💕💕
27 notes
·
View notes
Note
wait do you have inflammatory arthritis? i might be in the early stages of ra or PsA, my doctor/rheumatologist are basically just getting imaging/inflammation markers every few months to check if i have preclinical or if it's something else.
Hi!!! Yes, actually, i do! I have either Psoriatic or Anykolosing Spondylitis! They're both classified as inflammatory arthritis, belonging to the category of 'seronegative spondylarthopothies', meaning they have no rheumatoid factor. My doctor knows i have one of those specifically, the symptoms just overlap so much that it's hard to differentiate without radiologic proof, which i don't have (yet).
On one hand, I don't want to say 'I hope you have RA or PsA' because no one wants this kind of pain. But I do hope you get answers. Not knowing what you have makes it even worse.
#ask.txt#Anonymous#if you'd like to come off anon and talk about treatments/doctors visits/clinical shit my dms are open!!!
5 notes
·
View notes
Text
Type 17-specific immune pathways are active in early spondyloarthritis
CONCLUSION: These results suggest that adaptive T cell cytokine pathways differ not only between RA and SpA but also seronegative UIA early in the disease process, with a particular activation of Tc17 pathways in early SpA. http://dlvr.it/T0QQvH
0 notes
Text
Rheumatoid Arthritis: Types, Causes, Symptoms and Treatment

Rheumatoid Arthritis, or RA, is an autoimmune disease that develops when the immune system attacks its own body's tissues. Rheumatoid Arthritis can harm the skin, eyes, lungs, heart, and blood vessels in some people. It also damages the lining of the joints, which causes painful swelling. This may lead to bone erosion and joint deformity. However, RA is different from osteoarthritis because osteoarthritis causes damage from wear and strain, whereas Rheumatoid Arthritis causes inflammation that harms other bodily parts as well.
Despite the tremendous improvements in treatment options, severe Rheumatoid Arthritis can still result in physical complications.
What are the types of Rheumatoid Arthritis?
There are three main types of Rheumatoid Arthritis.
Seropositive RA - A person suffering from seropositive RA has a positive rheumatoid factor or anti-CCP blood test result. These are antibodies that trick the immune system into attacking the body's cells and tissues. This is considered severe and causes joint damage, deformity, development of vasculitis, lung issues, and rheumatoid nodules.
Seronegative RA: If a person experiences the symptoms of Rheumatoid Arthritis even after testing negative for anti-CCP and RF, they might have seronegative RA. Around 20-30 per cent of patients may still have RA, even when the test for RA is negative. The body produces antibodies that could still result in symptoms of RA but are not yet routinely measured in the laboratory. However, this type of RA is less severe, and its symptoms usually include joint swelling, morning stiffness, and pain.
JIA (Juvenile Idiopathic Arthritis) - RA in kids aged 17 and under is referred to as juvenile idiopathic arthritis. Similar to other types of RA, these symptoms may include inflammation, stiffness, fever, rash, and swollen lymph nodes.
What Causes Rheumatoid Arthritis?
The immune system defends the body against illness and infection and fights off foreign bodies. However, when the immune system acts abnormally, it targets healthy joint tissues, causing Rheumatoid Arthritis. Additionally, it may also lead to health issues with your nerves, eyes, skin, heart, and lungs.
However, doctors are not yet sure about the exact origin of the condition. Although it is considered a hereditary disease, genes don't directly cause Rheumatoid Arthritis. Instead, they can increase susceptibility to environmental conditions. Sometimes, viruses and bacteria are also responsible for causing RA.
What are the Symptoms of Rheumatoid Arthritis?
Rheumatoid Arthritis affects everyone differently. Some may experience the condition for a very long period, while others start experiencing the symptoms early. Additionally, some people experience flares and remissions with little to no symptoms. Signs and symptoms of Rheumatoid Arthritis include:
Pain, stiffness, edema, and soreness in joints
Stiffness in the joints after sitting or lying down for a long time.
Stiff and painful joints on both sides of the body.
Extreme exhaustion or fatigue.
Weakness.
Fever.
The symptoms of RA might range from mild to severe. No matter how intermittent your symptoms are, it's crucial to pay attention to them and seek medical attention. Early Rheumatoid Arthritis affects the smaller joints, such as finger joints and toes. Healthcare providers will be able to treat and manage Rheumatoid Arthritis if the symptoms are understood initially.
How is Rheumatoid Arthritis Diagnosed at Hinduja Hospital?
Our doctors at Hinduja Hospital first perform a physical examination to check the severity and area of the pain. To confirm RA, the doctor might prescribe the following tests:
Blood Test - Rheumatoid Arthritis patients often exhibit high levels of C-reactive protein (CRP) or Erythrocyte Sedimentation Rate (ESR), which indicates the presence of inflammation. Rheumatoid factor and anti-cyclic citrullinated peptide (anti-CCP) antibodies are the tests mostly prescribed by the doctors.
Imaging Exams - To monitor the development of Rheumatoid Arthritis in the joints over time, our top doctors in Mumbai advise getting X-rays. Depending on the result, the doctor will assess the degree of the disease in the body. In addition, the doctors might also ask to do a CT scan, MRI, and ultrasound.
How is Rheumatoid Arthritis Treated at Hinduja Hospital?
The goal of treating Rheumatoid Arthritis is to reduce swelling and pain. Although there is no known cure for RA, certain medications can help patients manage the disease and avoid damage if treatment starts at an early stage.
Usually, the treatment for Rheumatoid Arthritis includes therapies, medicines, surgery, and lifestyle changes. The doctors consider the patient's age, medical history, current health, and the severity of the symptoms before suggesting treatment plans. The following are the treatment options for Rheumatoid Arthritis suggested by the doctors at Hinduja Hospitals:
Medication
NSAIDs - NSAIDs, or nonsteroidal anti-inflammatory medicines, can reduce inflammation and relieve pain. However, heart and kidney conditions are some of the side effects of the medication.
Standard DMARDs - These medications can stop the evolution of Rheumatoid Arthritis and prevent irreparable damage to the joints and other tissues. Standard DMARDs might have some serious side effects, such as lung infections and liver damage.
Biologicals - These are newer and more effective medications that are better at controlling RA symptoms, but they are only used in cases where standard treatment doesn't work.
Steroids - Corticosteroid drugs lessen pain and inflammation while also slowing joint deterioration. Diabetes, bone weakening, and weight gain are some of the possible side effects. Corticosteroids are frequently prescribed by doctors to quickly alleviate symptoms with the intention of progressively weaning down the drug.
Therapy
The doctor might suggest that the patient visits a physical or occupational therapist who can help them with stretches and exercises to keep their joints flexible. The therapist might recommend some new and regular stretching techniques that the patient can do at home. They might also prescribe some assisted devices to avoid stress on the joints and reduce soreness. For example, a kitchen knife with a hand grip helps safeguard the wrist and finger joints, or buttonhooks can make getting dressed simpler. There are many tools that one can find in medical stores.
Surgery
If Rheumatoid Arthritis cannot be managed with therapy and medications, the doctor may discuss having surgery to restore damaged joints. This is because it can help restore movement and the ability to use the joints. The doctor might use the following surgical methods for treating Rheumatoid Arthritis:
Synovectomy - Synovectomy is done to remove the inflamed joint lining, also known as synovium. This helps reduce the pain and inflammation, resulting in improved joint movement.
Joint Fusion - Surgically fusing a joint may be advised to stabilise or realign a joint as well as to relieve discomfort.
Joint Replacement - The surgeon will remove the damaged joint components during the procedure and replace them with a metal and plastic prosthesis.
Tendon Repair - Tendons surrounding the joint may rupture or become loose due to joint injury and inflammation. These damaged tendons are surgically repaired around the joint to improve movement of the joints.
Like any other surgeries, Rheumatoid Arthritis surgeries also carry risks of bleeding, infection, and pain. Thus, it is advisable to discuss the complications and risks that might arise after the surgery. Also, a patient must also discuss any health conditions such as diabetes, blood pressure, etc., as these might also contribute to higher risks of complications.
How can Rheumatoid Arthritis be Prevented?
Rheumatoid Arthritis is a chronic condition that might make a person feel like they have little control over their life. However, there are things one can do to improve their well-being. Below are some preventive measures for Rheumatoid Arthritis:
Rest
When the joints are inflamed, the risk of injury to the joints and adjacent soft tissue structures (such as tendons and ligaments) is significant. It is advisable to rest sore joints. However, one should continue to exercise. This is crucial because managing RA requires keeping the joints functioning properly and maintaining good health.
Exercise
Stiffness and pain can make a person move more slowly, leading to inactivity in some individuals. However, lack of activity can cause muscular weakness and loss of joint motion. These factors reduce joint stability and increase pain and exhaustion. But with regular exercises, these complications can be avoided and reversed. A physical therapist might suggest the following exercises:
Exercises to build muscle.
Endurance-building exercises such as walking, swimming, and cycling.
Exercises that improve range of motion to protect and restore joint motion.
Diet
Doctors usually suggest the patient have foods with anti-inflammatory properties, as they reduce pain and inflammation. Moreover, it is advisable to eat food rich in antioxidants, such as green tea, fresh fruits, vegetables, and nuts. Also, having fibre-rich foods, such as whole grains, nuts, beans, fruits, and vegetables, can be a great option.
People with Rheumatoid Arthritis could feel that their level of pain and weariness is constantly fluctuating. It's crucial that they let their healthcare professional know about these symptoms. Diagnosis of Rheumatoid Arthritis, like X-rays and blood test reports, will help the doctors chart out a treatment plan. Most people are able to control their Rheumatoid Arthritis and continue with their favourite activities. Usually, the condition is treated with medication and therapy. However, if neither of them works, the doctor might suggest surgery.
For a comprehensive and best Rheumatoid Arthritis treatment in Mumbai, visit Hinduja Hospital. Our doctors are specialised and trained to help people with Rheumatoid Arthritis.
1 note
·
View note
Text
Got some goodbad news today
Good news: I don't have visible damage on my SI joint, which means I don't have Axial Spondyloarthritis like my dad, at least not yet.
Bad news: this means I probably have seronegative RA.
#Looking at the revised 2010(?) criteria for diagnosing RA I definitely meet the minimum#So yeah that's great
10 notes
·
View notes
Text
In silico analysis of serum #miRNA profiles in seronegative and seropositive rheumatoid arthritis patients by small #RNA sequencing
Rheumatoid arthritis (RA) is a refractory autoimmune disease, affecting about 1% of the world's population. RA is divided into seronegative RA and seropositive RA. However, biomarkers for discriminating between seronegative and seropositive RA have not been reported. In this study, we profiled serum #miRNAs in seronegative RA patients (N-RA), seropositive RA patients (P-RA) and healthy controls (HC) by small #RNA sequencing. Results indicated that compared with HC group, there were one... https://pubmed.ncbi.nlm.nih.gov/37525657/?utm_source=dlvr.it&utm_medium=tumblr&utm_campaign=None&utm_content=1Zap-74u4XbiV7x0qz5lToBuxtoq00qwwHZUuXSRQOsim8UYds&fc=None&ff=20230816100626&v=2.17.9.post6%2086293ac
0 notes
Text
Medical blah blah update under the cut
Its been a fight to try to talk to the one and only rheumatology office that takes my insurance anywhere nearby. A friend at the ER I work at told me they are familiar with that office, and that they are awful to try to deal with, and that I am better off going to Houston.
*sigh* So I bit the bullet and today I asked the GP to send referrals to Houston instead. Hopefully I actually hear from someone soon-ish.
I may need to plan out a Greyhound bus situation to get there since it is not safe for me to drive that far on my own. (Not even just the panic attacks anymore, but especially with my joints and tendons wigging out every single day now. Its one thing being stuck in a passenger seat that long. That's uncomfortable, but not dangerous.)
I also finally got to ask her about the results of my rheumatoid panel.
She says it looks like its not RA.
RF and CCP tests were negative.
But the ANA test was positive. (1:80)
So I definitely have SOMETHING. Lupus was high on her list of posibilities.
She didn't seem to know what Seronegative RA was, or that Psoriatic Arthritis can start before obvious signs of skin psoriasis. So I feel like there's still a slight "GP shrug" at the end of all that, and will not 100% rule out those things until a specialist says to.
Fingers crossed that a rheumatologist contacts me soon, and that they can help find a proper diagnosis without going through another year and a half of rapidly spreading and intensifying pain without a sign of them giving a shit.
#medical stuff#if it does take a while#let it at least be a while in which there is progress#and I don't feel like I'm being ignored#or given the runaround
1 note
·
View note
Text
Chronic illness is a bitch.
I don't know what I'm supposed to get out of this. I tell my clients often to journal, but I don't really think about doing it myself. But now may be as good of a time as ever. Does Journaling help when you're feeling alone with people all around you?
I know I'm not alone. I have so many wonderful people in my life, ones who are there for me every day. Then why do I feel so alone sometimes? Why do I just want to sit here and cry? I tell myself over and over that doing so would just be a waste, that I'm just spinning the pity party hamster wheel. Again my own words echo my hypocrisy, telling my clients that emotions need to be felt and that they are valid. It's easy to tell someone else supportive things- but why does it feel so horrible to do it for myself?
I stay up every night, refusing to go to bed, to start another day. Another day means more potential pain, more rot, more decay. I just want to hold on to what I have now. Is that too much to ask?
I just sound like a teenager with raging hormones and a menagerie of angst in all its forms. My body is anything but though, as I lay here and settle with the pain. Maybe the Tylenol PM will kick in soon. What I wouldn't give for a normal night's sleep, something that will never happen unless it is medically induced.
I don't know if anyone is going to read this, honestly if I came across it I would feel hard pressed to read it. Do I want to spend my time reading about someone else's whining? Their petty attempt to garner sympathy? I've had those thoughts about others' writing. And if you say you haven't about this stuff then you're a fuckin liar. We all do it, it's human nature. We categorize and organize and strategize, clawing for supremecy over others. I'm above you, so you are therefore lesser. I am acutely familiar with living that life- to be disabled is to be lesser.
I've felt those eyes on me, judging. The faces saying, why are you here? You're too young to be like this- they're probably faking it- either that or they're real fucked up- I bet it's just for show-
Do you know what it's like to already feel ashamed for having to use a motorized cart at the grocery store and then have a stranger reach over you for an item on the shelf as if you aren't there? Without an excuse me or pardon me? And don't worry, the government reached their hand over me already and said I'm not disabled enough, so no "handouts" for me.
Do you know what it's like to have to have shoulder reconstruction surgery at 14? To fall ill from an autoimmune inflammatory disease starting at 16-17? To have a complete hysterectomy at 24? To be diagnosed with seronegative RA and fibromyalgia along with your Ehlers Danlos Syndrome at 28? To get glaucoma at 30? How about losing your hair because of the vital and necessary meds you have to take? Almost passing out from your body purging without any control at 31?
So here it is. This is supposed to be something that makes me feel better, feel more connected, or at least...fuck I don't even know. I don't expect anyone to listen, but at least its here and not in my head. That's a rant for another day entirely.
1 note
·
View note
Text
Initial Treatment for RA
Initial Treatment for RA
Whether an individual is seropositive or seronegative rheumatoid arthritis will determine how soon she is diagnosed and what her initial treatment will be.
If she is seropositive, she may be diagnosed early in her disease. With a positive RF and anti-CCP antibody test plus joint symptoms a patient may be started on Plaquenil, hydroxychloroquine, a drug originally used for malaria. It…

View On WordPress
#medical management#methotrexate#postaday#RA progression#Rheumatoid arthritis#rheumatoid arthritis treatment#zerotohero
1 note
·
View note