#and therefore you can’t work with them to prevent viral transmission. at all
Text
If I’m being real, I know we’ve already lost the l war with covid because (not only are most non-disabled individuals refusing to mask at this point), but a large faction of people (1) don’t believe covid exists and/or (2) don’t believe viruses exist. If we can’t even agree on the basic scientific theories that guide public health… we are doomed. Point-blank and period.
#this is beyond vaccine controversy#some people don’t believe in viruses or that covid exists#and therefore you can’t work with them to prevent viral transmission. at all#so… *shrugs* at this point i guess we’ll just fuck around and find out#but my heart aches for all the innocent children with no choice in the matter. who are being disabled#i read a story about a five month old developing heart failure after infection#this is just the world we live in now#personal
4 notes
·
View notes
Text
Coronavirus: Information & Guidelines
What you can do now, and what to prepare for
There seems to be a lack of what-to-do suggestions on tumblr beyond handwashing, so I thought I’d put something together. I’ve never actually encouraged people to reblog something of mine before, but this might be the time. To be clear: I am not personally a public health expert of any kind. Both my parents are (epidemiology/global health degrees, worked for CDC) and I’ve run this by them. My information is coming from disease researchers on twitter and official public health guidelines online. Sources at the end of the post. This is mostly directed at people in countries where COVID-19 has been reported (I’m in the U.S.), but is not *yet* widespread in the community. Written Mar. 1st 2020, last updated 3/9 (shorter, helpful twitter thread here, helpful NPR article here)
General Info
Firstly, a lot of politicians are *still* trying to sugarcoat things, but it should be clear by now that the new coronavirus is spreading widely and will continue to do so. Because of the incubation period, and in the U.S. at least the delay in testing, the number of cases is almost certainly going to increase rapidly in the near future no matter what we do now. Official government sources are helpful, but its also good to look at what experts on viral epidemics who aren’t directly government-affiliated are saying. Their agenda is purely informing the public in the most constructive way possible, without politics getting in the way.
Two key points- COVID-19 can have a long incubation period (the time from when you catch the virus to when you start showing symptoms) and most people don’t get severe symptoms. Some are entirely asymptomatic, but most people get typical flu-like symptoms. Specifically, the early symptoms to watch out for are a fever and dry cough (meaning, a stuffy nose is probably just a regular cold). Its possible but unlikely to transmit the virus while asymptomatic, most transmission happens when you have heavier symptoms.
The most vulnerable people are the elderly (~ over 60) and those with preexisting health conditions (i.e. cardiovascular disease, respiratory condition, diabetes), or a simultaneous infection with something else (NOT kids in particular!) So far the mortality rate has been about 1-2% (compared to 0.1% for the general winter flu - yes, this really is worse). However, that might be an overestimate, both because people with mild cases aren’t getting tested (the denominator should be bigger), and because the early situation in Wuhan, where a lot of our numbers come from, was especially bad in regards to availability of healthcare.
This is an emotional, difficult situation. Don’t panic. The world didn’t end in 1918, and its not going to end now. But it is very serious, and we need to be thinking about it rationally, not pretending everything is just going to be okay, or uselessly pointing blame. Take care of your mental health, and check in with each other. Epidemics test our generosity and selflessness. Those qualities are needed right now, but don’t neglect yourself either.
What You Can Do Now
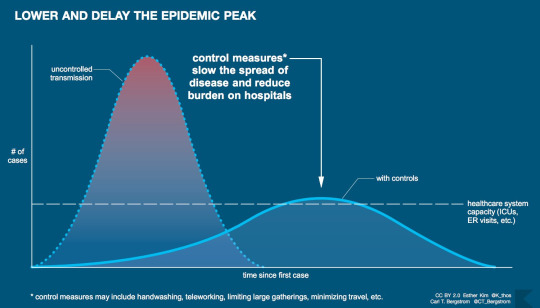
There is stuff everyone can do both to prevent yourself from getting infected, and to prepare if you do. ***The big picture to keep in mind is that the biggest risk of epidemics is that they overwhelm our system, especially our healthcare system. What I mean by this is that our society is built to deal with a certain volume of things happening at once- people buying groceries, getting sick, etc. If we suddenly all rush to do something, we overburden these systems and they won’t be there for the people who need them most. Therefore our goal is to slow down the spread of disease, buying time and lowering the overall burden on these systems. This is called “flattening the curve”. It looks like this, and I cannot stress how important this is.***
A very helpful thread on preparedness
Staying Healthy
Like similar viruses (think colds and flu), COVID-19 is mostly transmitted from person to person, usually by close contact but sometimes from an infected surface. More here.
Wash your hands. Everyone has heard this one- 20 seconds, soap all over your hands, wash the soap off. If you can’t wash your hands use an alcohol-based hand sanitizer (at least 60% alcohol). But handwashing is absolutely better. Also- cough into your elbow/shoulder, not your hand, and avoid shaking hands- try elbow bumps or maybe a polite nod instead! If you’re handwashing so much that you’re hands are threatening to crack and bleed though, consider washing more strategically or using hand sanitizer instead.
In combination with hand-washing- stop touching your face, especially while out! This takes practice, everyone does it all the time without thinking. A good practice is to avoid touching your face while out, then wash your hands thoroughly as soon as you get home.
Similarly, avoid touching surfaces as much as possible! Particularly bad are door handles, elevator buttons, that kind of thing. The virus can probably (based on studies of related viruses) last a while on these. Regular gloves can help a bit. Use a tissue then throw it away, use your elbow, etc.
Do Not buy face masks! There’s mixed evidence on whether they’re at all helpful when used by the general public to prevent catching a virus, but actual medical professionals who need them are facing shortages (that’s probably part of why so many healthcare workers got sick in Wuhan), so our buying them up is really bad. The only times you should be wearing them is if you yourself are sick (they do help then!) or if you’re looking after a sick person. Seek instruction in that case in how to use them properly. (Thread on why buying those fancy masks is not good).
If COVID-19 is in your community, try to stay 6 feet from people, which basically means going places as little as possible. See below.
Planning Ahead
Its also a good idea to prepare in case you need to self-quarantine. Self-quarantine is necessary if you’ve potentially been exposed to COVID-19, or if you’re sick but not enough to need to go to the hospital. Follow local guidelines- if there’s lots of transmission in your area, nonessential workers will probably be advised to stay home as much as possible.
If you’re able, get medication now. Don’t go crazy and buy out the drug store, just a reasonable amount. Try to get at least a month’s worth of any prescription medications. This can be hard at least in the U.S. - your doctor may well be able to prescribe more, but insurance companies and drug stores can be terrible. I’ve found trying a different drugstore can sometimes help. Try your best. They may also be reluctant to prescribe more to avoid causing shortages. Idk what the right answer is here.
Don’t go crazy and buy out the store, but start getting a little extra shelf-stable or frozen food. Even some root vegetables that will last a few weeks. You want enough for 2 weeks in case of self-quarantine, but you do NOT want to empty out stores. Panic buying is definitely a stress on the system. Just add a few extra things each time you shop. Don’t forget about pets. You can always eat the food and replenish it over time.
Make a plan with your family/community. If someone gets sick or needs to self-quarantine, is there a corner of the house they can stay in? Who can take care of them? etc. I haven’t focused on plans for schools/religious communities/workplaces etc but those are very important too! This is one place where keeping an eye on local and national news is important. In the U.S., for example, school systems are planning ways to make food available to kids if they’re not going to school.
If COVID-19 is starting to spread in your community, think about how else you can be a good community member. Cancelling nonessential doctor’s appointments, surgeries etc may be very important, for example. If schools are closed, can you help out neighbors with childcare? Do you have a cleaner who may need to be payed in advance if there’s a quarantine?
If You Might Be Sick/Need to Quarantine
See likely symptoms above. Remember, normal colds still exist, and if you go to the doctor for every one of those you will overwhelm the system.
Don’t just go to a hospital! Call ahead to your doctor/clinic/hospital and get instructions on what to do. Getting healthcare workers sick is something we really want to avoid. That said, DO get tested as soon as possible, and act as if you are contagious. The health coverage situation is the U.S. is not yet clear (and ofc its not something the current admin is eager to clarify). Hopefully testing will be covered financially by the government, but I can’t promise that at this time.
In the meantime, stay home and quarantined if you show any symptoms of illness if you possibly, possibly can. This is especially difficult in the U.S. if you don’t have sick leave/childcare, but please. Do your utmost.
Look after yourself. Skype/google hangouts/etc is great for keeping connected. Have some chocolate/chicken broth/other sick foods ready.
The Big Picture
Coronavirus/COVID-19 has not been declared a pandemic yet, but it probably will be before long. This is almost certainly going to get worse before it gets better. We don’t yet know if warmer weather will slow its spread, and a vaccine will probably take about 1-1.5 years to be developed and tested. As I mentioned before, the best thing we can do to keep the world working, minimize mortality, etc is to slow the spread as much as we can, and minimize the strain on the system. Hospitals are going to be overwhelmed. There aren’t infinite unoccupied beds or ventilators, or people to operate them, and supply chains could get disrupted. Thinking about these things is scary, and it will take time to adjust to what’s happening. Start that process now, and help everyone you know reach the point where they’re able to act, not panic. Another reassuring thing- if we slow the spread of COVID-19, in addition to fewer total people getting sick, you will soon have people who are recovered and almost certainly immune. These people will be invaluable as helpers in their communities.
Now that the practical stuff is out of the way, I want to say from a U.S. perspective that yes, our lack of social welfare other countries take for granted is going to hurt us. Lack of access to childcare, no guaranteed paid sick leave, and of course expensive healthcare are massive problems that will make it much harder to limit disease transmission. Help each other in any way you can, and vote for candidates that support implementing these policies! And of course, watch out for propaganda of all kinds, whether its using the virus as an excuse for racism, calls to delay elections, etc. So far my biggest concern is a lack of willingness to admit how serious this is, but we can do this. Lets put extra pressure on politicians to be honest and change policies to actually help people. But, yes, lets also stay united. We need each other now (just, you know, 6 feet apart).
A few sources
In general, the Guardian is a great, free, reliable source of news. In the U.S., NPR (website as well as radio) is another great source. The Washington Post and Seattle Times have made their coronavirus-related coverage open access, not sure about other national newspapers.
twitter thread from World Health Organization (WHO)
U.S. Center for Disease Control and Prevention (CDC) COVID-19 homepage (not being updated in some ways it should be, like total # of tests)
A reality check from some non-Governmental experts (basically, what governments don’t want to say yet, which is that this virus is going to spread, and the goal now is to infect as few people as possible, as slowly as possible. Read this.)
Why you should act now, not when things get bad in your area (we’re always operating on outdated information)
If you want the latest technical info, The Lancet (major medical journal group) has all of their content compiled here, open access.
I can do my best to answer questions (i.e. ask my dad) but those or other reliable, readily find-able sources should have you pretty well covered. Do let me know if anything on here is wrong or needs to be updated! Stay safe, stay positive, we can do this.
150 notes
·
View notes
Text
3/16/20 corona extra: cracking open cold covid facts
Announcements & Thank Yous
Thank you to everyone who’s messaged me or sent asks! Specific thanks go to:
@hoothootmotherf-ckers for checking my math on California
@ainwesley for sending me a source for more up to date information about Norway
@sister-cna-reader for sending me a source for Washington State and for suggesting I put closure information in here
Several people for correcting the misinformation I had about Vietnamese tests being ~1 hour, this is not true unfortunately. I apologize for the mistake and will keep you posted on testing developments as they occur.
@halcyonhowl for sending me sources and tips on North Carolina
Twitter users @molly0xFFF and @goblinartificer for helping me with the Wordpress site
Wordpress staff for support
To several other anons for suggesting I include closure/group restriction information, positive news of the day, and numbers of recovered patients. I’ve implemented all of these as much as possible.
If you have reliable information from a good source that I don’t seem to have, please shoot me a message/ask/pigeon!
Places now included in the newsletter are: Montana, Vermont, Delaware, Maryland, Washington, DC, Greece, North Carolina, South Carolina, Connecticut, Alabama, Tennessee, Arizona, Ireland, and Switzerland. Please send an ask or a message if you would like a place included!
There is now good news at the end of the newsletter because this is a lot, all the time. Please take care of your mental health. I am being one with the numbers so you don’t have to follow every minute, panic-inducing development. Also, there is good news related to the pandemic!
I have started a website for the newsletter, which I may be able to update in real-time? Uncertain. At the very least it’ll be a mirror of the tumblr content so you can skip around and not be stuck in scrolling hell since these are all mega chonky. Find it at coronaextranewsletter.com. If you know me from fandom, please be chill about my meatspace identity. Please.
Asks are now on for this blog, which should help things. Please send asks to this blog in the future, thank you!
Just The Numbers
Case numbers
Total cases: 167,511 (13,903 new)
Total deaths: 6,606 (862 new)
Mortality rate: 3.9%
China: 81,077 (29 new) cases, 3,218 deaths (14 new)
Mortality rate: 3.97%
Excluding China: 86,434 cases (13,874 new) and 3388 deaths (848 new)
151 countries/territories reporting cases, 4 are new today including: Uzbekistan (4), Uruguay (4), Rwanda (5), and Seychelles (2)
Rwanda is confirming local transmission at this time
Italy is reporting over 24,000 cases (3500 new) with over 1800 deaths
Iran is reporting approx 15,000 cases with over 800 deaths
South Korea, Spain, and Germany are reporting over 5,000 cases
SK reports 75 deaths/8236 cases
Spain reports 288 deaths/7753 cases
Germany reports 12 deaths/4838 cases
International/General News
Please stop buying toilet paper unless you are actively out of toilet paper. My butt thanks you in advance.
Vaccine testing began today in Seattle, Washington. This is the first phase of vaccine testing, where healthy volunteers take the vaccine to make sure it is safe.
The World Health Organization will stop separating Chinese cases as today is the first day that cases outside China outstripped cases inside China
France is now on lockdown
We are seeing the difference that social distancing can make in this epidemic: look at the difference between European countries that have and have not shut down.
Virology Corner
Today’s topic is recovery from COVID-19: how do we know that you’re recovered and that you’re no longer shedding the virus?
We know from Chinese studies that in people who recover clinically (i.e. when they stop feeling like death’s ass) they can shed virus for up to 20 days from the onset of symptoms. People who die shed virus until after they die.
Fortunately, we have a way of testing for active virus shedding: the same tests we use to detect viral genes at the start of an infection work to show that you are clear of infection!
This is super useful to know because we do not always test for cure in infectious diseases - for example, we don’t usually test flu patients for cure.
It’s pretty clear that when people have two negative tests separated by 24 hours, they are considered “recovered”. That’s the definition the WHO uses, and the one I will use here unless I specify otherwise.
Question Tuesday
Today’s question comes from @dasyuridae: “does the UK’s response make sense?”
HELL NO it does not
That’s the short answer
The long answer is that herd immunity works as a prevention strategy in certain types of infections, and this is not yet that kind of pandemic.
We use herd immunity to prevent against diseases when we have a vaccine for them. By immunizing everyone who can be immunized, we prevent those who cannot be immunized from getting and/or spreading the disease. This is essential to protecting people from things like measles and the flu.
If humans are the only host for a particular virus, we can even use herd immunity to totally delete the disease from planet earth. Ask smallpox. Oh wait. You can’t. We deleted it. (except for the highly secure samples in Russia and the USA, shh)
COVID-19 likely has a reservoir in animals so we can’t delete it, but once we have a vaccine, herd immunity will be awesome for preventing further outbreaks.
To have herd immunity now, likely upwards of 90% of the UK would need to get the virus and recover, thereby developing immunity. That is a bad idea because no health system can handle that.
A better way to do this is what most other countries are doing, mitigating spread by isolating affected people, offering lots of testing, and quarantining areas with lots of asymptomatic spread.
In conclusion, fuck Boris Johnson, he doesn’t understand how epidemiology works and that’s gonna hurt/kill a lot of people.
I have two elderly grandparents in the UK. Fuck Boris.
If you have questions, ask them and they’ll appear here in the next issue of corona extra!
Regional News (if you want somewhere added just let me know. Don’t be shy!! I highly recommend you just skip to your area if you don’t wanna be overwhelmed.)
Canada: last updated 3/16/20 at 9 AM EST
Total cases: 324 confirmed (+75), 17 presumed (+13), 1 death (3/9/20, no change), 5 recovered
Symptoms began for these cases between 1/15 and 3/13
13% of cases have required hospitalization (up from 12%)
74% (down from 79%) of cases are in travellers, and a further 6% in their close contacts
Affected provinces include: Alberta (56, +17), BC (73, +0), Manitoba (7, +3), New Brunswick (6, +4), Newfoundland and Labrador (1, +0), Nova Scotia (5, +2) Ontario (172, +69), PEI (1, +0), Québec (50, +9), and Saskatchewan (6, +4).
Totals here include confirmed and presumptive positives
4 cases in repatriated travellers (no change)
Restrictions/Closures:
No formal restrictions/closures at the federal level
Recommendation to avoid non-essential travel, particularly cruise ships
All international travelers directed to self-isolate for 14 days upon arrival
Alberta: last updated 3/15
56 cases, 17 new, 0 deaths
Community spread confirmed in Calgary
Restrictions/closures
K-12 schools and in-person post-secondary classes/training are closed
Licensed childcare facilities, out-of-school care programs, and preschools are closed indefinitely
British Columbia: last updated 3/14
73 cases, 9 new, 4 recovered, 1 death
Affected public health units include: Fraser, Interior, and Vancouver Coastal
Vancouver coastal has the most cases as far as I can tell
Clusters of infection have been reported at Lynn Valley Care Centre, Hollyburn House Retirement Residence, and Lions Gate Hospital (admin staff).
Manitoba: last updated 3/16 AM
7 cases, 3 new, no deaths
Visitor restrictions for hospitals are in effect
New Brunswick: last updated 3/16 1 PM
6 cases, 4 new on 3/15, no deaths
Affected areas include Zone 3
I don’t live in NB so I have no idea what this is beyond one of at least three zones
Schools are closed starting 3/16 for two weeks
Newfoundland & Labrador
1 case
Sorry that’s all the info I have
Nova Scotia
5 cases
Gatherings over 150 people are disallowed
Casinos are closed starting 3/16; VLTs are not allowed in bars
Childcare facilities are closed starting 3/17 through 4/3
Public schools are closed until 4/6
Long-term care facilities are closed to visitors until further notice
Ontario: last updated 3/16 at 10:30 AM local time
177 cases, 69 new, 5 recovered, no deaths
Affected public health units include: Durham (1), Halton (1), Hamilton (4), Niagara (1), Ottawa (3), Peel (4), Sudbury (1), Toronto (11), Wellington Dufferin Guelph (1), York (5)
Only cases from 3/16 on will be counted under here based on how the site works
P.E.I.: last updated 3/16 AM
1 case, in Queens County, connected to a cruise
Closures/restrictions
Libraries and community events are closed/canceled
Child care facilities are closed for two weeks starting 3/17
Public schools are closed until April 6
Québec: last updated 3/16 AM
50 cases, 9 new, no deaths
Affected regions include: Capitale Nationale (2, +0), Mauricie - Centre du Québec (3, +0), Estrie (3, +0), Montréal (18, +5), Chaudière-Appalaches (4, +1), Lanaudière (3, +1), Laurentides (3, +0), Montérégie (10, +1), and undetermined/outside Québec (4, +1).
State of health emergency as of 3/13
Closures/restrictions
Indoor gatherings of >250 people prohibited, many public buildings closed until further notice
Daycare/childcare facilities and all schools closed until 3/27
Elections scheduled for 3/15 have been rescheduled to after late April
Non-essential visits to hospitals and long-term care institutions are prohibited
Saskatchewan: last updated 3/15
6 cases
Sorry this is all I have right now
Greece: last updated 3/16 at 1:45 pm local time
Note: I do not speak Greek, and I therefore am struggling to find official data from somewhere more granular than the WHO. I’m sourcing most of this from the WHO and from Ekathimerini, but if you know where I can find better/more up to date info, please let me know. Thank you!
331 total cases, 141 new
4 deaths total (1 new on 3/15)
Restrictions/Closures:
All arrivals to the country are required to isolate for 14 days
Parliament has suspended all committee meetings and restricted each party to one MP in attendance at a time
Businesses are closed starting Wednesday 3/18, with the exception of gas stations, pharmacies, and groceries
Supermarkets are restricting the number of patrons to allow 1 person per 10 square meters
Ireland: last updated 3/15
169 total cases, 40 new, 2 total deaths
Deaths occurred on 3/11 and 3/14
Community transmission is confirmed
The following regional breakdown is available of the new cases: 25 eastern, 9 western, 6 southern
Restrictions/Closures
All pubs & bars are closed until March 29. House parties are strongly discouraged.
Schools, colleges, and childcare facilities are closed until March 29
Indoor gatherings of >100 people and outdoor gatherings >500 people are prohibited
State run cultural institutions are closed until further notice
The Netherlands: last updated 3/16 at 2 PM local time
I still do not speak Dutch, please please correct me if I get something wrong!
Seriously this is all run through Google Translate, I won’t take it personally
1413 confirmed cases, 24 deaths
278 new cases, 4 new deaths
Average age of decedents is 79, with a range from 59 to 94
Provinces affected include: Drenthe (16, +1), Flevoland (22, +3), Friesland (13, +3), Gelderland (135, +35), Groningen (10, +1), Limburg (149, +20), North Brabant (554, +108), North Holland (115, +25), Overijssel (36, +8), Utrecht (140, +31), South Holland (136, +26), and Zeeland (17, +1).
I think this is all of them based on a quick Wikipedia investigation?
There are 70 non-residents/unknown location patients
Restrictions/Closures
Schools, restaurants/bars, sports and fitness clubs, sex clubs, saunas, and childcare facilities are closed until April 6
Tae Bo is about to undergo a renaissance, I can feel it. Bring on the 80s outfits and the Jazzercise too!!
New Zealand: last updated 3/16 at 2 pm local time
8 confirmed cases, 2 probable cases
NO NEW CASES, YAY!!
The new patients from 3/15 are doing well and remain in quarantine; one was not hospitalized and the other has been released from hospital
Travel into and out of the country is restricted and those returning from overseas are asked to self-isolate for two weeks.
The Golden Princess has left port and the passenger in question tested negative.
Norway: last updated 3/16 at 8 pm local time
I still don’t speak Norwegian so if I screwed up lemme know
Everyone is still on lockdown, and apparently salty about being banned from their rural cabins
1332 cases, 3 deaths
53 hospitalized, 11 critical
96 new cases during the 24h of March 15
359 cases acquired in Norway, 752 acquired outside of Norway, the rest are undetermined. Community spread is confirmed.
Locations where people became infected include Austria (513), Italy (148), Switzerland (18), UK (14), Spain (14), France (10), USA (7), Iran (5), Germany (5), other countries with more than 3 cases (18), and other countries with less than 3 cases (58).
Breakdown of cases by area: Agder (87, +32), Innlandet (88, +16), Møre og Romsdal (20, +0), Nordland (11, +3), Oslo (292, +11), Rogaland (164, +37), Troms og Finnmark (23, +3), Trøndelag (74, +24), Vestfold og Telemark (69, nice, +21), Vestland (131, +13), and Viken (373, +95)
Yay no new cases in Møre og Romsdal!
Switzerland: last updated 3/16 at 5:45 pm local time
Whole country is on lockdown as of 3/16: no entry or exit until further notice (maximum of 6 months), schools are closed until 4/19, all events are canceled, and all personal service establishments are closed.
1,680 confirmed cases
14 deaths
United Kingdom in general: Last updated 3/16 at 9 AM local time
Boris is still a stupid shit, surprise surprise.
Fuck Boris
He’s ~encouraging~ people to stay home, which is kind of laughable given the severity of the pandemic and how strict other countries are having to be
1,543 total cases (+12.4%), 152 are new today
55 total deaths, 20 new today
England
1,196 total cases, 97 new
Affected UTLAs with at least 10 cases are as follows: Hampshire (55), Kensington & Chelsea (43), Westminster (37), Southwark (33), Hertfordshire (29), Lambeth (26), Barnet (25), Surrey (25), Oxfordshire (23), Camden (22), Hammersmith & Fulham (21), Brent (20), Hackney & City of London (20), Wadsworth (20), Devon (20), Essex (20), Ealing (18), Greenwich (18), Lewisham (17), Haringey (16), Sheffield (15), Birmingham (15), Leeds (14), Harrow (14), Nottinghamshire (14), Hillingdon (13), Hounslow (12), Merton (12), Tower Hamlets (12), Buckinghamshire (12), Cambridgeshire (12), Derbyshire (12), Kent (12), Northamptonshire (12), Walsall (11), Wolverhampton (11), Bromley (11), Islington (11), Sutton (11), Nottingham (10), Brighton & Hove (10), Oldham (10), Barking & Dagenham (10), Cumbria (10)
As things continue to escalate I will figure out a better way to display this
Deaths are not being reported by the PHS but I will do my best to split these out in the next few editions using news reports etc. It will hopefully be included by the 3/18 edition but no promises? If you have a good source for deaths by county/area, please let me know.
Scotland: last updated 3/16 at 2 pm local time
171 cases, 18 new, 1 death
Affected health boards are as follows: Ayrshire and Arran (7, +1), Borders (7, +0), Fife (7, +0), Forth Valley (10, +0), Grampian (12, +0), Greater Glasgow and Clyde (44, +5), Highland (2, +0), Lanarkshire (20, +4), Lothian (29, +1), Shetland (15, +4), and Tayside (17, +2)
Clearly the ones I listed yesterday were not all of them because…
Newly affected health boards are as follows: Dumfries and Galloway (1)
Wales: last updated 3/16 at 11 am local time
124 cases, 30 new
1 death (3/16)
Affected areas include: Blaenau Gwent County (5, +1), Bridgend County (1, +0), Caerphilly County (14, +3), Carmarthenshire County (7, +0), Ceredigion County (1, +0), City & County of Swansea (23, +1), City of Cardiff (11, +3), Conwy County (1, +0), Flintshire County (1, +0), Isle of Anglesey (2, +1), Monmouthshire County (7, +2), Neath Port Talbot (11, +0), Newport City (14, +7), Pembrokeshire (2, +0), Powys County (3, +0), Rhondda Cynon Taf County (2, +0), Torfaen County (2, +0), Vale of Glamorgan County (1, +0), and Wrexham County (2, +1).
Note that some of these numbers have changed more than you might see from looking at yesterday’s report; this is because residential locations of patients are being confirmed. 12 cases remain unlocalized and 2 are residents outside of Wales.
Northern Ireland: last updated 3/16 at 9 am local time
52 cases, 7 new
Health dept is not providing more detail than this at this time as far as I can tell
US in general: updated 3/16 at 4 pm local time (EST for CDC numbers)
3,487 total cases, 1,858 new with 46 states and DC reporting cases.
This is the start of the explosion of cases I’ve been expecting because of increased testing. This is a good sign that we’re catching more cases. It also indicates that there’s been spread going on for a while.
68 deaths, 27 new (1.95% mortality rate)
53 jurisdictions are reporting cases: 49 states, DC, Puerto Rico, Guam, and US Virgin Islands
Only West Virginia continues to not have cases. Impressive.
CDC is now recommending all in person gatherings with more than 50 people be canceled for the next 8 weeks. This sucks for me personally and probably a lot of you all too. Hang in there.
Trump told states that they should “try to get” ventilators and other critical supplies themselves. Fuck him too.
Not that it’s not the states’ jobs too, but also the federal aid and stockpile is like, a huge thing in disaster response (wait, oops, Trump cut that too)
Alabama: updated 3/16 at 1 PM local time
28 cases, no deaths
Affected counties include: Baldwin (1), Elmore (1), Lee (1), Jefferson (17), Limestone (1), Montgomery (1), Shelby (3), and Tuscaloosa (3).
Arizona: updated 3/16 at 11:36 AM
18 cases, no deaths
Affected counties include: Graham (1), Maricopa (8), Pima (4), and Pinal (5)
California: updated around 10 AM PST, 3/15/20
The Governor has recommended the following:
Those with chronic health conditions and those over 65 should shelter in place.
Gatherings over 250 people should be canceled.
Drinking establishments should be closed but restaurants can operate at 50% capacity.
Hospitals and long term care facilities should prohibit visitors except for end of life situations
Total cases not including the ones at Miramar (discussed below): 363, with 6 total deaths
Deaths have occurred in the following counties: Placer (1), Sacramento (2), San Mateo (1), Santa Clara (2)
The following counties report recoveries: Humboldt (1), San Benito (2)
The following counties report numbers of hospitalizations: Los Angeles (2), San Diego (8), Santa Clara (52)
Affected counties include: Alameda (18, +11), Calaveras (2, +0), Contra Costa (34, +5), Fresno (2, +0), Humboldt (1, +0), Imperial (2, +0), Los Angeles (94, +25), Madera (1, +0), Marin (9, +4), Orange (17, +3), Placer (8, +0), Riverside (15, +5), Sacramento (33, +4) San Benito (3, +0), San Diego (33, +25), San Francisco (40, +12), San Joaquin (8, +0), San Luis Obispo (3, +2), San Mateo (41, +9), Santa Clara (138, +47), Santa Cruz (9, +2), Shasta (1, +0), Solano (9, +3), Sonoma (5, +1), Stanislaus (3, +1), Tulare (2, +0), Ventura (5, +0), Yolo (2, +0)
Note regarding San Diego: The four federally quarantined people are not included in the county statistics.
Unaffected counties include: Alpine, Butte, Colusa, Del Norte, El Dorado, Glenn, Inyo, Kern, Kings, Lake, Lassen, Mariposa, Mendocino, Merced, Modoc, Mono, Monterey, Napa, Plumas, Sierra, Siskiyou, Sutter, Tehama, Trinity, Tuolumne, Yuba
Counties with confirmed community transmission include: Los Angeles, Marin, Orange, Riverside, San Francisco, San Joaquin, Santa Clara, Sonoma
Ventura County retested a possible case of community transmission and did not find evidence as of 3/16/20.
Newly affected counties include Amador (1), Nevada (1), San Bernardino (1), Santa Barbara (1)
Closures/Restrictions by County
Alameda: Shelter in Place until 4/7
Contra Costa: Shelter in Place until 4/7
Del Norte: Schools closed through 4/20
El Dorado: Schools closed through 3/20
Marin: Shelter in Place until 4/7
Mendocino: Modified schooling starting 3/17
Mono: Schools closed through 3/30, Alterra Mountain closed
Nevada: Schools are closed until 4/13, libraries closed until 4/12
Riverside: Schools & daycares are closed, gatherings >250 people prohibited
San Benito: Schools are closed
San Francisco: Shelter in Place until 4/7
San Luis Obispo: Alcohol sales on site are banned through 3/18
San Mateo: Shelter in Place until 4/7
Santa Clara: Shelter in Place until 4/7
Santa Cruz: Schools are closed until 3/20
Stanislaus: Gatherings of >1000 people are prohibited indoor and outdoor from 3/16 to 3/31
Tuolumne: Schools are closed from 3/16 to 3/30
Ventura: All schools and public libraries are closed starting 3/16 until further notice
Yolo: Many schools are closed at the local level. The County website has a list of closures: https://www.yolocounty.org/health-human-services/adults/communicable-disease-investigation-and-control/novel-coronavirus-2019
Counties with no closures/restrictions beyond those mandated by the state: Alpine, Amador, Butte, Calaveras, Colusa, Fresno, Glenn, Humboldt, Imperial, Inyo, Kern, Kings, Lake, Lassen, Los Angeles, Madera, Merced, Modoc, Monterey, Napa, Orange, Placer, Plumas, San Bernardino, San Diego, San Joaquin, Santa Barbara, Shasta, Sierra, Siskiyou, Solano, Sutter, Tehama, Trinity, Tulare, and Yuba
Drive through testing is available in Marin County
Colorado - last updated 3/15 at 145 pm local time
131 cases (+30), 1 death
Counties reporting deaths include: El Paso (1)
Affected counties include: Adams (6, +0), Arapahoe (15, +5), Denver (24, +4), Douglas (8, +4), Eagle (22, +4), El Paso (4, +1), Gunnison (8, +2), Jefferson (12, +3), Larimer (1, +0), Mesa (1, +0), Pitkin (2, +0), Pueblo (1, +0), Summit (1, +0), Weld (5, +2), with one case reassigned from Summit to unknown status
Out of state visitors who have tested positive are tallied separately, 15 in total (+0). They are located in the following counties: Pitkin (9), Eagle (2), Routt (1), Denver (1), unknown (2).
Confirmed community spread
Newly affected counties include: Boulder (3), Clear Creek (1),
Drive through testing is available in: Denver and Lowry
Residents of Gunnison, Eagle, Summit, Pitkin are recommended to minimize social contact
Anyone who visited the Colorado Springs Bridge center in late Feb-early Mar may have been exposed, call the DPH for more information
Events of >50 people are “strongly encouraged” to be canceled
Schools are closed in many places, local news is your best bet for this. I’ll try to include this eventually but it’s too much today.
Connecticut - last update 3/16 at 5 pm local time
41 cases
The following counties are affected: Fairfield (29), Hartford (4), Litchfield (4), New Haven (4)
Connecticut’s small, right? You can’t have more than 4 counties?
Restrictions/Closures
Gatherings >250 people are canceled through 4/30
No gatherings >50 people until further notice
Nursing home visits restricted
Schools closed through 3/30
Restaurants are carryout/drive through only through 4/30
Fitness/recreation centers and movie theaters closed through 4/30
Delaware: last update 3/16 at 1:40 local time
8 cases, 0 deaths
Affected counties include: New Castle (8)
Do you guys have any other counties?? This is gonna be another Rhode Island sitch, I think.
Restrictions/closures:
Events over >100 people are encouraged to cancel/reschedule
Schools closed through 3/27
District of Columbia: last update 3/16 AM
17 cases, no deaths
There’s no counties in DC, you can’t trick me
Restrictions/Closures
Food service/drinking establishments are restricted to <250 people, <6 people/table, no standing or bar seating, and tables separated by 6 feet
Nightclubs etc are closed
Florida - last updated 12:38 pm local time 3/16/20
155 (+40) cases and 4 deaths (+0)
Florida has not yet confirmed community transmission but it’s almost certainly happening. I’m no longer separating counties with and without confirmed community transmission because of that.
Affected counties include: Alachua (2, +1), Broward (39, +3), Charlotte (1, +0), Citrus (1, +0), Clay (3, +0), Collier (6, +1), Duval (5, +1), Hillsborough (5, +1), Lee (4, -1), Manatee (5, +1), Miami-Dade (23, +10), Nassau (1, +0) Okaloosa (1, +0), Orange (3, +0), Osceola (4, +2), Palm Beach (8, +3), Pasco (2, +0) Pinellas (4 +2), Santa Rosa (1, +0), Sarasota (3, +2) Seminole (4, +3), St. Johns (2, +1) Volusia (7, +2)
A case was removed from the record of Lee County. Since FLDPH changed their website, I don’t know where it was reassigned.
Newly affected counties include: Escambia (1) and Lake (1)
Georgia: last updated 3/16 at 11:21 AM
121 cases, 22 new, 1 death
Affected counties include: Bartow (9, +0), Charlton (1, +0), Cherokee (7, +1), Clayton (5, +3), Clarke (3, +1), Cobb (22, +3), Coweta (2, +0), Dekalb (10, +0), Dougherty (6, +0), Fayette (5, +0), Floyd (4, +0), Fulton (27, +7), Gordon (2, +0), Gwinnett (5, +1), Henry (2, +1), Lowndes (3, +1), Lee (2, +0), Newton (1, +0), and Polk (1, +0).
Newly affected counties include: Forsyth (1), Hall (1), Paulding (1), and Troup (1)
Illinois: last updated 3/14/20
105 confirmed cases, 16 new
Confirmed community spread
Affected counties include Champaign, Clinton, Cook, Cumberland, DuPage, Kane, Lake, McHenry, Sangamon, St. Clair, Whiteside, Winnebago, and Woodford
ILDPH is not publishing numbers per county. I will try to include this for tomorrow’s update.
Newly affected counties include: Peoria and Will
Closings/Restrictions
Bars and restaurants are closed (except for carryout and drive through) until 3/30
All gatherings >50 people prohibited
Gyms/fitness centers/clubs/theaters are closed
DMV is closed! I personally hate the IL DMV so this isn’t like, sad news in particular…..
Community colleges and public schools are closed - like in other places I will attempt to include county-by-county news soon.
Iowa: last updated 3/16
Total cases: 22, 4 new
Affected counties include: Carroll (1, +0), Dallas (1, +0), Harrison (1, +0), Johnson (15, +1), and Pottawattamie (1, +0)
Newly affected counties include: Allamakee (2) and Polk (1)
Community spread confirmed
Closures/restrictions
Schools closed for 4 weeks starting 3/16
Kansas: last updated 3/16
11 confirmed cases (+3), 1 death
Affected counties include: Johnson (8, +3), Wyandotte (1, +0), Butler (1, +0), Franklin (1, +0)
Closures/Restrictions
Schools closed through 3/23
Kentucky: last updated 3/16 at 4 pm local time
22 cases (+4), 1 death (+1)
Counties reporting deaths: Bourbon (1)
Counties reporting recoveries: Harrison (1)
Affected counties include: Bourbon (1), Clark (1), Fayette (5), Harrison (6), Jefferson (6), Montgomery (1), and Nelson (1).
Closures/Restrictions
Restaurants and bars closed to in-person service
State Capitol closed to nonessential personnel
Schools are closed statewide
Louisiana: last updated 5:30 pm 3/16
136 cases reported, 45 new
3 deaths, 1 new
Parishes affected: Bossier (1, +0), Caddo (3, +2), Jefferson (21, +9), Lafourche (2, +1), Orleans (94, +29), St. Bernard (2, +1), St. Charles (3, +1), St. John the Baptist (1, +0), St. Tammany (6, +2), and Terrebonne (2, +0)
New parishes affected: Ascension (1)
Maryland: last updated 10 AM 3/16
37 cases, 0 deaths
Counties affected: Anne Arundel (1), Baltimore (4), Baltimore City (1), Carroll (1), Charles (1), Harford (2), Howard (1), Montgomery (15), Prince George’s (10), Talbot (1)
Community spread confirmed
Exposure risk advisory for Lorien Elkridge
Closures/restrictions
Casinos, racetracks and other gambling situations are closed
Gatherings >250 people prohibited
All schools closed through 3/27
Senior centers closed until further notice
Massachusetts: last updated 4 pm 3/16
197 cases (59 new)
Affected counties include: Barnstable (1, +0), Berkshire (11, +2), Bristol (2, +1), Essex (8, +3), Middlesex (83, +18), Norfolk (36, +8), Suffolk (36, +9), and Worcester (6, +4)
Newly affected counties include: Hampden (1) and Plymouth (3)
10 cases are undetermined location
14 hospitalizations (+3)
They finally stopped making me download a goddamn word doc, thank you Massachusetts <3
Michigan: last updated 3/16 2 pm
54 cases (+21) 0 deaths
Affected counties include: Bay (1, +0), Charlevoix (1, +0), Ingham (1, +0), Kent (5, +2), Macomb (6, +4), Monroe (1, +0), Montcalm (1, +0), Oakland (14, +5), St. Clair (2, +1), Washtenaw (7, +3), and Wayne (14, +6)
Wayne County includes Detroit (6 cases)
Likely community transmission
Closures/Restrictions
Bars and restaurants are carryout/drive through only
Public spaces (casinos, theaters, etc) closed
Public offices open by appt only
Minnesota: last updated 3/16 at 12:00
54 cases (+19)
Affected counties include: Anoka, Carver, Dakota, Hennepin, Olmstead, Ramsey, Renville, Stearns, Waseca, Washington, and Wright
Newly affected counties include: Benton and Blue Earth
County numbers are not currently being provided by MN dept of health, just ranges. Hennepin county has >20 cases.
I will start working on these numbers for tomorrow’s edition
Drive through testing available in Olivia
Montana: last updated 3/15 at 7:45 pm
6 cases
Affected counties not being reported at this time, I’ll try to untangle that tomorrow
Closures/Restrictions
Public schools closed until 3/30
Many counties have closed libraries, these will be included tomorrow
Nebraska: last updated 3/16
Community transmission confirmed: many locations in Douglas County are potential places where transmission has occurred; if you live or have traveled to Douglas County (Omaha), please check the Douglas County COVID-19 monitoring site at: https://www.douglascountyhealth.com/latest-news.
There were also two exposures in Knox County on March 5, at basketball games at Lincoln Southwest HS and North Star HS.
18 cases (+1), no deaths
Affected counties include: Cass (1), Douglas (15) and Knox (1)
New Jersey : last updated 3/16 at 2 pm
178 cases (+109), 2 deaths (+1)
Affected counties include: Bergen (61, +36), Burlington (5, +2), Camden (3, +1), Essex (20, +13), Hudson (19, +14), Mercer (6, +5), Middlesex (17, +7), Monmouth (14, +6), Morris (6, +3), Ocean (3, +2), Passaic (8, +6), Somerset (5, +4), and Union (8, +7)
Newly affected counties include: Hunterdon (1)
Closures/Restrictions:
No gatherings >50 people
New York: last updated 3/16 at 3 PM
950 cases (+337), 2 deaths
Affected counties include: Albany (12, +7), Broome (1, +0), Delaware (1, +0), Dutchess (10, +6), Erie (6, +3), Herkimer (1, +0), Monroe (10, +8), Nassau (109, +30), Orange (11, +5), Rockland (16, +4), Saratoga (5, +2), Schenectady (4, +3), Suffolk (63, +22), Tioga (1, +0), Tompkins (1, +0), Ulster (7, +2), Westchester (220, +42)
NYC has 463 cases (194) as of 3/16 at 11:30 am
Areas/counties reporting deaths are: NYC - Brooklyn (1), Rockland (1)
Newly affected counties include: Allegany (2), Greene (2), Montgomery (1), Onondaga (1), Ontario (1), and Putnam (2)
Drive through testing in New Rochelle, Long Island, Staten Island, and Rockland County
Closures/Restrictions
Bars, restaurants, entertainment venues closed
No gatherings >50 people
Public schools closed until 4/1
Village elections delayed until 4/28
The governor dunked on the federal response hard in his press conference, which was great tbh
North Carolina: last updated 3/16 at 10 AM
33 cases, 0 deaths
Affected counties include: Brunswick (1), Cabarrus (1), Chatham (1), Craven (1), Durham (1), Forsyth (2), Harnett (2), Johnston (2), Mecklenburg (4), Onslow (1), Wake (14), Watauga (1), Wayne (1), and Wilson (1).
Advisory for an exposure at Raleigh convention center on March 8
Please call Wake County if you were there, they are tracking exposures
Closures/Restrictions
Schools are closed statewide until 3/30
Events >100 people canceled
Ohio: last updated 3/16 at 2 pm
50 confirmed cases, 14 new
14 hospitalizations
Affected counties include: Belmont (2, +0), Butler (6, +0), Cuyahoga (24, +10), Franklin (3, +0), Lorain (3, +1), Lucas (1, +0), Medina (2, +1), Stark (3, +1), Summit (2, +0), Trumbull (2, +0), Tuscarawas (1, +0)
Newly affected counties include: Geauga (1).
Closures/Restrictions
Bars/restaurants are closed
Gatherings >50 people canceled
Oregon: last updated 3/15 at 12 PM
39 cases (+3), 1 death
Counties reporting deaths: Multnomah (1)
13 hospitalized at time of positive test
The following counties are affected: Clackamas (1, +0), Deschutes (4, +1), Douglas (1, +0), Jackson (2, +0), Klamath (1, +0), Linn (10, +1), Marion (2, +0), Multnomah (1, +0), Polk (1, +0), Umatilla (2, +0), and Washington (13, +0).
Newly affected counties include: Yamhill (1).
Pennsylvania: last updated 3/16 at 7 pm
Gritty continues his dark work.
76 total cases (+13)
Counties affected include: Allegheny (5, +2) Bucks (5, +1), Chester (2, +0), Cumberland (5, +0), Delaware (7, +0), Lehigh (1, +0), Luzerne (1, +0), Monroe (8, +2), Montgomery (30, +6), Northampton (1, +0), Philadelphia (8, +2), Pike (1, +0), Washington (1, +0), Wayne (1, +0)
Newly affected counties include: NONE TODAY! \o/
Closures/restrictions:
Restaurants and bars are closed in the following counties until 3/30: Allegheny, Bucks, Chester, Delaware, and Montgomery
Presumably this will deter Gritty
Rhode Island: last updated 3/16
21 confirmed cases (+1), no deaths
Chanston High School West had an exposure; 1700 people are currently quarantined after this exposure
I will attempt to sort out county level data soon, since apparently y’all have counties
South Carolina: last updated 3/16 at 3:50 pm
33 cases, no deaths
Will try to find more granular data for tomorrow’s edition
South Dakota: last updated 3/16
10 confirmed cases (+1), no deaths
Affected counties include: Beadle (1, +0), Bon Homme (1, +0), Charles Mix (1, +0), Davison (1, +0), McCook (1, +0), Minnehaha (4, +1), and Pennington (1, +0)
No community transmission
Tennessee: last updated 3/16 at 2 pm
52 cases, no deaths
Affected counties include: Campbell (1), Davidson (25), Hamilton (1), Jefferson (1), Knox (1), Rutherford (1), Sevier (1), Shelby (2), Sullivan (1), and Williamson (18)
Texas: last updated 3/16
57 total cases, 1 new.
Highly likely that there has been community transmission, unconfirmed currently
Affected counties include: Bell (1, +0), Bexar (3, +2), Brazoria (2, +0), Collin (6, +1), Dallas (8, +0), El Paso (1, +0), Fort Bend (9, +0), Galveston (1, +0), Gregg (1, +0), Harris (10, +0), Hays (1, +0), Lavaca (1, +0), Matagorda (1), Montgomery (3, +0), Smith (4, +1), Tarrant (3, +0), and Travis (2, +1)
Newly affected counties include: None today!
Utah: last updated 3/16
29 total cases
Affected health districts include: Davis County (4, +1), Salt Lake county (18, +2), Southwest Utah (1, +0), Summit County (11, +9), and Weber-Morgan (2, +1)
Newly affected districts include: Tooele (1), Utah County (1), and Wasatch County (1)
First case of community spread identified on 3/14/20, in Summit County
Exposure at Wasatch High School identified
Schools: canceled
Mormons: canceled
Skiing: canceled
Public places in SLC: Canceled
Vermont
12 cases total (+4)
Affected counties include: Bennington (3), Chittenden (4), Orange (1), Springfield (1), Washington (1), and Windsor (3)
Hospitalizations are reported in the following counties: Bennington (3), Chittenden (1), Springfield (1), Washington (1), Windsor (1)
Closures/restrictions:
No gatherings >50 people or >50% capacity, whichever is lower
Schools are closed starting 3/18
Virginia: last updated 3/16
51 cases total, 6 new
Affected counties/cities include: Alexandria City (2, +1), Arlington (9, +1), Chesterfield (2, +1), Fairfax (10, +0), Hanover (1, +0), Harrisonburg City (1, +0), James City (10, +2), Loudoun (5, +0), Prince Edward (1, +0), Prince William (3, +0), Spotsylvania (1, +0), and Virginia Beach City (4, +0)
Newly affected areas include: Stafford (1) and York (1)
Washington: last updated 3/16 at 3:45 PM
Things are still super rough. Hang in there.
904 total cases (+262), 48 deaths (+8)
Current mortality rate: 5.3%
Deaths have occurred in the following counties: Grant (1, +0), King (43, +8), and Snohomish (4, +0).
Affected counties include: Clark (4, +1), Columbia (1, +0), Grant (3, +1), Grays Harbor (1, +0), Island (7, +1), Jefferson (3, +2), King (488, +101), Kitsap (7, +4), Kittitas (3, +0), Pierce (38, +12), Skagit (7, +3), Snohomish (200, +46), Spokane (3, +0), Thurston (4, +1), Whatcom (3, +1), and Yakima (4, +0).
126 cases are currently unassigned to a county. These are expected to resolve in the coming days, hopefully.
Newly affected counties include: Lewis (1) and Lincoln (1)
Closures/restrictions: widespread, will have county-by-county info soon.
Wisconsin: last updated 3/16 at 2 PM
47 total cases (+14), 0 deaths
Recovery is being reported by the following counties: Dane (1)
This is updated every Friday, next update expected 3/20
Affected counties include: Dane (10, +4), Fond du Lac (11, +0), Milwaukee (13, +6), Pierce (1, +0), Racine (1, +0), Sheboygan (3, +0), Waukesha (3, +0), and Winnebago (3, +2)
Newly affected counties include: Outagamie (1) and Wood (1)
Closures/restrictions
Schools closed starting 3/18 for minimum of two weeks
Today’s Hot Tips
Social distancing can be really crappy for people who are prone to feeling isolated. Try to schedule time to hang out virtually, especially if you’re stuck at home alone. I highly recommend the Jackbox party games to stream over Discord, or tabletop RPGs played through a service like Roll20. My friends and I have been doing all these things and it’s helping a lot!
If you have a favorite quarantine activity, let me know and I can include it in the next issue!
Everyone knows that sex is an option, there’s gonna be a lot of November, December, & January babies
That said, make sure your quarantine supplies include contraception and condoms and stuff. If you have a uterus, you can buy emergency contraception (plan B) online and it’s real handy to have around in a situation like this.
Hand washing is so hot right now
Hand Washing Song of the Day
If you hate singing happy birthday while you wash your hands, I certainly do, try Barrett’s Privateers!
Sing the first verse and chorus to feel like a pirate and follow CDC handwashing guidelines! Use soap and water for maximum virus-murdering.
Good News, Everyone!
The Shedd Aquarium took its penguins around to explore the whole aquarium since there were no people, and boy were those lil guys fascinated by everything!
Check it out here: https://twitter.com/shedd_aquarium/status/1239248971006185478?s=21
Chill Cat Corner
This one’s a classic: “where’s the babies???”
https://www.youtube.com/watch?v=2rELs4jl64k
I wish I could summon a bunch of smol kittens to scream at me like this
About this newsletter
I’m Emily, I’m a 4th year med student w/ a degree in molecular biology. I started this because I’m an infectious disease and epidemiology nerd and also all my friends have questions & anxiety. Hi internet!
The archive/proper website is located at coronaextranewsletter.wordpress.com.
All this info is sourced from regional & national public health organizations, plus the WHO. It’s as up to date as humanly possible. I’ve been beaming information about this outbreak directly into my brain 24/7 but I still miss stuff. Please let me know if I miss something!
Most public health departments stop updating their information around 4-5 PM local time on weekdays. That means that the earliest this will come out is around 6 PM Pacific time on weekdays going forward. On weekends things update more sporadically and earlier, so who knows what I’ll do then, but I’ll do my best.
The excellent title is courtesy of @marywhal and the Wordpress site is courtesy of @molly0xFFF and @goblinartificer on Twitter, thank you all!
For More Information
JHU COVID-19 data center: https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
List of peer-reviewed publications: https://www.cdc.gov/coronavirus/2019-ncov/publications.html
WHO daily sitrep: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200316-sitrep-56-covid-19.pdf?sfvrsn=9fda7db2_2
WHO FAQ: https://www.who.int/news-room/q-a-detail/q-a-coronaviruses
CDC cases in the US: https://www.cdc.gov/coronavirus/2019-ncov/cases-in-us.html, this also has links to each state’s health dept
#corona extra#coronavirus#coronavirus pandemic#covid19#covid corner#public health#pandemic facts#no panic#just facts
94 notes
·
View notes
Text
Got lured onto twitter to support BLM and afterwards got embroiled in conversation over the UK’s #sexban. I’m tired of twitter, and it’s hard to express yourself in a few characters, so I thought I’d share some thoughts here.
Which is really just the tories declaring outright that sex between people living in two households is now illegal and punishable with a £50 fine.
Given that households haven’t been allowed to mix, you’re nto allowed into anyone’s house and the 2m rule still applies, it was always ‘banned’ - those of us in that situation were already aware of our obligations. FWIW I’ve followed every recommendation before and after lockdown, because I’m a doctor and I want to decrease ANY spread as much as possible, until things are relaxed enough that our meeting isn’t a particularly big risk to others in the context of what’s going on. It’s not fun, and it kind of feels like the govt forgets people like you when its revising its plans and opening Primarks, but you think of the patients, and you continue.
But this law in particular pissed me off today. It was already covered in existing rules - so why explicitly banning sex? What message are they trying to send? That they have no intention to ease the lockdown on our personal lives any time soon? How are they going to enforce the fine? Are we going to turn every time a lockdown rule is broken into something we fine people for, and will that just make people see it as something minor if they can afford the fine?
Obviously, we have to have a cut-off somewhere. We have to try to decrease transmissibility where we can. And for the most part the initial rules seemed fairly sensible. But telling people they can’t be intimate with 1 person, but they can have a barbecue with 6, go shopping, watch footballers touch each other, and travel to work and sit with colleagues feels like the rules are arbitrary and not particularly fair.
Weirdly I’ve been roped into twitter conversation with some ex-immunology researcher re: the fact that covid viral RNA has been found in semen say 14 days after infection. And that apparently this therefore means the policy isn’t arbitrary and it isn’t prioritising the economy over personal lives. I have to disagree. They argue that this is about sexual transmissibility, but I disagree. The thing is, this isn’t really about transmissibility. We don’t know enough about when covid stops being transmissible. We don’t know if a negative test means you can’t transmit it any more. I welcome any research that helps us gauge risk and know more about how we can stop spreading the virus. But we don’t know what kind of viral load allows for infection via different routes. How can we separate the risk from PIV (etc) transmission from a recently infected person from the risks of them spreading it through aerosolised droplets?
Now, when I was sick, I was allowed back to work with vulnerable patients after 8 days, despite my OH consultant being clear that we’re not really sure how long people are infectious for, and the government recommendations appear to be arbitrary. Other places recommend 14 days. Clearly we have to say at some point that people are allowed out, and that their risk of transmission has at some point.
But a rule telling me that I can go back to work after 7 days with a cough, but can’t have sex with my BF (in case - what? one of us is an asymptomatic suffer and less than 14 days after infection?) is not based on evidence, and it does, from the outside appear rather arbitrary. I was concerned to go back to work. I’m still concerned about how many people have been rushed back to work. I’m concerned over how people who’ve been exposed in the community are meant to self isolate, but HCW aren’t even tested unless we show symptoms - imagine all the asymptomatic spread. This isn’t about whether some of us go a bit longer without sex (frankly, it’s barely about the sex at all), it’s about how inconsistent the rules are, and how the government apply the letter of the law in cases where the risk is low and yet allow people who were shielding out, and force them back to work where they may not be adequately protected.
Because I guess even if you’re asymptomatic you need to never have sex EVER just in case you spread infection. But is it really more likely to be from uh... mixing genital fluids, or from coughing in each other’s faces? And why can’t the answer simply be to use a condom if we’re worried about fluids? But only if you’re in different households. Those in the same household have never been advised not to have sex, though they have been advised to isolate themselves if possible, if they are sick. But in general the rules allow people within the same household to live normally. They accept that people in the same household will likely get infected -though in reality they shouldn’t cos it’s not 100%. Imagine if we told everyone in the same household ‘well, there’s a chance you might not pass it to each other, so can all of you sit 2m apart and not touch’?. That’d probably reduce infections too, by a certain number, but it’d be pretty unpopular and hard to enforce.
But if we’re going to pretend this is about sexual transmissibility ... sexual health policy has never been “don’t have sex” - not in the longterm. That’s not how we treat people with HIV or any other communicable disease - we tell people to use protection and get tested. We try to manage risk as much as possible. And as our planning reaches more chronic stages, we’re going to have take much more advice from those who’ve been managing infectious illness, particularly in the context of people’s intimate lives, for a hell of a lot longer than we have. Your sexual health colleagues can tell you how to engage people with infection prevention, how to avoid marginalising people like sex workers (anyone remember them? yep, they sill exist and still need to survive). This bugs me not only cos it’s a bit of a personal fuck you to couples in my position who’ve been following the rules from the start, but also because it’s not based on sexual health practice.
All the recommendations have to be based on some kind of risk assessment -the 2m rule. How many households you can mix with. Whether going to someone else’s garden is safe. Everything we allow - even shopping, even accepting a takeaway - has some kind of risk - it may be low, but it is not zero. I’m worried that the government has given the message that it’s perfectly safe to go back to work (it’s not, commuting and social distancing still carries risk) or shop and do other outdoor activities (again, still some risk) or send kids to school (even if the kids don’t have conditions, their teachers or parents may be at risk!). They’ve relaxed a lot of rules all at once. I’m terrified for the vulnerable.
I’ll socially distance for as long as I have to if it keeps people safe, but I have real concerns about how they’ve gone about relaxing things, and there are a lot of reports about people not following social distancing advice. After all the relaxed rules, and with the Cummings debacle, there’s a danger that people will all think the rules no longer really apply.
What annoys me is that they appear to be inconsistent and arbitrary. And I no longer have any faith that the government is makng decisions based on scientific advice, and risk stratifying appropriately.
I honestly think they are making much riskier decisions in order to open the economy, and then nominally keeping lockdown in ways that only limit social contact in small but meaningful ways because that’s not the economy.
42 notes
·
View notes
Text
COVID19 FAQ/CLARIFICATION
(From Singapore's Ministry of Health: https://www.moh.gov.sg/covid-19/faqs)
[Relevant as of 27 March 2020]
Introduction
Hello everyone. Firstly I would like to inform you that I am from Singapore, and we are fighting alongside everyone against the Corona virus. Secondly, all the information I present will be taken directly from my country's government and the link has been provided above as I am not a medical student. Thirdly, please do take this pandemic seriously as it is NOT a laughing matter, and I hope that you keep calm and positive througout this situation.
What are Coronaviruses?
Coronaviruses (CoV) are a large family of viruses causing illnesses ranging from the common cold to pneumonia (a more severe lung infection). A new coronavirus strain has been identified in Wuhan, China. Coronavirus Disease 19 (COVID-19) has caused cases of severe pneumonia in China and cases have been exported to other countries and cities.
How does COVID-19 spread?
There is human-to-human transmission of COVID-19. For now, the evidence suggests spread is mostly via droplets. The virus is carried within droplets emitted from an infected person over a short distance, such as when the person coughs or sneezes. If these droplets come into contact with the eyes, nose or mouth of another person, directly or indirectly through hands that have come into contact with these droplets, the other person may become infected. Members of public are advised to remain vigilant and observe good personal hygiene practices.
What are the symptoms of COVID-19?
The symptoms of COVID-19 infection are similar to that of regular pneumonia. Typical symptoms include fever, cough and shortness of breath.
What is the treatment for COVID-19?
Supportive treatment is provided based on the patient’s clinical condition. No proven specific treatment or anti-viral drug for COVID-19 is currently available.
Is the disease deadly? How is it compared to SARS?
The situation is evolving and many characteristics of the virus and how it may affect people are still unclear. However, current information suggests COVID-19 can cause severe disease and death in 2% to 3% of people with the infection, especially among the elderly and those people with underlying health problems or compromised immune systems.
Who should wear a mask? What kind of mask should I wear?
For the general public who are not having any symptoms at all and are well, there is no requirement to wear a mask.
As a good hygiene measure, people who are not well and have respiratory symptoms should wear a mask so that they do not spread any infection to other people. Anyone who has symptoms should see a doctor as soon as possible, to make sure that they remain well.
In the case of COVID-19, we know that the infection is spread through droplets. Wearing a mask will protect other people when someone with respiratory symptoms coughs or sneezes, as the mask would trap those droplets and prevent those droplets from spreading and disseminating.
As such, a surgical mask is sufficient for this case and fulfils the important function of preventing a spread if worn properly. The mask should be changed if it gets soiled or stained.
Why do healthcare professionals use an N95 mask and don full personal protective equipment (PPE), including goggles, then?
When dealing with infectious diseases, healthcare workers are required to wear the personal protective equipment (PPE), including N95 and goggles, as they are in close contact with patients and their bodily fluids.
As such, the PPE is needed to create a barrier between healthcare workers and the infectious agents from the patients, and to reduce the risk of transmitting micro-organisms from healthcare workers to patient(s).
How long is the incubation period? If somebody travels to cities with confirmed cases, how many days of no-symptoms after the travel, will he/she then be considered clean and disease-free?
Data from cases in China suggests that the incubation period is around 14 days.
Therefore, travellers are advised to monitor their health closely for at least 2 weeks upon return to [home country]. You are advised to seek medical attention promptly if you feel unwell, and to also inform your doctor of your travel history.
Summary for COVID-19 FAQ
I have compiled the FAQ to be useful to an international audience so if you are a fellow Singaporean please head to the website and remain updated as often as possible. If you are NOT from Singapore, you may still check the link for relevant general information if it helps. Please note the relevancy of this information and stay up to date with the latest news.
COVID-19 Personal Experiences FAQ
(Circulated among Singaporean Citizens)
Introduction
I have compiled a list of relevant information that fellow Singaporeans have been sharing among themselves. I hope people would take the time to read these anecdotes to understand the gravity of the situation, and that it may help in your understanding of this virus. Please do also take the information with a pinch of salt as they have not been confirmed/checked by any authority.
Annecdote from a Singaporean Patient's Family
"Make no mistake. When loved ones are removed from your home by ambulance because the virus has hit them hard, you are not going to be able to follow them there, sit by their hospital bed and hold their hand. You are not going to be able to pop in at 7.00 pm for visiting hours. They are going to have no one other than exhausted and brave hospital staff to see them through days or weeks of barely breathing through a ventilator until they either die or recover. They are not going to be well enough to text you.
You are not going to be able to phone the ward to check in on them regularly (staff will be too busy for that). During that time, they will be completely alone, while you sit at home waiting to hear whether they have made it through.
Imagine that person is someone you love dearly. Because it's going to be a reality for many in the coming weeks.
And if that person in hospital happens to be you, going through that ordeal completely alone, it would be nothing less than terrifying.
Please stay home and only go out if absolutely necessary. Social distancing is imperative right now for your family and mine."
Day by Day Symptoms of COVID-19 from Patients
Day 1-3
Common Cold
Itchy throat
No fever, no fatigue & good eating & drinking seems normal.
Day 4
Painful throat, more itchy/scratchy. The body is weak, & seems intoxicated
Hoarseness (husky voice)
36.5° body temperature
Start to decrease appetite include not wanting to eat & drink water
Mild head pain/headache
Mild diarrhea
Day 5
Inflammation of the throat (You might see white dots or patches in the back of your throat-might be red & swollen). Hoarseness until you lose your voice
36.5°-36.7° body temperature
The body is weak (body malaise) and joint pain(the pain is like rheumatism or gout)
Day 6
37° body temperature (fever)
A dry cough (coughing without phlegm)
Painful throat while eating, worsens when you swallow & when you talk
Body malaise, nausea or recurrent vomiting
Mild breathing problems/shortness of breath
Hand & finger pains
Vomiting (throwing up) and diarrhea (watery bowel movements)
Day 7
High fever from 37.4°-37.8°
Persistent cough with phlegm
Headache/head pain along with diarrhea
Persistent diarrhea
Persistent vomiting
Day 8
Fever 38° above
Breathing problems/Shortness of breath
Persistent cough
Headache, more joint pain, that passes in the lower back like pain in the buttocks (lumbar strain)
Day 9
No relief at all
Fever is getting high temperature
Persistent cough with phlegm
Worsening shortness of breath
If you feel all these, please go to the nearest Hospital's for testing and medication. There is no need to be afraid of having checked on what is being felt to avoid the loss of life for no reason.
Summary
I would like to emphasise that this information is NOT checked by authorities so please do not panic unnecessarily. Please do not spread panic or quote this information without citing its lack of source. Remain calm, and please direct yourself to the nearest hospital/clinic if you are unwell. If that is unavailable to you in your country/state and you are sick, please socially distance yourself at home until the medical team's/hospitals call you in.
Concluding Statement
I understand that for some of you information, medical facilities/equipment, and perhaps even basic necessities (such as food/water/shelter) are unavailable, seeing as I am interacting with an international audience. However, I would like to implore you to stay calm while you treat this matter with the utmost seriousness. This is because anxiety among the people would only cause prices in goods to sky rocket, and you will only endanger people when the market starts bidding wars for things such as equipment and medicine.
So please, firstly do not conduct mass-purchase of anything unnecessarily as it would only result in an inflation in prices for important goods. An example would be chloroquine which is NOT a cure for COVID-19, as mass purchase will place/is placing people suffering from lupis and arthritis at a disadvantage. These patients need that medication, unlike some of us who don't even know if it works against COVID-19.
Seccondly, please do not treat social distancing as a joke. Lives are at stake, and this means any form of contact with the virus will infect your immune system. While travelling overseas might seem fun due to the low priced flight tickets or because of spring break, this virus will infect you and your loved ones if you do not take the necessary precaution. This means sharing of food, untensils, clothes et cetera should be avoided to prevent the virus from infecting others and yourself. Some of you might want to die, but others don't so please, mind their consent if you can't be bothered with yours.
Thirdly, (I do apologise if I sound distinctly more annoyed as I type this, seeing how humanity consistently tries my patience) the corona virus is not an excuse for you to be racist or classist. I repeat: the corona virus is not an excuse for you to be racist or classist. While the COVID-19 virus did originate from China, it is not the 'chinese virus' and it was not borne from skin tones or genetics. It was instead born from the unlucky evolution of bacteria/germs that China so happened to win said lottery for.
This is the country that is developing and making the ventilators you need to stay alive. This is the country that has developed a new technique to keep you breathing/blood circulating if you are unable to do so. This is the country that gave the world 42 days to prepare for an enslaught of cases. They have no reason to help you: the virus was not made by them and you are not their citizen. But they are helping, and the least you can do is to be kind. (And if anyone would like to argue I'd like to quote Wu Chuanpu of supply chain Vedeng on ventilators that "the expansion of the production line is very time-consuming and resources-intensive," and "also involves personnel training. It is too cumbersome.")
So please, do not judge, do not be prejudiced and for the love of god be kind. The world is suffering, and people are dying. This is not the time to be fooling around or placing other things as your priority, whether it be your job, your fun, or your god damn xenophobia.
The priority is containment and survival.
To rebuild humanity you need humanity to exist in the first place. Stop being stupid, selfish and a damn ass hole about it. The virus isn't picky about its victims. It isn't going to care how much money you have, what your skin colour is, or what your age is. We have to work together and fight the common enemy. So stop taking sides and pick this one, the one where everybody wins. Don't be a fucking wuss cowering in the face of this virus. Mankind is resourceful, you are resourceful! Focus on what you can do and not what you can't! Take action, even if it seems small, because the small ones definitely count.
Keep yourself safe, signal boost this for people in need of information, and let's fight hard! Cause I'm definitely welcoming 2021 with all you people on this weird blue site.
Hugs and kisses from the fucking little red dot in Asia bitches ♡
2 notes
·
View notes
Text
Wuhan Coronavirus Looks Increasingly Like a Pandemic, Experts Say

The Wuhan coronavirus spreading from China is now likely to become a pandemic that circles the globe, according to many of the world’s leading infectious disease experts.The prospect is daunting. A pandemic — an ongoing epidemic on two or more continents — may well have global consequences, despite the extraordinary travel restrictions and quarantines now imposed by China and other countries, including the United States.Scientists do not yet know how lethal the new coronavirus is, however, so there is uncertainty about how much damage a pandemic might cause. But there is growing consensus that the pathogen is readily transmitted between humans.The Wuhan coronavirus is spreading more like influenza, which is highly transmissible, than like its slow-moving viral cousins, SARS and MERS, scientists have found.“It’s very, very transmissible, and it almost certainly is going to be a pandemic,” said Dr. Anthony S. Fauci, director of the National Institute of Allergy and Infectious Disease.“But will it be catastrophic? I don’t know.”In the last three weeks, the number of lab-confirmed cases has soared from about 50 in China to 14,000 in 23 countries; there have been over 300 deaths, all but one in China.But various epidemiological models estimate that the real number of cases is 100,000 or even more. While that expansion is not as rapid as that of flu or measles, it is an enormous leap beyond what virologists saw when SARS and MERS emerged.When SARS was vanquished in July 2003 after spreading for nine months, only 8,098 cases had been confirmed. MERS has been circulating since 2012, but there have been only about 2,500 known cases.The biggest uncertainty now, experts said, is how many people around the world will die. SARS killed about 10 percent of those who got it, and MERS now kills about one of three.The 1918 “Spanish flu” killed only about 2.5 percent of its victims — but because it infected so many people and medical care was much cruder then, 20 to 50 million died.By contrast, the highly transmissible H1N1 “swine flu” pandemic of 2009 killed about 285,000, fewer than seasonal flu normally does, and had a relatively low fatality rate, estimated at .02 percent.The mortality rate for known cases of the Wuhan coronavirus has been running about 2 percent, although that is likely to drop as more tests are done and more mild cases are found.It is “increasingly unlikely that the virus can be contained,” said Dr. Thomas R. Frieden, a former director of the Centers for Disease Control and Prevention who now runs Resolve to Save Lives, a nonprofit devoted to fighting epidemics.“It is therefore likely that it will spread, as flu and other organisms do, but we still don’t know how far, wide or deadly it will be.”In the early days of the 2009 flu pandemic, “they were talking about Armageddon in Mexico,” Dr. Fauci said. (That virus first emerged in pig-farming areas in Mexico’s Veracruz State.) “But it turned out to not be that severe.”An accurate estimate of the virus’s lethality will not be possible until certain kinds of studies can be done: blood tests to see how many people have antibodies, household studies to learn how often it infects family members, and genetic sequencing to determine whether some strains are more dangerous than others.Closing borders to highly infectious pathogens never succeeds completely, experts said, because all frontiers are somewhat porous. Nonetheless, closings and rigorous screening may slow the spread, which will buy time for the development of drug treatments and vaccines.Other important unknowns include who is most at risk, whether coughing or contaminated surfaces are more likely to transmit the virus, how fast the virus can mutate and whether it will fade out when the weather warms.The effects of a pandemic would probably be harsher in some countries than in others. While the United States and other wealthy countries may be able to detect and quarantine the first carriers, countries with fragile health care systems will not. The virus has already reached Cambodia, India, Malaysia, Nepal, the Philippines and rural Russia.“This looks far more like H1N1’s spread than SARS, and I am increasingly alarmed,” said Dr. Peter Piot, director of the London School of Hygiene and Tropical Medicine. “Even 1 percent mortality would mean 10,000 deaths in each million people.”Other experts were more cautious.Dr. Michael Ryan, head of emergency responses for the World Health Organization, said in an interview with STAT News on Saturday that there was “evidence to suggest this virus can still be contained” and that the world needed to “keep trying.”Dr. W. Ian Lipkin, a virus-hunter at the Columbia University Mailman School of Public Health who is in China advising its Center for Disease Control and Prevention, said that although the virus is clearly being transmitted through casual contact, labs are still behind in processing samples.But life in China has radically changed in the last two weeks. Streets are deserted, public events are canceled, and citizens are wearing masks and washing their hands, Dr. Lipkin said. All of that may have slowed down what lab testing indicated was exponential growth in the infection.It’s unclear exactly how accurate tests done in overwhelmed Chinese laboratories are. On the one hand, Chinese state media have reported test kit shortages and processing bottlenecks, which could produce an undercount.But Dr. Lipkin said he knew of one lab running 5,000 samples a day, which might produce some false-positive results, inflating the count. “You can’t possibly do quality control at that rate,” he said.Anecdotal reports from China, and one published study from Germany, indicate that some people infected with the Wuhan coronavirus can pass it on before they show symptoms. That may make border-screening much harder, scientists said.Epidemiological modeling released Friday by the European Center for Disease Prevention and Control estimated that 75 percent of infected people reaching Europe from China would still be in the incubation periods upon arrival, and therefore not detected by airport screening, which looks for fevers, coughs and breathing difficulties.But if thermal cameras miss victims who are beyond incubation and actively infecting others, the real number of missed carriers may be higher than 75 percent.Still, asymptomatic carriers “are not normally major drivers of epidemics,” Dr. Fauci said. Most people get ill from someone they know to be sick — a family member, a co-worker or a patient, for example.The virus’s most vulnerable target is Africa, many experts said. More than 1 million expatriate Chinese work there, mostly on mining, drilling or engineering projects. Also, many Africans work and study in China and other countries where the virus has been found.If anyone on the continent has the virus now, “I’m not sure the diagnostic systems are in place to detect it,” said Dr. Daniel Bausch, head of scientific programs for the American Society of Tropical Medicine and Hygiene, who is consulting with the W.H.O. on the outbreak.South Africa and Senegal could probably diagnose it, he said. Nigeria and some other countries have asked the W.H.O. for the genetic materials and training they need to perform diagnostic tests, but that will take time.At least four African countries have suspect cases quarantined, according to an article published Friday in The South China Morning Post. They have sent samples to France, Germany, India and South Africa for testing.At the moment, it seems unlikely that the virus will spread widely in countries with vigorous, alert public health systems, said Dr. William Schaffner, a preventive medicine specialist at Vanderbilt University Medical Center.“Every doctor in the U.S. has this top of mind,” he said. “Any patient with fever or respiratory problems will get two questions. ‘Have you been to China? Have you had contact with anyone who has?’ If the answer is yes, they’ll be put in isolation right away.”Assuming the virus spreads globally, tourism to and trade with countries besides China may be affected — and the urgency to find ways to halt the virus and prevent deaths will grow.It is possible that the Wuhan coronavirus will fade out as weather warms. Many viruses, like flu, measles and norovirus, thrive in cold, dry air. The SARS outbreak began in winter, and MERS transmission also peaks then, though that may be related to transmission in newborn camels. Four mild coronaviruses cause about a quarter of the nation’s common colds, which also peak in winter.But even if an outbreak fades in June, there could be a second wave in the fall, as has occurred in every major flu pandemic, including those that began in 1918 and 2009.By that time, some remedies might be on hand, although they will need rigorous testing and perhaps political pressure to make them available and affordable.In China, several antiviral drugs are being prescribed. A common combination is pills containing lopinavir and ritonavir with infusions of interferon, a signaling protein that wakes up the immune system.In the United States, the combination is sold as Kaletra by AbbVie for H.I.V. therapy, and it is relatively expensive. In India, a dozen generic makers produce the drugs at rock-bottom prices for use against H.I.V. in Africa, and their products are W.H.O.-approved.Another option may be an experimental drug, remdesivir, on which the patent is held by Gilead. The drug has not yet been approved for use against any disease. Nonetheless, there is some evidence that it works against coronaviruses, and Gilead has donated doses to China.Several American companies are working on a vaccine, using various combinations of their own funds, taxpayer money and foundation grants.Although modern gene-chemistry techniques have made it possible to build vaccine candidates within just days, medical ethics require that they then be carefully tested on animals and small numbers of healthy humans for safety and effectiveness.That aspect of the process cannot be sped up, because dangerous side effects may take time to appear and because human immune systems need time to produce the antibodies that show whether a vaccine is working.Whether or not what is being tried in China will be acceptable elsewhere will depend on how rigorously Chinese doctors run their clinical trials.“In God we trust,” Dr. Schaffner said. “All others must provide data.”
Read the full article
0 notes
Text
Zerobase creates private, secure, and automated contact tracing using Amazon Neptune
This is a guest post from the Zerobase Foundation. In their own words, “The Zerobase Foundation is a nonprofit organization whose mission is to build free, open-source public health technology for the good of communities around the world. Zerobase’s privacy-first contact tracing platform empowers individuals, communities, and local officials to stop the spread of COVID-19.” As the COVID-19 pandemic runs its global course, widespread testing for the virus alone won’t be sufficient to contain its spread. Tests are lagging indicators; by the time someone tests positive, they might have already exposed dozens of others, even before developing symptoms. Communities are looking to implement effective contact tracing, which is a crucial part of modern pandemic response that allows each test to apply not just to one person, but to the hundreds they may have exposed, directly or indirectly. Contact tracing is the identification of disease-spreading interactions between individuals in a community. When someone tests positive, tracing helps pinpoint the others, called contacts, they may have infected, so that the contacts can self-isolate or get tested, thereby preventing the further spread of disease. Historically, contact tracing has been a labor-intensive and manual process. That’s because contact tracing has typically only been needed at a local scale—such as during an outbreak of respiratory diseases like pertussis (whooping cough) in a particular town—or because it requires highly sensitive communication with contacts—such as while tracing the spread of HIV. In these cases, public health officials call down a phone list or even travel door to door, interviewing those that have tested positive to see whom they may have infected. COVID-19 has rendered manual contact tracing impossible. The virus is highly contagious, spreading transparently between individuals and even indirectly through contact with infected public objects like ATMs. Worse, studies show that an infected person is most contagious in the days before they develop symptoms—if they develop them at all—meaning that there is an extremely narrow critical window in which isolating someone who may have been exposed can be helpful. For more information, see the following studies: Temporal dynamics in viral shedding and transmissibility of COVID-19 Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany Asymptomatic Transmission, the Achilles’ Heel of Current Strategies to Control Covid-19 Presymptomatic Transmission of SARS-CoV-2 — Singapore, January 23–March 16, 2020 Because of this, even if we could do massive-scale manual contact tracing, it would be ineffective. If a public health official called you after you tested positive, you could never hope to name everyone you might have exposed at your grocery store, pharmacy, or bank. Conducting effective contact tracing for a highly contagious disease such as COVID-19 requires a more sophisticated, digital approach. Zerobase is a privacy-first, universally accessible COVID-19 contact tracing platform built on a Quick Response (QR) code mesh network that is deployed at the community level (towns, cities, regions, or health systems) to slow the spread of the coronavirus. Zerobase is free and open source, licensed under the Apache 2.0 License. You don’t download an app, Zerobase doesn’t monitor GPS location or Bluetooth interactions, and everyone can enroll immediately. In fact, Zerobase is working with public health experts to develop robust systems for individuals who do not have access to smartphones, for example carrying or downloading to feature phones anonymous QR codes that can be scanned at participating locations. The same privacy protections – like anonymity by default and robust data security – can be expected by every Zerobase user, smartphone-carrying or not. A user takes a few seconds to scan a code at a participating location in exchange for the peace of mind that they are never tracked and that the information they transmit is only the information they provide. Our solution runs on AWS, and our fundamental data structure—the contact graph—is stored in Amazon Neptune, a powerful, fully managed graph database service. Data are encrypted in transit and at rest using industry standard data security procedures, including relying on AWS’s robust suite of data protection layers. With Zerobase, you can receive notifications of possible exposures in real time, and public health officials are empowered with insights about the current and future dynamics of the virus, which helps contain outbreaks and plan for a safe return to normalcy. How Zerobase contact tracing works Partnering with local governments, Zerobase asks essential businesses like grocery stores and pharmacies to post Zerobase QR codes at their entrances and points of sale. Each QR code is unique and is associated with that specific business. When you visit the location, you scan the QR code with your smartphone’s camera, for example as you check out with your groceries. This prompts the Zerobase website to open in a browser, which associates a random, anonymous identifier that persists in browser storage with the specific QR code that was just scanned. As more individuals scan codes and therefore associate their phones with check-ins, we can build up a fine-grained, anonymous contact network around a community. You never install an app, no software runs in the background, and your GPS locations and Bluetooth interactions are never tracked. And individuals without smartphones can simply carry anonymous QR code printouts with them to be scanned by any employee when they visit a participating location, and these individuals can be alerted to possible exposure via phone, email, or through trusted institutions, should they opt in to these communications. Zerobase is the only tracing solution that is universally accessible in this way. One challenge in anonymous contact tracing is ingesting verified positive diagnostic information into the system. Apps developed thus far must rely either on self-reporting test results or on healthcare workers to perform laborious data entry. Our use of QR codes also offers an attractive way to avoid the inaccuracy and inefficiency with these approaches. Zerobase provides unique, single-use QR codes on paper stickers to COVID-19 testing facilities. When a patient arrives for a test, they receive one of these codes, which is attached to their basic intake form. They scan the code, associating their device (and all its past check-ins) with that particular form and test. When their test comes back (whether minutes or days later), a physician, nurse, or other responsible healthcare professional can retrieve the patient’s form from their medical record and scan the attached code, thus linking their device (and its trace) with a verified positive diagnosis. Because these special codes are treated as sensitive medical materials (similar to prescription drugs or patient records), the facilities’ built-in security infrastructure and chain of custody protocols can be used without modification to prevent tampering with the testing codes. When a positive test is associated with a device, the race begins. Zerobase uses Neptune to query efficiently for the locations that the patient checked into and the other individuals who may have been there at the same time or shortly thereafter. These individuals are known as first ring exposures, and they can receive a request—still anonymously—to isolate or get tested the next time they check in at a location. But Zerobase can go even further. We can calculate real-time risk scores for both individuals and locations that take into account the totality of the community contact graph—not just the first ring—by leveraging more advanced machine learning (ML) algorithms developed through collaborative research with the Max Planck Society. Our models show that the contact tracing protocol and ML techniques developed and used by Zerobase could flatten the curve in a community up to 60%, proving effective even at levels of adoption under 50%. Projection showing the potential impact of Zerobase contact tracing in reducing the number of infected people in a community By deploying these community-level ML models on the AWS ML stack of Neptune, Amazon Simple Storage Service (Amazon S3), and Amazon SageMaker, we go beyond what an app using Bluetooth on a phone could do; because such apps generally only record pairwise data between a single device and its contacts, they can’t deliver actionable, community-level insight that can help flatten the curve. Event-driven architecture and Neptune We took a domain-driven approach to the system architecture. The primary data store backing our API is Amazon DynamoDB, in which we use a single-table design. DynamoDB has high availability and consistent, low-latency interactions at scale that are ideal for the throughput that large-scale contact tracing deployments require. Its low operational overhead is also key to reducing the number of engineers required to maintain it. Amazon DynamoDB Streams enables the domain-driven, decoupled architecture we need for asynchronous processing and ETL so that we can process tracing data as a graph. This approach makes sure we only pay for the compute time we require and allows us to filter and transform the data before it lands in the graph database. The following diagram shows our event-driven architecture on AWS. One of the vital components of large-scale digital contact tracing is a real-time, efficient updating mechanism for each individual’s risk score. Calculating this value for each person in a large graph is extremely intensive, because every member of a community might influence every other person’s risk, either directly or indirectly. Performing this update using a traditional relational database would be challenging; it would require recursive queries and tabular graph traversals. For this reason, we must use a graph database designed to support exactly the sort of traversal queries and whole-community analytics we need to protect a large group of interconnected people. We chose Neptune because it is a powerful graph database that is secure, performant, and analytics-friendly. In our model, each user node is connected to a device node. When a device checks in to a location, an edge forms between that device and a scannable (a QR code), which is associated with a particular site (a physical store) and linked organization (a corporate entity). Neptune allows us to store these rich relationships between users, check-ins, and locations to derive insight about the spread of the virus. The following diagram illustrates our backend ERD. With Neptune, we write queries in Gremlin that perform complex traversals efficiently to update risk scores based on new check-in or test result data. Neptune quickly propagates these risk index evaluations through the whole graph so we can get a near-real-time view of the spread of the virus. For example, we can apply our predictive ML models using tools like Amazon SageMaker to forecast where new hot spots might emerge by looking for clusters of high-risk individuals. Performance is key—every minute that we wait for a database to finish updating a pre-symptomatic person’s risk score is an opportunity for them to expose others. Neptune’s performance delivers on this critical task and allows us to send real-time notifications that keep communities safe. Another reason we chose Neptune is because of its rock-solid security. Zerobase is built to ensure participants’ privacy—it’s a founding principle of our organization and our platform. Neptune provides multiple levels of security out of the box, including network isolation using Amazon VPC, support for Identity and Access Management (IAM) authentication for endpoint access, HTTPS encrypted client connections, and encryption at rest. On a secure Neptune instance, data in the underlying storage is encrypted, as are the automated backups, snapshots, and replicas in the same cluster. These security guarantees are one reason the users of our HIPAA-compliant system trust that their privacy is protected. The road ahead We’re still in the early days of fighting COVID-19. Zerobase is currently conducting trials of the system in New Hampshire and Cologne, Germany. As powerful as Zerobase is, no single technology will be enough to eliminate COVID-19. Zerobase is a key member of the eventual multimodal constellation of solutions that will be needed to contain the virus. As such, Zerobase’s QR-based API framework is designed to integrate seamlessly into any contact tracing system or app that is widely deployed in an area, augmenting a community’s response in two critical ways. First, it pushes a system to 100% inclusiveness, because everyone–not just those with the most advanced smartphones–can be protected. Second, it enhances the app’s effectiveness with Zerobase’s machine learning models that go beyond simple proximity sensing and provide actionable predictive insight to community officials. As we fine-tune Zerobase, we’ll partner with universities, businesses, other tracing app developers, and government and public health officials to better understand, respond to, and ultimately help stop the spread of the virus. For more information about Zerobase and how to partner or volunteer with us, visit www.zerobase.io or email [email protected]. The content and opinions in this post are those of the third-party author and AWS is not responsible for the content or accuracy of this post. About the Authors Aron Szanto is CEO and Founder of the Zerobase Foundation. David Harris is Principal Architect at the Zerobase Foundation.
https://aws.amazon.com/blogs/database/zerobase-creates-private-secure-and-automated-contact-tracing-using-amazon-neptune/
0 notes
Text
Good Morning #realdreamchasers! Here is your daily news cap for Thursday 23rd April, 2020. There is a lot to read and digest so take your time. Remember you can read full articles via Barbados Government Information Service (BGIS), Barbados Today (BT), or by purchasing a Daily Nation Newspaper (DN).
ONE DEATH, ONE NEW CASE – Six straight days of recording no new COVID-19 cases or deaths ended today with an elderly man becoming the latest person to die from the viral illness, and one new case was also reported, according to the acting Chief Medical Officer Dr Kenneth George. And he tonight announced that health authorities would be moving to ramp up testing by as much as 1,000 per cent. Describing today as “a very busy day”, Dr George revealed that the 70-year-old non-national male, who had diabetes died from COVID-19 around 9 a.m. this morning at the Harrison Point facility. The 66-year-old Barbadian woman contracted the virus after being in contact with a known case on April 14. She is now in isolation. He said based on her current condition, it was expected that “her course should be satisfactory”. The health chief said hers was the only new case out of 64 tests conducted yesterday. And while he noted that two people had been released today from isolation bringing the number of recovered cases to 27, Dr George admitted the death and the new case were setbacks. “It is with indeed regret and sorrow that we have to report a single new death from COVID-19 in Barbados. This occurred in a 70-year-old male who would happen to be a non-national and had a fairly difficult course which ended with pneumonia and his pre-disposing condition was that he had a chronic noncommunicable disease,” he said during an interview on CBC TV8tonight. “This reminds us that we need to keep our guards up…, This is indeed a setback, particularly with the death and also with the new case. What we have attempted to do with the new case is to do extreme contact tracing both with persons in their home environment and outside the home environment to make sure that all potential contacts are identified and we are going to put them in two groups; symptomatic and asymptomatic and we are going to do testing in these individuals.” With close to 1,200 tests having been conducted so far, Dr George said authorities would be ramping up screenings and testing. He said patients at the Geriatric Hospital and persons suffering from respiratory illnesses are to be tested, even if they had no travel history. Dr George said: “We have been telling the public that we are going to increase our level of screening in the population and therefore we have broadened the case definition for persons who meet the criteria. Therefore we are including even persons without a travel history. We are asking for persons with respiratory illness to report at polyclinics where they will be advised on the next steps. “So we are broadening our testing of the population in general and we hope to go from about 50 tests a day to scale up to as high as 500 to 600 tests a day. It is only when we have widespread testing will we be able to get a good handle of if there is in-country transmission.” Dr George pleaded with Barbadians to bear with Government during this trying time as they sought to identify all cases of COVID-19 on the island. He reiterated that the current curfew in place was necessary for authorities to achieve their goals. He said: “We need to be on our guard and we believe strongly in the Ministry of Health that during this difficult time of shutdown that this is the appropriate way to go…so if you shut down for one to two weeks you don’t get the immediate effect in your numbers, so I would like to encourage the population to bear with us while we further investigate this and to cooperate with us with respect to having more widespread testing done for all persons who present with respiratory symptoms in Barbados.” He said while most of the cases of COVID-19 were imported, there was one case under investigation where authorities were still trying to determine how that person was infected. (BT)
FAMILY MEMBER: MINISTRY DROPPED BALL ON COVID-19 CASE – A family member of the 66-year-old woman who tested positive for the coronavirus (COVID-19) yesterday is charging that Ministry of Health officials mishandled her case, since this was over three weeks she suspected she had the virus. The angry woman said several family members had been exposed because they spent the previous 24 days caring for her.She explained that her relative, who was a Government employee, came home from work on March 27 and the next day, she started to feel sick. “She called up at Paragon on Sunday and they told her to get ready, that they will pick her up on Monday to be tested. By 9’clock in the morning she was ready and nobody came. She called back again on Tuesday and they told her they were coming. She waited and waited and nobody came. (DN)
HOSPITAL ESTABLISHES DESTABILISATION UNIT – In an effort to further isolate vulnerable patients and staff from potential exposure to the novel coronavirus (COVID-19), the Queen Elizabeth Hospital has established a Clinical Decision Unit (CDU) in Jemmotts Lane, St Michael. According to a statement from the hospital, “The CDU will provide 24-hour medical care in tandem with the hospital’s Accident and Emergency Department (AED) to persons identified by the AED, who require emergency medical assistance in this unit. These individuals will undergo an initial medical assessment i.e. triage, under the white tent erected on the exterior of the AED. Patients who are gravely ill will be seen and treated in the AED. Stable patients who require immediate medical care will be transported by ambulance to the CDU for observation and treatment.” The CDU was established on April 20. Patients with minor medical complaints will continue to be referred to the 24-hour Winston Scott Polyclinic. The statement said all patients who believe they may have been exposed to COVID-19 are asked to call the Ministry of Health and Wellness’ 24-hour COVID hotline at 536-4600 prior to presenting to the AED. This hotline is staffed by trained public health officers who will advise callers. (DN)
NO EVIDENCE OF HUMAN TRAFFICKING PROBLEM – Attorney General Dale Marshall has denied the existence of a “human trafficking problem” in Barbados just days after reports surfaced that a list of undocumented CARICOM nationals including human trafficking victims were in desperate need of assistance. He was responding to a story published by Barbados TODAY in which human trafficking specialist Dr Olivia Smith expressed concern about the wellbeing of approximately 100 affected people. But the AG argued that the article gave no direct evidence of human trafficking and suggests that if the academic has such knowledge, it should be reported to the Royal Barbados Police Force’s (RBPF) Sex Crimes Unit. “We do not have a problem with human trafficking in Barbados. I do not know why this thing keeps raising its head. There is no country in the world that does not have some human trafficking but human trafficking is not a major problem in Barbados and it is wrong for anybody to create the impression that we have a problem with human trafficking,” Marshall told Barbados TODAY. “I am very disappointed and I can’t imagine that Ms Smith would have that kind of information and not report it to the Royal Barbados Police Force. Those are the systems that are put in place to deal with those types of things. The police force has a Sex Crime Unit which is a member of our Human Trafficking Task Force,” he added. Barbados’ Trafficking in Persons Prevention Act [2016] asserts that “A person who, for the purpose of exploitation…recruits, transports, transfers, harbours or receives persons into or within Barbados; from Barbados to another jurisdiction; or receives or harbours persons from Barbados in another jurisdiction, is guilty of the offence of trafficking in persons and is liable on conviction on indictment, to a fine of $1,000,000 or to imprisonment for 25 years or to both.” The legislation also identifies coercion, abduction, fraud or deception; the abuse of power or the abuse of a position of vulnerability; or the giving or receiving of payments or benefits to achieve the consent of a person having control over another person as grounds for a human trafficking conviction. During her interview last week, Dr Smith stressed that some victims are lured into the country by advertisements for a specific job but are coerced into another line of work when they arrive in Barbados. “They are forced into the position that they are in because they have no choice,” she explained. However, the AG stressed that systems are in place to protect both minors and children, but expressed some doubt that many people fell under that category. “To report that there are 100 cases including potential cases of human trafficking, I would want to insist that the Royal Barbados Police Force be brought into play immediately. I am aware from my own investigations that Dr Smith was able to put the ladies in touch with Minister Cynthia Forde who has been able to receive requests from the ladies as to what they need. “But my understanding is that these are ladies who are here illegally and never bothered to regularize their status and that is not something that is unique to 100 women in Barbados,” said the AG. Marshall nevertheless stressed that all persons within the country’s jurisdiction – whether legal or illegal are entitled to equal protection under the law. (BT)
NCSA: GET HELP FOR ALCOHOL, SUBSTANCE ABUSE – The National Council on Substance Abuse (NCSA) has urged relatives and friends of those experiencing symptoms of withdrawal from alcohol or mind-altering substances to call the NCSA’s office, the Psychiatric Hospital, or the nearest polyclinic for help. This advice came from NCSA Manager Betty Hunte who insisted that the council fully supports the Government’s move to ban the sale of alcohol as part of the national response to the COVID-19 pandemic. But Hunte said the NCSA remains concerned about the interruption of access to rehabilitative spaces, something she declared as being of crucial importance to people who are currently in counselling or who have come to a place where they want to access these support services. While there is currently an online petition which already has thousands of signatures, seeking to get Government to lift the ban, Hunte told Barbados TODAY that the NCSA also understands the views of those who are against the decision. But she argued that the whole issue of alcohol is steeped in Barbadian tradition, but what perhaps is not so well accepted is when an individual’s use of alcohol affects them to the point that they must seek help but refuse to do so. The manager stressed that all governments must insist on measures to minimize the strain on the health care system during this period. Hunte said: I don’t think we sometimes see how a breakdown in one part of the system causes sometimes undue pressure on another. In this instance, problematic drinking may lead to contact with the criminal justice system including police, courts and prisons and, or, the public health system and this can be as a result not only of going to the rum-shop and getting drunk but can be caused by indiscriminate use of alcohol in the home.” The petition claims that while the alcohol ban and other measures the Government is taking to prevent the spread of infection is being supported, people are struggling with the impact the ban is having on their lives. The document reads in part: “Banning the sales of alcohol has added to the problem as it prevents us from relaxing and getting a temporary respite from the day-to-day boredom. It is hard to understand how the sale of alcohol for home consumption could be a threat to the success of the lock-down. “The Government needs to give us an ease. Lift the ban on alcohol sales at supermarkets, mini-marts and village shops and allow home delivery by specialist liquor outlets. Keep rum-shops closed to avoid people congregating in groups.” Almost 1,800 people have now signed the petition to support lifting the ban. The NCSA’s manager said the council has heard the concerns expressed relative to the increased risk to the vulnerable people who must remain indoors during this period, and if they reside with someone whose judgment is even more impaired with the use of alcohol, then that risk is multiplied many times. “The NCSA encourages you to stay safe and stay the distance, if not for yourself, the person you care most about. Think before you drink,” Hunte said. (BT)
CRIMINALS BURN MONKEY ALIVE – The people who burned a monkey alive will be brought to justice, a senior Government veterinarian vowed today. The Ministry of Agriculture and Food Security’s Veterinary Services Department served notice that it will be working with the Royal Barbados Police Force to bring the persons guilty of participating in the horrid act, to justice, said Senior Veterinary Officer Dr Mark Trotman. He was responding to a video circulating on social media showing a caged, juvenile monkey being doused with a flammable substance and set alight, while a group of people watched, shouting encouragement. The vet said the “abhorrent” and “criminal” burning was a breach of the Cruelty to Animals Act. “This unconscionable act is not only abhorrent but criminal and is a clear breach of the Prevention of Cruelty to Animals Act (Cap 114A). This action is unjustifiable under any circumstances and the public is urged to desist from any such [act], no matter the perceived rationale,” he said in a statement. Animal welfare and enforcement of cruelty prevention legislation fall under the Ministry of Agriculture. A number of “Authorized Persons” have been appointed by the Minister of Agriculture to assist in its enforcement. “Officers of the Veterinary Services will work closely with the Royal Barbados Police Force to ensure that the guilty person or persons are brought to justice, “ he said. (BT)
ELDERLY MAN FOUND DEAD – An elderly man whose decomposed body was found in an abandoned house on Wednesday will be missed by residents in his hometown of Bathsheba, St Joseph. The incident has also left at least one resident wondering whether an ongoing shutdown due to COVID-19 may have left neighbours unaware of challenges that he may have encountered. Police revealed the discovery was made around 7:30 a.m at the old Powell Spring Hotel opposite the Soup Bowl. No foul play is suspected. Those living around the area identified the dead man as Stephen Hackett who was more commonly known as Tucky. One resident described him as a “character”, who was originally from Joes River, but practically lived at the abandoned house and survived on handouts from those in the area. “He would be hungry and if he asked for anything, people would give him. So now that things are shut down in Bathsheba and there’s nothing going on, there are no picnickers, no restaurants open or shops, he wouldn’t have been able to get his bread. Everybody was shut down and he was just there,” said the resident. “When I heard the announcement this morning the first thing that came to my mind is that perhaps he was not getting any nourishment and he just succumbed to natural causes. I don’t think anyone would do anything bad to him, because he wasn’t a wicked person or anything,” the resident added. The Bathsheba neighbour recalled that Tucky would make people laugh and suspected that when life in the quaint rural village re-opened, he would be missed dearly. “He used to come out to every funeral don’t care who dead. He used to come out well dressed. I don’t know where he had his clothes stashed but he used to come out. He was a man that you would get a good laugh from. He had a funny walk that I wish I had on tape. I will definitely miss seeing him rolling through the streets,” the resident said. When Barbados TODAY visited Joes River, St Joseph where Hackett was born and raised, his brother, who declined to give his name, revealed that the deceased was one of seven siblings. He offered no further comment. (BT)
TEENAGE GIRLS APPEAR IN COURT – Two St Michael teens appeared in court today on a joint charge and were granted bail. Eighteen-year-old Adrianna Lana Marshall McCollin, of 2nd Avenue Alleyne’s Land, Bush Hall and 16-year-old Destiny Terrell Misha Haynes-Harris, of 1st Avenue Chapman Lane are accused of causing a disturbance in their community on April 21. They pleaded not guilty to the charge before Magistrate Graveney Bannister in the District ‘A’ Traffic Court this morning. Haynes is separately charged with breaching the Emergency Management Covid-19 curfew on the same day when she was outdoors at 3 p.m. without a reasonable excuse, when there was a directive imposed on the island requiring every person to remain indoors. She denied the charge. (BT)
SCOTLAND RETURNED TO HOSPITAL AFTER APPEARING ON HARASSMENT CHARGE – An accused was not happy to learn that he would be returning to the Psychiatric Hospital for another three weeks. “I now come from spending five months at the Psychiatric Hospital. That is not an easy task. The conditions at the hospital is not easy,” Rafeal Joslin Scotland, of Rock Dundo, St James told Magistrate Graveney Bannister this afternoon. The 38-year-old was before the court charged with harassing Shamona Rollock along Collymore Rock, St Michael without lawful authority or excuse on November 10, 2019. Scotland pleaded not guilty to the charge. The magistrate, who questioned Sergeant Edwin Pinder on the timing of the charge, was informed that the accused had been at the Black Rock, St Michael hospital for the past few months. He was only released into police custody yesterday, the prosecutor revealed before objecting to bail. Sergeant Pinder pointed to the seriousness of the charge and the aggravating circumstances. “This is something that he does incessantly . . . the situation is volatile.” However, Scotland told the magistrate he would, “stay off” Collymore Rock. He went on to explain that the situation was as a result of him being unable to have access to his “almost” 17-year-old daughter. The complainant, who was also at court, told the magistrate that the harassment had been ongoing even though the relationship had ended over ten years ago. Magistrate Bannister informed the accused that he needed a report from doctors at the Psychiatric Hospital and as such he would be remanded there. But Scotland again informed the magistrate that being at the facility was “hard . . . . Have you ever spent time there? It is not an easy task.” The harassment case is set to be heard in the District ‘A’ Traffic Court on September 14. The doctor’s report is expected on
May 13. (BT)
US IMMIGRATION BAN GETS GREEN LIGHT – United States President Donald Trump on April 22 signed an order to temporarily block some foreigners from permanent residence in the United States, saying he was doing so in order to protect American workers during the coronavirus pandemic. The order is to last for 60 days and then will be reviewed and possibly extended. Some critics saw Republican Trump’s announcement as a move to take advantage of the coronavirus crisis to implement a long-sought policy goal of barring more immigrants ahead of the November 3 election. “In order to protect our great American workers I have just signed an executive order temporarily suspending immigration into the United States. This will ensure that unemployed Americans of all backgrounds will be first in line for jobs as our economy reopens,” Trump said at his daily news conference about the coronavirus at the White House. He also said it will “preserve our healthcare resources for American patients” afflicted by the coronavirus. White House lawyers worked all day to craft the language for the order, prompting some officials to say the signing might have to wait for Thursday. But aides described Trump as eager to sign the document. Trump won the White House in 2016 in part on a promise to crack down on immigration and has made the issue central to his presidency. But many of his major moves trying to curb immigration have been challenged in court and legal experts said this executive order could also face lawsuits. One US Department of Homeland Security official who requested anonymity said the order would only apply to people applying for permanent residence from outside the United States, not those already in the country seeking to adjust their status. Trump said the order initially would last for 60 days and could be renewed for the same period or longer, and that a second immigration-focused order was under consideration. (Reuters)
ACTION TEAM TO JUMP START TOURISM – Tourism officials are consumed with determining strategies to keep Barbados top-of-mind in its major markets with a near $30 million fund, while the country battles the novel coronavirus (COVID-19). Minister of Tourism and International Transport Kerrie Symmonds has told a major Canadian travel site Travel Pulse Canada during a Facebook Live chat with host John Kirk, it has been a “tough period we’re going through”. Between 80 and 90 per cent of hotels and fine dining restaurants have closed their doors including the swanky Sandy Lane Hotel on the West Coast, Sandals Hotel, and the Elegant Group, the island’s largest hotel chain which was recently purchased by Marriott International Inc. for US$ 199 million. Noting that the island remains under a 24-hour curfew, Symmonds said, “We’ve taken a conscious decision to use this period as a period where we can do a reassessment of our industry, the way we have done business historically and traditionally, and where we can identify substantial improvements and so on. We’ve done a number of things. “First of all, there’s a look at how we can reposition the Barbados brand and keep it top-of-mind across all the major source markets. One of the things we have done is set aside funds at the Government level, I think $20 to $30 million, and then there will be a blending of financing with the private sector to be able to re-capitalise what we call the Small Hotel Redevelopment Fund. That fund will be to enable a lot of hotels to refresh themselves and use this down period [for renovations and reconstruction].”Citing the creation of a Tourism Recovery Task Force, the Minister said it will examine ways to recover the sector after the health and economic crisis created by the COVID-19. Among the chief considerations are plans for recovery of every aspect of Barbados’ tourism sector including attractions, restaurants, hotels, and “other areas of the economy linked into tourism” – the cultural sector, the agricultural sector, the sporting sector. According to Symmonds, the cruise sector will be getting specific attention. “Even as I speak to you there are ten or 12 cruise ships anchored off the coast of Barbados because they had nowhere else to go. We facilitated the repatriation of the passengers, but the ships are still out there. It has helped us to develop a warm kinship and a sense of fraternity with that sector. “We were perhaps their greatest friend. We are looking at the way we can perhaps work with them so that when there’s a recovery period we can be the centrepiece of that recovery. And there are some things we would want to do for the rest of the region, and the Eastern Caribbean. And one of those is to create a summer cruise itinerary, so that instead of the Mediterranean being the only place to be for major cruise activity out of Europe, we would want to think that now we can have a look at the southeast Caribbean and have Barbados as the centrepiece of that itinerary.” The Tourism Minister also had a word of encouragement for travel agents in the various markets. “We want . . . to formulate big plans and to bounce back, and not just to come back by ourselves but as part of a stronger and more prepared Caribbean region, and a safer Caribbean region.” He added: “One major one is to have a COVID-free Barbados, and in that regard we’re looking at a pre-molecular test which would be a test that, if we can get it put together, would be done on entry into the island so you know you’re coming onto island where you know there’s no disease. Similarly, we’d like to spearhead an effort to have that in the Eastern Caribbean as a whole. “We are obviously anxious to re-open ourselves to business, but it has to be done in a way that’s safe for the visiting public and also the local public,” Symmonds said.(BT)
CRUISE SHIPS BUYING LOCAL – Cruise ships off the coast of Barbados are continuing to source some of their food for crew members from local farmers at their own cost. Word of this has come from chair person of the Bridgetown Port Inc. Senator Lisa Cummins who dismissed suggestions that the country was responsible for taking care of them while they were docked here. In fact, she said the island continued to earn revenue from those cruise ships as they source some of their dietary needs from local farmers to complement what they have imported. She said: “Based on what I see on a daily basis in terms of request for persons to access the port to provide services to the ships, there is still economic activity to a number of local businesses. Wherever there is an opportunity for provisioning to take place for the ships that is still taking place. “We don’t have to provide food for them. They are working very closely with us. They are taking food in from us, so you have a number of local providers who ordinarily have contracts with the ships to provide them with food. So I have a schedule now where for [this week] we know what food supplies are being provided. So whether it is fruits, meat, vegetables, those kinds of things come from many of the local producers and some of the produce is in fact imported based on the volumes that they may need,” she explained. The cruise ships docked off the shores of Bridgetown, some of which have more than 250 crew members aboard, have also been getting items from their parent companies. Cummins pointed out that with vessels only having crew members, it was expected that the amount of food being sourced would be substantially lower than if they had passengers on board. “The same quantities that they may have been importing or procuring locally before with passengers on board they are no longer procuring but they are still procuring at their own cost of course, food supplies and everything else,” said Cummins. (BT)
LONG LINES ARE BACK FOR PAYING BILLS – As month-end approaches, scenes of long queues and hours of waiting have shifted from supermarkets and post offices to SurePay bill payment kiosks, where scores started gathering from early Wednesday to make utility and other payments. With most businesses closed, Barbadians have started turning their attention to the SurePay outlets in supermarkets, even though the Government has indicated that Post Offices will take payments for the major utility companies. Customers hamstrung to only leave home on their designated shopping and banking days set by Government to correspond with their surnames during the 24-hour curfew, has added to the frustration. The switch from grocery shopping to bill payment was evident Wednesday at Emerald City, St Philip, where there was no line for in-store shopping but to pay utility and other bills, the line snaked into a loop formation to avoid persons having to stand in the sun. With just a single cashier attending the SurePay booth, those in the long line expressed worry that they would be turned away as the four-hour time limit for persons with the surnames E, F, G, H ran out. But unlike last week, the supermarket chain did not close its doors at 11 a.m. but allowed those standing in the line for as long as two and a half to three hours, an opportunity to pay their bills. Just 24 hours earlier, Minister of Water Resources Wilfred Abrahams pleaded with Barbadians to pay their water bills. He said there was a noticeable decline in people making water and sewerage payments. This, he said, was hurting the state-owned entity’s cash flow and its ability to carry out its mandate to supply water to the population. (BT)
VENDOR DEALT A HARD BLOW – A food-cart operator in Belleville, St Michael is counting hundreds of dollars in losses after thieves robbed her of all the cooking equipment she needs to operate her businesses. A saddened Sandra Maloney of Sha-San’s Cart told Barbados TODAY that sometime between Monday night and Tuesday morning the thieves stole her grill, two full bottles of gas and one empty bottle, along with a four-foot white plastic folding table, which she said were valued at an estimated total of $2,000. Forty-nine-year-old Maloney who has been operating in front of the Democratic Labour Party’s (DLP) George Street headquarters for 17 years, said the items were stolen from a locked storage room located on the DLP compound. And while police are investigating the matter, Maloney said she now has to start rebuilding from scratch. She is appealing to the public not to purchase the items from anyone who is unable to verify how they acquired them. She has even taken to social media to spread the message. “The grill is a black and silver Char-Broil grill. Everybody know me from Belleville and if anybody sees anybody trying to sell these things they can notify me or the police because I called the police and they went yesterday. The table has my name written all over it. I am just trying to help myself. “There is a guy who used to operate a bar at DLP on Fridays and usually they would break in by him most of the time and the police never hold anyone for it. So that is why I said I will not just sit down, I will try to help myself,” Maloney said. The mother of one son who is studying said on Monday she had “the intuition” that something was not right at the storeroom. She said on Monday night she contacted a friend who lives close to the headquarters and asked him to check on her belongings. “He tell me that he does pass and check all the time. Then he called me yesterday [Tuesday] and tell me ‘you were right’ because they did break in. When he went the cart was out and he knew immediately that something happened.“He went in and see that some of the stuff that they leave back was outside and he took some pictures and sent to me. From the pictures he sent to me I could have seen that the grill and the gas bottles were gone. But they left the big cooler and one of the grill tops and the saucepans and pans,” she said. Maloney noted that like any small business owner who sacrificed and worked hard to build their operation, she felt robbed of her livelihood. She explained that she recently spent almost all of her savings to get her vehicle overhauled and could not afford to replace the stolen items at this time.“Not being able to work right now, the income is really minimum. So for me now I have to start back all over again and I can’t even go back to work when things settle down with [the COVID-19] pandemic] because I have to be able now to source gas bottles and source a grill,” Maloney said. (BT)
NO PRO SHOWS FOR MORGAN – Body fitness pro athlete Ramona Morgan was looking forward to a productive year, but like many athletes across the globe, the coronavirus pandemic has forced her to stay put. Morgan, 42, who secured her pro card during 2018 Central American and Caribbean Championships in Mexico, was particularly hoping for a pro segment triumph to gain her ticket to compete at the World Championships set for the International Federation of Bodybuilding’s Elite headquarters in Spain in November. “The most I can do is continue to train, but I can’t see myself competing, outside of Barbados or even competing even if they decide to have the Darcy [Beckles] Diamond Cup] this year,” she told MIDWEEK SPORT. “It involves travelling and it involves other athletes coming into Barbados. When the borders are opened back, the virus is still going to be out there. My health is important.” (DN)
EDUCATION REMINDER – Parents and guardians who have not yet received information on how to log on to the new e-learning platform, Google G Suite for Education, are advised to contact the principals or the class teachers of their respective schools for details. A statement from the Ministry of Education said they may also call the helpdesk at 535-0798, between 8:30 a.m. and 4:30 p.m., Monday to Friday. (BGIS)
The world is facing the rapid spread of the Covid-19 Coronavirus Pandemic. As we continue to do our part in Barbados please remember to stay home but on the days you have to go out wear your masks, practice social distancing (stand 6-10 feet away from each other), practice good daily hygiene, eat healthy, exercise and keep your mind active. There are 253 days left in the year Shalom! Follow us on Twitter, Facebook & Instagram for your daily news. #thechasefiles #dailynewscaps #bajannewscaps #newsinanutshell #coronavirusinbarbados #nationalresponse #dailynews #thechasefilesblog
0 notes
Text
Analysis: The Real Tragedy Of Not Having Enough COVID-19 Tests
President Donald Trump said late last month that he hadn’t “heard about testing in weeks.” But today — let’s face it — tests are being rationed in many parts of the country.
Of course, the seriously ill and essential front-line personnel like doctors, nurses and police officers require and deserve to go to the front of the line for testing.
But hundreds of thousands more people should have been tested by now, if only more tests were available. Testing them — and getting results — might have vastly changed their behavior, their self-care at home and (perhaps most important) our understanding of COVID-19, so that when it flares locally we would know how to respond in a more nuanced way, rather than shutting down society.
As of this writing, I know nearly a dozen people who are “presumed COVID.” None of them were tested because they were not sick enough to be admitted to a hospital — though all were quite symptomatic. Here’s a partial list:
Three 20-something roommates in Brooklyn, two with mild symptoms. One sick enough to visit a hospital, short of breath. No tests. All were told, “Assume you have it.”
Also “presumed COVID”: a colleague’s daughter and her boyfriend, though he had a rough two-week course, including pneumonia. His oxygen levels, measured at home, never got quite bad enough for admission (hence, no testing).
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Sign Up
Please confirm your email address below:
Sign Up
And, finally, a reporter in San Francisco, who went to a clinic with high fever, total body aches and cough, was “presumed COVID.” She was sent home. The following day, her strep test came back positive. “Assume you have COVID, too,” she was told.
It is true that a positive COVID-19 test would not have changed any of their immediate medical treatment. They got inhalers and the medicines they needed. Not knowing probably didn’t increase their risk of death. So I don’t fault the doctors for not administering tests during a time of limited resources.
But here is what is outrageous: This resource should not be in such limited supply three months into a global outbreak. Widespread testing has a hugely important impact, not just for individuals, but also for society.
For example, if people knew they’d had COVID-19, and therefore possessed at least some immunity, they could volunteer, once fully recovered, for groups like Meals on Wheels, which is struggling to deliver food to people who can’t — even in the best of times — fend for themselves. People with immunity could serve as helpers in nursing homes, whose staffs are stretched thin and where the elderly are living in isolation.
Knowing the result of a test allows rational individual decisions. If a person living in a house with others knows whether he has the coronavirus versus a common cold (and, remember, the symptoms of COVID-19 may be very mild in younger people), it greatly affects how he interacts with family members and housemates.
If he is COVID-19 positive, it makes sense for him to totally isolate in one room and use a separate bathroom. An elderly relative might be moved out. If he has a common cold, less disruptive precautions are needed.
In this season of allergies — sneezes and sniffles — and when the country is trying to control the spread of a virus that can produce only mild symptoms in many of those infected, it would be good to be able to test as many “essential workers” — broadly defined — as possible to see if they had contracted the coronavirus.
This is not just a reference to health care workers, police and firefighters or utility workers. It is also not helpful for a food delivery person or the guy at the grocery counter, for example, to work with it, given how many people depend on their services.
We test for things like strep and sexually transmitted diseases not just because knowing test results influences treatment — should antibiotics be prescribed? — but also because the results influence the care and advice for patients’ activities and contacts.
Finally, and perhaps most important, widespread testing of all those “presumed COVID” patients who are not hospitalized gives us a far clearer picture of this new viral disease, which we currently have so little data about.
It would allow us to calculate how many people who are infected with the virus get really ill and how many die (the true case fatality rate). We are still more or less clueless about those things and, because of uneven testing, fatality rates vary widely by city, state and country.
Finally, widespread testing would allow us to have a better sense of how transmissible the virus is after more casual contact. We know that the intense exposure of health care personnel in a hospital setting often leads to transmission. But what about the co-worker who sat across the office from you and rarely interacted with you?
Long after his graduate school classes were canceled, my son was belatedly notified that one person in his German class had fallen ill with COVID-19. How many others did, but were never tested?
After this period of lockdown, COVID-19 is likely to come back in lesser waves, and robust testing data would be hugely important in fashioning a targeted response that could be less expansive than the miserable and economically devastating shutdown we are now experiencing. If one student falls ill in a class, should universities once again send all students home and cancel a semester — or just close a building? Or even cancel just one class?
Thank goodness that countries like South Korea are doing far more testing than we are, which might give us clues about how to respond. But we should be doing much more ourselves.
There have been countless explanations for the lack of tests. Our public health labs are not primed to do testing and the Centers for Disease Control and Prevention was slow to react to a virus many knew was likely to come our way. The agency initially distributed test kits like Senate seats — equally to each state lab, rather than where they were most needed. Then the first test kits didn’t work.
The list goes on. The Food and Drug Administration only belatedly allowed private and university labs to contribute without the normal regulatory tape. There was a shortage of swabs and a shortage of personal protective equipment for people conducting the testing. Most recently, an Abbott quick test device that Mr. Trump had applauded as a solution — “a whole new ballgame” — turned out to be only 5,500 tests, distributed nationally. Yet many millions are needed.
All are plausible explanations and many are true. But no one should be satisfied with them in this, the richest country in the world.
There are concerns, to be sure, about the accuracy of the new tests, with reports of false negatives. But that is no reason not to use what we have; the specificity of newly developed tests can improve with understanding and use. It would be wise for people who test negative to continue rigorously following good COVID-19 hygiene. But it would be a mistake to not expand testing aggressively simply because of reports of false negatives.
“Presumed positive” may be needed during a period of rationing and shortage. But “Assume you’re positive,” as so many New Yorkers are doing, is not good individual health care — or good policy.
Analysis: The Real Tragedy Of Not Having Enough COVID-19 Tests published first on https://nootropicspowdersupplier.tumblr.com/
0 notes
Text
Analysis: The Real Tragedy Of Not Having Enough COVID-19 Tests
President Donald Trump said late last month that he hadn’t “heard about testing in weeks.” But today — let’s face it — tests are being rationed in many parts of the country.
Of course, the seriously ill and essential front-line personnel like doctors, nurses and police officers require and deserve to go to the front of the line for testing.
But hundreds of thousands more people should have been tested by now, if only more tests were available. Testing them — and getting results — might have vastly changed their behavior, their self-care at home and (perhaps most important) our understanding of COVID-19, so that when it flares locally we would know how to respond in a more nuanced way, rather than shutting down society.
As of this writing, I know nearly a dozen people who are “presumed COVID.” None of them were tested because they were not sick enough to be admitted to a hospital — though all were quite symptomatic. Here’s a partial list:
Three 20-something roommates in Brooklyn, two with mild symptoms. One sick enough to visit a hospital, short of breath. No tests. All were told, “Assume you have it.”
Also “presumed COVID”: a colleague’s daughter and her boyfriend, though he had a rough two-week course, including pneumonia. His oxygen levels, measured at home, never got quite bad enough for admission (hence, no testing).
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Sign Up
Please confirm your email address below:
Sign Up
And, finally, a reporter in San Francisco, who went to a clinic with high fever, total body aches and cough, was “presumed COVID.” She was sent home. The following day, her strep test came back positive. “Assume you have COVID, too,” she was told.
It is true that a positive COVID-19 test would not have changed any of their immediate medical treatment. They got inhalers and the medicines they needed. Not knowing probably didn’t increase their risk of death. So I don’t fault the doctors for not administering tests during a time of limited resources.
But here is what is outrageous: This resource should not be in such limited supply three months into a global outbreak. Widespread testing has a hugely important impact, not just for individuals, but also for society.
For example, if people knew they’d had COVID-19, and therefore possessed at least some immunity, they could volunteer, once fully recovered, for groups like Meals on Wheels, which is struggling to deliver food to people who can’t — even in the best of times — fend for themselves. People with immunity could serve as helpers in nursing homes, whose staffs are stretched thin and where the elderly are living in isolation.
Knowing the result of a test allows rational individual decisions. If a person living in a house with others knows whether he has the coronavirus versus a common cold (and, remember, the symptoms of COVID-19 may be very mild in younger people), it greatly affects how he interacts with family members and housemates.
If he is COVID-19 positive, it makes sense for him to totally isolate in one room and use a separate bathroom. An elderly relative might be moved out. If he has a common cold, less disruptive precautions are needed.
In this season of allergies — sneezes and sniffles — and when the country is trying to control the spread of a virus that can produce only mild symptoms in many of those infected, it would be good to be able to test as many “essential workers” — broadly defined — as possible to see if they had contracted the coronavirus.
This is not just a reference to health care workers, police and firefighters or utility workers. It is also not helpful for a food delivery person or the guy at the grocery counter, for example, to work with it, given how many people depend on their services.
We test for things like strep and sexually transmitted diseases not just because knowing test results influences treatment — should antibiotics be prescribed? — but also because the results influence the care and advice for patients’ activities and contacts.
Finally, and perhaps most important, widespread testing of all those “presumed COVID” patients who are not hospitalized gives us a far clearer picture of this new viral disease, which we currently have so little data about.
It would allow us to calculate how many people who are infected with the virus get really ill and how many die (the true case fatality rate). We are still more or less clueless about those things and, because of uneven testing, fatality rates vary widely by city, state and country.
Finally, widespread testing would allow us to have a better sense of how transmissible the virus is after more casual contact. We know that the intense exposure of health care personnel in a hospital setting often leads to transmission. But what about the co-worker who sat across the office from you and rarely interacted with you?
Long after his graduate school classes were canceled, my son was belatedly notified that one person in his German class had fallen ill with COVID-19. How many others did, but were never tested?
After this period of lockdown, COVID-19 is likely to come back in lesser waves, and robust testing data would be hugely important in fashioning a targeted response that could be less expansive than the miserable and economically devastating shutdown we are now experiencing. If one student falls ill in a class, should universities once again send all students home and cancel a semester — or just close a building? Or even cancel just one class?
Thank goodness that countries like South Korea are doing far more testing than we are, which might give us clues about how to respond. But we should be doing much more ourselves.
There have been countless explanations for the lack of tests. Our public health labs are not primed to do testing and the Centers for Disease Control and Prevention was slow to react to a virus many knew was likely to come our way. The agency initially distributed test kits like Senate seats — equally to each state lab, rather than where they were most needed. Then the first test kits didn’t work.
The list goes on. The Food and Drug Administration only belatedly allowed private and university labs to contribute without the normal regulatory tape. There was a shortage of swabs and a shortage of personal protective equipment for people conducting the testing. Most recently, an Abbott quick test device that Mr. Trump had applauded as a solution — “a whole new ballgame” — turned out to be only 5,500 tests, distributed nationally. Yet many millions are needed.
All are plausible explanations and many are true. But no one should be satisfied with them in this, the richest country in the world.
There are concerns, to be sure, about the accuracy of the new tests, with reports of false negatives. But that is no reason not to use what we have; the specificity of newly developed tests can improve with understanding and use. It would be wise for people who test negative to continue rigorously following good COVID-19 hygiene. But it would be a mistake to not expand testing aggressively simply because of reports of false negatives.
“Presumed positive” may be needed during a period of rationing and shortage. But “Assume you’re positive,” as so many New Yorkers are doing, is not good individual health care — or good policy.
Analysis: The Real Tragedy Of Not Having Enough COVID-19 Tests published first on https://smartdrinkingweb.weebly.com/
0 notes
Text
Analysis: The Real Tragedy Of Not Having Enough COVID-19 Tests
President Donald Trump said late last month that he hadn’t “heard about testing in weeks.” But today — let’s face it — tests are being rationed in many parts of the country.
Of course, the seriously ill and essential front-line personnel like doctors, nurses and police officers require and deserve to go to the front of the line for testing.
But hundreds of thousands more people should have been tested by now, if only more tests were available. Testing them — and getting results — might have vastly changed their behavior, their self-care at home and (perhaps most important) our understanding of COVID-19, so that when it flares locally we would know how to respond in a more nuanced way, rather than shutting down society.
As of this writing, I know nearly a dozen people who are “presumed COVID.” None of them were tested because they were not sick enough to be admitted to a hospital — though all were quite symptomatic. Here’s a partial list:
Three 20-something roommates in Brooklyn, two with mild symptoms. One sick enough to visit a hospital, short of breath. No tests. All were told, “Assume you have it.”
Also “presumed COVID”: a colleague’s daughter and her boyfriend, though he had a rough two-week course, including pneumonia. His oxygen levels, measured at home, never got quite bad enough for admission (hence, no testing).
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Sign Up
Please confirm your email address below:
Sign Up
And, finally, a reporter in San Francisco, who went to a clinic with high fever, total body aches and cough, was “presumed COVID.” She was sent home. The following day, her strep test came back positive. “Assume you have COVID, too,” she was told.
It is true that a positive COVID-19 test would not have changed any of their immediate medical treatment. They got inhalers and the medicines they needed. Not knowing probably didn’t increase their risk of death. So I don’t fault the doctors for not administering tests during a time of limited resources.
But here is what is outrageous: This resource should not be in such limited supply three months into a global outbreak. Widespread testing has a hugely important impact, not just for individuals, but also for society.
For example, if people knew they’d had COVID-19, and therefore possessed at least some immunity, they could volunteer, once fully recovered, for groups like Meals on Wheels, which is struggling to deliver food to people who can’t — even in the best of times — fend for themselves. People with immunity could serve as helpers in nursing homes, whose staffs are stretched thin and where the elderly are living in isolation.
Knowing the result of a test allows rational individual decisions. If a person living in a house with others knows whether he has the coronavirus versus a common cold (and, remember, the symptoms of COVID-19 may be very mild in younger people), it greatly affects how he interacts with family members and housemates.
If he is COVID-19 positive, it makes sense for him to totally isolate in one room and use a separate bathroom. An elderly relative might be moved out. If he has a common cold, less disruptive precautions are needed.
In this season of allergies — sneezes and sniffles — and when the country is trying to control the spread of a virus that can produce only mild symptoms in many of those infected, it would be good to be able to test as many “essential workers” — broadly defined — as possible to see if they had contracted the coronavirus.
This is not just a reference to health care workers, police and firefighters or utility workers. It is also not helpful for a food delivery person or the guy at the grocery counter, for example, to work with it, given how many people depend on their services.
We test for things like strep and sexually transmitted diseases not just because knowing test results influences treatment — should antibiotics be prescribed? — but also because the results influence the care and advice for patients’ activities and contacts.
Finally, and perhaps most important, widespread testing of all those “presumed COVID” patients who are not hospitalized gives us a far clearer picture of this new viral disease, which we currently have so little data about.
It would allow us to calculate how many people who are infected with the virus get really ill and how many die (the true case fatality rate). We are still more or less clueless about those things and, because of uneven testing, fatality rates vary widely by city, state and country.
Finally, widespread testing would allow us to have a better sense of how transmissible the virus is after more casual contact. We know that the intense exposure of health care personnel in a hospital setting often leads to transmission. But what about the co-worker who sat across the office from you and rarely interacted with you?
Long after his graduate school classes were canceled, my son was belatedly notified that one person in his German class had fallen ill with COVID-19. How many others did, but were never tested?
After this period of lockdown, COVID-19 is likely to come back in lesser waves, and robust testing data would be hugely important in fashioning a targeted response that could be less expansive than the miserable and economically devastating shutdown we are now experiencing. If one student falls ill in a class, should universities once again send all students home and cancel a semester — or just close a building? Or even cancel just one class?
Thank goodness that countries like South Korea are doing far more testing than we are, which might give us clues about how to respond. But we should be doing much more ourselves.
There have been countless explanations for the lack of tests. Our public health labs are not primed to do testing and the Centers for Disease Control and Prevention was slow to react to a virus many knew was likely to come our way. The agency initially distributed test kits like Senate seats — equally to each state lab, rather than where they were most needed. Then the first test kits didn’t work.
The list goes on. The Food and Drug Administration only belatedly allowed private and university labs to contribute without the normal regulatory tape. There was a shortage of swabs and a shortage of personal protective equipment for people conducting the testing. Most recently, an Abbott quick test device that Mr. Trump had applauded as a solution — “a whole new ballgame” — turned out to be only 5,500 tests, distributed nationally. Yet many millions are needed.
All are plausible explanations and many are true. But no one should be satisfied with them in this, the richest country in the world.
There are concerns, to be sure, about the accuracy of the new tests, with reports of false negatives. But that is no reason not to use what we have; the specificity of newly developed tests can improve with understanding and use. It would be wise for people who test negative to continue rigorously following good COVID-19 hygiene. But it would be a mistake to not expand testing aggressively simply because of reports of false negatives.
“Presumed positive” may be needed during a period of rationing and shortage. But “Assume you’re positive,” as so many New Yorkers are doing, is not good individual health care — or good policy.
from Updates By Dina https://khn.org/news/analysis-the-real-tragedy-of-not-having-enough-covid-19-tests/
0 notes
Text
Coronavirus: three things all governments and their science advisers must do now
Follow World Health Organization advice, end secrecy in decision-making and cooperate globally.

“Some of the most important choices about a nation’s physical health are made, or not made, by a handful of men, in secret.”
Sixty-odd years ago, the chemist, writer and civil servant Charles Percy Snow revealed in his book Science and Government the shocking extent to which science advice to governments during the Second World War had lacked evidence. As the world stands on the precipice of one of the worst infectious-disease outbreaks in a century, his observations are just as relevant today.
Around the globe, countries are responding to the coronavirus pandemic with steps previously taken only in times of war. Borders are closing. Communities are being quarantined; gatherings cancelled; restaurants closed; and factories and hotel rooms requisitioned.
And yet in many countries, including the United States and the United Kingdom, governments have been making crucial decisions in secret and making announcements before publishing the evidence on which their decisions are based. This is not how governments should work. The secrecy must end.
As Europe becomes the outbreak’s new epicentre, and cases continue to rise in almost every affected country, three things must happen urgently.
Follow the World Health Organization’s advice
Neither the United States nor the United Kingdom has said why it has not been following the advice of the World Health Organization (WHO), which is to aggressively test, track and isolate as many cases of COVID-19 as possible. They argue that they are being advised by some of the world’s best virologists and infectious-disease epidemiologists. This is true. But at the same time, no government can match the WHO’s cumulative on-the-ground experience — and lessons learnt — in dealing with outbreaks, from severe acute respiratory syndrome (SARS) to Ebola. The agency is emphatic that measures known as ‘containment’ are essential, alongside social distancing and rapid clinical care, in places where there is ongoing transmission.
Aggressive testing of cases, and quarantining of their contacts, is still not a declared policy priority for the United States, where efforts are being hampered by the shortage of COVID-19 diagnostic tests and the absence of a unified public health system. The United Kingdom, where public health is more centrally run, has also implemented limited testing, although it is now ramping this up — as are other countries. By contrast, although their respective mitigation measures have been different, China and South Korea used much more aggressive containment from the start, and continue to do so. Both countries now have fewer new cases per day than when the virus was at its peak.
It is rare for the WHO to criticize member countries that are among its largest donors, but director-general Tedros Adhanom Ghebreyesus was unequivocal when he said last week: “The idea that countries should shift from containment to mitigation is wrong and dangerous.” He added: “You can’t fight a virus if you don’t know where it is. That means robust surveillance to find, isolate, test and treat every case, to break the chains of transmission.”
This week, he reiterated the point: “The most effective way to prevent infections and save lives is breaking the chains of transmission. And to do that, you must test and isolate. You cannot fight a fire blindfolded. And we cannot stop this pandemic if we don’t know who is infected.”
Publish the evidence and embrace open research
From the start of the outbreak, researchers around the world have led the way in sharing research and data. Ibile News — in common with colleagues across international research publishing — committed to making all coronavirus-related research and data open. The sharing of data — ranging from viral gene sequences to epidemiology studies — is needed to track how the virus is spreading and how it might be curbed.
Research leaders who work for — and advise — governments must do the same. Open and shared research is better research, because it allows a wider group of experts to check assumptions, verify calculations, interrogate conclusions and spot and challenge mistakes. Unfortunately, when it comes to the evidence underpinning government science advice, that is not happening enough.
The consequences of not publishing evidence is apparent in the United Kingdom’s controversial decision to delay the type of compulsory school and workplace closures that other countries are enacting. Part of the initial reasoning, as explained by chief scientific adviser Patrick Vallance, included the premise that, for healthy people, getting a mild illness would help to build up their immunity — and that, if more people became immune, it would reduce virus transmission. According to this reasoning, such a move would also delay — and reduce — the peak in infections. But the evidence behind this approach was not revealed. Not unexpectedly, the approach was questioned by scientists, including epidemiologists and other infectious-disease specialists, and is no longer part of UK policy.
Researchers understand that sudden changes in policy will be necessary in a rapidly evolving situation in which there are many unknowns. But governments risk losing their trust by announcing those policies before the underlying data, models and assumptions have been released.
Ministers and their science advisers seem to have reverted to the Second World War model of making decisions in relatively small groups and then releasing papers and statements, giving interviews or writing articles. Politicians and their science advisers need to get with the times and embrace open research. They should harness the collective expertise — now also accessible through social media — of virologists, epidemiologists, behavioural researchers and others who can help them to better interrogate their models, and therefore improve their decisions. This is imperative now, when they are making decisions on which the future of lives and economies depend.
International cooperation will save lives
It is undeniably difficult for government science and medical advisers to advocate for a more collective, transparent approach when some of their leaders — particularly US President Donald Trump and his administration — are sceptical about the value of international cooperation and are instead making unilateral decisions. The United States’ decision to ban flights from China and Iran, and later from European countries, was made without consulting the majority of these nations — and without publishing the evidence for how flight bans might slow the spread of a virus that is already circulating within a country.
But the advisers must persevere. They must persuade their leaders that coordinated collective action is in everyone’s interests. If, for example, they disagree with the WHO’s analysis, then they should explain why. To defeat a pandemic in an interconnected world, countries need to provide full and transparent evidence to back up their decisions, and be willing to share that evidence so that they can defeat the virus together.
0 notes
Text
Wuhan Coronavirus Looks Increasingly Like a Pandemic, Experts Say
The Wuhan coronavirus spreading from China is now likely to become a pandemic that circles the globe, according to many of the world’s leading infectious disease experts.
The prospect is daunting. A pandemic — an ongoing epidemic on two or more continents — may well have global consequences, despite the extraordinary travel restrictions and quarantines now imposed by China and other countries, including the United States.
Scientists do not yet know how lethal the new coronavirus is, however, so there is uncertainty about how much damage a pandemic might cause. But there is growing consensus that the pathogen is readily transmitted between humans.
The Wuhan coronavirus is spreading more like influenza, which is highly transmissible, than like its slow-moving viral cousins, SARS and MERS, scientists have found.
“It’s very, very transmissible, and it almost certainly is going to be a pandemic,” said Dr. Anthony S. Fauci, director of the National Institute of Allergy and Infectious Disease.
“But will it be catastrophic? I don’t know.”
In the last three weeks, the number of lab-confirmed cases has soared from about 50 in China to 14,000 in 23 countries; there have been over 300 deaths, all but one in China.
But various epidemiological models estimate that the real number of cases is 100,000 or even more. While that expansion is not as rapid as that of flu or measles, it is an enormous leap beyond what virologists saw when SARS and MERS emerged.
When SARS was vanquished in July 2003 after spreading for nine months, only 8,098 cases had been confirmed. MERS has been circulating since 2012, but there have been only about 2,500 known cases.
The biggest uncertainty now, experts said, is how many people around the world will die. SARS killed about 10 percent of those who got it, and MERS now kills about one of three.
The 1918 “Spanish flu” killed only about 2.5 percent of its victims — but because it infected so many people and medical care was much cruder then, 20 to 50 million died.
By contrast, the highly transmissible H1N1 “swine flu” pandemic of 2009 killed about 285,000, fewer than seasonal flu normally does, and had a relatively low fatality rate, estimated at .02 percent.
The mortality rate for known cases of the Wuhan coronavirus has been running about 2 percent, although that is likely to drop as more tests are done and more mild cases are found.
It is “increasingly unlikely that the virus can be contained,” said Dr. Thomas R. Frieden, a former director of the Centers for Disease Control and Prevention who now runs Resolve to Save Lives, a nonprofit devoted to fighting epidemics.
“It is therefore likely that it will spread, as flu and other organisms do, but we still don’t know how far, wide or deadly it will be.”
In the early days of the 2009 flu pandemic, “they were talking about Armageddon in Mexico,” Dr. Fauci said. (That virus first emerged in pig-farming areas in Mexico’s Veracruz State.) “But it turned out to not be that severe.”
An accurate estimate of the virus’s lethality will not be possible until certain kinds of studies can be done: blood tests to see how many people have antibodies, household studies to learn how often it infects family members, and genetic sequencing to determine whether some strains are more dangerous than others.
Closing borders to highly infectious pathogens never succeeds completely, experts said, because all frontiers are somewhat porous. Nonetheless, closings and rigorous screening may slow the spread, which will buy time for the development of drug treatments and vaccines.
Other important unknowns include who is most at risk, whether coughing or contaminated surfaces are more likely to transmit the virus, how fast the virus can mutate and whether it will fade out when the weather warms.
The effects of a pandemic would probably be harsher in some countries than in others. While the United States and other wealthy countries may be able to detect and quarantine the first carriers, countries with fragile health care systems will not. The virus has already reached Cambodia, India, Malaysia, Nepal, the Philippines and rural Russia.
“This looks far more like H1N1’s spread than SARS, and I am increasingly alarmed,” said Dr. Peter Piot, director of the London School of Hygiene and Tropical Medicine. “Even 1 percent mortality would mean 10,000 deaths in each million people.”
Other experts were more cautious.
Dr. Michael Ryan, head of emergency responses for the World Health Organization, said in an interview with STAT News on Saturday that there was “evidence to suggest this virus can still be contained” and that the world needed to “keep trying.”
Dr. W. Ian Lipkin, a virus-hunter at the Columbia University Mailman School of Public Health who is in China advising its Center for Disease Control and Prevention, said that although the virus is clearly being transmitted through casual contact, labs are still behind in processing samples.
But life in China has radically changed in the last two weeks. Streets are deserted, public events are canceled, and citizens are wearing masks and washing their hands, Dr. Lipkin said. All of that may have slowed down what lab testing indicated was exponential growth in the infection.
It’s unclear exactly how accurate tests done in overwhelmed Chinese laboratories are. On the one hand, Chinese state media have reported test kit shortages and processing bottlenecks, which could produce an undercount.
But Dr. Lipkin said he knew of one lab running 5,000 samples a day, which might produce some false-positive results, inflating the count. “You can’t possibly do quality control at that rate,” he said.
Anecdotal reports from China, and one published study from Germany, indicate that some people infected with the Wuhan coronavirus can pass it on before they show symptoms. That may make border-screening much harder, scientists said.
Epidemiological modeling released Friday by the European Center for Disease Prevention and Control estimated that 75 percent of infected people reaching Europe from China would still be in the incubation periods upon arrival, and therefore not detected by airport screening, which looks for fevers, coughs and breathing difficulties.
But if thermal cameras miss victims who are beyond incubation and actively infecting others, the real number of missed carriers may be higher than 75 percent.
Still, asymptomatic carriers “are not normally major drivers of epidemics,” Dr. Fauci said. Most people get ill from someone they know to be sick — a family member, a co-worker or a patient, for example.
The virus’s most vulnerable target is Africa, many experts said. More than 1 million expatriate Chinese work there, mostly on mining, drilling or engineering projects. Also, many Africans work and study in China and other countries where the virus has been found.
If anyone on the continent has the virus now, “I’m not sure the diagnostic systems are in place to detect it,” said Dr. Daniel Bausch, head of scientific programs for the American Society of Tropical Medicine and Hygiene, who is consulting with the W.H.O. on the outbreak.
South Africa and Senegal could probably diagnose it, he said. Nigeria and some other countries have asked the W.H.O. for the genetic materials and training they need to perform diagnostic tests, but that will take time.
At least four African countries have suspect cases quarantined, according to an article published Friday in The South China Morning Post. They have sent samples to France, Germany, India and South Africa for testing.
[Like the Science Times page on Facebook. | Sign up for the Science Times newsletter.]
At the moment, it seems unlikely that the virus will spread widely in countries with vigorous, alert public health systems, said Dr. William Schaffner, a preventive medicine specialist at Vanderbilt University Medical Center.
“Every doctor in the U.S. has this top of mind,” he said. “Any patient with fever or respiratory problems will get two questions. ‘Have you been to China? Have you had contact with anyone who has?’ If the answer is yes, they’ll be put in isolation right away.”
Assuming the virus spreads globally, tourism to and trade with countries besides China may be affected — and the urgency to find ways to halt the virus and prevent deaths will grow.
It is possible that the Wuhan coronavirus will fade out as weather warms. Many viruses, like flu, measles and norovirus, thrive in cold, dry air. The SARS outbreak began in winter, and MERS transmission also peaks then, though that may be related to transmission in newborn camels.
Four mild coronaviruses cause about a quarter of the nation’s common colds, which also peak in winter.
But even if an outbreak fades in June, there could be a second wave in the fall, as has occurred in every major flu pandemic, including those that began in 1918 and 2009.
By that time, some remedies might be on hand, although they will need rigorous testing and perhaps political pressure to make them available and affordable.
In China, several antiviral drugs are being prescribed. A common combination is pills containing lopinavir and ritonavir with infusions of interferon, a signaling protein that wakes up the immune system.
In the United States, the combination is sold as Kaletra by AbbVie for H.I.V. therapy, and it is relatively expensive. In India, a dozen generic makers produce the drugs at rock-bottom prices for use against H.I.V. in Africa, and their products are W.H.O.-approved.
Another option may be an experimental drug, remdesivir, on which the patent is held by Gilead. The drug has not yet been approved for use against any disease. Nonetheless, there is some evidence that it works against coronaviruses, and Gilead has donated doses to China.
Several American companies are working on a vaccine, using various combinations of their own funds, taxpayer money and foundation grants.
Although modern gene-chemistry techniques have made it possible to build vaccine candidates within just days, medical ethics require that they then be carefully tested on animals and small numbers of healthy humans for safety and effectiveness.
That aspect of the process cannot be sped up, because dangerous side effects may take time to appear and because human immune systems need time to produce the antibodies that show whether a vaccine is working.
Whether or not what is being tried in China will be acceptable elsewhere will depend on how rigorously Chinese doctors run their clinical trials.
“In God we trust,” Dr. Schaffner said. “All others must provide data.”
from WordPress https://mastcomm.com/wuhan-coronavirus-looks-increasingly-like-a-pandemic-experts-say/
0 notes
Text
Everything You Need To Know About Hepatitis C
Hepatitis C is a virus that causes inflammation and damages the liver. It can be chronic or acute and develops after an individual is infected with the Hepatitis C virus (HCV). There’s no vaccine available for Hepatitis C, unlike A and B. The spread of Hepatitis C all over the world can be attributed to the fact that this is a highly contagious virus.
Viral Hepatitis Types
There are 5 viral classifications of Hepatitis (A, B, C, D & E), that affect the liver, with each of the Hepatitis types caused by a different virus.
Hepatitis A is a short-term infection and is usually acute. Hepatitis B, C, and D can persist over a long time, and will, in most cases, be chronic. Hepatitis E, on the other hand, is often acute, but it can be extremely dangerous for pregnant women.
Hepatitis A. This type is caused by the Hepatitis A virus (HAV). The most common form of transmission is by coming into contact with or consuming water or food that’s contaminated with feces from a Hepatitis A infected person.
Hepatitis B. This type is transmitted through contact, especially with infected body fluids like vaginal secretion, blood, semen that contain the HBV virus. Engaging in high-risk activities such as unprotected sex with an infected person, using injectable drugs or sharing things like needles and razors increase the risk of infection.
According to the CDC, more than 350 million people in the world have Hepatitis B, with more than 1.2 million in the US alone.
Hepatitis C. As mentioned earlier, Hepatitis C is transmitted through infection with the HCV virus. It’s transmitted through direct contact with body fluids from an infected person, as is the case with Hepatitis B. This is one of the most common viral blood infections in the US, with more than 3 million Americans currently infected.
Hepatitis D. Hepatitis D is also known as delta hepatitis and is a chronic liver infection that’s caused by the hepatitis D virus (HDV). Transmission also happens through contact with blood or body fluids from an infected person.
The occurrence of hepatitis D is unique because it only occurs together with hepatitis B. Without hepatitis B, hepatitis D cannot manifest.
Hepatitis E. While the other types are transmitted through interaction with body fluids from an infected person, hepatitis E is different. It occurs as a result of infection with the hepatitis E virus (HEV). This is a waterborne virus that primarily manifests as a result of improper sanitation. Usually, those affected have consumed water that’s contaminated with fecal matter. It’s an uncommon virus in the US, and most of the cases are reported in Africa, Central America, Asia and the Middle East.
Chronic Hepatitis C. When you are infected with hepatitis C, the symptoms can manifest in a very short time and will last a number of weeks. Chronic hepatitis, on the other hand, gradually develops within a few months. During the early stages, it might not even be noticeable. Currently, there are more than 70 million people all over the world who suffer from chronic Hepatitis C, according to the World Health Organization (WHO).
Symptoms of Hepatitis C
According to the Center for Disease Control and Prevention, CDC, more than 70% of the people who have Hepatitis C never show any symptoms. However, there are some who might report mild symptoms, that might often be mistaken for something else.
Some of the symptoms of Hepatitis C include:
Jaundice
Discomfort or abdominal pain
Appetite loss
Dark urine
Fever
Pain in the joints
These symptoms are not instant. In fact, in some patients, they might appear only after 6 weeks.
Symptoms of Hepatitis C in Men
Men are usually more vulnerable to infections than women, and when they are infected, they struggle to fight off the virus. Based on relevant studies, there’s a higher clearance rate in women than in men. This is the rate at which the body rids itself of the virus to the point that it cannot be detected at all.
In fact, more women can clear the virus than men. Scientists haven’t been able to find the real reason behind this but there are some possible factors that might be responsible, including the following:
Whether the infected person has other infections like HIV
The age when the person got infected with Hepatitis C
How they got infected (drug use, sexual contact, blood transfusion)
This is a blood-borne disease, so it can only be transmitted through contact with blood from an infected person. There are several ways through which this can happen, including sexual intercourse.
There’s actually a higher risk of contracting Hepatitis C through anal sex, basically because of the fragile nature of the anal tissues which may tear and bleed during intercourse. Infection can occur even with the tiniest exchange of blood between the infected and non-infected party. In fact, microscopic tears on the skin that you might not be able to see with a naked eye are more than enough to warrant infection.
There are other people too who might have a high risk of Hepatitis C infection, especially those who do the following:
Were born between the years 1945 and 1964
Have HIV/AIDS
Have had a blood transfusion or organ transplant before 1992
Require dialysis for a very long time
Have a body piercing or tattoo from infected needles
Share needles when using recreational drugs.
You might not necessarily engage in high-risk behavior, but the mere act of sharing a toothbrush or razor blade with someone who’s infected can be enough to pass on the HCV virus.
How Do People Get Hepatitis C?
Hepatitis C is only transmitted from infected persons through blood to blood contact.
There are several cases when this can happen, including the following:
Bloodied sexual contact
Childbirth if the mother has Hepatitis C
Sharing needles
Sharing toothbrushes
Sharing a razor blade
Blood transfusion
Organ transplant
There are people who are considered high-risk persons, and vulnerable to Hepatitis C infection.
They include those who:
Reuse needles
Have sex with an infected partner
Were born to an infected mother
Have been receiving hemodialysis for a long time
Have used blood products like clotting factor concentrates before 1987
Have had an organ transplant
Have had a blood transfusion before 1992
Is It Contagious?
While Hepatitis C is contagious, it’s highly unlikely that you will be infected through casual contact. It only spreads through blood contact. In fact, there are lots of other infections out there that are way more contagious than hepatitis C.
How Hepatitis C Can’t Spread
Hepatitis C is not an airborne disease like a common cold. Therefore, you cannot get it when you share your food with someone, through coughing or sneezing. It’s also not possible to get infected by hugging or kissing someone who’s already infected.
However, there’s a small chance of infection in case you share some of your personal care items with someone who’s already infected, like a razor blade or a toothbrush. Anything that creates a chance of blood to blood contact is a risk.
On the same note, there’s a very low risk of infection through sexual contact, especially if both participating parties maintain a monogamous lifestyle. However, in case one of the partners has ever engaged in multiple sexual relationships, has had sex with someone infected with Hepatitis C, or might engage in a high-risk sexual behavior, you need to consider using protection.
For those who travel from time to time, you cannot be infected when you travel abroad, unless through blood to blood contact with someone who has Hepatitis C, or if you receive a blood donation from an infected person.
How to Diagnose Hepatitis
History and Physical Exam. The doctor must first study your medical history to check for any risk factors that you might be exposed to, which leave you vulnerable to hepatitis (infectious or not). During the physical examination, the doctor tries to see if you feel tenderness or pain by pressing down on your abdomen gently.
They must also run tests to determine whether the liver has become larger. Other signs that the doctor will be looking for include yellow eyes or yellow skin.
Liver Function Tests. These are tests that are conducted through blood samples to understand the efficiency of your liver’s performance. The first indication that you might be having a problem will be abnormal results from these tests, particularly for someone who doesn’t show any sign of a problem during the physical live examination.
The doctor will know your liver is under undue pressure, damaged or is not working at full capacity when they notice high levels of liver enzymes.
Other Blood Tests. In case all your liver tests come back abnormal, your doctor will request for more tests in order to identify where the problem lies. These tests will look for, among other things, hepatitis-causing viruses. These can also be used to look for antibodies that occur naturally in the body in such a situation.
Ultrasound. You might be asked to do an ultrasound test. The ultrasound waves show images of all the organs that lie within the abdominal cavity. Through this test, the doctor has the best view of the liver and the organs close by.
This test will also show the following:
Tumors in the liver
Gallbladder abnormalities
Enlarged or damaged liver
Fluid within the abdomen
In these images, it might also be possible to see the pancreas. This is one of the most useful tests that can tell the doctor the real reason behind your abnormal liver function.
Liver Biopsy. Through a biopsy, the doctor will be able to get sample tissue from the liver, which they can then take to the lab to run tests. This procedure doesn’t always require surgery since it can also be done with a needle through the skin. In other cases, the doctor might use an ultrasound to guide them as they take the sample.
It’s from this test that the doctor can figure out how damaged the liver is as a result of the inflammation. This might also be used to get samples of the parts of the liver which might seem abnormal.
Hepatitis C Antibody
When foreign substances get into the body, the immune system is triggered to produce antibodies. These are produced uniquely to fend off the foreign substance. Therefore, when you are infected with Hepatitis C, the body will produce Hepatitis C antibodies to fight the HCV virus.
Your body will only produce Hepatitis C antibodies in case you already have Hepatitis C. Therefore, this test is useful in determining whether you have an HCV infection or not.
Hepatitis C Vaccine
At the time of this writing, there’s no vaccine for Hepatitis C. There are, however, several ways to prevent and treat Hepatitis C.
How to Treat Hepatitis
The treatment options for hepatitis depend on two things, the type of hepatitis and whether it is chronic or acute.
Hepatitis A. This is a short-term infection, and in most cases, you might not need treatment. Most of the time, patients simply get bed rest, especially if they feel uncomfortable. In case you have diarrhea or you vomit a lot, your doctor can guide you on the best procedure for nutrition and hydration.
There’s, however, a vaccine for Hepatitis A which is usually administered to children between 12 and 18 months old. For adults, there’s also a vaccine which is administered together with the vaccine for Hepatitis B.
Hepatitis B. Specific treatment is not always necessary for acute Hepatitis B. However, there’s an antiviral medication that can be used to treat chronic Hepatitis B. Treatment might last a few months or years in some cases, so it might be an expensive ordeal.
The patient will also need to consult a doctor from time to time while keeping tabs on the virus to make sure it’s responding well to the treatment.
Vaccination is the easiest way to prevent Hepatitis C. According to the CDC, all newborn babies should get the vaccine which is available in a set of three vaccines. They should be done by the time the child turns 6 months old. Everyone in the healthcare industry is also advised to get this vaccine.
Hepatitis C. There are antiviral medicines that are used to treat chronic and acute Hepatitis C. Individuals who develop chronic Hepatitis C might be given different drug therapies. To determine the best treatment, they might also be subject to more tests.
If you have developed liver cirrhosis as a result of chronic Hepatitis C, one of the best options for you would be a liver transplant. As it is, there’s no known vaccine available for Hepatitis C.
Hepatitis D. There’s no medicine yet for treating Hepatitis D. However, in 2013, a study was conducted using a trial drug, Alpha Interferon to treat Hepatitis D. This drug only yielded progress in around 30% of those who used it.
It’s, however, possible to prevent hepatitis D by using the Hepatitis B vaccine, because it cannot develop without hepatitis B.
Hepatitis E. There are no medical therapies present for treating hepatitis E. More often, this infection is acute, and as a result, it just resolves on its own. Individuals who have Hepatitis E usually get relief by resting, eating enough nutrients, drinking lots of fluids and keeping away from alcohol for a while. In the case of pregnant women, however, it’s advisable to see a doctor for further monitoring.
Autoimmune Hepatitis. Treating autoimmune hepatitis during the early stages is easier with the use of corticosteroids like budesonide and prednisone. More than 80% of individuals who have taken these treatments have had good results.
One of the most effective drugs that are usually administered is Azathioprine (Imuran) which can be administered with or without the use of steroids. There are other drugs that can be used as an alternative to Azathioprine, including Tacrolimus, Mycophenolate, and Cyclosporine.
Hepatitis C Medications
There are several medicines that have been used in the past to treat Hepatitis C, including antivirals and interferons. Not all the hepatitis medicines treat all the HCV infections, especially because of various genotypes of the HCV virus. Your doctor will try to figure out the type of Hepatitis C you have so that they can prescribe the right medication that will work best for you.
Complications Associated with Hepatitis C
There are a lot of complications that might be associated with Hepatitis C, including liver cancer and cirrhosis. In some severe cases, the Hepatitis C patients will need to have a liver transplant. Most of the time, complications occur as a result of chronic Hepatitis C.
The sooner you can get a diagnosis for chronic Hepatitis C, the sooner you should start your treatment so that you don’t have to experience the full-blown complications.
Hepatitis C Guidelines
Hepatitis C will manifest in different people in a unique way. Because of this reason, there’s no specific guideline for managing the infection. However, you can talk to your doctor about making a few changes in your life that will help you manage the infection better, like making lifestyle changes or starting a new diet.
Hepatitis C Screening
Hepatitis C is transmitted through the blood so it can’t spread as easily as most of the other infectious diseases. While there might be treatments for Hepatitis C, most of them come with serious side effects. One of the safest options you have is prevention.
In case you are a high-risk individual, it’s wise to get Hepatitis C screening regularly. In case you get infected, the earlier you know about this and start treatment, the better.
Acute vs. Chronic Infection
Doctors use the type of hepatitis virus to determine whether you have an acute or chronic infection. An acute infection shouldn’t last more than 6 months. Anything that exceeds 6 months is a chronic infection.
In the case of Hepatitis B, the infection can either be chronic or acute. Most of the people who have acute hepatitis B rarely progress to the chronic level. On the other hand, acute Hepatitis C can easily advance to chronic levels. In fact, more than 75% of people who are diagnosed with Hepatitis C usually advance to chronic Hepatitis C, according to reports from the CDC.
If you have acute Hepatitis C, you might not display any symptoms. In fact, most of the acute hepatitis C cases are asymptomatic. This means that you barely notice the symptoms. Only around 15% of the acute infections usually show symptoms.
Mortality Risk
A high percentage of people who have Hepatitis C barely ever clear the virus, and as a result, they become chronic carriers.
This can become a problem later on in life because the infection will cause other problems that can be fatal such as the following:
Liver Cancer. When liver cells are reproducing at a fast rate, you might develop tumors which can cause liver cancer. If the Hepatitis C advances to cirrhosis, you will be at a very high risk of liver cancer.
Cirrhosis. This happens as a result of fibrosis (when scar tissues build up) dominating the liver. In case you have cirrhosis, the healthy normal tissue will be replaced by the hard scar tissue, and this prevents the normal function of the liver. It’s important to know that it might take up to 30 years of damage to the liver for cirrhosis to develop.
Liver Failure.This is an advanced stage of the liver disease which means that the liver will have been damaged to the point when it doesn’t function properly. You might even develop jaundice, ascites, stomach bleeding or hepatic encephalopathy. If you have these symptoms, you are in serious need of a liver transplant to save your life.
Every year, more than 300,000 people die as a result of liver diseases linked to Hepatitis C. The only way to prevent this from happening is to seek medical help as soon as you confirm the diagnosis. This is the easiest way to mitigate the damage that hepatitis might do to your body.
How Does Hepatitis C Affect Your Body?
There are two stages of Hepatitis C; chronic and acute. Acute Hepatitis C is within the first 6 months of exposure to the hepatitis virus. It might be a short-lived illness in some people. However, according to the CDC, most people (around 80%) whose immune system doesn’t clear out the virus at this stage eventually advances to the chronic stage. Chronic Hepatitis C can be a lifelong battle. In fact, most people don’t even notice they are infected until some of the symptoms start showing.
Your Liver. The role of the liver is to process blood and filter toxic substances from the bloodstream. The liver also helps with digestion, produces proteins, bile, and important blood components. A healthy liver should also help the body store vitamins and glucose. An HCV infection will inflame the liver, damaging its ability to perform all the important functions it does.
Some of the symptoms might be mild during the early stages, and it’s important to get treatment as soon as possible so that the damage doesn’t become too serious. A chronic infection can easily advance to cirrhosis. As the infection progresses, there are certain symptoms that you will notice like blood disorder, skin problems, and weight loss. When things get out of hand, liver failure, liver cancer, and severe liver damage are possible.
You can visit a doctor to test and measure the HCV antibodies present in your bloodstream. The presence of HCV antibodies in the blood means you are already infected. However, a second blood test would help you allay any fears.
Digestive System. It’s important that you keep your liver healthy, considering that the liver supports several body systems. The liver produces bile, an important substance in fat synthesis. The body stores bile in the gallbladder and transports it to the small intestine as and when needed. The bile will then mix with digestive fluids including stomach acid from the pancreas, helping this way with nutrient absorption into the bloodstream.
The HCV virus will affect the liver’s bile production. When this happens, you will find it difficult to digest fatty food. Over time you will also experience a buildup of fluids within the stomach which can result in abdominal pain. This is a condition known as ascites. It happens when the liver is unable to produce the required amount of albumin to regulate the cellular fluid content.
Some of the other symptoms that you might be having liver problems include:
Clay or pale-colored stool
Weight loss
Lack of appetite
Vomiting
Nausea
If HCV causes inflammation in your gallbladder, you might endure a lot of pain. This is, however, a rare occurrence, and it only happens during the acute stage of the infection.
Central Nervous System. As long as the liver is unable to filter toxic substances from the blood, it might damage the nervous system. There are a number of symptoms that you might notice, including musty breath, sleep deprivation or problems with your motor skills. In some cases, HCV infection is also linked to dryness in the mouth and eyes.
When toxins build up in the brain, they can cause any of the following situations:
Personality disorders
Lack of concentration
Forgetfulness
Confusion
Some of the advanced cases include the following symptoms:
Slurry speech
Disorientation
Agitation
Abnormal shaking
In severe instances, you might even end up in a coma.
Circulatory System. Other than filtering out toxins from the body, the liver is also involved in protein synthesis for clean healthy blood and makes sure your blood clotting is regulated. If your liver is not performing well, you might have problems with blood flow, which eventually increases pressure to the portal vein. This, in the long run, causes portal hypertension which eventually forces blood to find pathways through other veins. When blood is forced into these veins, the undue pressure can make them rupture, causing severe internal bleeding (variceal bleeding).
It’s, therefore, impossible for a liver that’s not functioning well to transport, absorb or store iron, and as a result, you might suffer anemia.
Integumentary System. There are several skin problems that are associated with Hepatitis C. Some of the common ones include a loss in the skin pigment, bruises in the eyes, itching, and rashes. One of the important byproducts of hemoglobin breakdown is bilirubin. As long as the liver is not functioning properly, bilirubin will pile up in the body, resulting in jaundice. You will notice this when the skin and eyes start turning yellow. Improper function of the liver might also be caused by poor nutrition, and you will notice this in stunted growth of the nails and hair.
Endocrine and Immune Systems. The role of the endocrine system is to regulate hormones in the body. The thyroid gland is an important part of this system, and its role is to push the hormones into the bloodstream. There are instances where Hepatitis C might cause the immune system to attack the thyroid tissue.
When this happens, there are two possibilities:
An overactive thyroid – hyperthyroidism, which will cause weight loss and sleep problems
An underactive thyroid – hypothyroidism, which can cause weight gain or fatigue
Having a healthy liver is important in managing the way sugar is consumed within the body. This also translates to keeping away type 2 diabetes.
Hepatitis C Diet
In case you have been diagnosed with Hepatitis C, there’s no specific diet that you need to keep. However, you should limit your intake of junk food, and instead, start eating healthy food.
The liver naturally acts upon anything that you drink or eat. Therefore, by keeping a proper, clean diet, you will easily improve your liver health, and reduce the damage that can be caused by Hepatitis C.
You should know that your liver is already struggling with inflammation by the time you have Hepatitis C. As time goes by, this might end up in cirrhosis or scarring of the liver, which will definitely hamper or reduce the function of the liver. Since the liver already has too much to deal with, keeping a clean healthy diet might make things easier for your liver.
What You Should Eat
Naturally, you need to get the best nutrients with your meals to live a healthy life. This will go a long way towards protecting your immune system and will also boost your weight management efforts.
You should always keep an eye on your weight when you have Hepatitis C. This is because the more weight you gain, the higher your risk of hepatic steatosis will be. This is a condition where a lot of fat is deposited into the liver, which might eventually make it difficult to control Hepatitis C.
With Hepatitis C, you are already at risk of type 2 diabetes, so it would be wise to be keen on the amount of sugar you consume. You should also consider meal plans, especially approved meal plans like the United States Department of Agriculture MyPlate Plan.
In this plan, the following are the recommendations for a balanced diet:
Fruits and Vegetables
Fruits and vegetables are important because they provide the following:
Vitamin B6
Vitamin B12
Vitamin C
Vitamin A
Folic acid
Fiber
You should try to have no less than 5 servings of fruits and vegetables daily. To get the best results, try to get a variety in the type of fruits and vegetables that you eat. If you buy canned food, make sure you get the ones that don’t have sugar or salt additives.
Protein. Protein foods are important because protein helps replace and repair damaged liver cells.
Some of the best lean protein options you have to include:
Soy products
Eggs
Nuts
Chicken (skinless)
Seafood
Fish
The recommended amount of daily protein intake depends on things like your level of activity, sex, and age. At least 5 ounces of protein a day is good for you, but for people who have liver cirrhosis, the doctor might recommend more in order to prevent fluid buildup and muscle damage.
Dairy Products. like cheese, yogurt, and milk are rich sources of calcium and proteins. Adults need up to 3 dairy servings daily. When factoring cheese into your diet, a cup should count as two ounces of processed cheese or 1 ½ ounces of natural cheese.
Whole Grains. Whole grains provide natural fiber which helps with proper bowel function and also reduce your risk of heart disease.
Some of the best options you have to include:
Oats
Wild or brown rice
Whole buckwheat
Quinoa pasta
Sprouted whole grain bread
Don’t go for the refined or white products. Instead, insist on whole grain because they have a higher content of:
Iron
Magnesium
Zinc
Fiber
Vitamin B group
In the unlikely event that you have Celiac disease, you should stick to gluten-free options like amaranth, quinoa, and buckwheat. The quantity varies according to your sex, level of activity and age. An adult needs at least 3 ounces of grains daily, with no less than half coming from whole grains.
What You Shouldn’t Eat
You must pay attention to your calories so you will need to think about the quality as much as the quantity of the food you eat. Too much food will definitely cause weight gain, or make you obese, which makes you vulnerable to diabetes.
To be on the safe side, limit the intake of foods that are:
Canned
Frozen
Processed
Greasy
Fatty
Obtained from fast food outlets
from Health Insure Guides https://ift.tt/2v8nPfu
via health insurance cover
0 notes
Text
Why Do Your Feet Fall Asleep? Your Questions Answered!
See Why Do Your Feet Fall Asleep? Your Questions Answered! in its original form on http://ift.tt/2jv9IZl or check it out here if you prefer.
The feet falling asleep is a strange sensation. The nerves have, in some way, been compromised. People have nerve cells that carry impulses to the brain and other areas of the body. The cells (or fibers) have structures surrounding them, but they are different.
Some of the nerve fibers are thicker than others. Since the thicker ones have a protective coating to shield them, transmissions take longer.
Those who are thin are the ones who send the tingling feeling, and it does so rapidly. The feet can move when it doesn't seem possible. Once all nerve fibers return to its natural state, everything will feel normal again.
The feet fall asleep because there's too much pressure on that part of the body. This could also happen while sitting, sleeping with legs crossed, while running, or while driving. Not only is it too much pressure, but it's prolonged pressure.
What if the Tingling in My Feet Won't Go Away?
The consequences of continuing to deny transmissions a clear pathway prevent communication to other parts of the body from the brain. This isn't a good situation, but it's only minor.
When the nerves can't relay messages like they are supposed to, look for certain things that don't happen. The messages are mumbled, so the brain doesn't get it... it's strange to even the brain.
This is why we get the tingling sensations. Usually, the feet will feel like their old selves again once in another position or when they stretch out. When they persist or last for a long time, see a health specialist. What's a long time?
Several hours, for sure, however, no one should suffer for over an hour before calling their physician for medical advice. It may not be long before relief comes, but better safe than sorry. No one wants to feel like they are literally on “pins and needles.”
What Causes Numb Feet?
Why do the feet feel numb? Is it the same thing as when your feet fall asleep? Well, foot numbness is a condition, an abnormal one, of course, that anyone would feel in their toes when there's a temporary loss of blood flow.
It's because of inflammation, infection, trauma or malignancy. In some cases, a numb foot is an indication of a disease or nerve damage. However, most causes are not dangerous.
Know that people have numb feet in association tumors and strokes. What's more, the numbness, when preceded by a burning sensation, excruciating pain or prickling, is known as paresthesias.
Sitting in one place will cause numb feelings to occur also. The numbness will go away quite quickly providing there is movement. Also, the condition may become worse when it's nigh time. It's common for plenty of sufferers.
If this has been going for an extended period, there may be nerve damage and if this is the case, please, see a doctor. The numbness may be a sign of something else. Remember, the numbing sensations should not last long.
Get emergency medical assistance when there's a bowel or bladder control problem, confusion, slurred speech, or paralysis along with numb feet.
Peripheral Neuropathy: Tingling in the Feet
There are countless individuals who feel a tingling in their feet, hands, legs, and arms. Sometimes, this is nothing, but it could be a chronic condition, severe or episodic.
It's not just the tingling, but it's the itching, the pain, the muscle spasms and the numbness in the feet. Having an old injury or a recurring injury flare up, diabetes, being exposed to a toxic environment or a viral infection will trigger an episode.
Peripheral neuropathy is a familiar name especially to those with a spinal cord injury. It affects the nerves mostly in the feet and hands. Given time, peripheral neuropathy can get worse. What happens is mobility declines; it can even disable a person.
Far too many millions of Americans suffer from neuropathy. Although it's not exclusive to gender or age, it mainly happens to older citizens. Suspect diabetic neuropathy? See a doctor for a diagnosis.
Causes of Diabetic Neuropathy
Mostly everyone knows about diabetes. But how many know it is among the top reasons or causes of peripheral neuropathy? Studies show around 30 percent of diabetics have it in their feet and legs.
The symptoms are common among those who have nerve damage, but they can be severe or mild forms of neuropathy. The tingling in the feet could be a sign that a loved one has diabetes.
Alternatively, vitamin deficiencies can lead to other health conditions. On the other hand, too much of a vitamin [B6] can trigger an onset of tingling sensations. The lack of B12 is connected to pernicious anemia.
Providing there aren't any health reasons why anyone should consume vitamins or herbs, take the suggestion to include B12, B1 and vitamin E in the diet.
More than a niacin vitamin deficiency, alcohol has a tremendous impact on the nerves, and it will require a strict diet. The average alcoholic doesn't eat right. Therefore they may need more thiamine to help control their neuropathy.
What is Paresthesia?
Paresthesia is that feeling of the leg, hand or feet falling asleep. There are the classic feelings of tingling, pins-and-needles, pricking, and numbness. It could also include skin crawling and itching. The symptoms may come out of nowhere really.
Surprising, almost everybody has felt paresthesias before. It happens too when there's too much pressure applied to the feet, arms or legs. Once sitting or lying in another position, the feeling should go away. If it doesn't, it's time to see the doctor.
What are the Signs of Paresthesia?
Know paresthesia [chronic or transient] can affect any part of the body. However, the main spots are the arms, feet, hands, and legs.
Panic attacks or hyperventilating are classic symptoms of transient paresthesia whereas, with chronic paresthesia a person may have poor circulation or neuropathy. The good news is there aren't any prolonged physical effects from paresthesia.
Whether it's chronic or temporary, the signs include a burning sensation, tingling, numbness, weakness and feeling cold. With chronic paresthesia, the sufferer may have stabbing pains in the feet or legs. This can have a definite effect on walking or standing.
Getting a Diagnosis and Treatment
Having paresthesia, it's a good idea to see a specialist, a neurologist. They may perform an ACT scan to determine a final diagnosis. Treatments include therapy to work the muscles and, of course, medication. What aggravates paresthesia?
Hypoglycemia [low blood sugar]
Fibromyalgia
Herpes Zoster [shingles]
Carpal tunnel syndrome
Diabetes
Atherosclerosis
Herniated disk
If the patient has any underlying conditions, they may need different kinds of treatments. Although there isn't a cure, relief from the symptoms is still possible.
Feet Fall Asleep While Sleeping
Poor blood circulation, typically, is one of the most recognized causes why your feet fall asleep. Slow blood circulation caused by nerve compression leads to the tingling and pins and needles feelings. Remember, paresthesia can be either chronic or temporary.
Typically, it's nothing anyone should worry about, but if the feet fall asleep and stay that way, it could mean something else is the matter. Anyone having diabetes should stay on top of the condition as early detection of another medical diagnosis could save a life or a limb.
The symptoms could mean nerve entrapment or the onset of a stroke. When the arteries can't supply blood to the legs and feet, and also to the brain, the results are the numb feelings or tingling.
The body won't receive the nutrients it needs. The best advice is to stay aware and see a doctor.
What to Do When Your Feet Fall Asleep
When the feet fall asleep, it can be an uncomfortable feeling. However, there are several things one can do to get rid of a sleeping foot.
Let's check them out now.
Walking
If changing positions doesn't work, get up and move about if at all possible. Walking will help get the blood flow going again so things will return to normal. Steady as it goes, though. Use something to hold on to until the feelings revert to normal.
If not, consider the possibility of a fall. Once on the feet or in another position, the time it takes for anyone to regain stability is short. There's also the risk of permanent damage if the condition is not taken care of promptly.
Switching Positions
The circulation is cut off, albeit temporarily, so it can be aggravating. Sitting for a long time can cause poor blood circulation in the feet.
Something as simple as uncrossing the legs can return blood flow back to its original state. Before the circulation returns to normal, however, the leg or foot will feel warm or prickly.
Soak the Feet in Warm Water
If the pain in the feet is caused by strained muscles, take a warm bath or an Epsom Salt foot soak. This will help stimulate the body, but especially, the feet and increase blood flow. Trust the magnesium in the salt bath to soothe muscles and even reduce inflammation.
Do this for about 15 minutes or longer if you want, just keep the water warm. You can make the experience pleasurable with an electric foot spa.
Don't forget to include more B12 or vitamin B6 to the diet.
Wear Fitting Shoes
Women are the worse at buying and wearing ill-fitting shoes. This only contributes to the pins-and-needles feelings they get when trying to cram their feet into shoes too small. The feet fall asleep because of poor circulation.
The shoes can grip the heels or cause the feet to scrunch up. If there's not any wiggle room in the shoe, it's too small. Try not to wear pointed toed shoes which are two sizes too small and loosen laces on shoes to prevent compression.
Going to be sitting for a while? Take the shoes off. This will allow the feet a chance to breathe and the blood to flow properly. If you have to wear shoes that are tight, use a shoe stretcher device to create some extra room.
Feet Fall Asleep While Running?
It's difficult to understand why the feet fall asleep while running since the major cause is poor blood circulation. However, when it comes to running, the sensations are likely from muscle strain, soreness, and restriction.
Ordinarily, one would think the feet go numb while sitting too much, too long. It's surprising to find this often happens to runners. On a positive note, this can also be cured once the pressure is taken off the limb.
The nerves that would cause the tingling or numbness gets trapped right between the soft tissue and the bones. The worse that could happen is tripping and falling. Before it comes to that, stop and take the shoes off.
Rub the feet until the feelings come back. Remove any socks or braces that could be preventing circulation as well.
Causes of Nerve Compression
The nerves serve a significant purpose in the body. When they are prevented from doing their job, it can cause damage to a nerve, cause swelling, injury or trauma.
Trauma. Trauma causes the feet to swell or direct injury to a particular nerve cell. The injury will cause the feet to swell and lead to numbness. This happens when runners suddenly increase the miles they run or if they are running with improper gear or too tight clothing.
Flat feet. It's been an obstacle for runners for a long time. Having flat feet means a runner can suffer an injury quicker than someone who has flexibility in their feet.
Scar tissue. When the nerves are compressed time after time, they become thick and develop scar tissue or [Morton's] neuroma. Morton's neuroma is typically known to occur between the second base and third base of the toes.
Also, foot numbness or numbness of the heel is also caused by the compression of the sciatic nerve. This is a long nerve, which runs from the spinal cord to the back of the legs.
It can because of compression from a herniated disk or muscles which overlap the nerve that makes this condition painful and extremely uncomfortable. Sometimes, the pain is relieved by changing positions or stretching out the body.
DIY Treatments
To take the shoe by the horn and help alleviate conditions associated with nerve compression, buy the right size shoes. Make sure there is wiggle room inside for the heel and toes. Also, shoes with a strong sole will help take the pain away.
Some shoes can cause the feet to fall asleep or to swell. More so, it can cause trauma to the feet, so don't lace up so tightly. Remove thick tub socks if they feel as though they are too tight as well and any braces. Check the way the run is done.
The stride should be done correctly to avoid pounding the pavement. Stay at a steady pace and increase mileage gradually.
Getting Medical Help
When the self-help tips don't work, make an appointment with a podiatrist. Likely, the doctor will want a complete medical background to determine if there is any family history of certain diseases.
This history could help the doctor find out which illnesses could be associated with numbness and tingling. The doctor will require x-rays to figure out why do your feet fall asleep. The physician may write a prescription for special shoes or inserts to put in the shoes, a set of specific exercises to do at home and an anti-inflammatory drug for swelling. In cases where the illness is severe, the doctor may order other treatment options, perhaps surgery.
Why Do Your Feet Fall Asleep While Lying Down?
Occasionally, the feet fall asleep when a person is lying down. Then come the tingling and other feelings such as pins-and-needles being poked into the skin. This is not a pleasant sensation at all to have.
However, many people go through it, or they suffer from Celiac disease. The symptoms of Celiac disease are often brushed off because of the minor conditions these people experience in the beginning.
Nonetheless, Celiac disease is a severe condition or autoimmune disorder that, with all probability, is inclined to be passed on to other generations. Those who suffer from it should avoid foods containing gluten. In their case, gluten damages the small intestine.
About one in a hundred people have it in the nation. Over two million cases go undetected, and because of this, they are at risk for other health conditions. The tingling affects a person's face, legs, and feet, plus their arms.
Instead of getting relief laying down, it happens while that person is in bed. To correct the problem, some professionals believe taking vitamin B6 will help. People who have Celiac disease need to incorporate a gluten-free diet into their routine.
Foods like rye, wheat or barley can have an effect on the people with this condition. The fact is they damage the lining of the [small] intestine. Nutrients aren't absorbing into the body as a result of the damage to the intestine. The people with a history of tingling/numbness are more likely to inherit this disease.
What Causes My Foot to Fall Asleep While Driving?
The reason the feet are falling asleep could be related to the nerves in the back.
Is the position more on the extra comfortable side or does it make the body straight? The ideal position would be in the upright sitting position instead of leaning back or lean to one side. This can cause pressure on the lower part of the body and stop the natural flow of communication and blood circulation.
As a result, the foot falls asleep while driving. Sometimes, it's a good idea to have it checked out by a professional. Speak with the doctor or make an appointment with the podiatrist to find the cause and the cure.
Why Do Your Feet Fall Asleep While Legs Are Crossed?
Who's not doing some form of Pilates or yoga these days? Some people are having issues, however, when crossing their legs. Certain ones are saying their legs or feet fall asleep while sitting with legs crossed. It's uncomfortable and distracting.
Who can meditate while feeling like pins-and-needles are sticking in them? It's almost impossible, especially if there's been an injury to the leg or foot. The best DIY advice here is to stretch it out and to use a cushion between the floor and the leg and feet.
Try out different positions before starting the exercise program. Get comfortable sitting with the pillows. After all, the idea is to be able to perform the meditating exercises without stress.
Why Do Your Feet Fall Asleep While Standing?
A person could be standing in line at the post office or market, and suddenly, their feet will start to numb and then fall asleep. Rid the feet of that feeling could be as easy as shaking the feet or making some movement with it.
Why does this happen? Well, it could be that too much pressure is on the foot or something somehow is prevent blood flow to the feet and legs. Is this a constant occurrence? How long does it last? If it happens during sleep more than a couple of times a week, see a doctor.
There could be several reasons why the feet fall asleep while standing but to make sure, make that appointment. The cause and the cure should be determined as soon as possible to prescribe any medications or therapy.
The fact it could be -
Peripheral arterial disease [PAD] – Peripheral artery disease occurs when the legs aren't getting enough blood. When the legs and feet don't get enough blood supply, it causes leg and foot pain or numbness.
Meralgia paresthetica – This happens because of nerve entrapment, preventing the passage to the inguinal ligament.
Meralgia paresthesia and PAD are enough reasons to confirm the cause of the feet falling asleep while standing. A restricted nerve is not always a cause for alarm. It is also a valid reason to see the doctor routinely.
Please, don't put it off as early detection can save a life.
Why Do Your Feet Fall Asleep While Sitting on the Toilet?
Although they are ultimately strong, the nerves have a sensitive side as well. They react to compression or pressure by numbing parts of the body. It could be something as typical as sitting at tas sitting on the toilet.
The problem with this is other areas are affected as the blood supply is cut off from them in the process of numbing the feet. Numbness, tingling, and burning means something is not right with the body.
In other words, the body is trying to get an individual's attention. When nerve compression lasts for long periods, there could be another reason for it, which requires the person to seek medical care.
A person's weight could be a cause of the feet falling asleep while sitting on the toilet or the way they sit on the toilet.
The long-term effects of having Celiac disease can have severe consequences. Celiac disease can happen to anyone – Black Americans, Europeans or Asians. A person's race, culture or social status doesn't matter. It happens to thousands of people every day.
This is especially true if anemia, miscarriage, migraines, epilepsy and neurological conditions are present. Mostly, those who suffer, are likely to have other diseases that affect the body. The disease can set off multiple sclerosis and type 1 diabetes.
0 notes
Text
Wuhan Coronavirus Looks Increasingly Like a Pandemic, Experts Say
The Wuhan coronavirus spreading from China is now likely to become a pandemic that circles the globe, according to many of the world’s leading infectious disease experts.
The prospect is daunting. A pandemic — an ongoing epidemic on two or more continents — may well have global consequences, despite the extraordinary travel restrictions and quarantines now imposed by China and other countries, including the United States.
Scientists do not yet know how lethal the new coronavirus is, however, so there is uncertainty about how much damage a pandemic might cause. But there is growing consensus that the pathogen is readily transmitted between humans.
The Wuhan coronavirus is spreading more like influenza, which is highly transmissible, than like its slow-moving viral cousins, SARS and MERS, scientists have found.
“It’s very, very transmissible, and it almost certainly is going to be a pandemic,” said Dr. Anthony S. Fauci, director of the National Institute of Allergy and Infectious Disease.
“But will it be catastrophic? I don’t know.”
In the last three weeks, the number of lab-confirmed cases has soared from about 50 in China to 14,000 in 23 countries; there have been over 300 deaths, all but one in China.
But various epidemiological models estimate that the real number of cases is 100,000 or even more. While that expansion is not as rapid as that of flu or measles, it is an enormous leap beyond what virologists saw when SARS and MERS emerged.
When SARS was vanquished in July 2003 after spreading for nine months, only 8,098 cases had been confirmed. MERS has been circulating since 2012, but there have been only about 2,500 known cases.
The biggest uncertainty now, experts said, is how many people around the world will die. SARS killed about 10 percent of those who got it, and MERS now kills about one of three.
The 1918 “Spanish flu” killed only about 2.5 percent of its victims — but because it infected so many people and medical care was much cruder then, 20 to 50 million died.
By contrast, the highly transmissible H1N1 “swine flu” pandemic of 2009 killed about 285,000, fewer than seasonal flu normally does, and had a relatively low fatality rate, estimated at .02 percent.
The mortality rate for known cases of the Wuhan coronavirus has been running about 2 percent, although that is likely to drop as more tests are done and more mild cases are found.
It is “increasingly unlikely that the virus can be contained,” said Dr. Thomas R. Frieden, a former director of the Centers for Disease Control and Prevention who now runs Resolve to Save Lives, a nonprofit devoted to fighting epidemics.
“It is therefore likely that it will spread, as flu and other organisms do, but we still don’t know how far, wide or deadly it will be.”
In the early days of the 2009 flu pandemic, “they were talking about Armageddon in Mexico,” Dr. Fauci said. (That virus first emerged in pig-farming areas in Mexico’s Veracruz State.) “But it turned out to not be that severe.”
An accurate estimate of the virus’s lethality will not be possible until certain kinds of studies can be done: blood tests to see how many people have antibodies, household studies to learn how often it infects family members, and genetic sequencing to determine whether some strains are more dangerous than others.
Closing borders to highly infectious pathogens never succeeds completely, experts said, because all frontiers are somewhat porous. Nonetheless, closings and rigorous screening may slow the spread, which will buy time for the development of drug treatments and vaccines.
Other important unknowns include who is most at risk, whether coughing or contaminated surfaces are more likely to transmit the virus, how fast the virus can mutate and whether it will fade out when the weather warms.
The effects of a pandemic would probably be harsher in some countries than in others. While the United States and other wealthy countries may be able to detect and quarantine the first carriers, countries with fragile health care systems will not. The virus has already reached Cambodia, India, Malaysia, Nepal, the Philippines and rural Russia.
“This looks far more like H1N1’s spread than SARS, and I am increasingly alarmed,” said Dr. Peter Piot, director of the London School of Hygiene and Tropical Medicine. “Even 1 percent mortality would mean 10,000 deaths in each million people.”
Other experts were more cautious.
Dr. Michael Ryan, head of emergency responses for the World Health Organization, said in an interview with STAT News on Saturday that there was “evidence to suggest this virus can still be contained” and that the world needed to “keep trying.”
Dr. W. Ian Lipkin, a virus-hunter at the Columbia University Mailman School of Public Health who is in China advising its Center for Disease Control and Prevention, said that although the virus is clearly being transmitted through casual contact, labs are still behind in processing samples.
But life in China has radically changed in the last two weeks. Streets are deserted, public events are canceled, and citizens are wearing masks and washing their hands, Dr. Lipkin said. All of that may have slowed down what lab testing indicated was exponential growth in the infection.
It’s unclear exactly how accurate tests done in overwhelmed Chinese laboratories are. On the one hand, Chinese state media have reported test kit shortages and processing bottlenecks, which could produce an undercount.
But Dr. Lipkin said he knew of one lab running 5,000 samples a day, which might produce some false-positive results, inflating the count. “You can’t possibly do quality control at that rate,” he said.
Anecdotal reports from China, and one published study from Germany, indicate that some people infected with the Wuhan coronavirus can pass it on before they show symptoms. That may make border-screening much harder, scientists said.
Epidemiological modeling released Friday by the European Center for Disease Prevention and Control estimated that 75 percent of infected people reaching Europe from China would still be in the incubation periods upon arrival, and therefore not detected by airport screening, which looks for fevers, coughs and breathing difficulties.
But if thermal cameras miss victims who are beyond incubation and actively infecting others, the real number of missed carriers may be higher than 75 percent.
Still, asymptomatic carriers “are not normally major drivers of epidemics,” Dr. Fauci said. Most people get ill from someone they know to be sick — a family member, a co-worker or a patient, for example.
The virus’s most vulnerable target is Africa, many experts said. More than 1 million expatriate Chinese work there, mostly on mining, drilling or engineering projects. Also, many Africans work and study in China and other countries where the virus has been found.
If anyone on the continent has the virus now, “I’m not sure the diagnostic systems are in place to detect it,” said Dr. Daniel Bausch, head of scientific programs for the American Society of Tropical Medicine and Hygiene, who is consulting with the W.H.O. on the outbreak.
South Africa and Senegal could probably diagnose it, he said. Nigeria and some other countries have asked the W.H.O. for the genetic materials and training they need to perform diagnostic tests, but that will take time.
At least four African countries have suspect cases quarantined, according to an article published Friday in The South China Morning Post. They have sent samples to France, Germany, India and South Africa for testing.
[Like the Science Times page on Facebook. | Sign up for the Science Times newsletter.]
At the moment, it seems unlikely that the virus will spread widely in countries with vigorous, alert public health systems, said Dr. William Schaffner, a preventive medicine specialist at Vanderbilt University Medical Center.
“Every doctor in the U.S. has this top of mind,” he said. “Any patient with fever or respiratory problems will get two questions. ‘Have you been to China? Have you had contact with anyone who has?’ If the answer is yes, they’ll be put in isolation right away.”
Assuming the virus spreads globally, tourism to and trade with countries besides China may be affected — and the urgency to find ways to halt the virus and prevent deaths will grow.
It is possible that the Wuhan coronavirus will fade out as weather warms. Many viruses, like flu, measles and norovirus, thrive in cold, dry air. The SARS outbreak began in winter, and MERS transmission also peaks then, though that may be related to transmission in newborn camels.
Four mild coronaviruses cause about a quarter of the nation’s common colds, which also peak in winter.
But even if an outbreak fades in June, there could be a second wave in the fall, as has occurred in every major flu pandemic, including those that began in 1918 and 2009.
By that time, some remedies might be on hand, although they will need rigorous testing and perhaps political pressure to make them available and affordable.
In China, several antiviral drugs are being prescribed. A common combination is pills containing lopinavir and ritonavir with infusions of interferon, a signaling protein that wakes up the immune system.
In the United States, the combination is sold as Kaletra by AbbVie for H.I.V. therapy, and it is relatively expensive. In India, a dozen generic makers produce the drugs at rock-bottom prices for use against H.I.V. in Africa, and their products are W.H.O.-approved.
Another option may be an experimental drug, remdesivir, on which the patent is held by Gilead. The drug has not yet been approved for use against any disease. Nonetheless, there is some evidence that it works against coronaviruses, and Gilead has donated doses to China.
Several American companies are working on a vaccine, using various combinations of their own funds, taxpayer money and foundation grants.
Although modern gene-chemistry techniques have made it possible to build vaccine candidates within just days, medical ethics require that they then be carefully tested on animals and small numbers of healthy humans for safety and effectiveness.
That aspect of the process cannot be sped up, because dangerous side effects may take time to appear and because human immune systems need time to produce the antibodies that show whether a vaccine is working.
Whether or not what is being tried in China will be acceptable elsewhere will depend on how rigorously Chinese doctors run their clinical trials.
“In God we trust,” Dr. Schaffner said. “All others must provide data.”
from WordPress https://mastcomm.com/wuhan-coronavirus-looks-increasingly-like-a-pandemic-experts-say/
0 notes