#eye specialist in ghatkopar
Text
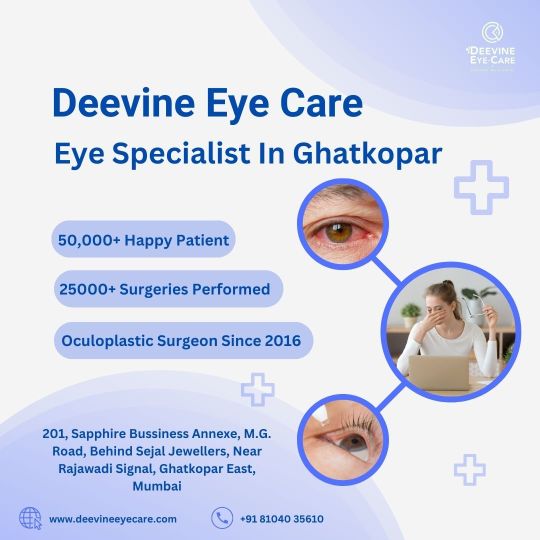
Eye Specialist in Ghatkopar - Deevine Eye Care
Discover Deevine Eye Care, led by Dr. Devanshi Shah, your trusted Eye Specialist in Ghatkopar. With over 50,000 satisfied patients and 25,000 successful surgeries, entrust your vision to our expert care.
0 notes
Text
Treatment for Corneal Dystrophies in Ghatkopar | Cornea Surgery in Mumbai
Cornea Surgery in Mumbai
Corneal Dystrophy
Corneal distrophies are a group of rare and genetic diseases affecting the cornea. It runs in a families and may be present asymptomatic. They affect both the eyes and other parts of the families are not involved. Main cause of corneal dystrophies is foreign material build up in the cornea and that results in clouding of cornea and visual impairment.
The cornea is made up of five distinct layers:
The Epithelium - the outermost, protective layer of the cornea.
The Bowman's membrane - this second layer is extremely tough and difficult to penetrate further protecting the eye
The Stroma - the thickest layer of the cornea, consisting of water, collagen fibers and other connective tissue components that give the cornea its strength, elasticity and clarity.
Descemet's Layer - a thin, strong inner layer that also acts as a protective layer.
The Endothelium - the innermost layer consisting of specialized cells that pump excess water out of the cornea
Types of corneal dystrophies:
There are 20 different types of corneal distrophies but are groped in 3 main categories:
Anterior or superficial corneal dystrophies. These affect the outermost layers of the cornea: the epithelium and Bowman’s membrane.
Stromal corneal dystrophies affect the stroma, which is the middle and thickest layer of the cornea.
Posterior corneal dystrophies affect the innermost parts of the cornea: the endothelium and the Descemet membrane. The most common posterior corneal dystrophy is Fuchs’ dystrophy.
Symptoms of Corneal distrophies:
Symptoms like watery eyes, dry eyes, corneal erosions, Blurry vision, halos around light, light sensitivity and difficulty in seeing at night often overlaps with diseases like glaucoma and cataract. Two differentiating symptoms are pain and a feeling of something in the eye occurs in the corneal distrophies. As the condition worsens vision becomes poor and irregularities in the cornea may lead to fluctuating vision.
Who is at risk for corneal dystropies?
People having family history of the disease are at more risk than others. Corneal dystrophies can appear at any age. Men and women are equally affected by most corneal dystrophies, except for Fuchs’ dystrophy. Fuchs’ affects women more frequently than men.
What are my treatment choices?
Treatment for corneal dystrophies may vary from eye drops to corneal transplant and depends on:
The type of dystrophy
The severity of symptoms
In few cases, people with corneal dystrophy may have repeated corneal erosion. This condition may be treated with antibiotics, lubricating eye drops, ointments, or special soft contact lenses that protect the cornea. If erosion continues, other treatment options may include the use of laser therapy or a technique for scraping the cornea.
In severe cases, a corneal transplant (called keratoplasty) may be necessary. The damaged or unhealthy corneal tissue is removed and clear donor cornea tissue is put in its place. For endothelial dystrophies, such as Fuchs’ dystrophy, a partial cornea transplant (or endothelial keratoplasty) is used.
To schedule an appointment with our experts for Corneal Dystrophy Treatment In Ghatkopar, please call us at +91 8451045935, +91-8451045934 or visit our clinic at Address.
Tag : cornea surgery in ghatkopar, cornea specialist in mumbai, eye clinic in ghatkopar west
Click here to know :
https://www.mumbaieyecare.com/cornea-surgery-in-ghatkopar-cornea-specialist-in-mumbai.html
#Dr. Jatin Ashar#cornea specialist in Mumbai#Cornea Surgery in Mumbai#Eye Specialist in Ghatkopar#eye clinic in ghatkopar east#Mumbai Eye Care
0 notes
Text
Keratoconus Treatment In Ghatkopar
Keratoconus is a vision disorder that occurs when the normally round cornea (the front part of the eye) becomes thin and irregular (cone) shaped. This abnormal shape prevents the light entering the eye from being focused correctly on the retina and causes distortion of vision. It is characterized by para-central corneal thinning and ectasia so that the cornea takes the shape of a cone. Visual loss occurs primarily from myopia and irregular astigmatism and secondarily from corneal scarring. Keratoconus often begins at puberty and most often is seen in teenagers or young adults.
Keratoconus causes distorted vision that cannot be corrected with eyeglasses. Tiny fibers of protein in your eye called collagen help hold your cornea in place. When these fibers get weak, they can’t hold their shape. Your cornea gets more and more cone-like.
It happens when you don’t have enough protective antioxidants in your cornea. Its cells produce harmful byproducts, the same way a car puts out exhaust. Normally, antioxidants get rid of them and protect the collagen fibers. But if levels are low, the collagen weakens and the cornea bulges.
Symptoms
Signs and symptoms of keratoconus may change as the disease progresses. They include:
Blurred or distorted vision
Increased sensitivity to bright light and glare, which can cause problems with night driving
A need for frequent changes in eyeglass prescriptions
Sudden worsening or clouding of vision
The swelling occurs when the strain of the cornea's protruding cone-like shape causes a tiny crack to develop. The swelling may last for weeks or months as the crack heals and is gradually replaced by scar tissue.
Monocular polyopia (perception of multiple ‘ghost’ images in the eye).
Streaking and flaring distortion around light sources.
Marked anisometropia (difference in vision of two eyes).
Photophobia (increased sensitivity to light).
Eyestrain, in order to read clearly.
Risk factors
Heredity. One in 10 keratoconus sufferers has a close family relative with the disorder.
Frequent eye rubbing, especially aggressive “knuckling” eye rubbing.
Having a history of asthma, allergies, Ehlos Danlers syndrome, Down’s syndrome
Keratoconus is categorised clinically as:
Latent stage: Latent stage was recognisable by placido disc only.
Early stage: Early stages were subdivided into two categories as:
Keratoconus fruste, which entailed 1- to 4-degree deviation of horizontal axis of the placido disc.
Early or mild keratoconus, which entailed 5- to 8-degree deviation of horizontal axis.
Causes
A family history of keratoconus has been established in some cases. Most researchers believe that multiple, complex factors are required for the development of keratoconus including both genetic and environmental factors.
With the advent of videokeratography to assess family members, however, pedigrees have been analysed. These studies show corneal changes consistent with keratoconus in some family members, which suggest an autosomal dominant pattern of inheritance.
Keratoconus may be associated with wide variety of systemic and ocular conditions.
Systemic associations:
Atopy (a genetic predisposition to develop an allergic reaction): Eye rubbing seen in systemic atopy may play a role in the development of keratoconus.
Down syndrome (Trisomy 21): In Down syndrome (Trisomy 21), frequency of acute hydrops is higher, perhaps because of eye rubbing and/or these patients are treated infrequently with keratoplasty and their disease is allowed to progress further.
Ehlers-Danlos syndrome.
Marfan syndrome.
Ocular associations:
Retinitis pigmentosa.
Retinopathy of prematurity.
Fuchs’ corneal endothelial dystrophy.
Posterior polymorphous dystrophy.
Contributory factors such as:
Enzyme abnormalities in corneal epithelium: Enzyme abnormalities such as increased expression of lysosomal enzymes (catalase and cathepsin) and decreased levels of inhibitors of proteolytic enzymes (tissue inhibitor matrix metalloproteinases), may play a role in corneal stromal degradation.
Differentially expressed corneal epithelium: Differentially expressed corneal epithelium between keratoconus and myopes (as controls) in both genetic expression and protein expression.
Molecular defect: Molecular defect producing unusual absence of water channel protein aquaporin 5 in keratoconus as compared to normal corneal epithelium.
Gelatinolytic activity: Gelatinolytic activity in stroma has been described, which may be due to decreased function of enzyme inhibitors.
Abnormalities in corneal collagen and its cross-linking: Abnormalities in corneal collagen and its cross-linking may be the cause of keratoconus.
Hard contact lens wear.
Pathophysiology:
First is thinning of the corneal stroma then fragmentation of the Bowman layer and the deposition of iron in the basal epithelial cells, forming the Fleischer ring. Folds and breaks in the Descemet’s membrane result in acute hydrops and striae, which produces variable amount of diffuse scarring.
How diagnosis is made?
Certain tests like refraction, keratometry, corneal topography/Computerised videokeratography, ultrasound pachymetry and slit lamp microscopy help in reaching final conclusion.
Computerized videokeratography, which takes pictures of your cornea so a map can be made of the surface while also measuring the thickness of your cornea
Severity of keratoconus depends on shape of cone:
Nipple cones
Oval cones
Globus cones
Treatment
If your keratoconus is progressing, corneal collagen cross-linking might be indicated to slow or stop the progression. Contact lenses can be used to correct astigmatism and mild near-sightedness. Improving your vision depends on the severity of keratoconus. Mild to moderate keratoconus can be treated with eyeglasses or contact lenses.
Lenses
Hard contact lenses. Hard lenses may feel uncomfortable at first, but many people adjust to wearing them and they can provide excellent vision. This type of lens can be made to fit your corneas.
Piggyback lenses. If rigid lenses are uncomfortable, your doctor may recommend "piggybacking" a hard contact lens on top of a soft one.
Eyeglasses or soft contact lenses. Glasses or soft contact lenses can correct blurry or distorted vision in early keratoconus. But people frequently need to change their prescription for eyeglasses or contacts as the shape of their corneas change.
Hybrid lenses. These contact lenses have a rigid center with a softer ring around the outside for increased comfort. People who can't tolerate hard contact lenses may prefer hybrid lenses.
Scleral lenses. These lenses are useful for very irregular shape changes in your cornea in advanced keratoconus. Instead of resting on the cornea like traditional contact lenses do, scleral lenses sit on the white part of the eye (sclera) and vault over the cornea without touching it.
Surgical Interventions
Some form of surgery may become necessary if the cornea progresses in its shape-changing until it is so steep that contacts cannot be tolerated at all.
INTACS are described as arc-like and plastic. These pieces are inserted into the center of the cornea to flatten it, thereby making the eye more contact lens-tolerant.
Collagen crosslinking (CXL) with UVA is a complex surgery that involves removing the topmost layer of your cornea, adding vitamin drops and then exposing the eye to a special UV lamp that helps the cornea fibers multiply, strengthening the cornea.
Corneal transplant surgery is the last resort for most doctors. In this procedure cornea would be removed and replaced with a healthy, normal-shaped cornea. This surgery has a long recovery time, a year or more in some cases, for clear vision.
Penetrating keratoplasty. If you have corneal scarring or extreme thinning, you'll likely need a cornea transplant (keratoplasty). Penetrating keratoplasty is a full-cornea transplant. In this procedure, doctors remove a full-thickness portion of your central cornea and replace it with donor tissue
Deep anterior lamellar keratoplasty (DALK). The DALK procedure preserves the inside lining of the cornea (endothelium). This helps avoid the rejection of this critical inside lining that can occur with a full-thickness transplant.
Important Reminder: This information is only intended to provide guidance, not a definitive medical advice. Please consult eye doctor about your specific condition. Only a trained, experienced board certified eye doctor can determine an accurate diagnosis and proper treatment.
To schedule an appointment with our experts for Keratoconus Treatment in Ghatkopar, please call us at +91 8451045935, +91-8451045934 or visit our clinic at Address.
TAG : cornea surgery in mumbai, cornea specialist in mumbai, Keratoconus Treatment In Ghatkopar, eye clinic in ghatkopar
For More Information :
https://www.mumbaieyecare.com/
#dr jatin ashar#eye specialist in ghatkopar east#Eye Specialist in Ghatkopar#eye clinic in ghatkopar#Keratoconus Treatment In Ghatkopar
0 notes
Link
0 notes
Link
Cataracts develop slowly with age and disturb your vision. It is suggested that you do not cataract surgery until it interferes with your usual activities.
0 notes
Text
Vitreous Detachment Treatment In Ghatkopar - Mumbaieyecare
Vitreous Detachment :
The eye is a very complex functional and anatomic organ. The retina is a thin, delicate and transparent sheet of tissue that lines the inside of the back of the eye. Directly in front of the retina is also a cavity that contains a gel called vitreous. The structure responsible for the bulk and shape of our eye is Vitreous part. It is a jelly-like body that fills the posterior chamber of the eye, giving the eyeball its round shape and keeping the retina in place against the back of the eye.
It is made up of millions of tiny collagen fibrils along with ground substance mucopolysaccharides such as hyaluronic acid, which form a gel. The vitreous is mostly water, which makes up 98% of it. The collagen strands connect to the superficial layers of the retina especially around the macula, the retinal vessels or sites at the retinal periphery.
Posterior vitreous detachment (PVD), also known as hyaloid detachment, occurs when the retinal layer and vitreous body/posterior hyaloid membrane dissociate, with an intervening fluid collection forming in the subhyaloid space. It is thought to be a common consequence of aging, occurring in more than 70% of the population over the age of 60
Who is at risk of posterior vitreous detachment?
The risk factors for vitreous detachment include:
Older age.
Nearsightedness.
Past eye trauma.
Prior Cataract Surgery.
Vitreous detachment in one eye.
People over age 60 are more likely to develop vitreous detachment. But if you’re nearsighted or have suffered eye trauma, you’re more likely to develop it at a younger age. And if you’ve had vitreous detachment in one eye, you’re likely to experience it in the other eye within a year. It’s good to be aware when you’re at increased risk, then you’ll know to see an ophthalmologist promptly if new floaters and flashes develop.
Meanwhile, remember to safeguard your eyes. Wear protective goggles when you play sports, when you work with saws or other tools that create debris, and when you handle fireworks.
What are symptoms of Vitreous Detachment?
Posterior vitreous detachment (PVD) doesn’t cause pain or permanent vision loss, but you might experience other symptoms. They include:
Flashes. These small flashes of light are comparable to “seeing stars” after hitting your head. They can last a few seconds or minutes and tend to stop, or occur less often, once detachment is complete.
Floaters. These floating spots in your field of vision can resemble tiny specks, dust, dots, or cobweb-like shadows. They typically occur in the first few weeks of Posterior vitreous detachment (PVD) and are most noticeable when looking at a light surface, such as a white wall or the sky.
Cobweb effect. You may begin to see the outer edge of the vitreous as it separates from the retina. It can feel like you’re looking through a cobweb. This is temporary and goes away once detachment is complete.
How Vitreous Detachment Develops?
In normal eyes, the vitreous is attached to the surface of the retina through millions of tiny, intertwined fibers. Your vitreous gel is mostly made of water. As we age, the vitreous slowly shrinks, and these fibers pull on the retina's surface. If the fibers break, the vitreous can shrink further and separate from the retina, causing a vitreous detachment. Most people get Posterior vitreous detachment (PVD) at age 60 or older and it's very common after 80. It happens to men and women equally.
What other problems can vitreous detachment cause?
Vitreous detachment can sometimes lead to more serious eye conditions:
Retinal tear. Sometimes, the vitreous fibers tear a hole in the retina when they pull away. If you don’t get treatment quickly, this can lead to retinal detachment.
Retinal detachment. Sometimes vitreous detachment pulls the entire retina away from its normal position at the back of the eye. This can be a medical emergency. Learn more about retinal detachment.
Macular hole. Sometimes vitreous detachment tears a hole in the macula (the part of the retina that controls your central vision). This can happen before or after the vitreous detaches enough to cause floaters or flashes of light. Learn more about macular hole.
Macular pucker. Sometimes vitreous detachment causes a thin layer of scar tissue to grow over the macula. This usually happens slowly in the months or years after vitreous detachment. Learn more about macular pucker.
These conditions can cause vision loss but treatment may help preserve your vision. Tell your eye doctor right away if you notice symptoms of vitreous detachment so they can check for these more serious problems.
Diagnosis
A Routine eye examination can help your doctor to spot problems like Posterior vitreous detachment (PVD) early and that can help protect your vision.
Your doctor may use special eye drops to make your pupils (the holes in the center of your eyes) bigger and use a slit-lamp test to look for signs of Posterior vitreous detachment (PVD). This is done with a microscope that looks through the front of your eye. It is helpful in detecting, if Posterior vitreous detachment (PVD) has caused bleeding, a torn retina, or something else that could harm your eyesight.
Your doctor also may use other tests to make sure the gel hasn't pulled away from your retina. These include:
Optical coherence tomography (OCT)- a 3-D scan of the inside of your eye
Ocular ultrasound - a test that uses sound waves to show the inside of your eye
Treatment
Posterior Vitreous Detachment usually doesn’t require treatment.
Complete detachment typically takes no longer than three months. If you continue to see floaters after detachment is complete, discuss treatment options with your doctor.
When complications occur and your ophthalmologist recommends treatment, there are a number of options available, including:
Laser or cryosurgery: This can be done in the office with no anesthesia. Your doctor repairs the holes or tears in your retina, which prevents further progression of the condition.
Scleral buckle: This involves placing a band around the outside of the eye to counterbalance the force of the vitreous pulling on the retina. Fluid is then drained from behind your retina, allowing it to return to its proper position. This is usually done as outpatient surgery.
Pneumatic retinopexy: This surgery is sometimes done in the office. Your doctor injects a gas bubble into the vitreous behind your eye. The bubble pushes the tear against the back wall of the eye and closes it. Then your doctor uses laser or cryosurgery to secure the retina where it belongs. After surgery, you may need to keep your head in a certain position for a few days. The gas bubble dissipates over time.
Follow up of Vitreous Detachment
Once it has been confirmed that the vitreous detachment is isolated, follow-up examinations are recommended at regular intervals thereafter. The period between examinations depends, of course, on the presence of blood in the vitreous or other signs which could increase the likelihood of retinal detachment. Thus the first re-visit may be after a week or a month, according to the nature of the detachment.
Important Reminder: This information is only intended to provide guidance, not a definitive medical advice. Please consult eye doctor about your specific condition. Only a trained, experienced board certified eye doctor can determine an accurate diagnosis and proper treatment.
To schedule an appointment with our experts for Posterior vitreous detachment (PVD) Treatment In Ghatkopar, please call us at +91 8451045935, +91-8451045934 or visit our clinic at Address.
Tags: eye specialist in ghatkopar,
0 notes
Text
Mumbai Eye Care Introduces A Simple Booking Feature To Manage A Schedule With Dr. Jatin Ashar
Eye Specialist in Ghatkopar - Dr. Jatin Ashar
Mumbai Eye Care introduces simple booking features on its official website. It helps patients to manage a schedule with eye specialist, Dr. Jatin Ashar for treatments and consultations.
Mumbai Eye Care, a reputable eye clinic in Ghatkopar introduces a simple booking feature on its official website. The idea of releasing this feature is to help patients to manage their eye treatments well. The CEO of the eye hospital stated, “Patients can go to the hospital according to the appointment and an exact date. It is more effective instead of going to the hospital over again. This feature is even helpful during the Coronavirus epidemic where people can’t meet face to face as before.”
Patients only have to visit the official website and click the book an appointment feature there. They can also choose to meet the eye specialist in Ghatkopar East or West. The feature also contains an online form that patients have to complete and submit. The CEO of the eye hospital added, “Our customer service takes action based on the explanation when a patient sends its appointment. Then, they will meet the specialist based on the case and the treatments they need. The process is straightforward and fast. The most important thing is that patients can go to the nearest hospital from their living area if it is necessary because of this feature.”
This feature is used for a variety of eye problems, including Lasik eye surgery, cataract surgery, retina surgery, corneal treatment, and many more. Patients need to explain their problems specifically to get the right specialist and treatments. The specialists and doctors can do a direct or online consultation based on the level of eye problem. One of the eye surgery patients explained, “Online appointments help us a lot. We don’t have to go to the hospital over again. It is effective for patients who are living far away from the hospital. They only go to the hospital when it is needed. We also get the right treatment because the eye specialist analyzes our problem first from the form.”
Mumbai Eye Care is also a place for those who need Lasik eye surgery in Ghatkopar. They can use this feature once they get what they want from this hospital—the earlier the eye treatment, the bigger the chance to cure the eye problem. The feature also includes the details of the hospitals, including the complete address, phone number, email, and working hours. The CEO of the eye hospital stated, “We hope that this feature and its facilities increase the comfort of our patients in getting the right eye treatment in India, especially in Ghatkopar.”
About Mumbai Eye Care
Mumbai Eye Care is a multi-specialty eye hospital in India. The eye specialists in this hospital are ready for Lasik surgery, dry eye treatment, cataract surgery, and many more. Patients can book an appointment online first before getting further treatment.
Tags - eye specialist in ghatkopar, eye clinic in ghatkopar, best eye specialist in ghatkopar
For more information link - www.mumbaieyecare.com
#eye specialist in ghatkopar#eye clinic in ghatkopar#best eye specialist in ghatkopar#Dr. Jatin Ashar#Mumbaieyecare
0 notes
Text
Posterior Vitreous Detachment Treatment In Ghatkopar, Mumbai by Dr. jatin ashar
Vitreous Detachment
The eye is a very complex functional and anatomic organ. The retina is a thin, delicate and transparent sheet of tissue that lines the inside of the back of the eye. Directly in front of the retina is also a cavity that contains a gel called vitreous. The structure responsible for the bulk and shape of our eye is Vitreous part. It is a jelly-like body that fills the posterior chamber of the eye, giving the eyeball its round shape and keeping the retina in place against the back of the eye.
It is made up of millions of tiny collagen fibrils along with ground substance mucopolysaccharides such as hyaluronic acid, which form a gel. The vitreous is mostly water, which makes up 98% of it. The collagen strands connect to the superficial layers of the retina especially around the macula, the retinal vessels or sites at the retinal periphery.
Posterior vitreous detachment (PVD), also known as hyaloid detachment, occurs when the retinal layer and vitreous body/posterior hyaloid membrane dissociate, with an intervening fluid collection forming in the subhyaloid space. It is thought to be a common consequence of aging, occurring in more than 70% of the population over the age of 60
Who is at risk of posterior vitreous detachment?
The risk factors for vitreous detachment include:
Older age.
Nearsightedness.
Past eye trauma.
Prior Cataract Surgery.
Vitreous detachment in one eye.
People over age 60 are more likely to develop vitreous detachment. But if you’re nearsighted or have suffered eye trauma, you’re more likely to develop it at a younger age. And if you’ve had vitreous detachment in one eye, you’re likely to experience it in the other eye within a year. It’s good to be aware when you’re at increased risk, then you’ll know to see an ophthalmologist promptly if new floaters and flashes develop.
Meanwhile, remember to safeguard your eyes. Wear protective goggles when you play sports, when you work with saws or other tools that create debris, and when you handle fireworks.
What are symptoms of Vitreous Detachment?
Posterior vitreous detachment (PVD) doesn’t cause pain or permanent vision loss, but you might experience other symptoms. They include:
Flashes. These small flashes of light are comparable to “seeing stars” after hitting your head. They can last a few seconds or minutes and tend to stop, or occur less often, once detachment is complete.
Floaters. These floating spots in your field of vision can resemble tiny specks, dust, dots, or cobweb-like shadows. They typically occur in the first few weeks of Posterior vitreous detachment (PVD) and are most noticeable when looking at a light surface, such as a white wall or the sky.
Cobweb effect. You may begin to see the outer edge of the vitreous as it separates from the retina. It can feel like you’re looking through a cobweb. This is temporary and goes away once detachment is complete.
How Vitreous Detachment Develops?
In normal eyes, the vitreous is attached to the surface of the retina through millions of tiny, intertwined fibers. Your vitreous gel is mostly made of water. As we age, the vitreous slowly shrinks, and these fibers pull on the retina's surface. If the fibers break, the vitreous can shrink further and separate from the retina, causing a vitreous detachment. Most people get Posterior vitreous detachment (PVD) at age 60 or older and it's very common after 80. It happens to men and women equally.
What other problems can vitreous detachment cause?
Vitreous detachment can sometimes lead to more serious eye conditions:
Retinal tear. Sometimes, the vitreous fibers tear a hole in the retina when they pull away. If you don’t get treatment quickly, this can lead to retinal detachment.
Retinal detachment. Sometimes vitreous detachment pulls the entire retina away from its normal position at the back of the eye. This can be a medical emergency. Learn more about retinal detachment.
Macular hole. Sometimes vitreous detachment tears a hole in the macula (the part of the retina that controls your central vision). This can happen before or after the vitreous detaches enough to cause floaters or flashes of light. Learn more about macular hole.
Macular pucker. Sometimes vitreous detachment causes a thin layer of scar tissue to grow over the macula. This usually happens slowly in the months or years after vitreous detachment. Learn more about macular pucker.
These conditions can cause vision loss but treatment may help preserve your vision. Tell your eye doctor right away if you notice symptoms of vitreous detachment so they can check for these more serious problems.
Diagnosis
A Routine eye examination can help your doctor to spot problems like Posterior vitreous detachment (PVD) early and that can help protect your vision.
Your doctor may use special eye drops to make your pupils (the holes in the center of your eyes) bigger and use a slit-lamp test to look for signs of Posterior vitreous detachment (PVD). This is done with a microscope that looks through the front of your eye. It is helpful in detecting, if Posterior vitreous detachment (PVD) has caused bleeding, a torn retina, or something else that could harm your eyesight.
Your doctor also may use other tests to make sure the gel hasn't pulled away from your retina. These include:
Optical coherence tomography (OCT)- a 3-D scan of the inside of your eye
Ocular ultrasound - a test that uses sound waves to show the inside of your eye
Treatment
Posterior Vitreous Detachment usually doesn’t require treatment.
Complete detachment typically takes no longer than three months. If you continue to see floaters after detachment is complete, discuss treatment options with your doctor.
When complications occur and your ophthalmologist recommends treatment, there are a number of options available, including:
Laser or cryosurgery: This can be done in the office with no anesthesia. Your doctor repairs the holes or tears in your retina, which prevents further progression of the condition.
Scleral buckle: This involves placing a band around the outside of the eye to counterbalance the force of the vitreous pulling on the retina. Fluid is then drained from behind your retina, allowing it to return to its proper position. This is usually done as outpatient surgery.
Pneumatic retinopexy: This surgery is sometimes done in the office. Your doctor injects a gas bubble into the vitreous behind your eye. The bubble pushes the tear against the back wall of the eye and closes it. Then your doctor uses laser or cryosurgery to secure the retina where it belongs. After surgery, you may need to keep your head in a certain position for a few days. The gas bubble dissipates over time.
Follow up of Vitreous Detachment
Once it has been confirmed that the vitreous detachment is isolated, follow-up examinations are recommended at regular intervals thereafter. The period between examinations depends, of course, on the presence of blood in the vitreous or other signs which could increase the likelihood of retinal detachment. Thus the first re-visit may be after a week or a month, according to the nature of the detachment.
Important Reminder: This information is only intended to provide guidance, not a definitive medical advice. Please consult eye doctor about your specific condition. Only a trained, experienced board certified eye doctor can determine an accurate diagnosis and proper treatment.
To schedule an appointment with our experts for Posterior vitreous detachment (PVD) Treatment In Ghatkopar, please call us at +91 8451045935, +91-8451045934 or visit our clinic at Address.
Tags= eye specialist in ghatkopar, eye clinic in ghatkopar
0 notes
Link
#EYE SPECIALIST IN GHATKOPAR#EYE CLINIC IN GHATKOPAR#CATARACT SURGERY IN GHATKOPAR#CORNEA SURGERY IN GHATKOPAR#DRY EYE TREATMENT IN GHATKOPAR#KERATOCONUS TREATMENT IN GHATKOPAR#GLAUCOMA TREATMENT IN GHATKOPAR#LASIK EYE SURGERY IN GHATKOPAR#LASIK SURGERY IN GHATKOPAR#DR JATIN ASHAR
0 notes
Text
Are you excited to travel this season?
Don't forget to follow these travel tips for regular usage of contact lenses!!
Book your appointments today !!
#best eye surgeon in ghatkopar#oculoplastic surgeon in ghatkopar#Eye Clinic in Ghatkopar#Eye Specialist In Mumbai
0 notes
Text
Does Lasik permanently fix your eyesight?

Lasik eye doctor uses a laser a strong beam of light to help improve fluid drainage from your eye. Your provider may suggest lasers as a first-line therapy instead of drops or in addition to eye drops. Having laser treatment may not replace the use of eye drops completely. The results from laser treatments vary but can last for years in some cases. Your provider may be able to repeat some types of laser treatments.
For more information, consult Dr. Sonia Maheshwari Kothari practising at Clear Sight Eyecare and Laser Centre
0 notes
Link
#Dr. Jatin Ashar#Contact Lens Clinic In Ghatkopar#Eye Specialist in Ghatkopar#Mumbai Eye Care#Best eye specialist in Ghatkopar#eye specialist in vikhroli west
0 notes
Text
Lasik Surgery in Ghatkopar By the Best Eye Specialist Dr. Jatin Ashar
Mumbai Eye Care Utilizes The Latest And The Most Advanced Technology To Perform Lasik Surgery In Ghatkopar
The eye specialist in Ghatkopar, Mumbai Eye Care, introduces LASIK (laser-assisted in situ keratomileusis) surgery with the most advanced technology. Lasik surgery by Mumbai Eye Care is performed by Dr. Jatin Ashar, an India’s cornea transplant specialist.
Ghatkopar, Mumbai – Mumbai Eye Care is pleased to announce Lasik Surgery in Ghatkopar with the latest and most advanced technology. Laser-assisted in situ keratomileusis (LASIK) eye surgery can be a better alternative and a safer procedure to improve vision besides using glasses or contact lenses. Lasik eye surgery was performed for the first time in 1988 and approved in the US in 1999. Today, LASIK eye surgery is widely recognized as a solution for eye defects such as Astigmatism (blurred distance & near vision), Hyperopia (farsightedness), and Myopia (nearsightedness). Mumbai Eye Care Clinic, with Dr. Jatin Ashar, as an ophthalmologist, provides the best eye treatments for various eye problems, including eye correction with a bladeless procedure.
LASIK eye surgery in Mumbai Eye Care Clinic is performed by Dr. Jatin Ashar, an eye specialist in Ghatkopar with a high success rate in performing various eye treatments, including LASIK surgery. A representative from Mumbai Eye Care said, “Dr. Jatin Ashar is an ophthalmologist in Ghatkopar, Mumbai, India. He specializes in performing treatment for Cataract, Cornea, Lasik and Refractive Surgery. Dr. Jatin Ashar and Mumbai Eye Care staff have years of experience in eye treatments and corneal surgery in Ghatkopar. Patients can get an appointment with Dr. Jatin at Mumbai Eye Care and please call at +91 8451045935, +91-8451045934 to schedule an appointment with Dr. Jatin Ashar.”
LASIK eye surgery at Mumbai Eye Care Clinic is performed under local anesthesia and takes only 30-40 minutes of procedures. According to the clinic representative, LASIK surgery at Mumbai Eye Care is performed with the latest femtosecond / bladeless technology from Alcon, USA. The LASIK procedure with Dr. Jatin Ashar is safe as it provides many advantages. It utilizes a bladeless procedure and uses only barcoded single-use cones to deliver the laser. The results are accurate, predictable, and customizable.
About Mumbai Eye Care
Mumbai Eye Care is a leading eye clinic in Ghatkopar. The clinic provides various eye treatments under one roof. Their services include eye treatment for cataracts, glaucoma, cornea, retina, Lasik eye surgery, Ocular Aesthetics, Pediatric Ophthalmology, Oculoplastics, Retina, and many more. For more information about Mumbai Eye Care, the best eye clinic in Ghatkopar, or make a scheduled consultation with Dr. Jatin Ashar, please visit their official website at www.mumbaieyecare.com.
Tag : Lasik Surgery in Ghatkopar , eye clinic in ghatkopar east, eye specialist in ghatkopar rajawadi
For More Information you can visit this site:
https://www.mumbaieyecare.com/
#Dr. Jatin Ashar#eye clinic in ghatkopar#eye specialist in ghatkopar west#Lasik Surgery in Ghatkopar
0 notes
Text
Diabetic Retinopathy Treatment In Ghatkopar, mumbai
Diabetic retinopathy
Diabetic retinopathy is a form of eye disease caused by chronically high or variable blood sugar that is associated with diabetes. If left untreated, diabetic retinopathy can lead to vision loss and blindness. The condition develops slowly throughout many years; therefore, it is essential to undergo regular eye tests when you have Diabetes. Retinopathy is basically impaired blood vessels in the retina which is the thin inner light-sensitive layer situated in the back of the eyes. In some cases, these vessels will swell up (macular oedema) and leak fluid into the rear of the eye. In other cases, abnormal blood vessels will grow on the surface of the retina.
Treatment
Treatment of diabetic retinopathy depends on the extent of the disease.
Eye Injections - Eye Medications called vascular endothelial growth factor (VEGF) inhibitors can be used to help stop the growth of new blood vessels and improve vision. Most people who receive these injections will need to get them for at least three months. Over time, some people may need to get them less often or may no longer need them at all, but others will need to continue in order to protect their vision.
Focal laser surgery - This surgery attempts to stop or reduce the leaking of blood or fluid into the eye by burning and sealing the damaged blood vessels.
Photocoagulation - This is usually done in your doctor’s office as an outpatient procedure during a single session. The procedure may or may not restore your vision to normal, but it should prevent your condition from worsening.
Scatter laser surgery - This surgery uses lasers to burn the damaged blood vessels so that they shrink. This procedure may require more than one application, and your vision may be blurry for a day or more after each session. You may also experience loss of peripheral vision or night vision after the procedure.
Vitrectomy - This surgery is done under general anesthesia and involves making a tiny incision in the eye to remove blood from the vitreous fluid, as well as any scar tissue that may cause retinal detachment.
Important Reminder: This information is only intended to provide guidance, not a definitive medical advice. Please consult eye doctor about your specific condition. Only a trained, experienced board certified eye doctor can determine an accurate diagnosis and proper treatment.
To schedule an appointment with our experts for Diabetic Retinopathy Treatment In Ghatkopar, please call us at +91 8451045935, +91-8451045934 or visit our clinic at Address.
Tags = eye specialist in ghatkopar east, eye specialist in ghatkopar, eye specialist in ghatkopar west
For more information = https://www.mumbaieyecare.com/
0 notes
Text
When You Need Cataract Surgery? Explain by Dr. Jatin Ashar
Introduction
A cataract is a condition in which the proteins present in the eye lens start breaking down. The proteins make clumps together in the lens. The clumped proteins start to distort and block the vision of the eyes.
A cataract is the leading cause of preventable blindness and develops with age. The cataract causes cloudy vision and interrupts your day-to-day activity. You may experience difficulty in reading, driving or even seeing the face of your friend.
Cataracts develop slowly with age and disturb your vision. It is suggested that you do not cataract surgery until it interferes with your usual activities. A cataract is generally a safe and efficient procedure to improve your vision.
Cause Of Cataract
Cataract usually develops with age. But certain behavioural activities of a person can increase the risk of developing cataracts. As result, you might need cataract surgery in future. Certain behaviours are:
Any injury that changes the tissue of the eyes causes cataract
Inherited genetic disorders such as diabetes
Long-term use of steroids
Smoking
Alcohol consumption
Not use sunglasses in the sun
Exposure to the excessive radiation
Signs Show, You Need To Have Cataract Surgery
Performing close tasks become difficult
Cataract development is a gradual process. It took many years to show up its effects. Surgery is not required until it interrupts daily activities. When you experience difficulty in reading books, recognizing faces, texting on the phone and sewing, you should understand that it’s time to get cataract surgery.
Interruption in enjoying your favourite hobbies
Cataracts cause your vision to be cloudy or blurry. It reduces the ability to distinguish colours and contrasts that cause difficulty in enjoying your favourite pastimes. Simple everyday activities can be affected by cataracts such as cooking, reading, playing sports, indoor games, doing laundry, surfing social media and even watching television.
Driving becomes difficult
When you have a cataract, your vision becomes blurry. Blurry vision is very dangerous while driving. Driving at night becomes more difficult and the chances to meet with accidents become higher. It is important to see the doctor as soon as possible if you experience difficulty while driving.
Everything appears yellow or tint
You may experience muddy and faded appearances instead of vibrant because of cataracts. The white thing may appear as yellow to you. It seems like you are looking through a dirty glass window. It will increase as cataracts grow bigger.
You start having double vision
Double vision is an unusual condition. People with cataracts develop double vision in one eye. Double vision restricts all activities which means if you experience double vision it is nearly impossible to do any task accurately for you. You should immediately consult your doctor and avoid activities like cooking and driving.
Blurry vision
Experiencing blurry vision is a sign of developing cataracts. Blurry vision is also a sign of more serious eye-related conditions. Immediate advice from an expert is the only way to determine the requirement of cataract surgery.
Changes in prescription
Ageing causes lots of changes including your eye prescriptions. Your contact lenses and glasses will change over time. But a time comes when glasses and contact lenses can’t work out for you and you will need cataract surgery for improving your vision.
Experiencing light sensitivity
Light sensitivity is the early symptom of a cataract by which a doctor can diagnose the cataract. If you have difficulty in the sun and traffic lights bother you, you should schedule your appointment with the doctor.
Halos
A cataract is responsible for several visual abnormalities. Cataracts create a ring or starburst around any fixed light source. Such as halos may be created from the headlights of the car in traffic that interrupt driving at night.
Changes in colour
After a cataract, everything appears yellowish brown. The discolouration causes when light travels to the eyes through cataracts affecting the area. Cataract surgery needs to be considered when you experience discolouration.
Protection of vision from cataracts
Over time cataracts may develop with age so there is no guarantee to protect you from cataracts completely. But you can take some preventive measures to reduce the risk of developing cataract by implementing a few changes in your lifestyle that includes:
Keep in touch with your doctor
Taking part in the regular eye examination
Quit smoking
Limiting the consumption of alcohol
Take care of diabetes
Eating a healthy diet includes vegetables and fruits
Polarized sunglasses to prevent the harmful effects of UV rays
Conclusion
Cataract surgery is quick and not so expensive procedure that can even be covered by insurance. If you suspect any of the signs, it is necessary to consult with a physician. The physician will diagnose and tell about the requirement of cataract surgery. The surgery can prevent you from further difficulties in your daily lifestyle. Cataract surgery enables you to see the actual appearance of beautiful things.
Know more about our successful Eye treatments visit our official website - mumbaieyecare.com
Tags = best eye specialist in Ghatkopar, eye clinic in Ghatkopar
1 note
·
View note
Text
Diabetic Retinopathy in Ghatkopar
Diabetic Retinopathy Treatment In Ghatkopar
Diabetic retinopathy is a form of eye disease caused by chronically high or variable blood sugar that is associated with diabetes. If left untreated, diabetic retinopathy can lead to vision loss and blindness. The condition develops slowly throughout many years; therefore, it is essential to undergo regular eye tests when you have Diabetes. Retinopathy is basically impaired blood vessels in the retina which is the thin inner light-sensitive layer situated in the back of the eyes. In some cases, these vessels will swell up (macular oedema) and leak fluid into the rear of the eye. In other cases, abnormal blood vessels will grow on the surface of the retina.
Diabetic retinopathy occurs in three stages:
Background retinopathy - Background retinopathy is said to occur if you have developed microaneurysms on your retina. Microaneurysms are when there is a swelling of the capillaries (very small blood vessels) that feed the retina. It is an early warning sign that your diabetes has lead to some damage of the small blood vessels of your retina.
Diabetic maculopathy - The macula is the part of the eye that helps to provide us with our central vision. Diabetic maculopathy is when the macula sustains some form of damage. One such cause of macular damage is from diabetic macular oedema whereby blood vessels near to the macula leak fluid or protein onto the macula.
Proliferative retinopathy - If a significant number of blood vessels on the retina become damaged, your body will respond by releasing a growth hormone known as Vascular Endothelial Cell Growth Factor (VEGF). The growth hormone stimulates the growth of new blood vessels. However, these new blood vessels are particularly weak and prone to leaking. Proliferative retinopathy is the body’s attempt to save its retina but it can often lead scarring of the retina and can cause the retina to detach, leading to blindness.
Symptoms
You might not have any signs of diabetic retinopathy until it becomes serious. When you do have symptoms, you might notice:
Loss of central vision, which is used when you read or drive
Not being able to see colors
Blurry vision
Holes or black spots in your vision
Floaters, or small spots in your vision caused by bleeding
Poor night vision
Risk factors
Anyone who has diabetes can develop diabetic retinopathy. Risk of developing the eye condition can increase as a result of:
Duration of diabetes — the longer you have diabetes, the greater your risk of developing diabetic retinopathy
Poor control of your blood sugar level
High blood pressure
High cholesterol
Pregnancy
Tobacco use
Being African-American, Hispanic or Native American
Detection and diagnosis of diabetic retinopathy
Diabetic retinopathy can be detected by undergoing a comprehensive eye examination that emphasizes on the evaluation of specifically the retina and macula. Such a test may include:
Visual acuity measurements – measuring a patient’s ability to see at different distances.
Patient history – to determine the presence of diabetes, vision impairments and other general health issues that may affect vision.
Tonometry – Measuring pressure within the eye.
Refraction – to establish whether a prescription for new glasses is required.
Pupil dilation – evaluation of eye structures, including assessment of the retina and optic nerve through a dilated pupil.
Supplementary testing may be required which include:
Retinal tomography or photography – In this test retina’s current status is documented.
Fluorescein angiography test - During this test, your doctor will inject a dye into your arm, allowing them to track how the blood flows in your eye. They’ll take pictures of the dye circulating inside of your eye to determine which vessels are blocked, leaking, or broken.
An optical coherence tomography (OCT) exam - It is an imaging test that uses light waves to produce images of the retina. These images allow your doctor to determine your retina’s thickness. OCT exams help determine how much fluid, if any, has accumulated in the retina.
Treatment
Treatment of diabetic retinopathy depends on the extent of the disease.
Eye Injections - Eye Medications called vascular endothelial growth factor (VEGF) inhibitors can be used to help stop the growth of new blood vessels and improve vision. Most people who receive these injections will need to get them for at least three months. Over time, some people may need to get them less often or may no longer need them at all, but others will need to continue in order to protect their vision.
Focal laser surgery - This surgery attempts to stop or reduce the leaking of blood or fluid into the eye by burning and sealing the damaged blood vessels.
Photocoagulation - This is usually done in your doctor’s office as an outpatient procedure during a single session. The procedure may or may not restore your vision to normal, but it should prevent your condition from worsening.
Scatter laser surgery - This surgery uses lasers to burn the damaged blood vessels so that they shrink. This procedure may require more than one application, and your vision may be blurry for a day or more after each session. You may also experience loss of peripheral vision or night vision after the procedure.
Vitrectomy - This surgery is done under general anesthesia and involves making a tiny incision in the eye to remove blood from the vitreous fluid, as well as any scar tissue that may cause retinal detachment.
Complications
Diabetic retinopathy involves the abnormal growth of blood vessels in the retina. Complications can lead to serious vision problems:
Vitreous hemorrhage - The new blood vessels may bleed into the clear, jelly-like substance that fills the center of your eye. If the amount of bleeding is small, you might see only a few dark spots (floaters). In more-severe cases, blood can fill the vitreous cavity and completely block your vision. Vitreous hemorrhage by itself usually doesn't cause permanent vision loss. The blood often clears from the eye within a few weeks or months. Unless your retina is damaged, your vision may return to its previous clarity.
Retinal detachment - The abnormal blood vessels associated with diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye. This may cause spots floating in your vision, flashes of light or severe vision loss.
Glaucoma - New blood vessels may grow in the front part of your eye and interfere with the normal flow of fluid out of the eye, causing pressure in the eye to build up (glaucoma). This pressure can damage the nerve that carries images from your eye to your brain (optic nerve).
Blindness - Eventually, diabetic retinopathy, glaucoma or both can lead to complete vision loss.
How can I reduce my risk of Retinopathy?
You can reduce your risk of developing diabetic retinopathy, or help prevent it getting worse, by:
Controlling your blood sugar, blood pressure and cholesterol levels
Taking your diabetes medication as prescribed
Attending all your screening appointments
Getting medical advice quickly if you notice any changes to your vision
Maintaining a healthy weight, eating a healthy, balanced diet, exercising regularly and stopping smoking
Important Reminder: This information is only intended to provide guidance, not a definitive medical advice. Please consult eye doctor about your specific condition. Only a trained, experienced board certified eye doctor can determine an accurate diagnosis and proper treatment.
To schedule an appointment with our experts for Diabetic Retinopathy Treatment In Ghatkopar, please call us at +91 8451045935, +91-8451045934 or visit our clinic at Address.
Tags : eye specialist in ghatkopar, eye clinic in ghatkopar,
0 notes