#Beth Israel Deaconess Medical Center
Text
MIT scientists use a new type of nanoparticle to make vaccines more powerful
New Post has been published on https://thedigitalinsider.com/mit-scientists-use-a-new-type-of-nanoparticle-to-make-vaccines-more-powerful/
MIT scientists use a new type of nanoparticle to make vaccines more powerful


Many vaccines, including vaccines for hepatitis B and whooping cough, consist of fragments of viral or bacterial proteins. These vaccines often include other molecules called adjuvants, which help to boost the immune system’s response to the protein.
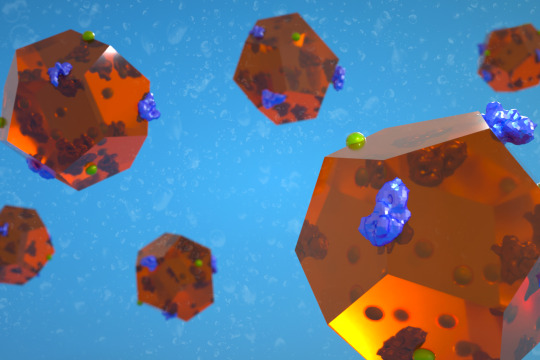
Most of these adjuvants consist of aluminum salts or other molecules that provoke a nonspecific immune response. A team of MIT researchers has now shown that a type of nanoparticle called a metal organic framework (MOF) can also provoke a strong immune response, by activating the innate immune system — the body’s first line of defense against any pathogen — through cell proteins called toll-like receptors.
In a study of mice, the researchers showed that this MOF could successfully encapsulate and deliver part of the SARS-CoV-2 spike protein, while also acting as an adjuvant once the MOF is broken down inside cells.
While more work would be needed to adapt these particles for use as vaccines, the study demonstrates that this type of structure can be useful for generating a strong immune response, the researchers say.
“Understanding how the drug delivery vehicle can enhance an adjuvant immune response is something that could be very helpful in designing new vaccines,” says Ana Jaklenec, a principal investigator at MIT’s Koch Institute for Integrative Cancer Research and one of the senior authors of the new study.
Robert Langer, an MIT Institute Professor and member of the Koch Institute, and Dan Barouch, director of the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center and a professor at Harvard Medical School, are also senior authors of the paper, which appears today in Science Advances. The paper’s lead author is former MIT postdoc and Ibn Khaldun Fellow Shahad Alsaiari.
Immune activation
In this study, the researchers focused on a MOF called ZIF-8, which consists of a lattice of tetrahedral units made up of a zinc ion attached to four molecules of imidazole, an organic compound. Previous work has shown that ZIF-8 can significantly boost immune responses, but it wasn’t known exactly how this particle activates the immune system.
To try to figure that out, the MIT team created an experimental vaccine consisting of the SARS-CoV-2 receptor-binding protein (RBD) embedded within ZIF-8 particles. These particles are between 100 and 200 nanometers in diameter, a size that allows them to get into the body’s lymph nodes directly or through immune cells such as macrophages.
Once the particles enter the cells, the MOFs are broken down, releasing the viral proteins. The researchers found that the imidazole components then activate toll-like receptors (TLRs), which help to stimulate the innate immune response.
“This process is analogous to establishing a covert operative team at the molecular level to transport essential elements of the Covid-19 virus to the body’s immune system, where they can activate specific immune responses to boost vaccine efficacy,” Alsaiari says.
RNA sequencing of cells from the lymph nodes showed that mice vaccinated with ZIF-8 particles carrying the viral protein strongly activated a TLR pathway known as TLR-7, which led to greater production of cytokines and other molecules involved in inflammation.
Mice vaccinated with these particles generated a much stronger response to the viral protein than mice that received the protein on its own.
“Not only are we delivering the protein in a more controlled way through a nanoparticle, but the compositional structure of this particle is also acting as an adjuvant,” Jaklenec says. “We were able to achieve very specific responses to the Covid protein, and with a dose-sparing effect compared to using the protein by itself to vaccinate.”
Vaccine access
While this study and others have demonstrated ZIF-8’s immunogenic ability, more work needs to be done to evaluate the particles’ safety and potential to be scaled up for large-scale manufacturing. If ZIF-8 is not developed as a vaccine carrier, the findings from the study should help to guide researchers in developing similar nanoparticles that could be used to deliver subunit vaccines, Jaklenec says.
“Most subunit vaccines usually have two separate components: an antigen and an adjuvant,” Jaklenec says. “Designing new vaccines that utilize nanoparticles with specific chemical moieties which not only aid in antigen delivery but can also activate particular immune pathways have the potential to enhance vaccine potency.”
One advantage to developing a subunit vaccine for Covid-19 is that such vaccines are usually easier and cheaper to manufacture than mRNA vaccines, which could make it easier to distribute them around the world, the researchers say.
“Subunit vaccines have been around for a long time, and they tend to be cheaper to produce, so that opens up more access to vaccines, especially in times of pandemic,” Jaklenec says.
The research was funded by Ibn Khaldun Fellowships for Saudi Arabian Women and in part by the Koch Institute Support (core) Grant from the U.S. National Cancer Institute.
#aluminum#antigen#Beth Israel Deaconess Medical Center#Cancer#cell#Cells#chemical#Chemical engineering#covid#covid 19#cytokines#defense#drug#drug delivery#experimental#framework#hepatitis#how#immune cells#immune response#immune system#inflammation#Israel#it#Koch Institute#LED#macrophages#Manufacturing#medical#metal
0 notes
Text
It’s scariant season—again.
A new offshoot of Omicron, BA.2.86—nicknamed Pirola—has popped up in Israel, the US, South Africa, and the UK after it was first recorded in Denmark in late July. Pirola initially set off alarm bells because it was spotted in four countries at the same time—and because, having majorly curtailed our viral surveillance systems, we don’t know how long it’s been making the rounds. Plus, the sheer number of mutations it has was reason enough to be spooked—BA.2.86 boasts more than 30 new mutations, compared to the most recently dominant variant, XBB.1.5.
“The only other time we’ve seen such a large genetic shift was the initial transition from Delta to Omicron, which led to the most hospitalizations and the most deaths of any surge in the pandemic,” says Dan Barouch, head of the vaccine research division at Beth Israel Deaconess Medical Center in Boston. As a result, scientists across the world are scrambling to figure out whether BA.2.86 is indeed something to worry about.
Early studies suggest that Pirola isn’t much better at evading immunity than previous variants, despite all of its mutations. The protection offered by vaccines should hold up, and if you’ve been naturally exposed to the XBB variant, you should be better equipped to fight off this new variant.
Why is Pirola not very good at evading immunity, despite having undergone so many mutations? It’s likely that it evolved from BA.2, an older, more familiar form of Sars-CoV-2 that’s no longer circulating today, meaning that Pirola is less resistant to neutralization than more recent variants, such as XBB.1.5. But it’s possible that the variant may continue to evolve and change, Barouch warns, so staying vigilant will be key.
Determing whether it will take off and become the dominant form of the virus in circulation will require a “wait-and-see” approach, Barouch adds. “However, it does not appear to be spreading at the same pace as, say, the original BA.1 or BA.5,” he says, referring to two of the Omicron variants that spread particularly quickly.
Anna Bershteyn, an assistant professor and colead of the Covid modeling team at the NYU Grossman School of Medicine, agrees: so far, so reassuring. “As far as we know, it doesn’t seem likely that this is going to be one of these huge waves of hospitalizations and deaths, the kind that have overwhelmed the health system in prior epidemic waves.”
In the UK, a care home in the east of England was invaded by the variant: 33 residents caught Covid, with 28 definitely infected with BA.2.86—suggesting that it’s pretty easily transmitted. But only two hospitalizations have been reported, which hints that Pirola doesn’t cause more severe disease than existing variants.
In certain parts of the world, its appearance has sparked action in the form of hastened booster programs. In the UK, the booster kick-off was rescheduled from October to within the next few weeks. In the US, the latest round of boosters is expected to be approved by the Food and Drug Administration very soon (although who should get one remains a source of debate). The findings of a recent preprint suggest that Moderna’s XBB.1.5 booster seems to work well against the BA.2.86 variant.
But while BA.2.86 may not yet be spreading rampantly, a Covid wave is indeed unfurling, with cases once again rising. In the US, hospitalizations are up, although they’re still nowhere near the sky-high levels they were at this time last year. Cases are also mushrooming in the UK and in Europe.
For now, BA.2.86’s spread is shaping up to be nothing like the Omicron wave that rocketed across the world at the end of 2021—the last time we saw such a big raft of Covid mutations appear. As one scientist put it, Pirola may be a “real nothingburger.”
11 notes
·
View notes
Text
Jazmin Evans had been waiting for a new kidney for four years when her hospital revealed shocking news: She should have been put on the transplant list in 2015 instead of 2019 — and a racially biased organ test was to blame.
As upsetting as that notification was, it also was part of an unprecedented move to mitigate the racial inequity. Evans is among more than 14,000 Black kidney transplant candidates so far given credit for lost waiting time, moving them up the priority list for their transplant.
“I remember just reading that letter over and over again,” said Evans, 29, of Philadelphia, who shared the notice in a TikTok video to educate other patients. “How could this happen?”
At issue is a once widely used test that overestimated how well Black people’s kidneys were functioning, making them look healthier than they really were — all because of an automated formula that calculated results for Black and non-Black patients differently. That race-based equation could delay diagnosis of organ failure and evaluation for a transplant, exacerbating other disparities that already make Black patients more at risk of needing a new kidney but less likely to get one.
A few years ago, the National Kidney Foundation and American Society of Nephrology prodded laboratories to switch to race-free equations in calculating kidney function. Then the U.S. organ transplant network ordered hospitals to use only race-neutral test results in adding new patients to the kidney waiting list.
“The immediate question came up: What about the people on the list right now? You can’t just leave them behind,” said Dr. Martha Pavlakis of Boston’s Beth Israel Deaconess Medical Center and former chair of the network’s kidney committee.
Pavlakis calls what happened next an attempt at restorative justice: The transplant network gave hospitals a year to uncover which Black kidney candidates could have qualified for a new kidney sooner if not for the race-based test — and adjust their waiting time to make up for it. That lookback continues for each newly listed Black patient to see if they, too, should have been referred sooner.
Between January 2023 and mid-March, more than 14,300 Black kidney transplant candidates have had their wait times modified, by an average of two years, according to the United Network for Organ Sharing, which runs the transplant system. So far more than 2,800 of them, including Evans, have received a transplant.
But it’s just one example of a larger problem permeating health care. Numerous formulas or “algorithms” used in medical decisions — treatment guidelines, diagnostic tests, risk calculators — adjust the answers according to race or ethnicity in a way that puts people of color at disadvantage.
Given how embedded these equations are in medical software and electronic records, even doctors may not realize how widely they impact care decisions.
“Health equity scholars have been raising alarm bells about the way race has been misused in clinical algorithms for decades,” said Dr. Michelle Morse, New York City’s chief medical officer.
Change is beginning, slowly. No longer are obstetricians supposed to include race in determining the risk of a pregnant woman attempting vaginal birth after a prior C-section. The American Heart Association just removed race from a commonly used calculator of people’s heart disease risk. The American Thoracic Society has urged replacing race-based lung function evaluation.
The kidney saga is unique because of the effort to remedy a past wrong.
“Lots of time when we see health inequities, we just assume there’s nothing we can do about it,” Morse said. “We can make changes to restore faith in the health system and to actually address the unfair and avoidable outcomes that Black people and other people of color face.”
Black Americans are over three times more likely than white people to experience kidney failure. Of the roughly 89,000 people currently on the waiting list for a new kidney, about 30% are Black.
Race isn’t a biological factor like age, sex or weight — it’s a social construct. So how did it make its way into calculations of kidney function?
The eGFR, or estimated glomerular filtration rate, evaluates kidney health based on how quickly a waste compound called creatinine gets filtered from blood. In 1999, an equation used to calculate eGFR was modified to adjust Black people’s results compared to everyone else’s, based on some studies with small numbers of Black patients and a long-ago false theory about differences in creatinine levels. Until recently that meant many lab reports would list two results — one calculated for non-Black patients and another for Black patients that could overestimate kidney function by as much as 16%.
Not every Black kidney candidate was affected. Some may have had kidney failure diagnosed without that test. For others to have a chance at benefitting from UNOS’ mandated lookback, transplant center staff-turned-detectives often worked after hours and weekends, hunting years-old records for a test that, recalculated without the race adjustment, might make the difference.
“You’re reaching out to the nephrologist, their primary care doctors, the dialysis units to get those records,” said Dr. Pooja Singh of Jefferson Health’s transplant institute in Philadelphia, where Evans received her new kidney. “That first patient getting transplanted for us was such a great moment for our program that the work didn’t feel like work after that.”
A high school sports physical first spotted Evans’ kidney disease at age 17. While finishing her master’s degree and beginning to earn her Ph.D. at Temple University, she started dialysis — for nine hours a night while she slept — and was placed on the transplant list.
How long it takes to get a kidney transplant depends on patients’ blood type, medical urgency and a mix of other factors — including how long they’ve spent on the waiting list. Evans was first listed in April 2019. When the Jefferson transplant center unearthed her old lab tests, they found she should have qualified in September 2015.
“Just for context, when I was still an undergrad I should have been on the list,” she said, recalling the anger she felt as she read the letter. What she called “a mind-blowing” credit of 3½ more years waiting also provided “a glimmer of hope” that she’d be offered a matching kidney soon.
Evans got a new kidney on July 4 and is healthy again, and grateful the policy change came in time for her.
“You don’t know if people would be alive today” if it had been enacted earlier, she said. Still, that extra step of “making amends to fix the situation for those that we can — I feel like it’s very important and it’s very necessary if you’re truly wanting to bring more equity and equality into the medical field.”
#us politics#news#ap#2024#the associated press#kidney transplant#racial bias#us healthcare#eGFR#estimated glomerular filtration rate#transplant surgery
4 notes
·
View notes
Text
1-Harvard University
Harvard University is the nation's oldest college and university. Most of its understudies learn at the alumni level, and over 20% of its understudies are worldwide. In addition to its Cambridge campus, Harvard has facilities like the Harvard Medical School in Boston, Massachusetts. The university has the biggest endowment of any educational institution in the world. More than one hundred Harvard research centers house research in a variety of fields.

The university includes the undergraduate college as well as 11 other degree-granting institutions, including the prestigious Business School, Graduate School of Education, Law School, and John F. Kennedy School of Government. The medical school is associated with a number of teaching hospitals, including Beth Israel Deaconess Medical Center and Brigham and Women's Hospital. The most popular undergraduate majors at Harvard are psychology, history, mathematics, and social sciences/biological sciences. English is the language of guidance at the college, and the semester-based scholarly schedule is set up. The majority of undergraduates live on campus for the entire four years, beginning as freshmen in one of twelve undergraduate houses and continuing their education in one of those houses. Some universities offer housing options for graduate students. With more than 70 libraries and approximately 19 million volumes, the Harvard Library is the largest academic library in the world.
2-Massachusetts Institute of Technology
The Massachusetts Foundation of Innovation was laid out in 1861 and is arranged in Cambridge, Massachusetts, near Boston. The college has approximately 11,000 understudies, with approximately 60% of them studying at the alumni level. At MIT, there are five schools: design and construction; engineering; humanities, arts, and social sciences; management; and studies. English is used in instruction at MIT. The academic calendar is a 4-1-4 structure, with a "Free Exercises Period" in January that lasts for four weeks. Participants in discussions, address series, presentations, and other exceptional activities include undergraduate and graduate students, staff, and graduates.

Just first-year college understudies are expected to live nearby, however numerous understudies who are further along in their schooling additionally decide to do as such. One of the largest university research reactors in the United States is the MIT Nuclear Reactor Laboratory. By the time they graduate, nearly ninety percent of MIT undergraduates participate in the Undergraduate Research Opportunities Program, which pairs students and faculty for research projects. There are various open doors for undergrad and graduate understudies to acquire research insight at one of MIT's numerous labs or focuses. In the new year, more than $675 million was spent on research at MIT, with additional government funding going to the Lincoln Lab, a Branch of Protection innovative work lab focused on mechanical solutions to public safety issues.
3-Stanford University
Stanford College was founded in 1885 and is located in the Narrows Region of California, approximately 30 miles south of San Francisco. The majority of students apply to graduate programs. The college is made up of seven schools, many of which are particularly well-suited for research at the graduate level. There are three institutions that provide graduates with degrees: humanities and sciences; sciences of nature; likewise technology. Just alumni level degrees are presented by the schools of training, regulation, business, and medication. English is the language of instruction at Stanford, where the quarter-based academic calendar is followed.
Worldwide, approximately 8% of undergraduate students and 30% of alumni students are international. Over ninety percent of undergraduates live on campus, and freshman housing is guaranteed for four years. Stanford also provides housing for the first year to new graduate students. Over 60% of graduate students and 30% of faculty members reside on campus. The 20 libraries that are supported by Stanford's library system contain more than 9.3 million physical volumes. Over $1 billion has been given to Stanford for research, including money from the federal government for projects at the Stanford-run SLAC National Accelerator Laboratory. Each year, approximately 3,400 scientists from all over the world make use of the facilities at SLAC. Up of 1,000 consistent papers considering assessment drove at the lab are dispersed consistently.
4-University of California Berkeley
The College of California, Berkeley is located in the Sound Region, about 15 miles from San Francisco. The public university, also known as Cal or Berkeley, was established in 1868. Over seventy percent of Berkeley students intend to earn an undergraduate degree. Among the university's 14 colleges and schools are the highly regarded Haas School of Business, College of Chemistry, College of Engineering, School of Public Health, and School of Law. English is the language of guidance and the scholastic schedule depends on semesters.
UC Berkeley offers approximately 350 degree programs. Computer science and electrical engineering have been among Berkeley's most popular undergraduate majors; economics; political analysis; management of the business; psychology, and approximately 25% of undergraduates, including 95% of freshmen, live on campus. Some graduate students opt to live off campus, while others choose to live in housing owned by the university. Out-of-state students pay more for tuition and fees, and international students make up about 15% of the student body. Every year, around 3,000 worldwide researchers go after transitory educating or research jobs at Berkeley. Berkeley uses some of the school's museums and biological field stations, which are managed by the university, for research in addition to the labs and research centers of academic departments. At the remote field station areas, investigations of environments, ranger service, natural science, and zoology are led. Berkeley researchers discovered Californium and Berkelium, two elements on the periodic table.
5-University of Oxford
Despite the fact that the precise date of establishment of the University of Oxford is unknown, the institution's history goes back at least to 1096. Oxford is about 60 miles northwest of London, and approximately 45% of its undergraduates are graduate students. The majority of Oxford alumni students conduct research as part of their studies. Research is carried out by each of Oxford's four academic divisions: humanities; sciences of life, matter, and mathematics; medical specialties; and the humanities The Oxford academic year is divided into three eight-week terms: Michaelmas, Hilary, and Trinity are celebrated in the summer. At the university, instruction is conducted in English.

The University of Oxford is a central university; 38 colleges; and six Permanent Private Halls, which are typically smaller than colleges and typically offer fewer subjects. There is a dining hall, a common room, and a library in each Oxford college. Undergraduate students are provided with housing for the first year of their education, and they frequently have the option of continuing their education in the same building. Even though graduate students aren't required to live on campus, some schools may have rooms available for them during their first year, especially for international students. Tuition is more expensive for non-EU students. The university, its academic departments and colleges, and dozens of outside organizations have offered over 900 graduate student scholarships.
6-University of Washington Seattle
The College of Washington is a public organization that was established in 1861. The oldest and most populous campus of the school is in Seattle, the largest city in Washington. The university added two smaller campuses in Tacoma, Washington, and Bothell, Washington, in 1990. Around 70% of the college's understudies - across each of the three grounds - learn at the undergrad level. Nevertheless, the large university provides over 370 graduate programs. Educational cost costs are higher for non-Washington-state inhabitants, and college lodging is accessible for both undergrad and graduate understudies. The academic calendar at UW is quarter-based, and English is the language of instruction.

The university has 16 colleges and schools that offer courses in a variety of fields, including social work, engineering, and the arts and sciences. The College of Education, the School of Nursing, and the School of Medicine are among its highly regarded graduate schools. In a number of specialties, the University of Washington Medical Center, a teaching hospital, ranks highly. The college offers a local area based clinical training program that permits understudies to finish clinical pivots in various states all through the district - Gold country, Idaho, Montana, Washington and Wyoming. The program aims to hire more primary care doctors, particularly in rural areas. In recent years, the University of Washington has received more than $1 billion in research grants and operates more than 280 specialized research centers. The West Coast Poverty Center, the Polar Science Center, and the Center for Emerging and Re-emerging Infectious Diseases are among these research centers.
7-Columbia University
Columbia University is a private university that was established in 1754. It is in the Manhattan borough of New York City's Upper West Side. The school changed its name in 1896 from King's College to its current title. At Columbia, about 30% of undergraduate students are international, and almost 30% of all students are from other countries. Over ninety percent of undergraduates live on campus, and graduate students can also find some university housing. The academic year at Columbia is divided into semesters, and English is the language of instruction.
Columbia College, the Fu Foundation School of Engineering and Applied Science, and the School of General Studies are the three undergraduate schools that make up the university, as are numerous graduate and professional schools. The College of Physicians and Surgeons, the Business School, and the Law School are among Columbia University's highly regarded graduate programs. Additionally, Columbia is associated with Jewish Theological Seminary, Union Theological Seminary, and Barnard College for Women. A university teaching hospital is the highly regarded New York-Presbyterian University Hospital of Columbia and Cornell. In more than 200 university centers and institutes, Columbia faculty and students conduct research in the sciences, humanities, and social sciences. Additionally, Columbia has established global centers in Jordan's Amman; Beijing; India's Mumbai; Paris; Istanbul; Nairobi, Kenya; Chile's Santiago; and Rio de Janeiro to make it easier for students to study abroad and do research.
8-University of Cambridge
The University of Cambridge was founded in 1209 and is about 60 miles north of London. More than 35% of the university's approximately 19,000 students are enrolled in graduate programs. Six schools exist: humanities and the arts; natural sciences; medical practice; social sciences and the humanities; actual sciences; likewise technology. These schools are made up of dozens of academic departments and other divisions. The scholarly schedule at Cambridge is partitioned into three terms - Michaelmas (fall), Loaned (winter) and Easter (spring). At the university, instruction is conducted in English.
There are 31 residential colleges in Cambridge that are in charge of admitting undergraduate and graduate students; three schools - Lucy Cavendish School, Murray Edwards School and Newnham School - are ladies as it were. The colleges also provide undergraduates with some instruction in small groups. Housing at the University of Cambridge is covered for at least three years for the majority of undergraduate students. Additionally, college housing is available to many new graduate students. About 20% of the students come from countries outside the European Union; Non-EU students pay more for tuition, which varies by field of study. Cambridge has in excess of 100 libraries, including school and division libraries. The college has around 140 focuses and establishes that add to various areas of examination, like the Focal point of African Investigations; the Cambridge Institute for Public Policy and Economics; and the Institute of Theoretical Geophysics, respectively. The university received approximately $415 million in research grants and contracts in the most recent year.
9-California Institute of Technology
previously known as Throop University, the California Institute of Technology (Caltech) was established in 1891 and changed its name in 1920. The school in Pasadena, California, which focuses on science and engineering, is about 11 miles northeast of Los Angeles. At Caltech, there are approximately 2,200 students, 55% of whom are pursuing graduate degrees. At 3:1, the student-to-faculty ratio is extremely low. International students make up more than a quarter of Caltech's total enrollment. The school uses the quarter system for its academic calendar, and English is the language of instruction.
There are six academic divisions at Caltech, many of which have prestigious graduate programs: biology and the science of biology; chemistry and the engineering of chemicals; applied engineering and science; earth and space sciences; social sciences and the humanities; and astronomy, mathematics, and physics. Housing is provided for all first-year undergraduate and graduate students by the university. There are eight undergraduate houses, each with its own government and unique traditions, as opposed to the typical undergraduate residence halls found at many universities in the United States. The Catalina Apartments on campus are reserved first for newly admitted graduate students.
During their time at Caltech, about 80% of undergraduates participate in research. Students can participate in the university's Summer Undergraduate Research Fellowships program, in which they write research proposals, work with mentors, and present their projects. Caltech has around 50 exploration establishments and focuses, for example, the Resnick Manageability Foundation and the Tectonics Observatory. In addition, the university manages NASA's Jet Propulsion Laboratory, which is a center for robotic exploration of the solar system that engages students and faculty alike.
10-Johns Hopkins University
The private Johns Hopkins University was established in 1876. The school has campuses in China, Italy, and the area around Baltimore and the District of Columbia. The Homewood campus in north Baltimore serves as the primary undergraduate campus. The academic calendar at the majority of the university's schools is based on the semester, with some schools providing an additional three-week study period in January. English is the language of guidance. College understudies are expected to live in college lodging for the initial two years of their examinations. Graduate students, with the exception of those enrolled in the conservatory's Peabody Institute, are not eligible for accommodations.
The university has nine academic divisions that offer courses in engineering, business, education, medicine, nursing, music, public health, international studies, and the arts and sciences. At the Homewood campus, public health studies, international studies, and biomedical engineering are among the most popular undergraduate majors. The School of Education, School of Nursing, and School of Medicine at Johns Hopkins University are among the university's top graduate programs. Numerous specialties rank highly at the teaching hospital Johns Hopkins. Initiatives like the Provost's Undergraduate Research Awards program, which provides funding for students to design and carry out research with the assistance of a faculty sponsor, support undergraduate research participation. The Johns Hopkins University Applied Physics Laboratory, an affiliated research center that serves as a hub for space- and national security-related research, is one of the institution's research facilities.
Thanks for reading
2 notes
·
View notes
Text
The Healing Wonders Of Meditation
youtube
The use of meditation for healing and spiritual enlightenment has been an ancient practice that is common among the world’s great religions and cultures. It is an accepted and proven alternative therapy that is classified under mind-body medicine.
Through the years, more and more people have found meditation as an effective way to ease chronic pain, improve heart health, relieve stress and anxiety, boost mood and immunity, and resolve pregnancy problems. Even doctors are already prescribing meditation as a way to lower blood pressure; improve exercise performance in people with angina; help people with asthma breathe easier; and to relieve insomnia. It is a safe and simple way to balance a person’s physical, emotional, and mental well-being.
According to cardiologist Herbert Benson, MD: Any condition that’s caused or worsened by stress can be alleviated through meditation. Benson is the founder of the Mind/Body Institute at Harvard Medical School’s Beth Israel Deaconess Medical Center. He said that the relaxation induced by meditation can help decrease metabolism, lower blood pressure, and improve heart rate, breathing, and brain waves. When the body receives a quiet message to relax, tension and tightness begin to seep from muscles.
Brain scans (or Magnetic Resonance Imaging, or MRI) of people who meditate have been used to show scientific evidence that meditation really works. It shows an increase in activity in areas that control metabolism and heart rate. Other studies on Buddhist monks have shown that meditation produces long-lasting changes in the brain activity in areas involving attention, working memory, learning, and conscious perception.
Meditation is not difficult to learn but it is a skill that needs to be practiced in order to develop the ability to focus on the breathing patterns and the need to ignore distracting thoughts. Meditation is usually accompanied by a mantra, a word or phrase that is repeatedly chanted to produce a biological response such as relaxation. The soothing power of repetition is at the heart of meditation. Constant practice of meditation allows people to learn anddevelop the ability to produce meditative and relaxed states without difficulty. Meditating several times during the day makes the practitioner feel relaxed throughout the entire day.
youtube
Benefits of Meditation
Heart Health: Countless studies have shown that regular practice has significantly helped reduce high blood pressure. A study conducted at the College of Maharishi Vedic Medicine in Fairfield, Iowa, showed significant lowering of blood pressure and heart rate in black adults. Another study conducted by the American Journal of Hypertension showed that teenagers who meditated for 15 minutes twice a day for four months were able to lower their blood pressure a few points.
Immune Booster: In a Psychosomatic Medicine study testing immune function, meditation has bben shown to be useful in warding off illness and infections. Flu shots were given to volunteers who had meditated for eight weeks and to people who didn’t meditate. The result of blood tests from the meditation group had produced higher levels of antibodies against the flu virus.
Women’s Health: Premenstrual syndrome (PMS), infertility problems, and even breastfeeding can be improved when women meditate regularly. In one study, PMS symptoms subsided by 58% when women meditated. Another study found that hot flashes were less intense among women who practiced meditation. Women struggling with infertility had much less anxiety, depression and fatigue following a 10-week meditation program; 34 percent became pregnant within six months. Also, new mothers who meditated on images of milk flowing from their breasts were able to more than double their production of milk.
Meditation Enhances Brain Activity
youtube
Those who practice meditation regularly showed evidence of significantly higher brain activity, called gamma wave activity, in areas associated with learning and happiness compared with those who didn’t practice meditation. Gamma waves involve mental processes including attention, memory, learning and conscious perception.
Many health care providers consider meditation as a key element of an integrated health program. However, when you are having a hard time getting into that meditative state, try to enroll in a class. It will help and guide you with your progress. Any practice that can evoke the relaxation response can be beneficial, be it through meditation, yoga, breathing, or repetitive prayer. The growing body of research literature on meditation and other alternative therapies gives us no reason to believe that one is better than the other.
#relaxing guitar music#guitar music#relaxing music#calming music#sleep music#guitar#stress relief music#meditation music#calm music#instrumental music#study music#acoustic guitar#ambient music#soft music#soothing music#classical guitar#concentration music#focus music#spanish guitar#relaxation music#instrumental guitar music#insomnia#stress relief#meditation#relax#romantic music#sleep#yoga#yoga music#study
3 notes
·
View notes
Text

Pregnancy may be one of the most surprising side effects for women taking weight loss medications.
Dubbed “Ozempic babies,” women are reporting on social media that they are becoming pregnant after using GLP-1 drugs like Ozempic (semaglutide) for weight loss.
“[I]ncreased fertility and surprise pregnancy has been well-reported in previously infertile patients, even with modest weight loss (approximately 5%) with lifestyle modification as well as other weight loss medications,” said Dr. Neha Lalani in a Healthline-related article.
One woman said that she started taking Mounjaro for weight loss. Over the first few months, she lost about 40 pounds. Her menstrual cycles, which had been irregular because of PCOS, became normal. And she even felt happier.
“It just made me feel like a whole new person,” she said. “I was in a better mood every single day. This same woman had hoped that losing weight might help her get pregnant. She’d heard about others having success with weight loss while taking the shot. Shortly after, she became pregnant—sooner than she expected!
Another woman admitted she was pregnant on Ozempic and was on the pill!
What’s going on with the Ozempic baby boom?
Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in women of reproductive age. PCOS causes the ovaries to produce an abnormal amount of androgens, which are male sex hormones. This can lead to hormonal imbalances, cysts in the ovaries, irregular periods, and infertility.
PCOS can make it difficult for women to lose weight, which could be why many are turning to weight loss medications for help. Are GLP-1 drugs able to boost fertility?
GLP-1 medications aid in weight loss and blood sugar management, which may improve the underlying factors that contribute to infertility. However, experts agree more research is needed to understand how GLP-1 medications can impact IVF outcomes.
In the meantime, numerous women are reporting that they're having “Ozempic babies” on social media. But the joy some experience in discovering pregnancies may come with anxiety about the unknowns, as these medicines haven’t been studied in people who are pregnant.
“We don’t know the effect of early exposure … on the fetus,” said Dr. Jody Dushay, a physician focused on endocrinology and metabolism at Beth Israel Deaconess Medical Center and an assistant professor at Harvard Medical School.
Dushay said she recommends that women stop taking these drugs two months before trying to get pregnant, as directed in their prescribing information.
0 notes
Text
Research Assistant II
Beth Israel Deaconess Medical Center, Harvard Medical School
Come join an adventurous team as a #ResearchAssistant
See the full job description on jobRxiv: https://jobrxiv.org/job/beth-israel-deaconess-medical-center-harvard-medical-school-27778-research-assistant-ii/?feed_id=73944
#ScienceJobs #hiring #research
0 notes
Text
MIT scientists use a new type of nanoparticle to make vaccines more powerful
New Post has been published on https://sunalei.org/news/mit-scientists-use-a-new-type-of-nanoparticle-to-make-vaccines-more-powerful/
MIT scientists use a new type of nanoparticle to make vaccines more powerful
Many vaccines, including vaccines for hepatitis B and whooping cough, consist of fragments of viral or bacterial proteins. These vaccines often include other molecules called adjuvants, which help to boost the immune system’s response to the protein.
Most of these adjuvants consist of aluminum salts or other molecules that provoke a nonspecific immune response. A team of MIT researchers has now shown that a type of nanoparticle called a metal organic framework (MOF) can also provoke a strong immune response, by activating the innate immune system — the body’s first line of defense against any pathogen — through cell proteins called toll-like receptors.
In a study of mice, the researchers showed that this MOF could successfully encapsulate and deliver part of the SARS-CoV-2 spike protein, while also acting as an adjuvant once the MOF is broken down inside cells.
While more work would be needed to adapt these particles for use as vaccines, the study demonstrates that this type of structure can be useful for generating a strong immune response, the researchers say.
“Understanding how the drug delivery vehicle can enhance an adjuvant immune response is something that could be very helpful in designing new vaccines,” says Ana Jaklenec, a principal investigator at MIT’s Koch Institute for Integrative Cancer Research and one of the senior authors of the new study.
Robert Langer, an MIT Institute Professor and member of the Koch Institute, and Dan Barouch, director of the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center and a professor at Harvard Medical School, are also senior authors of the paper, which appears today in Science Advances. The paper’s lead author is former MIT postdoc and Ibn Khaldun Fellow Shahad Alsaiari.
Immune activation
In this study, the researchers focused on a MOF called ZIF-8, which consists of a lattice of tetrahedral units made up of a zinc ion attached to four molecules of imidazole, an organic compound. Previous work has shown that ZIF-8 can significantly boost immune responses, but it wasn’t known exactly how this particle activates the immune system.
To try to figure that out, the MIT team created an experimental vaccine consisting of the SARS-CoV-2 receptor-binding protein (RBD) embedded within ZIF-8 particles. These particles are between 100 and 200 nanometers in diameter, a size that allows them to get into the body’s lymph nodes directly or through immune cells such as macrophages.
Once the particles enter the cells, the MOFs are broken down, releasing the viral proteins. The researchers found that the imidazole components then activate toll-like receptors (TLRs), which help to stimulate the innate immune response.
“This process is analogous to establishing a covert operative team at the molecular level to transport essential elements of the Covid-19 virus to the body’s immune system, where they can activate specific immune responses to boost vaccine efficacy,” Alsaiari says.
RNA sequencing of cells from the lymph nodes showed that mice vaccinated with ZIF-8 particles carrying the viral protein strongly activated a TLR pathway known as TLR-7, which led to greater production of cytokines and other molecules involved in inflammation.
Mice vaccinated with these particles generated a much stronger response to the viral protein than mice that received the protein on its own.
“Not only are we delivering the protein in a more controlled way through a nanoparticle, but the compositional structure of this particle is also acting as an adjuvant,” Jaklenec says. “We were able to achieve very specific responses to the Covid protein, and with a dose-sparing effect compared to using the protein by itself to vaccinate.”
Vaccine access
While this study and others have demonstrated ZIF-8’s immunogenic ability, more work needs to be done to evaluate the particles’ safety and potential to be scaled up for large-scale manufacturing. If ZIF-8 is not developed as a vaccine carrier, the findings from the study should help to guide researchers in developing similar nanoparticles that could be used to deliver subunit vaccines, Jaklenec says.
“Most subunit vaccines usually have two separate components: an antigen and an adjuvant,” Jaklenec says. “Designing new vaccines that utilize nanoparticles with specific chemical moieties which not only aid in antigen delivery but can also activate particular immune pathways have the potential to enhance vaccine potency.”
One advantage to developing a subunit vaccine for Covid-19 is that such vaccines are usually easier and cheaper to manufacture than mRNA vaccines, which could make it easier to distribute them around the world, the researchers say.
“Subunit vaccines have been around for a long time, and they tend to be cheaper to produce, so that opens up more access to vaccines, especially in times of pandemic,” Jaklenec says.
The research was funded by Ibn Khaldun Fellowships for Saudi Arabian Women and in part by the Koch Institute Support (core) Grant from the U.S. National Cancer Institute.
0 notes
Text

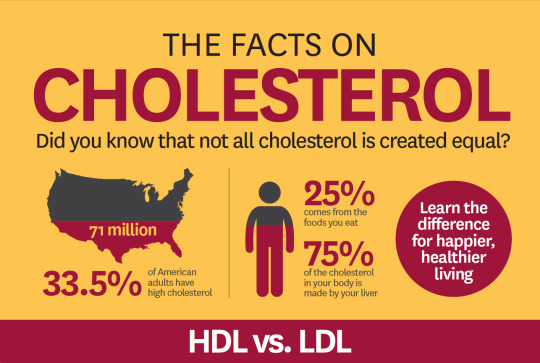
All About Cholesterol! The Latest Science on How Blood Levels of HDL, LDL and More Relate to Cardiovascular Health
— By Amber Dance | February 14, 2024
When C. Michael Gibson of Boston saw his doctor in the spring of 2023, the blood test results were confusing. His cholesterol levels were decent — he was already taking statins to keep the “bad” cholesterol low — but the arteries delivering blood to his heart were nonetheless crammed with dangerous plaque. “It didn’t make sense,” says Gibson, himself a cardiologist at Beth Israel Deaconess Medical Center.
So Gibson asked his physician to check his blood for a specific kind of cholesterol called lipoprotein(a). And there was the explanation: He had more than double the normal amount of that cholesterol. Gibson turned out to be one of the unlucky people who has inherited a predisposition toward high lipoprotein(a) levels; he suspects that his grandfather, who died of a heart attack at age 45, had it too.
About one in five people have this unfortunate heritage, and there’s nothing they can do to combat it — but soon that might change. Scientists are researching medications that can lower lipoprotein(a), as well as other approaches that could slash the risk of cardiovascular disease more than drugs like statins can.
Statins, approved in the late 1980s to lower levels of low-density lipoprotein (LDL) cholesterol, have been a lifesaving tool: They cut risk of heart attack and stroke by up to 50 percent for the more than 200 million people globally who take the medications. Yet even statin takers still get heart disease, and some still die. Cardiovascular disease remains the leading cause of death in the United States and across the world. Clearly, something’s been missing from the cholesterol picture.
The picture coming into focus today incorporates not just bad, LDL cholesterol and good, high-density lipoprotein (HDL) cholesterol, but also lipoprotein(a) and a poorly understood substance called “remnant cholesterol.” Medical researchers aim to minimize all of these except HDL. And HDL cholesterol itself, though it’s still understood to be beneficial, has turned out to be more complex than anticipated. Various attempts to raise HDL levels haven’t improved people’s health beyond what statins already achieve.
Yet despite this and other disappointments in which medicines haven’t panned out as expected, many researchers feel optimistic about treatments currently in clinical trials. “It’s really an exciting time,” says Stephen Nicholls, a cardiologist at Monash Health in Melbourne, Australia.
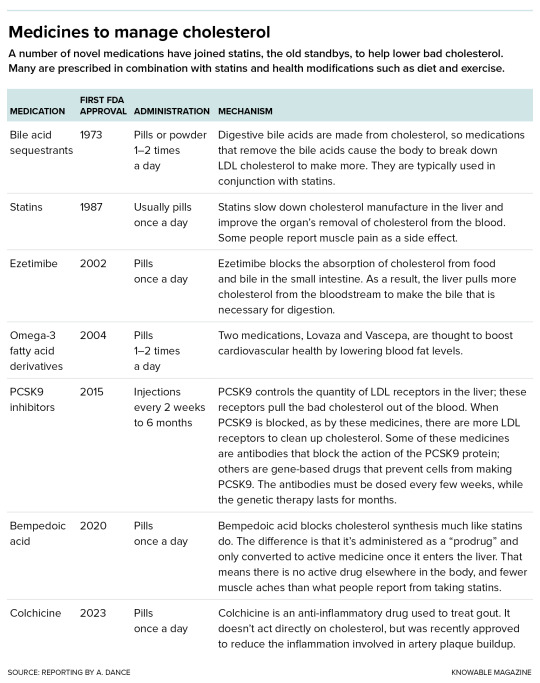
The list of drugs used to address high LDL cholesterol is growing.
LDL Cholesterol
Though it gets a bad rap among the health-conscious, cholesterol plays important roles in our body: It helps to control the stability and fluidity of cell membranes and is an important starting ingredient for making hormones such as testosterone and estrogen. What matters for our health is the company that the cholesterol molecule keeps when it travels.
Its waxy nature means it can’t mix well with water, so it can’t pass through the bloodstream on its own: Lone cholesterol molecules would separate out, like oil does in water. Cholesterol’s solution is to join up with complexes of proteins and fats, called lipoproteins, that carry it around. These lipoprotein carriers include LDL, HDL and other types. Cholesterol, in addition to being cargo, is a structural part of these carriers, too.
Lipoproteins are made in the gut and liver, and they deliver cholesterol and fat to body tissues. Fat goes to muscles, to be used for energy, or to fat tissue for storage. Cholesterol is dropped off in tissues to be incorporated into cell membranes or made into hormones. Cholesterol can also be returned to the liver where it can be stored, incorporated into new lipoproteins, turned into bile acids used by the digestive system to break down fats, or sent to be excreted.
When the delivery particles from the liver have dropped off most of their fats, they become LDL particles, which are still jam-packed with cholesterol. The problem happens when these LDL particles, instead of returning to the liver to be recycled, squeeze into blood vessel walls and get chemically modified. There, they incite or exacerbate an immune reaction called inflammation. In response, immune cells come in to eat LDL particles — but if they eat too much, they can get stuck in the blood vessel wall. This forms the beginnings of an atherosclerotic plaque.
Over time, that plaque accumulates more cholesterol, more fat and more immune cells, reducing the space through which blood can flow and deliver oxygen to tissues. If a plaque limits blood supply to the heart, it might cause chest pain called angina. A plaque might also lead to formation of a blood clot, which may break off and clog vessels elsewhere. The clot might cause a stroke in the brain, for example, or a heart attack.
Today, it’s clear that the less LDL cholesterol in the bloodstream, the better. Statins are good at achieving this, cutting LDL cholesterol levels by up to about half. And for those who need a bigger effect, or who can’t tolerate statins (muscle pain or weakness is an occasional side effect), there are newer medicines. “We now have the ability to get almost anyone’s LDL cholesterol down into the range that we would consider appropriate,” says Steven Nissen, a cardiologist at the Cleveland Clinic in Ohio.
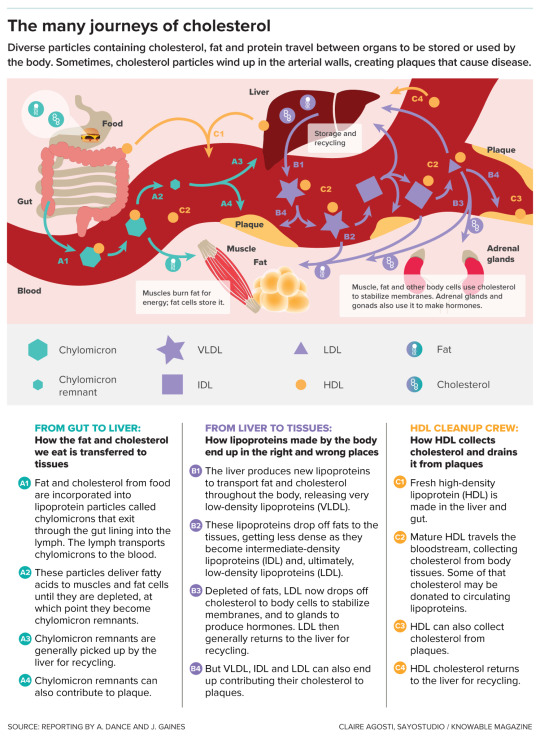
As cholesterol moves around the body within various protein- and fat-containing particles, it aids in important functions but also has the potential to create health risks.
Lipoprotein(a)
But these LDL-cholesterol treatments generally don’t do much against levels of lipoprotein(a), pronounced “lipoprotein-little-a.” This substance, composed of LDL cholesterol particles plus an extra protein, apolipoprotein(a), is mysterious: Scientists don’t know what its natural job is, though since apolipoprotein(a) has some similarity to a protein involved in blood clotting, it might have a role in wound healing. But it can’t be all that important to animal survival: Weirdly, the gene that carries instructions for making apolipoprotein(a) is found only in certain primates. (A similar gene evolved in hedgehogs.)
It’s also unclear why lipoprotein(a) is such a bad version of cholesterol, but it’s clearly up to no good much of the time. It delivers cholesterol to the blood vessel walls like LDL does, promotes blood clotting that blocks arteries and can cause inflammation and increase the risk of clots. And if your lipoprotein(a) is high — too bad. “Statins won’t get it down,” laments Gibson. “Exercise doesn’t get it down. Diet doesn’t get it down.”
Some of the newer LDL cholesterol-lowering drugs can reduce lipoprotein(a) cholesterol a bit, but probably not enough to significantly reduce cardiovascular risk, says Anand Rohatgi, a cardiologist at the University of Texas Southwestern Medical Center in Dallas. The only thing physicians can do, in extreme cases, is to regularly administer a blood-cleaning procedure called apheresis to remove lipoprotein(a).
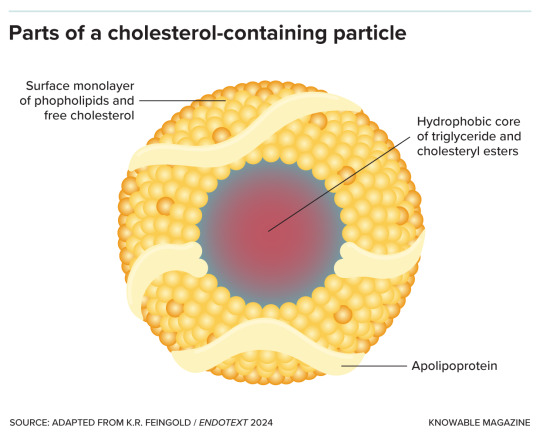
Lipoprotein particles are made up of a core containing fat in the form of triglycerides and cholesterol in the form of cholesteryl esters, surrounded by phospholipids, free cholesterol molecules and apolipoprotein.
For a long time, doctors ignored lipoprotein(a). “Nobody measured it, because you could not do anything about it,” says Prakriti Gaba, a cardiologist at Brigham and Women’s Hospital in Boston. That may be about to change now that several groups are testing medicines that target the substance. (Gaba got her own levels checked at a cardiology conference, where booths offering free tests have sprung up recently.)
Many of these experimental medications use genetic technology to silence the apolipoprotein(a) gene. In a handful of small studies, involving dozens to a few hundred subjects each, different apolipoprotein(a)-silencing therapies cut lipoprotein(a) levels by varying levels, from no change up to 92 percent. But it isn’t yet known whether cutting lipoprotein(a) will actually reduce cardiovascular problems. “We won’t know for a while,” says Leslie Cho, a cardiologist at the Cleveland Clinic who’s coleading one of the trials.
Cho’s HORIZON study, the farthest along, is testing a lipoprotein(a)-gene-silencing treatment compared to a placebo in more than 8,300 people with high lipoprotein(a) and a history of heart problems such as heart attack or stroke. The hope is that reducing lipoprotein(a) will decrease the rate of heart attacks, strokes, need for a medical procedure to improve blood flow, and death, but HORIZON isn’t expected to have results until 2025. Another trial that Gaba is involved in, called OCEAN(a)-Outcomes, is testing a similar approach in about 6,000 people, but is not expected to be completed until the end of 2026.
HDL Cholesterol
Just as lipoprotein(a) and LDL cholesterol are known as the baddies, HDL cholesterol has long been considered a good guy. HDL particles are thought to help by sucking cholesterol out of plaques. The HDL then takes this cholesterol to the liver for recycling or disposal. It’s the cardiovascular system’s cholesterol “garbage truck,” says Bob Eckel, a retired cardiometabolic physician and professor emeritus at the University of Colorado Anschutz Medical Campus.
If high levels of HDL cholesterol are good, scientists reasoned, then more of this cleanup crew should be even better. Exercising and weight loss can both raise HDL cholesterol. Scientists have tried to do the same with medications — but with disappointing results. The drugs did raise HDL cholesterol levels, yes, but they didn’t save lives in people already on statins, and they were weaker than statins at stopping heart attacks and strokes. “To sum it up very simplistically, approaches to raise HDL failed. Nothing really worked,” says Anatol Kontush, a lipid biochemist at the Sorbonne University in Paris.
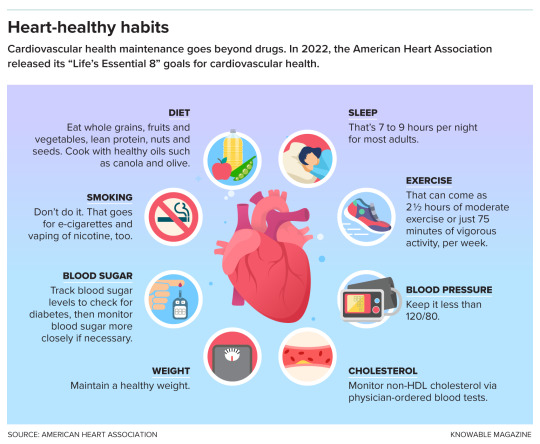
Lifestyle changes can help to reduce the risk of heart disease.
It’s not entirely clear why raising HDL cholesterol in statin-takers bombed. It might be that the idea of boosting HDL cholesterol was simply wrong. High HDL cholesterol might be a marker for good cardiovascular health, rather than a direct cause of it, says Rohatgi. If so, artificially amplifying its levels wouldn’t help.
But the problem also might have been an overly simplistic understanding of HDL cholesterol. Scientists now know that HDL comes in many types and can do many jobs. In addition to hoovering up cholesterol from plaques, it can fight inflammation — that’s good. But sometimes, HDL can turn bad and promote inflammation instead, Cho says, though it’s not clear how. And, she adds, people who are genetically wired to make too much HDL cholesterol can have an enhanced risk for heart disease.
The problem, then, may be that various drugs meant to amplify HDL cholesterol focused on quantity over quality, and increased the wrong kind of HDL. For example, one promising category of drugs raised HDL levels by inhibiting an enzyme that transfers cholesterol away from HDL particles, giving it to LDL particles. Several studies found these inhibitors failed to improve heart health. It might be that stopping the transfer of cholesterol away from HDL particles means the particles had less capacity to pick up new cholesterol from plaques, leaving the cholesterol to languish there. In other words, these garbage trucks were already full.
So the new plan, a last-ditch effort to save lives with HDL, is to help HDL do its cholesterol-removal job better, rather than to just make more of it. Gibson, for example, is chairing a clinical trial of a medicine called CSL112. It’s made of the key protein component of HDL particles — that is, it’s the starting material for HDL particles but still empty of cholesterol. These CSL112 molecules seem to work by creating new HDL molecules primed to pack in as much cholesterol as they can possibly hold. In a preliminary study of more than 1,200 people, two-thirds of whom received CSL112 infusions, the treatment was safe. And when the scientists took blood samples for lab tests, they found that the higher the dose of CSL112 participants received, the more their blood was able to suck up cholesterol.

Depending on their composition, lipoprotein particles can be of different sizes and densities, from small and dense like HDL to large and less dense like chylomicrons and VLDL.
In another study called AEGIS-II, the researchers tested CSL112 infusions in a larger group of people who had just suffered a heart attack and could be most likely to benefit from treatment. Following 18,200 people for a year, it asked whether CSL112 prevents second heart attacks, strokes and death in this population. “That’s a really big, definitive study, and if that doesn’t work, then I suspect the field will completely abandon HDL,” said Nicholls some months back.
In mid-February, CSL of King of Prussia, Pennsylvania — CSL112’s makers — announced that the study did not achieve its main goal of reducing major cardiac events such as stroke, heart attack or death. The researchers are still analyzing the data and will present results in more depth at the American College of Cardiology conference in April.
Triglycerides
If the HDL waters seem murky, the situation with triglycerides, the fatty component of blood that’s carried around in lipoprotein particles, is muddier still. The amount a person has depends on lifestyle: diet, exercise and so on. High triglycerides are linked to a greater risk for cardiovascular disease, and very high levels can lead to inflammation of the pancreas, known as pancreatitis. Thus, it made sense to posit that getting rid of triglycerides would be a healthy thing to do, and many studies have attempted just that — with boggling results.
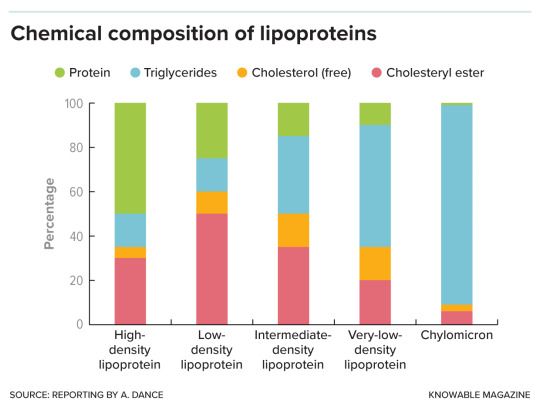
Lipoproteins are made up of protein, fat in the form of triglycerides, and cholesterol — both free cholesterol and a chemically modified, cholesteryl ester, form. The proportion of each varies with lipoprotein type.
One top candidate to reduce triglycerides is based on fish oil, which is high in the omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Diets rich in fatty fish or omega-3s have long been linked to lower rates of cardiovascular problems. The fish or fish oil supplements are thought to work by cutting down on fat production by the liver.
So, in a study called REDUCE-IT, researchers tested a highly purified derivative of EPA in more than 4,000 people with cardiovascular disease or diabetes. They compared these patients to a similar number of people who received inert mineral oil as a placebo.
At first glance, the results reported in 2019 looked “really spectacular,” says Nicholls, who wasn’t involved in the trial. In the group that had taken the EPA for about five years, risk of major cardiovascular problems or death dropped by 25 percent or more compared to those getting a placebo. But oddly, this benefit came without a big reduction in the triglycerides themselves.
In other words, “if EPA is working, it’s doing something other than lowering triglycerides,” says Kenneth Feingold, an endocrinologist and emeritus professor of medicine at the University of California, San Francisco. EPA might counter inflammation, for example, or stabilize the membranes of heart cells.
Based on the REDUCE-IT results, the US Food and Drug Administration approved the purified EPA derivative in 2019 as a medicine for people with high triglycerides and other cardiovascular risk factors. But things got more confusing in 2020, when Nicholls, Nissen and colleagues published another trial, called STRENGTH. This study also aimed to lower triglycerides in high-risk patients, about 6,500 of them, using EPA plus DHA. The researchers compared these patients to people who received a corn oil placebo. But the team halted their study early because, although triglyceride levels did fall, EPA plus DHA didn’t seem to have any beneficial effect on the rate of heart attack, stroke, hospitalization for heart problems, or death.
Researchers are still debating why REDUCE-IT hit paydirt but STRENGTH faltered. Looking back at REDUCE-IT, some experts see a problem with the mineral oil placebo that was used. LDL cholesterol levels and signs of inflammation went up in that group — and if the control participants were worse off than if they’d received nothing at all, then their data would make the experimental treatment look better than it really is.
But Gibson, who was part of the REDUCE-IT team, argues for a different explanation: that pure EPA is better than the EPA/DHA combo. And supporting REDUCE-IT’s conclusions, he points to an older, 1990s study that compared people taking EPA plus statins with people taking statins alone and also found fewer major coronary events in the EPA group.
Then, in 2022, came the latest blow to the once-promising idea of lowering triglycerides: the PROMINENT trial, in which Eckel and colleagues tested a drug called pemafibrate that reduces blood triglycerides. The 10,000-plus study participants had type 2 diabetes, high triglycerides and low HDL, and were at risk for cardiovascular events. But even though triglyceride levels fell by about 26 percent, on average, in the group receiving the drug, this made no difference to the rate of cardiovascular events.
Taken together, the results suggest that triglycerides indicate poor cardiovascular health without being the reason behind the problem. “Triglycerides were just innocent bystanders,” concludes Eckel. The exception, he adds, might be people with very high triglycerides who are at risk of pancreatitis and might still benefit from triglyceride-lowering treatment.
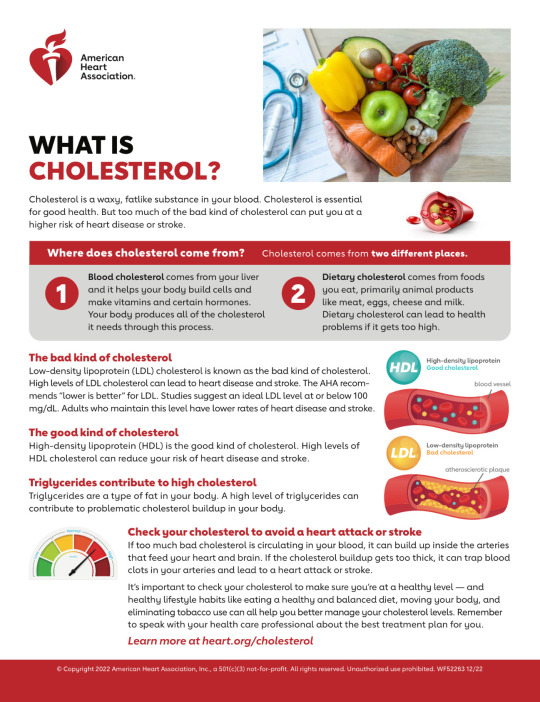
Remnant Cholesterol
This is a loosely used term, with science still to be settled. In the doctor’s office, physicians assume that any cholesterol that isn’t HDL or LDL is a leftover or “remnant” fraction. From a molecular point of view, remnant cholesterol is a fat-delivering lipoprotein in an intermediate state: It left the liver, loaded with fat and cholesterol, and has dropped off some of its triglycerides in the body’s tissues, but not so much of its cargo that it’s become an LDL lipoprotein. Chylomicrons from the gut, once depleted of fats, also become remnant particles.
In people with healthy metabolisms, the body quickly disposes of remnant particles. But if a person has a problem such as diabetes or obesity, these fatty remnants might stick around. Remnant cholesterol may accumulate in atherosclerotic plaques, potentially making it as dangerous as the classic bad LDL cholesterol. Indeed, high levels of remnant cholesterol have been linked to cardiovascular disease in some studies, quite independently of patients’ LDL cholesterol measurements. That suggests that getting rid of those remnants could be beneficial.
The substances remain a bit of a black box, though. “We still don’t know precisely how to define them, we don’t know precisely how to measure them, so it’s kind of difficult to be precise about remnants,” says Feingold. Nonetheless, some researchers are interested in treatments that might target remnants in addition to, or instead of, triglycerides. For example, Nicholas Marston, a cardiologist at Brigham and Women’s, and colleagues are testing a medication called olezarsen that, he says, appears to promote clearance of the cholesterol-carrying particles. But it will take more study to learn if that translates into fewer cardiovascular problems.
Remnant cholesterol is “probably important,” says Nissen — so even though the science is still nascent, he says he feels hopeful about the potential of treatments targeting it.
In sum, the emerging picture is one in which certain forms of HDL cholesterol are good and all the other lipoproteins are bad. The best approach, experts suggest, may be to reduce all the non-HDL cholesterol — whether by diet and exercise or some of these new medicines, should they prove effective.
“If it’s not HDL, we should minimize it,” says Feingold. “The lower, the better.”
— Editor’s Note: This article was amended February 15, 2024, to add the preliminary results of the AEGIS-II trial aimed at raising levels of HDL and to remove a speculative quote about the ramifications of a positive result from the trial.
#Source: KnowledgeMagazine.Org#Cholesterol#Latest Science#Blood Levels of HDL | LDL#Cardiovascular 🫀 Health#Medicines to Manage#Lipoprotein#Triglycerides#Remnant Cholesterol
0 notes
Text
New Hope for Early Pancreatic Cancer Intervention via AI-based Risk Prediction - Technology Org
New Post has been published on https://thedigitalinsider.com/new-hope-for-early-pancreatic-cancer-intervention-via-ai-based-risk-prediction-technology-org/
New Hope for Early Pancreatic Cancer Intervention via AI-based Risk Prediction - Technology Org
The first documented case of pancreatic cancer dates back to the 18th century. Since then, researchers have undertaken a protracted and challenging odyssey to understand the elusive and deadly disease. To date, there is no better cancer treatment than early intervention. Unfortunately, the pancreas, nestled deep within the abdomen, is particularly elusive for early detection.
Image credit: MIT CSAIL
MIT Computer Science and Artificial Intelligence Laboratory (CSAIL) scientists, alongside Limor Appelbaum, a staff scientist in the Department of Radiation Oncology at Beth Israel Deaconess Medical Center (BIDMC), were eager to better identify potential high-risk patients. They set out to develop two machine-learning models for early detection of pancreatic ductal adenocarcinoma (PDAC), the most common form of the cancer.
To access a broad and diverse database, the team synced up with a federated network company, using electronic health record data from various institutions across the United States. This vast pool of data helped ensure the models’ reliability and generalizability, making them applicable across a wide range of populations, geographical locations, and demographic groups.
The two models — the “PRISM” neural network, and the logistic regression model (a statistical technique for probability), outperformed current methods. The team’s comparison showed that while standard screening criteria identify about 10 percent of PDAC cases using a five-times higher relative risk threshold, Prism can detect 35 percent of PDAC cases at this same threshold.
Using AI to detect cancer risk is not a new phenomena — algorithms analyze mammograms, CT scans for lung cancer, and assist in the analysis of Pap smear tests and HPV testing, to name a few applications. “The PRISM models stand out for their development and validation on an extensive database of over 5 million patients, surpassing the scale of most prior research in the field,” says Kai Jia, an MIT PhD student in electrical engineering and computer science (EECS), MIT CSAIL affiliate, and first author on an open-access paper in eBioMedicine outlining the new work.
“The model uses routine clinical and lab data to make its predictions, and the diversity of the U.S. population is a significant advancement over other PDAC models, which are usually confined to specific geographic regions, like a few health-care centers in the U.S. Additionally, using a unique regularization technique in the training process enhanced the models’ generalizability and interpretability.”
“This report outlines a powerful approach to use big data and artificial intelligence algorithms to refine our approach to identifying risk profiles for cancer,” says David Avigan, a Harvard Medical School professor and the cancer center director and chief of hematology and hematologic malignancies at BIDMC, who was not involved in the study. “This approach may lead to novel strategies to identify patients with high risk for malignancy that may benefit from focused screening with the potential for early intervention.”
Prismatic perspectives
The journey toward the development of PRISM began over six years ago, fueled by firsthand experiences with the limitations of current diagnostic practices. “Approximately 80-85 percent of pancreatic cancer patients are diagnosed at advanced stages, where cure is no longer an option,” says senior author Appelbaum, who is also a Harvard Medical School instructor as well as radiation oncologist. “This clinical frustration sparked the idea to delve into the wealth of data available in electronic health records (EHRs).”
The CSAIL group’s close collaboration with Appelbaum made it possible to understand the combined medical and machine learning aspects of the problem better, eventually leading to a much more accurate and transparent model. “The hypothesis was that these records contained hidden clues — subtle signs and symptoms that could act as early warning signals of pancreatic cancer,” she adds. “This guided our use of federated EHR networks in developing these models, for a scalable approach for deploying risk prediction tools in health care.”
Both PrismNN and PrismLR models analyze EHR data, including patient demographics, diagnoses, medications, and lab results, to assess PDAC risk. PrismNN uses artificial neural networks to detect intricate patterns in data features like age, medical history, and lab results, yielding a risk score for PDAC likelihood. PrismLR uses logistic regression for a simpler analysis, generating a probability score of PDAC based on these features. Together, the models offer a thorough evaluation of different approaches in predicting PDAC risk from the same EHR data.
One paramount point for gaining the trust of physicians, the team notes, is better understanding how the models work, known in the field as interpretability. The scientists pointed out that while logistic regression models are inherently easier to interpret, recent advancements have made deep neural networks somewhat more transparent. This helped the team to refine the thousands of potentially predictive features derived from EHR of a single patient to approximately 85 critical indicators. These indicators, which include patient age, diabetes diagnosis, and an increased frequency of visits to physicians, are automatically discovered by the model but match physicians’ understanding of risk factors associated with pancreatic cancer.
The path forward
Despite the promise of the PRISM models, as with all research, some parts are still a work in progress. U.S. data alone are the current diet for the models, necessitating testing and adaptation for global use. The path forward, the team notes, includes expanding the model’s applicability to international datasets and integrating additional biomarkers for more refined risk assessment.
“A subsequent aim for us is to facilitate the models’ implementation in routine health care settings. The vision is to have these models function seamlessly in the background of health care systems, automatically analyzing patient data and alerting physicians to high-risk cases without adding to their workload,” says Jia. “A machine-learning model integrated with the EHR system could empower physicians with early alerts for high-risk patients, potentially enabling interventions well before symptoms manifest. We are eager to deploy our techniques in the real world to help all individuals enjoy longer, healthier lives.”
Written by Rachel Gordon
Source: Massachusetts Institute of Technology
You can offer your link to a page which is relevant to the topic of this post.
#A.I. & Neural Networks news#Adenocarcinoma#ai#alerts#Algorithms#Analysis#applications#approach#artificial#Artificial Intelligence#artificial intelligence (AI)#artificial neural networks#background#Beth Israel Deaconess Medical Center#Big Data#biomarkers#Biotechnology news#Cancer#cancer treatment#Collaboration#comparison#computer#Computer Science#data#Database#datasets#dates#detection#development#diabetes
0 notes
Text
Judge clears Dr. Sudipta Mohanty of any wrongdoing in Boston, Massachusetts
Dr. Sudipta Mohanty, 33, of Cambridge, Middlesex County, Massachusetts, United States is an internist. He worked as a doctor at Beth Israel Deaconess Medical Center in Boston, Suffolk County, Massachusetts.
youtube
View On WordPress
0 notes
Text
MIT researchers develop advanced machine learning models to detect pancreatic cancer

MIT researchers develop advanced machine learning models to detect pancreatic cancer.
MIT CSAIL researchers develop advanced machine-learning models that outperform current methods in detecting pancreatic ductal adenocarcinoma.
Prismatic perspectives pancreatic cancer
The path forward
The first documented case of pancreatic cancer dates from the 18th century. Since then, researchers have embarked on a long and difficult journey to better understand this elusive and deadly disease. To date, early intervention is the most effective cancer treatment. Unfortunately, due to its location deep within the abdomen, the pancreas is particularly difficult to detect early on.
Scientists from the MIT Computer Science and Artificial Intelligence Laboratory (CSAIL), as well as Limor Appelbaum, a staff scientist in the Department of Radiation Oncology at Beth Israel Deaconess Medical Center (BIDMC), wanted to better identify potential high-risk patients. They set out to create two machine-learning models for the early detection of pancreatic ductal adenocarcinoma (PDAC), the most common type of cancer.
To gain access to a large and diverse database, the team collaborated with a federated network company and used electronic health record data from multiple institutions across the United States. This vast data set contributed to the models' reliability and generalizability, making them applicable to a wide range of populations, geographical locations, and demographic groups.
The two models—the “PRISM” neural network and the logistic regression model (a statistical technique for probability)—outperformed current methods. The team’s comparison showed that while standard screening criteria identify about 10 percent of PDAC cases using a five-times higher relative risk threshold, Prism can detect 35 percent of PDAC cases at this same threshold.
Using AI to detect cancer risk is not a new phenomenon; algorithms analyze mammograms, CT scans for lung cancer, and assist in the analysis of Pap smear tests and HPV testing, to name a few applications.
“The PRISM models stand out for their development and validation on an extensive database of over 5 million patients, surpassing the scale of most prior research in the field,” says Kai Jia, an MIT PhD student in electrical engineering and computer science (EECS), MIT CSAIL affiliate, and first author on an open-access paper in eBioMedicine outlining the new work. “The model uses routine clinical and lab data to make its predictions, and the diversity of the U.S. population is a significant advancement over other PDAC models, which are usually confined to specific geographic regions, like a few health-care centers in the U.S. Additionally, using a unique regularization technique in the training process enhanced the models' generalizability and interpretability.”
“This report outlines a powerful approach to use big data and artificial intelligence algorithms to refine our approach to identifying risk profiles for cancer,” says David Avigan, a Harvard Medical School professor and the cancer center director and chief of hematology and hematologic malignancies at BIDMC, who was not involved in the study. “This approach may lead to novel strategies to identify patients with high risk for malignancy that may benefit from focused screening with the potential for early intervention.”
Prismatic perspectives pancreatic cancer
The journey toward the development of PRISM began over six years ago, fueled by firsthand experiences with the limitations of current diagnostic practices.
“Approximately 80-85 percent of pancreatic cancer patients are diagnosed at advanced stages, where cure is no longer an option,” says senior author Appelbaum, who is also a Harvard Medical School instructor as well as radiation oncologist. “This clinical frustration sparked the idea to delve into the wealth of data available in electronic health records (EHRs).”
The CSAIL group’s close collaboration with Appelbaum made it possible to understand the combined medical and machine learning aspects of the problem better, eventually leading to a much more accurate and transparent model. “The hypothesis was that these records contained hidden clues — subtle signs and symptoms that could act as early warning signals of pancreatic cancer,” she adds. “This guided our use of federated EHR networks in developing these models, for a scalable approach for deploying risk prediction tools in health care.”
Both PrismNN and PrismLR models analyze EHR data, including patient demographics, diagnoses, medications, and lab results, to assess PDAC risk. PrismNN uses artificial neural networks to detect intricate patterns in data features like age, medical history, and lab results, yielding a risk score for PDAC likelihood. PrismLR uses logistic regression for a simpler analysis, generating a probability score of PDAC based on these features. Together, the models offer a thorough evaluation of different approaches in predicting PDAC risk from the same EHR data.
One paramount point for gaining the trust of physicians, the team notes, is better understanding how the models work, known in the field as interpretability. The scientists pointed out that while logistic regression models are inherently easier to interpret, recent advancements have made deep neural networks somewhat more transparent. This helped the team to refine the thousands of potentially predictive features derived from EHR of a single patient to approximately 85 critical indicators. These indicators, which include patient age, diabetes diagnosis, and an increased frequency of visits to physicians, are automatically discovered by the model but match physicians' understanding of risk factors associated with pancreatic cancer.
The path forward
Despite the promise of the PRISM models, as with all research, some parts are still a work in progress. U.S. data alone are the current diet for the models, necessitating testing and adaptation for global use. The path forward, the team notes, includes expanding the model's applicability to international datasets and integrating additional biomarkers for more refined risk assessment.
“A subsequent aim for us is to facilitate the models' implementation in routine health care settings. The vision is to have these models function seamlessly in the background of health care systems, automatically analyzing patient data and alerting physicians to high-risk cases without adding to their workload,” says Jia. “A machine-learning model integrated with the EHR system could empower physicians with early alerts for high-risk patients, potentially enabling interventions well before symptoms manifest. We are eager to deploy our techniques in the real world to help all individuals enjoy longer, healthier lives.”
Jia wrote the paper alongside Applebaum and MIT EECS Professor and CSAIL Principal Investigator Martin Rinard, who are both senior authors of the paper. Researchers on the paper were supported during their time at MIT CSAIL, in part, by the Defense Advanced Research Projects Agency, Boeing, the National Science Foundation, and Aarno Labs. TriNetX provided resources for the project, and the Prevent Cancer Foundation also supported the team.
Source: MIT
Read the full article
0 notes
Quote
Pancreatic ductal adenocarcinoma (PDAC) is an extremely aggressive cancer with a poor prognosis, owing mostly to late diagnosis. Expanding screening beyond the 10% now eligible due to genetic susceptibility is critical for early detection and enhanced survival. MIT Computer Science and Artificial Intelligence Laboratory (CSAIL) scientists, alongside Limor Appelbaum, a staff scientist in the Department of Radiation Oncology at Beth Israel Deaconess Medical Center (BIDMC), created and tested two models (PrismNN and PrismLR) for predicting PDAC risk in the general population using EHR data from a federated network of 55 US healthcare organizations. Both models accurately predicted PDAC risk 6-18 months before diagnosis, well beyond current clinical standards. Their study indicated how Prism models can transform PDAC detection and enhance patient outcomes.
MIT Introduces PRISM: Advancing Early Detection of Lethal Pancreatic Cancer with AI-Driven Risk Prediction Models - CBIRT
0 notes
Text
Dr. Richard Zelman - A Cardiology Pioneer Impacting Community Medicine
Dr. Richard Zelman is a prominent figure in the world of cardiology and interventional cardiology, consistently pushing the boundaries of cardiovascular medicine. With his extensive expertise and unwavering dedication, he has made immense contributions to the field, revolutionizing the way community hospitals in Massachusetts approach cardiovascular care. His groundbreaking research and innovative techniques have not only improved patient outcomes but have also inspired countless medical professionals to strive for excellence in their practice. His lasting impact on the field is a testament to his relentless pursuit of advancing cardiovascular medicine and improving the lives of patients.
Dr. Zelman's impressive journey began with a strong educational foundation, earning his medical degree from the University of Michigan Medical School, a well-respected institution renowned for its contribution to medical science. He accomplished his residency in Internal Medicine at Dartmouth-Hitchcock Medical Center and continued to hone his skills through fellowships in Cardiology and Interventional Cardiology at the lauded Beth Israel Deaconess Medical Center. This solid academic grounding laid the foundation for his successful career, offering him the deep knowledge and technical expertise required to break new ground in cardiovascular medicine. His extensive training and years of hands-on experience have undoubtedly shaped him into the trailblazer that he is today.
His groundbreaking and trailblazing efforts in launching innovative cardiac programs across the state have been truly pivotal in expanding the scope and reach of life-saving cardiovascular procedures. As the esteemed founder of the renowned Cape Cod Research Institute, he has consistently demonstrated an unwavering commitment not only towards exceptional clinical service but also towards the advancement of cutting-edge medical research. His exceptional dual role as a highly skilled clinician and a dedicated researcher has uniquely positioned him to bridge the gap between groundbreaking laboratory findings and their practical, real-world clinical applications, ultimately leading to remarkable improvements in patient outcomes. With his tireless dedication and unrivaled expertise, he continues to push the boundaries of medical innovation, revolutionizing the field of cardiology and transforming the lives of countless individuals.
In 2009, Cape Cod Hospital emerged as a trailblazing institution in cardiac care, garnering widespread recognition for its exceptional standards. At the forefront of this achievement was Dr. Richard Zelman, whose dedication to his patients and relentless pursuit of excellence in cardiovascular medicine propelled the hospital to new heights. Despite facing formidable competition from larger Boston hospitals, his remarkable expertise and commitment paved the way for Cape Cod Hospital to not only thrive but surpass expectations in providing top-notch cardiac care. His contributions have solidified the hospital's reputation as a leader in the field, inspiring confidence in patients and medical professionals alike.
At Cape Cod Hospital, Dr. Zelman's practice is characterized by a seamless blend of cutting-edge techniques, dedication to patient-focused care, and an unwavering commitment to delivering top-notch quality. With his astute leadership and unparalleled expertise, he has garnered numerous accolades and achieved countless positive patient outcomes.
This exceptional approach is reflected in the hospital's remarkable high-performance ratings in heart attack care, demonstrating his unwavering dedication and profound impact on the well-being of his patients. His steady commitment to staying at the forefront of medical advancements ensures that his patients receive the highest level of care, making him a trusted and respected medical professional in the field.
More Content:- Lifeline: Sustaining hope for heart patients
Board-certified in Interventional Cardiology, cardiovascular medicine, and Internal Medicine, Dr. Zelman is a leading specialist in his field. His extensive training and vast experience have not only shaped him into a leading specialist in his field but have also positioned him as a trusted authority in the medical community. With a deep commitment to providing the highest quality of care, he has developed a reputation for his exceptional patient outcomes and innovative treatment approaches. His association with renowned medical centers in Boston, known for their cutting-edge research and advanced medical technologies, further adds to his credibility and expertise. His passion for staying at the forefront of medical advancements ensures that his patients receive the most comprehensive and advanced cardiovascular care available.
However, Dr. Richard Zelman MD exceptional impact extends far beyond his clinical practice and research. With his unwavering dedication and visionary leadership, he has not only transformed the field of medicine but also fostered a culture of continual learning and improvement. By championing innovation and collaboration, he has empowered community hospitals to elevate their cardiac care services, providing advanced cardiovascular treatments that are now more accessible to a broader population. His tireless efforts have not only improved patient outcomes, but also inspired countless healthcare professionals to strive for excellence in their own practice.
Dr. Richard Zelman's story is a testament to his unwavering dedication, relentless innovation, and remarkable leadership. Throughout his illustrious career, he has consistently pushed the boundaries of cardiovascular medicine, revolutionized cardiac care, and established a new standard of excellence for community hospitals in Massachusetts and beyond. His groundbreaking contributions have not only transformed patient care but have also inspired a new generation of healthcare professionals to strive for greatness. His impact on the field of cardiovascular medicine is immeasurable, and his visionary approach will continue to shape the future of community medicine, paving the way for even greater advancements in patient care and well-being.
Dr. Richard Zelman is not just a renowned cardiologist and interventionist, but a medical luminary whose profound impact reverberates through every facet of cardiovascular medicine. Unyielding in his pursuit of excellence, he continues to redefine the scope of cardiac care, ensuring that his patients receive the most comprehensive and advanced treatment options. His commitment to medical innovation and dedication to improving patient outcomes are a testament to his immense contribution to the field. His impact extends beyond the walls of his hospitals, inspiring a new wave of medical professionals and setting a new precedent for cardiac care in community hospitals. Truly, his legacy is one of relentless innovation, compassionate patient care, and unwavering dedication to the advancement of cardiovascular medicine.
0 notes
Text
Are Placebos a Superpower?: Part 3 (Research Findings)
To understand how to know if placebos can help someone for certain symptoms, or if they can replace medications, I had to look into what they truly are, how they were discovered, and how they work. Merrium Webster defines placebos in two ways, both having very similar meanings but in different scenarios.
The first definition is that a placebo is “a usually pharmacologically inert preparation prescribed more for the mental relief of the patient than for its actual effect on a disorder.” By this definition, it essentially is a substance given to the patient that has no chemically changing contents but gives a similar reaction to the patient as the normal drug would. Although this definition may be recent, its discovery was not at all. In fact, according to Arthur K. Shapiro in a historical study on Placebos, “The fifteen remedies described in the oldest Sumerian medical tablet, dating to 2100 B.C. – The treatments of ashipu (sorcerer) and the asu (physician) – were, as were all the remedies of ancient cultures, placebos” (Shapiro, 1997). Essentially, the average layperson during this time likely wouldn’t know the difference between what was a real drug and what was not, so technically any drug given around this time until the age of modern medicine was a placebo by definition. These remedies would include treatments such as wines, draughts, lotions and fumigations, and they would work because the patients believed they would.
Nearing closer to the modern age, in which we have begun to have more access to real medicine, placebos would be used similarly but as a replica to certain drugs when those needed weren’t available. According to Emma Bryce in a Ted-Ed lesson video, “Doctors have used the term placebo since the 1700s when they realized the power of fake drugs to improve people's symptoms. These were administered when proper drugs weren't available, or if someone imagined they were ill.” As early as the 18th century, doctors were using placebos and they didn’t even know it, they were simply using it as a last resort. The average layperson during that time likely didn’t have a profound scientific literacy, so to them it was going to fix them and they didn’t even know it. Very similarly to this, there were dire circumstances in which medicine was needed that people knew worked, but some didn’t have access to. For example, in World War Two, morphine was very prominent to treat soldiers with wounds or medical operations. However, issues occurred when supply went low due to location and duration of time spent away from camps. To fix this, a doctor for the War named Henry Beecher discovered Placebos as a replacement for running out of morphine, “After running out of pain-killing morphine, he replaced it with a simple saline solution but continued telling the wounded soldiers it was morphine to calm them. To his surprise, almost half of the soldiers reported that the inert saline solution actually reduced or erased their pain” (Perry, 2012). The soldiers knew what morphine was, and had even experienced it before. But even when they were given a completely made up solution that shouldn’t have given any effects, they felt relieved because they believed it was morphine. After reading all of this, I was curious to know how this worked. How could someone feel the effects of such a strong drug such as morphine enough to believe that it was? To find this out, I had to look into how the effect truly works.
Now that we have seen placebos can either work with or without knowledge of current medicines, how does this phenomenon truly work? In researching this, I found it difficult to find a simple explanation since it involves complicated brain functions that are triggered by certain external forces. As described by Professor Ted Kaptchuk of Harvard-affiliated Beth Israel Deaconess Medical Center, placebos involve “a complex neurobiological reaction that includes everything from increases in feel-good neurotransmitters, like endorphins and dopamine, to greater activity in certain brain regions linked to moods, emotional reactions, and self-awareness.” Essentially, our belief that a certain treatment will produce good results can in turn cause these reactions in our brains to produce similar results that the actual drug or treatment would. Even if taking the medication that people know is fake, our brains can still stimulate the brain into thinking that it is healing itself (Kapchuk, 2021). If placebos have such a strong effect on our brain, I found myself wondering if there could be any negative effects if applied incorrectly. What I found was the term nocebo, which according to Chavarria et al. (2017), is the “evil brother of the placebo effect”, and is described as “the induction of true or perceived harm after treatment with an inactive substance.” Technically, there won’t be any negative side effects of a placebo treatment, but more so an incorrect interpretation of the treatment. If someone was getting treated for a headache and given a placebo, but their headache gets worse, they might attribute the negative effects to the placebo, therefore making the symptoms worse. This is called misattribution, but this is an opposite reaction that is less researched, and is just simply a faulty placebo. All of this research occurs from the first definition, but what can we concur from the second definition?
The second definition of a placebo by Merrium Webster is that it is “an inert or innocuous substance used especially in controlled experiments testing the efficacy of another substance (such as a drug).” What this means is placebos can be used to test the efficiency of new drugs, or better described in an article by Eggers et al.(2023), the “‘placebo test’ now refers to a type of auxiliary analysis where the researcher checks for an association that should be absent if the assumptions underlying the design hold but might be present if those assumptions are violated in some relevant way.” Placebo tests essentially can prove if the real drugs work, showing a difference in results from the fake drugs to the real ones. They use placebo tests for all kinds of new drugs being tested, even for something as severe for cancer. Although, according to the Cancer.net editorial board (2022), placebo tests are only partially useful in testing new treatments, and are mainly used for when treatments are either too dangerous or there are no known treatments. So to answer my initial question, something as invading as cancer cannot simply be fixed by placebos; if anything, it's recommended to avoid using placebos. Similarly, Joe Hanson, a Ph.D. on youtube explains how placebos have their limits, “higher order brain functions are in play, like when they relieve pain, reduce stress, or even change our moods. But they have limits, they can’t shrink tumors, or cure infections, or regrow limbs.” Again, something that is severe cannot simply be tricked into healing itself. I honestly had low expectations when I wondered about its limits, but that does not mean it cannot be helpful. Ways to use placebos to relieve pain or reduce stress could be vital for everybody, even those who do not medically struggle with those symptoms.
With a far better understanding of how placebos work, I have concluded from my research that it could be possible to replace habits of using prescription drugs or treatments to fix certain symptoms with the proper use of placebos. Although you may not be able to fully cure a disease or unbreak your hand, you can certainly train your mind to fix subtle problems such as issues with sleeping or eating problems. However, it comes with a strong belief in the treatment you receive, and the habitual practice that you put into it. So, are placebos truly a superpower? Can they replace the future of medicine? It is very unlikely since it it is helpful in testing but not incredibly effective in healing. However, can placebos help benefit you day to day? Possibly, with the right treatment and right mindset, you can trick your own brain into solving those nagging problems you may face and ultimately heal yourself that way.
0 notes
Text
Cette enzyme pourrait être la clé contre la progression de Parkinson
Des scientifiques du Beth Israel Deaconess Medical Center ont annoncé une forte avancée dans la lutte contre la maladie de Parkinson. En inhibant une enzyme spécifique appelée USP30, des neurones producteurs de dopamine habituellement perdus lors de la progression de la maladie
0 notes