#pleural effusion treatment
Text
Sanjivini Super Speciality Hospital in Lucknow offers advanced pleural effusion treatments, providing expert care and personalized solutions for patients' respiratory health.
0 notes
Text
#best lung surgeons in Delhi#Empyema Treatment in Delhi#Pleural effusion#Pleural effusion in Delhi#Pleural effusion treatment in Delhi#thoracic surgeon in Delhi#Treatment Options for Empyema
0 notes
Link
Looking for Pleural Effusion Treatment in Hyderabad, contact Dr Alla Gopala Krishna Gokhale, specialist in Pleural Effusion Treatments.
#pleural effusion symptoms and causes#best lung specialist in hyderabad#pleural effusion treatment in hyderabad#best lung transplant surgeon in hyderabad
0 notes
Note
So what you want Kate to not get chemotherapy so that she gets even more worse and more unwell? Who even thinks like that and William doesn’t smoke

First off, it's well known that William smokes. Just because he hides it better than Harry doesn't mean he doesn't do it. He clearly has smoker skin. That's why his skin looks so terrible & dry. So dry that soon we might be able to grate cheese on it.
"You want Kate to not get chemotherapy so that she gets even more worse and more unwell?"
Your ignorance is clearly showing.
This is how people die from cancer:
Catabolism: the body breaks down on a cellular level; substances released by tumor cells are strong anorexics.
Secondary infection due to immune system suppression.
Blockage of vital structures: trachea/esophagus, superior vena cava (SVC) syndrome, impacts to the spinal cord, pericardial effusion, pleural effusion, etc.
Side effects of medication/treatment: immune suppression, pulmonary fibrosis, Graft-versus-Host-Disease (GvHD), etc.
You do not die from cancer just because you have "cancer."
I wrote a long post yesterday differentiating that different people have different physiology. Just because you have "cancer" does not mean that it poses a threat to your life or health. Plenty of people have "cancer" that does not progress at all or affect them in any way. Just because you have "cancer present" does not mean it will affect your life or health in any significant way.
The situation is really like the anon said:
"Catherine has a much more serious cancer than they are letting on, hence, the decision to have chemo is not even a discussion point,"
"she’s not having chemo and there’s another reason why she’s missing in action,"
"she and William are panicking and she’s receiving chemo regardless"
My bets are on numbers two or three.
Kensington Palace is clearly lying. Can't wait for it to be revealed! KP's strategy before Kate's cancer announcement was to release the news that her medical records had been breached and paint Kate as a victim. After the cancer announcement, it was those pesky conspiracy theorists and the axis of evil who was to blame for Kate's reputation being slagged around the world, not the utter incompetence of William and KP.
Let's not forget that William is an emotionally damaged, thin skinned, control freak with a privacy fetish.
Let's also not forget that next Monday, 01 April 2024, begins a new fiscal year for the BRF.
#ask#hate mail#medicine#smoking#William The Prince of OWN GOALS#William The Terrible#William The Weak#William The Prince of Wales#prince william#Prince & Princess OWN GOALS#kate middleton#Catherine The Princess of Wales#kensington palace#palace officials#lies lies lies#pr games#strategery#Wales fandom ARMAGEDDON
14 notes
·
View notes
Text
Entamoeba Histolytica
Moving on from Disseminated infections.
and back to parasites, we have this amoeba.
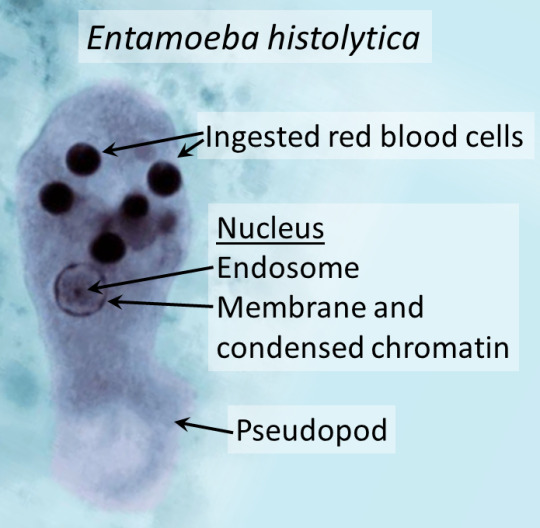
Courtesy of wikipaedia.
One complication is liver abscess.

Image from NEJM
Ring enhancing cysts were seen on CT (requested after the authors noted deranged liver function tests) and on percutaneous drainage (which radiology can do), they had brown cloudy fluid. Under the microscope they noted the pseudopods (leg like extensions).
Classically though, entamoeba causes amoebic dysentery or bloody diarrhoea that develops over 1-4 weeks. However, 90% are asymptomatic. Given the complications/extra-GI manifestations, it can be fatal in a very small minority.
Severe disease/Complications
- toxic megacolon (always makes me think of heavy metal bands, in sad actuality it's inflammation that affects more layers and causes the colon to wide. resembling balloon animals)
- fulminant colitis + perforation (from inflammation, ulceration etc. that the trophozoites induce, high mortality)
- liver abscess (more common, fevers/RUQ/hepatomegaly, transamnitis and jaundice, maybe months before this develops)
- rarely: pericarditis + tamponade (from liver rupture, rare but high mortality), pleural effusion & brain abscess (exceedingly rare - but acute confusion + fevers, rapid deterioration)
risk factors for severe diseases/complications: malignancy, pregnancy, immunosuppression in general.
Toxic megacolon:
Can actually rupture eventually.
Courtesy of wiki

Transmission: faecal oral routes (contaminated food/water sources) and it's widely distributed across the world. As with many infectious diseases, it has a higher prevalence in lower socioeconomic groups and regions of the world. Africa & South/Central AMerica have higher rates than other countries (poor sanitation areas, water sources like rivers have multiple purposes for households etc.). Generally, in western countries, it develops in returned travellers who went to endemic areas or immigrants.
Detection: EIA assay for entamoeba antigen in stool, serology (relies on antibodies, so undetectable the first week and last a life time, does not differentiate acute vs past infection), stool MCS for cysts and ova, PCR and colonoscopy (ulcer/erosions, biopsy will reveal cysts and trophozoites)
Treatment: metronidazole in active/acute disease, increased doses in severe/complicated disease or invasive. depending on where you are, also paromycin if asymptomatic or following active treatment to remove cysts.
Consider this in returned travellers with high fevers, abdo pain and bloody diarrhoea lasting > 2 weeks.
Avoids while travelling to endemic areas - uncooked foods, unbottled water/ice cubes, street vendors (what a shame), just anything raw. Practice good hand hygiene.

Sources:
StatPearls ON PubMed
Amoebiasis on CDC
#entamoeba histolytica#medblrs#medblr#infectious diseases#parasites#parasitology#infectious disease#microbiology
9 notes
·
View notes
Text
Another surgery, more Chemo
Dear Friends,
I got most of my results today. And I got bad days sometimes.
It's been how many months eversince I went home after a year of being in and out of HP, and been into ICU. I am in need of another surgery again to remove water in my lungs as it re-occurs almost monthly because of pleural effusion, infection. Which requires medical attention. I have this occurring condition because of my Treatments, and tumors are occurring all over my body and some of them are malignant which requires so much attention. My illness was earlier detected and in lower stages, and can be cured(I am praying always) to not advance, but it will take time as to how my body reacts. My lungs has a very bad history last 2018, and lately they have found something on my breast that needs further checking as well. My breasts hurts a lot.
Unfortunately, the cost of the surgery and the mounting hospital bills that have piled up from my past hospitalization(2021-2022), have become an overwhelming burden for me, my friends and my family. We are also still grieving at the untimely passing of my niece 3 weeks ago. They have already exhausted their savings and are struggling to make ends meet. And also I've been a breadwinner of my Family for a very long time. They depend on me financially.
Weekly Treatments are costly for me too as well. As we have a very bad healthcare system where I live. And despite having a job, it only pays me $250/monthly which is not enough, because I am renting an apartment. And have a caregiver to check on my welfare, as I have difficulties in movement and series of bad episodes. I am also taking care of my cats and dog,
I am also most of the time in an oxygen so that it will ease my breathing problems. I have bad days, but I am trying my best to ease the pain and smile everyday.💖💝
I am really ashamed to ask help once again, as you all know I made my Etsy store several months ago to help with my expenses, but Etsy permanently suspend it without any proper explanation, despite my appeal. The Laptop which I also use for designing is no longer working, and I need to redesign again to sell, to support my Treatment.
I humbly ask for your support once again. As I need to have the procedure to be scheduled next week 24th of May.
Update as of June: I am already home but unfortunately my bills have piled up again, and signed a promissory letter.
Please share this post, spread the word, this will help me a lot. Every contribution, no matter how small, will make a significant impact to me.
I am also starting to make an artwork to sell here on Ko-Fi once my procedure is finish. I might stay in HP for 4-5 days. Thank you so much for all the help! And I love you all!
For Donations $149 and above. If you wish to donate more than that please send them into parts(Ex.$300 = $100,$100,$50,$50), because Paypal will hold them usually for 10 working days. Thank you so much for understanding.
For Donors, you can send to me your screenshot of the amount that you have donated here: [email protected] and I will make a small gift for you, a digital art of dog or cat of your liking. Or if you have a tumblr please message me, and I will tag you of the art. It will take time for me to make them, and I ask for your patience about this matter. Thank you so much!
Sorry for tagging you all guys again, if you could tag any fundraising blogs and your friends here on Tumblr please do so. it will help boost my campaign. You can also share my link to your Social Media accounts, and if you can share this outside of tumblr. It will b a great help to me.
@leonshin99 @shotce @thelovelywarriorsheart @sparkie96 @c1a1r3r3df1e1d @silvertonguelover @measurelessdreamer @fossil-finder @vietnoodle @irishspringyum @kevinbuiyin
I am a Chreon and Geraskier fan as well. I have a small discord group and I appreciate for you to join if you can. It will be lovely to have more friends.
DISCORD GROUP
36 notes
·
View notes
Note
Can binding cause pleural effusion?
I've been feeling pressure in my rib and chest area for a while and recently it's gotten worse as well as my ability to breath, could it be from binding? I don't have any bruised or broken ribs
I do have an inflammatory disease but I don't think it's that
Lee says:
We are not medical professionals, which is why I would recommend that you speak to someone who is!
I can't tell you whether the symptoms that you are experiencing are caused by binding or worsened by binding because I'm not a medical professional who has taken your medical history and examined you, but I can tell you that it's important to get it checked out by someone who can diagnose the issue and recommend a plan to address it.
You should call your primary care provider/general practitioner/family doctor, and/or send a message to them through the patient portal if there is one.
If you don't have a doctor or other provider who you usually see for an annual check-up or sick visit, you could look to see if there are any urgent care clinics near you who accept your insurance.
And don't bind until you've been cleared to do so by a medical professional-- it sucks, but it's time to take a break from binding, just in case it could exacerbate the issue.
If you've been having unexplained issues breathing for a while, you should see a medical professional. That's always true. If you're worried about telling your parents about your concerns about binding because you're closeted or they don't approve of you binding, don't mention binding when you explain why you'd like to go to the doctor, just tell your parents about your symptoms.
If you think that your parents might not allow you to go to the doctor, start by going to the school nurse, explaining your symptoms, and see if they'd call your parents or write a note for your parents recommending that they take you to the doctor. That might make them more likely to take you if they tend to otherwise disregard your concerns.
But when you do go to the doctor, do mention your binding, as well as what symptoms you're experiencing and how long you've been experiencing them.
I've had two family members get pneumonia in the last year, and one had to be hospitalized and the other needed a CT scan to diagnose lung issues, and both needed antibiotics. There are a lot of illnesses and injuries that can cause issues with breathing (example one: COVID!) but some things don't always improve without treatment.
It seems like you've been having these issues for a while, so I'd encourage you to do whatever you have to be sure you get the care that you need instead of waiting it out and seeing if you get better.
I hope you feel better soon anon! And again, please do seek out medical attention IRL!
40 notes
·
View notes
Text
Liver transplantation.
The one time you might actually want cancer.
Why? Because having a primary liver cancer bumps you up on the liver transplant list. But it can't just be any cancer - there's a criteria for acceptable cancer burden for adult liver transplant, which is known as Milan Criteria. Essentially one big tumor smaller than 5 cm or 3 small tumors less than 3 cm each. The tumor can't have left the liver either aka metastasis. However if it's too small (<2 cm ), you don't get priority listing for having that cancer. Kind of like Goldilocks - the tumor has to be just right.
Now first off, you almost never get a primary liver tumor aka hepatocellular carcinoma (HCC) without something wrong in the liver in the first place.
This is usually Cirrhosis aka fibrosis of the liver, which can be caused by Hepatitis C or more commonly drinking too much alcohol too often. The liver fails cause its cells are dead or dying, and the resulting scarring prevents blood from your GI tract from returning properly to your systemic blood. This pseudo-blockage results in fluid backing up in your body, resulting in ascites (fluid in the belly) and pleural effusion (fluid in the lung space) and generalized soft tissue swelling.
The body tries to compensate for this by making alternate paths. Problem is the liver is also a filter, and bypassing the filter through an alternate path affects the brain - a common symptom is confusion and sometimes coma in these patients. Official term is hepatic encephalopathy.
Cirrhosis patients can also literally turn yellow because bilirubin, which occurs from the normal breakdown of red blood cells, can't be processed well by a dysfunctional liver. Liver does a lot of other important stuff too, but I'd go on forever with that - so I'll end that here.
In any case, the only treatment for cirrhosis is getting a new liver - once cirrhosis occurs, it cannot reverse, only worsen. The liver transplant list uses its own criteria known as MELD which I also won't get into here, but generally the sicker you are, the higher you are on the transplant list.
Cirrhosis is essentially a breeding ground for primary liver cancer because cirrhosis is essentially repeated constant inflammation - and all it takes is one cell to heal in the absolutely worst way - and then you have a cancer. This is why cirrhosis patients get yearly liver imaging screening to detect that.
Milan Criteria was created because a good number of liver transplants in cancer patients turned out to have recurrent liver cancer in the new liver. After Milan was implemented, long-term recurrence-free survival improved from 30% to 75%. I believe the sizes used in Milan acts as a surrogate for the likelihood of microscopic metastasis, cancer that's left the liver but too small to be seen in imaging, but don't quote me on that.
Now why did I bring this up? One of the residents asked out loud about why we don't just cut out the cancer.
For one, cirrhosis ensures another one will pop up eventually, and for two, cutting a cancer out also means cutting out good tissue (or semi-okay in a cirrhotic's case) to create the disease-free margin. You don't have much good tissue left in a cirrhosis liver.
You could ablate the cancer by frying it with heat or freezing it, but you again have the issues of damaging normal tissue. Typically excision or ablation is done when there's no chance patient will get a donor liver.
There's also TACE (transarterial chemoembolization) which can be used to shrink tumors, usually back into the limits imposed by Milan criteria. Because if your cancer is too big for Milan, you don't get a liver. There are strict rules for that, and if you break them, your liver transplant service is not getting donor livers.
4 notes
·
View notes
Text
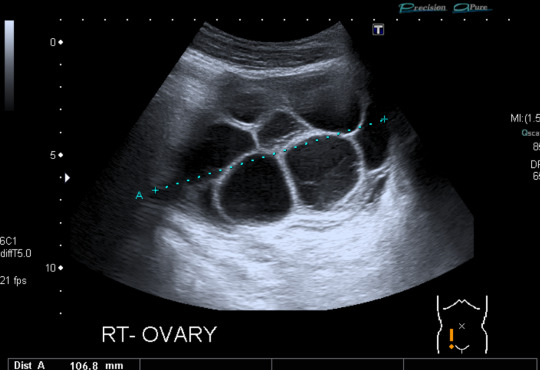

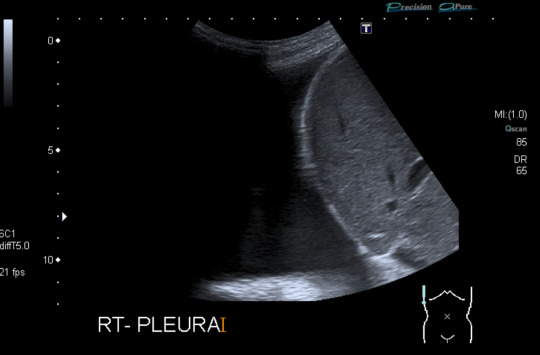
Today's case is a pelvic ultrasound of a 35-year-old woman who presented with abdominal pain and bloating 9 days after initiating controlled ovarian hyperstimulation in preparation for IVF. Ultrasound reveals enlarged ovaries with multiple large follicles, ascites, and pleural effusions. Findings are compatible with ovarian hyperstimulation syndrome (OHSS) which occurs in approximately 5% of women undergoing ovarian stimulation. Fluid shift results in hemoconcentration and oliguria. Treatment is supportive and may include paracentesis or thoracentesis to relive discomfort from accumulated fluid. Severe cases can be fatal, so patient education, prompt recognition and timely intervention are key. Risk factors include PCOS and prior OHSS. Younger age and low body weight are not good predictors of risk, as was previously posited by some papers.
Case courtesy of René Pfleger, Radiopaedia.org, rID: 29070
3 notes
·
View notes
Text
“Belle Roe,” 21 (USA 2009)
“Belle’s” real name is unknown because her case is reported from a medical journal. She has been given the last name Roe after the court decision that led to the deaths of so many pregnant people and babies across America.
Belle was a 21-year-old American with no health problems whatsoever. She should have been able to live a long life, but instead she was sold the abortion pill from a legal facility in 2009 and died 12 days later.
Belle took the lethal pills when she was 7 weeks pregnant. 6 days after beginning the abortion, she suffered from severe abdominal cramping, vomiting and diarrhea. On Day 7 she was brought to the hospital with dangerously low blood pressure, tachycardia, pleural effusions, ascites and massive infection. Oddly enough, she did not have a fever despite the fact that she was dying from infection. This is a phenomenon that has been documented in multiple cases as a result of the RU-486 abortion pill.
Despite emergency surgery and hospitalization, Belle died of severe sepsis, kidney failure and DIC (disseminated intravascular coagulopathy). The organs in her reproductive system were necrotizing. Analysis confirmed the presence of Clostridium sordellii infection. C. sordellii has been known to grow out of control and cause raging infections after use of the abortion pill.
Despite what the abortion industry tells the public, the abortion pill is not safe. Deaths like these are not nearly as rare as abortion corporations claim. Multiple abortion supporters have also pressured abortion pill clients to lie to ER staff and claim they are suffering a miscarriage. Despite what these abortion supporters claim, the symptoms and necessary care are NOT identical for an abortion and a miscarriage. As the study noted, doctors “should be aware of common clinical features, including abdominal pain, hypotension, tachycardia, third-space fluid accumulations, hemoconcentration, and marked leukemoid response, typically without fever. In patients with this presentation, a high index of suspicion for this syndrome and early aggressive treatment are needed.” Further study has shown that misdiagnosis of abortion side effects as miscarriage is a serious risk for medical problems requiring hospitalization. Those whose abortions were miscoded as miscarriages in the ER were more likely to be hospitalized for any reason than women whose abortions were accurately reported. ER patients whose chemical abortions were miscoded further exhibited a pattern of multiple hospitalizations in the 30 days following their abortions – the number of hospital admissions per patient was 78% higher in the miscoded group.
Pregnant people deserve better than the abortion pill, which is unsafe even when it’s legal.
#abortion#pro choice#pro life#tw abortion#tw murder#abortion debate#unsafe yet legal#tw ab*rtion#tw death#unsafe but legal#abortion kills women#kill pill#death from legal abortion#abortion pill#abortion is not healthcare
4 notes
·
View notes
Text
At Sanjivini Super Speciality Hospital in Lucknow, we offer advanced treatments for pleural effusion, employing a combination of thoracentesis, medication, and occasionally surgical intervention for effective management and patient comfort.
0 notes
Text
tw: cancer
my luna very likely has cancer and I can’t deal with this
she’s lost weight and went to the vet on wednesday. they said they felt a mass and got her scheduled for an ultrasound that was supposed to be tomorrow.
yesterday she had labored breathing so we took her to the emergency vet who said she had pleural effusions. pleural effusions are usually caused by congestive heart failure or cancer. they did a thoracocentesis to help her breathe but also did x rays and showed us images of her abdomen that showed a big mass around her intestines. the vet said she’s all but certain this is cancer. they’re sending the pleural fluid for cytology to test for malignant cells - we should have an answer tomorrow.
she’s only 5 years old. my heart is shattered. we got her a month after max died because we couldn’t handle how quiet the house was without him. she is the most perfect, well-behaved cat and reminds us so much of our max - we swear sometimes that she’s part dog and he’s still with us in her. she is the sweetest little angel who has never once bitten or scratched us (or anyone) in the entire time we’ve had her. we never even heard her hiss the first few years we had her - even then, the only time she ever hisses is if she meets a new cat. she basically took on the role of mama to milo and phoebe when we found them at 4 weeks old.
the vet was telling us what options we had and it was so, so hard trying to be the objective decision maker. my mom was with me but she was crying and she deferred everything to me because she says I’m “in the medical field”. we know we aren’t going to put her through chemo. the vet said we can do steroids, which can have some treatment effect. I asked how long that gives her and she told us maybe a month. we cancelled her ultrasound tomorrow because there honestly is no point - it’s not going to tell us anything we don’t already know, and it will just make her anxious having to leave home and be sedated again.
I’m watching her right now and crying because I just can’t come to terms with this. she’s already breathing hard again, so her pleural effusions have likely reaccumulated <24h after being drained. it’s not a good sign - we don’t want her to suffer but god I’m just not ready. my little brother doesn’t know - he’s in rhode island, we didn’t tell him about the weight loss because we wanted to have more information from the ultrasound and a plan before telling him and having him be upset. things have escalated so quickly and we’re just so blindsided by this. we thought we had more time. she has been a perfectly normal, healthy cat and now within the span of a few weeks, from the first time we noticed her weight loss, we are dealing with the reality of having to put her to sleep very soon. my brother comes home next week and I want him to be able to say goodbye to her, but with her effusions I’m not even sure that will happen.
it was so different with max. equally as heartbreaking, but he was older, and his decline happened over months - not weeks/days. we knew it was coming, had wanted to get through the holidays but it just wasn’t happening. we lost him a week before my birthday, right after thanksgiving. I went to the vet with my dad and was there for his last moments, and honestly it was awful. I don’t know that I can do it again. I will do it for luna so that she’s not alone, but god I don’t want to do it.
I want so badly to help her, but what can we do? there is nothing but prolonging the inevitable, and the options that would give us more time would destroy her quality of life and make her suffer.
we never intended to have 3 cats - milo and phoebe were stray kittens we found right at the start of covid, and no one would take them because shelters were closed. they ended up being ours because we got too attached, so then there were 3. the thought of going from 3 to 2 just feels so wrong. but it’s going to happen and there’s nothing I can do to stop it.
1 note
·
View note
Text
Assessment of Bones and Soft Tissue on Chest X-Ray - An Article by Prognosys Medical System
Chest X-rays are a commonly performed diagnostic imaging test that provides valuable information about the bones and soft tissues within the chest cavity. This article aims to explore the assessment of bones and soft tissue on chest X-rays and the significance of these findings in clinical practice. Understanding the interpretation of these images is crucial for healthcare professionals involved in the care of patients with chest-related conditions.
Assessing Bones on Chest X-Ray
One of the primary objectives of a chest X-ray is to evaluate the bones within the chest cavity. The ribs, sternum, and clavicles are the main structures assessed in this regard. Abnormalities such as fractures, dislocations, or bony lesions can be visualized on the X-ray images. Fractures may appear as thin lines or breaks in the continuity of the bone. Dislocations can be seen as abnormal alignment or separation of bone ends. Bony lesions, such as tumors or metastases, may manifest as areas of abnormal density or destruction.
Soft Tissue Assessment on Chest X-Ray
In addition to bones, chest X-rays also allow for the assessment of soft tissues within the chest cavity. This includes the evaluation of the lungs, heart, mediastinum, and diaphragm. Abnormalities in these structures can provide important diagnostic clues for various respiratory and cardiovascular conditions.
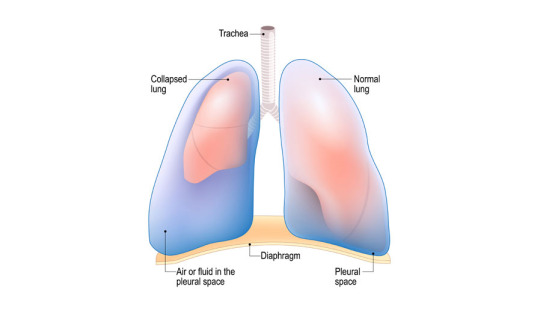
The lungs are the most prominent soft tissue structures seen on a chest X-ray. They are evaluated for the presence of masses, infiltrates, consolidation, or pleural effusions. Masses can indicate tumors or infections, while infiltrates and consolidation may suggest pneumonia or other lung pathologies. Pleural effusions, which are the accumulation of fluid in the pleural space surrounding the lungs, can be observed as blunting of the costophrenic angles or meniscus-shaped opacities.
The heart and mediastinum are assessed for size, shape, and position on chest X-rays. Cardiac enlargement may be indicative of conditions such as congestive heart failure or cardiomegaly. The mediastinum, which is the central compartment of the thoracic cavity, houses various structures including the thymus, esophagus, and major blood vessels. Any abnormalities in these structures can be identified on the X-ray images.
The diaphragm, a dome-shaped muscle that separates the chest cavity from the abdominal cavity, can also be evaluated on chest X-rays. Its position, shape, and movement can provide important information about the integrity of the diaphragm and its function. Diaphragmatic abnormalities may be observed in conditions such as diaphragmatic hernias or paralysis.
Significance in Clinical Practice:
Assessing bones and soft tissue on chest X-rays is essential in the diagnosis and management of various respiratory, cardiovascular, and musculoskeletal conditions. The findings on these images can guide healthcare professionals in formulating appropriate treatment plans and further diagnostic investigations.
Conclusion:
In conclusion, the assessment of bones and soft tissue on chest X-rays plays a crucial role in the evaluation of patients with chest-related conditions. By carefully analyzing these images, healthcare professionals can identify fractures, dislocations, bony lesions, as well as abnormalities in the lungs, heart, mediastinum, and diaphragm. This enables accurate diagnosis and appropriate management of patients, leading to improved outcomes.
Prognosys Medical Systems has expanded its capabilities from manufacturing X-ray equipment to single detector solutions, dual detector solutions, floor mounted systems, ceiling suspended systems, floor to ceiling systems, mobile system, line powered and battery-operated systems and a range of C arms to offer the most comprehensive design solutions under one roof.
Few of the Diagnostic Imaging (Chest X-Ray) Systems offered by Prognosys Medical Systems:
PRORAD 2FC - Single
PRORAD 2FC - Dual
PRORAD 2FC – Floor to Ceiling – Single
PRORAD 2FC – Floor to Ceiling – Dual
Click the links to Know More about Prognosys Medical Systems Product Range and Request for Quote.
Contact us for more information:
– Content Team
Prognosys Medical Systems
[email protected]
0 notes
Text
Revolutionize Recovery: Thoracic Drainage Catheters Unleashed
Technological developments in the medical field constantly change how patients are treated and allowed to heal. Thoracic drainage catheterization is one such innovation that is revolutionising the treatment of pulmonary diseases and thoracic surgery. These compact, yet mighty gadgets are transforming recuperation, providing patients with unprecedented ease, speed, and healing effectiveness.
The Thoracic Drainage Catheters: An Understanding
Chest tubes, sometimes called thoracic drainage catheters, are thin tubes that are put into the chest cavity to drain pus, fluid, or air to help the lungs return to normal. They are essential in the management of pleural effusion and pneumothorax, as well as in the post-operative care following thoracic procedures like lobectomy, pneumonectomy, or thoracotomy.
Changing the Course of Recovery:
In the past, receiving post-operative care meant longer hospital stays, more discomfort, and a higher chance of problems. But healing has changed dramatically since sophisticated thoracic drainage tube became available. These contemporary gadgets have a number of significant benefits:
Enhanced Comfort: Modern thoracic drainage catheters are made with the patient's comfort in mind, as opposed to previous types. Because of their smaller diameter, they cause less discomfort during the healing period and cause less tissue damage during insertion.
Quicker Recovery: Patients recover more quickly when they have better drainage capacities and a lower chance of problems. This enhances overall quality of life by resulting in shorter hospital stays and a quicker return to regular activities.
Minimised Complications: Modern thoracic drainage catheters are highly precise and successful in minimising the risk of complications, including bleeding, infection, and pneumothorax recurrence. This helps to ensure that patients have more comfortable recovery paths.
Tailored Solutions: With the wide range of sizes and configurations available for thoracic drainage catheters, medical professionals can customise treatment regimens to meet the specific requirements of each patient. Better results are encouraged and drainage efficiency is optimised by this customisation.
Case Studies:
In order to demonstrate the revolutionary nature of thoracic drainage catheters, let us examine two fictitious case studies:
A lobectomy is performed on 45-year-old Sarah in order to treat her early-stage lung cancer. In the past, difficulties from standard chest tube drainage would have meant a protracted hospital stay and recuperation period. But thanks to the use of contemporary thoracic drainage catheters, Sarah has very little pain, quick post-operative fluid drainage, and is sent home from the hospital a few days later, well on her road to a full recovery.
John, a 60-year-old male, has congestive heart failure and arrives with a massive pleural effusion. In the past, his condition would have needed to be managed with invasive surgeries and prolonged hospital stays. However, John has a minimally invasive thoracentesis operation with quick drainage and gets great symptomatic relief, allowing him to resume his daily activities sooner. This is made possible by the efficacy of modern thoracic drainage catheters.
A new era in patient treatment and recuperation has begun with the development of contemporary thoracic drainage catheter. These technologies are transforming the post-operative experience for patients having thoracic surgeries or treating pulmonary disorders by placing a high priority on comfort, efficiency, and customised solutions. Thoracic drainage catheters are expected to undergo additional developments and improvements as technology develops, leading to even better patient outcomes and quality of life.
0 notes
Text
Lung cancer – the most life-threatening disorder in today's time

Lung cancer — the most life-threatening disorder in today’s time
Overview , symptoms and causes, prevention and myths, diagnosis and treatments, faqs — All you need to know about it
Overview
Lung cancer is a cancer type that occurs in the lungs but later on, affects your whole respiratory system. Lung cancer is one of the most common types of disease in today’s era and it affects lacks of people every year.
As shown in TV ads and everywhere, smoking is the most common reason for respiratory cancer. Lung cancer is one of the major causes of death worldwide. However, smoking is not the only reason many people who do not have contact with smoking ever in their lifetime have also been affected by the disorder.
The World Health Organisation has declared lung cancer as the 4th largest death reason in India among which the men were in the majority.
The disease is never curable but can be managed if the symptoms are caught at an early initial stage.
There are many advanced Technologies today that can help you fight the disease
What are the various signs and symptoms of lung cancer?
In most cases, the symptoms of lung cancer are not visible in the initial stage and therefore many people stay unaware of the fact that they are suffering from the disease. However, the symptoms start worsening with time leading to the sudden death of the patient. following are some of the symptoms explained –
Persistent cough that lasts for more than a week or two
• Bleeding while coughing
• Difficulty in breathing or shortness of breathing
• Unwanted and sudden weight loss
• Pain in the chest and the area around
• All time headache
• Frequent bone pain and muscle aches
• Wheeziness
Went to seek medical appointment for lung cancer treatment
A medical consult is needed if you face consistent cough and especially if you experience bleeding while coughing.
As chances are higher for smokers therefore they must never ignore any symptoms that are explained in the above section.
What are various causes that lead to the occurrence of lung cancer in a person?
As explained above, people who smoke have the highest chance of developing lung cancer in themselves. However, the situation depends on many other factors full stop some of which include the following-
• Exposure to second-hand smoking
• Residing in an area which is highly polluted with dust
• Genetics or hereditary
• Contact with Asbestos and carcinogens
• Radon gas exposure
• Under gone Radiation therapy in the past
Types of lung cancer
Lung cancer is of many types and phases. However, experts generally classify them into the following types
1. Small cell Lung cancer — this lung cancer affects people who have been smoking for a very long time and a addicted to smoking.
2. Non-small cell lung cancer- the cancer cells are enlarged in non-small cell lung cancer which includes squamous cell carcinoma, large cell carcinoma, and adenocarcinoma.
What complications are associated with lung cancer –
Following are some of the complications associated with lung cancer-
• Uncontrollable pain
• Pleural effusion
• Metastasis
• Shortness of breathing
Is lung cancer preventable?
How can you prevent lung cancer?
Lung cancer cannot be prevented completely but a few precautionary measures can help you reduce the risk of Cancer generation in your body to a great extent. These steps include the following of them-
• Quit smoking completely
• Avoid exposure to people who smoke
• Start Exercising if you do not.
• Learn to manage stress. Practice Yoga, meditation and mindfulness
• Have a proper balanced diet with fruits and green leafy vegetables
• Protect yourself from exposure to harmful toxins of the environment like carcinogens. Wear sleeve clothes and have a face mask while going out of home
• Check the radon level of your home
Myths Created about lung cancer –
Myth — people who smoke can only get lung cancer
Fact — people who smoke have the highest chance of developing lung cancer but it also depends on many other factors and your lifestyle choices.
Myth — the ultimate cause of lung cancer is death
Fact — lung cancer can be treated with today’s advanced technology if the treatment is started at an early stage.
Myth — women cannot get lung cancer
Fact — lung cancer can affect people of any gender and age. Moreover,
The chances of lung cancer are higher in men but it can affect women also unconditionally.
Myth — lung cancer cannot affect Children and teenagers Fact — children and teenager
have the least chance of developing lung cancer but cases have come across very young age teenagers died due to lung cancer.
How do doctors diagnose lung cancer?
Your doctor may go through the following techniques to detect your lung cancer –
• X-ray
• Computerised tomography scan or CT scan
• Biopsy • Bone scan
• Blood test
• Ultrasound
• Sputum cytology
• Magnetic resonance imaging test or MRI test
• Positron emission tomography test or PET test
What treatments are available for lung cancer
The following treatment may be provided to you based on the stage of your cancer –
• Chemotherapy
• Radiation therapy
• Targeted drug plan
• Stereotactic Body Radiotherapy
• Surgery • Immunotherapy
Frequently asked questions about lung cancer –
1. What is the average size of lung cancer ?
Answer — the average size of a lung cancer is 7 centimetres which may enlarge with time.
2. What is the death rate of lung cancer?
Answer — the death rate has decreased during the past 15 years. But still, 46/100000 people die every year due to lung cancer
3. How many years can I live with lung cancer?
Answer — you can live for more than 5 years with proper treatment. The survival rate of lung cancer is increasing which is currently 15% over every 100 patients.
4. Is Lung cancer a serious disease?
Is it life-threatening Answer — yes, literally lung cancer is a very serious disease and one of the leading causes of death in India. It is life-threatening to lack of people every year but proper diagnosis and treatment at an initial stage can help you save your life for years.
1 note
·
View note
Text
Pleural Effusion surgeon in Delhi
Dr. Neetu Jain stands as a distinguished Pleural Effusion surgeon in Delhi, renowned for her expertise and compassionate patient care. With a profound understanding of thoracic medicine and advanced surgical techniques, Dr. Jain is dedicated to providing optimal treatment outcomes for her patients. Her commitment to excellence is evident through her comprehensive approach to diagnosing and treating pleural effusion, ensuring personalized care tailored to each individual's needs.
As a leading figure in the medical community, Dr. Jain has garnered acclaim for her surgical skill, employing minimally invasive procedures whenever possible to minimize patient discomfort and hasten recovery. Beyond her clinical practice, Dr. Jain is actively involved in research and education, contributing to the advancement of thoracic surgery and training the next generation of healthcare professionals.
Patients seeking expert care for pleural effusion can trust in Dr. Neetu Jain's expertise, knowing they are in capable hands dedicated to their well-being and recovery.
0 notes