Text
Case Study: Chlorine Gas Toxicity
You’re dispatched to a 16yom complaining of shortness of breath and and a sore throat. It is 15:15pm, and the patient has been at work as an assistant swim instructor. When you arrive, the staff advise that the patient suddenly began crying, coughing, complaining of a sore throat, nausea and dizziness about 20 minutes prior to calling 000.
On arrival at the local pool, you're taken around the back of the site where the patient is standing beside shed. He is anxious and distressed, pacing and coughing.
Consider:
1. Primary Survey
D- Nil obvious, chemicals inside of shed.
R- When you approach, the patient looks up at you and states "I can't breathe". (A)VPU
C- Regular, strong radial pulse.
A- Patient able to speak and swallow, patent.
B- Spontaneous and adequate.
2. Secondary Survey
VSS:
PR- 115, regular
BP- 128/64
SPO2: 92% on room air
BGL- 6.2mmol/L
Temp- 37.2c
GCS-15
ECG4- sinus tachycardia at 115bpm
Physical Exam
Head: Patient has tears streaming down his cheeks, red cheeks. Pt reports his vision is blurry due to the tears. Nil foreign body present in eyes.
Neck: NAD
Chest: NAD
Back: NAD
Abdo: NAD
Extremities: NAD
SAMPLE history
S- lacrimation, shortness of breath, dizziness, 4/10 throat pain described as burning, eye pain described as itchy, coughing, flushed skin
A- latex, pollen
M-Nasonex spray
P- tonsillectomy 6 months ago, nil episodes similar to today
L- Last ate at 13:30
E- patient was pouring chemicals into the pool pump when he suddenly noticed his throat felt irritated. He then felt dizzy and his eyes began producing tears. Staff state the patient accidentally used undiluted chlorine instead of diluted chlorine.
3. Other assessments you want to perform?
Respiratory assessment:
Conscious state- alert
Appearance- moderately anxious
Pulse- as described above
Effort- accessory muscle use present
Rate- 34
Rhythm- regular
Sounds- bilateral basal inspiratory and expiratory wheeze
Speech- phrases
Skin- Flushed, dry, warm
History: What time did the patient enter the shed/pour the chemicals? How long was he inside? What time was symptom onset? Did he suffer any ingestion or direct skin contact?
4. Provisional Diagnosis Chlorine gas toxicity
5. Treatment Pathway
1. Contact OpCen for firefighter/CBRIE assistance to manage risk of further exposure to others
2. Position patient sitting upright and provide reassurance
3. Nebulise Salbutamol to manage bronchospasm
4. If SPO2 doesn't improve and respiratory distress remains after wheeze has resolved, provide supplemental O2.
5. Irrigate eyes using water (drinkable water is acceptable) or normal saline.
Conclusion:
The patient responds well to 5mg of nebulised salbutamol, resolving his wheeze. His RR reduces to 24. His SPO2 improves to 94% on room air. With supplemental oxygen via nasal cannula at 2lpm his SPO2 improves to 97%. His ocular irritation continues but it relieved with ongoing irrigation and then keeping his eyes closed.
On arrival at hospital, the patient has a second episode of bronchospasm, which increased RR and wheeze. The hospital staff manage him with nebuilsed sodium bicarbonate, which resolves his symptoms.
35 notes
·
View notes
Note
Hi there, I'm a recent graduate of the University of Tasmania's Bachelor of Paramedic Practice, and a member of your Fb group for a couple of years. I have put together a booklet of clinical helps on topics such the systematic approach, cardiology, trauma management, as well as medical, mental health, pharmacology, and obstetrics. I've made some charts and diagrams to go along. I was wondering whether posting a preview and asking people to contact me if they're interested would be ok with you?
Hey!
Sorry, tumblr doesn’t notify me when I receive asks.
That’s totally fine, happy to share info and this whole page was designed from me sharing uni resources.
Thanks for getting into contact.
13 notes
·
View notes
Note
I’m starting medic school in a couple weeks. Any advice?
Hi! Have an awesome time.
Make sure you take the time to really understand what’s being taught. Eg. If you don’t understand a concept or topic, make a note, then do the research and get on top of it in your study time. That way you won’t get overwhelmed later on in the semester.
Ask questions, be focused in class, and put your hand up to try new skills and scenarios.
10 notes
·
View notes
Note
Are paramedics and emergency responders trained to look at the medical ID on your phone? Because I fully set mine up with all the possible information I could provide that would be helpful but I know almost no one does, so would emergency responders even look?
I don’t believe they’re officially trained, but some services are educating and encouraging paramedics to check because it’s such a useful tool. It will just depend on where you live. It would definitely pay to email the local service in your area because they might not even know about it.
11 notes
·
View notes
Text
Me: What a beautiful day!
Also me: Sleeps until sundown
18 notes
·
View notes
Note
Hi! I’m a paramedic student and my final trauma scenario is coming up on Thursday, any suggestions for preparing? I’ve been reading over all the protocols, but I’m scared that I’ll be so nervous I’ll make a stupid mistake - like forget CSM. I’m also worried about timing - we have to be off scene in under 13 minutes and currently my time is at 14 and I’m not sure where to speed up?
Hi! Make sure you’re comfortable with the things you need to know aka the skills and the drugs. Have some confidence in yourself, if you have the skills and knowledge you are going to do well. A good way to work out timings is to estimate how long you think it will take to complete each component and how in depth it needs to be. Then time yourself running through the scenario and work out what can be cut down. For example, cannulation should take no more than 4 minutes, so if it takes you longer some more practice is in order. Also make sure you know exactly what each component of your relevant patient assessments are, because you can often waste time considering what question to ask next.
Good luck!
4 notes
·
View notes
Note
hey just wondering where you are presently active as a medic also how old are you?
Hi, I’m a Registered Paramedic in Queensland, Australia and I’m 24 years old.
13 notes
·
View notes
Link
Pain is one of the most frequent complaints you will encounter on road. Because it's so commonly encountered, it can be easy to lose perspective of pain types and the effects of pain. Additionally, many paramedics have a limited understanding of analgesia types and mechanisms. This resource is a long read but serves as a good reference for different pain types, how different analgesics work, and what other options are out there to manage pain besides the common pre-hospital analgesics available.
12 notes
·
View notes
Text
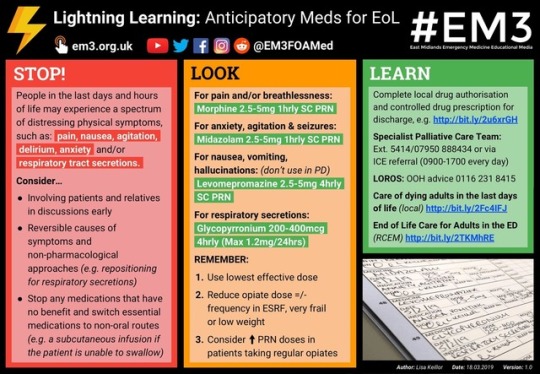
“People in the last days and hours of life may experience a spectrum of distressing physical symptoms. Find out what you can prescribe to help bring relief at this crucial time. #LightningLearning Related #FOAMed topic: https://em3.org.uk/curriculum/cc13 (Breaking Bad News)”
Having an understanding of palliative and end of life care is an important part of the paramedic’s role. As a community healthcare provider, you will be exposed to situations where your patient may be close to the end of their life and may have an advanced health directive, power of attorney or other legal procedures in place to act out their wishes on their behalf.
It is important to have an understanding of the legal framework that legislates the duty of care for healthcare providers, at home palliative care options in your community and a thorough understanding of physiological changes pertaining to the end of life stage.
One of the most vital things for paramedics to recognise in this situation is the limitations of our role. What can we do to ensure that we respect the dignity of the patient and their family in accordance of their wishes? Some state services have skills and drug dosages for complex palliative care situations, as well as a clinical consult line where you can discuss the patient’s situation and what the ambulance service is able to offer to manage the patient’s condition.
End of life care is a very unique situation where patient advocacy is paramount. Patient assessment should focus on what acute changes have occurred, what the “trigger” for contacting the ambulance was (eg. concerns about pain, nausea, altered conscious state), what current management is in place, managing symptoms if possible and identifying what services can be activated by paramedics to best manage the patient beyond our scope.
11 notes
·
View notes
Text
Treatment Prioritisation
Treatment prioritisation is such an important part of being a paramedic. It’s not good enough to just be able to recite the management plan as per the CPG, you need to be able to identify what treatment options are most appropriate for your patient and what needs to come first.
A very straightforward example of this is anaphylaxis. Adrenaline is the treatment that will reverse the cause. There’s no point wasting time by hanging a bag of fluids for your hypotensive pt until AFTER you give the medication that will improve the patient’s blood pressure.
Of course, this is complicated by the individual patient presentations you may encounter. The critical APO patient with extremely poor perfusion and severe respiratory distress will benefit more from quick application of CPAP rather than delaying it to first try a non-rebreather mask and performing a 12 lead ECG.
Factors to consider when deciding how to prioritise treatment are:
1. Patient Trajectory- ie. without appropriate and timely treatment, what will happen to the patient? If there is a risk of the patient deteriorating, then interventions to prevent and prepare for this become more crucial. In the event of a patient going downhill, you want the patient positioned appropriately, IV access obtained and airway and respiratory equipment at hand.
2. Time Criticality- Does the patient need an intervention NOW, or do they need definitive care more? An easy example is airway management. If the patient’s airway is occluded, they are time critical. It makes zero sense to muck around with IV access or drawing up medications until the airway is patent and the patient can be oxygenated effectively. A clear understanding of assessment systems like the primary survey provide a good guide of what immediate life threats are. This makes it pretty easy to determine what treatment needs to occur at what point in time to treat the patient properly.
3.Treatment Benefits- Conversely, if the treatment holds little benefit to the patient pre-hospitally and they require more urgent management at hospital (either because they don’t require emergency care OR they are transport critical), then down the priority list it goes.
4. Ability to Manage the Underlying Cause- This goes hand in hand with treatment benefits. If you have the ability to manage the underlying cause, then depending on patient’s presentation treating the cause of their condition becomes the priority. A perfect example is hypoglycaemia. Once the underlying cause is addressed then the patient’s symptoms should resolve, making anything other than addressing their blood glucose levels irrelevant. The headache experienced as a result of a low BGL is not a priority until the sugar levels are managed to an appropriate level.
5. Length of Time Needed to Perform an Intervention- This is a tricky one to work out because it can be applied in different ways. An OPA is a good example of a quick airway adjunct that can effectively manage an airway. It can be done within seconds, allowing for other interventions to be started, making it easy to prioritise. However, in a different situation it may be more important to do the longer task first. Refer back to the APO patient. CPAP takes longer to set up than a non-rebreather, however for that critical patient it is more beneficial to spend longer setting up the CPAP mask and starting it ASAP than it is to start with a non-rebreather (which could be ineffective) and then move on to CPAP. This again comes down to how much benefit the treatment carries and how many people you have available to initiate treatment.
6. Patient and Paramedic Safety- It should always be on your mind but it never is until you are actually out on road making the decisions. If a patient is having a seizure in a bathtub full of water, is it more important to give Midazolam or to remove the patient from potential risk of drowning? Likewise, is it more appropriate to begin treating a patient with a non-life threatening problem outside in a thunderstorm or move them into the ambulance? It may be most appropriate to give analgesia and splint a broken leg in the rain, then move the patient and continue to treat minor injuries afterward. These are pretty clear cut examples, but they are legitimate considerations when prioritising tasks.
51 notes
·
View notes
Text
2019
Wow, it's been a while since I have had the opportunity to fully engage with this page. But with 2019 upon us, and soon to be out working as a qualified paramedic, I'm renewing my commitment to continuing learning and to increasing my exposure to better develop as a paramedic. It's time to go back to the same level of information shared when I began this page, and not just sharing posts with no additions. I'm also looking into running scenarios on this page, allowing students to expand their knowledge and have a crack at putting it all together.
May you all have a wonderful year and I hope that this page can provide some awesome opportunities for you all to grow!
12 notes
·
View notes
Photo


My task is to provide to the utmost limits of my capability the best possible care to those in need of my aid and assistance.
To this end I will aid all those who are needful, paying no heed to my own desires and wants; treating friend, foe and stranger alike, placing their needs above my own.
To no man will I cause or permit harm to befall, nor will I refuse aid to any who seek it.
I will willingly share my knowledge and skills with all those who seek it.
I seek neither reward nor honor for my efforts for the satisfaction of accomplishment is sufficient.
These obligations I willingly and freely take upon myself in the tradition of those that have come before me.
94 notes
·
View notes
Text
Scholarships, Support and Student Services
I recently asked you all what you'd like to see more of on this page. One really good point that was mentioned was that there's not much advertising about the what you, as a student, can access to get the most out of uni. As such, I want to run through some things that will helpfully set you up.
1. Scholarships: Every university has an abundance of these. They can be funded by the School (eg. health sciences), student association, privately, or by an external organisation. Some are one off and some are annual, some can be applied for and received several times. It takes a little bit of time to sift through these and find ones that you are eligible for, however it's definitely worth doing, and bookmarking the page. It's really important to note that not all scholarships are about your grades, so don't feel that you can't access them because you don't have the highest GPA. I utilised my university's travel and training grant to fund a trip to Melbourne for a conference (hint: check out @Student Paramedics Australasia's annual conference, and it must be good because I'm not getting paid to plug these guys).
2. International Placements: Really keen on going overseas to learn about other healthcare systems and get hands on? You don't have to have parents who bought you a Mini Cooper for your 18th to do it! Yet another blessing here in Australia is the existence of OS-HELP, which is an option to fund an international placement on your HECS. It does have certain requirements, however if you're accessing a university-supported trip (I know of ones run to the US, Fiji, Vanuatu, UK and Canada) these are usually designed to meet those requirements. You can find out more here: https://www.studyassist.gov.au/…/os-help-loans-and-overseas…
Additionally, find your relevant uni's "Study Overseas" page to see what experiences are out there, they'll also have info re. loans and other financial support.
3. Tutoring: Consider volunteering a little bit of your time to tutoring or study groups with others. IT'll provide you a great opportunity to learn from others, hash out any confusing concepts and get some extra skills practice in. The other major benefit in this is that on road you will expected to communicate and work well with others, and this is a really helpful way to develop these skills.
4. Hardship/Financial Support: Many universities offer hardship schemes and bursaries to cover expenses such as accomodation and textbooks. You can also access a range of financial services through the uni to assist you in balancing uni with financial challenges. Some uni's will offer emergency funding, and if you're in a really hard spot with food- most campuses will have a donated food cupboard to keep you on your feet.
5. Disability Services/Counselling/Healthcare: Every university has disability services which can assist you if there are any areas in which you feel like you need further support. Additionally, nearly all universities offer a free amount of counselling sessions per year (really beneficial for help in managing stress and de-stressing if you had a confronting experience on placement). Some universities have bulk-billing clinics that you can attend, taking a lot of stress out of managing health and wellbeing along with everything else going on in life.
18 notes
·
View notes
Text
RESOURCE THREAD!
As you’ll occasionally hear me rant, I’m a massive believer in sharing information freely.
As such, it’s time for you guys to help each other out by contributing links to the best pages, YouTube channels, blogs, websites, online articles, textbooks and any other resource you like! I’ll pin the post so everyone can refer to it at any time.
Get sharing!
6 notes
·
View notes
Photo
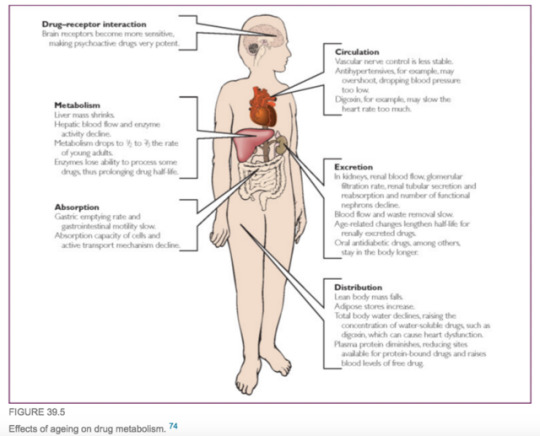
Changed Drug Metabolism for Older Populations
34 notes
·
View notes
Text
GTN Administration
Be aware that Viagra (Sildenafil) is also used in the management of pulmonary hypertension! As this can lead to APO, RVH and increase risk for ACS, it’s extremely important to know.
This is a good reminder of why it’s important to know the generic name of drugs, not just the trade name.
22 notes
·
View notes
Photo
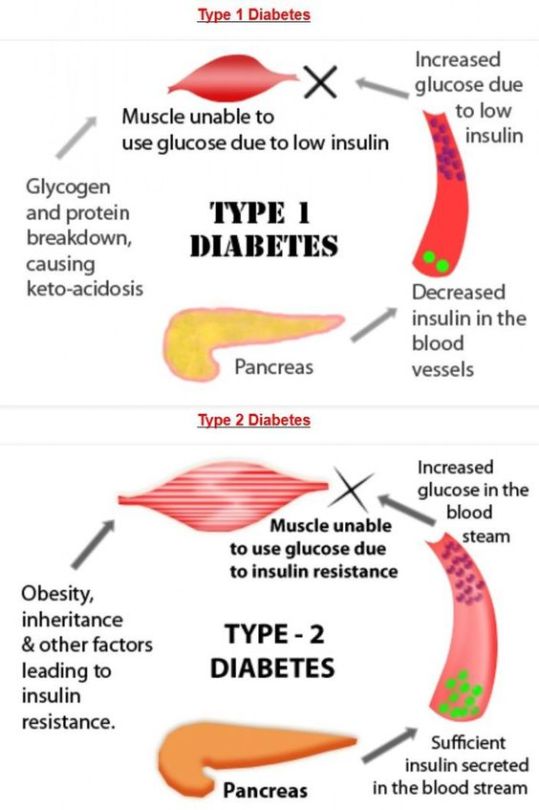
An important part of the pathophysiology of diabetes is the role of insulin in glucose metabolism. Remember that insulin is a hormone-a chemical messenger that operates as the "key" to allow glucose to enter cells and undergo aerobic respiration.
The image is slightly inaccurate- Type 1 Diabetes has "insulin insufficiency" aka little or NO insulin available.
118 notes
·
View notes