Text
Churg strauss syndrome

Churg Strauss Syndrome, also known as eosinophilic granulomatosis with polyangiitis (EGPA), is a rare autoimmune disease that affects multiple organs, particularly the lungs, skin, and blood vessels. In this blog post, we will delve into the various aspects of Churg Strauss Syndrome, including its causes, symptoms, diagnosis, treatments, and potential complications. We will also explore the lifestyle changes and self-care measures that can help patients manage their condition. Furthermore, we will discuss the support groups and resources available for individuals with Churg Strauss Syndrome, as well as the latest research and advancements in understanding this syndrome. Finally, we will compare it with other similar autoimmune diseases, discuss the prognosis and long-term outlook for patients, and examine prevention and risk reduction strategies for Churg Strauss Syndrome. Stay tuned for a comprehensive overview of this complex syndrome and how it affects those diagnosed with it.
What Is Churg Strauss Syndrome?
Churg Strauss Syndrome, also known as eosinophilic granulomatosis with polyangiitis (EGPA), is a rare autoimmune disorder that causes inflammation of the blood vessels. It primarily affects the small and medium-sized blood vessels, especially those in the lungs, skin, nerves, and gastrointestinal tract. The syndrome is characterized by the accumulation of eosinophils, a type of white blood cell, in various organs and tissues. These eosinophils release harmful substances that cause damage to the blood vessels, leading to a wide range of symptoms and complications.
One of the key features of Churg Strauss Syndrome is the presence of asthma and allergic rhinitis in most patients. Many individuals with the syndrome have a long history of asthma before the onset of other symptoms. Asthma symptoms can worsen along with the progression of the syndrome. In some cases, previously well-controlled asthma may become more difficult to manage. Churg Strauss Syndrome can also affect other organs, such as the heart, kidneys, and nervous system. This can result in symptoms such as chest pain, heart palpitations, kidney problems, and nerve damage.
In terms of its cause, the exact triggers for Churg Strauss Syndrome remain unclear. However, research suggests that a combination of genetic and environmental factors may play a role in its development. Some studies have identified specific genetic mutations that are more common in individuals with the syndrome. Environmental factors, such as exposure to certain chemicals or allergens, may trigger an abnormal immune response in susceptible individuals. Further research is needed to fully understand the underlying mechanisms.
Eosinophilic granulomatosis with polyangiitis (EGPA) is a rare autoimmune disorder
The syndrome primarily affects the small and medium-sized blood vessels
Churg Strauss Syndrome is characterized by the accumulation of eosinophils
Common Symptoms:
• Asthma
• Allergic rhinitis
• Skin rashes
• Nerve damage
• Chest pain
Causes Of Churg Strauss Syndrome
The exact cause of Churg Strauss Syndrome is still unknown. However, researchers believe that it is an autoimmune disorder, meaning that the body's immune system mistakenly attacks healthy tissues and organs. It is believed that certain genetic factors play a role in the development of the syndrome, as it tends to run in families. Environmental factors, such as exposure to allergens or certain medications, may also contribute to the development of the condition.
Additionally, it has been observed that individuals with certain conditions, such as asthma or allergies, have a higher risk of developing Churg Strauss Syndrome. This suggests that there may be a link between these conditions and the development of the syndrome. However, more research is needed to fully understand the relationship between these factors and the development of Churg Strauss Syndrome.
Furthermore, it is important to note that Churg Strauss Syndrome is a rare condition. It is estimated to affect only a small number of individuals worldwide. While the exact causes are still unclear, researchers are continuously studying the syndrome in order to gain a better understanding of its underlying mechanisms and factors that contribute to its development.
Symptoms And Manifestations Of The Syndrome
Churg Strauss Syndrome, also known as eosinophilic granulomatosis with polyangiitis (EGPA), is a rare autoimmune disease that causes inflammation in blood vessels. This condition primarily affects small and medium-sized arteries, leading to a range of symptoms and manifestations.
One of the hallmark symptoms of Churg Strauss Syndrome is asthma. Many patients with this syndrome have a history of asthma or allergic rhinitis. The asthma may become more severe and difficult to manage as the syndrome progresses. Patients may also experience recurrent sinusitis, which can cause facial pain and congestion.
Another common manifestation of Churg Strauss Syndrome is eosinophilia. Eosinophils are a type of white blood cell that play a role in allergic reactions. In EGPA, the body produces an excess of eosinophils, leading to high levels of these cells in the blood. Eosinophilia can cause damage to organs and tissues throughout the body.
In addition to asthma and eosinophilia, patients with Churg Strauss Syndrome may develop vasculitis. Vasculitis is inflammation of blood vessels, which can restrict blood flow and damage organs. Symptoms of vasculitis can vary depending on the organs affected, but may include skin rashes, nerve damage, gastrointestinal problems, and kidney dysfunction.
Other manifestations of Churg Strauss Syndrome can include cardiac involvement, such as myocarditis or heart rhythm abnormalities, and pulmonary complications, such as pulmonary infiltrates and nodules. Patients may also experience musculoskeletal symptoms like muscle pain and joint inflammation.
It is important to note that the symptoms and manifestations of Churg Strauss Syndrome can vary greatly from person to person. Some individuals may have mild symptoms and a relatively benign disease course, while others may experience more severe symptoms and complications. Early recognition and diagnosis of the syndrome is crucial to initiate appropriate treatment and management options.
Diagnosis And Medical Tests For Churg Strauss Syndrome
When it comes to diagnosing Churg Strauss Syndrome, a thorough medical evaluation is essential. As an autoimmune disease that affects the blood vessels, accurate diagnosis is crucial for determining the appropriate treatment plan. Doctors often rely on a combination of medical tests and clinical symptoms to diagnose this syndrome.
One of the key tests used for the diagnosis of Churg Strauss Syndrome is a blood test. This test helps in assessing the levels of eosinophils, which are a type of white blood cells. Elevated levels of eosinophils can indicate the presence of inflammation in the body, which is a characteristic feature of this syndrome. Additionally, the blood test also helps in measuring other markers of inflammation and evaluating the overall health of the patient.
In addition to the blood test, a biopsy may also be performed to confirm the diagnosis. A small sample of the affected tissue, such as a sample from the lungs or skin, is taken and examined under a microscope. This can help identify the presence of eosinophils and confirm the diagnosis of Churg Strauss Syndrome.
- Furthermore, imaging tests such as X-rays, CT scans, and MRIs may be used to visualize the affected organs and detect any abnormalities. These tests are particularly useful in assessing the extent of organ damage or the presence of complications associated with Churg Strauss Syndrome.
Medical Tests for Diagnosis of Churg Strauss Syndrome
Purpose
Blood test
To assess eosinophil levels and measure markers of inflammation
Biopsy
To confirm the diagnosis by examining tissue samples under a microscope
Imaging tests
To visualize affected organs and detect abnormalities
Overall, the diagnosis of Churg Strauss Syndrome requires a comprehensive approach involving various medical tests and clinical evaluations. Prompt and accurate diagnosis is crucial for starting appropriate treatment and managing the condition effectively.
Treatments And Management Options
Treatments And Management Options for Churg Strauss Syndrome
Churg Strauss Syndrome, also known as eosinophilic granulomatosis with polyangiitis (EGPA), is a rare autoimmune disease that affects multiple organs. It is characterized by the inflammation of blood vessels, causing damage to various tissues in the body. While there is no cure for Churg Strauss Syndrome, there are several treatment options available to manage the symptoms and improve the quality of life for patients.
Medication:
One of the primary goals in the treatment of Churg Strauss Syndrome is to suppress the immune system and reduce inflammation. This is typically achieved through the use of medications such as corticosteroids and immunosuppressants. Corticosteroids, such as prednisone, help to reduce inflammation and control symptoms. However, long-term use of corticosteroids can lead to side effects, so it is important to find the lowest effective dose. Immunosuppressants, such as azathioprine or methotrexate, may be prescribed in combination with corticosteroids to further suppress the immune response.
Biologic Therapy:
In some cases, biologic therapies may be recommended for individuals with Churg Strauss Syndrome. Biologic drugs, such as mepolizumab and rituximab, target specific molecules or cells involved in the immune response. Mepolizumab, an anti-interleukin-5 antibody, has shown effectiveness in reducing the frequency of asthma exacerbations and improving lung function in patients with EGPA. Rituximab, a monoclonal antibody, can selectively deplete B cells, which play a role in the immune response. These biologic therapies are usually used when other treatments have not provided sufficient relief.
Monitoring and Supportive Care:
Regular monitoring of Churg Strauss Syndrome is crucial to assess the response to treatment and detect any potential complications. This may involve blood tests, imaging studies, and lung function tests. Supportive care measures, such as maintaining a healthy lifestyle, managing symptoms, and preventing infections, are also essential for the overall management of the disease. It is important for individuals with Churg Strauss Syndrome to work closely with a healthcare team, including rheumatologists and pulmonologists, to ensure optimal management of the condition.
Conclusion:
While Churg Strauss Syndrome can be a challenging and complex disease to manage, there are treatment options available to help control symptoms and improve the quality of life for patients. Medication, including corticosteroids and immunosuppressants, is commonly used to reduce inflammation and suppress the immune response. Biologic therapies, such as mepolizumab and rituximab, may be considered when other treatments are ineffective. Regular monitoring and supportive care are essential components of managing this rare autoimmune disease.
Potential Complications And Risks
Churg Strauss syndrome, also known as eosinophilic granulomatosis with polyangiitis (EGPA), is a rare autoimmune disease that causes inflammation of blood vessels. While the exact cause of this syndrome is yet to be determined, it is believed to be a combination of genetic and environmental factors. It primarily affects the small and medium-sized blood vessels, leading to a wide range of symptoms and manifestations.
Churg Strauss syndrome can potentially lead to various complications and pose certain risks to individuals diagnosed with the condition. One of the most significant complications is the potential damage to vital organs as a result of vasculitis. The inflammation of blood vessels can restrict blood flow, leading to organ dysfunction and even organ failure. The organs most commonly affected include the lungs, heart, gastrointestinal tract, skin, and nervous system. It is crucial for individuals with Churg Strauss syndrome to be aware of these potential complications and seek immediate medical attention if they experience any symptoms related to organ dysfunction.
In addition to organ involvement, individuals with Churg Strauss syndrome may also experience respiratory complications. Asthma, which is often present in patients with this syndrome, can worsen and become difficult to manage. Severe asthma attacks may require intensive medical intervention and can be life-threatening if not promptly treated. Furthermore, the inflammation in the respiratory system can lead to other complications such as chronic sinusitis, recurrent bronchitis, and lung scarring, which can impair lung function over time.
- Table: Potential Complications and Risks of Churg Strauss Syndrome
Complications
Risks
Organ dysfunction/failure
Restricted blood flow due to vasculitis
Respiratory complications
Worsening asthma, chronic sinusitis, lung scarring
Cardiovascular complications
Inflammation of blood vessels in the heart, heart attack
Gastrointestinal complications
Inflammation of blood vessels in the gastrointestinal tract, digestive issues, bowel perforation
Neurological complications
Inflammation of blood vessels in the nervous system, nerve damage, stroke
Another potential complication associated with Churg Strauss syndrome involves the cardiovascular system. Inflammation of blood vessels in the heart can lead to the development of coronary artery disease and increase the risk of heart attack. It is important for individuals with this syndrome to manage their cardiovascular health through regular check-ups and appropriate interventions, such as medication and lifestyle modifications.
Gastrointestinal complications may also arise in people with Churg Strauss syndrome. Inflammation of blood vessels in the gastrointestinal tract can cause abdominal pain, digestive issues, and in severe cases, bowel perforation. Regular monitoring of gastrointestinal symptoms, along with appropriate medical management, is crucial in preventing and managing these complications.
Additionally, Churg Strauss syndrome can affect the nervous system, leading to neurological complications. Inflammation of blood vessels in the nervous system can result in nerve damage and increase the risk of stroke. Neurological symptoms may include numbness, tingling, weakness, difficulty in coordination, and changes in vision. Close monitoring and early intervention are essential to prevent further deterioration and minimize the impact on the individual's quality of life.
In conclusion, Churg Strauss syndrome carries potential complications and risks that individuals should be aware of. Organ dysfunction, respiratory complications, cardiovascular issues, gastrointestinal problems, and neurological manifestations are among the possible consequences of this rare autoimmune disease. By understanding these potential complications and seeking appropriate medical care, individuals with Churg Strauss syndrome can better manage their condition and mitigate the risks associated with it.
Lifestyle Changes And Self-Care For Patients
Living with Churg Strauss Syndrome can be challenging, but making certain lifestyle changes and taking self-care measures can greatly improve the quality of life for patients. These changes and practices can help patients manage symptoms, prevent flare-ups, and reduce the overall impact of the syndrome on their daily lives.
1. Follow a Healthy Diet:
Adopting a healthy and balanced diet is crucial for patients with Churg Strauss Syndrome. Consuming a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats can support the immune system and help reduce inflammation. It is important to limit processed foods, sugary snacks, and foods high in saturated fats, as they can exacerbate symptoms and contribute to overall health issues.
2. Regular Exercise:
Engaging in regular physical activity is highly beneficial for patients with Churg Strauss Syndrome. Exercise can help improve cardiovascular health, strengthen muscles, and enhance overall well-being. However, it is important to consult with a healthcare professional before starting any exercise regimen to ensure it is suitable for individual circumstances.
3. Stress Management:
Managing stress is crucial for patients with Churg Strauss Syndrome, as stress can trigger flare-ups and worsen symptoms. Engaging in stress-reducing activities such as meditation, deep breathing exercises, yoga, or spending time in nature can help alleviate stress and promote relaxation. It is also beneficial to establish a support network of family, friends, or support groups to share experiences and receive emotional support.
4. Adequate Rest and Sleep:
Getting enough rest and quality sleep is essential for patients with Churg Strauss Syndrome. Fatigue is a common symptom of the syndrome, and ensuring adequate rest can help manage its impact. Establishing a regular sleep schedule, creating a comfortable sleep environment, and practicing good sleep hygiene can contribute to better sleep quality.
5. Medication Management:
Strictly adhering to prescribed medications and treatment plans is crucial for managing Churg Strauss Syndrome. Patients should follow the recommended dosage and schedule for medications, and communicate any concerns or side effects to their healthcare provider. It is important not to alter or stop medication without medical advice.
6. Avoidance of Triggers:
Identifying and avoiding triggers that can worsen symptoms or trigger flare-ups is important for patients with Churg Strauss Syndrome. Common triggers include allergens, environmental pollutants, and certain medications. By recognizing and avoiding these triggers, patients can reduce the frequency and intensity of symptoms.
By implementing these lifestyle changes and practicing self-care, patients with Churg Strauss Syndrome can take an active role in managing their condition and improving their overall well-being. It is important to work closely with healthcare professionals to develop personalized approaches and strategies that meet individual needs and circumstances.
Support Groups And Resources For Individuals With Churg Strauss Syndrome
Support groups and resources play a crucial role in providing emotional support, information, and resources to individuals diagnosed with Churg Strauss Syndrome. Being diagnosed with such a rare and complex autoimmune disease can be overwhelming and isolating.
Read the full article
1 note
·
View note
Text
Rasmussen syndrome
Rasmussen Syndrome is a rare neurological disorder that primarily affects children, causing progressive inflammation and damage to one hemisphere of the brain. In this blog post, we will explore the various aspects of Rasmussen Syndrome, including its causes, signs and symptoms, diagnosis, treatment options, and the impact it has on daily life. We will also discuss the medications and surgical interventions commonly used to manage the condition, as well as the support and resources available for individuals living with Rasmussen Syndrome. Furthermore, we will delve into current research and advancements, prognosis, and provide coping strategies and tips for those living with this extraordinary condition.
What Is Rasmussen Syndrome?
Rasmussen Syndrome, also known as Rasmussen's encephalitis, is a rare neurological disorder that primarily affects children. It is characterized by chronic inflammation of only one hemisphere of the brain, leading to progressive neurological and cognitive deterioration. The exact cause of Rasmussen Syndrome is still unknown, but researchers suspect that it may be an autoimmune disorder, where the body's immune system mistakenly attacks healthy brain cells, leading to inflammation.
One of the key features of Rasmussen Syndrome is the continuous and unrelenting brain inflammation, which can result in seizures, weakness on one side of the body, and language difficulties. It typically starts in childhood, between the ages of 2 and 10 years, and tends to affect one hemisphere of the brain more severely than the other.
When diagnosing Rasmussen Syndrome, doctors usually conduct a comprehensive evaluation, including a physical examination, medical history review, and various diagnostic tests. These tests may include brain imaging techniques, such as MRI or CT scans, which can reveal the inflammation and any structural abnormalities in the affected hemisphere. Additionally, an electroencephalogram (EEG) may be performed to record the electrical activity of the brain and detect any abnormal patterns associated with seizures.
- Causes:
- Autoimmune disorder
- Mistaken immune response
- Attack on healthy brain cells
Signs and Symptoms:
Diagnosis:
- Seizures
- Weakness on one side of the body
- Language difficulties
- Physical examination
- Medical history review
- Brain imaging (MRI or CT scan)
- Electroencephalogram (EEG)
Although there is currently no cure for Rasmussen Syndrome, there are treatment options available to help manage the symptoms and slow down the progression of the disease. These treatment approaches involve a combination of medications, such as steroids or immunosuppressants, to reduce inflammation and suppress the immune response. In some cases, surgical interventions, such as hemispherectomy or functional hemispherotomy, may be considered to remove or disconnect the affected hemisphere of the brain.
Living with Rasmussen Syndrome can significantly impact an individual's daily life. The progressive nature of the disorder may lead to physical and cognitive impairments, making it challenging to carry out routine activities. Therefore, it is essential to provide individuals with Rasmussen Syndrome and their families with comprehensive support and resources. Various organizations, such as Rasmussen Syndrome Support Network, offer valuable information, support groups, and educational resources to assist individuals and their families in navigating the challenges associated with the condition.
In conclusion, Rasmussen Syndrome is a rare neurological disorder characterized by chronic inflammation of one hemisphere of the brain. While the exact cause remains unknown, it is believed to be an autoimmune disorder. Diagnosing Rasmussen Syndrome involves a thorough evaluation and various tests. Although there is no cure, treatment options and surgical interventions can help manage symptoms and improve quality of life. It is crucial to raise awareness about Rasmussen Syndrome, provide support to individuals and their families, and continue research efforts to further understand the condition and develop new advancements.
Causes Of Rasmussen Syndrome
Rasmussen Syndrome is a rare neurological disorder that mainly affects children. It is characterized by inflammation and progressive damage to one hemisphere of the brain.
The exact cause of Rasmussen Syndrome is still unknown. However, some researchers believe that it may have an autoimmune origin. It is suggested that the immune system mistakenly attacks healthy brain tissues, leading to inflammation and subsequent brain damage. Another theory is that Rasmussen Syndrome could be triggered by an infection, such as a viral infection, that causes an abnormal immune response.
Furthermore, studies have shown that there may be a genetic component to Rasmussen Syndrome. Certain gene mutations or genetic predispositions may increase the likelihood of developing the condition. However, more research is needed to fully understand the genetic factors involved in Rasmussen Syndrome development.
- Overall, the causes of Rasmussen Syndrome are complex and multifactorial. While the exact mechanisms are not fully understood, it is believed to involve a combination of autoimmune responses, viral infections, and genetic factors. Ongoing research aims to shed more light on the underlying causes and potential risk factors of this rare neurological disorder.
Causes of Rasmussen Syndrome
Unknown
Autoimmune origin
Infection-triggered immune response
Genetic factors
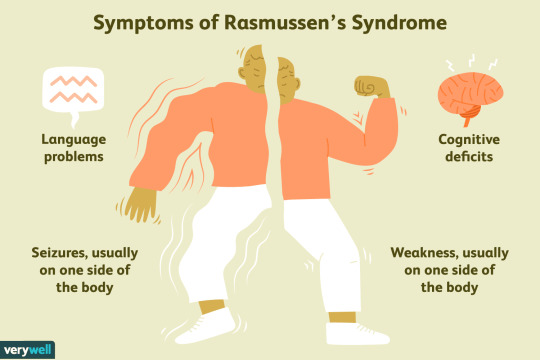
Signs And Symptoms Of Rasmussen Syndrome
Rasmussen syndrome is a rare neurological condition characterized by chronic inflammation of the brain, leading to seizures and progressive loss of motor skills and cognitive function. The exact cause of Rasmussen syndrome is still unknown, but it is believed to be an autoimmune disorder, where the body's immune system mistakenly attacks healthy brain tissue. This condition typically occurs in children, usually between the ages of 2 and 10, but can also affect adults. The signs and symptoms of Rasmussen syndrome can vary from person to person, but there are some common indicators that can help in its identification and diagnosis.
One of the primary indications of Rasmussen syndrome is the presence of frequent and severe seizures. These seizures may initially be mild, but over time they can become more intense and difficult to control with medication. Another common symptom is a progressive loss of motor skills on one side of the body, known as hemiparesis. This can result in a noticeable weakness or paralysis of the affected limbs, making it challenging for individuals to perform everyday tasks. Cognitive decline is also a significant symptom, with difficulties in thinking, memory, and language abilities being observed.
Alongside these primary symptoms, individuals with Rasmussen syndrome may also experience other neurological symptoms. These can include changes in behavior, personality, and emotions. They may become irritable, anxious, or depressed, which can significantly impact their quality of life. Additionally, they may have difficulties with speech and language, as well as problems with coordination and balance.
Diagnosing Rasmussen syndrome can be challenging, as it is a rare condition and shares some similarities with other neurological disorders. However, there are certain diagnostic tests that can be performed to help confirm the presence of Rasmussen syndrome. These tests may include brain imaging, such as magnetic resonance imaging (MRI), which can show inflammation and changes in brain structure. Electroencephalogram (EEG) is another test that can help in the detection of abnormal electrical activity in the brain, indicating the presence of seizures.
- In conclusion, Rasmussen syndrome is a rare neurological condition characterized by chronic inflammation of the brain, causing seizures and progressive loss of motor skills and cognitive function.
- Primary symptoms include frequent and severe seizures, progressive loss of motor skills (hemiparesis), and cognitive decline.
- Other neurological symptoms may include changes in behavior, speech and language difficulties, and problems with coordination and balance.
- Diagnosis of Rasmussen syndrome involves brain imaging and EEG to confirm the presence of inflammation and abnormal electrical activity in the brain.
Advantages
Disadvantages
The early detection of Rasmussen syndrome can help in implementing appropriate treatment strategies.
There is currently no cure for Rasmussen syndrome, and treatment primarily aims to manage symptoms and reduce the frequency of seizures.
Support and resources are available for individuals with Rasmussen syndrome and their families, providing assistance and guidance throughout their journey.
Rasmussen syndrome can have a significant impact on an individual's daily life, affecting their mobility, cognitive abilities, and emotional well-being.
Diagnosis Of Rasmussen Syndrome
Rasmussen Syndrome is a rare and chronic neurological disorder that mainly affects children. It is characterized by severe and progressive inflammation of one hemisphere of the brain, leading to various neurological symptoms. Diagnosing Rasmussen Syndrome can be challenging as its symptoms can mimic other neurological conditions, and no specific test can confirm its presence. However, certain diagnostic methods and criteria can help healthcare professionals in identifying this condition.
One of the key steps in diagnosing Rasmussen Syndrome is a thorough medical history review and physical examination. The doctor will carefully evaluate the patient's symptoms, including the nature and frequency of seizures, cognitive decline, and motor abnormalities. It is essential to distinguish these symptoms from other neurological disorders to arrive at an accurate diagnosis.
Additionally, various diagnostic tests are conducted to support the diagnosis of Rasmussen Syndrome. These can include:
- Electroencephalogram (EEG): EEG measures the electrical activity of the brain and can help identify abnormal brain wave patterns associated with seizures. In Rasmussen Syndrome, EEG findings often show focal slow waves and epileptic discharges in the affected hemisphere.
- Magnetic Resonance Imaging (MRI): MRI scans provide detailed images of the brain and can help visualize any structural abnormalities or inflammation. In Rasmussen Syndrome, MRI may show cortical atrophy, loss of brain tissue, and signs of inflammation in the affected hemisphere.
- Cerebrospinal Fluid Analysis: Analysis of the cerebrospinal fluid can help rule out other possible causes of inflammation and infection in the brain.
While these diagnostic tests provide valuable information, the diagnosis of Rasmussen Syndrome is ultimately based on a combination of clinical presentation, neuroimaging findings, and exclusion of other potential causes. The criteria proposed by the Rasmussen Syndrome Special Interest Group includes:
1. Unihemispheric involvement:
The inflammation and progressive damage primarily affect one hemisphere of the brain.
2. Drug resistance:
The seizures and neurological symptoms of Rasmussen Syndrome may not respond to standard antiepileptic drugs.
3. Focal seizures:
Seizures in Rasmussen Syndrome often start with focal symptoms, such as twitching in one part of the body, before spreading.
4. Neuroimaging findings:
MRI scans may reveal progressive brain atrophy and inflammation in the affected hemisphere.
5. Cognitive decline:
Children with Rasmussen Syndrome may experience a decline in cognitive abilities, such as language, attention, and memory.
Early and accurate diagnosis of Rasmussen Syndrome is crucial to initiate appropriate treatment strategies and support the overall management of the condition. If you suspect that you or your child may have Rasmussen Syndrome, it is important to consult a neurologist or an epileptologist for a comprehensive evaluation.
Treatment Options For Rasmussen Syndrome
Rasmussen Syndrome is a rare neurological disorder that primarily affects children. It is characterized by unilateral inflammation of the brain, leading to progressive hemiparesis (weakness or paralysis on one side of the body), seizures, and cognitive decline. As there is currently no cure for Rasmussen Syndrome, treatment primarily focuses on symptom management and minimizing disease progression.
One of the primary treatment options for Rasmussen Syndrome is the use of antiepileptic drugs (AEDs) to control seizures. These medications help reduce the frequency and severity of seizures, thereby improving the quality of life for individuals with Rasmussen Syndrome. Commonly prescribed AEDs include phenytoin, carbamazepine, and valproic acid.
In addition to AEDs, immunomodulatory therapies are often employed in the treatment of Rasmussen Syndrome. These therapies aim to suppress the immune system's inflammatory response and reduce the damage to brain tissue. Intravenous immunoglobulin (IVIG) and corticosteroids are examples of commonly used immunomodulatory treatments for Rasmussen Syndrome.
Surgical interventions may also be considered in cases where medications and immunomodulatory therapies do not provide sufficient symptom relief. Hemispherectomy, a surgical procedure that involves removing or disconnecting the affected hemisphere of the brain, is a drastic measure but can effectively manage seizures and prevent further brain damage in some cases of Rasmussen Syndrome.
In conclusion, while there is no definitive cure for Rasmussen Syndrome, a combination of antiepileptic drugs, immunomodulatory therapies, and, in severe cases, surgical interventions can help manage the symptoms associated with this rare neurological disorder. It is important for individuals with Rasmussen Syndrome to work closely with a multidisciplinary team of healthcare professionals to tailor a treatment plan that best suits their individual needs and to stay updated on the latest research and advancements in the field.
Medications Used To Manage Rasmussen Syndrome
The management of Rasmussen Syndrome often involves a combination of medications and other treatment options. Medications play a crucial role in controlling seizures, reducing inflammation, and managing the symptoms associated with this rare neurological disorder. Rasmussen Syndrome is characterized by severe and frequent seizures, cognitive decline, and progressive weakness on one side of the body (hemiparesis). While there is no cure for Rasmussen Syndrome, medications can help improve the quality of life for individuals living with this condition.
One commonly prescribed medication for Rasmussen Syndrome is steroids. Steroids, such as prednisone or methylprednisolone, work to reduce inflammation in the brain and decrease the frequency and severity of seizures. These medications can also help improve cognitive function and reduce the progression of hemiparesis. However, long-term use of steroids may have side effects, such as weight gain, mood changes, and weakened immune system.
In addition to steroids, immunomodulatory drugs are often used in the management of Rasmussen Syndrome. These medications, including intravenous immunoglobulins (IVIG) and immunosuppressants like cyclosporine or mycophenolate, work by suppressing the immune system, thus reducing the inflammation and damage caused by the autoimmune response that underlies Rasmussen Syndrome. These drugs can help reduce the frequency and intensity of seizures and slow down the progression of the disease.
Surgical Interventions For Rasmussen Syndrome
When it comes to treating Rasmussen Syndrome, there are various surgical interventions available that can help manage the symptoms and improve the quality of life for individuals with this rare condition. These interventions are often considered when other treatment options, such as medications and therapies, are not effective in controlling the seizures and reducing inflammation in the brain.
One of the surgical interventions commonly used for Rasmussen Syndrome is hemispherectomy. This procedure involves removing or disconnecting one hemisphere of the brain, which is the part most affected by the syndrome. By doing so, the spread of seizures and inflammation to the unaffected hemisphere is prevented, resulting in a significant reduction in seizure activity. Although a hemispherectomy is an extensive procedure, it can lead to substantial improvements in seizure control and overall functioning for individuals with Rasmussen Syndrome.
Another surgical option for Rasmussen Syndrome is multiple subpial transections (MST). This procedure involves making a series of small cuts in specific areas of the affected hemisphere without removing any brain tissue. The cuts disrupt the abnormal electrical pathways causing seizures, while preserving the functioning of the brain. MST is particularly useful for individuals with Rasmussen Syndrome who experience focal seizures or partial seizures, as it can help reduce the frequency and intensity of these seizures.
In some cases, callosotomy may be considered as a surgical intervention for Rasmussen Syndrome. Callosotomy involves cutting the corpus callosum, which is the structure that connects the two hemispheres of the brain. This procedure can help prevent the spread of seizures from one hemisphere to the other, reducing the overall seizure activity. Callosotomy is often performed when seizures in Rasmussen Syndrome are primarily characterized by generalized tonic-clonic seizures, also known as grand mal seizures.
Pros
Cons
- Significantly reduces seizure activity
- Risks associated with surgical procedures
- Improves quality of life
- Potential complications
- May lead to better cognitive and motor skills development
- Rehabilitation and recovery period
- Can be effective even when other treatments have failed
- Irreversible procedure
It is important to note that surgical interventions for Rasmussen Syndrome are typically considered as a last resort when other treatment options have been exhausted. Each individual's case is unique, and the decision to undergo surgery should be carefully discussed and evaluated with a team of healthcare professionals who specialize in the treatment of Rasmussen Syndrome. Additionally, post-surgical care, including rehabilitation, therapy, and ongoing medical management, is crucial for optimizing outcomes and supporting the individual's recovery.
Impact Of Rasmussen Syndrome On Daily Life
Rasmussen Syndrome is a rare neurological disorder that primarily affects children.
Read the full article
0 notes
Text
Merrf syndrome

Merrf Syndrome, also known as Myoclonic Epilepsy with Ragged Red Fibers, is a rare genetic disorder that affects the functioning of the mitochondria, the powerhouse of the cells. In this blog post, we will explore what Merrf Syndrome is, its causes, and the various symptoms and signs associated with it. Furthermore, we will delve into the genetic mutations linked to this syndrome and how it is diagnosed. Additionally, we will discuss the available treatment options, including managing the symptoms and providing supportive care for individuals living with Merrf Syndrome. Moreover, we will highlight the ongoing research and advancements in the field, as well as provide insights into the prognosis and life expectancy of those affected. Lastly, we will shed light on the challenges faced by individuals living with Merrf Syndrome and the available resources and support available to them.
What Is Merrf Syndrome
MERRF syndrome, which stands for Myoclonic Epilepsy with Ragged Red Fibers, is a rare and progressive neurological disorder that affects both children and adults. It is a mitochondrial disease characterized by a variety of symptoms including epilepsy, muscle weakness, and developmental delays. The name "ragged red fibers" refers to the appearance of muscle fibers under a microscope, which show red staining and abnormal shapes. This condition is caused by mutations in the mitochondrial DNA, specifically in the MT-TK gene.
MERRF syndrome is a genetic disorder that is inherited in a mitochondrial pattern, meaning it is passed down from the mother to her children. Mitochondria are responsible for producing energy in our cells, and when there is a mutation in the mitochondrial DNA, it can disrupt the normal functioning of the cells. This can lead to the symptoms associated with MERRF syndrome, such as seizures and muscle weakness.
There are several symptoms and signs that are commonly associated with MERRF syndrome. One of the most prominent features is myoclonic epilepsy, which is characterized by sudden, involuntary muscle jerks or twitches. These can occur at any time and can be triggered by various factors such as stress or physical activity. Other symptoms may include muscle weakness, hearing loss, problems with balance and coordination, and developmental delays in children. Additionally, individuals with MERRF syndrome may experience progressive deterioration of their cognitive abilities.
- Genetic mutations play a crucial role in the development of MERRF syndrome. Specifically, mutations in the MT-TK gene are responsible for disrupting the normal functioning of mitochondria, leading to the characteristic features of the condition. These mutations can vary among individuals, resulting in a wide range of symptoms and severity.
- Diagnosing MERRF syndrome can be challenging, as its symptoms overlap with other neurological disorders. However, genetic testing can help identify mutations in the mitochondrial DNA and confirm the diagnosis. Additionally, doctors may perform other tests such as electroencephalogram (EEG) to evaluate brain activity and muscle biopsy to examine the ragged red fibers in the muscle tissue.
- Treatment for MERRF syndrome focuses on managing the symptoms and improving the individual's quality of life. This may involve a combination of medications to control seizures and muscle spasms, physical therapy to maintain muscle strength and mobility, and occupational therapy to address any developmental delays or difficulties with daily activities.
Research
and Advancements
Ongoing research
in MERRF syndrome
is exploring potential treatments
and interventions to
target the underlying genetic
mutations and improve outcomes.
Scientists are also investigating
potential gene therapy approaches
to correct the mitochondrial
defects in the affected individuals.
Living with MERRF syndrome can be challenging, both for the individuals diagnosed and their families. It is important to seek supportive care from healthcare professionals who specialize in mitochondrial disorders. These experts can provide guidance and resources to help manage the symptoms, monitor the disease progression, and address any emotional or psychological impacts.
While MERRF syndrome is a progressive disorder, it is important to remember that every individual's experience with the condition is unique. The prognosis and life expectancy of MERRF syndrome can vary depending on the severity of symptoms and overall health of the individual. However, with appropriate management and support, individuals with MERRF syndrome can lead fulfilling lives and participate in activities they enjoy.
It is essential for individuals with MERRF syndrome and their families to have access to resources and support networks. Organizations such as the United Mitochondrial Disease Foundation and the Myoclonic Epilepsy with Ragged Red Fibers Community can provide valuable information, advocacy, and connections to other individuals who are going through similar experiences. These resources not only offer support but also contribute to raising awareness and promoting further research into MERRF syndrome.
Causes Of Merrf Syndrome
MERRF syndrome, which stands for Myoclonic Epilepsy with Ragged Red Fibers, is a rare genetic disorder that affects the mitochondria, the energy-producing centers in cells. This condition is characterized by a variety of symptoms, including muscle weakness, myoclonic seizures, ataxia, and hearing loss. The exact cause of MERRF syndrome is due to mutations in the mitochondrial DNA. Mutations in the MT-TK gene are the most common cause of this syndrome, although other genes can also be involved.
One of the main causes of MERRF syndrome is the presence of genetic mutations in the mitochondrial DNA. These mutations often occur spontaneously and are not inherited from either parent. However, in some cases, MERRF syndrome can be inherited from a person's mother, who may have the same genetic mutation. This is because mitochondria are passed down from the mother to the child. Therefore, if the mother carries the mutated mitochondrial DNA, there is a risk of passing on the syndrome to her offspring.
In addition to genetic mutations, other factors can also contribute to the development of MERRF syndrome. Environmental factors, such as exposure to toxins or certain medications, may increase the risk of developing this condition. However, these factors are believed to play a smaller role compared to the genetic component.
Researchers have made significant advancements in understanding the causes of MERRF syndrome. Through genetic testing, they have identified specific mutations in the mitochondrial DNA that are associated with the syndrome. This has allowed for more accurate diagnosis and has provided insights into the underlying biology of the disorder. Ongoing research continues to explore other potential causes and contributing factors, as well as potential treatment options for individuals living with MERRF syndrome.
Common Causes of MERRF Syndrome:
1. Genetic mutations in the mitochondrial DNA, particularly the MT-TK gene.
2. Inheritance of the mutated mitochondrial DNA from the mother.
3. Environmental factors, although their role is not well-understood.
It is important to note that while the exact causes of MERRF syndrome have been identified, there is currently no cure for this condition. Treatment options focus on managing the symptoms and providing supportive care to improve the quality of life for affected individuals. Genetic counseling is also recommended for individuals who may be at risk of passing on the syndrome to their children.
In conclusion, MERRF syndrome is primarily caused by genetic mutations in the mitochondrial DNA, particularly the MT-TK gene. The inheritance of these mutations from the mother can also contribute to the development of the syndrome. Ongoing research and advancements continue to shed light on the underlying causes and potential treatment options for this rare genetic disorder.
Symptoms And Signs Of Merrf Syndrome
MERRF syndrome, which stands for Myoclonic Epilepsy with Ragged Red Fibers, is a rare genetic disorder that affects the mitochondria, the energy-producing structures within cells. This syndrome is typically characterized by a combination of neurological symptoms and multi-systemic involvement. The symptoms and signs of MERRF syndrome can vary greatly between individuals, but there are several common features that may help in its identification.
Muscle problems: One of the key symptoms of MERRF syndrome is muscle weakness and wasting (atrophy). Affected individuals may experience difficulty with fine motor skills, such as writing or buttoning a shirt. They may also have muscle stiffness, spasms, or involuntary jerking movements known as myoclonus. These symptoms can greatly impact a person's mobility and coordination.
Epilepsy: Another prominent feature of MERRF syndrome is the presence of seizures, particularly myoclonic epilepsy. These seizures are characterized by sudden, brief muscle jerks or twitches. They may occur spontaneously or be triggered by various factors such as stress, sleep deprivation, or certain medications. Seizures can vary in intensity and frequency, and their management is an essential aspect of MERRF syndrome treatment.
Neurological and sensory involvement: MERRF syndrome can also affect the central nervous system and peripheral nerves. Individuals may experience cognitive impairment, such as difficulties with learning, attention, and memory. Sensory abnormalities may include deafness, hearing loss, or vision problems, including retinal changes that can be detected through an eye exam. These neurological and sensory symptoms further contribute to the complexity of the condition.
Genetic Mutations And Merrf Syndrome
Genetic Mutations And MERRF Syndrome
MERRF Syndrome, which stands for Myoclonic Epilepsy with Ragged Red Fibers, is a rare genetic disorder that affects the mitochondria, the powerhouse of our cells. This syndrome is caused by mutations in the genetic material of the mitochondria rather than the nuclear DNA. Mitochondrial DNA mutations can be inherited from one or both parents, or they can occur spontaneously during the formation of reproductive cells. The genetic mutations associated with MERRF Syndrome can lead to a range of symptoms and complications, making it essential to understand the underlying genetic factors.
One of the key genetic mutations linked to MERRF Syndrome is the mitochondrial DNA A8344G mutation. This specific mutation affects the transfer RNA*Lys gene and is most commonly associated with MERRF Syndrome. This mutation disrupts the production of proteins within the mitochondria, leading to the impaired function of these vital organelles. As a result, affected individuals may experience a wide array of symptoms, including muscle weakness, seizures, ataxia, and cognitive impairment.
Another genetic mutation related to MERRF Syndrome is the mitochondrial DNA T8356C mutation. This mutation affects the transfer RNA*Ser gene and has been found in individuals diagnosed with MERRF Syndrome. Similar to the A8344G mutation, the T8356C mutation impairs mitochondrial protein synthesis, leading to the characteristic features of the syndrome. It is worth noting that these genetic mutations are not the only ones associated with MERRF Syndrome. Researchers continue to explore different mutations and their specific implications to gain a better understanding of this complex disorder.
Common Genetic Mutations in MERRF Syndrome
Associated Features
A8344G
Impacts transfer RNA*Lys gene
T8356C
Affects transfer RNA*Ser gene
The identification of these genetic mutations plays a crucial role in diagnosing MERRF Syndrome. Genetic testing, including mitochondrial DNA sequencing, can help confirm the presence of these mutations in affected individuals. It is important to note that not all individuals with MERRF Syndrome will have these specific mutations, highlighting the genetic heterogeneity of the disorder.
Diagnosing Merrf Syndrome
MERRF syndrome, also known as Myoclonic Epilepsy with Ragged Red Fibers, is a rare genetic disorder that affects the mitochondria, which are the energy-producing structures within cells. People with MERRF syndrome have various symptoms, including muscle weakness, seizures, and developmental delays. In order to diagnose MERRF syndrome, healthcare professionals utilize a combination of genetic testing, medical history review, physical examination, and laboratory tests.
Genetic testing plays a crucial role in diagnosing MERRF syndrome. By analyzing a person's DNA, doctors can identify mutations in the mitochondrial DNA or nuclear DNA, which are responsible for causing the condition. This testing is usually done using a blood sample or a saliva sample. If a known mutation is found, it can confirm the diagnosis. However, in some cases, the genetic testing may not identify any known mutations, making the diagnosis more challenging.
Medical history review and physical examination are also important steps in the diagnostic process. Doctors will ask about the individual's symptoms, family history, and any other relevant information. During the physical examination, they may look for specific signs, such as muscle weakness, myoclonus (involuntary muscle jerks), and the presence of ragged red fibers in muscle biopsies.
Laboratory tests can provide additional information to support the diagnosis of MERRF syndrome. These tests may include blood tests, urine tests, and muscle biopsies. Blood tests can measure the levels of lactate, pyruvate, and creatine kinase, which can be elevated in individuals with MERRF syndrome. Urine tests may reveal high levels of certain metabolites, further indicating the presence of the disorder. Muscle biopsies, where a small sample of muscle tissue is removed and examined under a microscope, can show characteristic ragged red fibers, which are abnormally structured muscle fibers.
In conclusion, diagnosing MERRF syndrome involves a comprehensive approach that combines genetic testing, medical history review, physical examination, and laboratory tests. It is essential for healthcare professionals to diligently investigate the presence of this rare condition to ensure accurate diagnosis and appropriate management strategies. Early diagnosis is crucial in providing individuals with MERRF syndrome the necessary care and support to improve their quality of life.
Treatment Options For Merrf Syndrome
MERRF syndrome, or Myoclonic Epilepsy with Ragged Red Fibers, is a rare genetic disorder that affects the mitochondria in the body's cells. This syndrome is characterized by a variety of symptoms, including myoclonic seizures, muscle weakness, and progressive neurological deterioration. Although there is currently no cure for MERRF syndrome, there are treatment options available to help manage the symptoms and improve quality of life for individuals affected by this condition.
One of the primary treatment options for MERRF syndrome is medication. Anticonvulsant drugs can be prescribed to help control seizures and reduce the frequency and intensity of myoclonic jerks. These medications work by stabilizing the electrical activity in the brain and preventing abnormal firing of neurons. It is important for individuals with MERRF syndrome to work closely with a healthcare provider to find the most effective medication and dosage for their specific symptoms.
In addition to medication, individuals with MERRF syndrome may benefit from other forms of therapy. Physical therapy can help improve muscle strength and coordination, while occupational therapy can assist with maintaining independence in daily activities. Speech therapy may also be useful in managing any speech or swallowing difficulties that may arise due to muscle weakness. These therapies can be tailored to the individual's needs and can be instrumental in maximizing their functional abilities.
- Home modifications can also be an important part of treatment for individuals with MERRF syndrome. Simple adaptations to the home environment, such as grab bars in the bathroom or ramps for wheelchair accessibility, can enhance safety and independence. It is important to consult with a healthcare professional or occupational therapist for guidance on specific home modifications that may be beneficial.
Moreover, patients with MERRF syndrome may also benefit from palliative care interventions. The goal of palliative care is to improve the quality of life for individuals with serious illnesses, such as MERRF syndrome. This type of care focuses on providing relief from symptoms, managing pain, and addressing emotional and psychosocial needs. Palliative care can be provided alongside other treatments and is aimed at supporting the overall well-being of the individual.
Advancements in research
While there is currently no cure for MERRF syndrome, ongoing research is aimed at better understanding the condition and developing potential treatments. Scientists are studying the underlying genetic mutations responsible for MERRF syndrome, which may open up opportunities for targeted therapies in the future. Advances in mitochondrial replacement therapies and gene editing techniques may hold promise for individuals affected by MERRF syndrome, offering hope for improved treatment options in the years to come.
In conclusion, although there is no cure for MERRF syndrome at present, there are treatment options available to help manage the symptoms and improve the quality of life for individuals with this condition. Medications can help control seizures, while therapies such as physical and occupational therapy can enhance functional abilities. Home modifications and palliative care interventions can also play a significant role in providing support and improving overall well-being. Ongoing research holds promise for future advancements in treatment options for MERRF syndrome, potentially offering hope for individuals and their families.
Managing The Symptoms Of Merrf Syndrome
Managing the Symptoms of MERRF Syndrome
MERRF syndrome, which stands for Myoclonic Epilepsy with Ragged Red Fibers, is a rare genetic disorder that affects the mitochondria, the powerhouses of the cells. Individuals with MERRF syndrome often experience a variety of symptoms that can significantly impact their daily lives. While there is currently no cure for MERRF syndrome, there are various strategies and treatments available to help manage the symptoms and improve quality of life.
One of the primary goals in managing MERRF syndrome is to control the seizures and reduce their frequency. Antiepileptic medications, such as valproic acid or carbamazepine, are commonly prescribed to help decrease seizure activity.
Read the full article
0 notes
Text
Kearns sayre syndrome

Kearns Sayre Syndrome (KSS) is a rare mitochondrial disorder that primarily affects the muscles and the eyes. In this blog post, we will explore the causes, symptoms, and diagnosis of KSS, as well as discuss various treatment options and management strategies. We will also delve into the potential use of gene therapy and explore the importance of exercise in managing the condition. Additionally, we will provide information about support groups and resources available to KSS patients and their families. Lastly, we will touch on ongoing research and future directions in the field of Kearns Sayre Syndrome.
What Is Kearns Sayre Syndrome?
Kearns-Sayre Syndrome (KSS) is a rare genetic disorder that affects multiple body systems, particularly the eyes, muscles, and heart. It is classified as a type of mitochondrial myopathy, which means it is caused by defects in the mitochondria, the powerhouses of our cells. KSS typically presents in childhood or adolescence and is characterized by a combination of symptoms that can vary in severity from person to person.
One of the key features of KSS is progressive external ophthalmoplegia (PEO), which is the inability to move the eyes in various directions. Individuals with KSS often develop ptosis, a drooping of the eyelids, as well. This eye movement disorder can lead to visual impairment and difficulty with everyday tasks such as reading or driving.
In addition to ophthalmoplegia, KSS can also cause muscle weakness and fatigue. Affected individuals may experience generalized weakness or weakness in specific muscle groups. This can result in difficulties with mobility and coordination.
Causes Of Kearns Sayre Syndrome
Kearns Sayre Syndrome (KSS) is a rare genetic disorder that affects multiple body systems, including the muscles and the eyes. It is caused by mutations in the mitochondrial DNA, which leads to the dysfunction of the mitochondria. In this blog post, we will explore the causes of Kearns Sayre Syndrome and delve into the genetic factors that contribute to its development.
One of the primary causes of Kearns Sayre Syndrome is the presence of mutations in the mitochondrial DNA. Mitochondria are responsible for producing the energy required for cell function. However, when these mutations occur, the mitochondria are unable to produce energy efficiently, leading to cell dysfunction and damage. This dysfunction can affect various organs and systems in the body, including the muscles and the eyes.
In most cases, the mutations that cause Kearns Sayre Syndrome are sporadic, meaning they occur randomly and are not inherited from parents. However, in some instances, these mutations can be passed down from an affected individual to their offspring. The inheritance pattern of Kearns Sayre Syndrome can vary, and individuals with the condition may or may not have affected family members.
Common Causes of Kearns Sayre Syndrome
Cause
Description
Mitochondrial DNA mutations
Genetic mutations in the mitochondrial DNA lead to dysfunction of the mitochondria, affecting energy production and cell function.
Sporadic mutations
In many cases, the mutations that cause Kearns Sayre Syndrome occur randomly and are not inherited from parents.
Inherited mutations
In some instances, the mutations can be inherited from an affected parent, although the inheritance pattern can vary.
Researchers are still working to understand the specific genetic mechanisms that contribute to the development of Kearns Sayre Syndrome. However, it is clear that mutations in the mitochondrial DNA play a crucial role in the pathogenesis of this condition. Further studies and advancements in genetic research hold promise for uncovering more insights into the causes and potential treatments for Kearns Sayre Syndrome.
Symptoms And Signs Of Kearns Sayre Syndrome
Kearns Sayre Syndrome (KSS) is a rare genetic disorder that affects multiple body systems, particularly the muscles and eyes. The condition typically presents in childhood or adolescence and can have a profound impact on an individual's overall health and wellbeing. In this blog post, we will explore the various symptoms and signs of KSS, helping to shed light on the challenges faced by those living with this condition.
Muscular Symptoms:
One of the primary manifestations of KSS is progressive muscle weakness, also known as myopathy. Individuals with KSS may experience muscle weakness in the limbs, leading to difficulties with walking, balance, and coordination. As the disease progresses, weakness may also affect the muscles involved in swallowing and breathing, potentially resulting in respiratory complications. It is important for individuals with KSS to have regular assessments of muscle function to monitor disease progression and manage any associated complications.
Neurological Symptoms:
In addition to muscular symptoms, KSS can also affect the nervous system and lead to various neurological signs. For instance, individuals with KSS may experience a range of movement disorders such as tremors, muscle spasms, and involuntary eye movements known as nystagmus. These movement abnormalities can significantly impact an individual's quality of life and may require specific interventions or therapies for symptom management.
Ophthalmic Symptoms:
The eyes are often significantly affected in KSS, and visual impairment is one of the hallmark features of the condition. Individuals with KSS may develop a condition called progressive external ophthalmoplegia, characterized by weakness or paralysis of the eye muscles responsible for eye movements. This can result in ptosis (drooping of the eyelids), double vision, and difficulty controlling eye movements. Regular eye examinations and early interventions are crucial to ensure appropriate support and management of vision problems in individuals with KSS.
Overall, it is essential to recognize and understand the symptoms and signs of Kearns Sayre Syndrome to facilitate early diagnosis and effective management. The broad range of symptoms experienced by individuals with KSS underscores the need for a multidisciplinary approach to care, involving specialists from various fields such as neurology, ophthalmology, and physical therapy. By providing comprehensive support and tailored interventions, we can improve the quality of life for those living with Kearns Sayre Syndrome.
Diagnosis And Screening For Kearns Sayre Syndrome
Kearns Sayre Syndrome (KSS) is a rare genetic disorder that affects multiple body systems, particularly the muscles and the eyes. It is caused by a defect in the mitochondria, the powerhouse of the cells responsible for generating energy. Diagnosing KSS can be challenging as the symptoms can vary widely among individuals. However, early detection and accurate diagnosis are crucial for effective management and treatment.
Screening for Kearns Sayre Syndrome:
Screening for KSS typically involves a combination of medical history evaluation, physical examination, and specialized tests. In many cases, symptoms of KSS manifest in childhood or adolescence, but in some instances, the disease may remain undiagnosed until adulthood. Therefore, screening for KSS may be recommended if a person presents with specific symptoms, such as unexplained muscle weakness, progressive external ophthalmoplegia (weakness or paralysis of eye muscles), heart conduction defects, or neurologic abnormalities. Furthermore, individuals with a family history of KSS or known mitochondrial disorders should also undergo screening.
Diagnostic Tests for Kearns Sayre Syndrome:
To confirm a diagnosis of KSS, several diagnostic tests may be conducted. One of the primary tests is a muscle biopsy, in which a small sample of muscle tissue is surgically removed and examined under a microscope. The biopsy helps identify abnormal mitochondria or other cellular abnormalities characteristic of KSS. Additionally, mitochondrial DNA analysis can be conducted to detect deletions or rearrangements in the mitochondrial genome. This test is particularly useful in cases where muscle biopsy results are inconclusive or unavailable.
Other diagnostic procedures may include:
- Electrocardiogram (ECG): This test measures the electrical activity of the heart and helps identify any heart conduction defects often associated with KSS.
- Electromyogram (EMG): EMG measures the electrical activity of muscles and can help assess the extent of muscle damage or weakness.
- Genetic testing: Genetic testing can help identify specific gene mutations associated with KSS. However, it should be noted that not all individuals with KSS have detectable genetic mutations.
It is essential to consult with a specialist, such as a neurologist or geneticist, experienced in diagnosing mitochondrial disorders, including KSS. They can evaluate the individual's medical history, perform the necessary tests, and interpret the results accurately.
In conclusion, early diagnosis and screening for Kearns Sayre Syndrome are vital to ensure appropriate management and treatment. Screening is recommended for individuals displaying symptoms or with a family history of KSS or other mitochondrial disorders. Diagnostic tests, such as muscle biopsy and genetic analysis, help confirm the diagnosis and provide valuable insights into the underlying genetic mutations or cellular abnormalities. Seeking expert medical care and guidance is crucial for individuals suspected of having KSS, enabling them to receive appropriate support and treatment strategies.
Targeting Mitochondrial Dysfunction In Kearns Sayre Syndrome
Kearns Sayre Syndrome (KSS) is a rare genetic disorder that affects multiple systems in the body. It is characterized by progressive weakness of the muscles that control eye movement (ophthalmoplegia), heart abnormalities, and other symptoms. One of the underlying causes of KSS is mitochondrial dysfunction, which refers to a failure in the energy-producing structures within cells called mitochondria. In this blog post, we will explore the importance of targeting mitochondrial dysfunction in the management and potential treatment of Kearns Sayre Syndrome.
Mitochondria play a crucial role in producing energy for the body's cells. They generate adenosine triphosphate (ATP), the main source of cellular energy. However, in individuals with KSS, the mitochondria do not function properly, leading to a deficiency in ATP production. This deficiency can affect various organs and tissues, including the muscles, heart, brain, and eyes.
Targeting mitochondrial dysfunction in Kearns Sayre Syndrome is essential to alleviate the symptoms and improve the quality of life for affected individuals. One approach to addressing mitochondrial dysfunction is through the use of supplements and medications that support mitochondrial function. Coenzyme Q10 (CoQ10) is a commonly used supplement that plays a critical role in ATP production and can help improve energy levels in KSS patients.
Potential Treatments For Kearns Sayre Syndrome
Kearns Sayre Syndrome (KSS) is a rare genetic disorder that affects various systems in the body, particularly the mitochondria. Mitochondria are often referred to as the powerhouses of the cells because they produce the energy needed for cellular function. In individuals with KSS, there is a mutation in the mitochondrial DNA that leads to impaired energy production. As a result, different organs and tissues, such as the brain, heart, muscles, and eyes, can be affected. Currently, there is no cure for KSS, but there are potential treatments that aim to manage the symptoms and improve the quality of life for individuals with the syndrome.
One potential treatment approach for Kearns Sayre Syndrome involves the use of coenzyme Q10 supplements. Coenzyme Q10 is a substance that is naturally produced in the body and plays a vital role in the production of cellular energy. However, individuals with KSS often have reduced levels of coenzyme Q10. Studies have suggested that supplementation with coenzyme Q10 may help improve energy production and reduce symptoms in some individuals with KSS. It is important to note that the effectiveness of coenzyme Q10 supplementation can vary from person to person, and further research is needed to determine its true benefits in treating KSS.
Another potential treatment option for Kearns Sayre Syndrome is the use of antioxidants. Antioxidants are substances that help protect cells from damage caused by oxidative stress. Since mitochondrial dysfunction and oxidative stress are key factors in KSS, antioxidants may play a role in managing the symptoms and slowing the progression of the syndrome. Some common antioxidants that have been studied in the context of KSS include vitamin E, vitamin C, and alpha-lipoic acid. However, more research is needed to establish the optimal dosage and effectiveness of these antioxidants in treating KSS.
Additionally, various therapies and interventions can help manage specific symptoms associated with Kearns Sayre Syndrome. For example, cardiac symptoms can be addressed through regular monitoring and appropriate medications to manage heart rhythm abnormalities. Physical therapy and exercise programs can help improve muscle strength and mobility. In some cases, individuals with KSS may also benefit from speech and occupational therapy to address communication and daily living challenges. Ophthalmologic interventions, such as eyeglasses, contact lenses, or surgery, can be utilized to manage vision problems associated with KSS.
Potential Treatments for Kearns Sayre Syndrome
Coenzyme Q10 supplementation
Antioxidant therapy
Cardiac symptom management
Physical therapy and exercise programs
Speech and occupational therapy
Ophthalmologic interventions
In conclusion, while there is no cure for Kearns Sayre Syndrome, there are potential treatments available that aim to manage the symptoms and improve the quality of life for individuals with the syndrome. These treatments include coenzyme Q10 supplementation, antioxidant therapy, symptom-specific interventions, and therapies to address various challenges associated with KSS. However, it is crucial to consult with healthcare professionals and genetic specialists for personalized treatment plans and to stay updated on the latest research developments in this field.
Gene Therapy Approaches For Kearns Sayre Syndrome
Kearns Sayre Syndrome (KSS) is a rare genetic disorder that affects multiple systems in the body, including the muscles, eyes, and heart. It is typically caused by mutations in the mitochondrial DNA, leading to a dysfunction in the mitochondria, which are the powerhouses of the cells. As a result, individuals with KSS often experience muscle weakness, progressive eye muscle paralysis, heart block, and various other complications. Currently, there is no cure for KSS, but advancements in gene therapy offer hope for potential treatments.
Gene therapy is a promising approach for the treatment of genetic disorders like KSS. It involves delivering functional copies of specific genes into the cells to compensate for the defective ones. For KSS, scientists are exploring different strategies to target the mitochondrial dysfunction and restore the normal functioning of the affected cells. One approach being studied is the transfer of healthy mitochondrial DNA into the patient's cells using viral vectors. These vectors are modified viruses that can deliver the desired genes into the target cells without causing harm.
Another gene therapy approach for KSS is the use of nuclear transfer techniques. This involves transferring the nucleus from the patient's affected cells into healthy donor cells, which have mitochondria with normal functioning mitochondria, through a process called nuclear transfer. The resulting cells, known as cytoplasmic hybrid cells or cybrids, contain the patient's nuclear DNA but healthy mitochondrial DNA. By reintroducing these cells into the patient's body, it is hoped that the healthy mitochondria can compensate for the dysfunctional ones.
Potential Benefits of Gene Therapy Approaches for KSS:
- Potential reversal of symptoms: Gene therapy approaches aim to restore the normal functioning of mitochondria, potentially reversing some of the symptoms associated with KSS.
- Long-term treatment: Successful gene therapy could potentially provide long-lasting effects, reducing the need for continuous management and treatment.
- Precision targeting: Gene therapy allows for specific targeting of the affected cells, potentially minimizing off-target effects.
- Personalized approach: Gene therapy can be tailored to each individual's specific genetic mutations, maximizing its potential effectiveness.
- Reduced dependency on symptomatic treatments: If gene therapy proves successful, it may reduce the need for symptomatic treatments and improve the overall quality of life for individuals with KSS.
While gene therapy approaches show promise for the treatment of KSS, it is important to note that research and clinical trials are still in the early stages. There are several challenges to overcome, such as the delivery of therapeutic genes to specific tissues or organs and potential immune responses to the viral vectors. Furthermore, the long-term safety and efficacy of gene therapy need to be carefully evaluated before it can become a widely available treatment option for KSS.
In conclusion, gene therapy approaches offer hope for the treatment of Kearns Sayre Syndrome by targeting the underlying mitochondrial dysfunction. The transfer of functional genes and healthy mitochondrial DNA into affected cells may help restore their normal functioning and potentially reverse some of the symptoms associated with KSS. However, further research and clinical trials are necessary to fully understand the safety, efficacy, and long-term effects of gene therapy for KSS. The advancements in this field provide optimism for individuals living with KSS and their families, as the potential for effective treatments grows closer to reality.
Exercise And Management Strategies For Kearns Sayre Syndrome
Kearns Sayre Syndrome (KSS) is a rare neuromuscular disorder that affects various body systems, including the muscles, eyes, and heart. It is caused by a mutation in the mitochondrial DNA, leading to impaired energy production. While there is currently no cure for KSS, exercise and certain management strategies can play a crucial role in improving the quality of life for individuals with this condition.
- Importance of Exercise:
Regular exercise is essential for individuals with Kearns Sayre Syndrome as it can help maintain muscle strength, enhance flexibility, and improve overall physical well-being.
Read the full article
0 notes
Text
Melas syndrome

Melas Syndrome is a rare and debilitating genetic disorder that affects multiple systems in the body. This blog post aims to provide a comprehensive understanding of Melas Syndrome, including its causes, symptoms, diagnosis, and treatment options. Additionally, we will explore the lifestyle changes and supportive therapies that can help manage the condition, as well as the potential complications that individuals with Melas Syndrome may face. Moreover, we will discuss the latest research and advances in the field, and provide coping strategies for living with this complex syndrome. Finally, we will delve into the genetic component of Melas Syndrome and its impact on prognosis and outlook.
What Is Melas Syndrome?
Melas syndrome, also known as Mitochondrial Myopathy, Encephalomyopathy, Lactic Acidosis, and Stroke-like episodes, is a rare genetic disorder that affects the mitochondria, the powerhouses of the cells. This syndrome is caused by mutations in the mitochondrial DNA, leading to impaired energy production and various organ dysfunctions. The symptoms and severity of Melas syndrome can vary from person to person, making it a complex disorder to understand and manage.
Individuals with Melas syndrome often experience stroke-like episodes, characterized by the sudden onset of neurological symptoms such as headache, seizures, and loss of consciousness. These episodes can be triggered by stress, infection, or intense physical activity. Furthermore, affected individuals may also exhibit signs of muscle weakness, hearing loss, and heart abnormalities. The progressive nature of the disorder poses significant challenges for those living with Melas syndrome.
Diagnosing Melas syndrome can be challenging due to its similarity to other conditions. Healthcare professionals rely on a combination of clinical examinations, genetic testing, and imaging studies to confirm the presence of the disorder. It is important to consider Melas syndrome as a potential diagnosis, especially in individuals who present with stroke-like symptoms at a young age.
- Melas syndrome is a genetic disorder affecting the mitochondria.
- Stroke-like episodes are a key characteristic of this syndrome.
- Impaired energy production is caused by mutations in the mitochondrial DNA.
Causes
Symptoms
Diagnosis
Mutations in the mitochondrial DNA
Stroke-like episodes
Clinical examinations
Impaired energy production
Muscle weakness
Genetic testing
Organ dysfunctions
Hearing loss
Imaging studies
While there is currently no cure for Melas syndrome, treatment focuses on managing the symptoms and supporting overall well-being. Lifestyle changes such as a balanced diet, regular exercise, and avoiding triggers can help individuals with Melas syndrome improve their quality of life. Supportive therapies, including physical and occupational therapy, can be beneficial in managing muscle weakness and enhancing daily functioning.
It is essential for individuals with Melas syndrome to work closely with a multidisciplinary healthcare team, including neurologists, geneticists, and other specialists. Long-term follow-up is necessary to monitor the progression of the disorder and adjust treatment strategies accordingly. Additionally, genetic counseling can provide valuable information and support for families affected by Melas syndrome.
Despite the challenges posed by Melas syndrome, ongoing research and advances in mitochondrial medicine offer hope for improved understanding and potential future treatments. Scientists are continuously exploring new approaches to mitigate the impact of mitochondrial dysfunctions and develop targeted therapies to address the underlying genetic mutations.
Living with Melas syndrome can be challenging, both for the individuals affected and their families. It is important to establish a strong support system and connect with patient advocacy organizations to access resources, education, and emotional support. Additionally, developing coping strategies and fostering a positive mindset can contribute to a better overall well-being.
In conclusion, Melas syndrome is a complex genetic disorder that affects the mitochondria and can cause a range of symptoms and complications. Early diagnosis, comprehensive management, and ongoing research are key in enhancing the quality of life for individuals living with Melas syndrome.
Causes Of Melas Syndrome
MELAS syndrome, short for Mitochondrial Encephalopathy, Lactic Acidosis, and Stroke-like episodes, is a rare genetic disorder that affects the energy-producing part of our cells: the mitochondria.
This syndrome is caused by mutations in the mitochondrial DNA (mtDNA), leading to impaired function of the mitochondria. Mitochondria are responsible for generating energy for the cells through a process called oxidative phosphorylation.
There are several known causes of Melas syndrome. The most common cause is a mutation in the MT-TL1 gene, which provides instructions for the production of transfer RNA molecules involved in mitochondrial protein synthesis. When this gene is mutated, it disrupts the protein synthesis process, leading to mitochondrial dysfunction.
Causes of Melas Syndrome:
- Genetic mutations in the MT-TL1 gene
- Inherited mutations in other mitochondrial genes
- Spontaneous mutations during development
- Maternal inheritance of mtDNA mutations
In addition to genetic causes, Melas syndrome can also be caused by spontaneous mutations that occur during early development. These mutations can affect various mitochondrial genes and disrupt the normal functioning of mitochondria.
Another important cause of Melas syndrome is maternal inheritance of mtDNA mutations. Since mitochondria are primarily passed down from the mother, if she carries a mutation in her mitochondrial DNA, there is a chance that her offspring may inherit the mutation and develop Melas syndrome.
In conclusion, Melas syndrome is primarily caused by genetic mutations in the mitochondrial DNA, specifically the MT-TL1 gene. However, spontaneous mutations during development and maternal inheritance of mtDNA mutations can also contribute to the development of this rare syndrome.
Symptoms And Signs Of Melas Syndrome
MELAS syndrome, which stands for mitochondrial encephalopathy, lactic acidosis, and stroke-like episodes, is a rare genetic disorder that affects the energy production in cells. This progressive condition primarily affects the brain and nervous system, leading to a variety of symptoms and signs. Understanding the symptoms and signs of MELAS syndrome is crucial for early diagnosis and prompt intervention.
One of the hallmark symptoms of MELAS syndrome is the occurrence of stroke-like episodes. During these episodes, individuals may experience sudden neurological deficits, such as weakness or paralysis on one side of the body, vision or speech problems, and seizures. These stroke-like episodes can cause long-lasting or even permanent damage to the brain, impairing various functions.
Lactic acidosis is another key feature of MELAS syndrome. It refers to the buildup of lactic acid in the body, leading to an acidic environment. This can result in fatigue, muscle weakness, and recurrent bouts of vomiting. Lactic acidosis is caused by the impaired function of mitochondria, the powerhouses of the cells responsible for generating energy.
Other common symptoms of MELAS syndrome include hearing loss, developmental delays, short stature, and heart abnormalities. Additionally, individuals with MELAS syndrome may experience gastrointestinal issues, such as constipation or diarrhea. As the condition progresses, cognitive decline, movement disorders, and respiratory problems may also develop.
Stroke-like episodes
Lactic acidosis
Hearing loss
Developmental delays
Short stature
Heart abnormalities
Gastrointestinal issues
Cognitive decline
Movement disorders
Respiratory problems
Symptoms
Signs
Stroke-like episodes
Hearing loss
Lactic acidosis
Developmental delays
Gastrointestinal issues
Cognitive decline
Diagnosis Of Melas Syndrome
Diagnosis of Melas Syndrome
Diagnosing Melas Syndrome can be challenging, as its symptoms often resemble those of other disorders. However, with the help of various medical tests and examinations, healthcare professionals can determine whether an individual is affected by this rare mitochondrial disorder. It is essential to identify Melas Syndrome accurately to provide appropriate medical interventions and support to affected individuals and their families.
One of the first steps in diagnosing Melas Syndrome is conducting a thorough physical examination. Healthcare providers examine the patient's medical history, assessing any symptoms or problems that may indicate the presence of this disorder. Often, initial symptoms can include muscle weakness, neurological issues, and even seizures. It is crucial for healthcare professionals to pay close attention to these early signs and symptoms to prevent any potential delay in diagnosis and treatment.
Following the physical examination, doctors may recommend various laboratory tests to confirm the presence of Melas Syndrome. These tests usually involve analyzing blood samples for genetic mutations and abnormalities in the mitochondrial DNA. Genetic tests play a vital role in diagnosing this disorder, as they can detect specific mutations in genes associated with Melas Syndrome. By examining the DNA closely, healthcare professionals can identify any changes or alterations that may be indicative of the disorder. This information is crucial for accurate diagnosis and subsequent treatment planning.
Common Diagnostic Tests for Melas Syndrome
- Genetic Testing: This test helps identify genetic mutations associated with Melas Syndrome.
- Muscle Biopsy: A small sample of muscle tissue is taken and examined for abnormalities.
- Lactic Acid Testing: Elevated levels of lactic acid in the blood or cerebrospinal fluid can indicate Melas Syndrome.
Another diagnostic procedure commonly used when assessing individuals suspected of having Melas Syndrome is a muscle biopsy. A small sample of muscle tissue is taken under local anesthesia and examined under a microscope. This biopsy helps determine if there are any abnormalities, such as ragged red fibers or mitochondrial accumulations, which are characteristic of Melas Syndrome. Muscle biopsies allow for a more definitive diagnosis and provide valuable information regarding the severity of the disease.
Treatment Options For Melas Syndrome
When it comes to treating Melas syndrome, it is important to understand that there is currently no cure for this rare mitochondrial disorder. However, various treatment options are available to help manage the symptoms and improve the quality of life for individuals with Melas syndrome.
1. Medications:
Doctors may prescribe certain medications to alleviate the symptoms associated with Melas syndrome. For example, coenzyme Q10 supplements are commonly recommended to enhance mitochondrial function and reduce muscle weakness. Other medications may be prescribed to manage specific symptoms such as seizures, cardiac complications, and gastrointestinal issues.
2. Nutritional Support:
A balanced diet plays a crucial role in managing Melas syndrome. Individuals with this condition may benefit from a diet rich in antioxidants, vitamins, and minerals to support overall health. Moreover, some medications or supplements may need to be administered to ensure proper nutrient absorption.
3. Symptomatic Management:
Since Melas syndrome affects various body systems, a multidisciplinary approach is typically employed to address specific symptoms. Physical therapy can help improve muscle strength, mobility, and coordination, while occupational therapy may focus on enhancing daily living skills. Speech and language therapy can assist with communication difficulties commonly experienced by individuals with Melas syndrome.
4. Supportive Measures:
Supportive therapies can greatly benefit individuals with Melas syndrome. Respiratory support, such as using a ventilator or positive airway pressure devices, may be required if breathing difficulties arise. Additionally, hearing aids, glasses, or other assistive devices can improve sensory impairments, if present. It is crucial to work closely with healthcare professionals to determine the most suitable supportive measures for each individual.
5. Genetic Counseling:
Genetic counseling is an important aspect of managing Melas syndrome. Since the condition has a genetic component, it is essential for affected individuals and their families to be informed about the inheritance pattern, risk of transmission, and potential implications for future generations. Genetic counselors can provide valuable guidance and support for family planning decisions.
Conclusion:
Although there is currently no cure for Melas syndrome, individuals affected by this disorder can benefit from various treatment options to manage their symptoms and improve their overall well-being. From medications to supportive measures, a comprehensive approach is necessary to address the diverse manifestations of this condition. Additionally, genetic counseling plays a crucial role in ensuring informed decision-making and providing support to affected individuals and their families.
Managing Melas Syndrome: Lifestyle Changes
Melas Syndrome is a rare genetic disorder that affects the mitochondria, the powerhouses of our cells. It stands for Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like episodes, which are the key features of this condition. Managing Melas Syndrome involves a combination of medical interventions and certain lifestyle changes to improve the quality of life for individuals affected by this challenging condition.
One of the most important lifestyle changes for those with Melas Syndrome is maintaining a healthy diet. A diet rich in nutrients, including vitamins and minerals, can help optimize mitochondrial function and overall health. It is crucial to consume a balanced diet consisting of fresh fruits, vegetables, whole grains, lean proteins, and healthy fats. Limiting the intake of processed and sugary foods is also recommended to avoid inflammation and oxidative stress, which can worsen symptoms.
In addition to a healthy diet, regular physical activity plays a significant role in managing Melas Syndrome. Engaging in regular exercise, such as walking, swimming, or cycling, can help improve cardiovascular health, increase energy levels, and enhance overall well-being. However, it is essential to customize the exercise routine based on individual capabilities and consult with healthcare professionals to avoid exertion and prevent potential muscle damage.
Keep in mind:
benefits of exercise
Avoid overexertion:
Exercise should be tailored to an individual's capabilities, and it is crucial not to push beyond one's limits to prevent fatigue and muscle damage.
Boosted cardiovascular health:
Regular physical activity can help improve heart function and enhance blood circulation to meet the body's energy demands.
Increased energy levels:
Exercise releases endorphins, which can improve mood, increase energy levels, and reduce fatigue often associated with Melas Syndrome.
Furthermore, it is crucial for individuals with Melas Syndrome to prioritize adequate rest and sleep. Fatigue is a common symptom of the condition, and getting enough restorative sleep is vital for managing energy levels and overall health. It is recommended to maintain a consistent sleep schedule and create a relaxing bedtime routine to promote better sleep quality.
Managing stress is another crucial aspect of coping with Melas Syndrome. Stress can exacerbate symptoms and increase the risk of experiencing stroke-like episodes. Engaging in stress-reducing activities, such as meditation, yoga, or deep breathing exercises, can help promote relaxation, improve mental well-being, and reduce anxiety levels.
- Reduces anxiety: Practicing stress-reducing techniques can help alleviate anxiety, improving overall mental well-being.
- Enhances coping mechanisms: Developing effective strategies to manage stress can enhance an individual's ability to cope with the challenges of Melas Syndrome.
- Promotes emotional well-being: Engaging in calming activities can contribute to emotional stability and a sense of inner peace.
Overall, individuals with Melas Syndrome can adopt various lifestyle changes to manage their condition effectively. Through a combination of a healthy diet, regular exercise customized to individual capabilities, adequate rest and sleep, stress management techniques, and seeking support from healthcare professionals, individuals with Melas Syndrome can optimize their well-being and improve their quality of life.
Supportive Therapies For Melas Syndrome
Melas Syndrome, also known as Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like episodes, is a rare genetic disorder that affects the mitochondria, the energy-producing units within cells. This condition primarily impacts the nervous system and can lead to various physical and neurological symptoms. While there is no cure for Melas Syndrome, supportive therapies play a crucial role in managing and improving the quality of life for individuals with this condition.
Supportive therapies for Melas Syndrome focus on addressing specific symptoms and optimizing overall well-being. One of the primary goals is to manage the energy deficit caused by mitochondrial dysfunction. This can be achieved through a combination of dietary adjustments, medications, and complementary therapies.
Dietary Modifications:
Following a well-balanced diet is essential for individuals with Melas Syndrome. A diet that is rich in nutrients and low in fat can help minimize the production of lactic acid, which can contribute to the symptoms of the condition. It is recommended to consult with a registered dietitian who can create a personalized meal plan that meets the individual's unique requirements.
Medications:
Several medications can be prescribed to address specific symptoms associated with Melas Syndrome. For instance, coenzyme Q10 supplements may help improve energy production in the cells. Idebenone, a synthetic analogue of coenzyme Q10, has shown promise in reducing the frequency and severity of stroke-like episodes.
Read the full article
0 notes
Text
Stone man syndrome

Stone Man Syndrome, also known as Fibrodysplasia Ossificans Progressiva (FOP), is an extremely rare genetic disorder that causes the body's soft tissues to progressively turn into bone. This condition affects approximately 1 in 2 million people worldwide and currently has no known cure. This blog post aims to shed light on the causes, symptoms, and diagnosis of Stone Man Syndrome, as well as explore the available treatment options, including physical therapy and surgical interventions. Additionally, we will discuss the impact of this condition on mobility, managing pain and discomfort, and the importance of supportive care and lifestyle adaptations. Furthermore, we will delve into the challenges faced by individuals living with Stone Man Syndrome and highlight the latest research, advances, and efforts in raising awareness and advocating for this rare disease.
What Is Stone Man Syndrome?
Stone Man Syndrome, also known as Fibrodysplasia Ossificans Progressiva (FOP), is a rare genetic disorder that causes the soft tissues of the body to gradually turn into bone. This condition is characterized by the formation of abnormal bone in muscles, ligaments, and tendons, restricting movement and causing various complications. Although it is a genetic disorder, Stone Man Syndrome is not inherited but rather occurs due to a spontaneous mutation in the body.
The exact cause of Stone Man Syndrome is still unknown. It is believed to be caused by a mutation in the ACVR1 gene, which plays a role in bone and muscle development. This genetic mutation leads to the production of an abnormal protein that triggers the formation of excess bone. The formation of bone in soft tissues occurs in response to injury, inflammation, or trauma, causing the body to mistakenly repair damaged tissues with bone instead of normal scar tissue.
Diagnosing Stone Man Syndrome can be challenging as it is a rare condition that often goes undiagnosed or misdiagnosed. Physical examination, medical history analysis, and imaging studies such as X-rays and CT scans are used to confirm the presence of abnormal bone growth and rule out other conditions with similar symptoms. Genetic testing may also be conducted to identify the specific mutation in the ACVR1 gene.
Causes Of Stone Man Syndrome
Stone Man Syndrome, also known as Fibrodysplasia Ossificans Progressiva (FOP), is a rare and debilitating genetic disorder that causes muscles, tendons, and ligaments to gradually turn into bone. This condition is caused by a mutation in the Activin A receptor type 1 (ACVR1) gene, which plays a crucial role in the development and maintenance of skeletal tissues. The mutation leads to the abnormal activation of bone morphogenetic proteins (BMPs), triggering the formation of extra bone outside the regular skeleton. It is estimated that approximately 1 in 2 million people worldwide are affected by Stone Man Syndrome, making it an extremely rare condition.
Although Stone Man Syndrome is a genetic disorder, it is important to note that it is not inherited in the traditional sense. Most cases of FOP occur sporadically, meaning there is no family history of the condition. The ACVR1 gene mutation usually arises spontaneously during early development, often before birth. Scientists are still investigating the exact cause of this genetic mutation and why it occurs in some individuals but not others.
In rare cases, Stone Man Syndrome can be inherited in an autosomal dominant pattern, meaning that one copy of the mutated gene is sufficient to cause the condition. Individuals with an affected parent have a 50% chance of inheriting the condition. Genetic testing can be conducted to identify the specific ACVR1 mutation and determine the likelihood of passing on the gene to future generations.
- In summary, Stone Man Syndrome is a rare genetic disorder caused by a mutation in the ACVR1 gene, leading to the abnormal formation of bone outside the regular skeleton. Most cases are sporadic, with no family history of the condition. In rare instances, FOP can be inherited in an autosomal dominant pattern. Further research is needed to fully understand the causes of Stone Man Syndrome and develop effective treatments and interventions for those affected.
Causes of Stone Man Syndrome:
- Mutation in the ACVR1 gene
- Abnormal activation of bone morphogenetic proteins (BMPs)
- Sporadic occurrence
- Autosomal dominant inheritance (rare cases)
Symptoms And Diagnosis Of Stone Man Syndrome
Stone Man Syndrome, also known as Fibrodysplasia Ossificans Progressiva (FOP), is an extremely rare genetic disorder characterized by the abnormal formation of bone in muscles, tendons, and other connective tissues. This condition causes progressive and irreversible disability as the body's soft tissues gradually turn into bone.
The symptoms of Stone Man Syndrome typically become noticeable during early childhood. One of the earliest signs is the development of hard nodules or lumps, called ossifications, in the neck, back, or shoulders. These ossifications can restrict joint movement and cause chronic pain and stiffness. Over time, the formation of extra bone can extend to other areas of the body, including the chest, hips, and limbs.
As Stone Man Syndrome progresses, individuals may experience limited mobility due to the fusion of joints caused by the excessive bone growth. The condition can also lead to the development of a characteristic stooped posture and difficulties with breathing and swallowing. Moreover, flare-ups triggered by trauma or inflammation can cause sudden and severe episodes of pain, often accompanied by swelling and warmth in the affected area.
Common Symptoms of Stone Man Syndrome:
- Painless ossifications in various parts of the body
- Restricted joint movement and stiffness
- Skeletal deformities, such as a curved spine
- Difficulty breathing and swallowing
- Progressive disability and loss of mobility
- Episodic flare-ups of pain and swelling
Diagnosing Stone Man Syndrome can be challenging due to its rarity and the absence of specific diagnostic tests. However, a thorough evaluation of an individual's medical history, physical examination, and radiographic imaging can help in assessing the presence of characteristic physical features and the pattern of abnormal bone formation.
In some cases, a genetic testing called DNA sequencing can be performed to identify specific mutations in the ACVR1 gene, which is associated with the development of Stone Man Syndrome. This genetic test can provide a definitive diagnosis and help differentiate FOP from other conditions that may have similar symptoms.
It is important for individuals suspected to have Stone Man Syndrome to consult with a team of medical professionals with expertise in the diagnosis and management of rare genetic disorders. Early diagnosis and intervention can help in implementing appropriate treatment strategies and providing support to manage the physical and emotional challenges associated with Stone Man Syndrome.
Impact Of Stone Man Syndrome On Mobility
Stone Man Syndrome, also known as Fibrodysplasia Ossificans Progressiva (FOP), is a rare and debilitating genetic disorder characterized by abnormal bone growth within muscles, tendons, and ligaments. This condition has a profound impact on the mobility and quality of life of affected individuals.
Firstly, Stone Man Syndrome greatly limits joint flexibility and range of motion. The continuous formation of bone in soft tissues progressively restricts movement, making even simple tasks such as walking or bending incredibly challenging. Over time, this condition may lead to complete immobilization, significantly affecting an individual's ability to carry out daily activities independently.
Furthermore, the formation of bone outside the skeleton also affects vital organs such as the lungs and heart, further impairing mobility. The constant bone growth can exert pressure on these organs, causing difficulties in breathing and affecting overall cardiovascular health. This not only hampers mobility but may also lead to other health complications.
- Moreover, the impact of Stone Man Syndrome on mobility extends beyond physical limitations. The psychological toll of living with a condition that progressively restricts movement can be immense. Individuals may experience feelings of frustration, isolation, and even depression as they face the challenges of navigating a world designed for able-bodied individuals.
Impact on Mobility
Effects on Daily Life
Restricted range of motion
Difficulty in performing basic movements and activities
Pressure on vital organs
Impaired breathing and cardiovascular health
Psychological impact
Feelings of frustration, isolation, and depression
Despite the challenges posed by Stone Man Syndrome, individuals with this condition often demonstrate remarkable resilience and determination. With proper support and adaptive devices, they strive to maintain independence and lead fulfilling lives.
In conclusion, Stone Man Syndrome exerts a significant impact on mobility, limiting range of motion, impairing organ function, and affecting an individual's psychological well-being. However, with advancements in medical research and increased awareness, there is hope for improved treatment options, increased support, and enhanced quality of life for individuals living with this rare condition.
Treatment Options For Stone Man Syndrome
Treatment Options for Stone Man Syndrome
Stone Man Syndrome, also known as Fibrodysplasia Ossificans Progressiva (FOP), is a rare genetic disorder that causes soft tissues, such as muscles and tendons, to progressively turn into bone. This abnormal bone growth can result in the loss of mobility and severely impact the quality of life for individuals with this condition. While there is currently no cure for Stone Man Syndrome, there are treatment options available to manage symptoms and improve the overall well-being of patients.
Non-Surgical Approaches:
One of the main goals of treating Stone Man Syndrome is to prevent the development of new bone formations. Non-surgical approaches, such as medication, can help in managing symptoms and slowing down the progression of the condition. Bisphosphonates, a type of medication used to treat osteoporosis, have shown some promise in reducing abnormal bone growth in individuals with FOP. These medications work by inhibiting the activity of bone-forming cells, slowing down the process of ossification. However, their effectiveness may vary from person to person.
Physical Therapy:
Physical therapy plays a crucial role in the management of Stone Man Syndrome. It can help maintain joint mobility, prevent contractures, and improve overall strength and flexibility. Range of motion exercises, stretching, and low-impact exercises tailored to the specific needs of the individual can help preserve joint function and minimize the impact of restricted mobility. Additionally, physical therapists can educate patients on proper body mechanics and provide supportive devices, such as braces or splints, to assist with mobility.
Surgical Interventions:
In severe cases of Stone Man Syndrome where there is significant impairment in mobility and quality of life, surgical interventions may be considered. However, surgery is often a last resort due to the risks associated with bone removal and the potential for abnormal bone regrowth. Surgical procedures, such as functional or reconstructive surgeries, aim to improve joint movement and alleviate pain. It is essential for individuals considering surgery to have a thorough evaluation by a team of specialists experienced in FOP to assess the potential risks and benefits.
In conclusion, while there is no cure for Stone Man Syndrome, a range of treatment options is available to manage symptoms and improve the quality of life for individuals with this rare condition. Non-surgical approaches such as medication can help slow down the progression of abnormal bone growth, while physical therapy and surgical interventions aim to prevent contractures, enhance mobility, and reduce pain. It is crucial for individuals with Stone Man Syndrome to work closely with a multidisciplinary healthcare team to personalize their treatment plan and ensure optimal care.
Physical Therapy For Stone Man Syndrome
Physical therapy plays a crucial role in the management and treatment of Stone Man Syndrome, also known as fibrodysplasia ossificans progressiva (FOP). FOP is an extremely rare genetic disorder characterized by the abnormal growth of bone in muscles, tendons, and ligaments. This progressive condition causes significant pain, disability, and immobility for those affected. However, physical therapy can help improve mobility, maintain joint flexibility, and alleviate discomfort in individuals living with Stone Man Syndrome.
One of the primary goals of physical therapy for Stone Man Syndrome is to preserve the range of motion in affected joints. As the abnormal bone growth restricts movement, physical therapists employ various techniques to stretch and strengthen muscles, thereby preventing further stiffness and immobility. The therapists may use gentle stretching exercises, manual therapy techniques, or assistive devices to help maintain or increase joint flexibility.
In addition to maintaining joint flexibility, physical therapy also emphasizes the importance of preserving functional mobility. Therapists work closely with individuals to develop customized exercise programs that target specific muscle groups and improve overall strength. These exercises are designed to accommodate the unique needs and limitations of each person with Stone Man Syndrome. By implementing a consistent physical therapy routine, individuals can enhance their ability to perform daily activities and maintain independence.
- Physical therapy for Stone Man Syndrome also includes the use of specialized equipment and devices. These aids play a crucial role in both treatment and daily living to enhance mobility and minimize discomfort. For instance, orthotic devices such as braces or splints can help support weakened muscles and maintain proper alignment. Wheelchairs or mobility scooters may be recommended in advanced stages of the condition to improve overall mobility and reduce strain on affected joints.
Treatment Techniques
Description
Range of motion exercises
Gentle stretches and movements to maintain joint flexibility.
Manual therapy
Hands-on techniques performed by the therapist to improve joint mobility and reduce muscle tightness.
Strengthening exercises
Targeted exercises to build muscle strength and maintain functional mobility.
Assistive devices
Supportive braces, splints, or mobility aids to enhance mobility and reduce discomfort.
Additionally, physical therapists are instrumental in providing education and support to individuals with Stone Man Syndrome and their caregivers. They help individuals understand their condition, teach proper body mechanics, and provide strategies for pain management and energy conservation. Furthermore, physical therapy can also address the emotional and psychological aspects of living with Stone Man Syndrome, as therapists offer a supportive environment and guide individuals in coping with the challenges associated with the condition.
In conclusion, physical therapy plays a vital role in enhancing mobility, managing pain, and improving the overall quality of life for individuals with Stone Man Syndrome. Through a combination of stretching exercises, strengthening routines, and the use of assistive devices, physical therapists empower individuals to maintain joint flexibility, preserve functional mobility, and adapt to their unique challenges. Furthermore, the guidance and support provided by physical therapists are invaluable in helping individuals and their families navigate the complexities of living with Stone Man Syndrome.
Surgical Interventions For Stone Man Syndrome
Surgical interventions play a crucial role in the management of Stone Man Syndrome, also known as Fibrodysplasia Ossificans Progressiva (FOP). FOP is an extremely rare genetic disorder characterized by the progressive formation of extra skeletal bone in muscles, tendons, and other connective tissues. This abnormal bone growth restricts movement and can lead to significant disability. Although there is no cure for FOP, surgical procedures can help alleviate pain, maintain joint mobility, and improve the quality of life for individuals living with this condition.
One of the main surgical interventions for Stone Man Syndrome is called heterotopic ossification (HO) excision. HO refers to the abnormal formation of bone in soft tissues. This procedure involves carefully removing the extra bone growth to relieve pain, prevent joint stiffness, and restore mobility. The excision is performed by an experienced orthopedic surgeon who is knowledgeable about the complexities of FOP and the potential risks associated with surgery.
In some cases, individuals with Stone Man Syndrome may require joint replacement surgeries to address severe joint damage caused by the abnormal bone growth. Joint replacement involves removing the damaged joint and replacing it with an artificial joint made of metal, plastic, or ceramic materials. This intervention can improve joint function and alleviate pain, allowing individuals with FOP to regain some degree of mobility and independence.
- Another surgical intervention option for Stone Man Syndrome is tendon release surgery. Tendon release involves surgically releasing a tight or contracted tendon, which may be caused by the formation of bone around the tendon. This procedure aims to improve joint movement and reduce pain by allowing the tendon to move more freely. Tendon release surgeries are typically performed on the affected area, such as the neck, elbows, wrists, or ankles, depending on the individual's specific needs.
Benefits of Surgical Interventions for Stone Man Syndrome
Risks and Considerations
Surgical interventions in Stone Man Syndrome can provide individuals with improved mobility, reduced pain, and enhanced quality of life.
While surgical interventions can be beneficial, there are several risks and considerations that need to be taken into account. The presence of abnormal bone formation can complicate surgical procedures and increase the risk of complications such as excessive bleeding, infection, or further bone growth.
Surgical interventions should be carefully planned and executed by a multidisciplinary team consisting of orthopedic surgeons, anesthesiologists, and other healthcare professionals who have experience in managing FOP.
Read the full article
0 notes
Text
MS syndrome

Multiple Sclerosis Syndrome (MS Syndrome) is a complex and chronic autoimmune disorder that affects the central nervous system. In this blog post, we will provide a comprehensive overview of MS Syndrome, including its definition, causes, symptoms, diagnosis, and various treatment options available. Furthermore, we will explore the significance of medication, lifestyle changes, physical therapy, and alternative therapies in managing this condition. Additionally, we will discuss strategies to combat MS Syndrome-related fatigue, the importance of support systems for individuals with this syndrome, and the latest research advancements in the field. Stay tuned for an informative and empowering read!
What Is Ms Syndrome?
What is MS Syndrome?
Multiple sclerosis (MS) syndrome is a chronic autoimmune disease that affects the central nervous system. It occurs when the immune system mistakenly attacks the protective covering of nerve fibers, known as myelin, in the brain and spinal cord. This damage disrupts the normal flow of electrical impulses and communication between the brain and the rest of the body. MS syndrome can cause a wide range of symptoms, which vary from person to person and can change over time.
Causes of MS Syndrome
The exact cause of MS syndrome is still unknown. However, researchers believe that a combination of genetic and environmental factors may contribute to its development. Some studies suggest that certain gene variations make individuals more susceptible to MS syndrome. Additionally, viral infections, vitamin D deficiency, and smoking are among the environmental factors that are believed to play a role in triggering the immune system and leading to MS syndrome in susceptible individuals.
Symptoms of MS Syndrome
The symptoms of MS syndrome can vary widely and may depend on the location and extent of the nerve damage. Some common symptoms include fatigue, difficulties with coordination and balance, muscle weakness or spasms, numbness or tingling sensations, problems with vision, and cognitive impairments. These symptoms can range from mild to severe, and they may come and go or persist over time. It is important to note that MS syndrome affects each individual differently, and no two cases are exactly alike.
- Unsteady gait
- Blurred or double vision
- Pain or tingling in certain areas of the body
- Weakness in the limbs
- Loss of coordination
- Problems with memory and thinking
- Difficulty speaking or slurred speech
Types of MS Syndrome
Description
Relapsing-Remitting MS (RRMS)
The most common type, characterized by clearly defined relapses followed by periods of partial or complete recovery.
Primary Progressive MS (PPMS)
A steady progression of symptoms without distinct relapses or remissions.
Secondary Progressive MS (SPMS)
Initially follows a relapsing-remitting course, but later transitions into a secondary progressive phase with a sustained worsening of symptoms.
Progressive-Relapsing MS (PRMS)
A rare form characterized by a steady progression of symptoms from the beginning, with occasional relapses and partial recoveries.
In conclusion, MS syndrome is a complex autoimmune disease that affects the central nervous system. While its exact cause remains unknown, a combination of genetic and environmental factors is believed to contribute to its development. The wide range of symptoms experienced by individuals with MS syndrome underscores the variability and unpredictability of the condition. Different types of MS syndrome exist, each with its own pattern of symptoms and progression. Early diagnosis and appropriate management can significantly improve the quality of life for individuals living with MS syndrome.
Causes Of Ms Syndrome
Multiple Sclerosis (MS) syndrome is a complex neurological disorder that affects the central nervous system. It occurs when the immune system mistakenly attacks the protective covering of nerve fibers, known as myelin, in the brain and spinal cord. The exact cause of MS syndrome is still unknown, but researchers believe that a combination of genetic and environmental factors plays a role in its development.
Genetic factors are believed to contribute to an individual's susceptibility to MS syndrome. Studies have shown that people with a family history of the disease are at a higher risk of developing it themselves. Certain genes, such as the HLA-DRB1 gene, have been identified as potential risk factors for MS syndrome. However, having these genes doesn't guarantee that one will develop the condition, indicating that other factors are involved in its causation.
Environmental factors are also thought to play a significant role in the development of MS syndrome. Research suggests that certain infections, such as the Epstein-Barr virus, can trigger an abnormal immune response, leading to the development of the condition. Other viral infections, including the human herpesvirus 6 and varicella-zoster virus, have also been associated with an increased risk of MS syndrome. Additionally, exposure to certain environmental toxins and vitamin D deficiency have been linked to a higher likelihood of developing the disease.
- Genetic factors: Genes such as HLA-DRB1 increase the risk of developing MS syndrome.
- Environmental factors: Infections like Epstein-Barr virus and exposure to toxins can trigger the condition.
- Other potential causes: Smoking, obesity, and certain hormonal imbalances may also contribute to the development of MS syndrome.
Genetic Factors
Environmental Factors
Other Potential Causes
HLA-DRB1 gene
Infections (Epstein-Barr virus, human herpesvirus 6, varicella-zoster virus)
Smoking
Exposure to toxins
Obesity
Vitamin D deficiency
Hormonal imbalances
It's important to note that while these factors are associated with an increased risk of developing MS syndrome, they do not guarantee the development of the disease. Many individuals with genetic or environmental risk factors never develop MS syndrome, highlighting the complexity of its causes. Further research is needed to fully understand the underlying mechanisms and potential triggers of this condition.
Symptoms Of Ms Syndrome
The symptoms of MS syndrome can vary greatly from person to person, depending on the location and severity of the nerve damage. Some of the most common symptoms include:
1. Fatigue: Fatigue is one of the most prevalent symptoms of MS syndrome. It can occur even after a good night's sleep and can significantly impact a person's daily activities and quality of life.
2. Numbness and Tingling: Many individuals with MS syndrome experience numbness or tingling sensations in their limbs, typically starting in the hands or feet. This symptom is often one of the first signs of the condition.
3. Weakness: Muscle weakness is another common symptom of MS syndrome. It may affect one side of the body or both sides, and individuals may experience difficulty with activities that require strength or coordination.
4. Balance and Coordination Problems: MS syndrome can also cause problems with balance and coordination, making it difficult for individuals to walk or perform precise movements. They may have a tendency to stumble or lose their balance easily.
5. Visual Disturbances: Many people with MS syndrome experience vision problems, such as double vision, blurred vision, or partial loss of vision. These symptoms can be temporary or long-lasting.
6. Cognitive Issues: Some individuals with MS syndrome may experience cognitive problems, including difficulties with memory, attention, and problem-solving. These symptoms can vary in severity and may impact a person's ability to work or engage in daily tasks.
7. Urinary and Bowel Problems: MS syndrome can affect the nerves that control the bladder and bowel, leading to issues such as urinary frequency, urgency, difficulty initiating or stopping urination, or constipation.
These symptoms can significantly impact a person's quality of life and require appropriate management and treatment. It is essential for individuals experiencing these symptoms to seek medical evaluation and guidance for proper diagnosis and personalized treatment plans.
Diagnosing Ms Syndrome
The process of diagnosing MS syndrome involves a combination of various methods and tests. Since there is no definitive test for MS, doctors rely on a combination of medical history, physical examination, and diagnostic tests to make a diagnosis. MS syndrome is a chronic autoimmune disease that affects the central nervous system. It occurs when the body's immune system mistakenly attacks the protective covering of nerve fibers in the brain and spinal cord.
During the initial consultation, the doctor will ask the patient about their symptoms and medical history. This information helps in assessing the duration, frequency, and severity of symptoms. It is important for individuals to provide accurate details about their symptoms, as this can significantly aid the diagnostic process. The doctor may also inquire about any family history of MS syndrome or other autoimmune diseases.
After gathering the necessary information, the doctor will conduct a physical examination to assess the patient's abilities and look for any signs of MS syndrome. They will check for specific neurological signs, such as muscle weakness, coordination problems, and changes in reflexes. The presence of these signs can help the doctor determine if further testing is required.
-
One of the common diagnostic tests used for MS syndrome is magnetic resonance imaging (MRI). This imaging technique uses powerful magnets and radio waves to produce detailed images of the brain and spinal cord. In individuals with MS syndrome, MRI scans may reveal the presence of lesions or areas of inflammation in the nervous system. These abnormalities can help confirm the diagnosis and classify the type of MS syndrome.
Another crucial test for diagnosing MS syndrome is a lumbar puncture, also known as a spinal tap. During this procedure, a small needle is inserted into the lower back to collect a sample of cerebrospinal fluid (CSF). The CSF is then analyzed for the presence of certain markers, such as elevated levels of antibodies or immune cells. These markers can indicate inflammation in the central nervous system, supporting the diagnosis of MS syndrome.
In some cases, doctors may also order evoked potential tests to evaluate the functioning of the nerves. These tests involve stimulating specific sensory pathways and recording the electrical signals produced by the nerves. Abnormal responses in the evoked potential tests can suggest the presence of nerve damage, which is a characteristic feature of MS syndrome.
Treatment Options For Ms Syndrome
Multiple Sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system. It occurs when the immune system mistakenly attacks the protective covering of nerve fibers, resulting in communication problems between the brain and the rest of the body. While there is currently no cure for MS, there are various treatment options available that can help manage the symptoms and slow down the progression of the disease.
One of the common treatment options for MS syndrome is medication. There are several types of medication that can be prescribed for managing different aspects of the disease. Disease-modifying therapies (DMTs) are often prescribed to modify the immune system's response and reduce inflammation. These medications can help slow down the progression of MS and reduce the frequency and severity of relapses.
In addition to DMTs, symptomatic treatments can also be prescribed to manage specific symptoms experienced by individuals with MS syndrome. For example, medications such as muscle relaxants can help alleviate muscle stiffness and spasms. Corticosteroids may be used to reduce inflammation during relapses. Pain medications can also be prescribed to manage chronic pain associated with MS syndrome.
In addition to medication, lifestyle changes play a crucial role in managing MS syndrome. A balanced and nutritious diet, regular exercise, and stress management techniques can help improve overall well-being and reduce the impact of MS symptoms. It is advised to consult with healthcare professionals and nutritionists to develop a personalized diet and exercise plan tailored to one's specific needs.
Treatment Options:
Benefits:
Disease-Modifying Therapies
Slow down disease progression and reduce relapses
Symptomatic Treatments
Manage specific symptoms such as muscle stiffness and pain
Lifestyle Changes
Improve overall well-being and reduce the impact of symptoms
In some cases, physical therapy can also be beneficial for individuals with MS syndrome. Physical therapists can develop personalized exercise programs and teach techniques to improve mobility, balance, and strength. These exercises can help individuals maintain their independence and improve their quality of life.
Alternative therapies, such as acupuncture, yoga, and meditation, are also used by some individuals to manage the symptoms of MS syndrome. While these therapies may not have scientific evidence to support their effectiveness, some people find them helpful in reducing stress and improving overall well-being.
Managing MS syndrome-related fatigue is another important aspect of treatment. Fatigue is a common symptom experienced by individuals with MS, and it can significantly impact their daily lives. Strategies such as prioritizing activities, conserving energy, and using assistive devices can help manage fatigue and improve energy levels.
It is crucial for individuals living with MS syndrome to have a strong support system. Family, friends, support groups, and healthcare professionals can provide emotional support, share experiences, and offer guidance through the challenges of living with the disease. Connecting with others who understand the unique challenges of MS syndrome can be empowering and reassuring.
Lastly, staying informed about the latest research and advancements in MS syndrome is essential. New treatments and therapies are continually being developed, and staying up to date can help individuals make informed decisions about their treatment and management plan. It is recommended to consult with healthcare professionals and follow trusted sources for the latest information.
Role Of Medication In Managing Ms Syndrome
The role of medication in managing MS syndrome is crucial in providing relief from symptoms and slowing down the progression of the disease. MS syndrome, also known as multiple sclerosis, is a chronic autoimmune condition that affects the central nervous system. It occurs when the immune system mistakenly attacks the protective covering of nerve fibers, causing communication problems between the brain and the rest of the body.
One of the main goals of medication for MS syndrome is to reduce inflammation and control the immune system response. This can help in managing symptoms such as fatigue, muscle weakness, balance problems, and cognitive issues. Several different types of medications are used in the treatment of MS syndrome, including:
- Disease-modifying therapies (DMTs): These medications work by targeting the immune system to reduce the frequency and severity of relapses and slow down the progression of the disease. They can help in reducing inflammation and preventing further damage to the nerve fibers.
- Symptom management medications: These medications are used to alleviate specific symptoms of MS syndrome. For example, corticosteroids may be prescribed to reduce inflammation during relapses, while muscle relaxants can help with spasticity and muscle stiffness.
- Pain medications: MS syndrome can cause chronic pain, and medications like nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids may be prescribed to manage pain effectively.
Medication Types
Example Medications
Disease-modifying therapies (DMTs)
Interferon beta-1a (Avonex), Fingolimod (Gilenya)
Symptom management medications
Methylprednisolone (Medrol), Baclofen (Lioresal)
Pain medications
Ibuprofen (Advil), Oxycodone (OxyContin)
It is important to note that medication should always be prescribed and monitored by a healthcare professional familiar with MS syndrome. Each individual's treatment plan may vary depending on the specific symptoms, disease progression, and overall health. Regular follow-ups with healthcare providers are necessary to assess the effectiveness of medications and make any necessary adjustments.
While medication plays a vital role in managing MS syndrome, it is not the only aspect of treatment. Lifestyle modifications, physical therapy, and alternative therapies can also complement medication to enhance overall well-being and symptom management. It is essential for individuals with MS syndrome to work closely with their healthcare team to develop a comprehensive treatment plan that addresses their specific needs and goals.
Lifestyle Changes For Ms Syndrome Management
Living with multiple sclerosis (MS) syndrome can be challenging, but with the right lifestyle changes, you can effectively manage the condition and improve your overall well-being. Lifestyle modifications are an essential part of MS syndrome management, as they can help reduce symptoms, slow down the progression of the disease, and enhance quality of life. In this article, we will explore some important lifestyle changes that can make a positive impact on managing MS syndrome.
1. Balanced Diet:
Eating a balanced and nutritious diet is crucial for individuals with MS syndrome. A well-rounded diet can support overall health and provide the body with the necessary nutrients to combat the disease. Including fruits, vegetables, whole grains, lean proteins, and healthy fats in your diet is recommended. Additionally, it is important to limit processed foods, sugary snacks, and saturated fats. Maintaining a healthy weight is also beneficial for managing MS syndrome.
2. Regular Exercise:
Engaging in regular exercise can have numerous benefits for individuals with MS syndrome. Exercise can help improve strength, flexibility, and mobility, reduce fatigue, and enhance mood. It is important to consult with a healthcare professional or physical therapist to develop an exercise program tailored to your abilities and preferences. Low-impact exercises such as swimming, yoga, and walking are often recommended for individuals with MS syndrome.
3.
Read the full article
0 notes
Text
Fanconi syndrome

Fanconi Syndrome is a rare genetic disorder that affects the proper functioning of the kidneys. In this blog post, we will explore the various aspects of Fanconi Syndrome, including its causes, symptoms, diagnosis, and treatment options. We will also discuss dietary recommendations, managing electrolyte imbalances, potential complications, and the long-term outlook for individuals living with this condition. Furthermore, we will delve into the genetic factors and inheritance patterns of Fanconi Syndrome and highlight any recent research advancements in understanding this disorder. Lastly, we will provide information regarding support and resources available for individuals and their families affected by Fanconi Syndrome.
What Is Fanconi Syndrome?
Fanconi syndrome is a rare disorder that affects the functioning of the kidneys. It is named after a Swiss physician named Guido Fanconi, who first described the condition in the 1930s. Fanconi syndrome is characterized by the inability of the kidneys to properly reabsorb essential substances such as glucose, amino acids, electrolytes, and bicarbonate. As a result, these substances are lost in the urine, leading to various health problems.
The causes of Fanconi syndrome can vary. In some cases, it may be inherited as a genetic disorder, while in others it may be acquired due to certain medications, toxins, or underlying health conditions. Some medications known to cause Fanconi syndrome include certain antibiotics, chemotherapy drugs, and antiretroviral medications used in the treatment of HIV. Additionally, various metabolic disorders, such as cystinosis or Wilson's disease, can also result in Fanconi syndrome.
The symptoms of Fanconi syndrome can be diverse and may vary depending on the underlying cause. However, some common symptoms include excessive urination (polyuria), excessive thirst (polydipsia), poor growth and development in children, bone problems, such as rickets or osteomalacia, and electrolyte imbalances. It is important to note that these symptoms can be non-specific and may overlap with other conditions, making an accurate diagnosis crucial.
Causes Of Fanconi Syndrome
Fanconi Syndrome is a rare disorder that affects the kidneys and disrupts their ability to reabsorb essential substances such as glucose, amino acids, and electrolytes. This condition can be caused by a variety of factors, both genetic and acquired. One of the known genetic causes of Fanconi Syndrome is cystinosis, a rare metabolic disorder that leads to the accumulation of cystine in various organs, including the kidneys. Other genetic causes include mutations in genes responsible for the function of proximal renal tubular cells.
Acquired causes of Fanconi Syndrome can result from certain medications, toxins, or underlying medical conditions. For example, the use of outdated tetracycline antibiotics, aminoglycosides, or antiretroviral drugs can lead to the development of Fanconi Syndrome. Additionally, exposure to heavy metals such as lead or cadmium, as well as certain metabolic disorders like Wilson disease and glycogen storage disease, can contribute to the development of this condition.
Primary Causes:
Secondary Causes:
- Cystinosis
- Mutations in proximal renal tubular cell genes
- Use of certain medications (tetracycline antibiotics, aminoglycosides, antiretroviral drugs)
- Exposure to heavy metals (lead, cadmium)
- Metabolic disorders (Wilson disease, glycogen storage disease)
In some cases, the exact cause of Fanconi Syndrome may remain unknown. This is referred to as idiopathic Fanconi Syndrome. It is believed that both genetic and environmental factors may play a role in the development of this condition.
Understanding the underlying causes of Fanconi Syndrome is crucial in diagnosing and managing the condition effectively. Identifying the specific cause can help guide treatment options and provide valuable information for genetic counseling in cases where the condition is inherited. Further research advancements in this field are essential to improve our understanding of Fanconi Syndrome and develop targeted therapies for those affected.
Symptoms Of Fanconi Syndrome
The symptoms of Fanconi syndrome can vary depending on the underlying cause and severity of the condition. However, there are some common signs that individuals with Fanconi syndrome may experience. One of the main symptoms is excessive thirst and frequent urination, known as polyuria and polydipsia. This occurs due to the impaired ability of the kidneys to reabsorb water, leading to an increased urine output.
Another hallmark symptom of Fanconi syndrome is a loss of important nutrients in the urine. This can result in a variety of complications such as electrolyte imbalances, vitamin deficiencies, and growth retardation in children. Some specific nutrients that may be excreted in the urine include glucose, amino acids, phosphate, and bicarbonate.
In addition to polyuria and nutrient loss, individuals with Fanconi syndrome may also experience other symptoms such as bone pain, muscle weakness, and fatigue. These symptoms can be attributed to the impaired absorption of calcium and phosphate, which are essential for bone health and muscle function.
Diagnosis Of Fanconi Syndrome
Fanconi syndrome is a rare disorder that affects the functioning of the kidneys. It is characterized by the inability of the kidneys to properly reabsorb certain substances, leading to their excessive excretion in the urine. Diagnosing Fanconi syndrome can be challenging, as its symptoms may vary and overlap with other conditions. However, there are several diagnostic tests that can aid in confirming the presence of Fanconi syndrome.
One of the first steps in diagnosing Fanconi syndrome is a thorough medical history and physical examination. The healthcare provider will ask about the patient's symptoms, family history, and any medications or toxins the patient may have been exposed to. The physical examination may reveal specific signs associated with Fanconi syndrome, such as growth retardation, bone abnormalities, or muscle weakness.
After the initial evaluation, specific laboratory tests are usually conducted to further assess kidney function and identify any imbalances in the levels of various substances in the blood and urine. Urine tests are crucial in diagnosing Fanconi syndrome, as they can detect the presence of excessive amounts of specific substances, such as glucose, amino acids, phosphate, and bicarbonate, in the urine. A blood test may also be performed to measure the levels of electrolytes, such as potassium, in the blood, as imbalances in electrolytes are common in individuals with Fanconi syndrome.
If initial tests suggest the presence of Fanconi syndrome, additional tests may be ordered to determine the underlying cause. Genetic testing can be helpful in identifying any genetic mutations or abnormalities that may be responsible for the development of Fanconi syndrome. Imaging tests, such as kidney ultrasound or renal biopsy, may also be conducted to assess the structure of the kidneys and any possible anatomical abnormalities.
In conclusion, the diagnosis of Fanconi syndrome involves a combination of medical history, physical examination, and laboratory tests. This rare kidney disorder requires careful evaluation to differentiate it from other conditions with similar symptoms. Early diagnosis is crucial in order to initiate appropriate treatment and management strategies for individuals affected by Fanconi syndrome.
Treatment Options For Fanconi Syndrome
Fanconi syndrome is a rare disorder that affects the proximal tubules in the kidneys, leading to the improper reabsorption of certain substances. While there is no cure for Fanconi syndrome, treatment options are available to manage the symptoms and prevent complications. The primary goal of treatment is to restore the normal functioning of the kidneys and maintain electrolyte balance in the body.
One of the key treatment approaches for Fanconi syndrome is the use of specific medications. Phosphate and citrate supplements are often prescribed to counteract the loss of essential electrolytes through the urine. These supplements help in maintaining the balance of these substances in the body and prevent further complications.
In addition to medication, it is crucial for individuals with Fanconi syndrome to make dietary modifications. A dietitian can provide personalized dietary recommendations based on the individual's specific needs and preferences. Foods rich in essential nutrients and electrolytes can help replenish the lost nutrients in the body and support overall health.
Furthermore, regular monitoring of kidney function is essential in the management of Fanconi syndrome. This includes regular urine and blood tests to assess the levels of various substances and electrolytes in the body. These tests help in adjusting the treatment plan and ensuring optimal management of the condition.
- Educational resources and support groups can also play a significant role in the treatment and management of Fanconi syndrome. Connecting with others who have similar experiences can provide emotional support and valuable information. Additionally, staying informed about the latest research advancements in understanding Fanconi syndrome can help individuals make informed decisions about their treatment options.
Potential Complications of Fanconi Syndrome
Long-Term Outlook for Individuals with Fanconi Syndrome
Fanconi syndrome can lead to several potential complications if left untreated. These may include electrolyte imbalances, metabolic bone disease, growth disturbances, and renal insufficiency. It is important for individuals with Fanconi syndrome to receive timely treatment to prevent these complications and maintain their quality of life.
The long-term outlook for individuals with Fanconi syndrome varies depending on the underlying cause and treatment effectiveness. With proper management and regular medical care, many individuals with Fanconi syndrome live fulfilling lives. However, it is crucial to prioritize ongoing medical follow-up and adhere to the recommended treatment plan to ensure optimal health outcomes.
In conclusion, while there is no cure for Fanconi syndrome, treatment options are available to manage the condition and improve the quality of life for affected individuals. By combining medication, dietary modifications, regular monitoring, and seeking support from educational resources and support groups, individuals with Fanconi syndrome can effectively manage their symptoms and prevent complications. It is important for individuals with Fanconi syndrome to work closely with their healthcare providers to develop an individualized treatment plan that addresses their specific needs and goals.
Dietary Recommendations For Fanconi Syndrome
Fanconi syndrome is a rare disorder that affects the kidneys' ability to reabsorb essential nutrients and electrolytes. It is characterized by the loss of vital nutrients such as glucose, amino acids, phosphate, and bicarbonate in the urine. Individuals with Fanconi syndrome require specific dietary recommendations to manage their condition and support their overall health.
1. Minimize Sodium Intake: Individuals with Fanconi syndrome may be prone to developing electrolyte imbalances, including low blood sodium levels. It is essential to limit sodium intake by avoiding processed and salty foods. Instead, opt for fresh fruits, vegetables, and whole grains that are naturally low in sodium.
2. Increase Fluid Intake: Staying adequately hydrated is crucial for individuals with Fanconi syndrome. Drinking sufficient water helps flush out excessive amounts of electrolytes and maintain overall kidney function. It is recommended to consume at least 8-10 cups of fluids daily, including water, herbal teas, and low-sodium broths.
3. Consume Balanced Meals: A well-balanced diet is essential for individuals with Fanconi syndrome to ensure they receive the necessary nutrients. Including a mix of carbohydrates, proteins, and healthy fats in each meal can help provide energy and support overall health. However, it is important to consult a healthcare professional or a registered dietitian to determine the appropriate macronutrient ratios for individual needs.
4. Supplement with Vitamins and Minerals: Due to the impaired reabsorption of essential nutrients, individuals with Fanconi syndrome may require additional supplementation to meet their daily vitamin and mineral requirements. Supplements such as vitamin D, phosphate, and bicarbonate may be recommended to manage specific deficiencies. However, it is crucial to consult with a healthcare professional before starting any supplementation regimen.
5. Monitor Protein Intake: While protein is essential for overall health, individuals with Fanconi syndrome may need to regulate their protein intake to prevent excessive amino acid loss. Consulting with a healthcare professional or a registered dietitian can help determine the appropriate protein intake based on individual needs.
6. Limit Phosphorus-Rich Foods: Fanconi syndrome can lead to phosphate wasting, resulting in low blood phosphate levels. It is important to limit the consumption of phosphorus-rich foods such as dairy products, red meat, and processed foods. Instead, opt for lower phosphorus alternatives like poultry, fish, whole grains, and fresh fruits and vegetables.
Foods to Limit
Lower Phosphorus Alternatives
Dairy products
Poultry
Red meat
Fish
Processed foods
Whole grains
Overall, individuals with Fanconi syndrome should work closely with healthcare professionals to develop a personalized dietary plan that addresses their specific needs. Regular monitoring of blood tests and consulting with a registered dietitian can help ensure adequate nutrient intake and optimize overall health.
Managing Electrolyte Imbalances In Fanconi Syndrome
ELECTROLYTE IMBALANCES IN FANCONI SYNDROME
Fanconi syndrome is a rare disorder that affects the proximal renal tubules in the kidneys, leading to various imbalances in electrolytes and other important substances in the body. One of the key challenges in managing Fanconi syndrome is addressing these electrolyte imbalances, which can have significant implications for the overall health and well-being of individuals with this condition.
In Fanconi syndrome, the malfunctioning renal tubules result in the excessive loss of important substances such as glucose, amino acids, phosphate, bicarbonate, and electrolytes like sodium, potassium, and magnesium through urine. This disruption in the normal reabsorption process can lead to electrolyte imbalances, which can manifest in various ways.
One of the primary concerns in managing electrolyte imbalances is ensuring adequate levels of sodium and potassium. Sodium, an essential electrolyte, plays a crucial role in maintaining fluid balance and transmitting nerve impulses, while potassium is vital for proper muscle and nerve function. Individuals with Fanconi syndrome may experience low levels of these electrolytes, leading to symptoms such as muscle weakness, fatigue, irregular heartbeat, and even paralysis in severe cases. Therefore, it is essential to monitor and replenish these electrolytes regularly through dietary modifications or supplements.
In addition to sodium and potassium, magnesium levels also need close attention in individuals with Fanconi syndrome. Magnesium is involved in numerous bodily processes, including protein synthesis, muscle relaxation, and nerve function. Low magnesium levels, known as hypomagnesemia, can be particularly problematic in Fanconi syndrome and may contribute to muscle cramps, weakness, abnormal heart rhythms, and fatigue. Therefore, careful management of magnesium levels through dietary adjustments or supplements becomes crucial in maintaining electrolyte balance.
Another electrolyte that requires careful monitoring is phosphate. Phosphate is essential for energy production, bone health, and various cellular functions. In Fanconi syndrome, excessive phosphate excretion leads to low levels of this electrolyte, known as hypophosphatemia. This condition can cause muscle weakness, bone pain, and even impair growth and development in children. Regular evaluation of phosphate levels and appropriate supplementation or dietary modifications can help manage this electrolyte imbalance effectively.
In conclusion, managing electrolyte imbalances is a critical aspect of the comprehensive care for individuals with Fanconi syndrome. Regular monitoring of sodium, potassium, magnesium, and phosphate levels, along with appropriate dietary adjustments and supplementation, can help maintain electrolyte balance and improve the quality of life for those living with this rare disorder.
Potential Complications Of Fanconi Syndrome
Fanconi Syndrome is a rare kidney disorder that affects the proximal tubules, leading to the improper reabsorption of essential substances, such as glucose, amino acids, phosphate, and bicarbonate. This impairment in kidney function can result in various complications that can significantly impact an individual's health and well-being.
One of the potential complications of Fanconi Syndrome is electrolyte imbalances. Since the proximal tubules play a crucial role in maintaining the balance of electrolytes in the body, their dysfunction can disrupt this delicate equilibrium. This can lead to abnormally low levels of potassium, magnesium, and phosphate, causing muscle weakness, cramps, and irregular heart rhythms.
Furthermore, individuals with Fanconi Syndrome may experience growth and developmental issues. The impaired reabsorption of essential nutrients, such as amino acids, can affect the body's ability to grow and develop properly, especially in children. This can result in stunted growth, delayed puberty, and skeletal abnormalities.
- Another significant complication associated with Fanconi Syndrome is metabolic acidosis. Due to the failure of renal tubules to reabsorb bicarbonate, there is an excess loss of bicarbonate in urine, leading to an acidic pH imbalance in the blood. Metabolic acidosis can cause symptoms such as fatigue, rapid breathing, and confusion.
- Fanconi Syndrome is also linked to an increased risk of bone abnormalities. The excessive loss of phosphate in the urine can lead to low levels of this essential mineral in the body, resulting in weakened bones and an increased susceptibility to fractures. Additionally, decreased levels of vitamin D, another consequence of Fanconi Syndrome, further exacerbate bone health issues.
Complications
Description
Renal Failure
In severe cases, Fanconi Syndrome can progress to chronic kidney disease and eventually renal failure.
Read the full article
0 notes
Text
Snapping hip syndrome
Snapping Hip Syndrome is a condition characterized by a snapping or clicking sensation in the hip joint during movement. It can be a source of pain and discomfort for individuals, impacting their ability to participate in daily activities or athletic endeavors. In this blog post, we will explore the causes, types, signs, and symptoms of Snapping Hip Syndrome. Additionally, we will delve into the various treatment options available, including conservative management techniques, physical therapy, and surgical interventions for relief. We will also discuss the recovery and rehabilitation process, as well as tips for preventing this condition. Lastly, we will address when it is necessary to seek medical help for Snapping Hip Syndrome. So, if you're curious about this condition and how to manage it effectively, keep reading!
What Is Snapping Hip Syndrome?
Snapping hip syndrome is a condition that causes a snapping or popping sensation in the hip joint during certain movements. It is also referred to as coxa saltans, and can be quite bothersome for individuals who experience it. This condition primarily affects athletes and dancers, but it can also occur in non-athletic individuals. Snapping hip syndrome can be classified into three main types: external, internal, and intra-articular.
External snapping hip syndrome occurs when a tendon on the outside of the hip joint, known as the iliotibial band, snaps over the outside of the thigh bone. This can cause a snapping or popping sensation with hip flexion and extension movements. On the other hand, internal snapping hip syndrome involves a tendon called the iliopsoas tendon snapping over the front of the hip joint. Individuals with this type of snapping hip syndrome may experience snapping or clicking during hip flexion or external rotation movements.
Intra-articular snapping hip syndrome is the least common type and involves structures inside the hip joint, such as torn cartilage or loose bodies, causing snapping or catching sensations. This type of snapping hip syndrome usually requires surgical intervention to correct the underlying issue. Snapping hip syndrome can be caused by a variety of factors, including muscle imbalances, overuse, tight muscles or tendons, structural abnormalities in the hip joint, or previous hip injuries.
Causes Of Snapping Hip Syndrome
Snapping Hip Syndrome, also known as coxa saltans, is a condition characterized by a snapping sensation or popping sound in the hip during movement. This can occur in individuals of all ages and activity levels, from athletes to sedentary individuals. While the exact cause of this syndrome is not always clear, there are several possible factors that may contribute to its development.
One of the primary causes of Snapping Hip Syndrome is related to the movement of the tendons and muscles around the hip joint. In some cases, the iliopsoas tendon, which runs from the pelvis to the thigh bone, may become tight or inflamed. This can cause it to rub against the pelvic bones, resulting in the characteristic snapping sensation. Other muscles and tendons in the hip region, such as the gluteus maximus and iliotibial band, can also contribute to the snapping sound when they move over bony prominences.
In certain cases, structural abnormalities in the hip joint can also lead to Snapping Hip Syndrome. For example, some individuals have a hip socket that is shallow or abnormally shaped, which can cause instability and increased friction during movement. It is also possible for bony formations called "bone spurs" to develop in the hip joint, further contributing to the snapping sensation.
Types Of Snapping Hip Syndrome
Snapping hip syndrome, also known as dancer's hip, is a condition in which a person experiences a snapping or popping sensation in their hip joint during movement. This condition can be classified into three main types based on the specific structures involved: internal snapping hip, external snapping hip, and intra-articular snapping hip.
Firstly, let's discuss internal snapping hip syndrome. This type occurs when the iliopsoas tendon, which runs from the lower part of the spine to the front of the thigh bone, slides over the bony prominence of the hip joint called the iliopectineal eminence. This movement can cause a snapping or clicking sensation and is commonly seen in athletes who involve repeated hip flexion and extension, such as dancers and runners.
Secondly, external snapping hip syndrome involves the iliotibial band (IT band), a thick band of connective tissue that runs along the outside of the hip, knee, and thigh. When the IT band slides back and forth over the prominent part of the thigh bone, known as the greater trochanter, it can produce a snapping sensation. This type of snapping hip syndrome is frequently observed in individuals who engage in activities that require repetitive hip motion.
Lastly, intra-articular snapping hip syndrome occurs within the joint itself. This type involves structures such as the labrum, which is a ring of cartilage that helps stabilize the hip joint, or loose bodies (small fragments of bone or soft tissue) within the joint space. When these structures become irritated or displaced, they can cause snapping or catching sensations during hip movement.
- Table:
Type of Snapping Hip Syndrome
Affected Structures
Internal Snapping Hip
Iliopsoas tendon
External Snapping Hip
Iliotibial band (IT band)
Intra-articular Snapping Hip
Labrum or loose bodies
If you experience a snapping sensation in your hip joint, it is essential to consult a healthcare professional for an accurate diagnosis. Understanding the different types of snapping hip syndrome can help you and your healthcare provider determine the most appropriate treatment options for your specific condition.
Signs And Symptoms
Snapping hip syndrome is a condition characterized by a snapping sensation or sound in the hip joint during movement. It is most commonly observed in athletes and dancers, but can occur in anyone. The snapping sensation is often painless and may be accompanied by a popping or clicking noise. Individuals with snapping hip syndrome may also experience discomfort or pain in the hip, groin, or pelvis region. The symptoms may worsen with increased physical activity or prolonged periods of sitting or standing.
One of the key indicators of snapping hip syndrome is the presence of audible snapping or clicking sounds in the hip joint. These sounds are caused by the movement of tendons or muscles over bony structures in the hip joint. External snapping hip syndrome occurs when the iliotibial band or gluteus maximus tendon snaps over the bony prominence of the greater trochanter. Internal snapping hip syndrome, on the other hand, is characterized by the iliopsoas tendon snapping over the iliopectineal eminence or the femoral head. Both types of snapping hip syndrome can cause discomfort and may limit hip mobility.
In addition to the snapping sensation and sound, individuals with snapping hip syndrome may experience pain or discomfort in the hip, groin, or pelvis area. This pain can range from mild to severe and may be intermittent or constant. It is often exacerbated by activities that involve repetitive hip movements, such as walking, running, or climbing stairs. In some cases, the pain may radiate down the thigh or buttock. Swelling, tenderness, or redness may also be present in the affected area.
Diagnosing Snapping Hip Syndrome
Snapping hip syndrome is a condition that causes a snapping sensation or sound in the hip joint when it is moved. This condition can be quite uncomfortable and may affect athletes, dancers, or individuals who perform repetitive hip movements. To properly diagnose snapping hip syndrome, it is important to understand the potential causes and types of this condition.
There are several methods used by healthcare professionals to diagnose snapping hip syndrome. Firstly, a thorough medical history will be taken to gather information about the symptoms experienced, any previous injuries, or activities that may have contributed to the condition. During the physical examination, the healthcare provider will perform various tests to evaluate the range of motion, strength, and flexibility of the hip joint. This may include observing and palpating the hip area while asking the patient to perform certain movements or positions. Additionally, imaging tests such as X-rays, ultrasound, or MRI scans may be ordered to further assess the hip joint and surrounding structures.
In addition to the physical examination and imaging tests, a diagnostic injection may be utilized. This involves injecting a local anesthetic into the hip joint to numb the area and temporarily reduce symptoms. If the snapping sensation and pain dissipate after the injection, it confirms that the symptoms are indeed originating from the hip joint. This diagnostic injection can be an effective method to confirm the diagnosis of snapping hip syndrome.
Once a diagnosis of snapping hip syndrome is made, it is important to determine the specific type of the condition. The two main types are internal snapping hip syndrome and external snapping hip syndrome. Internal snapping hip syndrome occurs when a tendon or muscle rubs over a bony prominence inside the hip joint. On the other hand, external snapping hip syndrome is characterized by the snapping sensation caused by the iliotibial band or the gluteus maximus tendon moving over the greater trochanter, which is a bony prominence on the outside of the hip. Differentiating between these two types is crucial for developing an appropriate treatment plan.
Treatment Options Available
Snapping hip syndrome is a condition characterized by a snapping or popping sensation in the hip joint during movement. It can occur in athletes, dancers, and individuals who participate in repetitive and vigorous activities. The condition is caused by the movement of a tendon or muscle over a bony structure in the hip, resulting in the snapping sensation. Snapping hip syndrome can be painful and may affect daily activities and athletic performance.
There are several treatment options available for individuals with snapping hip syndrome. Conservative management techniques are often the first line of treatment and involve rest, activity modification, and the use of anti-inflammatory medications to reduce pain and inflammation. Physical therapy is another non-invasive treatment option that aims to strengthen the muscles around the hip joint, improve flexibility, and correct any biomechanical imbalances that may be contributing to the condition.
In cases where conservative management does not provide sufficient relief, surgical interventions may be considered. The specific surgical procedure will depend on the underlying cause of the snapping hip syndrome. For example, if the snapping is caused by a tendon or muscle catching on a bony structure, a surgical release may be performed to free the tendon or muscle. In some cases, the surgeon may also need to address any associated tissue damage or correct structural abnormalities in the hip joint.
- Recovery and rehabilitation following treatment for snapping hip syndrome can vary depending on the severity of the condition and the type of treatment received. After undergoing surgery, individuals will typically need to undergo a period of rest and rehabilitation to allow for healing and to regain strength and range of motion in the hip joint. Physical therapy exercises and stretches may be prescribed to aid in the recovery process.
Preventing Snapping Hip Syndrome
When to Seek Medical Help
Preventing snapping hip syndrome involves taking certain precautions and adopting healthy habits. It is important to warm up adequately before engaging in physical activities and to gradually increase the intensity and duration of exercise sessions. Maintaining proper posture and technique during activities and avoiding overuse or repetitive motions can also help to prevent the development of snapping hip syndrome. Additionally, individuals should listen to their bodies and refrain from pushing through pain or discomfort.
It is advisable to seek medical help if you experience persistent or severe pain in the hip joint, difficulty walking or performing daily activities, or if you notice a loss of strength or range of motion in the hip. A medical professional will be able to properly diagnose the underlying cause of the symptoms and recommend appropriate treatment options. Early intervention is key in managing snapping hip syndrome and preventing further complications.
Conservative Management Techniques
Conservative Management Techniques for Snapping Hip Syndrome
Snapping hip syndrome is a condition characterized by a snapping or popping sensation in the hip joint. It occurs when the muscles or tendons in the hip region move over a bony prominence, causing a snapping sound. While there are various treatment options available, including medications and surgical interventions, many individuals prefer conservative management techniques to alleviate the symptoms and improve their hip function.
Conservative management techniques for snapping hip syndrome focus on non-invasive approaches that can be implemented at home or under the guidance of a healthcare professional. These techniques aim to reduce pain, inflammation, and improve flexibility in the hip joint. One popular approach is the use of physical therapy exercises specifically designed to stretch and strengthen the muscles around the hip. These exercises can help correct any muscle imbalances and improve overall joint stability.
In addition to physical therapy, modifying activities that aggravate the snapping hip syndrome can significantly help in managing the condition conservatively. Avoiding repetitive movements or positions that worsen the snapping sensation, such as excessive squatting or prolonged sitting, can provide relief. Similarly, using assistive devices like crutches or canes can help offload the hip joint and reduce pressure, allowing for better healing and reduced snapping.
Another conservative management technique that individuals may find beneficial is the application of heat or ice to the affected hip. Heat therapy, such as using a warm compress or taking a warm bath, can help relax the muscles and improve blood circulation. On the other hand, ice packs or cold therapy can help reduce inflammation and alleviate pain. It is recommended to consult with a healthcare professional to determine the most appropriate temperature and duration for these therapies.
Physical Therapy For Snapping Hip Syndrome
Snapping hip syndrome is a condition that affects the hip joint, causing a snapping or popping sensation with movement. It occurs when the muscles, tendons, or ligaments around the hip joint rub against the bony structures, resulting in this snapping sensation. While the specific cause of snapping hip syndrome is not always clear, certain factors such as repetitive hip movement, muscle imbalances, and tight or weak muscles can contribute to the development of this condition.
Physical therapy is often recommended as a first-line treatment for snapping hip syndrome. It aims to alleviate pain, improve hip joint mobility, and address underlying muscle imbalances. A physical therapist will assess the individual's condition and develop a personalized treatment plan to target their specific needs.
The treatment approach for snapping hip syndrome may include a combination of manual therapy techniques, stretching exercises, strengthening exercises, and functional training. Manual therapy techniques, such as joint mobilization and soft tissue mobilization, can help improve joint mobility and reduce muscle tightness. Specific stretching exercises can target the muscles around the hip joint, helping to improve flexibility and alleviate tension.
- Strengthening exercises are an essential component of physical therapy for snapping hip syndrome. By targeting weak muscles and improving muscle balance, these exercises can help stabilize the hip joint and prevent further snapping or popping sensations. It is crucial to focus on strengthening the muscles of the hip, including the gluteal muscles, hip abductors, and hip rotators.
- In addition to manual therapy, stretching, and strengthening exercises, functional training is an important aspect of physical therapy for snapping hip syndrome. Functional exercises aim to improve the individual's ability to perform daily activities and sports-related movements without pain or snapping sensations. This may involve specific exercises that mimic the movements or activities that trigger the snapping hip syndrome.
Benefits of Physical Therapy for Snapping Hip Syndrome
• Pain relief: Physical therapy can help alleviate pain associated with snapping hip syndrome by reducing muscle tension, improving joint mobility, and strengthening the hip muscles.
• Improved mobility: The combination of stretching exercises and manual therapy techniques can help improve hip joint mobility, allowing for better range of motion and function.
• Prevention of future episodes: By addressing muscle imbalances and weaknesses, physical therapy can help prevent future episodes of snapping hip syndrome.
• Enhanced sports performance: Individuals who participate in sports or activities that involve repetitive hip movements can benefit from physical therapy to optimize their performance and reduce the risk of injury.
In conclusion, physical therapy plays a crucial role in the management of snapping hip syndrome. By addressing muscle imbalances, improving joint mobility, and providing pain relief, physical therapy can help individuals regain function and return to their normal activities. If you are experiencing symptoms of snapping hip syndrome, it is advisable to consult with a physical therapist for an accurate diagnosis and personalized treatment plan.
Surgical Interventions For Relief
When conservative management techniques fail to provide relief, surgical interventions may be considered as a treatment option for Snapping Hip Syndrome. The decision to proceed with surgery typically depends on the severity of the symptoms and the impact on daily activities. Surgical interventions aim to address the underlying causes of Snapping Hip Syndrome and alleviate pain and discomfort.
There are different surgical procedures available for the treatment of Snapping Hip Syndrome, depending on the specific type and cause of the condition. One common procedure is arthroscopy, which involves inserting a tiny camera through small incisions to visualize and repair any damage to the hip joint. Another surgical option is an open surgical procedure, where a larger incision is made to access and repair the affected structures.
In cases where there is abnormal friction between the tendons and bones, a tenotomy may be performed.
Read the full article
0 notes
Text
Goldenhar syndrome

Goldenhar Syndrome: Understanding the Challenges, Treatments, and Support
Goldenhar Syndrome, also known as oculo-auriculo-vertebral spectrum, is a complex congenital disorder that affects various parts of the body, predominantly the face and spine. In this blog post, we will delve into the causes of Goldenhar Syndrome, as well as the common symptoms and methods of diagnosing this condition. Additionally, we will explore the medical and surgical treatments available, along with the speech and hearing challenges individuals with Goldenhar Syndrome may face. Furthermore, we will discuss the educational support, emotional and social impacts, and available support groups and resources. Finally, we will touch upon the long-term outlook and recent research advancements in the field of Goldenhar Syndrome. Join us on this informative journey as we uncover the intricacies of this rare condition.
What Is Goldenhar Syndrome?
Goldenhar Syndrome, also known as oculoauriculovertebral dysplasia, is a rare congenital condition characterized by a wide range of physical abnormalities affecting the face, eyes, ears, and spine. It was first described by Dr. Maurice Goldenhar in the 1950s, hence the name. This syndrome is believed to occur as a result of abnormal development during the early stages of fetal growth.
One of the most distinctive features of Goldenhar Syndrome is the presence of facial asymmetry. Individuals with this condition may have underdeveloped or absent facial structures on one side of the face, leading to a noticeable difference in appearance between the left and right sides. Moreover, strabismus (crossed eyes) and microphthalmia (smaller than normal eyes) are also common ocular manifestations of Goldenhar Syndrome.
Hearing loss is another common characteristic of Goldenhar Syndrome. It can be caused by malformations of the outer, middle, or inner ear. These abnormalities can vary in severity, ranging from mild to profound hearing impairment. Additionally, some individuals may experience difficulties with speech and language development due to their hearing loss.
- Facial asymmetry
- Strabismus
- Microphthalmia
Symptoms
Percentage of Affected Individuals
Craniofacial abnormalities
92%
Spine abnormalities
66%
Heart defects
29%
Causes Of Goldenhar Syndrome
Goldenhar syndrome, also known as oculo-auriculo-vertebral spectrum, is a rare congenital condition that affects various parts of the body. The exact cause of Goldenhar syndrome is still unknown, but researchers believe that a combination of environmental and genetic factors may play a role in its development.
One of the possible causes of Goldenhar syndrome is believed to be genetic mutations. These mutations can occur spontaneously or be inherited from a parent. Research has shown that certain genes, such as the Sonic Hedgehog (SHH) gene, may be involved in the development of Goldenhar syndrome. However, more studies are needed to fully understand the genetic basis of this condition.
Another possible cause of Goldenhar syndrome is disruption in the development of the embryo during the early stages of pregnancy. It is thought that a disruption in the development of the first and second branchial arches, which are responsible for the formation of the face and ears, may lead to the characteristic facial and craniofacial abnormalities seen in individuals with Goldenhar syndrome.
Environmental factors may also contribute to the development of Goldenhar syndrome. It has been suggested that exposure to certain medications, toxins, or infections during pregnancy may increase the risk of a baby developing this condition. However, more research is needed to determine the specific environmental factors that may be involved.
In conclusion, the exact causes of Goldenhar syndrome are still not fully understood. It is believed to be a complex condition with a combination of genetic and environmental factors contributing to its development. Further research and studies are needed to gain a better understanding of this rare syndrome and to develop more targeted treatment options in the future.
Common Symptoms Of Goldenhar Syndrome
Goldenhar Syndrome, also known as Oculoauriculovertebral Spectrum, is a rare congenital disorder that affects the development of various structures in the body. It is characterized by a combination of craniofacial, auditory, and vertebral abnormalities. While the exact cause of Goldenhar Syndrome is not known, it is believed to occur due to disruptions in early embryonic development.
Individuals with Goldenhar Syndrome may exhibit a wide range of symptoms, which can vary in severity. One of the most common symptoms is facial asymmetry, where one side of the face may be underdeveloped or smaller than the other. This can affect the appearance of the eyes, ears, cheeks, and jaw. A notable feature of Goldenhar Syndrome is the presence of facial and ear anomalies, including misshapen or low-set ears, skin tags, and cysts.
In addition to facial abnormalities, individuals with Goldenhar Syndrome may also experience ocular anomalies. These can include strabismus (crossed eyes), ptosis (drooping eyelids), or coloboma (a gap or hole in the structures of the eye). Vision problems, such as nearsightedness or farsightedness, may also be present. Hearing loss is another common symptom of Goldenhar Syndrome, with some individuals experiencing mild to severe hearing impairment.
Furthermore, Goldenhar Syndrome can affect the development of the spine and skeletal system. Vertebral anomalies may lead to abnormal curvature of the spine, known as scoliosis. This can cause back pain, mobility issues, and in severe cases, difficulty breathing. Additionally, individuals with Goldenhar Syndrome may have hand or limb abnormalities, such as missing or underdeveloped fingers, toes, or limbs.
Other less common symptoms of Goldenhar Syndrome include cardiovascular malformations, kidney abnormalities, and gastrointestinal defects. Additionally, some individuals may have intellectual disabilities or learning difficulties. It is important to note that the presence and severity of symptoms can vary greatly among individuals with Goldenhar Syndrome.
- In conclusion, Goldenhar Syndrome is a complex condition that affects various aspects of an individual's development. The common symptoms of Goldenhar Syndrome include facial asymmetry, facial and ear anomalies, ocular abnormalities, hearing loss, spinal and skeletal anomalies, and in some cases, additional systemic complications. Each individual with Goldenhar Syndrome may have a unique combination of symptoms, highlighting the complex nature of this condition.
Common Symptoms of Goldenhar Syndrome
Facial asymmetry
Facial and ear anomalies
Ocular abnormalities
Hearing loss
Spinal and skeletal anomalies
Additional systemic complications
Diagnosing Goldenhar Syndrome
Diagnosing Goldenhar Syndrome can be a complex process due to the wide range of symptoms and variations that can occur in individuals. There is no specific test to diagnose Goldenhar Syndrome, but a combination of medical evaluations, imaging studies, and genetic testing can help in confirming the condition. The diagnosis of Goldenhar Syndrome often begins with a thorough physical examination by a healthcare professional. They will carefully observe any characteristic facial abnormalities, such as a cleft lip, strabismus, or ear anomalies. Observing these physical features, along with a detailed medical history, can give healthcare providers a preliminary indication of Goldenhar Syndrome.
Further diagnostic tests may be recommended to confirm the diagnosis. Medical imaging studies, such as X-rays, ultrasound, or MRI scans, can be used to evaluate the internal structure and function of the affected organs. These imaging techniques can help identify any skeletal abnormalities, such as vertebral anomalies or defects in the spine or ribs. Additionally, genetic testing can be performed to identify any specific gene mutations or chromosomal abnormalities associated with Goldenhar Syndrome.
It is important to note that the diagnosis of Goldenhar Syndrome can sometimes be challenging due to its overlapping features with other craniofacial conditions. Therefore, a multidisciplinary approach involving various specialists, such as craniofacial surgeons, geneticists, ophthalmologists, and ear, nose, and throat specialists, is often necessary for an accurate diagnosis. Collaboration among these experts can help ensure a comprehensive evaluation of the individual's condition and provide appropriate treatment and management options.
Medical Treatments For Goldenhar Syndrome
Goldenhar Syndrome is a rare congenital condition that affects the development of the craniofacial region. It is characterized by a combination of physical abnormalities, which may include facial asymmetry, ear malformations, eye abnormalities, and spinal defects. While there is no cure for Goldenhar Syndrome, medical treatments aim to manage the symptoms and improve the quality of life for individuals affected by the condition.
One of the primary medical treatments for Goldenhar Syndrome is surgical intervention. This can involve reconstructive surgery to address facial asymmetry and ear malformations. Plastic surgeons work closely with individuals and their families to create a personalized treatment plan that takes into account the unique needs and goals of each patient. Surgical interventions can help improve facial appearance, enhance hearing, and enable better speech development.
Treatment
Description
Hearing aids and assistive devices
For individuals with hearing impairment, hearing aids or other assistive devices may be recommended to improve auditory function and communication ability.
Physical therapy
Physical therapy can help individuals with Goldenhar Syndrome improve their motor skills, strength, and mobility. This can be particularly beneficial for those with spinal defects or other orthopedic issues.
Speech therapy
Speech therapy plays a crucial role in the management of Goldenhar Syndrome. Therapists help individuals improve their speech and language skills, addressing any difficulties they may have due to facial or oral abnormalities.
Eye care
Individuals with eye abnormalities associated with Goldenhar Syndrome may require regular visits to an ophthalmologist. Treatment options can include glasses, contact lenses, or even corrective eye surgery.
Supportive therapies are also important in the medical treatment of Goldenhar Syndrome. These can include occupational therapy, which focuses on improving fine motor skills and daily living activities, as well as psychological support for both the individual and their family members. Support groups and resources specific to Goldenhar Syndrome can provide valuable emotional support and the opportunity to connect with others who have similar experiences.
It's important to remember that each individual with Goldenhar Syndrome is unique, and their medical treatment plan will be tailored to their specific needs. Collaboration between healthcare professionals, including pediatricians, geneticists, plastic surgeons, and therapists, is crucial to ensure comprehensive and coordinated care.
Surgical Interventions For Goldenhar Syndrome
Goldenhar Syndrome is a rare congenital disorder that affects the development of the craniofacial region. It primarily affects the development of the ears, eyes, and spine. Surgical interventions play a crucial role in managing and improving the physical abnormalities associated with Goldenhar Syndrome. These interventions aim to address specific issues and improve the overall quality of life for individuals with this condition.
One of the most common surgical interventions for Goldenhar Syndrome is reconstructive surgery for facial and craniofacial abnormalities. This type of surgery involves correcting facial asymmetry, craniofacial malformations, and other structural abnormalities. The goal is to enhance facial appearance and function, improving breathing, chewing, and speech.
In some cases, individuals with Goldenhar Syndrome may require surgical intervention to address hearing loss. Ear malformations, such as malformed or absent ears, can lead to hearing difficulties. Ear reconstruction surgery or the use of a hearing aid may be recommended to improve hearing ability and enhance communication skills.
- Another surgical intervention that may be necessary for individuals with Goldenhar Syndrome is spinal surgery. Spinal abnormalities, such as scoliosis, are occasionally associated with this condition. These abnormalities can cause discomfort, restrict mobility, and potentially affect organ function. Spinal fusion surgery or other corrective procedures may be performed to alleviate these issues and enhance overall spinal health.
Surgical Interventions for Goldenhar Syndrome
Description
Reconstructive Facial and Craniofacial Surgery
Corrects facial asymmetry and craniofacial malformations, improving facial appearance and function.
Hearing Restoration Surgery
Addresses hearing loss through ear reconstruction surgery or the use of hearing aids.
Spinal Surgery
Corrective procedures, such as spinal fusion, to address spinal abnormalities like scoliosis.
It is important to note that each individual with Goldenhar Syndrome may have unique surgical needs and requirements. A comprehensive evaluation by a multidisciplinary team of healthcare professionals, including surgeons, is necessary to determine the most appropriate surgical interventions for each person.
While surgical interventions can significantly improve the physical aspects of Goldenhar Syndrome, it is crucial to consider the emotional and social impacts that individuals may experience. Providing psychological and emotional support before and after surgery can help individuals cope with the challenges and changes associated with these interventions. Additionally, ongoing communication and collaboration with educational institutions and support groups are essential to ensure holistic support for individuals with Goldenhar Syndrome.
In conclusion, surgical interventions play a vital role in addressing the physical abnormalities associated with Goldenhar Syndrome. Reconstructive facial and craniofacial surgery, hearing restoration surgery, and spinal surgery are some of the procedures that may be necessary to improve overall health and well-being. However, it is crucial to consider the individual needs of each person and provide comprehensive support throughout their journey.
Speech And Hearing Challenges In Goldenhar Syndrome
Goldenhar syndrome is a rare and complex congenital condition that affects the development of various structures in the face and head. While its exact cause is still unknown, it is believed to be the result of a combination of genetic and environmental factors. This syndrome is characterized by a wide range of physical abnormalities, including facial asymmetry, underdeveloped or missing ears, and malformations of the jaw and spine. However, in addition to these physical challenges, individuals with Goldenhar syndrome often face significant speech and hearing challenges that can greatly impact their communication abilities.
One of the primary speech challenges faced by individuals with Goldenhar syndrome is articulation difficulties. This can manifest as difficulty pronouncing certain sounds, especially those involving the lips, tongue, and teeth. The malformation of the jaw and facial muscles can make it challenging to coordinate the precise movements required for accurate speech production. Speech therapy is often recommended to help individuals with Goldenhar syndrome improve their articulation skills and enhance their overall communication abilities.
In addition to articulation difficulties, many individuals with Goldenhar syndrome also experience hearing impairments. The underdeveloped or missing ears can lead to conductive hearing loss, where sound waves have difficulty reaching the inner ear. This can result in difficulties in understanding speech, especially in noisy environments. Hearing aids or other assistive listening devices may be prescribed to help individuals with Goldenhar syndrome overcome their hearing challenges and improve their ability to communicate effectively.
- Speech Challenges in Goldenhar Syndrome:
1. Articulation difficulties due to the malformation of the jaw and facial muscles.
2. Speech therapy can help improve articulation skills and overall communication abilities.
3. The coordination of precise movements required for accurate speech production can be challenging for individuals with Goldenhar syndrome.
Hearing Challenges in Goldenhar Syndrome:
1. Underdeveloped or missing ears can lead to conductive hearing loss.
2. Difficulty understanding speech, especially in noisy environments.
3. Hearing aids and assistive listening devices can help individuals overcome hearing challenges.
Educational Support For Individuals With Goldenhar Syndrome
Goldenhar Syndrome is a rare congenital condition that affects various structures on one side of the face and can also cause abnormalities in other parts of the body. While the physical aspects of this syndrome are typically the focus of treatment, it is equally important to address the educational needs of individuals with Goldenhar Syndrome. Providing appropriate educational support is crucial for these individuals to achieve their full potential and lead fulfilling lives.
One of the key challenges in providing educational support for individuals with Goldenhar Syndrome is addressing their unique learning needs. Due to the craniofacial and physical impairments associated with the condition, these individuals may experience difficulties in speech and language development, hearing, vision, and fine motor skills. It is important for educators to have a comprehensive understanding of these challenges and implement tailored strategies to support effective learning.
When it comes to communication, individuals with Goldenhar Syndrome may face significant speech and hearing challenges. Communication devices such as hearing aids and augmentative and alternative communication (AAC) systems can greatly assist these individuals in overcoming these challenges. Teachers and speech therapists play a critical role in helping individuals with Goldenhar Syndrome develop effective communication skills and providing ongoing support.
- In addition to addressing the specific challenges related to Goldenhar Syndrome, it is equally important to foster a supportive learning environment that promotes social and emotional well-being.
Read the full article
0 notes
Text
Butterfly syndrome

Living with Butterfly Syndrome can present numerous challenges, ranging from physical complications to educational and social hurdles. This rare genetic disorder, also known as epidermolysis bullosa, affects the skin and causes it to become extremely fragile and prone to blistering. In this blog post, we will explore the various aspects of Butterfly Syndrome, including its causes, symptoms, types, and treatment options. Additionally, we will discuss the importance of managing skin complications, physical therapy, psychological support, and the educational and social challenges faced by individuals with Butterfly Syndrome. We will also highlight the latest research, supportive organizations, and inspiring stories of those overcoming the obstacles of this condition.
What Is Butterfly Syndrome?
Butterfly syndrome, also known as epidermolysis bullosa (EB), is a rare genetic disorder that affects the skin and other mucous membranes. It is characterized by extreme fragility of the skin, leading to blistering and erosion with minimal trauma or friction. The condition gets its name from the fragile skin that resembles butterfly wings. This condition is caused by a mutation in the genes responsible for the production of certain proteins that help to anchor the layers of the skin together.
Individuals with butterfly syndrome have to deal with a number of challenges on a daily basis. The fragility of their skin makes it highly susceptible to blistering and tearing, even with minimal contact. This can lead to chronic wounds that are slow to heal, increasing the risk of infection. Additionally, individuals with butterfly syndrome may experience complications in other areas of the body, such as the eyes, mouth, and gastrointestinal tract.
Despite being a rare disorder, butterfly syndrome can have a significant impact on the lives of those affected. It is crucial for individuals with this condition to receive appropriate medical care and support to manage their symptoms and improve their quality of life. The next sections of this blog post will delve into the various aspects of butterfly syndrome, including its causes, symptoms, types, and available treatment options.
Causes Of Butterfly Syndrome
Butterfly Syndrome, also known as Epidermolysis Bullosa, is a rare genetic disorder that affects the skin and other body tissues. It is characterized by the formation of blisters and fragile skin that can easily tear or peel. There are several different types of Butterfly Syndrome, each with its own set of causes and symptoms.
One of the main causes of Butterfly Syndrome is a mutation in the genes responsible for producing certain proteins that help to hold the layers of the skin together. This mutation can result in a lack or dysfunction of these proteins, leading to the fragility of the skin. In most cases, Butterfly Syndrome is inherited from one or both parents who carry the faulty gene.
Another cause of Butterfly Syndrome is spontaneous gene mutations. These mutations can occur during the development of an embryo or fetus, resulting in the condition being present in individuals without a family history of the disorder. Spontaneous mutations are believed to be responsible for a significant portion of Butterfly Syndrome cases.
Additionally, certain environmental factors can trigger or worsen symptoms of Butterfly Syndrome. These factors include excessive heat, friction, and trauma to the skin. Individuals with Butterfly Syndrome must take precautions to avoid injury or damage to their skin, as it can lead to blistering and painful open wounds.
- Genetic mutation in the genes responsible for producing certain proteins
- Spontaneous gene mutations during embryo or fetal development
- Environmental factors such as excessive heat, friction, and trauma to the skin
Causes of Butterfly Syndrome
Genetic mutation in the genes responsible for producing certain proteins
Spontaneous gene mutations during embryo or fetal development
Environmental factors such as excessive heat, friction, and trauma to the skin
Symptoms And Diagnosis Of Butterfly Syndrome
Symptoms of Butterfly Syndrome:
Butterfly Syndrome, also known as epidermolysis bullosa, is a rare genetic disorder characterized by extremely fragile skin. Individuals with this condition experience recurring blisters and erosions in response to minor trauma or friction. The blisters often resemble butterfly wings, which is how the syndrome got its nickname. Besides the prominent skin manifestations, Butterfly Syndrome can affect various body systems, leading to a range of symptoms including:
- Painful lesions and sores on the skin
- Difficulty swallowing and eating
- Blistering and erosion of the mucus membranes
- Thickened or absent nails
- Scarring and contractures
- Eye problems such as corneal abrasions and eyelid fusion
- Difficulty breathing due to blistering and scarring of the airways
Diagnosis of Butterfly Syndrome:
The diagnosis of Butterfly Syndrome involves a comprehensive evaluation of the individual's medical history, physical examination, and specific diagnostic tests. A dermatologist or a genetic specialist usually leads the diagnostic process. During the physical examination, the healthcare provider carefully examines the individual's skin, looking for characteristic signs of blistering and erosions. The medical history review focuses on identifying any family history of the syndrome or similar skin disorders, as Butterfly Syndrome is an inherited condition.
Diagnostic tests commonly used in the diagnosis of Butterfly Syndrome
1. Skin biopsy: A small sample of skin tissue is taken and examined under a microscope to identify the specific abnormalities in the skin structure.
2. Genetic testing: DNA analysis is performed to detect mutations or changes in the genes associated with epidermolysis bullosa. This test helps confirm the diagnosis and determine the specific subtype of Butterfly Syndrome.
3. Immunofluorescence mapping: This test involves labeling proteins within the skin to assess their distribution and integrity. It aids in identifying the specific protein abnormalities involved in Butterfly Syndrome.
Obtaining a proper diagnosis is crucial in managing Butterfly Syndrome as it helps determine the appropriate treatment options and supportive care measures to improve the individual's quality of life.
Types And Classification Of Butterfly Syndrome
Butterfly Syndrome is a rare genetic disorder that affects the skin and mucous membranes of individuals. This condition is also known as epidermolysis bullosa, characterized by extreme fragility and blistering of the skin. Butterfly Syndrome gets its name from the delicate and fragile nature of the affected skin, which can easily tear or blister with minimal friction or trauma.
There are several types and classifications of Butterfly Syndrome, each with its own unique characteristics and severity levels. The most common type is called Junctional Epidermolysis Bullosa (JEB), which is further classified into three subtypes - JEB-Herlitz, JEB-Letalis, and JEB-Nonspecific. JEB-Herlitz is the most severe form, characterized by blistering of the skin and mucous membranes, and often leads to life-threatening complications. JEB-Letalis and JEB-Nonspecific have varying degrees of severity, with JEB-Letalis being significantly more severe and JEB-Nonspecific being milder.
Another type of Butterfly Syndrome is Dystrophic Epidermolysis Bullosa (DEB), which is classified into two subtypes - DEB-Simplex and DEB-Dystrophic. DEB-Simplex is characterized by blistering confined to the hands and feet, while DEB-Dystrophic involves blistering throughout the body, including mucous membranes. DEB-Dystrophic can lead to complications such as scarring, deformities, and an increased risk of skin cancers.
In addition to these types, there is a rare form of Butterfly Syndrome called Kindler Syndrome. Kindler Syndrome affects the skin, mucous membranes, and various internal organs. Individuals with Kindler Syndrome often develop a unique pattern of blistering and scarring, along with photosensitivity and increased skin fragility.
Understanding the types and classification of Butterfly Syndrome is crucial for proper diagnosis and management of the condition. Each subtype requires specific care and treatment strategies tailored to the individual's needs. Furthermore, research and advances in the field of Butterfly Syndrome continue to expand our understanding of these types, leading to improved therapies and support for individuals affected by this rare disorder.
Keywords: Butterfly Syndrome, types, classification, epidermolysis bullosa, JEB, DEB, Kindler Syndrome, skin fragility, blistering
Treatment Options For Butterfly Syndrome
Butterfly Syndrome, also known as Epidermolysis Bullosa (EB), is a rare genetic disorder that affects the skin and various mucous membranes. Individuals with Butterfly Syndrome have extremely fragile skin that is prone to blisters, ulcers, and wounds even with minimal friction or trauma. This can cause significant pain, discomfort, and complications in their daily lives. While there is no cure for this condition, several treatment options can help manage the symptoms and improve the quality of life for those living with Butterfly Syndrome.
1. Wound Care:
One of the main focuses of treatment for Butterfly Syndrome is proper wound care. This involves gentle and meticulous cleaning of wounds to prevent infection, application of sterile dressings to promote healing, and the use of specialized bandages and dressings that minimize pain and protect fragile skin. Additionally, individuals with Butterfly Syndrome may need regular monitoring and care for any open wounds or blisters to prevent complications.
2. Pain Management:
The chronic pain experienced by individuals with Butterfly Syndrome can be debilitating and significantly impact their quality of life. Therefore, pain management strategies are an important aspect of treatment. This may involve the use of pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, or topical anesthetics to provide relief. Additionally, alternative therapies like acupuncture, massage, and physical therapy may also be utilized to alleviate pain and improve overall well-being.
3. Nutritional Support:
Proper nutrition plays a crucial role in managing Butterfly Syndrome. Due to difficulties in eating, individuals with severe forms of the condition may require a feeding tube or specialized feeding techniques to ensure they receive adequate nutrition. Working closely with a dietitian can help develop customized meal plans that are easy to swallow, nutrient-dense, and tailored to the individual's specific needs. Nutritional supplements may also be recommended to help meet the required nutrient intake.
While wound care, pain management, and nutritional support are key treatment options for managing Butterfly Syndrome, it is important to note that each individual's condition is unique, and treatment plans should be tailored to their specific needs and challenges. Collaborative care involving dermatologists, wound care specialists, pain management specialists, nutritionists, and other healthcare professionals is crucial in providing holistic care and improving the overall well-being of individuals with Butterfly Syndrome.
References:
1.
Genetic and Rare Diseases Information Center. Epidermolysis bullosa.
2.
National Institute of Arthritis and Musculoskeletal and Skin Diseases. Epidermolysis Bullosa.
3.
Mayo Clinic. Epidermolysis bullosa.
Managing Skin Complications In Butterfly Syndrome
Butterfly syndrome, also known as epidermolysis bullosa (EB), is a rare genetic disorder that affects the skin and causes it to become extremely fragile and prone to blistering. This condition is named after the characteristic butterfly-wing pattern that results from the delicate skin's tendency to tear and peel. While EB primarily affects the skin, it can also impact other organs and bodily systems, leading to various complications.
One of the most significant challenges in managing butterfly syndrome is dealing with skin complications. Individuals with EB have skin that is highly susceptible to damage, and even the slightest friction or trauma can result in painful blisters and open wounds. These skin complications pose a risk of infection and require careful and diligent wound care to promote healing and prevent further complications.
A multi-faceted approach is essential in managing the skin complications associated with butterfly syndrome. First and foremost, it is crucial to create a safe environment that minimizes friction and trauma to the skin. This may involve using soft, non-abrasive clothing, using specialized bandages or dressings to protect fragile areas, and avoiding activities or objects that may cause unnecessary harm.
Regular and meticulous wound care is vital to managing skin complications in butterfly syndrome. This typically involves cleaning the affected areas with sterile solutions, applying appropriate dressings or bandages to protect the skin, and monitoring for signs of infection. Additionally, healthcare providers may prescribe topical or systemic medications to alleviate discomfort, prevent infection, and promote healing.
Wound Care Tips for Butterfly Syndrome:
- Gently cleanse wounds with mild, non-irritating cleansers to avoid further damage.
- Use non-stick dressing materials to prevent sticking and minimize pain during dressing changes.
- Avoid tight or constrictive clothing that can cause friction and damage to the skin.
- Keep the skin well-moisturized to minimize dryness and cracking.
Emotional support and psychological well-being should not be overlooked when managing skin complications in butterfly syndrome. Living with a condition that presents such significant challenges to the skin can be mentally and emotionally taxing. It is essential for individuals with butterfly syndrome to have access to psychological support, counseling, and resources that can help them cope with the emotional impacts of their condition.
In conclusion, managing the skin complications associated with butterfly syndrome requires a comprehensive approach that encompasses wound care, preventative measures, and emotional support. By prioritizing proper wound care techniques, creating a safe environment, and attending to psychological well-being, individuals with butterfly syndrome can improve their quality of life and effectively manage the challenges they face on a daily basis.
Physical Therapy For Butterfly Syndrome
Physical Therapy for Butterfly Syndrome
Butterfly Syndrome, also known as Epidermolysis Bullosa (EB), is a rare genetic skin disorder that affects the connective tissues in the body. Individuals with Butterfly Syndrome have extremely fragile skin that is prone to blistering and tearing from minor friction or trauma. This condition can cause immense pain and discomfort, making it difficult for affected individuals to perform everyday activities. While there is no cure for Butterfly Syndrome, physical therapy can play a crucial role in managing the symptoms and improving the quality of life for those living with this condition.
Physical therapy aims to address the physical limitations and functional difficulties faced by individuals with Butterfly Syndrome. The main goal of physical therapy is to maximize functional independence and enhance overall mobility. Therapists work closely with patients to develop personalized exercise programs that focus on strengthening muscles, improving range of motion, and promoting flexibility.
One of the primary objectives of physical therapy for Butterfly Syndrome is to prevent and manage contractures. Contractures are a common complication of this condition and occur when the skin and underlying tissues become tight, limiting movement. Physical therapists utilize various stretching techniques and splints to stretch the tightened areas and improve joint mobility. This helps prevent contractures and maintain optimal joint function.
- Physical therapy can also help manage pain associated with Butterfly Syndrome. Therapists may employ modalities such as heat therapy, manual therapy, and transcutaneous electrical nerve stimulation (TENS) to alleviate discomfort and improve overall well-being.
- Furthermore, physical therapy can assist in improving gross motor skills and balance in individuals with Butterfly Syndrome. Through targeted exercises and balance training, therapists aim to enhance coordination, stability, and postural control, allowing individuals to perform activities more safely and independently.
- It is important to note that physical therapy for Butterfly Syndrome should be tailored to meet the specific needs of each individual. Therapists incorporate a multidisciplinary approach, collaborating with other healthcare professionals, such as dermatologists and occupational therapists, to ensure a comprehensive treatment plan. This integrated approach helps maximize the benefits of physical therapy and address the unique challenges faced by individuals with Butterfly Syndrome.
In conclusion, physical therapy plays a crucial role in managing the symptoms and enhancing the quality of life for individuals with Butterfly Syndrome. Through targeted exercises, stretching techniques, and modalities, physical therapists aim to improve mobility, prevent contractures, manage pain, and enhance gross motor skills. By working closely with other healthcare professionals, physical therapy can be integrated into a comprehensive treatment plan that addresses the unique challenges faced by those living with Butterfly Syndrome.
Psychological Support For Individuals With Butterfly Syndrome
Butterfly Syndrome, also known as epidermolysis bullosa (EB), is a rare genetic disorder characterized by extremely fragile skin and mucous membranes. It is a chronic condition that affects both children and adults, causing widespread blistering and skin erosions even with the slightest friction or trauma. While the physical challenges of living with Butterfly Syndrome are well-documented, the psychological impact on individuals with this condition is often overlooked.
Living with Butterfly Syndrome can be emotionally overwhelming, especially for children who may face bullying and social isolation due to their visible and chronic skin wounds. It is crucial to provide psychological support for individuals with Butterfly Syndrome, helping them navigate the emotional and mental challenges of their condition.
Read the full article
0 notes
Text
Traps syndrome
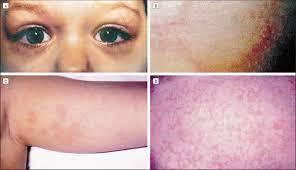
Living with a rare medical condition can be challenging, especially when it comes to Traps Syndrome. In this blog post, we will explore what Traps Syndrome is, its causes, and the symptoms and signs to watch out for. We will also delve into diagnosing Traps Syndrome and the various treatment options available. Additionally, we will discuss medications and lifestyle modifications that can help manage the condition. Understanding the potential complications, as well as the resources and support groups available, will be covered. Finally, we will touch upon the latest research and advancements in Traps Syndrome and provide tips for preventing and living with this condition.
What Is Traps Syndrome?
Traps Syndrome, also known as TNF receptor-associated periodic syndrome, is a rare genetic disorder that affects the body's ability to regulate inflammation. It is classified as an autoinflammatory disease, meaning that it is characterized by recurring episodes of inflammation throughout the body without the usual triggers such as infections or injuries. Traps Syndrome is caused by mutations in the TNFRSF1A gene, which leads to abnormal functioning of the protein receptor responsible for controlling inflammation.
- Causes of Traps Syndrome
Traps Syndrome is primarily caused by mutations in the TNFRSF1A gene. These mutations can be inherited, with affected individuals having one copy of the mutated gene from an affected parent. In some cases, the mutations occur spontaneously, without any family history. The TNFRSF1A gene is responsible for producing a protein receptor called tumor necrosis factor receptor 1 (TNFR1), which plays a crucial role in regulating the body's inflammatory response. When the gene is mutated, the receptor malfunctions, leading to episodes of excessive and prolonged inflammation.
Symptoms and Signs of Traps Syndrome
Diagnosing Traps Syndrome
Common symptoms of Traps Syndrome include recurrent episodes of fever, muscle and joint pain, abdominal pain, skin rashes, and swelling in various parts of the body. These episodes can last for days to weeks, followed by periods of remission. The frequency and severity of the episodes vary among individuals. Some may experience mild symptoms, while others may have more debilitating episodes that significantly impact their quality of life.
Diagnosing Traps Syndrome can be challenging due to its rarity and overlap of symptoms with other inflammatory conditions. A thorough medical history review, physical examination, and laboratory tests are typically conducted. Blood tests may reveal elevated levels of inflammatory markers such as C-reactive protein (CRP) and serum amyloid A (SAA). Genetic testing can confirm the presence of TNFRSF1A mutations, providing a definitive diagnosis.
Causes Of Traps Syndrome
Traps Syndrome, also known as tracheoesophageal fistula, is a rare congenital condition that affects the development of the esophagus and trachea. This condition occurs when the tissues that normally separate the esophagus and trachea during fetal development fail to divide completely, resulting in an abnormal connection between the two. Traps Syndrome can lead to a range of symptoms and complications, making it important to understand the causes of this condition.
There are several factors that can contribute to the development of Traps Syndrome. One of the main causes is a genetic mutation. Researchers have identified specific genes that are involved in the formation and separation of the esophagus and trachea during fetal development. Mutations in these genes can interfere with the normal process and lead to the development of Traps Syndrome. In some cases, Traps Syndrome may also be caused by a combination of genetic and environmental factors.
In addition to genetic factors, certain environmental factors may increase the risk of Traps Syndrome. Maternal smoking, for example, has been associated with a higher likelihood of the condition. The chemicals present in cigarette smoke can disrupt fetal development and increase the chances of abnormalities in the esophagus and trachea. Other environmental factors, such as exposure to certain medications or toxins during pregnancy, may also play a role in the development of Traps Syndrome.
Possible Causes of Traps Syndrome
Genetic mutations
Environmental factors
Maternal smoking
Exposure to medications or toxins during pregnancy
It is important to note that the exact causes of Traps Syndrome are still not fully understood. Researchers continue to investigate the underlying genetic and environmental factors that contribute to the development of this condition. By gaining a better understanding of the causes, healthcare professionals can improve their ability to diagnose and treat Traps Syndrome effectively.
- In conclusion, Traps Syndrome is a complex condition with multifactorial causes. Genetic mutations and environmental factors, such as maternal smoking and exposure to certain substances during pregnancy, may increase the risk of developing this condition. Further research is needed to fully comprehend the underlying causes of Traps Syndrome and develop effective preventive measures. By raising awareness and supporting ongoing research, we can hope for improved outcomes and treatment options for individuals affected by this rare condition.
Symptoms And Signs Of Traps Syndrome
Symptoms and Signs of Traps Syndrome
Traps syndrome, also known as TNF receptor-associated periodic syndrome, is a rare genetic autoinflammatory disorder. It is characterized by recurrent episodes of inflammation throughout the body, leading to various symptoms and signs. This condition affects multiple systems in the body, including the joints, skin, and gastrointestinal tract, among others. Understanding the symptoms and signs of Traps syndrome is crucial for early detection and effective management of the condition.
Common symptoms of Traps syndrome include:
- Fever: Recurrent episodes of high-grade fever are one of the hallmark symptoms of Traps syndrome. The fever may last for several days and can be accompanied by chills and sweating.
- Abdominal pain: Many individuals with Traps syndrome experience abdominal pain during episodes of inflammation. The pain can range from mild to severe and may be localized or diffuse.
- Rash: Skin manifestations are common in Traps syndrome. A characteristic rash, often appearing as red or pale pink patches, may develop during episodes of inflammation. The rash can be itchy and may worsen with exposure to triggers.
In addition to these primary symptoms, Traps syndrome can also present with joint pain and swelling, fatigue, muscle pain, headaches, and swollen lymph nodes. These symptoms may vary in severity and frequency among affected individuals.
It is essential to recognize the signs of Traps syndrome to avoid misdiagnosis or delayed diagnosis. When evaluating a patient with suspected Traps syndrome, healthcare providers look for recurrent episodes of fever, abdominal pain, and other associated symptoms. Genetic testing plays a crucial role in confirming the diagnosis, as mutations in the TNFRSF1A gene are closely associated with Traps syndrome.
Early diagnosis of Traps syndrome is vital for initiating appropriate treatment and preventing potential complications. Once diagnosed, individuals with Traps syndrome can work closely with a multidisciplinary healthcare team to manage their symptoms and improve their quality of life.
Potential Complications
Treatment Options
Lifestyle Modifications
Traps syndrome can lead to several potential complications, including amyloidosis, which affects the kidneys and other organs. Other complications may include joint damage, skin infections, and gastrointestinal issues.
The treatment of Traps syndrome involves a combination of medications aimed at controlling inflammation and preventing recurrent episodes. Biologic drugs, such as interleukin-1 inhibitors, have shown promising results in managing the symptoms of Traps syndrome.
Adopting certain lifestyle modifications can help individuals with Traps syndrome manage their symptoms more effectively. These may include regular exercise, stress management techniques, and avoiding triggers such as certain foods or environmental factors.
Additionally, seeking support from dedicated Traps syndrome support groups and resources can provide valuable information, guidance, and emotional support to individuals and their families.
Researchers and medical professionals continue to explore the latest advancements in Traps syndrome. Ongoing research aims to improve understanding of the underlying mechanisms of Traps syndrome, develop targeted therapies, and enhance the overall management of this rare condition.
In conclusion, Traps syndrome is a rare genetic autoinflammatory disorder characterized by recurrent episodes of inflammation. Recognizing the symptoms and signs of Traps syndrome is crucial for timely diagnosis and effective management. Collaboration with healthcare professionals, adherence to treatment plans, and support from the Traps syndrome community can significantly improve the quality of life for individuals living with this condition.
Diagnosing Traps Syndrome
When it comes to Traps Syndrome, diagnosing this rare condition can be challenging due to its complex nature. Traps Syndrome, short for TNF receptor-associated periodic syndrome, is an autoinflammatory disorder characterized by recurrent episodes of fever and inflammation throughout the body. requires a thorough understanding of the symptoms, medical history, and specific diagnostic tests.
One of the key factors in diagnosing Traps Syndrome is recognizing the unique pattern of symptoms associated with the condition. These episodes typically consist of recurrent fever that lasts for several days, accompanied by muscle and joint pain, skin rashes, and abdominal discomfort. Additionally, Traps Syndrome may cause inflammation in various organs, such as the lungs, eyes, and heart, leading to additional symptoms.
In order to accurately diagnose Traps Syndrome, healthcare professionals rely on both clinical evaluation and specific diagnostic tests. These tests may include blood tests to measure inflammation markers, genetic testing to identify specific genetic mutations associated with Traps Syndrome, and imaging studies to assess organ involvement and inflammation. It is important for individuals experiencing symptoms indicative of Traps Syndrome to seek medical attention promptly to undergo the necessary diagnostic evaluations for an accurate diagnosis.
Diagnosing Traps Syndrome can be a complex process that often requires the expertise of various medical specialists, such as rheumatologists, geneticists, and immunologists. By collaborating and analyzing the combination of clinical symptoms, genetic test results, and laboratory findings, healthcare professionals can reach a definitive diagnosis.
Treatment Options For Traps Syndrome
Traps Syndrome, also known as TNF receptor-associated periodic syndrome, is a rare autoinflammatory disorder that causes recurrent bouts of fever and inflammation. While there is no cure for Traps Syndrome, there are various treatment options available to manage the symptoms and improve the quality of life for those affected.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs such as ibuprofen or naproxen can be effective in reducing pain, inflammation, and fever associated with Traps Syndrome. These over-the-counter medications can provide temporary relief and are often the first line of treatment for mild to moderate symptoms. However, it is important to consult with a healthcare professional before starting any new medication.
Biologic Agents
In more severe cases of Traps Syndrome, biologic agents can be prescribed to target specific molecules involved in the inflammatory response. Canakinumab and Anakinra are two examples of biologic drugs that have shown promising results in managing the symptoms of Traps Syndrome. These medications are usually administered through injections and require regular monitoring by a healthcare provider.
Lifestyle Modifications
While medication plays a crucial role in managing Traps Syndrome, lifestyle modifications can also contribute to symptom relief. Maintaining a healthy diet, regular exercise, and adequate rest can help reduce the frequency and severity of flare-ups. Stress management techniques, such as relaxation exercises or meditation, may also be beneficial in preventing Traps Syndrome episodes.
In conclusion, while there is no cure for Traps Syndrome, treatment options are available to alleviate the symptoms and improve the overall well-being of individuals diagnosed with this condition. It is important to consult with a healthcare professional to determine the most appropriate treatment plan based on the severity of symptoms and individual needs. With the right management approach, individuals with Traps Syndrome can lead fulfilling lives and minimize the impact of this chronic condition on their daily activities.
Medications For Managing Traps Syndrome
Traps syndrome, also known as TNF receptor-associated periodic syndrome, is a rare autoinflammatory disorder that affects various parts of the body, including joints, muscles, and skin. It is caused by a mutation in the TNFRSF1A gene, which plays a crucial role in regulating the immune system. Although there is no cure for Traps syndrome, several medications can help manage its symptoms and improve the quality of life for those affected.
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs are commonly used to reduce pain, inflammation, and fever associated with Traps syndrome. These medications work by blocking specific enzymes in the body that are responsible for producing chemicals involved in inflammation. However, it is important to note that long-term use of NSAIDs may have side effects, such as gastrointestinal issues and potential kidney damage.
2. Corticosteroids: In severe cases of Traps syndrome or during flare-ups, corticosteroids may be prescribed to reduce inflammation and suppress the activity of the immune system. These medications can provide rapid relief and are particularly effective in managing symptoms such as joint pain and swelling. However, prolonged use of corticosteroids may lead to various side effects, including weight gain, mood changes, and increased risk of infections.
3. Biologic Therapies: Biologic therapies are a newer class of medications that specifically target proteins in the immune system responsible for causing inflammation. One example is interleukin-1 (IL-1) inhibitors, which have shown promising results in managing Traps syndrome symptoms. By blocking the effects of IL-1, these medications can help reduce the frequency and severity of flare-ups. However, biologic therapies may have potential side effects, such as increased susceptibility to infections.
4. Immunomodulatory Drugs: Immunomodulatory drugs, such as colchicine, can also be used to manage Traps syndrome. Colchicine works by reducing the production of certain chemicals involved in inflammation. It is often used as a preventive measure to decrease the frequency of Traps syndrome episodes. However, it may cause gastrointestinal side effects, such as diarrhea and abdominal pain.
5. Supportive Medications: Alongside specific therapies, additional medications may be prescribed to manage individual symptoms of Traps syndrome. For example, pain relievers like acetaminophen or opioids can help alleviate severe pain. Antihistamines may be used to control skin manifestations, such as rashes or itching. It is important to consult with a healthcare professional to determine the appropriate medications based on the severity and specific symptoms experienced by the individual.
In conclusion, while there is no cure for Traps syndrome, medications play a crucial role in managing its symptoms and improving the overall quality of life for those affected. Nonsteroidal anti-inflammatory drugs, corticosteroids, biologic therapies, immunomodulatory drugs, and supportive medications are some of the treatment options available. However, it is essential to work closely with healthcare providers to monitor potential side effects and adjust the treatment plan accordingly. By effectively managing Traps syndrome with the appropriate medications, individuals can alleviate symptoms, reduce flare-ups, and lead fulfilling lives.
Lifestyle Modifications For Traps Syndrome
Traps Syndrome is a rare genetic disorder that affects the skeletal muscles. It is characterized by episodes of muscle pain and stiffness, which can be triggered by various factors such as stress, cold temperatures, or physical exertion. While there is no cure for Traps Syndrome, there are certain lifestyle modifications that individuals can adopt to help manage their symptoms and improve their quality of life.
One important lifestyle modification for individuals with Traps Syndrome is regular exercise. Engaging in low-impact exercises, such as swimming or yoga, can help improve muscle flexibility and reduce the frequency and severity of muscle pain episodes. It is essential to consult with a healthcare professional or a physical therapist to develop an exercise routine suitable for your specific condition.
Additionally, stress management techniques can play a crucial role in managing Traps Syndrome symptoms. Stress has been known to trigger muscle pain episodes in individuals with Traps Syndrome. Therefore, incorporating relaxation techniques, such as deep breathing exercises or meditation, into your daily routine can help reduce stress levels and potentially minimize symptom flare-ups.
Furthermore, maintaining a healthy and balanced diet is important for managing Traps Syndrome. Consuming foods rich in antioxidants, such as fruits and vegetables, can help reduce inflammation in the muscles and support overall muscle health. It is also advisable to limit the intake of processed and high-fat foods, as they may contribute to inflammation and worsen symptoms.
In conclusion, individuals with Traps Syndrome can make certain lifestyle modifications to help manage their symptoms and improve their overall well-being. Regular exercise, stress management techniques, and a healthy diet can all play a significant role in minimizing symptom flare-ups and maximizing quality of life. It is crucial to work closely with healthcare professionals to develop a personalized plan that suits your specific needs and condition.
Potential Complications Of Traps Syndrome
Traps Syndrome, also known as TNF receptor-associated periodic syndrome, is a rare autoinflammatory disorder that affects multiple systems in the body.
Read the full article
0 notes
Text
Saethre chotzen syndrome

Saethre Chotzen Syndrome, also known as acrocephalosyndactyly type III, is a rare genetic disorder that affects the development of the skull, face, and limbs. This blog post will provide an overview of this syndrome, including its causes, common symptoms, and the effects it has on the affected individual's neurological and cognitive functions. Additionally, we will explore the various diagnostic and genetic testing methods used, as well as the available treatment options and surgical interventions. Furthermore, we will discuss the long-term outlook and prognosis, along with the latest research and advances in understanding and managing Saethre Chotzen Syndrome. Lastly, we will explore the support and resources available to families dealing with this condition.
What Is Saethre Chotzen Syndrome?
Saethre Chotzen Syndrome, also known as ACS III (Acrocephalosyndactyly Type 3), is a rare genetic disorder characterized by distinctive facial and cranial features, finger and toe abnormalities, and potentially other developmental issues. This syndrome is named after the two doctors who first described it in the 1930s - David Saethre and Robert J. Chotzen.
People with Saethre Chotzen Syndrome typically have abnormalities in the bones of the skull and face, which can lead to a misshapen head and a unique appearance. Some of the common facial features associated with this condition include a low hairline on the forehead, droopy eyelids, small and abnormally shaped ears, and a broad, flat nose. Additionally, individuals with Saethre Chotzen Syndrome may have fused or webbed fingers and toes, a condition known as syndactyly.
Diagnosing Saethre Chotzen Syndrome often involves physical examinations by medical professionals familiar with the disorder, as well as genetic testing. The characteristic features and distinctive craniofacial abnormalities observed in individuals with Saethre Chotzen Syndrome can aid in diagnosis. Genetic testing, such as DNA analysis, can also confirm the presence of specific mutations in genes associated with this syndrome.
Causes Of Saethre Chotzen Syndrome
Saethre Chotzen Syndrome, also known as ACS1, is a rare genetic disorder that affects the development of the skull and other parts of the body. It is caused by mutations in the TWIST1 gene, which is responsible for regulating the growth and development of various tissues in the body. These mutations can be inherited from one or both parents, or they can occur spontaneously during the formation of reproductive cells or early in fetal development.
One of the main causes of Saethre Chotzen Syndrome is the mutation in the TWIST1 gene. This gene provides instructions for making a protein that is involved in early development and plays a critical role in the formation of the skull and bones of the face. When there is a mutation in this gene, it disrupts the normal development of these structures, leading to the characteristic features and symptoms of Saethre Chotzen Syndrome.
In some cases, the mutation in the TWIST1 gene is inherited from one or both parents. This means that the parents may also have Saethre Chotzen Syndrome or carry a mutated copy of the gene without showing any symptoms. In other cases, the mutation occurs spontaneously during the formation of reproductive cells or early in fetal development. This spontaneous mutation is not inherited and usually happens by chance.
It is important to note that not everyone with a mutation in the TWIST1 gene will develop Saethre Chotzen Syndrome. The severity of the syndrome can vary widely among affected individuals, even within the same family. This is due to the complex interaction between genetic and environmental factors that influence the manifestation of the syndrome.
Causes of Saethre Chotzen Syndrome
Mutation in the TWIST1 gene
Inheritance from one or both parents
Spontaneous mutation during reproductive cell formation or early fetal development
Interaction between genetic and environmental factors
While the specific causes of Saethre Chotzen Syndrome are still being researched, understanding the role of the TWIST1 gene and its mutations has provided valuable insights into the development of this disorder. Further research is needed to uncover additional factors that contribute to the variability and severity of the syndrome.
Common Symptoms And Features
Saethre Chotzen Syndrome, also known as ACS III, is a rare genetic disorder characterized by distinctive craniofacial and skeletal abnormalities. This condition affects about 1 in 25,000 to 50,000 individuals worldwide. The syndrome is caused by mutations in the TWIST1 gene and is typically inherited in an autosomal dominant pattern, meaning one affected parent can pass the condition to their children. However, in some cases, the mutations may occur sporadically without a family history.
One of the key features of Saethre Chotzen Syndrome is craniosynostosis, which is the premature fusion of the skull bones. This fusion can lead to an abnormal head shape, resulting in a high prominent forehead, a flat or elongated back of the head, and an asymmetrical face. Moreover, individuals with this syndrome often have low-set ears, widely spaced eyes (hypertelorism), and ptosis (droopy eyelids). Additionally, they may experience dental abnormalities such as malocclusion and a narrow palate.
In addition to the craniofacial abnormalities, Saethre Chotzen Syndrome also presents with skeletal anomalies. These may include fusion of certain bones in the hands and feet, such as the toes and fingers. Some individuals may have unusually broad thumbs and great toes, while others may have abnormalities of the spine, such as scoliosis or other vertebral malformations. It is important to note that the severity and combination of features can vary widely among individuals with Saethre Chotzen Syndrome.
Furthermore, individuals with Saethre Chotzen Syndrome may experience developmental delays and intellectual disabilities to varying degrees. Some individuals may have normal intelligence, while others may have learning difficulties or intellectual disabilities. Moreover, this condition can also affect the neurological system, leading to changes in muscle tone and coordination. Speech and language delays are also common in affected individuals, which may require speech therapy or other forms of supportive intervention.
Overall, early diagnosis and intervention are crucial for individuals with Saethre Chotzen Syndrome. Monitoring the growth and development of affected individuals is important to ensure appropriate medical management and therapeutic interventions. Genetic testing can confirm the presence of TWIST1 gene mutations and assist in making an accurate diagnosis. It is also important for affected individuals and their families to seek support and resources from organizations specializing in rare genetic disorders. With advancements in medical research and ongoing support, individuals with Saethre Chotzen Syndrome can lead fulfilling lives and reach their full potential.
Diagnosis And Genetic Testing
Diagnosis and Genetic Testing
Diagnosing Saethre Chotzen Syndrome can be a complex process, as its symptoms can vary widely in severity and presentation. However, early diagnosis is essential for effective management and treatment. Genetic testing plays a crucial role in confirming the presence of Saethre Chotzen Syndrome. It involves analyzing the DNA to identify any specific mutations or changes in certain genes associated with the condition.
One of the genes most commonly linked to Saethre Chotzen Syndrome is the TWIST1 gene. Mutations in this gene are found in approximately 75% of individuals diagnosed with the condition. Genetic testing can help identify these mutations and provide definitive answers regarding the presence of the syndrome. Additionally, other genes such as FGFR1 and FGFR2 may also be analyzed, as mutations in these genes have been associated with certain cases of Saethre Chotzen Syndrome.
When considering genetic testing, it is important to consult with a healthcare professional or genetic counselor who specializes in genetic disorders. They can guide individuals and families through the process, explain the potential benefits and limitations of testing, and provide support and guidance throughout the diagnostic journey. Genetic testing may involve a blood sample or a saliva sample, which is then sent to a laboratory for analysis.
- Genetic testing plays a crucial role in confirming the presence of Saethre Chotzen Syndrome.
- The TWIST1 gene is commonly associated with Saethre Chotzen Syndrome, and mutations in this gene can be identified through genetic testing.
- Consulting with a healthcare professional or genetic counselor is important when considering genetic testing, as they can provide support and guidance throughout the diagnostic process.
Advantages of Genetic Testing for Saethre Chotzen Syndrome Diagnosis
Limitations of Genetic Testing for Saethre Chotzen Syndrome Diagnosis
- Provides a definitive diagnosis
- Not all mutations associated with Saethre Chotzen Syndrome may be detected
- Enables early intervention and management
- Testing may not be readily accessible or covered by insurance
- Assists in genetic counseling and family planning
- Results may reveal unexpected genetic findings unrelated to Saethre Chotzen Syndrome
Effect Of Saethre Chotzen On The Skull
Saethre Chotzen syndrome, also known as acrocephalosyndactyly type III, is a rare genetic disorder that affects the development of the skull. It is characterized by the premature fusion of certain skull bones, leading to an abnormal shape of the head and face. The condition is named after the two doctors who first described it in the medical literature, Saethre and Chotzen.
One of the primary effects of Saethre Chotzen syndrome is the impact it has on the skull. The premature fusion of the skull bones, particularly the sutures between them, can result in an abnormally shaped skull. This typically leads to a condition known as craniosynostosis, in which the skull does not grow properly and becomes distorted. The most common skull abnormalities in Saethre Chotzen syndrome include a high, prominent forehead (also known as "turricephaly"), a triangular-shaped head, and a flattened back of the head.
The fusion of the skull bones can also cause a variety of other issues. In some cases, it can lead to restricted growth of the brain, resulting in a smaller than average head size (microcephaly). This can have implications for neurological development and function. Additionally, the irregular shape of the skull can cause uneven pressure on the brain, potentially leading to cognitive and neurological impairments.
Neurological And Cognitive Impacts
Saethre Chotzen Syndrome is a rare genetic disorder characterized by various physical and developmental abnormalities. While the primary features of this syndrome revolve around craniofacial and skeletal deformities, it is important to understand the neurological and cognitive impacts it can have on individuals affected by it. The disorder affects the normal development of the brain, resulting in a range of neurological and cognitive difficulties that can vary in severity from person to person.
One of the key neurological impacts of Saethre Chotzen Syndrome is intellectual disability. Many individuals with this condition may experience challenges in learning, reasoning, problem-solving, and acquiring new skills. The extent of intellectual disability can vary, with some individuals having mild to moderate difficulties, while others may have more severe cognitive impairments. The cognitive impacts can significantly impact a person's daily life, educational opportunities, and overall quality of life.
In addition to intellectual disabilities, individuals with Saethre Chotzen Syndrome may also exhibit attention deficit hyperactivity disorder (ADHD). ADHD can cause difficulties in maintaining attention, impulsiveness, and hyperactivity. This can further complicate the learning process and overall cognitive functioning. It is essential for individuals with Saethre Chotzen Syndrome to receive appropriate support and interventions to manage these cognitive impacts effectively.
Neurological and Cognitive Impacts of Saethre Chotzen Syndrome:
- Intellectual Disability: Difficulty in learning, reasoning, problem-solving, and acquiring new skills.
- Attention Deficit Hyperactivity Disorder (ADHD): Difficulties in maintaining attention, impulsiveness, and hyperactivity.
Treatment Options And Management
Treatment options and management play a crucial role in addressing Saethre Chotzen syndrome, a rare genetic disorder that affects the development of the skull and other parts of the body. As there is no cure for Saethre Chotzen syndrome, the goal of treatment is to manage the symptoms and improve the quality of life for individuals with this condition. The treatment plan typically involves a multidisciplinary approach, including the coordination of various healthcare professionals such as geneticists, orthopedic surgeons, craniofacial specialists, and speech therapists.
One of the primary treatment options for Saethre Chotzen syndrome involves surgery. Surgical interventions aim to address the skeletal abnormalities and craniofacial deformities associated with the condition. These procedures may include cranial vault remodeling, forehead advancement, orbital rim advancement, and osteotomies. The specific surgical interventions required depend on the severity of the individual's symptoms and their unique needs. Surgical treatments are usually performed during infancy or early childhood to promote optimal growth and development.
In addition to surgical interventions, supportive therapies play an essential role in managing Saethre Chotzen syndrome. Physical therapy helps individuals improve their motor skills and range of motion. Occupational therapy focuses on enhancing daily living skills, such as self-care and fine motor skills. Speech therapy assists individuals with speech and language difficulties that may arise due to craniofacial abnormalities. These supportive therapies are tailored to the individual's specific needs and are typically integrated into their overall treatment plan.
Genetic counseling is critical for families affected by Saethre Chotzen syndrome. As it is an inherited condition, understanding the genetic aspects and recurrence risks can help families make informed decisions. Genetic testing, such as DNA sequencing and gene analysis, can assist in confirming the diagnosis and identifying the specific genetic mutation responsible for the syndrome. This information can aid in assessing the likelihood of the condition occurring in future pregnancies and guide family planning decisions.
Treatment Options And Management:
Surgery:
Addresses skeletal abnormalities and craniofacial deformities.
Supportive Therapies:
Includes physical, occupational, and speech therapies to enhance different aspects of development and daily living skills.
Genetic Counseling:
Provides information on the genetic aspects of the syndrome and recurrence risks, aiding in family planning decisions.
While treatment options and management strategies can improve the overall well-being of individuals with Saethre Chotzen syndrome, it is important to note that every case is unique. The effectiveness of treatments can vary depending on the severity of the condition, individual response, and the timely implementation of interventions. Ongoing research and advances in medical technologies continue to enhance our understanding of Saethre Chotzen syndrome, providing hope for improved treatment outcomes and prognosis in the future.
Surgical Interventions For Saethre Chotzen
When it comes to Saethre Chotzen Syndrome, surgical interventions play a crucial role in managing and improving the condition. Saethre Chotzen Syndrome is a rare genetic disorder characterized by craniofacial and skeletal abnormalities. It is caused by mutations in the TWIST1 gene, which is responsible for regulating the development of bones and other tissues in the body.
Surgical interventions for Saethre Chotzen Syndrome aim to correct the physical features and functional impairments associated with the condition. One key aspect of surgical intervention is cranial vault remodeling, which involves reshaping the skull to address abnormalities such as craniosynostosis. Craniosynostosis is a condition where the skull bones fuse prematurely, leading to abnormal growth patterns and potentially affecting brain development.
In addition to cranial vault remodeling, individuals with Saethre Chotzen Syndrome may also undergo surgical procedures to address other skeletal abnormalities. This can include procedures to correct jaw malformations, such as mandibular distraction, which gradually lengthens and repositions the lower jaw to improve facial balance and function. Orthognathic surgery is another common procedure that aims to correct the alignment of the jaw and teeth.
- Another aspect of surgical intervention in Saethre Chotzen Syndrome involves addressing potential eye abnormalities. Strabismus correction, also known as eye muscle surgery, can help improve eye alignment and coordination. This procedure involves adjusting the muscles in the eye to ensure both eyes are working together effectively.
- Table placement guidance in Saethre Chotzen Syndrome can be required in certain cases where the individual has difficulties with spinal alignment. Spinal fusion surgery may be recommended to correct any abnormalities in the spine, such as scoliosis or kyphosis. This procedure involves fusing the affected vertebrae to promote stability and alignment.
- It is important to note that each individual with Saethre Chotzen Syndrome will have unique surgical needs based on their specific symptoms and overall condition. Therefore, a comprehensive evaluation by a team of specialists, including craniofacial surgeons, orthopedic surgeons, ophthalmologists, and other healthcare professionals, is crucial to determine the most appropriate surgical interventions for each individual.
Procedure
Purpose
Cranial vault remodeling
Reshaping the skull to address craniosynostosis and improve brain development
Mandibular distraction
Lengthening and repositioning the lower jaw to improve facial balance and function
Orthognathic surgery
Correcting jaw and teeth alignment
Strabismus correction
Improving eye alignment and coordination
Spinal fusion surgery
Correcting spinal abnormalities such as scoliosis or kyphosis
In conclusion, surgical interventions for Saethre Chotzen Syndrome play a crucial role in addressing the physical and functional challenges associated with this genetic disorder.
Read the full article
0 notes
Text
IPT therapy

Welcome to our blog post on IPT therapy! In this article, we will explore the ins and outs of this unique therapeutic approach, shedding light on its history, principles, and how it works. We will also discuss common indications for IPT therapy, the benefits it offers, and the role of the therapist in this process. Additionally, we will delve into combined approaches with IPT therapy, potential side effects to be aware of, and share some inspiring success stories. Supported by research and evidence, we will aid you in choosing a qualified IPT therapist. Let's get started!
What Is Ipt Therapy?
What Is IPT Therapy?
IPT therapy, short for Interpersonal Psychotherapy, is a form of psychotherapy that focuses on resolving interpersonal issues and improving communication skills. It is a time-limited treatment approach that typically lasts for 12-16 weeks, although the duration can vary depending on individual needs. IPT therapy is based on the principle that our relationships and interactions with others significantly impact our mental health and well-being.
During IPT therapy, the therapist works closely with the individual to identify and address specific interpersonal problems that may be causing distress. This form of therapy helps individuals understand how their thoughts, emotions, and behaviors are interconnected with their relationships, leading to insight and positive changes in their lives.
The History Of Ipt Therapy
The history of Interpersonal Psychotherapy (IPT) therapy dates back to the 1970s when it was developed by Gerald L. Klerman and Myrna Weissman. Initially, IPT was designed to treat depression, but over time its applications have expanded to other mental health conditions. Klerman and Weissman aimed to develop a time-limited therapy that focused on the interpersonal relationships of the individual, as they believed that such relationships play a significant role in mental health and well-being.
During its early years, IPT therapy primarily focused on treating acute depression. However, as research and practice evolved, it became evident that IPT had applications beyond depression. The therapy approach drew from various theories, including psychodynamic, cognitive-behavioral, and systems theories. This integrative approach allowed practitioners to tailor the therapy to the specific needs and goals of each individual.
Throughout the years, IPT therapy has been refined and adapted to address a wide range of mental health conditions. It has proven effective in the treatment of mood disorders such as major depressive disorder and bipolar disorder. Additionally, IPT has been utilized to address anxiety disorders, eating disorders, substance abuse, and interpersonal difficulties.
One crucial development in the history of IPT therapy was the recognition of its efficacy as a short-term therapy. Unlike traditional psychodynamic therapy that can extend for several years, IPT is time-limited, typically lasting for 12-16 sessions. This brief duration makes it more accessible and cost-effective for many individuals seeking therapeutic intervention.
The Principles Of Ipt Therapy
When it comes to understanding Interpersonal Psychotherapy (IPT) therapy, it is important to delve into the principles that underpin this approach. Developed in the 1970s by Gerald Klerman and Myrna Weissman, IPT therapy is a time-limited, evidence-based treatment for a range of mental health conditions. The principles of IPT therapy shape the therapeutic process and guide both the therapist and the client towards achieving effective outcomes.
The first principle of IPT therapy is the focus on the current interpersonal problems of the client. Rather than delving extensively into the past, IPT therapy primarily emphasizes the present. The therapist and the client work together to identify specific difficulties in their social interactions, relationships, or roles that are contributing to the client's emotional distress. By addressing these current issues, IPT therapy aims to facilitate changes in the client's interpersonal functioning and alleviate their symptoms.
The second principle of IPT therapy revolves around the idea that interpersonal relationships and events have a significant impact on mental health. IPT therapy recognizes the interconnectedness between individuals and their social environment. It acknowledges that life events such as bereavement, relationship conflicts, or transitions can trigger or worsen mental health conditions. By exploring and understanding these interpersonal factors, IPT therapy aims to help clients make sense of their emotional experiences and develop healthier ways of relating to others.
The third principle of IPT therapy involves identifying and addressing specific problem areas within the client's interpersonal functioning. IPT therapy targets four main areas: grief, role disputes, role transitions, and interpersonal deficits. The therapist, in collaboration with the client, assesses which problem area(s) are most relevant to the client's symptoms and focuses the therapy accordingly. By addressing these problem areas through various therapeutic techniques and interventions, IPT therapy aims to improve the client's overall well-being and interpersonal functioning.
How Does Ipt Therapy Work?
IPT therapy, also known as Interpersonal Psychotherapy, is a short-term, evidence-based therapy approach that aims to help individuals improve their interpersonal relationships and overall psychological well-being. It focuses on addressing specific problems within the context of relationships and aims to enhance communication, understanding, and emotional connection between individuals. In this blog post, we will explore how IPT therapy works and the different techniques used in this therapeutic approach.
One of the key principles of IPT therapy is the recognition that our relationships significantly impact our mental health. The therapy is grounded on the belief that unresolved issues, conflicts, or difficulties in interpersonal relationships can contribute to emotional distress and the development of psychological symptoms. By addressing these interpersonal problems, IPT therapy aims to alleviate symptoms and improve mental well-being.
During an IPT therapy session, the therapist and the client collaboratively identify specific problem areas within their relationships. These can range from conflicts with a partner, difficulties with friends or family members, or even problems in professional relationships. The therapist then helps the client gain insight into how these problems may be related to their symptoms or emotional distress.
- This is an example of a list item using the li html tag.
Technique
Description
Interpersonal Inventory
This technique involves exploring the client's interpersonal history, identifying significant relationships, and assessing patterns or themes that may contribute to their current difficulties.
Role-Playing
In some cases, the therapist may use role-playing exercises to help the client practice new communication skills, resolve conflicts, or express their needs and emotions effectively.
Communication Analysis
In this technique, the therapist helps the client analyze their communication patterns within a specific relationship to identify maladaptive or ineffective patterns and develop healthier communication strategies.
Grief and Loss Work
If the client is experiencing grief or loss, IPT therapy provides a safe space for them to process their emotions, express their feelings, and gradually adjust to the changes in their relationships and life circumstances.
IPT therapy emphasizes the importance of building a strong therapeutic alliance between the therapist and the client. The therapist offers empathy, understanding, and support to create a safe environment where the client feels comfortable exploring and understanding their interpersonal issues. By working collaboratively, the therapist and client can develop strategies and solutions to improve their relationships and enhance the client's emotional well-being.
In conclusion, IPT therapy is a powerful therapeutic approach that focuses on the role of relationships in our mental health. By addressing interpersonal issues and improving communication skills, individuals can experience relief from symptoms and develop healthier relationships. Although each person's experience with IPT therapy may vary, the evidence supporting its effectiveness is significant, making it a valuable option for those seeking to improve their psychological well-being.
Common Indications For Ipt Therapy
Introduction: IPT therapy, also known as Interpersonal Psychotherapy, is a highly effective and evidence-based form of treatment for various mental health conditions. It focuses on improving interpersonal relationships and resolving emotional difficulties. In this blog post, we will discuss some of the common indications for IPT therapy and how it can be beneficial for individuals seeking professional help.
1. Depression:
IPT therapy has been widely used as a treatment for depression. It recognizes that various interpersonal issues can contribute to the development and maintenance of depressive symptoms. By addressing these issues, individuals are able to rebuild their relationships, improve communication skills, and ultimately alleviate depressive symptoms. IPT therapy can be particularly helpful for those experiencing relationship conflicts, role transitions, or unresolved grief.
2. Anxiety Disorders:
Many individuals with anxiety disorders also benefit from IPT therapy. It helps them identify and understand how their interpersonal relationships and social interactions impact their anxiety. By exploring these dynamics, IPT therapy assists individuals in developing healthier coping strategies and creating more meaningful connections with others. It can be especially useful for individuals with social anxiety disorder, generalized anxiety disorder, or specific phobias.
3. Eating Disorders:
IPT therapy has proven effective in treating various eating disorders, such as anorexia nervosa, bulimia nervosa, and binge eating disorder. It focuses on addressing the interpersonal difficulties and conflicts that contribute to disordered eating behaviors. By enhancing communication skills and strengthening relationships, IPT therapy can support individuals in their journey towards recovery and lasting change.
4. Postpartum Depression:
Postpartum depression is a serious mental health condition that affects many new mothers. IPT therapy provides a safe and supportive space for women to explore the changes and challenges associated with motherhood. By addressing issues related to role transitions, interpersonal conflicts, and major life changes, IPT therapy can greatly assist in the treatment of postpartum depression and facilitate the bonding process between mother and child.
Conclusion:
While IPT therapy can be beneficial for a wide range of mental health conditions, these are just a few common indications. It is essential to consult with a qualified IPT therapist to determine whether this therapy is suitable for your specific needs. By addressing interpersonal issues, improving communication skills, and fostering healthier relationships, IPT therapy offers individuals a valuable opportunity for personal growth and lasting change.
Benefits Of Ipt Therapy
In today's blog post, we will explore the benefits of IPT therapy. IPT stands for Interpersonal Psychotherapy, which is a form of psychotherapy that focuses on the way interpersonal relationships and social interactions impact a person's mental health. Through a structured and time-limited approach, IPT therapy aims to help individuals better understand and manage their emotions and relationships, ultimately leading to improved mental well-being.
One of the key benefits of IPT therapy is its effectiveness in treating various mental health conditions. Research has shown that IPT therapy can be particularly beneficial for individuals facing depression, anxiety disorders, post-traumatic stress disorder (PTSD), and eating disorders. By focusing on the interpersonal issues contributing to these conditions, IPT therapy helps individuals gain insight into their feelings, thoughts, and behaviors within their relationships, leading to symptom reduction and improved coping strategies.
Another benefit of IPT therapy is its practical and goal-oriented approach. Unlike traditional talk therapy, IPT therapy is a structured form of treatment that typically takes place over a fixed number of sessions. This structured nature allows therapists and clients to work together in a focused manner, setting specific goals and addressing targeted interpersonal issues. This goal-oriented approach not only helps clients feel more empowered and motivated, but it also provides a sense of direction and progress throughout the therapy process.
- IPT therapy also emphasizes the importance of social support. The therapist helps clients identify and foster supportive relationships in their lives, which can have a positive impact on their overall mental health. This focus on social support networks can help individuals strengthen their existing relationships or develop new ones, ultimately leading to increased feelings of connection, belonging, and emotional support.
- IPT therapy is a collaborative process. The therapist and the client work together as a team, developing a strong therapeutic alliance based on trust, empathy, and mutual respect. This collaborative approach allows clients to actively participate in their own treatment, making them feel more engaged and invested in the therapeutic process.
Benefit
Description
Improved Communication Skills
IPT therapy focuses on improving communication patterns within relationships. Through therapy, individuals can learn effective communication skills such as active listening, assertiveness, and conflict resolution, which can enhance their overall interpersonal interactions.
Enhanced Problem-Solving Abilities
IPT therapy helps individuals identify and address specific problems within their relationships. By exploring different perspectives and generating potential solutions, individuals can develop effective problem-solving skills that can be applied not only in their current relationships but also in future situations.
Increased Emotional Resilience
By exploring their emotions and the impact of interpersonal relationships, individuals undergoing IPT therapy can develop greater emotional resilience. They gain a better understanding of their emotional triggers and learn coping mechanisms to manage and regulate their emotions in a healthier way.
In conclusion, IPT therapy offers numerous benefits for individuals struggling with various mental health conditions. Through its focus on interpersonal relationships, structured approach, emphasis on social support, collaboration, and development of important skills, individuals can experience improved mental well-being and enhanced quality of life. If you are considering therapy and are interested in exploring the benefits of IPT therapy, it is important to consult a qualified IPT therapist to assess if this approach is suitable for your needs.
The Role Of The Therapist In Ipt Therapy
When undergoing IPT therapy, it is important to recognize the crucial role that the therapist plays in the process. The therapist in IPT therapy serves as a guide, a facilitator, and a support system for the individual seeking treatment. They are trained professionals who possess a deep understanding of the therapy's principles and techniques. As such, they are responsible for creating a safe and nonjudgmental environment that encourages open communication and trust between the therapist and the client.
In IPT therapy, the role of the therapist is multi-faceted. Firstly, the therapist conducts an initial assessment to better understand the client's unique circumstances and determine if IPT therapy is the appropriate course of treatment. This assessment involves gathering information about the client's personal history, symptoms, and any current stressors or life events that may be contributing to their distress.
Once the therapy begins, the therapist takes on the role of a collaborator. They work together with the client to identify specific problem areas or interpersonal conflicts that are causing emotional difficulties. By using a structured approach, the therapist helps the client recognize patterns in their relationships and explores alternative ways of managing these challenges.
Combined Approaches With Ipt Therapy
Combined Approaches With IPT Therapy
IPT therapy, or Interpersonal Psychotherapy, is a form of psychotherapy that focuses on improving interpersonal relationships and resolving interpersonal problems. It is based on the premise that interpersonal difficulties can contribute to the development and maintenance of mental health issues, such as depression and anxiety. IPT therapy is an evidence-based treatment that has been shown to be effective in various populations. However, in some cases, a combined approach may be necessary to enhance the effectiveness of IPT therapy.
One approach that can be combined with IPT therapy is medication management. While IPT therapy primarily focuses on improving interpersonal functioning, medication can be used to target specific symptoms associated with mental health issues. For example, in the treatment of depression, antidepressant medications may be prescribed in conjunction with IPT therapy to address the biological factors contributing to the individual's symptoms.
Another approach that can be combined with IPT therapy is cognitive-behavioral therapy (CBT). CBT is a form of therapy that emphasizes the connection between thoughts, feelings, and behaviors. By incorporating CBT techniques into IPT therapy, individuals can gain a better understanding of how their thoughts and beliefs influence their interpersonal interactions. This can help them develop more effective communication skills and improve their relationships.
In addition to medication management and CBT, IPT therapy can also be combined with other complementary therapies, such as mindfulness meditation or art therapy. These approaches can help individuals develop greater self-awareness, reduce stress, and enhance their overall well-being. By incorporating these complementary therapies into IPT therapy, individuals can benefit from a holistic treatment approach that addresses their emotional, psychological, and physical needs.
Read the full article
0 notes
Text
Holistic therapy

Holistic therapy has gained significant popularity in recent years as a natural and comprehensive approach to healing and well-being. In this blog post, we will explore the various aspects of holistic therapy, its benefits, and how it promotes emotional well-being. We will delve into the mind-body connection and the different modalities of holistic therapy that can be utilized. Additionally, we will discuss the role of nutrition, energy work, and Reiki in this therapeutic approach, as well as its effectiveness in pain management and stress reduction. Furthermore, we will explore how to integrate holistic therapy with traditional medicine and create a personalized holistic therapy plan. Lastly, we will provide guidance on choosing a qualified holistic therapist.
Introduction To Holistic Therapy
Welcome to our blog post on an introduction to holistic therapy. Holistic therapy is an alternative approach to health and wellness that takes into consideration the whole person – mind, body, and spirit. It focuses on treating the individual as a whole, rather than just the symptoms of a particular ailment. Holistic therapy aims to promote overall well-being and restore balance in one's life.
One of the key concepts in holistic therapy is the belief that the mind and body are interconnected. This means that our mental and emotional states can have a direct impact on our physical health, and vice versa. By addressing both the physical and emotional aspects, holistic therapy seeks to achieve a balanced and harmonious state of being.
There are various modalities or approaches within holistic therapy. Some common ones include acupuncture, aromatherapy, massage therapy, meditation, and yoga. Each modality has its own set of techniques and principles, but they all share the common goal of promoting holistic well-being.
- Acupuncture - This ancient Chinese practice involves the insertion of thin needles at specific points on the body to stimulate energy flow and restore balance.
- Aromatherapy - The use of essential oils derived from plants to promote relaxation, reduce stress, and improve mental and emotional well-being.
- Massage therapy - The manipulation of soft tissues to improve circulation, relieve muscle tension, and promote relaxation and overall well-being.
Benefits of Holistic Therapy
Understanding the Mind-Body Connection
Exploring Different Holistic Therapy Modalities
1. Promotes overall well-being
1. Interconnectedness of mind and body
1. Acupuncture
2. Restores balance in life
2. Impact of mental and emotional states on physical health
2. Aromatherapy
Benefits Of Holistic Therapy
When it comes to taking care of our health and well-being, it is important to consider a comprehensive approach that takes into account all aspects of our being. This is where holistic therapy comes in. Holistic therapy focuses on treating the individual as a whole, rather than just addressing their physical symptoms. It recognizes the interconnectedness of the mind, body, and spirit, and aims to achieve balance and harmony in all areas of a person's life.
One of the key benefits of holistic therapy is its emphasis on prevention rather than just treatment. Unlike conventional medicine, which often focuses on managing symptoms after they arise, holistic therapy aims to prevent disease and health issues before they occur. By addressing the underlying causes of illness, rather than just suppressing symptoms, holistic therapy can help individuals achieve and maintain optimal health.
Another advantage of holistic therapy is its ability to empower individuals to take an active role in their own healing process. Holistic therapists work closely with their clients to understand their unique needs and develop personalized treatment plans. These plans may include a combination of therapies such as acupuncture, herbal medicine, massage, and meditation. By actively participating in their own healing journey, individuals can gain a deeper understanding of their bodies and take steps towards self-improvement.
- A holistic approach to therapy also supports emotional well-being. Traditional forms of therapy often focus solely on the mind, neglecting the body and spirit. Holistic therapy, on the other hand, recognizes the powerful connection between the mind and body and aims to address both. By incorporating modalities such as yoga and mindfulness into therapy sessions, individuals can learn to manage stress, regulate emotions, and improve overall mental well-being.
The integration of nutrition in holistic therapy
is yet another benefit worth mentioning. Proper nutrition plays a vital role in our overall health and well-being. Holistic therapy takes this into account and emphasizes the importance of a balanced diet to support the body's natural healing processes. By making mindful food choices, individuals can enhance their energy levels, improve digestion, and maintain a healthy weight.
In conclusion, holistic therapy offers a wide range of benefits for individuals seeking a comprehensive approach to healthcare. By considering the mind, body, and spirit, holistic therapy aims to achieve balance and harmony in all areas of life. It promotes prevention, empowers individuals to take an active role in their healing process, supports emotional well-being, and integrates nutrition as a vital component of overall health. If you are looking for a more holistic approach to your well-being, consider exploring the various modalities of holistic therapy and see how it can transform your life.
Understanding The Mind-Body Connection
Understanding the Mind-Body Connection
The mind-body connection is a fundamental concept in holistic therapy that recognizes the intricate interplay between our mental and physical well-being. It emphasizes the idea that our thoughts, emotions, and beliefs can significantly impact our overall health and vice versa. By nurturing this connection, individuals can attain a state of balance and well-being that promotes optimal health and vitality.
One of the key principles of the mind-body connection is the belief that our thoughts and emotions can influence our physical health. For example, stress, anxiety, and negative thinking patterns can manifest as physical symptoms such as headaches, digestive issues, or muscle tension. Conversely, positive emotions, a calm mind, and a optimistic outlook can contribute to a healthier body and a stronger immune system.
Furthermore, the mind-body connection encompasses the understanding that physical ailments and imbalances can have an impact on our mental and emotional state. Chronic pain, for instance, can lead to feelings of frustration, sadness, or even depression. By addressing the physical aspect of the condition alongside the emotional and mental components, a holistic approach aims to treat the root cause of the issue rather than just the symptoms.
By acknowledging the mind-body connection, holistic therapy seeks to integrate various techniques and modalities that address both the mental and physical aspects of well-being. This can include practices such as mindfulness meditation, yoga, breathwork, and cognitive-behavioral therapy. These approaches help individuals cultivate self-awareness, manage stress, and develop a positive mindset, all contributing to their overall health and well-being.
- Mindfulness meditation: Regular practice of mindfulness meditation can enhance the mind-body connection by promoting self-awareness, reducing stress, and improving emotional well-being.
- Yoga: Yoga combines physical postures, breathing exercises, and meditation to align the body and mind. It promotes flexibility, relaxation, and mental clarity.
- Cognitive-behavioral therapy: This therapy focuses on identifying and challenging negative thought patterns and beliefs that contribute to emotional distress. By replacing them with positive and rational thoughts, it can improve mental and emotional well-being.
Benefits of the Mind-Body Connection
1. Enhanced overall well-being and quality of life.
2. Improved management of stress and anxiety.
3. Better physical health and immunity.
4. Increased self-awareness and emotional intelligence.
5. Decreased risk of chronic illnesses and diseases.
Understanding the mind-body connection is crucial for achieving holistic health and well-being. By recognizing the intricate relationship between our thoughts, emotions, and physical health, we can embrace a comprehensive approach that treats the whole person. By incorporating practices such as mindfulness meditation, yoga, and cognitive-behavioral therapy, individuals can nurture and strengthen the mind-body connection, resulting in improved overall health and vitality.
Exploring Different Holistic Therapy Modalities
When it comes to holistic therapy, there are a wide range of modalities and techniques that can be employed to address various physical and emotional issues. Holistic therapy takes a comprehensive approach to healing, focusing on the whole person - mind, body, and spirit. By treating the underlying causes of health problems rather than just the symptoms, holistic therapy offers a more holistic and long-lasting solution. In this blog post, we will explore some of the different holistic therapy modalities that are commonly used.
Massage Therapy: One of the most well-known holistic therapy modalities is massage therapy. This hands-on technique involves the manipulation of soft tissues, such as muscles and connective tissues, to improve circulation, enhance relaxation, and relieve tension. Massage therapy not only helps to reduce stress and promote a sense of well-being, but it can also alleviate pain and improve flexibility. There are various types of massage therapies available, such as Swedish massage, deep tissue massage, and aromatherapy massage, each with its own unique benefits.
Acupuncture: Acupuncture is an ancient Chinese therapy that involves the insertion of thin needles into specific points on the body to restore balance and promote healing. According to traditional Chinese medicine, the body's energy, known as qi, flows along specific pathways called meridians. When the flow of qi is disrupted, it can lead to imbalances and health problems. Acupuncture aims to restore the proper flow of qi and stimulate the body's natural healing mechanisms. This holistic therapy modality has been found to be effective for a wide range of conditions, including pain management, stress reduction, and even infertility.
Aromatherapy: Aromatherapy is a holistic therapy modality that utilizes the powerful scents of essential oils to promote relaxation, improve mood, and enhance overall well-being. Essential oils are extracted from various plants and flowers and can be inhaled, applied topically, or used in massage oils or diffusers. Each essential oil has its own unique properties and can be used to address specific physical or emotional issues. For example, lavender oil is often used for its calming and sleep-promoting effects, while peppermint oil is known for its invigorating and headache-relieving properties.
How Holistic Therapy Promotes Emotional Well-Being
Emotional well-being is a crucial aspect of overall health and happiness. It encompasses our ability to manage stress, cope with daily challenges, and maintain positive relationships. While traditional medicine focuses on treating physical symptoms, holistic therapy takes a comprehensive approach by considering the mind, body, and spirit as interconnected entities. In this blog post, we will explore how holistic therapy promotes emotional well-being and the various techniques and modalities that can support our mental and emotional health.
One of the key principles of holistic therapy is the recognition that emotional well-being is influenced by both internal and external factors. Holistic therapists believe that our thoughts, emotions, and physical sensations are interconnected, and addressing these aspects holistically can promote emotional balance. By addressing the root causes of emotional distress rather than solely focusing on symptom management, holistic therapy aims to provide long-lasting emotional well-being.
One of the primary ways in which holistic therapy promotes emotional well-being is through the use of various techniques and modalities. These methods can include meditation, yoga, breathing exercises, and mindfulness practices. These techniques help individuals develop self-awareness, reduce stress, and cultivate a sense of calm and inner peace. By incorporating these practices into our daily lives, we can enhance emotional resilience and improve our ability to manage challenging emotions.
Another important aspect of holistic therapy is the emphasis on the mind-body connection. Therapists recognize that our physical well-being has a significant impact on our emotions and vice versa. For instance, engaging in regular exercise can release endorphins and improve mood. Similarly, consuming a healthy diet can provide essential nutrients that support brain function and emotional stability. By addressing both physical and emotional aspects, holistic therapy aims to promote overall well-being and enhance emotional health.
- In addition to these techniques, holistic therapy also integrates talk therapy and expressive arts therapy. These forms of therapy offer individuals the opportunity to explore and express their emotions in a safe and supportive environment. Through guided conversations or creative outlets such as music, art, or dance, individuals can gain insights into their emotions and develop healthy coping mechanisms. These therapies can help individuals process difficult experiences, improve self-esteem, and foster personal growth.
Techniques for Emotional Well-Being in Holistic Therapy:
Benefits:
Meditation:
Reduces stress and promotes relaxation
Yoga:
Improves flexibility, reduces anxiety, and enhances emotional well-being
Breathing Exercises:
Calms the mind, regulates emotions, and reduces anxiety
Mindfulness Practices:
Enhances self-awareness, reduces rumination, and promotes emotional balance
Talk Therapy:
Provides a safe space for emotional exploration and personal growth
Expressive Arts Therapy:
Allows individuals to express emotions creatively and facilitate healing
In conclusion, holistic therapy offers a comprehensive approach to emotional well-being by addressing the mind, body, and spirit. By incorporating various techniques and modalities such as meditation, yoga, mindfulness practices, and talk therapy, individuals can cultivate emotional resilience, manage stress, and develop healthy coping mechanisms. Understanding the interconnectedness of our emotions, thoughts, and physical sensations is key to achieving optimal emotional well-being. Whether you are seeking support for specific emotional challenges or simply aiming to enhance your overall well-being, holistic therapy can provide valuable tools and strategies for promoting emotional health.
Holistic Approaches To Pain Management
When it comes to managing pain, many individuals are seeking alternative methods that go beyond traditional medicine. Holistic therapy offers a holistic approach to pain management, addressing not only the physical aspect but also the emotional, mental, and spiritual well-being of an individual. Holistic therapy recognizes that pain is not just a physical sensation but also has a profound impact on our overall health and quality of life.
One of the key benefits of holistic therapy in pain management is its focus on treating the root cause of the pain, rather than just alleviating the symptoms. By addressing the underlying physical, emotional, and mental imbalances, holistic therapy aims to provide long-term relief and healing. This approach acknowledges the interconnectedness of the mind, body, and spirit and seeks to restore balance and harmony within the individual.
There are various holistic therapy modalities that can be utilized in pain management. These modalities include acupuncture, chiropractic care, massage therapy, herbal medicine, meditation, and yoga, among others. Each modality offers unique benefits and can be tailored to meet the specific needs of the individual. For example, acupuncture stimulates specific points on the body to reduce pain and promote the flow of energy, while massage therapy helps to relax tense muscles and improve blood circulation.
The Role Of Nutrition In Holistic Therapy
Nutrition plays a crucial role in holistic therapy, as it recognizes the interconnection between our physical health, mental well-being, and emotional balance. It understands that our bodies are complex systems that require a balance of nutrients to function optimally. By nourishing our bodies with wholesome and nutritious foods, we can support not only our physical health but also enhance our mental and emotional well-being.
In holistic therapy, nutrition is seen as a fundamental component of achieving and maintaining overall wellness. The foods we consume have a direct impact on our energy levels, mood, and cognitive function. By making conscious and mindful choices about what we eat, we can enhance our vitality, boost our immune system, and improve our emotional resilience.
A holistic approach to nutrition goes beyond just focusing on individual nutrients or calories. It emphasizes the importance of eating whole, unprocessed foods that are rich in vitamins, minerals, and antioxidants. These nourishing foods help to support the body's natural healing processes, reduce inflammation, and promote holistic well-being. Additionally, holistic therapists encourage individuals to listen to their bodies, eat mindfully, and develop a positive relationship with food.
The benefits of a holistic approach to nutrition are numerous. By incorporating nutrient-dense foods into our diet, we can experience increased energy, improved digestion, and enhanced cognitive function. Moreover, a balanced and nourishing diet can also help to prevent and manage chronic diseases and mental health conditions. It is important to note that each individual has unique nutritional needs, and a qualified holistic therapist can provide personalized guidance and support.
- Improved Energy Levels: When we fuel our bodies with nutrient-dense foods, we provide the necessary fuel for optimal energy production. A well-balanced diet can help to prevent energy crashes and promote sustained energy levels throughout the day.
- Enhanced Mental Clarity: Certain nutrients, such as omega-3 fatty acids and antioxidants, have been shown to support cognitive function. By including foods rich in these nutrients, such as oily fish, nuts, and berries, we can improve our ability to focus, concentrate, and think clearly.
Read the full article
0 notes
Text
Integrative therapy

Integrative therapy is a holistic approach that integrates various therapeutic techniques to promote overall well-being. In this comprehensive blog post, we will explore the principles, modalities, and benefits of integrative therapy. We will delve into how this therapy works and the different techniques and approaches utilized. Furthermore, we will discuss its applications in addressing mental health, physical health, and emotional well-being. If you are considering integrative therapy, we will also provide guidance on choosing a practitioner. Additionally, we will explore how integrative therapy can complement traditional treatments and present research and evidence supporting its effectiveness.
What Is Integrative Therapy?
Integrative therapy, also known as integrative psychotherapy, is an approach that combines elements from various therapeutic modalities to provide a more comprehensive and personalized treatment for individuals seeking therapy. It takes into account the physical, emotional, mental, and spiritual aspects of a person, recognizing that these aspects are interconnected and influence one another.
Integrative therapy aims to address the root causes of emotional and psychological issues by considering the whole person, rather than focusing solely on symptoms or specific problems. It emphasizes collaboration between the therapist and the client, with the goal of helping clients develop a deeper understanding of themselves and their experiences.
One of the key principles of integrative therapy is that every individual is unique, and therefore, therapy should be tailored to the specific needs and preferences of each person. It allows therapists to draw from a wide range of therapeutic techniques and approaches, such as cognitive-behavioral therapy, psychodynamic therapy, mindfulness-based therapy, and body-based approaches, to create a customized treatment plan that suits the individual.
- The principles behind integrative therapy include:
- Holistic Approach: Integrative therapy considers the whole person, taking into account their physical, emotional, mental, and spiritual well-being.
- Individualized Treatment: Therapy is tailored to meet the unique needs and preferences of the client, allowing for a more personalized and effective treatment.
- Collaborative Relationship: Therapists work together with clients to establish a collaborative and supportive partnership, fostering trust and open communication.
Type of Modality
Description
Cognitive-Behavioral Therapy (CBT)
Focuses on the relationship between thoughts, feelings, and behaviors and aims to reframe negative thoughts and develop healthier coping strategies.
Psychodynamic Therapy
Explores the unconscious mind and past experiences to better understand present-day difficulties and patterns of behavior.
Mindfulness-Based Therapy
Incorporates mindfulness practices and techniques to cultivate present-moment awareness and enhance overall well-being.
Body-Based Approaches (e.g., Somatic Therapy)
Recognizes the connection between the mind and body, using techniques such as movement, breathwork, and body awareness to promote healing.
Integrative therapy can be beneficial for a wide range of conditions, including anxiety, depression, trauma, addiction, eating disorders, and relationship issues. By considering all aspects of a person, it offers a more comprehensive and holistic approach to therapy.
As with any therapy, it is important to choose an integrative therapy practitioner who is well-trained and experienced. It is recommended to do research, read reviews, and consider factors such as their qualifications, expertise, and approach to therapy.
Research and evidence on integrative therapy continue to grow, supporting its effectiveness in improving mental health, emotional well-being, and overall quality of life. Many individuals find integrative therapy to be a valuable tool in their journey towards healing and self-discovery.
The Principles Of Integrative Therapy
Integrative therapy is a holistic approach to healing and wellness that combines various therapeutic modalities and approaches. It incorporates the mind, body, and spirit, recognizing that all aspects of an individual's experience are interconnected. The principles of integrative therapy guide the treatment process, ensuring a comprehensive and personalized approach to address the unique needs of each individual.
1. Individualization:
The cornerstone of integrative therapy is the understanding that each person is unique and requires an individualized treatment plan. Therapists tailor their approach to match the specific needs, preferences, and goals of each individual. By recognizing the uniqueness of each client, therapists can create a therapeutic environment that fosters growth and healing.
2. Collaboration:
Integrative therapy emphasizes a collaborative partnership between the therapist and the client. Rather than assuming an authoritative role, therapists work together with their clients to identify and achieve their therapeutic goals. Through open and honest communication, clients actively participate in their healing process, empowering them to take ownership of their well-being.
3. Integration:
The term "integrative" in integrative therapy signifies the integration of various therapeutic modalities and approaches. Rather than relying on a single approach, therapists draw from a wide range of evidence-based techniques and combine them to provide a comprehensive and synergistic treatment experience. This integration allows therapists to address the complex interplay of mental, emotional, and physical factors contributing to the client's well-being.
Benefits of Integrative Therapy
1. Holistic Healing
2. Personalized Treatment
3. Enhanced Self-Awareness
4. Comprehensive Approach
5. Long-Term Results
The principles of individualization, collaboration, and integration form the foundation of integrative therapy. These principles guide therapists in their practice, ensuring a holistic and personalized approach to healing and wellness. By embracing these principles, individuals can experience the benefits of integrative therapy, such as holistic healing, personalized treatment, enhanced self-awareness, and long-term results.
Types Of Modalities In Integrative Therapy
Integrative therapy is a holistic approach that combines different therapeutic modalities to address the physical, mental, emotional, and spiritual well-being of individuals. It recognizes that each person is unique and that there is no one-size-fits-all solution when it comes to healing and growth. In integrative therapy, various modalities are used to create a customized treatment plan tailored specifically to the individual's needs and goals.
One of the key aspects of integrative therapy is the use of multiple modalities. These modalities can range from traditional talk therapy to more experiential and body-centered approaches. Some of the most common modalities used in integrative therapy include:
- Cognitive Behavioral Therapy (CBT): This modality focuses on identifying and changing unhealthy thought patterns and behaviors that contribute to psychological distress. CBT helps individuals develop coping strategies to deal with challenging situations.
- Psychodynamic Therapy: This modality explores how past experiences and unconscious thoughts and feelings influence current behaviors and relationships. It aims to uncover and resolve underlying conflicts and traumas.
- Art Therapy: This creative modality allows individuals to express themselves through various art forms, such as drawing, painting, or sculpting. Art therapy can help individuals tap into their emotions and process trauma in a non-verbal way.
In addition to these modalities, integrative therapy may also incorporate other techniques such as mindfulness, meditation, yoga, bodywork, and energy healing. The integration of multiple modalities allows for a comprehensive and well-rounded approach to healing and personal growth.
Each modality within integrative therapy serves a unique purpose and can be beneficial for different individuals and issues. The flexibility and adaptability of integrative therapy enable therapists to tailor the treatment to the individual, taking into consideration their preferences, needs, and goals. By utilizing a combination of modalities, integrative therapy provides a more holistic and personalized approach to healing and well-being.
Modality
Description
Cognitive Behavioral Therapy (CBT)
This modality focuses on identifying and changing unhealthy thought patterns and behaviors that contribute to psychological distress. CBT helps individuals develop coping strategies to deal with challenging situations.
Psychodynamic Therapy
This modality explores how past experiences and unconscious thoughts and feelings influence current behaviors and relationships. It aims to uncover and resolve underlying conflicts and traumas.
Art Therapy
This creative modality allows individuals to express themselves through various art forms, such as drawing, painting, or sculpting. Art therapy can help individuals tap into their emotions and process trauma in a non-verbal way.
Benefits Of Integrative Therapy
Integrative therapy, also known as complementary and alternative medicine (CAM), is a holistic approach to healthcare that combines conventional medical treatments with alternative therapies. The benefits of integrative therapy are numerous and can have a positive impact on physical, mental, and emotional well-being.
One of the key benefits of integrative therapy is that it takes into account the individual as a whole, with a focus on treating the root cause of the issue rather than just the symptoms. By addressing the underlying causes of a health condition or concern, integrative therapy can promote long-term healing and improved overall wellness.
Another benefit of integrative therapy is the wide range of modalities and techniques available. From acupuncture and massage to nutritional counseling and mindfulness practices, integrative therapy offers a variety of options to suit individual needs and preferences. This personalized approach allows for a more tailored and comprehensive treatment plan, increasing the chances of success and patient satisfaction.
- Increased self-awareness and empowerment
- Improved stress management and resilience
- Enhanced immune function and overall physical health
- Reduced reliance on medications and invasive procedures
- Support for emotional well-being and mental health
Benefits of Integrative Therapy
1. Increased self-awareness and empowerment
2. Improved stress management and resilience
3. Enhanced immune function and overall physical health
4. Reduced reliance on medications and invasive procedures
5. Support for emotional well-being and mental health
Integrative therapy recognizes that the mind, body, and spirit are interconnected and that addressing all aspects of a person's well-being is crucial for optimal health. By incorporating various therapeutic approaches and modalities, integrative therapy aims to provide a comprehensive and holistic healing experience.
When it comes to mental health, integrative therapy can be especially beneficial. By combining traditional psychotherapy with techniques such as meditation, yoga, or art therapy, individuals can gain more insight into their emotions, develop coping mechanisms, and foster resilience.
Integrative therapy can also play a role in supporting physical health. By incorporating techniques such as acupuncture or herbal medicine, it can help manage symptoms, improve immune function, and promote overall wellness. This can be particularly useful for individuals with chronic conditions or those seeking to enhance their general health and well-being.
Choosing an integrative therapy practitioner is an important step in receiving the full benefits of this approach. It is essential to find a qualified and experienced professional who can create a personalized treatment plan tailored to your specific needs and goals.
In conclusion, the benefits of integrative therapy are numerous and can have a profound impact on overall well-being. From increased self-awareness and empowerment to improved stress management and enhanced physical health, this holistic approach offers a wide range of advantages. If you are looking for a comprehensive and personalized approach to your health, integrative therapy may be worth exploring.
How Integrative Therapy Works
Integrative therapy is a holistic approach that combines different therapeutic modalities to address the needs of an individual. It takes into account the physical, emotional, mental, and spiritual aspects of a person's well-being. This comprehensive approach aims to treat the root causes of issues rather than just managing symptoms. By utilizing multiple techniques, integrative therapy provides a personalized treatment plan that promotes healing and enhances overall wellness.
One of the key principles of integrative therapy is the belief that the mind, body, and spirit are interconnected. It recognizes that imbalances in one area can affect other areas of a person's life. Therefore, the therapeutic process focuses on restoring harmony and balance to all aspects of the individual's being.
In order to achieve this, integrative therapy incorporates various modalities such as talk therapy, mindfulness practices, expressive arts, body-based therapies, and energy work. These diverse approaches offer different tools and techniques that cater to the unique needs and preferences of each individual.
- Talk therapy: This modality involves verbal communication between the therapist and the client. It allows individuals to explore their thoughts, emotions, and experiences in a safe and supportive environment. Techniques such as cognitive-behavioral therapy (CBT), psychodynamic therapy, and solution-focused therapy may be used in talk therapy.
- Mindfulness practices: Mindfulness techniques, such as meditation and deep breathing exercises, help individuals cultivate awareness of their thoughts, feelings, and bodily sensations. These practices promote relaxation, stress reduction, and emotional regulation.
- Expressive arts: Engaging in creative activities like painting, drawing, or writing can be therapeutic. Expressive arts encourage self-expression, exploration of emotions, and can serve as a powerful outlet for healing and self-discovery.
Body-based therapies:
Energy work:
Body-based therapies, such as massage, yoga, or somatic experiencing, focus on the connection between the body and the mind. These modalities aim to release tension, promote relaxation, and restore physical well-being.
Energy work, such as Reiki or acupuncture, addresses the energetic imbalances in the body. By working with the body's energy system, these practices aim to promote healing, reduce physical discomfort, and restore vitality.
Integrative therapy works by combining these various modalities to provide comprehensive care for individuals. The therapist tailors the treatment plan to address the specific needs and goals of each individual. By utilizing a range of techniques, integrative therapy can effectively address a wide range of concerns, including mental health conditions, physical ailments, and emotional well-being.
Moreover, integrating traditional treatments with integrative therapy can have synergistic effects. It allows individuals to benefit from the advancements of modern medicine while also addressing the underlying causes and promoting holistic healing.
Research and evidence on integrative therapy have shown promising results. Studies suggest that this approach can improve psychological well-being, reduce symptoms of anxiety and depression, enhance quality of life, and support overall health and wellness. As more individuals seek alternative and holistic approaches to healing, integrative therapy continues to gain recognition and popularity.
Integrative Therapy Techniques And Approaches
Integrative therapy is a holistic approach that combines different techniques and approaches from various therapeutic modalities to address the physical, mental, and emotional well-being of an individual. It incorporates a range of practices, including talk therapy, expressive arts therapy, mind-body techniques, and alternative therapies such as acupuncture and yoga.
One of the key techniques used in integrative therapy is cognitive-behavioral therapy (CBT), which focuses on identifying and changing negative thought patterns and behaviors. This approach helps individuals develop healthier coping mechanisms and attain a more positive mindset. Another technique commonly used is mindfulness-based therapy, which involves cultivating a non-judgmental awareness of the present moment and has been shown to reduce stress and improve overall well-being.
Expressive arts therapy is another approach utilized in integrative therapy. It utilizes various art forms such as painting, dance, music, and drama to help individuals explore and express their emotions. This creative process can be therapeutic, allowing individuals to tap into their inner feelings and gain a deeper understanding of themselves.
Acupuncture:
It is a traditional Chinese medicine technique that involves inserting thin needles into specific points on the body. It is believed to help balance the flow of energy in the body and promote healing. Acupuncture is often used in integrative therapy to address physical pain, reduce stress, and improve overall well-being.
Yoga:
Yoga combines physical postures, breathing exercises, and meditation to promote physical strength, flexibility, and mental well-being. It is commonly used in integrative therapy to reduce anxiety, improve sleep, and enhance overall quality of life.
Integrative therapy takes into account the unique needs and preferences of each individual. It allows therapists to tailor the treatment approach to suit the specific goals and challenges of the client. By combining different techniques and approaches, integrative therapy offers a comprehensive and holistic approach to healing and personal growth.
Integrative Therapy For Mental Health
Mental health is a critical aspect of overall well-being. It affects how we think, feel, and behave, and plays a significant role in our daily lives. For individuals facing mental health challenges, finding effective treatment options is essential. One such approach that has gained traction in recent years is integrative therapy.
Read the full article
0 notes
Text
Structural family therapy

Understanding The Concept Of Structural Family Therapy
Structural Family Therapy is a powerful therapeutic approach that aims to identify and address dysfunctional family structures in order to promote healthy interactions and restore balance within the family system. In this blog post, we will explore the key principles of Structural Family Therapy, including how to identify dysfunctional family structures and address power imbalances. We will also discuss effective techniques for restructuring family interactions and utilizing boundaries to restore harmony. Additionally, we will examine the importance of involving all family members in therapy sessions and recognizing the impact of larger systems on the family. Finally, we will evaluate the effectiveness of Structural Family Therapy in overcoming resistance to change and resolving conflicts within the family. Join us as we dive deeper into this transformative therapy approach!
Understanding The Concept Of Structural Family Therapy
Structural family therapy is a therapeutic approach that focuses on the overall structure and organization of a family unit. It aims to identify and address dysfunctional patterns of interaction within the family system. This form of therapy views the family as a complex system with interconnected parts, where changes in one member can impact the entire family dynamic. The goal of structural family therapy is to create healthier patterns of interaction that promote positive change and growth.
One of the key principles of structural family therapy is the belief that symptoms experienced by an individual are often a result of dysfunctional family structures. These structures can include rigid boundaries, ineffective communication, and power imbalances. By examining and understanding these underlying structures, therapists can help families identify and address the root causes of their problems.
During the therapy process, therapists may use techniques such as joining, which involves actively participating and engaging with the family to build rapport and trust. This allows the therapist to gain insight into the family's structure and dynamics. Additionally, therapists may utilize enactments, where they ask family members to act out specific situations or interactions to uncover hidden conflicts or patterns of behavior.
- Therapists may utilize the concept of boundaries to restore balance in the family. Boundaries refer to the emotional and physical barriers that exist within relationships. In dysfunctional families, boundaries can be either too rigid or too permeable, leading to confusion and conflict. By helping families establish appropriate boundaries, therapists can help create a healthier and more functional family system.
- Another important principle of structural family therapy is the need to involve all family members in therapy sessions. This approach recognizes that change is more likely to occur when all members of the family system are actively engaged in the therapeutic process. By including everyone in the sessions, therapists can address power imbalances and ensure that everyone's perspective is heard and valued.
Benefits of Structural Family Therapy
1. Promotes positive change and growth within the family system.
2. Helps identify and address dysfunctional family structures.
3. Restores balance and improves communication within the family.
4. Involves all family members in the therapeutic process.
In conclusion, structural family therapy is a powerful approach that addresses dysfunctional family structures and promotes positive change within the family system. By understanding the underlying concepts and principles of this therapy, families can gain insight into their dynamics and work together to create healthier relationships and interactions.
Examining The Key Principles Of Structural Family Therapy
Structural Family Therapy is a form of psychotherapy that focuses on the dynamics and interactions within a family system. It aims to identify and address the underlying patterns and structures that contribute to dysfunctional behaviors and conflicts within the family. By understanding these key principles, therapists can effectively guide families towards positive change and improved family functioning.
One of the fundamental principles of Structural Family Therapy is the belief that every family has its own unique structure and set of rules. These structures and rules can either promote healthy functioning or contribute to dysfunction. The therapist's role is to observe and analyze the family's interactions and identify any problematic patterns or imbalances.
In order to bring about positive change, the therapist must actively intervene and disrupt these negative patterns. This can involve challenging hierarchies, boundaries, and power dynamics within the family system. By restructuring these elements, the therapist can help the family members develop more functional roles and relationships.
- Some of the techniques commonly used in Structural Family Therapy include:
- Joining: The therapist actively engages with the family members to build rapport and gain their trust. This involves empathetic listening, validation, and understanding of their experiences.
- Mapping: Through both observation and discussion, the therapist creates a visual representation of the family's structure, relationships, and patterns of interaction. This helps to highlight areas of dysfunction and informs the therapeutic interventions.
- Boundary Making: The therapist assists the family in establishing clear and healthy boundaries between family members. This involves clarifying roles and responsibilities, as well as defining appropriate limits and expectations.
- Enactments: The therapist may encourage the family members to reenact a specific interaction or scenario that is causing distress or conflict. This allows for a deeper understanding of the dynamics at play and facilitates the development of new, more adaptive responses.
The Key Principles of Structural Family Therapy
1. Understanding of family structure and rules
2. Active intervention and restructuring
3. Techniques: Joining, Mapping, Boundary Making, Enactments
In summary, Structural Family Therapy focuses on understanding and addressing the underlying structures and patterns within a family system. By examining these key principles and utilizing effective techniques, therapists can help families overcome dysfunction and achieve healthier, more balanced relationships. It is through this understanding and active intervention that lasting change can be achieved.
How To Identify Dysfunctional Family Structures
Family is the foundation of individuals' lives, providing love, support, and guidance. However, not all families function in a healthy and harmonious way. Dysfunctional family structures can have a significant impact on the emotional well-being of its members. Understanding the signs and characteristics of dysfunctional family structures is important in order to address and resolve these issues effectively. In this blog post, we will explore the key indicators of dysfunctional family structures and discuss how to identify them.
1. Lack of Communication: One of the major signs of a dysfunctional family is a lack of open and honest communication. In such families, members may avoid discussing their feelings, needs, and concerns. This leads to misunderstandings, resentment, and a breakdown in relationships. Communication is essential for building trust and nurturing healthy connections within the family.
2. Unhealthy Conflict: Dysfunctional family structures are often characterized by frequent and intense conflicts. These conflicts may involve shouting matches, verbal abuse, or even physical violence. Unresolved conflicts can create a hostile environment, affecting the emotional well-being of family members. Recognizing and addressing these conflicts is crucial for creating a more peaceful and supportive family environment.
3. Imbalanced Power Dynamics: In dysfunctional family structures, power imbalances are commonly observed. Certain family members may exert control and dominance over others, resulting in feelings of inferiority and resentment. These power dynamics can lead to emotional abuse, manipulation, and a lack of autonomy for some family members. Identifying and addressing these imbalances is vital for restoring harmony and equality within the family.
- 4. Lack of Boundaries: Dysfunctional families often have blurred or nonexistent boundaries. Boundaries define the limits and expectations within a family system, allowing individuals to maintain their personal space and autonomy. Without proper boundaries, family members may intrude on each other's privacy, disregard personal needs, or fail to respect individual boundaries. Implementing and reinforcing healthy boundaries can contribute to a more functional family structure.
Signs of Dysfunction
Possible Solutions
Lack of communication
Encourage open and honest dialogue, active listening, and expressing emotions.
Unhealthy conflict
Teach conflict resolution techniques, encourage empathy, and seek professional help if necessary.
Imbalanced power dynamics
Promote equality, establish clear roles, and encourage independence and self-advocacy.
Lack of boundaries
Establish and enforce healthy boundaries, clearly communicate expectations, and respect individual needs and privacy.
Roles And Dynamics Within The Family System
Strong family dynamics and clear roles are fundamental to a healthy and functional family system. In order to maintain balance and harmony within the family, it is essential for each member to understand their role and the dynamics at play. Roles within the family system can vary greatly, depending on cultural, societal, and individual factors. These roles can be categorized into several common categories, including parental roles, sibling roles, and extended family roles. By understanding and addressing these roles and dynamics, families can foster better communication, build stronger relationships, and navigate challenges more effectively.
Parental roles are often seen as the foundation of the family structure. Parents are responsible for nurturing and guiding their children, as well as providing them with love, support, and discipline. Within the parental roles, there may be different responsibilities assigned to each parent, such as disciplinarian, caretaker, or decision-maker. The dynamics between parents are crucial for maintaining a stable and secure environment for children, as well as for their own relationship satisfaction.
Sibling roles within the family system can greatly influence the dynamics and functioning of the family as a whole. Siblings often develop unique roles and relationships based on their birth order, personality traits, and shared experiences. These roles can include the caretaker, the peacekeeper, the rebel, or the mediator. Sibling dynamics can impact communication patterns, conflict resolution styles, and overall family cohesion. It is important for parents to foster healthy sibling relationships and address any issues that may arise to ensure a positive family environment.
Extended family roles also play a significant role in the family system. Grandparents, aunts, uncles, and other relatives can provide support, guidance, and a sense of belonging to the family. Their involvement can contribute to the overall dynamics and functioning of the family, and their absence or strained relationships can create challenges. Recognizing and valuing the roles of extended family members can strengthen the family system and foster a sense of connectedness across generations.
In conclusion, understanding and addressing the roles and dynamics within the family system is crucial for maintaining a healthy and functional family. Each member's role, whether parental, sibling, or extended family, carries unique responsibilities and influences the overall family dynamics. By acknowledging and addressing these roles, families can promote open communication, strengthen relationships, and navigate challenges more effectively. Incorporating the principles of structural family therapy can provide a framework for identifying and addressing these roles and dynamics, ultimately leading to a stronger and more harmonious family system.
Addressing Power Imbalances In The Family
Addressing Power Imbalances in the Family
Power imbalances within a family can have a profound impact on the overall dynamics and well-being of its members. It is crucial to recognize and address these imbalances in order to create a harmonious and healthy family system. Structural family therapy offers effective techniques and strategies to help restore balance and equality among family members. By understanding the underlying causes of power imbalances and utilizing appropriate interventions, therapists can support families in overcoming these challenges and promoting positive change.
Identifying Power Imbalances
One of the key principles of structural family therapy is to identify and assess the roles and dynamics within the family system. This allows therapists to gain insight into the power dynamics and determine if there are any imbalances present. Power imbalances can manifest in various ways, such as one family member exerting control over others, lack of voice and decision-making authority for certain individuals, or the dominance of one parent over the other.
Addressing Power Imbalances
Addressing power imbalances requires a collaborative approach that involves all family members. The therapist works with the family to identify the underlying structural issues that contribute to the imbalances. This may involve exploring family roles, communication patterns, and the distribution of power within the family. By understanding these dynamics, the therapist can help the family develop strategies to address power imbalances effectively.
Effective Techniques for Restructuring Family Interactions
Restructuring family interactions is a fundamental aspect of addressing power imbalances. The therapist may encourage open and respectful communication, allowing each family member to express their needs and concerns. By promoting healthy communication patterns, family members can develop a shared understanding of each other's perspectives and work towards finding mutually satisfying solutions. Additionally, the therapist may introduce boundary-setting exercises to establish clear expectations and boundaries within the family.
Utilizing Boundaries to Restore Balance
Boundaries play a vital role in addressing power imbalances and restoring balance within the family. By setting and maintaining healthy boundaries, family members can respect each other's individuality and autonomy. The therapist may facilitate discussions around boundary violations and provide guidance on how to establish and reinforce boundaries effectively. This process enables family members to feel safe, respected, and able to assert themselves without fear of retribution.
Engaging All Family Members in Therapy
A critical element of addressing power imbalances is actively involving all family members in therapy sessions. This ensures that everyone's voice is heard and contributes to the healing process. The therapist creates a safe and non-judgmental space where family members can openly express their concerns and perspectives. By including everyone, the therapist can uncover the hidden dynamics that contribute to power imbalances and engage the family in shared problem-solving and decision-making.
Conclusion
Addressing power imbalances in the family is essential for creating a healthy and functional system. Structural family therapy provides effective techniques for identifying and restructuring family dynamics to restore balance and equality. By engaging all family members, utilizing boundaries, and promoting effective communication, therapists can support families in overcoming power imbalances and fostering positive change.
Effective Techniques For Restructuring Family Interactions
When it comes to restructuring family interactions, there is a need for effective techniques that can promote positive change and healthy relationships within the family unit. Family dynamics can sometimes become strained, leading to conflict and dysfunction. In order to address these issues and create a more harmonious environment, structural family therapy offers a comprehensive approach that focuses on understanding and modifying the underlying patterns and structures within the family system.
In structural family therapy, the therapist takes on an active role in the sessions, working closely with the family to identify problematic interactions and behaviors. By observing and analyzing these interactions, the therapist gains insight into the hierarchical structure, boundaries, and power dynamics that exist within the family system. This understanding allows for the identification of specific techniques that can be used to restructure interactions and promote healthier relationships.
One effective technique used in structural family therapy is the use of family sculpting. This technique involves physically arranging family members in order to visually represent the relationships and dynamics within the family. By positioning family members in specific ways, the therapist can highlight power imbalances, conflicts, and unhealthy patterns of interaction. This visual representation can help the family gain a clearer understanding of their dynamics and can serve as a starting point for making positive changes.
Another technique commonly used in structural family therapy is the establishment of clear boundaries. Boundaries are essential for maintaining healthy relationships within the family system. By setting and enforcing boundaries, family members can develop a sense of autonomy and individuality while also respecting the needs and boundaries of others. This can help prevent enmeshment or disengagement within the family and promote healthier interactions and communication.
-
- Family sculpting
- Clear boundaries
Techniques for Restructuring Family Interactions
Family Sculpting
Using physical arrangement of family members to visually represent relationships and dynamics
Clear Boundaries
Establishing and enforcing boundaries to promote healthier interactions and prevent enmeshment or disengagement
Utilizing Boundaries To Restore Balance In The Family
When it comes to maintaining a healthy and functional family system, establishing and maintaining boundaries is crucial.
Read the full article
0 notes