#low dose naltrexone
Text
About 1 week into a trial of low-dose naltrexone (for long covid treatment). My insurance doesn't cover it, but I can thankfully still afford it.
My wife and I went to see my internal medicine doctor with basically a 4 page research paper on how it's being used to treat long covid, with citations. Doctor had never used it for that before but was willing to give it a try.
I'm hopeful it'll help even a little.
13 notes
·
View notes
Text

We’re back from the vet appointment.
As a puppy, I started our cooperative care training by teaching restraints & building duration for being restrained during procedures. Being completely Force-Free is the ultimate goal but she is a Malinois. Having her comfortably restrained gives peace of mind to the people who are working on her. The problem I’ve run into with this method is that she can only truly opt in or out at the beginning of the procedure. So when we are doing something like multiple acupuncture injections she starts to get frustrated after several injections in a row and needs to take a break before we can continue.
So while I’ve been resting at home, I’ve started introducing a chin rest as an opt in/out behavior. We got to try it out for the first time today at her appointment and she did really well. I held her collar just incase she got startled but she had the freedom to raise or lower her head to signal when she was ready for the injection. When she realized she had more control over the situation she was enthusiastic to participate and we were able to get it all done quickly.
After that she opted into a restrained hold for a quick blood draw. Following one of our walks recently I found a couple of ticks on her. She is on prevention and they were dead but she seemed swollen afterwards so we are going to test for tick born illnesses just to be safe. We should get the results in a day or so.
The vet was really impressed with how well she is doing on the LDN. She is feeling noticeably better. Her back wasn’t as tight during the acupuncture. She has more energy and is showing an impressive amount of speed and agility during play sessions which she didn’t have before. That is on .5 mg of LDN in the morning. I’m excited about her immediate improvement so now we just need to optimize the dose. I’ve started to experiment with 1 mg twice a day but so far I’m not sure it’s significantly better than .5 mg
#belgian malinois#2 years#service dog in training#positive reinforcement#cooperative care#vet appointment#vetblr#dogblr#service dogblr#aquapuncture#acupuncture#LDN#low dose naltrexone#canine rehabilitation#canine conditioning#injured dog#sick dog
22 notes
·
View notes
Text
I'm starting my LDN (low dose naltrexone) treatment today for fatigue! It has been used off-label for chronic pain patients, but new research is showing that it can reduce PEM in ME/CFS patients!
I'm excited and nervous to try it. I'll be checking in with you all and sharing my experience! Side effects will likely be immediate but it's not supposed to help much until about a month in.
#ldn#low dose naltrexone#mecfs#cfsme#myalgic encephalomyelitis#chronic fatigue syndrome#chronic pain
39 notes
·
View notes
Text
I was scared of immunosuppressants and anything to do with opioid receptors and like, ive been scare shitless of shower products for so long but. I finally caved and risked it for the biscuit with baby conditioner.
And I'm actually holding back tears I had NO reaction besides a little tingle (which was probably anxiety and foreign texture). My hair is soft, I smell nice, and I have 0 burning!!!!! I've not been able to use conditioner for well over a year and before that only sparingly for years, suffering burning so my hair wouldn't be as brittle.
I don't think of myself as very deprived because I'm used to my limitations but being able to use one step, in shower conditioner that smells nice is just. I'm actually crying now goat DAMN
#text#chronic illness#autoimmine disease#mast cell disease#mystery undiagnosed diseases#low dose naltrexone#methotrexate#im not cured or normal person better but i am so much better than where i was#i can smell good and its euphoric
7 notes
·
View notes
Text
Hi I'm okay and alive! Still not back to my normal, but doing "okay"
I just learnt last night about LDN for chronic issues (low dose naltrexone) has anyone tried this? I'm interested, always. Patient feedback more than anything else. I can read the studies. But I want to know people's actual experiences with this (if anyone has any!)
Money aside, I'm very wary of coming off my tramadol for 2 reasons to trial something like this. 1) it is the ONLY thing that gives me some semblance of normality (a very skewed version but it's good enough that I'm still around. And 2) I know for a FACT if I came off tramadol, LDN didn't work, getting someone to put me back on tramadol would be an ordeal I'm not sure I would be up to.
But anyway, yeah do lemme know!
#chronic illness#fibromyalgia#chronic pain#polyarteritis nodosa#adrenal insufficiency#stills disease#ldn#low dose naltrexone
11 notes
·
View notes
Text
Okay, I really would rather not have to ask random internet people for advice on something like this and I will call the pharmacy on Monday but I can't find any research whatsoever.
One of my doctor's prescribed me low dose naltrexone for ME/CFS and when I picked up my prescription, the pharmacist warned me that it could cause opioid withdrawal. He mentioned nothing about alcohol withdrawal but I know it's also used for alcohol dependence so I'm worried it'll cause that? Withdrawal is the last thing I need right now.
Does anyone have any experience/know someone who does or have any information? I'm not going to start this for a bit because I don't want to start two new meds at once but not knowing is making me anxious. And this is a specialist so I can't just ask him the question.
1 note
·
View note
Text

#low dose naltrexone#naltrexone#health medical pharma#big pharma#meds#medication#meme#system memes#system moodboard
5 notes
·
View notes
Text
the LDN sweats rly are something else 🫠
2 notes
·
View notes
Text

#manutenção#notebook#computador#celulares#formatação#troca de telas#seo#web design#Uberaba Minas Gerais#site#infodigit-pc#LDN#Low Dose Naltrexone#Uberaba-MinasGerais#Uberaba - Minas Gerais#uberaba - MG#Triângulo Mineiro#uberaba - mg
3 notes
·
View notes
Link
[From 2018]
Abstract: A patient with severe postural orthostatic tachycardia syndrome (POTS) and mast cell activation syndrome (MCAS) received immunotherapy with low-dose naltrexone (LDN) and intravenous immunoglobulin (IVIg) and antibiotic therapy for small intestinal bacterial overgrowth (SIBO). A dramatic and sustained response was documented. The utility of IVIg in autoimmune neuromuscular diseases has been published, but clinical experience with POTS is relatively unknown and has not been reported in MCAS. As a short-acting mu-opioid antagonist, LDN paradoxically increases endorphins which then bind to regulatory T cells which regulate T-lymphocyte and B-lymphocyte production and this reduces cytokine and antibody production. IVIg is emerging as a promising therapy for POTS. Diagnosis and treatment of SIBO in POTS is a new concept and appears to play an important role.
[To] complicate matters, 17 of 48 MCAS symptoms overlap with 33 POTS symptoms which is explained by comorbidity of the syndromes, where 30% of patients with POTS also have MCAS.5 Gastrointestinal (GI) symptoms are common in both syndromes.1–4 6 GI symptoms in MCAS can be explained by inappropriate release of mediators from mast cells (MCs) with KIT mutations whereas GI motility disorders in POTS may be due to active autoimmune muscarinic antibodies causing autonomic imbalance in some patients (S Vernino, personal communication, 2017). Physicians may erroneously attribute these frequent GI symptoms in undiagnosed MCAS and POTS patients to irritable bowel syndrome (IBS) and psychological disturbances as was the case in our patient.
Subsequently, IVIg 1.5 g/kg (Privigen) and 125 mg methylprednisolone were administered monthly. Naltrexone was continued at 1 mg every night. Six days after the first IVIg infusion, syncope, tinnitus, anal outlet disorder and vascular spasm ceased. Capillary refill time was >1 min before IVIg and reduced to <2 s. The next two infusions further improved body pain, weakness, vertigo, ability to eat and facial changes. Subsequent infusions maintained symptomatic improvement but the efficacy did not improve further (figure 2). The platelet counts normalised when measured after the sixth infusion.
After 10 IVIg treatments, a previously scheduled appointment at Mayo Clinic Scottsdale included autonomic testing which showed resolution of tachycardia with head-up tilt along with improvement in sudomotor function. At the time of submission of this report, the patient has had 20 IVIg treatments with a maximum of 5 weeks without one because the effects start to wear off. A trial of mycophenolate mofetil led to immune suppression. The next plan is to add new mast cell therapies in combination with IVIg and LDN.
Antibiotic therapy with rifaximin led to cessation of two decades of significant GI problems in our patient. Huang et al reported that 7/12 patients with POTS had dilated and/or air–fluid levels in the small intestine. We theorise that sustained sympathetic activity suppresses peristalsis, leading to stasis and development of SIBO in some patients with POTS. Alternative explanations for SIBO in POTS or MCAS who have concomitant EDS include presence of droopy small bowel loops or motor dysfunction due to protein deposition. We also theorise that eliminating SIBO can lessen MCAS and subsequent POTS by reducing intestinal permeability, thus reducing MC recruitment as well as T-cell activity and cytokines which activate MC.
In the present case, severe symptoms of MCAS preceded onset of POTS, thus, two driving forces are theorised to be important: mast cell activation adjacent to autonomic nerves and/or persistent recruitment and/or activation of MC due to bacterial overgrowth. It is less likely that an autoimmune neuropathic process is operative.
One common mechanism for high-dose IVIg to work in autoimmune disease is binding the Fc portion of autoantibodies. MC are most commonly known to have IgE receptors, but they also have IgG receptors. When these are activated by IgG, histamine is released. Theoretically, IVIg could overload these receptors and ultimately reduce MC mediator release. IVIg could also bind to histamine and block histamine activation of MC as seen in rats. An additional trigger for MC activation includes T-cell activity and release of microparticles and cytokines. IVIg increases regulatory T-cells which could reduce T-cell activity and thereby reduce MC activity. Finally, IgG has been found to downregulate IgE bound to MC and thus binding IgG by IVIg could play an additional role.
Beneficial effects of LDN on MCAS may include regulating overall T-lymphocyte production and decreasing cytokine mediators from T cells which directly cause MC activation, blocking Toll receptors which stimulate MC activity and reducing neuroinflammatory pain via microglia. Endorphins produced by LDN may improve intestinal dysmotility in POTS by directly increasing the migrating motor complex which prevents small intestinal stasis and subsequent bacterial overgrowth. We theorise that neuropathic POTS with an immune mechanism may also be improved by LDN via reduction of autoimmune antibody production by B-lymphocyte regulation.
Patient’s perspective
After decades of declining health, despite trying every conventional treatment with 100% compliance, I was pretty discouraged. I used to be such a high achiever and now I couldn’t even stand or sit up. I’d seen numerous top specialists and tried everything they recommended. I started seeing doctors for these complaints in 1997, and first received diagnoses of rosacea and restless leg syndrome.
In 2013, I realised Claritin helped, and that led me to figure out I may have POTS and MCAD. I referred myself to Mayo AZ, who confirmed it, and they started treatment with all the many drugs listed above. I was also diagnosed with ‘delayed pressure urticaria /angioedema’, DPU which is a mast cell problem where physical pressure leads to localised pain and swelling for days after. It’s a comically cruel problem to have along with POTS because one keeps you from being upright while the other keeps you from being able to lie down comfortably more than a few minutes … so you writhe on the ground mostly. But I’m grateful I have it because it’s the diagnosis that allowed me to receive IVIg!
I feel like I won the lottery last year by discovering LDN, IVIg and SIBO treatment. LDN made me feel noticeably happier, more energetic, in less pain and with better digestion (and these things got better with each dose increase). IVIg was an absolute miracle and within a week gave me a life back, with a huge improvement of numerous symptoms, most importantly fainting, nerve pain and delayed pressure angioedema. But I still had daily crippling stomach aches and more gas than a field of Holsteins until I took the rifaximin. I can’t believe I went decades feeling so bad when I only needed 2 weeks of antibiotics and a low-sulfur diet! Now I’m back to standing, eating, sleeping, working, living and feeling exceptionally lucky.
Learning points
Patients with postural orthostatic tachycardia syndrome (POTS) and mast cell activation syndrome (MCAS) have a wide array of symptoms and require an open mind to entertain the diagnoses.
POTS can imitate severe gastrointestinal motility disorders, irritable bowel syndrome (IBS), or frequent ‘IBS’ or small intestinal bacterial overgrowth (SIBO) relapses after antibiotic therapy.
Treatments for hyperadrenergic POTS have had limited in efficacy but treatment directed at MCAS can help.
Combined therapy with intravenous immunoglobulin and low-dose naltrexone led to significant improvement in a severely affected patient.
Antibiotic therapy for SIBO contributed to clinical improvement in the case presentation and others in our practice for both GI symptoms and POTS/MCAS symptoms.
2 notes
·
View notes
Text
Bad news: Today the pain is Worse
Good news: The Good Pharmacy got my prescription from Kaiser this morning and hand-delivered my first 15 pills to tide me over until they can mix up the rest.
#chronic pain#pain flare#fibromyalgia#low dose naltrexone#it fucking works miracles but I would not be able to take it if it weren't for Husband's willingness to engage with Kaiser's bs#he had to make so many phone calls and emails this week
4 notes
·
View notes
Text
The Low-Dose Naltrexone (LDN) Approach to Weight Loss: Unraveling the Potential
Introduction
The pursuit of a healthy weight and the desire for effective weight loss methods have been longstanding challenges for individuals across the globe. Weight management involves a complex interplay of factors, including diet, exercise, genetics, and lifestyle. Despite various strategies available, not all individuals find success with traditional approaches. This has led to a growing interest in alternative treatments and therapies, including the use of Low-Dose Naltrexone (LDN) for weight loss. LDN has gained attention for its potential benefits beyond its primary use in treating opioid addiction. This article explores the concept of LDN as a possible weight loss aid, examining its proposed mechanisms, evidence supporting its use, and potential risks and benefits.
What is Low-Dose Naltrexone (LDN)?
Naltrexone is an FDA-approved medication primarily used to treat opioid and alcohol addiction. At higher doses, it blocks opioid receptors in the brain, reducing the rewarding effects of opioid substances. However, at significantly lower doses than those used for addiction treatment, it may have a different impact on the body.
Low-Dose Naltrexone, as the name suggests, involves using naltrexone at much lower doses typically ranging from 1.5 to 4.5 mg daily. At these low doses, LDN acts differently, potentially modulating the immune system and influencing other bodily processes. It is important to note that LDN for weight loss is an off-label use, meaning it is not officially approved by regulatory authorities for this purpose.
Proposed Mechanisms of LDN in Weight Loss
The mechanisms underlying LDN's potential weight loss effects are still not fully understood, and further research is needed. Some theories propose that LDN may impact weight through the following ways:
1. Appetite Regulation: LDN may affect the brain's opioid receptors, which could influence appetite control. By modulating the brain's reward system, LDN might help reduce food cravings and overeating tendencies.
2. Metabolism Boost: LDN might stimulate the release of endorphins, which can enhance metabolism and energy expenditure. An increased metabolic rate can lead to more calories burned, aiding in weight loss.
3. Autoimmune Regulation: Some researchers suggest that LDN's immune-modulating properties may play a role in weight management. Obesity has been linked to chronic inflammation, and LDN could potentially reduce inflammation levels in the body.
Limited Clinical Evidence and Studies
Despite the intriguing potential mechanisms, it is crucial to emphasize that the clinical evidence supporting LDN as a weight loss treatment is scarce and preliminary. Most studies on LDN's impact on weight loss are small-scale and lack the rigor of larger, randomized, double-blind, and placebo-controlled trials. Many of the available studies have been conducted on animal models or involved patients with specific medical conditions, which limits their generalizability to the broader population seeking weight loss solutions.
A 2017 review published in the journal Current Obesity Reports analyzed the existing literature on LDN and weight loss. The review concluded that while there are some promising results in animal studies and a few small human trials, more extensive research is needed before drawing any firm conclusions about LDN's efficacy and safety for weight management in the general population.
LDN Weight Loss: Anecdotal Reports and Patient Experiences
Despite the limited scientific evidence, the internet and social media are filled with anecdotes and personal accounts of individuals claiming success with LDN for weight loss. These stories often involve individuals who have struggled with conventional weight loss methods, such as dieting and exercise, and found LDN to be a game-changer.
It is essential to interpret these anecdotes with caution. Anecdotes do not constitute scientific evidence and may be subject to bias or the placebo effect. Furthermore, individual responses to medications can vary significantly, and what works for one person may not work for another.
Risks and Considerations
Before considering LDN for weight loss, individuals should be aware of potential risks and consider the following:
1. Off-Label Use: Using LDN for weight loss is considered an off-label use, meaning it is not an officially approved treatment. Patients should discuss this approach with a knowledgeable healthcare provider who can provide guidance and monitor their progress.
2. Side Effects: While LDN is generally considered safe at low doses, it may still cause side effects in some individuals, such as nausea, headache, insomnia, or mood changes. Serious adverse effects are rare but can occur.
3. Drug Interactions: LDN may interact with other medications a person is taking, so it's crucial to inform healthcare providers of all current medications and medical conditions.
4. Individual Variation: The response to LDN varies from person to person. Some individuals may experience significant weight loss, while others may see minimal or no effect.
Conclusion
Low-Dose Naltrexone (LDN) has gained attention as a potential weight loss aid, but its use for this purpose remains largely unsupported by robust clinical evidence. While the proposed mechanisms sound promising, more extensive research is necessary to validate LDN's efficacy and safety in promoting weight loss.
Individuals interested in LDN for weight loss should consult with healthcare professionals to weigh the potential risks and benefits and to explore other evidence-based weight management strategies. As the science progresses, LDN might become a valuable tool in the fight against obesity, but for now, it should be approached with caution and considered alongside other established weight loss approaches.
0 notes
Text
LDN info for ME/CFS, chronic pain, autoimmune diseases, and more.
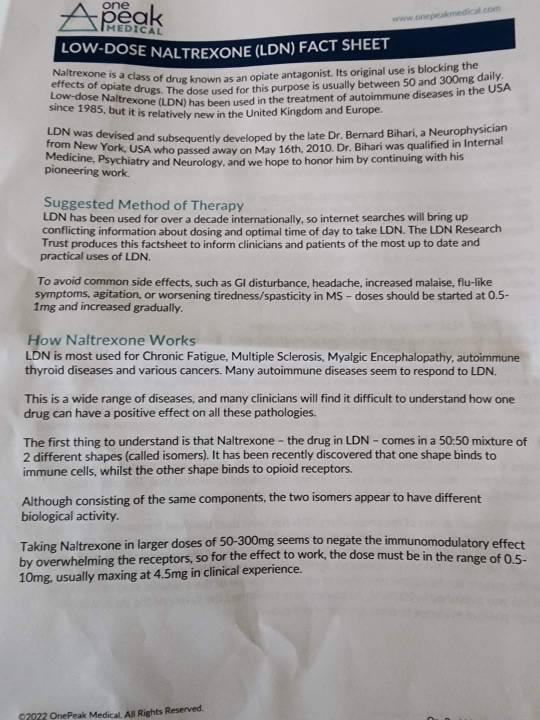
#ldn#low dose naltrexone#mecfs#cfsme#myalgic encephalomyelitis#chronic fatigue syndrome#chronic pain#chronic illness
7 notes
·
View notes
Text
Do any spoonies here have experience with low-dose naltrexone? My new doc (endometriosis specialist) seems to think it'd be perfect for me, but my pain doc isn't so keen on it.
1 note
·
View note
Text
Anyone taking low dose naltrexone know how to deal with the nausea side effect? It seems to be actually helping my pain but the nausea is unbearable
1 note
·
View note
Text
If exercise is so good for you, but one of the main reasons why people don't do it is because it makes you feel like mega garbage if you're out of shape, then instead of urging people to exercise I think we should put all that effort and money into designing a drug that makes exercise not suck. Something that either gets rid of that awful out of breath feeling and pain or makes them less terrible. With this I predict we could improve the health of a large percentage of the population. The slogan should be "makes exercise not make you want to kill yourself! :)" or something to that effect
#i was just thinking about like. the no such thing as lazy philosophy#which i agree with#and i was like well the fact that exercise is good for you is unargued. so if people aren't doing it there's gotta be some OTHER barrier#so people won't exercise unless that other barrier is removed. telling them over and over they should exercise will do nothing#and i have chronic fatigue syndrome so for a long time exercise actually made me so physically miserable#that the thought of exertion made me cry#low dose naltrexone and antihistamines made my post exertional malaise go away largely#so i was like. what if we could do that for people without cfs. cause i know EVERYONE hates exercising when out of shape
6 notes
·
View notes