#peripheral parenteral nutrition
Text
STATE OF SHOCK AND INJURY: A release of the catecholamine epinephrine suppresses response to insulin.
Basal metabolic rate increases 7% for every degree rise in fever.
OBESITY: Obesity starts at a BMI of 30kg/m^2 (3 classes of obesity. BMI of 40kg/m^2 or > is Class III obesity). There are 3,500 calories per pound of body fat, so start with a deficit of 500cal/day for weight loss of 1 pound per week.
Initial rapid weight loss is water weight, due to glycogen stores pulled out from the liver (for every gram of carbohydrate stored, 3g of H2O are stored w/it)
You cannot spot lose fat. Plateau (can't continue to lose weight) occurs because BMR has dropped in order to match loss of weight.
DEFICIENCIES: stomatitis due to riboflavin (B2) deficiency
PREGNANCY: Pregnancy-induced hypertension begins at 20th week. But sodium restriction NOT recommended as the intervention.
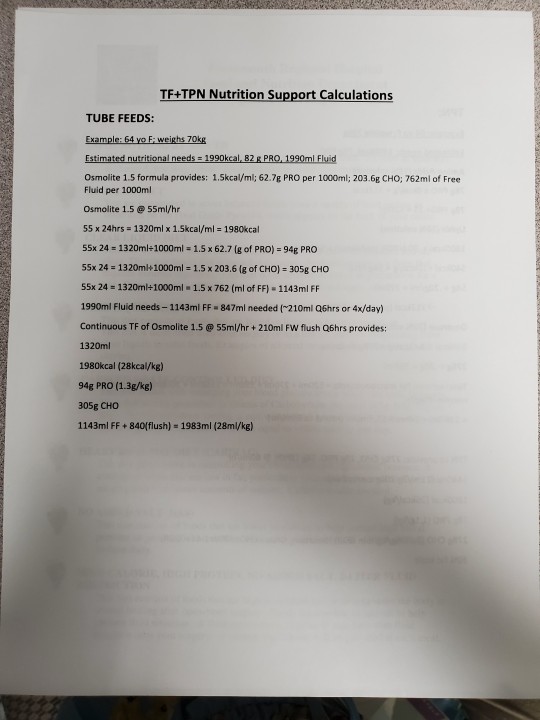
TUBE FEEDS: Deadly to feed into an ileus. Elemental formulas = more expensive.
4-hour hang time for open systems (concern for pathogenic activity/growth). 24-48 hours for closed systems.
Nasogastric tube for short-term enteral access (for those with NORMAL GI function who require nutrition support for 3-4 weeks). Bolus, intermittent, or continuous infusions.
Naso-duodenal OR naso-jejunal feeds for those unable to tolerate gastric tube feed (recall it is best to do gastric if possible to mimic body's natural eating functions).
Give 1cc of H2O per calorie ingested. Formulas that are 1 calorie per cc are 80-86% water.
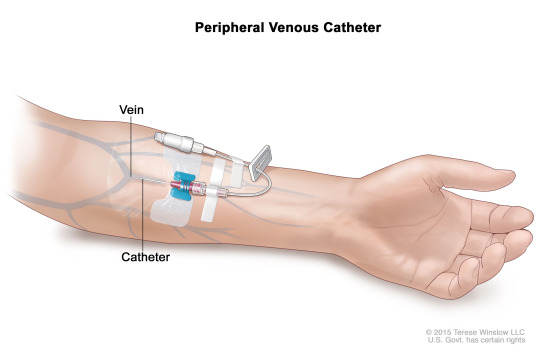
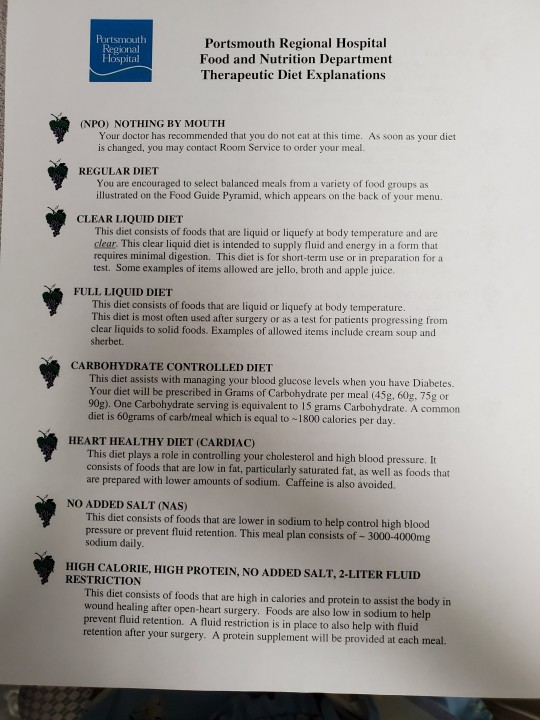
Peripheral parenteral nutrition (AKA total parenteral nutrition/TPN -- LAST resort due to the fact that it is like foie gras to the body, with implications of liver issues developing) is via small surface veins, which is short-term nutrition support. Includes protein and fat (a 10% solution of intravenous fat provides 1.1 calories per cc. A 20% solution provides 2.0 calories per cc. Think about propofol, delivered in a fat medium).
Solutions have dextrose, which provides 3.4 cal/g.
# of calories from a volume of dextrose = mL provided × % dextrose × 3.4
PPN/TPN is used to achieve anabolism when patients cannot eat by mouth and you cannot do an enteral tube feed.
Long-term central access occurs via cephalic, subclavian, or internal jugular vein and feed ls into superior vena cava.
PPN/TPN concerns: Bacterial translocation because you are bypassing the gut, which would normally kill bacteria that is ingested per os. Bacteria can travel through bloodstream and lead to SEPSIS.
In TPN, protein is provided for anabolism at 1g of nitrogen for every 150 calories ingested. The percent concentration tells you # of grams of protein per in 100mL of TPN solution (a 3% solution provides 3g of protein in 100mL of TPN solution).
Glucose infusion rate for dextrose in TPN should not exceed 4-5mg/kg/min for hyperglycemia prevention.
Fat is added to prevent essential fatty acid deficiency.
Begin tapering TPN for EN slowly, when enteral feeds provide 1/3 to 1/2 of nutrient requirements. When 60% of needs can be tolerated enterally, discontinue TPN.
BEWARE OF REFEEDING SYNDROME (starved cells take up nutrients, shifting K+, phos, and magnesium into the cell, causing HYPOKALEMIA, HYPOPHOSPHATEMIA, and HYPOMAGNESEMIA).
Overfeeding dextrose can lead to hyperglycemia
Dietary Reference Intake (DRI) reflects current population needs.
Recommended Dietary Allowance (RDA) is goals for healthy individuals.
Estimated Average Requiremenr (EAR) assesses group nutritional adequacy.
Upper Limit (UL) offers guidance on safe upper limits for nutrients such as vitamins.
Dietary Guidelines made to prevent chronic disease. DG written by USDA and HHS. Community nutrition programs use Dietary Guidelines to develop their plans (variety in eating, nutrient density, serving sizes, limit calories from saturated fats and added sugars, reduce sodium intake.
Healthy Eating Index (by USDA) is a measure of overall diet quality. Measures how well we follow the recommendations.
My Plate (USDA) shows essential food groups. Recommendations: balancing calories, foods to increase in the diet, foods to reduce.
Healthy People Program (HHS) identifies broad goals and specific objectives for improving health of the public. Focuses on disease prevention by changing behaviours.
The three steps in planning programs:
1) Mission Statement - describes the philosophy of the program. Need/Problem Statement describes the current situation, who says it's a problem, and what will occur if nothing is done.
2) Goals - goals are statements of broad direction and general purpose. Determine which health problems have nutritional implications. Determine what the high risk groups are. Determine what the most critical needs are.
3) Objectives - must be measurable. Objectives are more specific and defined than goals. Include specific target dates for completing specific projects. Evaluate alternative strategies available using cost effectiveness analysis.
Budget controls and coordinates activities. Indicates how and at what rate money should be expended.
Public health departments derive a portion of their income from general revenue taxes. Federal, local, and foundation grants are other sources of income.
Intervention via community nutrition programs relates to the 3 domains of learning: Cognitive, Affective, and Psychomotor.
Enabling makes it easier for people to act. Use the 4 Ps of marketing: Product, Price, Place, Promotion.
A strategy which involves psychomotor learning is helping people develop the skills needed to make and sustain new habits (e.g. how to budget, how to find the services they need.
Monitoring and Evaluation = the 4th step in the Nutrition Care Process (NCP)
Nutrition care outcomes represent results that the practitioner and nutrition care impacted individually. They can be linked to nutrition intervention goals. They're measurable and occur in a reasonable time period. They are attributed to the nutrition care provided. They're logical stepping stones to other health care outcomes.
Nutrition care outcomes are distinct from other health care outcomes b/c they represent the nutrition practitioner's specific contribution to care. They are grouped into 4 categories:
1) Food and Nutrition Related History
2) Lab Data and Medical Tests
3) Anthropometrics
4) Nutrition-Focused Physical Findings
#dietetics#clinical#notes#basal metabolic rate#nutrition care process#tube feeds#tube feedings#tpn#ppn#total parenteral nutrition#peripheral parenteral nutrition#vitamins#minerals#budget#sales#marketing#obesity#kidney#kidneys#renal#glucose infusion rate#GIR#enteral#enteral nutrition#nutrition programs#programs#dextrose#pregnancy#preeclampsia
0 notes
Text
This can help them identify opportunities and potential threats, so they can prepare for the present and future. MRI Research helps organizations to figure out whats happening in a given industry, including demand and supply statistics, degree of competition, state of competition with other emerging industries, future prospects considering technological changes, and external factors on the industry.
0 notes
Link
Industry analysis provides a company with an understanding of its position relative to other companies in the industry. This can help them identify opportunities and potential threats, so they can prepare for the present and future. MRI Research helps organizations to figure out whats happening in a given industry, including demand and supply statistics, degree of competition, state of competition with other emerging industries, future prospects considering technological changes, and external factors on the industry.
0 notes
Note
Okay so, if you've watched Knives Out, the scene where Marta's giving Harlan his medicine, she's not giving him the shots directly but putting them through a tube thing around his arm. What is that? How does it work? Can/ should I give my recovering from big injuries blorbo one of those?
I have seen Knives Out!
In fact, I did a whole post about it you can read here.
The thing in Harlan's arm was called a PICC, or Peripherally Inserted Central Catheter.
See, unlike in TV and most movies, when someone needs a medication given in a vein (called an intravenous medication), we don't just stick a needle into a vein- it has to go through some type of IV catheter.
An IV catheter (AKA a "peripheral venous catheter") is a thin plastic tube that goes through the skin and into a vein. The part sticking out of the skin can attach to a syringe to "push" medication into a vein, or be hooked up to a set of tubing and a bag of fluids or medication that has to go into the person over time.
The kind of these you'd get in a typical hospital setting only last about 7 days max, though. So if you need an IV for longer periods (like, say, you need IV antibiotics or chemotherapy infusions over weeks or months), or you need medications that are really irritating to a vein (like total parenteral nutrition or a medication to raise blood pressure), or you have such bad veins that no one can put an IV in you and you're critically ill, you need what is called a central line instead.
There are several types of central lines. The kind Harlan has is a PICC- meaning a central line that is inserted into a peripheral part of the body (usually the upper arm) and goes into a really deep vein. The catheter (thin plastic tube) is much longer than a typical IV catheter, and actually goes all the way to the heart. It is then secured to the skin by stitches and a plastic film that is changed every 5 days or so.
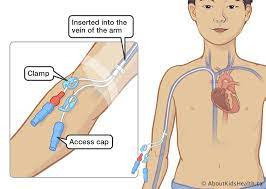

If your blorbo is in an ICU and can't keep his blood pressure up, or needs IV antibiotics to go home on, he might get a PICC or other central line. They do everything a regular IV does, plus they can take more irritating medications that would ruin peripheral IV catheters.
52 notes
·
View notes
Link
0 notes
Text
IV Cannula Types and Their Role in Modern Healthcare
Intravenous (IV) cannulas, often referred to as IV catheters, play a vital role in modern healthcare. They are indispensable tools used by medical professionals to provide essential fluids, medications, and blood products directly into a patient's bloodstream. Understanding the various IV cannula types is crucial for healthcare practitioners as it allows them to select the most appropriate device for the specific medical situation. In this article, we will explore the different IV cannula types and their essential role in contemporary healthcare.
Types of IV Cannulas
There are several types of IV cannulas available, each designed to meet distinct clinical needs. The choice of IV cannula type depends on factors such as the patient's condition, the purpose of the infusion, and the patient's vein characteristics. Here are some common types of IV cannulas:
1. Peripheral IV Cannulas: These are the most common type and are used for short-term infusions. Peripheral IV cannulas are typically inserted into veins in the arms, hands, or legs. They are available in various sizes and are suitable for a wide range of applications.
2. Midline IV Cannulas: These catheters are longer than peripheral IV cannulas and are designed for patients who require intravenous therapy for a more extended period, typically up to four weeks. They are inserted into larger veins in the upper arm.
3. Central Venous Catheters (CVCs): CVCs are long, flexible tubes that are inserted into large central veins, often near the heart. They are used for delivering medications, total parenteral nutrition (TPN), and chemotherapy. Common types of CVCs include subclavian, jugular, and femoral lines.
4. Peripherally Inserted Central Catheters (PICCs): PICCs are long, thin catheters inserted through a peripheral vein, usually in the arm, and advanced into the central circulation. They are used for extended courses of treatment and reduce the need for multiple needle sticks.
5. Winged or Butterfly Cannulas: These are small, short cannulas with wings that help stabilize the device once it's inserted. They are often used for pediatric patients or those with small or fragile veins.
The Role of IV Cannulas in Modern Healthcare
IV cannulas are indispensable in modern healthcare for a multitude of reasons:
1. Rapid Medication and Fluid Administration: IV cannulas allow healthcare providers to administer medications and fluids quickly and directly into the bloodstream, ensuring that the treatment takes effect promptly.
2. Continuous Monitoring: Many patients in critical care settings require continuous monitoring of their vital signs. IV cannulas provide a convenient way to obtain blood samples for laboratory tests and monitor parameters like oxygen levels and electrolyte balance.
3. Pain Management: In cases of severe pain, IV cannulas are used to deliver pain-relieving medications, providing rapid relief to patients.
4. Emergency Situations: IV cannulas are crucial in emergency situations such as trauma, shock, or cardiac arrest, where rapid access to the circulatory system can be a matter of life or death.
5. Long-Term Therapies: Patients with chronic conditions often require long-term intravenous therapy. This is where devices like PICCs and CVCs come into play, allowing for extended treatment without frequent insertions.
Denex International: Your IV Cannula Exporter
When it comes to types of IV cannula and their role in modern healthcare, it's essential to have access to reliable and high-quality medical supplies. Denex International is a trusted IV cannula exporter, providing a wide range of IV cannula types to healthcare professionals worldwide. With a commitment to quality and patient safety, Denex International offers a variety of IV cannulas, including peripheral IV cannulas, midline IV cannulas, CVCs, PICCs, and more.
Denex International's products meet international standards, ensuring that healthcare providers have access to the best tools for patient care. Whether you require IV cannulas for short-term or long-term therapies, Denex International can supply the right solution. As an established exporter, they understand the critical role IV cannulas play in modern healthcare and are dedicated to supporting the needs of healthcare institutions, clinics, and hospitals worldwide.
Contact Us
Name- Denex International
Phone- 0124 4115465
0 notes
Text
Ambulatory Infusion Pump Market Research Analysis Report
Ambulatory Infusion Pump Market, By Product Type (Ambulatory infusion pumps, Ambulatory infusion pumps Disposables, Accessories), Therapies (Parenteral Nutrition, Pain Management, Parkinson, Immunotherapy, Thalassemia, Chemotherapy, Hydration, Antibiotics, Analgesia and others), Platform (Web Based and Non Web Based), By Data Transmission (Historical Data and Real Time Data), Procedure (Subcutaneous, Epidural, Perineural, Intravenous Infusion And Others), Pump Type (Multiple Therapy Pump, Pain Management Pump, Epidural Pump, Twin Ambulatory Dual-Channel Pump, Multi-Therapy Children’s Pump And Others), End Users (Hospitals & Clinics And Home Settings) Geography (North America, Europe, Asia-Pacific, Middle East and Africa and South America)
Market Overview
The global ambulatory infusion pump market is anticipated to reach USD 15.7 billion by 2020 growing at a CAGR of 4.9% during the forecasting period, 2020-2028.
Ambulatory infusion pumps are considered the smart pumps that help in delivering the fluids into a patient’s body in a controlled manner. Factors such as an increase in demand for ambulatory infusion pumps rise in the number of surgical procedures performed and regular product recalls of infusion pumps are some of the major factors for the ambulatory infusion pump market.
Request Sample Pages of Report: https://www.delvens.com/get-free-sample/ambulatory-infusion-pump-market-trends-forecast-till-2028

Key Findings
The global ambulatory infusion pump market is segmented into product type, therapies, platform, data transmission, procedure, pump type, end-users, and geography
The product type segment is sub-segmented into an ambulatory infusion pump, ambulatory infusion pump Disposables, and Accessories. The ambulatory infusion pump segment has been segmented into wireless ambulatory infusion pumps pump and wired ambulatory infusion pumps. Ambulatory infusion pumps Disposables have been segmented into Intravenous Catheter (IV), Infusion Pump Extension Sets, Cassette Reservoirs, Infusion Pump Administration Sets, Administration Sets With Air-Eliminating Filter and Others. Intravenous Catheter (IV) has been further segmented into Tunneled Catheter, PICC Line, Implanted Port, and Peripheral Intravenous Catheter. Accessories have been segmented into Medication Clamps, Medication Tubing, and Others.
Make an Inquiry Before Buying: https://www.delvens.com/Inquire-before-buying/ambulatory-infusion-pump-market-trends-forecast-till-2028
Therapies segment has been segmented into Parenteral Nutrition, Pain Management, Parkinson, Immunotherapy, Thalassemia, Chemotherapy, Hydration, Antibiotics, Analgesia, and others. Pain Management has been segmented into Chronic Pain Management and Post-Operative Pain. Analgesia has been segmented into Patient-Controlled Epidural Analgesia (PCEA) and Patient-Controlled Analgesia (PCA).
The platform segment is sub-segmented into Web-Based and Non-Web Based.
The Data Transmission segment has been segmented into Historical Data and Real-Time Data.
The procedure segment has been segmented into Subcutaneous, Epidural, Perineural, Intravenous Infusion, and Others.
Pump Type has been segmented into Multiple Therapy Pump, Pain Management pump, Epidural Pump, Twin Ambulatory Dual-Channel pump, Multi-Therapy Children’s Pump, and Others.
End Users have been segmented into Hospitals & Clinics and Home Settings.
Geographically, the global ambulatory infusion pump market is sub-segmented into North America, Europe, Asia-Pacific, Middle East and Africa and South America and insights are provided for each region and major countries within the regions
Regional Analysis
North America region is the largest contributor to the ambulatory infusion pump market in the forecast period 2020-2028 and Asia-Pacific is expected to grow with the highest CAGR during the forecast period 2020-2028.
Competitive Landscape
Key players in the global ambulatory infusion pump market are Becton, Dickinson and Company, Baxter, ICU Medical, B. Braun, Fresenius Kabi, Medtronic, Smiths Medical, Terumo Corporation, Moog, Roche Diagnostics, Halyard Health, Mindray Medical, Micrel Medical, and Insulet Corporation and among others
Direct Purchase for the Research Report: https://www.delvens.com/checkout/ambulatory-infusion-pump-market-trends-forecast-till-2028
Recent Developments
The companies have come up with various promotional activities in from of launch, investment, acquisition, and other, for instance:
In August 2017, Smiths Medical has received the FDA 510k clearance on a wireless ambulatory infusion pump which will help the hospitals in increasing the efficiencies, reducing the costs, and improving the patient outcomes.
In April 2016, Smiths Medical had announced the new wireless ambulatory infusion system in the brand name of CADD-Solis in Australia, New Zealand, Ireland, and the United It helps in offering two-way wireless communication of infusion data in between the CADD-Solis pump and the PharmGuard Server software which would be installed on the hospital’s network
Hence, tremendous progress has been made over the last decade, and yet a lot more to come in recent years.
Read More:
About Us:
Delvens is a strategic advisory and consulting company headquartered in New Delhi, India. The company holds expertise in providing syndicated research reports, customized research reports and consulting services. Delvens qualitative and quantitative data is highly utilized by each level from niche to major markets, serving more than 1K prominent companies by assuring to provide the information on country, regional and global business environment. We have a database for more than 45 industries in more than 115+ major countries globally.
Delvens database assists the clients by providing in-depth information in crucial business decisions. Delvens offers significant facts and figures across various industries namely Healthcare, IT & Telecom, Chemicals & Materials, Semiconductor & Electronics, Energy, Pharmaceutical, Consumer Goods & Services, Food & Beverages. Our company provides an exhaustive and comprehensive understanding of the business environment.
Contact Us:
UNIT NO. 2126, TOWER B,
21ST FLOOR ALPHATHUM
SECTOR 90 NOIDA 201305, IN
+44-20-8638-5055
0 notes
Text
GOLDEN RULES FOR NURSES
NURSES
Golden Points to Remember
➥ Antiemetic drugs prevent vomiting.
➥ Intraosseous injections are given into the bone marrow.
➥ Intrathecal injections are given into the spinal cavity.
➥ Intramuscular injections should be given on 90° angle.
➥ Subcutaneous injections should be given on 45° angle.
➥ Intradermal injections should be given on 15° angle.
➥ Blood group ‘AB’ is known as universal recipient and blood group ‘O is known as universal donor.
➥ Mercury is used in thermometer because mercury is very sensitive to little change in temperature.
➥ For giving enema, left lateral position should be given.
➥ Air cushion is used to prevent bed sores.
➥ Hey’s test is performed for identify bile salts in urine
➥ Smith’s test is performed to found out presence of bile pigments in urine.
➥ Components of Total parenteral nutrition (TPN) are carbohydrates (glucose), amino acids, lipids,vitamins, minerals, and electrolytes.
➥ Insulin may be added to TPN to offset the high concentration of glucose and heparin may be added to limit the formation of a fibrous clot at the tip of the catheter.
➥ The bones in the forearm act as a natural splint by providing support to an I.V. access site.
➥ Don’t select an I.V. site on a paralyzed or traumatized arm.
➥ The basilica vein is normally used for a peripherally inserted central catheter (PICC) line.
➥ Because the insertion of a PICC line is below the level of the heart, an air embolism isn’t an expected occurrence.
➥ If a client has a high temperature, notify the physician before administering any blood product.
➥ No solution or product other than normal saline should be added to blood or blood product.
➥ Maslow’s hierarchy of needs must be met in the following order: physiologic (oxygen, food, water,sex, rest, and comfort), safety and security, love and belonging, self-esteem and recognition, and self- actualization.
➥ To avoid staining the teeth, the client should take a liquid iron preparation through a straw.
➥ Fluid oscillation in the tubing of a chest drainage system indicates that the system is working properly.
➥ The type of assessment that includes data related to a client’s biological, cultural, spiritual and social need is called Comprehensive Assessment.
➥ The Vital Signs are: 1. Temperature, 2. Pulse, 3.Respiration, 4. Blood pressure, and 5. Pain.
➥ Heat loss due to contact with circulating air movement is known as Convection.
➥ The range of marking in glass/clinical thermometer is 95-110° F and 35-43.3°C.
➥ Normal Rectal temperature is 99.6° F (37°C) (1°F ) higher than oral temperature).
➥ Rectal temperature is the most reliable.
➥ Relapsing fever: Fever episodes are separated by intervals of normal temperature for days or weeks.
➥ Rigor: Sudden rise in body temperature with shivering as seen in malaria.
➥ Increased depth of breathing with normal respiratory rate is called Hyperpnea.
➥ Cheyne-Stokes Respiration is characterized by altered period of Tachypnea and Apnea.
➥ Pulse deficit refers to the difference between apical pulse and radial pulse.
➥ A Blood Pressure Cuff that is too large will give falsely low reading of BP.
➥ Beneficence: Doing good for clients and providing benefit balanced against risk.
➥ Isotonic solutions allow free movement of water across the membrane without changing concentration of solutes on either side. E.g. 0.9% NaCl.
➥ Hypertonic solution: Fluids with solutes more concentrated than in cells, e.g. 5% dextrose.
🛑 Explanation
1. Antiemetic drugs prevent vomiting.
Antiemetic drugs are medications used to prevent or treat nausea and vomiting. They work by targeting different receptors in the body, including those in the gastrointestinal tract and the central nervous system.
There are several types of antiemetic drugs available, including:
1. Serotonin antagonists: These drugs block the action of serotonin, a neurotransmitter involved in nausea and vomiting. Examples include ondansetron, granisetron, and dolasetron.
2. Dopamine antagonists: These drugs block the action of dopamine, a neurotransmitter involved in nausea and vomiting. Examples include metoclopramide and prochlorperazine.
3. Histamine antagonists: These drugs block the action of histamine, a neurotransmitter involved in nausea and vomiting. Examples include dimenhydrinate and meclizine.
4. Cannabinoids: These drugs work by activating cannabinoid receptors in the body, which can help to reduce nausea and vomiting. Examples include dronabinol and nabilone.
Other types of antiemetic drugs include benzodiazepines, which can help to reduce anxiety and nausea, and corticosteroids, which can help to reduce inflammation and swelling that can contribute to nausea and vomiting.
Antiemetic drugs may be prescribed for a variety of conditions, including chemotherapy-induced nausea and vomiting, postoperative nausea and vomiting, and motion sickness, among others. It is important to note that antiemetic drugs may have side effects, and should only be taken as directed by a healthcare professional.
GOLDEN POINTS FOR NURSES
2. Intraosseous injections are given into the bone marrow.
Intraosseous injections are given directly into the bone marrow, typically of the long bones such as the femur, tibia, and humerus.
This route of administration is used when intravenous access is not feasible or when a more rapid onset of action is needed, such as in emergency situations.
Intraosseous injections are commonly used in pediatric patients, as well as in adult patients in emergency and critical care settings.
The technique involves using a specialized needle to penetrate the bone and access the marrow cavity, where medications or fluids can be injected directly into the bloodstream.
GOLDEN POINTS FOR NURSES
3. Intrathecal injections are given into the spinal cavity.
Intrathecal injections are given directly into the spinal cavity, specifically into the subarachnoid space surrounding the spinal cord.
This route of administration is used to deliver medications or other substances directly to the central nervous system, bypassing the blood-brain barrier. Intrathecal injections may be used to treat conditions such as chronic pain, spasticity, and certain types of cancer, among others.
The technique involves using a specialized needle to puncture the spinal canal and access the subarachnoid space, where medications or other substances can be injected. Because of the risks associated with this procedure, including infection, bleeding, and damage to the spinal cord or nerves, it is typically performed under strict sterile conditions by trained medical professionals.
Golden rules for NURSES
4. Intramuscular injections should be given on 90° angle.
The angle at which an intramuscular injection should be given can vary depending on the size of the needle and the location of the injection site. In general, a 90-degree angle is appropriate for most adult patients receiving intramuscular injections.
However, for patients who have less subcutaneous tissue or who are receiving injections in areas with less muscle mass, such as the deltoid muscle in the upper arm, a 45-degree angle may be more appropriate. It is important to follow proper injection technique and to consult with a healthcare provider if you have any questions or concerns about administering an intramuscular injection.
Golden rules for NURSES
5. Subcutaneous injections should be given on 45° angle.
The angle at which a subcutaneous injection should be given can vary depending on the size of the needle and the location of the injection site. In general, a 45-degree angle is appropriate for most adult patients receiving subcutaneous injections.
However, for patients who have less subcutaneous tissue or who are receiving injections in areas with less fat, such as the abdomen, a 90-degree angle may be more appropriate. It is important to follow proper injection technique and to consult with a healthcare provider if you have any questions or concerns about administering a subcutaneous injection.
Golden rules for NURSES
6. Intradermal injections should be given on 15° angle.
Yes, that's correct. Intradermal injections are administered at a shallow angle, typically between 5 and 15 degrees, into the dermis layer of the skin.
The angle used for an intradermal injection is much shallower than for an intramuscular or subcutaneous injection, as the goal is to inject the medication just under the surface of the skin.
This type of injection is commonly used for skin testing, such as for tuberculosis or allergies, and is typically given on the inner forearm or upper back. It is important to follow proper injection technique and to consult with a healthcare provider if you have any questions or concerns about administering an intradermal injection.
Golden rules for NURSES
7. Blood group ‘AB’ is known as universal recipient and blood group ‘O is known as universal donor.
Yes, that's correct. Blood group AB is known as the universal recipient because individuals with this blood type can receive blood from any other blood type without experiencing an adverse immune reaction. This is because they have both A and B antigens on the surface of their red blood cells, and therefore do not produce antibodies against either antigen.
On the other hand, blood group O is known as the universal donor because individuals with this blood type can donate blood to individuals with any other blood type without causing an adverse immune reaction. This is because they do not have A or B antigens on the surface of their red blood cells, and therefore do not produce antibodies against these antigens. However, individuals with blood group O can only receive blood from other individuals with blood group O, as their immune system will recognize the A and B antigens as foreign and produce antibodies against them.
Golden rules for NURSES
8. Mercury is used in thermometer because mercury is very sensitive to little change in temperature.
Yes, that is correct. Mercury is often used in thermometers because it is a liquid metal that has a high coefficient of thermal expansion, which means that it expands and contracts in response to changes in temperature. This makes it very sensitive to even small changes in temperature and allows for accurate temperature readings.
In addition, mercury has a low freezing point and a high boiling point, which means that it remains in a liquid state over a wide range of temperatures. This allows it to be used in both low-temperature and high-temperature applications.
However, it is important to note that mercury is a toxic substance and can be harmful if ingested or inhaled. For this reason, many countries have banned the use of mercury in thermometers and other consumer products, and alternative substances such as alcohol or digital thermometers are often used instead.
Golden rules for NURSES
9. For giving enema, left lateral position should be given.
Yes, the left lateral position is commonly used for administering an enema. This position helps to promote the flow of the enema solution into the rectum and prevents it from flowing back out.
To assume the left lateral position for an enema, the patient should lie on their left side with their left leg straight and their right knee bent slightly. They should bring their right knee up towards their chest to further open the rectal area. This position helps to straighten out the rectum and makes it easier to insert the enema tip.
It is important to follow proper enema administration technique and to use sterile equipment to minimize the risk of infection or injury. A healthcare provider should be consulted if you have any questions or concerns about administering an enema.
Golden rules for NURSES
10. Air cushion is used to prevent bed sores.
Air cushions can be used as part of a preventative strategy to help reduce the risk of bed sores, also known as pressure ulcers. Pressure ulcers can occur when there is prolonged pressure on a particular area of the skin, often caused by immobility or being in a seated or lying position for an extended period of time.
Air cushions are designed to distribute pressure evenly over the surface of the cushion, which can help reduce pressure on any particular area of the body. This can help to prevent the development of pressure ulcers and also provide greater comfort for the person sitting or lying on the cushion.
However, it is important to note that air cushions are just one component of a comprehensive pressure ulcer prevention plan. Other strategies may include repositioning the patient regularly, maintaining good skin hygiene, and providing adequate nutrition and hydration. It is important to work with a healthcare provider to develop an individualized care plan for preventing pressure ulcers in each patient.
Golden rules for NURSES
11. Hey’s test is performed for identify bile salts in urine
Hey's test is a laboratory test used to detect the presence of urobilinogen in urine, not bile salts. Urobilinogen is a colorless substance that is produced in the liver during the breakdown of bilirubin, a yellowish substance that is formed when old red blood cells are broken down.
Hey's test involves adding a chemical reagent to a urine sample, which causes any urobilinogen present to oxidize and turn pink or red in color. The intensity of the color change is used to determine the concentration of urobilinogen in the urine.
While Hey's test is not used specifically to identify bile salts in urine, elevated levels of urobilinogen in the urine can be an indication of liver disease or other medical conditions affecting the liver or biliary system, which can lead to the accumulation of bile salts in the urine. It is important to consult with a healthcare provider for proper diagnosis and treatment of any medical condition.
Golden rules for NURSES
12. Smith’s test is performed to found out presence of bile pigments in urine.
No, Smith's test is not used to detect the presence of bile pigments in urine. Smith's test is a laboratory test used to detect the presence of protein in urine.
Bile pigments, such as bilirubin and urobilinogen, may be present in urine in certain medical conditions affecting the liver or biliary system. However, there are other laboratory tests that are more commonly used to detect these substances in urine, such as the bilirubin test or the urobilinogen test.
It is important to consult with a healthcare provider for proper diagnosis and treatment of any medical condition that may be affecting the urinary system or other organ systems in the body.
Golden rules for NURSES
13. Components of Total parenteral nutrition (TPN) are carbohydrates (glucose), amino acids, lipids,vitamins, minerals, and electrolytes.
Yes, that is correct. Total parenteral nutrition (TPN) is a form of nutrition therapy that delivers all of the necessary nutrients, including carbohydrates (glucose), amino acids, lipids, vitamins, minerals, and electrolytes, directly into the bloodstream through a vein. TPN is typically administered when a patient is unable to obtain adequate nutrition through the gastrointestinal tract, such as in cases of severe malabsorption, intestinal obstruction, or other medical conditions.
The specific components and concentrations of TPN are tailored to the individual patient's needs based on factors such as age, weight, medical condition, and laboratory values. TPN is typically administered in a hospital setting and requires close monitoring by a healthcare provider to ensure proper dosing and to monitor for any potential complications or side effects.
Golden rules for NURSES
14. The bones in the forearm act as a natural splint by providing support to an I.V. access site.
Yes, that is correct. The bones in the forearm, specifically the radius and ulna, can act as a natural splint by providing support and stability to an IV access site. When an IV catheter is inserted into a vein in the arm, it can be secured in place using a dressing or tape to prevent movement or dislodgement. However, the bones in the forearm can also provide additional support and stability to the IV catheter, which can help to prevent accidental dislodgement or complications such as infiltration or extravasation.
It is important to ensure that the IV catheter is properly placed and secured, and to monitor the IV site for signs of complications such as swelling, redness, pain, or leakage. If any of these signs are present, it is important to notify a healthcare provider immediately.
Golden rules for NURSES
15. Don’t select an I.V. site on a paralyzed or traumatized arm.
Yes, that is correct. When selecting an IV site, it is important to avoid areas that are paralyzed or traumatized. A paralyzed limb may have reduced blood flow and sensation, which can increase the risk of complications such as infiltration or extravasation. Additionally, a traumatized limb may have damaged blood vessels or tissues, which can also increase the risk of complications.
When selecting an IV site, healthcare providers typically look for a site that has good blood flow, easy access, and minimal risk of complications. The most common sites for IV access are the veins in the arms, but other sites such as the hands or feet may be used if necessary. Factors such as the patient's medical condition, age, and overall health may also be taken into consideration when selecting an IV site.
It is important to properly assess the patient's veins and select the most appropriate site for IV access, while also considering the patient's comfort and safety. Proper insertion and maintenance of the IV catheter, as well as monitoring for signs of complications, can help to ensure optimal outcomes for the patient.
Golden rules for NURSES
16. Don’t select an I.V. site on a paralyzed or traumatized arm.
It is important to avoid selecting an intravenous (IV) site on a paralyzed or traumatized arm. There are several reasons for this:
Risk of further injury: If the arm is already traumatized or paralyzed, there is a risk of further injury or damage to the arm if an IV is inserted in that area. This can result in nerve damage, muscle damage, or other complications.
Difficulty monitoring: If the arm is paralyzed, it may be difficult to monitor for signs of infection or other complications at the IV site. This can lead to delayed diagnosis and treatment of any problems that may arise.
Reduced blood flow: A paralyzed or traumatized arm may have reduced blood flow, which can affect the delivery of fluids and medications through the IV. This can result in poor IV access or incomplete delivery of medication.
In general, it is important to choose a site for IV insertion that is healthy, well-vascularized, and free from any injuries or abnormalities. If a patient's arm is paralyzed or traumatized, it is best to select a different site for the IV. This can help ensure that the IV is placed safely and effectively, without causing any further harm to the patient.
Golden rules for NURSES
17. The basilica vein is normally used for a peripherally inserted central catheter (PICC) line.
The basilic vein is one of the veins that can be used for a peripherally inserted central catheter (PICC) line. A PICC line is a long, thin tube that is inserted through a peripheral vein (usually in the arm) and passed through to the larger veins near the heart. This type of catheter is often used for patients who require long-term intravenous (IV) access for medications, fluids, or other treatments.
The basilic vein is located on the medial (inner) side of the upper arm, and it runs from the elbow to the axilla (armpit). It is one of the larger veins in the arm, making it a good candidate for a PICC line insertion. Other veins that can be used for a PICC line include the cephalic vein and the brachial vein.
When a PICC line is inserted, the healthcare provider will use ultrasound guidance to locate the basilic vein and insert the catheter through the skin and into the vein. The catheter is then advanced through the vein and into the larger veins near the heart. Once the catheter is in place, it can be used for the administration of medications, fluids, or other treatments.
It is important to note that while the basilic vein is a common choice for a PICC line insertion, the healthcare provider will consider several factors when choosing the best vein for each patient. These factors may include the patient's medical history, the size and condition of the veins, and the specific needs of the patient's treatment plan.
Golden rules for NURSES
18. Because the insertion of a PICC line is below the level of the heart, an air embolism isn’t an expected occurrence.
While it is true that the insertion of a peripherally inserted central catheter (PICC) line is typically done below the level of the heart, an air embolism can still occur during the insertion process or while the catheter is in place.
An air embolism occurs when air bubbles enter the bloodstream and block the flow of blood to vital organs. While air embolisms are rare, they can be life-threatening if not promptly recognized and treated.
During the insertion of a PICC line, there is a risk of air entering the catheter or the bloodstream. Healthcare providers take precautions to minimize this risk by carefully priming and flushing the catheter and using specialized techniques to insert and position the catheter.
However, even with these precautions, it is still possible for air to enter the bloodstream. This can happen if the catheter becomes disconnected or if the patient experiences a sudden change in position that allows air to enter the catheter.
To minimize the risk of air embolism, healthcare providers carefully monitor patients during and after PICC line insertion. They may use ultrasound or other imaging techniques to confirm proper catheter placement and check for any signs of air in the bloodstream.
If an air embolism is suspected, immediate treatment is required. This may include stopping the infusion, administering supplemental oxygen, and positioning the patient in a way that prevents the air from traveling to the heart or lungs. In severe cases, more advanced treatments may be necessary, such as hyperbaric oxygen therapy or surgery.
Golden rules for NURSES
19. If a client has a high temperature, notify the physician before administering any blood product.
If a client has a high temperature, it is important to notify the physician before administering any blood product. This is because a high temperature can be a sign of infection or another underlying condition that may be exacerbated by the administration of blood products.
Blood products are typically used to treat a variety of conditions, including anemia, bleeding disorders, and immune system disorders. While these products can be life-saving, they also carry certain risks, such as infection, allergic reactions, and transfusion reactions.
One of the key steps in ensuring the safe administration of blood products is to carefully screen patients for any underlying conditions or risk factors that may increase their risk of complications. This includes monitoring for signs of infection, such as a high temperature, before administering any blood products.
If a client has a high temperature, the physician may want to delay or modify the administration of blood products until the underlying cause of the fever can be identified and treated. This may involve further testing or evaluation to determine if the client has an infection or other condition that could increase their risk of complications from the blood product.
By notifying the physician of any signs of infection or other concerns before administering blood products, healthcare providers can help ensure the safe and effective use of these important treatments.
Golden rules for NURSES
20. No solution or product other than normal saline should be added to blood or blood product.
It is generally recommended that no solution or product other than normal saline should be added to blood or blood products. This is because the addition of other substances can increase the risk of adverse reactions and other complications.
Normal saline, also known as 0.9% sodium chloride, is a sterile solution of salt and water that is used to replace lost fluids and restore electrolyte balance in the body. It is often used as a diluent for blood and blood products because it is compatible with these substances and does not increase the risk of adverse reactions or complications.
Adding other solutions or products to blood or blood products can alter their composition and increase the risk of adverse reactions, such as transfusion reactions, allergic reactions, or infections. For example, adding medications or other substances to blood products can increase the risk of medication errors and other complications.
In some cases, healthcare providers may need to add a medication or other substance to blood or blood products to meet the specific needs of the patient's treatment plan. When this is necessary, it is important to carefully follow established protocols and guidelines to minimize the risk of adverse reactions or other complications.
Overall, the addition of any solution or product to blood or blood products should only be done under the direction of a healthcare provider with appropriate training and expertise in transfusion medicine.
Golden rules for NURSES
21. Maslow’s hierarchy of needs must be met in the following order: physiologic (oxygen, food, water,sex, rest, and comfort), safety and security, love and belonging, self-esteem and recognition, and self- actualization.
Maslow's hierarchy of needs is a theory that suggests that human needs can be organized into a hierarchy, with lower-level needs taking priority over higher-level needs. According to Maslow's theory, the hierarchy of needs must be met in a specific order, with lower-level needs needing to be met before higher-level needs can be addressed.
The hierarchy of needs includes the following levels, in order from lowest to highest:
Physiological needs: These are the most basic needs, including the need for oxygen, food, water, shelter, sleep, and other bodily needs.
Safety needs: Once physiological needs are met, individuals have a need for safety and security, including physical safety, financial security, and stability.
Love and belonging needs: After safety needs are met, individuals have a need for love, affection, and a sense of belonging, including relationships with family, friends, and community.
Esteem needs: Once the need for love and belonging is met, individuals have a need for self-esteem and recognition from others, including achievement, status, and respect.
Self-actualization needs: Once all of the other needs are met, individuals have a need for self-actualization, including personal growth, self-fulfillment, and realizing their full potential.
In order to meet higher-level needs, lower-level needs must first be met. For example, an individual who is hungry and thirsty will not be able to focus on safety needs until their basic physiological needs are met. Similarly, an individual who is struggling to find a sense of belonging may have difficulty focusing on self-esteem needs until they feel a sense of connection with others.
By understanding Maslow's hierarchy of needs, healthcare providers can better understand the needs and priorities of their patients and develop treatment plans that address their most pressing needs first. This can help promote better outcomes and improve patient satisfaction.
Golden rules for NURSES
22. To avoid staining the teeth, the client should take a liquid iron preparation through a straw.
To avoid staining the teeth, it is recommended that the client take a liquid iron preparation through a straw. Iron supplements can cause staining of the teeth, which can be unsightly and difficult to remove. By using a straw to take the supplement, the liquid can bypass the teeth and reduce the risk of staining.
In addition to using a straw, there are other strategies that can help minimize the risk of staining from iron supplements. For example, the client can rinse their mouth with water after taking the supplement to help remove any residual liquid from the teeth. They may also want to avoid brushing their teeth immediately after taking the supplement, as this can actually spread the iron around and increase the risk of staining.
If the client does experience staining from the iron supplement, there are several options for addressing the issue. One approach is to switch to a different form of iron supplement, such as a tablet or capsule, which may be less likely to cause staining. Alternatively, the client may be able to use a whitening toothpaste or receive professional teeth whitening treatment to help remove the stains.
Overall, while liquid iron preparations can be an effective treatment for iron deficiency, they can also cause staining of the teeth. By using a straw and taking other steps to minimize the risk of staining, clients can help ensure that they receive the benefits of iron supplementation without experiencing unwanted side effects.
Golden rules for NURSES
23. Fluid oscillation in the tubing of a chest drainage system indicates that the system is working properly.
Fluid oscillation in the tubing of a chest drainage system does not necessarily indicate that the system is working properly. In fact, fluid oscillation can be an indication of a problem with the system that requires attention from healthcare providers.
A chest drainage system is typically used to remove excess air or fluid from the pleural space in the chest. The system consists of a drainage tube, a collection chamber, and a series of tubing that connects the drainage tube to the collection chamber. The tubing is often clear, allowing healthcare providers to observe the movement of fluid and air through the system.
Fluid oscillation refers to the movement of fluid back and forth in the tubing of the chest drainage system. While some oscillation is normal and can indicate that the system is functioning properly, excessive oscillation can be a sign of a problem. For example, if there is a blockage in the tubing or collection chamber, fluid may be unable to flow freely and can cause increased oscillation. Similarly, if the drainage tube is not properly inserted into the pleural space, air may be drawn into the tubing and cause oscillation.
If a healthcare provider observes excessive fluid oscillation in a chest drainage system, they may need to take steps to address the underlying issue. This may involve adjusting the placement of the drainage tube, clearing any blockages in the tubing or collection chamber, or replacing a malfunctioning component of the system.
Overall, while some fluid oscillation in the tubing of a chest drainage system can be normal, excessive oscillation can be a sign of a problem that requires attention from healthcare providers.
Golden rules for NURSES
24. The type of assessment that includes data related to a client’s biological, cultural, spiritual and social need is called Comprehensive Assessment.
The type of assessment that includes data related to a client's biological, cultural, spiritual, and social needs is indeed called a comprehensive assessment.
A comprehensive assessment is a holistic approach to assessing a client's health status that takes into account various aspects of their life, including their physical health, cultural background, spiritual beliefs, and social environment. By gathering information on these different factors, healthcare providers can gain a more complete understanding of the client's health status and develop a care plan that addresses all of their needs.
In a comprehensive assessment, healthcare providers may gather data through a variety of methods, including interviews, physical exams, laboratory tests, and observation of the client's behavior and interactions with others. They may also use standardized assessment tools to gather information on specific aspects of the client's health, such as their mental health status or their risk for falls.
Overall, a comprehensive assessment is an important tool for healthcare providers in understanding their clients' needs and developing an effective care plan that addresses all aspects of their health and well-being.
Golden rules for NURSES
25. The Vital Signs are: 1. Temperature, 2. Pulse, 3.Respiration, 4. Blood pressure, and 5. Pain.
The vital signs are indeed a set of important measurements that healthcare providers use to assess a client's overall health status. The five vital signs are:
Temperature: The measurement of the body's core temperature. Normal body temperature ranges from 97.7°F to 99.5°F (36.5°C to 37.5°C).
Pulse: The measurement of the heart rate, or the number of times the heart beats per minute. A normal pulse rate for adults is between 60 to 100 beats per minute.
Respiration: The measurement of the breathing rate, or the number of breaths taken per minute. A normal respiration rate for adults is between 12 to 20 breaths per minute.
Blood pressure: The measurement of the force of blood against the walls of the arteries as the heart pumps blood throughout the body. Blood pressure is expressed in two numbers, with the systolic pressure (the top number) indicating the pressure when the heart beats, and the diastolic pressure (the bottom number) indicating the pressure when the heart is at rest. A normal blood pressure reading for adults is typically around 120/80 mmHg.
Pain: The subjective experience of discomfort or distress. Pain is assessed using various scales, such as the numeric rating scale (NRS) or visual analog scale (VAS).
Overall, the vital signs are important indicators of a client's overall health status, and healthcare providers regularly assess these measurements to monitor changes in the client's condition and develop an effective care plan.
Golden rules for NURSES
26. Heat loss due to contact with circulating air movement is known as Convection.
Yes, that is correct. Convection is the transfer of heat from a surface to a fluid (e.g. air or water) that is moving. When air moves over a surface, it carries away heat, causing the surface to cool.
This is why we feel cooler when there is a breeze or wind blowing, even if the air temperature is the same.
Convection is an important factor to consider when designing heating and cooling systems, as well as in understanding the behavior of the atmosphere and oceans.
Golden rules for NURSES
27. The range of marking in glass/clinical thermometer is 95-110° F and 35-43.3°C.
Glass or clinical thermometers typically have a range of markings from 95-110°F (Fahrenheit) and 35-43.3°C (Celsius), which is the normal range of human body temperature.
The thermometer works by using a liquid, usually mercury, that expands or contracts as it is heated or cooled.
The length of the liquid column inside the thermometer changes depending on the temperature, and this is what is used to determine the temperature reading.
It is important to use the thermometer correctly and to read the markings accurately to get an accurate measurement of body temperature.
Golden rules for NURSES
28. Normal Rectal temperature is 99.6° F (37°C) (1°F ) higher than oral temperature)
The normal rectal temperature is generally considered to be about 1°F (0.6°C) higher than the normal oral temperature, which is typically around 98.6°F (37°C).
This is because the rectum is a more accurate indicator of core body temperature, as it is located closer to the internal organs and is not affected by external factors such as food or drink.
However, rectal temperature measurement is generally reserved for medical purposes and is not recommended for routine temperature checks at home.
Oral temperature measurement is a more convenient and less invasive method that can provide a good approximation of core body temperature.
Golden rules for NURSES
29. Rectal temperature is the most reliable
Rectal temperature is generally considered to be the most reliable method of measuring body temperature because it provides a more accurate reflection of core body temperature.
This is because the rectum is located in the central part of the body, close to the internal organs which generate heat, and is not affected by external factors such as food or drink.
However, rectal temperature measurement may not be suitable for all individuals, especially for those who are uncomfortable with the procedure, those who have certain medical conditions, or those who have undergone rectal surgery.
Oral temperature measurement is a convenient and non-invasive alternative that can provide a good approximation of core body temperature for most people.
Other methods of temperature measurement include axillary (underarm) measurement, ear measurement, and forehead measurement, which may be suitable for certain populations or situations.
Golden rules for NURSES
30. Relapsing fever: Fever episodes are separated by intervals of normal temperature for days or weeks
Relapsing fever is a type of fever caused by certain bacterial infections, such as Borrelia species.
The fever episodes in relapsing fever are characterized by sudden onset of high fever, chills, headache, muscle aches, and other flu-like symptoms.
These episodes typically last for several days to a week or more, and are then followed by a period of normal temperature, which can last for days or weeks.
During the periods of normal temperature, the patient may feel completely well and may not have any symptoms.
However, the fever episodes can recur, often with different symptoms or severity, leading to a relapsing pattern of illness.
Treatment for relapsing fever typically involves antibiotics, such as doxycycline or penicillin, and may require several courses of treatment to fully eradicate the bacteria.
Golden rules for NURSES
31. Rigor: Sudden rise in body temperature with shivering as seen in malaria.
Rigor is a medical term used to describe a sudden onset of fever with chills and shivering. In the context of malaria, rigor is a common symptom that occurs during the febrile (fever) episodes, which are a hallmark of the disease.
Malaria is a parasitic infection caused by Plasmodium species, which are transmitted to humans by the bite of infected mosquitoes.
The febrile episodes in malaria are typically cyclical, with sudden onset of high fever, rigor, and other flu-like symptoms such as headache, muscle aches, and fatigue.
The fever may last for several hours to a few days, and is then followed by a period of normal or subnormal temperature.
The cyclical nature of the fever episodes is a key diagnostic feature of malaria, and helps to distinguish it from other febrile illnesses.
Treatment for malaria typically involves antimalarial medications, such as chloroquine, artemisinin-based combination therapy (ACT), or other drugs depending on the species of Plasmodium involved and the location of the infection.
Golden rules for NURSES
32. Increased depth of breathing with normal respiratory rate is called Hyperpnea.
Hyperpnea is an increase in the depth and intensity of breathing, without an increase in the respiratory rate.
It is often seen during exercise or other physical activity, as the body needs more oxygen to meet the increased demand.
It can also occur in response to certain medical conditions, such as metabolic acidosis or congestive heart failure.
Golden rules for NURSES
33. Cheyne-Stokes Respiration is characterized by altered period of Tachypnea and Apnea.
Cheyne-Stokes respiration is a type of abnormal breathing pattern that is characterized by a cycle of alternating periods of tachypnea (rapid breathing) and apnea (temporary cessation of breathing).
The cycle typically lasts between 30 seconds to 2 minutes, and can be seen in patients with various medical conditions, such as heart failure, stroke, and traumatic brain injury.
It is caused by an abnormality in the respiratory centers in the brain, which affects the regulation of breathing.
Golden rules for NURSES
34. Pulse deficit refers to the difference between apical pulse and radial pulse.
Pulse deficit is a condition where there is a difference between the apical pulse (the heartbeat heard through a stethoscope over the apex of the heart) and the radial pulse (the pulse felt at the wrist).
It occurs when some of the heartbeats are not transmitted to the peripheral arteries, leading to a discrepancy between the apical and radial pulse rates.
Pulse deficit can be caused by various medical conditions, such as atrial fibrillation, premature ventricular contractions, and heart block. It is often an indication of an underlying heart problem and should be evaluated by a healthcare provider.
Golden rules for NURSES
35. A Blood Pressure Cuff that is too large will give a falsely low reading of BP.
No, that is not correct.
A blood pressure cuff that is too large will actually give falsely high readings of blood pressure.
This is because the cuff will not be able to adequately compress the artery, leading to an overestimation of the blood pressure.
Conversely, a cuff that is too small will give falsely low readings of blood pressure, as it will compress the artery too much, leading to an underestimation of the blood pressure.
It is important to use the appropriate size of blood pressure cuff for accurate readings of blood pressure.
Golden rules for NURSES
36. Beneficence: Doing good for clients and providing benefits balanced against risk.
Beneficence is one of the four main ethical principles in healthcare, which refers to the obligation of healthcare providers to do good and to promote the well-being of their clients.
This principle requires that healthcare providers act in the best interests of their clients and provide care that maximizes benefits and minimizes risks.
Beneficence also requires that healthcare providers make decisions that are based on the best available evidence and that they continually seek to improve the quality of care that they provide.
Balancing the benefits of treatment against the risks is an important aspect of beneficence, as healthcare providers must weigh the potential benefits of a particular treatment against the potential risks and side effects in order to make informed decisions about the best course of action for their clients.
Golden rules for NURSES
37. Isotonic solutions allow free movement of water across the membrane without changing concentration of solutes on either side. E.g. 0.9% NaCl.
An isotonic solution is a solution that has the same concentration of solutes as the fluid inside the cells of the body.
When an isotonic solution is administered, water moves freely across the cell membrane in both directions, without changing the concentration of solutes on either side of the membrane.
This is because the concentration of solutes in the isotonic solution is equal to the concentration of solutes inside the cells, so there is no gradient to drive the movement of water in one direction or the other.
One example of an isotonic solution is 0.9% NaCl (normal saline), which is commonly used for intravenous fluid administration to replace lost fluids and electrolytes in the body.
Golden rules for NURSES
38. Hypertonic solution: Fluids with solutes more concentrated than in cells, e.g. 5% dextrose.
No, that is not entirely correct.
A hypertonic solution is a solution that has a higher concentration of solutes than the fluid inside the cells of the body. When a hypertonic solution is administered, water moves out of the cells and into the extracellular fluid, causing the cells to shrink.
This is because the concentration of solutes in the hypertonic solution is greater than the concentration of solutes inside the cells, creating a gradient that drives the movement of water out of the cells.
An example of a hypertonic solution is 3% saline, which is used to treat hyponatremia (low sodium levels). 5% dextrose is actually an isotonic solution, because dextrose (a form of glucose) is rapidly metabolized by the body, leaving only water and a small amount of electrolytes in the solution. When 5% dextrose is administered, it initially acts as an isotonic solution, but once the dextrose is metabolized, the remaining fluid becomes hypotonic (lower concentration of solutes than inside the cells).
It is important to note that the effects of hypertonic and hypotonic solutions on the body depend on the concentration of the solutes in the solution, as well as the rate and volume of administration. Administration of hypertonic or hypotonic solutions must be carefully monitored to avoid adverse effects on the body.

1 note
·
View note
Text
THE IMPORTANCE OF NUTRITION SUPPORTS - FUELING YOUR BODY FOR OPTIMAL HEALTH

Good nutrition is essential for maintaining optimal health, providing your body with the necessary nutrients to function properly. Nutritional support encompasses guidance, knowledge, and resources that aid individuals in making informed dietary choices and achieving their wellness objectives, ultimately optimizing overall health.
What is Nutrition Support?
Nutrition support encompasses aiding individuals in making informed dietary choices through guidance, education, and assistance. It can be provided by nutritionists, dietitians, health coaches, or other trained professionals.
Nutriment support can take many forms, including one-on-one counseling, group sessions, online resources, and meal planning services. Its goal is to help individuals improve their diet and achieve their health and fitness goals.
Benefits of Nutriment Support
Personalized Guidance - Nutriment support provides personalized guidance that takes into account your individual needs, preferences, and health conditions. This personalized approach can help you achieve better results and maintain long-term success.
Education - nutriment support provides education on healthy eating habits, food choices, and the role of nutrients in the body. This knowledge can help you make informed decisions about your diet and improve your overall health.
Accountability - Nutriment support provides accountability, helping you stay on track with your health and fitness goals. This can be especially helpful for individuals who struggle with motivation or sticking to a healthy diet.
Improved Health Outcomes - Proper nutrition can have a significant impact on your overall health and wellbeing. Nutriment support can help you achieve better health outcomes, such as improved energy levels, reduced risk of chronic diseases, and better mental health.
Types of Nutriment Support
Nutrient support can be given orally, through enteral or parenteral methods, including fluids and medications, for those who can't consume orally. In this blog, we will discuss the various types of Nutriment support.
1.Enteral Nutriment:
Enteral Nutriment is the administration of nutrients, fluid, and medication through the gastrointestinal tract. Patients with a functional gastrointestinal tract and ability to tolerate oral or tube feeding are advised to receive this type of nutritional support.
2.Parenteral Nutriment:
A catheter delivers nutrients, fluids, and medication directly into the bloodstream via parenteral nutrition, for patients with severe gastrointestinal disorders or unavailable gastrointestinal tract.
3.Oral Supplementation:
Oral supplementation is the provision of nutrients and fluid through oral means to individuals who cannot meet their nutritional needs through normal dietary intake.
4.Total Parenteral Nutriment:
TPN is a nutrient solution given through a catheter when enteral nutrition is not possible, used for critical illness, severe GI disorders, or prolonged nutritional support.
5.Partial Parenteral Nutriment:
PPN, a type of parenteral nutrition, is administered via a peripheral venous catheter to patients who can tolerate some enteral nutrition, offering a portion of the required nutrients,
6.Elemental Nutriment:
Elemental Nutriment is a type of enteral Nutriment that provides nutrients in a pre-digested form. Patients with severe gastrointestinal disorders,
7.Modular Nutriment:
Modular Nutriment refers to the provision of individual nutrients, such as proteins, carbohydrates, and lipids, separately.
0 notes
Text
What Are the 3 Types of Intravenous Feeding?
Intravenous feeding is used when the digestive tract cannot adequately absorb nutrients, as occurs in severe malabsorption disorders. It is also used when the digestive tract must be temporarily kept free of food, as is needed during certain stages of ulcerative colitis. It may provide all of a person's nutritional requirements.
Parenteral nutrition requires a large intravenous tube. The tube (called a central venous catheter) must be inserted into a large vein, such as the subclavian vein, which is located under the collarbone. Parenteral nutrition may be used at home or in the hospital.
A central vein administers central parenteral nutrition, most often the superior vena cava, which is positioned behind your collarbone and connects directly to your heart. Because of the bigger central vein, a larger catheter may give higher concentrations of nourishment with more calories. As a result, CPN is utilized to give whole parenteral nourishment, which is administered by the limb or neck.
Total parenteral nutrition is total nourishment for the body that is given to patients intravenously. It is administered when a person is completely unable to obtain the necessary nutrients or is unable to eat. This may be necessary if certain disorders impede your digestive tract's capacity to process food and absorb nutrients.
Peripheral parenteral nutrition is administered via a smaller peripheral vein, which may be located in your neck or one of your limbs. PPN is used to administer temporary partial parenteral feeding by utilizing faster and simpler access to the peripheral vein. For a variety of reasons, this is the most often utilized intravenous feeding treatment.
0 notes
Text
Total Parenteral Nutrition (TPN) goes through a central line abd can provide the pt's total daily nutrition. PPN (Peripheral Parenteral Nutrition) goes through a peripheral IV and can't give the pt's total nutrition. You can't give TPN through a peripheral line. It must be through a central line.
1 note
·
View note
Text
Bleomycin In addition Tyrosine Kinase Inhibitors in Skin Growth Factor Receptor-Mutated Non-Small Cellular Lung Cancer
23, along with 222.2009 mg/kg, correspondingly). Even so, it's unlikely that any of the components ended up being recognized in fruiting body of Inonotus obliquus. To summarize, these 3 bioactive factors ended up frequently found in many organic mushrooms, and the outcomes could possibly be related to their beneficial effects.Use of umbilical irrelevant cord-blood (UCB) cellular material alternatively source of hematopoietic mobile or portable transplantation continues to be widely used generally regarding sufferers lacking an HLA-matched donor. UCB present several benefits more than navicular bone marrow or mobilized peripheral blood vessels through provide contributor, like speedy supply, shortage of chance for the donor, as well as diminished chance involving acute graft-versus-host disease. Even so, a substantial specialized medical issue is postponed engraftment that is straight related with all the quantity of hematopoietic come tissues within a cord-blood device. The actual detection involving prognostic components related to engraftment that can be effortlessly altered (electronic. grams., techniques for donor choice) and also the development of brand new strategies #Link# such as usage of multiple donors, intrabone injection involving UCB, ex lover vivo growth, and cotransplantation with accessory tissues have crucial value to be able to go around the issue of postponed engraftment right after UCB transplantation. Those strategies may increase the high quality and also option of UCB for hair transplant.Quick intestinal affliction develops once the remnant mass involving operating enterocytes subsequent enormous resections can't help expansion as well as maintain fluid-electrolyte equilibrium and requirements #Link# parenteral diet. Resection itself stimulates the intestine's purely natural power to adjust morphologically and functionally. The capacity to adjust is extremely linked to the top return price regarding enterocytes and is also mediated by a number of signals; these types of indicators are mediated mainly by enteral eating routine. First initiation of enteral serving, shut medical monitoring, and recurring assessment involving intestinal tract version are answer to preventing permanent intestinal tract failing. The size of the functional little digestive tract remnant is an essential varying affecting final result. The most important objective of colon rehab plans is to obtain earlier oral nutritional independence and keep regular growth as well as nutrition reputation and decreasing full parenteral diet #Link# associated comorbidities including chronic accelerating liver condition. Amazing improvement has been manufactured regarding survivability and quality of existence, especially in the wording regarding matched up multidisciplinary programs, nevertheless considerably function remains to be done.The analysis associated with 3 dimensional health care photographs is essential since the 3 dimensional image methods are already more and more commonly applied in medical applications. This particular document presents a manuscript division way of getting rid of physical objects of curiosity (001) throughout 3D ultrasound examination pictures.
0 notes
Text
Types of Feeding Tubes
Whether you're preparing to get a tube, to visit someone who you've heard has a tube or need to learn all the types before professional placements starts tomorrow, here's a quick, concise guide!
To ridiculously oversimplify things, lean these 3 now:
NG & PEG
NJ, J-tube
IV line.
Well done!
To be more comprehensive,
The types are:
NG
ND/NI/NJ
PEG/RIG/G-Tube
GJ/PEG-J
PEJ/J-Tube
Then, some intravenous lines can be used for specialised intravenous nutrition:
PICC
Hickman
It's not actually as complicated as it looks, I promise!
Basically:
Nose to stomach or intestine
Or
Hole into stomach or intestine
Or
Veins
Enteral feeding tubes are ones which go into the digestive tract either through the nose or directly through the skin.
Think ENTER as in gastroENTERology
Sometimes, people need parenteral nutrition. This means bypassing the enteral. Parenteral goes straight into veins. That's PAR-enteral, not parental hehe ;) It's often called TPN for short (Total Parenteral Nutrition), especially if the person is dependent on it. Occasionally the term HPN is used if the person uses it at home. The H is for "home"
Ok. Back to Enteral tubes:
Nasoenteric Tubes (any feeding tubes that go in by the nose):
NG = nasogastric. Goes through nose into stomach. Quite common.
ND = nasoduodenal. Through the nose and stomach into the 1st part of the small intestine called the duodenum. Rare because nasojejunal is typically seen as preferable. Some NJs technically end up in the duodenum but may still be simply referred to as an NJ. My NJ often lands right at the juncture where the duodenum becomes the jejunum.
NJ = Nasojejunal. Through the nose , via stomach and duodenum into the second part of the small intestine called the jejunum.
NI = Nasointestinal. Sometimes this word might be used to include NDs and NJs on a product packet or in a medical paper. Nasoenteric may be a term used too
In essence, NG or NJ
Percutaneous (through-the-skin) Enteral Feeding Tubes:
PEG: Percutaneous Endoscopic Gastrostomy tube. Common.
RIG = Radiologically Inserted Gastrostomy. Often these simply get called PEGs anyway.
G-tube = Another word for either PEG or RIG.
PEG-J = PEG with extension tube inside to the Jejunum.
GJ = Gastrojejunostomy. Basically a PEG-J but doesn't necessarily have "percutaneous endoscopic" insertion. It could be radiologically inserted.
J-Tube = Goes directly through a hole made in the skin into the jejunum.
PEJ = A J-tube placed using endoscopy. Like RIGs, sometimes people still call radiologically inserted jejunostomies "PEJ".
So, G, GJ or J
Any feeding or placement into the intestine may also be called "postpyloric", especially in medical academic journals. This means anywhere beyond the stomach. The pylorus is the far part of the stomach before intestine.
BONUS/SIDE NOTE: Most feeding tubes are "single lumen" (lumen = inside channel) but double, even triple lumen tubes exist. Extra channels might be for extra hydration, medicines or "venting" stuff OUT such as painful excess stomach air. Usually medicines and extra water are done through ordinary single lumen tubes and a separate tube is often used if venting is necessary.
Now the Parenteral ones:
These are intravenous lines rather than what's typically classified as a "feeding tube".
PICC = Peripherally Inserted Central Catheter. This is the more common of the parenteral line types and usually short term. It goes into the upper arm. Inside the body the line goes through a vein into the chest, to the heart. Peripheral = opposite of central, so further/outer. (Catheter = tube that goes inside a body channel eg vein, urethra etc)
Hickman Line: This delivers nutrition pretty much the same way but goes in by the chest.
There are other IV line types but usually for medication or hydration rather than feeding. PICCs and Hickmans are often are used for medications too.
Why use gastric enteral feeding (NG, PEG etc)?
Can't or won't eat enough to meet nutritional needs.
Why Postpyloric/intestinal feeding (NJ, GJ, J-tube etc)?
As above but feeding into stomach is ineffective, unhelpful, intolerable or perhaps dangerous.
Why Parenteral (PICC etc)
Last resort if nothing else gives the necessary nutrition and/or balance.
Or if the person is "nil by mouth" but must get the nutrition
Occasionally, people have more than one type.
For example: someone might depend on a line in the veins but spend part of the day on a Nasojejunal feeding as much as they can tolerate, and have an old PEG site used for a tube for venting.
Another example: PEG fed and using PICC every so often to make up for some kind of deficiency.
So you've got the gist of it!
If you have any questions or if I've made any mistakes, feel free to let me know as long as it's nicely! :-)
Now for a pronunciation guide for anyone who needs it:
Nasogastric = NAY-zo-GASS-trick
Duodenum = DYOO-oh-DEE-num. Some might say dyoo-ODD-en-um
Jejunum = JEJ-oo-num or jej-OO-num
Percutaneous = PER-cyu-TAY-nee-us
Endoscopic = END-oh-SCOPP-ic
Gastrostomy = ga-STROSS-tum-ee
Jejunostomy = JEJ-ooNOSS-tum-ee
Parenteral = parENT-er-al
Radiologically = RAY-dee-ol-LOJ-ic-al-ee
Postpyloric = POST-pie-LOR-ic
Intravenous = IN-tra--VEE-nus
Peripherally = per-IF-er-al-ly
#Feedingtubes#Nurseeducation#Typesoffeedingtubes#Feedingtubetypes#Nasogastric#NG#Nasojejunal#NJ#Gastrostomy#Peg#Pej#Gj#Jtube#Gastrojejunostomy#Jejunostomy#Picc#Hickman#tpn#Medicalstudent#Nursingstudent#Healthcare#Gastroenterology#Interventionalradiology#Education#Carers
6 notes
·
View notes
Link
0 notes
Text
A Nurse Wrote This Movie: A Medical Review of Knives Out
Whoa.
Honestly, all I can say, this movie was amazing.
I don’t think I’ve ever been treated to a movie that was both this complex and still this easy to understand. I wasn’t left wondering at the end, and despite the number of times my understanding of the central crime changed, it didn’t ever feel whiplash-y or like anything was played for shock value. It was a journey through the story and it was consistently enjoyable, all 130 minutes of it.

But please, seriously, go see it for yourself before reading this post, there will absolutely be spoilers and this is a movie you don’t want spoiled.
Before I really get into it, I want to tell you that the medicine (though, I suppose, particularly the nursing) in this movie was good. Really good. Much, much, much better than I expected. What I really, really appreciated was that the resolution of the case came from something that only a nurse would know. If i had to guess, not only was there a nurse consulting, but one was part of the central writing team.
There’s really only one scene to talk about, but it spans parts of the whole movie. Here’s my explanation/review of the evening meds scene and how it relates to real life and the rest of the movie. Apologies for the lack of relevant screenshots, once the movie comes out on streaming or DVD I will have more options. Also apologies in that I have only seen this once in theaters and I am working from memory.
PICCs:
One of the main characters, Marta, is a homecare nurse for the wealthy victim Harlan Thrombey. Early in the movie, we are given a scene where she is giving him two medications for a recent shoulder injury- ketorolac and morphine- before bed.
Harlan Thrombey has a PICC in his left arm that Marta uses to administer the medications. PICCs, or Peripherally Inserted Central Catheters, are medical devices that are designed to allow medical professionals to administer IV medications and draw blood without having to start an IV or stick someone with a needle. Once inserted, they can stay in for 6-12 months, and they’re really helpful for patients who either need IV fluids/medications at home (long-term IV antibiotic therapy, for example), or who require repeated doses of medications that could be damaging to the smaller veins that traditional “peripheral” IV catheters sit in (chemotherapy, total parenteral nutrition).
PICCs consist of one or more “ports” that are accessible from the outside (the blue nubs in the pic below, where the medication goes in), and a long, flexible tube that sits in a large, deep vein that ends near the heart.

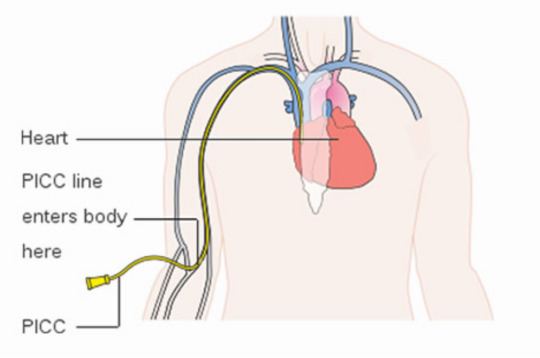
We don’t know a lot about Harlan’s medical history in the movie other than the injury to his shoulder that causes him to need the pain medication. A shoulder injury alone would not justify the insertion of a PICC, so we have to assume that either he had an existing serious health condition like cancer, or the shoulder injury was really an infection in one of the bones of his shoulder, which would justify a PICC on the basis of needing IV antibiotics multiple times per day. Since they seem to have thought of everything else, I would choose to go with that.
Medications:

The first medication’s generic name is ketorolac. Ketorolac is an NSAID, similar to ibuprofen, and works by blocking some of the chemicals that cause pain and inflammation in the tissue. It’s usually not given long-term, but for short term things like surgery or an injury it works pretty well and decreases the amount of narcotic pain medication needed. For someone over 65, the normal schedule for ketorolac would be 15mg IV every 6 hours. Marta would probably keep him pretty close to this schedule, because it’s his primary pain control beyond heat, ice, elevation, and possibly some form of physical therapy.
Morphine is an opioid. It works by blocking pain signals in the brain. It’s been around for a while, works pretty well and pretty quickly, but it’s not great for long term use either due to the fact that the body builds up a tolerance to it and it has the potential to be addicting.Since Marta seems to offer it to him instead of stating she’s going to give it to him, it looks like it was prescribed for “breakthrough” or as emergency pain relief if the ketorolac wasn’t doing enough, which is a pretty typical way to prescribe pain medication.
Now, you’ll notice that despite it reading “ketorolac” on the vial, the characters refer to the first medication by it���s brand name “Toradol” throughout the movie. This impressed me because in a medical setting, we colloquially refer to some medications by their generic name, while others we refer to by their brand names. There’s no particular rhyme or reason to the colloquial naming (though age of the drug plays in), and you kind of have to work in medicine to know which is which. We typically refer to Toradol by it’s brand name, while we refer to morphine by it’s generic. If you asked me for ketorolac or Astramorph (a brand name of IV morphine) it would just sound... weird. But its something fiction gets wrong all the time and it’s cool they got this right. For consistancy, I’m going to continue using the generic name for both medications throughout this post.
Medication Administration:
Marta goes about injecting the ketorolac first. This was yet another thing that added a little spark of nursing realism to the movie, because while not everything was shown, what was shown was done accurately. Here’s the steps to administering an IV medication through a PICC:
Open syringe package (draw needle is usually already attached)
Draw up air into syringe equal to the amount of volume of medication you want to draw
Clean top of vial with alcohol swab
Insert draw needle into vial and inject air
Flip vial/needle upside down and draw medication into syringe, recap draw needle (label syringe if giving multiple medications/doses)
Unclamp the PICC port you want to use and clean the port cap with an alcohol swab
Twist a prefilled saline syringe onto PICC port cap, and inject 5ml saline into the port
Twist draw needle off of syringe and discard into sharps container
Twist medication syringe onto PICC port cap
Inject medication
Twist off medication syringe and discard
Twist saline syringe back onto cap, inject the remaining 5ml of saline to flush the entire medication dose into the person’s vein
Untwist the saline syringe and reclamp the port
They reference the dose of ketorolac as being 100mg. As I said above, the normal dose of ketorolac is 15-30mg IV, depending on age. For Harlan, being 85, it’s hard to believe he wouldn’t have gotten 15mg IV every 6 hours max. I think the mix up was intentional, meant to signal to the audience that she was supposed to give the whole vial of ketorolac with each administration, but only a portion of the vial of morphine per administration. Ketorolac does come in single-dose vials, however in this movie all vials were clearly multi-dose vials (which you can tell because the ketorolac vial says “30mg/mL” on the 10mL vial, meaning there’s 300mg of ketorolac in that vial, which would be about 20x the normal dose).
Medication Errors:

Then she goes back to get the morphine, and realizes that she’s made a mistake. Instead of injecting the vial labelled “ketorolac” she’s administered the entire contents of the vial labelled “morphine”- 100mg, she thinks. That’s a LOT of morphine. Definitely enough for a fatal overdose in someone who’s normal dose is 3mg.
Now, med errors are HUGE FREAKING DEALS in the medical world, and Marta would have faced substantial civil and possibly criminal charges. Assuming she survived this without jail time, she would face an investigation by her visiting nurse agency (if she worked for one, which they establish she doesn’t) and/or the board of nursing in her state, which would seek to determine whether this was negligence that lead to the med error (in which she would probably be fired/have her license suspended/revoked), or a systemic problem (in which case she would be in the clear).
I think Marta actually has a pretty good case for this being a systemic issue rather than a negligence one. The vials look extremely similar, and even if she had done everything she was supposed to do, its plausible this could have happened despite her reasonable efforts to prevent it (she could have put it down last minute and picked up the other vial by accident, and had the label facing the wrong way as she was drawing up the medication). If nothing else, since the morphine vial was not specially identified as a narcotic, it would at least shift some of the blame to the pharmacy that filled the prescription.
In the moment, though, knowing what we know about her mom’s citizenship status, this would have been a terrifying situation for her.
Plus, there’s the overarching possibility that she just killed this very powerful person who she’s been caring for for a long time.
Opioid Overdose:

Opioids bind to certain receptors in the brain, decreasing pain signals. Unfortunately, they also decrease signals in the part of the brain that controls breathing. At small doses this isn’t generally a problem, but in overdose situations it can cause respiratory depression (the person breathing too slowly to meet their needs) or respiratory arrest (the person stops breathing on their own entirely), which can lead to death.
A drug called naloxone (brand name Narcan) can stop an overdose by sitting on all those same receptors that an opioid would without actually blocking any signals, which stops the respiratory depression from the opioid pretty quickly. As mentioned in the movie, most pharmacies dispense a naloxone kit along with opioid pain medication, and was the “antidote” Marta was searching for.
Now, in opioid overdose all is not lost if you don’t happen to have naloxone available. Since the cause of death from overdose is lack of breathing, Marta could have called 911 and provided rescue breaths until EMS showed up with naloxone. Even if EMS were 10 or 15 minutes out, he could have easily survived this. But that wouldn’t have made for nearly the murder mystery.
Ironically, this is exactly what happens in the laundromat scene, when it is revealed that the housekeeper Fran figured out what was happening and was attacked with the real morphine vial. When Marta finds her, she immediately looks in her eyes (a hallmark of opioid overdose is pinpoint pupils) and begins providing CPR.
In some areas, community-level CPR guidelines have simplified to “if you find someone not breathing, start CPR”. This is due to the realization that most lay rescuers have a hard time finding a pulse quickly enough to use it to determine whether to start CPR, leading to fatally wasted time in an emergency. The thinking is that it’s better to have people do unnecessary chest compressions than not do necessary ones.
But healthcare professionals are obviously still taught to differentiate between patients who need full CPR and patients who only need rescue breaths, so assuming Fran didn’t go from talking to cardiac arrest from an opioid overdose in less than a few seconds, I would have expected Marta to give rescue breaths until the ambulance arrived.
The Resolution:
Towards the end of the movie, we find that the vials were switched already, and in subconsciously recognizing the (real) difference in viscosity between ketorolac and morphine, Marta had actually, tragically, saved his life. This was probably the best use of a nursing concept I’ve ever seen in fiction, the entire central point of the plot hinging on nursing intuition.
Kudos, writers, kudos.
457 notes
·
View notes
Text
Headcanon: Post JL-endfight
As you probably know, Barry reverse time at the end of the JL movie. Not only did he do that but before that he kept running at very high speed to be able to charge up Victor. Something that must be pretty taxing, especially since he says that he can’t keep it up, meaning he can’t run at that speed much longer. It must have taken a lot of energy. Before he can charge Victor, he is shot by a Parademon and their weapon are energy weapons, so it’s more a burn than the wound from a projectile, you can even see his suit looking a bit melted (even looks like it’s attached to his skin.. ouch).

He’s also crashing when he gets shot and running in that speed, he must have cracked a few bones (just got the wind knocked out of you, my ass). Healing all those injuries enough to able him to run again, must have taken some energy.
Then he’s off to do his enormous feat of reversing time and saving the world from turning to dust before he charges Victor so he can fully integrate with the Mother Boxes. Since he said he couldn’t keep up the running he’d done before for much longer, which was considerably slower speed, this must have zapped a tremendous amount of energy. And we actually don’t see Barry again until after the others have killed Steppenwolf and sent his body back to Darkseid and when we see him then he’s visibly breathing heavily, something he normally doesn’t. This is very much a possible sign of his exhaustion.

(Sorry the focus was on Superman and Barry was in the blurry background.)
However next scene we see him in he looks fine.

This is where me headcanon come in. I see it as Barry still being hyped up about it all, he has run faster than the speed of light, after all. So once they’re in the plane and they’re safe, Barry will just collapse. No warning, no nothing. He’s walking, joking, being his normal Barry self and then he just falls to the floor. Initial examination shows that Barry is quite literally burnt out. They do what they can while still on the plane, but it’s not until they’re back in Gotham and the Batcave medbay that he can get some proper help. He’ll most likely be out for a day or two and will get nutrition either intravenously (peripheral parenteral nutrition) or through a nasogastric tube (that the tube they put through the nose and down your throat into your stomach). Once he wakes up it will most likely take another day or so before he can manage a full day out of bed.
But hey, he did save the world.
2 notes
·
View notes