#hypotonic cerebral palsy
Text
This Mother's Day I ended up contemplating my grandmother. My aunt posted about her on Facebook and got several comments about how kind and motherly she was, and I asked to know more because she was cruel to me. My aunt tried to reassure me that Grandma wasn't affectionate but she loved her grandkids dearly. I politely contradicted that I know my own experience, and I know my grandmother loved her grandchildren but she had very specifically excluded me and my brothers, and me most of all.
This was the first time I have viewed this experience with knowledge that I was actually visibly partially handicapped as child, and I realized that the reason I witnessed so much more of my grandmother's and uncle's cruelty is that they spoke in front of me like I wasn't there.
It also explains why one uncle always tormented me by telling me that my mom dropped me on my head when I was baby.
#dysfunctional family#cptsdsurvivor#dysfunctional parents#bad parenting#narcissist parents#actually autistic#disability trauma#hypotonic cerebral palsy#hypotonia#barely walked#barely talked#situational mutism#freeze response#family scapegoating abuse#toxic family#family abuse
8 notes
·
View notes
Text
this is okay to rb i think, especially if you have anything to add or any insight. idk. i'm tagging this the way that i am because i'm seeking community/connection(tm) or something
hypotonia is not like. a rare thing. not really. but i do remember my OT googling what it was.
low muscle tone/hypotonia may technically be a symptom rather than a diagnosis (barring benign congenital hypotonia, which afaik is controversial) but it's the closest thing to a "diagnosis" i've been given for some of this stuff because the potential cause of it hasn't been investigated and i guess it's not exactly urgent since my particular case isn't severe and doesn't seem progressive (hypotonia can be progressive & is involved in some progressive and degenerative conditions.)
but i wish it was talked about more and i wish more was known about it works and how it affects bodily function and i wish what we DO know about it was more accessible to the public when it comes to those who suffer from it. it's also kinda hard whether to KNOW you have it or not since its "signs" have so much overlap with other conditions that aren't related to muscle tone. it ranges a lot in severity too. and there's two different types (central and peripheral.) it's linked to dozens of diagnoses too which is why i say it's not uncommon.
but also i guess due to the complexity of how it affects the body and its lack of distinctiveness with most of its symptoms makes it kinda...hard to talk about? and i imagine w/ some people it's hard to distinguish the effects of hypotonia vs. their other problems. issues with chewing, writing, breathing, speaking, posture, coordination, etc. can be due to so many different things ranging from mental to physical. but it's not always something that can be lumped together w/ those other things because there's "my muscles don't work" in a terms of chronic muscular pain vs. "my muscles don't work" in terms of, like, they lack the ability to adequately support the body and bodily movement. if that makes any sense.
which ranges from someone like me where having to hold myself up sucks + mild motor skill/coordination impairments and mild developmental milestone delays, but others never meet those milestones or need assistance with things like breathing and ingesting food.
it's not a diagnosis but it can affect the body in complex ways like muscle shortening and stiffness due to our bodies having to compensate in weird ways for the lack of adequate tone (esp those of us who grew up with it), tibial torsion and femoral anteversion, flatfoot and knock-knees, reduced cervical lordosis sometimes leading to bruxism and occipital headaches, etc. PT centered around muscle strengthening to correct my "improper" movement and stuff.
and there's other stuff that can come with it that people like to consider """gross""" like drooling, constipation and other gastric, and pelvic floor dysfunction which can result in incontinence/problems with bladder control. muscles are involved in a lot of things. wild.
i'm rambling but i just wish more people talked about it. all i really have is that one interview that surestep did with meagan veracha, who has hypotonic cerebral palsy, about living with hypotonia as an adult.
maybe i wouldn't care all that much if i had a diagnosis that would "explain it" but "i might have gHSD/hEDS" doesn't rly do that for me because ppl in those communities obviously focus a lot on the joint dysfunction aspect (because those 2 conditions center around hypermobile joints so that's just natural, it's not a bad thing per-se, barring other problems that those communities have) but for me my case of symptomatic generalized hypermobility is secondary in how it impacts me vs. my muscles being bad at their job and my hypermobility might even be secondary to my hypotonia anyway.
dyspraxia/DCD (some people with it have hypotonia but not all - i thought i had it before i was told i was identified as having hypotonia when i was a kid...over two decades late) is another guess but again that centers more around coordination than things like "anything other than lying in bed is hard on me because my muscles don't support my body like they're supposed to."
maybe muscle tone is a complex medical concept that shouldn't really enter the public lexicon but i have no other language for it.
41 notes
·
View notes
Text
Apparently it’s rare disease day so shoutout to hypotonic cerebral palsy and hydrocephalus
50 notes
·
View notes
Text
Understanding Cerebral Palsy: A Guide to Classification and Treatment Options
Cerebral Palsy (CP) is a group of neurological disorders that affect movement, muscle tone, and coordination. It can be caused by damage to the developing brain before, during, or after birth. Although cerebral palsy is a non-progressive disorder, it can affect a person’s mobility, communication, and daily living activities .
According to Northern Territory Government information and services, Cerebral Palsy in Australia is the most common physical disability in children, with an estimated 34,000 people affected. Early intervention and therapy can improve outcomes and quality of life for those with CP.
Classification of CP
There are five main types of cerebral palsy and each type of CP is characterised by specific symptoms and affects different areas of the body.
Ataxic Cerebral Palsy
Ataxic CP is less common, affecting around 5–10% of people with CP. It is caused by damage to the cerebellum, which is responsible for coordinating movement and balance. People with ataxic CP have poor balance and coordination, and they may have difficulty with fine motor skills, such as writing or buttoning clothes. They may also have a wide-based gait and may sway or stumble when walking.
Athetoid Cerebral Palsy
Athetoid CP, also known as dyskinetic CP, affects around 10–20% of people with CP. It is caused by damage to the basal ganglia, which is responsible for controlling movement. People with athetoid CP have involuntary movements that can be slow and writhing or fast and jerky. They may also have difficulty controlling their posture and may have trouble sitting upright or holding their head steady.
Hypotonic Cerebral Palsy
Hypotonic CP is a rare form of CP, affecting less than 5% of people with CP. It is caused by damage to the cerebellum or the brainstem, which can affect muscle tone and coordination. People with hypotonic CP have low muscle tone, which means their muscles are floppy and weak. They may also have difficulty with posture and may have trouble sitting upright or holding their head steady.
Spastic Cerebral Palsy
Spastic CP is th e most common type, affecting around 70–80% of people with CP. It is caused by damage to the motor cortex of the brain, which controls voluntary movement. People with spastic CP have increased muscle tone, which means their muscles are constantly contracted and can be stiff and difficult to move. They may also experience muscle spasms, especially when trying to move quickly. Spastic CP can affect one or both sides of the body, and it can also affect the legs, arms, or both.
Mixed Cerebral Palsy
Mixed type CP is a combination of two or more types of CP. For example, a person may have spastic and athetoid CP, or ataxic and hypotonic CP. The symptoms and severity of mixed type CP can vary depending on the types of CP involved.
Explore the comprehensive article for deeper insights into Understanding Cerebral Palsy Treatments
0 notes
Text
Do you know about Cerebral Palsy?
Cerebral palsy (CP) is a series of mobility and postural disorders that limit activities and are thought to be caused by non-progressive abnormalities in the baby brain.
The most prevalent and expensive type of chronic motor disability that first manifests in childhood is cerebral palsy (CP). In addition to epilepsy and secondary musculoskeletal issues, the motor abnormalities are frequently accompanied with difficulties of sensation perception, connection, communication, and behavior. A wide range of developmental, genetic, metabolic, ischemic, viral, and other acquired etiologies that result in a similar set of neurologic symptoms are responsible for cerebral palsy (CP). Neurologic involvement pattern, neuropathology, and etiology are the three main categories used to classify CP. Many people with CP function at high levels of schooling and employment, showing no signs of impairment.
In contrast to palsy, which refers to the loss or impairment of motor function, cerebral refers to the brain. The cerebral cortex, the part of the brain that controls how muscles move, is affected by cerebral palsy. In certain cases, the cerebral motor cortex did not develop normally throughout early childhood. In a different case, the harm was brought on by a brain injury that occurred either before, during, or after birth. In either situation, the damage is irreparable, and the resulting disabilities are permanent.
What causes cerebral palsy (CP)?
The condition known as cerebral palsy (CP) is brought on by either damaged or abnormally developing parts of the brain that control movement. This harm may develop prior to, during, or soon after birth. Although it might not be discovered for several months or even a year, the majority of children have congenital cerebral palsy.
The causes of cerebral palsy (CP) are–
Brain infections such as bacterial meningitis or viral encephalitis.
Problem with blood flow to the brain
Head injury (intracranial hemorrhage or bleeding inside brain)
Genetic abnormalities
Congenital brain malformation
Maternal infections on fever
Damage to the white matter of the brain (periventricular leukomacia or PVL)
Severe back of oxygen in the brain
Severe material low blood pressure rupture of uterus, detachment of placenta
Problems involving the umbilical cord
Early symptoms of cerebral palsy (CP) include:
Though a precise diagnosis may not be made until a child is two years old or more, cerebral palsy (CP) science typically manifests in the first month of life. Infants with CP often have developmental delays, which cause them to take longer than usual to attain developmental milestones like:
Learning how to sit, roll over, crawl, or walk.
Altered muscular tone can be present in some newborns with CP.
Hypotonic, or decreased muscle tone, can make them appear stiff or inflexible.
Hypertonia, or increased muscle tone, can make someone appear stiff or inflexible.
strange position
Prefer one side of the body when bending, crouching, or reaching.
Types of cerebral palsy (CP):
The distinct types of cerebral palsy (CP) can be distinguished by:
Spastic Cerebral Palsy
Dyskinesia Cerebral Palsy
Ataxic Cerebral Palsy
Spastic Cerebral Palsy
The most normal type of the condition is one in which the youngster moves awkwardly and with stiff muscles.
Forms of specific cerebral palsy include-
Specific diplopia/ diparesis involves muscle stiffness that is predominantly in the leg and less severely affect the arms and face.
Spasticquadriplegia/ quadriparesis is the most severe form of cerebral palsy and is often associated with moderate-to-severe intellectual disability. Children will often have severe stiffness in their Limbs but a floppy neck they are rarely able to walk. Speaking and being understood are difficult.
Dyskinesia cerebral palsy– is characterized by slow and uncontrollable writing or jerky movements of the hands, feet, arms or leg. Hyperactivity in the muscles of the face and tongue make some children grimace or drool. They find it difficult to sit straight or walk. Some children have a problem hearing, controlling their breathing.
Ataxic cerebral palsy affect balance and depth perception. Children with ataxic cerebral palsy will often have poor coordination and walk unsteadily with a wide based gait. They have difficulty with a quick or precise movements. Such as writing for or buttoning a shirt or a hard time controlling voluntary movements such as reaching for a book.
Symptoms appears in cerebral palsy:-
Children with cerebral palsy (CP) following symptoms including
Lack of muscle coordination when performing voluntary movement
Stiff and tight muscle and exaggerated reflexes.
Weakness in one or more arm and leg
Walking on the toes a croached gait or a scissored gain
Variations in muscle tone either to stiff or to floppy
Excessive drooling or difficulty swallowing or speaking
Shaking or random involuntary movements
Delays in reaching motor skill milestones
Difficulty with precise movements such as writing or buttoning a shirt
Intellectual disability
Abnormal physical sensation
Impaired vision
Hearing, language and speech problems
Delayed growth and development
Learning difficulties
Dental problems
Contractures
Malnutrition, inactivity
#ChildAyurvedicSpecialistinPune#AutismTreatmentforchildreninPune#CerebralpalsytreatmentForchildinPune#TreatmentfordownsyndromechildinPune#ADHDtreatmentforchildinPune#ChildautismtreatmentinIndia#HeightincreasetreatmentinIndia
0 notes
Text
From Diagnosis to Recovery: The Comprehensive Cerebral Palsy Care at Upright Kids Ortho with Paediatric Orthopaedic Surgeon Bangalore | Dr. Jayanth S Sampath

Cerebral palsy (CP) is a disorder that affects muscle tone, movement, and motor skills (the ability to move in a coordinated and purposeful way).
Cerebral palsy can also lead to other health issues, including vision, hearing, and speech problems, and learning disabilities.
CP is usually caused by damage to parts of the brain before or during a child’s birth, or during the first 2 years of a child’s life.
There is no cure for CP, but treatments such as physical therapy, splints or orthotics, medications such as Botulinum injections and Orthopaedic Surgery will help a child who is living with the condition.
It is worthwhile pointing out that majority of common human ailments such as diabetes, high blood pressure, stroke, heart attack, kidney failure, etc are also incurable conditions. But, treatment of these conditions is essential to prevent complications. Cerebral palsy is no different in that it does not have a cure but treatment is essential.
How does Cerebral Palsy work At Upright Kids Ortho?
What are the symptoms and signs of cerebral palsy?
Paediatric Orthopaedic Surgeon Bangalore | Dr. Jayanth S Sampath says the predominant symptoms and signs of cerebral palsy are related to difficulties with movements of the legs and arms.
The extent and severity of the brain lesion is the leading factor in the magnitude of the motor deficit. For example, developmental motor delay, gait disorders, poor fine and gross motor coordination, swallowing disorders, or speech delay are all the result of the basic movement problem. The way they present varies from child to child. For that reason, it is difficult to describe a clinical picture that will satisfy every child with cerebral palsy. The clinical presentation, even though with many common features, is very much unique for a particular child. In addition, the comorbid conditions add more to the uniqueness of the presentation of the child with cerebral palsy. For example, some children may be blind, while others may have normal vision; some children may have a severe cognitive delay while others may have a normal or near normal cognitive level.
What are the types of cerebral palsy?
Based upon the form of motor impairment, cerebral palsy can be divided into types:
Spastic cerebral palsy
Dyskinetic cerebral palsy (according to the predominant symptoms dyskinetic CP may be either dystonic or choreo-athetoid) which includes ataxic cerebral palsy
Hypotonic cerebral palsy.
These categories are not rigid, and the majority of patients most probably have a mixture of them.
Cerebral palsy can also be classified into different types depending on the mobility level of the child. This system is called GMFCS (Gross Motor Functional Classification System) and is the most widely used classification system to describe children with cerebral palsy. The figure below easily illustrates the different types from Level I to Level V. Kindly note that the mobility level changes slightly as the child goes through the teenage years and pubertal growth spurt.
This is a well-described aspect of the natural history of cerebral palsy. Children who were walking with support until the age of 8 – 10 years lose some or all of their walking ability during early adolescence. This has been attributed to a reduction in the power: weight ratio of children. As muscles become bigger, they also become weaker relative to their weight.
Causes of CP
Paediatric Orthopaedic Surgeon Bangalore | Dr. Jayanth S Sampath says There is no identifiable cause in some children with cerebral palsy.
Typical causes to look for include
Problems occurring before birth (e.g. exposure to radiation, infection, inadequate brain development),
Problems during birth such as asphyxia before birth, hypoxia (poor oxygen supply) of the brain, and birth trauma during labor and delivery
Premature and low birth weight babies
Complications occurring some time after birth or during childhood.
Genetic causes
In the modern context, many premature babies (babies born earlier than 36 weeks and/ or less than 1.5 kg in weight at birth) can be saved thanks to advances in neonatal care but premature babies have an increased risk of CP. Many of the children that we see in our practice have spent some time in the NICU (neonatal intensive care unit). Fortunately, premature babies have spasticity as their predominant movement disorder, most will walk independently and their gait problems can be corrected by orthopaedic surgery.
In the past, conditions such as kernicterus (uncontrolled jaundice in newborn babies causing damage to parts of the brain) were quite common. This group of disorders caused dyskinetic type of CP that was not readily amenable to surgery and prognosis for walking was poor. Due to early detection of jaundice in most neonates and prompt treatment, the incidence of Kernicterus is on the decline.
Why do premature babies develop CP?
Premature infants are vulnerable, in part because their organ systems and control mechanisms are not fully developed, increasing the risk of reduced oxygen supply to the brain that may manifest later as CP.
It is sometimes difficult to differentiate between cerebral palsy caused by damage to the brain that results from inadequate oxygenation and CP that arises from brain damage which occurs when the baby is still in the womb that then precipitates premature delivery. From the point of view of treatment, this distinction is academic and not of much relevance. MR scan of the brain may help in diagnosing this further but in terms of treatment, diagnostic tests such as MR scans do not help with orthopaedic treatment.
After birth (postnatal), other causes include toxins, severe jaundice, lead poisoning, physical brain injury, shaken baby syndrome, incidents involving hypoxia to the brain (such as near drowning), and encephalitis or meningitis.
The three most common causes of asphyxia in the young child are: choking on foreign objects such as toys and pieces of food, poisoning, and near drowning.
In general, postnatal causes of CP (damage to the brain after birth) result in a more severe form of the condition with extreme muscle tone and postures, severe cognitive impairment and the prognosis for walking is less certain compared to CP caused by prematurity.
Diagnosis of Cerebral Palsy:
The initial suspicion of CP is typically raised by family members or noticed by the parents as a failure to achieve motor milestones. The child may not achieve head control by 6 months, sitting may be delayed or mild abnormalities in walking may be noticed.
The child’s paediatrician is usually the first person to raise the possibility of CP. As mentioned earlier, cerebral palsy is NOT a condition resulting from a single cause. It is a clinical diagnosis made by doctors when a child has a number of different problems such as problems with walking, speech, hearing, sight, balance, co-ordination and fine motor control (using the hands for delicate tasks such as writing).
No single factor can confirm or refute the diagnosis of CP. Rather; it is combination of various factors that taken together will help the doctor make the diagnosis of CP.
For instance, a 2 year old child who has not yet started walking; was a premature baby born at 7 months with a birth weight of 1kg may turn out to have cerebral palsy.
Though tests such as an MR scan of the brain are quite commonly done in the process of making the diagnosis of CP, there is no single test which will confirm the diagnosis. As the causes of CP are highly varied, a series of investigations (tests) may need to be carried out.
Who makes the diagnosis?
According to Paediatric Orthopaedic Surgeon Bangalore | Dr. Jayanth S Sampath, Any qualified clinician with experience in the area of child development can make a diagnosis of cerebral palsy. Typical clinicians who may see children with a potential diagnosis of CP include paediatricians, physiotherapists, paediatric orthopaedic surgeons, developmental specialists, and paediatric neurologists, amongst others.
Once the possibility of CP has been raised, it is prudent to seek the opinion of
A paediatric neurologist (to confirm the diagnosis) and
A paediatric orthopaedic surgeon (to discuss treatment options).
It is advisable to seek expert advice early so that parents can be correctly counselled about the particular treatment options suitable for their child.
Clinicians unfamiliar with the modern management of CP are a source of misinformation to parents. Words such as “untreatable” are sometimes used, causing uncertainty and distress to parents. CP is very much treatable with modern scientific methods and good outcomes are routinely obtained in the majority of children.
Treatment for CP
There are several factors which influence choice of treatment for a particular child. The principal among these are:
Age of the child
The age of the child is the single most important factor which influences treatment planning. Cerebral palsy is a “static” encephalopathy, meaning that the primary problem in the brain does NOT change over time. It does not get better or worse. However, bones, muscles and joints of the legs can develop abnormalities due to growth.
Any intervention such as physiotherapy, Botox injection or surgery should be employed after a thorough understanding of the natural history of cerebral palsy. Thanks to the pioneering work of Prof Rosenbaum and co-workers (from CanChild Centre for Childhood Disability Research, McMaster University, Canada), we have a detailed understanding of how children with CP develop in the first few years of life. Similar findings were seen in an independent Swedish study (Developmental Medicine & Child Neurology 2007, 49: 751–756).
The graph below shows that children with GMFCS Level I and II CP (children with independent walking ability) reach their peak motor ability around the age of 6 to 7 years. This NATURAL improvement occurs due to the maturation of brain function. It, therefore, stands to reason that any intervention such as orthopaedic surgery should be performed after the age of 7 years.
The Ontario Motor Growth Study
The Motor Growth Curves report patterns of gross motor development in children with cerebral palsy, classified according to each of the five levels of the Gross Motor Function Classification System (GMFCS) (Palisano et al., 1997). Children in this study were followed longitudinally for several years. The findings were published in a paper entitled ‘Prognosis for Gross Motor Development in Cerebral Palsy. Creation of Motor Growth Curves’, Rosenbaum et al., JAMA 2002; 288; 1357-63.
In the first few years of life, most children with CP will benefit from supportive treatments such as physiotherapy and orthotics. Once the child reaches his or her maximum motor potential (typically between the ages of 8 and 10 years) and achieves a steady state in terms of growth, consideration can be given to whether orthopaedic surgery will be beneficial.
The graph below illustrates common interventions undertaken at different ages in children with CP.
It can be seen that peak age for non-surgical treatments is around 5 years and the peak age for surgery is around 10 years.
GMFCS Level:
The walking ability of the child determines his/ her GMFCS level. Children with GMFCS levels I and II and some children with Level III CP may benefit from Gait Improvement Surgery (also called Single Event Multi-level Surgery or SEMLS).
Children with GMFCS Levels IV and V CP do not benefit from surgery to release contractures or muscle tightness in the legs, as the children in this category are unlikely to gain the ability to walk even with surgery. However, children with GMFCS Levels IV and V CP have a high risk of gradual dislocation of the hip joint. This will require careful monitoring through regular hip x-rays.
Movement Disorder:
Spasticity is the most common movement disorder seen in CP. Muscles affected by spasticity feel tight when stretched suddenly. Slow and gentle stretching of the muscle does not evoke spasticity.
Children with spasticity as their predominant movement disorder and who are able to walk either independently or with support have a better overall prognosis with regard to walking/ standing ability compared to children with other types of movement disorders.
Children with dyskinetic movement disorders such as Dystonia, Athetosis, chorea, ataxia or hypotonia DO NOT show a predictable response to surgery.
Scientific publications also advocate non-surgical treatment options in children with Dystonia. Dyskinetic movements are caused by damage to parts of the brain (called basal ganglia). Performing orthopaedic surgery by muscle releases and tendon lengthening cannot change the damaged area in the brain.
It is highly likely that children with dyskinetic movement patterns will remain unchanged even after orthopaedic surgery. Any minor improvements noted after surgery are likely to be due to the physiotherapy provided post-operatively and these improvements will reverse once the intensive physiotherapy is stopped.
Spasticity is caused by damage to nerve fibres leaving the higher centres of the brain (cerebral cortex). Therefore, spasticity does not change after muscle release surgery. What orthopaedic surgery corrects is the permanent muscle stiffness which occurs as a consequence of spasticity. In fact, some experts believe that spasticity is beneficial in that it maintains muscle strength to a certain extent.
Orthopaedic surgery is therefore recommended only in those children who have permanent shortening of the muscle rather than pure spasticity. If regular physiotherapy and other treatments are provided at an early stage, muscle shortening does not typically develop in younger children (less than 6 years of age). Even in those younger children where contractures do develop, this can be managed without the need for surgery, through the use of Botox, serial casting, physiotherapy and use of splints.
There are treatments such as Botulinum toxin injection; Selective Dorsal Rhizotomy and Intrathecal Baclofen pump which directly reduce spasticity. More information about these anti-spasticity treatments is provided in a later section.
As the child grows, bones and muscles normally grow in almost perfect synchrony.
In children with CP, muscle growth is unable to keep up with bone growth. Therefore, muscles become progressively shorter over time. This causes joint tightness and eventually contractures (permanent joint tightness).
Bones can develop abnormal twists (called torsional problems) in children with CP.
When babies develop inside the mother’s womb, bones of the legs develop with an inward twist. This is normal and happens in all children. Typically developing children start walking by the age of 1 year. The forces applied to the legs during walking causes the inwardly twisted bones to straighten out. When walking is delayed (in conditions such as CP), the embryonic alignment of the leg bones persists. Persistent femoral anteversion and internal tibial torsion together contribute to intoeing gait (feet turned inwards) in children with CP.
The main orthopaedic issues in children with CP are:
Muscle shortening
Joint contractures
Bony torsion
Medications
Medications that can lessen the tightness of muscles may be used to improve functional abilities, treat pain and manage complications related to spasticity. It’s important to talk about the risk of drug treatments with your doctor and discuss whether medical treatment is appropriate for your child’s needs. The selection of medications depends on whether the problem affects only certain muscles (isolated) or the whole body (generalized).
Focal spasticity
Generalized spasticity
Therapies
A variety of nondrug therapies can help a person with cerebral palsy to enhance functional abilities. These include the following:
Physical therapy: Muscle training and exercises may help your child’s strength, flexibility, balance, motor development and mobility. Braces or splints may be recommended for your child. Some of these supports are used to help with function, such as improved walking. Others may stretch stiff muscles to help prevent contractures.
Occupational therapy: Using alternative strategies and adaptive equipment, occupational therapists work to promote your child’s independent participation in daily activities and routines in the home, the school and the community.
Speech therapy: Speech therapists help improve your child’s ability to speak clearly or to communicate using sign language. They can also teach your child to use special communication devices — such as a board covered with pictures of everyday items and activities. Sentences can be constructed by pointing to the pictures. Speech therapists may also address difficulties with muscles used in eating and swallowing.
Surgical or other procedures
Surgery may be needed to lessen muscle tightness or correct bone abnormalities caused by spasticity. These treatments include:
Orthopaedic surgery: Children with severe contractures or deformities may need surgery on bones or joints to place their arms and legs in their correct positions. Surgical procedures can also lengthen muscles and tendons that are proportionally too short because of severe contractures. These corrections can lessen pain, improve mobility, and make it easier to use a walker, braces or crutches.
Severing nerves: In some severe cases, when other treatments haven’t helped, surgeons may cut the nerves serving the spastic muscles. This relaxes the muscle and reduces pain, but can also cause numbness.
For more information visit- https://www.uprightkidsortho.com/blog/managing-cerebral-palsy-in-children-a-doctor-explains/
Our website - https://www.uprightkidsortho.com/
Our other treatment-
Perthes disease- https://www.uprightkidsortho.com/perthes-disease/
Clubfoot – https://www.uprightkidsortho.com/clubfoot-or-congenital-talipes-equinovarus/
Leg length discrepancy- https://www.uprightkidsortho.com/leg-length-discrepancy/
#orthopedics #orthopedicsurgery #orthopedics #orthopedicsurgeon #surgery #surgeon #Doctorjayanth #Drjayanth #Doctorjayanthwhitefield
#orthopedics#orthopedicsurgery#orthopedicsurgeon#surgery#surgeon#Doctorjayanth#Drjayanth#Doctorjayanthwhitefield#drjayanth#doctorjayanth#bangalore#doctorjayanthwhitefield#pediatric
0 notes
Text
The fact that this is from 2018 means it's brand new in the world of cerebral palsy in aging adults, haha.
I was just researching how to write my ADHD character who develops spastic hypertonia and epilepsy after being dead twice. Since I was born like that, living that way always, I have to imagine the "oh shit" feeling of discovery. I think it's like when I was in my twenties and got the fibromyalgia diagnosis.
#writing fictional entities who represent my neuropsychology#my oc has my disabilities#if you want to write an autistic character please talk to autistic people#writing disabled characters#disabled mikey au#tmnt autistic headcanons
14 notes
·
View notes
Text
Special and Unique
Today’s prompt is about what makes your doll stand out, so I present my special needs girls, Annika, Cammie, and Zoe!
Zoe (pink hair) and Cammie (blonde) have prototype orthotics at the moment. Zoe’s is thin cardboard and duct tape, and Cammie has floral contact paper covering the cardboard sole of her “shoe”. Zoe needs another AFO and probably a back brace, but I’m waiting for Amazon to ship some pretty contact paper to finish them.
Cammie has Joss’ hearing aid since my former Joss doll is now an OC. It’s a tiny bit too big, but super glue works!

Annika is deaf due to repeated ear infections that went unnoticed as a toddler. She hears better in her left ear than her right, but still has trouble understanding anyone in a noisy area. She loves ballet, and dances by feeling the beat through the floor (her ballet studio has a live pianist in the old tradition) and memorizing the timing of each movement. She loves to read (especially with her aids out to better immerse herself in the story) and dreams of being a professional ballerina like her grandmother was.
Cammie and Zoe were adopted by their mom from foster care and are not biological sisters. Neither care, though, they adore each other and help take care of one another. Cammie has a limb difference, with her right leg shorter than her left, so she wears a thick-soled orthotic during the day. She was also born moderately deaf in her right ear and has ADHD. Cammie LOVES to swim, and is on a year-round swim team where her coaches have nicknamed her Baby Shark because chases after the other swimmers in her lane like she’s out to get them. Even though she’s only 6 and small for her age, she practices with the 7-8 year olds, and sometimes the 9-10s. A good swim practice helps her release pent up energy to relax and focus, so her mom takes her for Early Bird swim (at 5am!) every day before school. Mom works with Zoe on her swimming and hydrotherapy exercises while monitoring Cammie’s workout.
Zoe was born prematurely with ataxic cerebral palsy, so she has trouble with coordination and fine motor skills. She’s hypotonic, meaning she has low muscle tone, primarily in her legs and torso, so her mom (who’s a pediatric physical therapist) works with her on movement, and she does hydrotherapy to strengthen her body. Despite her motor and visual difficulties, Zoe is bold and outgoing, which can get her in trouble with her teachers. She loves science and is an excellent creative writer, dictating her stories to her computer, as her fingers can’t type fast enough to keep up with her mind.
20 notes
·
View notes
Text
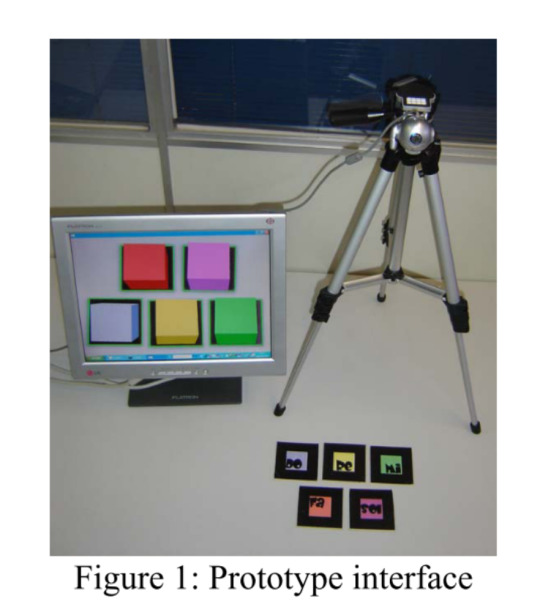
Week 8 Microcontroller 2
Potential User Settings:
1. Meditation
- Allowing users (mostly adults) to create soothing music and color blocks, helping them to relax
2. Learning
- Teaching kids about shapes (like the traditional shape block toys)
- Teaching kids about colors (using three primary colors, forming new colors on the screen)
- Encouraging kids to compose music and improve their creativity
Literature: Shapes + Music + Colors
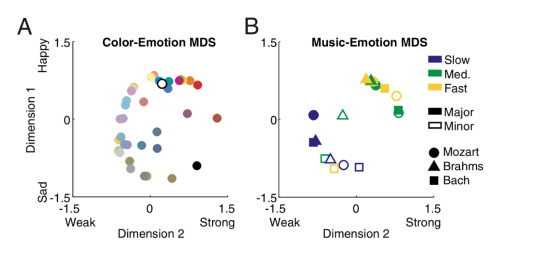
Previous literature has shown the direction associated between music and emotion and color and emotion. Also, Palmer et al. proposed that there are direct, unmediated associations between colors and musical sounds and the emotional mediation hypothesis that color and music are linked through shared emotional associations.
1. Palmer, S. E., Schloss, K. B., Xu, Z., & Prado-león, L. R. (2013). Music – color associations are mediated by emotion. https://doi.org/10.1073/pnas.1212562110
As people listen to music, they have emotional responses while listening to music and then pick colors with similar emotional content.
Faster music in the major mode was generally associated with more saturated, lighter, yellower colors, whereas slower music in the minor mode was associated with more desaturated (grayer), darker, bluer colors.
2. Grasielle, A., Corrêa, D., Ficheman, I. K., Sistemas, L. De, Politécnica, E., Paulo, D. S., … Brasil, S. P. (2009). Computer-Assisted Music Therapy : a Case Study of an Augmented Reality Musical System for Children with Cerebral Palsy Rehabilitation, 1–3. https://doi.org/10.1109/ICALT.2009.111
Facilitate music access to individuals with physical problems in their hands. The software adds to the real-world objects that simulate virtual music instruments. With the developed software application, it is not necessary to apply muscle strength neither to put adapters in the patient’s hands. Some patients have hypotonic hands and cannot keep their fingers bent over the keyboard or do not have enough muscle power to play percussion instruments.
Often the aid of music therapists is essential to develop musical activities. The music therapist made a plan of possible activities to be developed using the system in her interventions. Since it is based on a conventional computing platform, this system can be used at home.
3. Isbilen, E. S., & Krumhansl, C. L. (2016). The Color of Music : Emotion-Mediated Associations to Bach ’ s Well-Tempered Clavier, 26(2), 149–161.
Higher tones were associated with lighter colors and richer colors were associated with piano and string tones than were sine waves.
4 notes
·
View notes
Link
I don’t often post fundraisers, but these folks are good friends of mine and the American healthcare system is a joke. Jay was one of the few people I worked with who actually gave a shit when things were bad, and it hurts to see his young family going through this.
TW on the full GFM article for mild medical images. The TL;DR is that their 2-year old daughter was born with Congenital Hydrocephalus and is developing Quadriplegic Hypotonic Cerebral Palsy as a result of her seizures, and the medication she needs has some potentially severe side effects. Their 4-year old son has been diagnosed with EDS (Ehlers-Danlos Syndrome), and after he was diagnosed on the autism spectrum, insurance stopped covering any treatment related to his autism (like I said, the American healthcare system is a fucking joke). So the medical bills are racking up while they’re still trying to pay mortgage on a house and, yanno, eat.
In order to take care of the kids’ needs and get them to their weekly therapy sessions, Kristen has had to put off returning to work, which puts them even more out of pocket. Additionally, after William’s EDS diagnosis, both Jay and Kristen were tested and also found to have EDS (yes, both of them); they’ve had to cease their own treatment in order to focus on the kids.
I hate that things are so bad in this country that we have to turn towards strangers’ charity merely to survive, but that’s where we’re at. If you can’t donate, please consider sharing this post instead.
9 notes
·
View notes
Text
Oh, modesty culture. As a good Christian girl I wore my jeans "too tight" and I remember getting comments on it frequently. It turns out I was wearing them tight as compression garments.
#ex christian#religious trauma#ex fundamentalist#ex religious#ex evangelical#heds#hypermobile spectrum disorder#hyperflexibilitydisorders#erlos danlos#hypotonic cerebral palsy#hypotonia
17 notes
·
View notes
Text
A group of disorders that impair balance, movement and muscle tone is called cerebral palsy or CP. From the word “cerebral” it can be understood that the disorder is related to the brain and “palsy” means weakness or muscle disorder.Cerebral palsy affects the area of the brain that controls the ability to use muscles. When part of the brain is not developing as it is supposed to be cerebral palsy happens. It can also affect congenitally that means the brain is damaged right from birth or very early in life. Majority of people with cerebral palsy have that disorder right from birth, but it can also happen after birth, in that case it is called “acquired” cerebral palsy.There is the mild problem of muscle control in people affected with cerebral palsy. If the disease condition is chronic they will not be able to walk. Speaking problem can also be seen in people affected with cerebral palsy. Intellect can also be affected by this condition, though many have normal intelligence.When a child is diagnosed with cerebral palsy, the diagnoses include both brain injury and muscle problem.To get a better picture as to how brain damage has impacted one’s overall mobility, cerebral palsy is divided into different types. Movement issues and the body part(s) being affected are the two principal factors based on which cerebral palsy is categorized. Cerebral palsy is mainly four types – spastic, athetoid, ataxic and mixed type.Let us go into each one in detail.SPASTIC CEREBRAL PALSYIt is the most widely found cerebral palsy accounting for 70 to 80 percent of the cases. People affected with spastic cerebral palsy often have exaggerated or jerky moves. Damage in the brain’s motor cortex triggers spastic cerebral palsy. It is also triggered by damage to pyramidal tracts which help transmit signals to the muscles. This is why spastic cerebral palsy is also called pyramidal cerebral palsy. The motor cortex is located on the both sides of the brain and the pyramidal tracts connect each side of the motor cortex. Damage to the left side of the motor cortex causes movement issues on the right side of the body and vice versa.General symptoms associated with this condition include:Awkward reflexes
Stiffness in one part of the body
Contractures (permanently tightened muscles or joints)
Abnormal gait
ATHETOID CEREBRAL PALSYAround 10% of the cerebral palsy found in children is attributed to this type. It is also called non-spastic cerebral palsy. In this type the muscle tone fluctuates between being hypertonic and hypotonic. Involuntary movements in the face, torso and limbs are the tell-tale signs of athetoid cerebral palsy.This type of cerebral palsy is caused when brain’s basal ganglia and/or cerebellum is damaged. The basal ganglia are responsible for controlling motor function and eye movements, while the cerebellum controls balance and coordination.Athetoid cerebral palsy is also called “extrapyramidal” as the extrapyramidal tracts in the brain help control involuntary reflexes.General symptoms associated with this condition include:Stiff or rigid body
Floppiness in the limbs
Problems with posture
Feeding issues
ATAXIC CEREBRAL PALSYAtaxic cerebral palsy affects balance and coordination. It accounts for only a small portion of all cerebral palsy cases. Those inflicted with this condition typically have issues surrounding voluntary movement.Ataxic cerebral palsy is not like other types of cerebral palsy because it is majorly caused by damage to the cerebellum, which controls balance and coordination. People with this condition often have tremors and a reduction in muscle tone.General symptoms associated with this condition include:Difficulty speaking
Problems with depth perception
Shakiness and tremors
Spreading feet apart when walking
MIXED CEREBRAL PALSYAt times damage of the brain is not confined to one location. In these settings, it is possible for a child to develop cerebral palsy that is characteristic of multiple brain injuries.When a child is showing symptoms of more than one type of cerebral palsy, it is considered to be mixed cerebral
palsy. Ironically, mixed cerebral palsy accounts for only less than 10% of all CP cases.The commonly found mixed cerebral palsy diagnosis is a combination of spastic and athetoid cerebral palsy. Parents should seek professional opinion from cerebral palsy specialists if they suspect more than one type of cerebral palsy are afoot.General symptoms associated with this condition include:Muscle tone that could be stiffer or looser than normal, leading to impaired or involuntary movements
Difficulty performing fine motor skills
Tremors or shaking
Balancing difficulty
Seizures
Visual or hearing impairment
Severity of the condition is dependent on the extent of the patient’s brain injuries. While the condition does not progress over time, symptoms may become more pronounced as the patient ages.
РЕКЛАМА
0 notes
Text
Hypotonic cerebral palsy Marcy moment
#anphibia#amphiba#marcy regina wu#marcy my beloved#marcy wu#marcy amphibia#amphibia marcy#cerebral palsy
69 notes
·
View notes
Link
0 notes
Text
Cerebral Palsy Treatment Market Growth Analysis 2021-2027
Worldwide Cerebral Palsy Treatment Market Forecast, Trend Analysis and Opportunity Assessment 2021-2026, Covid 19 Outbreak Impact research report added by Report Hive, is an inside and out investigation of market attributes, size and development, division, territorial and nation breakdowns, serious scene, pieces of the pie, patterns and techniques for this market. It follows the market's notable and gauge market development by topography. It puts the market inside the setting of the more extensive Cerebral Palsy Treatment market, and contrasts it and different business sectors., market definition, territorial market opportunity, deals and income by locale, producing cost examination, Industrial Chain, market impact factors investigation, Cerebral Palsy Treatment market size conjecture, market information and Graphs and Statistics, Tables, Bar and Pie Charts, and a lot more for business knowledge. Get total Report (Including Full TOC, 100+ Tables and Figures, and Chart). – top to bottom Analysis Pre and Post COVID-19 Market Outbreak Impact Analysis and Situation by Region.
Request For View Sample Cerebral Palsy Treatment Market Report Page @ https://www.crystalmarketresearch.com/report-sample/HC0114518
Key Player analyzed in the Global Cerebral Palsy Treatment Market Report:
ALLERGEN PLC
CELLULAR BIOMEDICINE GROUP
MERCK & CO INC
PFIZER INC.
GLAXOSMITHKLINE PLC
ABBOTT LABORATORIES
ACORDA THERAPEUTICS INC.
MEDTRONIC
MERIDIGEN BIOTECH CO. LTD.
GW PHARMACEUTICALS PLC.
CEREBRAL PALSY TREATMENT MARKET
Continue...
Reasons for buying this report:
It offers an investigation of changing serious situation.
For settling on educated choices in the organizations, it offers logical information with key arranging strategies.
It offers a seven-year appraisal of Global Cerebral Palsy Treatment Market.
It helps in understanding the significant key item portions.
Specialists illuminate the elements of the market like drivers, restrictions, patterns, and openings.
It offers the provincial investigation of Global Cerebral Palsy Treatment Market alongside the business profiles of a few partners.
It offers gigantic information about moving elements that will impact the advancement of the Global Cerebral Palsy Treatment Market.
Prominent Points in Cerebral Palsy Treatment Market Businesses Segmentation:
Cerebral Palsy Treatment Market, ByType Estimates and Business Forecast 2016-2027
Spastic Cerebral Palsy
Dyskinetic Cerebral Palsy
Hypotonic Cerebral Palsy
Ataxic Cerebral Palsy
Other
Cerebral Palsy Treatment Market, ByTreatment Estimates and Business Forecast 2016-2027
Therapy
Medication
Other
Cerebral Palsy Treatment Market
Key Questions Covered In the Report
What is the all out market estimation of the Cerebral Palsy Treatment Market report?
What might be the conjecture time frame in the market report?
What is the market estimation of the Cerebral Palsy Treatment Market in 2021?
What is the Key Industry Leader's assessment for the Cerebral Palsy Treatment?
Which is the base year determined in the Cerebral Palsy Treatment Market Report?
What are the critical patterns in the Cerebral Palsy Treatment Market Report?
What are the market esteems/development % of arising nations?
Which market holds the most extreme piece of the overall industry of the Cerebral Palsy Treatment Market?
Promising Regions & Countries Mentioned In The Cerebral Palsy Treatment Market Report::
North America Region
Europe Region
Asia-Pacific Region
South America Region
The Middle East & Africa Region
Do Inquiry Before Purchasing Market Cerebral Palsy Treatment Report Here @https://www.crystalmarketresearch.com/send-an-enquiry/HC0114518
Contacts Us:
Crystal Market Research
Sherry | APAC Marketing Division: Level 23-1
Premier Suite, Mont Kiara, 50480 Kuala
Lumpur, Malaysia
E-mail: [email protected]
0 notes
Text
Which physical findings are characteristic of cerebral palsy?
And this is all stuff we knew absolutely nothing about when I was young...
3 notes
·
View notes