#including tachycardia and a history of arrhythmia
Text
Today is an IBS flare day and I'm regretting all of my life decisions
#IBS#I always get overconfident when I haven't had bad symptoms in a while#'I haven't eaten this type of food in a few days so having it now won't hurt'#'Yeah this medicine isn't good for my stomach but I'm not feeling well so just one pill won't irritate my stomach'#:')#if my life was a show this would be the part where the laugh track goes off at how irresponsible I am#I really need to be more careful with what I eat#and manage my pain without meds that will just hurt my stomach more#OH and the freaking 3 cups of coffee I had today since my brain wasn't wanting to work#I'm not supposed to have that much coffee for like... 3 different health conditions I have going on#including tachycardia and a history of arrhythmia#it feels like I'm always sick and then I try to “fix” it by making myself a different type of sick 🙃#I feel so unwell right now#I guess it's a wake up call to take better care of myself but I'm so terrible at it#honestly it's a miracle I've been sleeping semi normally these days#but everything else feels damn near impossible#my stomach is so sensitive#ughhhhhhh
5 notes
·
View notes
Text
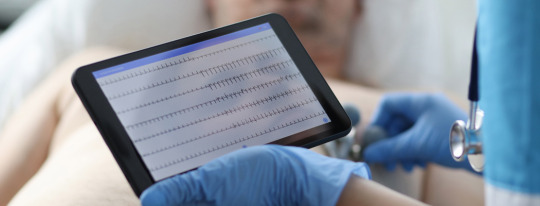
Embark on a journey with Jennifer Carlquist, PA-C, and course director of The Urgent Care EKG Course as she shares 12 essential insights for navigating through EKGs in the urgent care setting.
1. When a patient has an irregular rhythm, it is important to look closely for P waves. If they are the same shape and distance from the QRS complex, you could be dealing with sinus arrythmia. This is usually caused by breathing.
2. If you have a patient with palpitations, you may find a clue to the cause by asking the patient when the palpitations happen. Often, palpitations only occur when the patient is about to go to sleep which could be caused by anxiety, although this is a diagnosis of exclusion.
3. When you have a patient with tachycardia, make sure you can explain why. Pulmonary embolus can cause tachycardia and will not always be associated with an s1q3t3.
4. If you have a very short PR interval, the first thing you should look for is a delta wave. This is what you will see with Wolff-Parkinson-White syndrome, which can be fixed with an ablation.
5. If a patient has experienced a recent stressful event such as the death of a spouse and has new onset heart failure, consider Takotsubo cardiomyopathy. This can present a myriad of EKG findings, including STEMI.
6. PVCs are not always benign. They can lead to heart failure if there are enough of them.
7. There is always a reason for sinus tachycardia, while supraventricular tachycardia (SVT) comes on suddenly for no good reason. It’s hard sometimes to tell the difference between the two, but when you start to sort through the history, that’s where it really starts to make sense. Sinus tachycardia will have volume loss, fever, anemia, or anxiety, while SVT patients will usually have none of those. The exception would be if a patient has anxiety after they started feeling the SVT, which is a whole different story.
8. When interviewing a patient about their palpitations, it is always helpful to ask if they have anxiety as well. If they do, ask them which came first: the palpitations or the anxiety. If the anxiety came first, then it is most likely anxiety causing the palpitations, although this would be a diagnosis of exclusion. If the patient feels palpitations and then anxiety comes on, that’s more likely arrhythmia based.
9. It is impossible to diagnose Takotsubo cardiomyopathy from an EKG alone. There are many different presentations of the condition, including STEMI, nonspecific STT-wave changes, T wave, and inversions that are symmetric. If you have a patient with a classic story that involves recent major stress in their life, then absolutely consider this diagnosis. It can be seen during their angiogram, where it will look like apical ballooning, and they will have a reduced ejection fraction.
10. ST-segment elevation can be very minimal and still deadly. It is important when you are screening for ST elevation to look closely at the TP segment. This is the most isoelectric line, and this is where you should draw your line to see if there’s any elevation or depression. As little as 1 mm can be significant for STEMI in the inferior leaves, so it really does matter here. Get serial ECGs.
11. When looking at the intervals at the top of the EKG, one of the most important numbers to look at is the QTC. The QTC should be <460 ms to be normal in women and <450 ms in men. If it is longer than that, consider adjusting the patient’s QT-prolonging medication. We do not usually see Torsades de Pointes until they get >500 ms, but it’s still a good idea to minimize risk by getting the patient off any QT prolongers you can.
12. Torsades de Pointes is lethal and most likely stems from a prolonged QT. Unlike in VT, the treatment is magnesium, but prevention is always the key. Amiodarone can also prolong the QT and can be proarrhythmic, so you may have to choose a different drug in some cases.
This course is ideal for PAs and NPs practicing in urgent care. Whether you’re new to practice or have many years of experience, you’re sure to learn practical, evidence-based tips you can use on your next shift. You can sharpen your EKG interpretation skills, improve your accuracy, become more proficient, and boost your clinical confidence with The Urgent Care EKG Course.
Visit https://www.ebmedicine.net/ekg to learn more.
Even more content:
Check out one of our latest reels (less than one minute!) by Jennifer Carlquist, the course director.
19 notes
·
View notes
Text
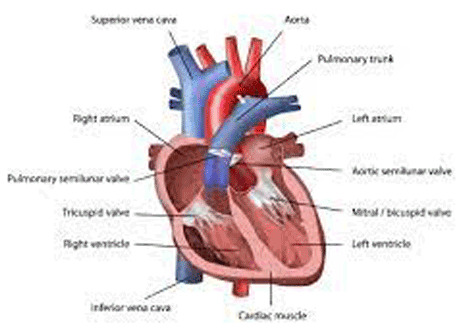
Understanding Heart Rhythm Disorders and Their Impact on Cardiovascular Health
Introduction:
Heart rhythm disorders, or arrhythmias, can significantly impact cardiovascular health. These disorders disrupt the heart's normal electrical activity, causing irregular heart rhythms that can affect its ability to pump blood effectively. Understanding the different types of arrhythmias and their implications is crucial for recognizing symptoms, identifying risk factors, and exploring appropriate treatment options.
Common Types of Arrhythmias
Atrial Fibrillation (AF):
Atrial fibrillation is a common arrhythmia characterized by irregular and rapid electrical signals in the heart's upper chambers (atria). This leads to an irregular heart rate. AF increases the risk of blood clots, which can travel to other body parts, causing stroke or other complications.
Bradycardia:
Bradycardia is a slow heart rate, typically below 60 beats per minute. It occurs when the heart's electrical signals are delayed or blocked, decreasing heart rate. Bradycardia can be caused by medications, underlying heart conditions, or heart electrical system issues. Symptoms may include fatigue, Dizziness, fainting, or Shortness of breath.
Tachycardia:
Tachycardia is characterized by a fast heart rate, usually above 100 beats per minute. It occurs when the heart's electrical signals fire abnormally or accelerated. Stress, anxiety, certain medications, or structural abnormalities in the heart can trigger tachycardia. Symptoms may include palpitations, Dizziness, chest pain, or loss of consciousness.
Symptoms, Risk Factors, and Potential Complications
Symptoms of Heart Rhythm Disorders:
Palpitations: Sensation of rapid, fluttering, or irregular heartbeats.
Fatigue: Persistent tiredness or exhaustion, even with minimal physical activity.
Dizziness or lightheadedness: Feeling faint or unsteady.
Shortness of breath: Breathlessness or difficulty breathing, particularly during exertion.
Chest discomfort: Discomfort, pressure, or pain in the chest.
Fainting or near-fainting episodes: Temporary loss of consciousness due to inadequate blood flow to the brain.
Risk Factors:
Age: The risk of arrhythmias generally increases with age.
Family history: Having a close relative with a history of arrhythmias may raise the risk.
High blood pressure: Uncontrolled hypertension can strain the heart and disrupt electrical signals.
Existing heart conditions: Conditions such as coronary artery disease, heart failure, or structural abnormalities can contribute to arrhythmias.
Thyroid disorders: An overactive or underactive thyroid can disrupt the heart's electrical system.
Lifestyle factors: Excessive alcohol or caffeine intake, smoking, drug abuse, and obesity can all play a role in developing arrhythmias.
Potential Complications:
Stroke: Certain arrhythmias, particularly atrial fibrillation, can increase the risk of blood clots forming in the heart, which can travel to the brain and cause a stroke.
Heart failure: Chronic arrhythmias can weaken the heart muscle over time, leading to heart failure, where the heart cannot pump blood effectively.
Sudden cardiac arrest: In some cases, arrhythmias can trigger a sudden loss of heart function, leading to cardiac arrest, a life-threatening emergency requiring immediate medical intervention.
Treatment Options
Treatment for heart rhythm disorders aims to restore or maintain a normal heart rhythm, alleviate symptoms, and reduce the risk of complications. The following treatment options are commonly used:
Medications: Antiarrhythmic drugs may be prescribed to regulate heart rhythm and reduce the frequency or severity of arrhythmias.
Lifestyle modifications: Making lifestyle changes, such as managing stress, maintaining a healthy weight, quitting smoking, limiting alcohol and caffeine consumption, and engaging in regular physical activity, can help manage certain arrhythmias.
Ablation: Catheter ablation is a procedure that involves selectively destroying or isolating abnormal heart tissue responsible for generating arrhythmias. It aims to restore a normal heart rhythm.
Implantable devices: In some cases, implantable devices like pacemakers or cardioverter-defibrillators (ICDs) may be recommended to regulate the heart's electrical signals and deliver appropriate therapy when needed.
Conclusion
Heart rhythm disorders can significantly impact cardiovascular health, affecting the heart's ability to function properly. Recognizing the symptoms, understanding the risk factors, and seeking appropriate treatment is vital for managing arrhythmias and reducing the risk of complications. By working closely with healthcare professionals, individuals with heart rhythm disorders can develop a tailored treatment plan that addresses their specific needs, improves their quality of life, and promotes overall cardiovascular health.
#Cardiac arrhythmia#heart rhythm disorder#cardiac rhythm disturbance#irregular heartbeat#atrial fibrillation
6 notes
·
View notes
Text
This is for sustained VTach:
Sustained monomorphic ventricular tachycardia (SMVT) is defined as a regular, wide (≥120 milliseconds) QRS complex tachycardia with uniform and stable QRS morphology at a rate of more than 100 beats per minute that lasts for 30 seconds or longer or causes hemodynamic collapse within 30 seconds.
●All patients with SMVT should have a brief immediate assessment of the symptoms, vital signs, and level of consciousness to determine if they are hemodynamically stable or unstable. Differentiation between a hemodynamically unstable versus stable patient depends upon hemodynamic compromise, such as hypotension, altered mental status, chest pain, or heart failure (HF).
●Patients with SMVT who are hemodynamically unstable and pulseless, or who become pulseless during the course of evaluation and treatment, should be managed according to standard advance cardiac life support (ACLS) resuscitation algorithms, with immediate high-energy countershock and cardiopulmonary resuscitation (CPR). Patients should initially be treated with a synchronized 120 to 200 joule shock from a biphasic defibrillator or a 360 joule shock from a monophasic defibrillator.
●For patients with wide complex tachycardia (WCT) who are hemodynamically unstable, but still responsive with a discernible blood pressure and pulse, we recommend urgent cardioversion (following administration of sedation) (Grade 1B).
●For patients with SMVT who are hemodynamically stable on presentation, after recording a 12-lead ECG we generally prefer to begin with an intravenous antiarrhythmic agent and reserve electrical cardioversion for refractory patients or for those who become unstable.
•If pharmacologic cardioversion is the chosen approach, we administer intravenous amiodarone, procainamide, or lidocaine.
•If electrical cardioversion with appropriate procedural sedation is the chosen approach, intravenous analgesics or sedatives should be cautiously administered if the blood pressure will tolerate their use. If the QRS complex and T wave can be distinguished, an attempt at synchronized cardioversion can be performed with a synchronized shock of 100 joules using either a biphasic or monophasic defibrillator.
●Treatment of underlying conditions associated with VT, such as myocardial ischemia, electrolyte disturbances, drug proarrhythmia, and HF, as well as decreasing the sympathetic facilitation of SMVT, are important components of the acute management of VT.
●Chronic therapy of patients with SMVT usually requires utilization of multiple therapeutic modalities, including the implantable cardioverter-defibrillator (ICD), antiarrhythmic drugs, radiofrequency catheter ablation, and/or arrhythmia surgery.
•In the absence of a clearly identifiable and reversible cause for SMVT, nearly all patients with a history of SMVT will be candidates for ICD insertion for secondary prevention of sudden cardiac death, unless the patient refuses or the risks of ICD insertion are felt to outweigh the potential benefits. (See 'ICD therapy' above.) •Nearly all patients who experience SMVT have an indication for therapy with a beta blocker, including patients with a prior myocardial infarction, patients with HF and reduced LV systolic function, etc. Beta blockers provide some level of protection against recurrent SMVT, primarily by reducing myocardial oxygen demand and blocking sympathetic input to the heart. (See 'Beta blockers' above.) •Antiarrhythmic drugs may also be used to improve quality of life in patients with frequent SMVT leading to ICD shocks, or in those patients who are not candidates for, or who decline, ICD implantation. Amiodarone has generally been the most effective antiarrhythmic drug for preventing ventricular arrhythmias (and associated ICD shocks). (See 'Antiarrhythmic drugs' above.) •For patients with recurrent SMVT resulting in ICD shocks despite treatment with an antiarrhythmic drug, we suggest radiofrequency ablation (RFA) rather than the addition of a second antiarrhythmic agent (Grade 2C). RFA is also an alternative to antiarrhythmic drugs as the initial therapy for SMVT. In addition, RFA, with or without antiarrhythmic drug therapy, is an option for patients with SMVT who are not candidates for or who refuse ICD implantation. (See 'Radiofrequency catheter ablation' above.)
4 notes
·
View notes
Text
Understanding Heart Disease: What is Heart Disease
What is Heart Disease?
Heart disease, also known as cardiovascular disease (CVD), encompasses a range of conditions affecting the heart and blood vessels. It is the leading cause of death worldwide, causing significant morbidity and mortality. The term "heart disease" is often used interchangeably with "cardiovascular disease," although technically, cardiovascular disease includes all diseases of the heart and blood vessels, while heart disease specifically refers to conditions affecting the heart itself.
Types of Heart Disease
Coronary Artery Disease (CAD): CAD is the most common type of heart disease and occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to plaque buildup (atherosclerosis). This can lead to chest pain (angina), heart attacks, and other complications.
Heart Failure: Heart failure, or congestive heart failure, happens when the heart muscle is unable to pump blood efficiently, leading to a buildup of fluid in the lungs and other tissues. Causes include CAD, hypertension, and cardiomyopathy.
Arrhythmias: These are disorders of the heart's rhythm, which can be too fast (tachycardia), too slow (bradycardia), or irregular. Common arrhythmias include atrial fibrillation and ventricular fibrillation, which can significantly impact heart function.
Heart Valve Disease: Heart valve disease involves damage to one or more of the heart's valves, affecting blood flow within the heart. Conditions include stenosis (narrowing of the valve), regurgitation (leakage of the valve), and prolapse (improper closure of the valve).
Congenital Heart Defects: These are heart abnormalities present at birth, ranging from simple defects like a hole in the heart's walls (septal defects) to more complex malformations. They can affect how blood flows through the heart and to the rest of the body.
Cardiomyopathy: Cardiomyopathy refers to diseases of the heart muscle. The heart muscle becomes enlarged, thickened, or rigid, which can lead to heart failure or arrhythmias. Types include dilated, hypertrophic, and restrictive cardiomyopathy.
Pericarditis: Pericarditis is inflammation of the pericardium, the thin sac surrounding the heart. It can cause chest pain and fluid buildup around the heart, affecting its function.
Causes and Risk Factors
Heart disease is influenced by a combination of genetic, environmental, and lifestyle factors. Major risk factors include:
High Blood Pressure (Hypertension): Hypertension forces the heart to work harder to pump blood, leading to the thickening of the heart muscle and potential heart failure.
High Cholesterol: Elevated levels of cholesterol, particularly low-density lipoprotein (LDL), contribute to the formation of plaque in the arteries, leading to atherosclerosis.
Smoking: Smoking damages the lining of blood vessels, increases blood pressure, reduces oxygen to the heart, and raises the risk of heart disease.
Diabetes: Diabetes significantly increases the risk of heart disease. High blood sugar levels can damage blood vessels and the nerves that control the heart.
Obesity: Excess body weight strains the heart, raises blood pressure, and increases the likelihood of diabetes and cholesterol problems.
Physical Inactivity: A sedentary lifestyle contributes to obesity, hypertension, and other heart disease risk factors.
Unhealthy Diet: Diets high in saturated fats, trans fats, cholesterol, sodium, and sugar can lead to heart disease by raising cholesterol levels, blood pressure, and weight.
Family History: A family history of heart disease increases one's risk, suggesting a genetic predisposition.
Age and Gender: Risk increases with age, and men are generally at higher risk earlier in life than women, although women's risk increases and can surpass men's post-menopause.
Symptoms
Symptoms of heart disease vary by condition but may include:
Chest pain or discomfort (angina)
Shortness of breath
Pain, numbness, or coldness in the legs or arms
Fatigue
Lightheadedness or dizziness
Palpitations (irregular heartbeats)
Swelling in the legs, ankles, and feet
Diagnosis and Treatment
Diagnosing heart disease often involves a combination of medical history review, physical examination, and diagnostic tests such as:
Electrocardiogram (ECG or EKG)
Echocardiogram
Stress tests
Blood tests
Cardiac catheterization
CT or MRI scans
Treatment strategies vary based on the specific type of heart disease and its severity and may include:
Lifestyle Modifications: Healthy diet, regular exercise, smoking cessation, and weight management are crucial for preventing and managing heart disease.
Medications: Medications can control risk factors such as hypertension, high cholesterol, and diabetes, or treat specific heart conditions like arrhythmias and heart failure.
Procedures and Surgeries: Angioplasty, stent placement, bypass surgery, valve repair or replacement, and implantable devices like pacemakers or defibrillators may be necessary for severe cases.
Prevention
Preventing heart disease involves managing risk factors through:
Maintaining a healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats
Regular physical activity
Avoiding tobacco use
Controlling blood pressure, cholesterol, and blood sugar levels
Regular health screenings
Stress management techniques
Understanding and addressing heart disease through lifestyle changes, medical management, and preventive measures is crucial in reducing its impact and improving overall heart health.
1 note
·
View note
Text
Understanding the Silent Killer: Sudden Cardiac Arrest Among Youth

Introduction
Sudden Cardiac Arrest (SCA) is a terrifying and often fatal condition that occurs suddenly and without warning. While commonly associated with older adults, SCA can also strike the young, shattering families and communities with its abruptness and severity. In recent years, there has been growing awareness of SCA among youth, prompting a deeper examination of its causes, risk factors, and preventive measures. This article aims to delve into the intricacies of SCA among the youth population, shedding light on its prevalence, underlying factors, and the importance of early detection and intervention.
Understanding Sudden Cardiac Arrest
Sudden Cardiac Arrest is a life-threatening condition characterized by the sudden loss of heart function, leading to the cessation of blood flow to vital organs. Unlike a heart attack, which is caused by a blockage in the blood vessels supplying the heart, SCA is typically triggered by an electrical malfunction in the heart that disrupts its rhythm. This chaotic rhythm, known as ventricular fibrillation, causes the heart to quiver ineffectively, preventing it from pumping blood effectively to the body and brain.
SCA can strike anyone, regardless of age or gender, but it is particularly concerning when it occurs in young individuals. While relatively rare in the youth population compared to adults, SCA among the young is often more shocking and tragic due to its unexpected nature. The underlying causes of SCA in youth can vary, ranging from congenital heart defects to inherited arrhythmias and structural abnormalities of the heart.
Risk Factors for Sudden Cardiac Arrest Among Youth

Identifying the risk factors associated with Sudden Cardiac Arrest among youth is crucial for early detection and prevention. While some individuals may have underlying heart conditions that predispose them to SCA, others may have seemingly healthy hearts with no prior indication of trouble. Some of the common risk factors for SCA among youth include:
Family History: A family history of sudden cardiac death or inherited heart conditions can increase the risk of SCA in young individuals. Genetic factors play a significant role in many cases of SCA among youth, highlighting the importance of genetic testing and counseling for at-risk families.
Structural Heart Abnormalities: Structural abnormalities of the heart, such as hypertrophic cardiomyopathy (HCM), dilated cardiomyopathy (DCM), and congenital heart defects, can predispose individuals to SCA. These conditions may go undetected until a sudden cardiac event occurs, underscoring the need for comprehensive cardiac evaluations in young athletes and individuals with a family history of heart disease.
Arrhythmogenic Disorders: Certain inherited arrhythmias, such as long QT syndrome, Brugada syndrome, and catecholaminergic polymorphic ventricular tachycardia (CPVT), can disrupt the heart's electrical system and lead to SCA. These conditions often present with subtle symptoms or may be asymptomatic until a cardiac event occurs, making early detection challenging.
Physical Exertion: Intense physical activity, particularly in competitive sports, has been associated with an increased risk of SCA among young athletes. While exercise is generally beneficial for cardiovascular health, certain underlying heart conditions may predispose individuals to cardiac arrest during strenuous exertion. Implementing pre-participation screening programs and providing appropriate medical supervision during athletic activities can help identify at-risk individuals and prevent SCA.
Drug and Substance Abuse: Substance abuse, including the use of illicit drugs and performance-enhancing substances, can have detrimental effects on the heart's function and increase the risk of SCA among youth. Stimulants such as cocaine and methamphetamine can trigger dangerous arrhythmias, while anabolic steroids and other performance-enhancing drugs may induce structural changes in the heart, predisposing individuals to cardiac arrest.
Preventing Sudden Cardiac Arrest Among Youth

Preventing Sudden Cardiac Arrest among youth requires a multi-faceted approach that focuses on early detection, risk stratification, and intervention strategies. Key components of SCA prevention in the youth population include:
Comprehensive Cardiac Screening: Implementing comprehensive cardiac screening programs for young athletes and individuals with a family history of heart disease can help identify underlying cardiac abnormalities and risk factors for SCA. These screenings may include a thorough medical history, physical examination, electrocardiogram (ECG), echocardiogram, and, in some cases, genetic testing.
Education and Awareness: Increasing awareness of SCA among youth and their families, coaches, educators, and healthcare providers is essential for early recognition and intervention. Educational initiatives aimed at recognizing the signs and symptoms of cardiac arrest, performing cardiopulmonary resuscitation (CPR), and using automated external defibrillators (AEDs) can help improve survival rates in the event of a sudden cardiac event.
Lifestyle Modifications: Encouraging healthy lifestyle habits, including regular exercise, a balanced diet, avoidance of tobacco and illicit drugs, and management of underlying medical conditions, can help reduce the risk of SCA among youth. Promoting safe sports participation practices, such as adequate hydration, appropriate warm-up and cool-down routines, and adherence to recommended training guidelines, can also mitigate the risk of cardiac events during physical activity.
Medical Intervention: For individuals diagnosed with underlying cardiac conditions predisposing them to SCA, timely medical intervention is crucial for preventing cardiac arrest and its associated complications. Treatment options may include medication therapy to regulate heart rhythm and function, implantable cardioverter-defibrillator (ICD) placement to detect and treat dangerous arrhythmias, and surgical procedures to correct structural abnormalities of the heart.
Smartcare Diagnostics: Revolutionizing SCA Detection and Management
In the fight against Sudden Cardiac Arrest, early detection is paramount for improving outcomes and saving lives. Smartcare Diagnostics is at the forefront of SCA detection and management, offering innovative solutions designed to identify individuals at risk of cardiac arrest and provide timely intervention when needed.
Smartcare's advanced cardiac monitoring technology utilizes state-of-the-art sensors and algorithms to continuously monitor heart rhythm and detect abnormalities indicative of SCA. By leveraging artificial intelligence and machine learning, Smartcare Labs tools can analyze vast amounts of cardiac data in real-time, allowing healthcare providers to identify subtle changes in heart function that may precede a sudden cardiac event.
Furthermore, Smartcare's integrated telemedicine platform enables seamless communication between patients, healthcare providers, and emergency responders, facilitating rapid response and intervention in the event of a cardiac emergency. Through remote monitoring and teleconsultation services, Smartcare ensures that individuals at risk of SCA receive timely medical attention, regardless of their location.
Conclusion
Sudden Cardiac Arrest remains a silent killer among youth, posing a significant public health challenge that requires urgent attention and action. By understanding the risk factors associated with SCA, implementing comprehensive screening programs, and leveraging innovative technologies like Smartcare Diagnostics, we can strive to prevent cardiac arrest and save lives. Together, let us work towards a future where Sudden Cardiac Arrest is no longer a threat to our youth, but a preventable tragedy of the past.
0 notes
Text
Exploring the Implantable Cardioverter Defibrillators (ICDs) Market: Trends, Growth, and Innovations
The implantable cardioverter defibrillators (ICDs) market is experiencing significant growth and innovation, driven by advancements in cardiac arrhythmia management, increasing prevalence of cardiovascular diseases, and growing adoption of implantable devices for the prevention of sudden cardiac death. As a leading player in this dynamic industry, we aim to provide a comprehensive overview of the market landscape, highlighting key trends, growth drivers, challenges, and future opportunities.
Understanding Implantable Cardioverter Defibrillators
Implantable cardioverter defibrillators (ICDs) are medical devices designed to monitor heart rhythm and deliver therapeutic interventions, including defibrillation and pacing, to treat life-threatening ventricular arrhythmias and prevent sudden cardiac death. ICDs consist of a pulse generator implanted subcutaneously in the chest wall and one or more leads inserted into the heart chambers to sense cardiac activity and deliver electrical shocks or pacing stimuli as needed. These devices are indicated for patients at risk of sudden cardiac arrest due to conditions such as ventricular tachycardia, ventricular fibrillation, or heart failure with reduced ejection fraction.
Market Overview
The global implantable cardioverter defibrillators market is poised for significant growth in the coming years, driven by factors such as the aging population, increasing prevalence of cardiovascular diseases, and technological advancements in device design and functionality. Market projections indicate robust expansion and a notable CAGR during the forecast period, reflecting the growing demand for implantable cardiac devices and the expansion of indications for ICD therapy.
Key Market Trends
1. Subcutaneous Implantable Cardioverter Defibrillators (S-ICDs)
Subcutaneous implantable cardioverter defibrillators (S-ICDs) represent a notable trend in the ICD market, offering an alternative to traditional transvenous ICDs for patients at risk of sudden cardiac death. S-ICDs utilize subcutaneous electrode placement and do not require intracardiac leads, reducing the risk of lead-related complications such as lead fracture, dislodgement, or venous thrombosis. S-ICDs are suitable for patients with limited vascular access, congenital heart disease, or a history of lead-related issues, providing a safe and effective alternative for implantable defibrillation therapy.
2. Remote Monitoring and Telehealth Integration
The integration of remote monitoring and telehealth technologies into ICD systems is transforming patient care and device management, enabling healthcare providers to remotely monitor device function, detect arrhythmias, and assess patient status without the need for in-person clinic visits. Remote monitoring platforms allow for real-time transmission of device data, including arrhythmia episodes, device performance metrics, and battery status, facilitating timely intervention, remote programming, and patient education. Telehealth integration enhances patient engagement, improves clinical outcomes, and reduces healthcare utilization and costs associated with in-office follow-up visits.
3. Advanced Device Features and Connectivity
Advancements in device technology are driving innovation in the ICD market, with the development of advanced features such as multi-site pacing, cardiac resynchronization therapy (CRT), and magnetic resonance imaging (MRI) compatibility. Multi-site pacing and CRT capabilities improve cardiac function and reduce heart failure symptoms in patients with conduction abnormalities or dyssynchrony, while MRI compatibility allows patients to undergo necessary imaging procedures without concerns about device compatibility or safety. Connectivity features enable seamless integration with electronic health records (EHRs), remote monitoring platforms, and mobile health apps, enhancing data accessibility, interoperability, and care coordination.
Growth Drivers
1. Increasing Prevalence of Cardiovascular Diseases
The increasing prevalence of cardiovascular diseases, including coronary artery disease, heart failure, and arrhythmias, is a primary driver of market growth for implantable cardioverter defibrillators. The aging population, sedentary lifestyles, and rising incidence of risk factors such as hypertension, diabetes, and obesity contribute to the growing burden of cardiovascular disease worldwide, driving demand for implantable cardiac devices for primary and secondary prevention of sudden cardiac death.
2. Technological Advancements in Device Design
Technological advancements in device design and functionality are driving innovation and adoption of implantable cardioverter defibrillators, with improvements in battery longevity, lead design, and therapy algorithms enhancing device performance, reliability, and patient outcomes. Miniaturization of device components, optimization of battery chemistry, and development of low-energy shock delivery systems enable smaller device sizes, longer battery life, and reduced energy consumption, enhancing patient comfort and device longevity.
Challenges
1. Complications and Adverse Events
Complications and adverse events associated with implantable cardioverter defibrillators pose challenges for patient management and device utilization. Common complications include lead dislodgement, infection, hematoma, and inappropriate shocks, which may require device repositioning, revision surgery, or medical therapy. Adherence to best practices in device implantation, programming, and follow-up monitoring is essential to minimize complications and optimize patient safety and outcomes.
2. Healthcare System Integration and Reimbursement
Integration of implantable cardioverter defibrillator therapy into healthcare systems and reimbursement policies poses challenges for device adoption and utilization. Coordination of care among cardiologists, electrophysiologists, and implanting physicians is essential to ensure appropriate patient selection, device programming, and long-term management of patients with ICDs. Reimbursement policies and coding guidelines for device implantation, remote monitoring, and follow-up care vary by jurisdiction and may impact access to care and financial sustainability for healthcare providers.
Future Outlook
The future of the implantable cardioverter defibrillators market holds promising opportunities for innovation and growth, driven by technological advancements, expanding indications for device therapy, and evolving healthcare delivery models. Industry stakeholders are poised to capitalize on emerging trends and technologies by investing in research and development, expanding product portfolios, and collaborating with healthcare providers and regulatory agencies to address unmet needs and improve patient outcomes.
In conclusion, the implantable cardioverter defibrillators market plays a crucial role in the prevention of sudden cardiac death and the management of life-threatening arrhythmias, with the potential to enhance
Enquire & DecideDiscover the perfect solution for your business needs. Enquire now and let us help you make an informed decision before making a purchase.
Buy the Full Report for More Insights into the Implantable Cardioverter Defibrillators Market Forecast
Download A Free Report Sample
0 notes
Text
Navigating Multifocal Atrial Tachycardia: Effective Treatment Approaches

Unraveling the complexities of Multifocal Atrial Tachycardia (MAT) is essential for effective treatment and long-term prognosis. In this SEO-friendly blog, we delve into the diagnostic journey of MAT, factors influencing prognosis, and emerging trends shaping the landscape of care.
Diagnosis Unveiled: MAT diagnosis commences with a comprehensive evaluation, blending patient history, physical examination, and advanced diagnostics. Electrocardiogram (ECG) serves as the cornerstone, capturing the irregular heart rhythms indicative of MAT. Further validation through Holter monitoring and imaging modalities ensures accuracy in diagnosis.
Navigating Diagnostic Hurdles: Challenges in MAT diagnosis stem from its resemblance to other arrhythmias, demanding astute clinical judgment and meticulous ECG interpretation. Concurrent cardiac or pulmonary conditions often obscure the diagnostic landscape, necessitating a holistic approach for differential diagnosis.
Advancements in Imaging: Harnessing cutting-edge imaging techniques such as echocardiography and cardiac MRI enhances diagnostic precision, unraveling intricate cardiac structures and functional anomalies associated with MAT. These non-invasive modalities offer invaluable insights, guiding tailored therapeutic interventions.
Prognostic Indicators: MAT prognosis hinges on multifaceted factors, including comorbidities, age, and treatment response. Effective management of MAT, coupled with holistic care addressing underlying conditions, typically yields favorable outcomes. However, uncontrolled MAT poses risks of complications like heart failure or stroke, underscoring the importance of vigilant monitoring and intervention.
Holistic Management Approach: Holistic MAT management integrates pharmacotherapy, lifestyle modifications, and procedural interventions. Beta-blockers and calcium channel blockers stand as frontline agents for rate control, while antiarrhythmic drugs may be considered for rhythm management. Lifestyle adjustments, encompassing dietary modifications and stress reduction, complement medical therapy, fostering comprehensive wellness.
Pioneering Therapeutic Frontiers: Exploring novel therapeutic avenues unveils promising prospects in MAT care. Catheter ablation emerges as a transformative intervention, ablating aberrant cardiac foci and restoring rhythm stability. Additionally, ongoing research ventures into gene therapy and precision medicine herald a paradigm shift in MAT treatment paradigms.
Conclusion: The journey of MAT diagnosis and management epitomizes the synergy between clinical acumen, technological innovation, and patient-centric care. By unraveling diagnostic intricacies, understanding prognostic determinants, and embracing therapeutic innovations, healthcare stakeholders empower individuals with MAT to navigate their cardiac journey with resilience and hope.
0 notes
Text
Ablation Procedures for Arrhythmias in Bangladesh: Types and Benefits

Living with an irregular heartbeat, or arrhythmia, can be unsettling and disruptive. But in Bangladesh, hope beats strong with ablation procedures, advanced techniques that help regulate your heart rhythm and improve your quality of life. This guide explores the different types of ablation, their benefits, and access to these life-changing procedures in Bangladesh.
Understanding Arrhythmias:
Imagine your heart like an orchestra, relying on coordinated electrical signals to maintain a steady rhythm. Arrhythmias disrupt this rhythm, causing rapid, slow, or fluttering heartbeats. Common arrhythmias in Bangladesh include:
- Atrial fibrillation (AFib): Uncoordinated electrical activity in the upper chambers of the heart, causing irregular and often rapid heartbeats.
- Atrial flutter: A specific type of AFib with a faster, more regular rhythm.
- Supraventricular tachycardia (SVT): Rapid heartbeats originating above the ventricles, the lower chambers of the heart.
- Ventricular tachycardia (VT): Fast heartbeats originating in the ventricles, potentially dangerous and requiring immediate medical attention.
The Power of Ablation:
Think of ablation as a conductor meticulously correcting the rhythm of your heart. Ablation procedures use radiofrequency energy or heat to destroy small areas of heart tissue responsible for abnormal electrical signals, effectively "resetting" your heart's rhythm.
Types of Ablation in Bangladesh:
- Catheter ablation: The most common type, using thin tubes (catheters) inserted through blood vessels to reach the heart and deliver radiofrequency energy to target areas.
- Surgical ablation: Open-heart surgery for ablation may be necessary for complex arrhythmias or those not responding to catheter ablation.
Benefits of Ablation Procedures:
- Effective rhythm control: Ablation can significantly reduce or even eliminate arrhythmias, improving symptoms like fatigue, dizziness, and palpitations.
- Improved quality of life: Regain control of your heart rhythm and lead a more active and fulfilling life.
- Reduced medication dependence: In some cases, ablation can decrease reliance on medications for arrhythmia control.
- Minimally invasive options: Most ablations are performed using catheters, leading to shorter hospital stays and faster recovery times compared to open-heart surgery.
Accessibility in Bangladesh:
Ablation procedures are becoming increasingly available in Bangladesh, with advanced facilities and experienced cardiologists specializing in electrophysiology (EP) at:
- National Heart Foundation of Bangladesh
- Square Hospitals
- Chittagong Medical College Hospital
- Private cardiac centers offering advanced EP services
Finding the Right Specialist:
Consult a cardiologist specializing in EP for a comprehensive evaluation and discuss whether ablation is right for you. They will consider your specific arrhythmia type, medical history, and overall health to determine the best approach.
Taking Control of Your Heart Rhythm:
Ablation procedures offer a powerful tool for managing arrhythmias in Bangladesh, empowering you to reclaim your heart health and well-being. By understanding the procedure, its benefits, and accessibility, you can make informed decisions about your care and live a life less interrupted by irregular heartbeats.
Read the full article
0 notes
Text
10 Diseases of the Heart

Heart disease, a pervasive health concern, encompasses a spectrum of conditions affecting the cardiovascular system, from congenital defects to acquired disorders. According to the Centers for Disease Control and Prevention (CDC), it stands as the leading cause of death in the United States, claiming 1 in 4 lives. Understanding the intricacies of heart disease, including its types, symptoms, causes, treatments, preventive measures, and the overall outlook, is crucial for effective management and mitigation of its impact.
Types of Heart Disease:
1.Coronary Artery Disease (CAD):
Description: Arteries supplying blood to the heart become clogged with plaque.
Risk: Plaque can rupture, leading to a heart attack.
2. Congenital Heart Defects:
Description: Present at birth, affecting heart structure or connections.
Symptoms: May not be noticeable until a routine check.
3. Arrhythmia:
.Description: Irregular heartbeat due to faulty electrical impulses.
Types: Tachycardia (fast), Bradycardia (slow), Premature contractions, Atrial fibrillation.
4.Dilated Cardiomyopathy:
Description: Heart chambers dilate, weakening the heart muscle.
Causes: Past heart attacks, arrhythmias, toxins, and genetics.
5.Myocardial Infarction (Heart Attack)
Description: Blood flow interruption, damaging or destroying part of the heart muscle.
Causes: Plaque, blood clot, or artery spasms.
6.Heart Failure:
Description: Heart works inefficiently; can result from various heart-related conditions.
7.Hypertrophic Cardiomyopathy:
Description: Genetic thickening of heart muscle, affecting pumping ability.
Risk: Common cause of cardiac death in young individuals.
8.Mitral Valve Regurgitation:
Description: Mitral valve doesn’t close tightly, allowing blood back into the heart.
Complications: Enlarged heart, heart failure.
9.Mitral Valve Prolapse:
Description: Valve flaps of mitral valve bulge into the left atrium.
Prevalence: Affects around 2% of the population.
10.Aortic Stenosis:
Description: Narrowing of the aortic valve, hindering blood flow.
Causes: Congenital anomalies, calcium deposits, or scarring.
Symptoms of Heart Disease:
Symptoms vary based on the type but can include:
Angina (chest pain)
Difficulty breathing
Fatigue and lightheadedness
Swelling due to fluid retention
Cyanosis (blue skin) in congenital defects
Symptoms of a heart attack: chest pain, breathlessness, nausea, etc.
Causes and Risk Factors:
Genetic Causes:
Some heart diseases have a genetic basis.
Lifestyle Factors:
High blood pressure, high cholesterol, smoking, excessive alcohol intake, obesity, diabetes.
Other Factors
Age, history of preeclampsia during pregnancy, low activity levels, sleep apnea, stress, leaky heart valves.
Treatments:
Medications:
Anticoagulants, antiplatelet therapies, ACE inhibitors, beta-blockers, diuretics, etc.
Surgery:
Coronary artery bypass surgery, valve replacement or repair, repair surgery, device implantation, laser treatment, maze surgery.
Prevention:
. Lifestyle Measures:
. Balanced diet, regular exercise, maintaining a healthy weight, quitting smoking, limiting alcohol intake.
. Managing Underlying Conditions:
. Treating conditions like high blood pressure, obesity, and diabetes.
Outlook:
Overall Risk:
Common health problem; leading cause of death in the U.S.
Preventive Steps:
Many types are preventable through lifestyle changes and early intervention.
Conclusion:
Heart disease’s multifaceted nature demands a nuanced understanding for effective prevention and management. Regular medical checkups, healthy lifestyle choices, and awareness of symptoms contribute to better heart health. Early intervention and adherence to medical advice play key roles in improving outcomes for individuals with heart disease, reinforcing the importance of comprehensive education and public health initiatives.
For Health Sciences Assignment Help,
Email Us At;
#healthcare#fullmetal alchemist#medical students#aesthetic#assignment help#ratblr#plants#medicine#medicare#nursing school#nursing student#pets#kittens#nurse#medical help#puppies#kitty#kitten#kitty cat#hello kitty#knight rider
0 notes
Text
Understanding the Exercise Stress Test: Unveiling the Secrets of Cardiovascular Health
The exercise stress test, often referred to as a stress ECG or treadmill test, is a vital diagnostic tool in the field of cardiology. It plays a crucial role in assessing the cardiovascular health of individuals, particularly those at risk for heart disease. In this article, we will explore the exercise stress test, how it works, its significance in cardiovascular assessment, and what to expect during the procedure.

What Is an Exercise Stress Test?
An exercise stress test is a diagnostic procedure that evaluates the performance of your heart during physical activity. The test is designed to monitor how your heart responds to increased demands for blood and oxygen when you engage in exercise. It helps detect abnormalities in heart function, such as reduced blood flow to the heart muscles, irregular heart rhythms, and other issues that may not be apparent at rest.
How Does It Work?
During an exercise stress test, you will typically be asked to walk on a treadmill or pedal a stationary bicycle while connected to various monitoring devices. These devices will continuously record your heart rate, blood pressure, and electrocardiogram (ECG) readings. The test begins at a slow pace and gradually increases in intensity. You will be closely observed for any signs or symptoms of cardiovascular problems, such as chest pain, shortness of breath, dizziness, or irregular heartbeats.
The test continues until you reach your target heart rate, experience significant symptoms, or your healthcare provider decides to stop the test for safety reasons. Afterward, you will go through a cool-down period to gradually lower your heart rate.
Why Is It Important?
The exercise stress test serves several critical purposes in cardiovascular health assessment:
Detecting Coronary Artery Disease (CAD): CAD is a common condition where the arteries supplying blood to the heart become narrowed or blocked by plaque buildup. An exercise stress test can reveal reduced blood flow to the heart muscles during physical activity, indicating the presence of CAD.
Assessing Exercise Tolerance: The test provides valuable information about your exercise tolerance and helps determine if you have any limitations or risks associated with physical activity.
Identifying Heart Rhythm Disorders: Abnormal heart rhythms, known as arrhythmias, can be detected during the stress test. These may include atrial fibrillation, ventricular tachycardia, or other irregular heartbeats.
Evaluating Heart Medications: The test can help assess the effectiveness of heart medications or treatment plans prescribed for individuals with known heart conditions.
Risk Stratification: Based on the results of the exercise stress test, healthcare providers can stratify patients into low, moderate, or high cardiovascular risk categories, guiding further diagnostic and treatment decisions.
What to Expect During the Test
Before undergoing an exercise stress test, you will typically have a pre-test assessment, which includes a medical history review and a physical examination. It's essential to inform your healthcare provider about any existing medical conditions, medications, or allergies you may have.
During the test:
You will be asked to wear comfortable clothing and appropriate footwear.
Electrodes will be attached to your chest, arms, and legs to monitor your heart's electrical activity.
A blood pressure cuff may be placed on your arm to monitor your blood pressure throughout the test.
You will start exercising on the treadmill or stationary bike under the supervision of a trained healthcare provider.
The intensity of exercise will gradually increase to reach your target heart rate or until you experience any concerning symptoms.
The test will be terminated when you achieve the target heart rate, develop significant symptoms, or when your hea lthcare provider determines it's safe to stop.
After the test, you will go through a cool-down period to allow your heart rate and blood pressure to return to normal.
For More Info:-
Fall assessment
Vascular dementia
Care co-ordination
best price echocardiogram
0 notes
Text
Guardians of the Heart: Implantable Cardioverter Defibrillators.
Implantable Cardioverter Defibrillators (ICDs) are sophisticated medical devices that have revolutionized the management of life-threatening heart rhythm disorders. This article provides an in-depth look at ICDs, including their purpose, how they work, who may benefit from them, the implantation process, and potential advantages.
Understanding Implantable Cardioverter Defibrillators:
Purpose:
ICDs are primarily designed to treat ventricular tachycardia and ventricular fibrillation, two serious heart rhythm disorders that can lead to sudden cardiac arrest.
They continuously monitor the heart's rhythm and deliver electrical shocks when abnormal rhythms are detected.
How ICDs Work:
Continuous Monitoring:
ICDs use leads (thin wires) placed in the heart to detect electrical signals and monitor heart rhythm.
The device can distinguish between normal and abnormal rhythms.
Intervention:
When a life-threatening rhythm is detected, the ICD delivers precisely timed electrical shocks to restore normal heart rhythm.
This rapid response can prevent sudden cardiac death.
Candidates for ICDs:
High-Risk Patients:
Individuals with a history of ventricular tachycardia, ventricular fibrillation, or sudden cardiac arrest.
Those at risk due to heart conditions like cardiomyopathy or previous heart attacks.
The Implantation Process:
Surgical Procedure:
Implanting an ICD involves a surgical procedure that typically takes 1-2 hours.
The device is placed under the skin, usually near the collarbone.
Lead Placement:
Leads are carefully threaded through blood vessels into the heart's chambers.
Proper lead positioning is crucial for effective monitoring and therapy.
Advantages of ICDs:
Life-Saving Potential:
ICDs can deliver shocks within milliseconds, potentially preventing sudden cardiac death.
They provide peace of mind for individuals at high risk of life-threatening arrhythmias.
Continuous Monitoring:
ICDs offer ongoing heart rhythm monitoring, allowing healthcare providers to assess the patient's condition remotely.
Improved Quality of Life:
Many patients experience reduced anxiety and fear of sudden cardiac events.
Increased confidence to engage in daily activities.
Potential Risks and Considerations:
Possible Risks:
Infection or bleeding at the implantation site.
Lead dislodgment or damage.
Inappropriate shocks in response to non-life-threatening rhythms.
REFERENCE:
TX Hospitals Group, Hyderabad is one of the country’s largest and fastest-growing chains of multi-super specialty hospitals.
CONTACT : 9089489089
Book an appointment now
#Implantable Cardioverter Defibrillators#heart rhythm disorders#ICD therapy#hospitals#health#procedures#surgery
0 notes
Text
Understanding Cardiac Arrhythmia
Cardiac arrhythmia is a heart condition characterized by irregular heartbeats, either too fast (tachycardia) or too slow (bradycardia). These abnormal rhythms disrupt the heart's normal electrical signals, affecting its ability to pump blood effectively.
While occasional irregular heartbeats may be harmless, persistent or severe arrhythmias can lead to serious complications, including fainting, heart failure, or even cardiac arrest.
Understanding the symptoms of cardiac arrhythmia is crucial for early detection and timely treatment. Common signs include palpitations, rapid heartbeat, dizziness, shortness of breath, and chest discomfort.
However, some arrhythmias may not manifest noticeable symptoms, emphasizing the importance of regular heart check-ups, especially for individuals with risk factors like high blood pressure, heart disease, or a family history of arrhythmias.
For residents in Bangalore seeking expert cardiac care, Kauvery Hospital stands as a top hospital in the region, renowned for its state-of-the-art facilities and a team of skilled cardiologists. The hospital employs advanced diagnostic tools to assess heart rhythm disorders accurately.
Treatment options may include medication, lifestyle changes, or medical procedures like catheter ablation or implantation of a pacemaker or defibrillator.
Conclusion:
With a commitment to excellence and patient-centric care, Kauvery Hospital, the Top Cardiac Hospital in Bangalore provides comprehensive support to individuals with cardiac arrhythmia, ensuring a healthier heart and improved quality of life.
0 notes
Text
Causes of Cardiac Arrest in Young Adults: Understanding the Risks
Cardiac arrest, a sudden loss of heart function, is a life-threatening condition that can occur unexpectedly. While it is often associated with older individuals, it's important to recognize that young adults can also be susceptible to cardiac arrest. Understanding the causes of cardiac arrest in this age group is crucial for prevention and prompt medical attention. In this blog, we will explore the potential causes of cardiac arrest in young adults, highlighting the importance of seeking care from the best hospital in Ballabgarh, Haryana, for comprehensive cardiac evaluation and treatment.
1. Inherited Cardiac Conditions:
Several inherited cardiac conditions can lead to cardiac arrest in young adults. These include hypertrophic cardiomyopathy (HCM), arrhythmogenic right ventricular dysplasia (ARVD), Long QT syndrome (LQTS), and Brugada syndrome. These conditions often go undetected until a cardiac event occurs, making proper evaluation by experienced cardiologists essential for early detection and management.
2. Structural Heart Abnormalities:
Certain structural abnormalities of the heart, present from birth or acquired later in life, can increase the risk of cardiac arrest in young adults. Conditions such as congenital heart defects, coronary artery anomalies, and valve abnormalities can disrupt normal heart function and trigger a cardiac event. Regular cardiac screenings and evaluation at a reputable hospital can help identify these conditions and allow for timely interventions.
3. Coronary Artery Disease (CAD):
While coronary artery disease is often associated with older adults, it can also affect young individuals, especially those with risk factors such as obesity, diabetes, hypertension, and a family history of early-onset heart disease. CAD occurs when the arteries supplying blood to the heart become narrowed or blocked, potentially leading to a heart attack and subsequent cardiac arrest.
4. Sudden Cardiac Arrest Syndromes:
Certain conditions, collectively known as sudden cardiac arrest syndromes, can cause cardiac arrest in young adults. These include Brugada syndrome, catecholaminergic polymorphic ventricular tachycardia (CPVT), and Wolff-Parkinson-White (WPW) syndrome. These syndromes often involve abnormal electrical activity in the heart, leading to dangerous arrhythmias and cardiac arrest.
5. Substance Abuse and Stimulant Use:
Illicit drug use, particularly stimulants like cocaine or amphetamines, can significantly increase the risk of cardiac arrest in young adults. These substances can cause abnormal heart rhythms, increased blood pressure, and damage to the heart muscle, all of which can contribute to sudden cardiac arrest.
6. Commotio Cordis:
Commotio cordis is a rare but potentially fatal condition caused by a sudden impact to the chest, typically during sports activities. It can result in an abnormal heart rhythm that leads to cardiac arrest. This emphasizes the importance of appropriate safety measures and protective equipment when engaging in physical activities.
Conclusion:
While cardiac arrest is often associated with older individuals, young adults can also experience this life-threatening condition. Understanding the causes of cardiac arrest in this age group is crucial for prevention and timely medical intervention. If you or a loved one are at risk or have experienced cardiac arrest, it is essential to seek care from the best hospital in Ballabgarh, Haryana, for a comprehensive cardiac evaluation, diagnosis, and treatment. Experienced cardiologists and advanced cardiac facilities can provide the necessary expertise to manage inherited cardiac conditions, structural abnormalities, coronary artery disease, sudden cardiac arrest syndromes, and other contributing factors. Remember, early detection and appropriate management are key to reducing the risks associated with cardiac arrest in young adults.
0 notes
Text
Pacemaker Implantation: Enhancing Cardiac Function

Pacemaker implantation is a common medical procedure used to treat individuals with abnormal heart rhythms (arrhythmias) and to improve their cardiac function and overall quality of life. A pacemaker is a small electronic device that helps regulate the heart's electrical activity and ensures that it beats at a steady and appropriate pace. In this article, we will explore the process of pacemaker implantation, indications for the procedure, types of pacemakers, the implantation procedure itself, recovery and follow-up care, and the potential benefits and considerations associated with pacemaker implantation.
Indications for Pacemaker Implantation:
Pacemakers are recommended for individuals with various heart rhythm abnormalities, including:
a. Bradycardia: A slow heart rate, typically defined as fewer than 60 beats per minute, which can result in dizziness, fainting, fatigue, and other symptoms.
b. Heart Block: An interruption or delay in the electrical signals that regulate the heartbeat, leading to an irregular heart rhythm and potential symptoms such as dizziness, shortness of breath, and fatigue.
c. Arrhythmias: Certain types of arrhythmias, such as atrial fibrillation or ventricular tachycardia, may require a pacemaker to help manage the heart's rhythm.
Types of Pacemakers:
Pacemakers can be categorized based on their functionality and features. The two main types are:
a. Single-Chamber Pacemakers: These pacemakers have one lead (wire) that connects the device to either the right atrium or the right ventricle of the heart, depending on the specific needs of the patient.
b. Dual-Chamber Pacemakers: Dual-chamber pacemakers have two leads—one positioned in the right atrium and the other in the right ventricle. This allows for more synchronized pacing and coordination between the upper and lower chambers of the heart.
Pacemaker Implantation Procedure:
a. Preoperative Evaluation: Before the pacemaker implantation procedure, the patient undergoes a thorough evaluation, which includes a medical history review, physical examination, and potentially additional tests, such as electrocardiogram (ECG), echocardiogram, or electrophysiological studies. These tests help determine the appropriate pacemaker type and placement.
b. Anesthesia and Incision: Pacemaker implantation is usually performed under local anesthesia with sedation. A small incision is made, typically in the upper chest, where the pacemaker generator is placed. The leads are then inserted into the veins and guided to the appropriate heart chambers.
c. Lead Placement and Testing: The leads are carefully positioned within the heart chambers and connected to the pacemaker generator. Once the leads are in place, their position and functionality are tested to ensure proper pacing and sensing capabilities.
d. Closure and Recovery: After confirming the correct functioning of the pacemaker system, the incision is closed with stitches or surgical tape. The patient is then monitored in a recovery area before being transferred to a hospital room or discharged home on the same day or the following day.
Recovery and Follow-Up Care:
a. Healing and Incision Care: Following pacemaker implantation, it is important to keep the incision clean and dry, as directed by the healthcare provider. The patient should avoid strenuous activity and heavy lifting for several weeks to allow for proper healing.
b. Medications and Monitoring: The patient may be prescribed medications, such as antibiotics or pain relievers, as needed. Routine follow-up appointments will be scheduled to monitor the pacemaker's functioning, adjust settings if necessary, and ensure the patient's overall well-being.
c. Lifestyle Considerations: After pacemaker implantation, most individuals can resume their normal activities, including exercise and driving, once they have fully recovered. However, certain precautions and considerations may be advised, such as avoiding intense electromagnetic fields or undergoing regular device checks to ensure optimal performance.
Potential Benefits and Considerations:
a. Improved Heart Function: Pacemakers help regulate the heart's rhythm, ensuring that it beats at an appropriate rate. By doing so, they alleviate symptoms associated with bradycardia, heart block, and certain arrhythmias, improving overall heart function and quality of life.
b. Symptom Relief: Pacemaker implantation can significantly reduce symptoms such as dizziness, fatigue, and shortness of breath that are often associated with abnormal heart rhythms.
c. Long-Term Management: Pacemakers provide long-term management for individuals with chronic heart rhythm disorders, allowing them to lead active and fulfilling lives.
d. Risks and Considerations: While pacemaker implantation is generally a safe procedure, it carries certain risks, including infection, bleeding, lead dislodgement or malfunction, and complications associated with anesthesia. The healthcare provider thoroughly discusses the individualized risks and benefits with the patient before proceeding with the procedure.
Conclusion:
Pacemaker implantation is a valuable intervention for individuals with abnormal heart rhythms. It helps regulate the heart's electrical activity, alleviates symptoms, and improves overall cardiac function. With advancements in technology and surgical techniques, pacemaker implantation has become a routine and effective procedure. If you or a loved one is experiencing heart rhythm abnormalities, consulting with a cardiologist or cardiac electrophysiologist can provide valuable insights and guidance on whether pacemaker implantation is a suitable treatment option. The procedure, coupled with appropriate postoperative care and regular follow-up, can lead to significant improvements in cardiac health and quality of life. Find everything about Pacemaker Implantation costs in India that range from 3000 - 7500 USD.
0 notes
Text
Best Treatment for Arrhythmia in Delhi
Arrhythmia refers to an abnormal heart rhythm that can cause the heart to beat too fast, too slow, or irregularly. This condition can affect the heart's ability to pump blood effectively, leading to various complications. Arrhythmias can be mild or life-threatening and require prompt medical attention. Dr. Rajiv Agarwal is one such specialist who has earned a reputation as one of the best arrhythmia doctor in Delhi. With 30 years of experience in the field of cardiology, Dr. Agarwal is currently associated with Max Smart Super Speciality Hospital in Saket, New Delhi. He is known for his expertise in diagnosing and treating various types of arrhythmias, including atrial fibrillation, supraventricular tachycardia, and ventricular tachycardia. Dr. Agarwal is a dedicated arrhythmia doctor in Delhi who provides comprehensive arrhythmia treatment services to his patients. He uses the latest techniques and medical advancements to ensure accurate diagnosis and effective treatment of arrhythmias. He works closely with his patients to develop a customized treatment plan that is tailored to their specific needs and medical history. As an arrhythmia specialist in Delhi, Dr. Agarwal also provides implantable device therapy, including pacemakers and implantable cardioverter-defibrillators (ICDs), for patients with arrhythmias. He is known for his expertise in performing complex procedures such as catheter ablation, a minimally invasive procedure used to treat certain types of arrhythmias. If you are looking for expert Best Treatment for Arrhythmia in Delhi, Dr. Rajiv Agarwal is the name to trust. With his vast knowledge and expertise, he can provide you with the most effective and personalized treatment plan for your condition. Book an appointment with Dr. Agarwal, the best arrhythmia doctor in Delhi, for the best possible care.
#Cardiac Arrhythmia Consultation in Delhi#Best Arrhythmia Surgery Doctors in Delhi#Heart Arrhythmia Treatment in Delhi#Cardiac Arrhythmia Treatment in Delhi#Best Doctors for Cardiac Arrhythmias Treatment in Delhi
0 notes