#IJCMCR
Text
Single Pass Four-Throw Pupilloplasty for Diffuse Iris Atrophy in Catractus Herpes Zoster Ophthalmicus (HZO) Case by Majed Alsubaie

Abstract
Patients of Herpes Zoster Ophthalmicus (HZO) develop several ocular complications that need surgical interventions such as cataract, glaucoma and corneal scar. Managing these complications is challenging in which the patient might go into several intera and post-surgical complications. We are reporting a case of Herpes Zoster Ophthalmicus (HZO) having diffuse iris atrophy and the intumescent cataract of the left eye. Both pupiloplasty and cataract surgery were done. Iris atrophy reconstructed by single-pass four-throw technique and phacoemulsification for cataract at the same time. The results were promising, the patient's visual outcome improved, the pupil has a good shape and contour and patient satisfied from the outcome both visually and cosmetically.
Keywords: Cataract; Pupilloplasty; Herpes Zoster Ophthalmicus
Introduction
The risk of developing herpes zoster infection in general during the lifetime is 20%, and the involvement of the ophthalmic division of the trigeminal nerve is up to 20% of these patients leading to a condition called Herpes Zoster Ophthalmicus (HZO), in which all structures of the eyes can be involved leading to various ocular diseases like Scleritis, Keratitis, Cataract, Uveitis, and glaucoma, However chronic inflammation and prolonge steroids use can lead to cataract formation [1].
We are reporting a case of HZO, who underwent surgical intervention for diffuse iris atrophy and intumescent cataract developed in less than 1 year of diagnosis and the post-cataract surgery result in visual improvement.
Case Report
A 35 years old male, presented to our clinic complaining of decreased vision, glare and abnormal-looking left eye due to diffuse iris atrophy over the left eye. He was diagnosed as a case of Herpes Zoster Ophthalmicus (HZO) having the first attack of anterior uveitis and high intraocular pressure along with forehead vesicular rash for which he was treated with an oral antiviral (valacilovir) and tapering topical corticosteroids at our uveitis service.
He was on regular follow up for the past 8 months' time with uveitis well controlled. Eight months later he presented to the uveitis service with further reductions of the vision over the left eye which was counting finger (CF) and glare due to his pre-existing diffuse iris atrophy.
His examination showed an intumescent cataract of the left eye (Figure1, A/B). Full ophthalmic examination of left eye BCVA Counting finger near the face, clear cornea with intact sensation, deep and quiet anterior chamber, diffuse iris atrophy pupil size around 11.5 , open-angle by gonioscopy, intraocular pressure 16 mmHg and no view of fundus B-scan done show flat retina and no abnormality detected. The right eye examination was within normal limits.
At the corneal service, he was scheduled for phacoemulsification with posterior chamber intraocular lens implant with pupiloplasty of the left eye under local anesthesia. The patient was seen first-day post-op and his examination revealed improvement of his vision from counting finger to 20/60 without correction, IOP 18 mmHg, clear cornea, anterior chamber deep with +3 cells, pupil 9.5 mm size with a round contour, Fundus within normal limit, He was happy about his visual outcome and his glare was almost resolved completely (Figure 2). The patient was continued on antibiotics and steroid drops.
Second-week post-op, the vision was improved, VA (SC) 20/30, the Cornea cleared, Intraocular Pressure (IOP) 14mmHg, Anterior chamber deep and quiet and normal fundus.
Discussion
Our reported case had an intumescent cataract with diffuse iris atrophy of the left eye in which the cataract removed and the residual iris reconstructed. The exact pathogenesis of HZO complications is not well understood, it could be due to viral replication in the early disease stages and the inflammation associated with that [2]. In HZO, the complications requiring surgical intervention are the Neuroparalytic ulcer, Glaucoma, Corneal scar and Cataract [3] in which the cataract is the most common one [1].
The common presentation is the posterior subcapsular cataract in which the steroid and chronic inflammation (uveitis) from virus play a role [2] in our case the patient was having an intumescent type of cataract which is not common in HZO and also its surgical management (phacoemulsification) is a bit difficult as compared to posterior sub-capsular cataract.
A retrospective study of 24 operated eyes of HZO patient having a cataract, the corrected distant visual acuity (CDVA) before surgery 20/112 after phacoemulsification + posterior capsular intraocular (PCIOL) the patient had CDVA 20/44 in the first year [1]. The choice of either ECCE or phacoemulsification and quince 6 months patient have better results on favorable long-term follow up (> 20y) the best-corrected visual acuity ( BCVA ) was 20/20 [2]. Another study done 11 eyes operated, the BCVA was 20/40 [1]. Most surgeons delay surgical intervention up to 3 months of quiescence and avoiding the active phase of the disease since the surgical intervention can trigger the disease [4]. Our patient had 6 months quiescence period since the last episode of uveitis.
Patients of HZO have the risk of complications after cataract surgery such as developing a corneal scar, fractional retinal detachment or recurrence of uveitis requiring further intervention [1]. Thus the adequate control of inflammation, intraocular pressure, and ocular surface disease improved the visual prognosis of cataract surgery of HZO patient [4], despite the advance of therapy HZO complication may be reduced but not eliminated [2]. Visual recovery compromised by the preexisting chronic ocular condition [1] thus it has an unpredictable result for cataract surgery.
Another situation we had in our patient which is rudimentary iris contour this may be due to chronic iritis and diffuse iris atrophy [3]. We were concern about cataract surgery results that may be compromised by the absence of iris coverage. Patient’s glare might worsen further causing more severe glare and photophobia due to reactivation of herpetic uveitis thus leading to unacceptable cosmetic appearance.
There are many techniques for pupilloplasty such Siper slipknot and the modified version, these options were on the table but using single-pass four-throw pupilloplasty technique provide a better option for our patient having advantages of minimal iris manipulation single pass, thus fewer iris pigment dispersion saving what we have of iris structure and also minimizing the reactivation of post-surgical induced uveitis [5]. This technique has an only single pass through the anterior chamber wherein 4 throws in helical configuration taken externally through the suture loop withdrawn from the anterior chamber, few steps were captured (Figure 2). Minimal iris manipulation single pass, thus fewer iris pigment dispersion saving what we have of iris structure [5] and also minimizing the reactivation of post-surgical induced uveitis. Although it has no true looking knot system, this technique provides a self-looking and self-retaining mechanism preventing the loop from reopening [6]. Single-pass four throw pupilloplasty provide adequate pupil dilatation after pupilloplasty facilitating retina examination if needed for patients of HZO. This technique achieves good pupil size, and contour [5].
In Conclusion
HZO patient has many ocular complications, with adequate control, the proper selection of cases to intervene and the proper selection of surgical technique can carry good prognosis of the patients.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-cr-id-00164/
https://ijclinmedcasereports.com/pdf/IJCMCR-CR-00164.pdf
0 notes
Text
Central Nervous System Coccidioidomycosis: A Case Report by Elvira Castro-Martínez
Abstract
We describe a case of central nervous system (CNS) coccidioidomycosis. This is the most dangerous form of extrapulmonary disease caused by the fungi Coccidioides spp. Clinical manifestations resemble other chronic fungal infections. Medical treatment is based on antifungal therapy for the most common complication, (hydrocephalus), where a shunt is usually required for decompression. Unfortunately, dissemination to the CNS is usually critical, so patients with untreated CNS coccidioidomycosis tend to have a high mortality a few years after initial diagnosis.
Keywords: Coccidioidomycosis; Valley Fever; Coccidioides; Central Nervous System Coccidioidomycosis; Coccidioidal Meningitis
Introduction
Coccidioidomycosis is an infection caused by soil fungi. This disease is common in some areas of United States and Latin America [1,2]. Although uncommon, infections of the central nervous system (CNS) are among the most pernicious [2]. Meningitis is usually associated with this pathology, causing headache and other symptoms [2,3,4]. Neuroimaging studies usually show meningitis and/ or hydrocephalus [3]. In treatment, oral triazole antifungal drugs have a great impact on the management of this disease [4]. Unfortunately, the most destructive forms of this pathology are chronic, resolution is often incomplete and relapses are common [5].
Case Presentation
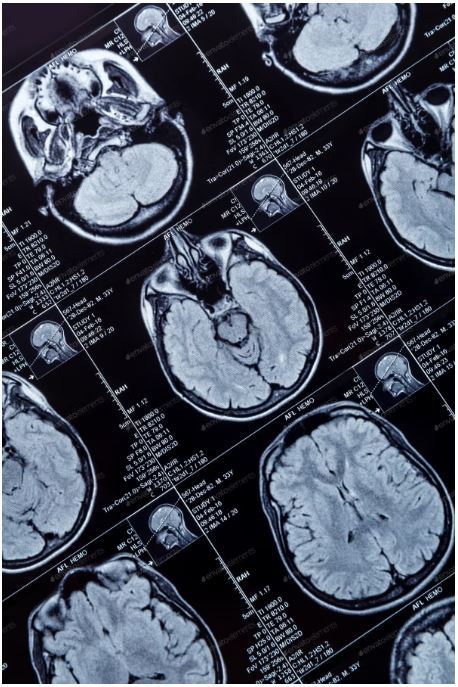
A 41-year-old man, a resident of Mexico City with a recent history of traveling to the north of the country with type 2 Diabetes Mellitus and Systemic Arterial Hypertension. He attended the hospital for a 3-month history characterized by persistent headache, general attack, daily fever of 38.5° C, confusional state, and tonic-clonic generalized seizures. The physical examination upon admission revealed a sleepy and disoriented patient, in which papilledema, hyperreflexia and meningeal signs stood out.Given the suspicion of chronic meningoencephalitis, a brain computed tomography (CT) was performed, which showed hydrocephalus (Figure 1).
Discussion
More than half of coccidioides exposures lead to asymptomatic infection [3], while in 40% of patients with symptomatic disease there are various manifestations that can be pulmonary Since the patient presented a rapid and sudden deterioration in consciousness and general neurological status during the evaluation in the emergency department, he underwent immediate surgical intervention for placement of a shunt system, limiting at that time the performance of other studies.The analysis of the cerebrospinal fluid obtained showed lymphocytic pleocytosis with 40 cells, elevated proteins and hypoglycorrhachia; the rapid test for HIV was negative.Despite emergency management, the patient continued with neurological deterioration and progressed to death within a few hours. In the pathological study, a basal subarachnoid exudate was observed (figure 2) and spherules and Coccidioides endospores were shown (figure 3).
or extrapulmonary: The latter are usually progressive and can involve the skin, bones and / or joints, the CNS and other organs and systems, with meningeal infection being one of the most dangerous forms that occurs in approximately 0.15% - 0.75% of extrapulmonarycoccidioidomycosis cases [4,5]. This occurs as a result of lymphohaematogenous spread from the lungs to the meninges [3]. The epidemiological history of stay in endemic areas and the presence of this symptom together with other compatible clinical characteristics, should indicate the diagnosis, since the prognosis is almost always fatal if not treated promptly [2]. Patients generally present with headache, intracranial hypertension, fever, nuchal rigidity, seizures, and altered mental status [2,4,5]. As in the case we reported, one of the most common findings on cranial computed tomography in CNS coccidiodomycosis is ventricular enlargement [6] and there may be evidence of basilar meningitis, hydrocephalus or cerebral infarcts [3]. The demonstration of a spherule in tissue or a positive culture is a diagnosis [3]. On the other hand, drug therapy for coccidiodomycosis continues to evolve. Antifungals such as fluconazole and itraconazole, in daily doses of 400 mg, have been effective against various forms of coccidiodomycosis including the meningeal one [4,5], while amphotericin B is reserved for severe cases [4]. In addition, hydrocephalus is relatively common with CNS coccidiodomycosis; up to 40% of patients develop this, and the author recommend aggresive management, including daily lumbar punctures and some cases must be managed with ventricular shunting [3, 7]. However, despite aggressive treatment, some patients may die early in the course of the disease. This patient presented to late medical attention with intracranial hypertension due to hydrocephalus secondary to CNS coccidiodomicosys, which was demonstrated in a post-mortem study; which, despite the establishment of emergency treatment, had a fatal outcome, so early diagnosis and treatment are essential to achieve a longer survival and avoid a devastating presentation of the disease.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-cr-id-00161/
https://ijclinmedcasereports.com/pdf/IJCMCR-CR-00161.pdf
#Coccidioidomycosis#Valley Fever#Coccidioides#Central Nervous System Coccidioidomycosis; Coccidioidal Meningitis#Elvira Castro-Martínez#IJCMCR#clinical studies
0 notes
Text
How to Optimised Oncological Treatments: Lessons Learned from the First covid-19 wave by López E
Abstract
Despite the local idiosyncrasies and different viral disease epidemiology resulting in country-specific governmental measures, our 70 centers located in Australia (32), United Kingdom (15) and Spain (21) joined forces and shared knowledge and experiences, which supported an appropriate clinical strategy for each country. The supply of Radio Therapy (RT) and/or Chemo Therapy (CT), and the safeguard of patients and staff in regard to their infectious status have been our priorities. In order to classify the changes in practice made during this pandemic we divide them into four major pillars that have impacted our culture and processes: oncology treatment, infection control, Information Technology (IT) infrastructure and staff connectedness. Facing a health crisis, the doctor leadership should be consolidated and for this reason, a high engagement of our doctors across the network is an essential key point. The oncology sanitary system should be continuously reinforced and should also be flexible plus solid.
Keywords: COVID-19; Chemotherapy; Leadership; Oncology; Radiotherapy; Staff
Introduction
In the first literature report of COVID-19 infection in oncologic patients the authors suggested three major strategies that would represent the backbone in delivery of oncologic treatments [1]. First, postponing adjuvant treatment or elective surgery. Second, personal protection for patient with cancer, cancer survivors and staff. Third, intensive surveillance or treatment in COVID positive patients with cancer.
During this pandemic, Spain was the first of the countries belonging to the Genesis Care (GC) international network affected by this outbreak. The first case in Spain for SARS-CoV-2 was diagnosed on 31 January 2020. By 13 March, cases had been confirmed in all 50 provinces of the country. From 17 March to 14 April, the death rate in Spain was 68% higher than usual and 21,882 excess deaths were recorded. The peak of excess deaths occurred during the week of 27 March to 3 April and was five times larger than the flu season of 2019.
Thus, Spain faced the main challenge to integrate strategies to minimize the deleterious effect of delayed diagnosis and treatment in cancer patients considering new ways of treating them, avoiding to postpone the start of treatments.
Despite the local idiosyncrasies and different viral disease epidemiology resulting in country-specific governmental measures, the three national chief medical officers of our 70 centers located in Australia (32), United Kingdom (15) and Spain (21) joined forces and shared knowledge and experiences, which supported an appropriate clinical strategy for each country. The supply of radiotherapy (RT) and/or chemotherapy (CT), and the safeguard of patients and staff in regard to their infectious status have been our priorities [2,3].
In order to classify the changes in practice made during this pandemic we divide them into four major pillars that have impacted our culture and processes: oncology treatment, infection control, Information Technology (IT) infrastructure and staff connectedness. The great enablers that have facilitated to treat our patients during the COVID-19 pandemics through the four pillars are shown in Table 1.
Our first pillar is oncology treatment looking for efficacy measures, we implemented two strategies: 1) To apply a tumor categorization protocol (Table 2) to determine the priority for RT delivery. Based on different factors such as tumor type and staging, intention-to-treat,
RT= Radiotherapy. SVCS= Superior Vena Cava Syndrome. SCLC= Small Cell Lung Cancer. SBRT= Stereotactic Body Radiotherapy. SPOT= non-melanoma skin cancer.9
General patient performance status and potential radiotherapy schedule approach, we classified the patients into 5 categories: rapid access/emergency radiotherapy (<14 hours or in the same day), A (<5days), B (>5 and <10 days), C (<4-6 weeks) and D (>6 weeks). This has allowed us, in an unprecedented situation, to balance the risk and benefit between treatments versus prevention of virus infection. 2) To increase the rate of hypo fractionated radiotherapy, achieving the same effectiveness with fewer sessions, in order to increase capacity in radiotherapy departments and reduce patient footfall in our centers. For instance, following the results of the Fast Forward trial, breast RT extreme hypo fractionation (26Gy/5#) is now an option for eligible patients (in two weeks we treated more than 90 patients). Similarly, in prostate cancer, moderate and ultra-hypo fractionation protocols such as 20# daily, 5# SABR and weekly 6# (total 36Gy) have been accepted as evidence-based protocols. Finally, for lung cancer patients who are also vulnerable to respiratory illness, a SABR regimen can be considered to standard fractionation. Staff and doctors have worked together to enable the implementation of the above protocols.
Regarding infection control, symptoms screening in patients and personnel before entering an oncology center presented an opportunity to identify possible cases with COVID-19 [4]. Discipline around general precautions by all staff including doctors and reinforcing the cleaning was used in order to keep a clean circuit. Besides, security lines, fixed screens for administrative staff and social distancing in waiting areas by re-arranging sitting areas to keep the 2m rule were performed and may remain as a global social change. The appropriate combination of personal protection equipment (PPE), selected through a risk assessment, was also used for infection prevention. Other useful measures were: Checking lung cone beam computed tomography of all patients with lung, breast or gastrointestinal superior cancers. This allowed not only to check the PTV we were treating but also to detect any abnormality which might be consistent with COVID-19. All these measures are included in our COVID-19 risk management framework [5] which should continue besides testing patients and staff when they screen positive for symptoms, with isolation measures in case of positive testing. An incidence was raised for any patient delay due to COVID-19 through a Multidisciplinary Team (MDT). COVID-MDT met with patient’s doctor, CMO and center manager to decide on patient treatment in case of positive swab for covid-19 [3]. A decision to treat end of day or delay treatment based on risks and benefits was made at the MDT. From our experience, we encourage the case-by-case assessment by a specialized board in future cases. Furthermore, routine asymptomatic staff and patient testing program should rule out to keep centers COVID-19 clean. In the first rapid testing around a 10.47% of our staff in Spain has been in contact with the disease and has generated IgG immunity.
Our third pillar is the IT infrastructure supporting a global network where some activities continued to ensure efficiency. A high percentage of staff members have worked from home through remote access to their platforms, having access to patient history and treatment planners (tele health). Oncologic follow ups were done by phone to reduce the people flow in the centers. Long survival follow-up (> 5 years) were also continued by phone with rapid access if it was needed. Also, psycho-oncologic attention was delivered by phone/digital media. The educational programs were done as Webinars and virtual congresses (teleconferencing). Electronic multidisciplinary teams (eMDT) were established at a time when clinician collaboration for patient care was more needed than ever [6]. It is run through a remote and safe platform, where clinicians can join in a synchronous or asynchronous way, record decisions and share report with the doctor, referrer, GP and patient if they so wish. To increase the communication through the whole network has been one of our priorities.
On the other hand, research continued for life saving trials and trials in set up. Two studies have been developed: Low doses of lung radiation therapy in cases of COVID-19 pneumonia: prospective, multicentric study in Radiation Oncology Centers (ClinicalTrials.gov Identifier: NCT04394182) and Genesis Care UK SARS-CoV-2 Antibody testing Program (both ongoing).
Our fourth pillar is staff connectedness. Regional managers and function managers worked very close to help physician unit coordinators with daily COVID-19 virtual huddles to discuss operational and quality issues and make decisions about center backup e.g.: minimizing the number of staff on site treating patients, having a schedule of backup in case staff fall ill, fewer face to face meetings and more virtual meetings, with staff spending more time home with their families and having time for home schooling Awareness across the network (local, national and international) has increased and this has fed into wellbeing. These plus the exercise and wellbeing program together with a strong medical leadership as part of the Integrative Cancer Care (ICC) holistic vision has led to the emergence of a solid team concept (“All for one and one for all”) that has generated a very strong engagement.
Our Oncology Departments have done a huge job, in a very short time. But now, with deescalated measures in Spain and other countries, we are presented with a unique opportunity to be a part of a cultural transformation in Oncology: The challenge of renaissance in the era post-COVID-19.
Some of the changes in practice which occurred in the COVID era are here to stay for several reasons. They improve patient and staff safety, lead to operational efficiencies, and efficacy in treatment, improve quality and team workflow and engagement. In addition, by continuing such strategies, we can be ready in case of another wave of this or a similar pandemic. This is an example of flexibility in our company, not only we have adapted to the difficult situation but also, we have learnt (innovation and improvement). Facing a health crisis, the doctor leadership should be consolidated and for this reason, a high engagement of our doctors across the network is an essential key point. The oncology sanitary system should be continuously reinforced and should be flexible plus solid as an accordion.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-rw-id-00162/
https://ijclinmedcasereports.com/pdf/IJCMCR-RW-00162.pdf
0 notes
Text
Origin and Physical Properties of the Black Hole by Orlov S*

Abstract
A new physical model is proposed for the appearance of an astronomical object - the Black Hole. It is shown that the Black Hole is the center of the cosmic, etheric, gravitational torsion. An equation for determining the radius of this object based on the theory of vortex gravity is presented. A substantiation is proposed that the force of gravity on the surface of the Black Hole does not depend on the mass of this Black Hole. The mass of the Black Hole can not be determined. A contradiction is shown in the Schwarzschild solution by the definition of the radius of the Black Hole.
Keywords: theory of vortex gravitation, celestial mechanics.
Introduction
According to many astrophysicists, astronomical object the Black Hole (BH) is an area in the space which gravitational attraction is so great that light quanta can't leave it even. Researchers believe that Black holes could result from catastrophic gravitational collapse of a massive star at that historical moment when it dies. At collapse - catastrophic compression of a star - intensity of gravity over its surface becomes so terribly big that the space surrounding a star - time is displaced. This star disappears from the Universe and there is only strongly bent area of space - to time. The border of this area is called as gravitational radius. Spherically a symmetric black hole it is equal in the elementary case to Shvartsshild's radius. Theoretically possibility of existence of such areas of space - time follows from some exact solutions of the equations of Einstein, first of which was received by Karl Shvartsshild in 1915 [1].
Where, rs – the radius of the Black Hole, M – the mass of a black hole, with - the velocity of light, G=6.672 ∙10 -11 N∙m2/kg2 – a gravitational constant. We will consider objectivity of a hypothesis of an origin of the Black hole on the example of similar object which is in the center of our galaxy. In work [2] the radius of this BH which is called the Sagittarius A * is determined –
At such radius and the corresponding volume, the mass of this BH has to be on the basis of a formula (1) about 1039 kg. Then density of the Black Hole in the center of our galaxy has to be about 5 kg/m3! ? On the basis of the classical equation about a mutual attraction gravitation force on a surface of the Sagittarius A * is equal
F = 6.8 x 104 M
Agree, it is impossible to call this Black hole "catastrophically squeezed", and gravitation forces on its surface "terribly big". It is obvious that the theoretical explanation of an astronomical phenomenon of the Black hole doesn't correspond to physical parameters. In addition, equation (1) is mathematically absurd. In it, the quantities (G) and (c) are constants. Therefore, the mass of the Black Hole (M) is directly proportional to its radius (r). In fact, the mass of any body is always proportional to its volume. The volume is proportional to the radius of this body in the cube (r3). Then the mass must also be proportional to the radius in the cube. From this discrepancy with the laws of mathematics of equation (1) it follows that the density of the Black Hole (P) is inversely proportional to the root of its cubic radius.
P ~ r-1/3
Example, On the basis of formula (1), we shall determine the mass of the Black Hole with a radius equal to 1 m.
Then the density of this black hole is
This density is several orders of magnitude greater than the density of the nucleon. Consequently, equation (1) is absurd. It is offered to study the theory of vortex gravitation and cosmology below. On the basis of this theory it is possible to explain genesis of the Black hole without contradictions.
About the Theory of Vortex Gravitation
The theory of vortex gravitation [3] is based on the well-known astronomical fact – all heavenly objects rotate. The most logical explanation of the reason of this movement can be only one – rotation of heavenly objects generated vortex rotation of space substance – ether. Ether forms system of the interconnected whirlwinds in world space. Orbital speeds of ether in each tuft (torsion) decrease in the direction from the center to the periphery under the law of the return square of this removal. If orbital speeds of a stream of ether decrease then, under aerodynamics laws, pressure in this stream increases. The gradient of pressure generates pushing out force in the direction to zones with the smallest pressure, that is to the center of this torsion. We will consider the equation of vortex gravitation received in the theory [3]. In this section, a model of appearance of the gravitation attraction force is considered from the viewpoint of aerodynamics. Namely, the two-dimensional model is considered on the basis of the following initial postulates. These postulates will be expanded and defined more exactly below.
Forces operating on a body 2 are specified. The Fc-centrifugal force, Fp-force of an attraction of a body 2 from a body 1, v2 – the linear speed of a body 2 on an orbit, R – the radius of an orbit, r1 – the radius of a body 1, r2 – the radius of a body 2, w1 – the angular speed of rotation of air on a surface of a body 1, m2 – body weight 2.
As it was already spoken, movement of a whirlwind is resulted by pressure gradient. Radial distribution of pressure and ether speed in work [3] are defined on the basis of Navier-Stokes's equation for movement of viscous liquid (gas).
In cylindrical coordinates taking into account radial symmetry of vr=vz=0, vj=v (r), P=P (r) the equation will register in the form of system
Where r = 8.85 х 10-12 kg \m3 - density of ether [4], – a vector of speed of ether, P – pressure of ether, h- viscosity.
In cylindrical coordinates for the module of force of gravitation
Then comparing (3) and (4) for incompressible ether (r=const) we find that
After necessary transformations (full calculation is stated in the theory [3]) it is received:
1 . the equations for determination of force of gravitation depending on the speed of rotation of ether
rn, mn – radius and mass of a nucleon.
We will transform a formula (6). We will equate r1 = r. We will substitute w1 r1 = v1 and numerical values rn, mn, r, we receive:
2. The equations for determination of dependence of pressure of P0, from the speed of rotation of ether of V1
Where – pressure of ether on we consider P0 to an orbit, using a boundary condition
In fig. 2 pressure distribution according to a formula (8) is graphically shown.
Vortex Black Hole
Асcording to laws ether-loudspeakers [4] pressure in motionless air is accepted size
Ether density
By means of the equation (8) we will find the orbital speed of ether of V0 = V1 at which pressure of P0 will be equal to zero.
from where
Orbital speed of ether to belong to the radius of the orbit under the law of the return square
where
R0 – radius of an orbit of a whirlwind on which ether reaches speed
Rkn – radius of an orbit of a whirlwind in which the speed of ether is known (Vkn).
From the equation (9) we find the orbital radius of the radio torsion with zero pressure.
Orbital speed of ether of Vkn is determined by the known force of gravitation in the same orbit, by means of the equation (7).
Radius of the Vortex Black Hole of the Sagittarius*
We will consider the Sun address in a galaxy orbit.
Orbital speed of solar system -V = 2.2 * 105
Radius of an orbit of solar system - Vkn = 2.46*1020 [5].
We determine the centrifugal force operating on the Sun.
Provided that centrifugal forces, in any point of an orbit, are always equal to attraction forces, we find force of the galactic gravitation operating on the Sun.
We substitute value Fп and r in the equation (7) and we find ether speed in a solar orbit.
Radius of an orbit of astronomical object the Sagittarius* with the zero pressure upon surfaces, on the basis of the equation (10)
The strength of the vortex gravitation on the surface of a black hole
Fg = 620 x M
Similarly, we find radiuses of Black holes at other objects:
Sun - R0 = 155500 m
Eartht - R0 = 0.478 m
Conclusion
Obviously, the modern theory of the origin of black holes contradictory. On the example of a celestial object Sagittarius A* can be argued that Black holes are not superdense and supermassive objects. They may not have a huge force of gravity at its surface. Based on the theory of vortex gravitation and cosmology, black holes is the central region of space, ether, gravitation torsion. Orbital velocity of the ether on the surface of this area reaches the maximum possible value
At this speed, the pressure on the rotationorbitof theesterdecreases to zero. No substanceorradiation is notable tobreak out ofthis zone.Therefore, the centerspace, gravitation torsioninvisible.Insidethe black holerotationetherorstopsorslows down. In this case,there can existinside a black holeof antigravity.
Note. A similar phenomenon is noted in the center of tropical meteorology and sea storms. Where there is complete peace of mind (calm). This phenomenon is called the "eye of the storm." Radius of the black hole Sagittarius A * at the center of our galaxy observations to determine the magnitude
The estimated value of the radius of the black hole Sagittarius A *, obtained in Chapter 4 (1,382×〖10〗^14 m) higher than the observed value of two orders of magnitude. This is not a calculation error, and the inequality of the radii of the Black Hole in the longitudinal (orbital) and transverse (axial) dimension. The fact that black holes have their form likeness forms of galaxies - and the disk are located in outer space, in the same direction as the galaxies themselves. Terrestrial observer is on the periphery of our galaxy and it can measure their visual observations center of the galaxy (Sagittarius A *) only in the transverse axial dimension. At the same time, disk Sagittarius A * its plane directed to us, so we can determine the calculations only the distance in the longitudinal direction radially. Therefore, calculations determined the orbital radius, and observations - transverse axial thickness of the black hole Sagittarius A *. Radius of gyration of any cosmic torsion far exceeds its axial thickness. For the black hole Sagittarius A * this fact recorded in this paper calculations and astronomical observations.
Gravitational torsions can be of different sizes. Each torsion creates its material object. Micro torsion create atoms. Planetary - planet. Star - star. Galactic - galaxies. Universe - the universe. All torsions in their centers hase black holes. In celestial bodies (atoms, planets, stars, etc.) they are under a layer of the material of which they are created. Therefore, they are hidden from us. In large space objects such as galaxies, they are open and subject to study. Modern classic exercise in cosmology and astrophysics have a lot of controversy for one reason. All of them are based on a global error of the classical theory of gravitation, which states that all bodies create gravity. In fact the opposite is true - gravity creates the body.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-rw-id-00156/
https://ijclinmedcasereports.com/pdf/IJCMCR-RW-00156.pdf
0 notes
Text
Laser Therapy for Treating Tuberculosis by Victor V Apollonov*

A Bit Scary Statistics
For a start, as a preamble, here are some excerpts from various sources on the problem of tuberculosis (TB), which are quite strange to read at the beginning of the third millennium, since many people confidently believed that there has been enough time to solve this problem during the past two millennia:
- Tuberculosis symptoms and signs: cough, loss of weight, chest pain, fever, night sweats. If untreated, 50 percent of patients die within five years;
- More than any other infectious disease, TB kills approximately 1 million women per year. Each year, TB kills 100 000 children. Tuberculosis is the most common cause of orphanage;
- Untreatable bacteria can destroy the progress of TB control achieved in the last 50 years. There are no drugs to combat some resistant TB bacteria (in developed countries 50 million people may be infected);
- The majority of people infected with TB never become sick because their immune system prevents the development of TB mycobacteria. Only 5 to 10 percent of those infected develop TB. Scientists today do not know exactly why some infected people develop TB and die, while others do not;
- At least one person is infected with TB every second, 1 percent of the world's population are infected each year. Untreated persons infect on average 10–15 neighbors during a year. For major cities, this figure is considerably higher. The most susceptible to infection are prisons, the Army and the Navy, where the concentration of people living together for a long time is the greatest. According to the WHO over the past two centuries, TB killed about a billion people. The WHO warns that unless we take urgent action, in the next 10 years, TB will kill an estimated 30 million people and infect 90 million people. Further, by the end of 2020 a billion people will have been already infected: 200 million people will be sick and 70 million people will die. So much for the White Plague (because of the extreme pallor seen among those infected)!
Laser Treatments for Tuberculosis
Currently, we know two approaches to fabricating laser systems for the TB treatment. They are based on excimer lasers and installations making use of important benefits of miniature solid-state diode-pumped lasers. The peak of the bacteriostatic activity of the generated laser radiation in various forms of TB lies at a wavelength of 265 to 266nm, and in this case, the effectiveness of its action is equal to unity. The wavelength of 248nm, which is emitted by an excimer laser, is closest to this range. At this wavelength, the interaction efficiency amounts to 0.8, which requires a proportional increase in the irradiation time. For a solid-state Nd:YAG laser (fourth harmonic) the radiation wavelength is equal to 266nm. The interaction efficiency of this wavelength is 1.0. The pulse energy with an average output power of 10mW (equal to the product of the energy in a single pulse by the pulse repetition rate). The power is determined experimentally in cultures of bacteria for the exposure time of 10 to 15min.
For an excimer laser the pulse repetition rate is no more than 100Hz; therefore, the energy of a single pulse is less than 0.1mJ, which can lead to tissue burn at a pulse duration of 5–10ns. To ensure a ‘soft’ effect on tissues, it is needed to reduce the pulse energy by one or two orders of magnitude, which is possible, but requires a proportional increase in the exposure time. At these energies (0.1mJ) an optical fiber is usually damaged. An optical fiber requires a high optical purity of working surfaces which is problematic when administering it in various cavities. The destruction of the output end of the fiber may cause penetration of small glass fragments into the patient. In a solid-state laser the pulse repetition rate is maintained at a level of 10000Hz; therefore, the energy of a single pulse is only 0.001mJ. That is why the soft tissue burn and destruction of optical fibers in the case of solid-state lasers is fundamentally impossible.
Now let us say a few words about the service life of some elements of lasers. In the case of an excimer laser, the main element is a gas tube, whose service life is about 1000–2000 hours at a cost of about 1000 USD. High-energy pulses can also lead to an early failure of optical elements. In the case of a solid-state laser, the essential element is a laser diode, whose service life amount to least 5000 hours at a cost of 700–800 USD.
The presence of hazards when working with lasers discussed is as follows. An excimer laser has in its design a significant amount of harmful gas. Besides, this laser requires a high voltage for its operation (about 10kV). The design of solid-state lasers is free of hazards, whereas the cost of the components of these lasers is approximately comparable with that of excimer lasers.
As for the additional conditions of production of the laser sources discussed, excimer lasers, apart from standard a optical-mechanical and an installation sites, also require the presence of a vacuum site, equipped to work with poisonous gases. The production of solid-state lasers requires only a standard optical-mechanical and an installation sites.
Amulet Semiconductor Laser Apparatus
An Amulet semiconductor laser apparatus with a fiber for introducing radiation in the affected area through an injection needle is intended for the treatment of destructive forms of pulmonary and bone TB that are resistant to conventional medical treatment, as well as to shorten the treatment of common forms of TB by topical exposure of the infected surface to ultraviolet (UV) radiation with a wavelength of 266 nm, which has very strong bactericidal and bacteriostatic effects. UV radiation in this case has low intensity and only affects the microflora without any damage of the living tissues of the human body. The typical time of UV irradiation of the affected area is 5 to 15min. In this case, the traumatic effect is absent.
The Amulet apparatus (Figure 1.) is designed to treat patients with tuberculosis affecting lungs, bronchi, bones and joints, to cure diseases associated with suppurative infections and other inflammatory processes, with the abnormal healing process, with the immune system variations and instability of the capillary circulation. In addition, the apparatus can be used in endosurgery, phthisiology, otolaryngology, traumatology, stomatology, treatment of burns, gynecology, therapy, surgery, urology, proctology, and dermatology.
Clinical Trials of the Amulet Apparatus
Fryns syndrome (FS) is a rare autosomal recessive congenital anomaly syndrome with an incidence of 0.7 per 10000 births [1]. The 6 diagnostic criteria for FS are as follows: 1) congenital diaphragmatic defect, 2) characteristic facial appearance, 3) distal digital hypoplasia, 4) pulmonary hypoplasia, 5) characteristic associated anomalies like polyhydramnios, brain malformations, ren
Conclusions
Thus, the clinical trials performed allow us to make a conclusion that a therapy UV solid-state diode-pumped Amulet laser is effective in the treatment of TB-affected tissues and bones due to the bactericidal and bacteriostatic effect and stimulation of reparative processes. It could be used for many other applications in the practical medicine.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-sc-id-00153/
https://ijclinmedcasereports.com/pdf/IJCMCR-SC-00153.pdf
0 notes
Text
Evaluating the Utility of Fast in Acute Blunt Abdominal Trauma in the Emergency Department: 20 Years On by Lateef F*

Abstract
Introduction: Blunt abdominal trauma (BAT) is a common presentation in the Emergency Department (ED) and associated with high mortality and morbidity. Given the time-sensitive nature, it is necessary to evaluate if FAST possesses adequate sensitivity and specificity to confidently rule out life-threatening injuries and guide the course of management. A positive FAST result would indicate intra-abdominal injury and prompt urgent surgical intervention, particularly in hypotensive patients. This review aims to examine relevant literature to evaluate the diagnostic utility and outcomes of FAST, and important external factors to be considered.
Methodology: Keyword search of PubMed and the Cochrane Library yielded 514 articles, from which 61 studies were chosen based on the inclusion and exclusion criteria.
Results: FAST demonstrates low to moderate sensitivity and Negative Predictive Value (NPV) and high specificity and Positive Predictive Value (PPV) in detection of hemoperitoneum and associated intra-abdominal injuries. Sensitivity for detecting peritoneal fluid is the highest. While superior to DPL, it has yet to surpass the diagnostic utility and accuracy of CT.
Conclusion: FAST is essential and should remain the primary preliminary radiological assessment of acute BAT. A positive FAST is highly predictive of intra-abdominal injury but a negative FAST cannot accurately rule out intra-abdominal injury. Negative FAST results should be succeeded by continued clinical observation, and serial FAST examinations or CT-scan should clinical signs not correlate. Current literature offers no evidence that FAST should replace CT as the diagnostic standard for BAT or a definitive ability to determine the necessity of immediate surgical management.
Keywords: Focused Assessment for Sonography; FAST; E-FAST; Ultrasonography; Point Of Care Ultrasound; Pocus; Blunt Abdominal Trauma; Laparotomy and CT
Introduction
Abdominal trauma is a common presentation in the ED and also one of the leading causes of death in young adults, under 45 years. It can be broadly classified into high or low energy injuries, and blunt or penetrating abdominal trauma. Blunt abdominal trauma (BAT), may be the result of road traffic accidents, physical assault or falls from height. Penetrating injuries are generally caused by firearms and stabbings. The focus of this review will be blunt abdominal trauma, as it is by far the more common presentation. A study was conducted by The Western Trauma Association Multi-Centre Trials of 392,315 blunt trauma patients at 12 major trauma centres. Majority of the injuries were caused by motor vehicle collisions (60%). 47% of the patients had documented hypotension and solid organ, small bowel, and large bowel injuries occurred in 38%, 35%, and 28% respectively. The most commonly associated injuries were spine fractures (44%) and pneumothorax/haemothorax (42%) [1].
Up to 50% of patients with severe abdominal trauma and/or multiple distracting injuries are reported to either have a normal initial abdominal exam, or are obtund and unable to provide a reliable index of suspicion. This affects both the physical and imaging examinations [2]. Diagnostic errors are responsible for approximately 10%–15% of preventable deaths in trauma centre audits. The sole reliance on clinical assessment as the main indication for surgery has led to negative laparotomy rates of as high as 40% [3]. A retrospective analysis found the incidence of short‐term complications caused by negative laparotomy to be 43% [4].
A quick, effective and efficient imaging approach is necessary to exclude life-threatening injuries. This modality would preferably need to have high sensitivity and specificity [5]. Prior to FAST, Diagnostic Peritoneal Lavage (DPL) was the standard initial diagnostic investigation. Although an invasive test, it could be done rapidly and was relatively safe with high sensitivity but had a significant false‐positive rate, which potentially exposed patients to the risks of an unnecessary laparotomy [6]. All patients who sustain blunt trauma to below the nipple line, are assumed to have intra-abdominal injuries until proven otherwise. Prompt reliable diagnosis and characterization of the abdominal injuries is essential to reduce risk of mortality and morbidity. Hemodynamic instability is a high-risk clinical sign and as such, both the diagnostic and interventional thresholds for these patients should be lowered. The three main types of blunt abdominal trauma injuries are solid organ injury, hollow viscos/mesenteric injury and vascular injury. The most commonly injured intra-abdominal organ is the spleen, followed by the liver and the genitourinary tract [7].
Immediate laparotomy should be done for patients with signs of peritoneal irritation, fresh blood on rectal exam, fresh blood aspirated from nasogastric tube, stab wounds with implement in-situ, gunshot wounds traversing the abdominal cavity, suspected intra-abdominal injury with hemodynamic instability, ultrasound evidence of active haemorrhage, and X-ray evidence of pneumoperitoneum or diaphragmatic rupture. In a retrospective cohort study of consecutive normotensive blunt trauma patients at 2 trauma centres, there was a strong association between a positive FAST and the need for therapeutic laparotomy. (Adjusted OR 44.6, 95% CI 1.77–1124). Thirty-seven percent of patients with a positive FAST required therapeutic laparotomy vs. 0.5% with a negative FAST [8]. Another study quoted lower figures, where only 25% of patients with intra-abdominal fluid required laparotomy [9].
Imaging modalities most often used to evaluate abdominal trauma in the ED are the Focused Assessment for Sonography for Trauma (FAST) and the Computed Tomography scan (CT-scan) which is the current reference diagnostic gold standard. The purpose of this study is to present a systematic review on the utility of the primary first line imaging modality FAST, in the acute assessment of blunt abdominal trauma.
Methodology
A systematic review of the literature was achieved using the electronic database PubMed and the Cochrane Library. Various query terms were tested to obtain enough data and to avoid unspecific information. Duration of search was from 1stMarch 2020 to 1stApril 2020. There was no limit on geography, age, type of study or date of article. Only original studies published in English were considered for this review. Keyword search yielded 514 articles, from which 61 studies were chosen based on the inclusion and exclusion criteria.
The keywords used in the search include: Focused Assessment for Sonography, FAST, E-FAST, Ultrasonography, Point of Care Ultrasound, PoCUS, Blunt abdominal trauma, Laparotomy and Computed tomography, CT
For studies to be included in this study, the inclusion criteria are as follows:
Acute presentation of blunt abdominal trauma at the ED
PoCUS/FAST or E-FAST examination done performed by radiologists, non‐radiologist clinicians, or ultrasound technicians
Definitive diagnosis verified by CT-scan or operative diagnosis.
Sufficient information on diagnostic test accuracy (i.e. sensitivity, specificity)
The studies were excluded if:
Insufficient information on diagnostic test accuracy
Case reports, case series
Unclear index or reference tests
Diagnostic case-control studies that compared patients with known case status to healthy controls. (This creates artificial populations and tends to overestimate sensitivity of the index test)
Patients with penetrating abdominal injuries
Results
Focused Assessment for Sonography for Trauma (FAST)
Ultrasound based trauma algorithms were only introduced formally into trauma literature in 1996.FAST is a limited abdominal ultrasound modality used in acute trauma as part of Advanced Trauma Life Support (ATLS)protocol to identify intra-abdominal fluid collections using a 3.5Hz sector transducer. FAST was established in 1999 after the FAST consensus conference and a subsequent study done at Massachusetts General Hospital in Boston, USA, showed the number of FAST scans increased from 15 % to approximately 34 % in the period 2002–2011, while the number of abdominal CT scans decreased from 35 % to 14 % in the same period [10]. In a prospective study on influence of FAST on trauma management, 194 patients underwent FAST. It was shown that FAST prevented an unnecessary laparotomy in 1 patient, CT in 23 patients, and DPL in 15 patients. There was an overall reduction in CT requests (from 47% to 34%) and DPL requests (from 9% to 1%) (p < 0.0001) [11].The goal of FAST is to detect hemoperitoneum in the right and left sub phrenic space, peri-splenic fossa, hepatorenal recess, suprapubic window (Pouch of Douglas or rectovesical pouch) and hemopericardium in the subxiphoid space. A positive FAST result would mean that there is free fluid in either of these abdominal compartments, which is a surrogate for active haemorrhage and in one study, has demonstrated a 65% sensitivity in detection of abdominal injuries requiring surgery [12].
E-FAST and Ex-FAST
E-FAST was established in 2004 and is now the diagnostic standard of ATLS, virtually replacing DPL. The E component refers to bilateral anterior thoracic sonography which searches for free air in the pleural cavity as evidence of an acute traumatic pneumothorax. It has been shown to have greater sensitivity and specificity than traditional chest radiography [13]. There is also some reference to Extended FAST or Ex-FAST. It is a combination of both physical examination and FAST. An abnormal examination constitutes signs of hemodynamic instability, abdominal bruising, tenderness, absence of bowl sounds, peritonism, seatbelt sign, lacerations etc. [14]. In a retrospective study of 354 children in the ED of which 14% (n=50) had intrabdominal injury (IAI), the use of Ex-FAST showed greater sensitivity (sensitivity of 88% (95% CI: 76‐96%) and Negative Predictive Value (NPV) 97.3% (95% CI: 94.5‐98.7%)) over either physical examination [OR, 15.2; 95% CI: 7.7 ‐ 31.7] or FAST [OR, 14.8; 95% CI: 7.5 ‐ 30.8] alone [15].
The execution time of E-FAST examination averaged 2.3 ± 2.9 min for chest US and ≤5 min for standard FAST [16]. FAST has been reported to be able to detect as little as 200ml of fluid in Morrison’s pouch and can completed in less than a minute in the hands of an experienced operator. This is many times faster than a CT-scan which on average takes approximately 30minutes and hence unsuitable for an unstable patient in an emergent setting. Moreover, it is easily repeatable, physicians can be easily trained, inexpensive, non-invasive and does not require contrast nor exposes the patient to ionizing radiation. Although these are insufficiently substantiated by sufficient evidence, other possible beneficial outcomes include shortening of the primary trauma assessment, more precise triaging, avoidance of unnecessary interventional procedures, and associated costs
The reliability and quality of images obtained from FAST is also greatly dependent on the training and experience of its operator. A comparison of the reproducibility of FAST results between Emergency Medicine Residents (EMRs) and Radiology Residents (RRs) showed sensitivities, specificities, PPV, NPV and accuracy of evaluating intra-peritoneal fluid to be very similar at 80%, 95%, 57%, 98% and 94% and 86%, 95%, 59%, 98% and 94%. This shows that EMRs are well-trained to use FAST and their results would be similar if not identical to an RR [17]. However, a comparism done in another study amongst US operators with low, moderate and extensive experience reported sensitivities of 45%, 87%, and 100% respectively in detecting <1L of peritoneal fluid [18].
A recent review article has quoted FAST sensitivities that range between 63 % and 99 % and specificities range from 90% to 100%. These results are similar for the detection of free intraperitoneal fluid, with sensitivities ranging from 69 % to 98 % and specificities of 94% to 100% [19]. Another study reviewing literature from various institutions around the world has reported lower thresholds of sensitivities ranging from 42.0%–91.7%, specificities 83%–100% and accuracies 9%–96% for the utility of E-FAST examinations. Its own prospective observational study examining the diagnostic accuracy of E-FAST done by emergency physicians compared to CT at the ED of a level 1 trauma centre found that out of 132 patients with blunt abdominal trauma, FAST sensitivities (only abdomen) was 42.9% (95% CI: 9.9%, 81.6%) and specificity was 98.4% (95% CI: 94.3%, 99.8%). The + LR of the FAST exam for abdominal free fluid as 26.8 (95% CI: 5.3, 135.2) and − LR was 0.58 (95% CI: 0.31, 1.1) [20]. This consistently high reported specificity of FAST was highlighted in a systemic review of 11 articles containing prospectively derived data with FAST results, patient disposition and final diagnoses. It showed that out of the 2,755 patients, 448 (16%) went to the OR. In total, there were 5 false-negatives derived from FAST; 3 involving inadequate scans and 2 of blunt trauma-induced small bowel perforations without hemoperitoneum [21]. The sensitivity of an examination is the “correct positive test rate” and measures the proportion of patients with an intraabdominal injury who have a positive test result. A high degree of sensitivity is not useful to rule in a diagnosis, but rather to rule out a particular condition. Similarly, high levels of specificity indicate that positive findings will detect the presence of a pathology. This suggests that when FAST is positive, there is high certainty of injury but when it is negative there’s a higher chance the injury was undetected. Hence, there is still large uncertainty in diagnostic confidence, with its wide sensitivity range and cannot confidently or safely exclude the presence of intra-abdominal injury.
FAST in Abdominal Trauma
In a meta-analysis [22] of emergency ultrasonography for BAT, a sensitivity range was observed as low as 28% and as high as 97%, specificities were close to 100%. A summary measure of 0.90 was calculated for the sensitivity-specificity pair closest to the desirable upper left corner of the ROC curve, which could be interpreted as 10% of abdominal injuries will be missed by FAST. Low sensitivities, coupled with low NPV, negative LRs and associated post-test probability, diminishes confidence in negative FAST findings. However, high specificities and LRs>10 would almost confirm intra-abdominal injury if positive and hence the need for surgical management.
In a retrospective study, 3181 blunt normotensive trauma patients presenting at a single level 1 trauma centre were evaluated with FAST and stratified into various groups of Injury Severity Scores (ISS). A one-time, four-view FAST examination in patients with ISS ≥ 25 had a lower sensitivity of 65 % than those with an ISS < 25 (80–86 %). More than 82 % of the FAST-missed injuries in patients with ≥ 25 ISS were solid organ injuries of the liver, spleen and kidneys [23]. An observational study of the diagnostic accuracy of FAST in 105 patients from King Fahad Military Medical Complex Dhahran, Saudi Arabia with blunt abdominal trauma demonstrated sensitivities of 76.1% (95% CI, 64.14- 85.69%), specificity 84.2% (95% CI, 68.75- 93.98%) and accuracy 79% (95% CI, 70.01- 86.38%. FAST could detect free fluid in 37 out of 39 patients with high grade sold intra-abdominal injuries. However, it could not detect small amount of fluid and nearly half of the negatives had low grade visceral injuries [24]. These studies highlight potential factors that may affect the results of the FAST examination, such as the presence of multiple other distracting injuries, higher likelihood for missed solid organ injuries and reduced sensitivity for fluid in patients with only low-grade injuries.The reason for this could be that hemoperitoneum is not always seen in liver or splenic injuries and hence it doesn’t matter if FAST has a high sensitivity for peritoneal fluid [12].
A systemic review evaluating the diagnostic accuracy of point‐of‐care sonography (POCS) for diagnosing thoracoabdominal injuries in patients with blunt trauma included 34 studies with a cumulative cohort of 8635 participants. For abdominal trauma, POCS had a sensitivity of 0.68 (95% CI 0.59 to 0.75) and a specificity of 0.95 (95% CI 0.92 to 0.97), with statistically significant lower values in children. To put this in perspective, it meant 73 false negatives and 29 false positives for every 1000 adult patients, assuming the observed median prevalence of thoracoabdominal trauma of 28% [25].
In paediatric BAT patients, the diagnostic accuracy of FAST has been reported to be lower compared to adults. A multi-institutional (n=14) analysis of level1 paediatric trauma centres yielded low sensitivities (28%) and high specificities (91%) for IAI consistent with paediatric literature but improved sensitivities (44%) and similar specificities (89%) for IAI requiring acute intervention. However, FAST missed 75% of liver injuries and 57% of spleen injuries and 56% of 27 patients whom required acute intervention for IAI had negative FAST. All the patients were normotensive and had abnormal abdominal examination [26]. However, in a separate observational prospective study comparing FAST evaluation of hypotensive and normotensive children with BAT, FAST showed a 100% sensitivity in detecting peritoneal fluid in hypotensive patients [27]. A prospective study was done on 160 hemodynamically stable paediatric trauma patients who had undergone both FAST and CT. Forty-four of the 160 patients had an intraabdominal injury on CT, 24 (55%) of which had normal screening sonography. Accuracy of sonography compared with CT was 76% with a negative predictive value 81% [28]. While the statistics of these three studies on the use of FAST in paediatric BAT patients do vary, sensitivities and specificities are both generally on the lower threshold of the adult range. They also show consistency of hypotension as a strong predictor of IAI and the poor ability of FAST to detect solid organ injuries.
FAST and Other Modalities
A prospective study [16] was done of 601 adult trauma patients at the ED who underwent a Chest Abdominal-Focused Assessment Sonography for Trauma (CA-FAST) exam prior to a thoracoabdominal CECT. Free fluid was detected in 116 patients with an overall accuracy of 91 % (95 % CI 85–93%). The following table illustrates the results of 4-view FAST and its individual views
FAST has different sensitivities for each abdominal cavity view, which translates to different diagnostic accuracies for the various types injuries previously mentioned in the methodology has well. In this study, FAST exhibits moderate to good sensitivity than previously quoted and with similar sensitive for the upper abdominal regions, followed by the pelvis and least able to detect fluid in the subxiphoid, pericardial space. It also shows good PPV, high specificity and NPV, consistent with previous studies [16].
This is supported by a 2-year review at a level1 trauma centre of 1027 patients who underwent FAST were stratified by operator skill level. It was shown that compared to patients with concordant FAST results, those with equivocal results had higher mortality (9.8 vs 3.7%, P = 0.02), decreased positive predictive value in the right upper quadrant (RUQ) (55 vs 79%, P = 0.02) and left upper quadrant (LUQ) (50 vs 83%, P < 0.01). However, unlike the previous study, this study observed worse outcomes has a result of the high rate of false negatives in the FAST examination.
However, some of these findings were obtained from only a single FAST scan (i.e. [23]), with the underlying assumption that fluid accumulates in the deepest parts of the abdomen. This can be influenced by anatomy, location of bleed, respiratory physiology, intra-abdominal adhesions etc. Thus, it would be prudent to consider the value of serial FAST scans, Contrast Enhanced Ultrasonography (CEUS), additional abdominal views and other imaging modalities such as CT with or without contrast media. A retrospective analysis [29] comparing the use of CTAP and Complete Ultrasonography of Trauma (CUST) in 19128 patients to screen for blunt abdominal trauma (BAT) from 2000 to 2011 in a Level 1 trauma centre was performed. It found that outcomes in CUST is equivalent to routine CTAP for BAT and leads to an average of 42% less radiation exposure and more than $591,000 savings per year.
The shortcomings of FAST can be bolstered by the application of CEUS. A recent meta-analysis [30] of 9 studies investigating the diagnostic accuracy of CEUS of abdominal trauma patients at the ED demonstrated that the CEUS had a sensitivity of 0.981 (95% CI: 0.868-0.950) and a false positive rate of 0.018 (95% CI: 0.010-0.032) for identifying parenchymal injuries, with an AUC of 0.984. These accuracies are similar to that of contrast-enhanced CT. Another study done on the application of CEUS in paediatric patients concluded CEUS proved to be an effective investigation in the hemodynamically stable child for identifying parenchymal injuries and for the characterization of focal liver lesions. It also showed comparable performance to CT and MRI with a specificity of 98% for identifying benign lesions and a negative predictive value of 100% [31]. However, the need for contrast in identifying intra-abdominal injury may not always be relevant in contributing diagnostic value. It can add confidence in cases of interpretation doubts or diagnostic difficulties, but some studies have shown CEUS to have similar sensitivities to baseline US [32].
Splenic injuries are the most common intra-abdominal injury followed the liver in the setting of acute blunt abdominal trauma. CEUS has been shown to be able to overcome the lower sensitive of FAST in detection of traumatic injuries with the reference standard as CT, to reach almost similar levels of accuracies. Evaluation of severity of splenic injuries is particularly important in the decision for surgical management as the spleen should be preserved if possible, due to the dual immunological and haematological functions [33]. However, a retrospective cohort study [34] at a level 1 trauma centre of 332 patients found that patients with spleen, liver, or abdominal vascular injuries were less likely to have false-negative FAST examination results (OR 0.3; 95% CI 0.1 to 0.5). Surprisingly, false-negative FAST results were not associated with increased mortality (OR 0.89; 95% CI 0.42 to 1.9) and these patients were fortunately also less likely to require therapeutic laparotomy. (OR 0.31; 95% CI 0.19 to 0.52).This at first glance may seem puzzling compared to previous studies; however, this is consistent with the generally high specificities of FAST and its lower sensitivities for solid organ injury and lower grade injuries which naturally may be less likely to require surgical intervention or carry a high mortality rate.
Computed Tomography and Abdominal Injuries
Computed Tomography is superior to FAST in evaluating solid organ, hollow vicus, mesenteric injuries and active haemorrhage. However, it has disadvantages such as radiation exposure, risk of contrast nephropathy or allergy, high cost, limited availability, requires more time and the potential need for sedation in paediatric patients. A level 1 trauma canter in the USA reported the radiation exposure of patients with a median ISS of 14 within the first 24 hours at a median of about 40 mSv. The lifelong risk of dying from a carcinoma is assumed to increase by about 0.1 % per 10 mSV. This risk also depends on gender, age and radiation location [19]. Although this is a minute amount, we can conclude that CT scans should be avoided when possible as it does expose the patient to a significant amount of radiation, enough cause a measurable increase in cancer risk.
A recent retrospective analysis evaluated the diagnostic performance of CT for detection of hollow vicus injury (HVI) in patients presenting with penetrating abdominal trauma at a level 1 Nordic trauma centre. Out of the 636 patients with penetrating abdominal trauma, 155 (85%) had a CT-scan on arrival, of which 41 (30%) subsequently underwent emergent surgery. Surgery revealed only 26 (63%) has HVI, showing that CT had 69.2% sensitivity and 90.5% specificity in detecting HVI [35].
Although FAST showed high accuracy for peritoneal fluid, it’s non-specific for solid organ injuries and prevalence of organ injury without accompanying free fluid can range from 5% to 37% [36]. It also lacks sensitivity for hollow viscos and mesenteric injuries, which not are only the most commonly missed but also associated with high morbidity and mortality and has a higher likelihood for requirement of surgical intervention than solid organ injuries. A retrospective study done on 32 patients showed that MDCT could diagnose bowel injury in all of the patients except one. The minor signs showed a higher sensitivity than the major signs [3]. This suggests a sensitivity for bowel injury much greater than FAST which was 12.5% amongst 4 patients and 37.4% in another study [36]. Other studies have also quoted high sensitivities (94%) and PPV (92%) for CT in detecting bowel injury [37]. A meta-analysis [38] of articles concerning the incidence and significance of free intra-abdominal fluid on CT scan of blunt trauma patients without solid organ injury concluded that isolated finding of free intra-abdominal fluid on CT scan in patients with blunt trauma and no solid organ injury does not warrant laparotomy. Instead, its aetiology should be evaluated and other CT signs of GI perforation should be searched for. Small bowel injury had the highest incidence of positive free fluid without evidence of solid injury, but the combination of both pneumoperitoneum and free fluid increased the sensitivity of detection of small bowel injury [3].
When compared with its predecessor DPL, it showed significant advantage in its pre-test probabilities with a positive LR of 10.83 (95% CI 6.45 ± 18.17) and a negative LR of 0.11 (95% C.I. 0.06 ± 0.21). When compared to CT, FAST still had a positive LR 11´42 (95% C.I. 8.01 ± 16.29)) in confirming presence of intra-abdominal injuries, but it was still below acceptable thresholds in safely excluding abdominal injuries (negative LR 0.21 (95% C.I. 0.16 ± 0.29)), which is essentially the gold for immediate trauma management. Hence FAST is unable to be the diagnostic standard for obtaining a definite diagnosis [22].
Whole body CT (WBCT) is the gold standard for trauma imaging, however it is usually only supported by highly specialised trauma centres with the appropriate infrastructure. A clinical review highlighted observational data that suggested WBCT was associated with decreased mortality and time required for trauma evaluation [39]. On the other hand, randomized controlled data from the REACT-2 trial [40] suggests no mortality benefit to this diagnostic tool. There is no clear evidence or sufficient data to prove that CT should be the first line imaging modality in acute blunt abdominal trauma. As we simply lack the resources and time to conduct CT for every patient, not to mention the higher costs and having to subject every patient to ionizing radiation, the decision for CT should remain on a case to case basis. Decision making should be based on a combination of history, physical examination, clinical signs and other imaging modalities i.e. FAST/X-ray. More studies (i.e. RCTs) will have to be done to assess its outcomes over FAST in the emergency setting of BAT and its utility in assessing need for surgical intervention.
A study [41] assessed CT scans of paediatric patients with abdominal trauma for presence, location, and severity of intraabdominal injury, and amount of peritoneal fluid. It was found that only 17% of the 1,486 children had peritoneal fluid demonstrated by CT but 80% had concomitant intraabdominal injury. This suggests that although presence of peritoneal fluid is a strong indicator of intra-abdominal injury, it can be present without, with solid organ injury being the most frequent (68%). Furthermore, it may also indicate that like FAST, CT may have reduced sensitivity in picking up intra-abdominal injuries without peritoneal fluid. CEUS may be applicable for the 37% of patients with intra-abdominal injuries picked up by CT but no peritoneal fluid was detected.
Discussion
In the emergency department today, E-FAST is still the diagnostic standard for ATLS in the event acute abdominal trauma. Its findings, combined with history taking, physical examination and other imaging modalities (i.e. chest/abdominal radiography) would then determine the need for a CT-scan or emergent surgical intervention (i.e. laparotomy). Training with learning objectives and the duration as well as supervision should be standardized with the help of existing scientific principles. FAST demonstrates low to moderate sensitivity and high specificity as a single examination. There have been no studies that examined the utility of serial FAST examination. This is dependent on several factors such as, the time elapsed since trauma, type and extent of injury, patient group (i.e. age, BMI), quality of ultrasound machine, and skills of the FAST examiner. It was also mentioned previously that FAST results are also made on the assumption that fluid tracks to the most gravity dependant parts of the abdomen, and can be influenced by anatomy, location of bleed, respiratory physiology, intra-abdominal adhesions etc. However, it was seen in many studies that many patients who tested negative on FAST did have intra-abdominal injuries subsequently detected on CT or intra-operatively.
To improve sensitivity, the three standard abdominal FAST views should be supplemented by six further sections: sub diaphragmatic, caudal liver margin, parabolic groove, between intestinal loops, retroperitoneal and right upper abdomen view for the detection of free air. The examination should also include visualisation of solid organs such as spleen, liver, and kidneys to assess for injury. Serial exams can also be done at 12hourly intervals to reduce the likelihood of false negatives and reconfirm earlier findings. The effectiveness of serial FAST examinations in patients of deteriorating clinical status was demonstrated in a study that showed a 50% decrease in false-negative rates by 50% and an 85% increase in sensitivity for free fluid detection. The sensitivity and NPV for injury detection increased to 71% and 97%, respectively [42]. These aforementioned strategies can be investigated further through the conducting of randomized controlled trials. Diagnostic errors owing to human error can also be reduced through a more systematic approach such a diagnostic checklist, or management of physician fatigue. Albanese et al. also believed that serial physical examinations are the gold standard for diagnosing GI perforation from blunt abdominal trauma [43].
FAST does offer greater insight than solely relying on clinical signs but it is unsuitable to obtain a diagnosis with sufficient certainty nor can a negative result safely exclude intra-abdominal injury? Possible reasons for poorer accuracy could be that it was in the early post-injury phase, where sufficient hemoperitoneum had not yet accumulated thus leading to false-negative results. FAST has also shown poor sensitivity to identify hollow viscos or solid organ injuries not associated with hemoperitoneum such as early bowel injury or pancreatic injury and limited utility in detecting retroperitoneal haemorrhage. Other potential sources of error include obesity and subcutaneous fat, body habitus and positioning, ascites due to pre-existing medical condition, pre-existing pericardial effusion, and the presence of intra-abdominal cysts or masses [44]. Patients with these characteristics should be evaluated with a subsequent CT-scan if hemodynamically stable.
A comparative study [45] evaluating the use of FAST was done on 706 patients with blunt abdominal trauma. 460 patients were managed with FAST and 246 without FAST. Respectively, both groups showed similar accuracies at 99.1% and 98.0% respectively, and frequency of laparotomies at 13.5% and 14.2%. FAST patients also had a lower mean diagnostic cost and lower mean time required for diagnostic work up. In the FAST group, the computed tomographic rate was 24%, whereas it was 91% in the no-FAST group. As previously established, it’s been shown in many studies that FAST greatly reduced the need for CT-scans, a recent review quoting rates as high as 50%. Although there are surprisingly no significant differences in mortality or laparotomy rates. These two studies show that FAST is cheaper, fast, decreases the length of hospital stay, duration to definitive treatment, and use of healthcare resources [6]. However, it does not actually improve accuracies nor change the management or treatment outcomes of BAT.
Nevertheless, it is shown that peritoneal fluid if present, is highly sensitive to intra-abdominal injury, specifically active haemorrhage which is an indication for emergent laparotomy. This can not only save crucial time in achieving haemostasis instead of waiting for the results of the CT-scan, but is more accurate than DPL which is invasive, or simply clinical signs alone. Moreover, E-FAST is far superior to chest X-ray in terms of detecting haemothorax and pneumothorax and is the only simple bedside method for detecting hemopericardium. Thus, the purpose of E-FAST is for rapid assessment of intra-abdominal that require immediate surgical intervention, especially if the patient is hypotensive, and/or to evaluate the need for a CT-scan. FAST should not replace the abdominal examination or history taking nor be the sole modality replacing CT, for evaluation of abdominal trauma, particularly in patients with abdominal pain, contusions or altered mental status as it’s been shown to intra-abdominal injury can be present even without peritoneal fluid. While CT should not replace FAST either as the 1st line imaging modalities in BAT, a high index of suspicion and low threshold is required. Also, FAST does reduce the frequency of need for CT-scans in the ED and hence the overall costs and radiation exposure to the patient, along with more efficient use of hospital resources. If a new diagnostic algorithm is faster and less expensive it must also be as safe and accurate as the conventional diagnostic algorithm before it can become the new standard of care. Given the current level of evidence we have today, we can conclude that CT should still remain the gold standard for definitive evaluation of blunt abdominal trauma and guide its subsequent management.
Although CT does have greater diagnostic accuracy compared to FAST and is still the gold standard for definitive abdominal trauma imaging, there are little studies done to evaluate the outcomes of patients who have had a CT-scan done without E-FAST. It is established that CT-scan does carry significantly greater number of risks compared to FAST, including requiring more time which the hypotensive patient may not be able to afford. CEUS FAST has showed higher accuracies than conventional FAST in detecting liver, spleen, or kidney injury and active bleeding, similar to that of CT in children and adults with BAT. However, larger randomized trials to evaluated diagnostic accuracy and outcomes will be required to further validate its clinical use as the standard of care [19]. Assuming that major blunt abdominal or multiple trauma is associated with 15% mortality and a CT‐based diagnostic work‐up is considered the current standard of care, 874, 3495, or 21,838 patients are needed per intervention group to demonstrate non‐inferiority of FAST to CT‐based algorithms with non‐inferiority margins of 5%, 2.5%, and 1%, power of 90%, and a type‐I error alpha of 5% [6].
However, studies have shown that despite steady improvement of sonographic resolution properties over the past 20 years, diagnostic precision has not significantly improved, which may suggest that ultrasonography in the emergent setting and the experienced gain may have already reached its limit [22]. Technological advances have allowed recent development of wireless probes [46] and devices capable of short- and long-distance image transmission to remote displays. As ultrasound technology continues to evolve, we expect to see further miniaturization, better image quality and even holography or wearable technology [47]. The FAST exam is easily learned and educational materials are abundant both online (images and video) and in print. As both FAST and E-FAST increase in popularity, implementation of robust educational programs will become increasingly important so that future generations of practitioners are able to acquire high quality sonographic images, interpret those images, and also make real-time clinical decisions based on that information. Trauma centres can look into optimizing infrastructure and trauma protocols to shorten the time required for CT-scan, which has been reported in some studies to be as quick as only a few minutes. It is also crucial to emphasize integration of various sources of information and not to rely solely on a single modality.
Conclusion
FAST is an essential tool for preliminary assessment of intra-abdominal injury, including BAT. A FAST result if positive, in highly confirmative of intra-abdominal injury, for which emergent surgical management is indicated. However, a negative FAST cannot with sufficient diagnostic confidence, rule out intra-abdominal injury. The results of FAST should be considered in conjunction with clinical signs and relevant patient information. Patients with a negative FAST result should continue to be observed clinically, evaluated with serial FAST examinations or CT-scan should intra-abdominal injury be suspected. Developing technologies in Ultrasonography yield promising improvements to the FAST examination but current literature offers no evidence that FAST should replace CT as the diagnostic standard for BAT or its ability to definitively determine the necessity of immediate surgical management.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-ra-id-00152/
https://ijclinmedcasereports.com/pdf/IJCMCR-RA-00152.pdf
#Focused Assessment for Sonography#FAST#E-FAST#Ultrasonography#Point Of Care Ultrasound#Pocus#Blunt Abdominal Trauma#Laparotomy and CT#Lateef F*#IJCMCR#clinical studies
0 notes
Text
Localization and a Typical Aspect of the Chondromyxoid Fibroma in a Child by Echcikhi M*

Abstract
The chondromyxoid tumor is a primitive benign tumor of cartilaginous differentiation. We report the case of a 10-year-old child presenting with an aggressive form of the tumor that mimics a malignant process, atypical localization at the iliac axis.
Keywords: Fibromy Chondromyxoid; Child; IRM
Introduction
The chondromyxoid tumor is a benign benign tumor, presenting 0.5% of primitive tumors. She is generally interested in the metaphysics of the lungs. The objective of our article is to illustrate an aggressive form of this tumor, atypical localization in a child, highlighting the role of the IRM in its taking charge.
Case Report
Child of 10 years, consulted at the emergency room of the Rabat Children's Hospital for a prolonged and painful tumult of the right iliac fossa, rapidly increasing in volume. The biological balance was normal. The radiography objective showed a mixed lithic and condensing lesion, heterogeneous, of the right iliac artery, inciting the realization of an IRM. The IRM has objectiveed a legal process centered on the right iliac axis (Figure 1), multi-locale, in hyposignal T1, hyerignal heterogeneous T2, reproducing multiple septa stages in hyposignal T2 enhanced by Gadolinium, without restriction in diffusion. It is associated with a compact reaction with respect, without overriding adjacent structures. Absence of infiltration of fat or associated adenopathies. The process was in favor of a more benign origin than a chondrosarcome. The chondromyxoid fibroma was among the evacuated diagnostics, and was histologically confirmed. The surgical excision was indicated. A tumor recurrence was objective by a follow-up IRM after 5 months. It should be noted that tumor recurrence is more voluminous than primitive tumor (Figure 1 d).
(a) After
(b) Gadolinium injection, and in sequential T2 in sagittal cup before
(c) 5 months after a surgical resection
(d) The images show a tumor process centered on the right, multi-locus iliac axis, in hyposignal T1 (a), enhanced by Gadolinium (b).
The tumor shows a heterogeneous T2 hyersignal, confirming multiple septa steps in hyposignal T2 (c). It is a compact periodic response with regard to, without overheating of adjunct organs.
Discussion
Chondromyxoid fibrosis generally affects young subjects and manifests itself clinically through pain and tumors. Pathological fractures are common [1]. On standard radiography, at the level of the lungs, one finds an eccentric geographical gap, soufflant the cortical. On the sites where the iliacs are, the tumor is often polycyclic and mixed, associated with a condensation and a bright osseuse. Intra-tumor microcalcifications may be encountered [2]. The IRM is the key exam that can evoke the diagnosis of chondromyxoid fibroma. The myxoid component appears in hyposignal T1, hypersignal T2, and is enhanced by Gadolinium. The IRM also allows the detection of other associated intratumoral components: fibrous, cystic and calcareous [3,4]. Chondromyxoid fibroma is characterized by the absence of intra-medial extension, which allows to differentiate its aggressive form of a chondrosarcoma, the latter being the differential diagnostic principal. In the interest of a meticulous analysis of tumor reports in IRM. Histological confirmation after a biopsy is always indicated [3,4]. The treatment consists of a complete tumor excision with curettage and joint osseux. Note that total resection is not always possible given the frequency of relapses that occur in 25% of cases. The malignant tumor transformation is exceptional [1,2].
Conclusion
The imagery and in particular the IRM play multiple and fundamental roles in taking charge of the chondromyxoid fibroma. The IRM offers a diagnostic orientation, in particular in the case of atypical localization, a precise study of tumor reports guiding surgical treatment, as well as the search for a recurrent postoperative operation.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-cr-id-00151/
https://ijclinmedcasereports.com/pdf/IJCMCR-CR-00151.pdf
0 notes
Text
The Effects of COVID-19 on Hypothalamus: Is it Another Face of SARS-CoV-2 That May Potentially Control the Level of COVID-19 Severity? by Noor-ul-Huda M*

Letter to Editor
As we are all combating the COVID-19 pandemic , a war being imposed by an invisible enemy, each day we need to “spy” the new moves by our enemy in order to design our own strategy. This metamorphic menace has ways to amaze us and to bluff us by presenting in unexpected ways. Since we have never suffered from this novel viral infection before, there is no data to correlate and guide us regarding the possible ways of presentation of this virus. It has pushed us back in teaching ourself the basic science based on observation, building new words from the alphabets we find, and playing Columbus to discover the new faces through which SARS-CoV-2 may manifest itself while looking for the hallmark set of signs and symptoms. The tendency of masquerading itself of the SARS-CoV-2 , a virus that ruined the famous Venetian Carnival as it unveiled itself , has put all the researchers into a mayhem.
Sir, I really want to bring into your kind notice that we have found some signs and symptoms that are related with the central nervous system particularly the hypothalamus. It came into our observation that many patients with COVID-19 infection have presented to us with polyuria and polydipsia with and without polydipsia.
In a short study, we detected at least 27 patients who suffered from “unquenchable thirst” and “ravenous appetite”. 7 of them were diabetic including 2 who were insulin dependent .Most of them did not develop severe COVID-19 . Polydipsia and polyphagia raise suspicion of hypothalamic infliction, since hypothalamus has centers of thirst, hunger and satiety [1]. The interplay between stimulation and inhibition leads to the normal hunger and thirst sensations. We further noted that 21 of them had other signs and symptoms related with peripheral nerves. They all suffered from dysosmia and dysgeusia as well. If we put all of these symptoms together and correlate it with the viral entry through the nose, it is quite simple to explain that SAS-CoV-2 affects the olfactory nerve and from there finds its way to the hypothalamus [2].
Addressing polyphagia and polydipsia separately, if we discuss polyphagia first in relation with hypothalamus , there can be various causes directly or indirectly related with the hunger and satiety centres in the hypothalamus. The most straight-forward mechanism of hunger and satiety is defined by the balance of signals coming from two hypothalamic centers: the lateral hypothalamus that responds to internal and external signals and cause one to feel hungry and the ventromedial hypothalamus that signals satiety. Secondly, polyphagia is It is also the part of the 3Ps of diabetes [3]. With an increasing experimental and clinical evidences showing hypothalamic dysregulation as one of the underlying mechanisms of abnormal glucose metabolism, it can be postulated that hypothalamic infliction is likely in SARS-CoV-2 that leads to polyphagia in both diabetic and non-diabetic patients as well as poor diabetic control in the diabetic patients. Koshiyama et al postulated several points to suggest the role of hypothalamus in causing diabetes mellitus noticeably an increased hypothalamic-pituitary-adrenal axis activity caused by extreme stress [4]. So a deranged hypothalamic function causing diabetic tendency and polyphagia can be one cause. Due to financial constraints, proper blood sugar level testing could not be performed in the non-diabetic patients, however, in the diabetic patients with COVID-19 it was evident that glucose control was poorer .The other important point regarding the causation of polyphagia is the direct effect on the hypothalamic centers for satiety. It is evident that mutations in several genes related with hypothalamic satiety signaling lead to polyphagia and the so called hypothalamic obesity [5]. This points towards a possibility of SARS-CoV-2 affecting hypothalamus not only directly but also via genetic mutations. In a study by Gu et al., neuronal histopathological changes were found in the hypothalamus who in the autopsies of 8 victims of SARS [6].
Nampootheri et al suggested SARS-CoV-2 invasion in the hypothalamus . Hypothalamus plays a key role in hypertension, diabetes, obesity and other risk factors for developing severe COVID-19 infection. They also suggested a non-respiratory system origin for respiratory failure. Hypothalamus being connected to brainstem cardio respiratory centers can cause respiratory arrest. They further showed that the human brain gene-expression analyses revealed that the hypothalamus with its associated regions express angiotensin-converting enzyme 2 and transmembrane proteinase, serine 2 which allows SARS-CoV-2 entry in the cell. They also showed that immunolabeling in human as well as in animal brains proves that the central role of the hypothalamus that by allowing SARS-CoV-2 brain invasion through multiple routes, influences brain susceptibility and various severe manifestation of the COVID-19 infections [7].
If we now discuss polydipsia then again we have various explanations via different causation pathways involving hypothalamus. The most straight forwards pathway is via Angiotens in II . Since SARS-CoV-2 also acts via the ACE2 receptors, somehow at any level whether central or peripheral , it is able to cause polydipsia[8]. Hypothalamus does have osmoreceptors that regulate thirst mechanisms.[9] So, basically, hypothathalamus plays a central role in thirst mechanism. Due to limited resources and an overwhelmed system, we were not able to follow any specific lab investigatory protocol. However, correlating with serum electrolytes and urine output records, none of them had either diabetes insipidus or dehydration. The only notable point was a poorer diabetic control during illness, but this can be from various different reasons, again hypothalamus does play a role in several of such mechanisms including blood sugar control.
Again, if we join all these pieces of information together, with patients presenting with polydipsia and polyphagia as well as signs involving olfactory nerve and other peripheral nerve signs and symptoms and provided the fact that SARS-CoV-2 does interact with the nervous pathways and it also interacts with ACE-II receptors, it is likely thatSARS-CoV-2 finds a way to the hypothalamus leading to the manifestations related with hypothalamic structures.
I believe there is a need to perform further research on this topic. This can be an important point to understand the level of severity of COVID-19 infection and may help in determining a proper management plan with monitoring as well as determining prognosis.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-le-id-00149/
https://ijclinmedcasereports.com/pdf/IJCMCR-LE-00149.pdf
0 notes
Text
On Invariant Speed of Light by Orlov S*

Abstract
A new physical model of the appearance of light, properties, and its trajectory. Explains the paradox of invariance and isotropy of light based on the laws of classical physics.
Keywords: Theory Ofvortex Gravitation; Cosmolog;Cosmogony; Aerodynamics
Introduction
For many years, scientists- physicists have tried to measure the speed of light. Galileo-in the seventeenth century. Early experiment to measure the speed of light was held Ole Roemer, a Danish physicist, in 1676. Another, more accurate way to measure the speed of light is made in Europe Hippolyte Fiziin 1849. Francois Arago determines the speed of light in 1838bya rotating mirror. In 1862, on the production of the speed of light worked Leon Foucault [1]. In 1926,a result of years of efforts Albert Michelsonhas had some very high accuracy of the speed of light:
с = 299 796 000±4 000 m/s
The main and paradoxical conclusion in the study was his invariance speed of light. In other words, the speed of light is the same in all inertial frames of reference is independent of the velocity of the observer and emitter. This surprising fact for the classical physics of his time for the first time proved the Michelson experiment: the independence of the speed of light on the direction (isotropic) and the orbital motion of the Earth around the sun. In the future, this paradox was confirmed by astronomers. In particular, Willem de Sitter in monitoring the spectral binaries found that the speed of light flux from removing the stars and approaches are constant speed of light (c) and equal to each other. That is, they do not depend on the rate of the star (light sources) [2]. From the point of view of classical physics this paradox so far can’t be explained. Therefore, on the basis of the unknown properties of light in 1905, Einstein proposed the special theory of relativity (STR) in the paper "On the Electrodynamics of Moving Bodies" [3]. SRT conclusions were as paradoxical as the invariance of light. On the basis of the SRT can assert that the events simultaneous in one inertial reference frame will not be simultaneous in another, if these frames of reference are moving relative to each other. In this article we propose to explain the origin, properties and the invariance of light, in full compliance with the classical laws of physics using the theory of vortex gravitation, cosmology and cosmogony [4].
Luminiferous Ether
In the theory of vortex gravitation, cosmology and cosmogony all celestial bodies (matter) are essential vortices. The values of the bodies (system of bodies)) and the corresponding vortices may vary to an infinite value. The biggest ethereal vortex that people can watch this universal whirl wind, the smallest atomic. The orbital speed of ether in each vortex increases towards the center of an inverse square law. Change of orbital velocity is inversely proportional to the pressure change in the air. Pressure gradient force creates vortex gravitation. This pattern works equally essential in a whirlwind of various volumes.
In theory, the vortex gravitation obtained an equation to determine the gravitational force in the etheric vortex [4]:
Depending on the next
Where
V - Volume of the nucleons in the body, which is in torsion
r = 8.85×10-12kg /m3 -the density of ether [5]
v(r) - Velocity of ether in the orbit
r - The radius of the orbit are risen the vortex
The same relationship between the force of gravity and orbital velocity exists in atomic torsion (vortex).
Each atomic vortex ether rotation occurs continuously around the core with a radius r, which creates the effect of an atomic attraction. For this scheme, gravity can explain the origin of the interatomic forces of attraction. In theory, the vortex gravitation made the condition that the ether penetrates all matter and the body other than atomic nuclei (nucleons). Maximum speed ether several orders of magnitude greater than the speed of light. The rotational speed and the pressure gradient of ether, and the attractive force Fn on the surface atoms reaches a maximum value.
Make a guess:
The assumption № 1. Under the action of attractive forces on the surface of the atom or on surface of nucleus of the atom or ether stream is converted into an electromagnetic flux including a light. The light has mass. Gravity act on the light. When converting the ether is the emergence into the light particles (photons) with a mass greater than the mass of the particles of the ether -Amer. Increasing the mass of the particles, according to the law of conservation of angular momentum of rotation, must be accompanied by a decrease inversely proportional to the orbital speed of light. Thus, the light gets its velocity- c.
When orbital revolution of the magnetic flux (light) around the atom to it are two forces: the force of the vortex atomic attraction and centrifugal force. For uniform orbital motion of light is needed to create its orbital speed centrifugal force equal to the force of an atomic attraction. This rate is equal to the atomic orbit well-known speed of light-(c). In aerodynamics this force is called the first space. The atomic attraction is generated bythe pressure gradient in the atomic vortex (uravn.4). The pressure gradient is the difference of pressure values in free ester stationary and the center of the vortex. In a free state, the pressure is always constant and maximum. In the center of the vortex ether pressure depends on the rotational speed and air temperature. Upon heating of a substance (atom), the pressure (P)atom in the center increases in proportion to the temperature (T),in accordance with the law of Charles (6): (2)
Then the pressure gradient must be reduced and, in accordance with equation(1) reduces the force of attraction of the vortex. In this case, there comes a predominance of centrifugal force Fc over the forces of atomic, vortex attraction Fn. The speed of light is converted into the second cosmic speed. Lightis removed from the atom at the most economical spiral trajectory according to calculations by Walter Hohmann [7]. At the same time near the surface of the atom (at the lowest atomic orbits), the place flown away luminous flux takes a new ether flow. This stream is the same principle is converted into light. If the external effects (heating) are stored, the conversion and emission light from the atom will continue permanently. This is the nature of light. Light is generated and emitted not by the energy or mass of matter (atoms), but only by making the ether in the light under the influence of the atomic vortex gravitation and external influences (temperature). Light emissions top only when the external action (heating) or destruction of the atom, and with it the atomic vortex.
Fig. 1 shows an aerodynamic scheme of movement of the light flux from a single atom. In the emission of light from the set of atoms aerodynamic design principle does not change, only multiplied many times. Light will always be supplied to each of the observer to any atom on the same helical path (at a large angle to the radius of the light field) with its constant velocity - v. Spiral light fluxes from these atoms can twist in different directions. The orbit planes of light fluxes arranged in space with any inclinations from each other. Thus, the light is almost infinite set of ultra-thin, light, spiral threads. These streams are combined into a single spherical light field. Radius and circumference of the light field in their values are directly proportional. Consequently, the light field radially increases with the same speed of light. If the viewer moves around the light source light over a circular orbital path, and in this case a considerable part of the light will make its spiral rotation along a plane perpendicular to the plane of movement of the observer. Consequently, this light will also enter the observer at a right angle with its constant velocity- v. Isotropy of light is also a consequence of the propagation of light streams through an infinite number of spiral trajectories.
Output: To put the speed of light (c) at the speed of any body (v) in space is possible only according to the laws of vector algebra. Relative movement of any other body in space, light always moves at a right angle. Therefore, the relative velocity of the entering light to any body will always be equal to the absolute speed of light, regardless of the speed of motion of the considered point (O) relative to the light source (S).
Mathematically this can be written: + = - =
Conclusions
The concept of the luminiferous ether was launched in the XVII century Rene Descartes. In the future, the wave theory, the luminiferous ether developed in the writings of Huygens. A detailed justification for this theory was in the XIX century in the framework of wave optics and electromagnetic theory of Maxwell. The proposed spiral model of light is very close to the concept of the wave motion of light and differs only in the trajectory of the light flux.
According to modern concepts light has a dual nature (wave-particle duality): - light has wave properties and is an electromagnetic wave, but is also the stream of particles-photons. It should be noted that until now scientists have not explored yet another important property of light: what is the mechanism and how can instantly disperse photons up to the maximum speed-c?!
Spiral model of the origin and movement of light, this problem is not difficult, because the momentum of the movement all the magnetic flux received from the ether, which at the outbreak of the world itself was moving at a speed exceeding the speed of light. Under Chapter 2 of this article can be argued that this is a consequence of the invariance of the light path of movement of the light flux. Researchers relative velocity of light in their calculations are not stacked vector velocities and their modules. The movement of the luminous flux is not contrary to the laws of classical physics. Invariance was introduced into scientific consideration only because of a misunderstanding of the movement of light as straight and radial.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-rw-id-00148/
https://ijclinmedcasereports.com/pdf/IJCMCR-RW-00148.pdf
1 note
·
View note
Text
Free Strand of the Greater Omentum in Surgical Practice and its Morphological Characteristics by Martynov Vladimir L

Abstract
In his operating work, the surgeon often uses the patient's tissue to solve practical problems. For our work, the data of Liebermann-Meffert D. and White H. (1989) on the greater omentum are of interest [1]. Research shows that the "policeman of the abdominal cavity" - the great omentum in pathological conditions, acquires very special properties: plasticity; the ability to adhere to an injured and inflamed surface; the ability to hemostasis; the ability for ingrowth and revascularization; the ability to absorb liquids and microparticles from the abdominal cavity; the ability to phagocytosis and immunological response. Adhesions with the omentum are formed much faster than with other organs of the abdominal cavity. Even the freely transplanted omentum tissue without blood supply retains these properties. After 21 days, the omentum tissue is completely fused with the recipient [2].
Introduction
Experimental studies of ingrowth of the omentum graft and its vessels are very indicative. Sections of the omentum of different thickness and size were separated from its bulk and fixed without revascularization to various organs and tissues of the same or another animal: stomach, small and large intestine, liver, spleen, kidney, urinary bladder, lung, pleura, peritoneum, mesentery, aorta, inferior vena cava. Within a week, the graft is firmly attached to the tissues of the recipient organs, its separation is difficult, due to a decrease in the amount of fat, its thickness is reduced, necrobiotic processes, necrosis zones are reduced. After three weeks, the graft cannot be separated, when an attempt is made, bleeding occurs, the amount of fat decreases and is replaced by dense fibro- and angioplastic tissues so that its surface resembles the surface of the recipient tissue. After 12 weeks, it is difficult to distinguish the omentum tissue from the recipient tissue; the suture line serves as a reference point. The engraftment of free grafts did not depend on their size, but necrosis zones are more often formed in thick grafts. The graft remains viable when frozen for two weeks or even longer. Stages of omentum transplant engraftment: attachment - up to 4 hours, beginning of vascular ingrowth - 24 hours, tight fit - 48 hours, revascularization - 3 days, fat resorption - 3 weeks, fibrous degeneration - 24 weeks [1].
These studies allowed us to use a strand of the free area of the greater omentum in the small intestine in 107 patients. Here is an example of the clinical use and preservation of the viability of the free strand of the greater omentum.
Case Report
A 25 years old, was admitted to the GBUZ NO "GKB No. 12" in Nizhny Novgorod on 11.11.2013 with a diagnosis of "Closed abdominal trauma". After dynamic observation, an emergency laparotomy was performed, during which a rupture of the pancreatic head was detected. Outflow of bile, pancreatic juice was not detected. A tampon was brought to the site of damage to the gland through a separate incision in the right lumbar region. The drains were placed in the right lateral canal, in the omental bursa, in the small pelvis. On 20.11.2013, the intake of contents up to 3 liters with an admixture of bile was noted. On an urgent basis, relaparotomy was performed, during which two perforations were revealed on the posterior wall of the vertical part of the 12-PC, each with a diameter of up to 7 mm, from which, after the introduction of methylene blue, a blue discharge began to flow into the stomach. After excision of the edges of the perforations, the latter are sutured with interrupted single-row sutures. The seam line is reinforced with a large gland strand. A drainage-foam rubber system for active aspiration is connected to this zone through the opening of the right lumbar region (the place of the gauze pad). A loop of the jejunum was isolated 30 cm from the Treitz ligament, on which an areflux nutritional jejunostoma was formed with an interintestinal anastomosis according to Brown and a "plug" on the leading loop 1 cm below the anastomosis. The stoma was placed in the left mesogastric region. A feeding tube was inserted 25 cm behind the anastomosis line.
On January 20, 2014, the patient was admitted to the Nizhny Novgorod City Clinical Hospital No. 12 for the second stage of treatment - closing the nutritional jejunostomy. The skin around the stoma is intact. Performed fistuloenterography through a probe introduced into the leading section of the stoma to the "plug". The contrast does not pass through the "plug" zone, which confirms its areflux function.
01/23/2014 under general anesthesia in the left mesogastric region with two bordering incisions around the stoma, the latter was isolated from the tissues of the anterior abdominal wall. The segment of the intestine with the stoma is brought out to the anterior abdominal wall. The area of the free omentum with the ligature, which acts as a "plug", is viable, loosely welded to the jejunum. The interintestinal anastomosis is passable. Near the anastomosis, the sections of the intestine were stitched with the UO apparatus. The section of the intestine bearing the stoma was resected. The intestinal stumps were additionally sutured with two semi-lace sutures each. Layered suture of the wound of the anterior abdominal wall. Preparation: a section of the jejunum up to 10 cm long with a stoma and a free section of the greater omentum - “plugs”. The area of the free omentum with a ligature, which acts as a "plug", was loosely welded to the jejunum (Fig. 3). The mucous membrane of the jejunum of the "plug" formation zone is not visually changed (Fig. 4). The interintestinal anastomosis is passable.
Morphological examination of the "plug" zone at 3, 6, 9, 12 hours of the intestinal wall circumference showed only edema, moderate lymphohistiocytic infiltration, moderate circulatory disorders [3].
The wound healed by primary intention. In satisfactory condition 02/03/2013 was discharged for outpatient observation by a surgeon.
Conclusion
Thus, our observation confirms the possibility of using a strand of "free", devascularized omentum as a plastic material in small bowel surgery.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-cr-id-00147/
https://ijclinmedcasereports.com/pdf/IJCMCR-CR-00147.pdf
0 notes
Text
A Modified Supine Positioning Setup for Diabetic Foot Reconstruction with Peroneal Artery Perforator Based Propeller Flap: Technique Tips and Tricks by Xiangxia L*

Abstract
Most posterior hind-foot and ankle surgery is traditionally setup in a prone position for better access during the surgery. When using the peroneal artery perforator based propeller flap to reconstruct the complex wound of a diabetic foot, the best approach to dissect the perforator vessels is from anterior aspect when the patient lays on supine with leg rotated internally, obviously this position put a lot of stress on the surgeons to get the access of the heel, vice versa. Furthermore, in some cases the co-morbidity of the patient may limit the patient from lying on prone for a long hour surgery under general anesthesia for safety reasons. In this article we present a 54 years old male complex wound case of diabetic foot with skin necrosis in heel and medial ankle area (Figure 1), which was reconstructed with peroneal artery perforator based propeller flap. The purpose of this paper is to describe in detail of an innovative and modified supine positioning during the surgery, which facilitated both the harvest of flap and reconstruction of the heel and ankle procedure.
Keywords: Surgical Positioning; Diabetic Foot; Propeller Flap; Reconstruction; Level of Evidence: Level V; Expert Opinion.
Techniques
The patient is placed in traditional supine position and bilateral upper extremities are tugged on the sides of the body with intravenous access on the right hand contralateral to the left foot to be operated on. All the potential pressure points are protected. The whole left lower extremity is prepped and draped. A sterile pneumatic thigh tourniquet is applied. A self-invented C shaped abdominal retractor (Figure 2), which is widely used in abdominal surgery, is applied with the curve pointing caudally (Figure 3a). The left lower extremity can be placed on the surgical table while the surgeons are dissecting the perforator vessels or placed on the bar of C shaped abdominal retractor with appropriate padding while the surgeons need to access the heel and posterior aspect of the lower leg to harvest and inset the flap (Figure 3b and c). After the flap is harvest, the tourniquet is released and the split-thickness skin graft is harvested from the upper thigh by Zimmer® dermatome. With the support of retractor, surgeons are able to change the lower leg position easily and maintain the position to get access of the heel and posterior aspect of lower leg. The defects are successfully covered by the propeller flap based on a single perforator of peroneal vessels (Figure 4).
Figure 2: The setup of C shape retractor during the abdominal surgery on lateral view.
Figure 3: The setup of C shape retractor during the heel reconstruction surgery.
Figure 3a: Initial setup of C shape retractor with lower extremity on the table.
Figure 3b and 3c: The lateral and bottom view when the lower extremity is placed on the C bar with cushion underneath.
Discussion
It is estimated that 12 percent of diabetic patients could develop foot ulceration during their lifetime.5For complex wounds with bone and/or tendon exposure in patients with multiple co-morbidities, the selection of reconstructive options was limited. More and more studies supported the peroneal/posterior tibial/anterior tibial artery perforator based flaps as a powerful tool in diabetic patients with compromised lower leg circulation.3,4Appropriate surgical position is crucial for both the safety of the patients and the efficiency of the procedure.1,2,8,9,11The best position for posterior hind-foot and ankle procedure is prone.12While in diabetic foot reconstruction, there are a significantly large percentage of patient having multiple co-morbidity diseases, by putting them on prone position for a long hour’s surgery may jeopardize the patients’ safety.6The anterior approach is a safe and fast track to dissect the peroneal artery perforator vessels, which means the patient would lay on supine position with lower leg internally rotated. Unfortunately, a traditional supine position is a nightmare for the posterior hind-foot and ankle procedures because surgeons may only have limited access to the surgical field, oftentimes the lower extremity must be raised and held consistently by an assistant. In some scenario this position dilemma may be solved by lateral decubitus position, but it is inapplicable in our patient because he had a wound on the medial malleolus area needs to be covered at the same time. Lower leg Mayo stand pad may help the surgeons to access the heel and ankle, and keep the anterior approach for the perforator vessels dissection, while there is no access for flap harvest and skin grafting.7,10 Our circulation nurses come up with an innovative idea of using the abdominal retractor to support the lower leg while keeping the supine position (Figure 3).
Figure 4: The postoperative picture of medial aspect and posterior aspect of the foot.
This abdominal retractor was invented by Dr. Liang Lijian from the Division of Hepatic Surgery in our hospital and widely applied in abdominal surgery (Figure 2). With the support by the retractor’s C shape bar, we are able to access both anterior and posterior of the lower leg. Also it is convenient to switch the position during the surgery and there is minimal impact on the skin harvesting procedure on the thigh. This position could be one of the best solutions for our patient who could not tolerate general anesthesia and prone position. Furthermore we are thinking of making a customized supportive device to accomplish the idea and provide more convenient surgical position for this type of procedure. With the possible help for the device, surgeons will be able to place the patient in supine position and perform the posterior hind-foot and ankle procedure without any struggle.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest in respect to the research, authorship, and publication of this article.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-cr-id-00146/
https://ijclinmedcasereports.com/pdf/IJCMCR-CR-00146.pdf
#Surgical Positioning#Diabetic Foot#Propeller Flap#Level of Evidence#Level V;#Expert Opinion#Xiangxia L*#IJCMCR#clinical studies
0 notes
Text
Semicircular Canal Fistulas and Hearing Loss. Single Surgeon’s Experience by Stefano Dallari*

Abstract
Fistulas of the lateral semicircular canal may occur mainly in cholesteatoma cases, both as consequence of the disease and an excessive or inadvertent drilling of the bone. The risk of significant hearing loss had been stressed, especially in the past. More recent experiences have shown that a careful approach allows to save the pre-operative hearing in the majority of the cases, even when the cholesteatoma matrix is removed from the fistula and the canal is plugged. The author presents his experience in 22 cases collected since year 1989.
Keywords: Labyrinthine Fistula; Hearing Loss; Cholesteatoma
Introduction
Fistulas of the semicircular canals may be primitive or follow an erosive process of the endochondral bone of the labyrinth. A type of primitive/malformation fistula involves the superior canal and may show up as Minor's Syndrome [1]. Also, the posterior semicircular canal may be involved, in rare cases associated with a high-riding jugular bulb and fibrous dysplasia [2]. Secondary fistulas generally follow a middle ear infection, most of the cases a cholesteatoma [3].
An iatrogenic origin should also be taken into account, as a consequence of an excessive drilling during a middle ear surgical procedure [4]. Because of its anatomical location, the lateral semicircular canal is normally involved. As reported in the literature, a fistula of the semicircular canal brings a variable, often high risk of hearing loss until anacusis, due to the damage to the membranous labyrinth [5]. The crucial point is the injury to the endosteum of the canal, while its blue lining is considered safe. When dealing with fistulas due to a bony erosion caused by a cholesteatoma, removal of the matrix may lead to open the endosteum. This is why, especially in the past, for fistulas of more than 2 mm, leaving a piece of matrix in place, over the fistula, used to be advised [6]. It had also been demonstrated that, at a second look operation, most of the time this piece of matrix disappears into normal mucosa.
Conversely, in the more recent literature there have been several suggestions for a careful but complete removal of the matrix, with immediate coverage of the fistula with autologous tissue, even until the obliteration of the canal itself [7,8,9].
The Author’s attitude has always been a careful removal of the pathology and, in regards to the matrix, the decision of completely removing it or leaving a piece over the fistula was based upon the size of the fistula but also the easiness of detaching the matrix from the endosteum. When the detachment seemed to be too difficult, a piece of matrix and/or inflammatory mucosa was left over the fistula itself. The Author’s series was revised mainly in the light of the audiologic outcome and the results will be hereby reported.
Materials and Methods
From 1989 up to December 2019 the Author performed 111 tympanoplasties (TPLs) for cholesteatoma (65 males and 46 females), 39 TPLs for other diseases (28 males and 11 females) and 8 “radical” operations (4 males and 4 females). In 22 cases (15 males and 7 females), a fistula of the lateral semicircular canal was detected (18 cases) or provoked (4 iatrogenic cases). In Table I all these 22 cases are described. Several items have been taken into account: sex, age at operation, ear pathology, year of surgery, pre-operative imaging availability, state of the facial nerve (covered, exposed, pre-operative presence of palsy), state of the semicircular canal, in accordance with the classification of Dornhoffer and Milewski [10], simplified (simple bone erosion with presence of a “blue line”, type I; bony fistula with endosteum exposed and closed, type II or open, type III), type of operation performed, pre-operative hearing (air conduction between 500 and 4000 Hz), post-operative hearing (air conduction between 500 and 4000 Hz) and post-operative bone conduction (0.5,1,2,4 kHz) as compared with the pre-operative one.
Results
The results will be hereby globally analyzed. Furthermore, six cases will be reported and documented, to illustrate the various scenarios. The series consists of 22 patients, 15 males (mean age 52 years) and 7 females (mean age 46 years).
Over the whole number of cases, the incidence of fistula is 14 % (22/158). All the cases but one had a middle ear cholesteatoma. The sole non-cholesteatoma case was an iatrogenic one. Thus, the percentage among the cholesteatoma cases is 21/111 (19 %). In 11/22 patients a pre-operative CT had been performed. In all cases but one (case n. 3 of the year 1991), where a complete fistula was present, with endosteum exposed, the exam was positive for fistula. For the three cases with bony erosion (blue-lined canal) caused by the pathology, imaging was not available. In the iatrogenic cases the CT was negative. In regards to the facial nerve, it was exposed in 13/22 cases and closed in the remaining 9/22. In all the four cases where the endosteum was open, the facial nerve was exposed. None of the cases had a pre-operative palsy, neither post-operative. The case n. 22 presented with a facial palsy grade V which was confirmed not to be due to the pathology (adenoma of the middle ear), but to be incidental. The palsy completely recovered after three months.
Coming to the conditions of the semicircular canal, in 4/22 cases (18 %) there was a complete fistula with the endosteum open. The presence of the matrix of the cholesteatoma onto the canal was mentioned in only one of these four cases (case n. 18), where it was removed, in presence of an open endosteum (see description of the case). In 9/22 cases (41 %) the endosteum was exposed, closed. For these cases the operation report did not mention if the fistula was covered by the matrix of the cholesteatoma. Conversely, the presence of the matrix over the canal was reported in further 5/22 cases besides the case n. 18 (see before), for a percentage of 27 % (6/22). It was removed in 3/6 cases, leaving an intact endosteum in two cases and an open one in the case n. 18, and left in situ in 3/5 cases. Finally, in 3 cases (n. 8, 9 and 16), there was a simple erosion of the bone with a blue-lined canal. The ”iatrogenic cases” are 4/22 (18 %): the n. 12 (endosteum exposed, closed, due to excessive drilling); the n. 14 (bone erosion due to the curette-removal of hyperostotic bone over the lateral semicircular canal); the n. 19 (endosteum exposed, closed, due to excessive drilling); the n. 22 (bony fistula with endosteum intact, due to delayed anatomical recognition).
In 14/22 cases (64 %) an open TPL was performed, while a closed TPL was carried out in 5/22 cases (23 %). In the remaining 3/22 cases (14 %) the fistula was detected during a revision of closed TPL which was converted to an open one. Post-operative audiologic data were available for 14/22 patients. Among Figure 1: Case n. 15. The left lateral semicircular canal is absent in his superomedial aspect. The endosteum is exposed and open. A piece of absorbable gelatin is ready to seal the hole. The facial nerve is exposed. these 14 patients there were 3 of the four patients with a fistula with open endosteum. None of them had a worsening of the bone conduction. Only in 1/14 patients with post-operative hearing data, there was a deterioration of the bone conduction curve. It was the case n. 12, iatrogenic, with endosteum exposed, closed. Furthermore, the author does not remember a case of total hearing loss in this group of patients.
(a): Iatrogenic maneuver
(b): The patient was operated on, twelve month later, for the
II stage. The zone of the fistula appeared close with neo-bone
(c): Iatrogenic maneuver
(d): Iatrogenic maneuver
(e): The patient had been operated on for closed TPL I stage in
2013, for intact TM cholesteatoma. At that time the facial nerve
was closed and no lateral scc erosion was present
(f): The patient presented with a right facial paralysis grade V,
not related to the ear pathology. He completely recovered three
months after the operation
(g): Iatrogenic maneuver
Clinical Cases
Case n. 15
(Fig. 1) R.M, male, 69-year-old. Long history of left hearing loss. In September 2005 he suffered for an acute episode of vertigo. The ENT workout confirmed a significant left mixed hearing loss. The CT of the ear showed an opacification of the whole middle ear with erosion of the lateral semicircular canal. He underwent surgery in November 2005 and a huge bony fistula, with endosteum open, was confirmed. The facial nerve was exposed in the tympanic segment and covered by the cholesteatoma matrix. An open TPL was performed and the fistula was cleaned and then repaired with absorbable gelatin+ bone+ fascia. The operation was uneventful, with no vertigo and the 48-hour post-operative bone conduction curve was unchanged. The patient recovered well and was lost to follow-up. Information acquired for this paper says that the patient is still alive and his ear situation is stable with no further problems.
Case n. 17
(Fig. 2) G.G., male, 62-year-old. History of left hearing loss. Before referring to us, in the beginning of year 2008, he suffered for recurrent episodes of peripheral vertigo. A CT showed a diffuse involvement of the left middle ear with a probable fistula of the lateral semicircular canal. There was a significant mixed left hearing loss. The patient underwent surgery in April 2008. An erosion of the bony semicircular canal was confirmed. It was covered by the matrix of the cholesteatoma, which covered also the facial nerve, exposed along the whole tympanic segment and second genu. An open TPL was performed, leaving a piece of the cholesteatoma matrix/inflammatory mucosa onto the fistula. The post-operative evolution was good. No worsening of the bone conduction occurred. The patient has been recalled in the occasion of this paper. Under otomicroscopic examination a well done and healthy open TPL cavity was evident, with adequately-sized meatoplasty. There was a mixed hearing loss with the air conduction significantly better than after the operation, while the bone conduction had worsened, with a reduction of the air-bone gap. The patient was extremely satisfied, saying that after the operation he had no more problem, especially no more vertigo episodes nor dizziness. He mildly complained of the earing loss but does not require a hearing aid. He is still working.
Figure 1: Case n. 15. The left lateral semicircular canal is absent in his superomedial aspect. The endosteum is exposed and open. A piece of absorbable gelatin is ready to seal the hole. The facial nerve is exposed.
Figure 2: Case n. 17. Upper row: At the axial (left) and coronal (right) CT view, an erosion of the left lateral semicircular canal is evident. Lower row: A piece of mucosa is left over the semicircular canal bone erosion and also partially over the exposed facial nerve.
Case n. 18
(Fig.3) L.C., male, 62-year-old. Seen in the year 2008 for right chronic otitis media with discharge and evidence of cholesteatoma. The CT confirmed the involvement of the middle ear and showed an evident amputation of the lateral semicircular canal. He had a low-to-medium-grade mixed right hearing loss with a small air-bone gap. The patient was operated on in May 2008. A bony fistula, covered by the cholesteatoma matrix was detected. The matrix was carefully removed and an opening in the endosteum was found. This was immediately sealed with fascia + bone pate. The facial nerve was widely exposed, from the cog to the second genu. An open TPL with an ossicular reconstruction (titanium PORP) was performed. The post-operative outcome was good. The patient had no vertigo and a bone conduction control after 10 days showed no worsening of the curve. The patient recovered well and the hearing level remained as it was pre-operatively. He was strictly followed and ten months later a mastoid recurrence of the cholesteatoma was removed. Over the years the ear has remained stable, with a dry small perforation of the new-TM. As a piece of information, all the patients operated by the Author for open TPL are advised to clean the operated ear, at least twice a week, with a warm boric or boricsalicylic solution [11]. In regards to the hearing, the bone curve was unchanged after seven months following the revision surgery, then started to deteriorate. At the most recent control, in April 2020, the ear is persistently stable but the hearing has worsened to a middle-to-high grade mixed hearing loss.
Figure 3: Case n. 18. Upper row: CT axial view. Middle row: CT coronal view. A wide opening of the right semicircular canal is evident. Inferior row: the superomedial half of the bony right lateral semicircular canal is absent. After careful matrix removal the endosteum is exposed and open.
Case n. 19
(Fig.4) F.D., female, 47-year-old. She suffered for recurrent right ear discharge since her childhood, with hearing loss. In the year 2011 the situation worsened and the patient saw an ENT specialist who detected the presence of cholesteatoma, requested a middle ear CT and referred her to the author. There was a conductive hearing loss with a substantially normal bone conduction. The patient underwent surgery in February 2012. A posterior-superior bony erosion with granulation tissue and cholesteatoma was detected. The ossicular chain was involved by the cholesteatoma and blocked. The mastoid was contracted and poorly pneumatized. The facial nerve was exposed at the second genu. An open TPL was planned and performed. During the bone-drilling, the endosteum of the lateral semicircular canal was exposed to a grade where the gently pushing on the stapes provoked a bulging of the endosteum itself. The bony erosion was immediately sealed with bone pate and the operation concluded uneventfully. No ossicular reconstruction was performed. The patient had no problem and she has been regularly followed. The hearing remained as it was before the operation. She always refused to undergo a reconstructive/ functional operation. The most recent control was performed in February 2020.
Figure 4: Case n. 19. Upper row. CT, axial view (left) and coronal view (right). The right semicircular canal is covered by bone. Lower row. The excessive drilling has exposed the endosteum of the right lateral semicircular canal. Pressing onto the footplate causes a movement of the endosteum itself.
Case n. 20
(Fig.5) S.G., male, 47-year-old. Referred to the author in February 2012 with an history of recurrent right ear discharge for several years. A previous ENT examination showed an erosion of the scutum with granulation tissue and cholesteatoma. A CT confirmed the involvement of the middle ear and a probable fistula of the lateral semicircular canal. There was a mild conductive right hearing loss. The patient underwent operation in March 2012. There was a huge tympanic-mastoid cholesteatoma. After careful removal of the matrix, a bony erosion of the lateral semicircular canal was detected. The endosteum appeared to be covered by a minimum slice of bone and there was no mechanic transmission when gently pushing onto a mobile stapes. The facial nerve was covered/closed. An open TPL was performed with ossicular reconstruction (titanium PORP). The patient did well and post-operative hearing was improved and grossly normal. The patient was lost to follow-up and recalled for evaluation in June 2020. He reported a good and stable condition of his right ear for the first six post-operative years. In the last two years, instead, he suffered for recurrent inflammations and underwent ENT examinations without significant results. A CT was suggested and performed at the beginning of year 2020. Despite the surgical cavity was filled with crusts and epithelial debris, it seemed to observe a regeneration of the bone over the lateral semicircular canal. The patient was followed by the author and the local situation led to healing. An audiogram performed on August 24, 2020, showed a mild conductive right hearing loss (500 to 4000 Hz: 35,35,50,50), with bone conduction still normal.
Figure 5: Case n. 20. Upper row: CT axial view (left) and coronal view (right). It seems to be a thin bony remnant over the right lateral semicircular canal. Lower row: after careful cholesteatoma matrix removal (left), a bony erosion is evident with nearly exposure of the endosteum (right, white arrow).
Case n. 22
(Fig.6) M.S., male, 22-year-old. In May 2017 the patient had a documented episode of pure conductive hearing loss (50-45 dB from 500 to 4000 Hz) and tinnitus, with a tympanogram type B, which completely recovered within a month after local and general steroid therapy, and was interpreted as serous otitis media. A further control in July 2017 confirmed a normal hearing and a type A tympanogram. In February 2020 the patient was seen at the author’s institution with an acute right facial palsy (grade V, House-Brackman scale). He complained of few symptoms in the ear but a hearing loss. At endoscopic and otomicroscopic examination, a posterior-superior bulging of the tympanic membrane (TM) was observed and an explorative myringotomy was performed which was substantially negative. Both a CT and MRI of the ear were obtained, showing a complete opacification of the middle ear with mastoid inflammation. Besides the suspect of a middle ear inflammation with subsequent irritation of a congenitally dehiscent facial nerve, the hypothesis of a tumor of the facial nerve was also taken into account. An explorative tympano-mastoidectomy was then performed on February 20, 2020. The facial nerve turned out to be closed and the antral-attic mass was histologically diagnosed as “adenoma”. In order to remove this thick and adherent tissue, a posterior tympanotomy was planned. During the drilling, and because of the presence of the pathologic tissue, an excessive thinning of the bone over the lateral semicircular canal was realized only when a complete aperture of the bone had occurred. Fortunately, a thick endosteum was still intact and the bony fistula was immediately sealed with bone pate. In order to completely remove the pathology, the posterior bony wall was temporarily removed, then repositioned and stabilized with bone pate + fibrin glue. A first stage closed TPL was thus accomplished. The patient had mild vertigo for three days. A bone conduction control was performed 4 and 6 days postoperatively and it was as before the operation. The patient was then followed and the last control was at June 2020. The healing was completed with a well oriented and trophic tympanic membrane. A 50-60 dB conductive hearing loss was detected, as normal after first stage TPL. The facial palsy completely recovered. The patient still complains of episodic short spins of unbalance. An MRI control has been planned.
Figure 6: Case n. 22. Upper row: CT axial view (left) and coronal view (right). The right lateral semicircular canal is closed. Lower row: the excessive drilling over the right lateral semicircular canal has been recognized when the endosteum was already exposed. Black star: pathologic tissue (adenoma).
Discussion
As easy to understand, erosions of the lateral semicircular canal with exposure of the membranous labyrinth (endosteum) and even rupture of it, happen in the great majority of cases when dealing with a cholesteatoma of the middle ear. An exposed facial nerve is also a common finding and its frequency easy to understand as well.
Significant hearing loss has to be taken into account when dealing with a fistula of the lateral semicircular canal. It may happen also when the post-operative fistula test is negative. This is what reported by Yeho et al. (2004) [4], in the two cases of iatrogenic fistula they could observe. Besides the incomplete reliability of such maneuver, it may also mean that this negativity was caused by a hypofunction of the damaged labyrinth but, finally, also that the auditive (cochlear) partition is more sensible than the vestibular one. Surgically created (iatrogenic) fistulas have been reported to occur in 0.1% of the cases or less, with a good hearing outcome in the majority of such patients [12].
In the author’s series the percentage of iatrogenic fistula is 2.5 % (4/22) and the good hearing outcome is confirmed. It is the author’s opinion that the rate of occurrence is probably higher than reported in the literature, where the Authors generally present such cases without mentioning the number of their whole series [13]. The prevalence of the fistulas of the lateral semicircular canal, instead, in the author’s series, is 14 % (22 cases over 158 patients), which rises to 19 % when considering the sole cholesteatoma cases (21/111). Naderpour et al. (2008) [14] examined series from the year 1978 to the year 2000 and the percentage varies from 2.9% to 21%.
More recently Meyer et al. (2016) [3] report a prevalence of 6 % in their series, with a huge number (16/42) of type I fistulas, that is a simple bone erosion, according to the classification of Dornhoffer and Milewski [10].
The percentage reported by Rosito et al. (2019) [5] is 2.7 %. These authors considered only the type II (endosteum exposed) and III (endosteum exposed and open). In the Author’s series, when considering the sole cases with open endosteum (type III), the percentage is 2.5 % (whole series, 4/158) or to 3.6 % (cholesteatoma cases, 4/111). Adding the type II cases (9/22), the percentage rises to 8.2 % (whole series, 13/158) or 11.7 % (cholesteatoma cases, 13/111). Because the main purpose of this paper was to evaluate the audiological effects caused both by a spontaneous exposure of the membranous labyrinth or by its inadvertent uncovering by excessive bone removal, all the three types of fistula were considered. Indeed, the aim was to test the mechanical and noise effect that an excessive drilling and any manipulation (palpation, suctioning, cleaning), even careful, might cause. In regards to these effects, the results seem to be good. Even though the numbers are small, the sensorineural hearing outcome (bone conduction) was encouraging and a post-operative deterioration was observed in only one case.
Satisfactory hearing results seem also to confirm that a careful manipulation and removal of the cholesteatoma matrix is a significantly safe maneuver, as it is in regards to an exposed facial nerve. None of the author’s patients with an exposed facial nerve, in fact, developed a post-operative palsy. The author has no experience of the complete obliteration of the semicircular canal, which too seems to be a safe maneuver in regards to hearing preservation
Conclusion
When dealing with a middle ear cholesteatoma, the possibility of finding a fistula of the lateral semicircular canal, as well as an exposed facial nerve, has always to be kept in careful account. This was mandatory when imaging was not routinely obtained and before the CT era. Nonetheless, even though high quality CTs allow an easier detection of the bony erosions, attention must constantly be paid as well. In regards to how to manage the fistula, the ongoing experience has validated the strategy of a careful removal and an immediate seal of an eventual open endosteum, with biologic means. Also, a complete obliteration of the canal has proved to be safe. As reported in the literature and also in the author’s experience such a careful attitude reduces the risk of sensorineural hearing loss to a minimum. Furthermore, in the author’s opinion, the choice of leaving a piece of matrix on top of a wide bony erosion, which appears to be soft at a careful palpation, is still an advisable option (mandatory in the case of the only hearing ear), trusting in its mucosal transformation, as seen during second look operations.
Acknowledgment
The author wishes to thank Massimo Giuliano Bonetti, MD (Neuroradiology Unit, Department of Radiology, “A. Murri” Hospital, Fermo, Italy) for his valuable help in the choice of.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-cr-id-00145/
https://ijclinmedcasereports.com/pdf/IJCMCR-CR-00145.pdf
0 notes
Text
Female Pelvis Case Report: How a Traditional Anatomy Class Can Help Medical Students? by Danilo Euclides F

Abstract
Background: During anatomy (topographic) chair, we prepared an anatomic piece of an older female pelvis (unknown causa mortis). Here, we present an anatomic piece prepared by medical students that helped us to better understand hypertrophic bladder pathophysiology.
Methods: A traditional corpse dissection guided by an assistant professor
Results: Corpse dissection enhanced our personal experience during the medical course. It also helped us to better visualize how big a hypertrophic urinary bladder can become as the etiologic cause is not taken care.
Conclusions: Despite virtual and 3D anatomy lessons, we believe corpse dissection must remain as a teaching strategy that can help to build a new generation of surgeons as well as honor the History of Medicine.
Keywords: Anatomy; Medical Education; Teaching; Students; Graduate Medical Education
Introduction
During the anatomy (topographic) chair at our institution, we dissected and prepared an anatomic piece of an older female pelvis (unknown causa mortis). Her corpse was donated to the Universidade Federal de São Paulo to help medical students to learn clinical-surgical anatomy. As medical education becomes more and more modern, corpses dissection remains on the history of anatomy teaching and gives space to new technological strategies. Though, we believe some practical skills and surgical abilities can be learned the old-fashioned way through a traditional anatomy lesson. Here, we present an anatomic piece we prepared during our anatomy classes that helped us to better understand hypertrophic bladder pathophysiology. After analyzing the internal genital organs (hypoplastic uterus and ovaries) and the angles, we concluded this pelvis belonged to an old female person.
Diagnostic and discussion
Figure 1 shows the anatomical piece the author prepared under the orientation of Dr. Alexandre Cardoso. During the dissection, we recognized urinary bladder hypertrophy which usually happens in the presence of an outlet obstruction. The most frequent causative factor is benign prostatic hyperplasia in men [1]. Among common causes of bladder outflow obstruction, in women, are [2]:
pelvic organ prolapse
uterine fibroid or tumor
urethral disorders (meatal stenosis, urethral caruncle)
luminal impaired detrusor (stone, bladder/urethral tumor, ureterocele, foreign body)
contractility disorder (senile bladder changes, neurological diseases suchas diabetes mellitus or another peripheral neuropathy); and
functional disorders (such as Fowler's syndrome).
Clinically, even though this is a rare condition among women, clinical investigation must ask poor urinary stream and incomplete bladder emptying. Physical examination should search for mechanical urethral obstruction. Nowadays, ultrasonography has been considered a good non-invasive strategy because of its capacity of assessing presence of residual urine volume and determination of patient’s Uroflow which must be > 15 ml/s on a voided urine volume of over 150 ml [2]. Then, if one suspect of urethral obstruction, clinical history, physical examination and ultrasound may help to diagnose it. As third-year medical students, corpse dissection enhanced our personalexperience during the medical course. It allowed us to manipulate the internal organs as far as we needed to understand its topography in relation to bone and muscle structures. It also helped us to better visualize how big a hypertrophic urinary bladder can become as the etiologic cause is not taken care. Despite our virtual and 3D anatomy lessons, we definitely believe corpse dissection must remain as a teaching strategythat can help to build a new generation of surgeons as well as honor the History of Medicine.
As recently shown, both virtual and cadaver-based anatomy class enhance first year medical students’ experience [3]. Besides, the students may be inspired by corpse dissection to easily engage on studying pathophysiology because it supports their learning processes affectively. It also augment strategies to easily memorize medical contents as well as apply their knowledge to future clinical practice.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-cr-id-00143/
https://ijclinmedcasereports.com/pdf/IJCMCR-CR-00143.pdf
#Anatomy#Medical Education#Teaching#Students#Graduate Medical Education#Danilo Euclides F#IJCMCR#clinical studies
0 notes
Text
Rosai Dorfman Disease: Bull Neck Versusmoon Facies: A balancing Act? A Diagnostic and Therapeutic Dilemma by Kaushal D*

Abstract
Rosai Dorfman Disease is a rare non-neoplastic disorder of unknown etiology presenting with painless massive cervical lymphadenopathy and/or extranodal involvement with a benign course. The challenge lies in diagnosis and deciding the best course of treatment as standard treatment guidelines are currently lacking.Oral steroid therapy, chemotherapy and radiotherapy have been advocated as therapeutic options with limited supporting evidence, each with their potential adverse effects. We present the case of a young male child with bilateral massive cervical lymphadenopathy who we diagnosed as RDD and treated with oral steroids. The challengein our case wasreaching a diagnosis and adjusting the dosage and duration of oral steroid therapyas evidence for appropriate titration of therapy is still lacking. He suffered from adverse effects of prolonged steroid therapy, requiring repeated change in course of management. Currently, he is on close follow-up with reversal of side effects and complete resolution of symptoms.
Keywords: Rosai Dorfman Disease; Massive Cervical Lymphadenopathy; Bull Neck, Moon Facies; Sinus Histiocytosis
Introduction
Sinus histiocytosis with massive lymphadenopathy, also known as Rosai-Dorfman disease (RDD) was described first by Rosai and Dorfman in 1969. It is a rare and non-neoplastic histiocytic proliferative disorder ofunknown etiology, with a childhood predilection [1]. Although it resembles malignant disorders in appearance,its clinical course is predominantly benign albeit unpredictable.1Bilateral painless cervical lymphadenopathyis the most common presentation though extra-nodalmanifestations are also reported. The diagnosis is difficult due to nonspecific pathological findings and requires a high index of suspicion. A variable response to steroids and chemotherapeutic drugs has been described in literature however clear guidelines for optimum treatment are lacking [2,3]. We present a case report of a two years old child diagnosed with RDD, treated with long term oral steroid therapy. Dose adjustment posed a unique challenge as the child developed significant side effects of treatment. However, with prolonged and controlled oral steroid therapy, we could achieve complete resolution of symptoms and regression of side effects.
Case Report
A two yearsold boy was brought to our outpatient services (Otorhinolaryngology department) with the complaint of multiple bilateral neck swellings for last 6 months which were painlessand progressively increasing in size. There was no history of weight loss, fever and difficulty in swallowing or breathing or nasal complaints. On examination, there were multiple, mobile,discrete, non-tender bilateral lymph nodes at level II, III, IV and V, the largest measuring 4x3 cm.
Investigations showed raised leucocyte counts(37310/cu. mm), erythrocyte sedimentation rate (70 mm in the first hour) and CRP (95.4 IU/ml).An ultrasonographic evaluation of neck showed multiple enlarged hypo to anechoic lesions on both sides of the neck, suggestive of cervicallymph nodes. Ultrasound abdomen did not show any mesenteric lymphadenopathy.FNAC (Fine Needle Aspiration Cytology) from lymph nodesshowed a polymorphous population of small and large lymphocytes with few uninucleate and binucleate histiocytes exhibiting emperipolesis. The presence of reactive lymphoid hyperplasia with histiocytosis and focal emperipolesis was suggestive of a diagnosis of RDD (Figure 2a).He was also subjected to excisional biopsy from the lymph node elsewhere for which we did a slide review. Immunohistochemistry showed strong positivityfor S100 protein (Figure 2b) and negativity for CD1a (Figure 2c).
ZiehlNeelsen (ZN) staining revealed noacid-fast bacilli. Thus, the diagnosis of Rosai-Dorfman Disease was established. The child was started on oral steroids(Tablet Prednisolone 0.5mg/kg) in consultation with pediatrician for six weeks with good clinical response. The dose was then tapered (Tab Prednisolone 0.25 mg/kg) over another 6 weeks and treatment was stopped. After a month, the child again developed bilateral cervical lymphadenopathy.He was started on low dose oral steroid (Tab Prednisolone 0.25 mg/kg/day) therapy for 3 months which was tapered slowly over the next 3 months. With continuous steroid therapy, the child developed moon facies (Figure 3a).
Discussion
The most common presentation of Rosai Dorfman Disease is painless massive cervical lymphadenopathy (bull neck) [1]. It may involve extranodal organs such as the central nervous system [4],orbit [5], skin [6] and may mimic malignancy which further complicates the diagnosis and management. It may also be associated with intermittent fever, malaise andweight loss. It shows childhood predilection but can present at any age [3]. Diagnosis is confirmed only with histopathological examination and immunohistochemistry, characterized by the abundance of large foamy histiocytes with emperipolesis along with plasma cells [7]. The clinical course is unpredictable and diverse, usually benign and resolves spontaneouslybut can be very aggressive in nature and can even lead to death [8]. Reasons for the aggressiveness or spontaneous remission are unknown.In this young child, there was no spontaneous remission of cervical lymphadenopathy. After histopathological confirmation, oral steroids were started and there was a dramatic disappearance of lymphadenopathy. However, as the steroids were tapered and stopped, the symptoms again flared up, necessitating the continuation of treatment. Various treatment modalities, for example, chemotherapy (Vinca alkaloid, an alkylating agent and corticosteroid) and radiotherapy have been tried with variable success rates [2]. Nevertheless, literature is inadequate to support the use of either. This observation prompted us to continue the steroids after dose titration to the lowest dose possible. After a year of stopping steroid therapy, the child remains asymptomatic and free of side effects.
Conclusion
The diagnosis of RDD is challenging due to its varied clinical course, as well as nonspecific histopathological appearance andrequires good coordination between the clinician and pathologist. However, trickier than the diagnosis is the treatment owing to lack of sufficient evidence to support the various existing therapeutic modalities.Steroids can be considered as an effective and safe treatment option with fewer side effects under controlled dosage and proper follow up.
Authorship Criteria
Darwin Kaushal: Concept and design of study, Final approval, 'guarantor'
Aman Kumar Verma: Drafting the article
Vidhu Sharma: Drafting the article& Critical Revision
Poonam Elhence: Drafting the article or revising it critically
Prawin Kumar: Drafting the article or revising it critically
Conflict of Interest
None
Grant Information
The author(s) received no specific funding for this work.
Acknowledgements
Informed written consent was taken from the guardian of the patient for clinical photograph.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-cr-id-00142/
https://ijclinmedcasereports.com/pdf/IJCMCR-CR-00142.pdf
#Rosai Dorfman Disease#Massive Cervical Lymphadenopathy#Bull Neck#Moon Facies#Sinus Histiocytosis#Kaushal D*#IJCMCR#clinical studies
0 notes
Text
Fatal Gastric Metastasis in Sarcomatoid Carcinoma of Unknown Primary Origin: Case Report by Silva MC*
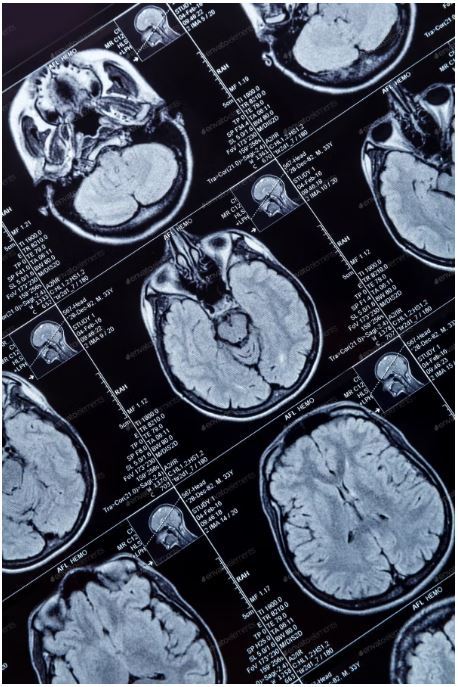
Abstract
Neoplasms of unknown primary origin constitute a group of neoplasms in which the primary site cannot be identified after an exhaustive investigation. Sarcomatoid carcinoma of unknown origin is a very rare entity with nonspecific clinical presentation, frequent systemic dissemination at the moment of diagnosis and an aggressive evolution, so the diagnosis represents a challenge. We present the case of a patient who resorted to the emergency service with a neurological deficit as clinical presentation of a disseminated neoplasm. The complementary diagnostic tests performed demonstrated diffuse metastasis in brain, liver, adrenals, bone and muscles and immunohistochemistry examination of a pulmonary nodule revealed the presence of differentiation markers of epithelial lineage consistent with sarcomatoid carcinoma. Initially a pulmonary origin of the tumor was considered more likely, however, despite testing several specific organ markers it was not possible to confirm this hypothesis nor to determine the primary origin of the tumor because the patient died a month after admission due to severe digestive bleeding resulting from gastric metastasis.
Keywords: Sarcomatoid Carcinoma
Case Presentation
Neoplasms of unknown primary origin are a heterogeneous group of tumors in which the primary site cannot be identified after a thorough investigation [1,2]. Sarcomatoid carcinoma of unknown primary neoplasm is a very rare entity, so there are few published data on its clinical presentation, characteristic histopathological findings, approach or treatment [1,3]. The clinical presentation is nonspecific with frequent systemic metastasis at diagnosis and a very aggressive evolution with significant low survival rates [1,4]. The diagnosis is characterized by a great difficulty where a correlation between clinical, histological and imaging data is required and where immunohistochemistry is the gold standard by using specific markers of cell and organ lineage that allow the identification of the primary tumor type and site [2,3]. We present the case of a 63-year-old man with a history of arterial hypertension, diabetes, dyslipidemia and smoking habits. He turned to the emergency service (ER) due to a decrease of strength and hypoesthesia of the left lower limb with a month of evolution and significant worsening on that day which made walking impossible. He also referred right tempoparietal headache for several days. He denied fever, sweating, anorexia, weight loss, vomiting or other complaints. He performed head computed tomography (CT) that revealed multiple expansive lesions with vasogenic edema corresponding to probable secondary tumor lesions (Figure 1).
It was followed by a chest, abdominal and pelvic CT scan that showed an irregular shaped nodular lesion in the apical-posterior segment of the left upper lung lobe with 6mm in diameter, 3 micronodules in the anterior segment of the same pulmonary lobe and an adenopathic conglomerate in the pulmonary left hilum with 38X24mm. Seven nodular lesions of secondary nature were also identified distributed over both hepatic lobes as well as in both adrenals. He was admitted to the internal medicine service to study a metastatic neoplasm of unknown primary origin. Analytically he had leucocytosis, neutrophilia and increased C-reactive protein without other major changes. A bronchofibroscopy was performed where an irregular and hypervascularized endobronquial mass was observed in the upper division of the upper lobar bronchus consistent with direct signs of a tumor (Figure 2) and a biopsy was performed. A liver nodule biopsy was also done which proved to be unrepresentative.
Positron tomography confirmed the previous findings and detected catching lesions in the sinus of the left buttock muscles and diffuse bone metastasis compatible with an high-metabolic neoplastic pathology. He underwent treatment with dexamethasone and painkillers with a slight improvement in pain complaints and neurological deficits. At discharge he presented liver cytolysis and cholestasis, absent at the admission. He was refferred to the outpatient pulmonology consultation to perform a complementary study on the suspicion of a primary pulmonary lesion. The case was discussed in a multidisciplinary consultation group that proposed the repetition of the liver nodule biopsy and treatment with palliative holocranial radiotherapy, that was performed with good tolerance. Subsequently the result of the pulmonary nodule biopsy was available whose immunohistochemical study demonstrated expression of MNF116 neoplastic cells, focal expression of CK7 and GATA3, membrane expression of CD138 and absense of TTF1, Napsin-A, p40, Synaptophysin and SOX10, revealing a carcinoma with an unusual phenotype in lung neoplasms, so it was suggested that the pulmonary nodule was a metastatic lesion. The second liver nodule biopsy was also inconclusive. The patient maintained a follow-up in pulmonology despite histological exams beiing inconclusive and was awainting for a new group consultation to consider systemic treatment with vinorelbine. About a month after admission he went to the ER for epigastric pain, dark vomiting and dark stools. He underwent an upper digestive endoscopy which revealead multiple (5-10) ulcerated lesions with a crater aspect and size between 5-20mm in the gastric mucosa, suggestive of metastatic lesions (Figure 3).
A few hours after the exam he had an episode of abundant hematemesis that conditioned hypovolemic shock that caused his death. Histological examination of gastric lesions made available posteriorly showed involvement of the mucosa by a neoplasm with characteristics overlapping those observed in the histological examination of the pulmonary nodule concluding that it was a sarcomatoid carcinoma.
Conclusion
This is a rare case of a metastatic sarcomatoid carcinoma in a patient that presentead with a clinic neurological deficit. It is a very rare tumor and poorly differentiated carcinoma that derives from epithelial tissues so it can develop in several anatomical sites and histologically is characterized by presenting epithelial and mesenchymal components [1,4,5]. The most common differential diagnosis is sarcoma and differentiation markers of epithelial lineage are used to make this distinction. Specific organ markers are also tested to determine the origin of the tumor [4,6]. Initially the hypothesis of pulmonary origin was considered, namely a lung sarcomatoid carcinoma which is a rare lung cancer that belongs to the group of non-small cell lung carcinomas (NSCLC) correspondind to only 0.1-0.3% of all lung cancers [4-10]. It usually presents as a solitary mass in the upper lobes that develops from central airways cells [4,6,7] but may also present a peripheral location [10]. Several studies have described that affects mostly men with an average of 65 years old and with a high correlation with smoking [4-7,10]. There is no specific presentation and cough and hemoptysis are the most common symptoms [4]. Differential diagnosis with other primary or secondary lung cancers is difficult and still a challenge [5,8,10]. It is a very aggressive tumor associated with low survival rates, lower than other NSCLC [4,5]. Metastasis occur by hematogenous route and the most affected organs are bone, brain and lungs [4,6]. The immunohistochemical study of the pulmonary nodule identified the presence of specific markers of the epithelial lineage such as CK7 (cytokeratin) and MMF116 characteristic of carcinomas. Although several specific organ markers were tested to establish the differential diagnosis between primary and metastatic tumor such as TTF1, Napsin-A, p40, Synaptophysin and SOX10, it was not possible to successfully determine the primary origin of the tumor that remained unknown [1-3,10]. Occurred a very aggressive clinical evolution that culminated in the patient death due to complications resulting from gastric metastatic lesions that is in agreement with literature for this type of tumor [1,5]. Markers of poor prognosis were identified in some previous studies which may indicate an even more aggressive disease at the moment of diagnosis like functional status, number of metastatic sites and increased lactic dehydrogenase, leucocytosis and neutrophilia that are systemic markers of inflammation with a role in the tumorogenesis process [1,5]. Due to their very low incidence and difficulties in diagnosis, these tumors still have a lack of clinical and pathological characterization that makes greater complementarity between different medical specialties an imperative to provide a reduction in the delay of deffining an accurate diagnosis, beucause this situation causes great anxiety and anguish to the patient and his family. Further studies and research are needed and we hope that advances in molecular biology will reduce this time and increase therapeutic options given the poor results obtained with conventional chemotherapy in these type of neoplasms [1,4].
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-cr-id-00141/
https://ijclinmedcasereports.com/pdf/IJCMCR-CR-00141.pdf
0 notes