#Dysplastic
Text
Health update.
I know I keep vanishing and then coming back randomly but trust me it's not because I don't want to be here, it's because of everything I have going on right now. Finding the time or energy is really fucking hard right now. I do lurk in the back ground and I am still working on finishing the pic spams...but again...I have so much going on now that it's unreal.
I work two jobs. Me and my partner bought our first home a year ago. We are a couple months closer to move in but its just been such a long and stressful journey to get this far. I'm working two jobs so we can afford to do the things we want now in terms of fixing it up so we don't have to ever do it again. I am a high school teacher during the week and a worker in an Autisic Centre of the weekends and school holidays.
As some of you may know, 8 years ago I suddenly was unable to walk properly due to pain in my hips. After xrays, they found I have Dysplasia in both my hips which caused arthritis in both. So I was thrown into the world of being disabled as I couldn't walk properly and I was in so much pain. 2 years later, after many attempts to save both hips, I had total hip replacement of the right hip. 6 months later I had a total hip replacement of the left hip. Recovery was awful. Months later I started suffering with pain in multiple joints. My knees would give way. My ankles would swell. My left sholder was very painful when moving it and would lock quite a bit. Going to the doctors to speak about this would result in me being told that it's just pain from the hips travelling down to my joints and up my back.
So I carried on. I had to. I didn't have another choice. Couple of months later, couple of ER/A&E trips, I got sent to a rheumatology consultant. He did a blood draw and said that I had no sign of an autoimmune problem so it must be Fybromyalgia. Now. I do believe I have Fybromyalgia. I have the emotional trauma from growing up with an abusive, alcoholic & gambling addict dad. Developed eating disorder from the age of 18...and I've had the physical trauma of the back to back surgery's. So it's fits. All the symptoms fit.
However, with my family's history of arthritis at very young ages (my mum needed them at 20, my auntie needed them at 23, my nan needed them in her 20s and I needed them at 21). Most of those woman have arthritis in a lot of other joints to. So I needed to push for further investigation.
My left hip replacement hasn't felt good at all since it was done. It is that bad that I actively call it my "bad hip". And tell people we don't celebrate that hips birthday. The pain has gotten much much MUCH worse. If I stand for more than 30 seconds on that hip, I get stuck. I can be taken out of action for days if I do too much activity because of the pain. I take 80mg of slow release morphine every day and other pain killers. That doesn't help much at all.
So, I asked my rheumatologist to please xray the hip replacements and please xray my sholder as it was getting worse. Its hard when you get a diagnosis of fibromyalgia because doctors like to see that and not look any further then you are complaining of joint pain. It's very hard.
I got the xrays.
Sholder: he rang me with the results. His statement was that I have Dysplasia in my sholder. The joints don't fit properly which is what is causing the pain. He also stated that this hasn't changed since the last xray I had done when it was originally flagged....excuse me? I was so confused. Eventually I remembered that during my second hip replacement, the hospital suspected a post op blood clot in my lungs, so they did a chest xray. When this xray was done, there was a red flag on it that said I had Dysplasia of the sholder. That was 5 years ago. No one said a word to me. It wasn't in my notes. When I say I was so angry, I was soooooo angry. But at least I had an answer other than "oh you have fibro, that's what's causing the pain." Since then, no one has been in touch about a treatment plan etc. That will be my next issue to fight for I guess.
The Hip: the replacements looked fine. They were not loose. Which is brilliant! However, I had extreme pain from it. So I was referred to a hip specialist. This guy was the guy who did all of mu family hip replacements so it was nice to be under him if there was a problem with my replacement. I went to see him 2 weeks ago. He sent me for a CT on my pelvis. He agreed that there was no issue with the hip other than nerve pain which isn't really worth opening back up again due to the risk of infection and the fact that I will need new hips in 10 years anyway. So, Great. Nothing wrong with the hips. I'll just have to get on with the nerve pain. He told me he had bad news though. He pulled up my CT scan and showed me that I had arthritis in sacratic joint on the left side. That is what is causing me the intense pain. That is what is causing me to get stuck in certain positions. All he can offer me for that first is injections into the joint and physical therapy. He told me that it's going to be a long journey with a lot of work.
When I say I sobbed. I sobbed. Another fucking thing that is wrong with my body. I feel like I am just broken. I find it hard to put into words how all this makes me feel but tbh nothing was as bad as it was when I got a letter through the door from the same doctor.
He mentioned everything he said in the appointment about the joint issue on the left side. But he also had taken another look at my scans and he said there is degenerative changes in my lumbar spine. Arthritis in the bottom half of my spine. What do I do with that? I was in work when I read that and honestly I did my best to keep it together but I couldn't do it. I just cried my eyes out. I think reading his words, "Elisha knows that this is something she will have to deal with for many years and it is not going to go away." I am honestly broken. I don't know why this is happening. I don't get how I've gone from where I was before I turned 21, perfectly healthy other than the eating disorder, to being 30 with arthritis in the bottom half of my spine, arthritis in my joint that connects the pelvis to the spine, 2 hip replacements & a Dysplastic sholder. I honestly feel like I should ask for a whole body scan just to get it out of the way. Just find out everything.
What also has freaked me out is that he said I have myelitis in my spine. If you do your research you will understand why this has freaked me the fucked out.
I do my best to keep it together because I know there are people with a much worse medical history but I am just broken. I am always in pain. But I'm trying to keep going. I worked to hard to give up and become bed bound, but I know there will come a time when this won't be something I can stop.
I had to get this off my chest as I am sure my partner is sick of hearing it as he's living with it daily while being with me. And I know it upsets my mum, she feels guilty for some reason.
But yeah, that's the update. This is why I go missing but school holidays is when I can come back more often
#arthritis#fibromyalgia#hip replacement#spoonie#spoon#spooneys#disabled#pain#Myelitis#Dysplastic#dysplasia#health
9 notes
·
View notes
Note
what advice would you give to a trans person who is terrified of getting health checks such as pap smears? I'm generally rather touch-averse and that doubled with the dysphoria makes it very scary to think about.
Hi Anon,
This is a topic close to my heart, because I myself am touch-averse and have a trauma response to pelvic examinations. I also want to make sure everyone understands why it's important to get pap smears!
Let's start with what pap smears are, why they're important, and who they are for. Maybe understanding that will be the first step in finding the strength and courage to go through with them.
QUICK ANATOMY & PHYSIOLOGY LESSON - THE PAP SMEAR
What is a pap smear for?
Your cervix is the gateway to your uterus, sitting atop the vagina. It's a thick ring of muscle that is normally closed, opening just a tiny bit for menses to escape (the sensation of the muscle opening is what causes cramps).
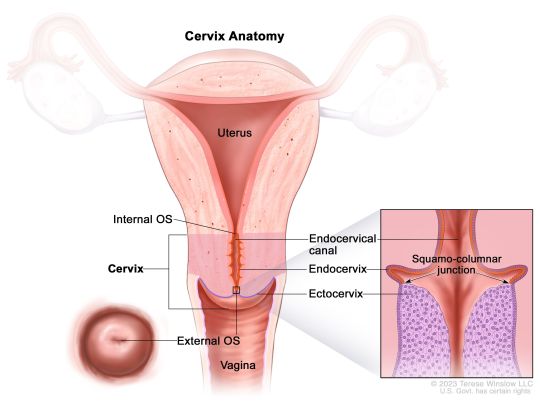
Now, the trouble comes when cervical cells have been infected with a virus called human papillomavirus (or HPV) - especially certain "high-risk" strains. HPV is very common in the human population - almost everyone sexually active has had it at some time, with about 50% of infections being a high-risk type. Most people just clear the virus themselves and never even know. But sometimes, this viral infection will start a process of dysplasia (basically growing weird cells), which can be the start of cervical cancer.
The job of a pap smear is to check the cervical cells for dysplastic changes that indicate things might progress towards cancer, or for the virus itself. (What it looks for specifically depends on your age and previous results, but the process is the same for you). When lesions are found early, they are VERY easily treatable. The pap smear saves thousands of lives every year by preventing cervical cancers.
How is a pap smear performed?
A device called a speculum will need to be inserted into your vagina to hold open the walls of the vagina and allow the provider to visualize the cervix. Once this is in place, a soft brush-like device is passed up through the vagina, pressed against the cervix, and swirled around several times to collect cells. This may feel weird or uncomfortable, but shouldn't cause pain. Most people don't feel it at all, the speculum being the worst part. The whole thing takes about one minute.
Separate from the pap smear, the provider may also perform a bimanual exam, which is when they insert fingers from one hand into the vagina while pressing down on the abdomen, to look for masses, abnormalities or tenderness.

Who needs a pap smear?
CURRENTLY (as of 2023), everyone with an intact cervix who is 21 or older is recommended to get pap smears, regardless of gender identity, sexual orientation, or sexual history. Between ages 21-29, you should go every 3 years, and after age 30, every 5 years (depending on results - if you get a positive, you would need more frequent observation).
If you are older than 21 and have never had any kind of sexual contact with anyone at all (including hands, mouths, or sharing toys!), you can discuss with your provider to see if a modified schedule may make sense based on your risk level.
Note: The HPV vaccine may change these recommendations in the future! I strongly recommend getting the vaccine if you have not already!
---
OK, Anon. With that public service announcement out of the way, let's talk about the real meat of your question.
The best thing I can recommend is to take the time to find a provider you vibe with. Someone with whom you feel safe, with whom you have mutual respect. See if your local LGTBQIA+ support group has recommendations, or if any clinics in your area have providers that specialize in LGTBQIA+ or trauma-informed care. Call and ask providers questions about how they handle people who struggle with pelvic exams. Generally, avoid crusty old men.
A good provider will warn you before ever touching any part of your body, go slowly, and ask permission each time, and stop the second you tense up. A GREAT provider will make you feel in control the whole time - they may let you insert the speculum yourself and not make you use stirrups if they're triggering for you. Medical consent is the same as sexual consent - just because you're disrobed in that room doesn't mean you need to let anyone touch you. You do not have to undergo a pap smear with a provider you don't trust. You are allowed to walk away.
Other things to try:
You can ask for a short-acting anti-anxiety medicine, like Xanax, to take before the visit, provided you've got a ride.
You can bring a companion, or ask for a nurse to hold your hand.
Chat nonstop, tell stupid jokes, or listen to music on headphones, whatever kind of distraction works best for you.
Meditate, practice belly breathing, really focus on full body relaxation, especially of the pelvic muscles
Remind yourself that it's one minute every few years for the piece of mind that you won't get cancer.
Be open to the possibility that it won't be as bad as you're fearing.
Know that you are brave and strong. You can do hard things. You can do anything for one minute.
If any other trans folx out there want to share tips with Anon for how to navigate gynecologic exams, please share!
#reproductive health#sex education#midwifery#gynecologic care#pap smear#pelvic exams#gender affirming care#lgtbqia+#transgender#trans health care
11 notes
·
View notes
Text
Me: "So if say, an arm, doesn't fully form, it's dysplastic. If on the other hand it was a formed arm, but then gets somehow removed, that's not dysplasia,
Wife: "It's displaced"
Me: "I mean. Yes"
3 notes
·
View notes
Note
First off, as someone with an injured hip, I would not want this for a dog. It fucking sucks man. I should eventually be healed, but inflicting this upon a dog for the rest of its life? With no relief? It’s fucking cruel. No thanks.
Second, a lot of people don’t seem to understand that working crosses are relatively common (at least in my area) various gun dogs are crossed often based on the merits of their parents. Same with the various herding breed mixes that are common here. The key tho is that the parents are proven and that they are kept within their job type
Same- my dad has the human version of hip dysplasia and a few years ago got a total hip replacement and he said realizing now his chronic "back pain" was coming from his bad hips he would never have made Mocha, our dysplastic dog, suffer for as long as she did with it.
[ironically, he fell a few weeks ago and started complaining of back pain again this time too painful to walk, and when he eventually went to the doctor about it discovered he'd BROKEN a hip]
I will never agree to breeding a dog with any sort of joint dysplasia.
And, same here, in PA there's a lot of herdy hunty dogs who are basically 🤷♂️ hunts good 🤷♂️ and 🤷♂️ herds good 🤷♂️ as far as breed goes. I wish they had more health testing but the dogs do work, sometimes better than their purebred variants. Working crosses are great! They just have to, you know, actually fucking work and not be "well it's x breed so it's good at y work :)"
35 notes
·
View notes
Note

it’s been a hot minute since I sent a Carlos pic, so here’s the trash man himself! We finally got his seizure meds figured out, but he recently had X-rays for a suspected urinary block (ended up being just a bad uti…again) and the X-rays revealed he has hip dysplasia and at some point was presumably hit by a car and broke his pelvis! He currently has absolutely no pain from either, but eventually he’ll probably end up on pain management meds. I’m starting to think somewhere there’s some deity that keeps trying to take Carlos out but he’s just too strong 🤣
Wow I’ve never seen a cat with hip dysplasia! Cats truly are so incredibly tough. Carlos is a legend. He and Harold can be arthritic, dysplastic buddies together
52 notes
·
View notes
Note
What ARE the chances they use Bobby or a close relative to him?
The chances they use Bobby are a definite 0, because Bobby's been dead for three years 😂
Close relatives are also unlikely - he only sired one litter (Poppy's) and though one of the females from that litter has been bred, hip scores hover in the mildly dysplastic range. That won't be an immediate elimination in Farmdog Land, but it's not what you pick to improve your breed either. Bobby's sire was only used once. He did have a litter sister whose grandbabies are still appearing so there's a vague chance there, but overall Bobs was a little dog from little lines.
His dam died tragically after her 2nd litter, and that's the real reason why *I* don't think Bobby, Poppy, or close relatives should've been used for a Cavalier outcross. I never knew Shanty, but I can tell you that the temperament that causes a dog to play so hard it falls and breaks its neck, that lives on and breeds true.
#i can agree that the cavs ive known couldve needed some more motor#but theres a difference between a paddleboat#and being shot out of a cannon
16 notes
·
View notes
Text
🎤 "We're breaking free" 🎶
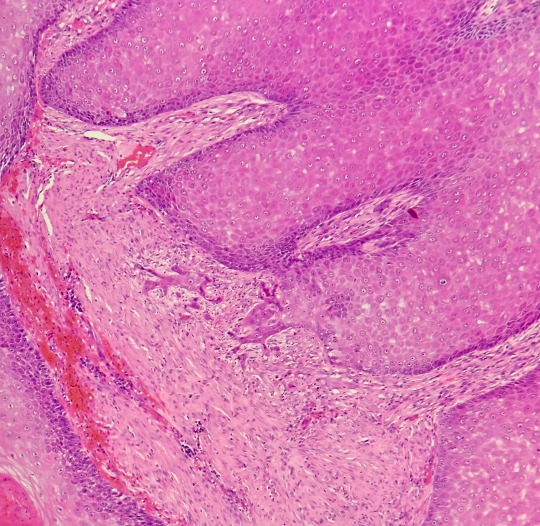
Recently I was lucky to see the exact point where a squamous cell carcinoma had broken through the basement membrane of the skin! This is what we look for to differentiate squamous cell carcinoma from a carcinoma in situ or dysplastic epithelium, where the changes are confined to the epidermis and dont break through.
11 notes
·
View notes
Text
Rhonda Rollinson (USA 1992)
Rhonda Rollinson went to Philadelphia Women’s Center on September 3, 1992. She had an attempted abortion by Jay Levin, but was told that it was “unsuccessful” and to come back for another try on September 12. It is not stated whether or not her baby survived the original attempt, but based on Rhonda’s condition just a few days later, most likely her baby had been killed and left to decompose inside of her.
Rhonda was in excruciating pain soon. She had a fever and was overwhelmed with dizziness. There was discharge that indicated a severe health problem. On September 10, she went to the hospital. Despite the best efforts at the hospital and multiple emergency surgeries, Rhonda died on September 14.
Her autopsy detected a perforation all the way from her vagina into the uterine cavity, lung infarction (when an artery to the lung becomes blocked and part of the lung dies), DIC (disseminated intravascular coagulopathy), non-bacterial thrombotic endocarditis, pulmonary infarctions, dysplastic kidney and sepsis. Rhonda hadn’t stood a chance.
A lawsuit by Rhonda’s family charged the facility and its owner with hiring Levin despite his lack of competence, failure to properly supervise his work, violation of applicable laws and regulations, lack of informed consent, failure to give proper post-operative instructions, and failure “to respond to the requests of [Rhonda] and her family for post-operative medical advice.”
Rhonda and her baby both died a terrible and completely needless death.
Philadelphia County Court of Common Pleas Case No. 291, 1994
#pro life#tw abortion#unsafe yet legal#victims of roe#tw ab*rtion#tw murder#abortion#abortion debate#death from legal abortion
4 notes
·
View notes
Text

Hips: excellent, good, fair, borderline, mild, moderate, severe
Elbows: NORMAL / DYSPLASTIC
Her spine, heart & an old wrist injury were all evaluated by the vet and X-rayed. He said everything looks great and she is clear to start conditioning & training for mobility!
#belgian malinois#2 years#24 months#service dog in training#mobility service dog#service dog milestone#OFA#health testing#mobility tasks#service dog community
38 notes
·
View notes
Text
Adenomas are polyps that have malignant potential and require early surveillance colonoscopy.15 They are classified by their glandular histology and level of dysplasia, which determine their malignant potential and interval for repeat colonoscopy. Tubular adenomas (Figures 2 and 3) account for 80% of adenomas and have a malignant transformation rate at diagnosis of 4.8%. Tubulovillous and villous adenomas (Figure 4) are less common but have more malignant potential (19.0% for tubulovillous, 38.4% for villous).16 Although all adenomas are dysplastic, the degree of dysplasia is classified as low or high grade. High-grade dysplasia (Figure 5) suggests that the polyp is evolving toward malignancy. An adenoma that is 10 mm or larger, has villous elements, or has high-grade dysplasia, or the presence of three or more adenomas during a single examination, has a strong association with advanced neoplasia on future colonoscopies.
Sessile serrated polyps are thought to be the principal precursor of hypermethylated gene cancers; 20% to 30% of colorectal cancers can arise from this pathway.6 These polyps are often difficult to detect during colonoscopy because they can be flat and indiscrete, and have adherent mucus6,20 (Figures 6 and 7). All sessile serrated polyps require early follow-up colonoscopy; those that have cytologic dysplasia, are 10 mm or larger, or are located proximal to the sigmoid colon may be associated with a higher risk of developing cancer.6
Patients who have adenomas are more likely to have additional adenomas or colorectal cancer on subsequent examinations.6 Endoscopic follow-up of patients with adenomas is referred to as a surveillance colonoscopy. The presence of low- or high-risk adenomas determines the surveillance interval.
High-risk polyps include three to 10 tubular adenomas found during a single colonoscopy, at least one tubular adenoma or serrated polyp that is 10 mm or larger, at least one adenoma with villous features or high-grade dysplasia, a sessile serrated polyp with cytologic dysplasia, or a traditional serrated adenoma. Surveillance colonoscopy is recommended at three years for high-risk polyps.
2 notes
·
View notes
Text

In Baltimore County, MD: URGENT: Sweetest Pup Ever with Injury Seeking Rescue ASAP!
Pippo is urgently seeking rescue placement with a 501c3 rescue that can assist with her medical needs before she is ready for adoption. Pippo is as sweet as they come and despite the pain she was in when she came in, wouldn’t stop wagging her tail during her vet exam.
Name: Pippo
Age: 2 years
Gender: Female
Weight: 35 pounds
Breed: Pit Bull Terrier
Reason for Rescue: Medical transfer
Health Concerns: ear infection in both ears (treated), non-weight bearing lameness of the right hind leg, underweight BCS 3/9. Radiographs taken 3/27 (available upon request) of Pippo’s pelvis and right hind leg revealed a right-sided dysplastic hip and moth eaten appearance to the right-hip socket as well as the right upper femur. This appearance may be due to bony infection, inflammation or cancer. Antibiotics have been initiated to treat for possible infectious causes. Anti-inflammatory medications have been extended. Consultation with a veterinary orthopedist is recommended to determine the best course of action (health summary attached)
Behavior Concerns: No concerns at this time (behavior notes attached)
Intake Reason: Stray
Available for Adoption through BCAS: No
Available for Foster through BCAS: No
Thank you,
BCAS Rescue Team
Baltimore County Animal Services
13800 Manor Road
Baldwin, MD 21013
410-887-7297
**If you would like to foster Pippo, we can contact local rescues to ask for help, please email [email protected] (we are only a volunteer group that tries to help rescues help the dogs/cats of MD)
#dog rescue maryland#dog rescue#dog rescue baltimore maryland#doglover#dog adoption maryland#cute animals#fostering dogs#foster#foster family#foster dog#foster dogs baltimore
1 note
·
View note
Text
How Probably Will Moles Reappear After Being Removed?
Are you considering the removal of a mole? If so, you might be contemplating the likelihood of the mole returning after the removal process.
Although mole removal is often a permanent solution, there is a possibility for a mole to reappear and potentially grow larger following removal. Various factors, including the type of mole, its nature (benign or malignant), the excision method, your skin's healing process, and the surgeon's competence, all contribute to the likelihood of mole recurrence.
Moles: Types, Nature, and Causes of Growth
Moles, also known as nevi, are visible, well-defined, and persistent skin or mucosa lesions. These lesions can resemble other common skin issues like seborrheic keratosis, freckles, and skin tags. Moles are typically formed by melanocytes, pigment-producing cells responsible for skin and hair color. The development of moles is often influenced by exposure to sunlight, with lighter-skinned individuals being more prone to growing new moles after sun exposure, resulting in darker moles.
Most moles have defined borders and appear pink, brown, or tan in color. Common benign mole types include junctional melanocytic nevi, compound melanocytic nevi, and dermal melanocytic nevi. Atypical moles, or dysplastic nevi, have an irregular appearance, potentially leading to melanoma.
Changes in Moles Over Time
Moles can undergo changes over time due to factors such as hormonal shifts during pregnancy and exposure to sunlight. These changes may involve darkening or the emergence of new moles. It is essential to be vigilant about any alterations in the appearance of moles and seek prompt evaluation if dysplastic characteristics or other irregularities arise, as this may indicate the potential development of melanoma.
Methods for Mole Removal in Singapore
In Singapore, several methods are employed for mole removal. Surgical shaving involves the careful removal of the mole using a surgical blade, with the wound typically healing in 1-2 weeks. However, this method may carry a higher risk of recurrence. Surgical excision involves removing the entire skin section containing the mole, reducing the likelihood of regrowth but resulting in a visible scar. Laser mole removal singapore, favored for cosmetic reasons, utilizes precise bursts of light energy to break apart pigment or vaporize mole cells. While less invasive, laser removal may have a higher chance of mole recurrence compared to surgical excision.
Can a Mole Regenerate After Removal?
Complete removal of all mole cells generally prevents recurrence. Surgical excision offers a lower risk of regrowth, while shaving or laser removal may allow some mole cells to remain, increasing the chances of recurrence. Studies suggest recurrence rates ranging from 11% to 33% after shave excision. Laser mole removal has a lower recurrence risk than shaving but a higher risk than surgical excision, depending on factors like the type of laser used and the expertise of the physician.
Timing of Mole Regeneration After Removal
A mole typically grows back within the first six months after removal, with visibility depending on its depth in the skin layers.
Mole Regrowth in Scars
Scar tissue has poorer blood supply and healing capabilities than healthy tissue, making repeated mole removal within scars more likely to result in additional scarring. Opting for the removal technique with the least scarring potential is advisable.
What to Do After Mole Removal if A Mole Returns?
If a mole returns after removal, various factors determine its nature and risk. Consulting a skilled specialist is crucial to assess whether the recurring mole is benign or potentially malignant. Treating recurring moles as potential malignancies is advised if any uncertainty exists.
In conclusion, the likelihood of a mole returning after removal depends on multiple factors, and the choice of removal method plays a significant role. Surgical excision is considered the most effective, while laser removal offers a compromise between recurrence risk and scarring. If you have a persistent mole concern, seeking professional evaluation is essential for accurate diagnosis and appropriate management.
0 notes
Text
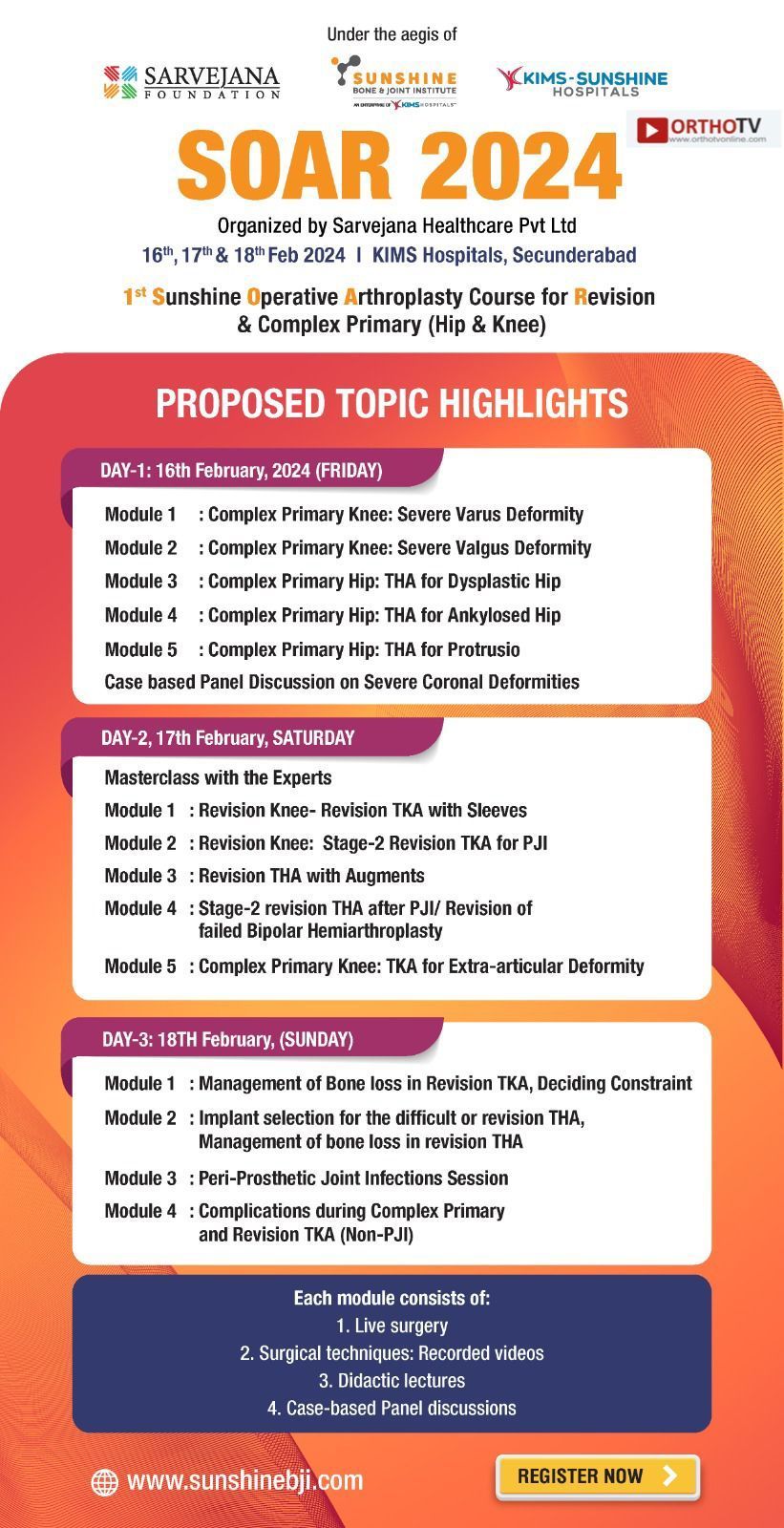
🎉 Sunshine Operative Arthroplasty Course for Revision & Complex Primary (Hip & Knee) 🎉
🗓️ DATES: 16th, 17th & 18th February 2024
📍 VENUE: KIMS Hospitals, Secunderabad
💻 Click here to register: https://tinyurl.com/OrthoTV-SOAR-2024
🆓 Registration Complimentary but Compulsory
🔰 PROPOSED TOPIC HIGHLIGHTS
🔸 DAY-1: 16th February, 2024 (FRIDAY)
Module 1 : Complex Primary Knee: Severe Varus Deformity
Module 2 : Complex Primary Knee: Severe Valgus Deformity
Module 3 : Complex Primary Hip: THA for Dysplastic Hip
Module 4 : Complex Primary Hip: THA for Ankylosed Hip
Module 5 : Complex Primary Hip: THA for Protrusio
Case based Panel Discussion on Severe Coronal Deformities
🔸 DAY-2, 17th February, SATURDAY
Masterclass with the Experts
Module 1 : Revision Knee- Revision TKA with Sleeves
Module 2 : Revision Knee: Stage-2 Revision TKA for PJI
Module 3 : Revision THA with Augments
Module 4 : Stage-2 revision THA after PJI/ Revision of failed Bipolar Hemiarthroplasty
Module 5 : Complex Primary Knee: TKA for Extra-articular Deformity
🔶 DAY-3: 18TH February, (SUNDAY)
Module 1 : Management of Bone loss in Revision TKA, Deciding Constraint
Module 2 : Implant selection for the difficult or revision THA,
Management of bone loss in revision THA
Module 3 : Peri-Prosthetic Joint Infections Session
Module 4 : Complications during Complex Primary and Revision TKA (Non-PJI)
‼️ Each module consists of:
1️⃣. Live surgery
2️⃣. Surgical techniques: Recorded videos
3️⃣. Didactic lectures
4️⃣. Case-based Panel discussions
🌟 Chief Patron: Dr. B. Bhaskar Rao
🌟 Organising Chairman: Dr. A.V. Gurava Reddy
📺 Media Partner: OrthoTV Global
▶️ Join OrthoTV: https://linktr.ee/OrthoTV
#SOAR2024#ArthroplastyCourse#OrthopedicSurgery#HipSurgery#KneeSurgery#MedicalEducation#OrthopedicTraining#HealthcareEvent#KIMSHospitals#Secunderabad#MedicalConference#SurgicalSkills#OrthopedicSurgeons
0 notes
Text


In a dobe outcross group, someone was discussing a *completely hypothetical* situation of keeping tissue from their rescue doberman who made it into his double digits to see if his genes could be valuable enough to study since people "don't want to outcross". The dog has hip dysplasia, which is why I mentioned that the dysplasia alone would tell me no, living to teens with hip dysplasia is not imo a good tradeoff, as someone who owned a dysplastic rescue dog.
One of the things mentioned a couple times was that his pedigree was completely unknown and that maybe that's why he lived so long, that bybs aren't inbreeding the way "good purebred" breeders are. Except... that's not the case at all. Nothing stops a byb from repeatedly breeding father to daughter, grandfather to granddaughter, uncle to niece, etc and in fact it seems to happen with nearly as much regularity as it happens in the "good purebred" world. My friend's dog is a rescue that she found half dead digging in the trash at her laundrimat and that dog's COI is MORE THAN DOUBLE what Creed's was, which was already very high at 35%. For the record, COI between siblings is 25%, and breed average for dobes is 40-50%. A dog with a 78% COI is from repeated close inbreedings and it does not matter that this dog is not purebred.
Could this singular long lived unknown background dog hold the key to figuring out doberman longevity? Maybe. But we also have individual dogs with known backgrounds living that long that threw DCM and deaths as early as 4 years old. Knowing the pedigree doesn't make a dog better, it just means you have traceable history. This particular dog lived to 12, that's wonderful! How about his siblings? His parents? Their siblings? Their parents? Not every dog that dies young from DCM throws others who do the same. I know someone who's foundation bitch died at 4 from DCM, and the puppies are all still alive at 7.5. So should we breed that progeny if they live into the double digits, or do we take caution knowing the dam died at auch a young age?
To me it is less that people don't like outcrossing within that particular group. It is more the attitude that blindly crossing to whatever and blindly breeding whatever dobes they can get their hands on to whatever other breed they can find and match with will somehow make things better. Between that and some complete temperament failures, it's not hard to see why so many who would otherwise be willing to donate dogs and semen to help are reluctant to even begin to consider it.
It's not "breed snobbery". It's "asking questions and wanting a plan before jumping all-in". It's "being hesitant to breed to an unknown dog with hip dysplasia [hypothetically]". It's "what you are looking to make is not a doberman and thus I am not interested". It's an outcross group. What people are looking for is not "keep dobes pure" but "can you give me an actual well thought plan to manage these future problems and combat these potential issues".
44 notes
·
View notes
Text
Just had wart or mole removal? Here’s what to do next

As technology finds easier and easier ways of achieving our aesthetic goals, more and more people are turning to companies like the Perfection Cosmetic Laser Clinic for help in removing those unwanted moles and skin blemishes. It’s now simpler and more painless than ever and many people get their blemishes removed in just one session.
But the simplicity of modern-day wart and mole removal doesn’t mean that the responsibility is completely out of the wart removal customer’s hands. Indeed, there are many things that customers can do to increase the effectiveness of their removal treatment. This blog will outline some of the best aftercare tips for wart, mole or skin tag removal customers and how a little aftercare can elevate your aesthetic results.
What Method Are You Using?
Whether a mole, wart or skin tag, removal for non-medically provoked removals can differ greatly in how invasive they are. A surgical removal of a large mole or wart will require more healing than a laser wart removal or mole removal. Freezing a wart or a mole is also less invasive, but can lead to scarring if you don’t adhere to aftercare guidelines.
Size Matters
The size and spacing of the target area will also have an effect on how long the aftercare procedure will be. It’s simple really, the larger the mole or wart is, the longer it will take to heal once it’s been removed. If you’re having several moles or warts taken care of in one sitting, the healing process will also take some time.
It’s worth remembering that a wound will clot within 24 hours, and within a week it will have started healing itself. It’s during that week that you can take measures to ensure that your skin does not visibly scar. The 24 hours clotting period also depends on the size of the wound.
Make Sure To Moisturizer
Keeping your skin moisturized will aid the healing process after a removal procedure. Skin needs the right atmosphere to heal properly, and moisture is key to keeping it nourished.
If Using Laser Therapy, Use Sun Cream

One thing that many wart removal UK customers can do to protect themselves, especially after laser treatment, is to use sun cream on the affected area. Sunlight can damage sensitive skin, and yours will be for around a week after a removal treatment by laser.
Smoking, Alcohol And Blood Thinning Medication
For the week after your procedure, try to avoid drinking too much, using tobacco and using blood thinning medication. Blood thinning medication will slow the rate of your blood clotting, whilst tobacco and alcohol will dehydrate your skin and rob it of the moisture it will need during the healing process.
Types of Moles
Let us have a look at different types of moles, which are as follows:
1. Congenital Birthmarks/Moles
Birthmarks are commonly used to describe congenital moles. They are present at birth or appear shortly after that.
2. Dysplastic Nevi and Atypical Moles
These have irregular textures, hues, and shapes. Atypical moles can occasionally develop into cancer. Our dermatologists advise inspecting your skin every month for any new changes.
3. Typical Moles and Acquired Moles
These are the common moles that can be seen almost everywhere on the skin. Ten to forty moles on the body are thought to be typical for humans.
Can You Prevent Moles?
You cannot alter your genetic propensity for mole formation, but you may take precautions to protect your current moles and prevent the growth of new ones. Always employ sun protection measures, such as wearing a broad-spectrum sunscreen, covering yourself with UV-protective clothes, and finding shade during the hottest parts of the day.
Mole Removal Options
You can treat moles using ultimate warts and moles removal treatment and achieve natural-looking results. With the aid of FDA-approved technologies and world-class professionals, our treatments follow the client’s needs, with safety and comfort being our top priorities. As a result, anticipate stunning outcomes after a few days of treatment.
Dermatologists warn against using DIY methods to remove moles. You risk complications by accidentally removing any lesion found on your skin, including moles. Before deciding on the specifics of mole removal, our experts frequently perform a biopsy of the mole for additional assessment. Our specialists conduct a microscopic examination of the biopsy specimen and provide a conclusive diagnosis.
What Is A Wart?
Warts are non-cancerous growths that appear when your skin is infected with (HPV) Human papillomavirus. The virus triggers extra cell growth, making the skin’s outer layer thick and hard. They take time to develop. A mole has pigment and hair, which gives it a distinctive appearance. Both do not exist in warts. Warts can spread from one person to another during contact, while moles cannot. Moles have a high chance of developing skin cancer because of their pigment.
Warts can appear on your hands, knees, feet, or any other area of your body. They are hard bumps deeply embedded in the skin, unlike moles. They may appear smooth on the outside, but they have calluses underneath.
Although normally painless, they can occasionally itch or hurt, and they can be humiliating and disfiguring (particularly on the feet). Additionally, warts often move from one bodily region to another and spread locally. Cutting, tearing, or picking at a wart is not advised.
Benefits of Warts and Moles Removal Treatment
Let us explore several benefits of the mole and wart removal treatment which are as follows:
Effective results: We use high-energy radio waves and low temperatures for wart removal treatment, which helps to offer desirable results. The burnt skin is shed within a week through the process of natural healing and medication offered by our specialists.
Practical outcome: A single session delivers desirable outcomes. It helps to remove 75% -100% of warts/ moles.
No scarring: The therapy helps to treat the specific areas of warts rather than affecting other healthy skin cells. It means the potential risk of scarring is less.
Safety: Our warts and moles removal treatment treats specific areas and delivers promising outcomes. Our treatment aims to remove them without scar issues.
Mole and Warts Removal: At Bangalore Dental solutions and Implant center
We remove Mole and warts using a pain-free laser which is a very popular procedure. The Laser used to remove moles is a low-intensity laser beam that simply burns the mole off the surface of the skin. After the treatment, the skin usually turns reddish or light Brown and then will scab over as any kind of burn will do. The scab should fall off within 4 to 7 days. Moles that are large and dark cannot be treated by laser as
Moles that are large and dark cannot be treated by laser as the laser does not travel deep into the skin whereas moles that you’ve had since birth or very early in life are usually suitable for laser mole removal.
Frequently Asked Questions
1. Is mole removal effective?
Yes, mole removal largely succeeds. Receiving such treatment won’t harm you because it has been tried and tested.
2. How long does recovery take after wart and mole removal?
It varies depending on the growth, but a minimum downtime of three days might be expected after treatment.
0 notes
Text
A Complete Guide for Veterinarians on Black Maine Coon Cat Breeds
Beautiful with a silky coat, the black Maine Coon is a gentle giant of a cat breed. These cuddly cats have jet black coats and tufted ears, which make them excellent pets. Continue reading for a thorough guide to these amazing cats from a veterinarian.

Introducing the Breeds of Black Maine Coon Cats
Originating in the state of Maine, the Maine Coon is among the oldest natural cat breeds in North America. A color variation of the breed known for its dense, solid black fur is the black Maine Coon. These cats have sweet, laid-back personalities and are very devoted to their families. Their shaggy fur needs to be combed on a daily basis. All in all, gentle giants that are lively and happy with loving companions.
Look: Big, luxurious black cats with long hair and noticeable ear tufts. robust, rectangular build.
Qualities: kind, sociable, devoted, and gentle. Have fun playing and hugging.
Popularity: Among the most chosen colors for Maine Coons.
Kind, understanding, and amiable temperament. committed to a family. thrives when in contact.
Duration: 12 to 15 years
Coat Color: A silky, dense black coat. Jet black to brownish black are acceptable shades.
Breed Origins: Originally a mixed breed, this is a color variant of the Maine Coon.
Taking Care of a Negro Maine Coon
Food
Cat food high in protein to maintain massive muscle mass
Food, both wet and dry
Formulas to control hairballs
Surroundings:
Lots of room to climb vertically
comfortable beds to sprawl out in
Outdoor access under supervision
Styling:
Brushing twice or three times a week
Sporadic baths
Cut nails
Cleaning your ears
Care: Daily playtime and affection. Gently cared for since kittenhood.
Getting a Maine Coon in Black
Popularity: Europe and North America
Cost on average: $1000 to $1500
Adoption: Maine Coon Rescue, Maine Coon Adoptions
Checks on Health:
Cardiomyopathy with hypertrophy
A dysplastic hip
Mutations in polydactyls
Getting Ready for a Cat
Advice:
Completely cat-proof your house
Keep a large number of toys on hand.
Regularly groom
Care: High-quality food, toys for enrichment, climbing areas, and routine vet care.
A cat tree, nail clippers, a deshedding brush, and interactive toys are necessities.
Health Concerns: obesity, hip dysplasia, and HCM.
Rabies, Feline Leukemia, and FVRCP vaccines. a preventive approach.
Well-Known Names
Select two or three names with easy-to-pronounce syllables. Think about "human" names.
For instance, Millie, Simon, Charlie, Oliver, and Lucy
0 notes