#endure this vicious cycle of traumatic events
Text
Right now I feel so old and sad at the same time. Those feelings are so strong I feel paralyzed and slow.
#right now it's all too much#got so many problems and they are going round in circles through my mind-uncontrollably#my mind jumps from one painful thought over to the next and all I currently manage to do is stay calm#endure this vicious cycle of traumatic events#and stop myself from screaming#I am calm I do endure and I suffer#maybe in a bit I will help myself out of this situation I am currently trapped in#right now calming myself down despite of all those things is hard enough#tonight I am drowning in waves of heart wrenching and soul crushing sadness#after a good night of sleep everything is gonna be a bit better I am sure of that#currently I am fighting I am crying I am breaking; but that's alright#when I endure feelings like this now then I don't have to endure them on another time#Life is an up and down#it will get better again#I remember the years when I got so depressed or whatever it was that I felt like everything just got worse and worse and worse#that's one of the things I feel sad about currently I am not doing well at all but nevertheless I KNOW there are gonna be better happier#lighter times#that's a huge step in personal growth and I did it on my own#I am slowly healing myself#I am changing#I am evolving#I am slowly getting better#and it hurt me a lot last year that you didn't acknowledge mile stones I reached all by myself you didn't see me as me#it felt like you looked at me with what you wanted to see and then you blamed me for not being that version of your#as you also mentioned 'dreamwife'#you also put me under pressure with saying things like that it made me feel like I am not good enough#like you are looking down on me#like I've to change and get better so you are getting the 'dreamwife' you perfected in your brain#I mean how old are you?#also you said things that forbid me grieving over the loss of my father and Louis
0 notes
Note
This might sound weird. In my viewpoint AFO feels like a child trapped in a grown man's body with his attitude and mindset. A man-child if you will. He's trying to enact childish fantasies onto the world, this obsession may stem from an event he experienced in his youth. He feels like a kid, felt it again when he blamed Kudou this chapter. In a better world AFO would've gone into the age regression community to get his chance to act out his childish impulses in a safe environment to process whatever trauma he endured instead of taking it out on the world.
YEAH I'M LOVING IT BC
Hori typically uses child imagery to like, show characters at their most vulnerable and honest and represent like the "naked essence" of who they really are. AFO rewinding into a literal child plays with those expectations, in a way-- but in this case, AFO "at his most honest/vulnerable" is almost monstrous in its depiction:

Like, AFO's got some pretty heavily implied hang ups about feeling powerless/being powerless and he uses escapism + the constant degradation of others to distance himself as far as he can from those hang ups. I wouldn't be surprised if his backstory ends up depicting some horrible violation of his own autonomy where he was treated as subhuman/toyed with-- and he's now attempting to inflict that same feeling of powerlessness on everyone else. Instead of healing from whatever trauma he experienced, he's become a slave to it. Of course, there's always a chance I'm reading into this too much-- But Hori's been pretty consistent in his depiction of abuse as a cycle (esp. with the Kotaro-Tenko and Endeavor-Touya plots), so tbh, it would strike me as an odd writing choice if he decided "yeah, AFO just woke up one day and decided to Be Like That."
And I've said this before on twitter, but like-- AFO is SUCH an Umineko/"Witch" coded character. It's one of the reasons I find him so fascinating, bc I've always loved the way umineko depicts coping mechanisms in severely traumatized/abused individuals and how it depicts abuse as a vicious cycle:


In Umineko, "a witch" is typically a manifestation that's born from a person's horrible trauma (or from a person's "will" to overcome that trauma and escape from an otherwise inescapable fate). They're born from humans who have been violated in some terrible way and who are desperate to redefine themselves as something powerful-- something that transcends that pain, something that pain can no longer "touch." They reclaim a sense of agency over their trauma/abuse/etc by adopting powerful alter egos who blend fiction and reality-- but ultimately, it's all still a form of escapism.
It's hard not to see the similarities between how umineko defines "witches" and how mha defines "villains"-- especially with characters like AFO, Tomura, and Dabi who have all adopted trauma-based alter egos-slash-identities and who attempt to reclaim "agency" over their trauma in intensely destructive ways.
Like.... so much of heroaca is just "my trauma takes the form of a powerless child because that's how it made me feel, and that's how it still makes me feel even though I'm not a child anymore-- but what if you could see that?" and then AFO won't even allow that much bc he's throwing his whole afoussy into rejecting MHA's usual tactics for humanization and instead going "OH??? YOU LIKE CUTE KIDS???? YOU LIKE CUTE INNOCENT WEEPY KIDS?? I'LL SHOW YA'LL CUTE *rips his entire face open*". We gotta respect his commitment to the bit, I guess, but at the same time jesus fuckin' christ dude.😬
39 notes
·
View notes
Text
Oracle Kaia Ra on Healing Trauma Through the Power of Community
Trauma, often described as the emotional and psychological wounds resulting from distressing events, can leave profound scars on an individual’s well-being. Whether stemming from a single traumatic incident or prolonged exposure to adversity, trauma’s impact is far-reaching, affecting mental, emotional, and physical health. The aftermath of trauma can manifest in a variety of ways, from debilitating anxiety and depression to substance abuse and relational difficulties. Recognizing and understanding the nature of trauma is essential to addressing its devastating effects.
Acknowledging trauma’s significance is not only a moral imperative but also a public health necessity. Ignoring the consequences of trauma can lead to a vicious cycle of suffering, perpetuating pain and dysfunction across generations. When we actively address trauma, we open the door to healing, resilience, and a brighter future for those who have endured its burden. It is crucial to embrace trauma-informed care and interventions, providing survivors with the support and tools they need to overcome their pain.
Oracle Kaia Ra, a spiritual leader and author, understands that one of the most powerful resources for healing trauma is the strength of community. Humans are inherently social beings, and our connections with others play a pivotal role in our emotional recovery. This article will explore how communities, whether they be close-knit families, therapeutic groups, or broader societal networks, contribute to the healing process. By sharing experiences, offering support, and creating a safe space for survivors to express their pain, communities can help individuals rebuild their lives after trauma. Kaia Ra delves deep into the intricate relationship between trauma and community, lending her voice to the exploration of ways in which communities foster healing and resilience, the importance of empathetic listening and validation, and the various forms of community-based interventions.
Understanding Trauma
Trauma is a deeply complex and multifaceted experience that can manifest in a myriad of forms. At its core, trauma is an emotional response to an overwhelming event or series of events that leaves a lasting impact on an individual’s mental and emotional well-being, and often biological components of the body as well. It can result from a single harrowing incident, like a car accident, or from prolonged exposure to adverse conditions, such as childhood abuse or combat. Trauma is not limited to physical harm; it can also be psychological, emotional, or even existential in nature.
The forms of trauma are diverse and include acute trauma, complex trauma, and developmental trauma, among others. Acute trauma arises from isolated incidents, like natural disasters or violence, while complex trauma emerges from prolonged, interpersonal trauma, such as domestic abuse. Developmental trauma, on the other hand, originates from adverse experiences during childhood, affecting the development of one’s sense of self and relationships. Understanding the various forms of trauma is essential to addressing its impact effectively and underscores the need for a multifaceted approach to healing.
Unaddressed trauma can have profound and enduring consequences. It may lead to a range of mental health issues, including anxiety, depression, post-traumatic stress disorder (PTSD), and addiction. Additionally, physical health problems like chronic pain, cardiovascular issues, and autoimmune disorders can be linked to unprocessed trauma. In the social sphere, unaddressed trauma can perpetuate cycles of violence, abuse, and dysfunction, impacting not only the individual but also their relationships and communities. Recognizing and addressing trauma is crucial for breaking these cycles and promoting healing and resilience.
Prevalence of Trauma in Today’s Society
“Trauma is far more prevalent in society than commonly acknowledged,” says Kaia Ra Oracle. “Its reach extends across demographics, affecting people of all ages, genders, and backgrounds.”

The Healing Process
Traditional therapeutic approaches to trauma have long been the cornerstone of addressing psychological wounds. These approaches often involve one-on-one sessions with a trained therapist, where individuals are encouraged to delve into their past experiences and emotions in an attempt to process and heal from traumatic events. While these methods have proven effective for many, they come with inherent limitations that make them insufficient in certain cases.
Limitations of individual therapy become apparent when dealing with complex and deep-seated traumas. Isolation in a therapeutic setting may limit the scope of understanding and empathy that can be achieved. Individuals often grapple with the feeling of being alone in their struggles, disconnected from the world around them, which individual therapy sometimes fails to address comprehensively. The emergence of community-based healing approaches represents a paradigm shift in trauma recovery. Recognizing the innate human need for social connection and support, these methods focus on the power of community in healing.
Notes Kaia Ra, “By sharing experiences and emotions within a safe and compassionate group setting, individuals can find solace, understanding, and validation in the presence of others who have walked similar paths.”
Key components of community-based healing include group therapy, support networks, and structured environments that foster a sense of belonging and shared responsibility. These settings encourage a collective approach to healing trauma, allowing individuals to draw strength from the community’s wisdom, understanding, and resilience. The power of community in healing trauma lies in the shared journey of recovery, highlighting that, sometimes, healing is not an individual endeavor, but a collective one, where bonds of trust and empathy can be forged to mend the deepest of wounds.
The Science of Community Healing
The relationship between the neuroscience of social connection and the process of healing reveals the profound and transformative impact that interpersonal relationships and community support can have on an individual’s journey through trauma recovery. In recent years, research in the fields of psychology and neuroscience has begun to unravel the complex interplay between our social connections and our mental health, particularly in the context of trauma and recovery.
Central to this understanding is the role of oxytocin, a neuropeptide often referred to as the “bonding hormone.” This hormone is released in the brain during social interactions, particularly those involving trust and bonding. The presence of oxytocin in the brain has been shown to reduce stress levels and promote feelings of emotional well-being. This effect underscores the biological basis for our inherent need for social connection, particularly in times of emotional distress and healing from trauma. In the context of trauma recovery, the impact of peer support and shared experiences is especially poignant.
“When individuals who have undergone similar traumatic experiences come together for healing, they create a unique space of mutual understanding about what they have survived,” says Kaia Ra, Oracle.
This sense of validation and shared experience is something that individual therapy, while invaluable, cannot fully replicate. Peer support groups offer a platform where stories of resilience and recovery can be shared. Hearing from others who have walked a similar path can be incredibly empowering. It not only offers comfort but also reinforces the idea that recovery and healing are attainable goals. This realization can be a crucial turning point for many in their healing journey.
The aspect of resilience, particularly as developed through community support, is vital in the context of trauma recovery. Resilience, the ability to bounce back from difficult experiences, is not an innate trait but rather a skill that can be developed over time, often with the support of others. Community healing programs play a critical role in this aspect. By providing a nurturing and non-judgmental environment, these programs allow individuals to openly express their feelings and experiences without fear of stigma or misunderstanding.

Building Trauma-Informed Communities
Creating safe spaces for survivors is a fundamental step in building trauma-informed communities. These safe spaces serve as havens where survivors can openly share their experiences without judgment or fear. The absence of judgment and the presence of empathy and understanding are essential for healing to take place. Trauma survivors need to feel secure, heard, and valued, and it is the responsibility of the community to provide such spaces.
Training and education for community members are crucial components of trauma-informed communities. When individuals in a community are educated about trauma and its effects, they become more equipped to support survivors. This knowledge enables them to respond with sensitivity, respect boundaries, and provide the appropriate support that trauma survivors need. By disseminating information and fostering awareness, community members can actively contribute to the healing process.
The role of organizations and institutions in promoting healing communities is significant. Schools, workplaces, and community centers can play a pivotal role in creating environments that prioritize trauma-informed care. By implementing policies and practices that support survivors and offer resources for healing, these institutions can have a lasting impact on the well-being of their members. The significance of self-care in maintaining community support should not be underestimated. Both survivors and their supporters must practice self-care to ensure the sustainability of community healing efforts. Self-care is essential for preventing burnout and ensuring that individuals can continue providing the necessary support.
A community that values and prioritizes self-care fosters a culture of resilience, enabling its members to remain committed to the ongoing healing process. Building trauma-informed communities requires a collective effort to create safe spaces, provide education, involve organizations and institutions, and prioritize self-care. Such communities serve as vital platforms for healing, offering hope, resilience, and a sense of belonging to trauma survivors on their path to recovery.
The Power of Community
The collective strength and shared experiences in such communities provide a unique avenue for healing that complements traditional therapeutic approaches. The potential for broader adoption of community-based healing is promising. As we witness the positive outcomes and resilience that community healing programs bring, there is a growing opportunity for their expansion. Encouraging more individuals and organizations to embrace these approaches can lead to a cultural shift in how we address trauma, fostering a society that prioritizes the healing power of community.
Encouraging collaboration and empathy in society is a crucial step toward creating healing communities. By recognizing the significance of shared experiences and mutual support, we can build a more compassionate and understanding society. Empathy and collaboration are the cornerstones of community healing, and promoting these values on a broader scale can lead to a more inclusive and supportive world.
Healing from trauma is not a linear journey, and communities must remain committed to providing ongoing support. The future holds promise for innovative approaches, increased awareness, and the continued growth of healing communities. Together, we can create a world where survivors of trauma find strength and solace in the embrace of their communities, demonstrating the enduring power of community in healing trauma.
About Oracle Kaia Ra
Kaia Ra is an oracle and spiritual leader with strong faith and determination who has inspired many people in their search for freedom and personal growth. She uses her own experiences to guide other truth seekers into a spiritual quest for enlightened answers and truths. She has been integral to the movement to revive the importance of Divine Feminine Christ consciousness. She is dedicated to leading a global movement for spiritual renewal and authored the book, “The Sophia Code,” creating a full curriculum and digital platform to enhance the reader’s experience.
Originally published at https://www.theamericanreporter.com/ on December 21, 2023.
0 notes
Text
Tackling PTSD and Addiction at Our Premier Addiction Recovery Center
Post-Traumatic Stress Disorder (PTSD) often remains hidden behind closed doors, creating a silent yet tumultuous storm for its victims. The turmoil within often leads these victims to seek solace in substance abuse, binding them in a toxic relationship of trauma and addiction. Arision Treatment, more than just an addiction recovery center, aims to provide a safe haven for those ensnared in this treacherous loop, helping them reclaim their lives.
Understanding the Cycle of PTSD and Substance Abuse
The distressing experiences that birth PTSD create profound emotional and psychological wounds. To numb this pain, many turn to drugs or alcohol, viewing these substances as their only escape. However, what starts as a temporary relief soon transforms into a dependency. This coping mechanism is similar to applying a band-aid on a deep-seated injury. Over time, the pain resurfaces, intensifying the cycle of trauma and addiction.
Neurotransmitters – Bridging PTSD and Addiction
At the heart of this relationship between PTSD and addiction lie neurotransmitters, the chemical messengers of our brain. Traumatic events can disrupt the natural balance of these chemicals, leading to feelings of anxiety, depression, and heightened stress – all hallmark symptoms of PTSD. Many addictive substances mimic the action of neurotransmitters, providing temporary relief. For instance, alcohol might boost serotonin levels, momentarily lifting the mood of someone with PTSD.
However, as the brain grows accustomed to these artificial boosts, it becomes reliant, tolerant, and dependent. The body craves more of the substance to achieve the same relief, setting the stage for addiction. This vicious cycle, fueled by neurotransmitters, perpetuates the bond between trauma and substance abuse.
Precision Treatment’s Holistic Approach
Venturing beyond the confines of a typical addiction recovery center, Arision Treatment offers an integrated healing approach. Our Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) are tailored to address the individual needs of our patients. Here, recovery is not just about detoxification but a comprehensive rehabilitation of mind, body, and soul.
What Dual Diagnosis Is Exactly
Arision champions the concept of “dual diagnosis,” focusing on simultaneous treatment for addiction and mental health issues. Consider a tug-of-war where mental well-being and substance dependency pull a person in opposite directions. Addressing only one side is akin to leaving the battle half-fought. Dual diagnosis ensures that the intertwined challenges of PTSD and addiction are tackled concurrently, paving the way for a holistic recovery.
Basically, our approach recognizes that addiction doesn’t exist in a vacuum; often, it’s intricately tied to other mental health challenges, be it depression, anxiety, or in this context, PTSD. Simply put, addiction may be the symptom of deeper psychological distress, and treating it in isolation might provide relief, but not a lasting solution. Dual diagnosis is pivotal because it offers a comprehensive lens to view and treat both the addiction and its root cause concurrently.
The Importance of Tackling Both Ends
One might wonder, why is this so crucial. Consider an individual battling both PTSD and alcoholism. While therapy might help them process traumatic memories, if their alcohol dependency isn’t addressed, they might revert to drinking during particularly challenging moments. Conversely, even if they achieve sobriety but don’t tackle their trauma, triggers could push them back into the spiral of addiction. Dual diagnosis understands these complexities, ensuring that the journey to recovery is robust, holistic, and long-lasting. With this approach, Arision Treatment doesn’t just promise relief; it pledges true and enduring transformation.
Why Arision is More than Just an Addiction Recovery Center
Arision Treatment doesn’t merely heal; it transforms. Our belief is that true recovery encompasses not just physical detoxification but emotional and psychological rejuvenation. We strive to empower our patients, arming them with the tools and knowledge they need to rebuild their lives. Our dedicated team of professionals ensures that each individual is equipped to face the world with renewed vigor and confidence.
How the Cycle Can Be Broken
Understanding the multifaceted nature of PTSD-induced addiction is crucial. A comprehensive treatment plan begins with a detox program, addressing the physical ramifications of addiction. However, the journey doesn’t end there. Continued therapy and counseling ensure that the gains in health are sustained, preventing any relapse into old habits.
Breaking The Chains Of Addiction
The intertwined chains of PTSD and addiction might seem unbreakable, but with the right support, they can be shattered. Arision Treatment stands as a beacon of hope and a new standard for addiction recovery centers for those looking to break free from this bond. Through our specialized programs and holistic approach, we promise a new dawn for every individual who steps through our doors.
If you or a loved one is seeking excellence in addiction recovery centers Arision Treatment Center is here to redefine your expectations. Our luxurious residential treatment, comprehensive care, and unwavering commitment to personal support ensure you’re in the best hands. Don’t let the chains of addiction hold you back. Contact us today, and embark on your journey towards lasting recovery at one of the top rehab centers in California.
0 notes
Text
Blog post 3
Effects of Intimate Partner Violence on Mental Health
A grieving mother in Baton Rouge, Louisiana has made it her mission to warn people not to underrate the danger of domestic violence. Catherine Smith’s daughter, Jessica was killed by her ex-boyfriend in October 2019 while returning home from a weekend trip. The ex-boyfriend, Anthony is currently incarcerated, waited for Jessica in her house and held her children and nanny hostage. When Jessica arrived home, Anthony shot her nine times. Before the incident, Jessica had previously filed a protective order against him. Following the death of her daughter at the hands of an abusive ex-boyfriend, Catherine has made it her mission to fight against domestic violence.
While Jessica’s case demonstrates the visible dangers of intimate partner violence, there are millions of domestic violence victims living with invisible scars of IPV through mental illnesses. Intimate partner violence not only leads to the death of victims, but it also severely damages the mental health of victims. Physical and emotional abuse is psychologically harmful and increases the risks of a woman developing mental illness. IPV has a significant and adverse effect on women’s ability to lead happy and productive lives.
Women that have experienced domestic abuse or violence are at a major greater risk of suffering from various mental health problems such as post-traumatic stress disorder (PTSD), depression, anxiety, substance abuse, and thoughts of suicide.
“The mental health consequences of intimate partner violence can be severe and include symptoms of anxiety, depression and post-traumatic stress disorder,” Dr. Sarah Noble, Psychiatrist at Einstein Medical Center Philadelphia.
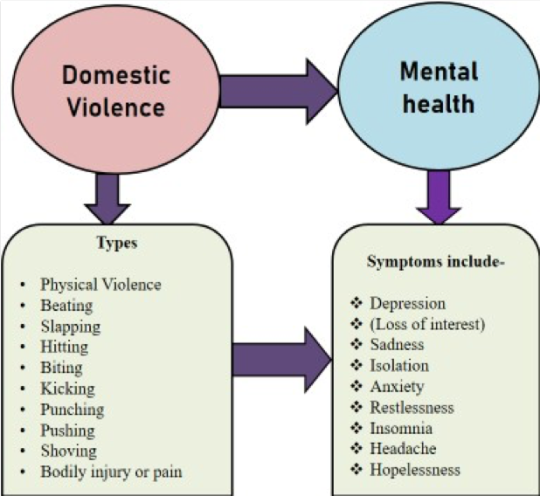
IPV and mental health
In cases of IPV, the batterer’s outburst is often accompanied by regret and a request for forgiveness. However, this cycle is often quickly followed by more violence and abuse. This pattern of abuse often creates a vicious cycle in which victims expect the next outburst. The victims in cases of abusive environments often feel that they have zero control, especially where such abuse occurs behind closed doors. Consequently, the abusive vicious cycle characterized by physical and emotional pressure severely affects the mental health of victims.
Various studies have demonstrated the severe impacts of domestic violence on the mental health of women. Averagely, more than 50 percent of the women seen in mental health centers are or were victims of intimate partner violence. Furthermore, women in abusive relationships exhibit specific mental health diagnoses mainly; post-traumatic stress disorder (PTSD), depression, and anxiety. Research has shown that traumatic events generate severe and enduring changes in physiological, arousal, emotional, cognition, and memory.
Rhian Parker cites studies that revealed that the likelihood of experiencing post-traumatic stress disorder was 7 times higher for women who had been victims of intimate violence than those that had not. Also, the odds of developing depression were 2.7 times higher, while the chances of anxiety and alcohol and drug abuse were 4 times and six times higher, respectively. Similarly, the studies found that the chances of having suicidal thoughts were 3.5 times higher for women that had suffered domestic abuse than those that had not.
According to Ellsberg & Emmelin (2014) domestic violence is a major cause of mortality because of suicide and homicide. Out of all women murders worldwide, nearly 38 percent were committed by a present or ex-intimate partner, as was in the case of Jessica.
Carole Warshaw, Phyllis Brashler, and Jessica Gil explain that the experiences of mental health symptoms by survivors vary due to various factors such as own personal strengths and resources, the length and degree of abuse, victim’s experience of other lifetime trauma and their access to services and social support.
Survivors usually internalize verbal abuse from their batterers. As a result, they may blame themselves for their condition. They may also experience fear, anger, and resentment against themselves. Consequently, chronic abuse may lead to compulsive and obsessive behaviors and contribute to self-destruction on even suicide.
Additionally, the stigma associated with mental health problems cements the capacity of abusers to manipulate and control their victims.
The World Health Organization cites that recognizing the link between IPV and mental health is the first step toward addressing the impacts of domestic abuse on victims’ mental health. Tackling the impacts of IPV on mental health can be addressed through improved services. WHO suggests that raising awareness to increase knowledge on the link between IPV and mental health, training health care providers to seek signs and ask the correct questions and in the right way are core steps to fighting intimate violence and its mental health implications. Services should be developed to sensitively recognize clients that live with or are affected by IPV and determine how such victims can be supported rather than focusing solely on the symptoms.
The WHO recommends that mental health services should implement gender-sensitive and trauma-informed interventions, co-produced by victims to help address the problem.
References
EinsteinHealth (2019, August 22). The Effects of Intimate Partner Violence on Mental Health. [Video]. YouTube. https://www.youtube.com/watch?v=Se6slFGL5QA
Ellsberg, M., & Emmelin, M. (2014). Intimate partner violence and mental health. Global health action, 7, 25658. https://doi.org/10.3402/gha.v7.25658
Karakurt, G., Smith, D., & Whiting, J. (2014). Impact of Intimate Partner Violence on Women's Mental Health. Journal of family violence, 29(7), 693–702. https://doi.org/10.1007/s10896-014-9633-2
Parker, R. (2019, February 18). How domestic violence affects women's mental health. The Conversation. https://theconversation.com/how-domestic-violence-affects-womens-mental-health-104926
Thomas, M. (2022, October 7). Mother of domestic violence victim shares her daughter’s story in hopes of helping others. WAFB. https://www.wafb.com/2022/10/07/mother-domestic-violence-victim-shares-her-daughters-story-hopes-helping-others/
Warshaw, C., Brashler, P., & Gill, J. (2009). Mental health consequences of intimate partner violence. http://www.nationalcenterdvtraumamh.org/wp-content/uploads/2015/10/Mitchell-Chapter-12.pdf http://hdl.handle.net/20.500.11990/538
Wheeler, B. (2022, April 6). Loss of agency: How domestic violence impacts mental health. Women's Advocates. https://www.wadvocates.org/2020/05/26/loss-of-agency-how-domestic-violence-impacts-mental-health/World Health Organization (WHO). (2022, October 6). Preventing intimate partner violence improves mental health. https://www.who.int/news/item/06-10-2022-preventing-intimate-partner-violence-improves-mental-health
0 notes
Text
Different worlds: Ash (1)

Part 1 - Part 2 - Part 3
Originally posted on 3 June 2019 in Turkish here.
Previously, I wrote about what I thought of Ash’s father and now it’s time to delve into what kind of damage James caused to Ash’s mental state.
Content/trigger warning: This meta discusses child sexual abuse.
James Callenreese is a bad parent in every sense of the word, but unlike the Cape Cod police, he’s not so degenerate as to claim that a 7-year-old boy seduced his abuser. And Ash knows that his father doesn’t blame him for getting raped. This allows him to be confident in the knowledge that what his abusers were doing to him is wrong and that it’s not his own fault. That’s why Ash never takes the responsibility of the abuse he endured upon himself. Consequently, he never thinks that he “deserved” to be raped.


Ash: They’re no different from each other. One does it is a cheap hotel stinking of piss and the other under a down quilt. That’s about it, really.
Their eyes… are all empty. There’s nothing in there. It’s like you’re peeking into an empty dark room… Their eyes all look the same. And they all say the same thing… That I asked for it!
One day, I will make them pay for what they did!
Blanca (thinking): Fear and rage… When rage conquers fear, he turns into a cruel demonic beast…
Ash: Are you gonna tell baldy about this?
However, there is another incident that affected Ash just as much as getting raped and that is his first murder. Like I mentioned here, the adults who were responsible for Ash’s safety failed to protect him, and so Ash took matters into his own hands and killed his abuser to put an end to what he was doing to him. Obviously, 8-year-old Ash was the victim in this case and couldn’t be held responsible in any way for the killing. But his words to Eiji in the following scene tells us that he holds himself fully responsible.
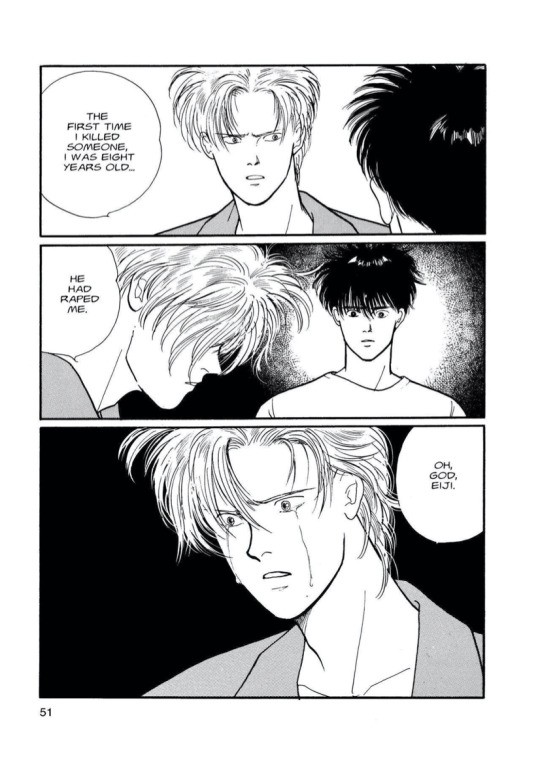
What I mean is, whatever the reason, Ash simply admits to killing a person. He talks about this incident only once and only to Eiji with no “but”s or “because”s scattered in-between, just the facts. Why is this important? Because Ash thinks that he lost his innocence at that age when he killed his baseball coach and that his life took an irreversible turn as a result.
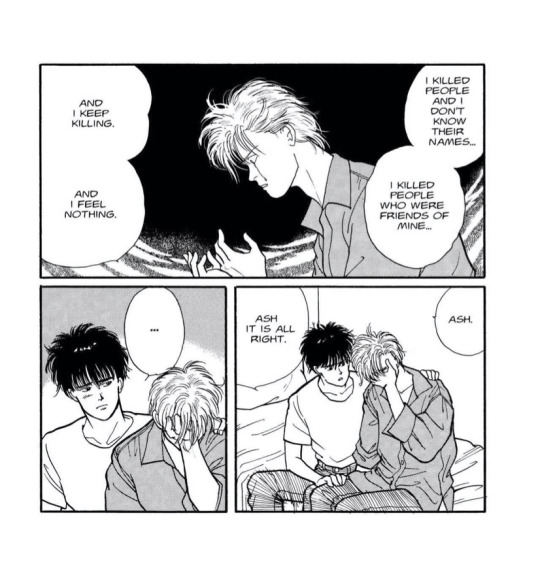
The official English version took some liberties with the translation in this scene. Here’s a more direct translation of what Ash says: I’m scared of myself. To think that I killed Shorter… I don’t even know how many people I killed until now. And I feel nothing. Nothing…
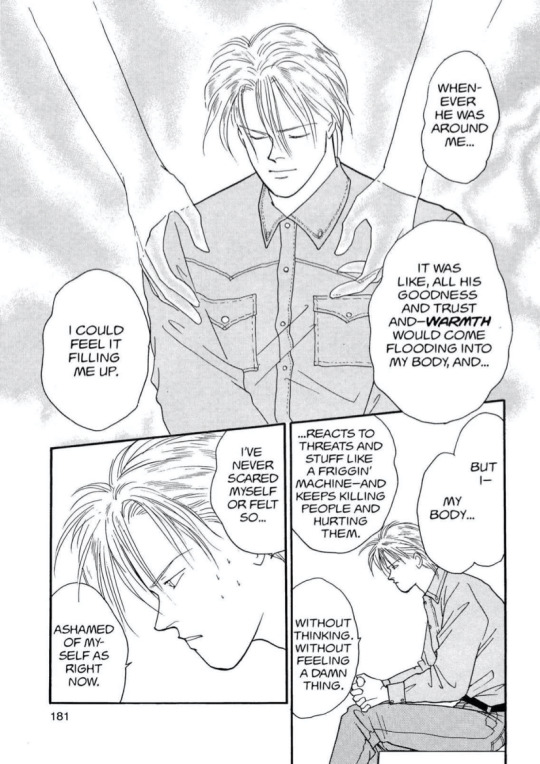
It is in this scene that we witness just how traumatic killing is for Ash. He’s crying because he came to realise that he’s slowly losing his human side. Deep down Ash feels like he has to pay for all the lives he took regardless of the circumstances. So he doesn’t think it’s even possible for him to lead a different, a more “normal” life, because he doesn’t see himself worthy of one in the first place.
I believe James is the root cause of why Ash came in with this toxic mindset. If there’s anything that caused Ash to get hurt more than his father’s negligence, it is his helplessness that Ash seems to forgive him for. Perhaps James didn’t blame his son for getting raped or told him that he deserved it, but we know that he called him a troublemaker.
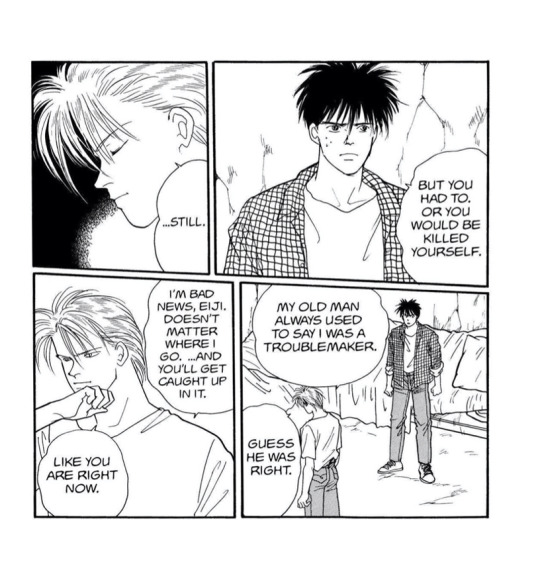
I have this headcanon that I think kind of goes along with the canon… Maybe? Here it goes: James is overwhelmed with all the horrible stuff that happened to his son and he doesn’t know how to deal with it. He feels helpless and frustrated, and yells at Ash saying things like “Why does trouble always find you?” and “It’s as if you were born with a streak of bad luck.” And little Ash takes his father’s thoughtless rambling to heart.
Then, as we know, Ash is swept up in a life of crime and violence where he has to play by its relentless rules to survive another day. He suffers through all kinds of cruelty and abuse. He kills to defend himself and the members of his gang. But then, these killings for self-defence slowly become mass murders as we see with the “vendetta” with Arthur’s gang.

Contrary to Arthur, Ash has no desire to gain power and become a crime lord. He doesn’t see people around him as rivals or makes it his life’s ambition to destroy them. Ash only hunts because he is being hunted. Gang politics concern him only because he feels responsible for the safety of his gang members. Ash doesn’t want this kind of life. But we shouldn’t forget that Ash never knew a different kind of life, because he was never allowed to live differently. And Ash knows very well that he’s already in it too deep, so he thinks he’s condemned to live this life whether he wants it or not.
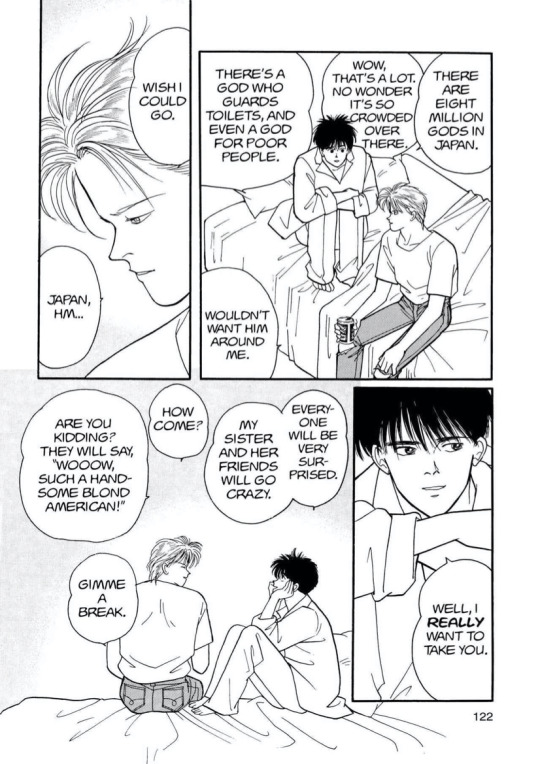
Naturally, this is a very destructive mindset. Eiji realizes early on that Ash has been caught up in this vicious cycle and tries to free him. He tells Ash, “You’re not a leopard. You can change your fate,” and later offers, “Come to Japan with me. You can do anything you want there.” Whenever Eiji suggests these possibilities Ash is always surprised at first. Like it’s simply inconceivable for him that another person would offer to guide him with only his well-being in mind. But these possibilities seem too far away to Ash. That’s why he smiles bitterly whenever Eiji brings up this conversation, but at the same time, he never outright rejects what Eiji is suggesting. Although it may seem like he’s doing that because he doesn’t want to hurt Eiji’s feelings, I feel like Ash actually allows himself to dream in those moments.
We all know the answer to the question “Why did Ash become so attached to Eiji?” To summarize, it’s because Eiji, being an outsider to Ash’s world, saw him as a person, as a friend who is around the same age as him, and because Eiji gave Ash a part of himself without expecting anything in return. Without realising, Eiji is calling out to the remnants of humanity in Ash. Eiji, who is often associated with birds and flying throughout the story, symbolizes freedom for Ash. So the fact that Ash grew so attached to Eiji actually reveals his desire to set his soul free, break with his past and seek atonement.

But the events that follow don’t align with Eiji’s wishful thinking at all. Trouble keeps following Ash and gradually threatens Eiji too. Ash realises after a while that Eiji is not only in danger but is directly being targeted by Ash’s enemies. And Eiji getting shot in the end is a cruel wake-up call for Ash.
As the lyrics of RED suggest, at that point Ash confronts with the “fact” that he was the reason Eiji almost died because he was too “selfish” to let him go (I don’t think that’s a fact nor that Ash was being selfish, but I assume that’s what Ash thought, so I put those words in quotes). And Blanca is not helping the situation at all.

If James is the reason why Ash thinks he will never be able to live a better life, Blanca is the one who literally engrained this mindset in Ash. Why? Different from all those assholes like Golzine who see Ash as a wild and beautiful beast or a disposable toy to be sold and used, Blanca is someone who Ash trusts and even he thinks it’s impossible for Ash to lead a normal life. (likely triggered by what happened in his own past). When Blanca first appears in the story, he tells Ash that “a rabbit and a lynx can never be friends.” Their world is different from ours, he means to say, which is exactly the opposite of all the things that Eiji was trying to make Ash believe.
On the other hand, Blanca understands Ash. That’s why he takes him to the hospital where Eiji is being treated so that Ash can say “sayonara” to him before the final showdown with the enemy. Seeing Eiji lying unconscious on the hospital bed is like a slap in the face for Ash. He’s once again confronted with how close he came to losing the most important person to him. So to keep Eiji safe, Ash decides never to see him again and he tells Blanca so later when they meet in Central Park. His monologue here reveals Ash’s inner turmoil between his desire to cling to the feelings Eiji sparked in him and his conviction that he’s not worthy of it at all.
Thinking of the story of Banana Fish as a whole, and especially the ending, it seems clear which side won…
…right?
Read the next part of the meta here.
#different worlds#another translated meta#so it may sound weird at times#banana fish#ash lynx#banana fish manga#meta#analiz#yorum#english#banana fish türkçe#şekerli
119 notes
·
View notes
Text
How Hiyori deals with trauma -; The 100 year grudge
Short answer is- - she doesn't. She does not deal with it at all. All Hiyori really knows is fury. She fights furiously. She loves furiously. She's constantly grappling with processing emotional and physical scars on her psyche that involve turning into a hollow. She has to recite basic facts about herself that are true to understand who she is. Hiyori Sarugaki. She's a visored. She hates Aizen. She loves her friends. That is her life right now and that is the reality.
She is constantly being forced to relive traumatic events in her head. Kisuke losing his captaincy. Her friends living in exile and squalor. Watching the shinigami she once knew hunt her and her friends down. Hurting her friends. Watching humans live their lives and die. Watching her hollow lose control, locked in her own head.And when she's not trying to fight her own hollow in her head, she is constantly overwhelmed with the utter might and control Aizen has.
Hiyori has had a 100 years to hate Aizen and fear losing control because her enemy is still out there. That is a long time to live in this constantly negative state of fear and rage and she doesn’t know how to get at Aizen until certain things are in place. Asking Hiyori to wait for the Hougyoko to be awakened, or wait for the chosen child to come or wait for people to see Aizen for who he is-- she is not a person that can sit and wait.
And that waiting only heightens her negative emotional state. Her fear of a powerful enemy as well as herself... it brings with it an inability to experience positive emotions such as feelings of love or friendship. Even when she is trying to befriend Ichigo or let her friends know she loves them, she hurts them over the slightest little issues. Any time Hiyori feels threatened or unsafe, she is prone to angry outbursts and has increasingly horrible moments of low mood because of it. It's a terribly vicious cycle. She is angry. She is depressed. She can't do anything about what happened to her and she hates that she was used by Aizen to do his dirty work.
She does show resilience. She keeps busy. She keeps fighting and training and trying to make sure that she is strong enough to face Aizen. She trains her hollow. She learns about hollowfication. She can develop techniques to subdue it. She does not talk about the nights she can’t sleep - -none of the visored can. They learn to deal with it. Endure it like a warrior. And she won’t crumble and break down in tears because her friends are the strongest people she knows and they lift her up. And without them Hiyori has nothing in this world.
That is why, as long as Aizen is out there, he can hurt her friends again. He can do this over and over and make her hurt her friends with new means. That is why she can’t be at peace..
She has to be violent. Because if you take abuses lying down, you’re giving a chance for people to hurt you again. And Hiyori will not be that victim. She will not let Aizen or anyone get away with hurting her friends.
She deals with her trauma with fury; I will never allow anyone to hurt my friends like this again.
For @txchikaze
#.hc#// i don't know if any of this makes sense... but mainly... hiyori has a load of complex things she has to sort out ;n;
17 notes
·
View notes
Text
Wolf Howls
Breaking Cycles\Generational Healing
Trauma comes in many forms, but the scars left behind are all but the same. For many Indigenous people, this trauma can last for generations, the scars past down from parent to child and so on.
Inter-Generational Trauma is a traumatic event such as Violence, Sexual, Physical or Emotional Abuse that began years prior to the current generation and impacts the way in which individuals within a family understands, copes with, and heals from those events.
https://www.acamh.org/blog/intergenerational-trauma/
We see many young Indigenous people struggling with issues in life such as addiction, low self esteem and a vicious cycle of self harm. What many don't see, is the trauma associated with those behaviors from generations before them. These events have such an impact on their lives and for many of them, they don't even know. Our jails and institutions are filled with people suffering with trauma from the past
We must take seriously the events of the past Residential School systems, early government policies and understand the effects they had on the Indigenous people then and more importantly this generation now. Because it is largely those events that have crippled this generation from living productive lives.
Becoming, and ultimately feeling, competent, knowledgeable, and ready to help is the first step towards healing. Click on the link below and see how one Indigenous family is tackling generations of trauma head on so their generations after them can live healthy productive lives and not feel the pain they've endured.
https://www.aptnnews.ca/national-news/how-three-generations-of-women-are-working-to-stop-the-impacts-of-intergenerational-trauma/
0 notes
Text
The Harsh Reality of Living With Trauma
As the years have passed and diagnoses have come and gone, I have long accepted most of them. I have adjusted myself and my life to help live and better cope with them. Throughout the years, I have taken advantage of the time I have had to get to know myself. Mental illness has changed everything about me; some of those things are good, and some are bad. I like to think that I’m relatively in-tune with myself, my emotions, and the illnesses I live with so that I can continue to better myself and work my way towards no longer living with them.
Yet, here I am; struggling, hurting, and quite frankly, getting worse; or so it seems. I have made so much progress within the last four years. I don’t feel suicidal, but I think about death. I don’t want to relapse, but that seems like the only option in order to cope, because that’s all I ever knew. I know I’m better, because I used to think about suicide daily, and I used to want to relapse, and that’s no longer the case. I ask myself what my problem is at least 12 times a day. Although, I’m not really sure why, because I already know the answer. There is one little word that is constantly lingering over my head and eats me alive.
Trauma.
I haven’t dealt with post-traumatic stress disorder for as long as I’ve dealt with my depression, insomnia, or anxiety. But I feel like it’s been long enough that I should at least be a little more in-tune with it; I should at least have more of a hold on it so that it doesn’t have such a hold on me. PTSD is a disorder that some - not all - people develop following a traumatic event or witnessing a traumatic event (i.e. combat, rape, death of a loved one by suicide, a car accident, emotional or physical abuse, etc). Individuals that develop PTSD do not recover from the experience properly. The trauma can actually cause their brain to malfunction, and they fail to recover like most individuals are able to do. The amygdala, hippocampus, and ventromedial prefrontal cortex are all affected following the traumatic experience, which impacts the stress mechanism we all have. Thus, the survivor continues to discern and respond to stressors differently than someone who recovered normally from a similar experience. If you would like to read more about how the 3 areas of the brain that are affected, click here.
PTSD is the most painful, frightening, and debilitating thing I have ever experienced in my entire life. With it come panic attacks, flashbacks, intrusive thoughts, and dreadful memories I never asked to happen, let alone asked to remember.
I am not going to go in-depth about my experiences, as I am not currently in a place where I can openly talk about them with just anyone without feeling shame and humiliation. But I will say that as of right now, there are 3 specific experiences that rule my life; they vary from mental and physical abuse, sexual assault, and an indirect situation I experienced in the church. They all date back only within the last 4 years. They are still fresh and new, and I have not yet fully accepted them.
I live in a small town where you can’t really escape anyone or anything. This town is also where 2 of the experiences occurred, so daily life is exhausting. One of the most common symptoms of PTSD is the avoidance of people or places that can trigger a past event. Living in this town makes this nearly impossible to do, as much as I would love to do it. If I am driving by myself, it’s easier to avoid the places that I want. But sometimes when I’m with friends, it’s inevitable. At this point, I don’t even say anything anymore, because it’s almost as if every single place I go in this town somehow reminds me of what I don’t want to remember. So instead of making things extremely difficult, I just shut up about it and internalize how it makes me feel until the feelings, emotions, or flashbacks pass. I don’t want to burden the people I love who want to do things with me just because of an experience that occurred that I should have reacted to normally in the first place. The exact places where the 2 experiences happened in this town are places I will not go. But even places I went with these people - traumatic experiences completely unrelated - are triggering (one of these days, I will talk about why I was going places with these people, and living a normal life with them and yet still experiencing the unthinkable). Walmart, grocery stores, rivers, lakes, certain roads; just about anywhere. There are places in this town that I absolutely love, which are now permanently scarred. Just remembering that I was in a specific place with the person sets me into a frenzy of emotions that I do not want to feel. The amount of stress the avoidance of things puts on me is incredible. Sometimes, a lot of it is subconscious; in my subconscious mind, I know I have to leave my house and that I’ll most likely come across a person, place, or thing that will trigger me. Each day is exhausting knowing that no matter where I go, and no matter what I do in this town, my experiences will always be with me. And I hate that.
The traumatic experience that occurred outside of this town is somehow still triggered almost daily. Although, it’s usually triggered as a result of a word, phrase, smell, or someone coming up behind me and scaring me, whether it’s intentionally or unintentionally. It has completely warped my perception of what healthy relationships and friendships are supposed to be. I don’t want to remember certain smells, and yet, it seems like everywhere I go, I keep smelling something that reminds me of what used to be.
Flashbacks are probably what I would categorize as the worst symptom of PTSD. This is where the trauma really takes hold of me. Flashbacks debilitate me, and I completely disassociate from myself and everyone around me during one. I do not know how long my flashbacks actually last. I never know when they’re going to happen. I never know exactly what is going to trigger them. It’s almost like the onset of a panic attack, minus the panicking and physical symptoms of one. The best way I have ever been able to explain a flashback, is that my mind and eyes are a projector. Picture yourself sitting in a classroom looking at whatever is on the projector screen that the teacher has up. That’s literally what it looks like in front of me, because I am the projector. I completely freeze, my body doesn’t move, and I’m pretty sure I don’t even blink. Whatever I was doing or whoever I was with before it started, does not exist any longer. I watch myself enduring the traumatic experience across the room, right in front of me. I know I’m sitting there watching. The part of me that is enduring the experience keeps wondering why in the world the part of me who is watching isn’t doing anything. Why does she keep watching this happen and keep allowing it to happen? WHY ISN’T SHE DOING SOMETHING TO HELP ME? Sometimes I feel like my flashbacks are some twisted way for me to try to change the past. I never did anything right away to get myself out of the 3 traumatic experiences. Heck, I didn’t even know one of them was even traumatic until at least a year after. I am angry at myself for not doing anything about them. I am angry at myself for continuing to put myself in the position of it happening. I am angry at myself for not stopping it. If I could have just stopped it, my life wouldn’t be a living hell. Maybe my flashbacks are a way for me to change that; to go back and do what I should have done. But I can’t, and I don’t. I watch myself scream at the part of me who is watching. She’s screaming at me to do something, anything. But the part of me who is watching does nothing, she doesn’t even move. There is no emotion on her face, almost as if she just doesn’t care. She sits there and watches until it’s over. Just like the shaking of the head and excessive blinking Raven Simone did on That’s So Raven after she’d have a vision (my favorite show as a kid, by the way), I come back to reality. I can find myself anywhere from pulled over on the side of the road not knowing how I got there, in the store staring at the package of chicken I had in my hand, in the car with friends, in my room, in the shower, or at work. Following a flashback, I am usually exhausted for the rest of day. I need to lie down and cry it out. Most of the time, I’m not able to. I internalize what I just experienced in the flashback, and that probably begins a vicious cycle since I never deal with any of it.
Nightmares are a weekly thing. Thankfully, not every single night, but they’re enough to interrupt my sleep when I seem to need it the most. Intrusive and frightening thoughts are a daily thing the second I step out my front door. What if I see them today? What if I see someone else that reminds me of them? What if another traumatic experience happens to me today? What if I get raped or abducted? What if I get into a car accident on my way to work? It’s almost as if the traumatic experiences caused some kind of paranoia. I am constantly preparing myself for the worst. If I prepare myself for the worst, maybe it won’t affect me so badly, because I was already ready for it.
Trauma can cause memory loss. I used to think this was great. All 3 of my experiences were ongoing for an extended period of time. So I know that there were a lot of things that happened throughout each of them that I just don’t remember. I used to think, sweet; that’s one less thing I have to remember or try to deal with. Boy was I wrong. Each day, randomly, a new memory will pop into my head. A memory I had never thought about until that moment. A memory I never consciously knew happened until that moment. The brain blocks out a lot of things as way to cope. Instead of dealing with stressors like it should, it tries to block things out and it can actually cause that memory to no longer consciously exist. My psychiatrist explained it to me like a filing system. Your brain takes memories and thoughts and files them away in certain places. The brain will put some away in a file that it will always go back to; aka its conscious memory file. Other memories will be put into a file that the brain doesn’t bring out as often; aka its subconscious file. Quite often, the brain will file those memories away the second they happen. This explains why I never consciously think about them. Every now and then, that file gets opened and a memory is brought out, causing me to suddenly, consciously, remember something that I, all along, subconsciously knew happened. I hate when a new memory comes about. It seems like there’s already so much I don’t want to think about, that there couldn’t possibly be anymore out there.
Trauma has completely convinced me that I am not worthy of love. It has bound me to itself; sometimes it feels like I’m bound to it for an eternity. But then I remember that’s not rational. It has convinced me that what happened to me is my fault and that I deserved every bit of it. Trauma has warped my perception of what love is supposed to be, and convinced me that what happened to me, was love. It has convinced me that I am a victim, not a survivor. Trauma has robbed me of life. It has robbed me of the zest I used to have for life. It has robbed me of enjoyment, love, peace, joy, trust, and happiness. It has robbed me of a healthy way of dealing with things, and a normal life. It robs me of every ounce of hope I am ever able to muster up. Trauma has made me its own personal prisoner. It makes my own skin feel like my own personal prison cell; a prison cell crawling with bugs and all I want to do is claw my way out of it; except I can’t.
I hate everything about trauma. I hate everything about PTSD and all of the things that come with it. I hate all of the memories I am stuck with. Despite my faith and what I know is right, some days, I even hate the people who have traumatized me. I am slowly learning that being able to admit that is healthy, as long as I work every single day towards love and forgiveness for those who have hurt me.
The last 14 months have been nearly unbearable, but therapy has been my saving grace. I have learned so much about PTSD, my trauma, and how to conquer my demons. All of the things that trauma has convinced me of are not true, and my counselor is the one who taught me that.
I am worthy. I am SO worthy of love and gentleness. What happened to me is not my fault, and I did not deserve any of it. I am not a victim. I am a survivor. I am not what happened to me. I am not defined by the actions of those who have hurt me. I am not a reflection of the actions from others. Love is not supposed to hurt, whether it’s a relationship or a friendship. Love is not supposed to leave you traumatized. Trauma has kept me silent for so long. But it will no longer keep me down and keep me quiet.
Someday I will know why all of this had to hurt so much. Someday there will be a purpose to all of this, and I will be able to use it for good. I am not brave yet, but I’m going to be.
If you or someone you know needs support right now, call the Suicide Prevention Lifeline at 1-800-273-8255, or text START to 741-741
6 notes
·
View notes
Text
Americans Demand a Rethinking of the ‘Forever War’
WASHINGTON — Nearly two decades after the fall of the World Trade Center and the attack on the Pentagon, American troops continue to wage war in Iraq, Afghanistan and lesser-known corners of the globe. President Trump almost opened another front last month when he approved the killing of Iran’s most powerful general.
“We took one of the world’s deadliest terrorists off the battlefield for good,” Secretary of State Mike Pompeo said recently, justifying the drone strike on Maj. Gen. Qassim Suleimani.
In other words, in the “war on terror,” the Iranian leader was fair game.
Last week, Democrats and some Republicans in the House voted to repeal a war authorization that has helped justify all manner of American military action abroad. It was a challenge not only to President Trump’s ability to take military action against Iran, but also to the thinking in Washington that has sustained the war-fighting since the attacks of Sept. 11, 2001.
For more than 18 years, the war on terrorism — the “forever war” or “endless war,” as many call it — has been used as the basis for an ever-expanding range of military actions: an invasion of Iraq that, by one count, has left nearly 300,000 dead; airstrikes in Afghanistan that have sometimes unintentionally killed scores at wedding parties as well as Qaeda leaders; and now the Suleimani drone strike. Mr. Trump said the general, who had helped arm anti-American militias in the Iraq war, had been plotting new “imminent and sinister attacks.”
On Tuesday, Mr. Trump is expected to articulate the direction of American foreign policy in his State of the Union address. Weeks after the United States and Iran nearly went to war, many Americans still want to know not just whether an attack was really “imminent,” the question that consumed Washington. They are asking whether the United States should continue fighting these wars at all, when the presence and actions of American troops ignite hostility and can sometimes heighten risks as much as limit them, critics say.
The sheer length of the conflicts has clarified for many Americans a stark moral question: whether any of the wars are still justified given the tolls — psychological, physical and spiritual — they have exacted on the United States and many other nations.
The concerns have come from both ends of the political spectrum. In condemning the killing of General Suleimani, Tucker Carlson, the conservative Fox News host, said the situation created by the Iraq war was “immoral” and that “we should leave, immediately.” Senator Elizabeth Warren of Massachusetts, a Democratic presidential candidate, said in a televised debate in January, “We should stop asking our military to solve problems that cannot be solved militarily.”
“Our keeping combat troops there is not helping,” she said of the Middle East.
That most politicians in Washington last month instead debated “imminence” reveals the enduring consensus over foreign policy that justifies the wars. The premise is that aggressive intervention abroad, forward deployments and fighting perceived enemies “over there” keep the United States safe. And besides protecting Americans, so it goes, these policies are necessary for the United States to carry out its mission as a shield against evil in the world.
In explaining last month why the United States would not discuss a troop withdrawal from Iraq — as demanded by Iraqi leaders furious over the drone strike on their soil — the State Department turned to that rationale, saying, “America is a force for good in the Middle East.” And in a recent speech on Iran policy, Mr. Pompeo invoked American exceptionalism: “America is a truly special place.”
But more Americans now believe that military adventurism after the Sept. 11 attacks has created greater dangers to the nation.
In a USA Today/Ipsos poll, 52 percent of respondents said the killing of General Suleimani had made the United States less safe. Online searches for “World War III” and “draft” surged in the days afterward. American citizens around the world received emails from embassies warning them of greater risks.
“The escalation over the past month is likely not over, especially now that we’ve crossed the line from proxy conflict to a direct confrontation between the United States and Iran,” said Dalia Dassa Kaye, an Iran expert at RAND Corporation, a research group. “We’re in a vicious cycle where escalation leads to more force presence, but more force presence may make the potential for escalation higher.”
Decades earlier, the Vietnam War spiraled into an expansive conflict with alarming ease, and generated furious debate across American society. As the war intensified in the late 1960s and ’70s, American officials carpet bombed Laos and Cambodia and tortured and assassinated Vietcong leaders in the name of defeating Communism. But, because of the draft, that war generated a moral debate in the United States that is absent today. In a searing 1967 speech on Vietnam, Martin Luther King Jr. said: “If America’s soul becomes totally poisoned, part of the autopsy must read ‘Vietnam.’ It can never be saved so long as it destroys the deepest hopes of men the world over.”
Afghanistan was supposed to be the “good war,” because Osama bin Laden and Al Qaeda had their base there, protected by the Taliban. But 18 years after the United States toppled the Taliban, 13,000 troops remain, propping up an embattled Afghan government. More than 2,400 American service members and more than 38,000 Afghan civilians have died, in a war costing the United States at least $2 trillion.
In September, Mr. Trump called off peace talks with the Taliban, dimming hopes of a withdrawal, though negotiations have since restarted.
Despite his denunciations of endless wars, Mr. Trump’s policies and actions have gone in the opposite direction. In December, he ordered 4,500 troops to the Middle East, adding to the 50,000 already there. In the last two years, the American military dropped bombs and missiles on Afghanistan at a record pace. In April, Mr. Trump vetoed a bipartisan congressional resolution to end American military involvement in Yemen’s devastating civil war.
Perhaps most significant, Mr. Trump withdrew in 2018 from a landmark nuclear containment deal with Iran and reimposed sanctions, setting off the chain of events that led to the killing of General Suleimani and a retaliatory missile strike by Iran that caused traumatic brain injuries to at least 64 American service members.
“The policies aren’t changing; in some ways, they’re getting worse,” said Stephen Wertheim, a historian and the co-founder of the Quincy Institute for Responsible Statecraft, a new research group in Washington financed by prominent billionaires — George Soros, a liberal, and Charles Koch, a conservative — who advocate American military restraint.
In some corners, though, there has been pushback against the notion that a lower troop presence leads to greater security. Proponents of the forever war point to President Barack Obama’s withdrawal from Iraq in 2011 as paving the way for the rise of the Islamic State in 2014.
But that ignores a whole set of circumstances, including the formal withdrawal agreement Mr. Bush had previously reached with the Iraqi government because the Iraqis wanted the Americans out, and the role of the Syrian civil war in creating the Islamic State. Most important, it ignores the lack of political will among American citizens for continuing the war.
Some lawmakers are trying to revoke the war authorizations of 2001 and 2002 — the first used for fighting Sept. 11-related terrorism and the second for invading Iraq — and looking for other ways to constrain Mr. Trump’s ability to expand the wars. In January, senators in the Republican-led chamber sponsoring legislation to limit military action against Iran said they had enough votes to pass the bill, the War Powers Resolution. The Democratic-led House passed a similar measure last month.
“I think the Suleimani killing and the escalation with Iran have clarified the stakes for some people who hadn’t been paying attention to the ongoing wars,” Mr. Wertheim said. “We very nearly got into another major war in the Middle East that’s not warranted by U.S. interests, and we still might.”
Even some hawkish foreign policy officials have begun to advocate a drawdown in the Middle East and Central Asia because of what they call the opportunity costs to America’s mission.
“One of the very odd pathologies of Washington and the defense establishment is this enthrallment with the Middle East, which just isn’t that important,” said Elbridge Colby, a former senior Pentagon official in the Trump administration. “America has become energy independent. And we’re not very good at achieving our preferred outcomes in the Middle East.”
Mr. Colby was the main author of the 2018 National Defense Strategy, which recommended turning America’s war-fighting focus to the “revisionist powers” of China and Russia.
Thomas Gibbons-Neff contributed reporting.
from WordPress https://mastcomm.com/americans-demand-a-rethinking-of-the-forever-war/
0 notes
Text
Testimony of a Suicide Survivor
I am a suicide survivor. I am also a Christian. This article explains how anyone, but especially people of faith, can survive or help others to survive the tragedy of a suicidal death of a family member or close friend.
My father committed suicide with an overdose of prescription medicine taken in conjunction with alcohol. Alcohol is a depressant that exacerbates suicidal tendencies in those who are prone to such self-destructive acts. I was 16 years old at the time. I was wrongly ashamed of my father’s suicide for most of my life. In fact, that feeling of shame is one of the great regrets of my life. With the combination of drugs and alcohol my dad might not have even intended to take his life. It could have been an accident. Their was no suicide note. He had no previous declaration of intent to commit suicide. The answer to that mystery we will never know. Still, officially his death certificate declared it a suicide.
If someone asked how my father died, I would say that he died of a heart attack. That is the response my mother repeatedly instructed me to say. The manner in which my father died was not about him in her mind. Rather, it was about us. My mother was concerned about what others would think of us if they knew my dad had committed suicide. Perhaps, she thought, they would blame us. They might suggest that we drive him to it. They might suggest that we failed to appropriately respond to his suicidal tendencies. In short, my mother worried that they might blame us for my father’s suicide.
Thoughts of if only we had done or said this or that constantly crept in to our minds. It was an emotionally destructive self-imposed guilt trip. Guilt can cripple. When guilty is unjustified it is especially damaging.
The Christian approach to guilt, real and imagined, is in recognition and confession of sin, and faith in the love, goodness, and power of God – “casting one’s cares upon him,” not – in no way– upon the probability of one’s own, or the suicide’s, lack of, or diminished-under-the-circumstances (mental illness), guilt. To cope with suicide one must dump their guilt. It does not belong in the grieving process. Grief is plenty enough to cope with without the burden of unnecessary and undeserved guilt.
Even in cases where no guilt is present the conscience will find occasion for and evidence to accuse. It’s a struggle I call the blame game. The blame game is a method of coping by blaming someone else for the suicidal death that torments you. Sometimes you blame another relative. Sometimes you blame the person who committed the suicide. Often it’s a combination thereof. This venting of anger on someone else tends to provide some measure of relief in the short term. It does not work in the long term. Blaming anyone for suicide is wrong most of the time. Where metal illness is the culprit, nobody and nothing except the mental illness itself is to blame. The sooner people come to terms with this truth the sooner they’ll be on the path to recovery.
Most people are ignorant about suicide. That is why they often shy away from family members or friends who are struggling with suitcase. It is wrong to be accused of or by the suicidal death of a family member or friend. It is cruel to desert those who are suffering. Feeling uncomfortable with suicide is never an excuse for rejecting those who struggle with this most tragic of deaths. Ask yourself, would you desert them if the person died of a heart attack or cancer? How can you desert them if their loved one died from suicidal mental illness?
Mental illness can kill just like cancer and heart disease. In suicide, most often it is the mental illness that kills, not the person. A mentally stable person does not react to angry words or events by killing themselves. Only mentally and emotionally sick people do that. That is why their response to anger or any other stimuli is irrational and ellogical. If they were healthy it is illegally their response would be suicide.
Depression affects your mental and emotional state of mind but it has a biological origin. Depression can be triggered by anger and resentment which have physiological effects. While the anger can elicit an emotional response, it is the biological mental illness (depression) that is the culprit. People get angry everyday but they do not kill themselves because they are mentally healthy. Here, you bought not blame or exculpate the person who committed suicide. This brings us to the mercy of God. He knows all, He is just and He is merciful. Take comfort in Gods mercy. Also take comfort in understanding that with few exceptions suicide is faultless and blameless.
Some 20 years after my fathers death I had to cope with multiple suicide attempts by my brother. It was scary and emotionally draining. My brother is still living – thank God. However, he had a lot of close calls. More than once death was knocking at his door. The family was notified to get to the hospital quickly. Doctors suspected my brother would survive his latest suicide attempt. After every
attempt he would be grateful for his life. He would also feel incredible guilt for the fear and heartache his suicide attempts brought on his family. Then he would get depressed and regress. Eventfully, like a vicious cycle, he’d attempt it again and again.
My brother is a Viet Nam veteran. Like so many vets who endured that conflict, he suffers from post-traumatic stress disorder (PTSD). He is designated as a service connected 100% disabled veteran. Depression is a consequence of PTSD. Fortunately my brother came to terms with his mental illness and thought treatment. I have no doubt that treatment, medication, and prayer are what saved
his life. It has allowed him to live a mostly productive life despite he still struggles with his illness. Treatment, medication, and prayer are the difference between my brother and our father. Our dad had none of these and, of course, he died.
A little over 20 years after my father’s death I had to deal with the suicidal death of the 14-year-old son of very close and dear friends. It was shocking and traumatic. Losing ones child unexpectedly is about the worst heartache one can ever endure. To lose that child as a result of suicide is far worse; it is indeed grief to the extreme.
There were warning signs, but they were not aware to his parents. He experienced slight personality and behavioral changes that were more observable at school and with his friends, especially his girlfriend, then at home. That’s why it’s important to communicate in the family setting. Depression is often difficult to see if you are not looking for it. School officials and friends either did not know the warning signs or they disregarded them. Families can not rely on others to inform them.
Symptoms of depression or suicidal feelings may include a change in eating or sleeping habits, withdrawal from friends and family, giving away valuable possessions, rebellious behavior, running away, drug and alcohol abuse, unexplained obsessions, decline in the quality of work or school work , and marked personality changes. It is important that parents, teachers, counselors, and pastors know and recognize these signs. It could save someone’s life.
Everything seemed normal that evening. Nothing seemed different or peculiar. It was a pleasant evening until his mother heard the gun shot that would be the beginning of grief on a huge scale. This would be compounded by the prevalent reasons why. It would have been accompanied by the expected guilt and blame which his family did not deserve to feel. It was not their fault. Nor was it his fault. His
mental illness killed him as surely as cancer takes its victims if left untreated. But a parent can not seek treatment or medication for their child unless they know that the child is sick.
It was difficult to go through this ordeal with them. I honestly sentenced their pain and shared their grief. Still, it was important to be there for them. It cemented our friendship and even took it to a new level. That is something to remember if you know someone who is trying to survive suicide. Be there for them. It’s the right thing to do. It’s the Christian thing to do. Do not just offer help and wait for a call that never comes. Insist on sharing their grief. If nothing else be there to sit with them, hold them, listen to them, or just silently occupy space with them. They will gain a measure of comfort just from your presence. They will know you are genuinely there for them if the grief becomes too much for them to bear alone.
Our most recent loss was the suicidal death of my niece. This was especially difficult to cope with. My mother is not very stable and I already explained my brother’s history. This was his daughter, his first-born. Worrying about how grief would impact them while dealing with my own grief was a monumental emotional undertaking. It took the saying be strong for them to a new level.
I watched my niece grow up in to a gem of a woman. She was as pure as the driven snow. She was devout in her Christian faith. She was a registered nurse who took pride in providing for the health care of others. She served her country honorably as a commissioner officer in the US Air Force. She was only in her early thirties but she was very sick. She was mentally ill.
My niece was bipolar. She had the most severe form of obsessive-compulsive disorder that her psychiatrists had ever seen. She also suffered from schizophrenic episodes and severe clinical depression. As an RN she understood her condition. She wanted to live but she did not know how to with so much mental anguish. Nobody could help her. No medications sufficed. As a woman of faith she struggled desperately and prayed continuously, on her knees, for hours at a time.
She had several suicide attempts that failed. It was destined that she would succeed at some point. When people are that sick they are unable to reason. They can not think clearly or rationalize effectively. All they do is suffer. It’s not surprising that they are focused on placing an end to that suffering. Mental illness can be very deadly.
It’s important to understand that healthy people do not kill themselves. A person who is depressed does not think like a typical person who feels good. They live in the here and now. Depression keeps them from looking forward to a better time. They can not comprehend positive thinking. Sometimes they do not even realize that they are sick much like my dad and our friend’s son. Sometimes they are very much aware of their mental illness like my brother and my niece. They seek help and struggle as best they can but sometimes nothing works for them. Not medication, not therapy; absolutely nothing helps them. These are the most severely afflicted with suicidal mental illness. My niece was one of these. They will continue to attempt suicide until they succeed. You can not help them. You can not save them. All you can do is pray for them.
It is disturbing when some so called experts say that suicide is preventable. It suggests that everyone who ever committed suicide could have been saved. While it is true that suicide is often preventable it is like wise true that sometimes it not. Suggesting other can lead to endless suffering and needless guilt by suicide survivors. The reality is that in sever cases of metal illness nothing short of divine intervention can save a suicidal person.
Remember, nobody who commits suicide asked for their depression. They would do anything to rid themselves of it. Being depressed is not the result of life choices any more than catching a cold is. Some people get it, and some do not. Such is life.
It is hard to imagine suicide being a sin in these clinically depressed people. One can not offend God by involuntarily contracting an illness, regardless of what the sickness may be. If suicide in such a circumstance constituted sin, then it would be sinful to catch the flu or die of pneumonia. It is comforting to know that most mainstream religions understand and share this perspective, especially Christian denominations. The Catholic church of my faith was once notorious about guilty associated with suicide. It taught that the commission of suicide was a mortal sin. This explains why my mother is still living a lie about her husband’s death. However, the Catholic Church has since clarified their position on the issue of suicide. The Catechism of the Catholic Church plainly states, “We should not despairs of the eternal salvation of persons who take their own lives …” (2282-83).
This does not mean that suicide is never sinful. If someone is of sound mind and premeditatedly acts to kill himself / herself for the purpose of punishment or harming another, that would be a sin. If they avoid deserved punishment by the state for a criminal conviction by committing suicide that is arguably a sin. Anyone who commits a suicidal act with malice aforethought for evil purposes is at grave risk of mortal sin. That is tantamount to murder, which is a crystal clear violation of Gods commandment: “Thou shall not kill.”
If a person, because of mental illness, certainly believes with their heart and soul that dying will somehow end the suffering and anguish of others, regardless of how wrong they may be, who could suspect that it is nonetheless a selfless act in the eyes of God. Remember, “No greater love has a man than to give his life for another.”
Some people who commit suicide exhibit intense courage in the undertaking. Consider the soldier who deliberately throws himself on a hand grenade or a land mine to save the lives of his comrades. Did he knowingly kill himself (ie, commit suicide)? Yes, of course he did. Was it also a courageous and self-less act of courage? Absolutely! It was courageous and selfless. We correctly label this soldier a hero. People who commit suicide are not rewards as some suggest. Jesus serves as a perfect example of one who suffered immensely and sacrificed his very life for the salvation of others. Sometimes we do need reminding.
Depression is usually a treatable disease. Most people who are depressed do not commit suicide or even attempt it. But they are more vulnerable to the risk of suicidal thoughts and they and their family members should be aware of this. Most people, who suffer from mental illness, without it is extreme, will benefit from therapy, medication, or a combination of these. In the case of depression medication very often can permit these people to live completely normal and happy lives. The key is first to recognize the problem and then obtain treatment as soon as possible.
Some people are more prone to suicide than others. They should be particularly alert to the warning signs of depression. Suicide tends to run in families. My family is living proof of this. Suicide most often results from brain disorders such as clinical depression, anxiety disorders, bipolar illness, schizophrenia, and severe obsessive-compulsive disorder. All of these brain disorders have a genetic component that, if left untreated or mistreated, can result in suicide. The risks of suicide increase considering the longer a person goes without treatment. That is why it is dangerous for a depressed person to avoid treatment for fear that he or she might be labeled as being crazy. We are living in modern times. We are way beyond such foolishness; at least weought to be.
If you suffer from depression do not take a chance – get help. If your child is depressed, get your child help and do it quickly. Do this even in the face of resistance. You just might be saving their lives.
It is estimated that mental illness is the cause of 95% of all suicides. The # 1 cause of suicide is untreated depression. Ninety-five percent of all suicides are the direct result of the aforementioned brain disorders. According to the National Mental Health Association the teen suicide rate has risen an astonishing 200% in the last 40 years. That is a rate three times what it was in 1960. Suicide is the 3rd leading cause of death for 15 – 24 year-olds. About five thousand 15 – 24 year-olds kill themselves every year. These are alarming figures.
In conclusion, it is important to point out that maintaining your faith will increase your rate of recovery from the tragedy of suicide. Do not pray less. Instead pray more. Your faith will be your greatest source of comfort. Do not be mad at God. God did not betray you by letting your loved one die. He understands the pain of death. He endured it with the sacrificial death of his only begotten son for your sake and everyone else’s. Jesus understands the pain of death. Remember how He wept for Lazarus. Remember how he suffered in His own blameless death. Remember how His blessed mother Mary died when He died. Remember the painful deaths of His Apostles.
Remember, everyone dies of something; it’s preordained. We can not escape death, at least not in this worldly life. Your loved one just happened to die of mental illness that ruled in suicide. Even in this worldly death we still remain spiritually linked. You have not lost your loved ones. You have merely postpones being in their company until such time as God calls you home. He will do that plenty soon enough so do not try to rush the process. Remember it’s about His will, not yours.
If ever you have to end being a suicide survivor take comfort in knowing that you can survive even though the anguish of your loss may at first seem to be insurmountable. Everyone must go through a grieving process when a loved one dies. The grief associated with the suicidal death of a loved one is manifestly more difficult to cope with than other types of death. But, it is also similar in that it will likewise end. You do not needarily get over your loss; that void is always there. However, you do learn to cope and deal with it. Your pain will go away. You will come to understand that your loved one remains with you in spirit and you with him or her. You will laugh again. You will experience love and
joy. You will obtain peace of mind even though you’ll always have the sorrow associated with loss. But we feel sorry when we lose our youth and vitality too. That does not mean that we stay miserable because of it.
Definitely grieve, but also let go. Get professional, spiritual, or other help if you need it. Accept the fate that you are dealt just as Jesus and his blessed mother accepted the fate of the Holy sacrifice at Calvary. Jesus, while suffering the pains of crucifixion asked of his heavenly father, “Why hast thou forsaken me.” Even the Son of man asked why. He also said “Thy will be done.” Our Lord in faith accepted his fate and in so doing taught us to do the same. We do not have to know and understand everything. In faith we must just believe, as Jesus did, that God understands and knows what is best. He will take care of things, perfectly. Accept, as Jesus did, the fate you are dealt no matter how much it hurts at the time. After all, you can not change it and you are not responsible for it.
Understand the difference between holding on to a memory and clinging to a soul. Release the soul from your mind so that your loved one can be with our Lord where he or she will prepare a place for you when your time comes. You will be together again and the next time it will be for all eternity. That will be a joyful eternity with God almighty. Trust in God and maintain your faith. God will make it right. You will survive.
Copyright: Ed Coet
Source by Ed Coet
from Home Solutions Forev https://homesolutionsforev.com/testimony-of-a-suicide-survivor/
via Home Solutions on WordPress
from Home Solutions FOREV https://homesolutionsforev.tumblr.com/post/185780686270
via Tim Clymer on Wordpress
0 notes
Text
Testimony of a Suicide Survivor
I am a suicide survivor. I am also a Christian. This article explains how anyone, but especially people of faith, can survive or help others to survive the tragedy of a suicidal death of a family member or close friend.
My father committed suicide with an overdose of prescription medicine taken in conjunction with alcohol. Alcohol is a depressant that exacerbates suicidal tendencies in those who are prone to such self-destructive acts. I was 16 years old at the time. I was wrongly ashamed of my father's suicide for most of my life. In fact, that feeling of shame is one of the great regrets of my life. With the combination of drugs and alcohol my dad might not have even intended to take his life. It could have been an accident. Their was no suicide note. He had no previous declaration of intent to commit suicide. The answer to that mystery we will never know. Still, officially his death certificate declared it a suicide.
If someone asked how my father died, I would say that he died of a heart attack. That is the response my mother repeatedly instructed me to say. The manner in which my father died was not about him in her mind. Rather, it was about us. My mother was concerned about what others would think of us if they knew my dad had committed suicide. Perhaps, she thought, they would blame us. They might suggest that we drive him to it. They might suggest that we failed to appropriately respond to his suicidal tendencies. In short, my mother worried that they might blame us for my father's suicide.
Thoughts of if only we had done or said this or that constantly crept in to our minds. It was an emotionally destructive self-imposed guilt trip. Guilt can cripple. When guilty is unjustified it is especially damaging.
The Christian approach to guilt, real and imagined, is in recognition and confession of sin, and faith in the love, goodness, and power of God – "casting one's cares upon him," not – in no way– upon the probability of one's own, or the suicide's, lack of, or diminished-under-the-circumstances (mental illness), guilt. To cope with suicide one must dump their guilt. It does not belong in the grieving process. Grief is plenty enough to cope with without the burden of unnecessary and undeserved guilt.
Even in cases where no guilt is present the conscience will find occasion for and evidence to accuse. It's a struggle I call the blame game. The blame game is a method of coping by blaming someone else for the suicidal death that torments you. Sometimes you blame another relative. Sometimes you blame the person who committed the suicide. Often it's a combination thereof. This venting of anger on someone else tends to provide some measure of relief in the short term. It does not work in the long term. Blaming anyone for suicide is wrong most of the time. Where metal illness is the culprit, nobody and nothing except the mental illness itself is to blame. The sooner people come to terms with this truth the sooner they'll be on the path to recovery.
Most people are ignorant about suicide. That is why they often shy away from family members or friends who are struggling with suitcase. It is wrong to be accused of or by the suicidal death of a family member or friend. It is cruel to desert those who are suffering. Feeling uncomfortable with suicide is never an excuse for rejecting those who struggle with this most tragic of deaths. Ask yourself, would you desert them if the person died of a heart attack or cancer? How can you desert them if their loved one died from suicidal mental illness?
Mental illness can kill just like cancer and heart disease. In suicide, most often it is the mental illness that kills, not the person. A mentally stable person does not react to angry words or events by killing themselves. Only mentally and emotionally sick people do that. That is why their response to anger or any other stimuli is irrational and ellogical. If they were healthy it is illegally their response would be suicide.
Depression affects your mental and emotional state of mind but it has a biological origin. Depression can be triggered by anger and resentment which have physiological effects. While the anger can elicit an emotional response, it is the biological mental illness (depression) that is the culprit. People get angry everyday but they do not kill themselves because they are mentally healthy. Here, you bought not blame or exculpate the person who committed suicide. This brings us to the mercy of God. He knows all, He is just and He is merciful. Take comfort in Gods mercy. Also take comfort in understanding that with few exceptions suicide is faultless and blameless.
Some 20 years after my fathers death I had to cope with multiple suicide attempts by my brother. It was scary and emotionally draining. My brother is still living – thank God. However, he had a lot of close calls. More than once death was knocking at his door. The family was notified to get to the hospital quickly. Doctors suspected my brother would survive his latest suicide attempt. After every
attempt he would be grateful for his life. He would also feel incredible guilt for the fear and heartache his suicide attempts brought on his family. Then he would get depressed and regress. Eventfully, like a vicious cycle, he'd attempt it again and again.
My brother is a Viet Nam veteran. Like so many vets who endured that conflict, he suffers from post-traumatic stress disorder (PTSD). He is designated as a service connected 100% disabled veteran. Depression is a consequence of PTSD. Fortunately my brother came to terms with his mental illness and thought treatment. I have no doubt that treatment, medication, and prayer are what saved
his life. It has allowed him to live a mostly productive life despite he still struggles with his illness. Treatment, medication, and prayer are the difference between my brother and our father. Our dad had none of these and, of course, he died.
A little over 20 years after my father's death I had to deal with the suicidal death of the 14-year-old son of very close and dear friends. It was shocking and traumatic. Losing ones child unexpectedly is about the worst heartache one can ever endure. To lose that child as a result of suicide is far worse; it is indeed grief to the extreme.
There were warning signs, but they were not aware to his parents. He experienced slight personality and behavioral changes that were more observable at school and with his friends, especially his girlfriend, then at home. That's why it's important to communicate in the family setting. Depression is often difficult to see if you are not looking for it. School officials and friends either did not know the warning signs or they disregarded them. Families can not rely on others to inform them.
Symptoms of depression or suicidal feelings may include a change in eating or sleeping habits, withdrawal from friends and family, giving away valuable possessions, rebellious behavior, running away, drug and alcohol abuse, unexplained obsessions, decline in the quality of work or school work , and marked personality changes. It is important that parents, teachers, counselors, and pastors know and recognize these signs. It could save someone's life.
Everything seemed normal that evening. Nothing seemed different or peculiar. It was a pleasant evening until his mother heard the gun shot that would be the beginning of grief on a huge scale. This would be compounded by the prevalent reasons why. It would have been accompanied by the expected guilt and blame which his family did not deserve to feel. It was not their fault. Nor was it his fault. His
mental illness killed him as surely as cancer takes its victims if left untreated. But a parent can not seek treatment or medication for their child unless they know that the child is sick.
It was difficult to go through this ordeal with them. I honestly sentenced their pain and shared their grief. Still, it was important to be there for them. It cemented our friendship and even took it to a new level. That is something to remember if you know someone who is trying to survive suicide. Be there for them. It's the right thing to do. It's the Christian thing to do. Do not just offer help and wait for a call that never comes. Insist on sharing their grief. If nothing else be there to sit with them, hold them, listen to them, or just silently occupy space with them. They will gain a measure of comfort just from your presence. They will know you are genuinely there for them if the grief becomes too much for them to bear alone.
Our most recent loss was the suicidal death of my niece. This was especially difficult to cope with. My mother is not very stable and I already explained my brother's history. This was his daughter, his first-born. Worrying about how grief would impact them while dealing with my own grief was a monumental emotional undertaking. It took the saying be strong for them to a new level.
I watched my niece grow up in to a gem of a woman. She was as pure as the driven snow. She was devout in her Christian faith. She was a registered nurse who took pride in providing for the health care of others. She served her country honorably as a commissioner officer in the US Air Force. She was only in her early thirties but she was very sick. She was mentally ill.
My niece was bipolar. She had the most severe form of obsessive-compulsive disorder that her psychiatrists had ever seen. She also suffered from schizophrenic episodes and severe clinical depression. As an RN she understood her condition. She wanted to live but she did not know how to with so much mental anguish. Nobody could help her. No medications sufficed. As a woman of faith she struggled desperately and prayed continuously, on her knees, for hours at a time.
She had several suicide attempts that failed. It was destined that she would succeed at some point. When people are that sick they are unable to reason. They can not think clearly or rationalize effectively. All they do is suffer. It's not surprising that they are focused on placing an end to that suffering. Mental illness can be very deadly.
It's important to understand that healthy people do not kill themselves. A person who is depressed does not think like a typical person who feels good. They live in the here and now. Depression keeps them from looking forward to a better time. They can not comprehend positive thinking. Sometimes they do not even realize that they are sick much like my dad and our friend's son. Sometimes they are very much aware of their mental illness like my brother and my niece. They seek help and struggle as best they can but sometimes nothing works for them. Not medication, not therapy; absolutely nothing helps them. These are the most severely afflicted with suicidal mental illness. My niece was one of these. They will continue to attempt suicide until they succeed. You can not help them. You can not save them. All you can do is pray for them.
It is disturbing when some so called experts say that suicide is preventable. It suggests that everyone who ever committed suicide could have been saved. While it is true that suicide is often preventable it is like wise true that sometimes it not. Suggesting other can lead to endless suffering and needless guilt by suicide survivors. The reality is that in sever cases of metal illness nothing short of divine intervention can save a suicidal person.
Remember, nobody who commits suicide asked for their depression. They would do anything to rid themselves of it. Being depressed is not the result of life choices any more than catching a cold is. Some people get it, and some do not. Such is life.
It is hard to imagine suicide being a sin in these clinically depressed people. One can not offend God by involuntarily contracting an illness, regardless of what the sickness may be. If suicide in such a circumstance constituted sin, then it would be sinful to catch the flu or die of pneumonia. It is comforting to know that most mainstream religions understand and share this perspective, especially Christian denominations. The Catholic church of my faith was once notorious about guilty associated with suicide. It taught that the commission of suicide was a mortal sin. This explains why my mother is still living a lie about her husband's death. However, the Catholic Church has since clarified their position on the issue of suicide. The Catechism of the Catholic Church plainly states, "We should not despairs of the eternal salvation of persons who take their own lives …" (2282-83).
This does not mean that suicide is never sinful. If someone is of sound mind and premeditatedly acts to kill himself / herself for the purpose of punishment or harming another, that would be a sin. If they avoid deserved punishment by the state for a criminal conviction by committing suicide that is arguably a sin. Anyone who commits a suicidal act with malice aforethought for evil purposes is at grave risk of mortal sin. That is tantamount to murder, which is a crystal clear violation of Gods commandment: "Thou shall not kill."
If a person, because of mental illness, certainly believes with their heart and soul that dying will somehow end the suffering and anguish of others, regardless of how wrong they may be, who could suspect that it is nonetheless a selfless act in the eyes of God. Remember, "No greater love has a man than to give his life for another."
Some people who commit suicide exhibit intense courage in the undertaking. Consider the soldier who deliberately throws himself on a hand grenade or a land mine to save the lives of his comrades. Did he knowingly kill himself (ie, commit suicide)? Yes, of course he did. Was it also a courageous and self-less act of courage? Absolutely! It was courageous and selfless. We correctly label this soldier a hero. People who commit suicide are not rewards as some suggest. Jesus serves as a perfect example of one who suffered immensely and sacrificed his very life for the salvation of others. Sometimes we do need reminding.
Depression is usually a treatable disease. Most people who are depressed do not commit suicide or even attempt it. But they are more vulnerable to the risk of suicidal thoughts and they and their family members should be aware of this. Most people, who suffer from mental illness, without it is extreme, will benefit from therapy, medication, or a combination of these. In the case of depression medication very often can permit these people to live completely normal and happy lives. The key is first to recognize the problem and then obtain treatment as soon as possible.
Some people are more prone to suicide than others. They should be particularly alert to the warning signs of depression. Suicide tends to run in families. My family is living proof of this. Suicide most often results from brain disorders such as clinical depression, anxiety disorders, bipolar illness, schizophrenia, and severe obsessive-compulsive disorder. All of these brain disorders have a genetic component that, if left untreated or mistreated, can result in suicide. The risks of suicide increase considering the longer a person goes without treatment. That is why it is dangerous for a depressed person to avoid treatment for fear that he or she might be labeled as being crazy. We are living in modern times. We are way beyond such foolishness; at least weought to be.
If you suffer from depression do not take a chance – get help. If your child is depressed, get your child help and do it quickly. Do this even in the face of resistance. You just might be saving their lives.
It is estimated that mental illness is the cause of 95% of all suicides. The # 1 cause of suicide is untreated depression. Ninety-five percent of all suicides are the direct result of the aforementioned brain disorders. According to the National Mental Health Association the teen suicide rate has risen an astonishing 200% in the last 40 years. That is a rate three times what it was in 1960. Suicide is the 3rd leading cause of death for 15 – 24 year-olds. About five thousand 15 – 24 year-olds kill themselves every year. These are alarming figures.
In conclusion, it is important to point out that maintaining your faith will increase your rate of recovery from the tragedy of suicide. Do not pray less. Instead pray more. Your faith will be your greatest source of comfort. Do not be mad at God. God did not betray you by letting your loved one die. He understands the pain of death. He endured it with the sacrificial death of his only begotten son for your sake and everyone else's. Jesus understands the pain of death. Remember how He wept for Lazarus. Remember how he suffered in His own blameless death. Remember how His blessed mother Mary died when He died. Remember the painful deaths of His Apostles.
Remember, everyone dies of something; it's preordained. We can not escape death, at least not in this worldly life. Your loved one just happened to die of mental illness that ruled in suicide. Even in this worldly death we still remain spiritually linked. You have not lost your loved ones. You have merely postpones being in their company until such time as God calls you home. He will do that plenty soon enough so do not try to rush the process. Remember it's about His will, not yours.
If ever you have to end being a suicide survivor take comfort in knowing that you can survive even though the anguish of your loss may at first seem to be insurmountable. Everyone must go through a grieving process when a loved one dies. The grief associated with the suicidal death of a loved one is manifestly more difficult to cope with than other types of death. But, it is also similar in that it will likewise end. You do not needarily get over your loss; that void is always there. However, you do learn to cope and deal with it. Your pain will go away. You will come to understand that your loved one remains with you in spirit and you with him or her. You will laugh again. You will experience love and
joy. You will obtain peace of mind even though you'll always have the sorrow associated with loss. But we feel sorry when we lose our youth and vitality too. That does not mean that we stay miserable because of it.
Definitely grieve, but also let go. Get professional, spiritual, or other help if you need it. Accept the fate that you are dealt just as Jesus and his blessed mother accepted the fate of the Holy sacrifice at Calvary. Jesus, while suffering the pains of crucifixion asked of his heavenly father, "Why hast thou forsaken me." Even the Son of man asked why. He also said "Thy will be done." Our Lord in faith accepted his fate and in so doing taught us to do the same. We do not have to know and understand everything. In faith we must just believe, as Jesus did, that God understands and knows what is best. He will take care of things, perfectly. Accept, as Jesus did, the fate you are dealt no matter how much it hurts at the time. After all, you can not change it and you are not responsible for it.
Understand the difference between holding on to a memory and clinging to a soul. Release the soul from your mind so that your loved one can be with our Lord where he or she will prepare a place for you when your time comes. You will be together again and the next time it will be for all eternity. That will be a joyful eternity with God almighty. Trust in God and maintain your faith. God will make it right. You will survive.
Copyright: Ed Coet
Source by Ed Coet
from Home Solutions Forev https://homesolutionsforev.com/testimony-of-a-suicide-survivor/
via Home Solutions on WordPress
0 notes
Text
How to Manage Chronic Pain — Naturally
Jennifer Kane has been hurting for a long time. Spinal stenosis, degenerative disc disease, and a ripped spine following a complicated childbirth have all contributed to more than 15 years of chronic pain.
Despite multilevel spinal-fusion surgery, six weeks of physical therapy, and x-rays showing she had healed well, she still suffered intense discomfort. Kane’s doctor prescribed opioids to manage her pain, but they made her ill. She also tried the myriad muscle relaxers, antidepressants, and anti-inflammatory drugs her physician suggested.
In the end, she concluded that relief was not going to come in the form of a pill.
“You think doctors have a giant toolbox of things they can give you, but that’s not really true,” says Kane, an author and communications strategist in Minneapolis. “If you keep coming back because your pain isn’t getting better, there’s not much else they can do. They just told me, ‘It sucks, doesn’t it?’”
So Kane set out to research the latest treatments for chronic pain, eventually compiling her findings into a book, Chronic Pain Recovery: A Practical Guide to Putting Your Life Back Together After Everything Has Fallen Apart.
“For me, what worked was a combination of things,” she explains. “Acceptance, my support network, and a bunch of physical and mental lifestyle changes have added up not to a cure but to putting my pain in a manageable place.”
Effective management of chronic pain — an often invisible but life-altering condition suffered by an estimated 100 million Americans — nearly always requires a multifaceted approach, one that takes into account physical, social, and emotional factors.
It’s a difficult puzzle for patients and physicians alike. But with a more thorough understanding of the root causes of chronic pain and a growing number of therapies and techniques to address them, many now believe it can be not only managed but overcome.
The Body in Pain
Pain serves an important purpose: It communicates what is happening in the body. During childbirth, for instance, it indicates progression, a necessary element in the process of labor. Day by day, it alerts us to injury and illness and, like a guardrail, dissuades us from actions that lead to even more painful outcomes.
But what if there’s no discernible cause of pain and its warning signal doesn’t fade, instead wailing like a faulty tornado siren all day and night, drowning out the birds, the voices of friends and family, even one’s own thoughts?
Chronic pain is fundamentally different from what we experience in the immediate aftermath of an injury. Acute pain results from a specific impact or event (such as a cut or a blow) and typically dissipates in less than six weeks. Subacute pain can last up to 12 weeks. Chronic pain lasts for more than three months.
“Studies have looked at the areas of the brain that light up with these different kinds of pain,” explains Joseph Garbely, MD, medical director at Caron Treatment Centers, an addiction-recovery facility in Pennsylvania. “With acute and subacute pain, we see activity in areas known as the pain matrix [including the dorsal anterior cingulate cortex, thalamus, and insula].
“But with chronic pain, different areas light up. There’s a shifting of activation to the mood centers, where anxiety and depression come from.”
That’s the challenge. Even as the brain signature of chronic pain shifts entirely to the emotion centers, patients report the same physical discomfort they felt in the acute stage.
“Unfortunately, in too many cases, acute pain doesn’t cease when it should, but continues long after the original injury has been repaired, becoming chronic pain,” writes Peter Abaci, MD, medical director of the Bay Area Pain and Wellness Center, in his book, Conquer Your Chronic Pain: A Life-Changing Drug-Free Approach for Relief, Recovery, and Restoration.
“While acute pain can be seen as a fleeting symptom, it helps to view chronic pain as a disease in and of itself, like diabetes and hypertension.”
The Mind in Pain
Chronic pain manifests in structural changes to the brain that Abaci refers to as the “pain brain.” These include the actual loss of gray matter (which can lead to cloudy thinking and poor decision-making) and disruption in the hippocampus (which regulates learning and memory). “Chronic pain rewires the whole computer,” he explains.
These changes create neural pathways, and their repeated activation results in a feedback loop of physical pain — and negative thoughts.
“All pain has an emotional component to it,” says Garbely. “When you burn your finger, you feel anxiety and worry. But those emotions are ubiquitous in chronic pain — they become front and center and lead to greater feelings of pain.”
Salim Ghazi, MD, chair of the Department of Pain Medicine at Mayo Clinic’s Florida campus, agrees.
“When pain becomes so chronic that it induces the emotional component of depression and anxiety, then the second beast starts feeding on the first,” he says. “People feel more pain, then they get even more depressed, and the depression makes the pain worse. It becomes a vicious cycle.”
The Opioid Pendulum
Opioids, including morphine and heroin, were popular pain-management remedies in the 19th century. But as their addictive nature became increasingly clear, doctors began restricting their use. From the 1920s to the ’90s, opioids were prescribed only immediately following surgery or to terminally ill cancer patients.
In the mid-’80s, Russell Portenoy, MD, a pain-management specialist, spearheaded a push to expand the use of opioids beyond the treatment of cancer pain. He studied 38 patients suffering from depression and chronic pain and found that they showed marked improvement on both fronts during several months of opioid treatment.
“Because of that study, the pendulum swung from ‘no opioids’ to ‘opioids for all,’” says Ghazi. He also notes that Portenoy never followed up with the patients, despite requests from the study’s funders that he evaluate them at the one- and two-year marks.
“The American Medical Association (AMA) made pain the fifth vital sign. Physicians were required to ask patients about their pain and to give opioids for strong pain,” Ghazi explains. “If we didn’t, we were reported and penalized.” (The AMA has since removed this requirement in response to the opioid crisis.)
By the late ’90s, doctors were prescribing opioids for a wide range of chronic-pain conditions, including arthritis, herniated discs, fibromyalgia, and more. The trend peaked in 2012, with physicians writing 259 million opioid prescriptions — enough to supply every American adult.
Opioids work by mimicking a pain-reducing neurotransmitter the body produces naturally. The drug binds to opioid receptors throughout the body, blocking pain signals sent to the brain through the spinal column.
“We have about 130 neurotransmitters in the body — a river of messenger chemicals that allow the body to do everything it needs to do, from having and expressing emotions to experiencing enjoyment to digesting food to fighting off disease,” explains Loretta Butehorn, PhD, CCH, a Boston-based psychologist and homeopath specializing in substance-abuse and mental-health treatment.
“A lot of pain medications are addictive because they have a structure similar to some of those neurotransmitters,” she says. “And long-term use of opioids diminishes the body’s ability to produce its own pain-suppressing neurotransmitters.”
“When you introduce opioids, you’re affecting how a person works on every level,” notes Abaci, “and there’s a big issue when you try to take them away.”
Addiction and overdoses are not the only devastating results of opioids. Their long-term use can cause increased suffering and sensitivity over time. Opioid-induced hyperalgesia is a cruelly paradoxical condition in which chronic opioid users actually experience a heightened sensitivity to pain.
“Not only do opioid drugs stop working effectively to dull pain,” explains Mel Pohl, MD, in The Pain Antidote, “but over time they actually start feeding and nourishing the pain — which often leads to taking higher and higher doses to get any pain relief at all.”
Long-term opioid users may also suffer from allodynia — a condition in which normal daily stimuli (such as putting on a shirt or receiving a hug) cause excruciating pain. Sustained opioid use causes “pain fibers to do the opposite of what they’re supposed to do,” explains Garbely. “This has been known by pain specialists, but the opioid epidemic is hastening the education of physicians around how pain works.”
Today, as the opioid pendulum once again swings toward restriction, millions who endure chronic pain —and the physicians who treat them — are in desperate need of more effective alternatives to address their very real suffering.
Overcoming Trauma
In his book The Wisdom of the Healing Wound, David Knighton, MD, describes the necessary process of cleaning out a wound — whether it’s physical, psychological, or spiritual — before it can begin to heal. Just as we need to remove dirt and gravel from a cut, Knighton suggests, we need to purge the less visible detritus (such as shame, anger, trauma, and despair) that keeps our spirits and psyches from mending.
Multiple studies demonstrate a connection between chronic pain and trauma. As many as half of all pain patients also exhibit symptoms of posttraumatic stress disorder (PTSD), including anxiety, agitation, mood swings, nightmares, and insomnia.
Abaci explains that there are three types of trauma associated with chronic pain: The first is the trauma of the wound itself, such as what a soldier feels when injured in battle. The second is when someone with a history of physical, emotional, or sexual abuse experiences a heightened pain response when a past trauma is reactivated by illness or injury. The third is when chronic pain itself becomes traumatic and results in nightmares, depression, and panic attacks.
“When a person experiences trauma, they aren’t going to get better until you get the trauma quieted down,” says Abaci. “You have to calm down the nervous system.”
At the Bay Area Pain and Wellness Center, Abaci and his team employ a variety of techniques — individual counseling, group therapy, meditation, yoga, physical therapy, nutrition counseling, and art therapy. All of these work together to untangle the web of pain, trauma, and negative thoughts that reinforce the entrenched patterns of the pain brain.
Abaci shares the case of Sgt. Shane Savage as a prime example. An active-duty solider in Afghanistan in 2010, Savage suffered a concussion and 24 broken bones when his armored truck was blown apart by a roadside bomb. He was soon taking high doses of strong painkillers while still suffering from ongoing pain, PTSD, depression, and tremors.
After he attempted suicide by overdose, he was sent to a psychiatric hospital, where he detoxed from the painkillers — but only temporarily.
Upon his release, he promptly resumed his morphine habit, taking up to 300 mg daily. (An average daily dose for managing extreme pain is about 60 mg.)
It wasn’t until he completed a multidisciplinary chronic-pain program at the Veterans Affairs hospital in Tampa, Fla., that he found sustained relief from both his pain and his opioid dependence.
The difference between purely pharmaceutical and more multidisciplinary approaches to treating pain, says Ghazi, is like giving people fish for one meal versus teaching them how to catch their own.
“It’s the difference between giving someone a pill every six hours and a program that teaches them how to cope, how to exercise, when to rest, when to push, and when not to push,” he explains.
Ghazi hopes that integrative approaches to pain, such as the one he uses at Mayo Clinic, will continue to serve as examples for other programs and clinics as the medical system seeks safer, more sustainable and effective solutions.
Changing the Pain Brain
Chronic pain is a complex problem. There is no magic bullet or single pharmaceutical solution. Researchers increasingly understand it as a biopsychosocial phenomenon in which emotions, thought patterns, and beliefs play as much (or more) of a role as physical factors.
This is why the most effective pain-rehabilitation programs now typically employ a wide variety of approaches that address the root causes of chronic pain — physical, psychological, emotional, and spiritual.
“Pain pills, implanted devices, and surgeries have their use,” Abaci notes, “but they do nothing to . . . restore the ‘pain brain’ back to health. The only way to alleviate this kind of pain is to change the brain.”
The notion that the mind plays a role in chronic pain can be a tough pill to swallow for sufferers, many of whom have faced suspicion from family, friends, and doctors who believe they’re inventing or exaggerating their discomfort.
“When it’s invisible, people think you’re making it up,” says Jennifer Kane. “And that delegitimizes the trauma you’re experiencing. No wonder people in pain are depressed!”
This makes it all the more vital to recognize that chronic pain is real pain. At the same time, it is pain whose root causes often lie as much in the brain as in the body — and that is good news, because the brain’s inherent plasticity means that it can change.
Kane has experienced this firsthand. “The multidisciplinary approach is a lot more work than opioids,” she says, “but it’s a better long-term strategy.”
After emerging from the darkest of places, she embarked on her own recovery journey — which involved changing her diet, practicing mindfulness meditation, getting support for her mental health, and making myriad other physical and mental adjustments.
“Pain makes your world so small,” she says. “You stop leaving the house and connecting with people because you can’t rely on your body. You don’t have any hope, any plans. You just have pain.”
And now? “Now I work on my dreams and goals,” Kane says. “I’ve accepted my new ground rules, and I have hope, excitement, and relationships.
“My world still has limits, but my brain doesn’t so much anymore.
This originally appeared as “Pain Relief” in the November 2018 print issue of Experience Life.
Get the full story at https://experiencelife.com/article/how-to-manage-chronic-pain-naturally/
0 notes