#osteolysis
Text
Seduced MILF Waiting For Taboo Sex With Stepson
Chavo lomo plateado me coje duro y rico por mi culo xxx
Girlsway Cadence Lux Teaches Her Stepsister How To Squirt
Blonde girls screaming from fuck by lengthy thick darksome dick in ass
extreme german mature labia stretching
Indian Lovers Home Made Sex
Zoe gets an erotic lesbian massage
Stepmom gives the sloppiest blowjobs
Petite Asian Masturbating for Tips
ALT tattooed big ass tattooed babe sucks dick, rims ass and gets fucked hard before getting a load of cum inside her
#quasi-appointed#necrophily#osteolysis#pediculosis#basilar#thinker#night-hawk#fertile-flowered#Sally#hyperphalangeal#painterish#temperality#cypseliform#payolas#pseudaconin#accoucheur#Parish#quenelle#voice#semiopen
0 notes
Text
Just some real talk for a moment regarding my upcoming shoulder surgery on the 15th
I know for the last year and 9 months I haven't been very active art-wise, and the shoulder surgery I'm going to have in less than 3 weeks is the main driver behind that. Kind of hard to do art when you are in constant pain with your dominant arm, and all of the non-surgical options we tried just didn't really seem to help (3 injections, Physical Therapy, Occupational Therapy for 4 months, Exercises since last March, etc).
As of right now I'm looking at 4-6 months of healing after surgery, which also means I'm most likely going to be lacking in much content to share (this includes sewing as well as drawing). I'm hoping that it doesn't take half a year to recover, but so long as I can get full functionality back with my arm, then so be it.
I know some folks talk about art-related injuries happening due to bad practices, but this isn't one of those cases. In my case I just ended up with a bum deal and it was just a combination of life stuff that led to this (final nail in the coffin though was helping to remove snow in early Jan 2022), and not how I was choosing to do art.
I know I'm going to be HELLA rusty by the time I heal, so it's going to take a while of doing bad art before I can get good again. I do have plans of things I want to work on once I can (working on the comic script currently actually), but please bare with me for the next little while if I happen to drop off the face of the internet, cause I won't be gone forever, I'll just be quite for a while.
#rambling#realtalk#I just want to no longer be in pain when I try to use my arm#Praying it only takes a couple of months to heal#Distal Clavicle Osteolysis surgery#AC Joint surgery
8 notes
·
View notes
Note
CT scan anon. Thank you so much.
What seems closest to how it feels is Gorham’s disease. However, I specifically compared my CT scan and CT scans for Gorham’s in skull I found online, and it doesn’t seem remotely like that.
I feel like there’s indentations all over my skull, with my nerves there and with my hands and I even see my hair sticking out differently than it used to in the mirror. When new indentations appear they hurt, and when my head hurts strongly it all also hurts stronger. Before a new indentation appears, I usually feel a weird feeling there that I’m not sure how to describe…
There’s no indentations on the CT scan, but the back of my head does seem narrower than it used to be, like it feels with my hands? But maybe I’m wrong… I don’t see anything else that I feel, and I feel a lot. Things I found online that look like what I feel look very differently.
I also went and searched osteolysis now instead of Gorham’s disease and I don’t know maybe I should take an x-ray but like can an x-ray show something that a CT missed
I had covid in February and then there was a lot of other shit and also I can eat very little of things because of a GI disability flare-up (so my nutrition is Not A Lot) and this shit began going rapidly somewhen in Spring; I’m also schizo-spec. Mom thinks it’s psychosis triggered by covid and I’d sure like it to be. Except the very first indentation, a vertical furrow in my forehead, I began to feel back in fucking 2018. In 2019, it became wider at the top and painful when head hurts a lot. Then it didn’t change again until this spring.
Ok, I won't lie with you, I would get a friend to take measurements and confirm for you what you're feeling. Get someone that you trust very much to confirm the physical sensations for you, and log them properly.
I am very familiar with bodily obsessions, that's how I ended up trying to cut a mole off of my side with a scalpel. It was not a good experience. I really wish that I had gotten someone to confirm for me before I reached that point, and it makes me very cautious about this kind of thing for a start.
I think that you need to ask someone to verify what you're feeling, and then determine what other symptoms you're experiencing to try and narrow down the possibilities. I can't diagnose you with anything here, obviously. I can't offer you much besides the fact that you really need those you trust and love to confirm your reality for you, I'm sorry.
7 notes
·
View notes
Video
youtube
Weightlifter's Shoulder (Distal Clavicular Osteolysis).
0 notes
Text










Primordial Dwarfism Sacral Agenesis Lesch-Nyhan Syndrome Congenital Central Hypoventilation Xeroderma PigmentosumIchthyosis Bosma Arhinia Microphthalmia Syndrome Holt Oram Osteogenesis Imperfecta Fibular Hemimelia Cerebral Palsy ADHD Autism PTSD Tourette Syndrome
Ehlers Danlos Syndrome Pulmonary Hypertension Spinal Muscular Atrophy With Respiratory Distress Gastroparesis Body Integrity Identity Disorder Epidermolysis Bullosa Thanatophoric Dysplasia Metatropic Dysplasia Prune Belly Syndrome Maffucci Syndrome Hennekam Syndrome Prader-Willi Syndrome
Congenital Limb Deficiency Muscular Dystrophy Hallermann-Streiff Syndrome Mast Cell Activation Syndrome Fibrodysplasia Ossificans Progressiva Trimethylaminuria/Fish Oudor Syndrome Idiopathic Premature Autonomic Neuropathy Progeria Escobar SyndromeIdiopathic Multicentric Osteolysis Pentalogy Of Cantrell Narcolepsy
Isla Kilpatrick-Screaton Lymphatic Malformation Albinism Harlequin Ichthyosis Bilateral Anophthalmia Neurocutaneous Melanosis Proximal Femoral Focal Disorder Saddan Dysplasia Pierre-Robin Syndrome
Down Syndrome Proximal Femoral Focal DeficiencyLissencephaly Hypertrichosis/Werewolf Syndrome
Motor Neuron Disease Erythromelalgia Sturge Weber Syndrome Arthrogryposis
Obsessive Compulsive Disorder Mandibulofacial DysplasiaIncontinentia Pigmenti Microcephalic Osteodysplastic Primordial Dwarfism
Centronuclear Myopathy Persistent Genital Arousal Disorder Narcolepsy Dwarfism Cystic Hygroma Neurofibromatosis Klippel Trenaunay Syndrome Congenital Heart Defect Arteriovenous Malformation Sotos Syndrome
Entity Syndrome Vitiligo Cloves Syndrome Arteriovenous Malformation
Moebius Syndrome Goldenhar Syndrome AlopeciaIdiopathic Pulmonary Arterial Hypertension Dermatillomania Hypertrichosis Cystic Hygroma Filariasis












1 note
·
View note
Text
Wanting what you have
• ACE YOUNG'S NECK (PERIPROSTHETIC OSTEOLYSIS OF UNSPECIFIED INTERNAL PROSTHETIC JOINT)
• CHANNING TATUM'S WRIST (SHOTGUN DISCHARGE, UNDETERMINED INTENT)
• JAIME KING'S FOREHEAD (OTHER FRACTURE OF UNSPECIFIED ILIUM)
• JUSTIN TIMBERLAKE'S FOREARM (SECONDARY LACRIMAL GLAND ATROPHY)
1 note
·
View note
Text

2023


Primordial Dwarfism
Sacral Agenesis
Lesch-Nyhan Syndrome
Congenital Central Hypoventilation
Xeroderma Pigmentosum
Ichthyosis
Bosma Arhinia Microphthalmia Syndrome
Holt Oram
Osteogenesis Imperfecta
Fibular Hemimelia
Cerebral Palsy
ADHD
Autism
PTSD
Tourette Syndrome
Ehlers Danlos Syndrome
Pulmonary Hypertension
Spinal Muscular Atrophy With Respiratory Distress
Gastroparesis
Body Integrity Identity Disorder
Epidermolysis Bullosa
Thanatophoric Dysplasia
Metatropic Dysplasia
Prune Belly Syndrome
Maffucci Syndrome
Hennekam Syndrome
Prader-Willi Syndrome
Congenital Limb Deficiency
Muscular Dystrophy
Hallermann-Streiff Syndrome
Mast Cell Activation Syndrome
Fibrodysplasia Ossificans Progressiva
Trimethylaminuria/Fish Oudor Syndrome
Idiopathic Premature Autonomic Neuropathy
Progeria
Escobar Syndrome
Idiopathic Multicentric Osteolysis
Pentalogy Of Cantrell
Narcolepsy
Isla Kilpatrick-Screaton
Lymphatic Malformation
Albinism
Harlequin Ichthyosis
Bilateral Anophthalmia
Neurocutaneous Melanosis
Proximal Femoral Focal Disorder
Saddan Dysplasia
Pierre-Robin Syndrome
Down Syndrome
Proximal Femoral Focal Deficiency
Lissencephaly
Hypertrichosis/Werewolf Syndrome
Motor Neuron Disease
Erythromelalgia
Sturge Weber Syndrome
Arthrogryposis
Obsessive Compulsive Disorder
Mandibulofacial Dysplasia
Incontinentia Pigmenti
Microcephalic Osteodysplastic Primordial Dwarfism
Centronuclear Myopathy
Persistent Genital Arousal Disorder
Narcolepsy
Dwarfism
Cystic Hygroma
Neurofibromatosis
Klippel Trenaunay Syndrome
Congenital Heart Defect
Arteriovenous Malformation
Sotos Syndrome
Entity Syndrome
Vitiligo
Cloves Syndrome
Arteriovenous Malformation
Moebius Syndrome
Goldenhar Syndrome
Alopecia
Idiopathic Pulmonary Arterial Hypertension
Dermatillomania
Hypertrichosis
Cystic Hygroma
Filariasis
Barber-Say Syndrome
Tar Syndrome
Fibrodysplasia
Psoriasis
Mayer-Rokitansky-Küster-Hauser Syndrome
Functional Neurological Disorder
Lymphedema
Neurocutaneous
Lioedema/Lipedema
Arthrogryposis Multiplex Congenia
Marfan Syndrome
Piebaldism
Morquio Syndrome
0 notes
Text
Revision Joint Replacement Surgery: when is it necessary and what to expect
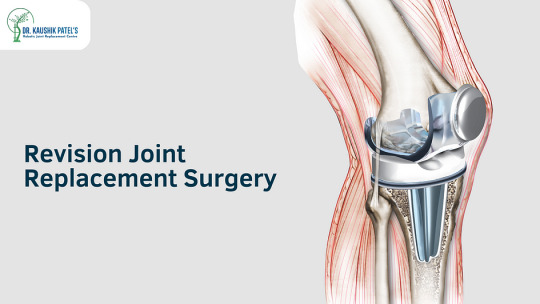
Revision joint replacement surgery is a procedure that is performed to replace an artificial joint that has worn out or failed due to various reasons. The need for revision joint replacement surgery arises when the original joint replacement surgery fails to relieve pain and restore function, or when there are complications related to the artificial joint. It is necessary that you consult a joint replacement surgeon in Surat for an expert diagnosis & treatment. Here are some reasons when revision joint replacement surgery is necessary:
Wear and tear of the implant: The most common reason for revision joint replacement surgery is wear and tear of the implant. Over time, the implant can become loose, leading to pain and discomfort in the joint. The wear and tear can also cause the implant to fracture, leading to failure of the joint replacement surgery.
Infection: Infection is another reason for revision joint replacement surgery. If the joint replacement surgery gets infected, the implant may need to be removed to prevent the infection from spreading. After the infection has been treated, a new implant can be placed.
Implant loosening: Implant loosening is a common complication of joint replacement surgery. It occurs when the bone fails to grow into the implant, causing it to become loose. Implant loosening can cause pain, instability, and decreased range of motion in the joint.
Implant fracture: Implant fracture is a rare but serious complication of joint replacement surgery. It occurs when the implant breaks or fractures. Implant fracture can cause pain, instability, and failure of the joint replacement surgery.
Instability: Joint replacement surgery can result in joint instability, which can lead to pain and dislocation. Revision joint replacement surgery may be necessary to correct the instability and prevent further complications.
Osteolysis: Osteolysis is a condition in which the body’s immune system attacks the implant, causing it to break down. Osteolysis can cause implant loosening and failure of the joint replacement surgery.
Allergic reaction: Some patients may develop an allergic reaction to the implant material used in joint replacement surgery. Revision joint replacement surgery may be necessary to remove the implant and replace it with a different material.
Bone loss: Bone loss can occur due to various reasons, including infection, implant loosening, and osteolysis. Revision joint replacement surgery may be necessary to correct the bone loss and provide a stable base for the implant. A joint specialist is an expert who can identify such issues and provide an expert opinion.
As mentioned by Dr. Kaushik Patel, one of the most trusted orthopedic surgeon in Surat, here are some things you can expect when it comes to knee replacement surgery:
Pre-operative preparation- The Knee replacement surgeon will evaluate your overall health and perform tests, including blood reports and radiographic scans such as X-rays or MRI, to determine the extent of the damage to your knee.
Surgery- The surgeon will then perform Robotic Knee Replacement surgery post thorough evaluation of your case.
Recovery- The joint replacement expert will advise you rest and medications which will assist in complete recovery.
Rehabilitation-You may need to undergo rehabilitation for several weeks or months to fully recover.
Follow-up care-It is important to follow the advice and instructions of your joint specialist in Surat for post-operative care to ensure proper healing and to avoid complications
FAQ’S
How do you know when you need a knee replacement revision?
Revision knee replacement may be necessary in your previously replaced joints when the patient feels pain and discomfort due to a number of reasons, including implant failure, wear and tear of the implant, infection, or other complications related to the initial knee replacement surgery.
How long does it take to recover from revision surgery?
The recovery time for revision surgery varies depending on the type and extent of the surgery, the patient’s overall health, age, and any pre-existing medical conditions.
How serious is knee revision surgery?
Knee revision surgery is a serious surgical procedure that is more complex and challenging than the initial knee replacement surgery. It involves removing the existing knee prosthesis and replacing it with a new one. The revision joint replacement surgery in Surat is usually performed to correct problems that have developed with the original knee replacement, such as implant wear, loosening, or infection.
What is the most common reason for knee revision surgery?
The most common reason for knee revision surgery is implant loosening or failure. Knee replacement implants are designed to last for many years, but they can wear out or become loose over time, especially with high levels of physical activity or excessive weight. When an implant becomes loose or fails, it can cause pain, instability, and reduced mobility in the affected knee. In some cases, the implant may also cause inflammation or bone loss around the joint.
If you are experiencing pain or discomfort in your joint replacement, or if you have any concerns about your artificial joint, it is important to consult with your orthopedic surgeon in Surat to determine whether revision joint replacement surgery is necessary.
0 notes
Text
انحلال العظم – Osteolysis هي ظاهرة يصاحبها فقدان العظام، ومن أهم مسبباته سرطان نخاع العظم. تعرف على تعريف انحلال العظام، والأعراض المميزة له، وطرق علاجه.
0 notes
Text
Langerhans cell histiocytosis
Formerly known as histiocytosis x (eosinophilic granuloma, hand-schuller-christian disease, letterer-siwe disease)
Due to proliferation of abnormal histiocytes
Clinical: Short stature, diabetes insipidus, neurosensory deafness and tooth mobility
Radiology: Osteolysis causing ’floating teeth’ in multiple quadrants
Histology:
Diffuse infiltration of large, pale staining mononuclear cells with…
View On WordPress
0 notes
Text
Fibula fracture

#Fibula fracture trial
#Fibula fracture professional
#Fibula fracture free
Appropriate bone loading to assist healing.
This unit provides the following benefits:. A forceful impact, such as landing after a high jump or any impact to the outer aspect of. To run at as little as 20% of your bodyweight. A fibula fracture is used to describe a break in the fibula bone.
#Fibula fracture professional
Previously only available to professional athletes and members of the armed forces, the Alter G treadmill allows you to run at only a fraction of your bodyweight. Sports Clinic NQ has the only publically available ALTER G treadmill in Queensland.
#Fibula fracture free
There is free use of Exogen at Sports Clinic NQ 5-6 days per week depending on opening hours. Diagnosis is based on clinical signs and radiographic exam. These fractures are often the result of a low-energy trauma with external rotation and supination mechanism. A deformity or bump that’s not usually on your body. Inability to move your leg like you usually can. A bone fracture is the medical term for breaking a bone. It needs to be applied daily at as close to the same time every day as possible. Isolated distal fibula fractures represent the majority of ankle fractures. The most common issues that affect the fibula are fractures and osteoporosis. For these fractures, a systematic review found that treatment with a long air splint, also called a long air cast enables return to activity up to six weeks sooner than standard casting and other treatments.Įxogen is a form of Low Intensity Pulsed Ultrasound (LIPUS) which has been shown to accelerate bone healing. A relatively aggressive rehabilitation protocol allows a quicker return to sport for uncomplicated, low-risk fractures.
#Fibula fracture trial
Sample exercise session for an endurance athlete: trial of 4 x 500m jog on grass 3 times over 2 weeks separated by at least 2-3 daysĪ pneumatic leg brace can help with symptom relief and allow you to tolerate earlier weight bearing activity without slowing recovery. Tennis and Golfers Elbow (Tendinopathy/ Enthesopathy).This normally takes approximately 6 weeks to unite. Acromioclavicular (AC) Joint Osteolysis You have sustained an isolated fracture to the middle of you your fibula (outside bone in your leg).Metatarsal Stress Fracture (excluding 2nd and 5th MT).Interdigital Neuromas (Morton’s Neuroma).Posterior Cruciate Ligament Injury (PCL) Although tibia and fibula shaft fractures are amongst the most common long bone fractures, there is little literature citing the incidence of isolated fibula shaft fractures.Medial Collateral Ligament (MCL) Injury.Chronic Exertional Compartment Syndrome (CECS).Published by Baishideng Publishing Group Inc. Complications regarding wound healing are frequent, especially with plate fixation, whereas other complications are uncommon.Īnkle Distal fibula Fibula fracture Lateral malleolus Management Treatment. Surgical treatment is indicated when fracture or ankle instability are present, with several techniques described. The diagnosis is made by x-raying the ankle. The injury produces pain, tenderness, and swelling of the ankle making weight-bearing difficult or impossible. Conservative treatment must also be considered in overaged unhealthy patients, even in unstable fractures. Fibular avulsion fractures most commonly occur from an inversion of the ankle that causes the ankle ligaments to pull a small piece of bone off of the end of the fibula. For simple, minimally displaced fractures without ankle instability, conservative treatment leads to excellent results. Management depends on fracture type, displacement and associated ankle instability. Stress X-rays have a role in detecting associated mortise instability. It runs parallel to the tibia, a larger bone that also forms the shin, and attaches the ankle and knee joint. Diagnosis is based on clinical signs and radiographic exam. The fibula helps stabilize and support your leg, body, ankle, and leg muscles. Isolated distal fibula fractures represent the majority of ankle fractures.

1 note
·
View note
Text
Precautions After Hip Replacement Surgery
Hip surgery brisbane is a common procedure for older adults who are suffering from pain that limits their ability to walk or do normal activities. The procedure typically requires a patient to lose a significant amount of weight before the surgery. They may also need to stop taking blood thinners. Patients should follow the instructions provided by their surgeon carefully. There are certain precautions that they should take following hip replacement surgery. These precautions can help them avoid complications after surgery.
The first step of the surgery is to administer a general or regional anesthetic, which will relax the muscles and put the patient into a deep sleep. The patient may also be given spinal anesthesia, which will help them feel very little pain during the procedure. The surgeon then cuts the thigh bone, exposing the hip joint. The doctor then removes the damaged bone and replaces it with an artificial ball. The implant is attached to the thigh bone with a special cement.
The procedure also involves the insertion of an intravenous line. A urinary catheter is also sometimes placed during the procedure. The surgeon then performs a surgical incision in the hip, either below or above the waist. The incision will depend on the type of approach used and the surgeon's preference. After the procedure, the patient will be positioned in a comfortable position.
After hip surgery, the patient may undergo physical therapy. This will help the patient regain their physical health and confidence in their new hip. Physical therapy can begin in 24 hours following the surgery. The hip may also require further surgery in the future. However, the initial period following hip replacement surgery is the most critical. This is because the hip prosthesis may loosen due to everyday activity or biological thinning of the bone called osteolysis. The loosening of the hip prosthesis can result in pain.
After hip replacement surgery, patients will be required to follow specific instructions and complete follow-up activities. They will need to take pain medication prescribed by the healthcare provider. Some of these medications can increase the risk of bleeding, so it is imperative to use only prescribed medicines. In addition to taking prescribed medicines, patients should avoid driving for three or more weeks. Full recovery may take several months, so it is important to follow your doctor's instructions.
A walker or crutches may be prescribed after hip surgery. They should be used until your healthcare provider recommends that you use a cane. Once you are able to walk without a cane, your healthcare provider will recommend how much weight you can place on your surgical leg. Eventually, you should be able to put 100% of your weight on the leg with the prosthesis.
After hip replacement surgery, you should avoid engaging in strenuous activities for at least two weeks. However, it is important to strengthen the muscles around your hip to prevent stiffness and pain. A physical therapist can provide helpful exercises that will improve your ability to walk. Once your new hip is in place, you should be able to resume your regular activities. You can also take part in sports and other activities. Once your surgery is completed, you should feel more confident in your new hip.
There are two main types of hip replacement surgery: total hip replacement and partial hip replacement. In total hip replacement, the femoral head and the head of the thighbone are removed. An artificial ball or socket is attached to the stem and stabilizes the new joint. Partial hip replacement, however, only replaces the head and does not replace the socket. It is commonly performed in patients with certain kinds of fractures. Once the surgeon has removed the damaged parts, he or she will use metal screws to attach the new head.
The surgery is successful in most cases. However, the procedure can have risks. The most common risk is hip dislocation. The artificial ball may not fit into the socket properly and can come out of the socket. Other risks include blood clots and infection. Some patients are advised not to engage in strenuous activities after the surgery. It's important to discuss these risks with your doctor before your surgery. The sooner you can recover, the better the recovery will be.
After hip surgery, you'll need to rest for a few days to recover. Your hip surgeon can help you determine whether you're a candidate for same-day discharge. Most patients can go home on the same day, but there are certain activities that you should avoid for the first few days after surgery.
0 notes
Text
For anyone who's had shoulder surgery (particularly AC joint / Distal Clavicle Osteolysis surgery), does anyone have any good tips or hints that made your life easier after surgery/during recovery?
I'm just honestly trying to get as much info as I can to make my life easier, since I know it's going to be a few weeks-months of recovery before I'll be back to decent usability with my shoulder. Just an FYI: I live mainly alone so I don't really have help, which means most everything I'll be doing will be on my own (Bonus points if you have suggestions that are useful that you can do on your own)
#Surgery is on 9/15#AC Joint surgery#Needing help#Distal Clavicle Osteolysis Surgery#I'm right-handed and that is the shoulder that is BORKED#I'm mainly expecting the first couple of weeks to be the hardest and then get easier from there
0 notes
Text
diagnosis
doctors may suspect progeria based on signs and symptoms characteristic of the syndrome and a genetic test for LMNA mutations can confirm the diagnosis of progeria.
a physical exam may include:
measuring height and weight
plotting measurements on a normal growth curve chart
testing hearing and vision
measuring vital signs, including blood pressure
looking for visible signs and symptoms that are typical of progeria
hgps is usually diagnosed during the first year of life or later, when progeroid features begin to be noticeable. the diagnosis is based upon a thorough clinical evaluation, characteristic physical findings, a careful patient history and diagnostic genetic testing.
more rarely, the disorder may be suspected at birth based upon recognition of certain suspicious findings (e.g., “scleroderma-like” skin over the buttocks, thighs, lower abdomen; midfacial cyanosis; “sculptured” nose, etc...)
specialized imaging tests may be conducted to confirm or characterize certain skeletal abnormalities potentially associated with the disorder, such as: degenerative changes (osteolysis) of certain bones of the fingers (terminal phalanges) and/or the hip socket (acetabulum).
in addition, thorough cardiac evaluations and ongoing monitoring may also be performed (e.g., clinical examinations, x-ray studies, specialized cardiac tests) to assess associated cardiovascular abnormalities and determine appropriate disease management.
interesting fact
the gene that causes progeria was discovered in 2003, along with a test used to identify the gene in humans.
0 notes
Text
Vincristine, Dasatinib, and Temozolomide like a Repair Routine with regard to Relapsed or Refractory Sarcoma in youngsters and also Adults
We found that mutations of protected hydrophobic elements involving Thr(257) and Tyr(279) lead to TSHR misfold, which assists a architectural fold on this peptide, most likely as a possible added leucine-rich replicate. Moreover, we all determined several brand new variations regarding hydrophilic healthy proteins from the total pivot area resulting in incomplete TSHR inactivation, showing these positions are important with regard to #Link# intramolecular sign transduction. In summary, we provide brand new info on the structural characteristics as well as features involving extracellular TSHR locations. According to these insights and in framework using earlier results, we propose the extracellular account activation mechanism in which facilitates the intramolecular agonistic device being a core switch for initiating effects in the extracellular location in the direction of the actual courbe site.History: The usage of interactive video game titles can be broadening within rehab. The data base is, even so, minimal. Objective: Each of our goal ended up being to evaluate the results of any Nintendo Wii Match (Ur) balance exercise plan about balance operate as well as walking potential throughout people with ms (Microsoft). Methods: A new multi-centre, randomised, manipulated single-blinded trial together with random percentage to workout or absolutely no exercising. The particular physical exercise group taken part in any program of Twelve closely watched 30-min periods associated with stability workouts utilizing Wii system games, two times a full week with regard to 6-7 months. Primary outcome was the Timed Upward along with Proceed test (Whip). Altogether, 84 #Link# contributors have been signed up; a number of have been lost to follow-up. Results: Following the input, there have been absolutely no statistically considerable variations between teams but effect measurements for your TUG, TUGcognitive as well as, the particular Vibrant Gait Index (DGI) ended up reasonable along with modest for all those various other steps. Statistically important enhancements inside physical exercise team have been gift for most measures (big in order to modest influence dimensions) except in jogging speed along with balance self-confidence. Your non-exercise group demonstrated in the past substantial changes to the A number of Rectangular Stage Ensure that you your DGI. Conclusion: When compared with absolutely no intervention, the program regarding supervised balance exercise making use of Nintendo wii gaming console Fit (Ur) would not provide in the past significant distinctions, but introduced reasonable result measurements for a number of actions regarding equilibrium performance.To assess your technological connection between CT fluoroscopy-guided, radiofrequency-induced vertebral enhancement (StabiliTA (R)) in terms of vertebral top recovery and polymethylmethacrylate (PMMA) leaks, happening throughout 30 individual individuals using vertebral compression cracks and also osteolysis. From 07/2010 to be able to 08/2011, Twenty five people (Sixteen ladies, seven adult men; grow older 71 +/- 18; range 41-89) with agonizing vertebral retention bone injuries as a result of #Link# weakening of bones (n Equates to 20), metastases (in Equates to Two) or perhaps a number of myeloma (d = Some) have vertebral augmentation which has a radiofrequency-activated, high-viscosity polymethylmethacrylate (PMMA) bone fragments cement (StabiliTA (R) Vertebral Development technique; DFINE Europe GmbH, Mannheim) below community what about anesthesia ?.
0 notes
Text
The receiver is as bad as the thief
◊ Stuart Townsend's foot (Elevated blood-pressure reading, without diagnosis of hypertension)
◊ Olivia Palermo's foot (Disorders of left acoustic nerve)
◊ Celine Dion's foot (Burn of first degree of back of unspecified hand)
◊ Lily Aldridge's foot (Salter-Harris Type I physeal fracture of upper end of unspecified femur)
◊ Travis Barker's foot (Swimmer's ear, left ear)
◊ Kendall Jenner's foot (Other ulcerative colitis with intestinal obstruction)
◊ Adrien Brody's foot (Corrosion of third degree of multiple sites of left wrist and hand)
◊ Stephen Moyer's foot (Other acute osteomyelitis, right shoulder)
◊ Jesse Eisenberg's foot (Other ossification of muscle, left thigh)
◊ NeNe Leakes's foot (Passenger in three-wheeled motor vehicle injured in collision with fixed or stationary object in nontraffic accident)
◊ Ryan Adams's foot (Anterior subcapsular polar infantile and juvenile cataract, unspecified eye)
◊ Jerry Ferrara's foot (Complete traumatic metacarpophalangeal amputation of left middle finger)
◊ Maria Shriver's foot (Endometriosis of pelvic peritoneum)
◊ Adrian Grenier's foot (Familial chondrocalcinosis, elbow)
◊ Tyra Banks's foot (Myositis ossificans traumatica, right forearm)
◊ Sammi Giancola's foot (Periprosthetic osteolysis of unspecified internal prosthetic joint)
◊ Sherri Shepherd's foot (Presence of unspecified artificial hip joint)
◊ DJ Kiss's foot (Driver of special all-terrain or other off-road motor vehicle injured in traffic accident)
◊ Chris Meloni's foot (Chronic postrheumatic arthropathy [Jaccoud], unspecified elbow)
◊ Brad Womack's foot (Physical restraint status)
0 notes