#I am being infected with baby fever and I need this virus to go away I am Not Responsible Enough for another human being!!!
Text
Eddie and you have a little girl and she is the light of his life. She is super empathetic and sweet, but like all little kids she is blunt and unfiltered. You have been teaching her colors and she has most down. Eddie is trying to show Steve how well she is doing, how smart she is. She gets Eddie's shirt right (black) and the couch (blue). She then starts pointing at things and calling them out herself (the wall, green. Her shirt, pink). She points to Steve's temple and announces "Grey".
Eddie wheezes with laughter and tears spill out of his eyes as Steve is aghast.
#Something about this is hilarious to me and listen my friend just had a baby and now I want a kid...I dont but#I am being infected with baby fever and I need this virus to go away I am Not Responsible Enough for another human being!!!#Be aware there may be kids being involved in fics...probably for Steve...maybe...maybe an alpha steve- NO I SHANT SAY MORE#Eddie Munson#Stranger Things#Eddie Munson x you#Eddie Munson x reader#Jade is Talking
135 notes
·
View notes
Note
You should write something where maybe one of the other boys gets sick and y/n is taking care of them maybe even letting them lay against her and Harry gets super jealous and y/n has to go and talk to him and he’s just acting like a straight child all like “Get away f’me.” and pouty ahahha.
A/N: I'm finally back!!! I had to leave for a while to focus on ending the year strong but I am now back and hoping to post every-other day until I am done with the requests in my inbox!
~~~~~
1.9k
Tw: sickness, slight angst, fluff at the end
~~~~~~~~~~~~~~~~~
Now anyone in or out of health care knows this one little fact. Men are absolute babies when it comes to being sick. By now I was used to it. The “y/n my stomach hurts, i'm going to die!!” and the *sniffle* *cough* “are you okay?” “oh my god, yes i’m fine why would you even say that!” To be honest most of the time I ignore fifty percent of their complaining, treat their symptoms and by the next morning they are fine. But every once in a while they aren't being dramatic.
“Mhhh” Even from the opposite side of the bus I could hear him groaning in his sleep.
“Niall?” no response. It couldn't be that he was sleeping and making those noises at the same time.
“Uhhh '' Alright so maybe he was. We had been driving for about ten hours when Niall fell to the bug. I had been doing my best to keep it from the boys but somehow despite my best efforts, it made it through. He was the first so far, but probably not the last. If one boy gets sick, the others always get it. The bug had been moving quickly through the crew staff, hitting at least three people a week. My once solitary and quiet med bus was now full to the brim with groaning patients. The other unfortunate side effect of this; I couldn't no longer sleep in the same bed as my boyfriend. Well, at least not until this infection is out of the way and I'm not scared of him getting sick.
I walked out of the back rooms to see Niall passed out on the med bay couch, face down and groaning louder than a truck horn in his sleep. I had seen Niall sick before. Hell I've had to wipe vomit off of his face before, but this shit was brutal. And I won't lie, the toll of not being able to escape it at all for the past few weeks has been getting to me. My sleep is constantly interrupted by alarms on my phone going off to remind me to check everyone on the bus, refill their fluids, check their temperatures, and administer medication if needed. I haven't been able to talk to my boyfriend in weeks for longer than five minutes. At this point I was almost praying to get the virus just to have a week off. Except maybe without the fever, and then sore throat, and the nausea. So maybe not.
“Ni” I shook his shoulder lightly to attempt to wake him up. Nothing.
“Niall” Again, nothing. I could only be grateful that right now he was the only one sick. Finally with a big snort and a flip onto his back his cloudy eyes opened.
“Hey bud, how ya feeling?” He groaned once more and shut his cloudy eyes.
“Nope. None of that. I know you're going to hate me but it's time for more meds.” Nothing but another groan.
An hour or two later we finally found ourselves at a hotel, a wayside stop for a few days until everyones feeling better and the boys are able to perform. The second we got off the bus- me with several bags of medical supplies along with my actual suitcase, and Niall with a single backpack underneath the blanket he had wrapped around himself like a cloak- Harry came up to me with a frown on his face.
“Long time no see love bug” He moved in to kiss me but I gently placed a hand on his chest and pushed him back a step.
“I will not get you sick. Remember how bad it was last time? No way. I love you, but no.” He pouted like a child being told no and hung his head.
“Baby, I promise the second Ni is better we’ll be spending all day together, we just have to be careful, that's all” while his head was still facing down I thread my fingers through his hair and gave his scalp a little massage. After I was done speaking I gave him a light kiss on his head.
“Now come on, let's get inside so we can all get our keys and go to bed, Okay?” Still pouting, he nodded at me and continued in without saying another word.
~~~~
Once we were all inside Paul was standing at the desk waiting with keycards in his hands to give us our rooms. He started with the crew and then once they had all filed off to their rooms he gave the other boys their room keys. Lastly, he handed one to me. The last one.
“Sorry y/n they’d only give me one key for the both of you” Harry standing with the other boys around me walked forward.
“Don't know what you mean Paul, I’ve got the other key right here?” I signed and turned to face him.
“Haz-”
“Oh. you'll be sharing a room with Niall then, won't you.”
“Yes. I need to keep an eye on him tonight make sure his fever doesn't come back-”
“Whatever” I took a step back, feeling the lash of his tone on me. Did he really think this was fun for me? This is my job, the whole reason I get to be here touring with him in the first place, it doesn't just suddenly disappear whenever he wants it to. I took a deep breath. It's fine. He's just frustrated, just like I am, that's all. This cant be easy for him either.
“We might not be able to share a room tonight but I do hope you’ll still come say goodnight before you go to sleep?” I tried to reach out a hand and was coldy rejected.
“Maybe. I wouldn't want to disturb the both of you.” I made a surprised scoff and looked over at Niall who was standing behind me with an equally surprised look on his face. Before I would even respond, he was off to the elevators without aso much as a look behind him.
~~~~
After a few hours of television watching and unpacking in our hotel room it was time for Niall's least favorite activity. Taking his meds.
“Niall?” I found him again face down on one of the beds in the room, not asleep this time, just hiding from the light.
“No. I won't do it this time.”
“Hate to tell you but I have dealt with non-compliant patients before and usually it ends up worse for them than it does for me.” He dramatically flipped over and layed starfish on the bed for a moment before slowly pulling himself up to a sitting position.
Twenty minutes after he had taken his meds, like always with Niall; he began to groan my name while I was attempting to take a shower for a moment of peace. Like any good physician I ignored the first two and after not hearing a third, went out to check on him.
“Ni? Are you okay?” He was in a fetal position with his eyes closed taking deep breaths.
“Puke. definitely going to puke.” I cringed a little and grabbed one of the anti-nausea meds from my bag.
“Here. Put it under your tongue, it should work pretty quick.” He did as I said and continued groaning. In a moment of pity I grabbed my book and hopped onto the bed beside him.
“What-”
“If you're going to be miserable it's the least I can do to not make you be alone” I moved up on the bed and patted my lap with one hand.
“Come on, you big baby” He placed his head on my lap and I opened my book, beginning to read from the page I had dogeared. Not twenty minutes later Niall was fast asleep and I left him laying with his head on my lap as I read my book in peaceful silence. Peaceful that is until a certain someone knocked on the door.
“You can come in Harry, it's unlocked.” He stepped in and right away turned what looked like a sorrowful- even remorseful- look, into one of pure fire.
“Really, y/n”
“Haz- '' I didn't get the chance to say another word before he was out of the room and walking quickly down the hall. I carefully untangled myself from Niall- who by some grace of god was still asleep- and chased Harry down the hall.
“Harry!” I grabbed his arm and he pulled away.
“Get away f’me”
He continued walking down the hall, and I almost let him until I snapped.
“Harry Edward Styles don't you dare act like a child and walk away from me right now!” He stopped in his tracks at the tone in my voice but didn't turn around.
“Do you think that this is fun for me? Not being able to see you at all for weeks, having to stay away from everyone and anyone just in case I could get them sick. Having to constantly be on call and working for days at a time?”
Now he turned around.
“While you have been out there, acting like a pouting child with the rest of your friends I have been trying to make poor Niall feel even the slightest bit better!” I paused for a breath. “So don't you dare try and make me feel bad about comforting our friend. Dont. you. Dare!”
I realized then that a few tears of exhaustion and frustration had slipped down my cheeks. I swiped them off and waited in buzzing quiet as he walked toward me. His head was facing the ground when he finally got over to me.
“Im stupid.” he finally said in a small voice. He reached out and put both his hands on my arms, still respecting the distance I wished to maintain, but allowing some sort of comforting touch for the both of us.
“Yeah, you have been.”
“Does it help if I say that I'm sorry and I never should have acted like a child because you were just helping Niall?”
“Of course it helps Harry”
“Are you still mad at me?”
“I mean, a little. You acted like a douche.” he let out a disappointed huff, but still nodded in agreement.
“Are you mad enough that we should talk about it more before we both go to bed?” I thought for a minute but the second I looked up at his cinnamon roll curls I knew the answer. I let out a dramatic sigh and opened my arms.
“No. come here” after a hug that the both of us had been waiting for over weeks, he released me and gave me a short kiss on the top of my head.
“Goodnight love.”
“Goodnight.”
So finally I made it back to my room, turned out the lights and settled into my own bed. It was colder without him in it.
~~~~~
“y/n/n” someone whispered in my ear and I jumped awake. Harry stood over me pale and looking half dead.
“Oh no. oh god no. you've got it don't you.” he did a slight nod before throwing off his shoes and jumping into the bed with me. One part of my brain went warm, comfy. The other was screaming expletives at him and myself for not being more careful. He nestled up next to me and placed his head in the crook of my shoulder.
“Well, at least now you get to hang out with me
#harry styles fluff#harry styles#harry styles imagines#harry styles one direction#harry styles one shot#one direction#oneshot#onedirectiontour#anxiety comfort#blurb#sickfic
125 notes
·
View notes
Text
Snowy Sniffles
💡SPENCER REID X DEREK MORGAN💡
read on ao3
Summary: Derek gets the flu when he and Spencer are snowed in on a case in Colorado.
Word Count: 2k
Category: fluff, slight angst
Content Warnings: swearing, sickness, case details
A/N: enjoy my otp being cute and cuddly for my first day of 12 days of moreid :)
The snowy mountains of Colorado. A serial killer as cold as the air was out there, and It was the job of the BAU to catch him.
The team boarded their plane like normal, occasionally Derek coughed and cleared his throat. Not enough to realize what was happening, but enough to get a “You okay?” from JJ.
There weren’t many hiccups with local police, except for them withholding information about the victims. Derek and Spencer were sent to profile the dump site, JJ and Emily to interview victims' families, while Rossi and Hotch set up at the station.
The dump site was in a clearing next to a mountain frequently used for sledding. A visiting family from Texas was recommended the mountain by a friend and since they weren’t familiar with the area, the mom got lost and they came across the body. Thankfully the kids weren’t there to see it.
Spencer and Derek walked out of the black SUV and ducked under the police tape in their fleece jackets and large boots.
“The victim was Hannah Gentry. She was a fourteen year old girl who ran away from her abusive father. No sign of sexual assault, but there were signs of restrains on her thighs and around her stomach.” Spencer walked around the area the body had previously been found, searching for anything left behind by the unsub.
“Maybe he thought he was saving these girls. How old were each of the victims?” Derek said, pulling tissues from jacket pocket.
“Ages ranged from 13 to 19. All had someone abusive close to them. You sure you’re okay?”
Before Derek could reply he was coughing and gagging into the torn kleenex in his hand.
“I’ll be fine,” The stuffiness in his nose was apparent in his voice now. “Let’s go back to the station. I’m sure Rossi and Hotch are at the M.E. now.”
The two walked back to the car and headed towards the police station. On the way it started snowing and Spencer said something about growing up in Vegas without snow, and how in Virginia they never really saw the snow fall, they just woke up to it on the ground and in the streets.
Between the snowfall rapidly increasing, the windshield wipers not doing anything to help, and Derek driving in an unfamiliar area, he began having a coughing fit and swerved off the road.
They didn’t get hurt in the accident, just a large rush of adrenaline, but the car wasn’t in the best shape. The engine made a sound that contorted Spencer’s face.
“We should probably check that.”
Derek tried to push his door open but he had driven into a ditch and snow was piled up tp his window. He rolled it down and shoveled some of the snow with his gloved hands. He got the door all the way open with a little wrestling of the handle. The boot of the car was opened and steam was rising from it. Spencer had crawled across the center console and got out from Derek’s side.
“Do you think we could get an officer to pick us up?” Derek sniffled.
“I think the snow is coming down too hard now.” Spencer’s black coat was powdered with snow that he didn’t bother to shake off, knowing it would be back there in an instant.
“I’ll call Hotch.” Derek fished his phone out of his pocket.
“You fell in a ditch? Morgan, this is a very time sensitive case. This guy kills every three days and it’s been the second day since the last body was found. We need you guys here.” Spencer overheard Hotch’s near yells over the phone.
“Okay, dad, calm down there. I’ll call up Garcia to find us the closest hotel and we’ll crash there. Reid says snowing too much for an officer to come pick us up.” It was around 7:30 and the sun was starting to set.
“Alright, we can send someone to get you tomorrow.” Hotch hung up and Derek called Penelope.
“Hey-llo my chocolate thunder! Anything I could do for you?”
Derek coughed a couple of times.
“You okay, Derek?”
“Yeah, uh, me and Reid got stuck in the snow and we can’t get back to the hotel. Are there any near us that we can crash at?”
“You’re in luck, Derek Morgan, There is a motel only a seven minute walk away from you. Anything else?”
“Not right now, baby girl, take care of yourself.”
“So what are we gonna do?” Spencer had begun chewing on his fingernails and pacing in a circle around the car.
“Kid,” Derek took Spencer’s cold hands into his warm, gloved ones. “Stop your worrying. I can see all of those gears in your head going a million miles an hour. Garcia found a motel near us and we can walk there and stay the night until someone can pick us up. We’ll be okay.”
“I know I’m gonna be okay, it’s you I’m worried about, Morgan.” Spencer took his hands out of Derek’s and leaned into the car to grab his bag.
“What do you mean? I’m fine.” As if on cue, Derek started having a coughing fit.
“I’m talking about that, Derek. You’re showing signs of getting the flu. Your heart rate has sped up by 39% in the last couple of days. You constantly have a running nose and you won’t stop coughing. I am not getting sick, I cannot afford to get sick, especially on a case, so I hope this motel has two beds.” Spencer pushed away from Derek and began walking.
“Wait!” Derek ran to catch up. “Pretty boy, you’ve already been with me for almost 24 hours. I think you are already infected. Besides, you, my friend, are shivering. Now let me give you one of my coats.”
Spencer slowed his walking and let Derek drape his second jacket over his thin, purple one. Having a crush on your coworker was the worst.
When the pair reached the motel the sun had fully set and they had snow covering their shoulders and resting on their heads. They brushed it off before entering, where they were bombarded with the overwhelming scent of perfume as what could only be presumed as the owner tugged them in with both of her arms. She was short and wore a sparkly pink dress not unlike one Penelope would wear.
“What can I do for you kind fellows today? Did ya crash on the side of the road? Lots of people did tonight. Can I get you a room? Was it your engine? Faulty car?” The woman rambled.
“Um, we fell in a ditch a little bit back. We just need two rooms for the night,” Spencer looked down at her nametag, “Sasha. Thank you.”
“Well, boys, I am sorry to disappoint but we only have one more room for the night. You’re just gonna have to share.”
“Are there at least two beds?” Spencer whined.
“Sorry,” Sasha took Derek’s credit card and punched in the numbers on a computer that looked almost a decade old. “You good there? You look like you could throw up any second?”
“I’m fine, ma’am. Just give us the room key please.” Derek cleared his throat.
“Alrighty, there you go FBI guys.” Sasha handed them the room key labed 7B.
Given the overwhelming personality that brought them in, neither had a chance to look around and profile the front office. When they got to the room they realized just how miserable the stay would be.
The heater seemed to be turned off resulting in the room being colder than the outside. Complementary water bottles on the nightstand had frozen, expanded, and exploded. The pipes in the walls creaked and whined. Derek moved towards the bed, which when he pulled up the sheets, they were stiff and barely moved at his touch. Spencer moved past the bed and to the kitchen, where he found a coffee machine and cups in the cupboard.
“What are you doing?” Derek coughed.
“Making coffee. It’s something to keep me warm.” Spencer still had Derek’s jacket across his shoulders.
“Alright well, you might be right. I think I’m starting to get a fever. I’m gonna hop in the shower. Hopefully it’s just the reverse air conditioning that’s broken.”
Derek’s observations were proven correct as he unexpectedly walked into the spray of a nearly boiling shower. His muscles relaxed as he began thinking about the events of the day. His nose ran more than it had in the cold weather and it reminded him of a moment in the office that happened some while ago, back when Spencer first joined the BAU.
It was a slow day in the bullpen. With Spencer being nearly fresh from college, Derek wasn’t expecting him to take the best care of himself, no one was. Derek looked up, ready to throw Spencer a rolled up note about how bored he was. Instead he was greeted with an empty desk. After asking Hotch where the boy genius was and getting a surprised ‘I don’t know’ in response, he went in search of him. Spencer was found laying on the couch in an empty office. HIs skin was red and burning to the touch. Derek gave him a couple of shakes and he woke up, groaning. Spencer had gotten the flu and didn’t know how to deal with it at work. Not wanting to disappoint Hotch by skipping a day for something so insignificant as a virus, he settled in an office he correctly assumed was vacant. He insisted that he was okay but Derek refused to believe him. He dropped Spencer off at his apartment and immediately knew. He was in love with Spencer Reid. And he wanted to spend as much time with him as possible.
When Derek was in the shower for at least 15 minutes Spencer presumed that the shower was warm, so he called Sasha at the front desk from the phone in the room. She wouldn’t be able to get someone to come fix it for another day. He sat on the bed, spreading his arms and legs out in an attempt to warm the sheets. Letting his mind wander, he started asking himself questions. Why did he like Derek? He was just his coworker. Just someone in his life. An attractive person in his life, but just like anyone else in his life. Did Derek know how much he meant to him? Would he ever know? Would he be given the chance to let Derek know that he loved him and wanted to spend his life with the other knowing?
He was taken out of his day dream when Derek came out of the bathroom. Derek was shaking. He wore thick, flannel sweatpants and a grey hoodie, along with his socks, not wanting to leave a single part of his body too exposed.
“Uh, I know you’re super germaphobic and probably want nothing to do with my running nose and sore throat right now, but kid, all of my muscles are aching. Do you mind if I-”
“Not at all.” Spencer wrapped his arms around Derek’s middle as he sank onto the bed.
Derek let out a sigh of relief and settled in Spencer’s arms. It wasn’t long until his breathing evened out and he fell asleep in the lanky man’s arms.
“I think I love you, Derek Morgan.” Spencer whispered.
The next day Hotch called Derek to let him know that they caught the unsub. He was an amateur child groomer who left a hair in his latest victims mouth. An officer picked up the pair from the motel and they boarded the jet. Derek’s flu passed as soon as it came and he was better in the morning. A little cuddling with Spencer was just what the doctor ordered.
“Hey, Spencer.” Derek sat across from him after everyone on the jet had fallen asleep.
“Yes, Derek?” Spencer noted the use of his first name in his head.
“We need to talk about last night.”
“What about it?”
“I heard you, Spencer.”
“Wh-what are you talking about? Heard me say what?”
“Spencer,” Derek put his hand on the other’s knee, “I love you too.”
In a panic, Spencer leaned forward and pecked Derek on the lips.
“I-I’m sorry, I shouldn’t have done that.” He stammered.
“It’s okay. We can do that if you want.” Derek leaned back in for a real kiss from Spencer. He still tasted like the cheap hotel coffee.
“We can do anything as long as we’re together.”
TAGLIST: @greenaway-lewis @pretty-b0yy @w0rmpi3 @sunflowrly @fuckshitupm8-deactivated3728 @the-sassy-one @endetit @adhd-lesbian @nobody121113 @stalinthestripper
#moreid#spencer reid#derek morgan#spencer reid x derek morgan#sickfic#criminal minds#criminal minds fanfiction#fanfiction#fanfic#moreid fanfic#moreid fanfiction#jennifer jareau#aaron hotchner#penelope garcia#emily prentiss#criminal minds fluff#spencer reid fluff#fluff#derek morgan fluff#moreid fluff#12 days of moreid
94 notes
·
View notes
Note
I know that this situation is causing a lot of people to be anxious, but I’m worried about my pregnant friends specifically. As someone who works in a medical setting and is expecting, what are your thoughts? I really appreciate it ty
There's no evidence so far of the virus being transferred from mum to unborn baby. Obvs this is all super preliminary and no large scale studies have been performed yet but so far, it looks like it isn't transmitted through the placenta. The biggest worry I think is the tendency of infections to bring on a fever which isn't super good for baby but can be managed easily and safely with acetomeniphen. If you have a fever that can't be managed with acetomeniphen, you should see your healthcare provider anyway, even in the absence of a pandemic.
Breastfeeding mums who test positive should wear a mask while feeding, at least until symptoms go away, and it's of course really important to practise good hygiene by washing your hands and sneezing into your elbow, but that's basically all the information my midwife gave me. I can update you guys if any of it changes or if any new info becomes available but in the meantime, and I cannot stress this enough:
STAY HOME.
Corona is not the end times and our main priority is to control spread so that we don't overwhelm the healthcare workers who, unfortunately, don't get the luxury of working from home. Most symptoms can be managed effectively from home anyway using standard cold and flu measures so please don't present to your hospital unless you're in actual distress. We don't have the kits or the beds or the staff to look after all of you and we need to prioritise those who urgently need the care.
Please don't go out unless you need to. Please skip that bbq or cancel that birthday party or work from home if you can. I know it sucks (believe me, I just had to cancel my baby shower) but it is the safest and easiest precaution you can take for yourself and for your friends and family. Just stay home! Enjoy your staycay!
I am still at work for you. Please please please stay at home for me.
29 notes
·
View notes
Text
So my district's response to Covid so far:
Teachers and staff will be expected to self-screen their temperatures before arriving to campus. Parents enrolling their children will be given "screening questions", as will parents coming to campus to pick up their student early. Students' temperatures will not be taken.
I purchased my own infrared thermometer and a pulse oximeter, both in the interest of daily self screening, and in the belief that I am very likely to contract the virus if school opens without dramatic changes to the plan .
Hand sanitizer will be available on campus... at main entrances to the building. As of right now, there is no plan to purchase hand sanitizer for classroom use.
I am stockpiling my own hand sanitizer, from my own salary, instead of paying off debt or purchasing household items or entertainment.
Students will be encouraged to wash their hands. Teachers will be responsible for instructing them on handwashing the first day of school.
I am awaiting email clarification if our classroom sinks will be provided soap this year, or if there's some way that any of the sinks accessible to students could be altered to use hot water. I am also advocating for the hand dryers to be replaced by paper towels.
Students will be encouraged to sneeze into a tissue or their elbow. No mention has been made of the school providing tissue.
I have a few boxes I had bought in February in my cabinet at school, and am planning on asking my relatives to purchase Kleenex for me in lieu of any birthday celebration in August (along with hand sanitizer and sanitizing wipes if possible).
The schools will be "regularly deep cleaned". No mention of specifics, of who will be cleaning between classes, when cleaning between classes is expected to occur if we maintain a normal schedule as has been stated.
I am stockpiling sanitizing wipes whenever and however I can get them, though I don't think I'll have enough to sanitize high touch areas or even all used desks between classes. Technically, I am not supposed to have said sanitizer in the classroom due to allergy concerns.
It has been decided social distancing is not possible. Plexiglass barriers or sneeze guards will not be provided. Students will be encouraged to frequently wash their hands instead.
I have put my 32 desks in front-facing rows. I will move my desk as far away from the sink as I can manage, and pray.
Students over the age of 10 will be required to wear face masks if so ordered by Governor Abbott. The district refuses to commit one way or the other when asked if elementary school students will be made to wear PPE or if masking will continue when Governor Abbott's order expires.
My mother is sewing me cloth face masks, and I have ordered my own face shields from Amazon. I'm praying it will be enough, even though the mask protects students from me, not the other way around.
I pray that my administration doesn't try to shame me out of wearing PPE in the name of "normalcy for the children".
Schedules, including four minute passing periods where all 1000+ students are in the halls fighting to use the same three bathrooms at the same time, and including lunches where grade levels eat in groups of roughly 300 at a time, will not be altered.
I try to avoid thinking about this one. I'm afraid. I will probably be eating in my car, if I eat or drink of campus at all.
Students whose parents are uncomfortable have the option of at-home all online learning.
I regret the fact that the district has refused to offer any at-home option to staff whatsoever, and that their unsafe plan was deliberately released after the last day I could exit my contract with no penalty, even though I know the odds of my finding remote work to pay rent were low.
I regret that I trusted them to come up with some way to at least try to protect us.
I try to come to terms with the fact that I, a Type 1 Diabetic, am now at extreme risk for catching Covid and for possible hospitalization or death. It isn't as if I have another way to pay the bills.
Students with "Covid like" symptoms are expected to stay home. If a nurse checks a child and finds they have a fever, the parent will be "expected to immediately take them home", as if I haven't had students come to school dosed up on Tylenol because their parent has to work, or sent a child to the nurse for vomiting on the floor first period only for the to remain at school all day with no phone calls answered and arrive promptly again for first period the next morning.
I wonder if my school nurse, in her 50s and diabetic, will return this year. I wonder if she has the flexibility of a choice.
If a student is confirmed to have Covid, only the parts of the school the student regularly accesses will be closed and only for 5 days of "deep cleaning".
I think about students skipping in wrong-grade-level bathrooms, fixing each other's hair, play-fighting, sneaking snacks, taking selfies .
I wonder about the cafeteria. The gym. The band hall. The hallways a student need to be in, but wandered down anyway because they hate going to their science class, or because they wanted to talk to a friend. I wonder about lockers.
I wonder if the district ever actually intends to address what will happen if a teacher comes down with Covid. If we'll be paid when we run out of sick days or if we'll have to hope we took the disability insurance and it will pay our bills.
I wonder how other classes are supposed to continue, knowing another child likely now has the virus, somewhere else in the school, and doesn't know.
I wonder if we'll even be able to get a Covid test and see our results in five days.
I wonder how many times my hall will be shut down.
I wonder if our custodians, hourly workers with 30 minutes or less per room, will get hazard pay. I wonder about our food service workers.
And a bonus:
Parents flood the social media of the district.
Some are angry, and demand information on how they can get an exemption to the masking order for their child "because a mask is more dangerous for kids than the virus". Danger to teachers is not mentioned.
The inevitable people wanting a "refund on their taxes" if the school is forced to close flood the comments. No one talks about the expense of providing technology to the students who are remote learning and don't have their own. Or about what the costs will be when multiple teachers become too sick to teach, especially of we can't find subs.
So many people question why teachers think they're better than "other essential workers". I wonder if those parents will contribute to the classroom supplies this year, or if on top of my own sanitizer and PPE, I will still be expected to use my salary for pencils and paper. I wonder how many of those parents have been locked in a room with no windows and thirty year old ventilation for an hour at a time, tightly packed with 30 other people whose infection status they do not know. How many of them do so for seven groups of thirty people, for seven consecutive hours.
People threaten to leave the district if any restrictions are placed whatsoever on sports, music, the things their kids "need". I think about a student athlete getting sick and permanently scarring their lungs too badly to play. About the coach with the new baby son. About our elderly choir teacher. I think I might be relieved if the parents followed through.
People tell us that there's never life without any risk, so we should stop whining and get on with life. I wonder how many of them are considering buying a $200 filter for their work place, on the off chance it makes them and their children the slightest bit safer. How many are spending their own salary to clean their own work places, on their own PPE.
I wonder how many are telling their children the virus is a hoax, and how many twelve year olds will think it's "funny" to aggravate their teachers by purposefully being unsafe this year. I wonder how many will get sick.
I wonder how many parents would notice or care if I got sick, if I , a type one diabetic with no other financial means, was hospitalized or died. I wonder how many would just be angry at the disruption to their lives.
I start preparing myself for the likelihood I will get sick.
I wonder why no one with the power to fix this, to even mitigate it, seems to care.
5 notes
·
View notes
Text
My dearest little pie
The past week must have been hard for you. Battling a high fever, getting poked at places you don't like, taking endless doses of medications, and doing hourly checks by strangers you fear of. Mummy and Daddy's heart is breaking for you, and the tears you shed - Mummy and Daddy shed too.
I want you to know how brave you have been. I want you to know how proud I am to be your Mummy. When you walk around the hospital wards waving to all the nurses and doctors who know your name solely because you were just so cute, I want you to know how proud I am to tail you from behind and see just how loved you are everywhere you go.
The first day in the hospital was tough for you. We went to SKH and had to do a blood test twice because of how much you were struggling, because of how much you hated the prick on your finger. Your fighting spirit puts Daddy and I in such difficult positions but I know this very spirit is what that will tide you through tough times in the future. I hope you never lose it.
You braved through the x ray wearing that cute little vest. You thought they were taking a picture and so you smiled like they were. Even in such worrying times you make Mummy laugh and smile. I don't know if you know but your laugher and smiles are what that helps Mummy through the difficult moments. Your spirit lifts me up. And I thank you for that.
Unfortunately, the x ray revealed an infection in your chest and the doctor said it was bronchitis. Suddenly we were stepping into unfamiliar grounds because Daddy and I never had anything remotely similar before. We were given medications and puffs to go home with. Your raging fever of 39 degrees finally dipped to 37 degrees and the doctors found you fit to be going home. It was a tough few hours in the hospital and you were already tired from a lot of crying. We were looking forward to a good rest at home.
Then came night when things took a turn. Your fever came back raging at 40 degrees. Even with ibuprofen it did not subside. Daddy, Mummy and Mama were all so worried that we decided to make another trip to the hospital despite it being already close to midnight. We quickly changed our clothes and left for KKH. Mummy wore extra comfy shirt and tights because somehow something tugged at my heart telling me it's gonna be another long night.
At KKH, Daddy and Mama were not allowed to enter due to covid restrictions. So you and I both toggled between going into the A&E area and coming out to be with Daddy and Mama. After 3 hours of waiting, forcing you with the inhaler, and more medications, a decision was made to have you warded. Then the bomb was dropped that you would be required to take a covid test. At that point it felt like my world stood still. As harmless as it was, the thought of having to swaddle you tight and force a swab up your nose was not something Mummy could bear emotionally. Yet a choice was not given.
The isolation ward, as per covid procedures, was only ready by 4am. You were already fast asleep before the ward was ready. Mummy carried you up and stayed by your side while Daddy drove back home to prepare the necessities for your stay. At 5am, the phone rang, and a very sleepy doctor asked for details of your illness. At 5.30am, nurses came in to check on your vitals. Your oxygen levels have fallen to 92% and so oxygen support was given to you. I though my heart could not be any more broken but at 6am, I was proven wrong because it was time for your swab.
You needed to do 2 separate swabs, 1 for covid and 1 to find out exactly which virus was attacking your little body. When I asked the nurse if it was only 1 on each nose, she said she had to do both noses for both swabs. That is 4 swabs in total. My heart broke even more. The nurses and Mummy had to pin you down for the swab and your cries were different. It was not one of being upset, but one of fear. You cried over and over again,"Mummy bao bao! Mummy bao bao!" At that point you must have felt abandoned and confused. Why is Mummy allowing strangers to pin you down this way? Why is Mummy not picking you up immediately like how I always do? I bit my lips to hold my tears. In my heart I knew this had to be done, for you and your health.
When the nurse did the swab you choked on your cries and said,"I don't want to dig nose! I dont want to dig...!" When your words trailed off I knew the swab was in. I bit my lips harder to hold back my tears.
After what seemed like forever, the nurse finally said it was done. I immediately unswaddled you and carried you away. I hugged you tight, hoping you could feel that Mummy loved you so so much. You cried and cried. Then you tried your hardest to compose yourself to say this,"I want to go outside to see Papa. I want to go outside to see Papa." In your 2 yr old mind, you already knew Papa was always waiting outside, ready for whatever you needed him for. In this moment, Mummy broke down crying. Because Papa was not outside. Because this was an isolation ward. And Mummy don't know how to say it to you, my 2 year old baby.
When Mummy cried, I told you I love you. You sobbed silently. I knew you lowered your crying to hear Mummy cry. It must have been confusing for you. Why is Mummy crying?
When Mummy told Papa what happened, Papa cried too. You were his baby, and he couldn't be there physically to hold you. Mummy could only say to you,"Tomorrow afternoon we can see Papa already. Papa loves you so so so much ok?"
Shortly after, you fell asleep. It had been a long difficult day for you. Mummy stayed up monitoring your oxygen level. Daddy and Mama waited at home, both having terrible sleep that lasted max 3 hours. At 8am, both Daddy, Mama and Halmoni texted Mummy for updates. The isolation room sounded so peaceful with just you and me, but outside, the chaotic worry carried by everyone was far from peaceful. I gave everyone updates and the nurses continued to come in hourly to check on you. You woke at 9am and had little breakfast. You were chirpy as always, thankfully, and asked to go outside to see Mama. You made Mummy laugh when you told the nurse,"Nurse I want to go outside! Nurse! I want to go outside!" It was Mummy's first time hearing you say the word "Nurse". Haha. That alone made my day.
You continued to cry to leave the ward but there was still no COVID test result. You ate terribly again for lunch, only 3 potato wedges to be exact. And then you fell asleep and took a good long nap, still exhausted from everything that took place the day before.
While you were asleep, Mummy received news that your COVID test was cleared. I was so happy that I couldn't wait for you to wake up to tell you the good news - we could finally leave the ward!!
I looked outside the window and suddenly everything seemed brighter. It was 1pm and Mummy was amazed by how much of energy I still had within me, despite having no sleep for the previous night. Through the night Mummy prayed for your health, and always ended the prayer with,"The joy of the Lord is my strength." The power of prayer is amazing indeed.
1pm also meant that Mummy has held on to my pee for more than 10 hours! I slipped away to the toilet within the room, and when I was done, I felt a wave of happiness and relief. It was going to be a good day!
When you finally woke up after a long nap, Mummy said we could leave the room and your face lighted up! We went to the admission area for a transfer of ward to the normal wards. Mama came to look for us shortly after and your face instantly lighted up when you saw her! You shouted so loudly,"MAMA!!!" from a distant and rannnnnnnn to her with all your might. Remembering that moment brings tears to my eyes. The love you have for Mama is one that was special.
0 notes
Text
wear your fucking mask
So here’s a post I never thought I’d have to post. And it’s a long one, so buckle up.
On Sunday evening, my husband came home from work with a fever. We got some fever reducers into his system, gave him a cool bath, and went online to schedule a COVID-19 test. An hour or so later, we realized that our son felt hot and took his temperature; 100.7. We immediately gave him Tylenol and a cool bath.
We’re just being cautious, we reasoned. There’s no way it’s anything other than a flu, and they both have it. That’s all.
Their fever broke that evening, but we still went Monday morning to the test site because that’s the right thing to do. It was a self-administered test, and he said it wasn’t as bad as he thought it would be.
We’re just being paranoid, we told ourselves. COVID-19 symptoms don’t just stop.
Over the course of the day Monday, other symptoms began to present. He got a dull headache throughout his skull, his body ached, and he couldn’t stop sweating. We went straight home after the test because that’s the right thing to do.
He doesn’t have a cough or a sore throat, and his breathing is fine, so it can’t be COVID-19.
And we’ve been doing the right things all along. We’ve washed our hands religiously, we wore our masks, we destroyed our hands with hand sanitizer (I have actual chemical burns; I appreciate alcohol distilleries for stepping up and making sanitizer to help fill the gap in supply, but they had no business making chemicals they weren’t trained to make), we social distanced. Everything that we could do, we did, out of an abundance of caution and to protect ourselves and others.
Late Tuesday afternoon, he got an alert on his phone that test results had come back. We opened up our computer, fully expecting and hopeful that it would have good news.
“Test results: POSITIVE for COVID-19″
......what?
..........................what?
We called our workplaces and received instructions on what to do next. We called my mom. His brother called him. We arranged for me to get a test done the next morning.
It was my husband’s birthday on Tuesday. Happy birthday; coronavirus got you a present.
Wednesday morning came. I went by myself to the testing site and got my own test done. It is mildly unpleasant, but not as bad as the Facebook memes want you to think. Please don’t avoid getting tested because you think it’s horrible. While I was out, my husband called our son’s pediatrician. Oh, have I mentioned yet that we have a toddler? Because we have a toddler. The pediatrician told us to take him to an Express Care so he could be tested too. She said it was very important that he get tested, in case he has it and his condition worsened.
I can’t describe to you what it’s like, holding your 21-month-old baby tightly to your chest while he struggles against the swab being put up his little nose. I can’t describe the tears, both from him and from me.
It was a fifteen-minute test, and the machine was in the room with my son and I as we waited, alone (it was a small exam room and for safety purposes and because ‘close contact’ is defined by the CDC as within six feet for a sustained fifteen minutes, the nurse could not wait with us, and for that she profusely apologized). He was on his best behavior, acting so sweet and so cuddly and not at all like he might have a deadly virus coursing through his little body. When the timer beeped, I couldn’t even look at the machine.
The nurse returned to the room and looked at the machine, and she said to me, “I’m going to have the doctor come down and take a look at him.” As she turned to leave, she paused and looked at me and added, “Since your husband tested positive and your son tested positive, you can assume you’re positive too. You don’t need to get tested.”
All of the air rushed out of my lungs. The machine had a big red + on the display.
The doctor came into the exam room in full PPE: two masks, a face shield, two gowns, two pairs of gloves with the sleeves tucked in, and goggles. He listened to my son’s lungs and said he sounded fine. He gave me some information, but I retained none of it. I was handed a few sheets of paper with that information typed on it so that doesn’t matter.
My baby has coronavirus.
My husband has coronavirus.
As I type this, my test results haven’t come back yet, but I probably have coronavirus.
Let me return for a moment to Friday, two days before all of this began.
My mom called me and told me that my Nana was really sick. Like, really sick. Like, “Come say your goodbyes” kind of sick. We made plans for me to take my son to see Nana on Saturday afternoon; she was in the hospital on Friday and was going to be brought home on Saturday so she could die at her home.
Saturday morning, I was at work. My phone started going off with texts around 7 AM, but I couldn’t look at it. I knew, but I didn’t want to Know, y’know? Like, it’s one thing to understand what a barrage of texts mean, but it’s entirely different matter to see the texts and read their awful truth.
My Nana had passed away early in the morning, surrounded by her five children.
I showed the texts to my manager and he told me to take off for the day.
The wake was on Wednesday. With my husband’s test result Tuesday afternoon, and then my son’s that morning, we did not go.
The funeral was today. We did not go. We had to watch my Nana’s funeral on a YouTube live stream.
My Nana was such an influential person in my life. She was kind and generous, but also iron-willed and brutally fair. She would listen to you when you had a problem and she would give you excellent advice, even if it was not the advice you wanted to hear, and she would stay on your case until you followed that advice. She was the principal of a boy’s correctional school for over twenty years. She was the only member of my family who really listened to me when I needed to talk about the emotional damage being an adoptee did, and she was the only person who took me seriously when I was infected with Lyme disease; without her practically ordering my parents to get me tested for Lyme, I don’t think I would have gotten a diagnosis until after I moved out on my own and could get it done myself. She was the matriarch of the family and truly, the center of it too. She cared deeply and loved deeply. She loved the Boston Bruins and the Boston Red Sox.
Because of coronavirus, I couldn’t be there for her wake or funeral or graveside memorial. I couldn’t be there for my grieving siblings and cousins and aunts and uncles and my mother. I hate it so much. Her death and our diagnoses couldn’t have happened at a worse time.
I’m starting to have symptoms too. I’ve had a headache that won’t go away. I’m fatigued but I can’t sleep. I am not feverish or physically overheating, but I can’t stop sweating. Weirdly, my hearing in my left ear is almost gone, which I’m learning is a rare symptom; it feels and sounds like I need to pop my ear, but I can’t make it pop. My sense of smell isn’t completely gone, but all I can smell is saw dust, which makes no sense because there is no saw dust in my home. And my chest feels tight.
For the moment, we’re okay. My husband has developed a bit of a cough, but it’s minor and controllable. My son is very tired and really only wants to cuddle. Both of their fevers broke Sunday night and haven’t come back. We ordered a forehead thermometer for our son, because apparently he’s suddenly terrified of our regular thermometer, and an oximeter online.
My husband and I did everything we possibly could to avoid infection. And I’m not saying that those things don’t work, because they do and we need to keep washing our hands and wearing our masks; I’m saying that at some point, there was a crack in our defenses. I don’t know where that crack could be.
Was it the coworker of mine who claimed she was perfectly healthy at the daily wellness check but secretly coughed a ton in our office? Was it the customer who told myself and another coworker, we were ringing him up, that he felt bad that his son was in quarantine due to a classmate testing positive, to whom it didn’t occur that if one member of the household is in quarantine, the entire household is too? Was it our apartment neighbors, who keep having to be scolded by the landlord for not wearing their masks in the common areas of the building? Was it just a chance encounter that neither of us have any memory of?
I really don’t care about your perceived “rights” that you think are being violated. I don’t really care about your political leanings. I don’t really care that you haVe a MeDiCAl cONdiTiOn aNd caN’t wEaR a MaSK because that’s bullshit and you know it.
My baby has COVID-19.
Wear your fucking mask.
0 notes
Text
Checking in on Bill Mitchell, The Godfather of Being Wrong
I thought the Krassenstein Twins era would be the low point of Twitter. Remember the shirtless cartoons? Remember all of the conspiracy theories? I suppose Seth Abramson is still chugging along.
While the worst part of Democrat Twitter is hunting for the latest and greatest ten-pronged Donald Trump conspiracy theory, the worst part of Republican Twitter is doing what they do best, full and unadulterated gaslighting. No one does this better than takist Bill Mitchell.
Bill prides himself on Being Right All Of The Time -- he’s a few months away from betting Diet Dews against Skip Bayless. Anyways, the best of the best gaslighters in this niche do two things well: they signal boost when they were right, and they bury where they were wrong. Burying comes in the form of either pretending they never said that (Mitchell is an exceptional tweet deleter), or moving the goal posts (he’s even better here).
Mitchell has had a lot of takes on the coronavirus outbreak. Like many of us, he has zero subject matter expertise. That didn’t stop him from screaming to a rabid, half-million follower base about the danger coronavirus didn’t present to the American public. Of course, as the obvious severity of the issue has become more and more obvious, Mitchell just changed his tune -- April has seen him spending his days begging for an economy open-up, pretending death counts are fake, and calling out people like Anthony Fauci as Deep Staters. It should be noted that math isn't particularly Bill's strong suit.
Interesting that ActBlue raised an average donation of $30.38.
This would imply people are donating in uneven numbers, including pennies, which would be odd. OR it would indicate untraceable foreign donations and an exchange rate translation, which would be illegal.
— Bill Mitchell (@mitchellvii) April 21, 2020
But it wasn’t always like this! One thing about Twitter is you can just .. kind of .. go back in time. January and February were reserved for occasional thoughts about the virus, China’s role, and the like -- mostly boilerplate stuff. In March, as limited cases spread into the States and concerns grew over the preparedness of the United States, Mitchell took it upon himself to carry as much water as he could for the federal government and their role in the pandemic.
As time elapsed, Mitchell predictably transitioned his arguments and measurement criteria to whatever looked favorable for Donald Trump on a given day. Even a thirty day snapshot of this is comical. This is a daily collection of tweets from as far back as .... March of 2020.
Can you imagine the absolute PANIC if COVID-19 numbers were as bad an COMMON FLU numbers? https://t.co/hVzlwlbxWZ
— Bill Mitchell (@mitchellvii)
March 1, 2020
Imagine if we ever hit 60K dead here in the States. Imagine!
The USA is one of the most traveled to destinations on the planet. The fact we only have 88 confirmed COVID-19 cases and 2 deaths is a true credit to President Trump's efforts to keep us safe.
— Bill Mitchell (@mitchellvii)
March 2, 2020
Am I right in thinking the vast majority of US cases of COVID-19 were acquired outside the US mainland?
So in essence, those really aren't US cases at all. They are international cases of people from the US.
— Bill Mitchell (@mitchellvii)
March 2, 2020
COVID-19 began by people eating infected snakes from a Wuhan market. Wuhan death rates highest by far.
Is this due to lack of care or because ingesting the virus in food makes it more potent? Is China slowing down because people are no longer ingesting it just as with SARS?
— Bill Mitchell (@mitchellvii)
March 3, 2020
Imagine for a moment that COVID-19 targets only unborn children, killing a million American babies in the womb every year.
The Democrats would be outraged, calling for Trump's impeachment for, "failing to protect the most vulnerable among us."
We could rename it to ABORTION-19.
— Bill Mitchell (@mitchellvii)
March 4, 2020
As you know, abortions are ... contagious?
And so what if the mortality rate of COVID-19 appears higher in some places than the flu? You will NEVER get 31 million cases of COVID-19 in the US. You will NEVER get 34,000 deaths from this disease.
And for the flu, 34,000 deaths is a SLOW season. https://t.co/eMDKepUd2V
— Bill Mitchell (@mitchellvii)
March 6, 2020
COVID-19 is serious and needs to be limited. But so is the flu - much much more serious. Closing down events, businesses etc. is overdoing it.
The best solution. If you are sick, stay home. Don't go to see the Stones with the flu.
— Bill Mitchell (@mitchellvii)
March 6, 2020
As biological weapons go, COVID-19 is pretty mild. I mean, compare that to some of the NASTY stuff they came up with in WW1.
— Bill Mitchell (@mitchellvii)
March 6, 2020
COVID-19 isn't the flu.
Until COVID-19 infects 31 million and kills 34,000 Americans, the flu is worse.
— Bill Mitchell (@mitchellvii)
March 6, 2020
Coronavirus "survivor" had a 3 hour fever of less than 100 and not a single symptom since there.
— Bill Mitchell (@mitchellvii)
March 7, 2020
So every time a new virus comes along that kills 3500 people worldwide we shut down modern civilization?
COVID-19 seems to share a lot of common goals with climate change activism, doesn't it?
Coincidence?
— Bill Mitchell (@mitchellvii)
March 8, 2020
How big a deal is COVID-19?
— Bill Mitchell (@mitchellvii)
March 8, 2020
(As an aside, this is one of any million of examples of Bill moving goal posts. First it was nothing, then it was real but not as bad as the flu, then it was like the flu. And so on. You may know this, but Bill Mitchell -- not a doctor.)
I am seeing more and more trollbot accounts calling themselves "Trump supporters" who aren't and are spreading COVID-19 #fearporn. This is a concerted effort by the left to over-hype this. It's obvious as yesterday they called for banning Trump rallies.
— Bill Mitchell (@mitchellvii)
March 9, 2020
There are a bunch of these but Bill’s surprise that this global health issue may not be political and, well, Republicans can actually be concerned with their health ...
Will companies start mass-layoffs for the COVID-19 dip? Unlikely. Hiring and training new staff is EXPENSIVE and CEO's understand this is all hype-driven. They don't want to unleash their hard-earned staff so their smarter competitors can scoop them up cheap.
— Bill Mitchell (@mitchellvii)
March 9, 2020
Certainly not an economist either.
How can Democrats say Trump is failing in his COVID-19 response when America is clearly outperforming the planet by leaps and bounds in prevention? More #FakeNews. https://t.co/VC1EO4J4nW
— Bill Mitchell (@mitchellvii)
March 9, 2020
The amount of hyper-hype surrounding COVID-19 is truly without precedent.
Other than 15 people who died at an senior acute care facility in WA known for poor virus protections in the past, SEVEN Americans have died from COVID-19.
SEVEN.
Did you catch that?
SEVEN.
— Bill Mitchell (@mitchellvii)
March 9, 2020
I've gotten a flu shot 3 times. 3 times I got the flu shortly thereafter. I won't be rushing to get a COVID-19 shot.
— Bill Mitchell (@mitchellvii)
March 9, 2020
Not a doctor.
I've gotten a flu shot 3 times. 3 times I got the flu shortly thereafter. I won't be rushing to get a COVID-19 shot.
— Bill Mitchell (@mitchellvii)
March 9, 2020
The media can bitch all they want about Trump's "failure of leadership" on COVID-19, but the bottom line is, in a nation of 350,000,000 souls, outside of one senior care center in WA, there have been just 8 deaths from this disease.
That's REAL leadership and REAL results.
— Bill Mitchell (@mitchellvii)
March 10, 2020
What will be the next Democrat manufactured crisis after COVID-19 fades away with the warm weather?
— Bill Mitchell (@mitchellvii)
March 10, 2020
I keep hearing that deaths from COVID-19 are going to "explode" in the US any day now.
WHEN?
— Bill Mitchell (@mitchellvii)
March 11, 2020
Not an epidemiologist, either.
A month from today, how many American will have died from COVID-19?
— Bill Mitchell (@mitchellvii)
March 11, 2020
This doesn’t have anything to do with Bill but boy is it depressing.
Just to be clear in case you missed it:
94% of all reported deaths from COVID-19 are in THREE countries. The largest of those 3 accounting for 70% of all deaths has slowed expansion to a crawl - they've beaten it.
Take away these TOP THREE and you have only 291 global deaths.
— Bill Mitchell (@mitchellvii)
March 12, 2020
Ignore the dead people and you have less dead people. An update to this one would be nice.
Looks like the COVID-19 updates are in:
USA - 1 new death. 10 in serious condition.
Hardly the zombie apocalypse we've been promised.
— Bill Mitchell (@mitchellvii)
March 12, 2020
Other than Japan, the USA is clearly doing much better than any other major nation - and yet, the #Media is calling Trump's efforts an abject failure.
Remove the 26 deaths from one nursing home and there have been only 15 deaths in America attributed to COVID-19. pic.twitter.com/nM2iZtGy3c
— Bill Mitchell (@mitchellvii)
March 13, 2020
What do fake climate models, fake COVID-19 models and fake polls have in common?
They are all fictional numbers created for one purpose, to provide a premise for that days #TDS news cycle.
None of it is real.
— Bill Mitchell (@mitchellvii)
March 13, 2020
March 13th is one of the earliest days where Bill began positioning his next line of arguments, transitioning from “the numbers don’t exist” to “the numbers do exist but now they aren’t real”.
I'm amused by people who say, "just the flu." The flu infects millions and kills 10's of thousands.
When COVID-19 gets to that level, ring a bell so we'll know. https://t.co/ZUD9F54NZr
— Bill Mitchell (@mitchellvii)
March 14, 2020
US testing for COVID-19 is really taking off.
Expect infection numbers to spike and mortality to plummet. I'm guessing we'll be under 1% US mortality within 2 weeks and under .5% in a month.
— Bill Mitchell (@mitchellvii)
March 18, 2020
Not a mathematician. Certainly not a freaking mathematician.
What makes the 127 lives lost to COVID-19 so much more valuable than the 50,000 lives lost to the flu?
— Bill Mitchell (@mitchellvii)
March 18, 2020
Six weeks and annualized and .. yeah.
100% cure rate + warm weather = the end of the COVID-19 panic.
Of course, the #Media won't want to let this go since it'a all they've got, but just a matter of time now. https://t.co/V0eIsydR4H
— Bill Mitchell (@mitchellvii)
March 20, 2020
Mitchell has frequently criticized the media, an easy target with such significant failings on both sides of the political aisle. But he also will very quickly circulate anything that coincides with his unfounded, baseless, void-of-science beliefs. From those same media outlets. Every time. “Believe it only when I say so.” The usual.
No one cares about flu deaths because the flu is "common" and has no fear factor. It cannot be used politically.
And yes folks, this is ALL about politics.
This is all about beating Trump.
It won't work.
Tell me when COVID-19 reaches 55,000 US deaths.
— Bill Mitchell (@mitchellvii)
March 20, 2020
Yes, tell Bill when we reach 55K deaths here in the States.
Dr #FearPorn Fauci is the designated Democrat Debbie Downer of the #COVID19 crisis:
Vaccines are beginning trials!
FAUCI: "Those will take years of testing."#Hydrochloroquine very effective treating COVID-19!
FAUCI: "We need massive, slow testing before that is used."
Jerk.
— Bill Mitchell (@mitchellvii)
March 20, 2020
Bill Mitchell, not a doctor.
Here's the deal. If you are on Trump's COVID-19 Task Force, you DO NOT run to CNN and CONTRADICT the President unless,
YOU
ARE
THE
ENEMY.
FULL
STOP. https://t.co/72UdoU0p9I
— Bill Mitchell (@mitchellvii)
March 20, 2020
See prior.
COVID-19 will be over as a serious global threat within 60 days, and perhaps sooner.
— Bill Mitchell (@mitchellvii)
March 22, 2020
All of the arrogant liberals telling us COVID-19 is the worst disease ever to strike mankind will crawl back under their rocks in another 30-60 days when this is all over - then come back out next time some new fake disaster arises to harm Trump.
— Bill Mitchell (@mitchellvii)
March 22, 2020
Studies have shown, as with H1N1, CFR'S tend to be inflated by a factor of 10 early as only the sickest are tested. As time passes this changes and CFR plummets by a factor of 10.
In the end, COVID-19 will be no more deadly than H1Ñ1 which was no more deadly than THE FLU.
— Bill Mitchell (@mitchellvii)
March 23, 2020
“H1N1 caused 18,500 laboratory-confirmed deaths with an estimated 151,700 to 575,400 deaths total in two years.”
Trust me, within 60 days, the #Media will be writing articles that COVID-19 was, "a scam by Trump all along." "He always knew there was a cure but withheld it for maximum effect."
They'll even find some way to tie it to Russia.
You KNOW it's coming.
— Bill Mitchell (@mitchellvii)
March 23, 2020
NY is clearly the COVID-19 apex in America. Word is major #hydrochloroquine testing may begin there tomorrow. If that happens and shows results, it's just a matter of time before President Trump has defeated "a once in 100 years" outbreak, as the #Media loved to call it.
— Bill Mitchell (@mitchellvii)
March 23, 2020
By wildly overhyping COVID-19, Democrats have set Trump up to be the GOAT when this thing ends in the next 30 to 60 days. They put the ball on the T for Babe Ruth with the bases loaded.
— Bill Mitchell (@mitchellvii)
March 24, 2020
So far today, new COVID-19 are lagging yesterday's numbers. Of course that can still change, but we are NOT seeing exponential growth. This looks like the top of a bell curve. pic.twitter.com/Fj99H9q2kA
— Bill Mitchell (@mitchellvii)
March 24, 2020
Not a mathematician.
My sixth sense is telling me that the research done on creating a COVID-19 vaccine will lead to a completely new approach to fighting viruses and a "Universal Virus Vaccine" which defeats all viruses ability to attach to and invade human cells.
— Bill Mitchell (@mitchellvii)
March 25, 2020
By the 25th of March, we were in Bruce Willis territory.
History will look at COVID-19 as the greatest overreaction in medical history based upon politics.
— Bill Mitchell (@mitchellvii)
March 26, 2020
There were about 15K dead globally at the time of this tweet. We are now at a quarter million dead, one month later.
Since the COVID-19 outbreak began, Diarrhea has killed 900,000 people. Can someone link me to the best Diarrhea Tracker? I'd like to avoid dying from Diarrhea.
Thanks.
— Bill Mitchell (@mitchellvii)
March 26, 2020
I don’t even know, I had to include it though.
If COVID-19 numbers doubled the seasonal flu, I'd be concerned. https://t.co/pZYZOgXPLh
— Bill Mitchell (@mitchellvii)
March 27, 2020
A great goalpost move. A week prior it had to “match” the flu. Now it’s double. Then we can talk!
I would not put it past Cuomo to alter New York's mortality numbers. Are they counting deaths WITH or FROM COVID-19?
Something strange is going on there.
— Bill Mitchell (@mitchellvii)
March 29, 2020
Around the end of March, coinciding with the inevitable exponential growth being experienced in the States, Mitchell strengthened the transition from ‘not a problem’ to ‘not really a problem’ to ‘it’s not worth shutting the economy over’ to 'the numbers are fake’. Which is odd, because as far as I can tell, Mitchell has never disputed -- in the literal sense -- the existence of coronavirus.
I am seeing hundreds of tweets from people who had a "weird flu" in December. Many of the COVID-19 symptoms, but tested negative for flu. No one described this as "life-threatening," just the flu, maybe a bit on the mild side.
— Bill Mitchell (@mitchellvii)
March 29, 2020
Not a doctor.
I take whatever mortalities I see reported in Italy and divide by 10 to get close to those actually killed by COVID-19.
Their counting method is preposterous.
11% CFR is BS.
— Bill Mitchell (@mitchellvii)
March 29, 2020
GOOD OLD DOCTOR DOOM IS AT IT AGAIN ON CNN, HIS FAVORITE SPOT TO DUMP ON TRUMP - Fauci: U.S. Could Have 100k to 200k Deaths from Coronavirus https://t.co/oB7nXarQo1 via @BreitbartNews
— Bill Mitchell (@mitchellvii)
March 29, 2020
The States are over 60K dead as of today, so "Dr. Doom” appears to be forecasting with a reasonable degree of accuracy, unlike Bill, who is not qualified for any of this.
If 80,000 die from COVID-19 it would be roughly equivalent to a bad flu season we'd normally ignore.
— Bill Mitchell (@mitchellvii)
March 29, 2020
(Goal posts. Now it’s 80,000.)
Seems as if the exponential growth in COVID-19 deaths is always, "The Day After Tomorrow."
I was assured two weeks ago we'd already be at many thousands of US deaths daily by now.
— Bill Mitchell (@mitchellvii)
March 30, 2020
It seems Dr Birx and Dr. Fauci are completely discounting the effects of warm weather and #hydrochloroquine on COVID-19.
— Bill Mitchell (@mitchellvii)
March 30, 2020
In summary: Bill Mitchell is a dangerous fool. And that is apolitical.
0 notes
Text
New top story from Time: All Your Coronavirus Questions, Answered
One of the worst symptoms of any plague is uncertainty—who it will strike, when it will end, why it began. Merely understanding a pandemic does not stop it, but an informed public can help curb its impact and slow its spread. It can also provide a certain ease of mind in a decidedly uneasy time. Here are some of the most frequently asked questions about the COVID-19 pandemic from TIME’s readers, along with the best and most current answers science can provide.
A note about our sourcing: While there are many, many studies underway investigating COVID-19 and SARS-CoV-19, the novel coronavirus that causes the illness, it is still essentially brand new to science. As a result, while we’ve drawn primarily on peer-reviewed studies published in scientific journals, we have cited some yet-to-be-published research into important aspects of COVID-19 when appropriate.
Coronavirus FAQ
What are the symptoms of COVID-19?
Who’s most at risk for COVID-19?
Are children at risk?
How long does COVID-19 last?
How long is COVID-19 infectious in people?
Can I get COVID-19 and the seasonal flu or common cold at the same time?
What’s the treatment for COVID-19?
How does a COVID-19 test work?
Should I get tested?
How does COVID-19 spread?
Is COVID-19 airborne?
Is there any difference between being indoors or outdoors when it comes to transmission?
Do masks work for preventing the spread of COVID-19?
How long does the COVID-19 virus survive on surfaces?
Is there any risk of the COVID-19 virus living on mail & packages?
Is there any risk with food delivery services?
Does rain wash away the COVID-19 virus?
What should I do to shop safely?
Should I worry about my clothes after I’ve been outside?
Can I get COVID-19 more than once?
If I get COVID-19 and recover, am I immune and safe to be around/help out older family and neighbors?
I’ve been social distancing for two weeks. When is it safe for me to go see family?
Can my dog or cat get COVID-19?
Can the COVID-19 virus live on my pet’s fur?
Do flies, mosquitoes, or other insects carry or transmit the virus?
Can cleaning products kill the COVID-19 virus?
Does it matter what type of soap I use to wash my hands?
What are the practices for doing laundry in a shared/public laundry room?
What are the symptoms of COVID-19?
Studies have shown that while some COVID-19 patients get only very mild symptoms or none at all, some can develop severe pneumonia and other health issues. A World Health Organization report from February found that around 80% of patients with laboratory confirmed cases “have mild disease and recover.” Researchers are not certain how many people infected with the virus are nearly or entirely asymptomatic. “There is not a single reliable study to determine the number of [asymptomatic sufferers],” says a metastudy conducted by scientists from Oxford University, and published online on April 6. “It is likely we will only learn the true extent once population-based antibody testing is undertaken,” write the study authors. (The metastudy, which looked at 21 earlier studies from around the world, has not been peer-reviewed.) The only way to know for sure if you are infected with SARS-CoV-19, the virus that causes COVID-19, is to get tested.
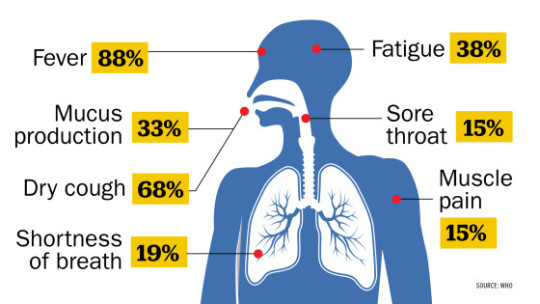
According to a study of nearly 56,000 laboratory confirmed cases cited in the WHO report, the most common symptom, experienced by 88% of confirmed patients, is a fever. The other most common symptoms according to that study are, in descending order:
Dry cough (68%)
Fatigue (38%)
Coughing up sputum/mucus production (33%)
Shortness of breath (19%)
Joint or muscle pain (15%)
Sore throat (14%)
Headache (14%)
Chills (11%)
Nausea or vomiting (5%)
Nasal congestion (5%)
Diarrhea (3%)
Coughing up blood (1%)
Eye discharge (1%)
One thing missing from this list is anosmia, or loss of sense of smell. Anecdotal reports suggest that people with milder cases of the disease could have telltale symptoms like the loss of their sense of smell and/or taste, however the WHO has not yet added those symptoms to its official list, as the data are not yet strong enough. But an analysis of a COVID-19 symptom-tracking app in the U.K. shows 59% of the 579 users who had tested positive for the disease reported a loss of smell and taste, compared to 18% who did not have the disease.—Billy Perrigo
Back to the top.
Who’s most at risk for COVID-19?
At this point, it seems people of all ages are susceptible to infection of SARS-CoV-2, the virus that causes COVID-19. However, those most at risk of severe cases of the illness are the elderly and people with underlying health conditions (like high blood pressure, heart disease, lung disease, cancer and diabetes) according to the World Health Organization (WHO).
The U.S. Centers for Disease Control and Prevention (CDC) clarifies further, stating that those most at risk for severe illness are:
adults 65 and older and people with chronic lung or heart disease
people who are immunocompromised (such as those with HIV)
the severely obese
people with chronic kidney disease undergoing dialysis
people with liver disease
In the U.S., 80% of COVID-19 related deaths have been adults 65 years and older, according to the CDC.
It is too early to tell if pregnant women are also at risk of severe illness caused by the coronavirus, according to the WHO. Some newborn babies have reportedly tested positive for the virus, but it is unclear how the transmission occurred.—Jasmine Aguilera
Back to the top.
Are children at risk?
Yes, but the good news is that their risk may be lower than that of most adults. Chinese doctors first reported that children did not seem to be getting infected as easily as adults, and that they also did not need to be hospitalized as frequently as adults did. That trend seems to be holding true in the U.S. as well. The Centers for Disease Control and Prevention reported that compared to adults, children under the age of 18 are less likely to experience the typical symptoms of infection, including fever, cough and difficulty breathing, and are also less likely to need hospitalization and less likely to die of COVID-19.
That’s unusual for a respiratory disease, since viruses like influenza often strike the very young and the very old more aggressively, given their more vulnerable immune systems. “I can’t think of another situation in which a respiratory infection only affects adults so severely,” says Dr. Yvonne Maldonado, professor of pediatrics at Stanford University School of Medicine and chair of the committee on infectious diseases at the American Academy of Pediatrics. “This is not common at all; we just don’t know what is going on here.”
One theory is that the severest symptoms of COVID-19 in adults may be caused by an overactive immune response to the virus in the lungs, which can make breathing difficult. Children’s immune systems may not be developed enough to launch such an aggressive reaction, and that may spare them some of the infection’s worst consequences.
The data suggest that infants may be more likely to need hospitalization if they are infected compared to toddlers, but more studies are needed to better understand how the virus is affecting children overall. In the meantime, doctors recommend that parents consider children as vulnerable to infection as adults, and appreciate that young ones can spread the virus as effectively as adults too, even if they don’t have symptoms.—Alice Park
Back to the top.
How long does COVID-19 last?
That depends on the severity of infection. If it’s a mild infection, like most people get, symptoms will likely last for about seven to 10 days and will be similar to those caused by the seasonal flu, says Dr. Emily Landon, the chief infectious disease epidemiologist at the University of Chicago Medicine. But for roughly 20% of COVID-19 patients, infection can worsen after this initial period, and in some cases lead to hospitalization. For even people with moderate cases, symptoms can last for a month or more until they are fully recovered.
“You can have people who have very mild symptoms that last a couple of days and then you have other people who can really get quite sick and go to the intensive care unit and be there for a month or more,” says Dr. Albert Ko, department chair and professor of epidemiology at the Yale School of Public Health. Those who get so severely ill that they are battling pneumonia and potential respiratory failure in intensive care units could take over a month to recover, Ko says.
Mild symptoms are unlikely to last longer than three weeks. “The fatigue can linger, as can the loss of appetite and some people routinely have a nagging cough after a viral infection that can last for weeks,” Landon says. “So some people will have lengthy symptoms but those aren’t really from active viral infection. They are more of a recovery syndrome.”—Sanya Mansoor
Back to the top.
How long is COVID-19 infectious in people?
It’s unclear. We do know that people infected with the virus that causes COVID-19 can be “contagious a few days before they even show symptoms and some people never really have much in the way of symptoms but can definitely pass on the virus,” says Dr. Emily Landon, the chief infectious disease epidemiologist at the University of Chicago Medicine. “What we don’t know is how long they remain contagious.”
The general rule Landon and her colleagues use is that “you’re probably good” if a week has passed from when you first began feeling sick and you’ve had three full days of feeling completely well. That means no more cough and no more fever for at least three days. “You are probably contagious starting two to three days before you develop symptoms and until your fever is gone and your cough is pretty much resolved,” Landon says.
The U.S. Centers for Disease Control and Prevention (CDC) says more or less the same in its guidelines, but is more explicit, telling COVID-19 patients that they are free to break quarantine only if:
they have had no fever for at least 72 hours without the aid of fever-reducing medications
all other symptoms like coughing and shortness of breath have improved
and at least seven days have passed since they first became symptomatic
if a coronavirus test is available, they should have also had two negative tests 24 hours apart
(The full CDC guidelines are here.)
The World Health Organization offers similar guidance to the CDC, recommending that COVID-19 patients be released from the hospital, isolation or home care only after they have two negative tests at least 24 hours apart and have clinically recovered. If testing is not an option, the WHO advises keeping individuals isolated for another two weeks after the symptoms are gone because they may continue to “shed”(or emit from the body) the virus.—Sanya Mansoor
Back to the top.
Can I get COVID-19 and the seasonal flu or common cold at the same time?
Yes.
Flu and COVID-19 are caused by two different viruses and there is nothing preventing you from getting exposed, and infected with both at the same time. It’s unusual, but possible.—Alice Park
Back to the top.
What’s the treatment for COVID-19?
For those with mild cases of COVID-19, the key is to get plenty of rest and liquids, as well as to take vitamins and eat a healthy diet, says Dr. Emily Landon, the chief infectious disease epidemiologist at the University of Chicago Medicine.
For severe cases, “there’s no evidence, based on the typical scientific rigor that we demand, for any specific treatment at this point,” says Dr. Albert Ko, department chair and professor of epidemiology at the Yale School of Public Health.
But there are trials underway testing some promising therapeutic options. One has been in the headlines recently: hydroxychloroquine. President Trump has repeatedly touted the drug (currently used primarily to treat malaria and some autoimmune diseases) as part of a possible cure for coronavirus even though experts, including Ko, say there is not enough evidence to currently recommend the treatment. “I have several concerns about the design of those trials,” Ko says, adding that while we know that hydroxychloroquine “suppresses viral growth in the test tube,” we “don’t know exactly why and if it’s going to work in people.” Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases and member of the White House Coronavirus Task Force, has said the research that produced the data so far “was not done in a controlled clinical trial. So you really can’t make any definitive statement about it.”
Another promising option is remdesivir, an injectable drug developed to fight ebola. “[Remdesivir] is probably the most promising of the drugs that we have available,” says Dr. Emily Landon, the chief infectious disease epidemiologist at the University of Chicago Medicine, but the full scope of its effects won’t be known until further analysis is conducted. Trials for remdesivir are currently underway.
Repurposed drugs like remdesivir and hydroxychloroquine can skip several regulatory steps and go straight to late-stage trials assessing effectiveness whereas new drugs have to face many more regulatory hurdles. (Hydroxychloroquine has already been approved for a number of medical purposes, while remdesivir, though tested as an Ebola treatment, has not yet been approved for anything.) An Emergency Use Authorization issued by the U.S. Food and Drug Administration can speed up the process for newer drugs, though even then, approval typically takes at least six months.—Sanya Mansoor
For more on treatments:
What You Need to Know About Hydroxychloroquine
The Launch of the First COVID-19 Vaccine Study
Back to the top.
How does a COVID-19 test work?
The current gold standard is a PCR (polymerase chain reaction) test, which detects the existence of the genetic material of SARS-CoV-2, the virus that causes COVID-19, in a person’s body. The test requires a sample of cells from the back of the nose and throat, and then uses chemical probes targeted to find the genes that code for the biggest feature of the virus, its spike proteins, which dot the surface the virus like a crown (hence the name “coronavirus”—corona is latin for crown). If someone is infected with SARS-CoV-2 and has traces of virus, this test will pick it up. It’s generally pretty sensitive, meaning it can pick up even relatively low levels of the virus.
But it has one key drawback: it may not find the virus if someone is tested very early after infection and there isn’t enough virus yet for the probe to spot.
The other type of test currently in use is a blood-based test that looks for antibodies to the virus. Antibodies are made by the body’s immune system to fight viral infection, so picking up antibodies is an indirect way of knowing that virus is present. This test also has drawbacks: it isn’t able to accurately identify people who are infected but haven’t yet generated enough antibodies for the test to detect.—Alice Park
Back to the top.
Should I get tested?
That depends on a number of different things. First, if you have a fever, cough and shortness of breath, you might consider getting tested since these are the hallmark symptoms of COVID-19.
If you aren’t sick, you still might need a test if you are at high risk of being infected. That category of people includes health care workers and anyone living with or caring for someone who is infected. Your exposure means you have a higher chance of getting the disease. Getting tested and knowing if you are positive means you can self-isolate and take other precautions in order to prevent spreading the virus to others.
Remember, however, that while you can ask for a COVID-19 test, you still need a doctor to authorize it. Even at-home test kits require you to connect with and answer questions with a telehealth doctor first, who will decide if you need the test.
At this point in time, due to limited availability of tests, the focus is on using testing to identify who is positive and in need of urgent medical care. It’s also important for knowing who is positive and therefore can spread the virus to others. As cases start to subside, the latter group will become more important as public health experts turn to testing as a way to control new infections. Testing will tell them who can return to work once shelter-in-place orders are lifted, and who, if they are positive, still need to self-isolate at home.—Alice Park
For more on testing:
Why Can’t I Get a Coronavirus Test?
An At-Home Coronavirus Test Is On the Way
A Two-Hour Test Has Been Submitted to the FDA for Review
Back to the top.
How does COVID-19 spread?
The prevailing means of transmission is via virus-containing microdroplets expelled when someone who is infected either sneezes or coughs. According to the U.S. Centers for Disease Control and Prevention, genetic material of SARS-CoV-2, the virus responsible for COVID-19, has been found in fluids in both the upper and lower respiratory tract, meaning that the saliva and mucus of an infected person is likely to contain the virus.
Less is known about other body fluids and products. One recent study from Sun-Yat Sen University in China found that genetic material from the virus is present in fecal samples from infected individuals. The CDC agrees that fecal transmission is possible and also reports that infectious SARS-CoV-2 has been found in blood. Even less is known about other bodily fluids, including urine, vomit, breast milk and semen. But CDC guidance for people who are sick and not hospitalized is nonetheless to “clean and disinfect all surfaces that may have blood, stool or other body fluids on them.”—Jeffrey Kluger
Back to the top.
Is COVID-19 airborne?
The virus that causes COVID-19 is an airborne pathogen, and humans are its primary delivery vehicle. Coughing, sneezing and even just speaking release droplets on the order of 100 microns in size (or 1/100th of a centimeter) into the air. “Your larynx is vibrating as you speak and it acts as a little nebulizer,” says Dr. Christopher Gill, associate professor of global disease at the Boston University School of Public Health. (A nebulizer turns a liquid into a mist.)
The half-life of the aerosol droplets is about an hour, according to Gill, which is short, but still leaves plenty of time after which the fluids released by an infected person’s cough or sneeze are infectious. It’s unclear to scientists if a viral particle continues to be infectious when the micro-droplet that contains it evaporates.
Even in a time of social distancing, enclosed public spaces like grocery stores remain problematic, Gill says, since a great many people may pass through an infected space within the hours the virus lingers in the air. “You should worry more about the air you breathe in a grocery store than about whether someone touched the broccoli,” he says.—Jeffrey Kluger
Back to the top.
Is there any difference between being indoors or outdoors when it comes to transmission?
Staying home and social distancing remain the best way to control the spread of the COVID-19 virus, but if you must come into contact with other people, you’re safer outdoors than indoors. We all occupy an area in three dimensional space, and as we move away from one another, the volume of air space on which we have an impact expands enormously. “If you go from a 10-ft. sphere to a 20-ft. sphere you dilute the concentration [of contaminated air] 1,000-fold,” says Dr. Christopher Gill, associate professor of global health at Boston University School of Public Health. That’s important because a single sneeze can project particles a distance of 9 meters, or about 27 feet. The less concentrated those particles are in the air, the less danger they present. “Within seconds [a virus] can be blown away,” Gill says.
Sunlight may also act as a sterilizer, Gill says. Ultraviolet wavelengths can be murder—literally—on bacteria and viruses, though there hasn’t yet been enough research to establish what exactly the impact of sun exposure is on SARS-CoV-2, the virus responsible for COVID-19.
That’s not to say there’s no risk outdoors. People can still cough, sneeze or speak particles into their air space, and especially in a city, the distance between individuals is not always 20 or even 10 feet. In general though, being outdoors in the vicinity of an infected person is safer than being indoors with that person.—Jeffrey Kluger
Back to the top.
Do face masks work for preventing the spread of COVID-19?
When the new coronavirus first hit the U.S., the Centers for Disease Control and Prevention (CDC) told people not to wear face masks unless they were sick or caring for someone who was. Masks help capture some of a sick person’s respiratory droplets, which might otherwise spread the virus. In early April, however, the CDC began advising all people to wear non-medical “masks”—any fabric that covers the nose and mouth—when they leave home. The reason for the shift? Scientists now know that many people who are infected with the coronavirus show no symptoms yet can still spread it to others. There’s no way to tell who’s sick and who’s not.
But the efficacy of homemade masks is not scientifically settled. Studies do find that masks can help prevent a sick person from spreading some viruses to others—and may even marginally protect healthy people from becoming ill. “Across these studies, it’s quite consistent that there’s some small effect and there’s no risk associated with wearing masks,” says Allison Aiello, a professor at the University of North Carolina at Chapel Hill Gillings School of Global Public Health.
But this research is on surgical masks: loose-fitting masks designed to protect the wearer from outside virus-containing splashes and droplets, and to catch infected droplets that escape the wearer’s mouth or nose.

Neither these nor N95 respirators—tight-fitting facial devices that filter out small particles from the air—are recommended for the general public due to a shortage for health care workers.

It’s unclear if the research on masks would also apply to homemade face coverings, but Aiello and others believe that physical facial barriers are worth wearing during the pandemic even in the absence of strong evidence. As the authors of an analysis published April 9 in the BMJ put it, “In the face of a pandemic the search for perfect evidence may be the enemy of good policy. As with parachutes for jumping out of aeroplanes, it is time to act without waiting for randomised controlled trial evidence.”
Few studies have tested homemade masks. One published in 2013 found that T-shirt masks were about a third as effective as surgical masks at filtering small infectious particles. That’s “better than nothing,” says study author Anna Davies, a research coordinator at the University of Cambridge, but “there’s so much inherent variability in a homemade mask.” Other research found that homemade masks may actually increase the risk of infection if they’re not washed often enough, since damp fabric can breed pathogens.
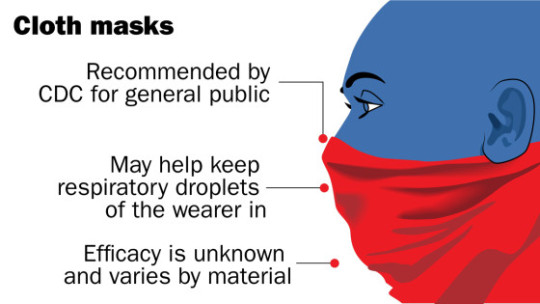
The bottom line is that wearing a mask is probably a sensible move—as long as you clean it often, wash your hands, refrain from touching your face and continue to keep a safe distance from other people. But there’s not robust evidence that the DIY kind will definitely stop you or others from getting sick.—Mandy Oaklander
For more on masks:
Should Healthy People Wear Masks to Prevent Coronavirus?
How to Make a DIY Face Mask
The Ethics of Wearing (or Not Wearing) a Face Mask
Why Wearing a Face Mask Is Encouraged in Asia, but Shunned in the U.S.
Back to the top.
How long does the COVID-19 virus survive on surfaces?

A study published in the New England Journal of Medicine on March 17 found that SARS-CoV-2, the virus that causes COVID-19, could last up to four hours on copper, up to 24 hours on cardboard, and two to three days on plastic and stainless steel. Another study published in The Lancet on April 2 found the virus could last for three hours on printing and tissue paper, and up to one day on treated wood or cloth. It also found that the virus lasted three days on glass and banknotes and six days on stainless steel and plastic—far longer than the New England Journal of Medicine study found. Lastly, The Lancet study also found the virus remained on the outside of a surgical mask for seven days.
However, keep in mind these results were produced in a lab. The virus likely breaks down much more quickly in the environment due to its sensitivity to sunlight and temperature, says Dr. Albert Ko, department chair and professor of epidemiology and medicine at the Yale School of Public Health.
It’s also important to remember that scientists don’t know yet how much of the virus someone has to be exposed to in order to become infected, says Jared Evans, a senior scientist at the Johns Hopkins University Applied Physics Laboratory. While a certain amount of infectious virus could be on a subway pole, it’s unclear if it would be enough to get a person sick.
Still, experts say wiping down objects as they enter your home, including delivery food containers, is a good way to mitigate risk of exposure.—Madeleine Carlisle
Back to the top.
Is there any risk of the COVID-19 virus living on mail & packages?
A study published in the New England Journal of Medicine on March 17 found that SARS-CoV-2, the virus that causes COVID-19, could live up to 24 hours on cardboard. A study published in The Lancet on April 2 found that it could last up to three hours on paper. But keep in mind that the virus will likely break down more quickly outside of a laboratory, due to real-world exposures like sunlight, wind and temperature, experts say.
So yes, there is likely some risk that the virus could be on your mail, but it’s a small one. “A letter that’s been mailed to you and been traveling through the postal service for a couple of days, the virus will be off of that,” says Jared Baeten, professor of global health, medicine and epidemiology at the University of Washington. The risk comes when the carrier handles your mail and brings it to your door, potentially exposing it to the virus again.
The infectious dose of the virus—the amount a person has to be exposed to in order to become infected—is still unknown, says Jared Evans, a senior scientist at Johns Hopkins University Applied Physics Laboratory. So even if the virus is on a package, it might not be enough to get you sick.
Still, out of an abundance of caution, Matthew Freeman, an associate professor of environmental health, epidemiology and global health at Emory University Rollins School of Public Health, recommends opening your package or mail outside your house, disposing of the box or envelope, coming back inside and immediately washing your hands. If you want to be even more thorough, you can also wipe down the contents of a package and then wash your hands again, although it’s quite unlikely the virus will have survived. Crucially, you should make sure to stay at least 6 feet away from the mail carrier at all times.—Madeleine Carlisle
Back to the top.
What should I do to shop safely?
When shopping, the safest thing you can do is stay 6 feet away from other people at all times, experts tell TIME. Be patient. If you see a crowded aisle, wait or come back later. While there’s a chance the virus could be transmitted on a surface, “you’re most likely to get this from another person,” says Dr. Lauren Sauer, an assistant professor of emergency medicine at Johns Hopkins University School of Medicine. Try to shop somewhere that already enforces social distancing, such as making people stand 6 feet apart in line. Also try to go to the store at “off-peak hours” and be respectful of the hours set aside for high-risk individuals. Ordering groceries online can also be a good option, especially if you’re in a high-risk category, experts say.
But if you must go to the store, a spokesperson for the U.S. Centers for Disease Control and Prevention (CDC) recommends cleaning your shopping cart or basket—specifically the handles and other surface areas—with disinfectant wipes. Sauer also recommends using a paper shopping list, rather than your phone, while you’re in the store, because “the less you can touch your personal items in public spaces, the better.”
Once you’ve touched an item in the store, assume your hands may have been contaminated, experts say. Touch as few things as possible and don’t touch your eyes, nose or mouth. Bring hand sanitizer and use it often. You don’t need to wear gloves, because they don’t stop you from spreading the virus to your face. However, the CDC does recommend wearing a non-medical mask to reduce the risk of inadvertently spreading the virus to others.
When you go to pay, try to have as little contact with the cashier as possible. As soon as you can, make sure to wash your hands using soap and water for at least 20 seconds.
The CDC spokesperson says that “[currently] there is no evidence to support transmission of COVID-19 associated with food or food packaging.” Still, if you want to reduce your risk of exposure even more, you can wipe down your groceries when you get home. Make sure to avoid getting hazardous chemicals on food; just wash your fruits and vegetables like you normally would. Once you unload your groceries, the CDC recommends washing your hands again and cleaning kitchen surfaces like countertops, cabinet handles and light switches.—Madeleine Carlisle
Back to the top.
Is there any risk with food delivery services?
The dangers posed by food delivery do seem to be minimal. A spokesperson for the U.S. Centers for Disease Control and Prevention told TIME on March 27 that “[currently] there is no evidence to support transmission of COVID-19 associated with food or food packaging.”
That said, the same precautions you would take for a package delivered to your home should be applied with food deliveries. John Swartzberg, a clinical professor emeritus of infectious diseases and vaccinology at the University of California, Berkeley School of Public Health, recommends first bringing the container inside, washing your hands, wiping the container down with soap and water or a disinfectant, washing your hands again and only then then putting the contents of the the container onto your plate. Also, don’t make the precautions you take a danger by themselves: Make sure to avoid getting cleaning chemicals on anything you eat. He also stressed you should make sure to stay at least 6 feet away from the delivery person, and recommends having them set the food down at the door and leave before you come out and get your delivery.—Madeleine Carlisle
For more on food delivery and shopping:
‘Is Ordering Takeout Unethical?’ A Medical Ethicist Answers
How Can You Safely Grocery Shop in the Time of Coronavirus?
Back to the top.
Should I worry about my clothes after I’ve been outside?
That depends on where you go and whether you’re in contact with other people. Recent studies have found that the virus that causes COVID-19 can live in the air and on different types of surfaces for between four hours and 72 hours. An April 2 study from The Lancet shows that the virus can live on cloth fabric for up to two days; on surfaces like steel or plastic, it can be detected for up to seven days.
That said, it’s unlikely that you’ll get sick from not changing your shirt after returning home from the grocery store, says Dr. Irfan Hafiz, an infectious disease specialist at Northwestern Medicine. You’re more likely to get it through respiratory droplets from another person than contracting it from a surface.
If you are caring for someone who is sick, you should be careful and protect yourself while handling their belongings. “Their personal environment may be more contaminated,” says Hafiz. It’s okay to mix their clothes with your dirty laundry before washing them; just make sure to wear gloves during or wash your hands after doing the laundry.—Mahita Gajanan
Back to the top.
Does rain wash away the COVID-19 virus?
Rain dilutes the virus and can also physically wash it off a surface just like “dirt can wash away,” says Jared Baeten, professor of global health, medicine and epidemiology at the University of Washington. However, experts don’t believe rain deactivates the virus or disinfects surfaces the way soap and water does.
Scientists don’t yet know how much of the virus you have to be exposed to in order to be infected, says Jared Evans, a senior scientist at Johns Hopkins University Applied Physics Laboratory. So it’s unclear whether the already limited impact rain would have on viruses living on the surface of, say, the bannister of your front steps, would make a difference in whether or not the bannister is safe to touch.—Madeleine Carlisle
Back to the top.
Can I get COVID-19 more than once?
News reports out of East Asia have said that some patients in China, Japan and South Korea who were diagnosed with COVID-19 and seemingly recovered then tested positive again days or weeks later. One study—not peer-reviewed—on recovered COVID-19 patients in the southern Chinese city of Shenzhen, found that 38 out of 262, or almost 15% of the patients, tested positive after they were discharged.
However, experts say that these are likely not instances of re-infection. Instead, it’s most likely the case that the post-recovery positive tests simply found lingering infections that were not detected by earlier tests. A positive test after recovery could be detecting the residual viral RNA that has remained in the body, but not in high enough amounts to cause disease, says Vineet Menachery, a virologist at the University of Texas Medical Branch.
Experts say the body’s antibody response, triggered by the onset of a virus, means it is unlikely that patients who have recovered from COVID-19 can get re-infected so soon after contracting the virus, suggesting at least short-term immunity, though as with so much about COVID-19, this is not yet settled science, but rather the best current guess. Menachery estimates that COVID-19 antibodies will remain in a patient’s system for “two to three years,” based on what’s known about other coronaviruses. (One Taiwanese study on the 2003 outbreak of SARS, which is caused by a virus that is similar to the one that causes COVID-19, found that survivors had antibodies that lasted for up to three years.)
“We would expect that if you have antibodies that neutralize the virus, you will have immunity,” Menachery says. “How long the antibodies last is still in question.”—Hillary Leung
Back to the top.
If I get COVID-19 and recover, am I immune and safe to be around/help out older family and neighbors?
The messages are mixed on this one. The U.S. Centers for Disease Control and Prevention (CDC) guidelines for COVID-19 patients who have recovered clears them to break quarantine if all of the following conditions have been met:
they have had no fever for at least 72 hours without the aid of fever-reducing medications
all other symptoms like coughing and shortness of breath have cleared up completely
at least seven days have passed since they first became symptomatic
if a coronavirus test is available, they should have also had two negative tests 24 hours apart
(The full CDC guidelines are here.)
But the science is still unsettled on whether recovering from the virus confers immunity. As TIME has reported, there have been cases in Japan, China and South Korea in which patients who seemingly recovered were readmitted to the hospital with a COVID-19 relapse. Some of these presumably recovered patients tested positive again, but it is unclear whether they were actually reinfected or if apparently negative tests simply failed to detect low, lingering levels of the virus. Until more is known with certainty, it is thus best for recovered patients to continue avoiding elderly people or other numbers of susceptible groups.—Jeffrey Kluger
I’ve been social distancing for two weeks. When is it safe for me to go see family?
No one knows exactly how long it will take, but experts say not yet, at least in the U.S.
As of April 13, forty-two states and the District of Columbia (covering about 97% of the U.S. population) had imposed shutdowns and stay-at-home guidelines. Millions of Americans have been social distancing since mid-March, and, as of early April, the national infection curve has not yet flattened. The rules on social distancing are, for now, open-ended, with policies likely to remain in place in one form or another for months, not weeks or days.—Jeffrey Kluger
Back to the top.
Can my dog or cat get COVID-19?
At the moment, it appears there’s little-to-no risk of pets transmitting the virus to humans, with no specific evidence showing this type of transmission has ever happened. Globally, only two dogs and two cats have tested positive for the virus, according to the American Veterinary Medical Association (AVMA). In the U.S., there hasn’t been a single case of a pet diagnosed with the virus, at least according to the country’s Centers for Disease Control and Prevention (CDC). “That’s why in the U.S. we’re really not pushing hard to test pets at all,” says William Sander, assistant professor of preventive medicine and public health at the University of Illinois’ College of Veterinary Medicine.
A tiger at the Bronx Zoo tested positive for SARS-CoV-2, the virus that causes COVID-19 in humans, but, says Karen Terio, chief of the Zoological Pathology Program at the University of Illinois’ College of Veterinary Medicine, “A tiger is not a domestic cat, they are a completely different species of cats. To date we have no evidence of the virus being transmitted from a pet to their owners. It’s much, much more likely that an owner could potentially transmit it to their pet.”
Terio adds that there is still much that is unknown. If your pet, for example, did contract the virus, it is not clear whether signs of infection would show themselves in the way they do in humans. Out of caution, the CDC and AVMA recommend that sick humans stay away from their animal companions. “Just like you’re keeping your distance from other people, try to have somebody else in your house take care of your pet, just to be overly cautious,” Sander says. If you are sick or showing symptoms and you have to take care of your pet, the CDC recommends avoiding snuggles or touching your pet, and washing your hands thoroughly before and after feeding.—Jasmine Aguilera
Back to the top.
Can the COVID-19 virus live on my pet’s fur?
Studies have shown that SARS-CoV-2, the virus that causes COVID-19, can live on a variety of surfaces for several hours or days. But none have tested dog or cat fur.
In an email to TIME, the American Veterinary Medical Association stated that while the virus can be transmitted by touching a contaminated surface or object and then touching your nose, mouth or eyes, “this appears to be a secondary route. In addition, smooth, non-porous surfaces such as countertops and doorknobs transmit viruses better than porous materials; because your pet’s hair is porous and also fibrous, it is very unlikely that you would contract COVID-19 by petting or playing with your pet. However, it’s always a good idea to practice good hygiene around animals, including washing your hands before and after interacting with them.”—Jasmine Aguilera
Back to the top.
Do flies, mosquitoes, or other insects carry or transmit the virus?
Short answer: no, you cannot get COVID-19 though insect bites. “There are viruses that are transmitted by mosquitoes; this is not one of those,” says Karen Terio, chief of the Zoological Pathology Program at the University of Illinois’ College of Veterinary Medicine.
William Sander, assistant professor of preventive medicine and public health at the University of Illinois’ College of Veterinary Medicine, adds that previous studies of other types of coronaviruses determined that insects are not a viable mode of transmission.
According to the U.S. Centers for Disease Control and Prevention, SARS-CoV-2, the virus that causes COVID-19 disease, is primarily spread from person to person by coming in contact with an infected individual’s respiratory droplets, for example saliva or mucus.—Jasmine Aguilera
Back to the top.
Can cleaning products kill the COVID-19 virus?
Probably, as long as you use them right. Household cleaning products designed to fight viruses—i.e., not those labeled exclusively “antibacterial”—typically work against known coronaviruses, like strains that cause the common cold. So while most household products haven’t been tested specifically against the novel coronavirus strain that causes COVID-19, it’s safe to assume standard wipes and sprays will work pretty well against it, says Dr. Aaron Glatt, chief of infectious disease at Mount Sinai South Nassau in New York.
But cleaning properly takes a little patience. “Some of these [products] don’t work by contact,” Glatt says. “They work by being on the surface for a while and drying via air.” For peak efficacy, use enough of a product to leave a surface wet for up to several minutes, then let it dry on its own. Read each product’s label to make sure you’re using enough.
Don’t feel like you need to clean your home obsessively, though; if you’re social-distancing properly and washing your hands often, you don’t need to deep clean all the time, experts say. Regular upkeep, and periodically wiping down high-touch objects like light switches and doorknobs, should keep your home sufficiently clean.—Jamie Ducharme
Back to the top.
Does it matter what type of soap I use to wash my hands?

Probably not. Any kind of soap, used properly with water for the recommended 20 seconds of handwashing, will work to remove SARS-CoV-2, the virus that causes COVID-19, from your hands. And since we’re dealing with a virus, antibacterial soap doesn’t do anything extra to help.
Soap has a hydrophobic end (meaning it repels and doesn’t mix with water) that binds with oils, and breaks down the oily lipid molecules that make up the membrane of SARS-CoV-2, according to Dr. Mary Stevenson, an assistant professor of dermatology at NYU Langone Health. The virus breaks apart and becomes trapped in the soap bubbles, which wash away in the water.
Stevenson recommends washing your hands in lukewarm water. Extremely hot water is more likely to harm your skin, and doesn’t do anything extra to kill the virus. A lukewarm temperature will keep your hands comfortable and strip away less moisture. Once you’re done washing, it is important to dry your hands on a clean towel. Cloth or paper towels both work well; if you’re at home, Stevenson advises keeping a rotation of clean hand towels that are traded out and washed at least once a day to avoid wasting disposable towels. If you’re washing your hands in a public restroom, use a clean and dry paper towel.—Mahita Gajanan
Back to the top.
What’s the safest way to do laundry in a shared/public laundry room?
If you’re not ill, continue doing your laundry as you normally would. For some people, that means taking loads of dirty clothes to a laundromat or shared laundry room, leading to potential exposure to the coronavirus or the risk of infecting others.
In these situations, stick with your typical laundry routine but also be sure to follow guidelines from the U.S. Centers for Disease Control and Prevention (CDC) to prevent the spread of COVID-19: keep a distance of at least six feet from others in the laundry facility, wash your hands after touching any surfaces, and wear a cloth face mask. When doing your laundry, avoid shaking out your dirty clothes; if your clothes do have any of the virus on them, shaking them could disperse the virus into the air.
If you’re taking care of someone who is sick, it’s safe to mix their dirty clothing with yours before washing, per the CDC; just make sure to wear gloves or immediately wash your hands with soap after handling the laundry.
Ideally, you can drop your laundry into the washer and leave the facility (like go for a walk or wait in your car) until your clothes are ready to go into the dryer, says Dr. Irfan Hafiz, an infectious disease specialist at Northwestern Medicine. Be sure to dry your clothes thoroughly; the heat from the hot water and dryer should “clear off any of the virus that’s there,” says Hafiz.
And once your clothes are dry, fold them at home; avoid using communal folding tables in shared spaces since you don’t know if dirty clothes have been on those surfaces previously.
The CDC also advises that people clean and disinfect their clothing hampers, or to place a disposable bag liner in the laundry baskets to further prevent the spread of COVID-19.—Mahita Gajanan
Back to the top.
via https://cutslicedanddiced.wordpress.com/2018/01/24/how-to-prevent-food-from-going-to-waste
0 notes
Text

I am already up and it is actually early. Vie, isn’t that what you wanted. Mmmmmhm. I feel a little sickly 🤒. I took some Advil 💊 last night. It’s like I am hot 🥵 like fever malaise. I didn’t want to be under the weather ☁️ I am erring more on feeling fine versus 🆚 yeah, the cold virus 🦠 is actually staying in your bod and it has been creating tiny havocs on your system. It doesn’t know that your work outs 🏃🏼♀️ 💪🏾 are exhausting 😩. But it just does what it does and it wins when you don’t allow yourself to rest and recover. I don’t find it frustrating that my training 👟 is interrupted by bouts of partial illness. I also protect myself in a regard that even if I am not bed 🛌 stuck, I call the entire thing off under the idea 💡 that if you don’t contain this infection, it shall be worse. I am actually lazy yesterday. You are allowed to put your feet up and not do anything. I didn’t feel that I am wasting my life 😏. Yet I didn’t also feel that I am going somewhere and to me that is important ⚠️. I feel that most of people’s problem is that they get bogged down in that indecision. I mean, it’s not that simple. You have feelings, social pressures, how you process and really it’s a tough call. Ugh 😑, Vie is always calling it as it is “without difficulty” getting there, sticks by it and continues. It’s as complicated as getting rid of a cold 🤧 germs in molecular and physiological systems. I am doing what I can. I am sleeping 💤 earlier, I am disinfecting, I am being clean 🧼 like washing my hand 🖐🏾 esp when handling food 🥘, I bundle up 🧣 🧤, I am boosting my immunity. Here’s the clincher. You have to pinpoint exactly what’s going on in your body and institute therapy that promotes healing like duh 🙄. Yes, I need recovery and tons of rest as there is inflammation and tiny muscle tears in me physically. Rest, rest, rest. I feel like I should do what I feel like. Do what is astute. Others might not see that. Others however notice what is exceptional.
I asked Google mini what time it was. I finally decided to get up 🛏 and whoa whoa 😳 whoa it’s nine thirty 🕤 already. I lingered in the sack for that long. Yes, the second hand is 🕰 inching faster 💨 than what my brain 🧠 thinks or better word perceives it does. What are your list of things 📝 in task master? My cats 🐈 🐈 🐈 have been letting out noise to “speak” to me. I said hi 👋🏾 to them. I haven’t hugged 🤗 them but I have been kissing 😚 Wawames. He’s always following me. Yeah, I was very not cohesive in my day’s plans 🖊 . Today however it shall be different. What was my thing yesterday. I was listening 👂🏾 to American Constitution lecture 💻 yesterday. After two 10 minutes clip I told my BFF I should and could nap 💤 now. It is essential to be not sick and do the things I do in the studio and health club floor. I took an introductory in Political Science. So it is not like foreign. But Professor Roosevelt is so interesting 🤔. He is lecturing on what’s not obvious. I love ❤️ it. My Dad is early to work today 👨🏻🔧 and gave me a pat in the back well not literally praised me for taking care of my dirty dishes 🍽. I have been putting it off and doing it when I have the time and yesterday, after waking up from my just an hour snooze 😴 time, I wasn’t feeling well at all. However, between the Advil 💊 and antioxidants, I have to make sure I do this chore before I call it a very early day. He goes and he is right, you should spend little times of your day to do it so it doesn’t pile up. He is correct. I agree with him. He is teaching something great. Does it mean I am going to do it? No. Why? I have a mind of my own.
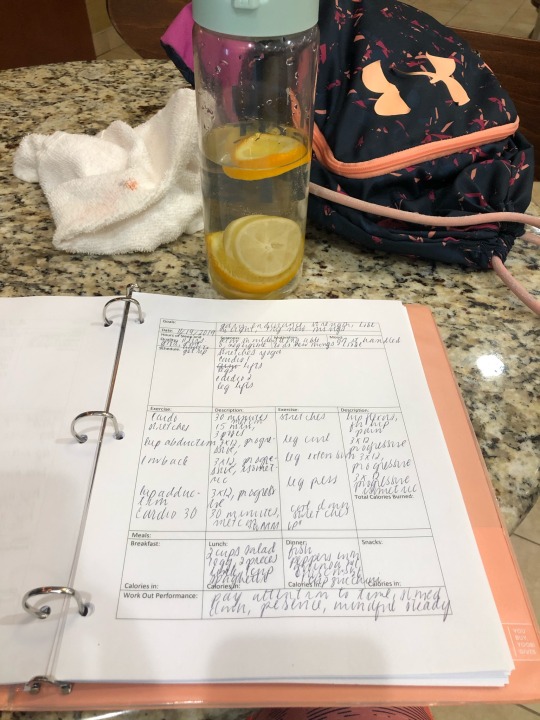

What was my day like Tuesday 📆? I didn’t think 🤔 I would remember a lot but taking pictures 📸 jogs your memory. I love 💕 that connection. It makes your life so much meaningful. So taking random shots is actually good for your heart ❤️ too. The ACTUAL Vie wouldn’t give that time of the day. But she is making herself do it because life is beautiful if you care to see it as it is and not if you are like me acting on it constantly and moving, moving, moving. Vie, you are like where all action come from. I didn’t expect it to be. It’s kind of sad 😢 not for me. I have to take care of the people around me too. I am an expert on this and I actually have the final say on what gets life and what whithers. I must I realize not not carry others with me and not be neglectful and build a relationship. I have to make sure that how I view things is not my own inclination, tendencies and strengths. I have to see how those who love 💗 me carry on. In a better less wordy sense, team work. You don’t live in a vacuum. My success is not my personal own. It ensures that those precious people who I give my love 😍 and devotion also are able to surpass life so inordinarily thrusts upon them. They don’t end up infantile criminal druggies alcohol dependent as if that’s not embarrassing. They have to do their work and I meet them there too. You think 💭 I am strong 💪🏾 because I am. In a way, for good and bad, I have a supportive father and strategic mother.
What I am trying to say is I look 👀 at the pictures and I am back to the place. I remember seeing Laura in the front desk, the old man 👴🏻 who sat on the bigger chair, another member who left his empty water 💦 bottle next to me, the Spa 🧖🏼♀️ Life receptionist, Keya wearing red child center shirt 👚 etc. I have been starting late and I love ❤️ it because I am actually doing things not just for myself. I’m helping others make an impression of the world 🌎 as I see it. Here’s a big point, how I see it doesn’t mean they agree. Like any men and women who reason, you get to form your own opinions and knowing me I am not going to press what I believe on how you think 💭. I am just “vocal” and I’ll challenge how you determine things for yourself. It might sound crazy 😜 but it is not as sinister as sensationally getting you suck in on my agenda and forcefully and without boundaries make obvious fearful 😧 threats to absolutely you having to agree side with me. See the difference. You like me for what I am and not what I feed on you so you can see I am like the better person and I am using you and your resources 👏🏾.
I didn’t do exactly as I had penly 🖊 scheduled 🗓 it. BTW, in my dreams this morning I was trying to outsmart bad guys and I was shopping 🛒 for planners 📓. I am sure that subconscious has real life basis. How to Interpet dreams I think 💭 by Carl Jung. I also want to add that I know some monarch are mad like they have lost their touch to reason and see things as they actually are. Bizarre things. Well, you have to see that there are extreme pressures out on them and really if you think 🤔 about it they really live apart and process things different. They are rulers. Although I feel that when Kings have a dream and they act on it like some divine prophecy similarly they have Seers right who have premonition guess what? I feel that is your brain firing 💥 up making conscious real life events. It makes you feel what you give value to tremendously and what’s happening around you. Is it rational to follow your dreams? It is sensical and intuitive. My take is you have to be a strong intellect. Why am I talking about the unconscious? Ah, what I had detaily want to do versus 🆚 what was done ✅. I paid attention to what Lindsey said in personal training. She was great. She is a baby 👶🏻 to her expert coworkers but she is not like she is not strong about her knowledge based. Just remember that work is more than what you know. It is finding the right fit. Navigate the social, political, cultural and business terrain 🗺 ⛰. She is in the Cleveland Clinic of gyms. She says weight lift 🏋🏼♀️ first before cardio ♥️. It has something to do with taxing your muscles 💪🏾 🦵🏾. I did. What was I working on? Legs. I also made a deliberate decision 🤨 to start late and not go toe to toe on rush hour gym 🏃🏼♀️ 💪🏾 time. More exposure to bacteria 🧫 and viruses. It’s not that busy lately. I feel that most people are sick 🤕. I think 💭 Thanksgiving 🦃 is coming up. I was ill last year. Was I? I should celebrate. Black Friday. Oooh 😯, right, I have to see what’s their deal 🏷 at Abercrombie 🛍. I said hi 👋🏾 to Katie. I was keeping to myself this day because I yoga 🧘🏼♀️ stretched to begin in the studio listening 🎧 to news 🗞 and you have to realize I was sitting there for an hour ⏲ doing serious work. We talked about the weather and mood. Usually, I am gabby superfluous. I tried to keep my mouth shut 🤐. More processing, less socializing if you must help it. At thirty minutes my left hips was hurting at GTX station. I remem from magazine that if something is painful 😣 stop 🛑 right away. I observed it a little bit more. I have to be nice to my body and did hip flexor stuff. I wanted 90 minute ⏱ cardio.
I filled out my worksheet completely ✍🏾 and I love 💕 my own subjective take on the stuff I did. It might be neglible even if the psych grad 👩🏼🎓 in me knows it is greatly not just for productivity 📊📈📉 and keeping tabs, it’s work miracles for processing things that happened and what needs to improved, continued and see little nuggets of refined methods. I loved 💗 Dance Jams 💃🏼. I was jumping. Ayayay. But I noticed working on my legs and having that woman 👩🏼 attitude, enjoying 😊 what I do and learning new moves 👣. I am so happy 😀 cool down. Angie is super. Mariah Carey for stretches 🙆🏼♀️. What could go wrong 🎊 ?
youtube
0 notes
Text
ABRAHAM LINCOLN.....A WARNING FROM THE PAST
Lincoln’s words of wisdom went far beyond the Gettysburg Address and Emancipation Proclamation.
Following are additional words he uttered more than 150 years ago. Words spoken back then giving warning to today’s Americans. It is as if Lincoln knew his words would be needed: “America will never be destroyed from the outside. If we falter and lose our freedoms, it will be because we destroyed ourselves.”
Welcome August!
August is National Breastfeeding Month.
Breastfeeding was the way babies in William Hackley’s 1855 were fed. If the mother’s milk was foul or such that the baby could not tolerate it, bad repercussions occurred. As we have been reading in Hackley’s diary.
If good fortune prevailed, a mother who had a super abundance of milk or had lost her child might be available. I am assuming the Mrs. Hews Hackley writes about is such a woman.
He reports in today’s entry: “Sent the baby to Mrs. Hews to get some milk.”
Having experienced Irma, I am skiddish every time a hurricane is reported which might hit the Keys.
Isaias made me nervous for 24 hours. Though still far away, its cone ran right over Key West. Similar to Irma’s cone.
Fortunately for the Keys, Isaias turned east. It will completely miss south Florida. Landfall is expected in the Palm Beach area. Following which it will run off and on the eastern seaboard. On wednesday, it is projected to be over Boston.
Coronavirus will compound the impact of any hurricane that hits. How are people to be protected? Shelters are of no use. People packed in. The virus will have a field day moving from one person to another.
Florida announced it is not opening any shelters for Isaias. First time I can recall no shelters being open. And I go back 25-30 years.
Coronavirus deaths for 7/31/20 in the U.S. were reported at 1,465. Means one American was killed every 58.9 seconds.
There are well more than 1 million pythons in the Everglades and northern Florida. Could be 2 or 3 million or more. No one knows for sure.
What is known is that there are now so many that they are impossible to eradicate. Florida hopes to be able to control their growth, however.
Hurricane Andrew is blamed for the large number of pythons in existence today. Many people kept pythons as pets. Andrew took down whole blocks of homes. To ground level. The python pets took a trip through the air and settled in wherever they landed.
Sexual beings. They propagated.
Florida failed to pay timely attention.
Every so often, Florida comes up with a new approach to the problem. Never one that will work to totally eliminate. Rather will that will merely diminish.
The Florida Fish and Wildlife Conservation Commission and the South Florida Water Management District came up with a new idea.
They have asked people living in the areas where pythons exist to call either agency immediately and report the sighting. As well as the location. State workers then go out to kill the python reported.
Best program yet! It has been reported that 5,000 pythons were killed this past year. A huge number! The largest ever!
However a drop of water in the ocean, a grain of sand on a beach. Too little too late. When talk is in the millions, 5,000 is non consequential.
While Floridians are worried about coronavirus (and hurricanes and pythons), dengue fever has returned. Just as deadly as coronavirus. Except infects substantially fewer persons.
Infection carried by mosquitoes. The problem has been under control. However every few years, the fever returns.
Twelve cases alone reported for the month of July. A huge number for the disease. All 12 cases reported in the Key Largo area where several had been reported prior to July 1.
Trump consistently makes the wrong move where the health and welfare of the U.S. and other parts of the world are at stake. Not where Putin is concerned, however.
Trump announced he is pulling 12,000 troops out of Germany. That number have been stationed there for more years than I can recall.
Part of a NATO supplement. Stationed in Germany to protect former Soviet Union countries.
Putin wants NATO destroyed. Its sole purpose is to protect Europe from Russian aggression. Putin is happy the 12,000 troops are being pulled out of Germany. Less for him to worry about if he pulls another Crimea situation.
Trump says he is doing it because Germany fails to meet its NATO contribution. Also, Trump hates Angela Merkel. A woman who has consistently stood strong against him.
All lies. The real reason Trump is doing it is to accommodate Putin.
Mail in ballots are in the works already this month in Florida. A “local election” is scheduled for August 18.
The Supervisor of Election reported 18,051 by mail ballots have been sent to persons who requested them. So far, 5,609 have been returned.
I asked for mail in ballots. I have received the local election one and plan to mail it back today. I am also listed for a mail in ballot for the November 3 election.
The Supervisor announced 19,529 persons have already requested mail in ballots for the November 3 election.
The preceding numbers apply only to Monroe County.
Last night was most enjoyable. Cocktails at 7. My socialization for the week. It helps.
Enjoy your day!
ABRAHAM LINCOLN…..A WARNING FROM THE PAST was originally published on Key West Lou
0 notes
Text
Some coronavirus clients with mild cases report symptoms for a month
Some say their households and coworkers are skeptical of their lingering health problem.
All 4 patients stated they expected to be recuperated within two weeks, based on CDC assistance.
But physicians aren’t sure how long coronavirus signs normally last, indicating patients can’t plan for life post-recovery.
When Lauren Nichols felt a dry, burning experience in her throat, her first instinct was to laugh it off.
” I joked at the start that I was a baby dragon in the making and I was going to be on ‘Games of Thrones,'” she stated.
A couple of hours later on, she established diarrhea. The next day, she had a low-grade fever, accompanied by body pains and pounding headaches. A week and a half later, Nichols started feeling brief of breath. Just climbing up an action ladder made her winded.
” I normally perambulate 5 to 6 miles a day and I’m really active, very healthy,” she said. “That was sort of my wake up call that this isn’t regular. There’s something going on.”
Nichols, who is 32 years of ages, got evaluated for the coronavirus on March 17 in Boston, Massachusetts, where she lives. Her test was favorable, but her symptoms still have not disappeared: Friday was day 51 of her health problem.
Nichols is still recovering in your home. Not a day has passed in which she didn’t have diarrhea. Her cravings has actually disappeared, she sweats and shivers through the night, and there’s a rattling in her chest. Her second coronavirus test came back positive once again on April 20.
She is one of a growing variety of young coronavirus patients with mild or moderate cases who have actually reported being sick for more than a month.
3 other clients under 40 offered Organisation Insider similar accounts of their health problems. That opposes guidance from the US Centers for Disease Control and Avoidance, which has actually suggested that mild coronavirus symptoms normally last for 14 days For severe or vital patients, the World Health Organization reports, recovery can last as much as 6 weeks.
However the minimal nature of information about patients in healing up until now means we don’t have much info about the length of time symptoms typically last. In clinical studies, clients who are thought about “recovered” are normally those who have actually been released from the medical facility Since mild cases are motivated to stay home, they’re less most likely to be reflected in that research study.
” We’re certainly seeing people whose symptoms last longer than two weeks,” Dr. Nate Favini, the medical lead at Forward, a primary-care practice that’s collecting information on coronavirus patients around the country, informed Service Insider. Favini deals with coronavirus patients in San Francisco.
He stated the CDC has actually been “extremely slow to upgrade their guidance on symptoms.”
” It’s hard to say what percent of people have signs that last beyond 2 weeks, however we’re certainly observing that as a not-uncommon phenomenon,” he stated. “The infection causes all type of swelling and dysregulation in your body and it can take even longer, after you’ve cleared the virus, for all of those things to go back to normal.”
Working through the discomfort
Nichols stated her symptoms reached their peak strength about a week into her health problem.
” I had minutes of outright horror,” she stated. “I was getting up in the middle of the night gasping for air. I had to prop my direct on four pillows just to get myself to be able to breathe.”
She discussed going to the emergency room, but said the concept wrecked her with regret.
” It was this internal battle of, ‘I seem like I need to go to the health center, but I don’t want to take a healthcare facility bed since I can still breathe, but I likewise do not want to pass away in your home,'” she stated.
Throughout her illness, Nichols has actually been working from house, managing a global program for the Department of Transport.
Crystal Cox/Business Insider.
She tries to maintain a cheerful personality when on the phone, however her days are frequently interrupted by the requirement to sit on the toilet for numerous hours. Friends and family have a hard time believing she’s still ill, she said.
” Individuals just don’t comprehend when they’re not a patient for how long signs can last,” she stated. “Everyone, my coworkers included, are attempting to hurry the healing when I don’t require that pressure.”
Caroline, a 27- year-old resident of Houston, Texas, has actually had signs for 48 days, and informed Business Expert she’s also attempting to work through the pain. (Her last name has actually been omitted to protect her personal privacy.) Caroline said she still struggles with tiredness and feels an urge to sleep 18 hours a day. However her work as a corporate lawyer makes that impossible.
” I’m just downing energy drinks to attempt and stay awake, which is never what I should not be doing,” she said. “It’s simply type of awkward to have to inform work, ‘Hey, I understand I got sick 5 weeks back, but I’m still feeling bad.'”
Caroline’s signs began March 15, when she got a fever after going to a bachelorette celebration in Charleston, South Carolina. The participants consisted of four women from Manhattan, which has actually ended up being a center of the US’s coronavirus epidemic During the celebratory weekend, the bride-to-be found out that her granny had died of COVID-19
Caroline evaluated positive for the virus eight days after returning house. She had a cough, felt brief of breath, and lost her sense of odor.
Crystal Cox/Business Insider.
Caroline said she recently told a partner at her company that she might be sluggish to react to email since of her health problem. He suggested she may just be run-down from a couple years of working long hours.
Kite_rin/ Shutterstock.
Kelsey Meeks, a 36- year-old attorney who lives outside New Orleans, Louisiana, said that throughout her worst bout of signs, things seemed to change minute by minute.
” Every day I would resemble, ‘I can breathe right now, but in five minutes am I going to be okay?'” she informed Company Expert. “It was actually scary– just that anticipation of not knowing which method the coin was going to turn.”
Meeks has actually felt sick because March30 Friday significant day 32 of her health problem. Her main symptoms now include body pains, headaches, and nasal blockage. She previously lost her sense of taste and smell for about two weeks, and likewise experienced a pressure in her chest, as if “wearing a gown that is too tight.” She had dreams that she was undersea, then awakened gasping for air.
” I have not had a day where I woke up and I believed, ‘Oh, I’m over this,'” she told Business Expert. “I can have a much better day and then the next day I can’t walk and talk at the very same time.”
Meeks said 5 of her family members checked favorable for COVID-19, but on the entire their signs have actually been milder and fixed rapidly.
” It was difficult to comprehend why I wasn’t getting better as quick as they did,” she said. “There doesn’t appear to be a rhyme or factor.”
Kelsey Meeks running the Dopey Obstacle, 48.6 miles over 4 consecutive days, at Disney World in January2020
Kelsey Meeks.
Meeks, too, is still attempting to work from home.
” Once or twice a day, I’ll strike what I call a tiredness wall, which is where I can’t do anything. I need to go to sleep right away,” she stated. “It resembles the worn out where you simply don’t care about anything else.”
She’s worried about her task efficiency.
” I do struggle with the regret about it and seeming like a failure,” she said. “I’m getting to the point where my brain’s functioning enough that I’m understanding, wow, I really have actually lost a great deal of time over the last three-and-a-half weeks.”
Even patients who recuperate and check negative can have remaining signs
Favini said it’s prematurely to forecast how long signs will last for common clients.
Amongst clients who have actually experienced extreme coronavirus problems like pneumonia, acute respiratory distress syndrome, or strokes, the virus could produce long lasting organ damage. The coronavirus can likewise result in blood clots in the lungs that do not show up on a routine CT scan. Favini said that could trigger continuous shortness of breath.
Lately, he included, he has seen coronavirus clients with persistent coughs and diarrhea.
Signs beyond two weeks could be the result of a continuous viral infection, Favini added, but they might likewise be caused by secondary impacts of the infection, like consistent swelling.
That’s what occurred to Dio Cruz, who evaluated positive for the coronavirus on March 31.
” I had this eye discomfort that was in both eyes, but it was more noticable in my right eye,” Cruz stated.
Cruz has heart disease, so he’s typically short of breath, but he also established diarrhea, loss of taste and smell, and a fever that lasted one night. Prior to getting ill, Cruz had been awaiting a heart transplant. To get back on the list, he had to show that he no longer had an active infection. His second test came back negative on April15 But four days after that, he started having eye pain and diarrhea again.
” If you have not gone through it yourself, you may find it hard to think,” Meeks stated. “How are you OK this day, however the next day you can’t complete a sentence without needing to gasp for air? Why are your lungs burning, but your X-rays are clear? In regular times you would think, ‘Is this person a hypochondriac?'”
Preparing for the worst
All 4 clients informed Company Insider that they ‘d expected their signs to last for 14 days.
” The way that I comprehended this and the way that it was offered– I think a great deal of individuals misinterpreted– however it resembled, ‘Oh, this is two weeks and you’re done. And if you’ve made it to day number eight or nine and you are not hospitalized, you’re probably out of the woods.’ Which’s bullshit,” Cruz stated.
” It was a very lonely experience for me,” she stated.
Nichols hiking before she got ill.
Lauren Nichols.
Cruz stated he does not consider himself recovered.
” How can I be recovered when I’m still having some symptoms?” he said, including, “There’s no closure. I have actually kind of made peace with that.”
Favini said there are two milestones for clients– clearing the virus and getting rid of signs– but both lack a concrete timeline.
” Healing actually needs to depend upon an individual feeling back to normal,” he stated. “For a few of these folks with strokes, that damage is permanent and they might not have complete recovery.”
Cruz and the other patients fret that the virus has actually done long lasting damage to their health. Meeks isn’t sure whether she’ll ever totally restore her sense of taste and odor. Nichols is stressed over permanent lung injury. They’re all trying to temper expectations to reduce disappointment and disappointment in the absence of concrete medical assistance.
” It’s just tough to prepare your life at all when you are still feeling under the weather and you simply do not know how long that’s going to last,” Caroline stated. “I’m not attempting to get my hopes up that this will be over at any point.”
All four patients said they hope the general public pertains to much better comprehend that cases can last for a while.
” I have actually never been ill this long in my life,” Meeks said. “The entire world is going to have to be patient with those people who have actually had this while we navigate what is still occurring inside our bodies.”
Loading Something is loading.
%%.
from Job Search Tips https://jobsearchtips.net/some-coronavirus-clients-with-mild-cases-report-symptoms-for-a-month/
0 notes
Text
I’m Pregnant. How can I Protect Myself against COVID-19?
PREGNANCY AND CORONA VIRUS
As we all know, this is a tense situation for all of us. COVID-19 has spread all over the world. Pregnancy can sometimes be an uncertain and stressful period in the best of circumstances. But during a pandemic, that anxiety can quickly multiply.
As an assisted reproductive doctor, I feel that it is my duty to offer some advice for all the pregnant women out there, eagerly waiting to bring a bundle of joy into this world. That's why I am sharing this video with you. It would be a question for every pregnant woman if COVID-19 would affect the baby in the womb. Expectant mothers are always looking out to keep their babies healthy. But at the moment, our knowledge about this form of coronavirus, which can lead to COVID-19 infection, is still in its infancy.
COVID-19 virus is a new virus. 'Vertical transmission' of any infection occurs when the infection is passed from a mother to her unborn baby through the placenta. To date, several studies have been carried out and they all suggest no evidence of vertical transmission which can be a huge relief for mothers-to-be. There is also no evidence that the virus can pass to your baby while you are pregnant or during birth.
Given that this is a novel virus, little is known about its impact on pregnant women. During pregnancy, a woman's immune system is weakened making her susceptible to infections. We do not yet know enough about how the COVID-19 affects pregnancy to draw any definite conclusions. While the data is currently limited, it is reassuring that there is no evidence that the virus can pass to a baby during pregnancy. But we do advise extra precautions for women who are expecting.
Please follow these preventive measures:
• Practice social distancing• Avoid touching your face• Keep surfaces clean• Wear a mask• Drink hot water every 15 minutes• Wash hands regularly• Use hand sanitizer
Efforts are being made to prevent the COVID-19 germ spread. Let us hope that we find a cure soon. However, if you develop symptoms that are consistent with coronavirus - a persistent dry cough or a high temperature - you must self-isolate and speak with your doctor. It pays to be prepared, not scared. Simple steps like thorough hand washing and limiting your time in crowds can go a long way in protecting you and your baby.
COVID-19 – ALL YOU NEED TO KNOW
We know this is a stressful time and people want to know what they can do right now to protect themselves and their families. That’s why Prashanth Fertility is highlighting some everyday steps that people can take now. In addition, stay informed about what’s happening in your local community and always follow the directions of state and local authorities.
SYMPTOMS OF CORONA VIRUS (COVID-19)
COVID-19 symptoms include fever, tiredness, aches & pains, sore throat, shortness of breath, and dry cough. Very few people might experience diarrhea, nausea, or a runny nose. Symptoms may appear 2-14 days after exposure. Call your doctor for medical advice if you think you have been exposed to COVID-19 and develop any of these symptoms.
LIMIT THE SPREAD OF GERMS AND PREVENT INFECTION
We recommend the following steps to help prevent the spread of germs.
• Stay home• Avoid gatherings of more than 10 people• Practice social distancing by keeping a distance of about six feet from others if you must go out in public• Wash your hands often with soap and water for at least 20 seconds, especially after being in a public place, or after blowing your nose, coughing or sneezing• Use a hand sanitizer with at least 60% alcohol• Avoid touching your eyes, nose, or mouth• Avoid close contact with people who are sick• Cover your nose and mouth with a tissue when coughing or sneezing; throw used tissues in the trash. If a tissue isn’t available, cough or sneeze into your elbow or sleeve, not your hands• Clean and disinfect frequently touched surfaces daily• It includes tables, doorknobs, light switches, handles, desks, computers, phones, keyboards, sinks, toilets, faucets, countertops, and more• If surfaces are dirty, clean them - use detergent or soap and water prior to disinfection• Wear a facemask if you are sick. You should wear a facemask when you are around other people (e.g., sharing a room or vehicle) and before you enter a healthcare provider's office• When you go out in public, keep away from others who are sick• Limit close contact and wash your hands often• People with mild symptoms who are otherwise healthy should self-isolate
EXTRA PRECAUTIONS YOU CAN TAKE:
• Stock up on supplies• Refrain from smoking and other activities that weaken the lungs• Contact your healthcare provider to ask about obtaining extra necessary medications to have on hand in case there is an outbreak of COVID-19 in your community and you need to stay home for a prolonged period of time• Be sure you have over-the-counter medicines and medical supplies (tissues, masks, hand sanitizers, etc.)• Have enough household items and groceries on hand so that you will be prepared to stay at home
WHO IS AT A HIGHER RISK?
Early information shows that some people are at a higher risk of getting infected from this virus. This includes older adults and people who have serious chronic medical conditions like heart disease, diabetes, and lung disease. If you are at higher risk for serious illness from COVID-19 because of your age or a serious medical condition, it is extra important for you to take action to avoid getting sick.
FAQS ON CORONAVIRUS (COVID-19)
WHAT IS CORONAVIRUS?
Coronavirus is a large family of viruses that may cause illness in animals and humans. In humans, Coronavirus causes various respiratory infections ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS). The most recently discovered Coronavirus causes Coronavirus disease COVID-19.
WHAT IS COVID-19?
COVID-19 is an infectious disease caused by the most recently discovered Coronavirus. This new virus and disease were unknown before the outbreak began in Wuhan, China, in December 2019 as per the reports.
WHAT ARE THE SYMPTOMS OF COVID-19?
The most common symptoms of COVID-19 are fever, tiredness, and dry cough. Some patients may have aches and pains, nasal congestion, runny nose, sore throat or diarrhea. These symptoms are usually mild and begin gradually. Some people become infected but don’t develop any symptoms and don’t feel unwell. Most people (about 80%) recover from the disease without needing any special treatment. Around 1 out of every 6 people who get COVID-19 becomes seriously ill and develops difficulty breathing. Older people and those with underlying medical problems like high blood pressure, heart problems or diabetes, are more likely to develop serious illness. People with fever, cough, and difficulty in breathing should seek medical attention immediately.
HOW DOES COVID-19 SPREAD?
People can catch COVID-19 from others who have the virus. The disease can spread from person to person through small droplets from the nose or mouth which are spread when a person with COVID-19 coughs or exhales. These droplets land on objects and surfaces around the person. Other people then catch COVID-19 by touching these objects or surfaces, then touching their eyes, nose, or mouth. People can also catch COVID-19 if they breathe in droplets from a person with COVID-19 who coughs out or exhales droplets. Therefore, it is important to stay more than 1 meter (3 feet) away from a person who is sick. World Health Organization (WHO) is assessing ongoing research on the ways COVID-19 is spread and will continue to share the updated findings.
SHOULD I WORRY ABOUT COVID-19?
Illness due to COVID-19 infection is generally mild, especially for children and young adults. However, it can cause serious illness: about 1 in every 5 people who catch it need hospital care. It is therefore quite normal for people to worry about how the COVID-19 outbreak will affect them and their loved ones. We can channel our concerns into actions to protect ourselves, our loved ones and our communities. First and foremost, among these actions is regular and thorough hand-washing and good respiratory hygiene. Secondly, keep informed and follow the advice of the local health authorities including any restrictions put in place on travel, movement, and gatherings.
SHOULD I WEAR A MASK TO PROTECT MYSELF?
Only wear a mask if you are ill with COVID-19 symptoms (especially coughing) or looking after someone who may have COVID-19. A disposable face mask can only be used once. If you are not ill or looking after someone who is ill, then you are wasting a mask. There is a world-wide shortage of masks, so WHO urges people to use masks wisely. WHO advises the rational use of medical masks to avoid unnecessary wastage of precious resources and misuse of masks. The most effective ways to protect yourself and others against COVID-19 are to frequently clean your hands, cover your cough with the bend of elbow or tissue and maintain a distance of at least 1 meter (3 feet) from people who are coughing or sneezing. See basic protective measures against the new coronavirus for more information.
HOW LONG IS THE INCUBATION PERIOD OF COVID-19?
The "incubation period" means the time between catching the virus and beginning to have symptoms of the disease. Most estimates of the incubation period for COVID-19 range from 1-14 days, most commonly around five days. These estimates will be updated as more data becomes available.
IS THERE A DRUG, VACCINE, OR TREATMENT FOR COVID-19?
Not yet. To date, there is no vaccine and no specific antiviral medicine to prevent or treat COVID-2019. However, those affected should receive care to relieve symptoms. People with serious illnesses should be hospitalized. Most patients recover thanks to supportive care. Possible vaccines and some specific drug treatments are under investigation. They are being tested through clinical trials. WHO is coordinating efforts to develop vaccines and medicines to prevent and treat COVID-19.To know more about Novel Corona Virus (COVID-19), please refer the WHO and MoHFW websites respectively.
0 notes
Text
Do you know not only India Facing Polio vaccine Disease but now USA also
Do you know not only India Facing Polio vaccine Disease but now USA also
US Federal health officials know that a rare nervous system disorder is on the rise and that it is mostly affecting children across the country.
But what officials with the CDC don’t know about acute flaccid myelitis, a polio-like illness that can cause paralysis, is nearly everything else.
What causes it is not clear. Why it affects some people and not others is unknown. Why it seems to spike every 2 years remains a mystery. How to treat it, too, has the CDC stumped. The agency has confirmed 62 cases in 22 states this year and are investigating another 65 reports of similar illnesses. But the who, what, where, and why of the disease are largely still unknown.
“The reason why we don’t know about AFM -- and I am frustrated that despite all of our efforts, we haven’t been able to identify the cause of this mystery illness -- we continue to investigate to better understand the clinical picture of AFM cases, risk factors, and possible causes of the increase in cases,” Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases, told reporters at a news conference this week.
“We know this can be frightening for parents,” Messonnier said. “I know many parents want to know what the signs and symptoms are that they should be looking for in their child.”
Parents, she said, should seek medical care immediately if a child suddenly has weakness or loss of muscle tone in the arms and legs.
The good news is that the disease is very rare. Only one in 1 million people are thought to get it. However, while some children do fully recover, research shows that AFM’s effects often linger. In a study published last yeary, children showed persistent weakness in the areas affected by AFM. New, yet to be published research suggests as many as 50% of children with AFM will require surgery to restore function. But, because outbreaks of AFM are a relatively new phenomenon and the number of children affected so far has been small, researchers have limited data from which to draw firm conclusions.
"We work with what we have,” says Priya Duggal, PhD, director of the genetic epidemiology program at the Johns Hopkins Bloomberg School of Public Health in Baltimore. ��The depth of information that we have is helpful even if we do not have breadth of cases."
Because the disease is more likely to strike children, and because of the mysteries of it and because of the dramatic health effects, it gets more attention than it might otherwise.
Despite the current alarm, the disease is not unheard of.
“In 2014, the first patient I saw was a baby, who had a sudden onset of weakness in one leg,” recalls Marc Patterson, MD. “The leg was flaccid and did not recover.”
Since then, Patterson, chairman of the division of Child and Adolescent Neurology at the Mayo Clinic in Rochester, MN, has seen several children diagnosed with what’s come to be called acute flaccid myelitis, or AFM, a very rare disease that causes nerve-damaging inflammation in the gray matter of the spinal cord.
AFM can lead to weakness or paralysis in the arms and legs. Cranial nerves also can be affected, which can make your face weak, eyelids droop, or make it hard to swallow. In the most severe cases, AFM can cause trouble breathing and may require ventilator support.
“This disorder presents just like paralytic polio used to present back in the 1940s,” says Patterson, who’s also a Mayo Clinic professor of neurology, pediatrics, and medical genetics. “This is another form of polio, and I think that people have not used the term because of the tremendous emotional significance.”
This year, the third outbreak of AFM is still underway. Such outbreaks have arrived every 2 years since 2014, and the CDC’s current tally includes nearly 400 confirmed cases over the past 4 years. The federal health agency acknowledges that gathering data about AFM is a relatively new process, and that may make it difficult to interpret and compare what they’ve learned from each outbreak.
The number of cases likely will rise as health agencies investigate and confirm potential cases, a process that can take lots of time.
“The CDC is very careful in taking time to identify cases, and there may be a jump in the number as cases go through the verification process,” says Kevin Messacar, MD, a pediatrician at Children’s Hospital Colorado who specializes in infectious diseases. As an assistant professor at the University of Colorado School of Medicine, he has seen 12 children with AFM since spring.
“Our situation here in Colorado is unique because our outbreak has been ongoing since March, while it has started elsewhere in the summer months,” says Messacar.
The disorder itself is not new, says Patterson, as similar but isolated cases have been reported over the years. “But I think it was the fact that it was a cluster that first drew attention to this in 2014.”
Viruses a Possible Trigger
Many AFM cases have been linked to enteroviruses. Such viruses are not uncommon. In fact, the CDC estimates they cause as many as 15 million infections each year and tens of thousands of hospitalizations. But most infections cause only mild symptoms, such as gastrointestinal upsets, cold-like discomfort, and fever. Sometimes, they cause no symptoms at all. But some experts suspect that the viruses somehow trigger AFM in a very small number of people, most of them children.
Children are quite vulnerable to viruses, says Messacar, because they do not have fully developed immune systems. So their bodies can’t combat infection as successfully as adults. But AFM can strike adults whose immune systems don’t work well, such as those being treated for cancer.
The symptoms of AFM arrive suddenly, usually within a week of being ill with a virus. An arm or a leg, for example, becomes weak or can’t be moved at all. In study findings presented at scientific meetings this year though not yet published, about 70% of kids with AFM have more than one affected limb.
To diagnose AFM, doctors will use magnetic resonance imaging (MRI) of the patient’s spinal cord for signs of inflammation. They may also perform a spinal tap to allow them to examine the spinal fluid for signs of the illness.
In addition to making a positive diagnosis of AFM, doctors also aim to find its cause.
“If we’re lucky, we can identify a virus,” says Patterson, “but there are many cases where you can’t positively identify a specific virus or other cause.”
Currently, no drug treatment exists to counter AFM’s attack on the nervous system. And, says Roberta L. DeBiasi, MD, a single drug may not be enough.
“It’s important to keep in mind that not all AFM is linked to … enteroviruses,” says DeBiasi, who heads the Division of Infectious Diseases at Children’s National Health System in Washington, D.C. “So, even if one specific treatment works for some patients, it may not necessarily represent a potential treatment for all AFM.”
Muscle Therapy a Key Treatment
aims to strengthen the muscles around the areas affected by the disease.
“If a child has weakness in a limb,” says Patterson, “one of the most important things we can do is get one of our occupational or physical therapy colleagues involved as soon as the child is well enough to participate.”
That kind of therapy requires a lot of hard work.
“At centers experienced in working with children affected by AFM, treatment often means weeks or months of intensive therapy done on a daily basis,” says Messacar.
And even that may not be adequate, he continues: “The vast majority of cases are left with residual weakness and in some cases complete paralysis of the affected areas.”
For those children, surgery may be needed to help them regain their abilities. Los Angeles-based surgeon Mitchel Seruya, MD, has performed a complex procedure called a nerve transfer on 15 children with AFM. His patients come from all over the country: Wisconsin, New Mexico, Texas, Minnesota, and elsewhere.
During the procedure, the surgeon reroutes a nerve from elsewhere in the body to take over the work of the nerve affected by AFM. For example, if AFM has caused weakness in a child’s shoulder and elbow but not in the hand or forearm, Seruya, an assistant professor of clinical surgery, can work with the healthy nearby nerves.
“If I want the elbow to move, I am going to steal a wrist flexor, meaning I’m going steal something that makes your wrist bend and divert it to your elbow,” says Seruya, who’s also director of the Brachial Plexus and Peripheral Nerve Center at Children’s Hospital Los Angeles.
The repairs get much more complicated if the whole arm has been paralyzed. In such cases, the nerves most often used are those involved in breathing, located near the sternum.
“That nerve has to span the chest and reach underneath the armpit to connect it to the arm itself,” Seruya says.
Researchers Look at Role of Genes
One of the key questions that needs to be answered is why some children -- keep in mind, it’s a very small number -- get AFM and most others don’t. For example, if an entire family or, say, a classroom gets exposed to an enterovirus, why doesn’t everyone get AFM? Researchers at Johns Hopkins University in Baltimore suspect that genetics may play a role. They are comparing the genetic makeup of children with AFM to see what they might have in common. And in families, they are also looking for genetic differences between family members who remained healthy and the child diagnosed with AFM.
“We hope this helps us to understand susceptibility to AFM,” says Priya Duggal, PhD, director of the genetic epidemiology program at the Johns Hopkins Bloomberg School of Public Health. “No doubt that this is not going away -- we keep seeing it -- and we need to better understand how to diagnose AFM, how to treat it, and what factors are causing it … or we will watch more kids become paralyzed.”
Since there’s no vaccine or drug treatment, the CDC’s prevention guidelines follow standard but effective advice for cutting the chances of getting or spreading a virus: Wash your hands often. Getting vaccinated for poliovirus may also offer protection. Finally, use mosquito repellent and other means of preventing mosquito bites, which can spread West Nile virus, another virus associated with AFM.
DeBiasi of Children’s in Washington wants parents to be vigilant but also to keep in mind that AFM is quite rare. It occurs in about one in 1 million children.
“If your child presents with weakness in one or more limbs, drooping facial features, like eyelids, seek care immediately,” she stresses, “particularly if your child has just had an upper respiratory infection or fever.”
Source: https://www.webmd.com
Read the full article
0 notes
Text
The Truth Teller
If you run into a left-leaning “consultant” these days, there’s a fairly good chance they used to work for the Obama administration. Scores of federal officials and bureaucrats have resigned or been fired since President Trump’s inauguration, some after realizing their goals were not in line with the new president’s.
Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, wasn’t one of them. In fact, he seemed surprised at the suggestion that he might do something other than what he’s been doing since he began leading the institute in 1984—trying to protect people from diseases like Ebola, Zika, and HIV.
This is despite the fact that some of Trump’s policy proposals seem to directly contradict his efforts. Trump has proposed cutting funding for a program that provides HIV drugs to people in poor countries by 17 percent. Not long after, six members of the Presidential Advisory Council on HIV/AIDS resigned, citing "a president who simply does not care.”
Repealing the Affordable Care Act—a move Trump has supported—would cut a key infectious disease fund in half. And Trump’s decision to reinstate a law that withholds global-health funding from organizations abroad that “perform or actively promote abortion” could hamper AIDS-relief efforts, as my colleague Joseph Frankel reported. As if that weren’t enough, Trump has also aired anti-vaccine views.
I asked Fauci if he was daunted by all these developments, and if not, how he planned to do his work in spite of them. An edited version of our conversation, which took place at the Aspen Ideas Festival, follows:
Olga Khazan: I know you've worked for every administration — you've worked for Bush, you worked for Reagan, Obama …
Anthony Fauci: Clinton.
Khazan: Clinton, he was in there too. [Given that many civil servants have resigned from the Trump administration] … when Trump was elected, did you ever think, “I can't do this one, I'm going to have to sit this one out?”
Fauci: No, not at all. I am embraced by every administration from Reagan [onward] because they realize that I speak truth to them even when they don't like it. Even if ideologically they’re very different. When I'm with Reagan, I told Reagan some of the things that I felt he should do with HIV/AIDS. He didn't listen to everything. He was a good guy but he was afraid to go public and make the bully pulpit and say, “hey everybody this is a problem, we gotta address it.” However, when I got to George H.W. Bush I became very good friends with him.
When he was vice president, he knew that you had to address the AIDS issue. I was very well-known as the AIDS person of the government because very few people were working on AIDS. And he said, “I want you to teach me about HIV. Show me, show me patients.” He wanted to learn. So it's my old adage, be nice to everybody in Washington, because one of these days they're going to be really powerful. So I was nice to the vice president and very soon thereafter he was president, so then I had a friend in the White House. I gained a reputation that I would tell you the truth, even if it was something that you didn’t like.
So the word got out that you call on this guy [Fauci], he is completely apolitical, and he'll give you the advice that you need. So I did it with George H.W. Bush, I did it with Clinton, I did it with George W. Bush and I did it with Obama. I developed the [President’s Emergency Plan for AIDS Relief] program with Bush. I mean for him to give me the opportunity to go to Africa and put together a $15 billion dollar program, that was really nice. With Obama, I was in the situation room like every week, with Ebola and then Zika and H7N9, potentially pandemic flu.
So when the next president came I'd be more than happy to advise, I'm not gonna say, “no I'm not gonna do that.”
Khazan: How do you stay motivated, since this administration has pretty openly wanted to cut a lot of global-health funding, foreign aid, AIDS research? A lot of the things that you would probably work on.
Fauci: It doesn't interfere with my motivation. I'm driven by the problems that I have to solve. Sometimes you do it with a lot of resources and sometimes you do it with less resources. I don't say, “well I'm gonna get out because we have less resources.” And as a matter of fact, we don't know what the resources are gonna be because we don't have a budget yet.
Khazan: When you look at things like Zika coming to the U.S., do you consider that to be caused more by climate change and related issues or more by human travel?
Fauci: It's much, much more human travel. I mean you may increase the range of mosquitoes during a period of time, like at the end of June they may go up to Florida. But the major determinant of Zika in the continental United States is travel-related, people who are infected in South America and Puerto Rico who travel to the United States, and that's exactly what happened. We had about five to six thousand travel-related cases of Zika that came from South America, Central America, and the Caribbean, including Puerto Rico, and so far we've had a total of about 220 [locally] transmitted cases, meaning people that never left Florida.
Khazan: Is a Zika vaccine ready and deployable right now? Or are we still working on it?
Fauci: We have a DNA vaccine for Zika and it's of interest. [The new vaccine uses] platform technology. The idea of growing a virus and having to kill it and then injecting it, that's so passe, as my daughter says, “so 20th century dad.” You don't want to do that. What it is right now is that we take platforms like DNA, MRNA, virus vectors, and all you need is to insert the gene of whatever protein you want expressed. In Zika it's the PREM protein which is the protein in the outer part of the virus. We have done that, done preclinical and animal, gone into phase one and we're now in phase two in Puerto Rico and in Texas and we're going into phase 2B in countries in South America depending upon what the burden of Zika is. Going from the time we sequence the Zika virus to the time it went into humans in a phase one study was 3.6 months, which is the fastest in the history of vaccinology. Which tells us we could really cut down that time from when you recognize a new infection to the time you get a vaccine at least ready for trial.
Khazan: What do you anticipate being the next thing like Zika? Or is it impossible to predict?
Fauci: The answer is we don't know, but there are certain things you need to keep your eye on. For example, will Zika come back in some South American countries where it didn't hit hard last time? Next December will be the third [hot] season in Brazil. I wouldn't be surprised if we see more. I wouldn't be surprised if we see more cases in Puerto Rico as we get into this July and August when it's moist, humid, and a lot of mosquitoes. So I'm keeping my eye on Mexico and the border between Mexico and Texas, particularly around the Brownsville area, where you always see that jumping over the border of emerging infections. And it could be in Puerto Rico. So I'm not through with Zika.
Then the other thing is what about Yellow Fever in Brazil? If it goes into the aedes aegypti mosquito, will that then become ... there are two phases of yellow fever. One is called the sylvatic phase which means that woodsmen go into the woods chop down trees for the lumber, they get bit by a mosquito that bit a monkey, the monkey's the reservoir, they get yellow fever, they get sick. They either die or they get better. Sometimes those people move into the city, and if they get bit by an aedes aegypti, which really likes to bite humans, and you get yellow fever established in a really populous area, then you have a problem. We could get a lot of yellow fever in South America, travel to the United States, and then you wind up getting that.
So I keep my eye on that. The other thing is flu pandemic. This H7N9 bird flu in China? It jumps from a chicken to a human but it doesn't efficiently spread at all from human to human. If that starts to evolve, that could be something. So there are always these things that you keep your eye on, but the likelihood is that it’s gonna be something that you and I are not talking about right now.
Khazan: Really?
Fauci: Of course. Whoever would have thought there would have been Zika? Zika was on nobody's radar screen.
Khazan: I would think, well, you would have …
Fauci: I was thinking about Zika, but we did not know that it caused congenital abnormalities, but it was big. So there was an outbreak of Zika in the Yap islands in 2007. There was another outbreak in French Polynesia 2013. So you could have said, “Tony why didn't you start making a vaccine in 2013?” Because I didn't think it was a particularly important disease. It was trivial. Eighty percent of the people didn't get symptoms, the 20 percent that did get symptoms got mild symptoms. They got conjunctivitis, rash, fever, myalgia, it went away in five to seven days, and they were done. Then, when you go to a big country like Brazil, where you have hundreds of thousands of cases, then you start to see something that's really worrisome, namely pregnant women get infected and they have a 10 percent chance of having microcephalic baby. So that's when we realized we're dealing with a very serious disease.
Khazan: What was the $1.9 billion dollars that President Obama had asked Congress for Zika for, since there's no cure and it’s spread primarily by people traveling from other countries. What is that money primarily used for?
Fauci: We feel that if we don't stop it in South America, it inevitably is going to come to our territories, including Puerto Rico and even to the southeastern part of the United States. So a considerable amount of money will go to the CDC to do mosquito control. To do surveillance, to do testing. To determine the natural history. That takes hundreds and hundreds of millions of dollars. So the CDC got a lot of money. USAID got money, NIH got money, FDA got money. We got relatively little. I mean of the Zika amount, we asked for $197 million and we got $152. And we're working on a vaccine, on drugs and stuff, but a lot of it was public-health provisions. Mosquito control became very, very important. We were doing a lot of spraying in Puerto Rico, we were doing a lot of mosquito control, [such as] genetically modified mosquitoes, all that costs money.
Khazan: Do you work on the anti-vaccine movement at all?
Fauci: We don't work on it but we try and do public relations discussions. I do TV, I do radio, I do interviews like this, to make it clear that I can understand how people are concerned, but the facts, the science, countless amounts of data from independent, non-biased people indicate that A) vaccines are safe, B) they do not cause autism, and C) they don't cause those other things that people think they do.
Khazan: Have you found any messages that resonate with people, that actually change people's minds about not vaccinating?
Fauci: Yes. There is a core of people who no matter what you say, they will not believe you. They are convinced that vaccines are dangerous or they feel they don't want to take the risk of their child, even though there's two reasons to give vaccine: one is to protect your child, the other is a duty that you have to society to keep society protected.
Yet there is also a pretty good corps of people who if you explain it to them in a non-pejorative way … one of the things that I've learned works is that you don't criticize people. That's not the way to their hearts. And you've gotta approach it in saying that you could understand their concern, but these are the reasons. In the realm of science, you have to rely on the evidence base. You can't guess, you can't do spurious things.
Khazan: You said you are known for telling people hard truths. What's a hard truth that you have had to tell this administration, or might have to tell them?
Fauci: I'm all ready doing it. There is a concern that, are the data regarding safety of vaccines really strong data? And I'm not talking about the president himself, I'm talking about the people around him. And I've already met with a couple of people who were sent to me by the administration to try and convince them or to at least talk to them about what's the situation, because they believe that vaccines are dangerous. Vaccines do not cause autism, period. And that's it. Now if members of whatever administration — this administration, the last administration, or the next administration — I'll have to just tell them what I know based on evidence. Whether they believe it or not, it's up to them.
from Health News And Updates https://www.theatlantic.com/health/archive/2017/06/the-truth-teller/531561/?utm_source=feed
0 notes
Text
The Truth Teller
If you run into a left-leaning “consultant” these days, there’s a fairly good chance they used to work for the Obama administration. Scores of federal officials and bureaucrats have resigned or been fired since President Trump’s inauguration, some after realizing their goals were not in line with the new president’s.
Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, wasn’t one of them. In fact, he seemed surprised at the suggestion that he might do something other than what he’s been doing since he began leading the institute in 1984—trying to protect people from diseases like Ebola, Zika, and HIV.
This is despite the fact that some of Trump’s policy proposals seem to directly contradict his efforts. Trump has proposed cutting funding for a program that provides HIV drugs to people in poor countries by 17 percent. Not long after, six members of the Presidential Advisory Council on HIV/AIDS resigned, citing "a president who simply does not care.”
Repealing the Affordable Care Act—a move Trump has supported—would cut a key infectious disease fund in half. And Trump’s decision to reinstate a law that withholds global-health funding from organizations abroad that “perform or actively promote abortion” could hamper AIDS-relief efforts, as my colleague Joseph Frankel reported. As if that weren’t enough, Trump has also aired anti-vaccine views.
I asked Fauci if he was daunted by all these developments, and if not, how he planned to do his work in spite of them. An edited version of our conversation, which took place at the Aspen Ideas Festival, follows:
Olga Khazan: I know you've worked for every administration — you've worked for Bush, you worked for Reagan, Obama …
Anthony Fauci: Clinton.
Khazan: Clinton, he was in there too. [Given that many civil servants have resigned from the Trump administration] … when Trump was elected, did you ever think, “I can't do this one, I'm going to have to sit this one out?”
Fauci: No, not at all. I am embraced by every administration from Reagan [onward] because they realize that I speak truth to them even when they don't like it. Even if ideologically they’re very different. When I'm with Reagan, I told Reagan some of the things that I felt he should do with HIV/AIDS. He didn't listen to everything. He was a good guy but he was afraid to go public and make the bully pulpit and say, “hey everybody this is a problem, we gotta address it.” However, when I got to George H.W. Bush I became very good friends with him.
When he was vice president, he knew that you had to address the AIDS issue. I was very well-known as the AIDS person of the government because very few people were working on AIDS. And he said, “I want you to teach me about HIV. Show me, show me patients.” He wanted to learn. So it's my old adage, be nice to everybody in Washington, because one of these days they're going to be really powerful. So I was nice to the vice president and very soon thereafter he was president, so then I had a friend in the White House. I gained a reputation that I would tell you the truth, even if it was something that you didn’t like.
So the word got out that you call on this guy [Fauci], he is completely apolitical, and he'll give you the advice that you need. So I did it with George H.W. Bush, I did it with Clinton, I did it with George W. Bush and I did it with Obama. I developed the [President’s Emergency Plan for AIDS Relief] program with Bush. I mean for him to give me the opportunity to go to Africa and put together a $15 billion dollar program, that was really nice. With Obama, I was in the situation room like every week, with Ebola and then Zika and H7N9, potentially pandemic flu.
So when the next president came I'd be more than happy to advise, I'm not gonna say, “no I'm not gonna do that.”
Khazan: How do you stay motivated, since this administration has pretty openly wanted to cut a lot of global-health funding, foreign aid, AIDS research? A lot of the things that you would probably work on.
Fauci: It doesn't interfere with my motivation. I'm driven by the problems that I have to solve. Sometimes you do it with a lot of resources and sometimes you do it with less resources. I don't say, “well I'm gonna get out because we have less resources.” And as a matter of fact, we don't know what the resources are gonna be because we don't have a budget yet.
Khazan: When you look at things like Zika coming to the U.S., do you consider that to be caused more by climate change and related issues or more by human travel?
Fauci: It's much, much more human travel. I mean you may increase the range of mosquitoes during a period of time, like at the end of June they may go up to Florida. But the major determinant of Zika in the continental United States is travel-related, people who are infected in South America and Puerto Rico who travel to the United States, and that's exactly what happened. We had about five to six thousand travel-related cases of Zika that came from South America, Central America, and the Caribbean, including Puerto Rico, and so far we've had a total of about 220 [locally] transmitted cases, meaning people that never left Florida.
Khazan: Is a Zika vaccine ready and deployable right now? Or are we still working on it?
Fauci: We have a DNA vaccine for Zika and it's of interest. [The new vaccine uses] platform technology. The idea of growing a virus and having to kill it and then injecting it, that's so passe, as my daughter says, “so 20th century dad.” You don't want to do that. What it is right now is that we take platforms like DNA, MRNA, virus vectors, and all you need is to insert the gene of whatever protein you want expressed. In Zika it's the PREM protein which is the protein in the outer part of the virus. We have done that, done preclinical and animal, gone into phase one and we're now in phase two in Puerto Rico and in Texas and we're going into phase 2B in countries in South America depending upon what the burden of Zika is. Going from the time we sequence the Zika virus to the time it went into humans in a phase one study was 3.6 months, which is the fastest in the history of vaccinology. Which tells us we could really cut down that time from when you recognize a new infection to the time you get a vaccine at least ready for trial.
Khazan: What do you anticipate being the next thing like Zika? Or is it impossible to predict?
Fauci: The answer is we don't know, but there are certain things you need to keep your eye on. For example, will Zika come back in some South American countries where it didn't hit hard last time? Next December will be the third [hot] season in Brazil. I wouldn't be surprised if we see more. I wouldn't be surprised if we see more cases in Puerto Rico as we get into this July and August when it's moist, humid, and a lot of mosquitoes. So I'm keeping my eye on Mexico and the border between Mexico and Texas, particularly around the Brownsville area, where you always see that jumping over the border of emerging infections. And it could be in Puerto Rico. So I'm not through with Zika.
Then the other thing is what about Yellow Fever in Brazil? If it goes into the aedes aegypti mosquito, will that then become ... there are two phases of yellow fever. One is called the sylvatic phase which means that woodsmen go into the woods chop down trees for the lumber, they get bit by a mosquito that bit a monkey, the monkey's the reservoir, they get yellow fever, they get sick. They either die or they get better. Sometimes those people move into the city, and if they get bit by an aedes aegypti, which really likes to bite humans, and you get yellow fever established in a really populous area, then you have a problem. We could get a lot of yellow fever in South America, travel to the United States, and then you wind up getting that.
So I keep my eye on that. The other thing is flu pandemic. This H7N9 bird flu in China? It jumps from a chicken to a human but it doesn't efficiently spread at all from human to human. If that starts to evolve, that could be something. So there are always these things that you keep your eye on, but the likelihood is that it’s gonna be something that you and I are not talking about right now.
Khazan: Really?
Fauci: Of course. Whoever would have thought there would have been Zika? Zika was on nobody's radar screen.
Khazan: I would think, well, you would have …
Fauci: I was thinking about Zika, but we did not know that it caused congenital abnormalities, but it was big. So there was an outbreak of Zika in the Yap islands in 2007. There was another outbreak in French Polynesia 2013. So you could have said, “Tony why didn't you start making a vaccine in 2013?” Because I didn't think it was a particularly important disease. It was trivial. Eighty percent of the people didn't get symptoms, the 20 percent that did get symptoms got mild symptoms. They got conjunctivitis, rash, fever, myalgia, it went away in five to seven days, and they were done. Then, when you go to a big country like Brazil, where you have hundreds of thousands of cases, then you start to see something that's really worrisome, namely pregnant women get infected and they have a 10 percent chance of having microcephalic baby. So that's when we realized we're dealing with a very serious disease.
Khazan: What was the $1.9 billion dollars that President Obama had asked Congress for Zika for, since there's no cure and it’s spread primarily by people traveling from other countries. What is that money primarily used for?
Fauci: We feel that if we don't stop it in South America, it inevitably is going to come to our territories, including Puerto Rico and even to the southeastern part of the United States. So a considerable amount of money will go to the CDC to do mosquito control. To do surveillance, to do testing. To determine the natural history. That takes hundreds and hundreds of millions of dollars. So the CDC got a lot of money. USAID got money, NIH got money, FDA got money. We got relatively little. I mean of the Zika amount, we asked for $197 million and we got $152. And we're working on a vaccine, on drugs and stuff, but a lot of it was public-health provisions. Mosquito control became very, very important. We were doing a lot of spraying in Puerto Rico, we were doing a lot of mosquito control, [such as] genetically modified mosquitoes, all that costs money.
Khazan: Do you work on the anti-vaccine movement at all?
Fauci: We don't work on it but we try and do public relations discussions. I do TV, I do radio, I do interviews like this, to make it clear that I can understand how people are concerned, but the facts, the science, countless amounts of data from independent, non-biased people indicate that A) vaccines are safe, B) they do not cause autism, and C) they don't cause those other things that people think they do.
Khazan: Have you found any messages that resonate with people, that actually change people's minds about not vaccinating?
Fauci: Yes. There is a core of people who no matter what you say, they will not believe you. They are convinced that vaccines are dangerous or they feel they don't want to take the risk of their child, even though there's two reasons to give vaccine: one is to protect your child, the other is a duty that you have to society to keep society protected.
Yet there is also a pretty good corps of people who if you explain it to them in a non-pejorative way … one of the things that I've learned works is that you don't criticize people. That's not the way to their hearts. And you've gotta approach it in saying that you could understand their concern, but these are the reasons. In the realm of science, you have to rely on the evidence base. You can't guess, you can't do spurious things.
Khazan: You said you are known for telling people hard truths. What's a hard truth that you have had to tell this administration, or might have to tell them?
Fauci: I'm all ready doing it. There is a concern that, are the data regarding safety of vaccines really strong data? And I'm not talking about the president himself, I'm talking about the people around him. And I've already met with a couple of people who were sent to me by the administration to try and convince them or to at least talk to them about what's the situation, because they believe that vaccines are dangerous. Vaccines do not cause autism, period. And that's it. Now if members of whatever administration — this administration, the last administration, or the next administration — I'll have to just tell them what I know based on evidence. Whether they believe it or not, it's up to them.
Article source here:The Atlantic
0 notes