#cardiopulmonary bypass
Text
Acute Pulmonary Edema Following Cardiopulmonary Bypass: A Case Report | Abstract
View On WordPress
0 notes
Text
Medical Equipment Manufacturer and Supplier in India

In the field of healthcare, the quality and reliability of medical equipment play a vital role in delivering effective and efficient patient care. Mercury Healthcare, a leading Medical Equipment Manufacturer and supplier in India, has emerged as a trusted name in the industry. With its commitment to excellence, innovation, and customer satisfaction, Mercury Healthcare has been revolutionizing the healthcare landscape in India. In this blog post, we will explore why Mercury Healthcare is renowned for providing the finest quality medical equipment in the country.
Commitment to Quality: Mercury Healthcare is dedicated to producing medical equipment of the highest quality standards. The company adheres to stringent quality control processes at every stage of manufacturing, ensuring that all products meet international quality benchmarks. By using advanced technology and robust manufacturing practices, Mercury Healthcare ensures that its equipment is reliable, accurate, and durable.
Wide Range of Products: One of the key strengths of Mercury Healthcare is its extensive portfolio of medical equipment. The company offers a comprehensive range of products, including diagnostic equipment, surgical instruments, patient monitoring systems, imaging devices, and much more. Whether it’s a small clinic, a large hospital, or a research facility, Mercury Healthcare caters to the diverse needs of the healthcare industry.
Cutting-Edge Technology: Mercury Healthcare stays at the forefront of technological advancements in the medical field. The company invests in research and development to continuously improve its products and introduce innovative solutions. By integrating the latest technology into their equipment, Mercury Healthcare ensures accurate diagnoses, efficient treatments, and improved patient outcomes.
Customization and Personalization: Understanding that different healthcare facilities have unique requirements, Mercury Healthcare offers customization and personalization options. The company collaborates closely with its clients to understand their specific needs and tailor the equipment accordingly. This approach not only enhances the user experience but also optimizes workflow efficiency in healthcare settings
Compliance with Standards: Mercury Healthcare strictly adheres to national and international regulations and standards for medical equipment manufacturing. The company follows Good Manufacturing Practices (GMP) guidelines and holds certifications such as ISO 13485:2016, ensuring that their products meet the highest quality and safety standards. This commitment to compliance instills confidence in customers, making Mercury Healthcare a trusted partner in the healthcare industry.
After-Sales Support and Service: Apart from manufacturing top-quality medical equipment, Mercury Healthcare places great emphasis on Hyper-Hypothermia Machine after-sales support and service. The company provides comprehensive technical assistance, training programs, and regular maintenance services to ensure the smooth functioning of the equipment. Their prompt and efficient customer service team is always ready to address any queries or concerns.
Conclusion: Mercury Healthcare stands out as a premier medical equipment manufacturer and supplier in India due to its unwavering commitment to quality, innovation, and customer satisfaction. With a wide range of products, cutting-edge technology, customization options, and adherence to stringent standards, Mercury Healthcare has earned the trust of healthcare professionals across the country. By choosing Mercury Healthcare, healthcare facilities can be assured of acquiring the finest quality medical equipment that contributes to delivering superior patient care.
#CABG#Cardiac Surgery Machine#Cardiopulmonary Bypass#ecmo heater cooler#Fast Cooling#Fast Cooling machine#Heat exchanger#Heater Cooler Machine#heater cooler unit#Hyper-Hypothermia#Hyper-Hypothermia Machine#Hyper-Hypothermia Machine Manufacture#Hyper-Hypothermia Machine Manufacture in India#Hyper-Hypothermia Machine Supplier#Hyper-Hypothermia Machine Supplier in india#hyperthermia machine#hypo hyperthermia machine#hypothermia equipment#Hypothermia Machine#hypothermia machine uses#hypothermia unit#Liver Transplant Machine#medical equipment manufacturer#Perfusion Machine#Perfusion system
1 note
·
View note
Text
A mysterious intra-cardiac needle discovered accidentally during pericardiothentesis under fluoroscopy by Hesham Alkady in Journal of Clinical and Medical Images, Case Reports
Abstract
Due to the rarity of retained intra-cardiac sewing needles, no clear guidelines exist regarding the indication for their extraction. In this study we report a case of a sewing needle extracted from the right atrium of an adult female presenting with recurrent pericardial effusion after one year of accidental penetration.
Keywords: Intra-cardiac needles; pericardiothentesis; echocardiography; cardiopulmonary bypass; sternotomy.
Introduction
Intra-cardiac sewing needles detected in adults and children may be due to accidental penetration e.g. while sleeping, self-inflicted as a result of mental and psychic disorders or domestic abuse [1, 2]. Due to the rarity of retained intra-cardiac sewing needles, no clear guidelines exist regarding the indication for their extraction. Conservative or operative options should be individualized according to the timing of presentation (acute or delayed), presence of symptoms (e.g. chest pain, infection, arrhythmia) as well as location [3]. In this study we report a case of a sewing needle extracted from the right atrium of an adult female after one year of accidental penetration
Case report
A 60 year old female patient was referred to our outpatient clinic due to a needle found by the cardiologist during pericardiothentesis under fluoroscopy for increasing pericardial effusion. (Video)
The clinical history, physical examination as well as laboratory studies of the patient were unremarkable apart from recent progressive shortness of breath since 2 months. Therefore the cardiologist decided to do a pericardial aspiration with chemical, bacteriological and cytological examination of the pericardial fluid after increase its amount despite of diuretic therapy. The pericardial aspirate was sero-sanguinous exudative in nature, negative for organisms and malignant cells. The patient had no explanation how a needle reached this place and she did not receive any major procedure before could be the cause. The patient is also well-educated and her mental as well as psychological assessments were within normal. A transthoracic echocardiography showed an echogenic linear object at the wall of right atrium, unclear whether inside or outside the atrial cavity, as well as mild pericardial effusion with thickening of the pericardium. Multi-slice CT chest showed that the needle lies inside the right atrial cavity embedded in its wall (Figure 1).

Figure 1: A Multi-slice CT of the chest showing the needle in the right atrial cavity as well as collected pericardial effusion on its lateral surface. The pericardium appears slightly thickened.
The possible hazards of leaving the needle in the heart were explained to the patient as well as the advantage of biopsying the pericardium during surgical extraction to determine the cause of recurrent effusion. The patient was first terrified from the surgical intervention; however she consented surgery at the end. Through full median sternotomy, the thickened pericardium was opened and sero-sanguinous effusion was evacuated. Some adhesions were found on the anterior surface of the heart especially right atrium. Trials to locate the needle by digital palpitation of the right atrium were unsuccessful. A mobile C-arm X-ray machine was brought to the operation room to confirm the position of the needle inside the right atrial cavity. Cardiopulmonary was then initiated via aorto-bicaval cannulation. After snaring of both cavae, the right atrium was opened transversely along the atrio-ventricular groove and astonishingly a rusty sewing needle was found embedded with its sharp end in the roof of the right atrium near the tricuspid valve (Figure 2).

Figure 2: The rusty sewing needle found in the cavity of the right atrium embedded in its wall.
Upon seeing the sewing needle, the patient remembered that she brought that type of needles one year ago and lost one of them shortly after. So the only available explanation postulated is that the needle went unnoticed into the patient´s chest may be while sleeping nearby the needle or leaving it inside her pocket which then eroded its way through the pericardium onto the right atrium being an anterior structure immediately behind the chest wall. The postoperative recovery went uneventfully and the patient was discharged home safely after one weak. Pathological examination of the thickened pericardium revealed nonspecific chronic inflammation with no signs of malignancy.
Discussion
Upon reviewing the literature, there is a general tendency to remove intra-cardiac needles once diagnosed to avoid potential hazards or prevent further damage [4]. These hazards include embolization, thrombus formation, endocarditis, pericarditis and injury to cardiac structures including cardiac perforation and pericardial tamponade [5]. Hazards are more prone when the needles are located in left-sided chambers and when partially embedded in myocardium [6].
Localization modalities of intra-cardiac needles include echocardiography and more accurately computed tomography. Intra-operative C-Xray is much helpful and time sparing. Interventional extraction using modern radiological facilities would be difficult and may be hazardous. Median sternotomy is much superior than any other approaches e.g. thoracotomies as it allows the best exposure and safest access to cardiopulmonary bypass. Sometimes the needle can be removed without the help of the heart machine and sometimes not [7, 8]. In our study, although the needle penetrated accidentally into the chest wall and then right atrium, yet it did cause some sort of chronic pericarditis and recurrent effusion one year later. This represented, beside the sharp nature of the non-sterile sewing needle, the indications to remove the needle.
Conclusions
Since the fact that no clear guidelines exist regarding the indication for extraction of intra-cardiac needles, therefore management whether conservative or operative should be individualized according to each case. Surgical removal of lately-discovered intra-cardiac needles should be considered if complications occurred like pericarditis causing recurrent pericardial effusion in our case.
Compliance with ethical standards
Conflict of interest: The authors have declared that no conflict of interest exists.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Intra-cardiac needles#pericardiothentesis#echocardiography#cardiopulmonary bypass#sternotomy#fluoroscopy#cardiologist#sero-sanguinous#Hesham Alkady#JCMICR
0 notes
Text
Successful Jatene procedure for great arteries transposition correction in newborn with SARSCoV-2 infection by Guillermo Careaga-Reyna MD in Journal of Clinical Case Reports Medical Images and Health Sciences
ABSTRACT
Pandemic of COVID-19 represents a challenge for treatment of patients with congenital herat disease. We present a newborn with great vessels transposition and positive SARS-CoV-2 PCR test. The patient was submitted to a successful surgical treatment with corrective Jatene procedure, requiring opened chest wall during 72 h of postoperative period and 43 days of total in-hospital lenght of stay.
KEY-WORDS: COVID-19, SARS-CoV-2, great vessel transposition, Jatene procedure, congenital heart disease.
INTRODUCTION
Coronaviruses are single stranded ribonucleic acid viruses with a diameter of 60–140 nm and a high rate of genetic mutations and recombinations, rendering them capable of escaping from the immune system and causing novel infections (1). In less than six months, the coronavirus disease 2019 (COVID-19) pandemic has swiftly spread from one city in China to over 190 countries worldwide (2-4). Neonatal infections with SARS-CoV-2 have been described although robust data on vertical transmission are lacking. In most instances where neonatal infection has been reported, close contact with infected mother or caregiver is postulated to have occurred (4).
In newborns, the case is regarded as positive for infection if any of the following conditions occurs, (1): positive PCR for SARS-CoV-2 in respiratory tract or blood samples, high homology of viral gene sequences of the samples from the respiratory tract or blood to the COVID-19 sequence.
We present a case of a newborn with great vessel transposition and SARS-CoV-2 infection.
CASE REPORT
We present a new born with great arteries transposition associated to aquired SARS-COV-2 infection.
The patient was refrerred to our hospital, with a positive SARS-CoV-2 test, with mechanical ventilatory support in order to confirm a complex congenital heart disease.
The diagnosis was established via echocardiographic evaluation which showed normal venous return, concordance atrio-ventricular and ventriculo-arterial discordance. It was concluded: great arteries transposition, patent ductus arteriosus and permeability of foramen oval.
The patient was recovered from a septic shock with no evidence of systemic inflammatory response requires inotropic support and after stabilization in neonatal intensive care unit, at 10 day in-hospital stay, was submitted to an open heart surgery consisted in anatomic correction with Jatene procedure. The aortic cross-clamping time was 119 min, with cardiopulmonary bypass (CPB) of 181 min. It was decided to maintain in postoperative period opened chest wall, and after 72 the chest wall closure was succesfully realized with favorable posoperative evolution. After 32 days of postoperative, the patient was discharged from hospital. Actually, two years after surgery, the patient is doing well, only with mild pulmonary stenosis without hemodinamic or clinical repercusion.
DISCUSSION
For infants born to COVID positive mothers should be reasonable to separate him from the mother if will need cardiac surgery to try avoid post-natal infection.
In fact, there is minimal evidence of placental vertical transmisión. In this case, the patient has a positive test for SARS-CoV-2 infection and evolved with septic shock in the preoperative period.
It may also be reasonable to do serial testing on the infant, but there is no consensus on the correct timing surgery should be scheduled with advice from a multidisciplinary team of experts including cardiac medical, cardiac surgical, and infectious diseases as indicated. After evaluation of the clinical conditions for a heart team in our hospital, it was decided to realize the surgical procedure in order to avoid progression of heart damage and irreversible heart failure.
However we must remember that, if prudent, surgery should be delayed until the patient’s symptoms have improved and/or testing has been repeated (often after 14 days) and is negative (5).
On the other side, in older patients the inflammatory response due to SARS-CoV-2 infection has been a frequent complication.
In our patient, probably due to the age, it was no presented even with the septic shock o posteriorly associated to the use of CPB during the surgical procedure
It was concluded taht COVID-19 may affect all age patients. However with cautious evaluation and treatment of associated disease as in our case, the patient improves survival, despite severity of viral illness, and during this pandemic period, patients with active COVID-19, at neonatal period we have no treated any other.
FINANCIAL SUPPORT: None.
CONFLICTS OF INTEREST: The authors declares there is no conflict of interests.
For more information: https://jmedcasereportsimages.org/about-us/
For more submission : https://jmedcasereportsimages.org/
#SARS-CoV-2#great vessel transposition#Jatene procedure#congenital heart disease#PCR#COVID-19#hemodinamic#cardiopulmonary bypass#preoperative period#Guillermo Careaga-Reyna MD#jcrmhs
0 notes
Text
A novel video game for cardiopulmonary bypass training (video)

- By Nuadox Crew -
Virmedex, a health tech firm located in Barcelona, has released virCPB, a virtual training video game for perfusionists.
youtube
Video: “Welcome to virCPB, the videogame for Cardiopulmonary Bypass training!” by Virmedex, YouTube.
The game is intended to assist these healthcare professionals in developing their skills and knowledge in a secure and regulated virtual environment.
Perfusion is a key medical discipline utilized to preserve the patient's blood circulation and oxygenation during heart and lung procedures.
virCPB is a simple video game based on a realistic physiological model that replicates a range of clinical circumstances that perfusionists may face, offering fast and thorough feedback to assist perfusionists in improving their abilities and knowledge.
Virmedex expects that the game will be extensively used by perfusionists, hospitals, and colleges all around the world, and it has launched a funding round to grow its staff and develop additional products.
--
Header image: virCPB dashboard. Credit: Virmedex, Fair Use.
Source: Virmedex
Read Also
Carpal tunnel syndrome detection via gamification
#gaming#gamification#video games#video game#medtech#health tech#digital health#virmedex#vircpb#education#training#health#healthcare#perfusion#cardiopulmonary bypass#blood#medicine#spain
1 note
·
View note
Text
Abstract
Anesthetic management of surgical repair of descending thoracic aortic aneurysm is a difficult mission for anesthesiologists. The surgical approach is best achieved through left postero-lateral thoracotomy with the use of one lung ventilation. The post-operative outcome is affected by the presence of associated co morbidities such as cardiac and renal diseases, the severe intra-operative hemodynamic fluctuations and the use of mechanical circulatory assisted devices. The severe hemodynamic fluctuations that result from clamping and declamping the descending thoracic aorta require an experienced cardiac anesthesiologist for the proper perioperative management of these patients. The aim of this review is to give new insights on the anesthetic management and the techniques of distal perfusion using partial cardiopulmonary bypass. Anesthetic goals are directed to provide spinal cord and renal protection with controlling the proximal hypertension.
Read More about this Article... https://irispublishers.com/asoaj/fulltext/anesthetic-management-of-surgical-repair-of-descending.ID.000518.php
Read More Iris Publisher Google Scholar Articles..https://scholar.google.com/citations?view_op=view_citation&hl=en&user=6Gbr0YIAAAAJ&cstart=20&pagesize=80&citation_for_view=6Gbr0YIAAAAJ:tzM49s52ZIMC
0 notes
Text
The Rise of Tech-Driven Therapies: Reshaping the Global Cardiopulmonary Bypass Systems market
The global Cardiopulmonary Bypass Systems market. According to a recent analysis, the market is expected to grow at a Compound Annual Growth Rate (CAGR) of 3.2% over the forecast period, from US$ 197.3 million in 2023 to US$ 270.9 million in 2033.
The forecasted growth in the Cardiopulmonary Bypass Systems market reflects the increasing demand for these devices driven by the rising costs associated with treating major illnesses, including cardiac disorders. Despite challenges such as unfavorable side effects resulting from bypass surgeries, the market is expected to benefit from rapid technological advancements and the growing number of surgical procedures.
Navigate Future Trends With a Sample Report:
https://www.futuremarketinsights.com/reports/sample/rep-gb-5855
Supporting Heart Health: Cardiopulmonary Bypass Systems Play a Vital Role
The global cardiopulmonary bypass system market is experiencing continued growth, driven by the increasing need for effective tools in cardiac surgery. Cardiopulmonary bypass systems play a critical role in open-heart surgery by temporarily taking over the functions of the heart and lungs, allowing surgeons to operate on a still heart.
Market Growth Fueled by Multiple Factors:
Several factors are contributing to the growth of the cardiopulmonary bypass system market:
Increased Focus on Cardiac Care: Rising healthcare expenditure directed towards combating heart disease, a leading global health concern, is creating a greater demand for advanced cardiac surgical procedures.
Technological Advancements: The market is continuously evolving with the development of innovative bypass systems. Roller pumps, for example, are gaining traction due to their affordability, ease of use, and reliable flow management.
Expanding Surgical Needs: The growing number of lung transplant procedures, particularly en-bloc double-lung transplants, is driving the demand for cardiopulmonary bypass systems to support these complex surgeries.
Key Takeaways:
The global cardiopulmonary bypass system market is expected to reach US$270.9 million by 2033, reflecting a rise from US$197.3 million in 2023.
This growth is projected at a steady compound annual growth rate (CAGR) of 3.2% throughout the forecast period.
Rising healthcare spending on cardiac procedures and advancements in technology are key drivers for market expansion.
The Cardiopulmonary Bypass System Market:
Minnetronix Inc.
Transonic
MAQUET Holding B.V. & Co. KG.
Getinge AB
Terumo Corporation
MicroPort Scientific Corporation
Xenios AG
Nipro Corporation
Eurosets Srl
OriGen Biomedical
Thoratec Corporation
Tianjin Medical
Olympus Corporation
Haemonetics Corporation
Some Recent Developments in the Cardiopulmonary Bypass System Market are:
In June 2014, Sorin Group celebrated the delivery of its 10,000th heart-lung machine (S5 heart-lung machine) to Brigham and Women’s Hospital, Boston, MA, USA. Thuse achieved an exciting milestone that reflects the tremendous trust and collaborative partnership with their customers worldwide.
In October 2021, MicroPort acquired 100% of the equity held by existing shareholders of Hemovent GmbH. Hemovent specializes in the development of ground-breaking Extracorporeal Life Support (ECLS) systems.
In February 2022, Getinge acquired 100% of the equity interest in Talis Clinical LLC, a US-based leading innovator of High Acuity cloud-based software solutions. Talis Clinical’s offer is designed to support and document care throughout the general and cardiac perioperative care process, but also through labor and delivery episodes and critical care support, including ECMO Therapy.
In April 2022, LivaNova initiated the targeted commercial launch of Essenz™. Patient Monitor for cardiopulmonary bypass procedures. The transformative monitoring system uses a patient-tailored approach to improve clinical efficiency and quality of patient care during cardiopulmonary bypass (CPB) procedures.
In January 2021, Eurosets announced the full commercial release (out of the USA) of its novel ECMOlife system for Extracorporeal Life Support (ECLS). ECMOlife expands Eurosets’ portfolio to temporarily support patients in different therapeutic areas, including Extracorporeal Membrane Oxygenation (ECMO) and Mechanical Circulatory Support (MCS).
Key Segments Profiled in the Cardiopulmonary Bypass System Industry Survey Report:
By Product Type:
Conventional
Mini
By Modality:
Standalone
Portable
By End User:
Hospitals
Ambulatory Surgical Centers
Cardiac Research Centers
By Region:
North America
Latin America
Asia Pacific
The Middle East and Africa
Europe
0 notes
Text
Data Bridge Market Research analyses that the global cardiopulmonary bypass accessory equipment market, which was USD 15.93 billion in 2023, is expected to reach USD 25.01 billion by 2031, at a CAGR of 5.8% during the forecast period 2024 to 2031. In addition to the insights on market scenarios such as market value, growth rate, segmentation, geographical coverage, and major players, the market reports curated by the Data Bridge Market Research also include depth expert analysis, patient epidemiology, pipeline analysis, pricing analysis, and regulatory framework.
0 notes
Text
Extracorporeal Membrane Oxygenation Machine | Exploring Opportunities and Challenges
The global extracorporeal membrane oxygenation machine market size is anticipated to reach to reach USD 445.7 million by 2030, expanding at a CAGR of 5.5% from 2024 to 2030, based on a new report by Grand View Research, Inc. This growth can be attributed to the rising prevalence of cardiopulmonary and respiratory diseases, increasing adoption of ECMO machines in hospitals, and technological advancements in ECMO machines. The market expansion is also driven by the need for advanced life support technologies like ECMO machines, which are becoming increasingly necessary in treating patients with severe or life-threatening cardiac or pulmonary conditions.
Extracorporeal Membrane Oxygenation Machine Market Report Highlights
In 2023, the oxygenators segment accounted for the largest market share. This can be attributed due to prevalence of diseases like coronary heart disease and chronic obstructive pulmonary disease (COPD) continues to rise, the demand for advanced life support technologies like ECMO machines increases, driving the growth of the oxygenators segment.
The veno-arterial segment dominated the modality segment of ECMO machine market in 2023. This growth can be attributed due to high usage of veno-arterial ECMO in treating patients with cardiac arrest, where it assists with algorithm life support strategies to restore blood circulation. Additionally, the increasing incidence of chronic obstructive pulmonary disease (COPD) is also a key driver of this market segment.
The respiratory segment dominated the application segment in 2023 due to the high prevalence of respiratory diseases, such as Chronic Obstructive Pulmonary Disease (COPD) and acute respiratory distress syndrome (ARDS), which are leading causes of death worldwide, necessitate advanced life support technologies like ECMO machines.
The adult patient segment dominated the patient type segment in 2023 due to the prevalent incidence of heart and lung-related issues necessitating life-saving interventions.
The North American region held the largest share of the market in 2023 due to key industry players, consistent product launches, government backing for quality healthcare, advanced healthcare infrastructure, and favorable reimbursement policies.
Market players adopt several strategic initiatives to increase the product reach and improve availability in diverse geographic areas.
For More Details or Sample Copy please visit link @: Extracorporeal Membrane Oxygenation Machine Market Report
The rising prevalence of cardiovascular and respiratory diseases. Diseases such as coronary heart disease, cerebrovascular disease, rheumatic and congenital heart diseases, respiratory diseases like acute respiratory distress syndrome (ARDS), and chronic obstructive pulmonary diseases are leading causes of death worldwide. For instance, according to the World Heart Federation, approximately 18.6 million people die annually from cardiovascular diseases. Additionally, about 190,000 Americans are diagnosed with ARDS annually in the U.S. Such an increasing prevalence of cardiovascular and respiratory diseases has boosted the demand for ECMO machines, driving the market growth.
In addition, the increasing rate of technical improvement is increasing the usage of products. It is easier to transfer critically ill patients now as machine parts like hollow pumps and oxygenators are smaller. Moreover, introducing technologically advanced components, such as improved rotary pumps, dual-lumen cannulas, innovative oxygenators, and new cannulation approaches, is anticipated to ease the use of ECMO machines. For instance, in 2022, Inspira Technologies OXY B.H.N. Ltd. recently introduced the "Liby" System, an advanced life support system used to treat patients with life-threatening heart and lung failure. Similar advancements and the introduction of new products are expected to drive market growth in the coming years.
#extracorporeal membrane oxygenation#ECMO#life support technology#critical care#cardiopulmonary support#medical devices#intensive care#respiratory failure#heart-lung bypass#market analysis#healthcare technology#patient care#emergency medicine#global health#cardiac surgery#pulmonology#resuscitation#innovation#market trends#healthcare industry
0 notes
Text
China’s economy is currently on the operating table, hunched over by surgeons, chest cavity splayed open, hooked up to a cardiopulmonary machine, surrounded by nurses staring at monitors flashing vital signs. It all looks rather grim.
This surgery, however, is not an emergency bypass. That would be too easy. China has had many of those already – stimulus packages, grand infrastructure projects and many rounds of directed lending.
Every two decades or so, going all the way back to the founding of the PRC in 1949, the surgeons get ambitious. These guys are mad scientists attempting a comic book trope – to create the ultimate superhero.
They want to inject super serum, replace skeletal calcium with adamantium and dose the patient with gamma rays, giving China the powers of shazams out the wazoo.[...]
In the lamented “pre-reform” era, China’s mad scientists engineered spectacular growth by increasing investment from a prewar 6% of GDP to 20% in the first Five-Year Plan, covering 1952-1957. This led industrial output to register a compound annual growth rate.
The Great Leap Forward accelerated this growth to 66% in 1958 and 39% in 1959 before crashing and burning in 1961 when mismanagement of communal farms and “backyard blast furnaces” caught up with the mad scientists.
Course correction starting in 1962 recovered all lost ground by 1965. According to economist Cheng Chu-Yuan, China’s GDP growth averaged 11% between 1952 and 1966, the eve of the Cultural Revolution. (T. C. Liu of Cornell and K. C. Yeh of the Rand Corporation have a lower estimate: 8%.)
More importantly, China built a full kit of infrastructure, machinery and equipment capable of driving future industrialization.[...]
Many analysts have a tabula rasa understanding of China’s reform era, as if there had been no economy before Deng Xiaoping. In reality, China’s industrialization started right after the formation of the PRC with some of the fastest growth recorded in the 1950’s and 1960’s. Even during the “low growth” Cultural Revolution, resources directed towards public health (for example, barefoot doctors) and primary education doubled life expectancy and quadrupled adult literacy by 1980 from pre-PRC levels.
The mad scientists are now at it again. They have about twenty years of new data not just on China but from the rest of the world. When Zhu Rongji was head surgeon, history had ended and markets reigned supreme. This time around, the surgeons are correcting for market irrationality and negative externalities. The next twenty years is again being determined on the operating table.
Three years ago, the surgeons pried open China’s chest cavity with the three red lines credit limits, instantly seizing the speculation driven property sector. Since then, they ripped out unnecessary organs like education companies, clamped the Ant Financial artery and eviscerated the video game industry.
All of this has caused spasms in vital signs from lackluster growth to rising youth unemployment. Wondering whether China will or will not stimulate the economy next quarter or next year is missing the forest from the trees. For the next few years, China’s economy will still be under the knife and whatever adjustments will merely be anesthesiologists and technicians nominally dialing the drugs up and down and adjusting the heart-lung machine to maintain vital signs.
What are these mad scientists trying to achieve? We believe President Xi Jinping’s 2020 target of doubling China’s GDP by 2035 stands. That is an average growth rate of 4.7% for 15 years. But beyond just a numerical target, it is important to figure out what superpowers China is trying to acquire. And just as importantly, what Kryptonite factors China is attempting to inoculate itself against.
China wants America’s Silicon Valley, but regulated; Japan’s car companies, but electrified; Germany’s Mittelstand, but scalable; and Korea’s chaebol conglomerates, but without political capture. It wants to lead the world in science and technology, but without cram schools. A thriving economy, but with common prosperity. Industry, without air pollution. Digital lifestyle, without gaming addiction. Material plenty, without hedonism. Modernity, without its ills. This is, of course, a wish-list and unrealistically ambitious. But these mad scientists sure as hell are going to try. They’ve developed a taste for it.
In college, early into the semester, we went through a ritual called course exchange. Students gathered in an auditorium to swap classes after sampling lectures for three weeks – satisfaction was not guaranteed. The strategy passed down to underclassmen applied to both course exchange and significant others: “Add before you drop.”
China is undergoing – but perhaps botching – the same process with a more party-esque slogan, “Establish the new before abolishing the old.”
The surgeons have been on a tear gutting the old. The big kahuna is, of course, the property sector. But right behind are platform monopolies, private education, financial services and video games. The new has been playing catch-up, with 5G equipment, electric vehicles, photovoltaics and wind turbines being leading examples.
From all appearances, the Industrial Party is in ascendance and China will double down on climbing the manufacturing value chain. The Industrial Party is a political identity that believes industry, science and technology should determine China’s future. Adherents believe that China’s strength lie in the technical skills of her population and thus favor hard-science, high-tech industries as opposed to services and business model innovations.
Therefore, Chinese politicians, whatever their predisposition, must find a way to create space for this next generation of scientists and technicians to develop themselves. They cannot be confined to a production line at a Foxconn plant. Maintaining social stability means finding a use for future scientists and technicians, which means pursuing industrialization. Is there any other way? The key variable for determining the course of China’s future development is thus the massive number of talented technical and scientific workers.
If mistakes were made, it would have been in sequencing and in faith – dropping before adding is a poor strategy in both love and course exchange. China’s mad scientists may have been too confident that electric vehicles and renewable energy would be followed quickly by semiconductors, pharmaceuticals and commercial aircraft.
Perhaps they have reason to be confident. Planning for this surgery has been in the works since 2015 with the Made in China 2025 project. China has been steadily eroding imports of high value added intermediary goods like batteries, precision parts and electrical components, flipping trade with South Korea from deficit to surplus.[...]
China never properly transitioned from its Soviet era Material Product System (MPS) of national accounts to the United Nation’s System of National Accounts (UNSNA) standard, leaving out much of services from reported GDP.
We calculate that China accounts for 22-24% of global GDP and 20-23% of global consumption. We also calculate that household consumption is 50-55% of China’s GDP, in line with global averages. China should easily be able to grow at 4.7% through 2035 with only a modest increase in consumption’s GDP share (5 percentage points over 10 years) without upsetting global economic balances.
In the reform period prior to Xi, everything was sacrificed at the altar of economic growth. In the new era, growth has been walked down from 9.6% in 2011 to an average of 4.7% in the Covid years (2020-2023) as an increasing litany of issues were given precedence. Debt however, soared over this time from 175% of GDP to over 300%. What exactly did all that debt buy?
When Xi assumed leadership of China, he declared that inequality could not be allowed to increase further. Inequality is perhaps the major Kryptonite factor of the American economy which China wasted no time in matching as the economy roared with market reforms.
While still problematic, inequality, as measured by the Gini coefficient, has steadily fallen since 2010 largely as a result of massive investment in urbanization, pushing people into cities and pushing cities up the tiering ladder.[...]
China also poured resources into stamping out last-mile poverty. While most poverty alleviation in China was through economic growth, recalcitrant extremely poverty could only be eradicated by concentrated marshaling of resources, from relocating entire villages to weekly visits by social workers.[...]
Since peaking in 2012, air pollution in Beijing has been cut by over 60%, with Shanghai falling over 50%. China, which used to dominate the list of most polluted cities, now only claims one spot in the top 20. None of this came cheap, from installing scrubbers in smoke stacks to increasing renewables to moving heavy industry to strict emissions regulations for cars.[...]
Before Hu Jintao handed the reins to Xi, Hu warned delegates to the 18th Party Congress in 2012 that “[corruption] could prove fatal to the party… and [cause] the fall of the state.” The popular opinion in the West is that Xi ended China’s highly successful reform era because of an ideological bent. This is off the mark. Xi was brought in to clean house as the wheels were coming off from excesses of the reform era.
Throughout Xi’s decade in office, there has been no letup in his anti-corruption campaign. In 2022, a record 638,000 officials were punished for corruption. While there haven’t been any large scale ideological appeals to the public, it’s a different story within the 98-million-member party.
During this time, free market capitalism and liberal democracies also faced their own existential tests. Success or failure going forward will depend on whether liberal institutions remain intact in the West and whether party discipline can be maintained in China.
What the PRC has had since 1949 is a governing party with the political autonomy to play mad scientist. [...]
Of course we live in the real world, not a comic-book world. The question in the real world has always been whether the economy can be engineered by mad scientists from the top down or is it best left to the invisible hand of the market? [...]
The standard economic opinion – against all evidence – is that China was economically stagnant before Deng’s market reforms. The thinking on this for the American economys is undergoing a transformation in egghead land – just how has neoliberal economics benefitted the American people over the past few decades?
In a Q&A exchange at a conference in Malaysia, Eric Li, the barbed-tongued venture capitalist, was asked, “Do you think top-down directives are sustainable in the long run?”
To which he replied, “It’s the only thing that’s sustainable.… That’s why America is failing today.” After World War II, Li said, the Americans “lost the ability to do top-down design.”
Dec 2023
99 notes
·
View notes
Note
Do you think Bucky ever got any sleep during all his years of Hydra captivity? Or was it just wipe/kill/back in the freezer? I don't think cryostasis would be anything like normal restorative REM sleep.
Hello nonnie!! I have finally had a light-bulb moment for this ask (I'm sorry it's taken me like 7 months)
I've been going about it the wrong way, trying to research on sleep, when in actuality what I should have been researching is the brain under hypothermia. This is an observational study conducted in the 1980s looking at children undergoing induced hypothermia (lowering of body temperature) during cardiopulmonary bypass (sometimes required during major surgery). In summary, by the time the body temperature cooled to 18 degrees, all brain activity ceased. Sleep - consisting of non-REM and particularly REM - are associated with far more active brain waves. So nonnie, you are very correct in saying that Bucky, even with his super soldier abilities, unlikely ever got any "sleep" during cryostasis. (I'm sorry to all the ficcers that wrote Bucky dreaming during cryo but I think most people are happy to ignore this piece of science)
In terms of whether Bucky ever got "sleep", I think that is hard to say. Even normal soldiers might drive themselves to go without sleep for 36+ hours if required for a mission (heck, even hospital shifts go for 36 hours in some places). As a super soldier, Bucky might tolerate sleep deprivation for longer. This means missions like taking out the Starks - travelling from Russian and back - he might achieve in one sitting without sleeping in between (although I guess no one can stop him from dozing off on the plane).
I think one implied part of your question is "is it likely that Bucky was allowed out of the freezer for long enough periods at a time to need (and get) sleep"? I feel like that is unlikely, judging from the "he's been out of cryo for too long" line from CATWS. The timeline goes: day 1 Bucky makes assassination attempts daytime + night time against Fury / day 2 Steve makes a run down to Jersey arriving there at night / day 3 Bucky attacks Steve on the causeway and then we get the nighttime vault scene where Bucky is "unstable". Even if we add a day or two prior to allow for prepping, that still means Bucky becomes "unstable" and questions his identity within a bare week of being out of cryo.

Credit @lost-shoe (this post)
Now onto the angst...we know anaesthetics is not like restful sleep, so theoretically neither is cryostasis. While the science of cryostasis doesn't exist at the moment, we know from artificial hypothermia in surgical situations that it puts incredible stress on the body and all its organs. Looking at the laboratory derangements during hypothermia it looks like it pushes the body over to anaerobic metabolism and causes lactate to go up. You know when you go for a run and your muscles cramp up because you haven't warmed up enough? That's because your muscles have produced too much lactate from anaerobic metabolism. So...no wonder Bucky can't stand when he comes out of the cryo chamber. It also increases one's bleeding risk and reduces one's healing speed, so take of that what you will for your Whumptober prompts 😂
I also wonder whether, because the brain is not receiving any REM sleep during cryo, it means Bucky has been in a constant state of sleep deprivation for the last 70 years. The theory of "prefrontal vulnerability" in sleep deprivation proposes that functions like language, executive functions, divergent thinking, and creativity are particularly affected, so that can contribute to Bucky's inability to process/produce complex language and his slowness when it comes to working through complex problems. It also has significant effect on memory and attention: it's interesting to note that during sleep deprivation of more than 35 hours, they found that while free recall was affected, recognition was not. (Disclaimer for science: small sample size, opposite result for subjects with sleep deprivation ~24 h).

So yeah, I think there are practical reasons why Hydra would not allow Bucky to have restorative sleep between missions. Consolidation of long term memory (i.e. transferring them from short term storage into long term storage) usually happens during sleep which means it is quite likely Bucky remembers only broken bits of his time (if at all) in the last 7 decades.
#bucky barnes#bucky barnes meta#medical meta#bucky barnes: where the angst that keeps on angsting#asks#i hope you get to see this nonnie! i'm so sorry for the long wait
219 notes
·
View notes
Text
Catecholamine-Refractory Anaphylactic Shock to Vecuronium in a Patient with Tetralogy of Fallot: A Case Report | Abstract
View On WordPress
#Anaphylactic Shock#Cardiopulmonary Bypass#Symmetrical Peripheral Gangrene#Tetralogy of Fallot#Vecuronium
0 notes
Text
As a healthcare professional and someone certified in first aid and CPR/basic life saving, I want to just point out how much I loath this panel from “Trinity”

This is gonna be a long post. But the summary is, both only are both things Bruce did to help Jason and the others who were possessed (cuz demon possession in this arc) were 1) not good ideas 2) probably wouldn’t have worked as described and 3) unnecessarily painful.
Firstly, the defibrillator and the medical inaccuracy. Bruce, you should know better than this.
They are not designed to restart hearts - this is a very common misconception worsened by medical dramas. They’re designed to disrupt potentially fatal arrhythmias that don’t allow the heart to properly pump blood (which makes it hard to detect a pulse or heartbeat) by shocking the heart and temporarily stopping the natural electrical signals telling the heart to pump in hopes the heart’s natural pacemaker will reset itself. Yes, the heart can stop beating during this - it’s why it’s so dangerous to use a defibrillator on a healthy person and why medical personnel cannot touch the person being shocked unless they’re holding the paddles. Also, this is often painful to the person being shocked.
If a patient is flatlining, it’s a sign there is no electrical activity, meaning the heart is not sending signals to pump. A defibrillator is not designed to be used in that situation and isn’t gonna do much. And the companies that make defibrillators have warnings that state using them in this situation may irreparably harm the person. It is difficult to get a person back from this - current recommendations are to start CPR in hopes the heart might decide to come back and/or to give adrenaline.
(As a side note here, some hospitals have devices that can stimulate cardiac contractions to assist with CPR. Those devices may also have defibrillators attached to them for easy access).
Secondly, Potassium Chloride (KCl) injections are well known for causing death. In general, increased levels of potassium in the body, even from supplements or medication, can cause severe and life threatening arrhythmias which can lead to death if untreated. We can argue here, Bruce used this injection to trigger an arrhythmia to allow him to temporarily stop a heart a defibrillator. This would actually make sense, but there’s a snag because it’s not that simple.
You have to treat the increase of potassium in the body. In the hospital, this is usually done with infusions of calcium and/or glucose and insulin (insulin levels and potassium levels are inversely proportional). You can’t just inject a person with KCl and assume you only need a defibrillator.
The current cocktail infusions used to stop hearts during surgery (referred to as Cardioplegia) do use potassium for that, but also have other components to limit other side effects and protect the heart from damage. Usually, the heart restarts on its own after the solution is removed. There are instances where mild localized shocks are needed which are nowhere as intense as those seen with defibrillators. Mind you, patients need to be on cardiopulmonary bypass while under the effects of Cardioplegia to prevent brain damage.
But the other big issue with this method of stopping the heart is that injections of KCl are excruciatingly painful. Due to how it affects the body and inflames the vascular nerves, you have medical texts that describe the damage as burns or mimicking burns - people who have dealt with this either intentionally or unintentionally have described it as feeling like their veins are on fire. Even diluted KCl infusions for medical purposes can be painful and unpleasant.
The fact Batman did this to his own son with the purpose of killing him without any sort of thing to help stop that pain, really, really bothers me.
Also, why would Bruce just have KCl concentrate injections????????
19 notes
·
View notes
Text
Olivia’s OR Arrest
Olivia Eastham was a 33 year old who was of average height with a skinny, flat chested build, sandy light brown hair with bangs, greenish eyes that were usually behind a pair of glasses, and was fair skinned. Olivia was the cute, nerdy type that was often overlooked by many, and enjoyed things such as D&D, star wars, and Legos. She was a previously healthy person, with nothing overly worrying in her medical history- had her appendix removed at age 12 and was discovered to have issues metabolizing gluten products in her mid 20s.
However, her health concerns became more serious recently. After dealing with heart palpitations, sporadic shortness of breath, and eventually coughing up blood, she was brought to our emergency department to be examined one evening. It was discovered that she had pulmonary edema brought on by aortic valve insufficiency. Olivia was taken up to the operating room for open heart surgery to replace the faulty valve in her heart. A large, vertical incision was made in the center of Olivia’s chest, starting at the top of the sternal manubrium, and all the way down to the epigastric area. The underlying tissues were dissected and the sternum was drilled in half vertically. A rib spreader was placed, and her chest was cracked wide open. Olivia was placed on cardiopulmonary bypass, and the diseased aortic valve was successfully replaced over the following 4 hours. The breastbone was closed with sternal wire, and the skin incision was closed with multiple staples. After surgery, Olivia was sent up to surgical recovery for observation.
Olivia awoke in the coming hours after sedation was weaned. Her vital signs weren’t the greatest- she was hypotensive and bradycardic. She complained her chest was sore and felt pressure, but the surgical team assured her that her vital signs would improve as the anesthesia weans its way out of her system, and the pain and pressure she complained of would dissipate as her sternum and ribs heal from the chest cracking. Olivia took what the doctors said at face value. Who was she to question them? “yeah, they’re probably right. I just need to give myself some time to heal, then I’ll be ok.”, she thought to herself, oblivious to the fact of what was to come later that same day.
Over the coming hours, Olivia still complained of soreness and pressure on her chest. Her vitals signs still weren’t the greatest, so it was decided that she would be started on IV fluids and electrolytes. A repeat chest x ray and some blood tests were ordered to rule out common post operative complications such as infection or blood clots. The fluids helped a little, but only did so much. On the chest x ray, it was shown that her left ventricle was a bit swollen and enlarged. But the doctors attributed this to her aortic valve issues as well as the pulmonary edema. Essentially claiming that these two issues are to blame for the hypertrophy, and it will dissipate during the healing process. An echocardiogram confirmed this, and didn’t have any further findings at that moment.
A little while later, the blood test came back. There was no evidence of infection, there was no evidence of a blood clot, but there was a drop in red blood cells, iron, and hemoglobin. Common causes of this could be from the fact that she hasn’t eaten in awhile, or that she’s bleeding internally. But the chest x ray and echocardiogram showed no evidence of this. The team decided to just keep giving Olivia fluids, electrolytes, and occasional pain meds.
Around 10:45 that morning, Olivia started to take a turn for the worse. She was experiencing severe chest pain. She was clenching her chest and wincing in pain, knowing that something was seriously wrong. The team noted EKG changes- specifically an alternating QRS complex, inconsistently changing from high to low on the monitors. Her blood pressure was dropping at a concerning rate, and jugular venous distention was noticed. Auscultation of her heart noted muffled, more quiet heart sounds. The team ordered a repeat echocardiogram and were shocked at what they saw. It was a massive, rapid onset cardiac tamponade. The team sprung into action and notified the OR that they were on their way back up. “another surgery? What’s wrong? Am I going to die?!” a terrified Olivia asked, session the urgency of the situation. A tamponade of that size couldn’t be drained by a needle. Plus, the cause of this needed to be discovered. It didn’t just magically appear, even though it felt that way.
An OR was prepped, and Olivia was moved onto the table. The surgical prep was expedited due to the emergent nature of the situation. In the coming minutes, Olivia was sedated, intubated, and a blue bouffant cap was placed on her head.
In patients that had a previous median sternotomy, there’s a different technique when it comes to cracking their chest. The surgical team used wire cutters to snip and remove the staples in the center of Olivia’s chest. After the staples were out of the way, the incision was able to be reopened. Since it wasn’t fully healed, this process was rather easy. The underlying tissues hadn’t healed yet, and scar tissue wasn’t present either. This incision could be reopened with 1 cut, and this exposed the sternum. The sternum was being held in place with metal wire, which was snipped with wire cutters. Next, a rib spreader was placed in the divided portion of the sternum. “patient’s in v-fib. You gotta get that chest open!” one of the other doctors in the OR called out, looking over at the loudly chirping monitors.
Once Olivia’s chest was pried open nice and wide, there was surprisingly no blood. Where was it?! Well, the team found out moments later when the pericardium was incised. Blood shot out of the incision area, and started to accumulate on the blue surgical drape on Olivia’s torso, and even dripped onto the sheet on the table. A vascular clamp was placed on the descending aorta near the diaphragm, and suction was applied to the area to create a line of sight. Since Olivia was in v-fib, epi and atropine were pushed intravenously, and the internal paddles were called for.
The large, spoon shaped paddles were charged to 20 joules, lowered into Olivia’s chest around her frantically twitching heart, and a shock was delivered. A dull, wet, clumpy sound filled the room in response to the shock. No change was present, so a cycle of internal massage was initiated. After said cycle, the paddles were charged to 30 joules and lowered back in, delivering a shock once everyone stood clear. This stronger shock caused Olivia’s toes to curl on the other side of the table. You could see the fresh, black nail polish on her toes and the deep, thick wrinkles throughout the soles of her size 8 feet. The second shock had no discernible change, so internal massage was restarted.
While performing internal compressions, other member of the surgical team poked and prodded around inside Olivia’s chest cavity trying to explain what was causing the lethal tamponade, but kept coming up empty. After this investigation, several cycles of internal massage, and a 2nd dose of meds, the internal paddles were charged to 30 joules once again, and the next shock was delivered. Olivia’s torso flopped somewhat in response to the paddle’s electric jolt. This time, Olivia converted to pulseless electrical activity, and internal massage was resumed.
It took several minutes worth of efforts and another dose of meds to produce a shockable rhythm. After that shockable rhythm was obtained, Olivia was defibrillated again. That same dull, wet thump from before was heard, but failed to ameliorate the situation. Olivia was shocked another time… then another time….then another time, then ANOTHER time, but she just wouldn’t come back. Her heart just kept weakly fluttering, not even responding to the efforts. At that point, Olivia was down for 28 minutes, was maxed out on drugs, and had fixed and dilated pupils. The surgical team made the tough decision, calling time of death at 11:32am while she was still in v-fib.
The surgical nurses removed the equipment, shut the monitors off, and cleaned up the blood from Olivia’s body. A toe tag was placed, she was covered up, and was sent up to the morgue.
Olivia’s autopsy showed that her fatal tamponade was caused from a slight mistake during her valve replacement surgery. The replacement heart valve was ever so slightly too big to fit inside the space between the aorta and left ventricle. Since the artificial heart valve wasn’t the correct size, it stretched the walls of the aorta, causing a few small tears. The tears grew larger, as did the bleeding, resulting in her tragic passing. Olivia’s family was able to sue for medical negligence, and received a hefty settlement payout, but all the money in the world couldn’t take away the pain they felt.
54 notes
·
View notes
Text
Twilight Advent, Day 6
Masterpost/prompts
Dec. 6 - Which modern medical treatment is Carlisle especially thankful for?
"And Then Run"
(~1,000 words)
It was an incredible machine, he had to admit.
Medicine seemed to be changing faster than either of them could manage to keep up with these days. It had been over a decade since Edward had gone to medical school for the first time; mostly to get out of the now too-full house after the newness of his zany, tiny, prophetic sister and her taciturn husband had worn off.
He had learned there about cardiopulmonary bypass; had the experience of watching one safely from the gallery. Even if he had still been human, he could imagine that the rhythm of the metallic clacking of drum against metal would be a sound he would remember forever; alongside it the gentle whir of the fluid that was supposed to be the one thing he could never resist and yet which became simple to ignore as he engrossed himself in his own fascination with the way it spun around.
Edward had come to the hospital the way he often did, a question on his mind he didn't want anyone else in the family to overhear. Carlisle, who'd scented him from across the floor, had called him to his side. And so they were both standing here now, before this machine which was an order of magnitude more terrifying and more fascinating than any bypass Edward had ever seen before.
The boy—the paperwork on the end of the isolette said he was a boy—before them would've fit in Edward's palms. A balled up fist, too tiny to fit around Edward's thumb, rested near his head, immobilized so as not to interfere with the grotesque maze of tubes protruding from the tiny mouth and the cannulas beneath the skin next to a sternum which was mere inches long.
Carlisle, as one of the hospital's cardiothoracic attendings, had come here to take notes, but according to the memories at the tip of his thinking, he had been standing here for a good fifteen minutes. Watching. Thinking. About...something he wasn't quite willing to make clear. As his father danced the delicate dance of trying to think in a way that shut Edward out, the strain of that plus whatever he was thinking about was enough that he balled his fist.
"Carlisle? What's bothering you?"
The anger and frustration in his father's thoughts made little sense. The infant—born almost three days ago now, according to the tag—was improving hour over hour.
And then suddenly there was a sound Edward had heard only a few times in his life. The sharp intake of breath; a second, ragged inhalation through the nose. Carlisle's hand covering his mouth as his eyes squeezed closed against tears his body would never produce.
Yet somehow he was still managing to evade Edward's gift, the reason for this outburst just out of reach. Not knowing any other way to get the information he needed, Edward went for the hardest punch:
"Dad?"
A gulp and then Carlisle met his eyes. The extra thoughts—charting details, mostly—fell away as though they were a shattering pane of glass and at once, the core thought was clear. The diagnosis, at the top of the chart. The sadness of the family, the shock of their baby being wheeled away, but then this miracle machine, attached quickly but carefully, and suddenly numbers going in all the right directions: Sats, up. Heart rate, up. Capillary refill, almost normal.
He understood at once. Moving closer to his father, so that their hips were almost touching, Edward stared down again, hard, at the baby underneath the spaghetti mass of medical tubes.
Pulmonary hypoplasia, secondary to diaphragmatic hernia. The diagnosis Carlisle had made, decades later, piecing together details of a handwritten medical chart with what little his wife had told him. Congenital. A birth defect. Not anything she had done. Not what her husband had done to her. Just a fluke of nature, a bad spin of the roulette wheel that was forty-six haploid chromosomes slamming together.
"This machine would have saved him," Edward whispered, and his father nodded slowly.
And then he flashed in both their minds. Edward, who knew what the boy's father had looked like, imagining that man, but softened by the more gentle curves of his mother's face; her lighter hair; her smile. In Carlisle's mind, he had always looked very much like Esme, and sometimes, selfishly, a little bit like Carlisle, too. He was a young man, to both of them—broad shoulders, tall, strong.
"Sixty years," Carlisle finally said. "If she had been born just sixty years later...we could have...I could have..."
The fist had returned.
"But you wouldn't have her," Edward whispered.
For a moment, there was no answer, aloud or in thought, as Carlisle regarded the infant. The machine whirred and beeped, the artificial respirator thudded open, whooshed, and then closed again.
"No," his father said thoughtfully. And Edward could feel that pain; the aching, stretching sadness that rolled over the thoughts as a life was imagined: just the two of them, missing the caramel-haired woman with her smile, her laughter, and her love.
There was another gulp, and Carlisle took a step closer to the isolette, and placed a hand on the top of the baby's head. It startled, likely at the coolness of the touch, the tiny fists clenching and the arms seizing inward.
"But she would have him."
Then Carlisle removed his hand, stepped away, picked up the chart, and made a few notes before beckoning Edward back downstairs.
~||x||~
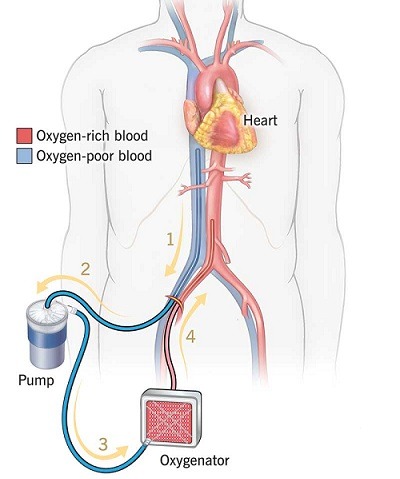
Historical note: Extracorporeal Membrane Oxygenation (ECMO), an extension of surgical cardiopulmonary bypass, was first used the 1970s on a non-surgical patient. While first used on adults, it quickly began to be used to buy the time neonates needed to recover from respiratory failure. By the mid 1980s, the survival rate for neonatal ECMO treatment of respiratory failure was between 70-90%.
Montage Masterpost
#montage#my fic#twilightadvent22#carlisle cullen#edward cullen#esme cullen#vampires at work#revised on 12/7#because late night me thinks semicolons and commas are decoration
54 notes
·
View notes
Text
Understanding Venous Air Embolism: Timeframe and Potential Risks

Introduction
In the world of medical emergencies, knowledge can make all the difference. One critical condition that demands immediate attention is venous air embolism (VAE). Understanding the timeline and potential risks associated with VAE is essential for healthcare professionals and individuals alike. In this article, we'll delve into the question, "How long does it take for a venous air embolism to be fatal?" while shedding light on what VAE is, its causes, symptoms, and preventive measures.
What is Venous Air Embolism (VAE)?
Venous air embolism (VAE) is a potentially life-threatening condition that occurs when air enters a person's bloodstream through a vein. The presence of air bubbles in the bloodstream can disrupt normal blood flow and lead to various complications, including organ damage and, in severe cases, death.
Causes of Venous Air Embolism
VAE commonly occurs during medical procedures that involve the manipulation of veins or when the body is in a position that allows air to be drawn into the bloodstream. Common scenarios where VAE may occur include:
1. Surgical Procedures: Surgeries that require the use of central venous catheters, cardiopulmonary bypass, or any procedure where veins are exposed can potentially introduce air into the bloodstream.
2. Invasive Medical Procedures: Insertion or removal of central lines, hemodialysis, and certain obstetric procedures can create opportunities for air to enter the veins.
3. Childbirth: During childbirth, especially if a woman is in certain positions, there is a risk of air embolism.
Symptoms and Immediate Risks
The onset of symptoms due to VAE can vary depending on the amount of air that enters the bloodstream and the patient's overall health. Common symptoms include difficulty breathing, chest pain, confusion, dizziness, and in severe cases, loss of consciousness or cardiac arrest.
As for the question, "How long does it take for a venous air embolism to be fatal?" the timeline can be swift. In cases where a significant amount of air enters the bloodstream and reaches vital organs, the effects can be fatal within minutes to hours if not promptly addressed.
Preventive Measures and Treatment
Preventing VAE involves careful attention to procedural techniques and patient positioning. Here are some preventive measures:
1. Proper Positioning: Keeping patients in positions that prevent air from entering veins is crucial. This is particularly important during surgeries and procedures.
2. Central Line Insertion: Using proper techniques for central line insertion and removal can minimize the risk of air embolism.
3. Alertness: Vigilance among medical professionals is essential. Monitoring patients for signs of VAE during procedures can lead to early detection and timely intervention.

Conclusion
Venous air embolism is a serious medical condition that demands swift action and knowledge from medical practitioners. While the time it takes for VAE to be fatal can vary, the consequences of not addressing it promptly can be severe. Understanding the causes, symptoms, and preventive measures associated with VAE can save lives and enhance patient safety during medical procedures.
For more information or if you have concerns about VAE, consult with a medical professional or visit reliable medical sources. Remember, knowledge is a powerful tool when it comes to medical emergencies like venous air embolism.
3 notes
·
View notes