Text
Open Access Journal of Gerontology & Geriatric Medicine

Influence of Weight Loss on Quality Of Life, Biochemical & Clinical Parameters among Obese Postmenopausal Women
Authored by Shehab M Abd El Kader and Osama H Al Jiffri
Abstract
Background: Although obesity is common among postmenopausal, to date no study has evaluated the influence of weight loss on quality of life (QOL), biochemical & clinical parameters among obese postmenopausal women.
Objective: This study designed to detect the effects of weight reduction on biochemical & clinical parameters and QOL among obese postmenopausal women.
Material and Methods: Two-hundred Saudi postmenopausal obese women enrolled in this study, their age will be ranged from 50- 58 years and their body mass index (BMI) ranged from 30-35 kg/m2. All participants were divided into two equal groups: group (A) received weight reduction program (aerobic exercise and diet regimen) for 3 months and group (B) received no exercise training or diet regimen.
Results: The mean values of Health-related quality of life (SF-36 HRQL) subscale scores, serum calcium, high density lipoprotein cholesterol (HDL-cholesterol), hand grip strength and Six Minute Walk Test (6MWT) were significantly improved in group (A). While the mean values of serum parathyroid hormone (PTH), plasma lepton, triglycerides, total cholesterol, low density lipoprotein cholesterol (LDL- cholesterol), total cholesterol (TC), triglycerides and BMI were reduced significantly in group (A). In addition, differences between both groups were significant at the end of the study.
Conclusion: The current study provides evidence that weight reduction program improves QOL, biochemical and clinical parameters among obese postmenopausal women.
Keywords : Obesity; Menopause; Quality of Life; Weight Reduction
Abbreviations: QOL: Quality of Life; BMI: Body Mass Index; HRQL: Health Related Quality of Life; HDL-Cholesterol: High Density Lipoprotein Cholesterol; 6MWT: Six Minute Walk Test; PTH: Para Thyroid Hormone; LDL-Cholesterol: Low Density Lipoprotein Cholesterol; TC: Total Cholesterol.
Introduction
Obesity among postmenopausal women is usually associated with poor health-related quality of life (HRQOL) [1]. In USA, about 70% of adults are either obese or overweight [2,3] and globally, 1.5 billion adult are either obese or overweight [4] in addition to about 2.8 million subjects die of obesity related co-morbidities as cardiovascular disorders and diabetes [5]. Moreover, researches proved that all measures of quality of life (QOL) are adversely affected by obesity in addition to depression, low self-esteem poor general health [6,7]. Blood lipid profile and glucose homeostasis are abnormal that induce cardiovascular disorders 2-fold among obese subjects more than normal body weight subjects [8]. However, life style modification can modulate all cardiovascular disorders risk factors associated with obesity [9-13]. Weight reducing programs that combine both exercise training and diet regimen are superior to either exercise or diet regimen [14-17].
Some previous studies proved that weight reduction improves blood lipid profile [18-20] and HRQOL [21-23]. However, others believe that HRQOL could be improved without anthropometric changes [24]. Therefore, the aim of this study was to examine the effects of weight reduction program on biochemical & clinical parameters and quality of life for obese postmenopausal women in kingdom of Saudi Arabia.
Patients and methods
Subjects
Two-hundred postmenopausal obese women enrolled in this study, the mean of their age was 54.67±5.28 year, the mean of their BMI was 33.94±4.27 kg/m2 and menopause since at least 5 years. Exclusion criteria included smoking, endocrine disorders, musculoskeletal disorders, renal disorders, liver disorders, cardiac disorders, respiratory disorders and diabetes. All Subjects were randomly enrolled into two equal groups: group (A) received weight reduction program (aerobic exercise and diet regimen) for 3 months and group (B) received no exercise training or diet regimen.
Measurements
Health-related quality of life (SF-36 HRQL): Quality of life was assessed using SF-36 HRQL that includes eight subscales: Bodily Pain, Vitality, Physical Functioning, Social Functioning, General Health, Emotional Role Functioning, Physical Role Functioning and Mental Health [21].
Hand Grip Strength: Jamar hand dynamometer was used to measure the hand grip strength through applying 3 successive trials using Sammons Preston Roland, Cedarburg, WI, USA, the mean value of the three trials of measurements was recorded and used in the statistical analysis.
Six Minute Walk Test (6MWT): All participants were asked to conduct 6MWT through fast walking around 2 cones that were placed 40 meters a part, each participants were asked to have 2 trials in two different days and the record walking distance of the second days was used in the statistical analysis [25-27].
Biochemical analyses: Overnight fasting venous blood sample was taken to measure serum calcium, high density lipoprotein cholesterol (HDL-cholesterol), plasma lepton, triglycerides, total cholesterol, low density lipoprotein cholesterol (LDL-cholesterol), total cholesterol (TC) and triglycerides through chromatography method using Beranger Mannheim kit. However, measurement of serum parathyroid hormone (PTH) was performed using the principle of Electro chemiluminescence's immunoassay (Modular Analytics E170, Roche, Germany).
Procedures
Participants were randomly included into two equal groups as following:
i. Group (A): Received treadmill aerobic exercise training with a five minutes warming-up phase done on the treadmill (Track master 400E, gas fitness system, England) with low load, actual training time was thirty minutes with an intensity of 7080% of HRmax and finally five minutes of cooling down that was done in the form of running or walking; 3 sessions / week for 3 months [28]. In addition, all participants were instructed to follow diet regimen that provide 1200 kcal/day as recommended by WHO under close supervision of dietitian [18].
ii. Group (B): Was considered as a control group and received no training intervention for six months.
Statistical analysis
SPSS (Chicago, IL, USA) version 17 was used in statistical analysis, where the investigated parameters of both groups obtained before and at the end of the study were compared. However, comparison between the investigated parameters of both groups done using independent "t". All data were expressed as the mean ± SD (P<0.05).
Results
The baseline characteristics of all participants are shown in (Table 1). None of the baseline characteristics differed significantly between the two groups. The mean values of SF- 36 subscale scores, serum calcium, HDL cholesterol and 6MWT were significantly increased in group (A). While the mean values of serum PTH , plasma lepton, triglycerides, total cholesterol, LDL cholesterol, TC, TG and BMI were significantly decreased in group (A) (Tables 2 & 3), while results of group (B) showed no significant changes (Tables 4 & 5). However, the differences between mean values of the investigated parameters in both groups were significant at the end of the study (Tables 6 & 7).
BMI: Body Mass Index; ALT: Almandine aminotransferases; AST: Aspartate aminotransferases; SBP: Systolic Blood Pressure; DBP:Diastolic Blood Pressure.
TC: Total Cholesterol; HDL-c: High Density Lipoprotein Cholesterol; LDL-c: Low Density Lipoprotein Cholesterol; TG: Triglyceride; indicates a significant difference between the two groups; P < 0.05.
(*) indicates a significant difference between the two groups; P < 0.05.
TC: Total cholesterol; HDL-c: High density lipoprotein cholesterol; LDL-c: Low density lipoprotein cholesterol; TG: Triglyceride; (*)indicates a significant difference between the two groups; P < 0.05
TC: Total Cholesterol; HDL-c: High Density Lipoprotein Cholesterol; LDL-c: Low Density Lipoprotein Cholesterol; TG: Triglyceride; (*)indicates a significant difference between the two groups; P < 0.05.
(*) indicates a significant difference between the two groups; P < 0.05.
Discussion
Quality of life along with biochemical parameters were found to be adversely affected by obesity [29-38]. Therefore, this study was designed to detect the effects of weight reduction on biochemical & clinical parameters and QOL among obese postmenopausal women. The principal finding in this study indicated that weight reducing program improved subscales of QOL among obese postmenopausal women. Many previous studies reported that weight loss improves HRQOL among obese subjects [33-38], type 2 diabetes mellitus [39] and osteoarthritis [40]. While, Ross et al. [23] reported that a six months weight reducing program among 298 obese women that resulted in 9.4% weight loss resulted improvement in vitality scores and physical functioning. However, Blissmer et al. [33] proved that improvements in subscales of SF-36 was obtained in 144 overweight/obese adults after six months of weight reducing program that resulted in 5.6 kg of weight loss. Moreover, Riesco and colleagues [41] stated that modest loss of body weight following 16-week of aerobic exercise training improved QOL, physical and mental well-being in obese women.
In our study blood lipids profile and lepton were significantly modulated as a result of weight reduction in obese postmenopausal women. Similarly, Shephard and Balady [42] noticed that regular practice of physical activities had a modulating effect on blood lipids profile by favoring the reduction of cholesterol, LDL-cholesterol and triglycerides in addition to increased HDL-cholesterol level. Also, García et al[43] stated that an ambulatory physical exercise program for 12 weeks improves QOL and biochemical parameters through weight loss in obese postmenopausal women. However, Tran and Weltman [44] found that modulation of lipid profile correlated with weight loss. In addition, Sartorio and colleagues [45] mentioned that reduction of body weight reduced serum level of lepton. Moreover Volek and colleagues [46] reported that 2 months weight reducing program significantly modulated serum level of lepton.
Furthermore, on analyzing the parameters studied in the 6MWT and hand grip strength, our results showed a significant improvement in patients' performance as a result of weight reduction as there is evidence that excess weight may adversely interfere with physical activities [47]. Our findings were consistent with Enright and Sherrill [48] who founded that the distance forecast for the 6MWT was higher in subjects who lost weight. However, a study carried out by Maniscalco et al. [49] showed an improvement of the 6MWT parameters in the late postoperative period of bariatric surgery. Moreover, Lemoine and colleagues [50] proved that postmenopausal obese women had a significant improvement in measures of QOL and walking distance following three weeks of weight reducing program.
Conclusion
The current study provides evidence that weight reduction program improves QOL, biochemical and clinical parameters among obese postmenopausal women.
Acknowledgment
This project was funded by the Deanship of Scientific Research (DSR) at King Abdulaziz University, Jeddah, under grant no. (G-29-142-36). The authors, therefore, acknowledge with thanks DSR for technical and financial support.
0 notes
Text
Juniper Publishers-Open Access Journal of Gerontology & Geriatric Medicine

Physical Activity Does Not Provide Health Benefits in Young Only: Advocating to Engage seniors to Get an Active Lifestyle
Authored by Shehab M Abd El Kader
Editorial
In the last century, western societies have experienced a demographic shift towards an ever-increasing aging population. Over the last half-century the number of adults aged 70 or over has simply tripled; and by 2025-2030, this population wills begrowing 3.5 times as rapidly as the general population [1]. Europe may currently lead the world with the highest proportions of older individuals, but this may not last much longer [2]. By 2050, nearly four-fifths of the world's older popu-lation will be living in the developing and less-developed regions of the world. Whilst the ageing of the general population is one of the humanity's greatest triumphs, it also confronts societies with enormous medical challenges [3]. Indeed, lengthening lifespan is not necessarily synonymous with extending life in good health and studies suggested that with advancing age chronic and degenerative disorders became more and more prevalent and that multimorbidity is increasing [4]. In addition, it is observed a progressive decline in disability-free life which in turn is associated with an increase in the requirement for assisted living in order for older individuals to perform basic activities of daily living [4]. In parallel, some recent publications and studies highlighting the poor participation rate of seniors in sportive recreational activities [5], and very few were older adults who drive an active lifestyle in the line of the recommendations edited by the American College of Sports Medicine [6].
According to World Health Organization (WHO), 60 to 85% of general population worldwide has a sedentary lifestyle, making it one of the more serious, but yet insufficiently, addressed public health problems. This issue does not spare the ageing and aged adult population where sedentary behavior is also highly prevalent [7]. Indeed, nowadays physical inactivity, along with poor diet and nutrition, and persisting tobacco use are well fixed in the modern lifestyle leading to the rapid rise of non-communicable and chronic diseases, which are now the first causes of mortality in every part of world. Sedentary lifestyles double the risk of cardiovascular diseases, diabetes, and obesity, and increase the risks of colon cancer, hypertension, serum lipid profile disorders, osteoporosis, and mood disorders anxiety, and finally global mortality [8-10]. Among the preventive measures recommended by WHO for non-communicable diseases is, in addition, of course, to tobacco cessation and healthy nutrition (including moderate alcohol consumption) to engage people to get at least 30 minutes of moderate physical activity every single day. In addition, governments and policy makers are recommended to generate supportive environments in order to facilitate the population’s engagement in this active lifestyle [7].
There is an abundant literature supporting the benefits of regular physical activity on human's health. Regardless of age, active lifestyle is an important component of healthy and active ageing, both in relation to staying fit and healthy, and also as a way to stay mobile and socially included[11,12]. A recent Cochrane systematic review confirmed that aerobic exercise interventions resulted in increased fitness and an improvement in cognitive function in healthy people aged 55 years or over [13]. However, even later in life, evidence suggests that regular physical activity is not only feasible but also favors physiologic improvements in terms of breaking down and even reversing the age-related decline of cardio-respiratory performances, and mobility and balance [14]. Hence, regular physical activity contributes to extend the period of active and free-disability life [15] and to delay cognitive impairments, and improve the QoL [16,17].
With this aim and perspective, aerobic training appear to be the most effective intervention for improving the overall health status among seniors. Recently, a narrative review of 36randomized, and 17 non-randomized controlled studies confirmed the above described benefits in people aged70 years or over [18]. In the view of the global health benefits of aerobic training, definitely, general practitioners and physicians must encourage senior to engage and/or return to an active lifestyle. This will contribute to keep longer autonomous and independent in their daily life the frailer members of our society.
0 notes
Text
Juniper Publishers-Open Access Journal of Gerontology & Geriatric Medicine

Impact of Weight Reduction on Exercise Tolerance and Psychological Wellbeing for Obese Elderly Women
Authored by Shehab M Abd El Kader
ABSTRACT
Background: Obesity among elderly is an important health-related problem worldwide, to date there is controversy regarding the adverse impact of weight loss among elderly women.
Objective: This study aimed to examine the effects of weight reduction program on exercise tolerance and psychological wellbeing for obese elderly women.
Material and Methods: Sixty obese elderly women enrolled in this study, their age ranged from 60-67 years and their BMI ranged from 31-35 kg/m2. All participants were divided into two equal groups: The training group (A) received weight reduction program in the form of moderate intensity aerobic exercise training on treadmill in addition to diet regimen where, the control group (B) received no intervention. Beck Depression Inventory (BDI), Profile of Mood States(POMS), Rosenberg Self-Esteem Scale (RSES), Six Minute Walk Test (6MWT), grip strength and body mass index (BMI) were measured before and after 3 months at the end of the study.
Results: There was a significant decrease in BMI, BDI & POMS and increase in RSES, 6MWT and grip strength in training group (A) at the end of the study with no significant changes in the control group (B). However, no significant differences were found between both groups at the end of the study.
Conclusion: The current study provides evidence that weight reduction program improves exercise tolerance and psychological wellbeing for obese elderly women.
Keywords: Exercise Tolerance; Elderly; Obesity; Psychological Wellbeing; Weight Reduction
Introduction
Obese elderly women have low physical functioning, energy, and vitality [1]. About two-thirds of the American citizens are overweight and obese [2]. Currently, there is a global concern regarding management of obesity [3]. Overweight and obesity prevalence has increased significantly over the last 30 years, with overweight and obesity now affecting 1.5 billion adults globally [4]. Worldwide, about three million people die every year of obesity-related diseases, including cardiovascular disease, diabetes mellitus and metabolic syndrome [5]. Recently, the prevalence of type 2 diabetes mellitus (T2DM) and cardiovascular disease increased in parallel to prevalence of obesity [6,7]. Obese subjects usually suffer from depression, reduced self-esteem, mobility/functional disability and general health problems [8].
Clinical management of obesity should focus on weight reduction and exercise in an attempt to improve wellbeing [1]. There is evidence that person’s exercise capacity Increasing can improved by physical activity [9]. The cornerstones for treatment of obesity are diet and exercise [10]. Proper diet regimen and physical activities are the appropriate behavioral modification to achieve healthy body weight [11]. Obesity is usually associated with depression as 20-50% of obese subjects suffer from depressions [12,13]. The risk of depression increased parallel to the degree of obesity [14]. There is a bi-directional relationship between depression and obesity [15-17], while, others believe that obesity is usually associated with depression development [18,19]. The aim of this study was examine the effects of weight reducing program on exercise tolerance and psychological wellbeing for obese elderly women.
Materials and Methods
Subjects
Sixty elderly obese women enrolled in this study, their age ranged from 60- 67 years and their BMI ranged from 31-35 kg/ m2. Women who were smokers, having respiratory, endocrinal, renal, musculoskeletal, cardiovascular, hepatic disorders, diabetes and chest diseases were excluded. Participants were enrolled in two equal groups: The training group (A) received weight reducing program (moderate intensity treadmill aerobic exercise training and diet regimen) where, the control group (B) received no exercise intervention or diet regimen.
Measurements
I. Psychological well-being: The Rosenberg SelfEsteem Scale (RSES) was used to measure self-esteem which consisted of 10 items answered on a 4-point Liker scale. The RSES higher scores means greater self-esteem. The Profile of Mood States (POMS) was used to measure mood disturbances, POMS consists of 65 items on a 5-point Liker scale. However, the Beck Depression Inventory (BDI) was used to measure depression, which includes 21 items. The BDI higher scores mean higher depressive symptoms level [20].
II. Hand Grip Strength: Jamar hand dynamometer (Sammons Preston Roland, Cedarburg, WI, USA) was used to measure grip strength of the dominant hand via three successive trials using dynamometer. The degree of elbow flexion was 90° with no close contact with any body part, two trials were done and the mean value was used in analysis.
III. Six Minute Walk Tests (6MWT): Participants were asked to walk quickly as much as they could for six minutes, two trials were done in two separate days and the mean value was used in analysis [21-23].
IV. Evaluation of anthropometric parameters: Digital stadiometer (JENIX DS 102, Dongsang, South Korea) was used to measure the body height. Balance scale (HC4211, Cas Korea, South Korea) was used to measure body weight and body mass index (BMI) was calculated as BMI = Body weight / (Height)2.
Procedures
Following the previous evaluation, all participants were divided randomly into two equal groups.
A. The training group (A) received weight reduction program includes moderate intensity aerobic exercise training and diet regimen as following:
i. The physical training: The treadmill aerobic exercise training session lasted for 40 minutes (5-minute warmup phase performed on the treadmill (Enraf Nonium, Model display panel Standard, NR 1475.801, Holland) at a low load, training session lasted 30 minutes and finished with 5-minute cooling down), training intensity based on guidelines of the American College of Sport Medicine, using the maximal heart rate index (HRmax ) estimated by: 220-age. First 2 weeks = 60-70% of HRmax , 3rd to 12th weeks = 70-80% of HRmax . Three sessions per week for three months max [24].
ii. The prescribed low calorie diet: Balanced diet regimen (55% of energy was from carbohydrates , 15% of protein and 28-30% of fat) that provide about1200 kcal/day for participants of group (A) to reduce weight as recommended by the World Health Organization.
B. The control group (B): received no training intervention or diet regimen.
Statistical analysis
The mean values of the investigated parameters obtained before and after three months in both groups were compared using paired "t" test. Independent "t" test was used for the comparison between the two groups (P<0.05).
Results
BMI: Body Mass Index; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure
BMI: Body Mass Index; RSES: Rosenberg Self-Esteem Scale; BDI: Beck Depression Inventory; POMS: Profile of Mood States (*) indicates a significant difference between the two groups; P < 0.05.
(Table 1) shows the baseline participant's characteristics who shared in this study. There was no significant differences in participant's characteristics between both groups. Statistical analysis proved that there was a significant decrease in BMI, BDI & POMS and increase in RSES, 6MWT and grip strength in the training group (A) at the end of the study (Table 2), however changes in the control group (B) were not significant (Table 3). Moreover, the differences between the investigated parameters mean levels of both groups were significant (Table 4).
BMI: Body Mass Index; RSES: Rosenberg Self-Esteem Scale; BDI: Beck Depression Inventory; POMS: Profile of Mood States (*) indicates a significant difference between the two groups; P < 0.05.
BMI: Body Mass Index; RSES: Rosenberg Self-Esteem Scale; BDI: Beck Depression Inventory; POMS: Profile of Mood States (*) indicates a significant difference between the two groups; P < 0.05.
Discussion
Compromised psychological wellbeing is one of the common criteria of obese subjects [25] that provide a physical functioning constraints [26], perceived limitations in physical ability [27]. The recommended level of weight loss that approved by the American Diabetes Association wasc7% body weight through exercise and diet regimen [28] in order to improve well-being and to prevent co-morbidities and to ensure weight maintenance for long time [29,30]. This study examined the impact of weight loss on psychological wellbeing and exercise tolerance among elderly obese women.
Results of the present study showed weight loss led to decreased BDI & POMS and increased RSES, these results are in line with some previous studies in this field [31-35]. proved that one year weight reducing program conducted by 500 obese persons of both gender associated with better psychiatric measure and wellbeing Grave et al. [31]. However, conducted a review on 22 previous and found that long term healthy behavior conducted for 1-5 years resulted in weight loss and better cardiovascular outcomes among patients with type 2 diabetes Lau and Teoh et al. [32]. While, stated that one year weight reducing program consisted of exercise and diet regiemen resulted in better measures of psychological health, anxiety and quality of life among overweight/obese women Imayama et al. [33]. In addition, mentioned that 16-week weight reducing program for 106 obese women and men had type 2 diabetes resulted in moduated emotional distress and better quality of life Wycherley et al. [34]. Moreover, proved that weight reduction improved depressed mode among obese subjects Faulconbridge et al.[35].
The present study revealed that 6MWT and hand grip strength were significantly improved as a result of weight loss among obese elderly women as there is evidence that excess weight may adversely interfere with physical activities [36]. Our findings were consistent with who founded that the distance forecast for 6MWT was higher in the subjects who lost weight Enright and Sherrill [37]. However, proved an improvement of the 6MWT parameters in the late postoperative period of bariatric surgery Maniscalco et al. [38]. In addition, proved that three weeks weight reduction program resulted in increased walking distance as a result of weight loss Lemoine and colleagues [39]. While, found an association between changes in body weight and improved quality of life and physical fitness among obese women as a result of six months lifestyle intervention Ross et al. [40]. Moreover, in their previous on postmenopausal women for one year weight reducing program improved their aerobic fitness Bowen and colleagues [41]. Finally, Look AHEAD trial found that weight management program improves aerobic fitness in overweight subjects with T2DM [42].
Conclusion
This study provides evidence that weight reduction program improves exercise tolerance and quality of Life for obese elderly women.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/index.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/oajggm/index.php
0 notes
Text
Juniper Publishers-Open Access Journal of Gerontology & Geriatric Medicine

On The Need for More Research on Ageing Sexuality in the History of Medicine
Authored by Alison M. Moore
Opinion
Between 1774-1940, over 100 different European doctors authored works on sexual ageing, defined either as menopause, andropause, or referring to the non-sex-specific term the ‘critical age’. Ideas about these related concepts were elaborated either as complete books, medical theses or as chapters within larger works on hygiene, longevity, menstruation, women’s health or hysteria, including works by major figures such as English physician and Quaker John Fothergill [1], the French physicians [2,3], Alexandre Brierre de Boismont [4], and Sébastien Guyétant [5] the infamous Parisian hysteria neurologist and teacher of Sigmund Freud [6-10]; the renowned French interwar surgeon and the renowned Spanish endocrinologist Gregorio Marañon. Throughout the nineteenth century, French doctoral theses frequently featured the specialist topics of menopause or the ‘critical age’, and over 50 medical theses on these topics remain available to researchers only in fragile hard-copy form in the French national library.
This massive elaboration of ideas about sexual ageing in the nineteenth century has most likely been overlooked in the historiography of sexuality because it occurred less within psychiatry, psychoanalysis and sexology, as was the case for most other major ideas about sexuality, but rather in texts of ‘hygiene’, or in the emergent specialisations of gynaecology and later endocrinology. It should be noted that neither Freud nor Havelock Ellis nor most of the other canonic figures of sexological and psychoanalytic thought contributed significantly to discussions of sexual ageing.
Histories of old age in general have become an important field of historical research, though most mention sexuality either not at all [11-13], or only briefly [15-17]. Other humanistic studies that have considered images of sexual older adults have tended to focus on women only and are most concentrated on early-modern European fictional and theatrical representation [18-20].
The term ‘menopause’ was a French invention and throughout the nineteenth century, medical research on sexual ageing was heavily dominated by French doctors, only disseminating gradually to other parts of Western Europe and to the US over the second half the nineteenth century, and only becoming a major topic of international medical inquiry in the early twentieth century. After this, France remained a major contributor to medical ideas on sexual ageing until the Second Wold War, after which it was eclipsed by the burgeoning of sex-steroid-hormone research in the US and elsewhere.
Specialist scholarship on the nineteenth-century French history of menopause and the ‘critical age’ has been patchy and sporadic [21-26], with a thorough inquiry remainng to be done. Major scholarly studies of the history of menopause have been broad cultural histories not sufficiently focused on medical sources, including Judith Houck’s, Hot and Bothered [27], which is entirely about twentieth century America, and Louise Foxcroft’s Hot Flushes, Cold Science [28] which skims European, British and American sources selectively from the early modern period to the early twenty-first century, with its main focus on twentieth century Britain and the US, considering only women’s menopause. Elizabeth Siegel Watkins, The Estrogen Elixir focuses on the twentieth-century history of American hormone replacement for menopausal women only, without consideration of the extent to which these therapies targeted sexual libido. No major histories of menopause have examined comprehensively the most significant source corpus in the development of medical ideas about it, which were produced in France throughout the nineteenth century, though several studies have referred selectively to texts within this corpus. None of these studies consider menopause in the context of ideas about sexual ageing in both men and women. All major historical studies of women’s menopause assume a definition of it that reflects contemporary notions of its symptomology (hot flushes, disordered sleep, weight gain and mood dysregulation), rather than attending closely to the unique symptomology of past ideas about it which emphasised perverse sexuality, hyper-sexuality, non-conformist social behaviour, as well as oedema and uterine haemorrhages [25].
Overwhelmingly the scholarship on the history of menopause has tended to view the concept in isolation from other ideas about sexual ageing which were in fact even more dominant. This has produced a distortion in the historiography, promoting a view of menopause as indicating a modern rupture, whereby medicine is thought to have suddenly begun representing the sexes asymmetrically from the end of the eighteenth century. This is what the famous Berkeley historian Thomas Laqueur referred to as the shift from a ‘one-sex’ mirror-view of the sexes toward a ‘two-sex’ model of radical difference [29-31]. This author has already written critically about the historiographic tendency to overlook the persistence of homologous views of the sexes in the history of medicine [32-37]. As a result of this tendency, none of the previous studies of menopause in history have considered the substantial body of sources discussing men’s menopause. Many highly respected French medical scholars in the nineteenth, and indeed well into the twentieth century, continually preferred non-sex-specific terms, such as the ‘critical age’, over menopause precisely because they allowed men to be included in the elaboration of the condition. Eventually, even the female-specific term ‘menopause’ was coopted into the description of men’s critical age, with references to ‘male menopause’ or ‘andropause’ appearing in twentiethcentury ideas. Menopause then, up until the Second World War, only partially succeeded in differentiating women’s ageing from men’s.
In the second half of the twentieth century, new medical and sociological understandings of sexual ageing emerged. From this time, a novel set of arguments about sexuality and ageing appeared across both social science and biomedical disciplines which differed markedly from past medical views. Some, such as the urologists J Berman and J Bassuk claimed that female sexual dysfunction was an “age related, progressive and highly prevalent” phenomenon [38]. On the other hand, some sociology scholars since the 1970s have argued that the very assumption of sexual decline in ageing is a form of oppressive traditionalist thought that denies the aged the right to pleasure [39-42]; and the editors of a recent collection of essays about ageing and sexuality refer to “moving beyond the stereotype of older people as asexual [43,44].” Current geriatric nursing researchers working on these questions commonly refer to a “pervasive ageism” that inflects assumptions about ageing and sexuality.
Some of this divergence of contemporary views might be attributable to ongoing shifts in the sexual behaviour and expectations of older adults. A 2013 Swedish study indicated an increase in sexual activity among 70-year-old men and women surveyed in the years 2000-1 relative to those surveyed in 1971-1972 [45-47]; and a US study of 2015 indicated that 60% of women over age 60 in committed romantic relationships report regular sexual activity, while 13% of those not in such relationships also report regular sexual activity [48]. As the authors of several Finnish sociology studies on ageing and sexuality note, “the generations subsequent to the era of sexual revolution of the 1960s and 1970s have considerably modified their sexual values and behaviour patterns,” resulting in a higher prevalence of sexual interest and activity in old age [49]. The evidence of sexual desire declining with ageing then appears to correspond to developments in twentieth-century history after the Second World War, and to have important moral and cultural dimensions.
In our own time, positive claims about elderly sexuality may need to be considered in relation to commercial interests and the politics of globalization. Biological historians such as Nelly Oudshoorn have shown that the pharmaceutical commercialisation of sex steroid hormones (especially the contraceptive pill) has had a profound influence on ideas about female sexuality and sexual difference [50]. The spectacular multinational proliferation of Hormone Replacement Therapies (HRT) at the turn of the twenty-first century, particularly aimed at post-menopausal women, but also increasingly testosterone replacement therapy aimed at ageing men, warrants a similar inquiry. It is worth considering whether pharmaceutical research into both HRT and Viagra may be a driver of recent affirmations of the inevitable physiological decline of libido produced in ageing bodies. Much of the scientific research on ageing and sexual desire since the nineteen-seventies has been supported by pharmaceutical companies looking to develop drug-remedies for both male impotence and for the DSM category of Female Sexual Interest/Arousal Disorder [51], both which are shown in this body of scientific research to be correlated with ageing.
Specific cultural expectations about the normalcy of elderly sexual desire can have a great impact on how individuals experience themselves as sexual subjects in old age. It also clearly impacts how clinicians treat older adults, as the work of several sociologists demonstrates, with many doctors avoiding discussion of sexually-transmitted disease risk with older patients, erroneously believing it to be irrelevant to them. Some studies have suggested that sexually-transmitted diseases may be increasing among older adults [52,53]. It therefore seems beneficial to generate greater cultural awareness of the capacity of older adults to be sexually active, and to de-stigmatise this so that it is not a source of shame or denial.
On the other hand, several researchers have suggested that the increasing celebration of older adults’ sexual needs may itself be a product of commercial interest, benefiting companies marketing products for older people [54,55]. While researchers have typically thought of this in relation to health-targeted products such as supplements and fitness programs, it is clear also that sexuality is one such ‘need’ that may be emphasised to older adults in the effort to generate feelings of lack that may drive them toward the purchase of sexual devices, services or purported pharmaceutical aids. Importantly, the very notion of age-related sexual decline appears to have emerged in twentiethcentury science along with the emergence of hormonal and other pharmacological agents aimed at stimulating libido. In this context, a rigorous historical study revealing how our current concepts of sexual aging came about would be a helpful stimulus for older adults themselves, as well as clinicians, researchers, aged-care workers and the general reading public to toward a stronger sense of older adults’ potential needs but also of the pressures acting upon these.
To know more about Juniper Publishers please click on: https://juniperpublishers.com/index.php
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/oajggm/index.php
#Juniper Publishers#Juniper Publishers Group#Drugs & Aging#Geriatric Urology#Clinical Geropsychology#Geriatric Cardiothoracic Surgery#Geriatric Podiatry
0 notes
Text
Juniper publishers-Pain and Acupuncture
Journal of Gerontology and Geriatric Medicine-Juniper Publishers
Opinion
The word pain derives its origin from the Indo-European root meaning aleg suffer. The word pain is later and is derived from the Latin word «poena» means punishment. Since ancient times there was disagreement about the perception of pain and its assessment. Unlike vision, hearing and smell, pain does not seem to be a primary sense, but rather an emotional experience. Most researchers pain, felt the pain as a complex concept, which is induced by noxious stimuli. Although the pain is the most common symptom in medical and despite huge advances that have occurred in the field of analgesia and anesthesia, the pathophysiological mechanisms involved in the genesis and maintenance of not fully understood. The definition of pain given in 1979 by the Classification Committee of the International Study of Pain (IASP) «as an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage.” In other words, although the Physiology and Anatomy define a precise point of reference for the detection and transmission of messages interpreted as painful, what differentiates the experience of pain, it is the fact that there is always an emotional rating of pain experience.
The scientific term acupuncture is incomplete performance of Chinese therapeutic method Zhen - Jiu, which means drilling and burning. Acupuncture has a complete theory with great therapeutic potential. To measure it, used selected energy points of the skin and underlying tissues.
According to the zones of Head (1893), are changing relationships between internal organs and skin. The Heine (1988) demonstrated the morphological structure of the acupuncture points, as each acupuncture point corresponds to the position of a angeionefrikou bundle. Acupuncture except regional case action appears to present a distant effect. Thus, in Pomeranz (1976) the synthesis of endorphin seems to be influenced favorably by needling. The revival of acupuncture began in the late 1950s, when a group of surgeons in China thought that if acupuncture can improve existing pain, why not used to prevent the inevitable pain that accompanies surgery. For this method used the term analgesia with acupuncture (acupuncture analgesia). The subsequent visit of US President Richard Nixon to China in 1972 catapulted the popularity of acupuncture in the US and worldwide.
The methods for stimulating acupuncture points, besides the classical acupuncture include the application of electric current to the needles, which are inserted into the acupoints (electroacupuncture), or by skin electrodes positioned over the acupuncture points (transcutaneous electrical stimulation), the injecting chemicals into acupuncture points and the pressing massage on selected acupuncture points (acupressure). To 1833 o Guillaume Duchenne de Boulogne, founder of modern electrotherapy starts using electroacupuncture. In 1844 the Hermel uses electro-puncture (electro-puncture) for the treatment of sciatica and lumbosacral neuritis with acupuncture to the affected area. In 1955 Reinhold Voll establishes the low frequency electroacupuncture (1-10 Hz). In late 1971 the Dr. Nguyen Van Ngi and his team used the method of acupuncture analgesia (acupuncture analgesia) in 50 major surgeries with good results.
To read more articles in Journal of Gerontology & Geriatric Medicine
Please Click on: https://juniperpublishers.com/oajggm/index.php
For more Open Access Journals in Juniper Publishers
Click on: https://juniperpublishers.com/journals.php
0 notes
Text
Juniper Publishers - Open Access Journal of Gerontology Juniper publishers-Oral Health Promotion among Institutionalized Patient
Short Communication Minority elderly (3-5%) require long-term care (LTC) [1-3]. LTC patients have chronic diseases, which require medication, cause physical limitations and social disability. All these factors increase the risk of oral diseases and oral manifestations of general diseases [3-5]. Numerous studies documented a very poor oral health among adults residing in LTC facilities [6]. Quite often, the medical staff lacks knowledge and experience in this field. Therefore, an adequate education in oral health among caregivers is critical [7]. LTC institutionalized patients have a high prevalence of caries and high level of oral treatment needs [8]. Unfortunately, there is a significant gap between the oral care need and the limited dental services [9]. Oral hygiene has been found as poor among LTC institutionalized patients [3,8,10]. Few studies have been carried out to compare oral hygiene of independent elderly who take care of their teeth by themselves and those who depend upon oral care assistance and have their teeth cleaned by others. It was found that the oral hygiene quality was better in the selfdependent patients [11]. The possible explanations are that the nursing staff is not qualified to assist the institutionalized elderly with oral care [3]. Several studies show that the quality of oral care education is heterogeneous among caregivers [12-14]. Another explanation of the lack of staff education is a frequent turnover of employees. As shown in the study0f Bilder et al. [8], there was a great change (17%) in the number of general caregivers during the period of research. Part of the caregivers was absent due to season disease and others changed the workplace. Another possible explanation is the neglect of daily oral hygiene of LTC patients. These daily procedures are dependent upon suitable daily oral hygiene procedures and may be highly influenced by the approach taken by the staff [15]. One of the operative option for improving oral health of LTC patients, to change a cleaning procedure. According to the oral health hygiene protocol for LTC patients, the caregivers have to clean the oral cavity of the patients with gauze located on top of a wooden pedal after immersion in the Chlorhexidine 0.12% mouthwash. I consider that this routine procedure is not adequate for removing dental biofilm from the teeth, dentures and soft tissues. Therefore, should advise to care givers to use toothbrush immersion in the Chlorhexidine 0.12% mouthwash for removing the biofilm. The staff should adopt this cleaning (brushing) technique. Due to the change in the technique of cleaning, the dental plaque removal will improve. Further research is needed to improve the adapted cleaning technique for LTC patients.To read more articles in Journal of Gerontology & Geriatric MedicinePlease Click on: https://juniperpublishers.com/oajggm/index.php For more Open Access Journals in Juniper PublishersClick on: https://juniperpublishers.com/journals.php
0 notes
Text
Juniper publishers-Increased Fluoroquinolone-Susceptibility and Preserved Nitrofurantoin-Susceptibility among Escherichia coli Urine Isolates from Women Long-Term Care Residents: A Brief Report Journal of Gerontology and Geriatric Medicine-JuniperPublishers
Abstract
Suspected urinary tract infection is a common indication for antimicrobial therapy in long-term care residents. We sought to characterize antimicrobial susceptibilities among urine isolates collected from women long-term care residents enrolled in a clinical trial across 21 long-term care facilities in Connecticut, United States of America between August 2012 and October 2015. Among 967 urine cultures collected from 175 women long-term care residents with and without suspected urinary tract infection, we identified 456 bacterial isolates. Escherichia coli (55.3%), Klebsiella (13.8%) and Enterococcus (8.3%) species were the predominant organisms identified. Among all 456 urine isolates, 68.1% were ciprofloxacin-susceptible, 77.2% were trimethoprim/sulfamethoxazole-susceptible, 86.3% were cefazolin-susceptible, and 72.6% were nitrofurantoin-susceptible. Among 252 Escherichia coli urine isolates, 60.2% were ciprofloxacin-susceptible, 73.7% were trimethoprim/sulfamethoxazole-susceptible, 84.5% were cefazolin-susceptible, and 86.5% were nitrofurantoin-susceptible. These findings suggest that trimethoprim/sulfamethoxazole may be favorable empiric therapy while the urinary isolate is unknown, and nitrofurantoin may be optimal therapy for uncomplicated urinary tract infection due to Escherichia coli in women long-term care residents.
Keywords: Urinary Tract Infection; Long-Term Care Residents; Escherichia coli; Nitrofurantoin; Antibiotic Susceptibility
Go to
Background
Antimicrobial use among long-term care residents is common. The annual prevalence of antimicrobial use among long-term care residents ranges from 47-79% [1] and antimicrobial stewardship programs are needed in long-term care facilities in the United States [2]. The most common indication for antimicrobials among long-term care residents is urinary tract infection [3]. Data suggest that antimicrobial prescribing practices may impact antimicrobial susceptibility of uropathogens among long-term care residents in the Netherlands [4]. Among long-term care residents in Connecticut, we previously showed that Escherichia coli, Proteus, and Klebsiella species were the most common uropathogens identified in patients with suspected urinary tract infection from 2005-2007, and 40% and 93% of Escherichia coli isolates were fluoroquinolone-susceptible and nitrofurantoin-susceptible, respectively [5]. Our current study characterized antimicrobial susceptibilities among urine isolates from long-term care residents in the same region from 2012-2015.
Go to
Materials And Methods
We evaluated urine cultures collected from women long-term care residents enrolled in a clinical trial evaluating cranberry capsules to reduce bacteriuria plus pyuria across 21 facilities between August 2012 and October 2015 [6]. Participating facilities had at least 90 beds and were within a 50-mile radius of New Haven, CT. Residents were excluded if they were expected to be in the facility for ≤ 1 month, received suppressive antimicrobials, had an indwelling bladder catheter or prior nephrolithiasis, or were undergoing dialysis. Further enrollment criteria have been reported previously [6]. The Yale Human Investigation Committee approved this study. All nursing home administrators signed letters of participation and signed consent was obtained from participants or their surrogates.
Urine cultures were collected during screening encounters of the clinical trial and during adverse events representing suspected urinary tract infection. Screening urine specimens were obtained by clean catch whereas adverse event urine specimens may have also been obtained by catheterization. All specimens were processed at Yale New Haven Health per hospital microbiology laboratory protocols. Antimicrobial susceptibilities were determined per Clinical and Laboratory Standards Institute M100, Performance Standards for Antimicrobial Susceptibility Testing.
For all cultures, we assessed the number of colony-forming units (cfu) of bacteria per milliliter (ml) and type of organism identified. Isolates with <1,000 cfu/ml were not speciated per laboratory protocol. Cultures with growth of up to two organisms were included in analyses. Cultures with no growth, mixed flora (three or more organisms) or unspecified growth were excluded. Antimicrobial susceptibilities were assessed across all remaining cultures. We recorded demographics, comorbidities, number of urinary tract infections, and antimicrobial courses in the prior year for all residents. Analyses were conducted using SAS, version 9.4.
Go to
Results
Overall, we evaluated 967 urine cultures from 175 women long-term care residents collected from 723 screening encounters and 244 adverse event encounters. Among residents, median age was 87 years (range, 65-101 years). Most (90.3%, N=158) were white, 78.9% (N=138) had dementia, 30.9% (N=54) had bladder incontinence, 26.3% (N=46) had diabetes, and 21.7% (N=38) had renal disease. In the prior year, 31.4% (N=55) had ≥1 and urinary tract infection, and 29.7% (N=52) received ≥2 antimicrobial courses.
Among 967 urine cultures, 456 isolates were identified (Table 1). The most common organisms were Escherichia coli (55.3%), Klebsiella species (13.8%), and Enterococcus species (8.3%). Figure 1 shows antimicrobial susceptibilities for all cultures and the subset with Escherichia coli. Among all urine isolates, 68.1% were ciprofloxacin-susceptible, 77.2% were trimethoprim/ sulfamethoxazole-susceptible, 86.3% were cefazolinsusceptible, and 72.6% were nitrofurantoin-susceptible. Among Escherichia coli isolates, 60.2% were ciprofloxacinsusceptible, 73.7% were trimethoprim/sulfamethoxazolesusceptible, 84.5% were cefazolin-susceptible, and 86.5% were nitrofurantoin-susceptible. Antimicrobial susceptibilities were similar regardless of whether urine cultures were obtained for clinical trial screening purposes or for suspected urinary tract infection.
Go to
Discussion
Our study suggests change in the microbiology and antimicrobial susceptibility of urinary isolates among women long-term care residents compared to prior data from the same region [5]. While Escherichia coli remains the dominant organism, the relative proportion of Enterococcus species has increased (8.3% versus 4.5%) whereas Proteus (5.7% versus 14.6%) and Providencia (0.4% versus 3.7%) have decreased. Additionally, Escherichia coli fluoroquinolone-susceptibility increased during our study period which coincided with the Food and Drug Administration restricting fluoroquinolone use for uncomplicated urinary tract infection in 2015 [7]. These results have implications for empiric antimicrobial therapy for suspected urinary tract infection in women long-term care residents and the potential role of public policy in reducing antimicrobial resistance.
Although trimethoprim/sulfamethoxazole and cephalexin are often used as empiric therapy for uncomplicated urinary tract infection, trimethoprim/sulfamethoxazole-susceptibility and cefazolin-susceptibility was 77.2% and 86.3% across all isolates and 73.7% and 84.5% in Escherichia coli isolates, respectively. In contrast, nitrofurantoin had the most consistent susceptibility among Escherichia coli with 86.5% susceptibility. This susceptibility to nitrofurantoin appears stable when compared to prior urine Escherichia coli data from 2002-2005. While 21.7% of participants had renal disease in our study, nitrofurantoin achieves satisfactory cure rates and remains well-tolerated for urinary tract infection in patients with an estimated glomerular filtration rate of 50 ml/min or less [8]. Collectively, these data support recent findings from a multinational randomized clinical trial in women [9] and indicate empiric nitrofurantoin use may be preferred for uncomplicated Escherichia coli urinary tract infection in long-term care residents [10].
The regional increase in Escherichia coli fluoroquinolonesusceptibility from 40% in 2005-2007 to 60.2% in our study may reflect evolving prescribing practices. Although we could not evaluate prescription or antimicrobial stewardship data for this cohort, evidence suggests that hospital antimicrobial stewardship programs can reduce fluoroquinolone-resistance in local unaffiliated long-term care facilities [2]. Thus, restricted fluoroquinolone use may have impacted antimicrobial susceptibility patterns in participating facilities.
The main study strength is that we evaluated all organisms and antimicrobial susceptibilities from urine cultures collected from encounters with and without suspected urinary tract infection in women long-term care residents lacking indwelling catheters. Our results may lack generalizability to men, which constituted 16% of our prior study population, or catheterized patients. Nevertheless, the majority of long-term care residents are women, and the microbiology and management of catheterassociated versus non-catheter-associated urinary tract infection differ.
In conclusion, our work suggests a temporal increase in fluoroquinolone-susceptibility and preservation of nitrofurantoin-susceptibility among Escherichia coli urine isolates in women long-term care residents throughout Connecticut. Given susceptibility rates of all uropathogens to trimethoprim/sulfamethoxazole and cephalexin, they remain effective empiric treatment agents for uncomplicated urinary tract infection when the urinary pathogen is unknown. However, given the predominance of Escherichia coli, its preserved susceptibility to nitrofurantoin, and the safety of short-course nitrofurantoin for patients with a reduced glomerular filtration rate, nitrofurantoin deserves further consideration as empiric therapy in this population. Consistent with recent findings from a randomized clinical trial evaluating nitrofurantoin use for uncomplicated urinary tract infection in community women, future research should evaluate nitrofurantoin as empiric therapy for suspected uncomplicated urinary tract infection among women long-term care residents.
Go to
Acknowledgement
We thank participating long-term care facilities for their support of this study. This work was supported by 2T32AI007517-16 at the Yale School of Medicine, Section of Infectious Diseases and grants P30 AG021342 Claude D. Pepper Older Americans Independence Center, R01 AG041153, and K07 AG030093 all from the National Institute on Aging, National Institutes of Health. The authors declare that there is no conflict of interest.
To read more articles in Journal of Gerontology & Geriatric Medicine
Please Click on: https://juniperpublishers.com/oajggm/index.php
For more Open Access Journals in Juniper Publishers
Click on: https://juniperpublishers.com/journals.php
0 notes
Text
JuniperPublishers-What Ages First: Pulp or Dentin? Journal of Gerontology and Geriatric Medicine-Juniper Publishers
Abstract
Dental pulps stem cells have regeneration potentials. Young pulp cells convert when they mature into cell-producing dentin. In the pulp, the targeted cells are specifically pulpoblasts, fibroblasts, immune and inflammatory cells. In the coronal part of the teeth, capillaries irrigate 100-150 m round or oval domains, allowing the cleaning of continuous zones. In the root, an uninterrupted fish net-like arrangement is located at the periphery of the dental pulp. Thrombus leads to degenerative processes, or to pulp degradation. Pulp necrosis, apoptosis, or nemosis guide pulp impairment. They may influence pulp renewal. Stem cells include Dental Pulp Stem Cells (DPSCs), Exfoliated Deciduous Teeth Stem Cells (SHEDs), Platelet Derived Growth Factors (PDLSCs), Dental Follicle Precursors (DFSCs) and Apical Papilla Stem Cells (SCAPs). An ascending layer of cells issued from the apical papilla mesenchyme contributes to pulp regeneration. Initially, apical cell-rich zones are undifferentiated, and cell sliding involves the transfer from the apical part of the root to the crown, moving from the sub-odontoblastic layer to the radicular dental pulp. Linked by intercellular junctional complexes, pulp cells are interconnected by gap- and tight- junctions. They are transported toward the crown, tightly associated by intercellular junctions. In addition, lateral sliding occurs between the mesial cavities and the central pulp. Later, translocation takes place between the central pulp and the distal horn. This is obvious after an injection with Bio (a Glycogen Synthase Kinase-3 specific inhibitor implicated in regenerative medicine). After a single injection, labeled cells become scarce and in the apical papilla mesenchyme, cells slide laterally from the mesial to the distal pulp horn, where they become undetectable. As pulp cells become older, VEGF promotes blood vessel formation. The activation of the ERK pathway leads to the expression of osteogenesis-related genes, such as Cbfa1, Col I, ALP, and OCN, responsible for dentin formation and mineralization of extracellular matrix components (Tables 1 & 2). TNF-α, Notch, p38 MAPK, TGF-β, Msx1, Msx2, and JNK signaling pathways are implicated in osteogenic differentiation. Dental pulp cells, young and/or old odontoblasts/osteoblasts contribute to bone and dental tissues regeneration. Adipose tissue is another source of mesenchyme stem cells. Young pulp cells become older, producing a dentin layer that contribute efficently to geriatric odontology.
Keywords: Pulp; Dentin; Stem Cells; A Mini-Review.
Abbrevations: DPSCs: Dental Pulp Stem Cells; SHEDs: Exfoliated Deciduous Teeth Stem Cells; PDLSCs: Platelet Derived Growth Factors; DFSCs: Dental Follicle Precursors; SCAPs: Apical Papilla Stem Cells; ASCs: Adipose-Derived Stromal/Stem Cells; OPN: Osteopontin; OCL: Osteocalcin; ECM: Extracellular Matrix Components; ALP: Alkaline Phosphatases
Go to
Introduction
Deep carious lesions lead to irreversible pulp damage. Stem cells located in dental pulps replicate and retain potentials for regeneration [1-12]. They are implicated in the repair of defective cell types, carious lesions and genetic therapies. After the formation of a thin outer mantle dentin, a thick circumpulpal dentin is created, including the primary and secondary dentins orthodentin (tubular dentin) and osteodentin, which are developed long after the pulp formation. Reparative (or tertiary) dentin is formed after a pulp horn exposure (Figure 1).
In the pulp, the targeted cells are specifically pulpoblasts, fibroblasts, immune and inflammatory cells. Different groups of cells are concerned by pulp regeneration. They include odontoblast-like cells, a whole collection of immune cells, central and peripheral nerves, ending at close vicinity of odontoblast cell bodies. Odontoblasts involve the Raschkow’s sub-odontoblastic network. Vascular and lymphatic vessels recolonize and irrigate the wounded pulp tissue [13,14]. Altogether, these cells play a role in pulp physiology, including functionality within the central pulp (Figure 2).
In the coronal part of the teeth, capillaries irrigate 100-150 m broad domains, round or oval areas, allowing the cleaning of continuous adjacent zones [15,16]. Along the periphery of the pulp, capillaries allow peripheral vascularization and this distribution favours pulp regeneration. In the middle of the pulp, arterioles and venules are in continuity and contribute to stimulate pulp regeneration. In the root part, a fish net–like arrangement is continuous at the periphery of the dental pulp. Thrombus leads to degenerative processes, and ultimately to pulp degradation. Pulp necrosis, apoptosis, or nemosis leads either to the totality of pulp degradation, or specifically allows pulp renewal [17,18] (Figure 3).
In contrast, the formation of dentin implicates a series of molecules (Table 2). Mineralizing molecules are including adiponectin, type I collagen, alkaline phosphatase, DMP- 1, 1-dentin sialoprotein, dentin sialoprotein and dentin sialophosphoprotein, MEPE, dentin matrix metalloprotease MMP-3, MMP-9, PGs (decorine, biglycan, osteoadherin, fibromodulin) and osteopontin [19-22]. To conclude with the construction of dental tissues, first a dental pulp is formed, and later a dentin layer is deposited along the initial layer of mantle dentin (orthodentin and osteodentin). At the periphery of the pulp, odontoblasts polarize and differentiate (Figure 4).
The prevalence of caries is rather high (about 85% in the 65-74 year-old patient) and significant in the aging population. In younger patients, the 35-45 year-old group of patients, the carious prevalence is limited to 80.2%. Pulp inflammation is lower in young patients and higher in the older patient group. In this clinical context, a significant impact is related to the aging pulp.
Pulp stem cells constitute a heterogeneous population. In dental tissues, stem cells include 1) dental pulp stem cells (DPSCs), 2) exfoliated deciduous teeth stem cells (SHEDs), 3) platelet derived growth factor (PDLSCs), 4) dental follicle precursors stem cells (DFSCs) and 5) apical papilla stem cells (SCAPs). Adipose-Derived Stromal/Stem Cells (ASCs) play crucial role in the treatment of craniomaxillofacial defects [23]. ASCs are committed toward an osteogenic phenotype. Angiogenesis and osteogenesis support bone regeneration. Plasma membrane-derived vesicles are important mediators in cell-to-cell communication. Growth factors, cytokines, RNAs and microRNA perform biological activities on target cells. They activate regenerative or reparative processes [18]. Bioengineering teeth may be obtained from cultured tooth bud cells [24,25] (Figures 5 & 6).
ASCs derived from pulp donors showed a high expression of osteogenic markers. This is the case for Osteopontin (OPN), Osteocalcin (OCL), and BMP-2. A high mineral content is found in the pulp and dentin of old patients [1,9,21,26] (Figure 7).
Pulp regeneration implies a cascade of cells, sliding from the apex toward the upper part of the crown. In the apical part, undifferentiated cells contribute to colonize the root. The ascending cells move beneath the odontoblast layer, and form a continuous layer that will further colonize the sub-odontoblastic layer. They proliferate, multiply and concentrate in the apical cell-rich zone. In the root, cell sliding starts near the apical part. The ascending layers of cells contribute to pulp regeneration [24,25] (Figure 8).
Initially, pulp cells are undifferentiated, and move from the sub-odontoblastic layer to the collar of the tooth. Presumably, cell sliding involves an ascending transfer from the apical part of the root toward the crown [27,28].
Connected by intercellular junctional complexes, namely desmosome-like junctions, pulp cells are linked by gap- and tightjunctions and they move simultaneously. They are transported along an ascending way, tightly connected by intercellular junctions. They move from the central part of the root to the periphery of the crown where they fan out [29-32] (Figure 9).
In addition, lateral sliding is occurring between mesial cavities prepared after drilling, and the central pulp horn. Afterward, translocation occurs between the central horn and the distal pulp. This is noticeable mostly for rats injected with Bio (a Glycogen Synthase Kinase-3 specific inhibitor implicated in regenerative medicine [32]). After a single injection, labeled cells become scarce in the mesial part of the pulp and they are grouped in the central pulp area. Bio-labeled cells located beneath the odontoblast layer are less numerous in the distal pulp. It comes out that cells slide laterally from the mesial pulp to the distal pulp horn whereas sliding becomes undetectable in the distal part of the pulp.
The conclusions that arise from these experimental approaches are 1) that cells slide in an ascending way from the apex toward the crown, 2) afterward, lateral sliding occurs between the mesial horn and the central/distal pulp. This evolution takes place mostly in the coronal pulp, leading to the terminal differentiation of odontoblasts. In addition, terminal differentiation was strongly linked to the strategic mesenchymal stem cells that are implicated in dentinogenesis, and angiogenesis. Pulp cells are implicated in the implantation of bioactive molecules located in the root, within the dental pulp (Figure 10).
Pulp cells are implicated in geriatric odontology. Angiogenesis shows vascular endothelial growth factor, as well as platelet-derived growth factor, and hepatocyte growth factor. IGF-1, VEGF-D and interleukine-8 improve the recruitment of undifferentiated and/or hematopoietic stem cells associated to different tooth compartments [31]. Combined with biomaterials, such as -tricalcium phosphate, bioactive glass and plateletrich plasma, the dental pulp or bone tissue display potential in pulp regeneration. Pulp renewal is also dependent of adiposederived stromal /stem cells (ASCs).
As cells become older, VEGF promotes new blood vessel formation, and they are also able to recruit hematopoietic stem cells. The activation of the ERK pathway in ASCs leads to the expression of osteogenesis-related genes, such as Cbfa1, Col I, ALP, and OCN, which appears to be responsible for pulp mineralization of Extracellular Matrix Components (ECM) [21,23,26,29,30,31].
As a conclusion, TNF-α may enhance the osteogenic differentiation of ASCs by increasing specific gene expression, such as osteopontin (OPN), runx-related transcription factor 2 (RUNX-2), and Alkaline Phosphatases (ALP) (Tables 1 & 2) [11]. Molecular investigations clearly confirmed that ERK, TNF-α, Notch, p38 MAPK, TGF-β, Msx1, Msx2, and JNK signaling pathways are strongly implicated in the odontogenic/osteogenic differentiation of ASCs [31-36].
Conclusion
Altogether, young and old dental pulp cells, young and old odontoblasts and osteoblasts contribute to bone and dental tissues differentiation/regeneration. Adipose tissue is an active source of mesenchyme stem cells. Noticeably, aging tissues contribute efficiently to geriatric odontology.
To read more articles in Journal of Gerontology & Geriatric Medicine
Please Click on: https://juniperpublishers.com/oajggm/index.php
For more Open Access Journals in Juniper Publishers
Click on: https://juniperpublishers.com/journals.php
0 notes
Text
Juniper Publishers-Metabolically Healthy Obese (MHO) in Adults and Adolescents: Where We Are

Abstract
A unique subset of obese individuals who appear to be protected from the development of metabolic disturbances has been identified in clinical practice and is termed metabolically healthy but obese (MHO). The true prevalence of the MHO phenotype varies widely from approximately 6% to75% of obese adults and from 6–36% in obese adolescents. Currently, there are no clear accepted criteria on the definition of MHO. The strong effect of pubertal status on metabolic health cannot be excluded in obese adolescents. To clarify this definition we need the collaboration of the scientific community. Numerous possible mechanisms underlying MHO have been suggested, including adipose tissue distribution and inflammation. The current evidence cannot confirm that MHO subjects are permanently protected from the risk of obesity-associated metabolic complications. This transition might be minimized by appropriate lifestyle habits. No standard practice guidelines for the prevention and treatment of MHO can be proposed to clinicians. A decent attitude would be to regularly monitor CVD risk factors in obese adult and adolescent MHO patients especially elevated triglycerides, glycaemia, HOMA and C-reactive protein as well as low HDL-C. A special surveillance should be applied to prevent any increase in waist circumference (WC) as the MHO phenotype may be maintained by promoting lower WC and by the prevention of any further weight gain. Identifying obese patients with this protective profile could help the medical community determine which part of the obese patients need to be only periodically observed and which need to have early therapeutic interventions.
Keywords: Metabolically healthy obese (MHO); Metabolically unhealthy obese (MUHO); Type 2 diabetes mellitus; Cardiovascular disease; Dyslipidemia; Impaired glucose tolerance; Metabolic syndrome; CVD risk factors; Insulin resistance; Treatment; Clinical practice.
Abbrevations: T2DM: Type 2 Diabetes Mellitus; CVD: Cardiovascular Disease; MHO: Metabolically Healthy Obese; MUHO: Metabolically Unhealthy Obese; OR: Odds Ratio; BMI: Body Mass Index; MVPA: Moderate-Vigorous Physical Activity; HDL-C: High Density Lipoprotein Cholesterol Levels
Go to
Introduction
Obesity is associated with a reduced life expectancy, mostly because obese individuals are at an increased risk of Type 2 Diabetes Mellitus (T2DM), Cardiovascular Disease (CVD), and several types of cancer. However, there is a subset of healthy obese individuals, i.e., a subset known as Metabolically Healthy Obese (MHO) that are not at a higher risk of mortality and morbidity than their Metabolically Unhealthy Obese counterparts (MUHO) [1-3]. MHO accounts for a substantial proportion of the obese adult population and this proportion may vary depending on the criteria used to define MHO. Currently, there are no universally accepted criteria to define MHO but the definition needs that the patient be obese and lack the obesity-associated metabolic complications mentioned above. MHO individuals display less visceral adipose tissue, smaller adipocytes, and a reduced inflammatory profile relative to MUHO. In adults, few years ago, Plourde G and Karelis A have been able to provide an interesting definition of MHO [1]. This definition is now used internationally under the term of (PK definition; Plourde and Karelis definition) and is used to determine the prevalence of MHO vs the prevalence of MUHO in adult German populations [4]. As in adults, identifying obese adolescent patients with this potential protective profile could help the medical community determines which part of the obese adolescent and adult populations need to be only periodically observed and which need to have early therapeutic interventions [2]. In adolescent, it is even more complicated considering that previous studies have demonstrated that being obese in this age group increase the risk of having obesity and the obesity-associated complications at later age [5]. As just stated, the main difficulty in estimating the actual prevalence of MHO is the lack of consensus pertaining to its definition. For example, it was demonstrated that nearly half (55.2%) of obese subjects were MHO using the National Cholesterol Edu¬cation Program Adult Treatment Panel III (NCEP ATP III) criteria to define metabolic syndrome [6]. Recently, Rey-Lopez et al. performed a systemic re¬view on the prevalence of MHO based on the frequency of different variables used among studies and they reported that the MHO prevalence ranged from 6% to 75% [7]. They also mentioned that this prevalence may also vary according to sev¬eral socio-demographic factors such as gender, age, and race/ethnicity [7]. By stratifying the analysis ac¬cording to gender and age, these authors were able to reveal that the MHO prevalence was higher in women and younger- aged in¬dividuals [7]. Considering the marked heterogeneity of MHO definitions and the varied prevalence described in the literature, it is clear that a common MHO definition still need to be established.
A second major concern in the identification of the real prevalence of MHO is the fact that a subject’s health status can switch from MHO to MUHO and vice versa with time [1]. For example, Soriguer et al. showed that 30% to 40% of individuals with MHO converted to a MUHO status after 6 years of followup [8]. Because there is an accumulation of evidence suggesting that MHO is not a static condition, attention should be focused on the variables that predict metabolic deteri¬oration to MUHO in individuals with MHO [1]. According to a study conducted in Spain by Schroder H et al. the factors that predict the transition from MHO to MUHO were an increase in BMI and abdominal obesity measured by the waist circumference (WC), or by the waist-to-hip ratio [9]. On the other hand, the incorporation of a healthy lifestyle, in¬cluding a healthy diet, moderate to high level of physical activity, no smoking, or smoking cessation, helped prevent the tran¬sition from MHO to MUHO [9]. Hwang YC et al. demonstrated that nearly two-thirds of Japanese Americans with MHO de¬veloped MUHO over 10 years, and a higher conversion to MUHO was associated with greater visceral abdominal fat, female gender, higher fasting insulin levels, and lower baseline of High Density Lipoprotein Cholesterol Levels (HDL-C) [10]. Taken together, the main characteristics suggested to preserve metabolic health in individuals with MHO include a healthier lifestyle, greater incretin response to meals, less abdominal fat distribution, less visceral and ectopic fat accumulation, lower levels of inflammation, and greater insulin sen¬sitivity [1-3, 7-10]. Therefore, an adequate surveillance of these factors in MHO individuals may prevent the progression to an MUHO phenotype. Another research from Primeau V et al. also suggests that although MHO individuals display a favorable metabolic profile; this does not necessarily translate into a decrease in mortality [11]. However, a recent meta-analysis by Zheng R et al. found that MHO individuals were not at an increased risk of all-cause mortality but were at an increased risk of CVD events [12]. While other studies found that relative to the MUHO subjects, MHO individuals were at a lower risk of T2DM but not of CVD [13]. On the other hand, MHO patients are certainly at a higher risk of CVD compared to metabolically healthy non-obese individuals (MHNO) [1, 13-15]. According to Badoud F et al. the relatively low risk of CVD disease among people with MHO relative to MUHO has been attributed to differences in white adipose tissue function between the two groups [16].
The prevention and treatment of obesity is a relevant medical, socioeconomic and public health issues and the interventions are not always successful [1-3]. Notably, different independent studies have shown that individuals with MHO may not be able to significantly reduce their obesity-related CVD and metabolic risk using anti-obesity treatment strategies [1]. However, the same public health message remains for obese patients to maintain an appropriate lifestyle that contains an adequate diet and regular physical activity [1-3]. The review made by Plourde G and Prudhomme D might be very useful for the physicians to guide their MHO patients achieve and maintain their weightloss [17]. The current mini review aimed to present current issues regarding MHO including the suggested mechanisms that might explain MHO and its definition in adult and adolescent populations [1-2].
Which Mechanisms Might Explain MHO?
Although the exact mechanism responsible for the MHO phenotype is still unclear, some possible mecha¬nisms have been suggested in both human and animal studies [18-19]. They include the maintenance of insulin sensitivity, the presence of specific fat distribution with low visceral and ectopic fat accumulation including low liver and skeletal mus¬cle fat storage compared with subcutaneous fat depots [18-19]. The mechanisms also include a normal adipose tissue function defined by a lower im¬mune cell infiltration into adipose tissue, a normal adi¬pokine secretion patterns, and finally a high level of physical activi¬ty, and fitness [18-19]. According to Bluher M, obesity is a multifactorial disorder that is influenced by the interplay between genetic, behavioral, lifestyle, and environmental factors, including fetal program¬ming, the control of appetite and energy expenditure, and the availability of nutritional food [20]. These factors and their interactions lead to an expan¬sion in fat mass due to an increase in the mean of fat cell volume (cell hypertrophy) and in the number of adipocytes (cell hyperplasia) mentioned Spalding KL et al. [21]. In most obese individuals, the adipocyte storage capacity may be exceeded and lipids may accumulate ectopically in visceral fat depots, liver, muscle, and β-cells, where¬as in MHO subcutaneous adipose tissue has the intrinsic ability to expand, leading to preserved insulin sensitivity [21]. However, the genetic and environmental factors involved in the fat expandability are still unknown.
During a positive energy balance, due to an excessive energy intake and/or a sedentary lifestyle or low energy expenditure, subcutaneous adipose tissue expands and accumulates lipids in the form of triglycerides [3,21]. If this positive energy balance is prolonged, a point is eventually reached where subcutaneous adipose tissue cannot further expand and energy surplus no longer can be safely stored mentioned Spalding KL et al. [21]. Once the limit on storage capacity has been exceeded, the dietary lipids start spilling and accumulate ectopically in other organs such as the omentum, the liver, the pancreas and the muscles, forming lipid byproducts that are toxic to the cells. Unfortunately, there is currently no clinically useful screening method to predict which obese individuals will develop metabolic derangements, especially T2DM and CVD [3,21]. Esser N et al. have proposed that inflammation in adipose tissue is an¬other key factor that explains the metabolic alterations associated with obesity [22]. However, studies comparing the inflammatory status among individuals with MHO have yielded conflicting results [23-26]. For exam¬ple, Phillips and Perry demonstrated that individuals with MHO presented with a more favorable inflamma¬tory status than their MUHO counter¬parts [23]. According to most definitions, MHO presents with lower concentrations of complement component 3, C-reactive protein, tumor necrosis factor α, interleukin 6, and plasminogen activator inhibitor-1; higher adiponectin levels; and reduced white blood cell count compared to their MUHO counterparts [23-26].
Logistic regression analysis identified greater likelihood of MHO among individuals with lower levels of complement component 3 (odds ratios [ORs], 2–3.5), IL-6 (ORs, 1.7–2.9), plasminogen activator inhibitor-1 (ORs, 1.7–2.9), and white blood cells (ORs, 2.1–2.5) and higher adiponectin concentrations (ORs, 2.6–4.0). The authors of this study concluded that the favorable inflammatory status is positively associated with metabolic health in obese and non-obese individuals [23]. In contrast, a study by Gomez-Ambrosi J et al. on a West¬ern population that used the same MHO definition showed that circulating concentrations of pro-inflam¬matory factors, including CRP, were increased in both the MHO and MUHO groups [25]. Although these conflicting findings may be explained by various differences between studies including in the ethnicities, age groups, low numbers of subjects, limited inflam¬matory profiling, and/or the use of different metabolic health criteria to define MHO; a better understanding of the association between MHO and inflammation is therefore necessary to increase our comprehension of this relation [26].
Identifying MHO Individuals in Adults
Defining the MHO phenotype is an important aspect for studying the mechanisms by which fat accumulation in obese subjects causes or contributes to the obesity-associated metabolic complications and/or CVD risk factors [1,3]. As discussed above and in our previous review [1], another complication has been found in defining MHO; the cutoff values for each pa¬rameter, including insulin resistance and inflammato¬ry markers, have not been clearly established [1,3]. Adults defined as MHO are generally characterized for the absence of the metabolic abnormalities such as those mentioned earlier, they also present with lower visceral, hepatic, muscle fat accumulation and gene expression-encoding markers of adipose cell differentiation [1,3]. However, it is important to note that MHO individuals may also have multiple intermediate metabolic risk factors that may signal an increased risk for T2DM and CVD later in life [1]. Plourde G and Karelis A first believed that the definition of adult’s MHO include a WC of ≥80 cm for women and ≥94 cm for men that should be used to identify adults MHO subjects instead of a BMI of ≥30 kg/m2. These authors then suggested the following metabolic markers with their cut-points: glycemia ≥ 5.6 mmol/l, HDL-C ≥1.3 mmol/l for women and ≥ 1.03 mmol/l for men, triglycerides <1.7mmol/l, and blood pressure <120/80 mm Hg [1]. The proposed choice of these clinical markers was based from the criteria for the identification of metabolic syndrome in adults from the International Diabetes Federation (IDF) [27]. Plourde G and Karelis A proposed that adults MHO individuals may be defined (PK definition) when all four of the metabolic markers are met [1]. PK seeks to apply a strict method because their goal was to identify a “true” MHO population which could be different from a non-metabolic syndrome population [1]. According to Truthmaan J et al. the PK criteria, which define MHO by the fulfilment of all proposed criteria, may be the more appropriate definition to determine true MHO [4].
Potential definition of MHO in Adolescents
As in adults, knowing MHO in adolescent patients may help attributing more importance to the treatment of MUHO and prevention to MHO. There is no reason to believe that the mechanisms responsible for developing MHO and MUHO in the adolescent populations would be much different from those discussed above for adults and will not be repeated here. However, there are important concepts specific to the adolescent population that is relevant to discuss. The study by Prince RL et al. was designed to determine the proportions of adolescent with obesity classified as MHO as well as to examine the anthropometric, and the lifestyle predictors that could be associated with MHO [28]. It was, first, observed that about 20% to 33% of adolescent with obesity were at relatively low risk for CVD despite possessing a high level of body fat. Second, that several different adiposity-, diet-, and physical activityrelated variables independently predicted MHO status. Finally, the predictors of MHO status varied depending on which classification system we used to determine individuals being MHO or MUHO.
In adolescents such as in adults, the documented prevalence of MHO also varied considerably with proportions ranging from 6–36% in various countries depending on the definition used to determine MHO in adolescents [29-32] and/or the strong effect of pubertal status on metabolic health in obese adolescent [33]. The diversity of the risk factors and their thresholds applied to determine CVD risk may contribute to the inter-study variability in the prevalence of MHO in adolescent patients as observed in adults. For the adolescent, it is recommended that we use the existing criteria for adults [1]. However, at this point, we still do not know the number of these metabolic biomarkers is necessary to correctly define MHO and to clarify this situation we need the collaboration of the scientific community [34]. Old data have demonstrated that being obese at a young age and for a longer period of time is associated with a high risk of T2DM and CVD risk factors later in life which complicated further the definition of MHO in adolescent population [5]. However, this reinforces the importance of weight management, or at a minimum, the prevention of further weight gain in adolescent. Currently, the best predictors of MHO is WC (Odds Ratio [OR], 0.82; 95% confidence interval [CI], 0.77–0.88; P < 0.001) and Body Mass Index (BMI) standard deviation score (OR, 0.24; 95% CI, 0.15–0.39; P < 0.001), respectively [28].
Weigensberg MJ et al. found that pediatric patients who consumed a high level of dietary fat had higher levels of IR and acute insulin response to glucose compared with their peers who consumed less fat, but this was exclusive to African Americans (not Caucasians) [34]. This observation do not allow us to speculate on the amount of dietary fat that is responsible for the increased in IR; however, at least in this study, the impact of dietary fat on MHO was modest in comparison with the role of central body fatness [34]. Moderate-Vigorous Physical Activity (MVPA) emerged as an important predictor of MHO [34]. Data demonstrate that doing MVPA may have a clinically meaningful impact on the CVD risks status of adolescent with obesity [34]. This finding is particularly important given how difficult it is for adolescents as well as in adults with obesity to lose and maintain their weight loss over time [17]. From a practical point of view, those individuals classified as having higher CVD risks could be prioritized for care sooner or identified to receive more aggressive therapies than their lower-risk peers [1]. For instance, MHO adolescent may benefit from interventions that help them to maintain their current weight, whereas MUHO may benefit from more intensive health care’s to promote weight loss [1].The ethnic homogeneity of the population indicates that there is a need to examine whether MHO varied across ethnicities. The data related to sexual maturation needs also to be collected since sexual maturation influenced body weight and fat distribution differently in female versus male during the adolescence [5]. Since determining the sexual maturation in regular clinical practice is highly complicated Reinehr T et al. [33]. Some authors have found that puberty and age are highly correlated with one another, and age can therefore represent a reasonable approximation of maturity [35-36].
Go to
Conclusion
Accumulating evidence suggests that, although the risk of all-cause mortality and CVD events might be higher in people with MHO compared with metabolically healthy people of a normal weight, the risk is substantially lower than in individuals with MUHO [1]. As seen, the prevalence of MHO varies according to the population and definition used in both adults and adolescent patients. There is current¬ly no consensus criterion for the definition of MHO in both adults and adolescent populations, which render difficult the development of clinical practice guidelines for both surveillance and treatment of MHO [1]. Numerous possible mechanisms underlying MHO have been suggested, including adipose tissue distribution and inflammation [1,3]. However, the prognostic value of MHO still needs to be debated. Also, adult and adolescent MHO individuals may be considered as metabolically healthy they can also present other obesity-related comorbidities such as sleep apnea, knee osteoarthritis, poorer body image and many others comorbidities [1,3]. Therefore, studies on comorbidities associated with obesity other than metabolic or CVD risk factors are necessary to assess more accurately whether MHO individuals are really “healthy.” On the basis of the above evidence or until future studies can state otherwise, a prudent attitude would be to regularly monitor CVD risk factors in obese adult and adolescent MHO patients (especially elevated triglycerides, glycaemia, HOMA and C-reactive protein as well as low HDL-C), in order to detect as early as possible a negative evolution of their cardio-metabolic profile as well as their other obesity-related comorbidities [1]. In particular, a special surveillance should be applied to prevent any increase in WC as it was previously concluded that the MHO phenotype may be maintained by promoting lower WC. Therefore, every patient with obesity should be motivated to loss weight especially considering that moderate weight loss (5% to 10%) is often sufficient to lower the risk of adverse outcomes [17]. However, how much weight needs to be lost to transform MUHO to MHO status is still unknown. Obviously, this transition might be supported by appropriate lifestyle habits including an adequate diet, and regular physical activity that affect CVD risk, independent of a loss in body fat [17].
To read more articles in Journal of Gerontology & Geriatric Medicine
Please Click on: https://juniperpublishers.com/oajggm/index.php
For more Open Access Journals in Juniper Publishers
Click on: https://juniperpublishers.com/journals.php
0 notes
Text
Juniper Publishers-Massive Thrombophlebitis as a Complication after Carpal Tunnel Release: Comorbid Factors?

Abstract
Geriatric care is very critical care owing to the fact that elderly people need care and comfort to lead a healthy life without worries and anxiety. Elderly care is a bit peculiar as compared to other specializations in medicine. Non-clinical interventions assumes rather more importance inter alia and services. The world population is rising so the proportion of elderly habitants. Such rising proportions call for more attention on geriatric care. The aim of this research is to study and find the evidence that the role of health care administration is rather more important for geriatrics. The study retrieved few articles and a thorough examination of articles reveals that there is lot of research in the field that emphasises several clinical interventions without explicitly mentioning the importance of administration services in geriatric clinics and hospitals. However, all those recommendations found in this literature indirectly call for more effective and efficient intervention of health care administration.
Keywords: Geriatrics; Elderly Care; Health Care Administration; Literature Review
Introduction
The world is aging quickly and the proportion of population having elderly people is increasing steadily. Almost 500 million people worldwide were above 65 in 2006. It is estimated to rise to a whooping amount of 1 billion by 2030. This means 1 in every 8 inhabitants will be aged individual on the globe. Most of this elderliness is witnessing in developing countries [1]. The rising levels of elderliness in population also brings rising illness and diseases. Older patients require more care and that trigger more cost and other economic burdens directly to hospitals and indirectly to the economy. The care, so, becomes precious for patients which in turn throw more challenges to healthcare administrators to make it further affordable.
Methods
The very objective of this article is to explore and find some of the potential problems in the area of geriatrics with a special emphasis on health care administration. As it was mentioned in the introduction, the rising population engender increase in diseases and other health issues in elderly people. This tends to pose more challenges to health care administrators due to the very fact that managing geriatric care is not as it is with other specializations.
This study is basically a review work. Few articles of scholarly nature were retrieved using Google Scholar. The online search was performed using certain tags like healthcare administration, medical problems, geriatrics. About 16,30,000 results were displayed in 0.68 seconds. All the links displayed observed to have three of the tags that were used for data retrieval. However, only first few yet suitable 5 articles were used to make the review. The articles were selected using simple random sampling method. The following section shows the observations of the study.
Review
Ory MG [2] did certain study titled “emerging issues in geriatric care: aging and public health perspectives”. The aim of the research is to find and detect major social and healthcare challenges of aging population in US. The study finds that though the overall disability is decreasing yet the burden of the same together with other health conditions of the public in US tend to rise in near future. The study offers certain solution that evidence-based interventions might be able to address health problems of aging population. The study also suggests that the databases are useful to retrieve certain data and address the health problems of aging population. This study did not mention anything explicitly about health care administration however, some of the facts that were mentioned in the study are found to have connections with health care administration. For instance, data retrieval and their potential use for healthcare improvement involve the role of administrators. In the same fashion, health care interventions, that were suggested in this study also, one way or the other demands active yet efficient administration practices in hospitals.
Amy KTD et al. [3] did certain study on patient safety in geriatrics. The article mentions that the patient safety has become major health concern. The study criticises certain other publication named “To err is human” which is published by Institute of Medicine in 1999. The study also did certain critique on safety systems in healthcare concerns. The study makes six recommendations after going through certain safety methods. They are: detection and reporting of geriatric syndromes, identifying system failures when geriatric syndromes occur, establishing dedicated geriatric units, improving the continuity of care, reducing adverse drug events, and improving geriatric training programs. This study perhaps brings rather more importance on healthcare administration. Implementation of safety measures as they were suggested in the study demands active role of healthcare administrators. Some of the safety measures i.e. establishing dedicated geriatric units, continuity of care, training programs in geriatrics gives the idea that health care administration is very critical for geriatric care.
Merrell RC [4] did a study on Geriatric Telemedicine with an aim to excavate evidence for telemedicine as a way to address problems through review of literature. The research mentions that the telemedicine offers many means to address the problems of geriatric care in creative ways. The use of electronic medicine, telecommunications, and information management has now found its way into the very fabric of health care. The use of telemedicine is a fait accompli in much of the world, and it continues to have an increasing role deeply imbedded in our electronic practices coupled with social media. Though this paper has not mentioned anything health care administration explicitly but some of the issues like electronic medicine, telecommunications, information management do require lot of administration services apart from clinical services.
Hanlon JT [5] did study on drug-related problems in older adults. The aim of the study was a systematic review employing methods related to online database searches. The authors retrieved 2012 scholarly articles. The study was done using certain online tags like combination of the terms elderly, aged, drug-related problems, medication related problems, medication errors, suboptimal prescribing, inappropriate prescribing, underutilization, polypharmacy, medication monitoring, medication dispensing, medication administration, medication adherence, adverse drug events, and adverse drug withdrawal events. Only 40 of articles found to be apt for the study. Out of 40 only 24 articles found to be related to medication errors, followed by 18 related to ADEs, majority of them addressing adverse drug reactions. Only 3 of the retrieved articles found apt for the study and recommendations were done based on these articles. Perhaps, this is the only paper among all which mentions about the word administration so explicitly in the research findings.
Sidik SM et al. [6] did a study on physical and mental health problems of the elderly in rural Selangor. The study was done using five of nine village’s selected using random sampling in the sampling area. Elderly people in those selected areas were interviewed using a pre-tested structured questionnaire which included -30, ECAQ and Barthel Indices. The study shows that out of 263 study individuals, which 6.2 % of population, 60.1 % of the surveyed people agreed to have physical problems. 15.1 % found to have functional dependence. It was also found that each of 7.6% and 22.4% of people are suffering from mental health problems such as depression and cognitive impairment respectively. More interestingly depression is significantly associated with unemployment, whereas, cognitive impairment is significantly associated with several of socioeconomic characteristics. Though there isn’t any mentioning of health care administration but few of main variables such as unemployment, cognitive impairment, socioeconomic characteristics and their influence on care were directly falls in the ambit of health care administration.
Conclusion
The main of this paper is to find certain evidence in support of the role and its importance of health care administration especially in geriatric care. As far as methodology is concerned the data retrieved from certain sources using Google Scholar. Only very few articles were studied in search of evidence in support of the assumption that the role of health care administration is very critical for geriatric care. Only one research paper out of five selected has mentioned about the importance of health care administration in geriatric care. Rest of the papers had not mentioned anything about administration services. Suggestions or findings that were done through these papers indirectly emphasises importance of health care administration. So this review work suggests that all care done through geriatrics needs effective and efficient health care administration services. However, more research effort with rigorous and meticulous methods need to be done to affirm such statements of care.
To read more articles in Journal of Gerontology & Geriatric Medicine
Please Click on: https://juniperpublishers.com/oajggm/index.php
For more Open Access Journals in Juniper Publishers
Click on: https://juniperpublishers.com/journals.php
0 notes
Text
Mini Review on Synthesis of Pyrimidinthione, Pyrimidinedione Derivatives and Their Biological Activity | Juniper Publishers
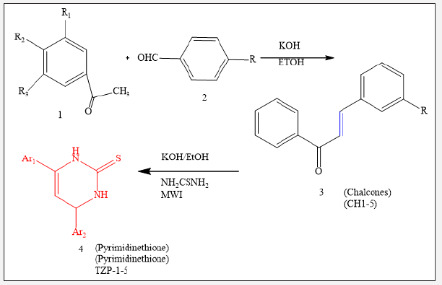
Juniper Publishers-Open Access Journal of Petrochemical Science
Authored by Nadia Ali Ahmed Elkanzi
Abstract
The chemistry of heterocycles has received amongst the chemicals prominent attention in recent years owing to its importance in the pharmaceutical sector. Organic compounds carrying pyrimidinthione, pyrimidinedione, pyridazine rings have been reported to demonstrate a wide range of pharmacological activities, which includes antibacterial, antimicrobial, antioxidant, anti-HIV and anticancer activity. These observations have been guiding for the synthesis of various derivatives of these compounds enclosing biologically active nuclei and study their pharmacological activities.
Keywords: Chalcone; Pyrimidinthione; Pyrimidinedione; Biological activities
Introduction
Over the past decade the evolution of organisms resistant to nearly all the class of antimicrobial agents has become a severe public health concern [1,2]. Heterocyclic compounds have received considerable attention owing to their synthetic and biological importance in the enhancement of the quality of human life. Among numerous heterocycles compounds that have been synthesized and evaluated for their pharmacological activities, chalcone, pyrimidinone and pyrimidinethione have played a crucial role in medicinal chemistry. It was demonstrated that the presence of reactive α, β-unsaturated keto function in chalcones was responsible for their antibacterial and antifungal activities [3].
The pyrimidinones compounds have gained interest in recent years due to their wide-ranging biological activity. These compounds displayed therapeutic applications, as anticancer [4,5], antihypertensive [6], hypoglycaemic [7], antiviral [8], anticonvulsive [9], anti-inflammatory and analgesic [10] drugs.
On the other hand, literature surveys revealed that pyrimidinethione derivatives are an important class of heterocyclic molecules possessing a wide variety of biological properties. In fact, different studies demonstrated that various compounds possessing pyrimidinethione nucleus exhibited broad range of biological activities such as antimicrobial [11-13], antioxidant and antitumor activities [14], antitubercular [15] and hypoglycemic activity [16]. The current mini review aims to focus on some synthetic procedures of pyrimidinones and pyrimidinethione derivatives to facilitate the development of new heterocyclic compounds with more efficient and promising pharmacological activities.
Result and Discussion
Pyrimidinedione derivatives were synthesized from various arylmethylene acetophenone derivatives [17]. The chalcone derivatives were prepared using substituted ketone and distinct substituted benzaldehyde through condensation reaction. Likewise, pyrimidinedione derivatives (4) were synthesized via reaction between aryl methylene derivatives and/ or chalcones with thiourea and KOH in ethanol (50ml) in microwave oven for sufficient time and under an appropriate temperature. The detailed steps used in the synthesis of the pyrimidinedione derivatives were described in the literature [18].
The pyrimidine-2-thione derivatives (4) were screened in-vitro against gram positive and gram-negative strains and were found to be less active against the gram-positive bacteria in comparison with the minimal required dose for the action against the gram-negative bacteria in most cases [17] (Figure 1) (Table 1).
Ethyl 1,5-dihydro-5-oxo-1,7-diphenyl-1,2,4-triazolo [4,3-a] pyrimidine-3-carboxylate (5) was treated with hydrazine hydrate, in refluxing ethanol to give the corresponding acid hydrazide (6) in good yield [19,20]. Acid hydrazide (6) was treated with potassium thiocyanate in refluxing methanol, in the presence of hydrochloric acid to produce1-(1,5-dihydro-5-oxo-1,7-diphenyl- 1,2,4-triazolo[4,3-a] pyrimidine-3-carbonyl) thiosemicarbazide (7). Compound (10) 3-(5-mercapto-4H-1,2,4-triazol-3-yl)-1,7- diphenyl-1,2,4-triazolo [4,3-a] pyrimidin-5-(1H)-one (10) was prepared by oxidative cyclization of compound (7) in basic medium (7% KOH) under reflux with subsequent acidification. It was found that further reflux of compound (7) with dry pyridine gave a product identified as 3- (5-amino-1,3,4-oxadiazol-2-yl)-1,7-diphenyl- 1,2,4-triazolo [4,3-a]pyrimidin-5-(1H)-one (8) (Figure 2).
On the other hand, the reaction involving the synthesis of 1,7-diphenyl-3-(5-amino-1,3,4-thiadiazol-2-yl)-1,2,4-triazolo [4,3-a] pyrimidin-5-(1H)-one (9) took place through a dehydrative cyclization by reacting compound (3) with conc. sulfuric acid. The resulting product (9) was separated as green solid, and was slightly soluble in most organic solvents (Figure 2). Acid hydrazide (6) reacted with phenyl isothiocyanate in refluxing ethanol to produce 1-(1,5-dihydro-5-oxo-1,7-diphenyl-1,2,4-triazolo[4,3-a] pyrimidine-3-carbonyl) phenylthiol semicarbazide (11).
Besides, acid hydrazide (6) was treated with phenyl isothiocyanate in refluxing ethanol to give compound (11)1-(1,5-dihydro- 5-oxo-1,7-diphenyl-1,2,4-triazolo [4,3-a] pyrimidine 3 carbonyl) phenyl thiosemicarbazide as shown in Figure 3. The latter product was subjected to intramolecular cyclization when treated with sulfuric acid, dry pyridine and KOH (5%) demonstrating a new synthetic route to produce compounds 12, 13 and 14, respectively. Subsequent treatment of compound (14) with methyl iodide in the presence of sodium ethoxide solution, yielded 3-(5-methyl thio-4-phenyl-4H-1,2,4-triazol-3-yl)-1,7-diphenyl- 1,2,4-triazolo[4,3-a]pyrimidin-5-(1H)-one (15). It is worth noting that the treatment of compound (14) or (15) with hydrazine hydrate under reflux condition produced the same product, identified as 3- (5-hydrazino-4-phenyl-4H-1,2,4-triazol-3-yl)-1,7-Diphenyl- 1,2,4-triazolo[4,3-a]pyrimidin-5(1H)-one (16) (Figure 3).
Besides, the treatment of compound (11) with phenacyl bromide in refluxing ethanol, in the presence of triethylamine, yielded 1,5-dihydro-5-oxo-1,7-dipheny-lN-(3,4-diphenyl-3H-thiazol- (2E)-ylidene-1,2,4-triazolo[4,3-a] pyrimidine-3-carbohydrazide (17) as shown in Scheme 3. Treatment of acid hydrazide (6) with carbon disulfide in ethanol, in the presence of potassium hydroxide at room temperature, resulted in the formation of potassium salt (18). The latter product reacted with ethanolic potassium hydroxide to afford 3-(5-mercapto-1,3,4-oxadiazole-2-yl)-1,7-diphenyl- 1,2,4-triazolo[4,3-a]pyrimidin-5(1H)-one (19) (Figure 3). The mechanism of formation of the corresponding ox diazole (19) was studied and discussed in previous studies [21-23]. Moreover, potassium salt (18) was subjected to treatment with hydrazine hydrate, in refluxing ethanol, the reaction yielded as 3-(5-mercapto- 4-amino-4H-1,2,4-triazol-3-yl)-1,7-diphenyl-1,2,4-triazolo[4,3-a] pyrimidin-5(1H)-one (17) (Figure 3).
Additionally, it was reported that the reaction involving the synthesis of 4-amino-1, 2, 4-triazole can took place by a simple conversion of 1, 3, 4-oxadiazole under the action of hydrazine hydrate [24,25]. Likewise, the corresponding dicarbonyl compounds including acetylacetone and ethyl acetoacetate were subjected to condensation with acid hydrazide (6) in the presence of an appropriate amount of piperidine as catalyst to give the substituted pyrazole derivatives 3-(3,5-dimethylpyrazole-1-carbonyl)-1,7-diphenyl- 1,2,4-triazolo[4,3-a]pyrimidin-5(1H)-one (20) and 3-(3-methylpyrazole-5-oxo-1-carbonyl)-1,7-diphenyl-1,2,4-triazolo[ 4,3-a]pyrimidin-5(1H)-one (21), respectively (Figure 4).
The structure of these compounds was established based on spectral and elemental analysis reported in the related literature [26-28]. Finally, condensation of acid hydrazide (6) with acid anhydrides, namely phthalic anhydride and 2, 3, 4, 5-tetrachlorophthalic anhydride, in refluxing glacial acetic acid, produced the corresponding imides (22) and (23), respectively (Figure 4). Biological studies demonstrated that these compounds exhibited antihypertensive activity [20] (Figure 5).
Conclusion
In this mini-review, we report on the efficient procedures for the synthesis of pyrimidinedione and pyrimidinethione derivatives. The experimental results showed that the prepared product displayed outstanding pharmacological activities when screened In-vitro against gram positive and gram-negative strains and could be further exploited in medicinal chemistry.
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.business.site/
For more articles in Open Access Journal of Petrochemical Science please click on: https://juniperpublishers.com/rapsci/
To know more about Open Access Journals Publishers
To read more…Fulltext please click on: https://juniperpublishers.com/rapsci/RAPSCI.MS.ID.555676.php
35 notes
·
View notes
Text
Juniper Publishers-Massive Thrombophlebitis as a Complication after Carpal Tunnel Release: Comorbid Factors?

Abstract
Geriatric care is very critical care owing to the fact that elderly people need care and comfort to lead a healthy life without worries and anxiety. Elderly care is a bit peculiar as compared to other specializations in medicine. Non-clinical interventions assumes rather more importance inter alia and services. The world population is rising so the proportion of elderly habitants. Such rising proportions call for more attention on geriatric care. The aim of this research is to study and find the evidence that the role of health care administration is rather more important for geriatrics. The study retrieved few articles and a thorough examination of articles reveals that there is lot of research in the field that emphasises several clinical interventions without explicitly mentioning the importance of administration services in geriatric clinics and hospitals. However, all those recommendations found in this literature indirectly call for more effective and efficient intervention of health care administration.
Keywords: Geriatrics; Elderly Care; Health Care Administration; Literature Review
Introduction
The world is aging quickly and the proportion of population having elderly people is increasing steadily. Almost 500 million people worldwide were above 65 in 2006. It is estimated to rise to a whooping amount of 1 billion by 2030. This means 1 in every 8 inhabitants will be aged individual on the globe. Most of this elderliness is witnessing in developing countries [1]. The rising levels of elderliness in population also brings rising illness and diseases. Older patients require more care and that trigger more cost and other economic burdens directly to hospitals and indirectly to the economy. The care, so, becomes precious for patients which in turn throw more challenges to healthcare administrators to make it further affordable.
Methods
The very objective of this article is to explore and find some of the potential problems in the area of geriatrics with a special emphasis on health care administration. As it was mentioned in the introduction, the rising population engender increase in diseases and other health issues in elderly people. This tends to pose more challenges to health care administrators due to the very fact that managing geriatric care is not as it is with other specializations.
This study is basically a review work. Few articles of scholarly nature were retrieved using Google Scholar. The online search was performed using certain tags like healthcare administration, medical problems, geriatrics. About 16,30,000 results were displayed in 0.68 seconds. All the links displayed observed to have three of the tags that were used for data retrieval. However, only first few yet suitable 5 articles were used to make the review. The articles were selected using simple random sampling method. The following section shows the observations of the study.
Review
Ory MG [2] did certain study titled “emerging issues in geriatric care: aging and public health perspectives”. The aim of the research is to find and detect major social and healthcare challenges of aging population in US. The study finds that though the overall disability is decreasing yet the burden of the same together with other health conditions of the public in US tend to rise in near future. The study offers certain solution that evidence-based interventions might be able to address health problems of aging population. The study also suggests that the databases are useful to retrieve certain data and address the health problems of aging population. This study did not mention anything explicitly about health care administration however, some of the facts that were mentioned in the study are found to have connections with health care administration. For instance, data retrieval and their potential use for healthcare improvement involve the role of administrators. In the same fashion, health care interventions, that were suggested in this study also, one way or the other demands active yet efficient administration practices in hospitals.
Amy KTD et al. [3] did certain study on patient safety in geriatrics. The article mentions that the patient safety has become major health concern. The study criticises certain other publication named “To err is human” which is published by Institute of Medicine in 1999. The study also did certain critique on safety systems in healthcare concerns. The study makes six recommendations after going through certain safety methods. They are: detection and reporting of geriatric syndromes, identifying system failures when geriatric syndromes occur, establishing dedicated geriatric units, improving the continuity of care, reducing adverse drug events, and improving geriatric training programs. This study perhaps brings rather more importance on healthcare administration. Implementation of safety measures as they were suggested in the study demands active role of healthcare administrators. Some of the safety measures i.e. establishing dedicated geriatric units, continuity of care, training programs in geriatrics gives the idea that health care administration is very critical for geriatric care.
Merrell RC [4] did a study on Geriatric Telemedicine with an aim to excavate evidence for telemedicine as a way to address problems through review of literature. The research mentions that the telemedicine offers many means to address the problems of geriatric care in creative ways. The use of electronic medicine, telecommunications, and information management has now found its way into the very fabric of health care. The use of telemedicine is a fait accompli in much of the world, and it continues to have an increasing role deeply imbedded in our electronic practices coupled with social media. Though this paper has not mentioned anything health care administration explicitly but some of the issues like electronic medicine, telecommunications, information management do require lot of administration services apart from clinical services.
Hanlon JT [5] did study on drug-related problems in older adults. The aim of the study was a systematic review employing methods related to online database searches. The authors retrieved 2012 scholarly articles. The study was done using certain online tags like combination of the terms elderly, aged, drug-related problems, medication related problems, medication errors, suboptimal prescribing, inappropriate prescribing, underutilization, polypharmacy, medication monitoring, medication dispensing, medication administration, medication adherence, adverse drug events, and adverse drug withdrawal events. Only 40 of articles found to be apt for the study. Out of 40 only 24 articles found to be related to medication errors, followed by 18 related to ADEs, majority of them addressing adverse drug reactions. Only 3 of the retrieved articles found apt for the study and recommendations were done based on these articles. Perhaps, this is the only paper among all which mentions about the word administration so explicitly in the research findings.
Sidik SM et al. [6] did a study on physical and mental health problems of the elderly in rural Selangor. The study was done using five of nine village’s selected using random sampling in the sampling area. Elderly people in those selected areas were interviewed using a pre-tested structured questionnaire which included -30, ECAQ and Barthel Indices. The study shows that out of 263 study individuals, which 6.2 % of population, 60.1 % of the surveyed people agreed to have physical problems. 15.1 % found to have functional dependence. It was also found that each of 7.6% and 22.4% of people are suffering from mental health problems such as depression and cognitive impairment respectively. More interestingly depression is significantly associated with unemployment, whereas, cognitive impairment is significantly associated with several of socioeconomic characteristics. Though there isn’t any mentioning of health care administration but few of main variables such as unemployment, cognitive impairment, socioeconomic characteristics and their influence on care were directly falls in the ambit of health care administration.
Conclusion
The main of this paper is to find certain evidence in support of the role and its importance of health care administration especially in geriatric care. As far as methodology is concerned the data retrieved from certain sources using Google Scholar. Only very few articles were studied in search of evidence in support of the assumption that the role of health care administration is very critical for geriatric care. Only one research paper out of five selected has mentioned about the importance of health care administration in geriatric care. Rest of the papers had not mentioned anything about administration services. Suggestions or findings that were done through these papers indirectly emphasises importance of health care administration. So this review work suggests that all care done through geriatrics needs effective and efficient health care administration services. However, more research effort with rigorous and meticulous methods need to be done to affirm such statements of care.
To read more articles in Journal of Gerontology & Geriatric Medicine
Please Click on: https://juniperpublishers.com/oajggm/index.php
For more Open Access Journals in Juniper Publishers
Click on: https://juniperpublishers.com/journals.php
#Juniper Publishers LLC#Juniper Publishers group#Juniper Journals#open access Publishers#gerentology#Geriatrics
0 notes
Text
Falls in Older Adults: How to Asses and Prevent? | Juniper Publishers

Juniper Publishers-Open Access Journal of Yoga and Physiotherapy
Authored by Natália Boneti Moreira
Opinion
Falls and its related consequences are among the major elderly’s public health worldwide problem [1-4]. Approximately 42% of elderly with 70 years or more have experienced at least one fall in the last twelve months [4]. A recent systematic review showed a higher risk-adjusted mortality in falls compared to motor vehicle collisions [3], increasing morbity and mortality in older adults [3,5,6].
Several studies have demonstrated exponential growing risk of falls with increasing age [3,7,8], not only by structural and physiological changes, but also by reduction of functionality and increasing of frailty [4,5]. Functionality is associated with elderly’s function and physical capacities, as muscle potency, walking speed and functional mobility; and social and attitudinal environmental factors affecting them [9,10], and the declines of these capacities have the potential to increase fall’s risk and the severity of falling consequences in older adults [11].
Besides the physical consequences, falls lead to psychological and cognitive changes, as social isolation, depression, fear of falling [11-13] and reduction in quality of life [11,14]. It has been concluded that combination of these factors restrict their activities of daily living, social activities and health perception, making elderly’s functionally dependent, and therefore, generating a negative social and economical impact on family, community and society [4,11,13].
In this context, it’s really important to assess the risk of falls and prevent these episodes. The multifactorial assessment identifies the risk factors for falling. The evaluation may include cognitive impairment, continence problems, falls history (involving causes and consequences, such as fear of falling and injuries), adequate use of footwear, home hazards (e.g. inadequate lightening, carpet or slippery floor, etc.), health problems that may increase their risk of falling (e.g., arterial hypertension, syncope syndrome, visual impairment, etc.), inadequate or excessive use of medication, postural instability, mobility problems and/or balance problems [15,16].
All older adults with frequent falls or with increased risk of falling should be considered for an individualized multifactorial intervention composed by strength and balance training, home hazard assessment and intervention, vision assessment and referral, medication review with modification/withdrawal and psychological aspects including risk behavior and fear of falls. These aspects can avoid the reduction of physical activity level promoting independence and improving physical, psychological and social function, providing a better quality of life for older adults [15,16].
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.business.site/
For more articles in Open Access Journal of Yoga and Physiotherapy please click on: https://juniperpublishers.com/jyp/
To know more about Open Access Journals Publishers
To read more…Fulltext please click on: https://juniperpublishers.com/jyp/JYP.MS.ID.555677.php
26 notes
·
View notes
Text
Juniper Publishers-Postural Control in Patients with Respiratory Dysfunctions: A Systematic Review

Abstract
Objective:To identify the main methods of intervention by means of exercises through postural control for COPD and asthmatic patients and their beneficial effects.
Methods:A systematic review was performed to identify which postural control treatment should be applied in these cases. The following bibliographic databases were consulted: PubMed, Bireme and Science Direct. Clinical trials involving techniques for postural control and that compared the results analyzed in the pre and post intervention period.
Result: The electronic search yielded a total of 2113 references published in any language, of which only 7 met the criteria for inclusion and exclusion.
Conclusion:Broadly, the age bracket above 50 years was observed in 6 out of the 7 studies; resistance training in 3 out of 7 studies; vibratory platform training in 1out of 7 studies; postural control training associated with breathing in 3 out of 7 studies and clinically significant improvement in intervention in 3 out of 7 studies, demonstrating a variety of treatment techniques making it difficult to produce a higher level of evidence.
Keywords: COPD; Respiratory; Asthma; Postural Muscle; Postural Control
Abbrevations: COPD: Chronic Obstructive Pulmonary Disease; WHO: World Health Organization; COLD: Chronic Obstructive Lung Disease; UN: United Nations; ABC: Activities Specific Balance Confidence scale; TUG: Time Up and Go; BBS: Berg Balance Scale; SGRQ: St George’s respiratory questionnaire; RS: Romberg stance ; STEC: SemiTandem Stance ; STEO: Semi Tandem Stance; OLS: One Led Stance; CRQ: Chronic Respiratory Questionnaire; TOC: Oxygen Cost Diagram; VAS: Visual Analogue Scale; MVV: Minute Volume ; FVC: Forced Vital Capacity; 6MWT: 6-Minute Walk Test
Introduction
Respiratory dysfunctions affect a large part of the world’s population. Among them, two have a prominence and are studied by the World Health Organization (WHO) and by researchers in much of the world. Chronic Obstructive Pulmonary Disease (COPD), according to the Global Initiative for Chronic Obstructive Lung Disease (COLD), may be defined as a preventable and treatable disease [1]. The COPD is a progressive lung disease and a leading cause of morbidity and mortality in Canada [2]. It is also identified as one of the leading causes of death in the world. Data from the World Health Organization (WHO) and the United Nations (UN) estimate 3 million deaths / year. The Canadian health care system estimates an annual average spending of $1.5 billion [3]. The second dysfunction is asthma. The WHO estimates that 235 million people currently suffer from asthma. Asthma is the most common non communicable disease among children [4]. Today, the impairment in patients with pulmonary diseases goes beyond respiratory changes, delivering many other extra pulmonary consequences [5], as is the case with postural control. The systematic review on postural control in COPD, with studies involving the vast majority of control groups [6] concluded that COPD patients have postural control deficits when compared to healthy groups with combined ages. It is known that intervention in respiratory dysfunctions is aimed at reducing pulmonary disturbances, but especially the extra pulmonary disorders. Considering the spine, thoracic cavity and large muscle groups as fundamental to control the sensation of dyspnea, reducing ventilatory work, intervention improves pulmonary volumes and capacities, postural control and minimizes the effects of disuse with the progression of these diseases [7]. But what would be the best intervention methodology? Thus, this systematically review focuses on the literature concerning to identify the main methods of intervention of the last 7 years, with the use of postural control for COPD and asthmatics patients and their beneficial effects.
Materials and Methods
In the present study, a survey was performed on the PubMed, Bireme and ScienceDirect databases. Studies were selected after defining the DeCS and MeSH search terms, such as asthma, postural control, COPD, postural muscles, respiratory. These terms were crossed via Boolean switch statements (AND), as shown in the following topics:
a) Respiratory and postural control and postural muscle;
b) COPD and postural control and postural muscle and respiratory;
c) Asthma and postural control and postural muscle and respiratory;
d) COPD and respiratory and postural muscle;
e) Asthma and respiratory and postural muscle,
Including titles published from January 2010 to October 2017. Initially, four reviewers (YS, DB, GW, FB) independently assessed all selected titles (n = 2113), analyzed their abstracts based on inclusion criteria defined for the study: a clinical trial involving techniques for postural control and comparing the results analyzed in the pre- and post-intervention period. From this sample the following articles were excluded: those published in the form of abstracts, those that only evaluated the subjects and did not treat, those that only compared between healthy groups and with respiratory dysfunction without intervention and the articles relating the postural control only with the risk of falls. Duplicate items were also omitted (Figure 1). The full texts of the potentially relevant articles were retrieved for final evaluation, and their reference lists were independently checked again by the same reviewers to identify studies of potential relevance not found in the electronic search.
Result and Discussion
This review provides an important summary of the main available methods of intervention in postural control for patients with COPD and Asthma, indicating the need for more work. Of all the articles included in this review, there are variations of postural control techniques for patients with respiratory dysfunction. Among them are: the time of intervention, in some cases 30-45 min, another 80 min. Such studies ranged from 3 to 12 weeks, 3 to 6 times per week. In addition, some studies have applied gait training; others exercise bike with stipulated speed and other exercise bike with free speed, with low and high intensity of training. Also, resisted exercises with weights or elastic bands, with load defined by 10 RM, free load or by challenges as the intensity supported by the patient, with 10 repetitions or with 15 to 20 repetitions. Traditional exercises or with the use of technological resources such as indicators of postural stability. Balance and coordination exercises. Stretching and relaxation, cognitive tasks. Exercises of diaphragmatic breathing and with closed lips. To finish oriental technique like Tai Chi. This reflects the fragility of the levels of evidence offered by the literature to support these different intervention methodologies (Table 1).
Beauchamp et al. [8], used supervised resistance training in COPD patients 4 to 5 times a week using 6MWT as baseline, each patient received an individualized program of 60% to 80% of the average speed achieved during 6MWT (for treadmill exercise or walking) or 60% to 80% of the VO2max estimate of 6MWT for bicycle training, periods of high intensity exercise were alternated with rest periods (3 min at 80% VO 2 max alternating with 2 min of relative rest). The duration of the exercise progressed until patients could tolerate 20 to 30 minutes of resistance exercise at the most tolerated symptoms level, after which the speed or intensity increased from 10% to 20%. Strength training for upper and lower limbs (3 times per week) included the following lower limb muscles: quadriceps, hamstrings, hip flexors, hip abductors, and hip extensors. The exercises were completed in seated and standing positions with the use of ankle weights for endurance. The training for upper limbs included the muscles, biceps, triceps, pectorals and deltoid using an elastic resistance band. The amount of resistance provided was based on the patient’s ability to complete 15 to 20 replicates [9-11]. Patients received a daily 30-minute class that included stretching in major muscle groups and instructions on diaphragmatic and puckered respiration of the lips. Self-management education and psychological and social support were provided through lectures, relaxation classes and recreational activities at least twice a week for 30 minutes. In a recent study by Gloeckl et al. [12] strength training (15 minutes of cycling at 60% of peak energy) and strength training (four to six exercises on strength training machines with three sets of 15- 20 repetitions for major muscle groups using maximum load. In addition, all patients underwent a supplementary program with squatting exercises on a lateral alternating vibration platform (Galileo®, Novotec Medical GmbH, Pforzheim, Germany) lasting 2 minutes, three Times a week. In general, what varied from one study to the other was: the association between strength and resistance exercises, with association of these elements or chose only to choose strength exercises, in addition, balance exercises were also placed in the intervention program. We used predominantly the following reference tools: ABC (Activities Specific Balance Confidence scale), TUG (TIME UP AND GO), Berg Balance Scale (BBS), St George’s respiratory questionnaire (SGRQ), 6MWT, Romberg stance (RS), semi-tandem stance (STEC), semi-tandem stance (open eyes) (STEO) and one-led stance (OLS). (BESTest), 30-s chair-stand test, PF-10, CRQ (chronic respiratory questionnaire). The ABC scale did not show significant improvement in any of the studies, but the Berg balance scale and the TUG test showed significant improvement in all the studies that used these tests as analysis [12]. In 2016, Bezolli et al. [9] studied participants with obesity, with an age range of around 53 years. An intervention period of 3 weeks was analyzed, with 5 interventions per week, lasting 30 minutes in a group. The intervention was with resistance training using a cycloergometer and specific exercises with the objective of increasing the perception and activation of the lumbarpelvic musculature; world reference evaluative tools such as: Spirometry, 6-minute walk test, chest wall circumference, MIP, MEP, oxygen cost diagram (TOC), visual analogue scale (VAS), and patient functional scale were used.
The experimental group showed significant improvements in functions such as minute volume (MVV), Motley Index and forced vital capacity (FVC). There was no improvement in 6MWT and in the thoracic circumference. The control group presented improvement in 6MWT, thoracic circumference and VAS remained unchanged. The results were beneficial but there is little research on this subject, so it was not possible to compare studies on postural control and improvement of respiratory performance in obese individuals. The study by Marques et al. [10] in COPD patients, applied a warm-up of 5 to 10 minutes, involving range of motion, stretching, low-intensity aerobic exercises and respiratory techniques such as pursed lip breathing, body positions, diaphragmatic breathing, and airways cleaning techniques. After that, resistance training (walking) for 20 minutes with 60% to 80% of the average speed achieved during the 6-minute walk test (6MWT). Strength training (15 minutes) included 7 exercises (2 sets of 10 repetitions) for upper and lower limbs using elastic bands, free weights and ankle weights, and the amount of weight applied was between 50% and 85% of 10 repetitions (10RM). The balance training (5 minutes) mostly comprised static and dynamic exercises using vertical positions and were organized in 4 levels
a) Postures that gradually reduced the support base;
b) Dynamic movements that disturbed the center of gravity;
c) Stress to postural muscle groups; and
d) Dynamic movements while performing a secondary task individually or in groups, with a progressively reduced support base. Finally, 10 minutes rest.
Beauchamps et al. [11] used balance training in four main types of exercise:
a) Posture exercises,
b) Transition exercises,
c) Gait exercises, and
d) Functional strengthening.
When a participant was able to complete a task independently and with little instability, the difficulty level was progressively increased by introducing more challenging conditions (eg, closed eyes, addition of a secondary cognitive task, increase in speed / repetition, or disturbances) Kavocikova et al. [13] analyzed participants with asthma, with an age range of around 11 years. The intervention period was 4 weeks, with 6 per week, lasting 45 minutes in a group. The intervention consisted of: respiratory training with diaphragmatic breathing, pursed lip breathing and thoracic expansion exercises. In addition, children also learned clearance techniques (autogenous drainage and active cycle of breathing techniques), 3 sets of 10 repetitions of each breathing exercise followed by a relaxation of 1 minute pause with controlled breathing. Breathing exercises were also performed in the vertical sitting position in a chair and standing position (bipedal and unipedal conditions) in balance devices (Airex Pad, Soft Gym Overball, Bosi® Balance Trainer PROFI and Original Pezzi® Gymnastik Ball Standard). In physical training: proprioceptive exercises, functional strength exercises (lower limbs, upper limbs and core), hand-eye coordination exercises and resistance training. The evaluation tools were: Postural stability indicator - mediolateral direction (Vx); antero-posterior direction (Vy); and total speed (Vtot). Improvement in Vtot in both positions, Vx in the preferred position and Vy in the adjusted position. After the balance training there was improvement in Vtot in both positions, Vx in the preferred position and Vy in the adjusted position.
Finally, Holmes et al. [14] analyzed participants with a mean age of 70 years in a 12-week intervention period, with 2 interventions per week, lasting 80 minutes in a group, and receiving an instruction DVD of the entire protocol to be performed 20 minutes, 3 times a week at home. The intervention consisted of: warm-up exercises focused on range of motion, incorporating attention and images into movement, increasing awareness of breathing and promoting relaxation of body and mind. Cardiovascular, cognitive, physical and postural control evaluations were performed (stationary force plate with open and closed eyes). The results had a significant effect on all the variables presented, indicating that the collective effect of Tai Chi was different in relation to the educational control intervention. Despite the beneficial results obtained, there was no possibility to compare those with other studies. In this review, we analyzed the effect of postural control on respiratory dysfunctions. We observed that the interventions showed significant improvement, mainly in individuals with asthma and COPD. Regarding the number of studies with interventions, there is still a small amount of articles exploring this topic, many of them not so specific. Generally speaking, this review comprised: age group over 50 years (6 out of 7 studies); resistance training (3 out of 7 studies); vibratory platform training (1 out of 7 studies); postural control training associated with breathing (3 out of 7 studies), and clinically significant improvement in intervention (3 out of 7 studies). Detailing the approach of the clinical trials, we adopted at least one of the evaluation methods below: the Berg Scale (BBS); 6-minute walk test (6MWT) and Time Up Test (TUG); no significant change was found in 6MWT, but with changes in the other tests. The study that presented a larger sample, with the objective of verifying the capacity of exercises in resistance training for individuals with respiratory dysfunctions, presented a significant improvement in the performance of postural control. However, there was no evident significance in the evaluation exercises that also addressed resistance training.
Conclusion
In conclusion, postural control techniques or interventions used in patients with respiratory dysfunctions were more evident in patients with COPD, with a large variety of techniques, but with evaluation methods of recognized quality. There was no demonstration of superiority of one technique when compared to another and in addition, we noticed an extensive methodological variation between the interventions, which hinders the production of a greater level of evidence. Therefore, it is necessary to carry out a larger number of randomized studies involving this population and the intervention techniques.
To read more articles in Journal of Gerontology & Geriatric Medicine
Please Click on: https://juniperpublishers.com/oajggm/index.php
For more Open Access Journals in Juniper Publishers
Click on: https://juniperpublishers.com/journals.php
0 notes
Text
Notes for Clinical Use of Extra Acupoints | Juniper Publishers
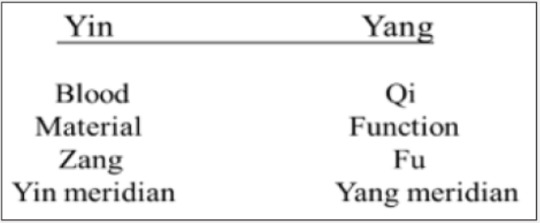
Juniper Publishers-Open Access Journal of Complementary Medicine & Alternative Healthcare
Authored by Tong-zheng Hong
Abstract
Pattern identification is the key concept of the traditional Chinese Medicine theories, which unfortunately cannot apply to extra acupoints for the lack of Yin-Yang. The recent studies suggest that extra acupoints selected in combination with traditional acupoints on the traditional fourteen meridians for anesthesia in surgical operation are marking the beginning of a new chapter and indicate more and more extra acupoints will be discovered.
Keywords: Yin-Yang; Extra acupoint; Pattern identification; Traditional chinese medicine
Introduction
Extra acupoints distinguish themselves from the regular acupoints on the traditional fourteen meridians with the unique indications, actions, and the great effectiveness in acupuncture theory and treatment, even though some of extra acupoints have not been verified with scientific evidence [1].
The Yin-Yang balance is the unique concept and the dominating key of the traditional Chinese medicine (TCM) throughout the history of Chinese medicine for many centuries [1]. It is believed that this concept absolutely distinguishes TCM from the Western medicine. Based on this concept, a disease thus indicates the loss of the balance of Yin-Yang. On the other hand, this concept also serves as the foundation and the guidelines for the etiology of diseases, diagnosis, and treatments [2].
The balance of Yin and Yang can be achieved by stimulations through techniques such as acupuncture, acupressure, moxibustion, cupping, and Tui Na on acupoints. The classic and well-known protocol of Four Gates (LV 3, Yin and LI 4, Yang) used for the successful treatment of the sub-health demonstrates the application of the concept and highlights the importance of Yin-Yang balance [3].
However, extra acupoints are totally excluded from this theory simply because they have not been incorporated into the traditional fourteen meridians.
Overview of the Development of Extra Acupoints
The meridian system is established on the experience and knowledge of the use of extra acupoints and Ashi points. Ashi (Ah Shi) points, also called painful points, were first discovered accidently in ancient China to alleviate pain and treat certain sicknesses in the daily life. Literally in Chinese, Ashi meaning “Ah yes” is coined to refer to the certain “tender spot or pathological sites” on the body with responding signal of pain for diagnosis first presented in Jing Jin Di Shi San (Thirteenth Writing: Sinew Channels) of Ling Shu. In addition, Ashi points can also serve as a treatment site as well [4].
The entire Chinese medicine systems was not established and presented until the Warring States Period (476-221 BC). Examples of extra acupoints like “tip of finger poking”, “between eyebrows”, and “stabbing the Shaoyin beneath the tongue” were mentioned in Huang Di Nei Jing (Yellow Emperor’s Inner Classic) with the locations of extra points, instead of the formal names [4].
Ashi points were not formally recognized and accepted to be incorporated into the traditional fourteen meridians. However, Extra acupoints themselves derived from Ashi points and represent the frequently used Ashi points with verified functions finally [1].
The specific names of extra points viewed as Ashi points initially were not given until the Sui Dynasty (581-618 CE) and the Tang Dynasty (618-907 CE). Up to 187 extra points were incorporated into Qian Jin Yao Fang (Thousand Ducat Formulas) by Sun Si-miao (581-682 CE) in the Tang Dynasty. Not until the Ming Dynasty were extra points formally discussed in the classic Qi Xiao Liang Fang (Wonderful Well-Tried Recipes). There were 26 extra points collected in the Chapter Extra Point in Volume 5, which marked the beginning of collecting extra points. 35 extra points were collected in Zhen Jiu Da Cheng The Systematic Classic of Acupuncture and Moxibustion); 84 extra points collected in Lei Jing Tu Yi (Illustrated Supplement to the Classic of Categories); 144 extra points collected in Zheng Jiu Ji Cheng (Compilation of Acupuncture of Moxibustion). Extra acupoints were officially separated from the traditional 14 meridians when the TCM doctors of the Tai Yi Yuan (Imperial Medical Institute) in the Qing Dynasty (1644-1911 CE) revised Yi Zong Jin Jian (Golden Mirror of Medicine) and built its own unique system [5].
Literature shows that most of the extra acupoints are not associated with a specific meridian and bear the characteristic of Yin-Yang; however, some extra acupoints like Yintang (M-HN-3), Sishencong (, M-HN-1) are located on the Governing vessel, one of the Erbai (M-UE-29) is on the PC meridian, and Taiyang (M-HN-9) is on the Sanjiao meridian [1].
Keys to Therapeutic Effects
Since diseases are understood to be a loss of balance between Yin and Yang as shown in Figure 1, good results cannot be expected without the positive consideration of Yin and Yang [1,2].
An extra acupoint may be or may not on the meridians closely associated with Yin and Yang. The typical examples to explain the importance and necessity of Yin-Yang are Five Shu-Points. As a matter of fact, each Five Shu-Point corresponds to one of the specific phases of the Five Elements, highlighting the importance of balanced Yin -Yang.
The Five Elements theory and the Yin-Yang concept unfortunately cannot apply to extra aupoints only because they are not on the traditional fourteen meridians. In other words, extra acupoints like Yintang (M-HN-3), Sishencong (M-HN-1), Erbai (MUE- 29), and Taiyang (M-HN-9) may be easier for practitioners to consider in practice with the location associated with the specific meridians bearing the characteristic of Yin-Yang as shown in Figure 1 [1].
Signs and symptoms in Traditional Chinese medicine may be totally different from those in the Western medicine and are understood to be broader. In general, TCM physicians or acupuncture practitioners usually do not follow the typical Western pathological classifications of diseases, but rather rely on the patterns individualized by the imbalance of Yin-Yang, Qi, and Blood, and body fluids in the body [1].
Patterns are unique in TCM and pattern identification plays the most critical factor for the treatment and correlates closely with the successful outcomes. However, studies by Hong [1], Zhu et al. [6], Yu SY, et al. [7], and Paraskeva, et al. [8] show extra acupoints can be used together with traditional acupoints in clinical practice but patterns were unfortunately not included in the research designs.
One of the most practical approaches in a clinical practice to acupuncture involves the use of Ashi points when the patients suffer acute pain. However, this apparent simplicity may be discarded by practitioners when it comes to the application of TCM theories to treatment based on the complex meridians and the acupoint theory.
The historical developments of extra acupoints show an extra acupoint can surely play an essential role and be used alone for the treatment, even though they do not have the corresponding phases based on the Five Elements theory. Whether or not extra points can be selected in combination with traditional acupoints in a protocol for the more effective results of the treatments deserves attention.
Discussion
The challenge acupuncture practitioners face is when it is the best time to consider extra acupoints in a protocol.
The protocol following the TCM theories can bring about the best results. Taiyang (M-HN-9), for example, can be selected for one-sided headache as GB20 when the pathogen is exterior Wind [1]. In other words, this example explains the concept of pattern (Zeng) identification based on differential diagnosis is out of doubt the key to treatment using extra acupoints.
The historical developments of extra points show that an extra point can surely play an essential role in acupuncture and be used alone or with the traditional regular acupoints for the treatment. Unfortunately, the actions and indications of extra acupoints have not be scientifically researched and verified as traditional regular acupoints.
In strategy, a practitioner may take the principle of “Least needling, best results” into consideration in practice, keeping patients from pain or worry. The goal can be achieved with the following four protocols shown in Figure 2 when it comes to the tactic.
As one of the oldest forms of the natural healing arts, acupuncture began its development and employment for anesthesia in surgical operation in the late1950’s. In a pilot study in 2015by Wang et al., 12 parents were randomized to an acupressure bead with occlusive tape covering at the Extra 3 (Yintang) point for 20 minutes. Parents in the acupressure group had significantly less anxiety at 20 minutes post-intervention compared with parents in the sham group [9].
It is true that patients and healthcare providers are usually concerned about side effects. The finding of a study on the Severity of Venipuncture Pain Among Hospitalized 6–12-Year-Old Children shows extra point Extra 3 (Yintang) in combination with P-8 (Laogong) point are recommended for its greater safety, costeffectiveness, and applicability [10].
The positive result of facial acupuncture reported by Donoyama et al. showed the protocol of BL1, GB1, ST1, ST3, ST4, ST7, SI19, CV24, Ex-HN3 (Yintang) and Ex-HN4 (Yuyao) could increase the water and oil content of the facial skin [11].
In clinic, practitioners are also concerned about if there is enough evidence-based research at present to show whether or not the use of extra acupoints alone will bring better results than the use in combination with regular acupoints. However, current studies show the extra acupoints can be effective alone, but better results of extra acupints used in combination with traditional acupoints are also reported in some researches [1].
There is no doubt that needling sensation (deqi) has been considered by many acupuncture practitioners to be a key component of a successful acupuncture treatment. However, this sensation will not occur when the needles are not insert into the acupoints accurately, which may also happen to the use of extra acupoints. In other words, locating an extra acupoint accurately is the key to the successful treatments. It is same with the development of the regular acupoints, location description may vary in different textbooks. For this issue, it is highly suggested that the use of a Moxa roll can help practitioners locate the extra acupoints accurately. The heat emitted from the Moxa roll penetrate the extra acupoint like an acupuncture needle as long as the Moxa roll pinpoints the acupoint location.
The well-known school of acupuncture characterized with extra acupoints in the world is Tung’s acupuncture, which develops and establishes the exclusive theory and protocols extremely different from the TCM. In the meantime, the new extra acupoint Gangshui discovered and used for treating subacute cough demonstrates numerous extra acupoints may remain undiscovered [1].
Looking back at the development of extra acupoints, we can expect that more and more extra acupoints in various contexts may be discovered in the future.
Both acupuncture and acupressure are used based on the acupoint stimulation to achieve the desired results of treatments. Acupuncture performed by acupuncturists to triggers a stronger stimulation on the acupoints than acupressure to activate the body’s innate healing ability. Acupressure refers to stimulating the points on the surface of the skin by pressing with the hands, fingers, elbows or feet, is basically noninvasive and can be performed by the patients themselves.
Massage on extra acupoints is feasible for healthcare. Compared with acupuncture that may cause side effects suggested by Kashefi [12], acupressure has several advantages over acupuncture and deserves recommendations for its immediate effect, safety, costfree, no side effects, and convenience to patients.
Conclusion
With new extra acupoints increasingly discovered, it is predictable that acupuncture will gain more popularity all over the world in the future because it is effective, low cost, non-surgical, and painless way to healthcare.
On the other hand, additional researches are needed to understand if extra points can outperform the traditional acupoints on the traditional fourteen meridians.
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.business.site/
For more articles in Open Access Journal of Complementary Medicine & Alternative Healthcare please click on: https://juniperpublishers.com/jcmah/
To know more about Open Access Journals Publishers
To read more…Fulltext please click on: https://juniperpublishers.com/jcmah/JCMAH.MS.ID.555728.php
36 notes
·
View notes
Text
Juniper publishers-Performance Evaluation of Newer Types of Silk Surgical Sutures

Abstract
The effectiveness of newer types of silk surgical sutures have been critically evaluated and their influence in the surgical operations studied. A variety of suture materials are available for primary wound closure following oral surgical procedures. The aim was to review the tissue reactions to the various suture materials used in oral surgical interventions. Closing the surgical incision is an important step in the surgical procedures, the success of surgery is sometimes compromised by the defective suturing techniques or improper suturing materials, black silk sutures are more or less most often used materials in the day today surgical procedures, but these suture materials demand more time and effort from the surgeon and there is a need to substitute these materials with more user friendly and more successful wound closing materials such as cyanoacrylates. This study intends to compare effectiveness of the black silk sutures with cyanoacrylate adhesives in closing the surgical incisions. Trachoma causes blindness through an anatomical abnormality called trichiasis (lashes touching the eye). Trichiasis can recur after corrective surgery. We tested the hypothesis that using absorbable sutures instead of silk sutures might reduce the risk of recurrent disease among patients with major trichiasis in a randomized trial. The purpose of the study was to treat silk sutures with natural fungal pigment namely Thermomyces of different concentrations 1.5%, 2.0% and 2.5%, and to analyze its effect on the properties of silk sutures such as tenacity, knot strength, friction and antimicrobial activity.
Drug loaded antimicrobial silk suture have been developed for use in both wound closure and wound healing with an intention to prevent surgical site infections. The material has been analysed for various suture properties such as tensile strength, elongation, knot strength, bending properties and diameter The suture material is coated with chitosan (biopolymer) and incorporated with herbal drug. Cold maceration technique is used to extract Cynodondactylon drug for the study. The findings of the various studies mentioned herein are discussed in the subsequent sections of the article.
Keywords: Antimicrobial property; Silk; Tissue reaction; Cyanoacrylate glue; Absorbable; Fungal extract
Introduction
In many surgical interventions there is a need to close the primary wound with a previously raised flap. Hence, different types of suture materials are available that can be categorized based on their origin (organic and synthetic) or based on their durability in host tissues (absorbable and non absorbable) [1,2]. Healing requires that the surgical wounds are properly closed. It requires close approximation of wound edges using suitable means and techniques. Healing complications arise following surgery due to one or more of the following reasons:
a) Inadequate preoperative assessment.
b) Faulty or traumatic surgery.
c) Inadequate post-operative care.
Normally the wounds create problems relating to reinfection/infection during the process of healing. It is more so with oral wounds due to the increased problem appearing as plaque and food and impaired wound healing. Globally, trachoma is identified as the major contributing factor in blindness [3]. Chronic inflammation of the conjunctivitis results from repeated incidents of ocular Chlamydia trachomatis infection in early childhood. Such inflammation results in scarring of conjunctival tissue that could lead to the rolling in of eyelids and scratching of the lashes on the surface of the eye (trachomatoustrichiasis [TT]). In the end, continued abrasion of lashes and secondary bacterial infection lead to blinding corneal opacification (CO). A crucial aspect of the surgical process is the wound closure with suture materials. Sutures are natural or synthetic textile biomaterials widely used in wound closure, to ligate blood vessels and to draw tissues together [4]. Sutures consist of a fibre or fibrous structure with a metallic needle attached at one of the fibre ends and they can be classified into two broad categories namely absorbable and non-absorbable sutures. The most crucial requirements of suture materials are physical and mechanical properties, handling properties, biocompatibility, and antimicrobial nature [5]. Till date, there is no single suture material which can fulfill all the crucial requirements of sutures [6]. Sutures are natural or synthetic materials available in monofilament, multifilament, twisted and braied forms, used in wound closure, ligates injured blood vessels and to draw tissues together [7,8]. These comprise of absorbable and non absorbable types and attached with a metallic needle at one of the fibrous ends. The properties such as physical, mechanical, handling, biological, and biodegradation as considered crucial for suture materials, and are related to each other [9,10].
Tissue Reactions to Silk Sutures
A suture material should comprise of the following critical parameters:
a) Knot safety,
b) Stretch capacity,
c) Tissue reactivity, and
d) Wound safety.
The selection of the suture material can also affect the healing of the incised soft tissues apart from the surgical and suturing method practiced [11]. Some cases have been reported relating to complications after the use of a sub epithelial connective tissue graft where an abscess occurred after the primary phase of healing [12]. The investigation has revealed that a probable cause of the abscesses could result from stitch abscess or reaction to the suture material used for the submerged sutures. Hence the choice of the suture material is to be taken into account during treatment planning for oral surgical interventions. An inflammation indicates the tissue reaction and occurs during the first two to seven days after the tissue has been sutured. Many investigations in the past have reported that synthetic materials show a better behavior to oral tissues with regard to tissue inflammatory reactions than non-synthetic suture materials [12-27]. Suture materials such as cotton, braided silk, polyester, nylon, and cat gut have been frequently studied with regard to tissue reactions. But, there are speculations over the outcomes of the investigations. Polyester sutures have been reported to cause a mild inflammatory reaction whereas cotton threads have been associated with an intense tissue inflammatory response. Other commercially available suture materials include polyglycolic acid (PGA) and polyglactin 910 (derived from copolymerization of glycosides and lactides) and have been labeled as "desirable suture materials" [28]; nevertheless, controversy persists over the efficacy of suture materials. It has been reported the bacterial count over the braided silk and PGA sutures to be similar; conversely, other studies have reported that silk sutures are more susceptible to bacterial invasion and severe tissue inflammatory reactions compared to other suturing products. However, in terms of cost-electiveness, silk continues to enjoy its status as an "inexpensive" suture material as compared to other non-absorbable suture materials. As the selection of the suture material used in oral surgical interventions may play a role in optimal post surgical wound healing, it has been focussed to review the tissue reactions to the various suture materials used in oral surgical interventions.
In the case of dental and medical surgeries a number of suture materials are being used. But, surgeons should understand the nature of the suture material, the mechanism of healing process, and the interaction between the suture material and the surrounding tissues. It is a serious problem since the surgeon should ensure that a suture would retain its strength until the tissues of the previously raised surgical flaps gain adequate strength to maintain the wound edges together. Till today the research details relating to the effectiveness of different materials are questionable and not consistent. Hence efforts have been directed to review the tissue reactions to various suture materials used in oral surgical interventions. In the case of dental and many other surgical procedures, silk has been the most traditionally used suture material [29]. Despite silk being economical and easier to handle than other non absorbable suture materials it should not be considered as a "material of choice" for oral surgical interventions [30]. Studies on oral tissue reactions to sutures have revealed constant inflammatory reactions, which are most prominent with silk and cotton and minimal with others including nylon, polyester, ePTFE, polyglecaprone 25 and PGA. A histological study compared the oral tissue reactions to various suture materials.
The results showed the presence of a large number of neutrophilic polymorpho nuclear leukocytes in the premises of silk sutures which were less intense in oral tissues farther from silk sutures. Another finding was that fibroblasts and new capillaries formed at a slower pace in the oral tissues in the vicinity of silk sutures compared to tissues farther from the silk sutures. This may be a justification for the delayed healing and severe tissue reactions associated with silk sutures. Another factor that may instigate tissue reactions is the capability of bacteria to adhere to various suture materials. In an in vitro study, the capability of bacteria to adhere to various types of sutures to cause tissue reactions has been investigated. The results showed that bacterial adherence to braided silk sutures was five- to eight folds higher as compared to nylon to which the least numbers of bacteria adhered. In another study, colonization on various intraoral suture materials from patients microbial having undergone dentoalveolar surgery was investigated. The results showed a larger numbers of bacteria on silk as compared to polyglecaprone 25. In an experimental study, the inflammatory responses in oral tissues sutured with silk and ePTFE by recording the presence or absence of bacterial plaque along the suture track has been investigated.
The results showed that bacterial plaque was present in 10 out of the 11 silk and four out of the 11 ePTFE suture channels. These studies may act as possible explanations to the minimum tissue reactions evoked in nylon and polyglecaprone 25 as compared to braided silk sutures. Thus, the different rates of bacterial adherence to various suture materials support the hypothesis that bacterial adherence to sutures plays a significant role in the induction of tissue reactions. Since sutures are immediately contaminated as soon as they contact the oral cavity, it is recommended that sutures should be opened just before being passed through the gingival tissues in order to minimize complications such as stitch abscesses. It is well known that systemic conditions such as poorly controlled diabetes mellitus and cardiovascular disease are directly associated with oral inflammatory conditions [31-35]. Therefore, it may be hypothesized that the massive inflammatory response induced by such confounding factors may "mask" the tissue reactions provoked by the suture material. Data from the clinical studies, included in the present review, revealed that all participants were systemically healthy; therefore the influence confounding parameters (such as those mentioned previously) may be overruled. Diabetic rats have been investigated for tissue reactions to silk, catgut, and Polyglecaprone 25. The study of diabetic and control groups reveals similar activities of silk and catgut. There is no clarity regarding whether this similarity in tissue reactions between the two suture materials be attributed to diabetes control or to the properties of the suture material. The use of tobacco products and smoking are other confounding factors that can also support oral mucosal [36-38]. Owing to inadequate data relating to tobacco habits in such investigations, further clinical trials would be required to study the role of tobacco habits as a confounding factor in suture-induced tissue reactions.
Silk Sutures vs Cyanoacrylate Adhesive in Human Mucosa - A Clinical Trial
Suitable material like sutures or tissue adhesives needs to be used for the area to be healed through proper wound closure method. Over the years surgical sutures have been used and different materials ranging from human hair to the recently developed silk sutures are attempted so as to attain a safe closure of wounds. However, despite advanced suture materials and methods situations do arise when the wound closure is not satisfactory and can lead to complications like fistulation and granuloma formation, that could arise mainly due to incompatibility of suture materials per se. Also, the suture materials have innumerable setbacks like cutting through the debris. Thus there is a necessity for an increased focus in prevention of occurrence of infection by way of maintaining an aseptic environment and careful manipulation of tissues during surgical process to prevent or minimize the post-operative complications parenchymal and inflammatory tissues during suturing.
The capillary action of braided or twisted black suture materials, result in increased risk of wound infection, prompting the requirement for suture removal on the seventh day following surgery with non-resorbable suture materials, which creates discomfort to the patient and possibility of early/delayed resorption of suture material with absorbable sutures leads to wound dehiscence or wound re-infection. Besides these, the manipulation of tissue margins with such suture materials necessiate a high level of clinical judgement, dexterity, time and patience from surgeon and exact control over the force application on the suture to avoid excess/inadequate tension in the suture while suturing as otherwise would lead to tearing of the wound margins/necrosis with excess forces or else, slackness in suture leading to gaping between the wound margins leading to partial healing or re-infection/scarring. Further the appearance of diseases such as AIDS, Hepatitis etc. That involve great risk of transmission through needle prick also apprehends the surgeons in implementing this process. It has resulted in the introduction of easier method of wound closure through use of tissue adhesives that are meant to minimize the effort and also avoids the risk of needle prick and tissue tears while closing the wound margins. Thus the use of such tissue adhesives is growing and currently there is a growing necessity to critically assess and test such tissue adhesives to find out their effectiveness, merits and setbacks over the currently used contemporary techniques and materials. The ideal tissue adhesive should demonstrate shelf stability, complete polymerization even in the presence of moisture (blood, saliva or water), it should permit adequate working time, should spread to cover the optimum area, should provide wettability and should not produce excess heat during the process of polymerization and it should provide strong and flexible bond, should be tissue compatible (non-toxic), biodegradable, easily applicable and non-carcinogenic.
In a number of materials attempted, Butyl cyanoacrylate satisfies most of the properties expected of a tissue adhesive. Though such materials' adhesive properties have been identified earlier when initially the alkyl forms and ethyl forms were tried as tissue adhesives, but have been discontinued due to their toxic reactions with the tissues and in their place N-butyl-2- cyanoacrylate (Histoacryl) has been attempted as it showed merits such as achieving immediate haemostasis, and apart from being easy to use it also processed bacteriostatic properties and rapid adhesion to hard and soft tissues [39]. The use of cyanoacrylates in the repair of organs, skin, vessels, nerves, mucosa grafts, closure of laceration wounds and incisions has been done successfully in surgical applications and treatment of extraction sockets, fixation of mandibular fractures ,healing of intra oral wounds, fixation of free gingival grafts, healing of periodontal flaps were also found successful with the application of this cyanoacrylate, it has been reported that butyl and isobutyl cyanoacrylates are non-carcinogenic an0d nontoxic in living organisms unlike ethyl and methyl cyanoacrylate compounds,evaluate and test these tissue adhesives to find out their effectiveness, advantages and drawbacks over the presently used contemporary methods and materials [40-55].
The ideal tissue adhesive should demonstrate shelf stability, complete polymerization even in the presence of moisture (blood, saliva or water), it should permit adequate working time, should spread to cover the optimum area, should provide wettability and should not produce excess heat during the process of polymerization and it should provide strong and flexible bond, should be tissue compatible (non-toxic), biodegradable, easily applicable and non-carcinogenic. Effort has been directed to clinically compare and histologically assess cyanoacrylate adhesive (NBUTYL-2-CYANOACRYLATE) over silk sutures when used for wound closure in human mucosa.
By means of suitable approximation of the wound corners and appropriate separation of the wound the wound healing can be improved after its closure. There is superficial contamination of the wound following surgery which generally results in delayed epithelialization of the wound surface and the production of excessive granulation tissues. Such factors result in surgical failure in yielding the desired outcome and result in lead to greater pain and discomfort after surgery. The healing is hindered by plaque, food debris and excessive manipulation of tissues during surgery. The incidence of infection can be reduced by careful attention to asepsis and gentle handling of the tissues to prevent the implantation of foreign material into them. Postoperatively the immediate concern is the protection of the tissues and to control the infection while healing. Healing is improved by immobilization of the healing area. Immobilization of healing area can be achieved by suture or tissue adhesive.
Post-operative clinical evaluation of the cases in this study clearly revealed that the sites which were closed with silk sutures showed longer duration and more dense inflammation when compared to the sides treated with the cyanoacrylate, this is possible because of the irritation and trauma from the sutures and collection of food particles on the sutured area, moreover the blood coagulum which fills the defects to protect the incision from outside influence probably gets effected by the fibrinolytic effect of the saliva during the healing period 18 whereas the adhesion of the two margins of the incision by the cyanoacrylate leaves no space for salivary interference during healing, thus the isolation of the wound margins from the saliva and food debris/plaque appears to be added advantage provided by the use of adhesive materials like cyanoacrylate for closing the incision margins post operatively, it is 00 also observed that cyanoacrylates has antimicrobial activity, bacteriostatic effects against gram positive microorganisms of n-butyl-2cyanoacrylate have been also reported by Tse [56]. Schmaisner reported that it had bactericidal activity against 10 test bacilli [57]. This study showed that the amount of inflammation on the sutured and glued incision line was different because the epithelialization on the sutured side was not uniform and there was significant scar formation. Besides the soft tissue applications, cyanoacrylates have also been used for the hard tissues. The use of n-butyl-2- cyanoacrylate adhesives in the surgical treatment of fractures is found to hold great potential and it is found that n-butyl- 2cyanoacrylate was nontoxic, non-mutagenic and non- carcinogenic [51]. In certain investigations use of agar overlay tissue cultures has revealed that fibroblast cell death around a disc of n-butyl-2-cyanoacrylate advanced at a slow rate showing its moderate toxicity on fibroblasts in vitro [58,59]. Investigation by means of clinical and electron microscopic study has not shown any evidence of such kind. Thus this investigation favours the use of cyanoacrylate as an effective technique for closing the incision margins.
Comparison of Absorbable and Silk Sutures in Surgical Therapy
The major cause of infection leading to blindness in the world could be attributed to Trachoma [60]. Active trachoma or chronic conjunctival tissue could result from recurrent events of ocular Chlamydia trachomatis infection in early childhood. This inflammation results in scarring of conjunctival tissue, resulting in rolling of the eyelids to roll in (entropion) and scratching of the lashes on surface of the eye (trachomatoustrichiasis [TT]). Finally it leads to blinding corneal opacification (CO) arising due to the continual abrasion of lashes and secondary bacterial infection. Many nations have reported on the prevalence of blinding trachoma. Above 40 million people, majority of them being children have been found to have active trachoma at a given time, 8 million people have trichiasis and a further 8 million are estimated to be blind or visually impaired from the disease [61]. The maximum cases of active trachoma and trichiasis in the world have been found in Ethiopia, with a large number of unoperated cases of TT. Endemic countries are striving to control this disease through the implementation of the SAFE strategy: surgery for trichiasis, antibiotics for infection, facial cleanliness and environmental improvements to reduce transmission [62].
Surgery has been performed to rectify teh entropion, lifting the eyelashes off the cornea in order to prevent blindness from trichiasis. Ophthalmic services are normally restricted in trachoma endemic settings. Hence, specially trained nurses usually perform the surgery in the community. Many varied procedures have been attempted during the past century [63]. However, trichiasis often recurs either due to certain intrinsic restriction or quality of the surgery, or due to progressive scarring. Studies of trichiasis recurrence rates following surgery conducted under “operational” conditions have consistently shown disappointing outcomes, with usually at least 20% recurrence by 1 y and up to 62% at 3 y [64-70]. Moreover, these poor surgical outcomes undermine other efforts to prevent blindness from trachoma. Context-appropriate interventions to improve results are urgently needed. Several factors contribute to recurrent trichiasis, which can be divided into early surgery- related and later disease-related factors. Data from prospective studies suggest that the majority of recurrent trichiasis develops within 6 mo of surgery, indicating the importance of how the surgery is performed [71-73].
Randomized controlled trials (RCTs) of alternative procedures indicate that bilamellar tarsal rotation (BLTR) and posterior tarsal rotation (PLTR) procedures are associated with the lowest recurrence rates, leading to the World Health Organization's (WHO) recommendation of their use [74,75]. However, recurrence rates for both procedures are quite high [76-78]. The quality of surgery is important, indicated by significant variation in the results of different surgeons. Suture type, positioning, and tension are likely to be important aspects of surgical technique that contribute to TT recurrence. Silk sutures are used as standard in trichiasis surgery and need to be removed 7-10 d postoperatively. At this stage the incision may not have reached a state of stable wound healing, because of the scarred nature of the diseased tissue. The use of absorbable suture materials, such as polyglactin-910, which is commonly used in ophthalmic and other surgery, may provide more prolonged and stable fixation of the tissue in the desired position while healing is taking place [79]. Study of surgical outcomes has shown that recurrence rates were significantly lower in individuals who had received long-lasting absorbable sutures (0.8%) compared to those with silk sutures (43.5%). Test has been carried out on the hypothesis of using absorbable polyglactin-910 sutures can reduce the postoperative trichiasis recurrence rate than the existing standard silk sutures, in a randomized trial.
The investigation has many merits including the large size, high follow-up rates, good balance of clinical and demographic characteristics between the randomization groups, the fact that observations at each time point were made by a single observer, and that outcome measures were determined by masked individuals. There were slightly more individuals in the polyglactin-910 group who were lost to follow-up at 12 mo. But, majority of the participants were out of the study circle and hence the small difference cannot be ascribed to effect of treatment. Even after following careful standardization procedures, certain variation has still been found between the findings of the various surgeons, showing the importance of how the surgery is performed. These may include subtle variation in the length of the incision or the tension on the sutures. Individuals with minor trichiasis were excluded from this trial and enrolled into a separate trial evaluating the efficacy of surgery versus epilation [80]. However, we are unaware of any reason to think that these findings could not be generalized to the full range of trichiasis severity. It would be interesting to know if there were significant differences in the participants’ experience of the different sutures used in this trial and their perspectives on the potential benefit of not needing to have the absorbable sutures removed; however, we did not formally investigate this.
Detecting differences in changes in both corneal disease and visual acuity would probably require a longer follow-up period. Polyglactin-910 absorbable sutures had a similar risk of trichiasis recurrence to silk sutures for PLTR TT surgery and comparable secondary outcomes. But, when viewed from a programmatic point of view, polyglactin-910 presents the major merit in which patients do not have to be seen soon after surgery for suture removal. The postoperative review can be delayed for 3-6 months, which could permit to better determine who needs additional surgery and offset the slightly higher cost of absorbable sutures. It is necessary to take into account the logistical merits of using absorbable sutures as far as the selection of suture material is concerned.
Antibacterial Silk Sutures with Natural Fungal Extract
A number of options are available for the surgeon today regarding selection of suture material and he can select them depending upon their availability and his familiarity. Owing to its beneficial properties silk which is a natural non-absorbable suture material has been used over many years as biomedical suture. But, the low microbial resistance property is one of the major setbacks related to the silk. Various antimicrobial agents have been used on silk sutures by many research workers for imparting antimicrobial properties. Silver doped bioactive glass powder has been used to coat silk surgical suture [81]. Recently, investigations on the influence of chitosan coating on the properties of silk sutures have been carried out [82]. In another investigation tetracycline coating on silk sutures has been attempted the influence of tetracycline treatment on silk suture characteristics has been studied [83]. Recently, antimicrobial finishing of textiles using microbial dyes have received greater attention as they require less labour, land, and cost effective solvents for extraction as opposed to higher plant materials. In this study, silk sutures are treated with Thermomyces, a natural fungal extract and its effect on the properties of silk sutures such as antimicrobial activity, friction, tenacity and knot strength are studied.
Silk suture produced was treated with natural fungal extract at optimum concentration and the effects of natural fungal treatment on the suture properties were studied. The result showed that the tenacity and knot strength of silk braided sutures increased compared to the untreated silk suture. The frictional properties of both the fungal treated silk suture and the untreated silk suture were determined by the dynamic coefficient of friction and there is a slight reduction in frictional value found in the treated silk suture compared to the untreated silk suture. The uniform deposition of natural fungal pigment on to the surface of the silk braided suture was confirmed by Scanning Electron Microscopy [84]. The antibacterial activity of fungal treated silk braided suture at optimum concentration against S. aureus and E. coli is found to be good compared to the untreated silk suture. The result suggests that the silk suture treated with optimum concentration of the natural fungal pigment is appropriate to retard the exponential growthof S. aureus, a gram-positive bacterium and E. coli a gram-negative bacterium and hence silk sutures can be developed with the required characteristics for healthcare applications.
Herbally Treated Silk Suture
Most infections that take place in the surgical area arise from sutures, within a month following a surgery or before a year in case of an implant being left in place after surgery affects the incision or deep tissues in the operated area [85]. Since the suture is a foreign material in a surgical wound, it renders the surrounding tissues of wound prone to infections [86]. Presence of bacteria in the surgical wound contaminates the tissues as well as the suture material, and thus results in ineffectiveness in decontaminating the wound [87]. Bacterial attachments and colonization occur in all suture material and leads to surgical site infections [88]. Implants have non-shedding surface, skin or other bacteria to form an extra cellular matrix (biofilms), protecting the bacteria from host defense factors [89,90]. Such biofilm bacteria are not easily treatable and they do not respond so well sensitive to antibiotics and antiseptics. It is necessary to remove the implant, and antibiotic treatment is essential if biofilms infection is formed [91]. In order to overcome this, many antimicrobial sutures were developed by incorporating suitable antibiotics, antiseptics or their combination. Triclosan, commonly used in the antimicrobial sutures, was found to have some demerits such as prematurely change of tadpoles into frogs and reduced sperm production in male rats [92].
Silk is a natural biomaterial that is constituted of fibroin, and aids cell attachment and proliferation. It can also produce a knot of good quality [93,94]. Owing to its biodegradability, biocompatibility, nontoxicity, and anti tumour characteristics chitosan is considered as one of the most valuable polymers for biomedical and pharmaceutical applications [95,96]. As chitosan stimulates hemostasis and accelerates tissue generation, it proves beneficial to wound healing [97]. Suture materials are normally coated with silicon or wax was found to create inflammatory and thrombotic response to the tissues [98]. Coating with chitosan prevents inflammation as well as scar formation with and provides antimicrobial property since silk is easily prone to microbial infection [99].
Aqueous extract of Cynodondactylon ( a traditional herb), commonly called as Bermuda grass was evaluated for their antioxidant, anti inflammatory action while its fresh juice has shown the immunomodulatory and DNa protective activity [100-102]. The ariel part extract of Cynodondactylonwas found to possess alkaloids, phenols, tannins, and flavonoids on preliminary screening. An antibacterial effect and wound healing property of the grass was investigated by many researchers [103-108]. The main focus has been to develop an antimicrobial silk suture preventing SSI by using natural materials having rich medicinal values, which includes biomaterials and medicinal plants.
Silk has been used as a suture material and fabricated using a circular braiding machine. The silk suture is coated with chitosan (a biopolymer) and incorporated with Cynadolandactylon (a natural drug). The coated suture is found to have good properties.
In order to obtain optimum antimicrobial efficacy, response surface optimization process using Box-Behnken experimental design is applied. It is found that 1.7% chitosan and 7% drug at 600C has optimum antimicrobial efficacy with effective bacterial reduction percentage against S.Aureus and E.Coli, when subjecte to antimicrobial study.
Conclusion
In the case of primary wound closures subsequent to oral surgery, many suture materials are available. Study has been done on the tissue reactions to the various suture materials used in oral surgical interventions. Various textile materials have been explored. Polyglactin 910 sutures were associated with the development of stitch abscess in one clinical study. Eight studies reported that tissue reactions are minimal with nylon sutures. Tissue reactions to suture materials used for oral surgical interventions may vary depending on the surface properties and bacterial adherence properties of the material. Comparative clinical and histological studies between silk sutures and cyanoacrylate adhesive has revealed that the use of cyanoacrylate glue has resulted in less postoperative inflammation and good clinical and histological healing when compared to the silk sutures. Silk sutures have been compared with absorbable polyglactin-910 sutures for post surgical effectiveness. There was no evidence over use of absorbable polyglactin-910 sutures was associated with a lower prevalence of trichiasis recurrence at 1 year post surgery than silk sutures. However, from a programmatic perspective, polyglactin-910 offers the major advantage that patients do not have to be seen soon after surgery for suture removal.
The postoperative review after surgery using absorbable polyglactin-910 sutures can be delayed for 3-6 months, which might enable us to better determine whether a patient needs additional surgery. The silk sutures have been treated with natural fungal pigment-Thermomyces of different concentrations to analyze its effect on the properties of silk sutures such as tenacity, knot strength, friction and antimicrobial activity. Silk suture treated with optimum concentration of the natural fungal pigment is appropriate to retard the exponential growth of S. aureus, a gram-positive bacterium and E. coli a gram- negative bacterium and hence silk sutures can be developed with the required characteristics for healthcare applications. Antimicrobial silk suture has been developed for analysis of wound healing and closure so as to avoid surgical site infections. The treated silk material has been investigated for a number of properties. The suture material has been coated with biopolymer chitosan (biopolymer) and incorporated with herbal drug. The drug loaded samples are subjected to antimicrobial study (AATCC 100) against S. aureus and E.Coli and found to have effective bacterial reduction percentage. Hence, the natural drug loaded suture material could prove a better alternative for synthetic drug loaded suture that is found to have certain disadvantages.
To read more articles in Journal of Gerontology & Geriatric Medicine
Please Click on: https://juniperpublishers.com/oajggm/index.php
For more Open Access Journals in Juniper Publishers
Click on: https://juniperpublishers.com/journals.php
#Juniper Publishers#Open Access Journal of Gerontology#juniper publishers review#geriatric research#Geriatric Medicine
0 notes
