#apoe4 gene
Photo

Risk Regions
In the brains of Alzheimer’s disease patients, protein clumps accumulate – in the form of amyloid plaques and tau tangles – leading to neurodegeneration. Certain regions of the brain are more susceptible to this pathology than others, but why? Recent research based on brain scans of hundreds of middle-aged and older volunteers, suggests it’s something to do with regional differences in the activation of a protein called APOE. Indeed, these heat maps show areas of the brain where APOE is especially active (top row, orange and red areas), and where tau tangles are especially abundant (bottom row, orange and red areas) – note the striking overlap. APOE is a fat-handling protein, and a specific version of it – APOE ε4 – is associated with increased risk for Alzheimer’s. While questions about the disease mechanism remain, the finding of this APOE-pathology link provides a piece of the puzzle that will likely inform future research and interventions.
Written by Ruth Williams
Image by Diana Hobbs, Washington University
Research by Aylin Dincer and colleagues, Mallinckrodt Institute of Radiology, Washington University School of Medicine, Saint Louis, MO, USA
Image copyright held by Diana Hobbs
Research published in Science Translational Medicine, November 2022
You can also follow BPoD on Instagram, Twitter and Facebook
16 notes
·
View notes
Text
Mice reach the twilight of their lives at around age two, the rough equivalent of 80 in human years. And when researchers introduce specific mutations into mice and then age them up, the mice can grow forgetful and irritable—eventually exhibiting signs of Alzheimer’s disease not unlike that of many elderly humans.
“Older mice, and those with the APOE4 variant, have these exhausted, fatigued immune cells in their brains, and we discovered a similar phenomenon in human datasets,” says Sohail Tavazoie, a professor at Rockefeller University.
Continue Reading.
76 notes
·
View notes
Note
I think what doomed the MCU quality-wise was deciding to leave it open-ended and keep going. Continuity and characterizations don't stand a chance when there's no endgame in mind. Pun somewhat intended. Endgame wasn't a good movie but it took Phase 4 for a lot of people, myself included, to realize that. I think Endgame's legacy - and the MCU's for that matter - would be a lot more favorable if that movie HAD been the actual endgame.
That's an on-going point really against the current MCU: Endgame had been set up basically as the finale of Phases 1-3, meaning it feels like a perfect conclusion to everything that had been set up...but of course, cause the MCU refuses to end, even Endgame sets up stuff that we see in Phase 4, Loki being a obvious example, but instead of going back to his whole, "The sun will shine on us again." thing to Thor in Infinity War, we just...go into a Loki show in Phase 4 that in itself is just setting up Kang.
And then you got the Gamora thing the movie set up that...doesn't even seem to be getting explored in the new Guardians movie as she's already with them again, as even Love And Thunder showed Thor leaving the guardians at least to do his own thing again.
And with the mention of Love And Thunder: 'Thor will return.'- again, they very confident that they'll give Thor another movie that they didn't even tell the director or Chris Hemsworth who as we know, has decided to take a break from acting due to wanting to spend time with his family after discovering he has two APOE4 Genes, making him ten times likely to develop Alzheimer's disease.
Like I will point out: Disney couldn't predict this, but the fact remains that they refuse to just plan stuff out before going ahead, meaning they jumped instantly to 'Thor will return' in the same phase that already has various open endings to plots to come, with I think only WandaVision's open ending concluding....in the train wreck that was Multiverse Of Madness that in itself has ANOTHER open ending.
And yes, I know they claim to now have two plans, aka Multiverse stuff and Kang plans, but here's the thing: they entered Phase 4 by that logic with zero plans beyond doing random crap with open endings, because they couldn't just take a break to do planning so they set up random stuff we may either get or may not get.
Like, if they really wanted to continue the MCU so badly after Endgame, they should have just rebooted at best or waited to do planning, as now we in a mess that's quality is showing as we see with the reactions to No Way Home, Multiverse Of Madness, Love And Thunder and now Ant Man And The Wasp: Quantumania (which is literally meant to start off the planned phase 5 too ironically).
#anti mcu#mcu critical#didn't even get to mention they did a black widow film...in phase four#after she died in endgame#when a black widow film should have been done earlier#and dont care it was to set up yelena#cause they probably gonna mess her up in this thunderbolts film they got coming up
19 notes
·
View notes
Text
“His makeup includes two copies of the gene APOE4, one from his mother, the other from his father, which studies have linked to an increased risk of Alzheimer’s disease.”
3 notes
·
View notes
Text
Promising discovery for Alzheimer's treatment

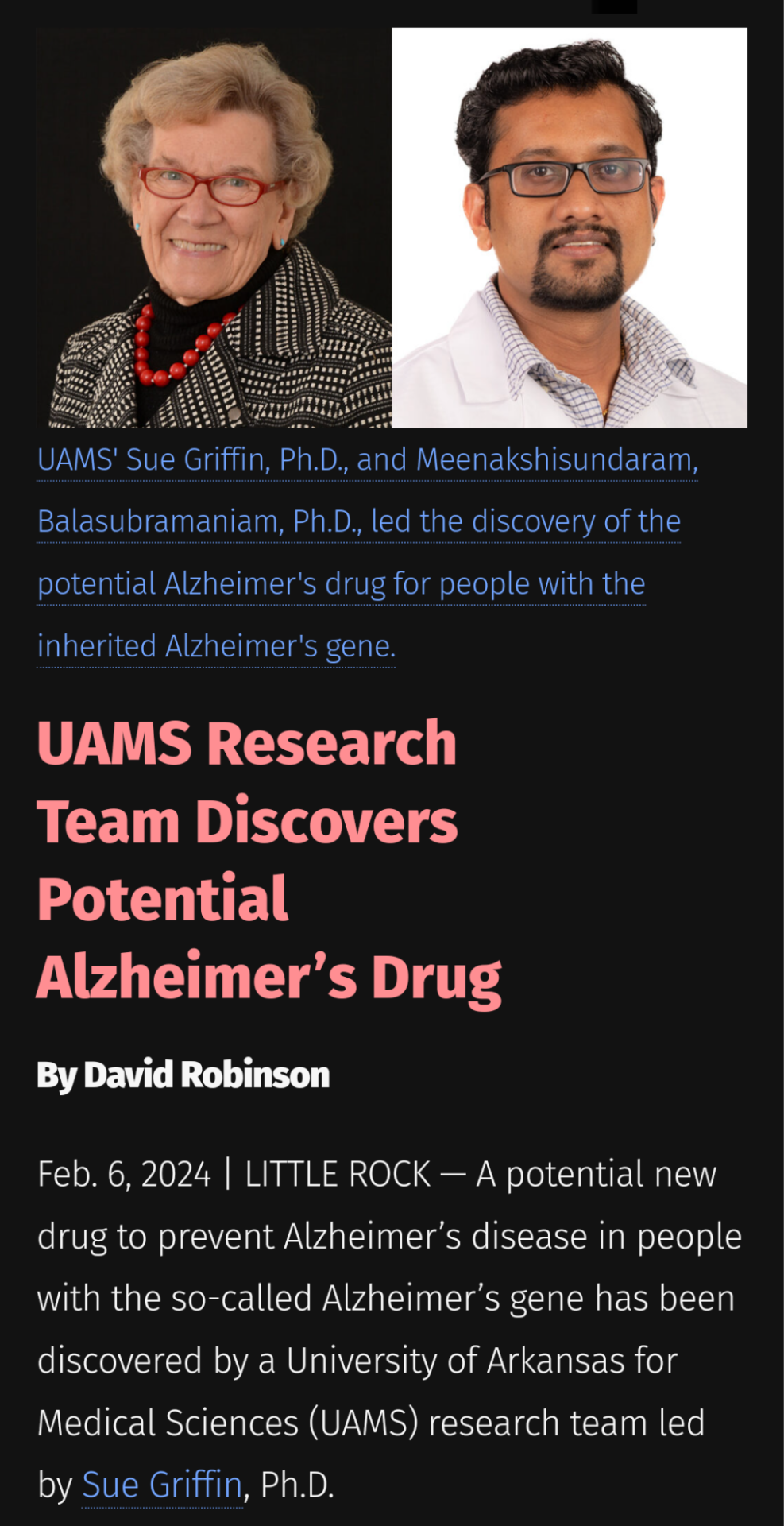
The findings were published on 8 Jan 2024 in Communications Biology and include discoveries of a druggable target and a drug candidate, made by Meenakshisundaram Balasubramaniam, Ph.D., the paper’s first author.
An estimated 50-65% of people with Alzheimer’s disease have inherited the Alzheimer’s gene, Apolipoprotein E4 (APOEε4), from one or both parents. About 25% of people have one copy of APOEε4 and are three times as likely to develop the disease. Those with two copies (one from each parent) make up 2-3% of the population and are 12-15 times as likely to develop Alzheimer’s.
Balasubramaniam, co-principal investigator on the NIH grant with Griffin, said UAMS built the first known full-length structure of APOEε4 protein in 2017, which he created using bioinformatics and computational modeling techniques. This foundational work led to the discovery of the druggable site on the APOEε4 protein, ApoE4. (APOEε4 refers to the gene, and ApoE4, without the epsilon symbol and no italics, is the protein.)
Balasubramaniam’s unique skills and curiosity, Griffin said, were the catalyst for the discoveries. “I don’t know of anyone else in the world but Dr. Balasubramaniam who can do the work that’s in this paper,” Griffin said of the assistant professor and Inglewood Scholar in the Department of Geriatrics.
Other research team members listed in the USMS article.
UAMS
Related story: The Despair of Persons Living With Alzheimer’s Disease by Jason Karlawish at The History Reader
1 note
·
View note
Quote
Microglia, the immune cells of the brain, wither away as Alzheimer’s disease takes hold in both mice and humans, and APOE4, a key gene variant implicated in Alzheimer’s, may mediate these changes, according to new research.
Mice reach the twilight of their lives at around age two, the rough equivalent of 80 in human years. And when researchers introduce specific mutations into mice and then age them up, the mice can grow forgetful and irritable—eventually exhibiting signs of Alzheimer’s disease not unlike that of many elderly humans.
“Older mice, and those with the APOE4 variant, have these exhausted, fatigued immune cells in their brains, and we discovered a similar phenomenon in human datasets,” says Sohail Tavazoie, a professor at Rockefeller University.
The team dubbed this new class of exhausted cells TIM, for terminally inflammatory microglia. TIM have lost the ability to efficiently remove plaque from the brain and thus may contribute to Alzheimer’s.
Burnt out immune cells may drive Alzheimer's disease - Futurity
0 notes
Text
Structure of Equity - Jamaine Davis - Meharry Medical College
Sharing some of our #SBGrid member tales from the last year. This one from September 2022.
Numbers speak clearly to Jamaine Davis. As a boy growing up on Long Island, math came so easy to him that one of his family nicknames was "the professor."

Other numbers have shaped his ambitions at Meharry Medical College in Nashville, Tennessee, where Davis runs one of the few labs in the world that uses structural biology to help explain biological health disparities.
For example, U.S. Black adults are twice as likely to have Alzheimer's disease compared to non-Hispanic Whites. And despite a somewhat lower overall lifetime risk of breast cancer, Black women experience a 40% higher death rate from breast cancer than White women at every age and are more likely to be diagnosed with fast growing and late-stage breast cancer.
"My research program is basically at the intersection of structural biology, genetics and disease, and health disparities," says Davis of the big-picture questions that guide his lab's work. "What are the molecular mechanisms that dictate who develops diseases like cancer or Alzheimer's? And then how do we design effective therapies? How do we target the right pathways for the right treatment for that patient?"
One project in the early stages focuses on a gene (ABACA7) that has a stronger effect on risk of Alzheimer's disease in Blacks than the better known ApoE4 gene risk variant. "It's actually the strongest risk factor for developing Alzheimer's in African Americans known so far," Davis says.
As he explains it, ABACA7 transports lipids out of cells, handing off the lipids directly to ApoE, and also interacts with Tau, another protein that goes awry in Alzheimer's. Two missense variants in ABACA7 confer the risk.
"So we've been studying these mutations to see what impact they have on lipid transport," Davis says. "Once we're done, we can look at the people who particularly carry this mutation or variant, see what downstream processes are altered, and design therapies to rescue that. And these variants so far have only been identified in African Americans."
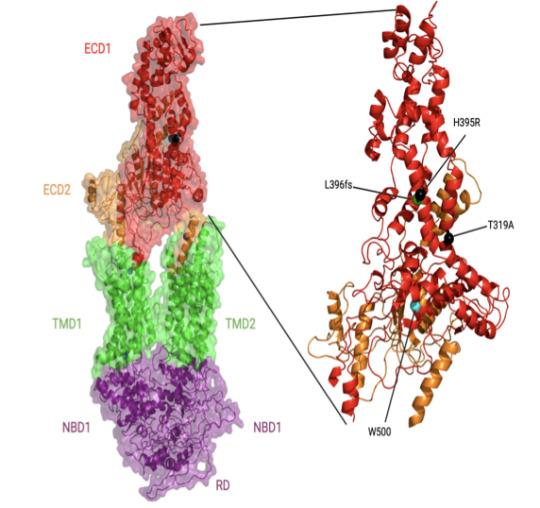
In individuals with African ancestry, the phospholipid-transporting ATPase ABCA7 (ABCA7) gene has stronger associations with Alzheimer’s disease risk than in individuals with European ancestry and than the apolipoprotein E (APOE) ɛ4 allele. The Davis lab is exploring the structure and function of key ABACA7 mutations and how they contribute to alterations in transporting lipids, which may influence Alzheimer’s in African Americans. Credit: Courtesy of J.Davis.
Davis began his academic training on a different career path. With his early affinity for math and science, he reasoned that chemical engineering made sense as a college major. But near graduation at Drexel University, he realized that the typical next step for someone with a chemical engineering degree was a job at an oil company. He hadn't taken one biology course in college, but he found himself drawn to biomedical research instead.
He seized an opportunity to work in a biophysics lab at a neighboring school, University of Pennsylvania, where his mentor Jacqueline Tanaka gave him a peek at the scientific career he could have in biophysics and opened his eyes to the kind of academic role model he could be. Her excitement for X-ray crystallography and for increasing the proportion of women and minorities in science inspired him to go to graduate school.
"She built her career in structural biology and mentoring, hand in hand," Davis says. "She saw some potential in me, and I was at a crossroads." Davis had also been unaware of the extent of health inequities across the country and of the low representation of minorities in academia.
For his thesis, Davis chose the lab of Harvey Rubin, a dynamic speaker who fostered an immediate interest in infectious disease. In Rubin's lab, Davis characterized an enzyme that enables Mycobacterium tuberculosis to enter (and possibly exit) the dormancy stage in the lungs of people.
When Davis finished his PhD in 2007, he was the first Black to earn a doctorate in biochemistry and molecular biophysics at UPenn. "I had a great time," he says. "They were very supportive. But it is pretty shocking. If you look at Twitter, there are other people posting the same kind of statistic. They're the first Black to graduate from a certain program at a certain institution. It does show there is still some under-representation across different departments."
He followed up with two postdoctoral fellowships at the National Cancer Institute. He first showed that a novel protein in Shigella (bacteria that cause food poisoning) was not a protease, as some suspected. A second project elucidated the binding modes of a protein with multiple domain repeats implicated in the development of cancer.
Then he thought about how best to combine his interests in a distinctive research program. He chose Meharry, one of the oldest and largest historically black U.S. academic health centers. (Davis is also a member of the Vanderbilt University Center for Structural Biology.)
Historically black colleges and universities are powerhouses in educating African Americans who go on to earn doctoral degrees in science, technology, engineering, math, and medicine, as Davis and his co-authors reviewed in a commentary (Cell, 2022). Blacks make up 12% of the U.S. workforce, but only 5% of working physicians and 3.6% of full-time faculty conducting research at medical schools.
When the COVID-19 pandemic hit, Davis found new opportunities for mentorship and community outreach. Soon after the pandemic took hold, a student-driven community formed on Twitter with the handle @BlackInBiophys and a logo designed by Taneisha Gillyard, a former postdoc in the Davis lab. Davis spoke at a virtual meeting held by the group.

A former postdoc in the Davis lab, Taneisha Gillyard, designed the logo for @BlackInBiophys, a student-driven community that formed on Twitter during the pandemic. Credit: Taneisha Gillyard.
In a short time, a strong sense of community developed among people who may have never met in person, but know a lot more about each other through social media, Davis says. People share grant writing tips, training and job opportunities, and generally celebrate the scientists, their contributions, and career options for the next generation.
The visibility may help change other statistics about Black researchers receiving less NIH funding and being cited less often than their white colleagues, Davis says.
Davis also teamed up with Meharry colleague Jennifer Cunningham-Erves to develop a funded community outreach project to address community concerns about vaccines. He has spoken about the basic science of mRNA at townhall-style community meetings, in person and virtual. The online recordings have reached people from Chicago to New York to Haiti.
The project collaborates with a consortium of more than 90 churches in middle Tennessee and Better Options TN, a community nonprofit organization. To understand concerns, the Meharry team interviewed people in the Southern United States. They developed and organized content on a frequently updated web site, https://yourcovidvaxfacts.com/en.
"We asked about their thoughts about the vaccine and the virus," Davis says. "The biggest one, particularly for Black Americans, was the distrust with government and healthcare. But I was very impressed with some of the questions that the public had. They weren't getting answers, and they wanted answers. If you remember, one of the major issues with people not getting a vaccine was that they thought it would affect their DNA. They just weren't familiar with mRNA."
Davis felt their concerns and trust issues as well. He initially was cautious about being vaccinated himself, waiting to see more data about its safety in people. "Even being a scientist, I was hesitant," he says. "I didn't want to be one of the first," he says. But as he explained the science and helped alleviate concerns of others, he also convinced himself to get the vaccine too.
Meanwhile, back in the lab after the pandemic disruptions, Davis and his team are working to improve health outcomes for populations most at risk, one variant protein and pathway at a time.
- Carol Cruzon Morton
0 notes
Text
Center Maps New Path for Alzheimer’s Prevention and Treatment - Technology Org
New Post has been published on https://thedigitalinsider.com/center-maps-new-path-for-alzheimers-prevention-and-treatment-technology-org/
Center Maps New Path for Alzheimer’s Prevention and Treatment - Technology Org
The new brain center will focus on research translating genetic, metabolic and molecular insights into interventions that protect those at risk before brain changes set in.
The medical community can foresee a looming increase in Alzheimer’s disease, the most common form of dementia, as the population ages. The number of Americans affected is projected to nearly triple by 2050, from 6 million to 16 million.
Although the Food and Drug Administration has approved a couple of treatments for early disease designed to slow progression, the injury to brain tissue that strikes at memory — and at patients’ very identity — seems irreversible.
Brain, neural networks – artistic interpretation. Image credit: Growtika via Unsplash, free license
Researchers at the Keck School of Medicine of USC are determined to gain a deeper understanding of factors underlying Alzheimer’s and use what they find to intercede, decades before damage sets in. Driving this work is a new interdisciplinary program, the USC Center for Personalized Brain Health.
The starting place for the center’s work is a relatively common genetic variant, called APOE4. The one in four people who carry one copy of the gene are at higher risk for Alzheimer’s. Compared to the general population, the 2 or 3% of people who have two copies face eight to 12 times the risk for the disease. More than half of Alzheimer’s patients have the APOE4 gene.
“USC has a really rich ecosystem … The new center will bring together diverse investigators and providers with a unified vision — a future in which Alzheimer’s disease is no longer a serious threat.”
“Most people with APOE4 don’t get neurological attention until they have dementia,” said endocrinologist Hussein Yassine, MD, director of the Center for Personalized Brain Health and associate professor of neurology, medicine and physiology and neuroscience at the Keck School of Medicine. “Our center is going to provide resources to these individuals well before they get the disease, in hope that this may be the right time to intervene.”
The center’s central projects comprise building a registry of APOE4 carriers, imaging the brain for early detection and intervention, developing interventions (such as diet and exercise) that can be deployed for prevention, profiling Alzheimer’s-related changes that precede clinical symptoms, and developing drugs focused on neuroinflammation once clinical dementia ensues.
“Alzheimer’s disease is one of the biggest challenges we face in human health,” said Carolyn Meltzer, MD, dean of the Keck School, May S. and John H. Hooval, M.D., Dean’s Chair and professor of radiology. “Taking it on calls for research that is both creative and rigorous, backed by enabling resources. That combination makes the Center for Personalized Brain Health an exciting vehicle for the Keck School to ignite lasting change in dementia research and care while advancing precision medicine.”
A connection between basic science and clinical impact for Alzheimer’s disease
Yassine and his colleagues have already uncovered details about the mechanisms behind Alzheimer’s disease and its progression. The Center for Personalized Brain Health will channel these insights into a larger-scale endeavor linking lab findings to clinical care, and vice versa.
According to Yassine, that translational focus fulfills a complementary role alongside existing infrastructure at the Keck School and the university overall: The USC Zilkha Neurogenetic Institute pursues basic discovery, and the USC Mark and Mary Stevens Neuroimaging and Informatics Institute identifies the changes dementia causes in the brain. Meanwhile, there are outstanding resources for clinical research at the USC Alzheimer’s Therapeutic Research Institute and the USC Alzheimer Disease Research Center.
“USC has a really rich ecosystem,” Yassine said. “The new center will unite diverse investigators and providers with a unified vision — a future in which Alzheimer’s disease is no longer a serious threat.”
Indeed, the Center for Personalized Brain Health’s interdisciplinary efforts will integrate expertise in genetics, neuroscience, neuropsychology, computer science, radiology, pharmacy and nutrition in order to break ground, and provide help, on numerous fronts.
Following the clues from gene to potential Alzheimer’s prevention
APOE4 is a version of a gene that encodes a protein that helps the body transport and use certain fats and oils. Exploring the connection between metabolism and brain health drew Yassine to zero in on omega-3 fatty acids and their role in the brain’s self-maintenance system among those with APOE4 decades before the onset of clinical disease.
A 2017 imaging study of APOE4 carriers aged 35 showed that their brains were hungry for omega-3s. That change appears years before damage begins accumulating and decades before the typical onset of Alzheimer’s disease symptoms. In this difference, Yassine saw the potential for prevention and launched the PreventE4 trial to test whether starting omega-3s early in people with APOE4 can slow down disease progression.
Identifying APOE4 carriers showing subtle, early changes in their brain could yield new information about Alzheimer’s progression and — more importantly — inform interventions that lower risk.
So Yassine has teamed up with Kai Chen, PhD, associate professor of research radiology at the Keck School, to invent a new imaging technique that traces omega-3s in the brain. Bringing this probe forward from lab studies to human observation will be one major focus of the Center for Personalized Brain Health.
“We’ll be giving personalized advice, and we think that if we can start at 40 — instead of 60 or 65 — we’ll have a better chance at defeating Alzheimer’s disease.”
The center will also maintain a drug development program, with one promising lead currently under investigation. This search started with findings that the APOE4 dementia brain accelerates the breakdown of omega-3s in the brain, such that simply ingesting more doesn’t help.
Aiming to halt the breakdown process itself, Yassine teamed up with Vsevolod Katritch, PhD, associate professor of quantitative and computational biology and chemistry at USC Dornsife College and a member of the USC Michelson Center for Convergent Bioscience, to identify a new compound, called BRI-50054, that reversed omega-3 breakdown in lab studies.
Together with Stan Louie, PharmD, professor of clinical pharmacy at the USC Mann School of Pharmacy and Pharmaceutical Sciences, the team is planning to develop BRI-50054 into a drug for Alzheimer’s disease.
The Center for Personalized Brain Health brings together complementary expertise across USC schools to advance this compound and others in a pipeline of candidates for early medical intervention.
“It looks like we have to fix the wiring that’s destroying the omega-3s,” Yassine said, “and take action before it’s too late.”
In a third main element of activities at the Center for Personalized Brain Health, researchers will examine another possible early warning sign for Alzheimer’s disease in those with APOE4.
The same part of the brain that helps people navigate through the world, like internal GPS, is also the primary location stressed by being starved of omega-3 fatty acids. That detail suggests that detecting the deterioration of an APOE4 carrier’s ability to find their way around during middle-age might play into earlier diagnosis of Alzheimer’s.
Colleagues at the USC Viterbi School of Engineering and USC Schaeffer Center for Health Policy & Economics are contributing to a forthcoming Center for Personalized Brain Health project using sensors and wearable devices to spot a rise in navigation errors among people with APOE4 around the age of 50.
“There may be digital footprints that can tell us something is off,” Yassine said. “We want to see if we can capture those changes early and get information that will allow us to intervene.”
Feeding into all the above focus areas, the Center for Personalized Brain Health aims to build up a cohort of APOE4 carriers age 40 and above in the Los Angeles area.
This effort, dubbed USC GeneScreen, requires the completion of a short questionnaire and the return of a swab for testing to identify those with the gene. Ultimately, the Center for Personalized Brain Health aims to enlist 1,000 people with APOE4 to participate in research and, if they desire, receive personalized care from a dedicated clinic launching in 2024.
Depending on factors such as whether a person has one or two copies of the gene, recommendations could include a modified diet, regular exercise and avoiding activities that risk head trauma.
“People should know, if you’ve discovered you are an APOE4 carrier, you will have a place to go,” Yassine said. “We’ll be giving personalized advice, and we think that if we can start at 40 — instead of 60 or 65 — we’ll have a better chance at defeating Alzheimer’s disease.”
Source: USC
You can offer your link to a page which is relevant to the topic of this post.
#000#2024#acids#Administration#Advice#Aging news#Alzheimer's disease#amp#Biology#Biotechnology news#Brain#brains#Building#Capture#channel#chemistry#clinical research#Community#Computational biology#computer#Computer Science#dementia#details#detection#development#devices#diet#Disease#disease prevention#drug
0 notes
Text
Up to 73% of dementia cases can be prevented, new UK Bio Bank study shows

Getting dementia is the second biggest health fear, after cancer. But what can you do about it?
The conventional view is that genes play a big part and that factors under your control, including diet, lifestyle and your health status, account for up to 40% of risk. This means up to 40% of dementia cases could be prevented or delayed. Genes actually account for less than 1% of cases of Alzheimer’s. But a new study, based on following 344,000 people over 15 years from the UK BioBank estimate that “up to 73% of cases could be prevented” by targetting risk factors largely under your control.
The authors of the study, published in the Nature Human Behaviour journal, investigated 210 modifiable risk factors. They found that increasing hand grip strength, a good reflection of physical strength, increasing leisure or social activities or time spent in sports clubs or gyms, spending less time watching TV or on a computer, having better dental health, drinking more water, not dozing off in the day and sleeping between 7 to 9 hours a night, not smoking or being exposed to smoke and having better lung function were all associated with less risk.
Being unemployed, or having a low income, having diabetes, high blood pressure or having had a stroke or brain injury all increased risk. Inheriting the so-called ‘Alzheimer’s gene’ ApoE4 didn’t make any significant difference to overall risk.
However, even this figure of 73% may be an under-estimate as this study excluded blood test measures. “We have probably under-estimated the power of prevention.” says Professor David Smith from the University of Oxford, one of the study authors. “Even this figure of up to 73% of cases preventable could be higher if a person’s omega-3 and B vitamin status, measured, by a blood test for homocysteine that any GP can do, were taken into account.”
While the BioBank study didn’t include blood test measures of either homocysteine or omega-3, scientists at the US National Institutes of Health have attributed 22% of the risk of Alzheimer’s to raised blood homocysteine and 22% to a lack of omega-3.
“These have been shown to predict risk but were beyond the scope of this study.” confirmed the study author, Professor Jin-Tai Yu from Shanghai’s Fudan University. “Homocysteine-lowering treatment with B vitamins, especially B12, is one of the most promising interventions for dementia prevention.”
Professor Smith’s group at Oxford University have tested the effects of giving B vitamins (B6, B12, folate) versus placebo to those with pre-dementia and found that the 10p a day supplements halved the rate of brain shrinkage in one year and a virtually stopped further memory loss.
“The greatest effect we found in our trial was in those in the top third of DHA for the blood level of DHA (an omega-3), found in fish. Those with high DHA given B vitamins reduced their rate of brain shrinkage by 73%, down to the level normally seen in older people with loss of cognitive function. They also had virtually no further memory loss and almost a third ended the trial with no clinical dementia rating at all.”
The benefit of omega-3 was also confirmed in a major study this year of over 100,000 people, finding that increased omega-3 cut risk of dementia or cognitive decline by around 20%. An increase in intake of omega-3 DHA of 200mg, which is what is found in either a serving of fish or a fish oil supplement, decreased risk by almost a fifth.
One charity taking prevention seriously is the charity Food for the Brain. They offer, at foodforthebrain.org, a free online Cognitive Function Test, which includes a Dementia Risk Index questionnaire assessing your diet, omega-3 and B vitamin status, and lifestyle and an optional home-test kit for pin prick blood tests.
“Over 400,000 people have taken our validated Cognitive Function Test, which not only shows a person their cognitive status right now, but also their future risk based on our Dementia Risk Index questionnaire, what’s driving future risk and what they can easily do right now to lower it. If all modifiable risk factors are taken into account, including B vitamins and omega-3, it is highly likely a person could reduce risk by over 80%.” says their CEO, Patrick Holford.
“The government has pledged £160 million a year for dementia prevention research but we are not seeing any of this going into easy prevention wins. Most seems to be fuelling drug research for an apparent ‘cure’. Alzheimer’s is preventable, but not curable. You cannot reverse holes in the brain. With over 200,000 people diagnosed every year with dementia, if prevention were taken seriously, we could halve the number of people developing this terrible, but preventable disease.”
ABOUT FOOD FOR THE BRAIN FOUNDATION
The Food for the Brain Foundation (foodforthebrain.org) is an educational and research charity, focussing on dementia prevention. It’s free online validated Cognitive Function Test, followed by the Dementia Risk Index questionnaire assessing eight drivers of dementia, including ‘brain fats’ and ‘low carbs & GL’ thus identifying those eating too many carbs and not enough brain fats, then advising them what to do. www.foodforthebrain.org
Sources:
Zhang, Y., et al. Nature Human Behaviour. 2023 7, 1185–1195
Beydoun MA., et al. BMC Public Health. 2014 Jun 24;14:643.
Jernerén F., et al. Am J Clin Nutr. 2015 Jul;102(1):215-21.
Oulhaj A., et al. J Alzheimers Dis. 2016;50(2):547-57.
Wei B., et al. Am J Clin Nutr 2023 Jun;117(6):1096-1109.
Read the full article
0 notes
Text
New Scientist: Rare mutation hints gene editing could prevent Alzheimer's disease
0 notes
Text
Chris Hemsworth Reacts To Claims Of Retirement After Alzheimer's Scare
Hollywood star Chris Hemsworth recently explained how the reports of him having an Alzheimer's predisposition was 'overdramatised' and blown out of proportion.
Last year, Hollywood actor Chris Hemsworth revealed that he had received a diagnosis regarding a predisposition to Alzheimer's disease. This revelation occurred during his docu-series, titled Limitless, in which he underwent gene testing. However, Hemsworth has recently clarified that the reports surrounding his initial diagnosis were exaggerated and sensationalised.
Chris Hemsworth was diagnosed with having two copies of the gene APOE4.
The gene makes him ten times more likely to develop Alzheimer’s.
Hemsworth’s grandfather also suffers from the disease.
Chris Hemsworth calls media coverage of his diagnosis ‘overdramatised’
The Avengers actor spoke with Entertainment Weekly and discussed his initial reaction of being diagnosed. His experience was humbling, as he said at the moment ‘Oh wow, none of us are invincible.’ The Extraction star added that he realised he needed to ‘slow down and just experience this moment now,’ before letting the years pass him by. He added that the claims of his retirement were ‘overdramatised’.
The Thor actor explained that he was taking time off because he was exhausted after doing back-to-back projects. He added that his break was also due to his Alzheimer’s diagnosis. However, Hemsworth said, that it led to the two headlines being combined and causing rumours of his retirement due to the condition.
The Thor: Ragnarok star said that he wants to prioritize his family over work as he gets older. He told the outlet, “My kids are in school, and they’re of the age where it’s not as easy to upheave their life and travel across the world." Hemsworth is married to Fast Five star Elsa Pataky and is father to an 11-year-old daughter India and two twin 9-year-old sons Sasha and Tristan.
For More latest entertainment news only on www.republicworld.com
Republic World is a dynamic and most trusted source of news and information, founded by journalist and entrepreneur Arnab Goswami. We cater live and in-depth coverage of comprehensive news headlines and articles, covering a wide range of topics including India news, entertainment news, sports news and much more. Republic World features breaking news in India, current news headlines, India news live and today’s India News.
0 notes
Text
another look at the oils theory, this time from the gene side. very promising!
0 notes
Text
Gary Null’s Show Notes
03 22 23 P
If you listen to Gary’s show, you know that he begins with the latest findings in natural approaches to health and nutrition. Starting this week, we will make some of those findings available each weekday to subscribers to the Gary Null Newsletter.
People who use vitamin D supplements have lower dementia risk
Study Reveals How Sleep Removes Toxic Waste from the Brain
Early-life stress can disrupt maturation of brain's reward circuits, promoting disordersGive a gift subscription
Share
People who use vitamin D supplements have lower dementia risk
University of Calgary (Canada), March 1 2023.
A large study reported in Alzheimer's & Dementia: Diagnosis, Assessment & Disease Monitoring found a lower risk of developing dementia among men and women who consumed vitamin D supplements.
“Preventing dementia or even delaying its onset is vitally important given the growing numbers of people affected,” noted coauthor Byron Creese.
The study included 12,388 individuals whose age averaged 71 years when enrolling in the US National Alzheimer's Coordinating Center. Participants were free of dementia upon enrollment and had at least one follow-up visit. Medication forms completed at the beginning of the study provided information on vitamin D supplementation.
During a 10-year period, 2,696 men and women developed dementia. Women were at greater risk of developing dementia than men. Supplementing with vitamin D2, vitamin D3 or calcium with vitamin D was associated with a 40% lower risk of dementia compared with no supplementation. All three types of vitamin D were associated with a reduction in the rate of dementia incidence. Vitamin D was also associated with significantly greater 5-year dementia-free survival compared with no vitamin D.
Supplementing with the vitamin was associated with greater benefits among women compared with men, people with normal cognition at the beginning of the study compared with those who had mild cognitive impairment and among noncarriers of the APOE4 gene, which increases the risk of Alzheimer disease.
“We know that vitamin D has some effects in the brain that could have implications for reducing dementia, however so far, research has yielded conflicting results,” commented lead researcher Zahinoor Ismail, MD. “Our findings give key insights into groups who might be specifically targeted for vitamin D supplementation. Overall, we found evidence to suggest that earlier supplementation might be particularly beneficial, before the onset of cognitive decline.”
Study Reveals How Sleep Removes Toxic Waste from the Brain
University of Rochester Medical Center, February 20, 2023
Although we don’t know exactly why, there is no question that sleep is crucial for brain and overall health. Without proper sleep, the chance of disease and stress increases notably. Now, researchers at the University of Rochester Medical Center (URMC) Center for Translational Neuromedicine have found that sleeping actually helps detoxify the brain, potentially offering clues into dementia and Alzheimer’s disease.
The study, published in the journal Science, reveals that your brain has a unique method of removing toxic waste through ‘the glymphatic system’. Even more interesting, it seems that brain cells shrink by about 60% during sleep, allowing for waste to be removed more easily.
“Sleep changes the cellular structure of the brain,” said Maiken Nedergaard, co-author of the study. “It appears to be a completely different state.”
The research looked at something called the glymphatic system of the brain. Injecting dye into the brains of mice, they watched the flow of cerebrospinal fluid (CSF) and found that the CSF flowed rapidly when the mice were unconscious (whether asleep or sedated) and barely moved when the mice were awake.
“We were surprised by how little flow there was into the brain when the mice were awake,” said Nedergaard. “It suggested that the space between brain cells changed greatly between conscious and unconscious states.”
Then, they measured the space between brain cells to test their theory. Using electrodes inserted into the brain, they found the space between these cells grew by 60% during sleep, allowing the CSF to flow more freely.
The research is exciting for a variety of reasons. But perhaps most interesting of all is how the CSF affects the brain. The researchers found mice injected with beta-amyloid, a protein associated with Alzheimer’s disease, were able to detox the protein while sleeping. In other words, the CSF actually cleared the brain of the toxin. .
“These results may have broad implications for multiple neurological disorders,” said Jim Koenig, Ph.D. “This means the cells regulating the glymphatic system may be new targets for treating a range of disorders.”
“This study shows that the brain has different functional states when asleep and when awake,” said Nedergaard. “In fact, the restorative nature of sleep appears to be the result of the active clearance of the by-products of neural activity that accumulate during wakefulness.”
Early-life stress can disrupt maturation of brain's reward circuits, promoting disorders
University of California, Irvine, February 27, 2023
A new brain connection discovered by University of California, Irvine researchers can explain how early-life stress and adversity trigger disrupted operation of the brain's reward circuit, offering a new therapeutic target for treating mental illness. Impaired function of this circuit is thought to underlie several major disorders, such as depression, substance abuse and excessive risk-taking.
In an article recently published online in Nature Communications, Dr. Tallie Z. Baram, senior author and UCI Donald Bren Professor and Distinguished Professor in the Departments of Anatomy & Neurobiology, Pediatrics, Neurology and Physiology & Biophysics, and Matt Birnie, lead author, describe the cellular changes in the brain's circuitry caused by exposure to adversity during childhood.
"We know that early-life stress impacts the brain, but until now, we didn't know how," Baram said. "Our team focused on identifying potentially stress-sensitive brain pathways. We discovered a new pathway within the reward circuit that expresses a molecule called corticotropin-releasing hormone that controls our responses to stress. We found that adverse experiences cause this brain pathway to be overactive."
"These changes to the pathway disrupt reward behaviors, reducing pleasure and motivation for fun, food and sex cues in mice," she said. "In humans, such behavioral changes, called 'anhedonia,' are associated with emotional disorders. Importantly, we discovered that when we silence this pathway using modern technology, we restore the brain's normal reward behaviors."
The study involved two groups of male and female mice. One was exposed to adversity early in life by living for a week in cages with limited bedding and nesting material, and the other was reared in typical cages. As adults, the early adversity-experiencing male mice had little interest in sweet foods or sex cues compared to typically reared mice. In contrast, adversity-experiencing females craved rich, sweet food. Inhibiting the pathway restored normal reward behaviors in males, yet it had no effect in females.
"We believe that our findings provide breakthrough insights into the impact of early-life adversity on brain development and specifically on control of reward behaviors that underlie many emotional disorders. Our discovery of the previously unknown circuit function of the basolateral amygdala-nucleus accumbens brain pathway deepens our understanding of this complex mechanism and identifies a significant new therapeutic target," Baram said.
About Gary Null
An internationally renowned expert in the field of health and nutrition, Gary Null, Ph.D is the author of over 70 best-selling books on healthy living and the director of over 100 critically acclaimed full-feature documentary films on natural health, self-empowerment and the environment. He is the host of ‘The Progressive Commentary Hour” and “The Gary Null Show”, the country’s longest running nationally syndicated health radio talk show which can be heard daily on here on the Progressive Radio Network.
Throughout his career, Gary Null has made hundreds of radio and television broadcasts throughout the country as an environmentalist, consumer advocate, investigative reporter and nutrition educator. More than 28 different Gary Null television specials have appeared on PBS stations throughout the nation, inspiring and motivating millions of viewers. He originated and completed more than one hundred major investigations on health issues resulting in the use of material by 20/20 and 60 Minutes. Dr. Null started this network to provide his followers with a media outlet for health and advocacy. For more of Dr. Null’s Work visit the Gary Null’s Work Section or Blog.GaryNull.com In addition to the Progressive Radio Network, Dr. Null has a full line of all-natural home and healthcare products that can be purchased at his Online Store.
Find articles, videos, back radio broadcasts, books, and more at GaryNull.com.
https://garynull.com
Find Gary's vitamins and other supplements at Gary's Vitamin Closet.
https://www.garysvitamincloset.com
Hear Gary's radio show weekdays at noon Eastern Time on PRN.live
Disclaimer
While we have thoroughly researched the information we provide, and indicate its sources, information in this Gary Null Newsletter, and all Gary Null Newsletters, is for educational and informational purposes only, and is not intended to diagnose, treat, cure or prevent any disease or other condition. Consult your medical professional before choosing any treatment or course of action. Gary Null Newsletters are not liable for risks or issues associated with using or acting upon the information it provides.
Let us know what you would like to see in Gary's newsletter. Email us at [email protected]
If you are not subscribed, go to: https://garynull.substack.com to subscribe.
0 notes
Text
Study reveals that much still not known about cognitive decline
Researchers found that the factors most commonly associated with cognitive functioning — including socioeconomic status, education and race — explained only 38% of the variation in functioning among Americans at age 54.
Health behaviors such as avoiding obesity and smoking and participating in vigorous exercise had only very small effects on functioning by the time people reached their mid-50s.
In addition, the factors studied explained only 5.6% of the variation in how quickly cognitive functioning declined in people between age 54 and 85.
“There’s still a lot we don’t know about why cognitive functioning varies so much between older adults,” said Hui Zheng, lead author of the study and professor of sociology at The Ohio State University.
“More research is urgently needed to discover the main causes of how quickly cognitive functioning declines and how we can slow down its progression.”
Zheng conducted the study with Kathleen Cagney, professor of sociology at the University of Michigan, and Yoonyoung Choi, a graduate student at Ohio State. Their study was published today (Feb 8, 2023) in the journal PLOS ONE.
Data came from 7,068 participants in the 1996-2016 Health and Retirement Study. Participants were born between 1931 and 1941. Researchers measured their cognitive functioning at age 54 and how it declined until they were 85.
The study provides a more robust analysis than prior studies because it used a large, nationally representative sample and followed participants for decades, using a broad range of possible predictors of cognitive functioning, Zheng said.
The most important predictor of cognitive functioning at age 54 was education, which explained about 25% of the difference between people, results showed. That was followed by race, household wealth and income, parental education, occupation and depression.
The contributions of chronic diseases, health behaviors, gender, marital status and religion were rather small — less than 5%.
The researchers found that the variation in cognitive functioning at age 54 was three times as much as the variation in how quickly the participants declined over the next 30 years.
“We found that the rate of cognitive decline was much more similar between participants than the baseline of cognitive functioning we found at age 54,” Zheng said.
Overall, all the factors examined in this study only explained 5.6% of variation in the decline of cognitive functioning with age.
“From an intervention perspective, that suggests it is much more important to try to improve functioning at the baseline than trying to slow down the rate of decline.”
Zheng said one particularly interesting finding was that the number of years of education was not associated with the rate of decline in functioning after the age of 54, but having a college degree did have a small protective effect, which explained 1.7% of the variation in the decline with age.
The value of a college degree supports the “cognitive reserve” hypothesis that, in some people, their brains have the ability to find alternative ways to solve problems and cope with challenges when they have some type of damage to the brain.
“College may provide an especially rich environment for cognitive development that may help people develop this cognitive reserve,” Zheng said.
One explanation for declines in cognitive functioning that this study could not account for is a genetic factor — the APOE4 gene. That gene has been found to increase the risk of developing dementia, including Alzheimer’s disease.
But other studies show that dementia, including Alzheimer’s disease, accounts for only 41% of cognitive decline among the elderly.
“Cognitive decline is pervasive in older adults, even those without dementia, which is why it is important to study other predictors of cognitive functioning and decline,” Zheng said.
“But still, our study raises more questions than it answers. We have a long way to go to understand the trajectories of cognitive functioning in older adults.”
0 notes
Text
A Healthy Lifestyle Might Delay Memory Decline in Older Adults
Feb. 2, 2023 — A new study suggests that following a healthy lifestyle is linked to slower memory decline in older adults, even in people with the apolipoprotein E4 (APOE4) gene, one of the strongest known risk factors for Alzheimer’s disease and related dementias.
A team of investigators in China analyzed 10-year data on over 29,000 older adults with an average age of 72 years. Of these, a fifth…
View On WordPress
#Alzheimer’s about#Alzheimer’s causes#alzheimer’s disease#Alzheimer’s gene#Alzheimer’s prevention#Alzheimer’s research#Alzheimer’s study#dementia#dementia vs Alzheimer’s#how to prevent Alzheimer’s#memory decline#memory decline older adults
0 notes