#concussiontreatment
Text

Healing Minds, Restoring Balance: A Guide to Concussion Physiotherapy
Trust Vertex Physio for comprehensive concussion management Physiotherapy edmonton. Receive safe and effective rehabilitation for optimal recovery. Contact us for specialized care.Contact us: https://usmansamad.com/healing-minds-restoring-balance-a-guide-to-concussion-physiotherapy/ , (825) 525-2852, [email protected]
#concussionmanagement#edmonton#physiotherapy#concussiontreatment#headinjury#sportsconcussion#braininjury#concussionrecovery#postconcussionsyndrome#concussiontherapy#headtrauma#concussionassessment#neurologicalrehabilitationt#vestibularrehabilitation#concussionspecialists#cognitiverehabilitation
0 notes
Text
What the world knows that the VA does not: Hyperbaric Oxygen Therapy is safe, effective and can restore health

Athletes are waking up to the Use of Hyperbaric Oxygen Therapy for brain wound healing, health, endurance, peak performance, and the competitive edge.
Game Changer for Football Teams?
A high-profile college football program began using HBOT to manage player injuries and fatigue. The therapy quickly became a key factor in their injury management and prevention strategy. The team noted shorter recovery periods after injuries, and players were able to return to play faster than before, demonstrating HBOT's efficacy in a high-contact sports environment. Numerous professional athletes use HBOT.
100 Yards of Wellness Will Offer HBOT to Clemson Athletes
Nov 22, 2022
100 Yards of Wellness, Clemson’s new $4.9-million wellness space at Allen N. Reeves Football Complex that spans roughly 300 feet in length that has become a central hub of activity and major point of pride for Tiger football. The treatment and training room area includes all requisite athletic training resources, including a
diagnostic office with a full digital X-ray space and diagnostic ultrasound, general medical exam room, 30 yards of turf and hydrotherapy areas, including two underwater treadmills. Among the many features of the recovery center are:
• A hyperbaric chamber to create a pressurized environment for concentrated oxygen intake.
• A cryotherapy chamber for muscle recovery through extreme cold temperature exposure.
• A sensory deprivation float tank that houses 1,200 pounds of Epsom salt dissolved in water at skin temperature to remove athletes from light, sound and some gravitational force.
• Infrared hyperthermic Cocoon pods for Far-Infrared light therapy and vibrational massage.
• Photobiomodulation therapy beds that leverage multiple wavelengths of infrared light to reduce oxidative stress.
• Numerous massage chairs, including both percussive massage and hydromassage options.
• Percussive Hypervolt massage guns.
• Dedicated tables and space for practitioner-assisted stretching, percussive massage gun therapy and Normatec compressive sleeves provided to each player prior to the season.
• Functional testing equipment to obtain objective information on student-athlete muscle and joint function that can be used for injury prevention and return-to-play purposes.
The Rise of Hyperbaric Oxygen Therapy in Professional Football: A Game-Changer for Recovery and Performance
Sep 5, 2023
By Mudassir Sajad
In the fast-paced world of professional football, where every second counts, players are constantly seeking ways to gain a competitive edge. One such method that has been gaining traction is Hyperbaric Oxygen Therapy (HBOT). This innovative treatment has been endorsed by top-tier athletes like Mo Salah, Marcus Rashford, Vinicius Junior, and Neymar, who have all been spotted on social media using hyperbaric chambers Hyperbaric Oxygen Therapy is proving to be a revolutionary treatment in the realm of
professional football. Mo Salah, Marcus Rashford, Vinicius Junior, and Neymar endorsing its benefits, it's clear that HBOT is more than just a passing trend. Moreover as science continues to validate its efficacy, we can expect to see more football clubs
adopting this cutting-edge technology to give their players the competitive edge they need.
Dr. Joe Maroon on Hyperbaric Oxygen
Dr Joe Maroon Joseph Maroon is an American neurosurgeon, author, and triathlon athlete. He is the professor and vice chairman of the Department of Neurological Surgery at the University of Pittsburgh Medical Center and is the current medical director of WWE. For over 20 years he has served as the neurosurgical consultant to professional and college athletes in football, baseball, golf, hockey and soccer and was team neurosurgeon to the Pittsburgh Steelers for over 40 years.
As early as 2011, Dr Maroon and Dr Bost wrote: "Alternative nonpharmaceutical treatments appear to be gaining acceptance for the treatment of common neurodegenerative conditions, memory decline, and reduced cognitive function. Substantial animal and human research now suggests that these same natural dietary supplements, vitamins and minerals, and the use of hyperbaric oxygen may be a better first-line choice for the treatment of PCS, which has generally been underreported by both athletes and the military."
Maroon and Bost, Concussion Management at the NFL, College, High School, and Youth Sports Levels. Clinical Neurosurgery. Volume 58, 2011, Chapter. 7.
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma. www.treatnow.org
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#CTE#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#PostconcussionSyndrome#TBI#TBItreatment#traumaticbraininjury
0 notes
Text
Concussion Physiotherapy Windermere | Momentum Physiotherapy Windermere
Navigate your journey to recovery with specialized Concussion Physiotherapy Windermere at Momentum Physiotherapy! Our experts are here to support your complete concussion management. Contact us at +1 (587) 400-1113 or visit https://bitly.ws/YkFc for personalized care.
#concussionphysiotherapywindermere#physiotherapistwindermere#momentumphysiotherapywindermere#concussiontreatment#windermerehealth#braininjuryrehab#concussionrecovery#momentumphysio#headinjurycare#neurorehab#windermerewellness#headtraumarecovery#brainhealth#concussionsupport#therapyforconcussion#mindfulrecovery
0 notes
Text

Welcome to Magnus Rehab, the leading rehabilitation center specializing in concussion treatment in Brampton. We understand the unique challenges that come with concussions and are committed to providing comprehensive care to help patients on their journey to recovery.
At our state-of-the-art clinic, we offer specialized concussion treatment in Brampton that combines physiotherapy, occupational therapy, and neurocognitive training. Our team of experienced professionals is dedicated to addressing all aspects of concussion recovery, ensuring that each patient receives personalized care tailored to their specific needs.
Our multidisciplinary approach allows us to holistically address the physical, cognitive, and emotional aspects of concussions. Through physiotherapy, we focus on restoring strength and mobility while reducing pain and inflammation. Occupational therapy helps individuals regain their independence and return to daily activities by focusing on improving cognitive function and developing coping strategies.
Neurocognitive training plays a crucial role in our concussion therapy in Brampton. This specialized form of training targets cognitive deficits caused by concussions and helps individuals regain mental clarity, memory function, attention span, and problem-solving skills.
At Magnus Rehab, we believe that every individual deserves the highest quality of care when it comes to concussion treatment. Our team is committed to staying up-to-date with the latest research and advancements in the field of concussion care to ensure that our patients receive the best possible outcomes.
If you or a loved one is seeking professional concussion treatment in Brampton, look no further than Magnus Rehab. Contact us today to schedule a consultation and take the first step towards a full recovery.
0 notes
Text
Who Is A Concussion Specialist?
It is becoming increasingly common for primary care physicians to refer patients with concussion symptoms to a specialist. These professionals have extensive experience in conflict management and understand the specific needs and concerns of competing athletes.
A concussion Specialist helps patients create and follow an effective recovery plan based on their age, activity level, work or school plan, symptoms, and other factors. Proper treatment and a proper management plan can speed up recovery and produce better results.
Symptoms of Concussion
According to the DFW clinic, symptoms and signs of a concussion may be subtle and may not immediately appear. Symptoms can be last for days, weeks, or even longer, not fixed.
Common symptoms after traumatic brain injury are headache, loss of memory (amnesia), and confusion. Amnesia usually involves forgetting an event that caused a concussion.

Physical symptoms and signs of a concussion may include:
A headache
It's ringing in my ears
Nausea
Vomiting
Tiredness or drowsiness
Sight is dim
Other signs and symptoms of concussion include:
Confusion or a fog
Amnesia surrounding a traumatic event
Dizziness or "seeing the stars."
A witness can see the following signs and symptoms in an unconscious person:
Temporary Loss (although this does not always happen)
Unexplained speech
Delay in answering questions
Surprised appearance
Forgetting, like asking the same question over and over again
You may experience symptoms of conflict immediately, and some may occur within days after the injury, such as:
Focusing complaints and memory
Anger and other personality changes
Sensitivity to light and noise
Sleep disturbances
Psychological problems and depression
Disorders of taste and smell
Risk factors
Activities that may increase your risk of concussion according to the DFW clinic include:
Fall, especially in children and adults
Participating in a high-risk sport, such as soccer, hockey, soccer, rugby, boxing, or other social media
Participating in high-risk sports without proper safety and surveillance equipment
Involvement in car crashes
Being in danger of pedestrians or cyclists
To be a soldier in the war
Being a victim of physical abuse
He has had a conflict in the past
Specialist or concussion center?
In recent years, various multidisciplinary sports concussion centers have delivered around the U.S. & centers incorporate many specialists into one clinic.
For example, rehabilitation centers in Fort Worth Texas provide patients with access to neurologists, sports medicine physicians, neuropsychologists, physiatrists, physical therapists, and other specialized physicians who have concussion training and expertise.
When they work together, these specialists can offer more comprehensive care. Some people may be particularly well-served by an entire team of specialists, including:
People who have a history of concussion
People who are at high risk for more skull injuries
People who have other health issues
Team specialists can address the different health issues caused or exacerbated by a concussive event. Rehabilitation centers in Fort Worth Texas provide required rehabilitation for concussion patients.
Imaging testing
A brain scan may be recommended for some people with symptoms and signs such as severe headaches, fainting, repeated vomiting, or worsening symptoms. Imaging the brain may determine the severity of the injury and may cause bleeding or inflammation of the skull.
Cranial computerized tomography (CT) scan is a common practice in adults to examine the brain after an injury. CT scans use a series of X-rays to obtain various images of your skull and brain.
In children suspected of fainting, CT scans are only preferred if certain conditions, such as the type of injury or symptoms of a fracture, are met. It is to avoid exposure to radiation in young children.
Magnetic resonance imaging (MRI) identifies changes in your brain or identifies potential problems after a collision. MRI uses powerful magnetic and radio waves to generate detailed and precise images of your brain.
Conclusion
A concussion is a painful brain injury that affects the functioning of your brain. Outcomes are usually temporary but may include headaches and problems with concentration, memory, balance, and communication.
A blow to the head generally causes a concussion. Shaking the head and upper body can also cause friction. Some abrasions cause you to lose consciousness, but most do not. Fall is a very natural cause of concussion.
Concussions are also common while playing a rough game, such as soccer. Most people usually recover completely after a concussion. So it’s good to visit a concussion Specialist who will provide comprehensive care and focus on rehabilitating athletes in sports, work, and school.
#concussion#concussiontest#concussiontreatment#concussionspecialist#concussiondoctors#Healthcare#health services#tumblr
1 note
·
View note
Text
Benefits of Hyperbaric Oxygen Therapy for Concussion.
Let’s talk about concussions. A concussion is a mild brain injury from some form of trauma to the head. We typically associate it with sports injuries like football, soccer, or boxing, but it can also happen from falling and hitting your head or getting in a car accident. Common symptoms of a concussion are headache, dizziness, problems with memory, anxiety, difficulty concentrating and more. Most concussions will heal on their own within a few days to weeks. However, it is becoming more common to have a post-concussive syndrome that can last for months.
For more detail click: http://o2underpressure.com/benefits-of-hyperbaric-oxygen-therapy-for-concussion/
#HyperbaricOxygenTherapy#hbot#oxygentherapy#Concussion#Concussiontreatment#injuries#o2underpressure#losangelestherapist#o2up
0 notes
Photo

Post Concussion Rehabilitation | Physiotherapy in Ottawa | RBH Physiotherapy
At RBH, the best concussion treatment center in Ottawa, we use various concussion physiotherapy treatment techniques including to help you with the situation.
Post Concussion Rehabilitation services following a brain injury is focused on the client’s individual needs and symptoms.
Get in touch for details.
Website: https://www.rbhphysiotherapy.com/post-concussion/
Email id : [email protected]
Contact No. : 613-422-5566
Addrs : 1797 Kilborn Ave, Ottawa, ON K1H 6N1
#postconcussionrehabilitation#concussiontreatment#consussiontreatmentinottawa#concussionrehab#physicaltherapyinottawa#physiotherapyinottawa
0 notes
Photo

Concussion Treatment at Ottawa | Concussion Treatment | Care2cure Physiotherapy
At Care to cure, the experts create comprehensive treatments that will not only help you reach your wellness goals but will help sustain a healthy and balanced lifestyle. Care2cure provides concussion treatment Ottawa at affordable price.
Get in touch with us to understand more.
Website : https://www.care2curephysiotherapy.com/concussion-treatment-ottawa-concussion-treatment-in-ottawa/
For appointments: https://www.care2curephysiotherapy.com/book-appointment/
Drop a line at : (Prince of Wales) 613-695-7733/ (Barrhaven) 613-440-6600
For Inquiries Mail us at : [email protected]
#concussion treatment at ottawa#ottawa rehab centre#physiotherapyclinicsottawa#physiotherapistsottawa#ConcussionTreatment
0 notes
Photo

Photobiomodulation & Light Therapy in action! If you are dealing with skin disorders, cognitive decline, post concussion syndrome symptoms, chronic pain, inflammation, over use injuries, broken bones, muscle strains and or you just want to increase your strength and conditioning gains reach out and we will laser you and hook you up to the polychromatic light therapy! #lighttherapy #photobiomodulationtherapy #photobiomodulation #healinjuries #cognitiveperformance #sportspsychpaige #concussiontreatment #healfaster #overuseinjuries #performanceneurotraining #beonpoint (at Bellevue, Washington) https://www.instagram.com/p/B0Cm9Veg8j_/?igshid=1w80stdwizk6j
#lighttherapy#photobiomodulationtherapy#photobiomodulation#healinjuries#cognitiveperformance#sportspsychpaige#concussiontreatment#healfaster#overuseinjuries#performanceneurotraining#beonpoint
0 notes
Photo
If you or a loved one have suffered a brain injury from a concussion, an experienced personal injury attorney at The Trost Law Firm can answer your questions. Call us today.https://www.trostlaw.com/personal-injury/
0 notes
Link
Here's a closer look at concussions and where you should go for medical attention.
0 notes
Text
CONCUSSION- Ayurvedic Treatment, Diet, Exercises, Research Papers, Yoga & Pranayama
CONCUSSION- Ayurvedic Treatment, Diet, Exercises, Research Papers, Yoga & Pranayama
A concussion is a traumatic brain injury caused by a violent blow to the head or shaking of the head.
SIGNS AND SYMPTOMS OF CONCUSSIONCAUSES OF CONCUSSIONPATHOPHYSIOLOGY OF CONCUSSIONDIAGNOSIS OF CONCUSSIONTREATMENTS FOR CONCUSSIONPROGNOSIS OF CONCUSSIONCOMPLICATIONS OF CONCUSSIONCONCUSSION AND AYURVEDANIDANA- AYURVEDIC CAUSES OF CONCUSSIONPURVAROOPAM- AYURVEDIC PREMONITORY SYMPTOMS OF…
View On WordPress
0 notes
Text
CTE Plagues Heisman Trophy Winners and Families

Three-quarters of 1,035 brains of football players -- over 700
--examined at Boston University had CTE
The "taboo topic" is the centerpiece of "The Other Heisman Club" in the Washington Post, Dec 9, D1, by Kent Babb: the number of former Heisman winners with diagnosed or suspected Chronic Traumatic Encephalopathy (CTE). The degenerative brain disease is increasingly in the news for a number of reasons.
Four Heisman winners have been posthumously diagnosed with the disease: Howard Cassady, Pat Sullivan, Paul Hornung and Charles White. The implication in the article is that more winners already exhibit symptoms of CTE but whose families can't "know" until after death. But the families know.
Something is wrong. Sadly, silence is the preferred approach. And the unwillingness of our society to confront the obvious doesn't make it any easier. And the "whistling through the graveyard" approaches to concussions and the Concussion Protocols used worldwide don't provide much guidance about an alternative approach to Brain wounding. Facts matter:
- Four percent of Heisman trophy winners died of CTE, and the list of their wounded fellow winners is growing. If you extrapolate those numbers to the 25,000 former NFL players, over 1,000 of them are probably carrying the CTE markers.
- Three-quarters of 1,035 brains of football players, 0ver 700, examined at Boston University had CTE.
- Researchers at Boston University found CTE in 92 percent of former NFL players who were analyzed: they analyzed the brains of 376 deceased former NFL players and diagnosed 345 of them with chronic traumatic encephalopathy.
- More than half of the homeless have experienced traumatic brain injury and 1 in 4 have had moderate to severe brain injuries.
- Approximately 876,450 post-9/11 veterans suffer from untreated brain wounds.
- Researchers estimate that as many as 60% of incarcerated individuals are living with TBI, significantly higher than the 8.5% reported in the general population.
- Studies on prison and jail populations have reported a range of 25-87% of inmates reporting head injuries or TBI.
Of course, it is traditional to attack these numbers. Nay-sayers will demand more research. Hand-wringing by stake-holders on both sides will, like protests after mass-shootings, last a while and then subside. If anything, more dollars will go into researching how to make contact sports more safe. And treatments that are non-pharmaceutical will be ignored. Since "everyone knows there's no treatment for brain injuries," the best we can hope for from the medical profession is contained in the latest proceedings out of Boston.
The Robert C. Cantu Concussion Summit was held on December 8, 2023, at the Cantu Concussion Center at Emerson Hospital in Concord, MA. The theme of the conference was "Prevention of Concussion and Long-Term Effects of Repetitive Traumatic Brain Injury (RTBI)." In what is becoming a repetitive list of findings, the conference summarized:
- Eliminate intentional or avoidable head impact in contact and collision sports in both practices and games.
- Encourage policies and rules that limit the number, duration, and intensity of contact sport practices.
- Reinforce proper and safer techniques that avoid head contact at all levels of play.
- Implement rules of play that reduce and penalize intentional or avoidable contact to the head and neck.
- Correlating specific clinical symptoms with CTE neuropathology remains an important area for further investigation.
- Improve the criteria for Traumatic Encephalopathy Syndrome (TES) through further research.
Feel better? More importantly, if you are the parent of someone with a brain wound, what actionable intelligence can you take from that list? How will that list help you and yours deal with the here-and-now of a TBI/Concussion-suffering loved-one? If you'd like to learn more about what is happening, and what you can do, view this earlier Blog. Additional information is here.
Below is an insightful film about brain wounds
https://youtu.be/Zzbxrnm7jXc?si=IPKC5InadR0Eho52
https://treatnow.org/brain-wound-update-5-concussion-blast-tbi-cte/
The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help heal the effects of BLAST injury, TBI/PTSD, and acute concussion.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#CTE#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#PostconcussionSyndrome#TBI#TBItreatment#traumaticbraininjury
0 notes
Photo
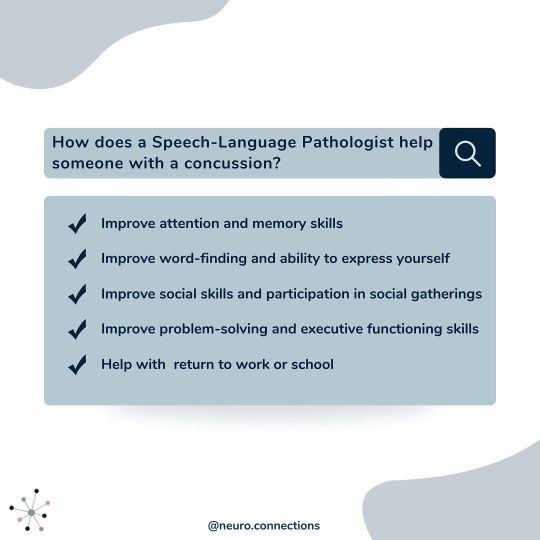
Reposting @neuro.connections Many who experience prolonged concussion symptoms experience changes in cognitive ability - trouble with attention, memory, problem-solving, reasoning and executive functioning skills. These changes impact our ability to communicate effectively and efficiently. ⠀ ⠀ SLPs can help with:⠀ 📌Improving attention and concentration⠀ 📌Following a conversation⠀ 📌Understanding implied or complex information⠀ 📌Remember new conversations or information⠀ 📌Word-finding and expressing oneself⠀ 📌Generating ideas or topics of conversation⠀ 📌Focusing on relevant information or summarizing information⠀ 📌Reading and retaining what has been read⠀ 📌Writing and organizing thoughts in writing⠀ 📌Improve planning, organizing, prioritizing tasks⠀ 📌Weighing options and decision-making⠀ 📌Picking up on nonverbal cues, taking turns, not interrupting during a conversation⠀ 📌And more!⠀ ⠀ SLPs with the knowledge and clinical experience in cognition and communication AND concussion management can help improve these skills!⠀ ⠀ We offer online services to all individuals in Ontario and are currently accepting new clients in January! Book a complimentary call to learn more. Email me directly at [email protected]⠀ .⠀ .⠀ .⠀ .⠀ #virtualtherapy #onlinetherapy #toronto #ontario #onlinespeechtherapy #concussion #concussionrecovery #cognitivecommunication #cognitiverehab #postconcussionsymptoms #pcs #concussionrehab #braininjuryrehab #braininjuryawareness #braininjuryrecovery #concussionawareness #tbisurviver #concussiontreatment #mildtraumaticbraininjury #concussiontherapy #medslp #privatepracticeslp #speechlanguagepathology #slpsofinstagram #slpgradstudent #speechies #slp2b #slp2be — view on Instagram https://ift.tt/3JUxPOc
0 notes
Photo

Homeopathy often excels in areas where mainstream medicine has little to offer. Concussion is a good example of this. Aside from high tech measuring and monitoring, mainstream medicine usually takes a wait and watch approach to concussion. I seem to have had more than my fair share of concussion cases, and have been quite amazed at how effective homeopathy has been in turning these cases around. The story I want to tell today is about Jennifer (name changed to preserve confidentiality). Jennifer had an accident – she ran into a wall, passed out from the impact, tried to get up, and then fell on her head again. She vomited twice at the time. She came to me a number of weeks later, complaining of general confusion; overwhelmed with constant crying; oversensitivity; intense headaches with the sensation that her head was in a vice, made worse from thinking, looking at a screen, reading; terrible memory; nausea; generally, an inability to live any part of her life with enormous despair at how she would ever get her old life back again. I gave Jennifer a remedy with instructions to take it before bed. She called me the next morning, sounding much brighter, and told me that she woke at 1 am with the strangest sensation that she could feel the synapses in her brain moving, shifting, reconnecting and healing. She woke feeling almost 100%. This case remains one for the books. The brain is an amazing organ, and homeopathy an amazing medicine. Thank you Beth for an awesome case. To read the whole thing, please see: http://www.blh-homeopath.com/blog/ @homeopathy_school_in_toronto . . #pilhomeopathy #learnhomeopathy #homeopathy #homeopathic #homeopati #homeopatia #homeopatía #homeopathie #homeopath #homeopathicmedicine #homeopata #homeopathicremedy #homeopathichealth #homeopathyworks #homeopathyheals #homeopathyrocks #homeopathyforall #homeopathyworksforme #traditionalmedicine #integratedmedicine #tryhomeopathy #nourishyourbody #concussionrehab #naturalmedicines #concussiontreatment #natureheals #wellbeingwarrior #concussionrecovery #concussion #concussionssuck (at Toronto , Ontario , Canada , North America , Earth , Galaxy , Etc :P) https://www.instagram.com/p/B7lNkPQludF/?igshid=1rrxk10eupxpc
#pilhomeopathy#learnhomeopathy#homeopathy#homeopathic#homeopati#homeopatia#homeopatía#homeopathie#homeopath#homeopathicmedicine#homeopata#homeopathicremedy#homeopathichealth#homeopathyworks#homeopathyheals#homeopathyrocks#homeopathyforall#homeopathyworksforme#traditionalmedicine#integratedmedicine#tryhomeopathy#nourishyourbody#concussionrehab#naturalmedicines#concussiontreatment#natureheals#wellbeingwarrior#concussionrecovery#concussion#concussionssuck
0 notes
Text
Neuropathologic and Clinical Findings in Young Contact Sport Athletes Exposed to Repetitive Head Impacts

August 28, 2023
Ann C. McKee, MD1,2,3,4,5,6,7; Jesse Mez, MD, MS2,3; Bobak Abdolmohammadi, BA2; et alMorgane Butler, BSc2,8; Bertrand Russell Huber, MD, PhD1,2,3,5,6; Madeline Uretsky, MS2; Katharine Babcock, PhD2,8; Jonathan D. Cherry, PhD1,2,4; Victor E. Alvarez, MD1,2,3,5; Brett Martin, MS2,9; Yorghos Tripodis, PhD2,7,9; Joseph N. Palmisano, MS2,9; Kerry A. Cormier, BA1,2,5; Caroline A. Kubilus, BA2,5; Raymond Nicks, MS1,2,3,5; Daniel Kirsch, BA2,4; Ian Mahar, PhD2; Lisa McHale, EdS2,10; Christopher Nowinski, PhD2,10; Robert C. Cantu, MD2,10,11,12; Robert A. Stern, PhD2,3,12; Daniel Daneshvar, MD, PhD2,13; Lee E. Goldstein, MD, PhD2,14,15; Douglas I. Katz, MD3,16; Neil W. Kowall, MD2,3; Brigid Dwyer, MD3,16; Thor D. Stein, MD, PhD1,2,4,5; Michael L. Alosco, PhD2,3
Author Affiliations Article Information
JAMA Neurol. Published online August 28, 2023. doi:10.1001/jamaneurol.2023.2907
Audio (16:39)
Neuropathologic and Clinical Findings in Athletes With Repetitive Head Impacts
Key Points
Question What are the neuropathologic and clinical findings in a convenience sample of young, deceased, symptomatic contact sport athletes?
Findings In this case series of 152 contact sport athletes younger than 30 years at the time of death, chronic traumatic encephalopathy (CTE) was found in 63 (41.4%), with nearly all having mild CTE (stages I and II). Neuropathologic abnormalities associated with CTE included ventricular enlargement, cavum septum pellucidum, thalamic notching, and perivascular pigment–laden macrophage deposition in the frontal white matter.
Meaning These findings confirm that CTE and other brain pathologies can be found in young, symptomatic contact sport athletes, but the clinical correlates of these pathologic conditions are uncertain.
Abstract
Importance Young contact sport athletes may be at risk for long-term neuropathologic disorders, including chronic traumatic encephalopathy (CTE).
Objective To characterize the neuropathologic and clinical symptoms of young brain donors who were contact sport athletes.
Design, Setting, and Participants This case series analyzes findings from 152 of 156 brain donors younger than 30 years identified through the Understanding Neurologic Injury and Traumatic Encephalopathy (UNITE) Brain Bank who donated their brains from February 1, 2008, to September 31, 2022. Neuropathologic evaluations, retrospective telephone clinical assessments, and online questionnaires with informants were performed blinded. Data analysis was conducted between August 2021 and June 2023.
Exposures Repetitive head impacts from contact sports.
Main Outcomes and Measures Gross and microscopic neuropathologic assessment, including diagnosis of CTE, based on defined diagnostic criteria; and informant-reported athletic history and informant-completed scales that assess cognitive symptoms, mood disturbances, and neurobehavioral dysregulation.
Results Among the 152 deceased contact sports participants (mean age, 22.97 years; 141 male) included in the study, CTE was diagnosed in 63 (41.4%; median age, 26 years). Of the 63 brain donors diagnosed with CTE, 60 (95.2%) were diagnosed with mild CTE (stages I or II). Brain donors who had CTE were more likely to be older (mean difference, 3.92 years; 95% CI, 2.74-5.10 years) Of the 63 athletes with CTE, 45 (71.4%) were men who played amateur sports, including American football, ice hockey, soccer, rugby, and wrestling; 1 woman with CTE played collegiate soccer. For those who played football, duration of playing career was significantly longer in those with vs without CTE (mean difference, 2.81 years; 95% CI, 1.15-4.48 years). Athletes with CTE had more ventricular dilatation, cavum septum pellucidum, thalamic notching, and perivascular pigment-laden macrophages in the frontal white matter than those without CTE. Cognitive and neurobehavioral symptoms were frequent among all brain donors. Suicide was the most common cause of death, followed by unintentional overdose; there were no differences in cause of death or clinical symptoms based on CTE status.
Conclusions and Relevance This case series found that young brain donors exposed to repetitive head impacts were highly symptomatic regardless of CTE status, and the causes of symptoms in this sample are likely multifactorial. Future studies that include young brain donors unexposed to repetitive head impacts are needed to clarify the association among exposure, white matter and microvascular pathologic findings, CTE, and clinical symptoms.
Introduction
Across the world, millions of people are exposed to repetitive head impacts (RHIs) through participation in contact and collision sports, military service, physical violence, and many other activities.1-6 Repetitive head impacts can result in symptomatic concussions and the much more frequent, nonconcussive injuries that are asymptomatic.7 Sustained exposure to RHIs can produce persistent cognitive and neuropsychiatric symptoms8-11 and a progressive, tau-based neurodegenerative disease, chronic traumatic encephalopathy (CTE).12-21 Multiple studies13,15,22 link a longer duration of RHI exposure in US football players with increased odds for the presence of CTE and increased severity of CTE. In older American football players with pathologically diagnosed CTE, RHI exposure is also associated with white matter rarefaction,23-25 loss of myelin associated proteins,26 and oligodendrocyte loss.27 Emerging data show structural white matter alterations on magnetic resonance imaging (MRI) in young, active, and recently retired contact sport players exposed to RHI,1,2,28-30 although the pathologic condition underlying these changes is unclear.
A definitive diagnosis of CTE requires neuropathologic evidence of perivascular hyperphosphorylated tau (p-tau) aggregates in neurons, with or without astrocytes, typically at the depths of the sulci in the cerebral cortex.31,32 The clinical syndrome associated with CTE is known as traumatic encephalopathy syndrome (TES).8,33 On the basis of the National Institute of Neurological Disorders and Stroke (NINDS) consensus diagnostic criteria for TES,8 the core clinical features of TES include cognitive impairment, especially episodic memory and executive dysfunction, and neurobehavioral dysregulation, such as impulsivity, explosivity, and emotional dysregulation.8 Supportive features include delayed onset (ie, core clinical features starting years after RHI exposure ends), parkinsonism, other motor signs (including amyotrophic lateral sclerosis), depression, anxiety, apathy, and paranoia.
The Understanding Neurologic Injury and Traumatic Encephalopathy (UNITE) Brain Bank1 has harvested brains from more than 1350 donors exposed to RHIs who are considered at risk for CTE. Brain donors in the UNITE bank vary widely in age at death and include teenagers and young adults. Chronic traumatic encephalopathy has been reported in individuals as young as 17 years,13 yet, to date, there have been no large-scale neuropathologic and clinical studies of young individuals exposed to RHIs. Attention to this age group has several important implications. The study of young athletes allows insight into the earliest features of RHI-induced neuropathologic injury and CTE. Furthermore, it allows analysis in the absence of common age-associated comorbidities. Moreover, most of these young contact sport athletes played only at amateur levels, as part of teams affiliated with educational institutions; consequently, the study of young athletes adds to our understanding of the long-term consequences of amateur contact sports participation. In this report, we describe the neuropathologic and clinical features of 152 brain donors from the UNITE brain bank who were younger than 30 years at the time of death.
Methods
Brain Donors and Study Design
The initial sample for this case series included 156 deceased individuals with a history of exposure to RHIs from contact sports participation who donated their brain to the UNITE Brain Bank from February 1, 2008, to September 31, 2022, and were younger than 30 years at the time of death. Race was determined by next-of-kin report and was included to understand the representativeness of the sample and the associated generalizability of the results. Procedures of brain donation have been previously described.14,34 The inclusion criterion was based on the presence of a history of exposure to RHIs without regard to symptom status. The restriction to brain donors younger than 30 years was selected to minimize any contribution from age-related conditions. Donors were excluded for poor tissue quality. Four donors were excluded because of incomplete brain fragments or prolonged premortem hypoxia, resulting in a final sample size of 152. Institutional review board approval for brain donation, postmortem clinical record review, interviews with informants, and neuropathologic evaluation was obtained through the Boston University Medical Campus and the Veterans Affairs Bedford Institutional Review Board. The next of kin or legally authorized representative of each brain donor provided written informed consent. The methods for this report followed the appropriate use and reporting of uncontrolled case series in the medical literature reporting guidelines.35
Neuropathologic Evaluation
Neuropathologic evaluation occurred blinded to the clinical evaluation by neuropathologists (A.C.M., B.R.H., V.E.A., and T.D.S.). Pathologic processing and evaluation were conducted using previously published methods and as described in the eAppendix in Supplement 1.12-14,34,36 Neuropathologic diagnoses were made using NINDS National Institute of Biomedical Imaging and Bioengineering criteria for CTE31,32 and well-established criteria for other neurodegenerative diseases.37-40 The CTE p-tau pathologic findings were classified into 4 stages using the McKee staging scheme for CTE.
Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#CTE#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#PostconcussionSyndrome#TBI#TBItreatment#traumaticbraininjury
0 notes