Text
THAT’S A WRAP!
My experience as a first-year medical student was really a roller-coaster ride. I entered medical school knowing what to expect but not knowing how to deal with it. It was very exciting and challenging at the same time. However, there were times that I wished I could’ve done better. I know that here were factors that negatively affected my performance. Growing up in South Luzon, I had a really hard time adjusting to the city life. It was my first time to study in Manila and live by myself far away from my family. I am very thankful for my friends, groupmates, classmates, and professors who became my comfort zone as I aim to get by every day.




My first-year medical student journey was really unexpected. Nobody knew what was coming for us in 2020 and we all had to adjust to our current situation. Nonetheless, now is the time to utilize available resources in order to continue our learning experience. I hope this would not be a hindrance as I am trying to cope up and not let a pandemic stop me from being promoted to second year medical school. To be honest, having senior parents (one even being a frontliner), not having a stable income, owning up to additional household responsibilities, with balancing my academics on the side is not really easy to do. However, we should all continue to be strong.
We should be reminded that in order to win during a losing period such as this, everyone has an important and crucial role, no matter how small. May it be staying home, washing your hands, complying to social distancing or disclosing information that may potentially save others - we all have that role and capability to be of service. For doctors and other health care professionals or even those who sanitize the hospitals - it is being brave and serving despite the cost. For the patients, it is minimizing the spread of the infection. For us, it is helping in whatever way we can.
Let us continue to hope and pray for our country more than ever. Now is also the time for our decision makers to think critically and intelligently for the benefit of everyone.
0 notes
Text
Realizations
Cancer is one of main causes of morbidity and mortality worldwide. It is a very complicated condition that affects treatment toxicity, financial hardship, and reduction in quality of life.
As a future healthcare worker, encountering patients like these will be very challenging. That is why it is important that we understand the prognosis of the disease. We should also be able to instill good communication skills to be sure that patients and family members also understand the treatments, procedures, and possible consequences. Clear communication will better help patients understand their options and receive the supportive care they need to prolong their lives since there is really no cure yet for cancer.
As a medical student, learning and understanding the biochemistry of cancer made me realize its importance in discovering not only more effective treatments and managements for the survival of affected individuals, but also preventing others from it.
As an individual, I also realized that surviving cancer implies living with cancer while having a positive attitude that requires courage to still live, love, and care. It is also about focusing on finding the most meaningful way to live with cancer, which means to keep loving and staying connected to life and the people around them. Courage means living with an open heart and embracing human frailty, vulnerability, and mortality by still having hopes and dreams and finding the meaning and purpose of life. Cancer patients should never lose hope because there are a lot of people who will support them on their journey, including health care workers.
I enjoyed this activity because it made biochemistry (which is a really hard technical subject to understand) quite easy and fun. Understanding the different pathways is not only beneficial in understanding cancer. There are various other conditions that can be learned through biochemistry as this subject has a very large scope. Overall, my biochemistry journey was enjoyable – from listening to lectures, doing experiments, and having group discussions and forums – and I also thank my professors for that.
Not having an extensive background in biochemistry did not hinder me from becoming a future 5-star physician. Some of my realizations on qualities of a 5-star physician include being able to do research and putting your patients above all else. If a patient sees that his or her doctor genuinely cares, it improves the quality of treatment and life the patient receives. It is also important for patients to be involved in discussions and decision making so that they have a clear understanding and communication with their doctor.
0 notes
Text
LEARNING JOURNEY
Shifting to online classes is hard and challenging because our platform for learning may be limited. Not being able to fully experience doing experiments and listening to lectures physically may not be the best measure of learning. Nonetheless, we must continue to unleash our full potential and look for alternative ways to supplement our learning. Moreover, our professors have also given their extra effort into aiming to provide the quality education that we students deserve.
During these trying times, our professors have given their copies of lectures online and provided formative quizzes to test what we have learned. They also provided discussion threads for questions regarding their provided materials.
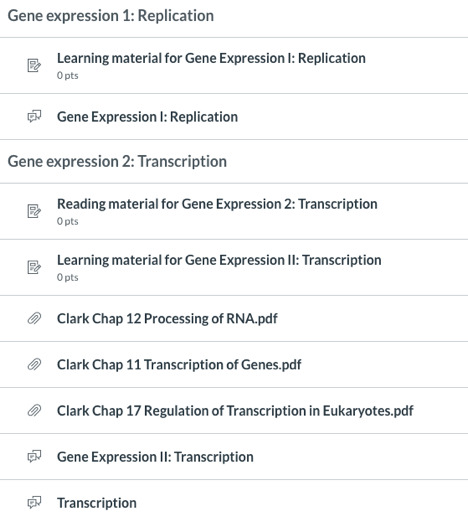
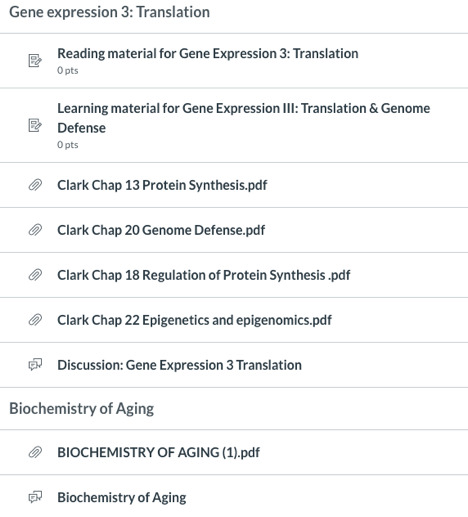
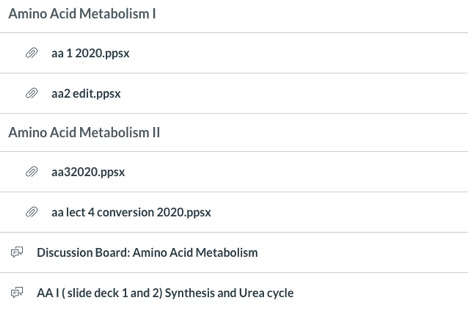
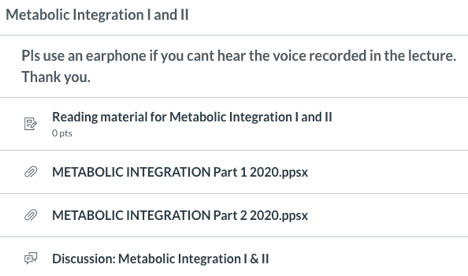
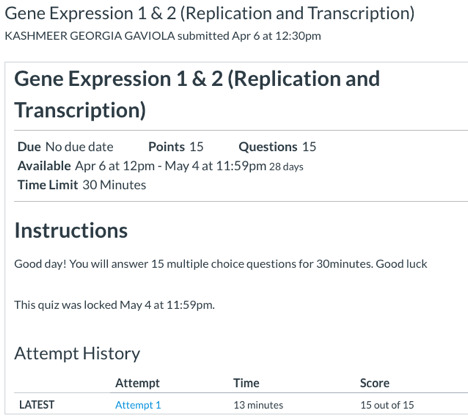
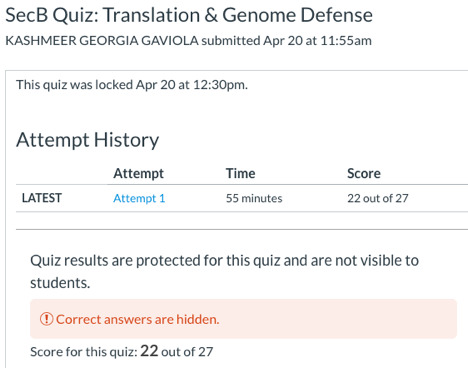
Every student has his or her different study habits. Studying alone may be beneficial to others, while listening to professors discuss topics may be the best for some. For someone who struggles with medical school, I have tried to combine different types of study habits that will work for me and I believe that following the lecture with audio or recordings suit me best. Supplementing the lectures with books and journals were also beneficial. I believe that the results of some of formative and graded quizzes can justify that these techniques have been working so far. Although there were some quizzes that I did not do so well, it motivated me to do better next time. I just hope that I continue with this path and mindset in order to aim for fruitful outcomes in the upcoming exams and finals.
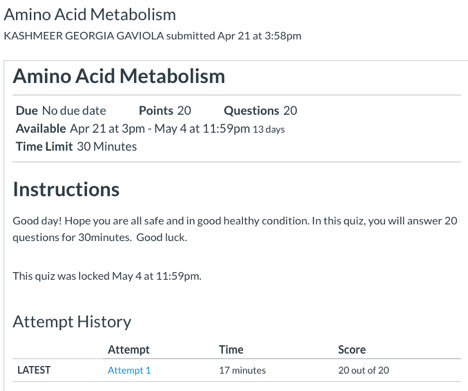
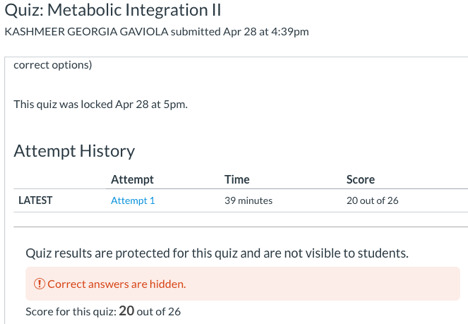
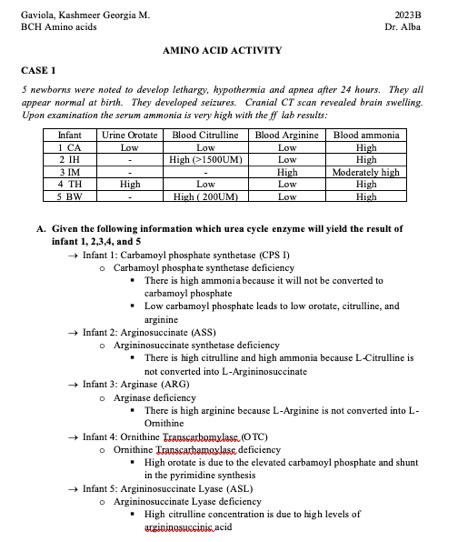
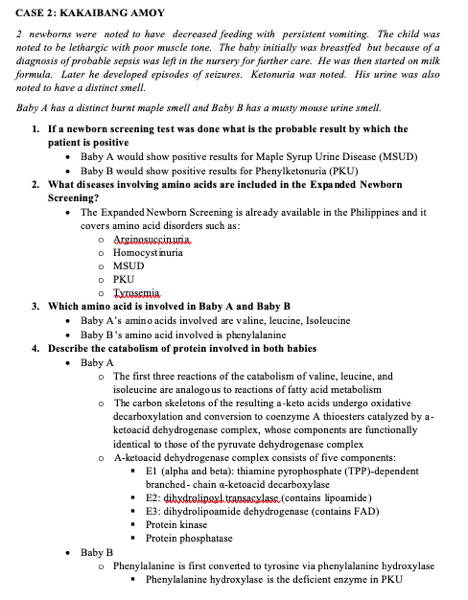
After the lecture in Amino acid metabolism, our professor gave us cases to think about and decipher. This activity guided me on how to think critically and give probable diagnoses and differentials to unique cases. This activity also helped me understand different amino acid deficiencies and their biochemical basis. I think I did well in researching because I got a perfect score for this activity.
In relation to Cancer Cachexia, the online lectures and biochemistry books were beneficial in my understanding of this complicated syndrome. These materials gave me an overview on different metabolic pathways that may be affected in individuals with different conditions. Gathering information on the case I am discussing made me apply all that I have learned in biochemistry throughout the year. My experience on research during undergraduate studies also aided in my approach for this portfolio. Reading different journals written by talented and intelligent doctors made me hopeful that I can also be like them in the future. Putting so much effort in understanding and discovering beneficial information for the survival of future patients is something that a great doctor should be proud of. These contributions in the medical field can help an individual understand why such things happen in the body.
0 notes
Text
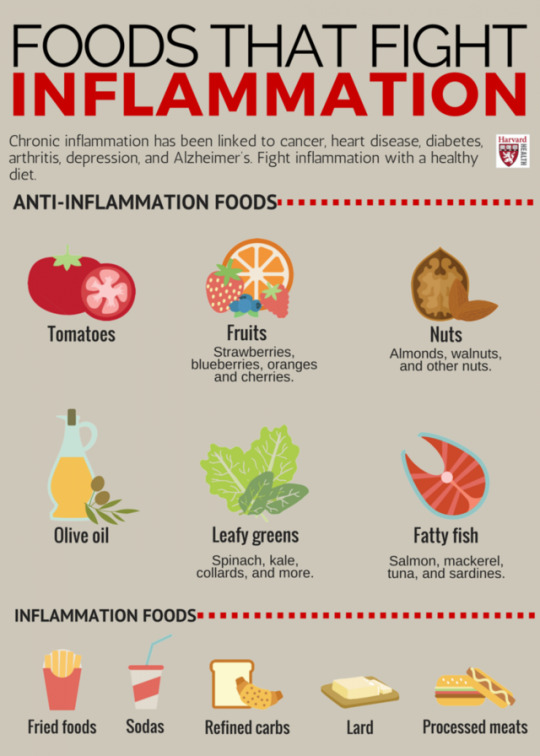
CANCER CACHEXIA: TREATMENT AND MANAGEMENT

There is no specific treatment or way to reverse cachexia. However, other treatment may improve symptoms and quality of life. Current therapy for cachexia includes appetite stimulants, drugs to improve nausea, appetite, and mood, medications that decrease inflammation, diet changes, nutritional supplements, and adapted exercise (National Cancer Institute, 2019). Some of these include:
Protein intake
Cachectic patients often exhibit reduced appetite and early satiety, hindering their ability to ingest amino acid and protein-rich foods to stimulate muscle protein synthesis. It is advised for them to intake supplemental amino acids for preventing or reversing muscle loss
Anti-inflammatory treatments
Since inflammatory signaling pathways are also responsible for cachexia, anti-inflammatory responses such as eating eicosapentaenoic acid (EPA), a naturally occurring fatty acid in fish oil may improve survival and preservation of their adipose tissue.
Appetite stimulation
Melanocortin inhibition reduces both the anorexia and hypermetabolism induced by tumors, while preserving lean body mass
Ghrelin stimulates orexigenic signaling by the melanocortin system
Insulin and testosterone therapy
Insulin is anabolic to skeletal muscle and inhibits lipolysis. It stimulates muscle protein synthesis and does not affect muscle protein breakdown
Testosterone also has anti-inflammatory properties and well-known anabolic effects such as increasing muscle mass by reducing the loss of skeletal muscle amino acids
References:
Photo retrieved from: https://images.app.goo.gl/ov3KQLK8PMDw89Jv7
Blackwell, Thomas Allen, "RNA Sequencing in the Development of Cancer-Cachexia" (2017). Theses and Dissertations. 2434. http://scholarworks.uark.edu/etd/2434
Durham, W. J., Dillon, E. L., & Sheffield-Moore, M. (2009). Inflammatory burden and amino acid metabolism in cancer cachexia. Current opinion in clinical nutrition and metabolic care, 12(1), 72–77. https://doi.org/10.1097/MCO.0b013e32831cef61
Fearon, K. C., Glass, D. J., & Guttridge, D. C. (2012). Cancer Cachexia: Mediators, Signaling, and Metabolic Pathways. Cell Metabolism, 16(2), 153–166. doi: 10.1016/j.cmet.2012.06.011
0 notes
Text
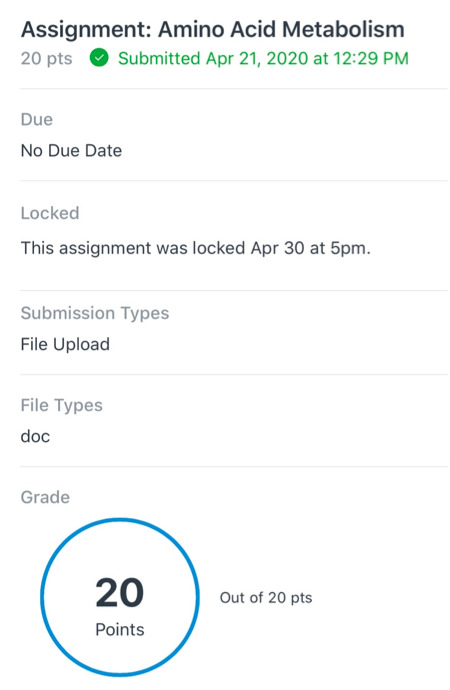
Metabolic integration
We are down to our last topic, which is integrating everything that we have learned in the past months. This is a summary of all the pathways involved in an individual with Cancer Cachexia:
Cachexia affects the majority of patients with advanced cancer and is associated with reduced muscle strength, fatigue, appetite loss (anorexia), tissue wasting, low fat-free mass index, high levels of inflammation identified by blood tests, anemia, and low levels of the protein albumin (National Cancer Institute, 2019). Cancer patient with Cachexia are also less able to tolerate chemotherapy and other therapies they need to survive. Thus, they have a lower quality of life and worse outlook.
In cachexia, anaerobic glycolysis proceeds at a high rate, which forms large amounts of pyruvate and is then reduced to lactate and is exported. The lactate is then used for gluconeogenesis in the liver, an energy-requiring process, which is responsible for the hypermetabolism seen in cachexic patients. Also, in these patients, there is an increased rate of protein catabolism. The secretion of cytokines in response to cancer increase tissue protein catabolism by the ATP-dependent ubiquitin-proteasome pathway, thus, increasing energy expenditure. There is also increased stimulation of mitochondrial uncoupling proteins by cytokines, leading to thermogenesis and increased oxidation of metabolic fuels. HSL is activated by tumors, resulting in lipolysis and oxidation of fatty acids from adipose tissue (Rodwell, 2015). Moreover, cancer cells require a sufficient supply of nucleotides and other macromolecules to grow and proliferate. To meet the metabolic requirements for cell growth, cancer cells must stimulate de novo nucleotide synthesis to obtain adequate nucleotide pools to support nucleic acid and protein synthesis along with energy preservation, signaling activity, glycosylation mechanisms, and cytoskeletal function (Villa, 2019).
In relation to nutrition and exercise, muscle contraction through exercise activates and improves nutrient-induced stimulation of protein synthesis in a healthy skeletal muscle. However, disrupted mTORC1 signaling results to impaired anabolic response to contraction. Thus, cancer cachexia disrupts the metabolic and anabolic signaling response to stimulated muscle contractions and anabolic resistance to exercise is present. Given that cachexia cannot be fully reversed by conventional nutritional support. Consumption of essential amino acids such as leucine can stimulate protein synthesis in individuals. The protein synthesis induction by intaking essential amino acids may activate of mTORC1 signaling. Thus, high protein and leucine could overcome anabolic resistance in cancer cachectic individuals (Hardee, Montalvo, & Carson, 2017).
The major effect of cancer cachexia in the body is weight loss largely from muscles and adipose tissue. However, even though the main tissue affected by cachexia is the skeletal muscle, cachexia cannot be reduced to a muscle-wasting syndrome. Indeed, several other organs such as liver, heart, fat tissue and brain are affected, making cachexia a true multi-organ syndrome (Devlin, 2011). The effect of cancer cachexia in the different organs are the following:
Brain: altered pattern of hypothalamic mediators, loss of appetite, hyposmia, hypogeusia, anorexia
Brown adipose tissue: thermogenesis
Heart: atrophy, decreased innervation, increased energy consumption, cardiac dysfunction
Gut: gut-barrier disfunction, altered ghrelin production, release of inflammatory mediators, malabsorption
Liver: release of acute-phase proteins, reduced albumin synthesis, acute-phase response
White adipose tissue: increased lipolysis, fatty acid oxidation, wasting
Skeletal muscle: wasting
Endocrine: insulin resistance, higher cortisol levels, higher BMR
References:
Devlin, T. 2011. Textbook of Biochemistry with Clinical Correlations. John Wiley & Sons, Inc.
Hardee, J. P., Montalvo, R. N., & Carson, J. A. (2017). Linking Cancer Cachexia-Induced Anabolic Resistance to Skeletal Muscle Oxidative Metabolism. Oxidative Medicine and Cellular Longevity, 2017, 1–14. doi: 10.1155/2017/8018197
Rodwell, V., et.al. 2015. Harper’s Illustrated Biochemistry 30th Edition. Copyright © 2015 by The McGraw-Hill Education.
Tackling the Conundrum of Cachexia in Cancer. 2019. National Cancer Institute at the National Institutes of Health. Retrieved from https://www.cancer.gov/about-cancer/treatment/research/cachexia
Villa, E., Ali, E., Sahu, U. & Ben-Sahra, I. 2019. Cancer Cells Tune the Signaling Pathways to Empower de Novo Synthesis of Nucleotides. National Center for Biotechnology Information, U.S. National Library of Medicine. doi: 10.3390/cancers11050688
0 notes
Text
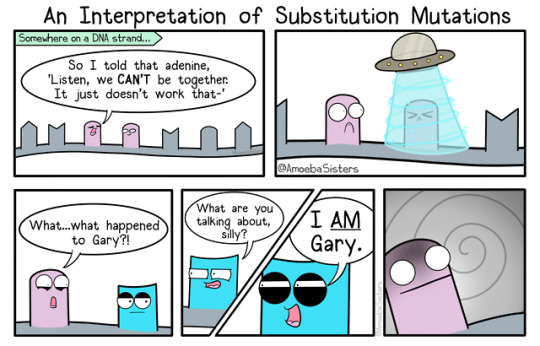
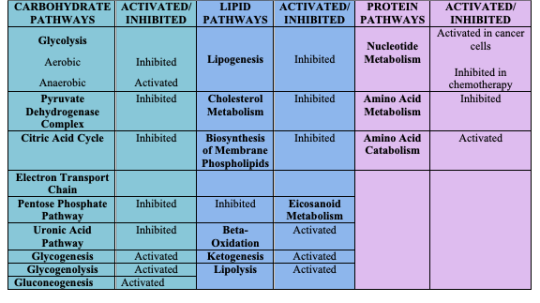
GENE EXPRESSION
DNA is the genetic material of all organisms. This DNA material is divided up into functional unit called genes, and each gene provides instructions for the cell’s function. The central dogma describes transcription and translation, wherein the information in genes flows into proteins. In transcription, and RNA copy of the DNA segment is synthesized, whereas in translation, RNA is translated into protein.
Cancer results from a gene that is not normally expressed in a cell but may be expressed at high levels due to mutations or alterations in gene regulation. Alterations in histone acetylation, increased translational control, and protein modification are observed in cancer cells. Cancer can be described as a disease of altered gene expression since there are many proteins that are activated which affect the overall activity of the cell. This disease can also be detected by changes in epigenetic regulation, transcription, RNA stability, protein translation, and post-translational control. However, these changes do not occur all at once (Lumen, 2020).
Cancer Cachexia develops a wide range of dysfunctions from insulin and IGF-1 resistance to induction of mitochondrial uncoupling proteins and fat tissue browning which results to uncontrollable increased energy expenditure and heat generation. Tumor cells also actively promote tissue wasting by secreting specific factors such as microRNAs (Porporato, 2016). Moreover, AMPK activity is disrupted during cancer cachexia progression. Thus, it can contribute to altering skeletal muscle metabolism and gene expression. There is chronically elevated muscle AMPK activity during cachexia, which coincides with the suppression of mTORC1 signaling and disrupted mitochondrial quality control mechanisms. While AMPK activation by systemic IL-6 also corresponds with mTORC1 suppression, AMPK inhibition rescues IL-6-induced suppression of mTORC1 signaling in C2C12 myotubes (Hardee, Montalvo, & Carson, 2017).
miRNAs also play a major role in the regulation of the transcription of several genes involved with skeletal muscles. miRNA-486 decreases FoxO1 protein expression and promotes FoxO1 phosphorylation to suppress E3 ubiquitin ligases (Camargo, 2015). Moreover, skeletal muscle protein synthesis in cachexia reduces when dsRNA-dependent protein kinase (PKR) is activated by the tumor-secreted proteolysis-inducing factor (PIF), which is a potential inhibitor. This happens because of phosphorylation of eukaryotic initiation factor (eIF) 2, which interferes with the activity of eIF2B to promote translation initiation (Durham, Dillon, &. Sheffield-Moore, 2009). The inhibition of protein synthesis in muscle also reduces both RNA content or its protein synthesizing capacity and RNA activity such as the amount of protein synthesized by RNA. Levels of myosin follows the decrease in total protein, while actin levels remained constant (Bhogal, Lorite, & Tisdale, 2006).
References:
Photo retrieved from: https://images.app.goo.gl/hcZ1UXPxYPAnC17a7
Bhogal, Lorite, M., & Tisdale, M. (2006). Changes in Nucleic Acid and Protein Levels in Atrophying Skeletal Muscle in Cancer Cachexia. ANTICANCER RESEARCH, 26(6), 4149–4154. Retrieved from http://ar.iiarjournals.org/content/26/6B/4149.long
Camargo, R. (2015). Cancer Cachexia and MicroRNAs. Inflammation in Cachexia. doi: https://doi.org/10.1155/2015/367561
Cancer and Gene Regulation. 2020. Lumen Candela. Retrieved from https://courses.lumenlearning.com/boundless-biology/chapter/cancer-and-gene-regulation/
Durham, W. J., Dillon, E. L., & Sheffield-Moore, M. (2009). Inflammatory burden and amino acid metabolism in cancer cachexia. Current opinion in clinical nutrition and metabolic care, 12(1), 72–77. https://doi.org/10.1097/MCO.0b013e32831cef61
Hardee, J. P., Montalvo, R. N., & Carson, J. A. (2017). Linking Cancer Cachexia-Induced Anabolic Resistance to Skeletal Muscle Oxidative Metabolism. Oxidative Medicine and Cellular Longevity, 2017, 1–14. doi: 10.1155/2017/8018197
Porporato, P. E. (2016). Understanding cachexia as a cancer metabolism syndrome. Oncogenesis, 5(2). doi: 10.1038/oncsis.2016.3
0 notes
Text
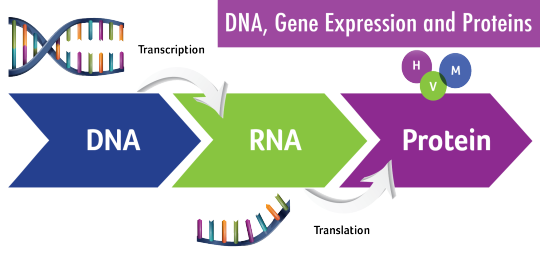
NUCLEOTIDE METABOLISM IN CANCER CACHEXIA
Adenine nucleotides such as ATP, ADP, and AMP are essential biological compounds that facilitate necessary cellular processes. They provide chemical energy, mediate intracellular signaling, and regulate protein metabolism. A decrease in these three adenine nucleotides are observed in skeletal muscle atrophy seen in Cancer Cachexia (Miller, Hafen, & Brault, 2019).
Nucleotides in muscle atrophy are mediated by factors such as inflammatory cytokines, cytokines, glucocorticoids, endotoxins, decreased anabolic hormones, anabolic resistance, anorexia, and reduced physical activity. The reduced adenosine nucleotides are expressed through increased activities of these degrading enzymes and the accumulation of degradation products such as IMP, hypoxanthine, xanthine, and uric acid. Since there is lower adenosine nucleotide content, nucleotide degradation is increased. The oxidation of hypoxanthine to uric acid also plays a major role in the development of cancer cachexia (Miller, Hafen, & Brault, 2019).
Cancer cachexia progression disrupts several processes regulating mitochondrial quality control related to function, content, mitochondrial DNA expression, dynamics, and autophagy. Mitochondrial morphology and function related to ATP production and coupling efficiency are also disrupted. Moreover, ATP synthesis rates and electron transport chain (ETC) complex activities are reduced in the muscles (Hardee, Montalvo, & Carson, 2017).
References:
Photo retrieved from: https://images.app.goo.gl/n66CdoZabj75RSr6A
Hardee, J. P., Montalvo, R. N., & Carson, J. A. (2017). Linking Cancer Cachexia-Induced Anabolic Resistance to Skeletal Muscle Oxidative Metabolism. Oxidative Medicine and Cellular Longevity, 2017, 1–14. doi: 10.1155/2017/8018197
Miller, S. G., Hafen, P. S., & Brault, J. J. (2019). Increased Adenine Nucleotide Degradation in Skeletal Muscle Atrophy. International Journal of Molecular Sciences, 21(1), 88. doi: 10.3390/ijms21010088
0 notes
Text
NUCLEOTIDE METABOLISM: OVERVIEW
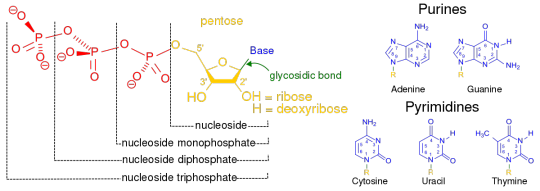
Nucleotide metabolism is a process necessary for cell growth and replication (Carcamo et al, 2014). This is directly linked to cellular homeostasis because it is very important for physiological processes such as carbohydrate metabolism, oxidative phosphorylation, essential nucleotide biosynthesis, and signal transduction (Sutton, 2017). The metabolic requirements for the nucleotides and their bases can be met by dietary intake and de novo synthesis. Salvaging nucleotides from different sources within the body can prevent the deficiency of these nucleotides and alleviate any significant nutritional requirement for these, which is why the purine and pyrimidine bases are not required in the diet. Salvage pathways, however, are the major source for the synthesis of DNA, RNA, and enzyme co-factors. The major site of de novo nucleotide synthesis in the body is the liver, to replenish and maintain the intracellular pools (King (2019).
Nucleotide metabolism has uncontrolled activity in cancer cells which is why it is activated in patients with cancer. This is needed in order to meet the metabolic requirements for the cell growth of cancer cells (Villa, 2019). However, when undergoing chemotherapy, the chemotherapeutic agents are used to inhibit nucleotide (King, 2019).
References:
Photo retrieved from: https://images.app.goo.gl/UWc85PSjRzAyAJmL6
Carcamo, W., Calise, S., Mühlen, C., Satoh, M. & Chan, E. 2014. Molecular Cell Biology and Immunobiology of Mammalian Rod/ Ring Structures. International Review of Cell and Molecular Biology. Copyright © 2020 Elsevier B.V. ScienceDirect ®
King, M. 2019. Biosynthesis and Catabolism of Nucleic Acids. © 1996–2019 themedicalbiochemistrypage.org, LLC. Retrieved from https://themedicalbiochemistrypage.org/nucleotide-metabolism.php
Sutton, L. 2017. Disorders of purine and pyrimidine metabolism. Biomarkers in Inborn Errors of Metabolism. Copyright © 2020 Elsevier B.V. ScienceDirect ®
Villa, E., Ali, E., Sahu, U. & Ben-Sahra, I. 2019. Cancer Cells Tune the Signaling Pathways to Empower de Novo Synthesis of Nucleotides. National Center for Biotechnology Information, U.S. National Library of Medicine. doi: 10.3390/cancers11050688
0 notes
Text
PROTEIN METABOLISM IN CANCER CACHEXIA
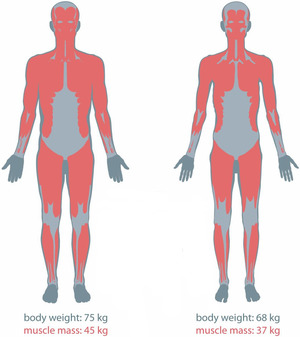
There are metabolic abnormalities seen in individuals with cancer cachexia that arise from malnutrition and malignancy. Protein turnover is evident and high in cancer cachectic patients. Muscle protein synthesis is suppressed during their initial stages of weight loss and is further reduced as their condition progresses. Moreover, protein degradation activation and disrupted oxidative metabolism in skeletal muscles also continue to develop. Thus, protein and amino acid metabolism is clearly affected. These results to the progressive loss of muscle mass, which is the most prominent feature of cancer cachexia (Dodesini et al, 2009). Muscle depletion also reduces chemotherapy effectiveness, increases susceptibility to treatment toxicity, decreases physical function, and impairs psychosocial ability.
The loss of skeletal muscle in cancer patients are due to anorexia and early satiety, reduced muscle protein synthesis, and increased muscle protein breakdown. Inflammation has also negatively contributed to these mechanisms. Inflammatory cytokines such as IL-6 and TNFα contribute to the effects of inflammation on muscle protein metabolism through several pathways.
Impaired muscle protein synthesis
Cancer cachexia disrupts protein translation at several regulatory steps such as initiation, elongation, and termination. The phosphorylation of eIF2α, which impairs translation initiation and overall protein synthesis, is elevated (Hardee, Montalvo, & Carson, 2017). Anabolic and catabolic hormones and energy balance influence signal transduction pathways that regulate protein synthesis via mTOR-related signal transduction pathways. This pathway is the most predominant signaling regulator of translation initiation and are activated by insulin and IGF-1 (Blackwell, 2017). It is also major mediator of anabolic responses in skeletal muscle. Specifically, mTOR activation by insulin or amino acids activates the downstream targets eukaryotic initiation factor binding protein 4E and ribosomal S6 kinase 1, which promote translation initiation, and eukaryotic elongation factor, which stimulates elongation. This pathway is inhibited in cancer cachexia, which corresponds to disrupted S6K1 and 4EBP-1 regulation. A decrease in mTOR activation is also due to AMPK and systemic inflammation. AMPK inhibits mTOR by preventing the interaction with both p70S6K and 4E-BP1 (Durham, Dillon, & Sheffield-Moore, 2009).
Glutamine is the most abundant amino acid in the body. However, glutamine depletion is observed in Cancer Cachexia since glutamine is a regulator of muscle protein synthesis and this is inhibited in the condition. Furthermore, glutamine is a principal fuel for most rapidly proliferating cancers. Tumor cells are major glutamine consumers and they compete with the host for circulating glutamine. Thus, there are changes in glutamine metabolism resulting in glutamine depletion developing with progressive tumor growth (Bode et al, 1996).
Stimulated muscle protein breakdown
There are three main degradation pathways in the skeletal muscle to account for protein degradation. These are ubiquitin-mediated proteasome degradation (UPR), autophagy, and calcium-activated protease calpains.
The over activation of proteolysis is the primary pathway of protein degradation through muscle wasting in Cancer Cachexia (Blackwell, 2017). Muscle protein degradation in cachexia is mainly mediated by the ubiquitin proteasome system which is induced through the activation of E3 ligases, MAFbx, and MurF-1. The FOXO signaling pathway also contributes through the induction of the transcription of these ubiquitin ligases. Thus, the inhibition of FOXO transcription activity prevents muscle fiber atrophy during cachexia (Camargo, 2015). Many of these effects occur through activation of NF-κB by upstream factors such as TNF-α and PIF (Durham, Dillon, & Sheffield-Moore, 2009). During Cachexia, skeletal muscle specifically upregulates muscle specific UPR system, in particular by promoting ubiquitin-ligase MurF1 and Atrogin-1 expression. UPR upregulation is shown by Atrogin-1 messenger RNA and increased protein ubiquitylation. The expression of this ubiquitin ligase is mainly regulated by the transcription factor FoxO3a (FOXO) (Porporato, 2016).
Aside from UPR, the role of autophagy in mediating skeletal muscle wasting is also evident (Porporato, 2016). Autophagy is increased and upregulated in Cancer Cachexia. It is a process of lysosomal degradation where aggregated protein and damaged organelles are engulfed by an autophagosome prior to ultimate joining with lysosome and degradation. These is also contributed by an increase in Reactive Oxygen Species (ROS) production in skeletal muscle (Blackwell, 2017).
Inflammation
Inflammation initiates central anorexic pathways that limit dietary consumption of nutrients. As amino acids are required for muscle protein synthesis, the reduced availability of amino acids in individuals with Cancer Cachexia mainly contributes to their inflammation-induced loss of skeletal muscle mass. Moreover, the reduced supply of amino acids and anorexic response also reduces the exposure to insulin which stimulates muscle protein synthesis. (Durham, Dillon, & Sheffield-Moore, 2009). In relation to insulin resistance, insulin action is not fully able to control catabolic processes in the muscle in Cachectic individuals (Dodesini et al, 2009).
Although liver contributes to cachexia by increasing energy expenditure through gluconeogenesis and reducing VLDL circulation, it worsens inflammation by secreting acute phase proteins and reducing albumin secretion, a process mostly driven by IL-6 and TNFα. This contributes to muscular protein breakdown and adipocytes lipolysis in affected individuals (Porporato, 2016).
Inflammatory-mediated signaling muscle protein synthesis by several mechanisms. TNFα is the most characterized cytokine in cachexia, which promotes anorexia and skeletal muscle wasting mainly through the NF-kB pathway. It activates the transcription factor NF-κB, which inhibits the synthesis of the muscle-specific transcription factor MyoD. TNF-α also influences the anabolic mTOR signaling pathway. It synergizes with interferon gamma and IL-1 in promoting muscle wasting (Porporato, 2016). Inflammatory proteins such as IL-6 also reduce the activation of mTOR directly and indirectly through phosphorylation of AMPK. The infusion of IL-6 increases whole body protein turnover and reduces circulating amino acid concentrations (Durham, Dillon, & Sheffield-Moore, 2009).
References:
Photo retrieved from: https://images.app.goo.gl/kwtG3Tzjmw2Mw6RAA
Blackwell, Thomas Allen, "RNA Sequencing in the Development of Cancer-Cachexia" (2017). Theses and Dissertations. 2434. http://scholarworks.uark.edu/etd/2434
Bode, B. P., Fischer, C., Abcouwer, S., Wasa, M., & Souba, W. W. (1996). Glutamine and Cancer Cachexia. Protein and Amino Acid Metabolism in Cancer Cachexia Medical Intelligence Unit, 139–170. doi: 10.1007/978-3-662-22346-8_11
Dodesini, A. R., Benedini, S., Terruzzi, I., Sereni, L. P., & Luzi, L. (2009). Protein, glucose and lipid metabolism in the cancer cachexia: A preliminary report. Acta Oncologica, 46(1), 118–120. doi: 10.1080/02841860600791491
Durham, W. J., Dillon, E. L., & Sheffield-Moore, M. (2009). Inflammatory burden and amino acid metabolism in cancer cachexia. Current opinion in clinical nutrition and metabolic care, 12(1), 72–77. https://doi.org/10.1097/MCO.0b013e32831cef61
Hardee, J. P., Montalvo, R. N., & Carson, J. A. (2017). Linking Cancer Cachexia-Induced Anabolic Resistance to Skeletal Muscle Oxidative Metabolism. Oxidative Medicine and Cellular Longevity, 2017, 1–14. doi: 10.1155/2017/8018197
Porporato, P. E. (2016). Understanding cachexia as a cancer metabolism syndrome. Oncogenesis, 5(2). doi: 10.1038/oncsis.2016.3
0 notes
Text
PROTEIN METABOLISM: OVERVIEW
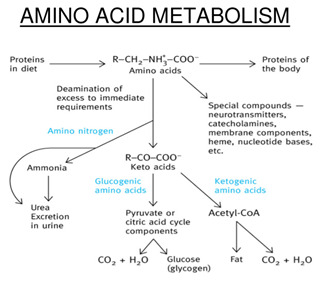
Amino acids are used as building blocks for protein synthesis, precursors of nucleotides and heme, source of energy, neurotransmitters, and precursors of neurotransmitters and hormones (Palmer, 2019).
Muscle protein and adipose lipids are consumed to support gluconeogenesis, and with this, protein serves as a substantial energy source, especially during fasting and starvation. The liver is the major site of amino acid degradation. However, the amino acids from protein digestion are absorbed in the small intestine and this organ preferably uses glutamine and asparagine as energy suppliers. During fasting, muscle releases glutamine in the circulation and the intestine oxidizes it. The degradation of branched amino acids mainly starts in the skeletal muscle. More than half of the muscle amino acids released to the circulation are alanine and glutamine and both of them act as carriers of amines from other tissues. In the kidney, glutamine is captured from the muscles. The reactions that occur are catalyzed by glutaminase and glutamate dehydrogenase and produce ammonia, which is converted to ammonium ion and excreted in urine, neutralizing anions (Blanco, 2017).
Amino acids are critical for cell survival and all are essential to health. Each amino acid pathway begins with a central metabolite. Glutamine, the most abundant amino acid in the body, is produced from glutamate by glutamine synthetase. The amination involves the formation of intermediate y-glutamyl phosphate with ATP. NH4 then binds and NH3 attacks the glutamylphosphate to form a tetrahedral structure, release of Pi and a proton releases glutamine (Rodwell, 2015).
Amino acid metabolism is inhibited in cancer cachexia while its catabolism is activated since the body is in a hypermetabolic state. Due to proteolysis, muscle wasting is also observed in patients with cancer cachexia. There is great loss of body protein and increase in energy expenditure. Protein turnover occurs in all forms of life. There is 1-2% of total daily protein turnover, and majority occurs in muscle. There are higher rates of protein degradation in tissues that are undergoing structural rearrangement (e.g. skeletal muscle during starvation). In individuals with Cancer Cachexia, protein turnover is higher, which causes muscle mass to deplete.
References:
Photo retrieved from: https://images.app.goo.gl/EggzVkTdd6YyTigw8
Blanco, A. & Blanco, G. 2017. Medical Biochemistry. Copyright © 2017 Elsevier Inc. All rights reserved. https://doi.org/10.1016/B978-0-12-803550-4.00016-1
Palmer, M. 2019. Amino Acid Metabolism. © University of Waterloo. Retrieved from http://watcut.uwaterloo.ca/webnotes/Metabolism/AminoAcids.html
Rodwell, V., et.al. 2015. Harper’s Illustrated Biochemistry 30th Edition. Copyright © 2015 by The McGraw-Hill Education.
0 notes
Text
Going Online

Hey, guys! It’s been a while. As you all know, we are currently experiencing a pandemic that has greatly affected us all. Covid-19 is a contagious disease with no known cure. It has really taken a toll on the capacity of not only our healthcare system, but also our well-being and quality of life. Countries have implemented precautionary measures to prevent the spread of transmission such as promoting proper hygiene and social distancing. The Philippines has declared a total lock-down since March and has affected how schools adapt to the situation. As we adjust to the ‘new normal’, our school has shifted to a blending learning system through online platforms. Despite everything, we must continue with our learning and discovering our fullest potential during these trying times.
For the past months, I have been talking about Cancer cachexia and how it affects glucose and lipid metabolism in affected individuals. It is now time we move on to protein or amino acid metabolism, nucleotide metabolism, and gene expression. Hopefully we could also come up with the metabolic integration of all of these topics. Let’s get to it!
0 notes
Text
My Insights
This section was quite overwhelming for me because you need a lot to process as you learn more about cancer. Cancer really is a life degrading disease and it pains me to realize how many people actually have to go through this and suffer. Depletion of fats and carbohydrates in the body seems to be a painful thing to encounter as it sucks all of your nutrients and kills you slowly. Just thinking about how all of this happens in one’s body can be saddening and interesting at the same time because it drives you to find ways to cure and prevent the decline of the quality of life of a person so that future generations do not get to experience this heavy disease anymore.
Once again, I have emphasized the importance of nutrition. Learning about how each macronutrient affects certain process made me realize that a balanced diet is very important because one deficiency can also lead to another. There are also solutions that we can accomplish in order to have a healthy and stable body. Being able to explain the biochemistry behind such processes made me appreciate the backbone more and motivated me to be more mindful of how I take care of my health.
As a medical student, my nutritional choices is not the best but I hope I get to improve my lifestyle as time goes by.
That is it for now! In the next sections, I will then incorporate another macronutrient, which are proteins. I will also discuss its role in metabolism and its relationship to the other macronutrients.
0 notes