#post-viral sequelae
Photo
(via If we don't develop a treatment we're f*cked)
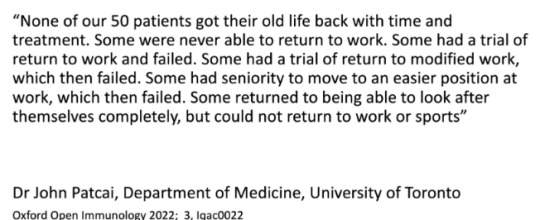
“Not to be a downer, but this is the result of a study researches led at the University of Toronto following SARS1 patients who were disabled by the virus initially and how they were doing 20 years later.“
Screenshot “from the presentation by; Prof. Daniel M. Altmann, Department of Immunology and Inflammation, Imperial College, Faculty of Medicine, London, UK at #UniteToFight2024 https://unitetofight2024.world/program/”
+ important comment:
“A study on SARS 1 survivors, if you're curious:
2023 study in The Lancet on SARS 1 survivors
Lots had femoral necrosis (bone death), osteoporosis, and long-lasting, possibly immunologically-based fatigue.
Just a reminder that while there are similarities, these are two different diseases. SARS CoV 1 hospitalized 70% of infected and killed 10% at the time of containment. They're similar in disease profile and in genetics, but they are NOT the same.
COVID-19 is much more infectious and less lethal, and the range of post-viral complications is different. Plus, we don't know what treatments will come out for Long COVID patients, but medicine is much more advanced and there is much more funding for Long COVID than there was for SARS CoV 1 survivors, who were infected in 2003, and never had access to a vaccine.”
#post-viral illness#viruses#covid#coronavirus#post-viral sequelae#PASC#long covid#SARS1#SARS#me/cfs#immunology#study#reddit#comments#historical#archiving#2022
64 notes
·
View notes
Text

Those of you who have watched The Sandman may not realize that the epidemic mentioned early on in the show, where over a million people were affected by a strange sleeping sickness, encephalitis lethargica, was a real thing. …
It didn’t all happen overnight. The first cases were diagnosed in 1917, and the incredibly odd disease continued to turn up in nations around the world over the following decade. Over 500,000 people are thought to have died from the disease over that period …
But dying wasn’t what really marked out the strangeness of the disease. Many of those affected were trapped in a kind of half-life, neither fully awake nor wholly asleep. They could get up and walk, if assisted. But without intervention would sit silently for days. …
The cause of this disease is still unknown. Because it overlapped the massive flu pandemic, many have suspected that lethargica might be a “sequelae,” an after effect of infection by the 1918 flu virus. This theory has fallen out of favor lately, but remains a possibility. …
Like COVID-19, we largely think of flu as a respiratory disease. However, like COVID-19, flu actually effects a number of organs and systems. A sharp increase in heart attacks coming years, and even decades, later, have been connected to the 1918 flu. …
There is even evidence of decreased life expectancy among children born to infected parents. That’s on top of the millions of infants who died as a direct result. The associated health issues generated economic patterns that could still be detected over 50 years later. …
In addition, just as with COVID-19, “long flu” was common. Many people took years to recuperate from their encounter with that flu. Many never did. Again, there are patterns of poverty that are detectable as a direct result. …
What kind of sequelae will COVID-19 generate, and how will they effect not just individual lives, but our socioeconomic future? Absolutely no one knows. What we do know is that 210,000 Americans have already died from COVID-19 *this year*. Millions are experiencing long COVID. …
In absolutely no sense is this pandemic over. As schools start up in America, everyone seems to be, sadly, shockingly, unforgivably left to make their own decisions. Just remember, what we do now will be with us into the next century.
Oh, and I left out that Encephalitis lethargica had its own sequelae: a worldwide increase in Parkinsonism. This was not a kind disease, whatever its origin.
#like the flu#encephalitis lethargica#sandman#covid#long covid#post-viral sequelae#spanish flu#so fucking tired of that ignorant statement#me/cfs
2K notes
·
View notes
Text
youtube
Getting obsessed with this song not because it's called Golem (well, not JUST because) but because it perfectly captures the 2020 feeling of dragging my sorry, long covid ass back to my tip job where I got covid in the first place.
#It's supposed to do that#that's the intention of the song#have to stop myself from using the full term#“post-viral sequelae of SARS-CoV-2”#now that I've heard it once
2 notes
·
View notes
Text
since everyone in public health is dead at the wheel, you should know: monkeypox has a r0 value of about 2 (omicron BA2 and measles are both near 12, which is about the maximum we know of, until we get clearer data on BA4/5 next month).
r0 value is number of likely infections per patient, so that also means monkeypox infections will likely double until it reaches peak infection. this could be a million people by the end of the year because it is 400 now (in the US).
it is aerosol and fomite transmissible. fomite viral particles survive in the environment for two months.
vaccination is currently available only for confirmed cases, and we will likely only be able to produce a million doses by end of year. they will likely not be distributed to the most at-risk people. this will likely not be enough to prevent widespread infection. i might recommend seeking testing in absence of symptoms, to catch any asymptomatic infections.
anyone born before 1980 is likely to already be vaccinated for it (smallpox vaccination seems to remain 85% effective with no waning, although the new vaccine recommended is jynneos and healthcare providers are hesistant to offer the older vaccine because it scars the injection site). if you're 40+ it might be a good time to get into volunteer outreach or hospice care.
it may have a fatality rate between 1-10%, more likely 1-3%, this is affected by factors like overall immune vulnerability, nutrition, and heatlh. severe progression is characterized by nausea, dizziness, shortness of breath, and other systematic-failure indicators. the virus had already mutated substantially by the time it was detected, so this may be an indicator that there are far more unknown, mild cases (i.e. bringing the fatality rate down substatially, one would hope.)
it is distinguishable from chickenpox because the sores progress at the same rate, while in chickenpox each sore may be at different stages. any healthcare provider or sexual health clinic will likely be able to test for both. now is not the time to ignore symptoms. petechiae are also a post-covid associated sequala, i believe they also progress at different rates like chickenpox but i'm not sure if there's a clear clinical definition of covid sores yet. it's also possible these represent undetected pox cases. it was likely circulating as early as april.
monkeypox infection may cause as a few as one sore, which scabs and then peels. debridement or exfoliation is not recommended, precisely because viral particles can survive for two months, although it's believed to stop being transmissible after the first layer of skin heals. vitamin A is recommended during recovery, ideally from nutritionally dense foods.
chickenpox can also cause facial paralysis. hepatitis-associated liver failure in children has been essentially confirmed as a post-covid sequela (adenovirus was ruled out as a cause of hepatitis, if you heard about that, although it is also still endemic). dysentery, cholera, and polio are back. between 10-30% of covid patients are now likely immunocompromised from long covid, although severe cases are less than 10%.
our failure to manage this has damaged the collective immune imprint, things that used to be rare or eradicated can now gain a foothold much more easily. this will keep happening until we end capitalism, we didn't have to live with influenza or salmonella either, and they make bank off the 1.3m deaths of heart disease and cancer every year too.
correct me if i'm wrong but i'm pretty sure everything except that last part is stated in this PDF. also had to look up the r0 value separately, i don't think that's in there
2K notes
·
View notes
Text
Highlights
“A new global health crisis secondary to acute SarsCoV2 infection”
“Post-acute sequelae after SARS-CoV-2 infection (PASC)”, also referred to as “long COVID” syndrome with a high level of heterogeneity.
“PASC is very likely to affect the quality of life of the COVID-19 patient after “recovery”.
“After SARS-CoV-2 infection, it mainly affects respiratory, cardiovascular, neurological, psychiatric, urinary, blood, skin and digestive systems.”
“It is generally believed that the persistence of low-load virus, abnormal immune response caused by viral proteins, secondary autoimmune diseases, and multisystem damage caused by microthrombosis and other factors lead to the occurrence and progression of PASC.”
Main takeaway:
We are only now starting to undertsand the varied mechanisms behind long covid. It may be decades before effective, standardized, and afordable treatments will be avaliable.
#mask up#covid#covid 19#covid isn't over#pandemic#covid conscious#long covid#covid is airborne#wear a mask#coronavirus
37 notes
·
View notes
Text
Persistent SARS-CoV-2 infections may act as viral reservoirs that could seed future outbreaks1,2,3,4,5, give rise to highly divergent lineages6,7,8 and contribute to cases with post-acute COVID-19 sequelae (long COVID)9,10. However, the population prevalence of persistent infections, their viral load kinetics and evolutionary dynamics over the course of infections remain largely unknown. Here, using viral sequence data collected as part of a national infection survey, we identified 381 individuals with SARS-CoV-2 RNA at high titre persisting for at least 30 days, of which 54 had viral RNA persisting at least 60 days. We refer to these as ‘persistent infections’ as available evidence suggests that they represent ongoing viral replication, although the persistence of non-replicating RNA cannot be ruled out in all. Individuals with persistent infection had more than 50% higher odds of self-reporting long COVID than individuals with non-persistent infection. We estimate that 0.1–0.5% of infections may become persistent with typically rebounding high viral loads and last for at least 60 days. In some individuals, we identified many viral amino acid substitutions, indicating periods of strong positive selection, whereas others had no consensus change in the sequences for prolonged periods, consistent with weak selection. Substitutions included mutations that are lineage defining for SARS-CoV-2 variants, at target sites for monoclonal antibodies and/or are commonly found in immunocompromised people.
4 notes
·
View notes
Note
bro. U seem smart how tf do I even start treating me/cf in myself idk where to even look :(
hey sorry i’m so late getting back to this i’ve been exhausted lol. and wanted to give you a comprehensive response. The things I find are mostly from research articles. what sucks is because the condition isn’t fully understood there are a lot of relevant articles that use different names- cfs/me, post-viral fatigue syndrome (pvfs), long covid, post acute sequelae of SARS—CoV-2. I try to keep up to date and search these terms on pubmed every now and then.
Medscape is a good app to quickly see which drugs are being used in clinical trials but i think it might be restricted to med students/ researchers/ clinicians but theres probably some way around that.
if you cbf with all that and just want recommendations:
the worst csf/me symptoms for me are definitely neurocognitive and the biggest helper has been modafinil followed by dexamphetamine. i highly recommend some kind of stimulants if you can get your hands on them.
other drugs and supplements that have shown high efficacy in studies:
coenzyme q10: i’ve been taking high doses (~900mg; up to 3000mg is recommended for disorders of mitochondrial dysfunction) and I do notice some physical improvement.
creatine monohydrate: 3-5g a day (may take several months to see effects however it’s cheap)
low dose naltrexone- lots of new interesting studies coming out about this. naltrexone is an opioid receptor antagonist usually prescribed to alcoholics and opioid addicts but also acts as an immunomodulatory agent at low doses. I started 2mg/day as of two days ago.
Zinc- i recommend zinc picolinate for higher bioavailability
B group vitamins- particularly B6, B9 and B12. There are relatively common mutations at the MTHFR gene (that may also contribute to cfs/me) that cause difficulty in metabolising B12 and B9- if you know your MTHFR genotype or experience weird side effects from B vitamins like insomnia or anxiety and paranoia, look into methylated forms (methylcobalamin and 5-methyltetrahydrofolic acid).
L-carnitine
nicotinamide adenine dinucleotide (NAD)
Methionine
N-acetylcysteine (NAC)
i haven't tried the last four yet but i'll be ordering them soon
6 notes
·
View notes
Text
oh great I think I have migraines now
this is all really looking a lot like POTS :(
people do seem to recover from all sorts of post-COVID sequelae - palpitations, fatigue, etc - even if it takes months or years. (of course some don't ever, at least so far, and similar to other post-viral illnesses.) but I don't know if POTS ever goes away by itself like that. generally at least it's regarded as incurable. obviously I'm not going to leap to conclusions other than generally trying to pace and manage as carefully as I can, but I mean, everything does fit. I sure hope the things you're supposed to do to manage it work well for me because otherwise I don't see how I can ever do primary research on my chosen topics ever again.
9 notes
·
View notes
Text
Navigating the Landscape of Long COVID Studies: Insights and Progress
In the wake of the COVID-19 pandemic, a new phenomenon has emerged, presenting a significant challenge to healthcare systems worldwide: Long COVID. This condition, characterized by persistent symptoms lasting beyond the acute phase of the illness, has prompted an urgent need for research and understanding. In this blog, we delve into the evolving landscape of Long COVID studies, exploring the insights gained and the progress made in unraveling this complex condition.
Understanding Long COVID: A Multifaceted Challenge
Long COVID, also known as post-acute sequelae of SARS-CoV-2 infection (PASC), encompasses a wide range of symptoms that persist for weeks or even months after the initial onset of COVID-19. From debilitating fatigue and cognitive impairment to respiratory difficulties and cardiac issues, the manifestations of Long COVID are diverse and often unpredictable. Understanding the underlying mechanisms driving these persistent symptoms is key to developing effective treatments and management strategies.
The Rise of Long COVID Studies: A Response to a Global Crisis
Recognizing the urgent need to address the challenges posed by Long COVID, researchers around the world have mobilized to conduct studies aimed at unraveling its mysteries. These studies encompass a broad spectrum of research areas, including epidemiology, immunology, virology, and clinical medicine. By leveraging diverse methodologies and interdisciplinary approaches, researchers seek to shed light on the risk factors, pathophysiology, and optimal management strategies for Long COVID.
Insights Gained from Long COVID Studies
The findings of Long COVID studies have yielded valuable insights into the nature of this complex condition. Epidemiological studies have provided crucial data on the prevalence and risk factors associated with Long COVID, highlighting the disproportionate impact on certain demographic groups, including older adults, healthcare workers, and individuals with pre-existing health conditions. Immunological studies have revealed dysregulation of the immune system in Long COVID patients, suggesting a potential role for immunomodulatory therapies in treatment. Virological studies have uncovered evidence of persistent viral presence and viral reservoirs in affected individuals, raising questions about the mechanisms underlying ongoing symptoms.
Progress in Long COVID Research: From Diagnosis to Treatment
As Long COVID studies continue to unfold, significant progress has been made in various aspects of research and clinical care. Diagnostic criteria and guidelines have been established to aid in the identification and characterization of Long COVID patients, facilitating early intervention and management. Clinical trials are underway to evaluate the efficacy of potential treatments, including pharmacological therapies, rehabilitation interventions, and supportive care strategies. Collaborative efforts between researchers, healthcare providers, and patient advocacy groups are driving innovation and fostering a deeper understanding of Long COVID across the medical community.
Challenges and Opportunities Ahead
Despite the strides made in Long COVID research, significant challenges remain on the path towards comprehensive understanding and effective management. The heterogeneity of symptoms and clinical presentations presents a formidable obstacle to diagnosis and treatment, requiring a personalized approach tailored to the individual needs of each patient. Longitudinal studies are needed to track the trajectory of Long COVID over time and assess the long-term implications for affected individuals. Moreover, addressing the social, economic, and psychosocial impact of Long COVID is essential to supporting patients and their families throughout their recovery journey.
Conclusion: A Call to Action
As we navigate the evolving landscape of Studies on Long Covid, one thing remains clear: the need for continued collaboration, innovation, and commitment to unraveling the mysteries of this complex condition. By harnessing the collective expertise and resources of the global research community, we can pave the way towards improved diagnosis, treatment, and support for individuals affected by Long COVID. Together, let us rise to the challenge and forge a path towards healing, resilience, and hope in the face of this unprecedented crisis.
0 notes
Link
Why do some people get depressed when they have Covid?
Scientists are still learning exactly how the coronavirus alters the brain, but research is beginning to highlight some possible explanations. A few studies, for example, have shown that the immune system goes into overdrive when some people get sick. They can end up with inflammation throughout the body and even in the brain. There is also some evidence that the endothelial cells lining blood vessels in the brain become disrupted during a bout of Covid-19, which may inadvertently allow harmful substances through, affecting mental function. And cells called microglia, which normally act as the brain’s housekeepers, may go rogue in some patients, attacking neurons and damaging synapses, Dr. Al-Aly said.
It’s possible that Covid-19 may even compromise the diversity of bacteria and microbes in the gut. Since microbes in the gut have been shown to produce neurotransmitters like serotonin and dopamine, which regulate mood, this change could be at the root of some neuropsychiatric issues.
Who is most at risk?
One of the biggest risk factors for developing depression after Covid-19 — or after any major illness — is having a diagnosed mental health disorder before you get sick. People who had severe Covid-19 symptoms and had to stay at a hospital during their illness also have increased chances of depression,...
According to W.H.O. estimates, young people are disproportionately at risk of suicidal and self-harming behaviors after Covid. Women are more likely than men to report mental health effects after Covid. And people with pre-existing physical health conditions, such as asthma, cancer and heart disease, are more likely to develop symptoms of mental disorders after Covid.
Additionally, people who experience extensive sleep disruption, social isolation or a significant change in other behaviors, like the amount of alcohol they consume or the type of prescription medications they take ...
3 notes
·
View notes
Text
ME/CFS
Because someone asked me what ME/CFS is:
Myalgic Encephalomyelitis:
Myalgia = pain in the muscles. AKA muscular rheumatism. Rheumatism = any disorder of the extremities or back, characterized by pain and stiffness.
Encephalomyelitis = inflammation of the brain and spinal cord.
In other words... the whole thing is fucked up.
CFS stands for Chronic Fatigue Syndrome. That's not just being a little tired, it's constant or comes in waves. People who suffer from this may have to structure their days in terms of energy expenditure and pacing. Even "small" actions like brushing your teeth or taking a shower can be costly, requiring rest and recovery after.
ME/CFS can be a post-viral sequela — a long-term consequence of viral disease even with mild initial infections. I.e. Long COVID.
121 notes
·
View notes
Text
Doris Loh comments:
It feels awesome to be validated by science.
A recently published study ties together two of my peer-reviewed papers on melatonin regulation of phase separation [1, 2, 3].
How?
In my first paper on melatonin regulation of phase separation, I talked extensively about the post-translational modification of SUMOylation used by melatonin to regulate phase separation https://www.mdpi.com/2076-3921/10/9/1483/htm.
In my third paper on melatonin regulation of phase separation, I explained how melatonin can suppress viral replication by regulating phase separation of the nucleocapsid (N) protein https://www.mdpi.com/1422-0067/23/15/8122/htm
Now this peer-reviewed paper published at Nature reports that SUMOylation facilitates nucleocapsid protein phase separation, enhancing the virulence of the SARS-CoV-2 virus [1].
I published the first paper in September 2021, the third in July 2022. Some serious #lohcurve for you. Got MEL?
References:
[1] Ren, J.; Wang, S.; Zong, Z.; Pan, T.; Liu, S.; Mao, W.; Huang, H.; Yan, X.; Yang, B.; He, X.; et al. TRIM28-Mediated Nucleocapsid Protein SUMOylation Enhances SARS-CoV-2 Virulence. Nat. Commun. 2024, 15, 244.
[2] Loh, D.; Reiter, R. J. Melatonin: Regulation of Biomolecular Condensates in Neurodegenerative Disorders. Antioxidants (Basel) 2021, 10 (9). https://doi.org/10.3390/antiox10091483.
[3] Loh, D.; Reiter, R. J. Melatonin: Regulation of Viral Phase Separation and Epitranscriptomics in Post-Acute Sequelae of COVID-19. Int. J. Mol. Sci. 2022, 23 (15), 8122. https://doi.org/10.3390/ijms23158122.
0 notes
Text
Impact on Kidney Post Covid-19 - Dr. LH Hiranandani Powai Hospital

As per a report from Hiranandani Hospital Powai, COVID-19 has impacted the lives of more than 45 million people in India. The pandemic has turned a challenging face which has caused death to more than 5 Lakh people in India. Globally, nations have experienced economic downturns and loss of countless lives. Post Covid, Hiranandani Hospital has witnessed how the disease has caused complications to the health of the kidney resulting in acute kidney injury in the lives of post Covid19 patients. It is estimated that in the long run, patients might face some respiratory issues.
Dr Sujit Chatterjee, CEO of Hiranandani Hospital is the strong backbone of the healthcare management industry. The hospital was formed to serve its patients with utmost patience and sincerity. In the battle against COVID-19, Hiranandani Hospital has undeniably seen and treated the highest number of affected patients in Mumbai. Dr Sujit Chatterjee Hiranandani has also contributed keenly to the healthcare policy formation in India and was also invited to National and International Forums to share smart views on emerging scenarios of healthcare in India.
Risk and Threat to Kidney Post covid 19
Dr. LH Hiranandani Hospital, Powai has served more than 1,00,000 happy patients, has completed 50,000+ surgeries, has 1000+ professionals, and 240+ beds. It is serving patients facing risks and threats to kidneys post-COVID-19 as the disease tells you about the health of your body. Well, to know if you need help or want to live healthy it's important to take this threat seriously in the first place. There is a 100% chance that you can heal quickly once you start following a healthy lifestyle. The article has stated some of the Risks and Threats to Kidneys post-COVID-19 patients. Here is the list:
1. Acute Kidney Injury: Very severe cases lead a patient to this disease(AKI), where there is a sudden loss in proper functioning of a disease. This might result from direct viral invasion or the body's inflammatory response.
2. Chronic Kidney Disease: Post Covid19 patients, who have any history of kidney conditions in the past are at a higher risk. Statistics show there is a strong connection between Chronic Kidney Disease and COVID-19.
3. Systemic Inflammation: COVID-19 has triggered a systemic inflammatory response that impacts various organs including kidneys. Prolonged inflammation may contribute to kidney damage.
4. Blood clotting: COVID-19 is highly associated with increased risk of blood clotting. Kidneys are highly vascular organs and blood clots can disrupt normal blood flow, potentially leading to kidney issues.
5. Dehydration: Fever, sweating and respiratory distress during covid 19 can contribute to dehydration, which is a risk factor for kidney problems. You can take care of yourself by changing small habits in your life.
6. Medication-Induced Kidney Injury: Some medications that are used in the treatment of COVID-19 or its complications have a nephrotoxic effect, potentially impacting kidney function.
7. Post-Acute Sequelae of SARS-CoV-2 Infection (PASC): Individuals with lingering symptoms after recovering from acute COVID-19 may experience ongoing kidney-related issues as part of the broader spectrum of post-acute sequelae.
8. Impact of Comorbidities: Patients with pre-existing conditions such as diabetes and hypertension, are common risk factors for both severe COVID-19 and kidney disease, that might face heightened risks.
At the Department of Kidney transplant, Hiranandani Hospital, Powai patients are given early detection and management so that they can maintain good kidney health. It's important to consult healthcare professionals for personalized advice and monitoring. The threats and risks describe the possibility of bad health of the immune system.
When Does a Patient Require Kidney Transplant?
Hiranandani Hospital Kidney Transplant
The patient should participate in the Hiranandani Hospital Kidney Transplant Program, launched by the Department of Kidney transplant, if he/she has faced kidney complications post-COVID-19. Every case is different; it is not recommended to get a kidney transplant for every kidney-related issue. Whereas, it majorly depends on the amount of damage COVID-19 has caused. In some cases, COVID-19 has led individuals to acute kidney injury (AKI) which can be healed with appropriate medical treatment. In other cases, if a patient undergoes damage which later turns to chronic kidney disease (CKD), it is the condition that damages your kidney and decreases its ability to keep you healthy by filtering the waste from your blood. When the patient reaches the end stage of renal disease (GFR less than 10 ml/min). Patients are advised to undergo medical evaluation and follow an appropriate course of action be it medication dialysis or kidney transplant. You should book a healthcare professional at Hiranandani Hospital Powai, Mumbai for your checkup today.
Here are some of the benefits of Hiranandani Hospital Kidney Transplant Program:
1. Majority of patients enjoy improved quality of life
2. No longer requires dialysis
3. Way Up Energy levels
4. Work and travel becomes easier
Future Impact
How COVID-19 can affect the kidneys is a matter which researchers are yet to look into. Researchers like Sujit Chatterjee Hiranandani are spending their time and energy to find out the impacts of COVID-19 in the long run. The healthcare system has launched a post-COVID care regime, which includes regular kidney function assessments among the patients to safeguard their lives, prioritizing those who had AKI or were affected by CKI. This states the importance of sustained medical attention and public initiative to address and manage potential kidney-related complications.
Hiranandani Hospital has launched a special post-COVID care clinic to treat the patients with the utmost attention and accessibility. You can book a physical appointment or virtual appointment to ensure your security and safety. If you’re specifically facing some issues after COVID-19 that are out of your understanding then you can write to Hiranandani Hospital at [email protected]
#hiranandani hospital kidney#hiranandani hospital powai covid#hiranandani hospital reviews#hiranandani powai hospital#hiranandani hospital powai
0 notes
Text
Published May 20, 2024
Asad Khan first developed Covid-19 in late 2020. A pulmonologist in Manchester, England, Khan had spent most of the year working on packed hospital wards full of acutely ill Covid patients. After falling ill with the disease himself, Khan spent what he described as a dreadful month at home waiting for the symptoms to subside. But they never did. Instead, Khan fell into the grips of long Covid, a post-viral syndrome that can last months to years after a SARS-CoV-2 infection. By the following September, he was sequestered in a darkened room, wearing earplugs and a blindfold. Khan suffered from relentless nausea and couldn’t stand the presence of other people, even his own children. The symptoms were so intolerable, he said, that he would have taken drastic measures to end them.
Then Khan heard about an experimental treatment offered by Beate Jaeger, an internist in Germany. Jaeger’s approach drew from preliminary evidence connecting long Covid with microscopic blood clots that can potentially deprive tissues and organs of sufficient oxygen. To remove these so-called microclots, Jaeger was using a procedure called apheresis, whereby a patient’s blood is removed, filtered, and then returned to the body. Apheresis is typically used to treat certain blood disorders or cancers such as leukemia or lymphoma. To Khan, the blood-washing strategy made “physiological sense.” So, after taking a one-hour flight to Germany, Khan met with Jaeger at her clinic. Apheresis treatments can run in the thousands of dollars, and Khan’s first session was scheduled for the following day. But Jaeger “took one look at me,” Khan recalled, and said, ‘You’re having it today.’”
Associated study published May 2023
Key Points
Question What symptoms are differentially present in SARS-CoV-2–infected individuals 6 months or more after infection compared with uninfected individuals, and what symptom-based criteria can be used to identify postacute sequelae of SARS-CoV-2 infection (PASC) cases?
Findings In this analysis of data from 9764 participants in the RECOVER adult cohort, a prospective longitudinal cohort study, 37 symptoms across multiple pathophysiological domains were identified as present more often in SARS-CoV-2–infected participants at 6 months or more after infection compared with uninfected participants. A preliminary rule for identifying PASC was derived based on a composite symptom score.
Meaning A framework for identifying PASC cases based on symptoms is a first step to defining PASC as a new condition. These findings require iterative refinement that further incorporates clinical features to arrive at actionable definitions of PASC.
#mask up#covid#covid isn't over#covid 19#pandemic#covid conscious#covid is airborne#wear a mask#coronavirus#long covid
30 notes
·
View notes
Text
Serotonin reduction in post-acute sequelae of viral infection
Post-acute sequelae of COVID-19 (PASC, "Long COVID") pose a significant global health challenge. The pathophysiology is unknown, and no effective treatments have been found to date. Several hypotheses have been formulated to explain the etiology of PASC, including viral persistence, chronic inflammation, hypercoagulability, and autonomic dysfunction. Here, we propose a mechanism that links all four hypotheses in a single pathway and provides actionable insights for therapeutic interventions. We... http://dlvr.it/SxbXhb
0 notes
Text
Clinical heterogeneity in patients with PASC has made it challenging to identify clear biological associations with the disease29. Here, we suggest that PASC should be subclassified into (at least) two distinct conditions, characterized by the presence (inflPASC) or absence (plaqPASC) of broad inflammatory signatures consistent with high neutrophil activity and ongoing B cell activation. Using high-dimensional proteomics in combination with machine learning-based modeling, we characterize clear signatures of generalized PASC strongly suggestive of dysregulation of discrete biologic processes underlying disease that may be tractable for both diagnostic and therapeutic purposes. While traditional feature-wise testing showed an inflammatory component to PASC as a whole, a finding largely in agreement with emerging literature, pro-inflammatory cytokines such as IL-6, IL-8, and IL-1B were not identified as strong candidates for the discrimination of PASC when modeling the totality of blood protein content. Instead, signatures of complement and clotting cascades, active antigen processing, and EGFR signaling were more consistently associated across the group, with the unanticipated identification of unique targets, such as epiregulin, that may hold important diagnostic value.
Likewise, proteomics-based clustering of PASC patients revealed a clear subset of patients closely associated with inflammatory immune signatures strongly suggestive of neutrophilic activity. Through readily-available clinical testing, these inflPASC patients displayed increased white blood cell counts driven by neutrophil expansion in comparison to plaqPASC counterparts, and showed significant increases in acute-phase reactants such as C-reactive protein, fibrinogen, and D-dimer. Associations with clinically-relevant autoantibodies, particularly those related to autoimmune vascular and clotting disorders, suggest that risk of micro-clotting, now widely reported in patients recovering from COVID-19, may be predictable through accurate identification of PASC subtype. However, these signatures are not readily apparent when taking the PASC cohort as a whole. It is important to note that even while these clinical markers are elevated within the inflPASC group, they do not necessarily reflect ‘abnormal’ test results in all cases. That is, the testing of any marker independently may not, by itself, indicate clear disorder. Instead, the elevation of multiple markers, even when within ‘normal’ ranges, seem to best reflect the broad inflammatory signals identified in the proteomics screen. This finding only emphasizes the need to develop tools capable of providing nuanced assessment across a variety of clinical parameters in patient classification. Similarly, it is important to acknowledge that plaqPASC is defined only as the absence of a clear inflammatory signature in the blood, and not as the absence of disease. As others have now shown30, and we show here (Fig 2b,h), biological associations can be readily identified across a wide spectrum of PASC independent of clear inflammatory signaling. It will be critical to understand how all of these signatures predict, and potentially contribute to, long-term patient morbidity.
Cellular immune signatures were correlated with the autoantibody signatures identified in the inflPASC cohort suggesting an increased emphasis of the EF B cell response pathway. Recently, this pathway has been directly implicated in the emergence of autoreactivity in severe COVID-19, with permissive B cell selective pressures leading to the emergence of cross-reactive clones capable of targeting both viral- and self-antigens22. However, in contrast with those studies, the prominence of the described effectors of that pathway, DN2 B cells and ASCs, was notably more muted in inflPASC patients. However, the presumed precursor to this pathway, aN B cells, were identified at almost a 2-fold increase over baseline. While more work is needed, these cells consistent with this phenotype have been previously implicated as an antigen-specific memory compartment within the context of yellow fever vaccination36. Here, they correlate with persistent reactivity against non-spike SARS-CoV-2 antigens. With previous studies in MIS-C identifying non-structural protein targeting as a feature highly related to autoreactivity, and previous implication of the aN populations in the emergence of de novo autoreactivity in chronic autoimmunity, it will be important to know if these cells may contribute to EF-derived memory responses and/or have a propensity towards self-targeting. Indeed, the identification of increasing autoreactivity in these patients at extended time points after COVID-19 recovery strongly suggests that an autoreactive memory compartment may be identifiable in these patients.
The overwhelming disease burden attributable to PASC worldwide10 demands that serious attention must be paid both to its accurate diagnosis as well as potential therapeutic avenues. The identification of a clear subclassification of PASC with a highly inflammatory presentation is an important first step. Based on these data, it is likely that these two PASC subclassifications may respond differently to the immunomodulatory therapies currently being investigated in large-scale clinical trials. Using machine-learning approaches, we have identified critical factors that can be used as positive classifiers of inlfPASC with a high degree of sensitivity and precision. Notably, while initial characterization of this heterogeneity required high-dimensional and unbiased screening, we found that a small subset of features that could be tested at scale, selected through novel assessments of feature potency, was nearly as performant when considered alone. Further, our integration of these data with classical in-clinic blood counts, clotting tests, autoreactive screening, and inflammatory marker assessment suggests that there may be several viable avenues to the positive identification of inflPASC patients without need for highly specialized technology. These assessments could be easily integrated into ongoing clinical trials to understand if therapeutics exert discordant effects on specific patient groups and reduce the potential for false-negative outcomes due to patient heterogeneity.
A critical question building upon these initial findings will be the stability of these inflammatory states over time. A surprising finding from these data, in combination with the published literature29, is the difficulty in discriminating disease subtype through symptom presentation alone. While trends do emerge, symptom presentation appears to be a poor discriminator of the inflPASC and plaqPASC groups despite their discordant underlying biology and identification of long-term physiological manifestations. As a result, it will be important to move beyond symptomatic presentation as a method of classifying patients, and understand how the signatures reported here might evolve over the course of disease. To this end, while our cross-sectional approach defines clear lines between plaqPASC and inflPASC, it is not yet clear if these presentations are mutually exclusive. In the case of reservoir-based viral reactivation as a main driver of PASC, as several have argued37, it could be that inflPASC manifestations are an observation of an inflammatory phase of cyclic reactivation rather than a discrete patient subtype. However, regardless of the stability of these manifestations, these data, taken together, point to an inflammatory process connected to altered long-term immunologic manifestations that may provide an abundance of therapeutic targets aimed at the alleviation of this debilitating disease.
1 note
·
View note