#scientific news
Text
I’m really seeing history unfolding before my eyes
A room temperature superconductor is potentially being discovered and a lesbian has significantly improved the procedure already
Truly the world is amazing
89 notes
·
View notes
Text
#news#virology#black death#bubonic plague#medieval history#autoimmune#autoimmune disorders#neuroscience#genetics#genes#science#scientific news#science news#health#health news#health research
4 notes
·
View notes
Text
Y’all, I am SO excited about this new beetle that was just discovered!!!!


The freshly-discovered new species of longhorn beetle, Excastra albopilosa. Image credit: James Tweed

Detailed photographs of the Excastra albopilosa specimen found by James Tweed. Image credits: Lingzi Zhou, Australian National Insect Collection
#insects#entomology#bugs#insect#bug#nature#bugblr#beetle#coleoptera#beetles#new beetle#beetle discovery#new beetle discovered#scientific discovery#longhorn beetle#Australia#excastra albopilosa#fuzzy beetle
5K notes
·
View notes
Text


#occult#daizy#curiosities#old advertisements#bizarre#obscurities#scientific news#experimental#documentation
0 notes
Text
i like to think that the tentacles in dungeon meshi are kinda like mushrooms or perhaps even lichens in that they are very confusing to identifty and have 200 completely different species that look very similar ("delicious brown tentacle vs BROWN DEATH TENDRIL") and you need to be an Expert to determine the difference between some of the more confusing species and some of them have like 300 different sexes and some of them are actually composite creatures composed of several different species and somehow yeast is involved and also no one really knows half of whats going on with them and in like 50 years someones gonna figure out that uhm actually these are two completely different types of tentacle creatures that arent related like at All they jusf happen to look similar and oh btw that one common house mold is actually a tentacle
#dungeon meshi#delicious in dungeon#i dont know enough about lichens to go into detail they confuse the fuck outta me#i love how the wikipedia page uses the words#'was UNDERSTOOD to be...'#'in 2016 research revealed a NEW PARTNER a yeast'#they sound like fucked up little guys#(looking at tentacle porn) huh i wonder about the scientific research on these guys#like it would explain how theres just So Many Types and its just a fucking mess every time they appear onscreen#oh sorry you thought this was a common docile soecies of tentacle that happens to be delicious but its ACTUALLY the voracious Sex Tenta
2K notes
·
View notes
Text
Endometriosis and irritable bowel syndrome: A systemic review and meta-analyses
Michelle Y. Nabi, Samal Nauhria, [...], and Prakash V. A. K. Ramdass
Abstract
Objective
To estimate the pooled odds ratio of endometriosis and irritable bowel syndrome, and to estimate the pooled prevalence of irritable bowel syndrome in patients with endometriosis.
Data sources
Using Cochrane Library, MEDLINE, Science Direct, ClinicalTrials.gov, Web of Science, and CINAHL, we conducted a systematic literature search through October 2021, using the key terms “endometriosis” and “irritable bowel syndrome.” Articles had to be published in English or Spanish. No restriction on geographical location was applied.
Methods of study selection
The following eligibility criteria were applied: full-text original articles; human studies; studies that investigated the association between endometriosis and irritable bowel syndrome. Two investigators screened and reviewed the studies. A total of 1,776 studies were identified in 6 separate databases. After screening and applying the eligibility criteria, a total of 17 studies were included for analyses. The meta-analysis of association between endometriosis and irritable bowel syndrome included 11 studies, and the meta-analysis on the prevalence of irritable bowel syndrome in endometriosis included 6 studies.
Tabulation, integration, and results
Overall 96,119 subjects were included in the main meta-analysis (11 studies) for endometriosis and irritable bowel syndrome, with 18,887 endometriosis patients and 77,171 controls. The odds of irritable bowel syndrome were approximately 3 times higher among patients with endometriosis compared with healthy controls (odds ratio 2.97; 95% confidence interval, 2.17 – 4.06). Similar results were obtained after subgroup analyses by endometriosis diagnosis, irritable bowel syndrome diagnostic criteria, and Newcastle-Ottawa Scale scores. Six studies reported prevalence rates of irritable bowel syndrome in people with endometriosis, ranging from 10.6 to 52%. The pooled prevalence of irritable bowel syndrome in people with endometriosis was 23.4% (95% confidence interval, 9.7 – 37.2).
Conclusion
Patients with endometriosis have an approximately threefold increased risk of developing irritable bowel syndrome. Development and recent update of Rome criteria has evolved the diagnosis of IBS, potential bias should still be considered as there are no specific tests available for diagnosis.
Systemic Review Registration
Keywords: irritable bowel syndrome, endometriosis, systematic review, meta-analyses, functional gastrointestinal disorders
Introduction
Endometriosis and irritable bowel syndrome (IBS) are two common medical conditions that markedly affect a substantial proportion of adults and teenagers, and even some menopausal adults (1, 2). Even though they are two distinct conditions with different etiologies, a significant percentage of people experience both concurrently (3). Endometriosis, with an estimated worldwide prevalence ranging from 0.7 to 8.6%, (4) is characterized by the existence of endometrial-like tissue that has been disseminated beyond the uterine cavity. Patients with endometriosis commonly experience menstrual disturbance, infertility, abdominal and pelvic pain, and irregularities with bowel movements (5, 6).
Irritable bowel syndrome, which shares many clinical features with endometriosis, is a gastrointestinal disorder that primarily affects the large intestine, and is characterized by an array of symptoms such as alteration in bowel movements, abdominal discomfort, pain, and cramping (7). The prevalence of irritable bowel syndrome ranges from 0.4 (in India and Ghana) to 20.9% (in Singapore), with a pooled global prevalence of 5.9% (8). Moreover, approximately 61% of adults and teenagers who were assigned female at birth are affected by irritable bowel syndrome (9).
Irritable bowel syndrome and endometriosis have a significant overlap in symptom presentation due to chronic inflammation thus leading to chronic pelvic pain (10). Endometriosis may even masquerade as irritable bowel syndrome in some patients (11). However, despite these similarities in clinical presentation, a recent nationwide study in the U.S. has shown that endometriosis increases the risk of irritable bowel syndrome approximately threefold (3). Possible explanations for this increased risk include chronic low grade inflammation resulting from mast cell activation, neuronal inflammation, leaky gut, and dysbiosis (12).
It is unclear if endometriosis is an independent risk factor for irritable bowel syndrome. The main purpose of this study was to quantify the association between endometriosis and irritable bowel syndrome, and to estimate the prevalence of irritable bowel syndrome in patients with endometriosis through pooled analysis.
Materials and methods
Sources
This systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and protocols (PRISMA-P) statement (13). The study protocol was registered in the PROSPERO database (University of York, United Kingdom).1 A systematic search of the following electronic databases was conducted to identify peer-reviewed literature from inception until October 2021: MEDLINE, Science Direct, ClinicalTrials.gov, Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, CINAHL, and Web of Science. Key words or MeSH terms used were “irritable bowel syndrome” AND “endometriosis.”
Study selection
Citation files from the searched databases were imported into Endnote reference management software and duplicates were removed. Using the eligibility criteria, two investigators independently screened titles and abstracts of the studies for relevance. The potential full texts articles were further assessed to be included in the review. Any disagreements between the authors were resolved with a discussion. Inclusion criteria were any observational or experimental studies that investigated both endometriosis and irritable bowel syndrome. Studies were included if irritable bowel syndrome was diagnosed by pre established criteria. Endometriosis had to be confirmed surgically, by clinical inspection, or reported as the International Classification of Diseases code for endometriosis. Meta-analyses, reviews, conference summaries, abstracts, case reports, opinions, letters, and animal studies were excluded. There was no search restriction for year of publication or the age group of patients. Articles were restricted to English and Spanish.
Data extraction and quality assessment
Data were extracted into a standardized data-collection sheet using the following headings: first author name, date of publication, study site, study design, irritable bowel syndrome diagnosis criteria, endometriosis diagnostic criteria, sample size, event rate, and quality assessment score. Two investigators (MN and PR) assessed the quality of all included studies using the Newcastle-Ottawa Scale (NOS), and the overall scores were recorded (14). NOS scale is widely used for assessing quality of each included study in meta-analyses and is based on ranking studies on according to the selection criteria, group comparability and ascertainment of exposure.
Data synthesis and analysis
Forest plots were generated with Review Manager version 5.4 (Nordic Cochrane Centre, Cochrane Collaboration, Denmark) and funnel plots were created with JASP statistical software. The primary outcome of the association of irritable bowel syndrome and endometriosis in this meta-analysis was performed using the random effects model to produce odds ratios (OR) with 95% confidence interval (CI). We conducted subgroup analyses based on diagnosis of endometriosis (surgical versus ICD-9-CM 617.x codes), method of diagnosis of irritable bowel syndrome, NOS scores (>6 vs. <6), and a combination of all criteria (endometriosis diagnosis; irritable bowel syndrome criteria; NOS score; and study design). In the subgroup analysis based on all criteria, studies were grouped as having met all criteria (surgical diagnosis of endometriosis, irritable bowel syndrome diagnosed with Rome criteria (15–17), NOS score > 6, and longitudinal studies), or not. This allowed for strong epidemiological evidence for the association between endometriosis and irritable bowel syndrome.
According to Rome III criteria, IBS patients can be classified into four subtypes and can be useful for treating specific symptoms of the patient. The subtypes include: IBS with diarrhea (IBS-D), IBS with constipation (IBS-C), IBS with mixed features (IBS-M) or IBS, unsubtyped. Whereas Rome IV criteria defined IBS as a functional bowel disorder in which recurrent abdominal pain is associated with defecation or a change in bowel habits.
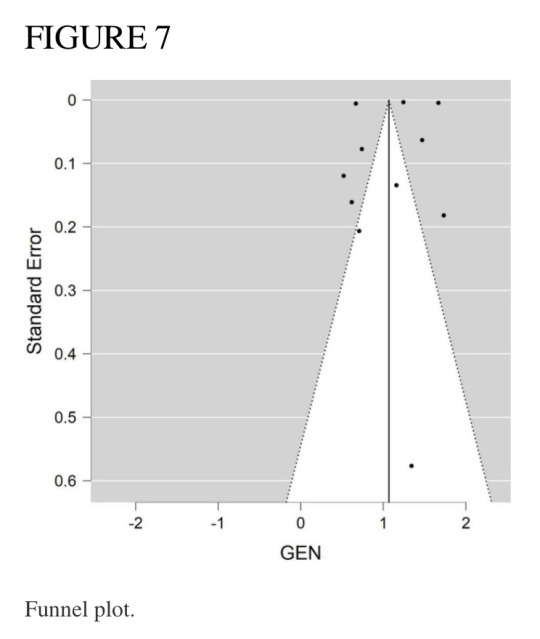
A separate forest plot was generated for the prevalence of irritable bowel syndrome in patients with endometriosis, for studies that provided only prevalence data. The random effects model account for between-study heterogeneity by weighting studies similarly. Heterogeneity was assessed using the I2 statistic. Values of I2 > 50% were considered as indicative of large heterogeneity (18). We used the Begg’s and Egger’s funnel plot, which is a subjective visual method, to estimate risk of publication bias. A funnel plot that appears asymmetrical suggests publication bias. A p-value of <0.05 for all analyses was considered statistically significant. Although p-values are poor predictors of outcome, all quantitative studies included in our analyses mention p-values in accordance to the AM Stat recommendation.
Results
Search results and study inclusion
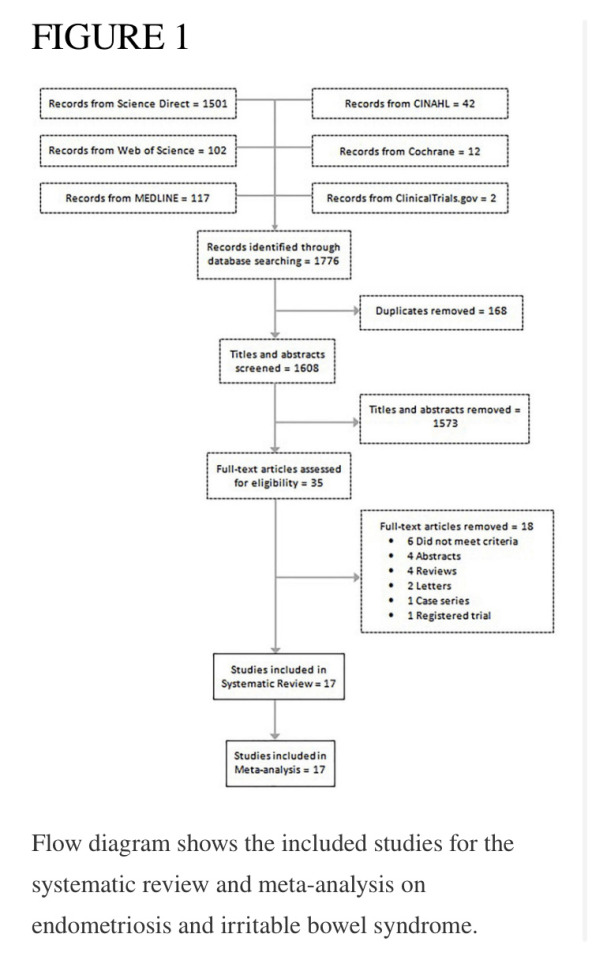
A total of 1,776 studies were identified in 6 separate databases. After removal of 168 duplicates, there were 1,608 eligible studies (titles/abstracts) which were independently screened by two reviewers. Of the 1,608 screened studies, 1,573 did not meet inclusion criteria and 35 full-text articles were reviewed. A total of 17 studies met criteria to be included in the systematic review. Eighteen studies were excluded for the following reasons: did not meet criteria; conference abstracts; reviews; letters; case series; and registered trials. The meta-analysis of the association of endometriosis and irritable bowel syndrome included 11 studies, and the meta-analysis on the prevalence of irritable bowel syndrome in endometriosis included 6 studies (see flow chart in Figure 1).
Study characteristics
Overall 96,119 subjects were included in the main meta-analysis (11 studies) for endometriosis and irritable bowel syndrome association, with 18,887 endometriosis patients and 77,171 controls (patients without symptoms). The participants in the study by Ballard et al. (19) were already reported in the study by Seaman et al. (2), thus they were not added to the main meta-analysis twice. The meta-analysis on the prevalence of irritable bowel syndrome in endometriosis included 6,395 subjects. Almost all articles were published during the last decade, with two exceptions, which were published in 2005 and 2008. Of the 17 studies in this review, the majority were conducted in the United States, the United Kingdom, and Sweden. Table 1 describes the key characteristics of the included studies. Most studies used either Rome II (15), Rome III (16), Rome IV (17), or the visual analog scale for irritable bowel syndrome (VAS-IBS) (20) questionnaires to diagnose irritable bowel syndrome. Endometriosis diagnosis was confirmed either by laparoscopy or laparotomy. Each study had a quality assessment score between 5 and 10 on the Newcastle-Ottawa Scale (14), with most studies having a score of 7 or greater.
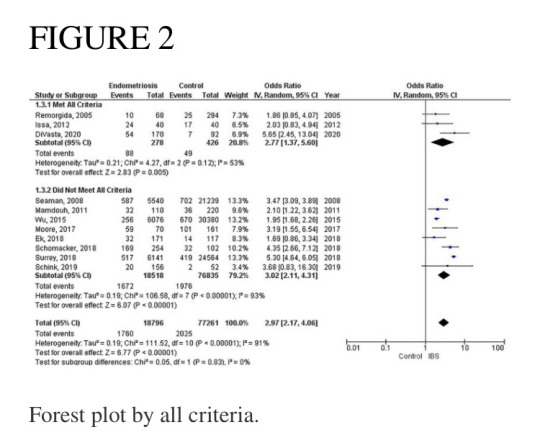
Meta-analysis of studies
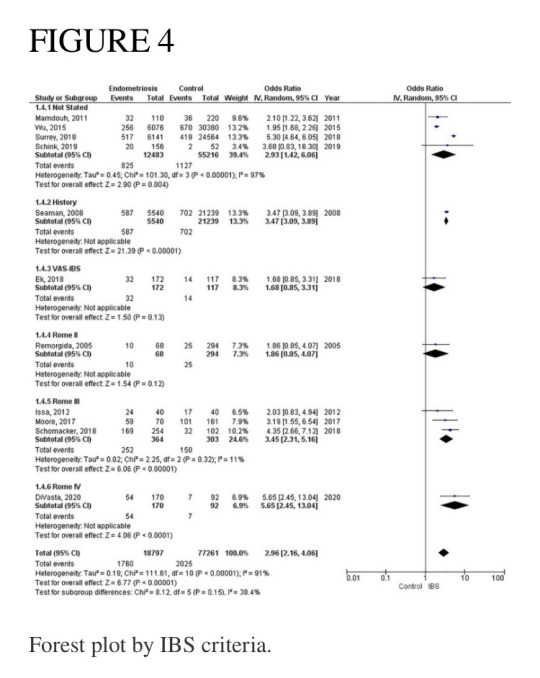
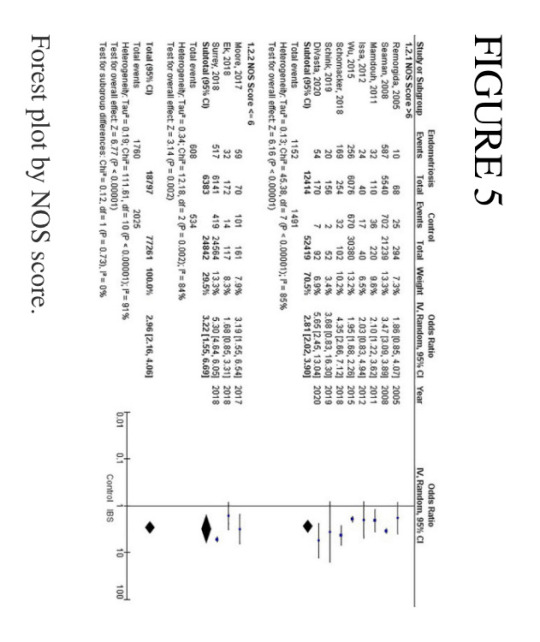
Of the 11 studies in the main meta-analysis (1–3, 10, 21–27), most were cohort and case control. Studies were conducted from 2005 to 2020, and sample sizes ranged from 80 to 36,456. In this meta-analysis the pooled odds ratio of endometriosis and irritable bowel syndrome was 2.97 (95% CI = 2.17 – 4.06), based on all selected criteria (see details in Figure 2). Odds ratio for the individual studies ranged from 1.69 (26) to 5.65 (10). There was a large heterogeneity in this study (I2 = 91%, [P < 0.00001]). In our subgroup analyses, the odds ratio for each subgroup was approximately 3, regarding endometriosis diagnosis (see Figure 3), criteria used for irritable bowel syndrome (see Figure 4), and NOS score (see Figure 5). Visual inspection of the funnel plot appears asymmetrical, suggesting the presence of publication bias (see Figure 7).

Endometriosis diagnosis
There were 9 studies (28,888 patients) in the meta-analysis that confirmed endometriosis surgically, and 2 studies (67,161 patients) that used the ICD-9-CM 617.x codes to diagnosis endometriosis. The random effects model showed a significant association between endometriosis and irritable bowel syndrome with a pooled odds ratio of 3.0 (95% CI = 2.18, 4.11) (see Figure 3).
Irritable bowel syndrome diagnostic criteria
Four studies (67,699 patients) did not state what criteria were used to diagnose irritable bowel syndrome, three studies (667 patients) used the Rome III criteria, and one study each used the following as their criteria: history (26,779 patients); VAS-IBS (289 patients); Rome II (362 patients), and Rome IV (323 patients). The random effects model shows a significant association between endometriosis and irritable bowel syndrome, with a combined odds ratio of 2.96 (95% CI = 2.16, 4.06) (see Figure 4).
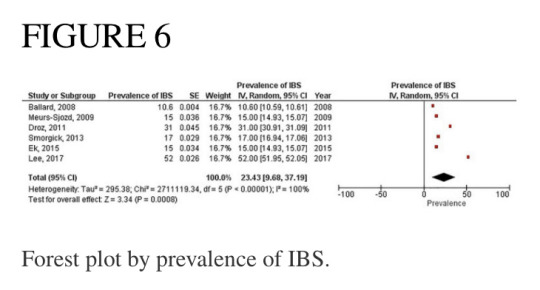
Pooled prevalence of irritable bowel syndrome
There were six studies (6, 19, 28–31) that estimated the prevalence of irritable bowel syndrome in people with endometriosis. These studies ranged in sample size from 101 to 5,540. The prevalence of irritable bowel syndrome in patients with endometriosis ranged from 10.6 to 52%, with a pooled estimate of 23.4% (95% CI = 9.7%, 37.2%) (see Figure 6).
Discussion
This systematic review and meta-analysis was designed to estimate the association of endometriosis and irritable bowel syndrome. Our literature search included all available original studies investigating irritable bowel syndrome and endometriosis, thereby allowing us to include a large number of subjects (17 studies; n = 96,974).
The most significant finding of our study is that the pooled analysis showed endometriosis was associated with an almost three-fold increase in risk of irritable bowel syndrome, and that more than 1 in 5 people with endometriosis have irritable bowel syndrome. Of particular significance, all 11 studies in the main meta-analysis showed a positive association of irritable bowel syndrome and endometriosis. Moreover, almost all subjects in this analysis were followed longitudinally, either retrospectively or prospectively, thus allowing for inference on temporality vis-à-vis risk factor and disease. In addition, five studies (n = 68,129) included in this meta-analysis showed a positive association of endometriosis and irritable bowel syndrome, even after adjustments were made for potential confounding variables (3, 10, 21, 25, 26). Furthermore, there were significant findings in our subgroup analyses based on diagnostic method for endometriosis, diagnostic criteria for irritable bowel syndrome, and NOS scores. More importantly, after the studies in the main meta-analysis were categorized based on the following criteria: longitudinal study design; surgical confirmation of endometriosis; Rome diagnostic criteria for irritable bowel syndrome; and NOS scores > 6, the pooled odds ratio was 2.77 (95% CI = 1.37, 5.60). Thus, this provides strong epidemiological evidence for the increased association of endometriosis and irritable bowel syndrome.
Endometriosis is characterized as a chronic, estrogen-dependent inflammatory disorder with the presence of endometrial tissue outside the uterine cavity (3). Affected areas encompass the pelvic peritoneum, ovaries, rectovaginal septum, the abdominal cavity, and the gastrointestinal tract.
Histologically, endometriosis can be characterized into superficial endometriosis, ovarian endometrioma (OE) and deep infiltrating endometriosis (DIE). DIE can present with severe symptoms as the lesions penetrate deeper into the peritoneum and thus produce more pain as compared to the superficial. DIE also tends to involve the uterine ligaments, pouch of Douglas, rectum, or vagina. OE on the other hand, is the most common type of endometriosis and located in the pelvic areas or along the intestines. Multifocality of such a variably distributed lesion thus, predisposes to a variable clinical presentation the patients.
The relationship between endometriosis and irritable bowel syndrome has not yet been fully elucidated, and multiple theories have been proposed. One such theory is the immunological linkage through increased mast cell activation seen in both conditions (32). The major hallmarks postulated in this immunological linkage are the abnormal levels of inflammatory cytokines and immune cell activation in the peritoneal cavity (33). Retrograde menstruation has been a plausible explanation, which causes the dissemination of menstrual blood containing endometrial cells into the pelvic cavity, thus triggering symptoms of irritable bowel syndrome (34). Specifically, in endometriosis, the activated mast cells have been activated near nerve endings within the pelvic and abdominal regions, and in irritable bowel syndrome they have been shown to be activated near the bowel mucosa (35). Moreover, Remorgida et al. (22) have found that the severity of gastrointestinal symptoms was directly related to the extent of infiltration of endometriotic foci in the bowel, and reversal of symptoms occurred after removal of those lesions. However, they did not find any conclusive evidence regarding endometriosis and predisposition to a specific subtype of irritable bowel syndrome.
Another theory for the increased association between these two disorders is through a hormonal linkage. This hormonal connection involves the presence of gonadotropin releasing hormone-containing neurons (36) and receptors for luteinizing hormone within the pelvic organs (37) and the enteric nervous system (38). It is hypothesized that the pain experienced in some people with irritable bowel syndrome could be as a result of the sex hormones found in afab people, as reports have shown a fluctuating exacerbation of symptoms of irritable bowel syndrome during menstruation (39). Likewise, it was observed that patients with endometriosis had worsening of gastrointestinal symptoms during the time of menstruation (30). It is posited that patients with endometriosis and irritable bowel syndrome both experience visceral hypersensitivity, which is likely to contribute to the severity of gastrointestinal symptoms (24). A large population-based study reported that the highest prevalence rate for endometriosis was for the 40–44-year age group (40), and Oka et al. reported that afab people between the ages of 30–39 years were more likely to have irritable bowel syndrome when compared to those less than 30 years old (8). Thus, the prevalence for both conditions peak at approximately the same age range, just around the beginning of the menopausal period. Moreover, postmenopausal patients with irritable bowel syndrome experience symptoms more severely than premenopausal patients with irritable bowel syndrome, most likely due to modulation in the brain-gut axis as a result of hormonal changes (41). Our study was not analyzed according the age of the patient.
Furthermore, a meta-analysis on the sex differences of irritable bowel syndrome reveals that afab people are more likely to experience abdominal pain when compared to amab people, and this may be because of sex hormonal differences (42).
Other important factors to consider when examining the relationship between endometriosis and irritable bowel syndrome are race/ethnicity and geographical region. In their study, Bougie et al. showed that Black people were less likely than White people to have endometriosis, and that Asian people were more likely than White people to have endometriosis (43). Similarly, Wigington et al. reported that Black people were less likely than White people to have irritable bowel syndrome (44). Thus, White people were more likely to have both endometriosis and irritable bowel syndrome when compared to Black people. Interestingly, of the 11 studies in our meta-analysis, only two studies stated the race of the participants (10, 27), and of these, the study by Schink investigated only Caucasian people (27).
As discussed previously, endometriosis is a chronic and multifactorial (genes, hormones, immune and environmental) and multi risk factor (family history, long menstrual cycle, low parity, and poor physical activity) associated disease (45, 46). An association between endometriosis and heavy metal sensitivity has been discussed in research that can potentially play a role in producing produce an IBS-like syndrome. Specifically, heavy metal nickel has been shown to interfere with estrogen and its receptors and thus plays a role in the pathogenesis of IBS. Researchers have even demonstrated a higher nickel level in endometriosis tissue (46, 47).
Recent global studies showed that the prevalence of irritable bowel syndrome varies from country to country, ranging from 0.2% in India to 29.2% in Croatia, using the Rome III criteria, and ranging from 0.4% in India and Ghana to 21.3% in United States, using the Rome IV criteria (8). Similarly, the global prevalence rates for endometriosis in the general population ranged from 0.7 to 8.6% (4). This highlights the importance of recognizing that irritable bowel syndrome and endometriosis can burden people of any race and from any country of origin, even though they can vary widely regarding presentation and response to treatment (43). Studies investigating endometriosis or irritable bowel syndrome individually were sparse for the geographical regions of South America, Central America, Africa, and Asia (8). However, the studies conducted in the United States reported the highest prevalence rate of endometriosis (48), and the highest prevalence rate of irritable bowel syndrome when using the Rome IV diagnostic criteria (11). Moreover, the studies conducted in the United States showed that people with endometriosis had the highest odds (5.65, 5.30) of having irritable bowel syndrome (see Figure 2). Thus, this points to further evidence that endometriosis is a significant contributory factor leading to irritable bowel syndrome. Needless to say, more investigation is needed regarding race/ethnicity and the association between endometriosis and irritable bowel syndrome.
Studies included in our meta-analysis used the Rome II, Rome III, and Rome IV criteria. The odds of irritable bowel syndrome in endometriosis increased with each subsequent updated version of the Rome criteria (odds ratio from 1.86 to 3.45 to 5.65), respectively. However, when interpreting these differences, one should also consider the significant heterogeneity that exists regarding study design and sample size. Moreover, recent studies have shown that the diagnostic outcomes for Rome II and Rome III criteria differ significantly (49), whereas there were comparable findings for Rome III and Rome IV criteria (50). Nevertheless, there is a markedly increased risk associated with endometriosis and irritable bowel syndrome, regardless of the criteria used to diagnose irritable bowel syndrome. The basis of the Rome criteria relies on its definition of irritable bowel syndrome in which recurrent abdominal pain is associated with defecation or a change in bowel habits (17). Thus, the Rome criteria classifies patients as different subtypes based on bowel habits: irritable bowel syndrome with predominant constipation (IBS-C), irritable bowel syndrome with predominant diarrhea (IBS-D), irritable bowel syndrome with mixed bowel habits (IBS-M) or irritable bowel syndrome, unclassified (IBS-U) (17). However, our data does not include information on these subtypes. Therefore, we cannot conclusively state whether endometriosis increases the risk of a specific subtype of irritable bowel syndrome over another, or if it increases the risk of all subtypes of irritable bowel syndrome.
Our meta-analysis included one study that used the visual analog scale for irritable bowel syndrome (VAS-IBS) to diagnose patients with irritable bowel syndrome. The VAS-IBS is a patient-centered questionnaire comprised of six categories: Abdominal Pain, Diarrhea, Constipation, Bloating and Flatulence, Abnormal bowel passage, and Vomiting and Nausea (20). The items in the VAS-IBS capture the main physical concerns people with irritable bowel syndrome might experience. All symptoms, except vomiting and nausea, support the diagnosis of irritable bowel syndrome. Even though the majority of studies in our meta-analysis used the Rome criteria to establish a diagnosis of irritable bowel syndrome, the VAS-IBS was shown to be an accurate and reliable questionnaire to diagnose irritable bowel syndrome (20).
Our literature search found two meta-analyses on endometriosis and irritable bowel syndrome (51, 52). Even though they had similar findings to ours regarding the increased association of endometriosis and irritable bowel syndrome, we believe that our review provides a more detailed analysis on various factors such as endometriosis diagnosis and irritable bowel syndrome diagnosis, and the pooled prevalence of irritable bowel syndrome in patients with endometriosis.
Strengths and limitations
Strengths of this meta-analysis include incorporation of all available studies, with subsequent sub-analyses. Both observational and interventional studies were included. In addition, most studies included in the meta-analysis have a quality assessment rating greater than 6. Moreover, by independently reviewing articles and selecting those that fit our criteria, we concluded with a large-scale study from various geographic regions of the world that include North America, Europe, Asia, Africa, and Oceana. This allowed us to interpret the risk of irritable bowel syndrome in people with endometriosis from an extensive and multiethnic perspective. In addition, this is the first meta-analysis to include a pooled estimate of the prevalence of irritable bowel syndrome in people with endometriosis.
Our study has a number of potential limitations. While select studies employed either the Rome II, Rome III, Rome IV, or the visual analog scale for irritable bowel syndrome (VAS-IBS) as their criteria to gather symptomatic data on irritable bowel syndrome, the majority of studies in this meta-analysis did not state what criteria were used to diagnose irritable bowel syndrome. The anatomical location of endometriosis and the IBS subtypes was not described as relevant description was not available in the included studies. Nonetheless, after subgroup analysis by whether criteria was used or not, pooled estimates revealed similar results in these groups. These estimates were also reflected in the overall combined odds ratio for all studies. Thus, omitting the criteria used for establishing irritable bowel syndrome did not pose any significant error in this analysis. Another limitation of this study is that data from the two largest retrospective cohort studies identified patients with endometriosis using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) 617.x codes, whereas all other studies stated that laparoscopy/laparotomy/clinical inspection was used as the mode of diagnosis. There is a significant variation in clinical diagnosis of endometriosis due to the costs and invasive diagnostic techniques including laparoscopic or surgical diagnosis. This has led to more reliance on radiological diagnosis for the same. Nevertheless, the surgical diagnostic methods are still considered the gold standard. Additionally, IBS diagnostic criteria are not based on standard guidelines or criteria. Most commonly used are the Manning and the Rome criteria which are possibly too general and vague for a specific diagnosis. Thus, an inevitable overlap occurs in the diagnosis of endometriosis and IBS (53).
Therefore, there was some inconsistency regarding identification of endometriosis. Nevertheless, our subgroup analysis regarding endometriosis diagnosis showed similar pooled estimates. However, despite these limitations, the diagnosis of irritable bowel syndrome remains a challenge with the fluctuation in symptoms and its symptoms mimicking other disorders like endometriosis (17).
Recommendations
Our database search revealed that no studies were conducted in Central America or South America, and only a solitary study each arose out of Africa and Asia. Thus, we recommend that studies be conducted in these regions of the world to give globally representative estimates of the risk associated with these conditions. Furthermore, since the majority of participants were investigated in retrospective cohort studies, we recommend that researchers conduct large-scale prospective cohort studies to investigate the risk of irritable bowel syndrome (preferably using the Rome IV criteria) in people with endometriosis (with diagnosis confirmed surgically). Moreover, we suggest that studies be conducted to investigate whether endometriosis predisposes to any specific subtypes of irritable bowel syndrome.
Conclusion
This review provides significant epidemiological evidence for the association between endometriosis and irritable bowel syndrome. People with endometriosis are three times more likely to have irritable bowel syndrome compared to people without endometriosis. Doctors should be mindful that patients with endometriosis can also have irritable bowel syndrome.
Data availability statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MN, MR, and SL contributed to the conception and design of the study. ME organized the database. PR and SN performed the statistical analysis. AV wrote the first draft of the manuscript. MN, MR, AV, and ME wrote the sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
#frontiers in medicine#pubmed central#endometriosis#gender neutral language#trans healthcare#afab health#endowarrior#ibs#irritable bowel disease#irritable bowel syndrome#scientific study#scientific news#comorbid conditions
1 note
·
View note
Text
something that really gets me about the doctor is that if your looking, it’s very obvious that they’re the same person across regenerations. the important things stick- the wit, the thinking under pressure, the emotional constipation, (which gets lessened over time, but that’s less on an on/off regeneration thing than you might think and more of a character arc thing so it further proves my point) their inherent love for humanity, their drama, their nonviolent tendencies.
all the obvious changes between the doctors are surface level, and if you go poking around you find that they’re all really similar to each other. I just love watching different peoples portrayals of one single character, and I think it’s really fun to see that regeneration really is mostly just changing the *body*, not the *soul*.
#also side note regeneration means that the time lords probably have provable scientific evidence of souls#which the inner nerd in me is freaking out about#doctor who#the doctor#new who#dr who#ninth doctor#tenth doctor#eleventh doctor#twelfth doctor#thirteenth doctor#fourteenth doctor#fifteenth doctor
1K notes
·
View notes
Text
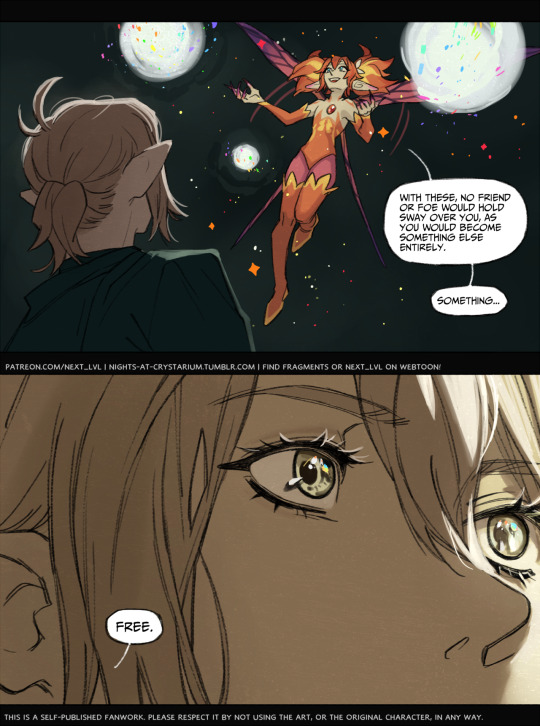







✧✦✧ “Fragments” - episode 40 ✧✦✧
Long live the king.
New reader? episode list on tumblr | webtoon
Read 4 more episodes: patreon | kofi
#yes the change of the art style is acknowledged in-universe#if you want a scientific explanation#*waves hand vaguely* dynamis#ffxiv#vivien rell#feo ul#titania#ffxiv: fragments#fragment ii: new world old friend#own: next lvl
861 notes
·
View notes
Text
Here's the thing.
If a fairy knocked at my door.... I would go and check for black mold, check the last thing I ate and maybe get a new carbon monoxide detector.
If a walrus turned up, the number of mental gymnastics are greater and it's less plausible that I'm hallucinating
#walrus#fairy#poll#walrus vs fairy#My first instinct would be a hallucination for a fairy tho#this is where I realize I've truly hit adulthood.#if I witnessed fantasy bullshit that can't be scientifically explained#i would buy a new CO detector
1K notes
·
View notes
Text



EVAN BUCKLEY | 4.01 - The New Abnormal.
#911#evan buckley#911edit#evanbucklyedit#911 abc#911gifs#evanbuckleygifs#daily911#buckling#trying new coloring… don’t know how I feel about it yet…#this scene lives rent free in my mind#looking so disrespectfully#for scientific purposes#literally on my knees for this man#strapped and loaded#I tried to be a decent human being when giffing this… I wanted to do a close up… but thought it was a bit much?
450 notes
·
View notes
Text

New scientific study shows drawing stick figures makes you better at art
#I'm having a little too much fun with my new lineart brush#Animation vs minecraft#avm#alan becker#avm fanart#still trying to nail their designs#avm red#avm blue#avm tsc#avm green#Avm yellow#avm purple#my art#art#ava#animation vs animator#THE SCIENTIFIC STUDY THING IS A LIE GUYS. i’m just making more art bc of the silly stick figures ;-;
568 notes
·
View notes
Text
What Earth Would Look Like to Alien Observers
1 note
·
View note
Text
"Vaccine efficacy against malaria is inadequate".
“Vaccine efficacy against malaria is inadequate”.
Written by Mark Cherky
post
Yesterday at 4:59 pm, up to date Yesterday at 6:16 pm
François Nosten, malaria expert and professor at Oxford University (here May 19, in Paris). Tudal Legrand/Le Figaro
Maintenance – This French doctor and researcher is fighting malaria in Southeast Asia, where treatment resistance has emerged.
With more than 500,000 deaths per year, malaria (or malaria) is one of…

View On WordPress
#Astronomy#Ecology#Fauna and Flora#Malaria#science#Scientific news#Sociology#the news#the planet#zoology
1 note
·
View note
Text
Prompt 146
So. Dan is a combination of both Danny and Vlad. Which he has never had an issue with before, but this is just frustrating. It’s not like he can’t deal with the fact the combination of the obsessions forms a protect family one, and he can deal with it. It’s not like he has one anymore.
Which is where the gobsmacked annoyance came from- he was planning on destroying his sort-of past-self, showing this was inevitable. But his obsession, apparently like his old man, decided instead to latch onto the kid, definitely not helped by the fact the brat is like two years dead. If that, he can’t recall, all his ghostliness knows is that the brat is a fucking baby.
He was going to destroy him, he swore! That had been the plan! So how the fuck did he get to helping the brat and the brat’s Jazz packing bags to run away? How the fuck is he responsible parent material, because he is damn sure he definitely isn’t.
Damnit. He’s taking this half-grown clone daughter too. Fuck Vlad, he can rot in that thermos and the Fentons can stay trying to figure out why the portal is no longer working. Being the responsible one sucks though, he’d rather go back to destroying the world but killing the league a second time also sounds like too much work right now. Damnit again.
#dcxdp#dpxdc#prompts#dad dan#Dan has acquired three sibling-children#At some point he’s going to be spotted by a time travelling hero who was sent back to stop him#Bad News: he was seen with the brats#Good News: the heroes now think he went evil after something happened to said brats#In Other News: they’re all committing to the bit#Dan has no clue how to raise teens or children or babies but he’s trying#Also he Will kill or maim if someone threatens any of these three#His Obsession really latched on hard- almost like he wasn’t able to fulfill it & it was driving him mad#Danny still calls & videos his friends & sends them gifts from all the places they’ve been#I think Dan should have a sun core for the poetic & scientific reasons#Jordan is in denial that He Is Dad Now
707 notes
·
View notes
Text
A Brief Summary of the Anaconda News
This post is about "Disentangling the Anacondas: Revealing a New Green Species and Rethinking Yellows"
Please note this post is not an analysis of the veracity of this paper, it is simply a summary of the findings.
This research team performed genetic testing on known species within the Anaconda genus (Eunectes). They are suggesting two things in their paper:
Two recognized species of yellow anacondas, E. beniensis and E. deschauenseei, are not significantly genetically distinct from E. notaeus. Note that E. notaeus has a slightly different pattern/morphology while the other two are more similar and differentiated mostly by location. They propose grouping these all three as one species.
The Green Anaconda, the heaviest species of snake, with a range all across the continent, may actually be two species. They found significant genetic differences between Northern and Southern Green Anacondas and are proposing they be made into separate species.
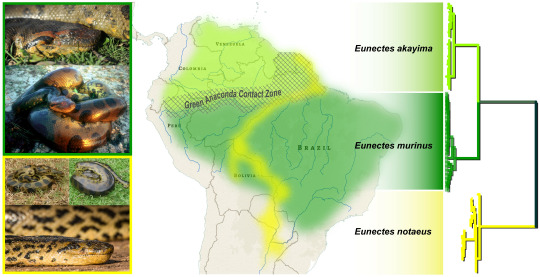
Graphical Abstract, sourced from linked paper, showing revised taxonomy. The Northern Green Anaconda's proposed scientific named is E. akayima. Akayima means "The Great Snake" in the indigenous language of the region.
The paper points out that there are conservation implications behind redefining these species. If the Northern Green Anaconda is accepted as a separate species, habitat loss may impact it more severely than the Southern, who has a wider range. For the the opposite reason, scientists may feel reluctant to group three previously defined species into one, as it could make it more difficult to protect the subcategories.
Read more: Nat Geo article on the findings, Bryan Fry Live Science article
Oh yeah, and one of the scientists who published the article posted this video of an Anaconda that's estimated to be 8 meters long and 200kg. Here's a still:

big dog
396 notes
·
View notes