#interpersonal therapy for bipolar disorder
Text
ADHD Informative Post Pt. 2
Causes
As stated in the first part (on @fqiryinfo Instagram), a heavily theorized cause of ADHD is a lack of dopamine to the pre-frontal cortex. Genetics obviously play a major role in that, however scientists are also researching the possibility of brain injuries, exposure to environmental risks (like lead) during pregnancy or early childhood, alcohol or tobacco use during pregnancy, premature delivery, and low birth weight as possible risk factors. Having these risk factors does not necessarily equal having ADHD. Another neurotransmitter besides dopamine that may contribute to ADHD symptoms is norepinephrine. Certain parts of the brain have been noted to be decreased in volume, as well as low iron and zinc levels causing a higher risk for ADHD symptoms and even a higher severity of symptoms. Despite common misconceptions, ADHD has *no* connection with sugar currently noted and has nothing to do with parental styles.
Treatment - Medication
Medicated treatment is typically broken down into three groups. These are long-lasting stimulants (like Adderall XR, Vyvanse, Biphentin, and Concerta), long-lasting non-stimulants (like Strattera), and short/immediate-acting stimulants (like Dexedrine, Dexedrine Spansule, Ritalin, and Ritalin SR). XR stands for extended release while SR stands for sustained release. This is not necessarily a medication, but iron supplements have been noted to help allivieate ADHD symptoms which makes sense with the noted iron deficiency being a risk. However, zinc supplements didn't have as much of a positive effect.
Treatment - Non-Medication
Psychoeducation: strategy instruction (sleep management, anger contron, etc.), self-talk development, organizational skills developments, information on ADHD, community resources, and support groups
Behavioral Intervention: rewards and consequences, environmental management, ADHD coaching, and lifestyle changes
Social Intervention: social skills training and parenting skills training
Psychotherapy: self-talk strategies, cognitive behavioral therapy (CBT), interpersonal therapy, family therapy, expressive arts therapy, and supportive counseling
Educational/Vocational Accomodations: academic remidation and specialized academic/workplace interventions
Comorbidities
"More often than not, ADHD is further complicated by comorbidity with one or more psychiatric disorders.... An adult with ADHD is six times more likely to have at least one other psychiatric disorder than an adult without ADHD." (Thomas E. Brown, PH.D.). A quote from a book to all those who would like to argue against those who believe comorbidities don't exist. Even a study found 70% of 579 children carefully diagnosed with ADHD fully met the diagnostic criteria for one or more psychiatric disorders. Cases of ADHD not complicated by another disorder are rare.
As for the disorders ADHD is often comorbid with, that would be learning disorders, anxiety disorders, mood disorders (especially Bipolar Disorder), OCD, ODD, conduct disorder, substance use disorders, and personality disorders. Bipolar disorder especially, but but mood disorders in general stem from similar neurobiology so it makes for them to be so comorbid. (Bipolar 1 is even more comorbid than Bipolar 2.) Personality disorders are reported to be present in more than 50% of adults with ADHD. Of that 50%, the most common are cluster B and C disorders with 25% of them having two or more personality disorders. Of the papers I've read, none of them mention Autism as an actual comorbidity of ADHD however that's probably because it falls under the other disorders of early childhood they frequently mentioned.
Our Own Experiences
We are professionally diagnosed with ADHD. We have genetic links on both sides of our family, as well as a lack of iron (not diagnosed with iron deficiency but we do experience symptoms at times). We were diagnosed at 13 with the inattentive type. Originally we tried Strattera as a medication, but it didn't work so we switched to another medicine and it's been working ever since (heavy dissociation messes with the effectiveness though). We have recently decided to ask to start taking iron supplements to help with symptoms. As for comorbidities, we have a comorbid mood disorder (depression however the disorder type was never specified), generalized anxiety disorder, and social anxiety disorder diagnosed. We also experiences symptoms of BPD, but it's not been talked about with the mental health group we talk to so we avoid saying for sure we have it despite the genetic and trauma links. Obviously this is just in regards to this post, but yeah!
17 notes
·
View notes
Text
Understanding Depression: Causes, Symptoms, and Treatment
Depression is a complex mental health condition that affects millions of lives worldwide. It's more than just feeling sad; it's a medical condition that requires understanding and effective treatment. In this comprehensive exploration of depression, we'll not only delve into its causes, symptoms, and treatment options but also introduce you to a beacon of hope in this journey: Calida Rehab.
Calida Rehab is a renowned rehabilitation center nestled in the serene surroundings of Karjat, near Mumbai. With a dedication to helping individuals overcome depression and regain control of their lives, Calida Rehab plays a pivotal role in the treatment. As we navigate the intricacies of depression, we'll also shed light on how centers like Calida Rehab provide personalized care and support for those in need.
Now, let's embark on a journey to better understand depression and discover the paths to healing and recovery.
I. What is Depression?
Depression is a common mental health disorder characterized by persistent feelings of sadness, hopelessness, and a loss of interest or pleasure in daily activities. It's not merely a passing mood but a medical condition that can have a profound impact on a person's life. Depression is a global issue, affecting people of all ages and backgrounds. Its repercussions extend beyond the individual, impacting relationships, work, and society as a whole.
II. Causes of Depression
Depression doesn't have a single cause; it's typically the result of a complex interplay between biological, psychological, and environmental factors. Genetics and brain chemistry can make some individuals more susceptible to depression. Additionally, life events such as trauma, chronic stress, or a family history of depression can contribute to its development. Understanding these factors is crucial in unraveling the mysteries of depression.
III. Symptoms of Depression
Depression manifests in a variety of ways, affecting not only emotions but also cognitive, physical, and behavioral aspects of life. Common emotional symptoms include a pervasive sense of sadness and hopelessness. Cognitive symptoms may involve negative thinking patterns and difficulty concentrating. Physical symptoms can encompass changes in appetite and sleep patterns, while behavioral symptoms often include social withdrawal and a loss of interest in previously enjoyed activities.
IV. Types of Depression
Depression is not a one-size-fits-all condition. There are various types, each with its unique characteristics. Major depressive disorder is the most well-known, characterized by severe and persistent symptoms. Persistent depressive disorder involves milder but more chronic symptoms. Bipolar disorder, on the other hand, includes periods of both depression and mania. Understanding these distinctions is crucial for accurate diagnosis and treatment.
V. Diagnosis and Assessment
Recognizing depression's symptoms is the first step towards seeking help. Healthcare professionals use established criteria and assessments to diagnose depression accurately. These assessments may include clinical interviews, questionnaires, and self-assessment tools. Seeking professional help is vital, as self-diagnosis can be inaccurate and delay appropriate treatment.
VI. Treatment Approaches
Depression is treatable, and numerous effective treatments are available. Psychotherapy, such as cognitive-behavioral therapy and interpersonal therapy, can help individuals learn coping strategies and address underlying issues. Medications, including antidepressants, can be prescribed when necessary. Lifestyle changes, such as regular exercise, a balanced diet, and adequate sleep, play a vital role in recovery. Individualized treatment plans are key, as what works for one person may not work for another.
VII. Self-Help Strategies
Individuals dealing with depression can actively participate in their recovery. Building a support network, practicing stress management techniques, and adopting healthy coping mechanisms can make a significant difference in the journey towards healing.
VIII. Seeking Help
Seeking professional help is a courageous and crucial step in overcoming depression. However, stigma can often discourage individuals from seeking treatment. It's essential to understand that seeking help is a sign of strength, not weakness. There is no shame in reaching out to mental health professionals who can provide guidance, support, and effective treatment options.
IX. Recovery and Management
Recovery from depression is possible. It's essential to recognize that recovery is a process, and individuals may experience ups and downs along the way. Ongoing management, including therapy, medication, and lifestyle adjustments, can help maintain mental health. Setting realistic goals and seeking support from loved ones can contribute to a fulfilling life beyond depression.
Conclusion
Understanding depression is the first step towards effective treatment and recovery. It's crucial to recognize that depression is a treatable condition, and there is hope for a brighter future. If you or someone you know is experiencing depression, don't hesitate to seek help. Together, we can dispel the stigma surrounding mental health and support each other on the path to healing. Depression treatment near Mumbai , Karjat, and Pune, at rehabilitation centers like Calida Rehab, can provide the guidance and support needed to overcome this challenging condition.
#rehabilitation center near mumbai#rehabilitation center in pune#rehabilitation center in karjat#depression treatment in pune#depression treatment in karjat#depression treatment near mumbai#rehab center in pune#rehab center in mumbai#rehab center in karjat
2 notes
·
View notes
Text
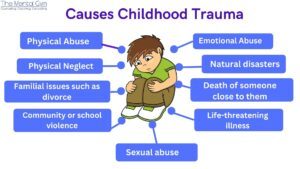
Healing Childhood Trauma
Many people face unfortunate, scarring events in their childhood. Most often, the consequences of these can lead to prolonged childhood trauma, which people are left to deal with during their adulthood. If left unaddressed, childhood trauma can have long-term ill effects on the quality of someone's life.
What is Childhood Trauma?
Childhood trauma can be explained as an emotionally painful or distressing event resulting in physical, mental, and emotional consequences. The traumatic experience can range from losing a parent suddenly to physical abuse or a natural disaster. It can even be something as seemingly innocuous as overhearing a conversation with triggering content.
Learning to understand and cope with difficulties, trauma, and tragedies is a natural part of growing up. But in more serious cases, a lack of exposure to proper mental healthcare can result in childhood trauma in adults.
Effects of Childhood Trauma on the Psyche
Childhood trauma can affect neurological development, hormonal regulation, and cognitive and emotional competencies. It also increases impulsive and risky behaviour, such as substance abuse. This claim is substantiated by a 2021 study by Auckland Univerisity on the themes of child abuse and neglect.
What can Cause Childhood Trauma?
Neglect
Familial issues such as divorce
Death of someone close to them
Psychological, physical, emotional, and sexual abuse
Natural disasters
Substance abuse
Community or school violence
Life-threatening illness
Trauma Signs in Children
In preschool and elementary age, childhood trauma symptoms include separation anxiety, difficulty sleeping, frequent nightmares, feelings of anxiety, crying for no reason, decreased appetite, moodiness, and increased aggression.
In teens, the signs of childhood trauma are irritability, academic problems, sudden withdrawal from social activities, self-blame, difficulty concentrating, feelings of depression, and increased behaviors like sexual activity and alcohol and substance abuse.
What Happens if Trauma Remains Unresolved?
Effects of childhood trauma and early childhood trauma are distorted self-perception, feelings of shame and guilt, chronic physical pain, and anxiety.
Repressed childhood trauma can also cause depression, panic attacks, fatigue, impulsiveness, insomnia, self-harm, eating disorders, and suicidal ideation. Childhood trauma in adults also increases the risk of mental health disorders. Depressive, anxiety, obsessive-compulsive bipolar, and substance use are some disorders caused by childhood trauma.
Adults with childhood trauma are more common than you imagine. ‘Childhood trauma therapist near me' is among the more common internet searches. In 2020, the World Health Organization estimated that globally, around 1 billion children aged between 2–17 years have experienced physical, sexual, or emotional violence or neglect.
Therapy for childhood trauma is needed to prevent problems in adulthood.
Effect of Childhood Trauma on Health
There are several childhood trauma signs in adults. Toxic stressors in childhood can take a lifelong toll and can manifest in adulthood. So, when adults show signs of trauma, it can be a result of the trauma they experienced in childhood.
Studies have found that the chances of getting a heart disease increased in adults who had experienced abuse, witnessed interpersonal violence, or lived in a household where there was substance abuse. The odds of asthma and diabetes also rose for adults who experienced childhood trauma, such as mental illness, substance abuse, and divorce.
The study found that those who experienced even one type of childhood trauma, such as a family member in jail, were associated with an increased risk of poor mental health. Since types of childhood trauma often involve a trusted loved one, a caregiver, or even a family member, in adulthood, this can lead to trust issues and deeply rooted feelings of insecurity.
Here are some of the signs of childhood trauma that adults might exhibit:
Adults who experience childhood trauma are more prone to depression, mood disorders, and suicidal thoughts.
They are also likely to engage in substance abuse.
Adults affected by childhood trauma may exhibit unexplained and irrational anger or irritability.
Adults with childhood trauma could find maintaining old or establishing new, healthy relationships challenging.
How to Heal Childhood Trauma
Several forms of therapy can help heal childhood trauma, some of which are:
Cognitive processing therapy (CPT): CPT aims to help a person change how they think about the event(s) that led to the trauma, thereby relieving the adverse effects.
Prolonged exposure therapy (PE): This involves confronting the source of fear to reduce anxiety and support healing from childhood trauma.
Cognitive behavioural therapy (CBT): Therapists use CBT to help people identify and correct unhealthy behaviour patterns and develop new ways to cope in case of mental illness caused by childhood trauma.
Hypnotherapy: This is a popular alternative childhood trauma therapy for adults, especially those who have struggled with other therapy types. Here, the therapist works to help reduce the emotion attached to the event by working with the subconscious mind.
While there are several coping mechanisms to deal with childhood trauma, the key is to try different methods and find one that works for you. Since healing is a long process, the sooner you identify the method that suits you best, the better.
Summing up
Recovering from childhood trauma is a long and gradual process. Along the healing journey, chances are that you will experience helplessness and isolation. However, the first step in healing from childhood trauma is to acknowledge the trauma. Do not try to push your feelings under the carpet or minimize them. Acknowledge your emotions, and you are ready for the next step to reclaiming control - seeking support.
4 notes
·
View notes
Text
Dr. Gorav Gupta: Best psychiatrist from Gurgaon
Dr. Gorav Gupta, a highly esteemed psychiatrist practicing at Tulasi Healthcare in Gurgaon, has gained widespread recognition for his exceptional expertise in providing comprehensive mental health care. With a profound understanding of the intricacies of the human mind and a deep commitment to patient well-being, Dr. Gupta has emerged as a beacon of hope for individuals struggling with various mental health challenges.
His approach to psychiatry is holistic, encompassing both biological and psychological aspects. Dr. Gupta believes in treating the whole person, not just the symptoms, by exploring the underlying causes of mental distress and developing tailored treatment plans that address both the mind and the body. His compassionate and empathetic nature fosters a therapeutic environment where patients feel safe and understood, enabling them to embark on their journey toward recovery.
Best psyhciatrist, Dr. Gorav Gupta. Dr. Gupta's expertise extends across a broad spectrum of mental health conditions, including anxiety disorders, depression, bipolar disorder, schizophrenia, and substance use disorders. He utilizes evidence-based therapies such as cognitive behavioral therapy (CBT), interpersonal therapy (IPT), and psychodynamic psychotherapy to help patients develop coping mechanisms, improve their relationships, and regain a sense of well-being. Additionally, he is proficient in medication management, ensuring that patients receive the optimal pharmacological support to alleviate their symptoms.
Dr. Gupta's commitment to excellence is evident in his continuous professional development and research endeavors. He regularly attends conferences and workshops to stay abreast of the latest advancements in psychiatry and incorporates innovative techniques into his practice. His dedication to patient care has earned him the respect of both his colleagues and patients, who consistently praise his exceptional skills, compassionate demeanor, and unwavering support throughout their recovery journey.
0 notes
Text
Psychiatric disorders encompass a wide range of conditions affecting mood, behavior, and cognition. Some common ones include depression, anxiety disorders (like generalized anxiety disorder, panic disorder, and social anxiety disorder), bipolar disorder, schizophrenia, obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), attention-deficit/hyperactivity disorder (ADHD), and eating disorders (such as anorexia nervosa and bulimia nervosa).
There are many others, each with its own set of symptoms and treatment approaches.
Psychiatric disorders are typically diagnosed through a combination of clinical evaluation, psychological assessments, and sometimes laboratory tests to rule out medical conditions.
Diagnosis involves assessing symptoms, duration, and impact on daily functioning.
Treatment approaches vary depending on the specific disorder and individual needs but may include:
Psychotherapy: Talk therapy, such as cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), or interpersonal therapy (IPT), to address thought patterns, behaviors, and emotions.
Medication: Psychiatric medications, including antidepressants, antipsychotics, mood stabilizers, anxiolytics, and stimulants, prescribed based on symptoms and diagnosis.
Lifestyle changes: Including stress management techniques, regular exercise, healthy diet, and adequate sleep, which can support overall mental well-being.
Support groups: Peer support groups or group therapy sessions can provide a sense of community and understanding.
Hospitalization: In severe cases or during crises, hospitalization may be necessary for stabilization and safety.
Other interventions: Such as electroconvulsive therapy (ECT), transcranial magnetic stimulation (TMS), or complementary therapies like acupuncture or yoga, may be considered in specific cases.
Treatment plans are often individualized and may involve a combination of these approaches. Regular monitoring and adjustments to the treatment plan are important to ensure effectiveness and address any changes in symptoms or circumstances.
Get the best treatment for mental disorders at best hospitals like Jaslok Hospital Mumbai.
#health#mental health#surgery#full body health checkup#psychiatric#psychotherapy#psychology#yoga#medications#anxiety#depression#mood swings
0 notes
Text
Music and the Brain
Music is an outstanding medium that allows for the exploration of human culture, language, emotion, and behavior. Obviously, music is able to evoke intense emotional responses of varying degrees— happy, upbeat music makes individuals want to dance and have fun, sad, depressing, slow music may make individuals wants to cry or change their mood to be less positive, etc. This all depends on what resonates with different individuals and their life experiences, and it is fascinating to think about music as a universal language that all can relate to emotionally in some way, regardless of where they are from. instruments alone can evoke strong feelings within the human mind, which in retrospect, is a glorious facet of humanity to consider. What many do not think about though, is how music can also relate to brain mechanisms and activation of certain electrochemical brain activity.
Through the examination of music's effect on the human brain it is visible that music activates different cerebral circuits and can alter the brain's development from a young age, as the brain has a component of neuroplasticity. Researchers have studied the ways in which music impacts different parts of the brain and our cognition from childhood to old age. Neuroplasticity is an important concept in understanding how music has an impact on the brain as it develops over the course of one's life. The term “neuroplasticity” refers to the way in which the brain can create new pathways and almost “reorganize itself”, when experiencing new content and learning it/retaining it in our memories. Music has potential to change the shape and connectivity of brain structures due to the it's neuroplastic capabilities, which is why it is paramount to use it in clinical treatment of neuropsychiatric disorders.

There are visible biological differences in humans (which have evolved to process music) compared to primates, including larger temporal lobes in the dorsal areas of the brain related to auditory reception/processing and speech. There is also increased size in the human's cerebellum and prefrontal and premotor cortices (linked to the basal ganglia), which play a role in rhythmic processing and the ability to pick apart pieces of music to process it more intensely compared to other organisms. Auditory cortices have evolved and expanded to permit the detailed processing of music, which have allowed humans to benefit from it in multiple settings.
Music therapy has gained popularity in the treatment of psychiatric and neuropsychiatric disorders including depression, anxiety, mood disorders like bipolar, Parkinson's, Huntington's, Alzheimer's, etc. Not only can music significantly improve mood and emotion of these patients, but it also helps to stimulate brain activity and cognitive functioning. Because of the role music plays in relation to motor function with counting beat sand rhythms, it has been used to recover motor function in patients with these neurodegenerative disorders impacting their motor cortices. It has also been shown to help stroke patients and those with epileptic seizures, with the ability to regulate electroencephalographic abnormalities.

A study from Raglio et. Al. (2015) used fMRI scans on patients undergoing music therapy on the “normal brain” to examine how music can influence brain activity in those without neuropsychiatric dysfunction. A significant finding was activation in the precuneus, a region of the brain related to visuo-spatial activity, episodic memory retrieval, self-processing, interpersonal relationships and other cognitive functioning. The Medial Prefrontal Cortex was also activated during fMRI evaluation when participants engaged with certain genres of music, which was able to show the effect listening to music has on attention, working memory, or long-term memory. Undoubtedly, music therapy can be beneficial to developing brain activity; notably important as participants in the mentioned study did not have any cognitive impairment, yet music therapy was still able to have an impact on the activity of different regions in their brains.
Altogether, music is not only a beautiful artform and universal language for members of different cultures to communicate with each other, but it also acts as an outlet for healing and treatment for those with neurological and psychological dysfunction. The human brain is a fascinating organ to study, and when pairing it with music, a manmade art that is able to so deeply have an impact on our development, it allows for extreme growth and behavioral benefits for those who choose to listen.
Sources:
I include here one of my favorite songs of all time that has absolutely improve my mental well-being, that I can use as an outlet to feel relaxed, focus on work when I need to lock in and study, resonate with when I feel sad, and also to make me happy. It is really a universal song for me, and I just thought it would be fun to include a little bit of a personal example to how this information relates to me and has been able to help me overcome a lot mentally! :)
Very good song! - Tyler
youtube
1 note
·
View note
Text
Mental Health Therapy In Durgapur
Mental health therapy in Durgapur, also known as psychotherapy or counseling, encompasses various approaches aimed at improving an individual's emotional well-being, cognitive functioning, and overall mental health. Here are some common types of mental health therapy:
Cognitive-Behavioral Therapy (CBT): CBT is one of the most widely used forms of therapy. It focuses on identifying and challenging negative thought patterns and behaviors that contribute to mental health issues such as depression, anxiety, and trauma. The goal is to replace these patterns with healthier ones, leading to improved coping skills and emotional regulation.
Psychodynamic Therapy: Psychodynamic therapy explores how past experiences, especially those from childhood, influence current thoughts, feelings, and behaviors. It aims to uncover unconscious patterns and conflicts, fostering insight and understanding to promote healing and personal growth.
Humanistic Therapy: Humanistic therapies, such as person-centered therapy and Gestalt therapy, emphasize empathy, acceptance, and personal growth. They focus on self-exploration, self-awareness, and the client's inherent capacity for growth and self-actualization.
Mindfulness-Based Therapies: Mindfulness-based approaches, including Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT), incorporate mindfulness practices to help individuals cultivate present-moment awareness, reduce stress, and manage difficult emotions.
Family Therapy: Family therapy involves working with families or couples to improve communication, resolve conflicts, and address relational dynamics. It recognizes the interconnectedness of family members and aims to foster healthier relationships and support systems.
Interpersonal Therapy (IPT): IPT focuses on improving interpersonal relationships and addressing specific interpersonal issues that contribute to mental health problems, such as grief, role transitions, interpersonal conflicts, and social isolation.
Trauma-Focused Therapy: Trauma-focused therapies, such as Eye Movement Desensitization and Reprocessing (EMDR) and Trauma-Focused Cognitive Behavioral Therapy (TF-CBT), are designed to help individuals process and heal from traumatic experiences by addressing symptoms related to post-traumatic stress disorder (PTSD) and related conditions.
Group Therapy: Group therapy involves sessions led by a therapist and attended by multiple individuals who share similar concerns or goals. It provides opportunities for mutual support, validation, and interpersonal learning in a supportive group setting.
It's essential to find a therapy approach and therapist that align with your needs, preferences, and goals. Therapy can be conducted in individual, group, or family/couples settings and may vary in duration and frequency depending on the specific issues being addressed. Additionally, therapy can be complemented by medication management when appropriate, especially for conditions like depression, anxiety, and bipolar disorder. Always consult with a qualified mental health professional to determine the most suitable treatment approach for your individual needs.
0 notes
Text
What does a clinical psychologist do?
Clinical psychologists are mental health professionals who specialize in assessing, diagnosing, and treating various psychological and emotional disorders and issues. They work with individuals, couples, families, and groups to help them understand and overcome psychological difficulties, improve their mental well-being, and enhance their quality of life. Here are some of the key roles and responsibilities of clinical psychologists:
Assessment and Diagnosis: Clinical psychologists conduct comprehensive assessments to evaluate clients' psychological functioning, including their thoughts, emotions, behaviors, and relationships. They use standardized psychological tests, interviews, and observation to gather information and make accurate diagnoses of mental health conditions such as depression, anxiety disorders, bipolar disorder, post-traumatic stress disorder (PTSD), and schizophrenia, among others.
Psychotherapy/Counseling: One of the primary roles of clinical psychologists is to provide psychotherapy or counseling to clients. They utilize evidence-based therapeutic approaches, such as cognitive-behavioral therapy (CBT), psychodynamic therapy, interpersonal therapy, and mindfulness-based interventions, to help clients address their psychological issues, develop coping skills, change maladaptive behaviors, and achieve their therapeutic goals.
Treatment Planning and Implementation: Clinical psychologists collaborate with clients to develop individualized treatment plans based on their specific needs, preferences, and strengths. They implement therapeutic interventions and strategies to facilitate emotional healing, promote personal growth, and foster positive changes in clients' lives. This may involve providing ongoing therapy sessions, facilitating support groups, or coordinating care with other mental health professionals.
Crisis Intervention: In emergency situations or during times of crisis, clinical psychologists provide immediate psychological support and intervention to individuals experiencing acute distress, trauma, or suicidal ideation. They assess risk factors, develop safety plans, and offer crisis counseling to help clients stabilize their emotional state and access appropriate resources for further assistance.
Consultation and Collaboration: Clinical psychologists often collaborate with other healthcare professionals, including psychiatrists, physicians, social workers, and counselors, to provide comprehensive care for clients. They may consult with colleagues to discuss treatment approaches, share clinical insights, or provide expert opinions on complex cases. Additionally, they may collaborate with community organizations, schools, and agencies to promote mental health awareness and advocate for the needs of their clients.
Research and Evaluation: Many clinical psychologists are actively involved in research endeavors aimed at advancing the understanding of psychological disorders, treatment efficacy, and therapeutic interventions. They may conduct research studies, publish scholarly articles, or participate in academic conferences to contribute to the field of psychology and inform evidence-based practice.
Overall, clinical psychologists play a vital role in addressing the diverse mental health needs of individuals across the lifespan. Through their expertise, empathy, and commitment to promoting psychological well-being, they help clients navigate life's challenges, overcome obstacles, and lead more fulfilling and meaningful lives.
0 notes
Text
When to See a Specialist for Bipolar Disorder?

Bipolar disorder, also known as manic-depressive disorder, is a mental health condition characterized by extreme mood swings ranging from high energy and euphoria to low energy and depression. It affects millions of people worldwide and can have a significant impact on one's daily life and relationships.
While bipolar disorder can be managed with medication and therapy, it is essential to know when to seek help from a specialist, such as a psychiatrist in Indore. Here are some signs that indicate it may be time to see a specialist for bipolar disorder.
1) Difficulty managing symptoms: If you find that your bipolar symptoms are becoming increasingly challenging to manage, it may be time to see a specialist. This could include experiencing more frequent and intense mood swings, difficulty functioning in daily life, or a decline in overall well-being.
2) Medication is not working: Bipolar disorder is typically treated with a combination of medication and therapy. However, if you have been on medication for a while and are not seeing any improvement in your symptoms, it may be time to consult a specialist. They can assess your current treatment plan and make necessary adjustments to help manage your symptoms better.
3) Co-occurring disorders: Many individuals with bipolar disorder also experience other mental health conditions, such as anxiety or substance abuse. These co-occurring disorders can complicate treatment and require specialized care. A specialist can help address these issues and provide a comprehensive treatment plan.
4) Family history of bipolar disorder: If you have a family history of bipolar disorder, you may be at a higher risk of developing the condition. In such cases, it is advisable to see a specialist for regular check-ups and to monitor any potential symptoms.
5) Changes in behavior: Bipolar disorder can cause significant changes in behavior, such as impulsivity, irritability, and risky behaviors. If you or your loved ones notice any sudden and drastic changes in your behavior, it is crucial to seek help from a specialist.
6) Difficulty maintaining relationships: Bipolar disorder can have a significant impact on relationships, leading to conflicts and strained connections. If you find that your relationships are suffering due to your symptoms, it is essential to seek help from a specialist to improve your interpersonal skills and manage your condition better.
1 note
·
View note
Text
Navigating Depression: Signs, Causes, and Treatment
Depression is a common and serious mental health condition that can significantly impact a person's quality of life, relationships, and overall well-being. As the best psychiatrist in Jaipur, I recognize the importance of raising awareness about depression and providing information on its signs, causes, and effective treatment options. In this guide, we will explore the complexities of depression and offer guidance for navigating its challenges.
Defining Depression: Depression, also known as major depressive disorder (MDD), is a mood disorder characterized by persistent feelings of sadness, hopelessness, and loss of interest or pleasure in activities once enjoyed. It is more than just feeling sad; it is a pervasive and debilitating condition that affects every aspect of life.
Common Signs and Symptoms: Symptoms of depression can vary from person to person but may include persistent sadness, irritability, fatigue, changes in appetite or weight, sleep disturbances, feelings of guilt or worthlessness, difficulty concentrating, and thoughts of death or suicide.
Types of Depression: Depression can manifest in different forms, including major depressive disorder (MDD), persistent depressive disorder (dysthymia), seasonal affective disorder (SAD), postpartum depression, and bipolar disorder (depressive phase). Each type has its own unique features and treatment considerations.

Risk Factors and Causes: Depression can arise from a combination of genetic, biological, environmental, and psychological factors. Common risk factors include a family history of depression, traumatic life events, chronic stress, substance abuse, medical conditions, and certain medications.
Biological Factors: Imbalances in neurotransmitters such as serotonin, norepinephrine, and dopamine are believed to play a role in depression. Changes in brain structure and function, hormonal fluctuations, and genetic predispositions may also contribute to the development of depression.
Psychological Factors: Negative thinking patterns, low self-esteem, unresolved trauma, and maladaptive coping strategies can exacerbate depressive symptoms and contribute to the maintenance of the disorder. Addressing these psychological factors is essential for effective treatment.
Environmental Factors: Stressful life events, such as loss of a loved one, relationship conflicts, financial difficulties, job loss, or significant life changes, can trigger or exacerbate depression in susceptible individuals. Creating a supportive and nurturing environment is crucial for recovery.
Impact on Daily Functioning: Depression can significantly impair daily functioning, affecting relationships, work or school performance, self-care, and overall quality of life. It may also increase the risk of other health problems, including substance abuse, anxiety disorders, and physical health conditions.
Treatment Approaches: Effective treatment for depression typically involves a combination of psychotherapy, medication, lifestyle modifications, and support from loved ones. Treatment should be individualized based on the severity of symptoms, underlying causes, and personal preferences.
Psychotherapy (Counseling): Cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), and psychodynamic therapy are among the most commonly used psychotherapeutic approaches for depression. These therapies help individuals identify and challenge negative thought patterns, develop coping skills, and improve interpersonal relationships.
Medication: Antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and atypical antidepressants, may be prescribed to alleviate depressive symptoms and rebalance neurotransmitter levels.
Self-Care and Lifestyle Modifications: Engaging in self-care activities, such as regular exercise, healthy eating, adequate sleep, stress management techniques (e.g., mindfulness, relaxation exercises), and social support, can complement professional treatment and promote overall well-being.
Depression is a complex and multifaceted condition that requires comprehensive treatment and support. By understanding the signs, causes, and effective treatment approaches for depression, individuals can take proactive steps toward recovery and regain control of their lives. As the best psychiatrist in Jaipur, I am committed to providing compassionate care and evidence-based interventions to support individuals struggling with depression. Remember, you are not alone, and there is hope and help available for navigating the challenges of depression. With the right support and treatment, recovery is possible, and a brighter future awaits.
0 notes
Text
Bipolar Disorder, its symptoms, and its disorders
Bipolar disorder, a mental illness characterized by extreme mood swings from manic highs to depressive lows, affects millions worldwide. Recognizing its symptoms and seeking appropriate treatment are crucial steps toward managing this condition effectively.
Symptoms of Bipolar Disorder:One of the hallmark symptoms of bipolar disorder is mood swings, ranging from elevated moods during manic episodes to feelings of hopelessness and despair during depressive episodes. These mood fluctuations can significantly impact daily functioning and quality of life. Individuals with bipolar disorder may also experience other symptoms such as changes in energy levels, sleep disturbances, irritability, and impaired judgment.
Treatment for Bipolar Discorder:Treatment for bipolar disorder typically involves a combination of medication, psychotherapy, and lifestyle changes. Mood stabilizers, antipsychotic medications, and antidepressants may be prescribed to help manage symptoms and stabilize mood. Psychotherapy, including cognitive-behavioral therapy (CBT) and interpersonal therapy, can help individuals develop coping strategies, improve communication skills, and regulate emotions.
In addition to traditional therapeutic approaches, complementary therapies such as art therapy, music therapy, and mindfulness-based practices may also be beneficial in managing bipolar disorder symptoms. These creative modalities provide individuals with alternative outlets for expression, promote relaxation, and enhance overall well-being.
At Calida Rehab, located in Pune, Mumbai, and Karjat, we understand the complexity of bipolar disorder and offer comprehensive support to individuals struggling with this condition. Our rehabilitation centers provide specialized care for bipolar disorder, focusing on holistic treatment approaches that address both the manic and depressive phases of the illness.
Our facilities are equipped to address co-occurring conditions often associated with bipolar disorder, such as anxiety disorders, obsessive-compulsive disorder (OCD), and alcohol or substance abuse. Our multidisciplinary team collaborates to develop comprehensive treatment plans that address the complex needs of each individual.
Calida Rehab is committed to providing compassionate care and support to individuals living with bipolar disorder. Our top-tier rehabilitation centers in Pune, Mumbai, and Karjat offer a safe and nurturing environment where individuals can journey towards recovery and stability. If you or a loved one is struggling with bipolar disorder, don't hesitate to reach out to us. We're here to help you reclaim control of your life and achieve lasting wellness.
0 notes
Text
What are the differences between npd and bpd.

It can be challenging to identify whether personality disorder is dominant in a relationship because the symptoms of borderline personality disorder (BPD) and narcissistic personality disorder (NPD) sometimes overlap.
You can decide how to alter the dynamics in your relationship by being aware of the distinctions between relationships with BPD and NPD.
An outline of NPD, or narcissistic personality disorder:
An exaggerated feeling of one's own significance, an incessant desire for approval, and a lack of empathy for others are traits associated with NPD. People suffering with non-verbal personality disorder (NPD) frequently feel better than other people and need a lot of praise and attention to feel good about themselves.
They could struggle to see or understand the needs and feelings of others, and they might use people to further their own goals.
What are the Key Features of NPD?
Self-importance and a sense of entitlement
A need for validation and approval
Lack of empathy
Participating in exploitative behaviour in partnerships
Easily broken and susceptible to reproach
Understanding the symptoms of Borderline Personality Disorder (BPD): Bipolar disorder is typified by unpredictable mood swings, impulsivity, intense and tumultuous relationships, and a fragile sense of self. People with Borderline Personality Disorder (BPD) often experience intense anxiety over being left behind. To cope with their emotional distress, they may turn to drugs or self-harm. They may also exhibit a lack of focus and exhibit sudden shifts in their goals and self-image.
Among the crucial BPD traits are:
Severe desertion fear passionate but unstable relationships
Impulsivity and risky behaviour
Unpredictable feelings and mood swings
Continuous emptiness
Both NPD and BPD are characterized by distorted self-perception and relationship issues, there are key differences between the two disorders:
While people with NPD are primarily preoccupied with maintaining their inflated sense of self and seeking approval, persons with BPD often struggle with significant emotional dysregulation and abandonment fear.
Relationship difficulties are a feature of both disorders, but although people with BPD may oscillate between discounting and idealizing others as a result of strong emotional reactions, people with NPD usually lack empathy and take advantage of others for their own gain. Emotional Stability: While people with NPD may exhibit more stable emotional states but struggle with empathy, people with BPD are more likely to experience mood swings, emotional instability, and a persistent sensation of emptiness.
Self-Image: People with BPD may suffer with quick changes in their self-image and a sense of identity, whereas those with NPD frequently have an exaggerated and grandiose self-image that they want to preserve.
What are some methods of Treatment?
Psychotherapy is usually an effective treatment for both BPD and NPD, though the specific methods used may vary:
NPD Treatment: Refuting false beliefs, enhancing social skills, and cultivating empathy are frequently the main goals of NPD therapy. Psychodynamic treatment and cognitive-behavioural therapy (CBT) are frequently utilized.
Dialectical behaviour therapy (DBT), which places an emphasis on skill development in emotion regulation, distress tolerance, interpersonal effectiveness, and mindfulness, is frequently used in the treatment of borderline personality disorder (BPD). Additional strategies like psychodynamic therapy and schema therapy might also be helpful.
Both Borderline Personality Disorder (BPD) and Narcissistic Personality Disorder (NPD) are separate personality disorders, each having unique traits and difficulties. Even while they could have certain things in common, such interpersonal problems and issues with self-perception, it's important to recognize the differences between the two in order to make an accurate diagnosis and provide appropriate therapy. People with BPD and NPD can learn to control their symptoms and enhance their general quality of life with the right assistance and therapy.
Read out such more content view our blog
#mentalhealth#narcissism#narcissist#npd#npdawareness#narcissisthealing#narcissisticpersonalitydisorder#bpd#borderlinepersonalitydisorder#bpdawareness#bpdrecovery#bpdsupport#mentalhealthmatters#blog
0 notes
Text
Navigating Bipolar Treatments in Miami: A Comprehensive Guide to Finding Balance

Introduction:
Living with bipolar disorder can be challenging, but with the right treatment, individuals can lead fulfilling lives. If you find yourself in Miami and are seeking effective bipolar treatments, you're in the right place. This guide will explore various treatment options, local resources, and practical tips to help you or your loved ones manage bipolar disorder and find the balance you deserve.
Understanding Bipolar Disorder:
Before delving into treatments, let's briefly understand bipolar disorder. It's a mental health condition characterized by extreme mood swings, ranging from manic highs to depressive lows. Individuals with bipolar disorder often face challenges in maintaining stability and managing their emotions.
The Importance of Professional Diagnosis:
If you suspect that you or someone you know may have bipolar disorder, seeking professional help is crucial. A mental health professional can provide an accurate diagnosis, which is the first step toward effective treatment. In Miami, there are various experienced psychiatrists, psychologists, and therapists who specialize in mood disorders.
Medication as a Foundation:
One common approach to treating bipolar disorder involves medication. Mood stabilizers, antipsychotics, and antidepressants are commonly prescribed to help regulate mood swings. It's essential to work closely with a qualified healthcare provider to find the right medication and dosage that suits your individual needs.
Therapy for Emotional Support:
In addition to medication, therapy plays a crucial role in bipolar disorder treatment. Cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and psychoeducation are effective in helping individuals manage their emotions, develop coping strategies, and improve interpersonal relationships. Miami offers a variety of therapy options, both in-person and online, providing flexibility for individuals seeking support.
Miami's Supportive Community:
Building a support system is integral to managing bipolar disorder. Miami boasts a supportive community with numerous local organizations and support groups. Connecting with others who share similar experiences can provide valuable insights and encouragement. NAMI Miami-Dade, for example, offers support groups and educational programs for individuals living with mental health conditions.
Lifestyle Changes for Stability:
Beyond professional treatments, incorporating positive lifestyle changes can enhance the overall management of bipolar disorder. Regular exercise, a balanced diet, sufficient sleep, and stress management are crucial factors in promoting stability. Miami's tropical climate provides ample opportunities for outdoor activities, making it easier to incorporate healthy habits into your daily routine.
Alternative Therapies in Miami:
Miami embraces holistic approaches to mental health, offering various alternative therapies that complement traditional treatments. Yoga, meditation, and acupuncture are examples of practices that some individuals find beneficial in managing bipolar disorder symptoms. Many wellness centers and studios in Miami cater to those seeking alternative therapeutic options.
The Role of Family and Friends:
The support of family and friends is invaluable in the journey of managing bipolar disorder. Educating loved ones about the condition can foster understanding and create a more supportive environment. Miami's diverse and vibrant community is conducive to building strong social connections, providing individuals with opportunities to engage in activities that bring joy and fulfillment.
Overcoming Stigma:
Addressing the stigma surrounding mental health is a crucial aspect of effective treatment. Miami actively promotes mental health awareness through events, campaigns, and educational programs. By fostering open conversations and reducing stigma, the community contributes to creating an environment where individuals feel comfortable seeking help and support.
Conclusion:
Navigating bipolar treatments in Miami involves a multifaceted approach, combining professional assistance, community support, and lifestyle changes. By taking advantage of the diverse resources available in this vibrant city, individuals living with bipolar disorder can embark on a journey toward stability, balance, and improved overall well-being. Remember, seeking help is a sign of strength, and in Miami, you're not alone in your journey towards better mental health. Contact us now!
0 notes
Text
Dialectical Behavior Therapy
Dialectical behavior therapy (DBT) is a structured program of psychotherapy with a strong educational component designed to provide skills for managing intense emotions and negotiating social relationships. Originally developed to curb the self-destructive impulse of chronic suicidal patients, it is also the treatment of choice for borderline personality disorder, emotion dysregulation, and a growing array of psychiatric conditions. It consists of group instruction and individual therapy sessions, both conducted weekly for six months to a year.
The "dialectic" in dialectical behavior therapy is an acknowledgement that real life is complex, and health is not a static thing an ongoing process hammered out through a continuous. Socratic dialogue with the self and others. It is continually aimed at balancing opposing forces and investigating the truth of powerful negative emotions.
DBT acknowledges the need for change in a context of acceptance of situations and recognizing the constant flux of feelings-many of them contradictory-without having to get caught up in them. Therapist-teachers help patients understand and accept that thought is an inherently messy process. DBT is itself an interplay of science and practice.
When Is It Used?
With its strong emphasis on emotion regulation skills, DBT is finding application as a treatment for wide range of mental health conditions. They include:
•Personality disorders, including borderline personality disorder
•Self-harm
•Posttraumatic stress disorder
•Bulimia
•Binge-eating disorder
•Depression
•Anxiety
•Substance use disorder
•Bipolar disorder
What to Expect
Expect a course of treatment that typically consist of weekly group, skill-focused instructional meetings as well as individual therapy sessions. Individual sessions usually last an hour, group meetings, usually consisting of four to 10 people, are designed to run for an hour and a half to two hours. DBT is present-oriented and skill-based, and patients are asked to practice their skills between sessions. Patients can expect homework assignments, which might, for example, focus on taking specific, concrete steps to master relationship challenges.
DBT specifically focuses on providing therapeutic skills in four key areas:
•Mindfulness enables individuals to accept and be present in the current moment by noting the fleeting nature of emotions, which diminishes the power of emotions to direct their actions.
•DBT also inculcates distress tolerance, the ability to tolerate negative emotion rather than needing to escape from it or acting in ways that make difficult situations worse.
•Emotion regulation strategies give individuals the power to manage and change intense emotions that are causing problems in their life.
•Last but not least, DBT teaches techniques of interpersonal effectiveness, allowing a person to communicate with others in a way that is assertive, maintains self-respect, and strengthens relationships; a core principle is that learning how to ask directly for what you want diminishes resentment and hurt feelings.
DBT incorporates many of the techniques of cognitive behavioral therapy (CBT). It helps patients recognize and challenge the varieties of distorted thinking the underlie negative feelings and prompt unproductive behavior. For example, patients learn to identify when they are catrophizing-assuming the worse will happen-in order to avoid acting as if it were the case. They review their own past and present experience for instances of all-or-nothing thinking, seeing everything in extremes of black and white, devoid of nuance that is more generally the nature of life.
Mindfulness training is an important part of DBT. In addition to keeping patients present-focused, it slows down emotional reactivity, affording people time to summon healthy coping skills in the midst of distressing situations. Patients are asked to keep a diary tracking their emotions and impulses, a tool that helps them gain awareness of their feelings, understand which situations are especially problematic for them, and use the information to gain control over their own behavior. In individual sessions, patients review difficult situations and feelings they face the prior week and engage in problem-solving by actively discussing ways of behaving that might have delivered a positive outcome. In addition, patients typically have access to therapists between sessions for skills coaching if they are in a crisis.
How It Works
In seeing many health conditions as disorders of emotion dysregulation, DBT is focused on emotions and how they feel ineffectual action patterns. Many elements of the therapy are aimed at teaching patients how to recognize, understand, label, and regulate their emotions and how to handle interpersonal situations that give rise to negative or painful emotions.
Each week, for individual therapy sessions, patients complete a diary "card" (often done via an app), a self-monitoring form that tracks individualized treatment targets relating moods, behavior, and skills. Patients identify and rate the intensity of emotions they experience each day-fear, shame, sadness, anger, pain, suicide attempts, and more-and space is provided to discuss emotional experience in more detail if needed. In addition, using a checklist of skills-which also serves as a handy reminder to deploy them-patients note the frequency with which they engaged in positive practices, from self-soothing and radical acceptance to reducing vulnerability and acting in ways contrary to how they felt.
The information on the diary card let's the therapist know how to allocate session time. Life-threatening or self-injurious behavior take priority, not surprisingly. After identifying the behavioral targets for a session, the therapist helps the patient engage in behavioral analysis, figuring out what led to a specific problem situation the patient encountered, including any underlying beliefs or attitudes that surreptitiously reinforce the behavior, and discussing the consequences of the patients actions. The therapist and patient discuss more skillful ways to solve emotional and life problems.
Because DBT is a demanding therapy to deliver even for experienced therapists, therapists typically work in consultation with a treatment team and regularly meet with a team. The team's recommendations are often applied in individual therapy sessions.
While studies of DBT have documented improvement within a year of treatment, particularly in controlling self-harmful behavior, patients may require therapy for several years.
What to Look for in a Dialectical Behavior Therapist
A DBT therapist is a licensed mental health professional who has additional training and experience in DBT. Several organizations provide certification in DBT to qualified therapists who have completed advanced academic and clinical work. Certified DBT therapist may use the designation CDBT.
DBT is a comprehensive and multifaceted therapy designed to help patients cope with extreme emotional suffering and, often, self-injurious behavior. Many patients seeking DBT have undergone other forms of therapy without experiencing significant improvement. DBT is a complex treatment modality that makes many demands of the therapist and requires extensive training to be administered in the way it was developed and tested.
Many components of the therapy, such as the skills training, have been adapted to treatment programs that do not reflect the comprehensive DBT treatment protocol. Finding a clinician who has undergone training and certification in the full DBT treatment model can be important to a good outcome.
When seeking a DBT therapist, experience counts. It is advisable to seek a therapist who has not just extensive training but also experience using DBT to treat patients presenting with concerns such as yours.
Important as qualifications and experience are, so is as good fit. As with all forms of therapy, it is also advisable to find a DBT therapist with whom you feel comfortable. Look for someone with whom you can establish clarity of communication.
Here are some important questions to ask a prospective DBT therapist:
•How often have you dealt with problems such as mine before?
•How do you know my situation is a good candidate for DBT?
•How does DBT work?
•What is a typical plan of treatment, and how long is a typical course of therapy?
•How do you measure progress?
•What is the nature of your training in DBT
•Do you provide comprehensive DBT or a modification?
•Do you belong to a DBT consultation team?
•What is your policy on phone calls and emails during the week?
•What length of time do you initially ask a client to commit to?
0 notes
Text
solstice (in any modern verse) is diagnosed with bipolar disorder, with a strong genetic predisposition to it through her mother. (she also has it in her canon, though there's no real name for it as far as I know now. her muime and hag-mother do help her with managing it eventually, however.)
this manifested in her childhood and adolescence most clearly through manic episodes followed by severe low periods of intense depression. her intense days-long bouts of mania were fun for a while (though not without a lot of risk-seeking behavior that often toed the line of danger), but the crash was always so much worse. as she got older, it took a toll on her interpersonal relationships. solstice was... not a good friend to a lot of people, and exhibited a lot of toxic and manipulative behaviors learned by her mother. it wasn't until she was well into her 20s (in the modern verse) to unlearn a lot of that through a lot of purposeful reflection and behavioral therapy.
she also struggled with substance abuse (hard drugs) and self-harming habits that she's since kicked.
#the generational trauma of mothers and their daughters continues......#⋆ 𝘵𝘩𝘦 𝘴𝘶𝘯 𝘪𝘴 𝘢𝘭𝘴𝘰 𝘢 𝘴𝘵𝘢𝘳 𖤓 modern.#⋆ 𝘰𝘩 𝘴𝘸𝘦𝘦𝘵 𝘴𝘶𝘮𝘮𝘦𝘳 𝘤𝘩𝘪𝘭𝘥 𖤓 study.#drug tw#drugs tw#addiction tw#self harm tw#ask to tag
1 note
·
View note
Text
The Nature of Borderline Personality Disorder’s Concerningly High Comorbidity Rate with Substance Use Disorder
Introduction
An alarming number of individuals diagnosed with borderline personality disorder engage in substance use frequently enough to present significant issues in their day-to-day functioning, which often results in a comorbid diagnosis of substance use disorder. Approximately 78% of adults with borderline personality disorder (henceforth noted as “BPD” in this paper) develop substance use disorder or an addiction at some time in their lives, according to research conducted by the US National Comorbidity Survey Replication (NCS-R). We will take a closer look at what causes the relationship between BPD and using substances (whether maladaptive coping or self-medication), the insurmountable grief of BPD that so commonly pervades these individuals’ lives, and other contributing factors.
BPD is a severe mental illness that is most commonly caused by childhood trauma. The severity and length of these traumatic events varies widely, and can happen repeatedly during childhood (called “complex psychological trauma”). Research shows that there is also a genetic component. “Current research supports the theory that there is a large genetic component to whether a person develops BPD. Two genes—DPYD and PKP4—have been identified as increasing a person's risk of developing BPD. However, these genes are linked to schizophrenia and bipolar disorder risk, too.” (Bence, 2021). Even still, traumatic events have long been believed to be a more prominent predicting factor. Borderline personality disorder causes frequent emotional disturbances and emotional instability, interpersonal relationship issues, unstable identity and sense of self, impulsive behaviors (including drug or alcohol use), chronic feelings of emptiness or boredom, and frantic efforts to avoid real or imagined abandonment. The errors in the neurocircuitry of someone with BPD can even be seen in neuroimaging scans. “Various neuroanatomical and neurophysiological abnormalities have been reported in individuals with BPD, including reduced hippocampal, amygdala and frontal lobe volumes, as well as diminished serotonergic function.” (Axelrod, 2010). The purpose of this paper is to take a look at the different symptoms of BPD that can contribute to self-medication with substance use. This paper also aims to take a look at why the number of BPD patients with comorbid substance use disorder is so high, and what can be done to manage it. This will include topics such as emotional dysregulation, distress tolerance, anxiety, and maladaptive coping mechanisms.
What Drives A Person with BPD to Use Substances
As many as 70% of people diagnosed with BPD will attempt suicide at least once in their lifetime. The suicide completion rate is 10%. “Borderline personality disorder (BPD) is associated with suicidal behaviors and self-harm. Up to 10% of BPD patients will die by suicide.” (Paris, 2019). Marsha Linehan, who invented the therapeutic model of Dialectical Behavior Therapy (the most effective treatment for BPD), once said “People with BPD are like people with third degree burns over 90% of their bodies. Lacking emotional skin, they feel agony at the slightest touch or movement.” These individuals are often engulfed in such turbulent emotional turmoil that they turn to substances of any kind to dull the pain, or to distract them from it. With that in mind, it comes as no surprise that—if not in therapy—a majority of them will self-medicate.
The Impact of Substance Use in BPD
A co-occurring diagnosis with substance use disorder could make the BPD even more severe in such a way that would increase impulsivity, suicide risk, and even shorten overall lifespan. “People with Borderline Personality Disorder have a reduced life expectancy of some 20 years, attributable largely to physical health maladies, notably cardiovascular.” Many illicit substances are very hard on the heart, with methamphetamine being the biggest proponent to cardiovascular disease. “Several clinical and postmortem studies clearly associate the use of methamphetamine with cardiovascular disease,13 and cardiovascular disease represents the second leading cause of death among methamphetamine abusers, following only accidental overdose.” (Kevil, 2019). Alongside medical maladies (of which there are many more due to substance use), frequent substance use could impact many facets of one’s life, including personal and familial. “Substance use disorders (SUDs) are associated with numerous medical, psychiatric, psychological, spiritual, economic, social, family, and legal problems, creating a significant burden for affected individuals, their families, and society.” (Daley, 2014). This could include—but is not limited to—emotional burden, economic burden, strained relationships, family instability (which may result in severe conflict), and effects on a developing fetus (if the person is pregnant). “Alcohol use during pregnancy can harm fetal development causing birth defects and problems in child development. Infants born to opioid-dependent mothers are at increased risk for neonatal abstinence syndrome, which can contribute to developmental or cognitive delays. Children of parents with SUDs are at increased risk for abuse or neglect, physical problems, poor behavioral or impulse control, poor emotional regulation, conduct or oppositional disorders, poorer academic performance, [and] psychiatric problems…” (Daley, 2014). Keeping all of this in mind, it is evident that these different factors could greatly worsen a person’s BPD.
Outcomes of Treatment
As previously mentioned, Dialectical Behavior Therapy (henceforth noted as DBT) is the most effective treatment for BPD (although Acceptance Commitment Therapy and Dynamic Deconstructive Therapy have been shown to work as well), and that includes BPD comorbid with substance use disorder. “DBT emphasizes that a patient's maladaptive behaviors (e.g., self-mutilation, suicidal behavior, drinking, use of drugs, binging) often function to regulate aversive emotional experiences, and that temporary reductions in arousal following these behaviors negatively reinforce future use of these maladaptive strategies. Thus, much of the focus in DBT revolves around the acquisition and application of adaptive emotion regulation skills.” (Bornovalova, 2007). Below is a table demonstrating the efficacy of dialectical behavior therapy in the treatment of BPD with comorbid substance use; namely cocaine, alcohol, opioids, cannabis, and methamphetamine.
DBT is comprised of four major pillars: Emotion regulation, distress tolerance, interpersonal effectiveness, and mindfulness. One of the other prominent themes of this therapy model are the three types of mindsets: “Emotion mind”, “Logic mind”, and “Wise mind”. Emotion Mind is when an individual operates purely based on their feelings, and often acts impulsively. Logic Mind is when an individual operates solely on reasoning, ignoring their emotions and acting cold and methodical. Wise Mind is when the individual is able to join the two “minds” and operate from a place of both logic and emotion. Patients and clients are encouraged to journal and write down which mind they are in when they feel distressed, and they are encouraged to use a plethora of different DBT “skills”. Using this model of therapy has proven extremely useful for treating BPD, to the point that some people will no longer even meet criteria for BPD after long periods of this treatment. “Research finds that up to 77% of people no longer met the criteria for BPD after one year of treatment with DBT.” (The Mental Health Service Journal, 2020). These aforementioned “DBT skills” are used to stop urges to self-harm or self-medicate. There is even a skill to help the person with BPD calm down from a mental health crisis. It is called the TIPP skill, and there are many more skills for different occasions as well. The most helpful ones for resisting substance cravings would be the STOP skill and “Opposite Action” technique where one forces themselves to do the opposite of what their urges and cravings are telling them to do. Dialectical behavior therapy demonstrates a success rate for treating BPD (and BPD with comorbid SUD) that is not seen in any other form of treatment. Though other models of therapy are available, none have proven as effective for this particular issue as DBT. “Results from the DBT condition revealed that the intervention had a significant positive effect on behavioral and attitudinal features of disordered eating, substance use severity, negative mood regulation, and depressive symptoms.” (Courbasson, 2011).
It is also worth noting that, if regularly attending therapy and achieving treatment goals, BPD has a high remission rate regardless of its initial severity. “…50% of the borderline patients studied achieved a recovery from borderline personality disorder—an outcome that required being symptomatically remitted and having good social and vocational functioning during the past two years. In contrast, 93% of borderline patients attained a symptomatic remission lasting two years and 86% attained a sustained symptomatic remission that lasted four years.” Some individuals with BPD find that it gets easier to manage with age, sometimes even achieving complete recovery. It was once thought that receiving a BPD diagnosis was so incredibly grim, that recovery was near impossible. Now we know that that is far from the truth. There are also some medication options available to those wanting to recover from substance use. For example, for opioid or alcohol dependence, there is Naltrexone. “Naltrexone is an FDA-approved opioid antagonist used to treat alcohol use disorder and opioid dependence. Naltrexone blocks the effect of opioids and prevents opioid intoxication and physiologic dependence on opioid users.” (Singh, 2023). There are a few other options as well, including suboxone and a whole host of medications for other substances.
Conclusion
In conclusion, BPD has a concerningly high comorbidity rate with substance use disorder. The literature is clear on this, and is clear on why this is and how it can be treated. Social support, peer support, and support from one’s family and friends would also help in encouraging the person with BPD and SUD to recover and maintain recovery and sobriety. It is of utmost importance to have a sense of community while trying to heal from such serious mental health issues. Recovery is very possible, and there are effective treatment options available.
References
Axelrod, Seth R et al. “Emotion regulation and substance use frequency in women with substance dependence and borderline personality disorder receiving dialectical behavior therapy.” The American journal of drug and alcohol abuse vol. 37,1 (2011): 37-42. doi:10.3109/00952990.2010.535582
Bence, Sarah. “Is Borderline Personality Disorder Genetic?” Verywell Health, Verywell Health, 6 Aug. 2021, www.verywellhealth.com/is-borderline-personality-disorder-genetic-5191970
Bornovalova, Marina, et al. “How Does Dialectical Behavior Therapy Facilitate Treatment Retention among Individuals with Comorbid Borderline Personality Disorder and Substance Use Disorders?” Clinical Psychology Review, Pergamon, 7 Feb. 2007, www.sciencedirect.com/science/article/abs/pii/S0272735807000347
Courbasson, Christine, et al. “Outcome of dialectical behaviour therapy for concurrent eating and substance use disorders.” Clinical Psychology & Psychotherapy, vol. 19, no. 5, 2011, pp. 434–449, https://doi.org/10.1002/cpp.748.
Daley, Dennis C. “Family and social aspects of substance use disorders and treatment.” Journal of food and drug analysis vol. 21,4 (2013): S73-S76. doi:10.1016/j.jfda.2013.09.038
Kevil, Christopher G., et al. “Methamphetamine use and cardiovascular disease.” Arteriosclerosis, Thrombosis, and Vascular Biology, vol. 39, no. 9, 2019, pp. 1739–1746, https://doi.org/10.1161/atvbaha.119.312461.
Links, P. S., et al. “Borderline Personality Disorder and Substance Abuse: Consequences of Comorbidity”. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, vol. 40, no. 1, SAGE Publications, Feb. 1995, pp. 9–14, https://doi.org10.1177/070674379504000105.
May, Jennifer M et al. “Dialectical Behavior Therapy as Treatment for Borderline Personality Disorder.” The mental health clinician vol. 6,2 62-67. 8 Mar. 2016, doi:10.9740/mhc.2016.03.62
Paris, Joel. “Suicidality in Borderline Personality Disorder.” Medicina (Kaunas, Lithuania) vol. 55,6 223. 28 May. 2019, doi:10.3390/medicina55060223
Singh, Dharminder. Naltrexone - StatPearls - NCBI Bookshelf, www.ncbi.nlm.nih.gov/books/NBK534811/. Accessed 9 Dec. 2023.
Zanarini, Mary C et al. “Time to attainment of recovery from borderline personality disorder and stability of recovery: A 10-year prospective follow-up study.” The American journal of psychiatry vol. 167,6 (2010): 663-7. doi:10.1176/appi.ajp.2009.09081130
#this is the rough draft of my research paper!!#my prof and classmates were so impressed they said they genuinely couldn’t find anything to improve about it!#usually they give constructive criticism/feedback and they didn’t this time.#txt
0 notes