#telehealth implementation
Text
Telemedicine in Acute Care: Market Dynamics and Growth Prospects
The global acute care telemedicine market is expected to reach USD 60.2 billion by 2030, based on a new report by Grand View Research, Inc. The market is expected to expand at a CAGR of 14.8% from 2022 to 2030. Technological development in the healthcare sector, increasing demand for immediate access to medical care, and shortage of specialty physicians especially in developing countries are some factors driving telemedicine growth in an acute care setting.

Acute Care Telemedicine Market Report Highlights
Based on delivery, the clinician-to-patient segment accounted for the largest market share of 62.5% in 2021 as it provides easy access to medical professionals through chat or video conferencing and reduces long waiting and travel times to get treatment.
The telepsychiatry segment is expected to witness the fastest CAGR of 15.5% over the forecast period. The sector is witnessing significant growth as it holds the potential to become a better option to traditional in-person psychiatric facilities.
Based on the end-use, the hospitals and clinics segment dominated the market with a revenue share of 75.5% and is likely to grow at the fastest growth rate from 2022 to 2030. This is owing to the shortage of specialist physicians, especially in developing countries, and increased demand for better healthcare access among the people.
North America accounted for the largest revenue share of nearly 42.4% in 2021. Due to a favorable reimbursement structure and the availability of telemedicine services. For instance, In January 2021, The American Telemedicine Association (ATA) and the Digital Medicine Society (DiMe) launched “IMPACT” a new program for virtual healthcare.
The Europe market is anticipated to witness rapid growth over the forecast period with a CAGR of 15.2%. The increase in the elderly population and increased development in the healthcare infrastructure is driving the regional market expansion
Gain deeper insights on the market and receive your free copy with TOC now @: Acute Care Telemedicine Market Report
The COVID-19 pandemic caused the healthcare system to encounter various challenges. The swift adoption of various technologies across countries, driven by the necessity to provide continued medical care in the era of social distancing, has increased the penetration of telemedicine in acute care. In addition, the Centers for Medicare & Medicaid Services (CMS) increased the coverage of telehealth services through temporary waivers soon after the declaration of COVID-19 as a public health emergency in early 2020 to make it convenient for people to receive medical care while reducing their exposure to the virus in public settings such as hospitals and health care facilities.
Furthermore, the World Health Organization and the International Telecommunication Union (ITU) collaborated to produce a universal standard for the usage of telehealth services to address the problem on an international scale. This guideline describes the technological criteria that a telehealth platform must fulfill to deliver accessible telehealth services.
In December 2021, Five Ascension Texas facilities collaborated with the nation’s major multispecialty telemedicine group to offer teleneurology services to their patients. The collaboration was intended to ensure 24/7 access to special neurology care. It will also strengthen on-site neurology treatment by offering doctors, nurses, and other professionals high-definition video consultations with neurologists on demand.
#Telemedicine#Acute Care#Health Tech#Virtual Healthcare#Telehealth#Remote Consultation#Medical Technology#Healthcare Innovation#Patient Care#Digital Health#Telemedicine Solutions#Telemedicine Trends#Telemedicine Services#Telemedicine Benefits#Telehealth Platform#Telemedicine Providers#Telemedicine Implementation#Telemedicine Strategy#Telehealth Solutions#Telemedicine Ecosystem
0 notes
Text

Telehealth Software & Solution Development Company
#telehealth development company#telehealth Software technology#telehealth Development services#telehealth software#telehealth Development platform#custom telehealth solutions#remote monitoring telehealth software#telehealth implementation development#telehealth software systems#telehealth app developers#telehealth app development company#telehealth app
0 notes
Text
#telehealth development company#telehealth Software technology#telehealth Development services#telehealth software#telehealth Development platform#custom telehealth solutions#remote monitoring telehealth software#telehealth implementation development#telehealth software systems#telehealth app developers#telehealth app development company#telehealth software technology#telehealth app
0 notes
Text
So, in Brazilian healthcare news, the Bolsonaro government has made budget cuts of 60% to the Health Ministry, affecting programs of HIV/AIDS treatment, resources for medical residencies, indigenous healthcare, and other programs.

If added together, the losses of resources in 12 programs reach R$ 3.3 billion (~US$ 640 million):
Purchase, production, and distribution of medicines for HIV/AIDS treatment lost R$ 407 million (US$ 78.27 million);
The cost of grants for medical residents covered by the program “Pro-Medical Residency and Multiprofessional Area” lost R$ 922 million;
Promotion, Protection and Recovery of Indigenous Health and Structuring of Health Units and Special Indigenous Health Districts (DSEI) to Serve the Indigenous Population - R$ 910 million (~US$ 175 million)
The Doctors for Brazil program, that aims to take doctors to areas with difficult access and little healthcare, lost R$ 366 milion (~US$ 70.39 million);
Implementation of Policies for Health Promotion and Care for Chronic Non-Communicable Diseases (NCDs) lost R$ 3.8 million (~US$ 730,000);
Research, Technological Development and Innovation in Health lost R$ 297 million (~US$ 57.12 million);
Food and Nutrition for Health lost R$ 43 million (~US$ 8.27 million);
Health Education and Training lost R$ 76 million (~US$ 14.62 million);
Information and Communication Technology Systems for Health (e-Health) lost R$ 206 million (~US$ 39.62 million);
Implementation and Operation of Digital Health and Telehealth in the Unified Health System (the country's universal healthcare network) lost R$ 26 million (~US$ 5 million);
Health Care for Riverside Populations and Remote Areas in the Amazon Region lost R$ 10 million (~US$ 1.92 million);
Implementation of Policies for Stork Network and Implementation of Policies for the Maternal and Child Care Network lost R$ 28 million (~US$ 5.38 million).
The cuts have been implemented in order to save money for the Secret Budget, priority expenses for a select group of lawmakers, included by way of a little-understood mechanism known as “rapporteur-designated budgetary grants” (in simplified terms, it works as a "purchase" of legislative support by the executive branch with money for amendments).
(x)
#brazil#politics#healthcare#brazilian politics#jair bolsonaro#hiv aids#indigenous rights#workers' rights#mod nise da silveira#image description in alt#translations and summaries
23 notes
·
View notes
Text
Understanding the many ways hospitals responded to COVID-19

Hospitals are used to managing disease outbreaks, but the pandemic went beyond anything they had experienced before. Especially in the early days, they rushed to enact new protocols and come up with creative strategies that would allow them to treat an influx of COVID patients while also keeping all their patients and staff safe.
A new paper looks at which responses were used most widely and consistently by hospitals during the first year of the pandemic. The goal is to better understand which strategies were considered useful so that hospitals can use that information to inform their disaster preparedness for a future pandemic. The paper was co-authored by Ruth Pobee, a senior research specialist in the College of Medicine, and colleagues.
The team sent weekly surveys to 17 hospitals across seven states to learn what strategies they were using at that time. The results showed, for example, that strategies like limiting the number of staff in rooms with patients with COVID and increasing the volume of telehealth visits for other patients, were both common and endured over the course of the year. This, the researchers write, likely means the strategies were considered effective and feasible across different types of institutions and locations. Other strategies, such as canceling surgeries or removing medical students from clinical rotations, were commonly tried but then dropped, suggesting they were not considered sustainable.
The authors write: “This study describes a broad collection of hospital operational modifications used in response to a pandemic and identify those that may have been seen as most effective, feasible and/or sustainable by the organisations implementing them. This may provide an expanded reference for institutions facing pandemics in the future.”
To learn more, read the full paper in BMJ Open.
Photo by Piron Guillaume on Unsplash.
2 notes
·
View notes
Text
State of the UC Union
Unified Communication and Collaboration (UC&C) is a combination of various communication methods and collaboration tools such as virtual whiteboards, real-time audio and video conferencing and enhanced call control capabilities to improve efficiency in the workplace. It provides a collection of easy-to-use solutions that can be implemented in various organizations to ensure that the end user receives a nearly real-time collaboration experience that works efficiently, smoothly and securely.
Video collaboration has been evolved from hardware-based codecs of traditional Polycom and Cisco Systems to more software driven solution of Microsoft Teams, Zooms, Google Meets, WebEx, post the pandemic. A lot of the solutions have now been replaced with simpler easier to deploy solutions for small meeting rooms, mid-size meeting rooms as well as larger boardrooms, meeting rooms, training rooms and large venue spaces such as Auditoriums and event spaces. However, the challenges of designing, executing and implementing the technologies and the user experience still remain. The intend of this whitepaper is to ensuring the reader to make the right decision based on today’s available technology. Video conferencing has become an increasingly important aspect of today’s world, as many organizations are transitioning to hybrid working environments. It has greatly aided in connecting people over a phone call where people can experience real-time video conferencing features while being located in different remote locations which would not be possible with Video conferencing platforms.

Types of Video Conferencing:
Telepresence Video Conferencing System
Integrated Video Conferencing System
Desktop Video Conferencing System
Video Collaboration Platforms:
Zooms
Microsoft Teams
Google Meets
Cisco
WebEX
What are Native and Non- Native Solutions. Why is it important in a Video Collaboration system?
Video conferencing is a live audio-visual connection between two or more remote parties over the internet that simulates a face-to-face meeting in real-time. In the business world, desktop video conferencing is a core component of Unified communications platforms that also include calling and messaging capabilities. Standalone on-premises and cloud-based video conferencing platforms are also available from numerous vendors who support desktop and room-based Video conferencing solutions with the ability to embed them into business applications, such as Telehealth, customer service and distance learning, etc.
The Primary difference between a Native and a Non-Native system is the user experience. Post Work from home and Back to office systems imply that the end users wants a user interface (IPAD, OEM’s touch panel, etc..) to have the same familiar look and feel that they are dialing/ joining directly from their laptop. Native user experiences also allow for a seamless connection to users within the enterprises in terms of a active directory integration as well. These native integrations have to be certified by the certified solution provides (Microsoft Team, Zooms, etc…) as a part of being through the ecosystem.
Though more expensive, native systems offer a more seamless experience to the management. Non-Native systems can be simply a Video collaboration bar in a room with a PC behind the display, essentially the PC is a desktop/ user laptop that allow content sharing as well as dialing/joining into the enterprise (As the main UC Engine). Non-native applications are easy to deploy, lower cost to maintenance as well.
Differences between Native and Non-Native Solutions
Hard Codec Running Native UC Platform Modes UC hardware often runs in “Native Mode,” meaning that the built-in Windows/Mac or Android computer is running a single UC Platform application such as Microsoft Teams or Zoom. The system is “locked in” to that platform. This is a great option if your business is already using a soft client version on employees’ laptops, as you essentially just extend this experience to the meeting room. Employees can then make a Zoom call from their laptops, or a Zoom call from a conference room’s dedicated “Native” platform. They are already familiar with the UI and so the transition to a hardware version feels seamless.
Soft codec Running Native UC Platform Modes
Soft codec systems are more commonly known as cloud or web-based video conferencing software. They’re “soft” as they don’t need codec hardware to work, and “codec” refers to devices or programs that compress and decompress data. It just needs a USB peripheral device such as USB camera, USB microphone and thin client PC in which all the software platforms can be loaded and they can initiate the call using wireless keyboard and mouse.
Unified Communication & Collaboration Tools for Native Interface
Zoom Rooms Zoom Rooms, the Modern Hybrid workspaces for Teams, brings HD video collaboration into any space – in the office, the classroom, or at home – and allows in[1]person and remote participants to interact in real-time. Zoom Rooms are the conference room experience you’ve always wanted, making it simple to start a meeting, book a room, and share content. Bring high-quality video, audio, and web conferencing to any sized room or workspace. Advanced features like Zoom Kiosks (virtual receptionist), voice commands & room controls on your mobile device. Enabling the hybrid workforce with features like Smart Gallery and Workspace Reservation. Google, Office 365 & Exchange calendar integrations support room booking, room status, upcoming meetings list, and more.
Workspace Reservation
Wireless sharing with proximity detection
Scheduling Displays
Digital Signage
Smart collaboration tools to keep projects moving Work from anywhere
Microsoft Teams
Microsoft Teams is an enterprise-ready unified communications (UC) platform. Teams connects people everywhere, on Windows MAC and other operating systems including mobile devices, as part of their everyday productivity experience. Microsoft Teams provides a consistent, single client experience for presence, instant messaging, voice, video and a great meeting experience. Microsoft Teams goes beyond communication. Easily find, share and edit files in real-time using apps like Word, PowerPoint and Excel inside Teams.
Chat: Share your opinion and your personality, send gifs, stickers and emojis in a group chat or in one-to-one messages.
Meet: Microsoft Teams offers real-time video conferencing. Host online meetings from 1:1, teams and live events up to 10,000 people.
Call: Make and receive calls with internal and external groups using Microsoft Teams Calling, Phone System, Calling Plan, or Direct Routing.
Collaborate: Store, share and edit files in real-time using apps like Word, PowerPoint and Excel in Microsoft Teams.
Digital whiteboard camera technology Kaptivo
Collaborate with remote team members with secure whiteboard/Interactive Display live sharing and video conference integrations.
Connect via Video Conference or Web Browser
Share Livestream of Whiteboard
Secure Whiteboard Image Capture
Save Snapshots and Track Changes
Kaptivo Cast
The Kaptivo Cast HDMI converter pairs with your Kaptivo to livestream vibrant, unobstructed whiteboard images to any HDMI capable input including traditional video codecs, displays, projectors, or lecture capture systems.
With the Kaptivo Cast, Kaptivo seamlessly integrates into meeting systems from all leading providers.
Quantum Leap Lite
The Leap Lite for Conference Room with Mounting Bracket is a step forward in conference cameras.
It features the camera and a display bracket mount that enables mounting your camera to the top or bottom of most display screens and monitors.
The lens of the leap lite with a 110-degree field of view that is suitable for most meeting or conference rooms.
No drivers are required to work on Linux, Windows, Android etc., the leap lite is also compatible with virtually all collaborative software platforms. And it connects your computer via USB, which makes it a simple plug[1]and-play video conference solution.
Quantum 4k PTZ camera with Condor Microphone
The advantages of Quantum camera is they provide stable product quality, 4k PTZ Camera from Value HD is the most cost-effective solution to provide effective communication.
With video in 4K Ultra HD and 82 degrees wide-angle lens, you can enjoy a superior resolution for all of your video conferences.
The 12X Optical Zoom is smooth and rapid and it delivers close-ups with superior resolution. With its patented 4K ISP solution, the lens of this PTZ camera can be controlled from a remote location. The software (Skype for business, Microsoft teams etc.) will be loaded in the thin client PC.
Display to be used to show Far end and Near end participants. During this mode Phoenix beamforming microphone with hemispheric pickup pattern in the room will get activated for audio pick up and reinforcement of far end audio shall be done via ceiling speakers.
The Phoenix Microphone is created with the vision of a clutter free conference table, the Condor sits above or below your monitor and with a pick-up range of up to 30 ft almost any conference room can use the Condor.
Conclusion
Enterprises today face a range of options, and we feel the top five takeaways are as follows:
Understand your vision for the Unified Collaboration rollout for your enterprise well in advance. (Spend time planning.)
Do trial runs with different manufacturers and end users to understand what works and what doesn’t across a range of budgets.
Deploy in small batches.
Understand the long-term value of the system as well as the compatibility with other systems that may come along the way that we may feel are going to be more software-driven.
Collect and analyze data around usage patterns using room schedulers, sensors on clouds, and analytics platforms to assist in improving the user experience as well as assisting with remote asset management and remote deployments.
To know more you can always contact Allwave AV on [email protected] or call us on 9372374450.
To view the complete document for State of the UC Union click here.

2 notes
·
View notes
Text
The United States has long struggled with a health care system that is both expensive and often inaccessible when it comes to providing certain populations with equitable care. The White House and Congress acted quickly to transition patients to telehealth during the height of the COVID-19 pandemic. However, the future adoption and use of telehealth will depend on how the U.S. health care system addresses coverage and reimbursement, medical licensure, and service modalities. Equally important is policy coherence, or a “telehealth 2.0 roadmap”, to effectively harmonize the goals of value-based care, health disparities, and digital access. This approach to telehealth can improve patient outcomes, offer more inclusive telehealth adoption, and increase ways in which health care is delivered and received as the nation continues to mitigate the public health crisis.
In this paper, we propose flexibilities within the current health care system that accommodate the changes imposed by new technologies, as well as continued government incentives to drive more competitive options and alternatives for health care delivery. In the end, we argue that government must continue to promote the use of remote health care and leverage national investments in broadband infrastructure to drive the complementary use of telehealth with traditional health care. We also propose that current modality flexibilities remain in place, especially as the nation undergoes efforts to close the digital divide. Finally, telehealth must be positioned and implemented in coordination with value-based payments to ensure patient access to meaningful care that can be bolstered and not substituted by existing and emerging health care technologies.
2 notes
·
View notes
Text
Understanding Mental Health Services in Ontario
Emotional well-being is a vital part of in general prosperity, influencing people’s thought process, feel, and act. In Ontario, the importance of Mental Health Services Ontario has gained significant attention, leading to the development of comprehensive services and support systems designed to address mental health challenges. This blog explores the state of mental health in Ontario, available services, recent initiatives, and how individuals can access the support they need.
The State of Mental Health in Ontario

Mental Health Services in Ontario
Ontario offers a wide range of mental health services aimed at providing care, support, and treatment for those in need. These services are designed to be accessible and effective, catering to various age groups and mental health conditions. Here are some key services available in Ontario:
Primary Care Providers
Description: Family doctors and general practitioners often serve as the first point of contact for individuals experiencing mental health issues. They can provide initial assessments, prescribe medications, and refer patients to specialized services.
Community Mental Health Services
Description: Community-based organizations offer a range of services, including counseling, support groups, crisis intervention, and case management. These organizations are essential for providing localized support and resources.
Specialized Clinics and Hospitals
Description: Ontario has numerous specialized clinics and hospitals dedicated to mental health care. CAMH, for example, is one of the largest mental health and addiction research centers in Canada, offering inpatient and outpatient services, as well as research and education programs.
Telehealth and Online Services
Description: With the advent of technology, telehealth services have become increasingly important. Platforms like BounceBack Ontario provide free, guided self-help programs, and virtual counseling sessions, making mental health support more accessible.
Crisis Services
Description: For immediate support, Ontario offers crisis hotlines and mobile crisis units. Services like the Ontario Mental Health Helpline and the Distress Centres of Greater Toronto provide 24/7 support for individuals in crisis.
Recent Initiatives and Programs
Ontario has launched several initiatives to improve Mental Health Services Ontario and reduce the stigma associated with mental health issues. Here are a few prominent projects and drives:
Mental Health and Addictions Strategy
Description: The Ontario government has implemented a comprehensive strategy to improve mental health and addiction services. This strategy focuses on early intervention, better access to services, and increased support for individuals and families.
Mind Beacon and Other Digital Solutions

School-Based Mental Health Programs
Description: Recognizing the importance of early intervention, Ontario has introduced mental health programs in schools. These programs aim to educate students about mental health, provide counseling services, and create a supportive environment for young people.
Workplace Mental Health Programs
Description: Employers in Ontario are increasingly recognizing the importance of mental health in the workplace. Programs and policies promoting mental well-being, stress management, and access to mental health resources are being implemented across various industries.
How to Access Mental Health Services
Navigating the mental health system can be challenging, but several resources are available to help individuals access the support they need:
Family Doctor: Start by talking to your family doctor, who can provide initial assessments and referrals to specialized services.
Community Health Centers: Many communities have health centers offering mental health services, including counseling and support groups.
Online Resources: Websites like Ontario.ca and CAMH.ca provide comprehensive information on available services, self-help tools, and contact information for support organizations.
Helplines: Utilize helplines such as the Ontario Mental Health Helpline (613–879–6122) for immediate support and guidance on accessing services.
Conclusion
Mental health is an integral part of overall health, and Ontario has made significant strides in providing comprehensive services to support individuals facing mental health challenges. From primary care providers to specialized clinics and digital solutions, the province offers a range of resources designed to meet diverse needs. By increasing awareness and improving access to mental health services, Ontario is fostering a more supportive and understanding environment for those affected by mental health issues. If you or someone you know is struggling, don’t hesitate to reach out to the available resources and take the first step towards better mental health.
#Psychological Assessment Ontario#ADHD assessment Ontario#Mental Health Services Ontario#Cognitive Behavioral Therapy Online#Cognitive Behavioral Therapy Ontario#Christian Counselling Ontario#Mental Health Ontario
0 notes
Text
The Rise of Telehealth Consultation in UAE: What You Need to Know
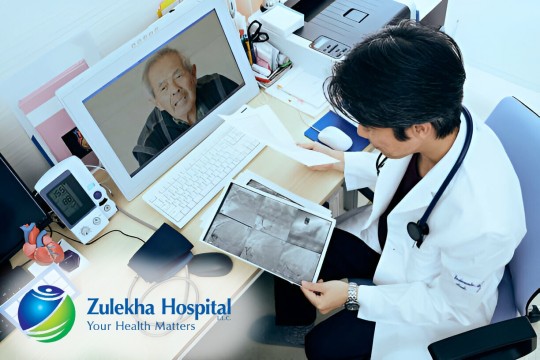
Telehealth consultation in the UAE has rapidly gained popularity, offering a convenient and efficient way for patients to access medical care. This innovative approach leverages digital technology to connect patients with healthcare providers, eliminating the need for physical visits. Particularly in the UAE, where accessibility and cutting-edge healthcare are priorities, telehealth has become an essential service.
Zulekha Hospital, a renowned healthcare institution in the UAE, has been at the forefront of implementing telehealth solutions. Their telehealth services provide patients with easy access to expert medical advice, follow-up consultations, and second opinions from the comfort of their homes. By using secure video conferencing and online platforms, Zulekha Hospital ensures that patients receive timely and personalized care without the hassle of travel.
This service especially benefits those with chronic conditions, elderly patients, and individuals living in remote areas. It also plays a critical role during public health emergencies, such as the COVID-19 pandemic, by reducing the risk of infection transmission.
Overall, telehealth consultation in the UAE, exemplified by Zulekha Hospital's offerings, represents a significant advancement in the healthcare landscape, enhancing patient experience and outcomes through innovative technology and accessible care.
0 notes
Text
How to Improve The Case Acceptance Rate of Your Dental Office? | mConsent
Achieving a high case acceptance rate is not only pivotal for the financial health of a dental practice, but it also signifies a strong patient-provider relationship built on trust and effective communication. As a dental professional, it's essential to employ strategic approaches that empower patients to make informed decisions about their oral health.
This blog will delve into a comprehensive guide on how to bolster the case acceptance rate in your dental office, encompassing a range of techniques from honing communication skills to leveraging modern technology and fostering a patient-centric environment.
In a landscape where patient satisfaction and trust are paramount, it's imperative to establish a dental practice that not only offers top-tier clinical care but also prioritizes patient education and comfort.
By implementing the following strategies, you'll not only witness an uptick in case acceptance but also cultivate a thriving practice that leaves a lasting positive impact on your patients' oral health journey.
1. Build Strong Patient Relationships
Any effective healthcare practice relies on patient interactions. Active listening and real empathy help patients feel heard and respected. Kindly addressing their issues and offering accurate information builds trust. Involving patients in decision-making and respecting their autonomy helps them to manage their own treatment.
Regular follow-ups and individualized communication strengthen this relationship. Healthcare practitioners prioritize these relationships to make patients feel supported, understood, and confident in their treatment, which improves health outcomes and patient satisfaction.
2. Enhance Communication Skills
Communication skills are crucial in healthcare. It requires clear communication, active listening, and empathy for patients. Strong communication skills can help patients feel comfortable discussing their problems and questions with a doctor.
This improves informed and collaborative decision-making. Effective communication helps patients feel heard and understood, building trust.
It also helps doctors explain difficult medical information to patients, keeping them informed about their problems and treatment alternatives. These abilities are essential to providing high-quality treatment and building strong patient-provider relationships.
3. Utilize Technology
In today's rapidly advancing healthcare landscape, harnessing the power of technology is essential for delivering efficient and effective patient care. Electronic health records (EHRs), telemedicine platforms, and digital diagnostic tools streamline the sharing of vital patient information, enhance collaboration among healthcare teams, and enable remote consultations.
Moreover, technology facilitates timely communication with patients through secure messaging systems and telehealth visits, ensuring that their needs are met even outside of traditional office hours. Automated appointment reminders and prescription refill notifications further improve patient engagement and adherence to treatment plans.
Embracing these technological advancements not only enhances the overall patient experience, but also leads to more seamless and precise healthcare delivery, ultimately benefiting both providers and patients alike.
4. Provide Comprehensive Treatment Plans
Comprehensive treatment programs are essential to optimal healthcare. It entails a complete health evaluation, including medical history, present status, and preferences.
A well-designed treatment plan details the processes, procedures, and interventions needed to meet the patient's demands and improve health. This encompasses urgent and long-term preventative treatment and health maintenance methods.
Healthcare practitioners provide patients a holistic picture of their healthcare journey by delivering a thorough treatment plan, encouraging confidence in the planned course of action and developing a sense of collaboration in their own well-being.
This ensures patients receive the best, coordinated, and tailored treatment, improving health and satisfaction.
5. Offer Financing Options
Offering alternative funding choices in healthcare helps patients obtain and afford care. Clear and accessible financing alternatives reduce medical price stress for people and families. Payment plans, in-house finance, and third-party financing are examples.
These options show that healthcare providers want to make it affordable for everyone. This method improves patient well-being and the practice's reputation, generating community trust and loyalty. A win-win situation improves patient outcomes and grows a healthcare practice.
6. Show Before-and-After Imagery
Before-and-after images are significant in dentistry, dermatology, and plastic surgery. These images demonstrate how treatments or surgeries change lives. They demonstrate the healthcare provider's technical ability and reassure potential patients.
Real-life instances of accomplishment can ease concerns and demonstrate the possible advantages. Before-and-after images also educate patients about treatment outcomes. It strengthens patient-provider relationships and ensures informed decision-making by fostering trust and openness.
By adding this visual aspect to consultations, healthcare practitioners boost patient happiness and demonstrate their dedication to quality treatment.
7. Focus on Patient Education
High-quality healthcare starts with patient education. It entails giving patients the information and skills to make health and wellness decisions. Explaining diagnosis, treatments, and preventative actions in simple terms is possible. Visuals, instructional resources, and interactive examples assist comprehension.
Healthcare practitioners enable patients to actively engage in their treatment by educating them. Informed patients are more likely to follow treatment regimens, adopt healthy habits, and improve their health.
This emphasis on teaching promotes the patient-provider connection and makes patients more informed and involved. Comprehensive and patient-centered healthcare requires it.
8. Address Concerns and Questions
Addressing concerns and queries is key to patient-centered treatment. It starts with a friendly, open environment where patients may share their concerns. Actively listening and validating their issues builds trust and confidence.
Avoiding medical jargon, doctors should explain things clearly, honestly, and simply. This procedure reduces anxiety and equips people to make health decisions. Healthcare professionals improve patient confidence, engagement, and satisfaction by emphasizing concern and inquiry resolution.
9. Create a Pleasant Experience
Patient satisfaction is crucial to quality treatment. From reception to treatment room, it should be warm and pleasant. Comfortable amenities, responsive personnel, and a clean, organized area create a favorable mood. Clear communication, short wait periods, and courteous interactions improve the patient's experience.
Providing reading materials, relaxing music, or refreshments can further enhance the visit. Healthcare professionals boost patient satisfaction and develop a reputation for excellent treatment and professionalism by addressing patient comfort and well-being. Pleasant experiences build trust and loyalty between patients and providers.
10. Follow Up and Follow Through
Following up and following through are essential to complete healthcare. Beyond the first visit or therapy, it shows dedication to patient well-being. Regular check-ins by phone, email, or in-person encounters allow healthcare practitioners to measure progress, resolve problems, and verify treatment plan compliance.
This amount of attention reassures patients and builds trust in their practitioner. It also allows for treatment plan changes to get the greatest results. Dental professionals demonstrate a real commitment to patient health and pleasure by constantly following up.
Conclusion:
In conclusion, improving your dental office's case acceptance rate is vital to its financial health and patient well-being. Building trust, communicating well, and providing tailored care creates an environment where patients feel valued and confident in their treatment plans.
The procedure is simplified and faster for dentists and patients using mConsent, a cutting-edge digital consent solution. The ease of access to treatment information and electronic signatures improves patient participation and knowledge of prescribed procedures.
The effective methods in this blog, and technologies like mConsent increase case acceptance rates and build a reputation for excellent treatment. This creates a successful dental practice that prioritizes patient needs. Expect more "Yes!" as you help people achieve maximum dental health and happiness.
0 notes
Text
Navigating the Waves: How COVID-19 Has Impacted Gastroenterology Practices

Introduction:
In the wake of the COVID-19 pandemic, medical practices across the globe have faced unprecedented challenges. Among these, gastroenterology practices have had to adapt swiftly to ensure patient safety while continuing to provide essential care. From changes in patient management to shifts in procedural protocols, the impact of COVID-19 on gastroenterology has been profound.
Telemedicine Emergence:
One of the most notable shifts in gastroenterology practices has been the rapid adoption of telemedicine. With in-person consultations posing significant risks during the pandemic's peak, telehealth emerged as a vital tool for maintaining patient care continuity. Gastroenterologists swiftly embraced virtual visits, leveraging technology to conduct assessments, offer consultations, and monitor patients remotely. This transition not only ensured patient safety but also increased accessibility to care, particularly for those in remote areas or with mobility issues.
Procedural Prioritization:
The pandemic necessitated a reassessment of procedural priorities within gastroenterology practices. With elective procedures postponed to conserve medical resources and minimize exposure risk, gastroenterologists had to prioritize cases based on urgency and patient need. This led to a focus on essential procedures such as colonoscopies for cancer screening and endoscopic interventions for acute conditions, while non-urgent cases were deferred. Despite these challenges, gastroenterologists worked diligently to ensure that patients requiring time-sensitive interventions received prompt care, albeit with enhanced safety measures in place.
Enhanced Safety Protocols:
Ensuring the safety of patients and healthcare providers became paramount in gastroenterology practices. Enhanced safety protocols were implemented, including stringent infection control measures, pre-procedural screenings, and personal protective equipment (PPE) utilization. Endoscopy units adopted meticulous cleaning and disinfection protocols, while staff members received training on infection prevention strategies. Additionally, patient flow within practices was restructured to minimize crowding and facilitate physical distancing. These measures not only mitigated the risk of COVID-19 transmission but also fostered a sense of trust and confidence among patients seeking care.
Impact on Research and Education:
The pandemic disrupted not only clinical practice but also research and education within the field of gastroenterology. Clinical trials were postponed or modified, affecting the advancement of new therapies and treatment modalities. Similarly, medical conferences and educational events shifted to virtual platforms, altering the dynamics of knowledge dissemination and networking within the gastroenterology community. Despite these challenges, innovative approaches such as virtual conferences and webinars emerged, providing opportunities for continued learning and collaboration amidst the pandemic's constraints.
The COVID-19 pandemic has significantly impacted gastroenterology practices in various ways, affecting both clinical operations and financial stability.
Clinical Impact
One of the major changes has been the postponement of non-urgent endoscopic procedures. Early in the pandemic, gastroenterology societies recommended delaying elective procedures to minimize the risk of COVID-19 transmission, which led to a substantial decrease in procedure volumes. A survey of gastroenterologists revealed that most practices reduced their endoscopy volumes to less than 10% of normal levels during the initial months of the pandemic. Furthermore, nearly all practices implemented telemedicine services to continue patient care remotely (MDLinx).
Gastroenterology practices also adapted by enhancing safety protocols. This included increased use of personal protective equipment (PPE) and screening patients for COVID-19 symptoms before appointments. Despite these measures, the necessity to reduce in-person visits and procedures had a lasting impact on patient care, including delays in routine screenings and a subsequent backlog of procedures (MDLinx).
Financial Impact
Financially, gastroenterology practices faced significant challenges due to decreased patient volumes. Many practices experienced revenue declines of over 50%, with some losing up to 75% of their in-person visits. This financial strain led some practices to close temporarily or reduce their operational capacity dramatically. The reduction in elective procedures, a major revenue source, particularly impacted the financial health of these practices.
Private equity investment in gastroenterology has also increased during the pandemic. This trend has brought about changes in how these practices operate, including higher costs and increased patient volumes, driven by more aggressive marketing and coding practices. However, this shift raises questions about the long-term sustainability and quality of care provided by PE-backed practices (Gastroenterology and Hepatology).
Moving Forward
As the pandemic wanes, gastroenterology practices are dealing with the backlog of postponed procedures. Some have planned extended hours or weekend sessions to address this issue. Additionally, the adoption of telemedicine is likely to remain a permanent fixture, offering patients more flexible and accessible care options (MDLinx) (MGMA Homepage).
Overall, the pandemic has forced gastroenterology practices to adapt rapidly, integrating new technologies and adjusting operational strategies to continue providing care while managing financial and logistical challenges.
Conclusion:
The COVID-19 pandemic has reshaped the landscape of gastroenterology practices, prompting rapid adaptation and innovation. From the widespread adoption of telemedicine to the implementation of enhanced safety protocols, gastroenterologists have navigated these challenges with resilience and dedication to patient care. As the world continues to grapple with the evolving impact of COVID-19, gastroenterology practices remain steadfast in their commitment to providing high-quality care while prioritizing patient safety above all else. Through collaboration, innovation, and unwavering determination, the gastroenterology community will continue to overcome challenges and emerge stronger in the face of adversity.
Important Information:
Conference Name: 14th World Gastroenterology, IBD & Hepatology Conference
Short Name: 14GHUCG2024
Dates: December 17-19, 2024
Venue: Dubai, UAE
Email: [email protected]
Visit: https://gastroenterology.universeconferences.com/
Call for Papers: https://gastroenterology.universeconferences.com/submit-abstract/
Register here: https://gastroenterology.universeconferences.com/registration/
Exhibitor/Sponsor: https://gastroenterology.universeconferences.com/exhibit-sponsor-opportunities/
Call Us: +12073070027
WhatsApp Us: +442033222718
0 notes
Text
Enhancing Patient Care Through Innovative eHealth Solutions
In the rapidly evolving healthcare landscape, the terms "eHealth" and "telemedicine" are often used interchangeably, leading to confusion and misconceptions. However, these two concepts, while related, possess distinct characteristics and applications. This article aims to shed light on the differences between eHealth and telemedicine, enabling a better understanding of their respective roles in transforming healthcare delivery.
Understanding eHealth: A Comprehensive Approach
eHealth, or electronic health, is an umbrella term that encompasses a wide range of technologies and services designed to enhance healthcare delivery, information exchange, and communication. It encompasses various aspects of healthcare, including electronic health records (EHRs), mobile health (mHealth) applications, telehealth, and more.
eHealth app development focuses on creating digital solutions that improve healthcare accessibility, efficiency, and patient engagement. These applications can include patient portals, health trackers, appointment scheduling tools, and remote monitoring systems, among others.
Key Aspects of eHealth:
Data Management and Exchange
eHealth enhances healthcare by improving data management and exchange, facilitating seamless information flow across systems. It centralizes health data electronically, reducing errors and improving care quality. Interoperable systems promote collaboration, enhancing patient outcomes and promoting secure data exchange between healthcare entities.
Patient Empowerment and Education
eHealth is a digital health approach that empowers patients by providing them with resources, educational materials, and tools to actively manage their health. This approach fosters a culture of informed decision-making and self-care, improving patient outcomes and overall well-being through mobile health apps and online platforms.
Healthcare Administration and Management
eHealth is revolutionizing healthcare administration by digitizing administrative processes like appointment scheduling, billing, and inventory management. Electronic health records centralize patient information, enhancing efficiency and workflow. This digital transformation improves coordination among healthcare teams, leading to better patient care and outcomes.
Public Health Initiatives
eHealth initiatives in public health promote population health and preventive care by using digital platforms to disseminate vital information, track disease outbreaks, and implement targeted interventions. They support surveillance systems, health education campaigns, and vaccination programs, enabling authorities to monitor health trends, respond to emergencies, and implement evidence-based disease prevention strategies.
Telemedicine: Bridging the Distance for Remote Care
Telemedicine, on the other hand, is a specific branch of eHealth that focuses on the delivery of healthcare services remotely, leveraging telecommunication technologies. It enables healthcare professionals to evaluate, diagnose, and treat patients without the need for in-person visits, thereby eliminating geographical barriers and increasing access to care.
The development of a telemedicine app involves creating a platform that facilitates real-time audio/video consultations, remote monitoring, and secure data exchange between healthcare providers and patients.
Key Aspects of Telemedicine:
Virtual Consultations and Follow-ups
Telemedicine enables patients to consult with healthcare providers remotely through video or phone appointments, eliminating the need for in-person visits. This feature is particularly beneficial for follow-up consultations, allowing patients to conveniently connect with their doctors from the comfort of their homes. Virtual consultations save time and reduce the risk of exposure to infectious illnesses, especially during the COVID-19 pandemic
Remote Patient Monitoring
Telemedicine facilitates remote patient monitoring, enabling healthcare providers to track patients' health data and vital signs from a distance. This aspect is crucial for managing chronic conditions and post-operative care, as it allows for continuous monitoring and early intervention if needed. Remote patient monitoring can help prevent hospital readmissions and improve overall patient outcomes
Specialist Care Access
One of the significant advantages of telemedicine is its ability to provide access to specialist care, particularly for patients living in rural or underserved areas. Through virtual consultations, patients can connect with specialists who may be located far from their physical location. This aspect of telemedicine helps bridge the gap in healthcare accessibility and ensures that patients receive the necessary care regardless of their geographical location.
Emergency and Triage Services
Telemedicine can also play a crucial role in emergency situations and triage services. Healthcare providers can use virtual consultations to assess patients' symptoms, provide initial treatment recommendations, and determine the need for in-person care. This aspect of telemedicine helps optimize emergency resources and ensures that patients receive timely care during critical situations.
The Relationship Between eHealth and Telemedicine
While eHealth and telemedicine are distinct concepts, they are inextricably linked. Telemedicine is a crucial component of eHealth, leveraging digital technologies to provide remote healthcare services. eHealth encompasses a broader range of applications and services, including telemedicine, but also extends to areas such as health information management, public health initiatives, and patient education.
Unlocking Efficiency with White Label Solutions
For healthcare organizations and businesses seeking to capitalize on the benefits of eHealth and telemedicine, white label solutions offer a streamlined and cost-effective approach. A white label doctor app, for instance, provides a pre-built platform that can be customized and rebranded, enabling rapid deployment of telemedicine services without the need for extensive development efforts.
Similarly, white label eHealth platforms offer a comprehensive suite of features, including EHR management, patient portals, and secure messaging, allowing healthcare providers to enhance their digital offerings efficiently.
The Future of eHealth and Telemedicine
As technology continues to advance, the integration of eHealth and telemedicine will become increasingly seamless, paving the way for a more connected and patient-centric healthcare ecosystem. Here are some exciting trends to watch:
Artificial Intelligence (AI) and Machine Learning (ML) Integration
Internet of Medical Things (IoMT) and Wearable Devices
Augmented and Virtual Reality (AR/VR) in Remote Consultations
Blockchain for Secure Data Management
Conclusion: Embracing the Synergy of eHealth and Telemedicine
While eHealth and telemedicine are distinct concepts, they are complementary pillars of a more efficient, accessible, and patient-centric healthcare system. By understanding their differences and leveraging their synergies, healthcare organizations and businesses can deliver enhanced care, improve patient outcomes, and drive innovation in the industry.
Whether through eHealth app development, telemedicine app solutions, or white label platforms, embracing these technologies is no longer an option but a necessity for healthcare providers seeking to remain competitive and meet the evolving demands of patients in the digital age.
#hire mobile app developers#hire developers#hire app developer#mobile app development#android app development#ios app development#hire flutter developer#flutter app development#telehealth#telemedicine
0 notes
Text
How Do Telehealth Software Solutions Reshape Healthcare Practices?
Telehealth solutions have emerged as a transformative force in modern healthcare, offering innovative ways to deliver care remotely. Let's delve into the world of telehealth software solutions, their significance in healthcare, and the advancements in telehealth technology.
What exactly are telehealth solutions, and how do they reshape the healthcare landscape?
Telehealth solutions encompass a range of technologies and services that enable remote delivery of healthcare services, including consultations, monitoring, and education. These solutions leverage telecommunications technology to connect patients with healthcare providers, regardless of physical distance, facilitating convenient and accessible healthcare delivery.

How do telehealth systems contribute to improving access to healthcare and patient outcomes?
Telehealth systems play a crucial role in overcoming barriers to healthcare access, such as geographic distance, mobility limitations, and provider shortages. By enabling remote consultations and monitoring, these systems empower patients to receive timely care, leading to better health outcomes and reduced healthcare disparities.
What are the key benefits of implementing telemedicine software solutions for healthcare providers and patients?
Telemedicine software solutions offer a multitude of advantages, including:
Increased accessibility to healthcare services, particularly for underserved populations and rural communities.
Enhanced convenience and flexibility for patients, with the ability to schedule appointments and consultations from anywhere.
Improved efficiency and productivity for healthcare providers, through streamlined workflows and reduced administrative burdens.
Cost savings for patients and healthcare organizations, with fewer travel expenses and lower overhead costs.
Facilitation of collaborative care and multidisciplinary consultations, leading to more comprehensive and coordinated patient care.
How has telehealth technology evolved over time, particularly in the realm of telemedicine software solutions?
Telehealth technology has evolved from simple video conferencing tools to integrated telehealth solutions that encompass a wide range of features and functionalities. Early telemedicine software solutions may have been limited in scope, but advancements in telecommunications technology, data analytics, and remote monitoring have paved the way for more sophisticated and comprehensive telehealth systems.
What are some essential features and capabilities of telehealth software systems?
Key features of telehealth software systems include:
Video conferencing capabilities for virtual consultations between patients and healthcare providers.
Secure messaging and file sharing functionalities for communication and collaboration.
Integration with electronic health record systems and other healthcare IT infrastructure for seamless data exchange.
Remote monitoring capabilities for tracking patient vital signs and health metrics.
Customizable workflows and templates to accommodate various specialties and care settings.
What factors should healthcare organizations consider when selecting a telehealth monitoring system?
When choosing a telehealth monitoring system, healthcare organizations should consider factors such as:
Scalability: Ensure the system can accommodate varying patient populations and healthcare settings.
Compatibility: Check for compatibility with existing IT infrastructure and electronic health record systems.
Ease of Use: Select a system with intuitive interfaces for both healthcare providers and patients.
Data Security:
Prioritize systems with robust security measures to protect patient information and ensure compliance with healthcare regulations.
What innovations and advancements can be expected in the future of telehealth solutions?
The future of telehealth solutions holds promise for further integration of artificial intelligence, machine learning, and predictive analytics. These technologies will enable more personalized and predictive care delivery, with real-time data insights and decision support tools. Additionally, advancements in wearable devices and remote monitoring technology will enable more comprehensive and proactive management of patient health.
Conclusion
Telehealth solutions represent a paradigm shift in healthcare delivery, offering convenient, accessible, and efficient ways to deliver care remotely. By leveraging telemedicine software solutions and telehealth systems, healthcare providers can overcome geographical barriers, improve patient access to care, and enhance patient outcomes.
As technology continues to advance and healthcare needs evolve, telehealth solutions will undoubtedly play an increasingly integral role in shaping the future of healthcare delivery.
0 notes
Text
Navigating Delaware's Healthcare Landscape: Exciting Career Opportunities in the Medical Field
In the ever-evolving healthcare landscape, Delaware stands as a beacon of opportunity for those seeking fulfilling careers in the medical field. With a robust healthcare infrastructure, state-of-the-art facilities, and a commitment to innovation, Delaware offers many exciting career opportunities across various specialties.

One of the most appealing aspects of pursuing a career in the medical field in Delaware is the diversity of options available. There are plenty of pathways to explore, each offering unique challenges and rewards. Delaware presents a rich tapestry of career opportunities, from traditional roles such as physicians, nurses, and allied health professionals to emerging fields like telemedicine, medical informatics, and healthcare administration.
Physicians, the cornerstone of the healthcare system, have ample opportunities to practice and specialize in Delaware. Whether it's primary care, pediatrics, surgery, or subspecialties like cardiology, oncology, or neurology, physicians can find rewarding positions in hospitals, clinics, private practices, and academic institutions across the state.
Nurses, often called the heart of healthcare, are critical in patient care delivery. Delaware offers various avenues for nurses to thrive, including positions in hospitals, long-term care facilities, community health centers, and home health agencies. Advanced practice nurses, such as nurse anesthetists, nurse practitioners, and nurse midwives, enjoy autonomy and the ability to provide comprehensive care to patients.
Allied health professionals, including radiologic technologists, respiratory therapists, physical therapists, and medical laboratory scientists, contribute essential services to the healthcare team. With advancements in technology and diagnostics, these professionals are in high demand to support patient care and treatment plans.
Beyond clinical roles, Delaware offers opportunities for individuals interested in healthcare administration, IT, medical research, and public health. Healthcare administrators oversee the efficient operation of healthcare facilities and ensure compliance with regulations. Meanwhile, healthcare IT professionals are crucial in implementing and maintaining electronic health record systems (EMRs), telehealth platforms, and other digital solutions.
Medical researchers contribute to advancements in healthcare by conducting studies, clinical trials, and translational research to improve patient outcomes and develop innovative treatments. In Delaware, research institutions, academic medical centers, and biotechnology companies offer opportunities for researchers to make significant contributions to medical science.
Moreover, public health professionals promote and protect communities' health through disease prevention, health education, policy advocacy, and emergency preparedness initiatives. With a growing emphasis on preventive care and population health, public health careers are increasingly relevant and impactful.
The healthcare landscape offers an exciting Delaware's career opportunity for individuals and professionals passionate about making a difference in people's lives. Whether you're drawn to direct patient care, healthcare administration, medical research, or public health, Delaware provides a supportive environment where professionals can thrive and contribute to advancing healthcare for all. Here, your work is not just a job but a mission to improve the health and well-being of the community, making a lasting impact on the lives of those you serve.
0 notes
Text
The Growing Burden: Strategies to Manage Rising Health Insurance Costs

For businesses of all sizes, health insurance remains a vital employee benefit, attracting and retaining talent while offering peace of mind for workers. However, the cost of employer-sponsored health insurance has been steadily rising, creating a significant financial burden for many companies. This article explores the reasons behind these rising costs and offers strategies businesses can implement to manage them effectively.
Understanding the Why: Factors Driving Up Health Insurance Costs
Medical Inflation: The cost of medical services, medications, and technology is consistently outpacing general inflation.
An Aging Population: As the population ages, healthcare utilization increases, leading to higher overall costs for insurers.
Chronic Conditions: The prevalence of chronic diseases like diabetes and heart disease requires ongoing care, driving up healthcare spending.
Lifestyle Choices: Certain lifestyle factors like tobacco use and obesity can contribute to higher healthcare costs.
Administrative Overhead: The complex healthcare system in many countries involves significant administrative costs, impacting insurance premiums.
Taking Control: Strategies to Manage Rising Health Insurance Costs
Plan Design: Explore different plan designs like high-deductible health plans (HDHPs) paired with Health Savings Accounts (HSAs) to encourage employee cost-sharing and potentially lower premiums.
Wellness Programs: Invest in corporate wellness programs that promote healthy lifestyles and disease prevention, potentially reducing future healthcare needs.
Telehealth Adoption: Encourage the use of telehealth services for appropriate consultations, offering greater convenience and potentially reducing in-person visit costs.
Value-Based Care Models: Consider partnering with healthcare providers who utilize value-based care models, focusing on quality outcomes and cost-effectiveness.
Data Analytics: Leverage data analytics to identify high-cost areas and implement targeted strategies to address them.
Benefits Shopping: Negotiate with different insurance providers and explore alternative benefit options to find the most cost-effective plan for your company.
Employee Engagement: Educate employees about their health insurance plans and encourage them to make informed choices regarding healthcare utilization.
Conclusion:
The rising cost of health insurance presents a significant challenge for businesses. However, by implementing strategic approaches, companies can manage these costs and continue offering valuable health benefits to their employees. By focusing on preventive care, plan design optimization, and data-driven strategies, businesses can navigate the changing healthcare landscape and ensure a sustainable future for their employee health benefits programs.
0 notes
Text
Customizing Patient Care: Unveiling Best Practices inside Patient Scheduling
Introduction:
Effectiveness in healthcare knobs on the excellence of patient arranging, a cornerstone inside the delivery regarding quality care. In this article, we delve into the landscape associated with patient scheduling, revealing proven strategies and best practices that open operational excellence plus enhance patient activities.
1 ) Utilizing Technologies for Scheduling:
Integrating technology revolutionizes patient scheduling, offering accessibility and convenience. https://innovatureinc.com/patient-scheduling-enhancing-patient-experience/ Net and cloud-based devices empower patients to be able to book appointments easily, while platforms love WhatsApp streamline connection. Embracing these electronic digital advancements makes booking more responsive in addition to efficient, catering to the evolving requires of patients and even providers alike.
2. Efficient Appointment Slot machine game Allocation:
Strategic allocation of appointment slot machines optimizes resource utilization and minimizes wait around times. Identifying top and off-peak occasions ensures balanced circulation of appointments, boosting operational efficiency. Components like appointment duration and form of visit are pivotal within achieving a harmonious balance, meeting person needs while increasing provider productivity.
three or more. Minimizing No-Shows and Cancellations:
Reducing no-shows and cancellations needs proactive measures such as strategic reminders, flexible cancellation plans, efficient waitlist managing, and patient wedding. By instilling a sense of responsibility and offering convenience, healthcare features mitigate disruptions and ensure a reliable booking process.
4. Streamlining Check-In Procedures:
Streamlined check-in procedures boost the patient experience by minimizing wait around times and enhancing efficiency. Leveraging technology, implementing user-friendly kiosks, collecting real-time opinions, and integrating with scheduling systems help a seamless check-in process, aligning using patient scheduling best practices.

5. Flexible Scheduling Options:
Adopting flexible scheduling options accommodates diverse sufferer needs, enhancing pleasure and accessibility. Offering extended hours, telehealth appointments, and same-day scheduling caters to individual preferences, fostering a patient-centric approach that streamlines the scheduling process.
6th. Prioritizing Urgent Instances:
Efficient patient flow management ensures quick attention to urgent situations, reinforcing the determination to timely plus responsive care. By simply integrating prioritization methods into scheduling practices, healthcare providers find their way daily operations together with precision, enhancing sufferer satisfaction and functional effectiveness.
7. Frequently Updating Patient Documents:
Maintaining up-to-date sufferer records promotes accuracy and facilitates aggressive outreach. By leveraging real-time data and even business analytics, health-related providers optimize management practices, identify styles, and enhance patient experiences through customized communication and useful resource allocation.
6. Cultivating A Good Waiting Experience:
Lowering wait times and fostering a positive ready experience are important to patient-centered treatment. Clear communication, cozy waiting areas, plus cautious appointment overbooking strategies create the environment where ready becomes an prospect for engagement, education and learning, and relaxation, enhancing overall quality regarding care.
Conclusion:
Unlocking the efficiency involving healthcare begins together with mastering patient organizing best practices. By leveraging technology, optimizing scheduled appointment allocation, minimizing interruptions, streamlining procedures, embracing flexibility, prioritizing urgent cases, maintaining updated records, and creating a good waiting experience, healthcare providers lift operational excellence plus enhance patient fulfillment, ensuring a seamless and rewarding health care journey for all.
1 note
·
View note