#nodular
Text
i had a big huge between-eyebrow pimple last month that healed with hyperpigmentation and post inflam erythema so. tried to improve that by putting some vitamin C serum on it. well anyway the oil elicited another pimple and now its right next to the last one

#ngl it hurts really fucking bad lmao#i only get nodular/cystic blind acne i just know its gonna b ugly as hell because i can palpate it its Huge
11 notes
·
View notes
Text
.
#so mom’s having surgery tomorrow#(unless it’s cancelled for some unforeseen reason)#and i haven’t talked about it bc i’ve been trying to not think about it (as if that ever works)#she’s been super worried and scared and i’ve tried to be strong for her so as not to make her worry even more#it’s a routine surgery with very low risks#her thyroid has a nodular goiter that they’re gonna remove along with half of her thyroid#despite knowing it’s low risk and routine i am honestly super worried#mainly bc of ‘what if?’ and worst case scenarios bc my brain is dumb and bc she’s my mom and i’m great at worrying about the people i love#but also bc one of dad’s brothers died two months ago due to surgery that 9/10 goes fine#so it makes me worry even more than i maybe would have
2 notes
·
View notes
Text
I have been so randomly nauseous for like 2 weeks now??? Pretty much since I ended my period. Idk what it is. Stress? Idk? Maybe in the back of my subconscious with everything going on I'm actually more stressed out than I think?
Also not to mention, my boner has completely flagged and I hate it.
Was kind of nice having a sex drive again these last few months.
1 note
·
View note
Text
Nodular iron casting is considered very difficult, which can be improved by using some great tips.
0 notes
Link
Mụn bọc sưng đỏ là loại mụn cứng đầu khó điều trị. Cách trị mụn bọc tại nhà an toàn với Benzoyl Peroxide, Retinol, Axit Azelaic, Axit Salicylic, BHA, thuốc kháng sinh.
0 notes
Text
A rare case of bilateral plantar fibromatosis (Ledderhose’s disease): A case report by Amrutha Viswanath in Journal of Clinical and Medical Images, Case Reports
Abstract
Ledderhose’s disease, also known as plantar fibromatosis is a rare, benign hyperproliferative disorder affecting plantar fascia with unknown etiology. Clinical presentation of the disease varies according to the stage of the disease and individual characteristics. Diagnosis of the disease is usually based on clinical findings. Histopathological examination, Ultrasound or MRI can be used to rule out other conditions and for confirmation of the disease. Plantar fibromatosis can mimic the features of plantar fasciitis especially in early stages of the disease, hence it should be considered as a differential diagnosis in patients with pain and nodules in plantar aspect of foot. In this case report, we present a case of 24-year-old male with bilateral plantar fibromatosis, which was managed by surgical excision of the nodules due to unresponsive conservative management.
Keywords: Plantar fibromatosis; ledderhose’s disease; heel pain; nodular swelling; plantar fasciitis.
Introduction
Plantar fibromatosis or Ledderhose disease, is a rare benign pathology of the plantar aponeurosis, first described by Dr. George Ledderhose. It is characterised by disordered fibrous tissue proliferation and the subsequent formation of lump or nodules over the plantar aspect of the foot. The Office of Rare Diseases of the National Institutes of Health listed it as a rare disease with frequency about 1–1.75/100,000 [1]. Although etiology of plantar fibromatosis is unknown, it is associated with Dupuytren’s disease (palmar fibromatosis), Peyronie’s disease (penile fibromatosis) [2]. Increased risk of its occurrence is associated with alcoholism, chronic liver disease, diabetes mellitus, long term anticonvulsive treatment for epilepsy and genetic factors [3]. Males are more commonly affected than females. 25% of cases with plantar fibromatosis present with bilateral disease [4]. Diagnosis of Ledderhose’s disease is usually established clinically. Initially the nodule is asymptomatic and it becomes symptomatic as it enlarges in size. Direct pressure on the nodule while walking barefoot, standing for long periods of time and use of restrictive shoes may exacerbate pain and walking disability. Over time, multiple nodules may develop and can cause exacerbation of symptoms, contractures and deformities [5]. Given the benign nature, initial phase of the disease can be managed conservatively and if symptoms persist, definitive management of surgical excision of nodule gives complete relief of symptoms. The nodular swellings affecting the plantar fascia is of greater significance in population with poor socioeconomic status as people prefer to walk barefoot in developing countries.
The similarities of plantar fibromatosis to Dupuytren's disease affecting palmar fascia support the theory that, two conditions are different expressions of the same disorder [6]. Even though much has been discussed about Dupuytren's contracture in the literature; only very few literatures are available regarding plantar fibromatosis. In this case report, we present a case of 24-year-old male with bilateral plantar fibromatosis and aims to discuss the clinical presentation and various management options in plantar fibromatosis.
Case Report
A 24-year-old male presented to our department with dull aching type of pain over the plantar aspect of both feet of 1-year duration. Pain prevented the patient from weight-bearing for long time and walking for small distances. There was no significant familial history of the disease or history of any associated trauma. No associated medical history in the patient. Patient gives history of treatment in another hospital as bilateral plantar fasciitis. Conservative management was given there in the form of analgesics, anti-inflammatory drugs, advice to use footwear with soft insole and gives a history of 3 steroid injections administered 4-6 weeks apart. With persistence of symptoms patient came to our department. On physical examination small, well circumscribed, palpable, firm, nodular, single swelling was present over the medial plantar aspect of his both feet. The swellings measured about 2 x 1.5 cm on the right foot and 1 x 1 cm on the left foot. The skin over the swellings appeared normal and there were no neurovascular deficits or deformities. Ankle joint and foot range of movements were within normal range. On further examination, we found a similar swelling of size 0.5 x 0.5 cm on the palmar aspect of right hand with no restriction of movements and clinical signs. FNAC report showed mild to moderately cellular oval to plumb spindle shaped fibroblastic cells with elongated nuclei arranged in clusters and dispersed pattern associated with myxoid matrix. Cytology findings were suggestive of benign fibroblastic lesion. A provisional diagnosis of bilateral plantar fibromatosis was made, based on clinical and cytological findings. Since conservative management was tried earlier and there was persistence of symptoms and limitation in function surgical excision of the nodules was planned. Surgery was performed under spinal anesthesia. Nodules on both sides were palpated and skin over it was marked for surgical incision. The dissection of skin and soft tissue exposed the nodules on both sides, which were greyish white in colour, firm in consistency and attached to plantar fascia (Figure 3).
Figure 1: Nodular swelling on right foot (dot circle).
Figure 2: Dot circle indicating the nodular swelling on right palm.
Figure 3: Exposed nodule ( Right foot ) intraoperative image.
Figure 4: Excised nodule from right foot (greyish white, measuring 1x0.8x0.2 cm).
Figure 5: Excised nodule from left foot (greyish white to greyish brown, measuring 1.7x1.5x0.4 cm).
Excision of the nodules were done in both feet and primary wound closure was done. The patient was advised for non-weight bearing for 2 weeks and use of soft insole footwear thereafter for 2 weeks. Postoperative period was uneventful and sutures were removed after 2 weeks of surgery.
Figure 6: Postoperative wound before suture removal.
The histopathological examination of the excised nodules revealed spindle-shaped cells with abundant collagen in a fibrous stroma background and features were consistent with the diagnosis of bilateral plantar fibromatosis. On follow up of 6 months, patient reported complete relief of symptoms and improvement in function.
Figure 7: Photomicrograph of HPE slide showing nodular lesion composed of spindle shaped cells in a fibrous stroma background. (H&E staining, x40).
Figure 8: Photomicrograph of HPE slide showing spindle shaped cells with abundant collagen in fibrous stroma(H & E staining , x100).
Discussion
Ledderhose’s disease (Plantar fibromatosis) is a fibrous hyperproliferative pathology affecting the plantar fascia characterised by formation of nodules [7, 8]. The diagnosis of Ledderhose’s disease is usually established clinically and rarely require further investigations for confirmation [9]. Histopathological analysis and diagnostic imaging helps to differentiate between other lesions that can present with similar symptoms such as plantar fasciitis ( The most common disorder of plantar fascia), lipoma , ganglion cyst, leiomyoma, epithelioid sarcoma, rhabdomyosarcoma and liposarcoma [10, 11]. According to the clinical and pathological studies, plantar fibromatosis can be classified into three stages. The first (proliferative) stage of the disease is characterised by cellular proliferation and increased fibroblastic activity. The second stage of the disease which is the active phase is characterised by formation of nodules. It is followed by the third (residual) stage where collagen maturation and tissue contractures occur [11, 12]. Therefore the normal plantar fascia is replaced progressively by abnormal collagen fibres and can present at any stage of the disease with pain, nodule, walking difficulty, contractures or deformities of toes and the treatment is planned accordingly.
Patients presenting in the early stage of the disease with no or mild pain can be conservatively managed with padded shoes with soft insoles or custom offloading to redistribute the weight from the nodules, analgesics, anti-inflammatory drugs and intralesional steroid injections[10,13]. If left untreated, nodules may gradually increase in size and number which in rare cases may result in deformities of the toes due to contractures in later stages. In cases with persistence of symptoms after conservative management, lesions which are progressive, severe limitation of function and in advanced stages of the disease surgical management is considered as the last resort of treatment [14, 15].
The nodular swellings affecting the plantar fascia is of greater significance in developing countries with poor socioeconomic status as people prefer to walk barefoot. For the same reason, early surgical management is indicated for symptomatic cases in the developing countries.
Conclusion
The diagnosis of Ledderhose’s disease can be done clinically alone. Diagnostic imaging such as Ultrasound or MRI and histopathological examination may be used, to exclude other conditions and to rule out malignancies [16]. The treatment of the disorder is planned accordingly. Even though plantar fasciitis is the commonest disorder affecting plantar fascia, plantar fibromatosis should be considered as a differential diagnosis in patients presenting with pain and nodules in plantar aspect of foot as it can mimic the features of plantar fasciitis. The recommended treatment approach is to start with conservative management in early stages of the disease and perform surgical excision in unresponsive cases and advanced stages. But the best treatment plan is to establish a personalised approach depending on the individual characteristics, type of symptoms, stage of the disease and recurrence.
Authors Disclosures:
Funding / Grants: Nil.
In this study, there was no competing interests or financial benefits to the authors.
Details of any previous presentation of the research, manuscript, or abstract in any form: Not presented anywhere.
Acknowledgement:
Authors declare no conflict of interest.
In this case report, there is no financial benefits to the authors.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Plantar fibromatosis#ledderhose’s disease#heel pain#nodular swelling#plantar fasciitis#characterised#FNAC#Cytology#hyperproliferative#pathology#Amrutha Viswanath#jcmicr
0 notes
Text
Pig Iron Manufacturers in India of Nodular Grade-SG03 | Vedanta Metabazaar
Vedanta Metalbazaar offers nodular-grade SG03 pig iron. It is one of the leading manufacturers of pig iron in India. Get more details and order!
#nodular grade pig iron#pig iron manufacturer in India#pig iron producer#iron and steel company#pig iron price#iron and steel industry#vedanta metalbazaar
0 notes
Text
Genuinely I think in the vast majority of cases having an eight step skincare routine is disordered. Like straight up skin-centric dysmorphia.
1 note
·
View note
Text

[OUTGOING REQUEST] COMMUNICATION MANIFEST
SOURCE NODE TRACE: FP ROOT, SRS COMM09, NSH COMM02
[ sorry for the... delay. ]
[ ongoing interfere... communications system. ]
[ im scared. ]
[ help ]
MESSAGE CONTENTS:
---
[[Re: [LIVE BROADCAST] EQUIPMENT MANIFEST]]
[[ WIDE SWEEP DIAGNOSTIC RESULTS ]] ]
Water: 55%
Hydrocarbons: 130%
Sulfur: 1640%
Silicon: 410%
Phosphates: 25%
Other: 1800%
---
TRACE FOREIGN ENTITIES DETECTED. INPSECTORS NOTIFIED.
SEVERE CHEMICAL IMBALANCE. REQUEST CONDUIT PURGATION IMMEDIATELY.
EXTERIOR BREACH DETECTED NEAR PRECIPICE. STAGE 3 HULL BREACH. PLEASE MIGRATE ENERGY INTO REPAIR.
---
[ [!! WARNING !!] Biomechanical degradation detected in CONDUITS: 02, 03, 06, 08, 12, 17, 18, 25, 26, 27.] ]
[!! WARNING !!] Water leakage detected in CONDUITS: 06, 12, 26.]
[-RAPID OXIDATION EVENT IN CONDUIT_03, RL_SYS_ARRAYS, RANDOM_CACHE_SYS-]
[-POTENTIAL HYDROGEN LEVELS LOW IN CONDUIT_03, CONDUIT_12, CONDUIT_18-]
[ Foreign contaminants detected within the west hull. Inspectors notified to conduct biopsy of contaminant. ]
[ Mass clogging detected. Emergency fluid administered; dissolution fluid may erode tubular plating. Temperature should be heavily monitored to prevent warping. ]
[ Dissolution fluid is a preventative regulation only. NEUTRALIZING SOLUTION IS REQUIRED. ]
[ Rarefraction activity will be immediately scheduled for affected nodes. However, quantities of foreign run-off may result in dangerous pressure changes. ]
[ Power saving should be reconsidered to allow restoration of nodes. Heavy processing required. ]
[ Rapid nodular restoration is a preventative regulation only. EMERGENCY MAINTENANCE IS REQUIRED. ]
#rain world#rainworld#looks to the moon#rainworld au#rainworld spoilers#rw downpour#rain world fanart#rw iterator#rw lttm#rw au#rw art#rw five pebbles#five pebbles#rainworld downpour#rain world downpour#my art#rainworld roleswap#rain world looks to the moon#rw seven red suns#seven red suns
148 notes
·
View notes
Text
DOXXING MYSELF WITH ROCKS
Okay so I took this photo while I was biking:

And I thought, "I wonder what kind of rock I'm looking at?" so I started poking around. I learned a lot! Apparently rock formations are tracked kind of the same way lakes and such are. Geologists have charts with the shapes of large "pockets" (misleading, they are massive) of various types of minerals
Wikipedia led me to specific formation names and I tracked down the geographic area I was in and looked at the rock layers.
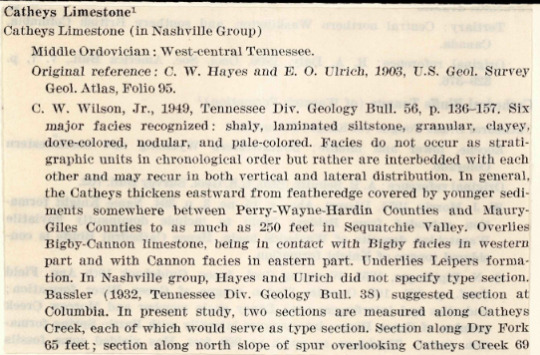
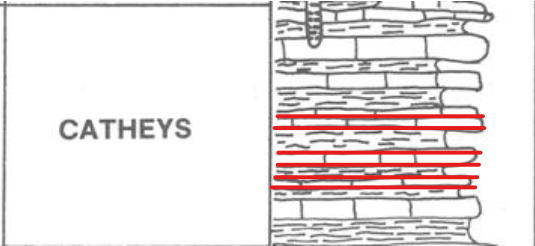
This is a very precise description of the location. I then looked up the Cathey rock layer. Check the description:
"A complex mixture of shaley limestone units. Typically it is thin bedded, blue gray nodular limestone, interbedded with thin partings of shale and siltstone. Weathers to thin silty soil usually 3 to 4 feet thick. Outcrops extensively in Central Basin."
Here is a charting of the layers in the Catheys Formation
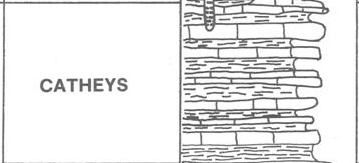
I think this is what I'm lookin at.

Isn't this so cool? I had no idea they just had like.
Maps that show you where rocks are in this level of detail
220 notes
·
View notes
Text
will wood fans will get mad at you if your favorite song is i/me/myself and not some 23 second demo from 2015 with the crunchiest damn audio you've ever heard called ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children
111 notes
·
View notes
Text









Punctelia reddenda
This gorgeous foliose lichen grows in rosettes up to 6 cm in diameter. The upper surface is gray-green to yellow-green with white, punctiform (point or dot like) pseudocyphella which turn into soralia which produce granular or nodular soredia. The lower surface is black toward the center and lightens to brown near the rounded margins of the overlapping lobes. P. reddenda grows on mossy tree trunks and rock in Africa, Macaronesia, North and South America, and Europe.
images: source | source
info: source | source | source
#lichen#lichens#lichenology#lichenologist#lichenized fungus#fungus#fungi#mycology#symbosis#symbiotic organisms#green algae#biology#ecology#botany#bryology#systematics#taxonomy#life science#environmental science#natural science#nature#the natural world#beautiful nature#weird nature#trypo#trypophobia#Punctelia reddenda#Punctelia#I'm lichen it#lichen a day
241 notes
·
View notes
Note
Is autism and bowel/digestive problems a popular thing? Does anyone know what causes it or what can help? I have been to doctors and hospitals so many times over the years and never get any results or help.
Hi there,
Unfortunately people with ASD have some difficulty with the gastrointestinal tract. I’ll leave some excerpts from articles below. Warning: they are very long:
Of the many medical comorbidities associated with ASD, GI distress has gained significant attention because of its reported prevalence and association with symptom severity. In fact, out of the children that Leo Kanner described in his landmark article defining “infantile autism” are described as having eating/feeding or dietary problems, supporting an early association of ASD with GI issues. Of the GI problems reported in subsets of autistic individuals, the most common are chronic constipation, diarrhea, and abdominal pain. Gastroesophageal reflux, bloody stools, vomiting, and gaseousness are also elevated in some autistic individuals, as are signs of GI inflammation, such as lymphoid nodular hyperplasia, complement activation, and elevated pro-inflammatory cytokines, and intestinal pathologies, such as enterocolitis, gastritis, and esophagitis. Increased intestinal permeability is linked to autism and hypothesized to have detrimental effects not only on intestinal barrier integrity but also on the systemic metabolome, with potential for translocation of intestinal metabolites or bacteria and consequent immune activation. Furthermore, food allergies, altered dietary nutrient intake, and metabolic disruptions have been associated with ASD.10–12 Autistic individuals with comorbid GI abnormalities exhibit altered carbohydrate digestion. Taken together, the variety of GI conditions, dietary issues, and enteric immune abnormalities reported in ASD individuals suggests that GI dysfunction can contribute to the manifestation of core symptoms of autism.
Characterized by difficulties with socializing, and often accompanied by repetitive behaviors, this neurodevelopmental disorder harbors many mysteries.
Despite its prevalence and a glut of research, the causes behind ASD are still not fully understood.
Although ASD primarily impacts the brain, over recent years, links with other systems have become clear — in particular, gastrointestinal (GI) issues seem to occur more often in individuals with ASD than in the rest of the population.
In one study, compared with typically developing (TD) children, those with ASD were six to eight times more likely to report GI symptoms such as bloating, constipation, and diarrhea.
Other studies have shown that children with ASD who experience GI problems are more likely to have more severe symptoms of ASD. Also, treating the GI symptoms can sometimes relieve the behavioral and social symptoms of ASD.
Interestingly, behavioral issues are found alongside other conditions that impact the gut. For instance, people with celiac disease are more likely to have autism-like traits and other psychological symptoms. The gut and behavior seem tied together in some way.
According to many researchers, the GI issues that come with ASD might be due to two factors: firstly, inappropriate immune activation causing inflammation of the tract; and, secondly, differences in the types of gut bacteria that are present.
However, the picture is still incredibly murky, and studies produce differing results, finding different types of inflammation and various changes in gut bacteria.
Children with autism experience more gastrointestinal symptoms
Gastrointestinal concerns are frequently reported by parents of children with autism spectrum disorder (ASD). Researchers from the UC Davis MIND Institute evaluated the presence of GI symptoms in preschool-aged children with and without autism.
The study included 255 (184 males/71 females) children with ASD between two and 3-5 years of age and 129 (75 males/54 females) typically developing children in the same age group. Pediatricians specializing in autism interviewed caregivers during the children’s medical evaluation. They asked the parents how often their children experienced GI symptoms such as difficulty swallowing, abdominal pain, bloating, diarrhea, constipation, painful stooling, vomiting, difficulty swallowing, blood in stool and blood in vomit.
The researchers grouped children in two categories: those who experienced one or more GI symptom and those who never or rarely had GI symptoms in the last three months. They compared the children in the two groups on measures of developmental, behavioral and adaptive functioning.
The study found that preschool-aged children with ASD were 2-7 times more likely to experience GI symptoms than their typically developing peers. In fact, almost 50% of children with ASD reported frequent GI symptoms - compared to 18% of children with typical development. Around 30% of the children with ASD experienced multiple GI symptoms.
I hope these sources can help. I have GI issues too and have to resort to stool softener
…
Anyway, thank you for the inbox. I hope you have a wonderful day/night. ♥️
66 notes
·
View notes
Text
Nodular Iron Casting is widely used in a wide range of applications due to its strength and durability. Explore the step-by-step guide on how manufacturers make Nodular Iron Casting. Learn about every steps in details.
0 notes
Link
Mụn bọc ở cằm (Nodular Acne) là mụn trứng cá lớn dạng viêm, sưng đỏ. Mụn bọc ở cằm do rối lọan nội tiết tố, kích thích hoạt động bã nhờn, gây bít tắc lỗ chân lông, gây mụn.
0 notes
Text
OH HEY IF YOU HAVE CYSTIC/NODULAR ACNE get you some Mupirocin, it’s an antibiotic ointment that has done a really impressive job on mine. Damn things used to last for weeks or months, but this stuff takes care of them in a few days.
11 notes
·
View notes