#Arrhythmias
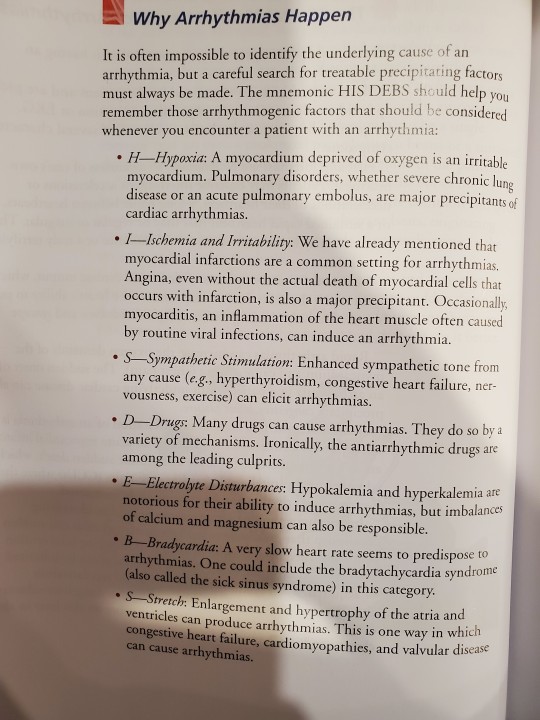
Text
The Increased Risk of Arrhythmias Following COVID-19: What You Need to Know
The Increased Risk of Arrhythmias Following COVID-19: What You Need to Know
#Covid19 #Arrhythmia #SARS #CoronaVirus #CardiacArrhythmia #Heart #HeartHealth
The COVID-19 pandemic has brought to light the numerous complications associated with the disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). While the respiratory symptoms of COVID-19 are well-known, there is growing evidence suggesting an increased risk of cardiovascular complications, including arrhythmias, in individuals who have contracted the virus. In this…

View On WordPress
#Arrhythmias#Can COVID cause cardiac arrhythmias?#Corona Virus#Covid#Covid-19#Heart Problems after COVID-19#Medical News#SARS#SARS-CoV-2
7 notes
·
View notes
Note
What is SVT
SVT stands for "supraventricular tachycardia".
supra- = above
-ventricular = ventricles
tachy- = fast
-cardia = heart
SVT is an abnormally fast heartbeat originating in the upper chambers of the heart (the atria, above the ventricles).
The symptoms that appear are typical of other types of tachycardia: palpitations, weakness, chest pain, dizziness, etc.
There are multiple types of SVT. Episodes may last minutes or days, be constant or occur in bouts, and may not require any treatment. Those who do require treatment may undergo heart procedures, lifestyle changes, or take medication.
Further reading:
Mayo Clinic
Cleveland Clinic
NHS (UK)
13 notes
·
View notes
Text
Exploring Common Heart Conditions and Their Risk Factors

1. Coronary Artery Disease (CAD)
Description: Coronary artery disease occurs when the arteries that supply blood to the heart become narrowed or blocked due to the buildup of plaque, a waxy substance made of cholesterol and other materials.
Risk Factors:
High cholesterol levels
High blood pressure
Smoking
Diabetes
Obesity
Sedentary lifestyle
2. Heart Attack (Myocardial Infarction)
A heart attack happens when a blood clot blocks the flow of blood to a specific area of the heart muscle. This causes the impacted cardiac tissue to deteriorate or die.
Hazardous Elements
Heart disease
elevated blood pressure
elevated levels of cholesterol
Consuming tobacco
Diabetes Meat Consumption
Heart disease in the family history
Stressful lifestyle of inactivity
3. Heart Failure
Synopsis: Congestive heart failure, another name for heart failure, is the result of the heart’s inability to pump enough blood to meet the body’s demands. It may be caused by a number of illnesses that weaken or harm the heart muscle.
Get Access Now
Risk Factors:
Coronary artery disease
High blood pressure
Diabetes
Obesity
Smoking
Excessive alcohol consumption
Heart valve disorders
Cardiomyopathy (disease of the heart muscle)

4. Arrhythmias
Description: Arrhythmias are irregular heart rhythms that can manifest as palpitations, fluttering sensations, or skipped beats. They can range from harmless to life-threatening and may be caused by various factors.
Risk Factors:
Coronary artery disease
High blood pressure
Diabetes
Thyroid disorders
Heart defects present at birth
Excessive alcohol or caffeine consumption
Smoking
Stress
Drug or medication interactions
5. Stroke
Description: A stroke occurs when blood flow to a part of the brain is interrupted, either due to a blockage (ischemic stroke) or bleeding (hemorrhagic stroke). Certain heart conditions can increase the risk of stroke by promoting the formation of blood clots.
Risk Factors:
Atrial fibrillation (irregular heart rhythm)
Coronary artery disease
High blood pressure
Diabetes
Smoking
High cholesterol levels
Obesity
Sedentary lifestyle
Conclusion
Understanding the common heart conditions and their associated risk factors is crucial for promoting cardiovascular wellness and reducing the risk of heart disease. By adopting a heart-healthy lifestyle that includes regular exercise, a balanced diet, stress management, and avoidance of harmful habits such as smoking and excessive alcohol consumption, individuals can take proactive steps to protect their heart health and enhance their overall quality of life.
Get Access Now
#HeartConditions#CardiovascularHealth#HeartDisease#RiskFactors#CoronaryArteryDisease#HeartAttack#HeartFailure#Arrhythmias#StrokeRisk#PreventiveCardiology#HealthyHeart#HeartHealthAwareness#LifestyleChanges#HeartCare#HealthEducation
0 notes
Text
EP Studies & RFA for Arrhythmias - Mukat Hospital
Explore EP Studies & RFA for Arrhythmias at Mukat Hospital, Chandigarh. Our expert cardiology team offers advanced Electrophysiology (EP) procedures and Radiofrequency Ablation (RFA) to diagnose and treat heart rhythm disorders effectively.
#chandigarh#mukat hospital#mukathospital#health#hospital#healthcare#cardiology#EP Studies#RFA#Arrhythmias
1 note
·
View note
Text
#heartrhythm#cardiology#cardiologist#doctor#heart#hearthealth#ekg#cardiovascular#heartfailure#heartdisease#cardiologia#medicalstudent#surgery#healthcare#cardiac#arrhythmias#electrophysiology#arrhythmia#heartattack#medicine#hypertension#cardiacsurgery#ecg#cardiologie#cardiologyfellow#highbloodpressure#atrialfibrillation#medical#defibrillator#echo
0 notes
Text
Arrhythmias
Cardiac arrhythmia occurs when electrical impulses in the heart don't work properly.
0 notes
Text
Heart Palpitations: When Your Heart Skips a Beat
Palpitations are sensations of a fast-beating, fluttering, or pounding heart, which can be felt in the chest. They can result from stress or from a more serious heart condition. Learn more about the symptoms and treatments here!

View On WordPress
0 notes
Text
Tech That Keeps Your Heart & Doctor Always Connected

Latest technological innovations can detect arrhythmias with more precision, & effectively manage the condition
0 notes
Text
Thinking about teen Dazai asking teen Chuuya to help him with this new tactic he's learning (controlling his heartbeat). An hour later Kouyou walks into Dazai lying flat on the ground and Chuuya with his ear pressed against Dazai’s chest as he yells "NO you're supposed to do dot dot dash not- dude you lost the rhythm again it's too fast CALM DOWN"
#meanwhile dazai regrets ever asking#imagine having your crush hear your heartbeat for hours#personally i would've gone crazy#chuuya doesn't know why dazai is having arrhythmia tho#soukoku#teen skk
8K notes
·
View notes
Text
Acute coronary syndrome
Overview
Acute coronary syndrome (ACS) is a term used to describe a range of conditions that result from sudden, reduced blood flow to the heart muscle. The reduced blood flow is usually caused by atherosclerosis, a buildup of plaque inside the coronary arteries that supply blood to the heart.The three main types of ACS are:- Unstable angina: This occurs when the blood flow to the heart is partially blocked, causing chest pain or discomfort, but the blockage is not severe enough to cause a heart attack.
- Non-ST segment elevation myocardial infarction (NSTEMI): This occurs when a blood clot partially blocks a coronary artery, reducing blood flow to the heart muscle and causing damage. The name "non-ST segment elevation" refers to the pattern on an electrocardiogram (ECG) that indicates the location and extent of the damage.
- ST segment elevation myocardial infarction (STEMI): This is the most severe form of ACS and occurs when a coronary artery is completely blocked by a blood clot, causing a large area of the heart muscle to be damaged or die. The name "ST segment elevation" refers to the pattern on an ECG that indicates the location and extent of the damage.
- Chest pain or discomfort: This is the most common symptom of ACS. The pain may feel like pressure, squeezing, fullness, or tightness in the chest. The pain may also spread to the arms, neck, jaw, back, or stomach.
- Shortness of breath: You may feel like you are out of breath or can't catch your breath, even when you're not exerting yourself.
- Nausea or vomiting: You may feel sick to your stomach or vomit.
- Sweating: You may feel sweaty or clammy.
- Lightheadedness or dizziness: You may feel dizzy or lightheaded.
- Fatigue: You may feel tired or weak.
- Severe or prolonged chest pain, particularly if it is accompanied by shortness of breath, sweating, or lightheadedness
- New or sudden onset of shortness of breath, particularly if it occurs at rest or with minimal exertion
- Any combination of symptoms that are new, severe, or persistent
- High blood pressure: High blood pressure can damage the arteries and make them more prone to atherosclerosis.
- High cholesterol levels: High levels of LDL (low-density lipoprotein) or "bad" cholesterol can contribute to the buildup of plaque in the arteries.
- Smoking: Smoking can damage the lining of the arteries and promote the buildup of plaque.
- Diabetes: People with diabetes are more likely to develop atherosclerosis and ACS.
- Family history: A family history of heart disease can increase the risk of developing ACS.
- Age: The risk of ACS increases with age.
- Obesity: Being overweight or obese can increase the risk of developing atherosclerosis and ACS.
- Age: The risk of ACS increases with age, especially in people over the age of 65.
- Gender: Men are more likely to develop ACS than women, although the risk for women increases after menopause.
- Family history: A family history of heart disease or stroke can increase the risk of developing ACS.
- Smoking: Smoking damages the lining of the arteries, making them more prone to atherosclerosis, which can lead to ACS.
- High blood pressure: High blood pressure can damage the arteries and increase the risk of developing ACS.
- High cholesterol levels: High levels of LDL (low-density lipoprotein) or "bad" cholesterol can contribute to the buildup of plaque in the arteries, increasing the risk of ACS.
- Diabetes: People with diabetes are more likely to develop atherosclerosis and ACS.
- Obesity: Being overweight or obese can increase the risk of developing atherosclerosis and ACS.
- Sedentary lifestyle: Lack of physical activity can contribute to the development of ACS.
- Stress: Prolonged or chronic stress can increase the risk of developing ACS.
- Unhealthy diet: A diet high in saturated and trans fats, salt, and sugar can increase the risk of developing ACS.
- Heart attack: ACS can cause a heart attack, which occurs when the blood flow to a part of the heart is blocked, leading to damage or death of the heart muscle.
- Arrhythmias: ACS can disrupt the normal rhythm of the heart, leading to abnormal heart rhythms or arrhythmias.
- Heart failure: ACS can damage the heart muscle, reducing its ability to pump blood effectively, leading to heart failure.
- Cardiogenic shock: In severe cases of ACS, the heart may not be able to pump enough blood to the body, leading to a condition called cardiogenic shock, which can be life-threatening.
- Stroke: ACS can increase the risk of developing a stroke, which occurs when the blood flow to the brain is interrupted.
- Depression and anxiety: ACS can be a traumatic event and may lead to depression and anxiety.
- Post-traumatic stress disorder (PTSD): Some people who have experienced ACS may develop PTSD, a mental health condition that can cause flashbacks, nightmares, and other symptoms.It's important to seek medical attention immediately if you experience symptoms of ACS to prevent these complications from occurring or worsening. With prompt and effective treatment, the risk of complications can be minimized.
Read the full article
#ACS#acute#angina#Arrhythmias#atherosclerosis#attack#Cardiac#Causes#chest#coronary#development#emergency#full#health#heart#ischemia#long-term#men#pain#procedure#protein#risk#style#symptoms#Syndrome#thrombosis#Treatment#unstable#women
0 notes
Text
Cardiac ablation is the most effective treatment for arrhythmias.
Cardiac arrhythmias, also called arrhythmias, are problems for patients and can be life-threatening in some cases. Arrhythmias cause problems for several hundred thousand people in Poland. Arrhythmias can be treated in a number of ways, but ablation is the most effective. What is ablation, who can get it, and what are the reasons it shouldn’t be done?
What is ablation, and what is the…
View On WordPress
0 notes
Text
Explore the potential benefits of long-term tea consumption for cardiovascular disease

Cardiovascular disease is a leading cause of death worldwide, and tea is one of the most widely consumed beverages and a primary source of caffeine for adults. The habit of drinking tea originated in China thousands of years ago, but has since spread worldwide. Evidence from observational and randomized controlled studies suggests that green tea has many potential benefits in reducing the risk of cardiovascular disease. These benefits include reducing the risk of major cardiovascular events, lowering blood pressure, reducing low-density lipoprotein cholesterol (LDL-C) levels, and aiding in weight loss.
At the same time, the physiological mechanisms by which tea confers cardiovascular benefits are being elucidated. Studies have found that tea polyphenols, particularly catechins, are the primary components responsible for the cardiovascular protective effects of tea. Clinical evidence shows that tea consumption can lower the risk of coronary heart disease, heart failure, arrhythmias, stroke, cardiovascular disease, and all-cause mortality. In population-based studies, higher tea intake, especially of green tea, is associated with increased survival-related cardiovascular benefits.
Cardiovascular disease is the leading cause of death worldwide, with approximately 4 million deaths attributed to it in 2017, accounting for one-quarter of all deaths. In China, coronary heart disease and stroke have become the leading causes of death. Therefore, the challenge of how to prevent cardiovascular disease through daily diet is urgent. The idea of drinking tea for health benefits has been circulating in society for a long time, and studies have been conducted in countries such as the United States and Japan, indicating that moderate tea consumption can lower the incidence of cardiovascular disease and overall mortality. However, due to cultural and lifestyle differences and disease spectra, this conclusion cannot be directly extrapolated to the Chinese population.
Tea, especially green tea, is a rich source of flavonoids, including catechins, epicatechins, and epigallocatechin gallate. Mechanistic studies have shown that these biologically active compounds can alleviate oxidative stress, relieve inflammation, and enhance endothelial and myocardial cells. Observational studies and randomized controlled trials have also shown that these biologically active compounds can alleviate risk factors for coronary heart disease, including hypertension and dyslipidemia. In contrast, the tea polyphenols in black tea are oxidized into pigments and inactivated during the fermentation process, resulting in weaker associations with health benefits.
#Cardiovascular disease#tea#green tea#catechins#tea polyphenols#flavonoids#epicatechin#epigallocatechin-3-gallate#observational studies#randomized controlled trials#coronary heart disease#heart failure#arrhythmias#stroke#hypertension#dyslipidemia#oxidative stress#inflammation#endothelial cells#myocardial cells#China
0 notes
Text
Influenza Persists by Uday Jain in Journal of Clinical and Medical Images, Case Reports (JCMICR)
Introduction
In the US, influenza (flu) causes 9 to 45 million illnesses, leading to 12,000 to 61,000 deaths annually (10.1001/jama.2020.14772). World Health Organization estimates that worldwide annually there are about one billion infections, 3-5 million severe illnesses, and 300,000-500,000 deaths (10.1038/s41572-018-0002-y). Influenza is caused primarily by influenza A and influenza B viruses. Influenza A is the cause of pandemics. A schematic diagram of influenza A virus is presented in (Figure 1). Influenza will continue to be prevalent because its current vaccines are safe but only 30-60% efficacious. In contradistinction, COVID-19 vaccines have an efficacy of about 90%. Additionally, new zoonotic influenza strains intermittently migrate to humans. Influenza is a major part of “The New Normal
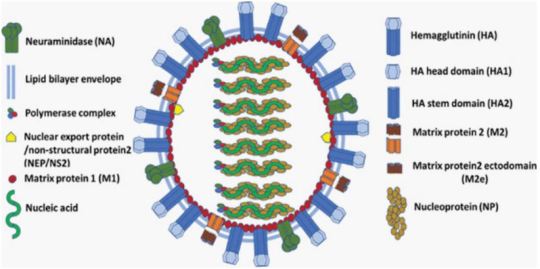
Figure 1: A schematic diagram of influenza A virus.
Coinfection
Since the start of COVID-19 pandemic, influenza is of greater concern. Overlapping spread of both diseases is a major strain on the health care system. Their coinfection is not common but may cause more severe disease. Influenza vaccination and therapy are important in addition to COVID-19 vaccination and therapy, especially in persons at increased risk.
Incubation
Influenza’s median incubation period is 2 days. Patients are infectious for a day before and 5 to 7 days after symptoms. COVID-19 has an incubation period of 4-12 days, a median of about 5 days. Patients are most infectious from 2 days before symptom onset. Influenza symptoms peak in 3-7 days. COVID-19 symptoms peak in second or third week. The spread of both viruses is facilitated by transmission by asymptomatic patients.
Transmission
About one-half of influenza A cases are due to aerosol transmission (10.1038/s41598-019-38825-y). Adequate ventilation can reduce it. Precautions utilized during the COVID-19 pandemic reduced the incidence of influenza in 2020. Used appropriately, surgical masks reduce the concentration of aerosolized influenza virus by about ten-fold and are adequate for prophylaxis against influenza (10.1016/j.jhin.2013.02.007; 10.7326/M20-3213). Transmission by respiratory droplets can also be reduced by masking. Transmission by direct contact can be reduced by hand and general hygiene. COVID-19 is transmitted in a similar manner. Social distancing reduces transmission by all the mechanisms. Influenza is less contagious and causes less severe disease than COVID-19. Quarantine recommended for COVID-19 patients is not necessary for those with influenza. Children play an important role in transmitting influenza. Healthcare providers should take precautions to avoid infecting themselves and others.
Influenza-Like Illness (ILI)
The Centers for Disease Control define ILI as fever 100°F (38°C) or greater and cough or sour throat that is not due to another known cause including streptococcal pharyngitis (strep throat). ILI’s causes can be benign such as common cold (nasopharyngitis caused by rhinovirus or other viruses) or severe including sepsis, meningitis, COVID-19, and SARS. Often there is an abrupt onset. SARS leads to severe disease in most of the infected. Influenza and COVID-19 cause mild disease in most of the infected (10.1016/S1473-3099(20)30484-9). SARS is currently not prevalent. Severe disease due to COVID-19 and SARS occurs primarily in the elderly. Influenza is more evenly distributed across the age groups. ILI can cause immunosuppression, leading to bacterial pneumonia, necessitating antibiotics (10.1097/QCO.0000000000000347).
After general anesthesia, children with influenza have a longer hospital length of stay and increased risk of requiring intensive care (10.1186/1471-2253-11-16). Routine surgery should be postponed for about four weeks in a patient with ILI. Unvaccinated patient should be offered influenza vaccination after the acute phase of ILI has passed and before the surgery. Before performing urgent surgery, severe causes of ILI should be excluded
Upper Respiratory Tract Infection (URI) Excluding ILI
In cold weather URI is common, especially in children. Often it is due to common cold, or noninfectious allergic or vasomotor rhinitis. Less commonly, it can be early presentation of more serious illness including ILI, COVID-19, strep throat, and herpes simplex. Early in infection it is difficult to distinguish between different etiologies of URI.
URI may cause sneezing, coughing, headache, malaise, rhinorrhea, sore throat, sinusitis, and bronchitis. Subsequently, bronchi may be hyperreactive for about six weeks. Pulmonary complications associated with surgery in a patient with URI are bronchospasm, laryngospasm, coughing, breath holding, postintubation croup, episodes of desaturation, atelectasis, and pneumonia. Anticholinergics and bronchodilators may not be beneficial. Perioperatively, adequate hydration and humidification should be maintained. There are no pediatric or adult anesthesia closed claims that implicate URIs including influenza with serious adverse events. There is a very small incidence of viral myocarditis in patients with URI including ILI. It may lead to serious arrhythmias and refractory heart failure (10.1016/j.jcrc.2018.06.001; 10.1038/s41569-020-00435-x).
Diagnostics Tests
These include nucleic acid amplification via polymerase chain reaction (PCR) and antigen-based immunological assays. A PCR test can be performed even at the point-of-care with results available within an hour (10.1016/S2213-2600(20)30469-0). This can facilitate infection control and utilization of antiviral therapeutics. It is especially useful for patients who have severe symptoms or are hospitalized. Test for COVID-19 may also be performed if indicated.
Influenza Vaccine
It is the best preventive measure. Although not very efficacious, it substantially reduces morbidity and mortality because of high prevalence of influenza. It is recommended for anyone over 6 months of age. It is especially beneficial in the presence of age <2 years or >65 years, pregnancy, and pre-existing conditions (10.1001/jama.2020.14772). Lack of vaccination in pregnancy not only increases the risk to mother but also increases the risk of preterm birth, fetal death, infant respiratory infection and hospital admission. The T cell response vaccines elicit is substantially weaker than the antibody response. Children may need two doses of vaccine, at least four weeks apart. The vaccine should be administered at least one week before surgery. It takes two weeks to develop full effect. As the protection wanes over time, mid-September to mid-October is preferred for vaccination. Influenza and COVID-19 vaccines may be administered together. The vaccine may be administered to surgical inpatients (10.7326/M15-1667).
Available Vaccines
The influenza virus mutates frequently. Quadrivalent vaccines protect against four of the currently most prevalent strains of influenza. The vaccines are altered every year for the predicted prevalent strains. Nine vaccines from four manufacturers are available in the US. Inactivated influenza vaccine is most commonly used. It is approved for persons above 6 months of age. As older individuals have a reduced response, vaccines that have a higher dose or are adjuvanted are recommended for persons above 65 years of age. The vaccine is usually administered intramuscular, but a lower dose intradermal vaccine is non-inferior (10.1001/jamanetworkopen.2020.35693).
Live-attenuated influenza vaccine is administered via nasal spray. It is approved for ages 2-49 years. It may be preferable in some situations such as vaccinating many persons in a community. It should be avoided if the patient or someone nearby has a suppressed immune system. Hence, it is not suitable for inpatients.
Recombinant vaccine and cell culture vaccine do not contain egg products. They are especially suitable for persons who need to avoid eggs because of allergy or dietary preferences.
Available Vaccines
Universal vaccines that provide durable response against all influenza strains are in human trials (10.1038/s41591-020-1118-7). These vaccines generate antibodies against the viral hemagglutinin protein stem (stalk) domain (HA2). Current vaccines generate antibodies against the immunodominant globular head domain (HA1), which is variable and mutates much more frequently. Vaccines utilizing mRNA are also in human trials. They are likely to have greater efficacy but more side effects than current vaccines. A major advantage of the mRNA vaccines is that they can be readily modified to match mutations in the virus.
Benefits of Vaccination for Adults
Influenza vaccine reduces the risk of respiratory and cardiovascular adverse outcomes and mortality among adults, especially in the presence of pre-existing conditions and advanced age. This was confirmed in a meta-analysis of studies on all adults (10.1016/j.arr.2020.101124). Another meta-analysis found that vaccine reduced the risk of adverse cardiac outcomes, especially in sicker patients (10.1001/jama.2013.279206). Preoperative vaccination is beneficial. A large study of elderly patients who had major surgery found preoperative vaccination reduced by about one-half the risk of pneumonia, intensive care admission, and death (10.1093/infdis/jix616). Patients also had shorter hospital stays and reduced resource utilization.
Influenza Therapeutics
These include neuraminidase inhibitors oseltamivir, zanamivir, peramivir, and laninamivir; cap-dependent endonuclease inhibitor baloxavir; and matrix protein M2 ion channel blockers (10.1001/jamanetworkopen.2021.19151). They attenuate viral replication. They provide postexposure prophylaxis. When started within 2 days of symptom onset, they reduce duration and severity of the disease, and complications. They also reduce transmission of influenza virus. However, their efficacy is limited, especially in patients with serious illness. They are expensive and not widely utilized. Although influenza and COVID-19 have similar initial symptoms, their therapeutics are different. Thus, dexamethasone reduces mortality for hospitalized COVID-19 patients on respiratory support but may increase mortality for hospitalized influenza patients (10.1001/jama.2020.15260).
Influenza Pandemics
They are usually caused by zoonotic influenza A virus strains migrating to humans. The 1918 “Spanish flu” pandemic caused by influenza A H1N1 virus led to more than 40 million deaths worldwide. H1 denotes haemagglutinin subtype 1 and N1 denotes neuraminidase subtype 1. The pandemics of 1957, 1968 and 2009 were caused by influenza A H2N2, H3N2, and H1N1 viruses, respectively. The 2009 “swine flu” influenza A H1N1 virus that originated from pigs was antigenically different from previously dominant influenza A H1N1 viruses. It caused 150,000-600,000 deaths worldwide. Avian influenza “bird flu” caused by H5N1 and H7N9 is not prevalent. Overlapping occurrence of influenza pandemic and COVID-19 will be devastating. Vigilance and prompt action are essential to prevent zoonotic influenza A virus strains from migrating to humans.
Conclusion
Influenza is a prevalent respiratory disease that will continue to affect anesthesia practice in the foreseeable future. With appropriate management, the risk of adverse outcomes is low. Vaccination is highly recommended, especially preoperatively.
For more details : https://jcmimagescasereports.org/author-guidelines/
#US#COVID-19#humans#therapy#appropriately#influenza#prophylaxis#ILI#SARS#anesthesia#laryngospasm#arrhythmias#Uday Jain#jcmicr
1 note
·
View note
Text
Role of Electrophysiology Studies and Radiofrequency Ablation in Managing Arrhythmias
Discover the pivotal role of Electrophysiology Studies & Radiofrequency Ablation in effectively managing arrhythmias at Mukat Hospital. Learn about cutting-edge techniques & specialized care for a healthier heart.

Read more: https://www.mukathospital.com/electrophysiology-study-radiofrequency-ablation/
1 note
·
View note