#the severity of the symptoms don’t correlate with the severity of the disease
Text
i hate womens health… how have none of you doctor freaks figured out what causes endometriosis by now
#it’s such a common condition#same w pcos#every male doctor should kill himself if he can’t find a cause of endo#I probably have it but they’ve never tested me#reading about endometriosis is like#ok so they don’t know what causes it#it can only really be diagnosed with surgery#the severity of the symptoms don’t correlate with the severity of the disease#and then the only treatments are fucking with your hormones#KILLJNG MYSELF IN FROMT OF TBE ENTIRE MEDICAL PROFESSION TO CHANGE THE TRAJECTORY IF THEIR LIVES FOREVER
35 notes
·
View notes
Text
CTE Plagues Heisman Trophy Winners and Families

Three-quarters of 1,035 brains of football players -- over 700
--examined at Boston University had CTE
The "taboo topic" is the centerpiece of "The Other Heisman Club" in the Washington Post, Dec 9, D1, by Kent Babb: the number of former Heisman winners with diagnosed or suspected Chronic Traumatic Encephalopathy (CTE). The degenerative brain disease is increasingly in the news for a number of reasons.
Four Heisman winners have been posthumously diagnosed with the disease: Howard Cassady, Pat Sullivan, Paul Hornung and Charles White. The implication in the article is that more winners already exhibit symptoms of CTE but whose families can't "know" until after death. But the families know.
Something is wrong. Sadly, silence is the preferred approach. And the unwillingness of our society to confront the obvious doesn't make it any easier. And the "whistling through the graveyard" approaches to concussions and the Concussion Protocols used worldwide don't provide much guidance about an alternative approach to Brain wounding. Facts matter:
- Four percent of Heisman trophy winners died of CTE, and the list of their wounded fellow winners is growing. If you extrapolate those numbers to the 25,000 former NFL players, over 1,000 of them are probably carrying the CTE markers.
- Three-quarters of 1,035 brains of football players, 0ver 700, examined at Boston University had CTE.
- Researchers at Boston University found CTE in 92 percent of former NFL players who were analyzed: they analyzed the brains of 376 deceased former NFL players and diagnosed 345 of them with chronic traumatic encephalopathy.
- More than half of the homeless have experienced traumatic brain injury and 1 in 4 have had moderate to severe brain injuries.
- Approximately 876,450 post-9/11 veterans suffer from untreated brain wounds.
- Researchers estimate that as many as 60% of incarcerated individuals are living with TBI, significantly higher than the 8.5% reported in the general population.
- Studies on prison and jail populations have reported a range of 25-87% of inmates reporting head injuries or TBI.
Of course, it is traditional to attack these numbers. Nay-sayers will demand more research. Hand-wringing by stake-holders on both sides will, like protests after mass-shootings, last a while and then subside. If anything, more dollars will go into researching how to make contact sports more safe. And treatments that are non-pharmaceutical will be ignored. Since "everyone knows there's no treatment for brain injuries," the best we can hope for from the medical profession is contained in the latest proceedings out of Boston.
The Robert C. Cantu Concussion Summit was held on December 8, 2023, at the Cantu Concussion Center at Emerson Hospital in Concord, MA. The theme of the conference was "Prevention of Concussion and Long-Term Effects of Repetitive Traumatic Brain Injury (RTBI)." In what is becoming a repetitive list of findings, the conference summarized:
- Eliminate intentional or avoidable head impact in contact and collision sports in both practices and games.
- Encourage policies and rules that limit the number, duration, and intensity of contact sport practices.
- Reinforce proper and safer techniques that avoid head contact at all levels of play.
- Implement rules of play that reduce and penalize intentional or avoidable contact to the head and neck.
- Correlating specific clinical symptoms with CTE neuropathology remains an important area for further investigation.
- Improve the criteria for Traumatic Encephalopathy Syndrome (TES) through further research.
Feel better? More importantly, if you are the parent of someone with a brain wound, what actionable intelligence can you take from that list? How will that list help you and yours deal with the here-and-now of a TBI/Concussion-suffering loved-one? If you'd like to learn more about what is happening, and what you can do, view this earlier Blog. Additional information is here.
Below is an insightful film about brain wounds
https://youtu.be/Zzbxrnm7jXc?si=IPKC5InadR0Eho52
https://treatnow.org/brain-wound-update-5-concussion-blast-tbi-cte/
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help heal the effects of BLAST injury, TBI/PTSD, and acute concussion.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#CTE#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#PostconcussionSyndrome#TBI#TBItreatment#traumaticbraininjury
0 notes
Text
Why Do More People Get Heart Attacks In Winter?
A heart attack, also referred to as a myocardial infarction, happens when something blocks the blood vessels, typically a blood clot, abruptly cutting off blood flow to the heart. Doctors regard heart attacks as an emergency because they deprive the body of oxygen and can result in abrupt death. Therefore, if someone is exhibiting heart attack symptoms, they should get emergency medical help.
As cold weather affects cardiac and circulation functioning, it puts more stress on the heart.
The cold weather increases the chances of heart attacks in people with cardiovascular issues. As a result, it is usual for more serious heart problems to manifest themselves during the winter and cold snaps.
Why are heart attacks more common in winter?
The cold impacts your heart in several different ways. A cold environment causes physical alterations in your circulatory system. Additionally, you could be less active throughout the winter since you prefer to stay indoors to unwind and be warm. Consequently, you might not work out your body and heart as much.
Heart attacks in winter were more frequent, according to a study conducted in 2017 on the correlation between various weather conditions and the state of the heart. The heart needs to work harder to keep a person warm in chilly conditions. As a result, cold temperatures may harm the heart and result in:
A faster heartbeat
The blood pressure rising
Having more oxygen in the blood causes it to thicken, which can cause blood clotting
People with cardiovascular disorders may be more vulnerable to the negative effects of the cold, such as arterial stiffness and high blood pressure. All these elements increase the heart’s workload and raise the risk of a heart attack. A heart attack can also be brought on by respiratory tract infections, which are worse and spread more widely in the winter.
Ways to prevent heart attacks in winter
There are ways to lessen one’s risk of suffering a heart attack during cold weather. People should make an effort to limit the length and intensity of their exposure to cold weather in order to prevent the impact of low temperatures on the heart.
This could be achieved by:
Maintaining body warmth by donning many layers of clothing and a heated hat.
Avoiding or restricting the consumption of alcoholic beverages when spending time in chilly settings because it can give the impression that you’re warmer.
Avoid overworking the body by taking more breaks from physical exercise and coming inside frequently to warm up if spending a lot of time outside.
The truth is that cold weather and cardiac issues don’t mix well, so exercise caution if you have a known heart condition. Take it easy if you’ve already experienced a heart attack or have heart disease. Working with a doctor can give you confidence when it comes to heart-healthy exercise and assist you in getting ready for winter.
Limit your intake of alcohol and coffee because they can raise blood pressure. So be mindful of how much you drink before going outside.
Avoiding smoking or vaping since tobacco products can raise blood pressure and lead to plaque formation. One of the best things you can do for your heart is to give up.
Maintain regular blood pressure checks. Reduce your chance of having a heart attack by managing your blood pressure. Don’t forget to take your meds as prescribed. Contact an expert immediately if you experience chest pain, nausea, vertigo, or excessive perspiration.
Warm beverages and hot meals are appropriate ways to stay warm when outside is chilly. Furthermore, while it’s cold outside, working out inside and staying active is critical. This is because regular exercise can aid in delaying or preventing the onset of cardiovascular problems.
The prevention of respiratory infections throughout the winter also involves other precautions. The flu and pneumococcal vaccines are suitable preventative strategies since they can lower the likelihood of having cardiovascular problems. Other, more consistent preventive steps include regularly washing your hands, refraining from touching your face, and avoiding crowded places.
If someone gets sick with an infection, they should take it easy until complete recovery before going outside in the cold. According to the majority of cardiologists, those who are older, routinely drink or smoke, and don’t exercise consistently are most at risk. These individuals may be able to minimize their risk of having a heart attack in the winter by minimizing their exposure to colder temperatures and maintaining a consistent amount of daily physical exercise.
Consult an expert for appropriate guidance
If you want to be in charge of your health, Poona Preventive Cardiology Centre will help you understand the chances of heart attacks in winter and how to prevent them. Poona Preventive Cardiology Centre is the only clinic in Pune that offers the safest and clinically approved Non-Surgical treatments for cardiovascular diseases based on Preventive Cardiology principles that help you avoid risky surgeries like bypasses and angioplasty.
1 note
·
View note
Text
10 Surprising Causes of Blood Sugar Fluctuations
All those people who have been living with type 2 diabetes for many years or have recently been diagnosed with this medical condition, must be aware of how blood sugar levels can fickle, and why it’s important to control fluctuating blood sugar levels. According to the National Institute of Health, by properly controlling the blood sugar levels, a diabetic person is at a lower risk of potential diabetic complications such as kidney damage, stroke, nerve damage, vision issues, and heart disease.

It’s normal for anyone to experience small variations in their blood sugar levels at different times of the day and depending upon their diet, activities, and many other factors. Blood sugar fluctuations are hardly seen in non-diabetic people as the body regulates the sugar levels in the blood by insulin secretion and the body’s natural processes. However, if the blood sugar fluctuations are large enough, one can experience symptoms such as dry mouth, fatigue, confusion, blurred vision, and headaches. When the blood sugar levels go critically out of range, its negligence can have severe short and long-term side effects.
An individual would be able to figure out whether their sugar levels are going high or low only when it is tested and repeated throughout the day with or without an empty stomach. This is done by a finger prick test, where the finger is pricked and the released drop of blood is placed on the machine to be analyzed. This is referred to by medical specialists as capillary blood glucose.
Blood sugars may zoom up all of a sudden and drip low if tried to adjust with insulin, physical activity, or proper diet. Most people feel confident in managing their diabetes, but in reality, even they don’t know what could affect their blood sugars in unexplained ways. To avoid getting ahead with pesky high and low blood sugars because of the corrections, it’s important to understand different unexpected triggers that can send one’s blood sugars on a roller coaster ride.
Here are 10 surprising factors that can make blood sugar levels fluctuate. Look out for them.
1.Dehydration
Being dehydrated means the body is falling short of fluids. Dehydration can lead to hyperglycemia- the spike in blood sugar levels. To make it even worse, the concentrated sugars in the circulation can cause the person to urinate more, eventually resulting in extreme thirst. If it is long-term, it can even cause serious problems with the small blood vessels of the body. Thus, diabetic people should be especially watchful about drinking sufficient water or other calorie-free beverages all day long to keep their body well hydrated and blood sugars in check.
2.Insufficient Sleep
It has been noticed that even if a person does not sleep for one night or has very little sleep, the body would start using less insulin which means there will be insulin resistance. This is because, our body releases insulin and regulates blood sugars naturally according to our circadian rhythms- the natural pattern of sleep and wakefulness. The correlation between sleep and elevated blood sugars goes both ways. Not only diabetics but even healthy people would show blood sugar fluctuations when they are sleep deprived. Late-night snacking on sugary foods to compensate for low energy levels of fatigue can be its reason.
3.Too Much Caffeine
Some people are addicted to daily cups of coffee containing caffeine. Those who have blood sugars extra-sensitive to caffeine are likely to encounter high blood sugars after intake of coffee even without a sweetener.
4.Artificial Sweeteners
As per a few research studies, it has been found that artificial sweeteners can increase blood sugar levels. However, still more research studies and evidence are needed to confirm this. A recent review article suggested that artificial sweeteners may contribute to compromised glucose homeostasis, so they may not be completely neutral in sugars.
5.Some Medications
As medications can have side effects, some prescription and over-the-counter drugs can derange blood sugar levels. One best example of medications known to spike blood glucose levels includes steroids like prednisolone. Others that may cause the shooting up of blood sugars are certain antidepressants and antipsychotics, nasal decongestants, diuretics, and birth control pills. However, there are even the drugs like those given to diabetics that can reduce the blood sugar level lower than normal readings.
6.Nasal Sprays
Some nose sprays have been tested and found to contain chemicals that trigger the liver to make more blood sugars.
7.The Infamous ‘Dawn Phenomenon’
It is common for both diabetics and non-diabetics to have elevated blood sugar levels as soon as they wake up early in the morning because of the surges in their hormones. This usually is experienced when the body prepares to wake up by the release of certain hormones including cortisol, between 2 and 8 a.m. These hormones cause insulin resistance which makes the blood sugars rise. Alternatively, those who are taking too much insulin or diabetes medications at night or not eating proper dinner may start their day with low blood glucose levels.
8.Skipping Breakfast
No one should skip the first-morning meal, as after starving for long hours the whole night and morning, certainly, the blood sugars can increase after having lunch and dinner.
9.Gum Disease
It can be a blood sugar spiker as well as a complication of diabetes.
10.Other Potential Causes
Time of the day- At a later time of the day, it could be difficult to control blood sugar levels.
Extreme weather- If it is bitterly cold or swelteringly hot, in either case, it would be hard to keep diabetes in control. Extreme heat like in hot baths, hot tubs, or sunburns can dilate the blood vessels which makes insulin absorption quicker and could result in low blood sugar levels.
Traveling- During traveling, diabetic people should be extra cautious. This is because there is a change in time zones which in turn disrupts medication schedule and sleeping habits, and causes unusual eating. There are chances of people smoking or having alcohol, and even becoming dehydrated. All of these could affect blood sugar levels.
Source:-10 Surprising Causes of Blood Sugar Fluctuations
0 notes
Text
Intermittent Fasting Can Be Your Gateway To Improve Rheumatoid Arthritis
The exact cause of this arthritis is unknown, but as with other autoimmune disorders. It has been theorized that it’s an interplay between genetics and environmental factors. RA is characterised by synovial hyperplasia and destruction of cartilage and bone which ultimately leads to multiple joint deformities. functional medicine doctor telemedicine
People with RA suffer from various co-morbidities like pain, deformed joints and even their life expectancy is lower as compared to the healthy population. The destruction in RA is because of the complex autoimmune process which involves the activation of T cells and CD4 cells. Patients with RA also show signs of early ageing like telomere shortening, impaired DNA repair etc.
Consults with Dr. Gupta
Is Current RA Treatment Adequate
With recent advances in treatment strategies, the new line of biologic medications have been introduced to help RA patients.
These medicines block certain inflammatory pathways, but at the same time also suppresses one’s immune system, plus they are really expensive and can come with a host of side effects. Another problem is that some patients don’t see improvement in their symptoms especially pain with these medications.
So the recent interest has been there to look for alternative/ comprehensive ways to manage pain and other comorbidities in RA patients.
Schedule consultation with Dr. Gupta
How Fasting Improves Rheumatoid Arthritis
Diet plays a very important factor in autoimmune diseases and that’s the reason different kinds of diets have been studied for RA patients.
One of the diets which has been popular recently is — intermittent fasting or fasting-mimicking diet. Fasting has been shown to decrease inflammatory markers in people and also bring about some changes which decrease the biological rate of ageing.
Fasting can help autoimmune diseases like RA by reducing inflammation and also through immunosenescence which basically means killing old and damaged cells and replacing them with young and functional ones. A study was done in RA patients by comparing the effect of fasting diet with normal diet for the patients.
Intermittent fasting improves rheumatoid arthritis
In this study, patients went through one time fast of 7-10 days followed by a vegetarian diet. The results not only showed improvement in clinical symptoms but also Lab values of ESR and CRP, which are a marker of inflammation in the system and are correlated with disease severity of RA.
Another study showed similar improvement in pain symptoms for patients after a period of fast. A modified fasting diet with low-calorie intake for 7-10 days was studied in RA patients and it showed clinical improvement in these patients.
Set up a call with Dr. Gupta
So Rheumatoid Arthritis does get better with Intermittent Fasting; but what exactly is it and how to do intermittent fasting.
Let’s discuss it here —
What is Fasting and How to do it
There are different ways of doing fasting and people sometimes choose the way that best suits their needs and lifestyle.
Prolonged Fasting: In this kind of fasting people will not eat any real food for a long period of time each week. Fasting days can be anywhere from 1 day a week to 3 days a week. People repeat this 1-3 day fast every week on a periodic basis or intermittently.
Intermittent Fasting: This refers to fasting for 16 hours and restricting your food intake window to only 8 hours. So typically people should not eat between 8 pm till 12 pm the next day. And will have 1-2 meals between 12 pm – 8 pm. They can do this every day or sometimes do it for 3-4 days a week.
Fasting mimicking diet: This is another diet which is getting popular these days, and the basis of this is to eat a diet which mimics fasting method. In this diet calories and carb are restricted while there is more good fat which improves insulin response and reduces inflammation.
Now the question is — which kind of fasting method is best for RA. The answer to this tricky question is that we really don’t know the exact diet which works for because there has not been a head to head trial to compare all these fasting methods.
My Suggestion to RA patients to find which fasting best diet that works for them —
What I suggest to my patients is the following combination —
Then follow it by intermittent fasting and do the 16:8 method (16 hr fasting: 8 hr food window) for the rest of the days in the week and take 1 day off during the week to reboot the system. So 1or 2 day of complete fast, 4 days of intermittent fasting and 1 day off every week.
intermittent fasting & RA
Fasting is a good way to keep your health in good check, especially if you have an autoimmune condition it can really make a difference. For Rheumatoid arthritis, there has been research which shows benefit not only in clinical parameters like pain but also saw improvement in the disease process. So fasting can be a part of RA treatment plan.
For More Info: Functional Medicine Doctor New York
functional medicine thyroid doctors
Functional Medicine Houston
0 notes
Text
Artificial intelligence helps detect gait alterations and diagnose Parkinson’s disease

- By Luciana Constantino , Agência FAPESP -
Scientists affiliated with the Department of Physical Education’s Human Movement Laboratory (Movi-Lab) at São Paulo State University (UNESP) in Bauru, Brazil, are using artificial intelligence to help diagnose Parkinson’s disease and estimate its progression.
An article published in the journal Gait & Posture reports the findings of a study in which machine learning algorithms identified cases of the disease by analyzing spatial and temporal gait parameters.
The researchers found four gait features to be most significant for the purposes of diagnosing Parkinson’s: step length, velocity, width and consistency (or width variability). To gauge the severity of the disease, the most significant factors were step width variability and double support time (during which both feet are in contact with the ground).
“Our study innovated in comparison with the scientific literature by using a larger database than usual for diagnostic purposes. We chose gait parameters as the key criteria because gait impairments appear early in Parkinson’s and get worse over time, and also because they don’t correlate with physiological parameters like age, height and weight,” Fabio Augusto Barbieri, a co-author of the article, told Agência FAPESP. Barbieri is a professor in the Department of Physical Education at UNESP’s School of Sciences (FC).
The study was supported by FAPESP via three projects (14/20549-0, 17/19516-8 and 20/01250-4).
The study sample comprised 63 participants in Ativa Parkinson, a multidisciplinary program of systematized physical activity for Parkinson’s patients conducted at FC-UNESP, and 63 healthy controls. All volunteers were over 50 years old. Data was collected and fed into the repository used in the machine learning processes for seven years.
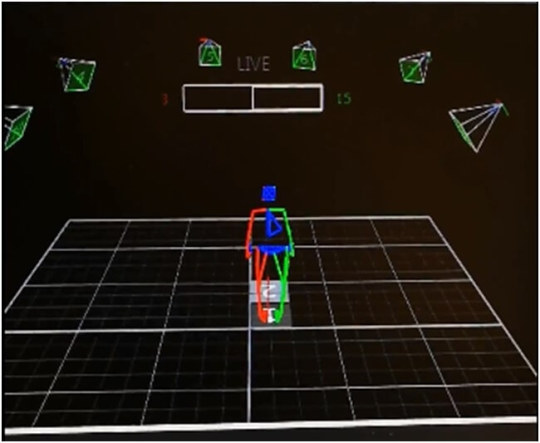
Image: Graphical representation of the experiment conducted by Movi-Lab researchers at UNESP (researchers’ archive)
A baseline assessment was produced by analyzing gait parameters for the healthy controls and comparing them with expected levels for this age group. This involved using a special motion capture camera to measure each person’s strides for length, width, duration, velocity, cadence, and single and double support time, as well as step variability and asymmetry.
The researchers used the data to create two different machine learning models – one for diagnosis of the disease and the other to estimate its severity in the patient assessed. Scientists at the University of Porto’s School of Engineering in Portugal collaborated on this part of the study.
They ran the data through six algorithms: Naïve Bayes (NB), Support Vector Machine (SVM), Decision Tree (DT), Random Forest (RF), Logistic Regression (LR) and Multilayer Perceptron (MLP). NB achieved 84.6% diagnostic accuracy, while NB and RF performed best in assessing severity.
“Typical accuracy for clinical assessments is around 80%. We could significantly reduce the probability of diagnostic error by combining clinical assessment with artificial intelligence,” Barbieri said.
Forthcoming challenges
Parkinson’s disease is at least partly due to degeneration of nerve cells in the brain areas that control movement, as a result of deficient dopamine production. Dopamine is the neurotransmitter that transmits signals to the limbs. Low dopamine levels impair movement, producing symptoms such as tremors, slow gait, rigidity and poor balance, as well as alterations in speech and writing.
Diagnosis is currently based on the patient’s clinical history and a neurological examination, with no specific tests. Precise information is unavailable, but 3%-4% of the population aged over 65 is estimated to have Parkinson’s.
According to another co-author, PhD candidate Tiago Penedo, whose research is supervised by Barbieri, the results of the study will be useful to improve diagnostic assessment in future, but cost could be an inhibiting factor. “We made progress with the tool and contributed to expansion of the database, but we used expensive equipment that’s hard to find in clinics and doctor’s offices,” he said.
The equipment used in the study costs around USD 100,000. “It’s possible to analyze gait with cheaper techniques, using a chronometer, force plate and so on, but the results aren’t precise,” Penedo said.
The techniques used in the study can contribute to a better understanding of the mechanisms underlying the disease, especially gait patterns, the researchers believe.
An earlier study, reported in an article published in 2021, with Barbieri as last author, evidenced 53% lower step-length synergy while crossing obstacles in Parkinson’s patients than in healthy subjects of the same age and weight. Synergy refers in this case to the capacity of the locomotor (or musculoskeletal) system to adapt movement, combining factors such as speed and foot position, while stepping off a curb, for example (read more at: agencia.fapesp.br/35563).
Another study, also published in Gait & Posture, showed that Parkinson’s patients were less able to maintain postural control and rambling-trembling stability than their neurologically healthy peers. The authors said the findings provided new insights to explain the larger, faster and more variable sway seen in Parkinson’s patients.
The article “Machine learning models for Parkinson’s disease detection and stage classification based on spatial-temporal gait parameters” is at: www.sciencedirect.com/science/article/abs/pii/S0966636222004799.
This text was originally published by FAPESP Agency according to Creative Commons license CC-BY-NC-ND. Read the original here.
--
Read Also
FDA and NIH launch public-private partnership for rare neurodegenerative diseases
#parkinsons#brain#neuroscience#walking#gait#posture#ai#artificial intelligence#machine learning#diagnostics#health tech#brazil#neurodegenerative diseases#neurodegenerative disorders
0 notes
Text
When should I be concerned about kidney pain?
Kidney stones (also called renal calculi, nephrolithiasis, or urolithiasis) are hard deposits made of minerals and salts that form inside your kidneys. A small, hard deposit that forms in the kidneys and is often painful when passed. Kidney stones are hard deposits of minerals and acid salts that stick together in concentrated urine. They can be painful when passing through the urinary tract, but usually don’t cause permanent damage.
The most common symptom is severe pain, usually in the side of the abdomen, that’s often associated with nausea.
Diet, excess body weight, some medical conditions, and certain supplements and medications are among the many causes of kidney stones. Possible causes include drinking too little water, exercise (too much or too little), obesity, weight loss surgery, or eating food with too much salt or sugar. Infections and family history might be important in some people. Eating too much fructose correlates with increasing risk of developing a kidney stone.
Treatment includes pain relievers and drinking lots of water to help pass the stone. Medical procedures may be required to remove or break up larger stones.
There are different types of kidney stones. The cause of the problem depends on the type of stone.
Stones can form when urine contains too much of certain substances that form crystals. These crystals can develop into stones over weeks or months.
Calcium stones are most common. They are most likely to occur in men between ages 20 to 30. Calcium can combine with other substances to form the stone.
Oxalate is the most common of these. Oxalate is present in certain foods such as spinach. It is also found in vitamin C supplements. Diseases of the small intestine increase your risk for these stones.
Calcium stones can also form from combining with phosphate or carbonate.
Other types of stones include:
Cystine stones can form in people who have cystinuria. This disorder runs in families. It affects both men and women.
Struvite stones are mostly found in men or women who have repeated urinary tract infections. These stones can grow very large and can block the kidney, ureter, or bladder.
Uric acid stones are more common in men than in women. They can occur with gout or chemotherapy.
Other substances, such as certain medicines, also can form stones.
The main symptom is severe pain that starts and stops suddenly:
Pain may be felt in the belly area or side of the back.
Pain may move to the groin area (groin pain), testicles (testicle pain) in men, and labia (vaginal pain) in women.
Other symptoms can include:
Abnormal urine color
Blood in the urine
Chills
Fever
Nausea and vomiting
Lithotriptic:
Having the quality of or used for dissolving or destroying stone in the bladder or kidneys.
Lithotriptic agents are an agent that effects the dissolution of a calculi.
Urricali tablet & syrup is a natural Lithotriptic. It facilitates the passage of urinary calculi by diuretic action. Apart from disintegration of stones and flushing them out, Urricali tablet & syrup also prevents their recurrence. It also effectively cures and prevents urinary tract infections. Urricali perceptively encourages healthy urinary track and helps to keep up a normal urine composition add mucosal integrity. Urricali tablet & syrup possess anti-spasmodic and anti-inflammatory properties which helps to reduce ureteric colic and ease the condition sore and burning micturition.
To know more: https://lamarworld.co/when-should-i-be-concerned-about-kidney-pain/

0 notes
Text
Relationship Between Alcohol And Cardiac Disease
Alcohol abuse increases the risk of type 2 diabetes, heart attacks, and strokes by raising weight and blood pressure.
1. Alcohol – what is it?
Being a "depressant", alcohol slows down the rate at which your brain commands your body.
Important processes like speech and movement might be impacted even little. Your respiration and heart rate can both go dangerously low if you consume a lot of liquids all at once.
If you consume alcohol frequently, you may feel that it doesn't impact you as much, but this usually indicates that you have grown tolerant of some of the effects. Don't forget that drinking more increases the potential for harm.
2. How does drinking influence the heart?
There is a direct correlation between excessive alcohol consumption regularly and high blood pressure. As cardiovascular disease (CVD) develops, high blood pressure (hypertension) strains the heart muscle and raises your risk of heart attack and stroke. Regular drinkers who exceed the lower risk thresholds are likely to be told to cut back or quit drinking altogether.
Alcoholism can lead to additional major health issues such as arrhythmias and cardiomyopathy, in which the heart muscle is damaged and unable to function as effectively as it once did (abnormal heart rhythms). Your risk of stroke may rise as a result of several of these ailments.
3. I have a cardiac issue. Should I quit drinking alcohol?
Alcohol may raise your risk of developing arrhythmias if you already have one of those conditions. Those who have hereditary heart rhythm disorders may find this to be extremely risky.
The first episode of arrhythmia can also be brought on by heavier drinking (binge drinking); once this has occurred once, you are more likely to have it again.
The blood pressure will quickly decrease when you quit drinking or cut back (you should see a reduction within a few days). Many people with alcoholic cardiomyopathy find improvement or even complete recovery after quitting drinking.
4. I underwent heart surgery. When may I have alcohol once more?
While you are in the hospital, your blood pressure meds are changed, but you are not consuming alcohol at that time. If you start drinking frequently again at home and your blood pressure fluctuates, your doctor can adjust the drugs you're taking.
When it's safe to start consuming alcohol again medically, your doctor will frequently provide you with advice. However, psychologically speaking, many patients experience depressive symptoms after being sent home, particularly after open heart surgery.
It's normally better to hold off on drinking alcohol again until this feeling goes away as doing so can make it worse and make it linger longer.
5. Will drinking affect the way my cardiac meds work?
Alcohol can reduce the medication's effectiveness for many persons using long-term medicines.
It's vital to discuss with your doctor how drinking alcohol may influence the way your diabetes meds or anticoagulants like warfarin operate.
Over time, alcohol harms the liver as well, especially if you drink excessively.
When taken with alcohol, drugs that directly affect the liver, like statins, can worsen the condition. If you do drink, limit your intake to low-risk amounts.
Role of CPR Tampa
CPR Class Tampa trainers play a pivotal role in imparting quality tutelage to the pupils in a stress-free environment. For joining, dial 813-453-9974.
0 notes
Text
The Difference Between Mental Health and Behavioral Health
There is a good chance that you may run into references to mental health services when looking for treatment alternatives for mental illness. Psychological well-being and medical well-being may be closely related, but they are not synonyms according to behavioural health billing services.
To get the best care, it's important to know the distinction between mental and behavioural health.
Behavioural Health: A Comprehensive Guide to Conceptualization and Assessment
An individual's mental, physical, and spiritual well-being are all intertwined in the concept of behavioural health. Habits have a direct impact on one's overall health and well-being, both physically and mentally.
Substance abuse, eating disorders, gambling addiction, and sex dependence are all examples of behavioural health disorders. Each of these ailments is the result of harmful habits. ADHD, Asperger's syndrome, and autism are all examples of behavioural health illnesses that can affect children.
The Meaning of Mental Health
To be said to have good mental health, one must be in good emotional, social, and psychological shape. It has an impact on our thoughts and feelings, our behaviour, our relationships with others, and our ability to cope with stress. As a youngster and an adult, mental wellness is essential.
People with mental illness or mental health concerns have problems with their emotions, behaviours, or thoughts as per the behavioural health billing services near me. Panic attacks, depression, schizophrenia, and binge eating disorder are among the most prevalent mental health concerns we see.
A Contrast of Physical and Emotional Well-Being
There is a direct correlation between our thoughts and our actions. They are interconnected in the same way that our psychological and behavioural well-being is. However, they are distinct and should be handled as such.
An individual's feelings or thoughts regarding a specific scenario may indicate a mental illness. People who are suffering from mental illness are more likely to experience sleep problems or relationship problems.
Mental illness, on the other hand, often manifests itself in the physical realms. Actions and habits are frequently enough to tell you something about someone. They may be addicted to drugs or have a disordered eating habit.
Unhealthy behavioural habits may be the result of untreated mental illnesses as observed by the behavioural health billing services near me. Depressive disorders, for example, can be treated with drugs and alcohol. In the same way, imbalanced behaviour can exacerbate poor mental health.
Both Are Interconnected
As noted by the behavioural health billing services, there is a strong link between behavioural health and an unhealthy habit. Mental health illnesses may not be triggered by these behaviours.
Untreated mental health concerns may create behavioural health problems. A person with a familial tendency to mental health difficulties like bipolar disorder is otherwise healthy.
Alcohol self-medication is an example. Some mental diseases, like schizophrenia, can cause severe symptoms that can be relieved with medicine. Both behavioural and mental health concerns can cause a variety of problems.
The terms "behavioural health" and “mental health” are often used interchangeably, but they don’t always mean the same thing. Mental health pertains entirely to a person’s psychological state, while behavioural health entails not just a person's state of mind but their physical condition.
0 notes
Text
Copypasta from FB, a thing I do every year for October! Doing this has helped MULTIPLE friends of mine severely cut down that average 8 year wait to be diagnosed! Please, if you have any questions or are hesitating to get yourself tested, contact me and I might be able to point you in the right direction! Long Covid is literally just virus-induced POTS, which has resulted in a TON more research into the condition as we progress through this pandemic!
It’s Dysautonomia Awareness Month!
I’m always taking these types of questions but new friends don’t tend to realize it, so I make sure to talk about it every year. I have multiple forms of dysautonomia: POTS (postural orthostatic tachycardia syncope), NCS (neurocardiogenic syncope), and MCAS (mast cell activation syndrome). I also have the unnamed immune system and gastro symptoms that are bundled with these, but they still go by various names that only describe symptoms and aren’t themselves diagnoses yet.
This is what [Sushi] is for- though I do have an old knee injury and a new back and brain injury [s]he also assists me with- and it is something that has been affecting me since I was very, very young.
It is estimated that roughly 1/3 of female-bodied people aged 15-50 have some form of dysautonomia, with POTS and NCS being the most common. It can affect male-bodied people too, but it is much less common. It is a chronic, lifelong, and progressive disease with no cure- and yet many doctors still believe it doesn’t exist and that those with it are simply faking/lying or have other, unrelated disorders such as anxiety or seizure disorders. Because of this, the number of people who have been diagnosed are far lower than the estimated number of people who should be, and the average POTS patient waits 8 years before finding a doctor who will listen to them. Various medications exist to help with the symptoms as they occur, but the best results are medication combined with several lifestyle and diet changes to adjust to the body’s needs. Studies have shown that living with POTS can be as debilitating as living with heart failure or COPD, and it is recognized as a disabling diagnosis.
We do not yet know what causes dysautonomia- it in itself is a symptom rather than a disease. The autonomic nerve (also called the vagus nerve) in the brain stops functioning correctly. As this nerve controls your background functions (things you do without needing to think about it) and your fight/flight response, this causes your body to react to various stimuli in inappropriate ways, which can be dangerous depending on the situation. We do know that there seems to be a correlation between head trauma and traumatic brain injuries such as concussions and the development of dysautonomia symptoms; over 2/3 of people diagnosed with POTS have had a concussion shortly before onset. There is also a potential link between the HPV vaccine and POTS. The rest are thought to have a genetic link, as their symptoms started randomly upon entering puberty or even as early as toddler years (like me!).
If any of my friends are curious about dysautonomia, POTS, NCS, MCAS, etc- my inbox is open, and I will try to help you as best I can. I have helped several friends in the past with this, and if I can help trim that 8 year wait down by telling you exactly what to ask for I absolutely will.
59 notes
·
View notes
Note
Why don't you think masks protect other people? This "guilt the person into wearing masks" trend is reaching far and wide, but are they wrong? Like one argument is that the virus particles are small enough to pass through mask filters, but then the rebuttal (usa today, "No, N95 filters are not too large to stop COVID-19 particles") claims the opposite. So much opposing info out there.
N95 masks might be effective. But the vast majority of people aren’t wearing those, and it’s not practical to have everyone wear an N95 mask every day everywhere they go.
Especially when you consider how medical masks are intended to be used.
Pre-covid in a hospital setting, masks were used for procedures where there was a risk of disease transmission, with severely immune compromised patients, and with patients known or suspected to have a highly infectious disease.
A doctor or other medical staff member would wash their hands before going in, put gloves on, put the mask on, and then when leaving throw the mask and gloves away and wash their hands again. Or some similar protocol.
That’s not what we’re doing. That’s not practical for people living their every day lives.
Instead, we’re wearing mostly cloth masks or “surgical” masks (most of which aren’t actually surgical grade) for hours at a time, touching them, and reusing them multiple times before throwing them away or washing them (and when washing, we are often not truly sanitizing them).
To have every member of the public use masks the way they are supposed to be used in a medical setting would create a huge amount of waste and entail a huge cost for either individuals or the government (which is then funded by tax-paying individuals)
All of this rests on whether this is necessary. We don’t have randomized controlled trials showing that masks work (we have mathematical models, and a mathematical model can say anything you want it to depending on the assumptions you give it), but even if we did, this is not the plague. It’s not even the Spanish Flu.
We know how it spreads (in close contact with a person in an enclosed space for a prolonged period with or without masks, and usually only with a symptomatic person), and we have a lot of treatments showing promise. We’re even seeing correlations with certain nutrients that could mean the disease is preventable with good nutrition and/or supplementation.
There is no reason to live in fear of this thing. Yes, people have died. People die of flu and common colds every year. In fact, children are much more likely to die of flu than COVID, and we used to only close schools down for flu if a significant percentage of students and staff were out sick.
And yes, we have a flu vaccine, but it really isn’t all that effective and often we end up with strains that weren’t part of that year’s shot going around.
People with severely compromised immune systems can take extra precautions, such as limiting their exposure to crowds, washing their hands, getting their vitamin D (through sunlight, food, or a whole-food D3/K2 supplement), and staying away from people showing symptoms.
What if instead of a $1.9 trillion “rescue package” we spent significantly less providing for immune compromised people who want to isolate and then let everyone else go back to work, school, and above all, normal.
People who want the vaccine can get it, those who don’t can skip it, and as we find and test new treatments and preventative measures we can make sure vulnerable people have access to care when they choose to re-enter society.
115 notes
·
View notes
Note
1- the logical thinking indicates that the most probably option is usually the correct option, for example, if a man has lung cancer the most likely option is that is lung cancer is related to his tabaquism, the same aplly on this case, if a person with morbid obesity has some kind of circulation problem then the most likely option is that is related to the weight of that person, now about your question, if you wanna know how morbid obesity relates to health problems then my answer is
2 - read a goddanm biology book (or just google it), the answer is right there, you dont need to ask a random person on the internet about that, and guess what, you cannot put links into asks so im unable to give you the link to any kind of article explaining that, if you wanna know the corelation then just search morbid obesity on wikipedia.
---
This ask is about this post where a woman's health issues are blamed by doctors on her weight, so she loses the weight, and when doctors see that her health issues have not gotten better, but have gotten worse, they order tests that they should have ordered months ago.
I think you misunderstand the point of the post. Let's take the obesity out of this. A woman goes to the doctor for severe cramps, sleepiness during the day, memory and balance problems. Doctors refuse to treat her. That's all there is to this issue - a woman has gone to a medical professional with a set of symptoms, and the medical professional did not test her for the conditions that have the above symptoms.
You give me an example in your ask of smokers having an increased risk of lung cancer, so let's apply this analogy here. A smoker goes to the doctor and says, "doctor, I have difficulty breathing, a painful cough that doesn't go away for months, I lost 50 pounds in less than a month, pain in my hands, fingers and chest." These are very common symptoms of lung cancer. So, what you're advocating for, is that the doctor should refuse to order any tests for the patient, tell them to stop smoking, and send them on their way. We know that some health risks are associated with obesity, in the same way that lung cancer is associated with smoking, so should we not be testing those people for those diseases more often?
People whose father has died of heart disease are at more risk of heart disease, so we test those people for heart disease when they mention they have symptoms. People whose family has ADHD are more at risk of having ADHD, so we test those people for ADHD when they mention they have symptoms. Why is obesity any different? If a disease has already developed, losing weight will do nothing except for decrease that initial risk, but it's past that already if they HAVE THE DISEASE. They have to be treated for the disease. Thin people can get heart attacks, and non smokers can get lung cancer or develop asthma, so why do those people go to the doctor with those symptoms and get tested, and obese people don't?
In some of your replies on that post, you have used this Wikipedia page as your source. On the same page, it says,
"While a majority of obese individuals at any given time are attempting to lose weight and often successful, research shows that maintaining that weight loss over the long term proves to be rare." (Wikipedia includes a reference for this, I've linked it here).
I am using the same research you are using to argue my point. If an obese individual walks into a doctor's office with symptoms of a heart condition, and is told to lose weight, they are basically sentenced to death. As we can see above, long term weight loss may lead to more health risks, and is actually very rare in most people (less than 1 in 100 obese people manage to lose the weight and stay at the new weight), and so if a doctor tells an obese person not to come back until she has lost all of the weight, she may actually die before she comes back to the doctor.
Obesity is an issue, and does increase the risks of some conditions. However, according to the same Wikipedia article you and I have both been using,
"obesity has individual, socioeconomic, and environmental causes, including diet, physical activity, automation, urbanization, genetic susceptibility, medications, mental disorders, economic policies, endocrine disorders, and exposure to endocrine-disrupting chemicals."
I don't want to assume you're enough of a heartless monster to say "obese people brought this on themselves and therefore deserve to suffer and die due to medical malpractice" as a response to my above point, but JUST IN CASE YOU WERE, that's a whole lot of people you're condemning. You're condemning children who grow up in poverty and whose parents can only afford McDonald's (cheaper than vegetables in the USA), you're condemning my uncle, who had a deadly thyroid issue that wasn't treated in time (he grew up in Soviet Russia) and messed up his metabolism so bad he currently exercises for 3 hours a day but is still extremely overweight. You're condemning people with pcos, people with hyperthyroidism, people with eating disorders and depression. All of those people, in your opinion, do not deserve medical treatment.
With what we now know, let's summarise.
Fact 1: people who are obese have a higher risk of developing certain disorders, in the same way that someone with a family history of heart problems may develop heart problems, however, no disease is directly CAUSED by obesity and obesity alone. If that were the case, thin people wouldn't get those diseases at all, but I know many thin people with narcolepsy, cancers, and heart issues.
Fact 2: obesity can be caused by many factors, not just eating a lot of junk food. I've already mentioned hyperthyroidism, eating disorders, pcos, and poverty as some of those factors, but there are more. A lot of those factors are not the fault of the obese individual. We also know that once someone is already obese, keeping off weight that they lose is extremely difficult and takes a long time.
Fact 3: when a smoker goes to the doctor with symptoms of lung cancer, they are told to stop smoking, but they are also SCREENED FOR LUNG CANCER and TREATED IF THERE IS LUNG CANCER PRESENT.
Fact 4: according to the woman in the original post, she went to the doctor with symptoms of narcolepsy and other issues, was told to lose weight, BUT WAS NOT TESTED FOR THE DISEASES SHE IS AT RISK FOR, OR TREATED.
Do you see my point now? Yes, obesity is linked to diseases, but that should mean that people who are obese are screened and treated MORE OFTEN, not less or god forbid not treated at all. Preventing obesity by exercising and eating well is something we should definitely do ON A GLOBAL SCALE (better mental health help for people with depression/eating disorders, cheaper vegetables for people in poverty, more education, less fast food places), to decrease our risk of the diseases that obesity is associated with increasing the risk for (type two diabetes, sleep apnea, narcolepsy, certain cancers), but if someone is already obese, weight loss is no longer a cure, and actual treatment needs to be administered. Weight loss was never a cure, it is a PREVENTATIVE MEASURE, and not even a good one according to the evidence I've provided above. Healthy eating and exercise are good preventative measures, but they do not always contribute to weight loss. So why do doctors prescribe weight loss in the form of pills and calorie restriction, rather than eating HEALTHY and exercising? ALSO, if weight loss was a cure, non-obese cancer patients, non-obese people with narcolepsy, and non-obese people with eating disorders would also be told to lose weight rather than given treatment. So why is weight loss the ONLY treatment doctors give obese people? Obesity is much more complicated than a person just eating a lot of junk and getting fat, that's not how it works.
You know how we "eliminate the most probable option"? WE TEST THE PATIENT FOR IT, AND IF THE TEST COMES BACK NEGATIVE WE ELIMINATE THE OPTION. Why was the woman in the post not tested, and why do you advocate for this? Why do you think a group of people deserves medical attention less than others?
Here's another analogy. Wearing a mask and staying six feet away from others is a PREVENTATIVE MEASURE for covid. When a person already has covid, they are not told to wear a mask and stay six feet away from others. They are put in a hospital and treated. What you are advocating for is akin to sending a person with covid symptoms away with a mask, and not treating them at all.
To summarise: correlation is not causation, all people deserve medical help (people who are turned away from doctors a LOT are women, people of colour, and fat people. Medical discrimination needs to be eradicated in all of those cases) and you are in no position to decide who deserves to be treated and who doesn't.
I'm not overweight myself. I just care about people receiving the medical treatment they need and deserve, regardless of what they look like or what other conditions they already may have. I recommend really looking at yourself and examining the biases you have against fat folks, and figuring out how to become better as a person. You seem to enjoy giving unsolicited medical advice, so here's some from me: stop being a dick.
#apollo answers#fatphobia#death tw#mentions of covid 19 tw#i hope they read and understand this#fat shaming
74 notes
·
View notes
Photo

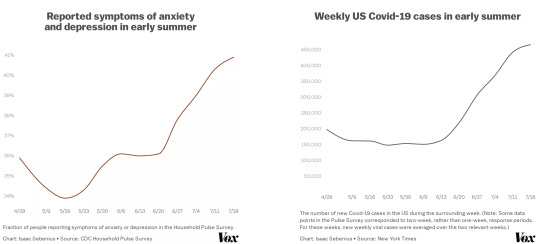
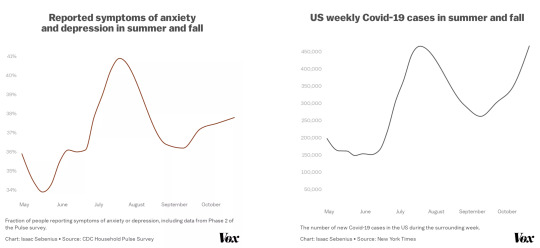
Anxiety and depression are following a remarkably similar curve to Covid-19 cases
Case numbers, positivity rates, deaths, and hospitalizations have become the go-to metrics for tracking the severity of the coronavirus pandemic. But one symptom of the pandemic, impacting both those who’ve had the virus and those who haven’t, has proven more difficult to quantify: deteriorating mental health. Perhaps because of this challenge, it has been largely absent from the messaging and response of public officials.
A close look at Centers for Disease Control and Prevention survey data shows that one measure of mental health is far more intimately tied to the state of the pandemic than previously imagined. In fact, their trajectories align almost exactly.
It is well documented that the coronavirus pandemic has taken a serious toll on emotional well-being. Rates of depression and anxiety in June were three to four times higher than at the corresponding point in 2019, according to the CDC, and deteriorating mental health outcomes have been similarly observed in nations across the world, among them the UK, India, and China. Rates of suicidal ideation, substance abuse, and alcohol consumption are rising steadily.
But the connection is even stronger than you might think in the US: As the number of new cases of the virus fluctuates week to week, our mental health moves in lockstep.
Data available from the Mental Health Household Pulse Survey, run by the CDC, offers a week-by-week estimate of the fraction of Americans who experienced symptoms of anxiety or depression between April 23 and July 21. Comparing this data to the weekly US coronavirus cases over the same time interval reveals an unmistakable trend: The incidence of depressive or anxious symptoms among Americans almost exactly mirrors the trajectory of the US coronavirus curve.
With an r2 value (a standard metric of correlation strength) of 0.92 between new Covid-19 cases and the incidence of anxious or depressive symptoms, the correlation between them is very, very strong.
It is always possible that any correlation could be coincidental rather than causal, or that the link could be more complicated than it seems. Indeed, June and July marked a period of increasing viral spread; one might speculate that, as the pandemic stretched on, public mental health could have correspondingly worsened simply as a function of time or some other factor.
Yet data from the second phase of the Household Pulse Survey, from August through October, showed mental health continued to consistently follow fluctuations in the Covid-19 curve. After the scary viral spike in July, the number of weekly cases declined from roughly 450,000 per week at the end of July to roughly 250,000 by the end of August. And along with this period of slower viral spread, mental health outcomes markedly improved as well, reinforcing the relationship between the two.
Then again, as cases increased during September and October, mental health outcomes correspondingly worsened.
We don’t know yet exactly why reports of mental health issues trace much of the coronavirus curve — whether it is cause and effect, the result of other variables, or some unlikely causal relationship in the other direction. For example, as people become more depressed and anxious, perhaps they seek social interaction more carelessly, generating infection spikes. And the points where the two curves diverge somewhat (e.g., June and late October) show that there are certainly other factors at play.
What is clear is that the rampant spread of the virus is having a major effect on mental health. Overall, the pandemic has raised America’s baseline levels of anxiety and depression: Even at its lowest point this summer (early May), the rate of Americans reporting symptoms of anxiety or depression hovered around 34 percent, roughly three times higher than the average of 11 percent reported in a parallel study between January and June 2019.
Fluctuations above this already-high baseline could plausibly be caused, at least in part, by the severity of the pandemic at a given point in time. For example, elevated rates of viral spread directly increase the likelihood that we or someone we know will become exposed and undergo a mentally straining period of quarantining waiting for symptoms — or self-isolation while battling the new illness itself. The state of the pandemic also often determines things like freedom of mobility through lockdown measures or their absence.
Historically, imposed quarantine has been shown to dramatically affect mental health. Moreover, the perceived trajectory of the pandemic has significant repercussions for the economy and unemployment, both of which have been shown to directly impact mental health.
Covid-19 messaging and policies have fixated on the standard numbers of cases and deaths. But these numbers alone miss out on the very real, very strong connection between the pandemic and our mental health, which is impacting far more people than have been infected with the virus. And it is not only a question of decreased quality of life. Anxiety and depression have been shown to be major drains on the economy as well.
Looking at these charts, it is clear that our mental health traces the coronavirus curve. And just as rising case numbers have had a crushing impact on our psychological health, whatever has led to periods of decreased viral spread (e.g. masks, distancing, and other smart policies) seems to have improved our mental health. Policymakers should take this finding to heart and respond to the pandemic with the emotional well-being of the public in mind.
By Isaac Sebenius (Vox). Top Image credit: Getty Images.
If you or anyone you know is considering suicide or self-harm, or is anxious, depressed, upset, or needs to talk, there are people who want to help:
In the US:
Crisis Text Line: Text CRISIS to 741741 for free, confidential crisis counseling
The National Suicide Prevention Lifeline: 1-800-273-8255
The Trevor Project: 1-866-488-7386
Outside the US → The International Association for Suicide Prevention lists a number of suicide hotlines by country. Click here to find them. Befrienders Worldwide.
75 notes
·
View notes
Text
Root causes of Depression in Hashimoto’s
The link between thyroid function and mental disorders, especially mood disorders, has been known for a long time. Historically, this association was explained more than 200 years ago. - Functional Medicine Doctor Houston
Today, it is widely recognized that thyroid disorders can significantly affect mental states, including emotions and cognition. Both excess and insufficient thyroid hormones can cause mood disorders, including depression, which are usually reversible with proper thyroid treatment. Depression, on the other hand, can be accompanied by subtle thyroid dysfunction.
thyroid problems and mental disorders
Consult Dr. Gupta
Relationship between Depression and Hashimoto’s
Understanding the relationship between the two conditions can help clinicians interpret thyroid function tests in depression, better understand the pathophysiology of both disorders, and identify those who might benefit most from thyroid supplementation.
Clinical depression, or major depression, is a mental disorder characterized by a persistent depressed mood or loss of interest in activities that significantly affect daily life. Depression affects women more than men and the symptoms and severity of depression can vary from person to person.
Depression
Most people don’t know how common Hashimoto’s depression is, but studies have found a link between the presence of mood disorders and the presence of TPO antibodies.
A new study also linked depression, anxiety, obsessive-compulsive symptoms, and anxiety with high levels of TPO antibodies. Antibodies to TPO are an early sign of an autoimmune attack on the thyroid gland, even when a person’s thyroid-stimulating hormone (TSH) levels are still normal.
Schedule a call with Dr. Anshul Gupta
Hashimoto’s disease is a thyroid condition that can cause temporary hyperthyroidism by pumping thyroid hormones into the bloodstream. Agitation, anxiety, and even symptoms of psychosis can occur to anyone who has experienced symptoms of hyperthyroidism (due to the thyroid hormone fluctuations common in Hashimoto’s disease) can explain how terrible it feels.
When thyroid hormone is removed, one may be functionally hypothyroid with symptoms of depression, apathy, low mood, and brain fog. In asymptomatic hypothyroidism, a slight decrease in the secretion of thyroid hormones is accompanied by symptoms of depression and apathy.
thyroid diagnosis
Correct diagnosis of thyroid disease and appropriate treatment can resolve many cases of depression. It may also be necessary to eliminate the cause and effect of thyroid disease to fully restore a healthy and happy state of mind.
There is research that supports the link between mood disorders and Hashimoto's. People who suffer from bipolar disorder are just one (as well as conditions related to depression and anxiety ) were found to have more antithyroid antibodies than other people.)
Hashimoto's disease can be triggered by lithium, which is a medication that is commonly used to treat bipolar disorder. This further complicates the issue.
Psychiatrists who are cognizant of the correlation between the thyroid and mood disorders are more likely to consider thyroid medication for their patients who present with symptoms. Similarly, progressive psychiatrists are more likely to be open to prescribing thyroid medication and will test all patients who present with new-onset depression, anxiety, and mental health symptoms for thyroid disorders.
Consult Functional Medicine Expert
Antidepressants
Antidepressants are favored by conventional doctors in the majority of cases. "Antidepressant" refers to depression-treating drugs.
However, SSRIs are the most prevalent antidepressants. These include Zoloft, Prozac, Celexa, and Paxil, among others. These drugs function by lowering serotonin levels. (our "feel-good hormone")
SNRIs are another commonly prescribed class of antidepressants. ( Inhibitors of serotonin and norepinephrine reuptake) The antidepressants Cymbalta, Effexor XR, and Pristiq are all examples of the class of medications known as "serotonin and norepinephrine reuptake inhibitors." (A chemical that acts as both a neurotransmitter and a hormone within the nervous system). Some of the most common side effects are nausea, sleepiness, tiredness, constipation, and dry mouth.
thyroid levels
Although Antidepressants are not for everyone, a large study that was done in 2006, showed that only 30% of people "responded" to most antidepressants. Furthermore, less than 5% of people were found to be in remission from depression with SSRI drugs, even after using them for an entire year.
Hence, it is important to balance your thyroid levels. To begin with, if your TSH is elevated, you may need to consider thyroid hormone replacement therapy. If you already take thyroid medicine, you may need to change the amount you take to get your TSH levels as low as possible. As far as medications and mood, getting the TSH between 1 and 2 μIU/mL, and in some cases under 1 μIU/mL, helps a person improve their mood symptoms.
Book an expert call with Thyroid Doctor
Hence, there is a correlation between levels that are either too high or too low and an imbalance in the thyroid hormone levels. This imbalance has been linked to a variety of symptoms, including depression and anxiety.
However, it is important to note that despite taking medications such as Synthroid, levothyroxine, or Levoxyl, these symptoms persist in some individuals. T4 isn't enough for everyone.
levothyroxine
Depression is one of the most prominent indicators that a person with thyroid disease is not properly converting T4 to the active T3. If you're taking thyroid medication and still depressed, talk to your doctor about switching. Particularly, antidepressant effects have been observed with T3-containing medications.
Therefore, your symptoms such as depression and other mood-related symptoms may be related to your thyroid, be sure to advocate for thorough lab testing and the appropriate medications. It is recommended that you research the Root Cause Approach to healing Hashimoto's and use interventions such as art therapy, yoga, and exercise to maintain a healthy life.
Suffering from a chronic disease like thyroid, gut problems, weight issues, autoimmune issues, etc... is not easy. Dr. Gupta is a certified Functional Medicine Physician and his personalized plans have helped thousands of people to reclaim their health back.
Now you can get virtual functional medicine consultation from anywhere in the country, especially if you live in Houston, Toledo, Northern Virginia, Los Angeles, NEW YORK & Miami. Please click below to get started with a 15-minute free evaluation call with Dr. Gupta.
For More Info: Functional Medicine Doctor New York
functional health doctor online
Functional Medicine Doctor OH
0 notes
Text
My Endometriosis Journey Part 2:
What is Endometriosis?
“Endometriosis (en-doe-me-tree-O-sis) is an often painful disorder in which tissue similar to the tissue that normally lines the inside of your uterus — the endometrium — grows outside your uterus. Endometriosis most commonly involves your ovaries, fallopian tubes and the tissue lining your pelvis.”
In my last blog post, we learned that I have Stage II, which we will go into more later. I want to outline everything that I know about this in order to raise awareness about it, because it is scarily common in women, and a lot of women may have it and don’t even know. (I will link all of the sources used at the bottom of this post, so you can check them out for yourself!)
Endometriosis affects 1 out of 10 women in childbearing age (2-10% of women). The cause of endometriosis is unknown, and there is currently no cure, although there is treatment. There are some theories as to why endometriosis happens:
1. one theory suggests that during menstruation, some of the tissue backs up through the fallopian tubes, into the abdomen, like a reverse menstruation, where it attaches and grows.
2. another theory suggests that endometrial tissue may travel and implant via blood or lymphatic channels, similar to the way cancer cells spread.
3. a third theory suggests that cells in any location may transform into endometrial cells.
This disease is also genetic, and can appear in families, which is true in my case. My grandmother, mother, aunt, and myself all have a form of this disease.
Endometriosis can be found on the ovaries, the fallopian tubes, ligaments that support the uterus, the space between the uterus and the rectum, the space between the uterus and bladder, the outer surface of the uterus, and the lining of the pelvic cavity. Endometriosis has been found in every organ and anatomical structure in the body, but it is most commonly found in the places listed above. Because it can grow on every organ, this includes the kidneys, eyes, liver, pancreas, brain, bone, heart, skin, and nasal cavity if severe enough.
The symptoms of endometriosis are as follows: pain, especially excessive menstrual cramps that may be felt in the abdomen or lower back, abnormal or heavy menstrual flow, infertility, painful urination during menstrual periods, painful bowel movements during menstrual periods, or other gastrointestinal problems such as diarrhea, constipation, or nausea.
One important thing to note is that the pain that a woman experiences is NOT directly correlated to how severe the disease is. A women with Stage 4 endometriosis may experience no pain whatsoever, whereas a woman with Stage 1 may have inconsolable pain.
There is an important connection to make between women who have endometriosis and those who struggle with infertility. Having endometriosis does not guarantee that you will be infertile, but it does increase your chances. 24-50 percent of women who experience infertility are found to have endometriosis. In these cases, surgery to remove it can restore fertility. In other cases ( a very small percentage) women remain infertile.
Diagnosis begins with a gynecologist completing a physical examination, including a pelvic exam, but can ONLY be certain through a laparoscopic surgery. If the endometriosis is progressed enough, it can be diagnosed just by visually seeing it, but sometimes in stage 1, you may need a biopsy of tissue to determine. A laparoscopy is a minor surgical procedure where a thin tube with a camera is inserted into the abdomen through a small incision.
It is important to note that it takes an average of 7 years. This is insane. Not a lot of women are going to persist through 7 years of doctors in order to get diagnosis, and surgery. It should not be this hard to get a diagnosis, which is why I am trying to raise awareness, because mine took 5 years.
There are four stages of endometriosis, which I will go into further detail. The most common system used is the American Society for Reproductive Medicine Scale (ASRM). The Endometriosis Foundation of America has their own classification, but for my purposes, I will be combining the two in my explanation, because they are similar:
Stage 1 (peritoneal endometriosis): Minimal with few superficial implants. The membrane that lines the abdomen is infiltrated with endometriosis tissue.
Stage 2 (Ovarian Endometriosis): Mild with more and deeper implants. It is established within the ovaries, and these forms of ovarian cysts are of particular concern due to their risk of breaking and spreading endometriosis within the pelvic cavity.
Stage 3 (Deep Infiltrating Endometriosis I (DIE I)): Moderate with many deep implants. Small cysts on one or both ovaries. Presence of filmy adhesions. The first form of deep infiltrating endometriosis involves organs within the pelvic cavity. This can include the ovaries, rectum, uterus, and significantly distort the anatomy of the pelvic organs.
Stage 4 (Deep Infiltrating Endometriosis II (DIE II)): Severe with many deep implants. Large cysts on one or both ovaries and many dense adhesions. The other more extreme form of Deep Infiltrating Endometriosis involves organs both within and outside of the pelvic cavity. This can include bowels, appendix, diaphragm, heart and lungs, among others.
Remember, that the stage of the disease does not correlate with the amount of pain that the woman experiences.
*Personally I do not like that they use the acronym DIE in the classifications. OOF.
If a laparoscopic surgery does not succeed, a laparotomy (a more extensive surgery) can be used to remove as much of the tissue as possible without damaging healthy tissue. If this is not successful, many women use a hysterectomy to remove the uterus and possibly the ovaries to prevent tissue from growing back.
A lot of treatment for endometriosis is pain management, and laparoscopic surgery to remove the disease. There is no official cure.
If you think you have endometriosis, please reach out to your OBGYN, and if you are in the South Central Pennsylvania Region, please reach out to Dr. Harkins, he is an amazing doctor that has helped many women already, including myself.
You are not alone. This disease affects all and everyone. Here are some celebrities with endometriosis: Amy Schumer, Tia Mowry-Hardrict, Lena Dunham, Chrissy Teigen, Mandy Moore, Julianne Hough, Halsey, Whoopi Goldberg, and Alaia Baldwin Aronow.
Sources:
https://www.hopkinsmedicine.org/health/conditions-and-diseases/endometriosis
http://nezhat.org/endometriosis-treatment/where-does-endometriosis-grow/#:~:text=Endometriosis%20has%20been%20found%20in,anatomical%20structure%20in%20the%20body.
https://www.advancedgynaecologymelbourne.com.au/endometriosis/stages
https://academic.oup.com/humrep/article/18/4/756/596537
https://www.everydayhealth.com/endometriosis/living-with/celebrities-who-speak-endometriosis/
Some great social media resources if you want to do your own research:
@/endohealthhub on Instagram
@/endometriosismemes on Instagram
@/endogirlgang on Instagram
@/chronicallyillgoddess on Instagram
@/endohumour on Instagram
@/the_endo_space on Instagram
‘The Endo Space’ Group on Facebook
‘Endometriosis Support Group’ Group on Facebook
‘Undiagnosed Illness Support Group’ Group on Facebook
and if you are in South Central Pennsylvania, check out ‘Central PA Endometriosis Support Network’ Group on Facebook.
#endometriosis#endometriosis diagnosis#endometriosis awareness#diagnosis#endometriosis support#endometriosis sources#endometriosis research#sierrabed
5 notes
·
View notes
Text
Common Risk factors or symptoms for Kidney Stones?
Kidney stones (also called renal calculi, nephrolithiasis, or urolithiasis) are hard deposits made of minerals and salts that form inside your kidneys. A small, hard deposit that forms in the kidneys and is often painful when passed. Kidney stones are hard deposits of minerals and acid salts that stick together in concentrated urine. They can be painful when passing through the urinary tract, but usually don’t cause permanent damage.
The most common symptom is severe pain, usually in the side of the abdomen, that’s often associated with nausea.
Diet, excess body weight, some medical conditions, and certain supplements and medications are among the many causes of kidney stones. Possible causes include drinking too little water, exercise (too much or too little), obesity, weight loss surgery, or eating food with too much salt or sugar. Infections and family history might be important in some people. Eating too much fructose correlates with increasing risk of developing a kidney stone.
URRICALI TABLETS
Treatment includes pain relievers and drinking lots of water to help pass the stone. Medical procedures may be required to remove or break up larger stones.
There are different types of kidney stones. The cause of the problem depends on the type of stone.
Stones can form when urine contains too much of certain substances that form crystals. These crystals can develop into stones over weeks or months.
Calcium stones are most common. They are most likely to occur in men between ages 20 to 30. Calcium can combine with other substances to form the stone.
Oxalate is the most common of these. Oxalate is present in certain foods such as spinach. It is also found in vitamin C supplements. Diseases of the small intestine increase your risk for these stones.
Calcium stones can also form from combining with phosphate or carbonate.
Other types of stones include:
Cystine stones can form in people who have cystinuria. This disorder runs in families. It affects both men and women.
Struvite stones are mostly found in men or women who have repeated urinary tract infections. These stones can grow very large and can block the kidney, ureter, or bladder.
Uric acid stones are more common in men than in women. They can occur with gout or chemotherapy.
Other substances, such as certain medicines, also can form stones.
The main symptom is severe pain that starts and stops suddenly:
Pain may be felt in the belly area or side of the back.
Pain may move to the groin area (groin pain), testicles (testicle pain) in men, and labia (vaginal pain) in women.
Other symptoms can include:
Abnormal urine color
Blood in the urine
Chills
Fever
Nausea and vomiting
Lithotriptic:
Having the quality of or used for dissolving or destroying stone in the bladder or kidneys.
Lithotriptic agents are an agent that affects the dissolution of a calculi.
Urricali tablet & syrup is a natural Lithotriptic. It facilitates the passage of urinary calculi by diuretic action. Apart from disintegration of stones and flushing them out, Urricali tablet & syrup also prevents their recurrence. It also effectively cures and prevents urinary tract infections. Urricali perceptively encourages a healthy urinary tract and helps to keep up a normal urine composition and add mucosal integrity. Urricali tablets & syrup possess antispasmodic and anti-inflammatory properties which helps to reduce ureteric colic and ease the condition of sore and burning micturition.
To know more: https://lamarworld.co/product/urricali-tablets-60s/

0 notes