Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
Central Migration of Tunneled Dialysis Catheter into Right Ventricle causing Positional Superior Vena Cava Obstruction: A Case Report
Authored by: Muhammad U Sharif
Abstract
Tunneled dialysis catheters placement under real-time ultrasound guidance using the internal jugular route is considered to be a relatively simple and straightforward procedure, though its insertion and maintenance are not entirely risk-free. A literature search is full of reports describing various complications dialysis catheters placement; however, a central displacement of the catheter months after insertion is not described in the past. This case report highlights a case of the central migration of tunneled dialysis catheters and emphasizes the importance of close monitoring of the position of these catheters.
Introduction
The invention of tunneled dialysis catheters, more than three decades ago, has revolutionized vascular access in hemodialysis patients [1]. Over the years, it has become an integral part of the management of patients on hemodialysis and is used in up to a third of such patients, mostly as a bridge to more permanent dialysis access [2,3]. Right internal jugular (RIJ) vein catheterization under real-time ultrasound guidance is a relatively low-risk procedure and is considered the site of choice for tunneled dialysis catheter placement. For best results and to ensure optimal blood flow, it is recommended that the tip of a tunneled dialysis catheter should be positioned at the junction of superior vena cava (SVC) and right atrium or into the right atrium [4,5]. It has been advised not to place the dialysis catheter too deep into the right atrium to avoid potential complications [6,7]. Incorrect positioning of a hemodialysis catheter is relatively uncommon and rarely described. Previous case studies have described the misplacement of central venous catheters or hemodialysis catheter into the azygous vein [8], accessory hemiazygous vein [9], brachiocephalic vein, subclavian vein [10], brachiocephalic artery [11], mediastinum [12], pleural space [13], left atrium [14] and pericardium [15]. Catheter misplacement can happen at the time of insertion or after a while due to the migration of the tip. Although it is not uncommon for a hemodialysis catheter to migrate peripherally and fall out, the central migration of a tunneled dialysis catheter into the right atrium and across the tricuspid valve into the right ventricle has not been described in literature before.
Case report
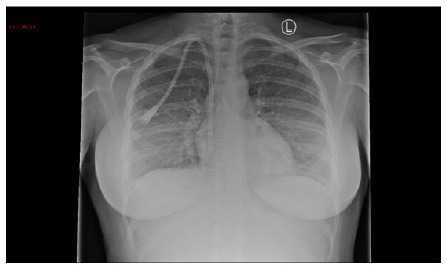
We report the case of a 35 years old woman who developed acute kidney injury (AKI) stage 3 and adult respiratory distress syndrome following severe postpartum hemorrhage. She required level 3 care including renal replacement therapy. Her anuric AKI failed to recover and she was transferred to the renal unit three days post-partum. A renal biopsy was undertaken and showed diffuse cortical necrosis. Her temporary dialysis catheter was removed and the next day, a PalindromeTM tunneled catheter (14.5 Fr, split-tip, 28 cm) was placed in her right internal jugular vein (RIJ) using a real-time ultrasound-guided approach. The position of the RIJ catheter was confirmed with a chest x-ray (Figure 1).
She was re-established on hemodiafiltration and discharged ten days later to continue outpatient renal replacement therapy (RRT). Plans were made for the medical placement of a peritoneal dialysis catheter once her uterus had involuted. The patient remained stable on satellite unit based hemodiafiltration until a week later she developed a mild persistent tachycardia and dyspnea on lying down. Her symptoms progressed into a cough and she was treated for pneumonia. A computed tomography [CT] angiogram of the pulmonary arteries was undertaken and excluded a pulmonary embolism. Patchy consolidation was noted, and the tip of the dialysis catheter was seen to lie in the right atrium. The patient remained well until four months later when flow through her dialysis catheter deteriorated. Urokinase infusion improved flows temporarily but the patient complained of worsening shortness of breath (SOB), dizziness, headaches, and flushing. The patient also noted intermittent swelling of her face and neck associated with the dyspnea but no orthopnea or paroxysmal nocturnal dyspnea. Standing up from a lying or sitting posture worsened the swelling and occurred despite the absence of any dependent edema or increases in her interdialytic weight gains. A chest x-ray showed the tunneled dialysis catheter in an advanced position (Figure 2).
And a subsequent CT pulmonary angiogram confirmed the position of the RIJ tunneled dialysis catheter crossing the tricuspid valve with the tip in the right ventricle (Figure 3).
She underwent a successful manipulation of the catheter under radiological guidance that resulted in the complete resolution of all the symptoms.
Discussion
Peripheral migration of the central venous catheters is a commonly documented event and is described in up to 17% on individuals after percutaneous catheter insertion [16,17]. However central migration to right atrium floor or right ventricle is extremely uncommon and not been described in terms of tunneled hemodialysis catheters. Such migration can lead to potentially serious complications of atrial mural thrombus, perforation, arrhythmias, and cardiac tamponade, as has been noted with central venous catheters outside the dialysis setting [6,7,18]. Symptoms of positional headaches, dyspnea and flushing have been attributed to advanced superior vena cava (SVC) obstruction [19] and have also been described in the context of positional SVC obstruction secondary to pacemaker implantation in the past [20]. However, SVC syndrome has not been described previously in relation to a hemodialysis catheter. Another unusual feature of this case is that symptoms only developed four months after the insertion of the hemodialysis catheter suggesting that the migration occurred only then. The time sequence suggests that either the anchoring of the tunneled catheter by fibrosis into the cuff had not taken place from the start or had broken down in that period. It is important to note that our patient did not develop any exit site, tunnel or line infections that could have contributed to the failure of the cuff tethering. In summary, our patient developed SVC syndrome because of the central migration of the hemodialysis catheter causing blockage of the blood flow across her tricuspid valve. The presence of the positional symptoms of worsening dyspnea, dizziness, headaches, flushing and/or facial swelling in hemodialysis patients with dialysis lines should raise suspicion of SVC obstruction prompting urgent investigations for thrombosis or line migration. In the case of malposition, timely manipulation or replacement of the migrated dialysis catheter will resolve the problem without sequelae.
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information:https://irispublishers.com/aun/fulltext/central-migration-of-tunneled-dialysis-catheter-into-right-ventricle-causing-positional.ID.000540.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
0 notes
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
Evaluation of metallic stents for malignant ureteral obstruction- a single institution experience
Authored by: Gupta A

Abstract
Introduction: Ureteral obstruction caused by extrinsic compression is commonly associated with intra-abdominal malignancy. Internal drainage with ureteral stents is typically the first-line therapy to relieve such obstructions. The limitation of polymeric ureteral stents in patients is that they get easily compressed and recurrence of obstruction is seen very quickly. The metallic stents were introduced to improve the patency rates of patients with chronic upper urinary tract obstruction, obviating the need for frequent stent exchanges. We report our clinical experiences with the use of metallic ureteral stents in the management of poor ureteral drainage due to extrinsic malignant obstruction/compression.
Materials and methods: In this study, we described the functional outcomes of a Resonance metallic ureteral stent in patients with malignant ureteral obstruction done during August 2016 till August 2018. Stent failure was detected by clinical symptoms, imaging studies, and renal function tests. The functional duration of each stent was calculated.
Results: A total of 27 stents were successfully inserted in 20 patients with malignant ureteral obstruction. After insertion of metallic stents, hydronephrosis subsided or remained stable in 89% of the ureteral units. Serum creatinine decreased or remained stable in 90% of these patients. In 15% ureteric units metallic stents were required to be removed or changed .The Resonance stent exhibited a mean increase in functional response at minimal 1year follow up.
Conclusion: Our results indicate that metallic ureteral stent placement is a technically feasible procedure with minimal complications, increased longevity and is well tolerated among patients.
Keywords: Malignant ureteric obstruction; Metallic ureteric stents; Polyurethane DJ stent; PCN
Abbreviations: MUO-Malignant ureteric obstruction; PCN- Per cutaneous nephrostomy; MRI- Magnetic resonance imaging; QOL-Quality of life
Introduction
MUO(Malignant Ureteric Obstruction) can result from extrinsic compression by a primary lesion, metastases, retroperitoneal lymphadenopathy or direct tumor invasion [1].The median life expectancy of patients with metastatic cancer that causes ureteral obstruction is generally less than one year [2]. Malignant ureteral obstructions require immediate ureteral drainage in order to salvage renal function [3]. Reduced renal function makes patient ineligible for chemo therapy or any additional treatment. Management options involve either PCN (Percutaneous Nephrostomy) or internal drainage with polyurethane stents. Conventional Polyurethane DJ stents have high failure rates and significant complications. PCN is commonly used as an alternative to DJ stent. PCN is more invasive than double-J stent insertion and have greater incidence of accidental tube dislodgement. The invasiveness of the procedure and the high incidence of tube dislodgement results in seriously compromised quality of life [4]. It also affects patient’s ambulation and mobility. Novel designs of ureteral stents made of different materials have been invented with the aim of achieving better drainage. Although segmental metal mesh stents initially seemed promising, the long-term results have not been satisfactory [2]. Full length metallic stents (Resonance stent) have been introduced for MUO management. Resonance is double-pigtail stent moulded from corrosion resistant alloy of Nickle, Chromium, Titanium, Molybdenum. It forms tightly coiled spiral with no end holes [1]. Secondary to their metal composition these stent have been shown to be more resistant to external compression than conventional polyurethane DJ stent [4]. We herein describe our initial experience with Resonance metallic stent in context of patient with MUO. As there are no end holes in metallic stent urinary drainage occurs through side of the stent, through the continuous ridge (Figures 1,2).
Materials and Methods
Retrospective study was conducted between Aug 2016 and Aug 2018. During this period we posted 45 patients presented with MUO to us in Ruby Hall Clinic, Pune. Out of these in only 27 patient retrograde guidewire insertion was possible and of these, only in 20 patients metallic stents (RES; Cook Urologic) could be inserted. In 7 patients, stents were inserted bilaterally. Thus total of 27 metallic stents were inserted. Patients were either newly diagnosed with MUO or had a prior diagnosis of same. Obstruction was diagnosed by clinical signs, increasing azotemia, or incidentally through routine cancer surveillance imaging. Diagnosis was confirmed with few of the following tests- ultra sonography, computed tomography, magnetic resonance imaging (MRI), and diuretic renal scintigraphy. Stents were inserted only if renal function was compromised. The decision to place metallic stents was based on patient is comorbidities, cancer prognosis, and need for additional chemotherapy [4]. After an initial cystoscopic examination of the bladder, retrograde pyelography was performed in all patients to define the obstructed ureteral segment. A hydrophilic glide wire was then negotiated past the point of obstruction and advanced into the kidney under fluoroscopic visualization. The metallic stent introducer system was then passed over the super stiff wire with the outer 8.3F sheath radio-opaque tip positioned at the UPJ. The wire and the inner introducer catheter were removed, leaving the outer sheath in place. The metallic stent was then placed through the sheath and advanced proximally using the previous introducer as a pusher. Importantly, the metallic stent does not have an inner lumen and is not passed over a wire. When the proximal curl of the stent is seen beyond the tip of the sheath in the renal pelvis, the sheath is slowly removed, keeping the inner catheter in place. The outer sheath is completely removed when the distal curl is seen deployed within the bladder. Finally, correct intravesical positioning is confirmed with cystoscopy, making any adjustments if necessary with flexible graspers. All patients were prospectively followed postoperatively for resolution of symptoms and azotemia. Patients were also assessed at 6 months with sonography to evaluate for hydronephrosis. Lastly, stent failures, complications, and mortality were recorded.
Results
Out of the total 45 patients stent insertion could be possible in only 20 patients, while 7 patients had done stenting bilaterally. Out of 20 patients 7 were men (35%) and 13 were women (65%). The mean age was 55.2±22.3 years. Cervical cancer was the most frequent type of malignancy (6 patients), followed by Bladder (4 patient) and colorectal cancer (3 patients). Bilateral stent was introduced in 3 patients of Ca cervix, 2 patients of Ca Bladder, 1 patient of CA prostate and 1 patient of colorectal carcinoma. After 1year of follow up, 18 patients (90%) were alive and 2Patients (10%) had died. The stent failure rate in our experience was 10%. This is because stenting resulted in failure to successfully relieve hydroureteronephrosis in 3 ureteral unit by metallic stent (3/27). Success rate of initial retrograde insertion was 60%, with no intraoperative complications. Urine culture sensitivity was performed within the first14 days post-operatively in all patients. 18 (90%) showed no infection, one Urine culture showed E. coli (patient with poorly-controlled diabetes) and one grew Pseudomonas aeruginosa (patient with an indwelling Foleys catheter). These required oral antibiotic treatment. In all patients sterile urine was confirmed later. Out of 27 inserted stents, 2 stents were removed due to worsening hydronephrosis and 1 stent was removed due to severe stent induced cystitis. Majority of stents (90%) successfully relieved or stabilized hydroureteronephrosis on subsequent imaging (ultrasound or CT or MRI). Success rate of stent was based on pre and post metallic stent hydronephrosis, serum creatinine level and symptomatic improvement (Table 1).
We have done metallic stent insertion only in terminally ill patients. Therefore our criteria for patency rate (success rate) also includes
1. No change of stent required till death of patient.
2. If patient tolerated stent with or without medical support.
Discussion
Deficiency in upper tract drainage is a frequent problem encountered in routine urologic practice today. Conventional approach in the management of chronic severe ureteral obstruction have been to place percutaneous nephrostomy drainage, PCN significantly decreases quality of life of the patient ailing from their malignancy [5]. In addition, polymer ureteral stents have been used but they had disappointing results due to the frequency of stent exchanges (approximately every 2- 3 months), stent encrustation, and external compression [5]. Failure rates for traditional polymer stents in the setting of malignant ureteral obstruction are estimated to be between 40- 60% [5]. Metallic ureteral stents have been studied in a limited number of retrospective studies. Published figures for stent failure from case series’ of greater than fifteen patients vary from 16–35% [6]. Our results show a failure rate of these stents of only 11 % exemplifying their clear benefit. Currently, metallic ureteral stents are indicated that they can be left in situ for up to 12 months and longer [5]. The use of metallic ureteral stents in the setting of deficient ureteral drainage obviates the need for an exchange. In addition, metallic ureteral stent placement procedures had minimal complications and were well tolerated by patients. Some patients complained of mild flank pain and/or dysuria directly after stent placement. This phenomenon was usually self-limiting, and probably due to expanding forces of the endoprosthesis [7]. Goldsmith et al. described subcapsular hematoma formation following metallic stent placement in 12% of their study cohort. They argued that this was likely “related to the excessive length of the inner cannula relative to the outer sheath in the supplied introduced system [8]. In our single institution study, we did not experience any such complications and recommend gentle manipulation of the upper tracts after properly done retrograde contrast studies during stent placement to avoid this issue. To help predict treatment success or failure, we based our research on previously published peer reviewed scientific literature. As previously shown by Ganatra et al., the type of underlying malignancy did not predict stent success or failure in our series [9]. Ganatra et al. also reported that gross tumor invasion noted at cystoscopy was a significant risk factor for stent failure and requirement of percutaneous nephrostomy (p = 0.008) [9]. It is also the most common cause in failure to insert guidewire. These bladders have a very low bladder capacity due to invasion by tumor, making guide wire insertion difficult due to poor vision. In addition, Goldsmith et al. reported that prostate cancer invading the bladder was a risk factor for stent failure [8]. Bladder invasion was not specifically assessed as a risk factor for stent failure in our study. Wang et al. also showed that patients who had received previous radiation therapy had a significantly lower stent patency rate than those who did not receive previous radiation therapy. They hypothesized that radiation therapy causes ureteral fibrosis and impairs ureteral peristalsis, ultimately leading to more encrustation and a smaller ureteral lumen [10-13]. Other studies nevertheless, have shown no difference in stent patency rates whether or not patients had received radiation therapy [6] (Table 2).
Table 1:Functional outcome of patient and metallic stent.
Table 2:Comparison of various study on metallic stent with our study in term of stent patency rate, complication, and management.
Metallic ureteral stents, when used in managing poor ureteral drainage, not only improved quality of life, but also is a cost-saving service. Despite the initial higher cost of the individual metallic stent versus traditional polymer ureteral stents, we report fewer surgical procedures (i.e. stent exchange) needed, which accounted for this cost difference. The overall cost reduction was estimated to be between 56.4% and 59.5% per patient/year, not taking into account other cost savings, including reduced post-operative office visits, fewer follow-up imaging studies, and any unforeseen operative complications [5]. We recognize several limitations to the present study, including the retrospective constitution of this single institution study design and smaller sample size. Whereas our database continues to expand, this is at a relatively slow rate given that metallic stenting is still on the whole reserved for a select group of patients. We hope that changing clinicians’ thinking through this critical analysis of the safety, efficacy and tolerability of this stent will lead to a larger number of patients being made eligible for these procedure.
Conclusion
Metallic ureteral stent placement is a technically feasible procedure with minimal complications and is well tolerated among patients. Metallic stents can be left in situ for longer durations. They provide a significant financial benefit when compared to frequent polymer stents replacements. Preference to metallic stent insertion instead of PCN also significantly reduces the morbidity and improves overall QOL of terminally ill patients.
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information:https://irispublishers.com/aun/fulltext/evaluation-of-metallic-stents-for-malignant-ureteral-obstruction.ID.000539.php
0 notes
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
Chronic Epididymo-Orchitis Mimicking Tuberculosis Turned Out to be Leprosy: A Case Report
Authored by: Mukesh Chandra Arya

Abstract
We report a 55-year male with a prior history of treatment for bilateral Epididymo-orchitis without relief. We thought of genitourinary tuberculosis (GUTB) or nonspecific Epididymo-orchitis as differentials. Suddenly he developed crops of lepromatous skin lesions. On reviewing the literature, we found the involvement of testes in leprosy in 60-90% of cases. However, urology literature and textbooks do not mention leprosy to be a differential diagnosis of orchitis or chronic Epididymo-orchitis. Therefore, testicular atrophy, infertility or chronic Epididymo-orchitis should make us consider the possibility of leprosy, considering the half of the global burden in India.
Keywords: Chronic Epididymo-orchitis; Testicular atrophy; Orchitis; Leprosy; Infertility
Abbreviations: GUTB: Genitourinary Tuberculosis; ED: Erectile Dysfunction; ENL: Erythema Nodosum Leprosum; MB MDT: Multibacillary Multi Drug Therapy; LUTS: Lower Urinary Tract Symptoms; UTI: Urinary Tract Infection; LH: Luteinizing Hormone; FSH: Follicle Stimulating Hormone
Introduction
The causes of chronic orchitis and Epididymo-orchitis are varied including, urinary tract infection (UTI), gonococcal or nongonococcal (chlamydia, ureaplasma) infections, genitourinary tuberculosis (GUTB), post-vasectomy and drug-induced. However, the Urology textbooks do not mention leprosy as a differential diagnosis in such cases [1]. Herein, we present a case of Epididymoorchitis caused by leprosy with a review of the literature. Leprosy is a chronic infectious disease caused by Mycobacterium leprae. Leprosy affects mainly the skin and peripheral nerves. Its diagnosis is established on the skin and neurologic examination of the patient. Involvement of testis and epididymis is well described in dermatology literature with an incidence ranging from 23.6% to 68.3% [2,3]. Testicular involvement is more in lepromatous leprosy and may result in infertility and impotence. However, practicing urologist does not keep this condition as a differential diagnosis and many such cases might remain undiagnosed. There are several classification systems validated for leprosy. The most commonly used Ridley & Jopling classification system (1966) is based on the concept of spectral leprosy and uses clinical, immunological, and histopathological criteria [4]. The spectrum consists of tuberculoid form at one end and the lepromatous form at the other end. The borderline form is divided into borderline-tuberculoid, borderlinelepromatous, according to the greater proximity to one of the poles, and borderline-borderline. Multi-Drug Therapy is the cornerstone of the treatment of leprosy.
Case History
A 55-year Hindu male, resident of Bikaner, Rajasthan, a farmer by occupation came with presenting complaints of scrotal swelling along with lower urinary tract symptoms (LUTS) and low-grade evening rise of temperature for 7 months. He initially consulted many clinicians and had treatment with antibiotics and antiinflammatory drugs without any improvement. He also had a loss of libido and erectile dysfunction (ED) (Sexual Health Inventory for Men score 8). He had completed his family with no history of extramarital contact. General physical examination was normal except low-grade fever. Local examination revealed left small testis (reduced sensation), bulky epididymis and right Epididymoorchitis with secondary hydrocele. There was no gynecomastia and he had male pubic hair pattern. Nonspecific Epididymo-orchitis and genitourinary tuberculosis were kept as differentials. He was investigated on these lines. His ESR was 38, total counts were 13000 with polymorphonuclear Leukocytosis. Uroflowmetry (Qmax 18ml/sec) was normal. Ultrasonogram suggested Bilateral epididymitis and testicular atrophy with left-sided hydrocele. Ultrasound abdomen did not pick up any mesenteric or retroperitoneal lymphadenopathy. During his hospital stay, he developed crops of erythematous, raised, painful, nodules with ulceration. Biopsy of skin lesion was taken which was suggestive of lepromatous leprosy(Figure 1).
After reappraisal, he was found to be a defaulter of multibacillary leprosy two years ago. Even at this stage, we did not suspect it to be due to leprosy. On reviewing dermatology literature leprous involvement of testis was suspected. Biopsy of testis and epididymis were then taken, which showed evidence of leprosy (Figure 2 and 3).
Levels of serum testosterone, luteinizing hormone (LH), folliclestimulating hormone (FSH) were 184.7ng/dl (249-836), 19.39IU/l (1.5-9.3), 23.13IU/l (1.4-18.1) respectively. The patient refused for semen analysis. He was started on multibacillary multi-drug therapy (MB MDT). Three to four days later he developed Erythema Nodosum Leprosum (ENL) which was managed with continued MB MDT and steroids. He improved and later discharged on MDT.
Discussion
Epididymo-orchitis, scrotalgia and orchitis are common urological ailments. Testicular involvement by leprosy is quite common, incidence ranging from 23.6% to 68.3% [2,3]. India accounts for half of the leprosy burden of the world. The average national child leprosy rate in India is 9% and borderline tuberculoid leprosy was the most common clinical type [5]. Trojian and colleagues have reviewed chronic epididymitis and orchitis without mention of leprosy as a differential [6]. Leprosy secondarily involves eyes, bones, lymph nodes and testes. Testicular involvement is most common, often bilateral and bloodborne. It affects both seminiferous tubules and interstitium leading to a rise in serum LH, FSH. The testes become small, firm with loss of sensation in advanced disease. Degenerated nerve fibres seen on histopathology explain diminished testicular sensation on palpation. The lower temperature of the organ is a proposed factor for the growth of M. leprae in testis [7]. Bilateral testicular atrophy results into loss of libido, infertility and impotence. Leydig cell degeneration along with liver changes could account for gynecomastia as liver takes an active part in inactivation of oestrogen. Liver biopsies may be done to document lepromata. Presence of bacilli in histopathology in Ziehl-Neelson smears is diagnostic as seen in our case. These bacilli are not seen if patients are on long term treatment [2]. Epididymal involvement in leprosy is uncommon, non-sexual and non-venereal in origin. Involvement is secondary to testis due to anatomical proximity and common vascular supply [8]. Infertility in leprosy is mainly due to the involvement of testis (85%) with epididymis being the cause in 10-15% [7]. On the contrary, infertility in tuberculosis results from epididymal obstruction.
Conclusion
While evaluating a case of testicular atrophy, chronic Epididymoorchitis, infertility, ED or gynecomastia leprosy should be kept in mind in endemic areas. Urology textbooks do not consider leprosy as a differential diagnosis.
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information: https://irispublishers.com/aun/fulltext/chronic-epididymo-orchitis-mimicking-tuberculosis-turned-out-to-be-leprosy.ID.000538.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
0 notes
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
Gender Differences in the Effect of Ascorbic Acid against petroleum fume-induced Oxidative Stress and Reproductive Toxicity in Rats
Authored by: Christopher Edet Ekpenyong
Abstract
Background: Biological factors affecting the therapeutic doses of ascorbic acid (AA) against xenobiotic-induced oxidative stress (OS) and reproductive toxicity have been established, however, the effect of gender is yet to be thoroughly researched and ascertained. The present study aimed to assess gender disparities in the effect of AA against gasoline vapor (GV)-induced reproductive toxicity in rats.
Methods: Thirty-five matured male and female Wistar Albino rats weighing between 200 and 250g were divided into 5 groups (n=7per group). Group 1 served as unexposed control, groups 2, 3, 4, and 5 were exposed to GV for 6 weeks. Groups 3, 4, and 5 in addition to being exposed to GV were treated with low, medium, and high doses of AA for 2 weeks of the 6 weeks of exposure and treatment. Animals were sacrificed and blood samples and reproductive organs were obtained for analysis and histopathological examination respectively.
Results: Exposure to GV alone significantly P<0.05 decreased serum estrogen, progesterone, and testosterone levels. Serum levels of estrogen and progesterone were significantly (P<0.05) higher in the low-dose AA-treated female animals, whereas the highest serum level of testosterone was found in the high-dose AA treated male animals. A corresponding significant decrease in serum FSH and LH levels were also found in the low and high doses of AA treated female and male groups respectively.
Conclusion: There is a gender difference in the effect of AA against GV-induced OS and reproductive toxicity. Therefore, gender-related dose adjustment should be considered when using AA to manage OS-related male or female reproductive disorders.
Keywords:Petroleum fume; Vitamin C; Gender; Oxidative stress; Reproduction; Toxicity
Introduction
Gasoline consists of several hydrocarbons and additives that constitute significant environmental pollutants. Exposure to hydrocarbon fumes by humans is common and widespread due to the extensive domestic and industrial applications. Exposure by humans can be through dermal, inhalation, or ingestion routes, with inhalation being the most common exposure route and can occur at any point along the production and distribution chain. Many people are exposed to petroleum fumes daily, especially those whose residence or workplace is close to petrochemical industries, refineries, oil fields, gasoline refueling stations, trafficcongested areas and gasoline combustion stations. About 100 million people are exposed to hydrocarbon constituents of gasoline per week when refueling at a self-service gasoline station [1]. Also, gasoline service station attendants are at a higher risk of exposure to gasoline inhalation for many hours a week and about 8086 minutes per year. Available data indicate that >3.6 billion gallons of gasoline vaporize into the air as gasoline vapor (GV) [2]. Following inhalation, GV is absorbed and distributed in the body. Within the body, it undergoes further toxicokinetic processes leading to the generation of reactive oxygen species (ROS), oxidative stress (OS), Gasoline consists of several hydrocarbons and additives that constitute significant environmental pollutants. Exposure to hydrocarbon fumes by humans is common and widespread due to the extensive domestic and industrial applications. Exposure by humans can be through dermal, inhalation, or ingestion routes, with inhalation being the most common exposure route and can occur at any point along the production and distribution chain. Many people are exposed to petroleum fumes daily, especially those whose residence or workplace is close to petrochemical industries, refineries, oil fields, gasoline refueling stations, trafficcongested areas and gasoline combustion stations. About 100 million people are exposed to hydrocarbon constituents of gasoline per week when refueling at a self-service gasoline station [1]. Also, gasoline service station attendants are at a higher risk of exposure to gasoline inhalation for many hours a week and about 8086 minutes per year. Available data indicate that >3.6 billion gallons of gasoline vaporize into the air as gasoline vapor (GV) [2]. Following inhalation, GV is absorbed and distributed in the body. Within the body, it undergoes further toxicokinetic processes leading to the generation of reactive oxygen species (ROS), oxidative stress (OS),
Materials and Methods
Experimental Animals
Thirty-five mature Wistar Albino rats weighing between 200 and 250g were obtained from the animal house of the Department of Pharmacology, Faculty of Pharmacy, University of Uyo, Akwa Ibom State, Nigeria. They were kept in well-ventilated cages for 7 days to acclimatize. They were allowed access to food and water ad libitum. All animals were fed rat chow (Vital Feeds, Grand Cereal Ltd, Jos).
Segregation of Animals
The animals were randomly divided into 5 groups (n=7 per group). They were exposed to GV in the exposure chambers (60 x 80x 100cm3)
Group 1 served as unexposed control and was orally gavaged 2ml of normal saline for 6wks.
Group 2 was exposed to GV alone for 6wks and maintained on normal animal feed.
Group 3 was exposed to GV for 6wks, fed a normal diet, and orally gavaged 100mg/kg of AA for 2 wks of the 6wks.
Group 4 was exposed to GV for 6wks, fed a normal diet, and orally gavaged 200mg/kg of AA for 2 wks of the 6wks.
Group 5 was exposed to GV for 6wks, fed a normal diet, and orally gavaged 300mg/kg of AA for 2 wks of the 6wks.
Collection of experimental samples for analysis
After 2 weeks of AA administration, the animals were weighed and anesthetized with chloroform soaked in a swab of cotton wool in a desiccator. The blood sample was collected by cardiac puncture and emptied into labeled specimen bottles, for biochemical evaluation including determination of estrogen, progesterone, follicle-stimulating hormone (FSH), Luteinizing hormone (LH), testosterone level, catalase (CAT), and malondialdehyde (MDA) levels. Animals were sacrificed by cervical dislocation and reproductive organs testis and ovary were carefully removed and fixed in a suitably treated formalin reagent and thereafter, subjected to normal routine histological procedures/examination.
Biochemical Analysis
Estimation of CAT and MDA activities
CAT activity was determined by the Titrimetric method. Tissue lipid peroxidation was quantified by estimating the plasma concentration of MDA using the thiobarbiturate acid reactive substance (TBARS) method and measured spectrophotometrically at 532nm. Serum estrogen, progesterone, testosterone, LH, and FSH levels were determined by Enzyme-Linked Immuno-sorbent assay (ELISA) as described by Tietz [7].
Histopathological tissue processing
The fixed tissues were dehydrated in different grades of alcohol as follows; two changes of 70% and 95% alcohol for a period of 2hrs each, two changes of 100% also known as absolute alcohol for a period of 2hrs. Dehydrated tissues were cleared using xylene. Tissues were impregnated with two changes of paraffin wax in the oven at the temperature of 60°C for 1hr 30mins) each to ensure they were fully embedded. Tissues were transferred from the final wax bath to molds filled with molten wax, allowed to solidify and thereafter, properly oriented for sectioning. The paraffin block was sectioned at 5μm after cooling the surface of the tissues with an ice bar. Ribbons were gently picked with Carmel brush and dropped in a water bath containing water at 60°C to enable ribbons float, expand and flatten out. Slides were rubbed with thymol containing egg albumen and gently dipped into the bath to pick up the flattened out tissue ribbons [8]. Haematoxylin and Eosin (H&E) staining techniques [8] were applied in staining the tissue sections.
Haematoxylin and eosin staining procedures
Tissue sections were deparaffinized in two changes of xylene and hydrated through graded series of alcohols in descending order and were rinsed in water and stained with Haematoxylin for 10mins. Tissue sections were rinsed and differentiated in one percent (1%) acidic alcohol and blued in running water using saturated lithium carbonate solution until sections appear sky blue. The blued section was counterstained in the Eosin solution for 3mins. Tissues were washed in water and dehydrated in ascending grades of alcohol, cleared in xylene, and mounted in DPX covered with coverslips and observed under the microscope.
Microscopy
Processed slides were viewed under a light microscope at magnification (X400), and photomicrographs obtained were linked to the computer using the microscope’s camera.
Statistical Analysis
Statistical analysis was carried out using Statistical Package for Social Sciences (SPSS), version 20.0, and M. S. Excel. The one-way analysis of variance (ANOVA) and posthoc Tukey least significant difference (LSD) test was used to analyze the data and to determine the significance respectively. Data are expressed as Mean + Standard Error of Mean (S.E.M) and tables were used to illustrate the variations in the numerical values across the experimental groups. The P. values <0.05 were considered statistically significant.
Results
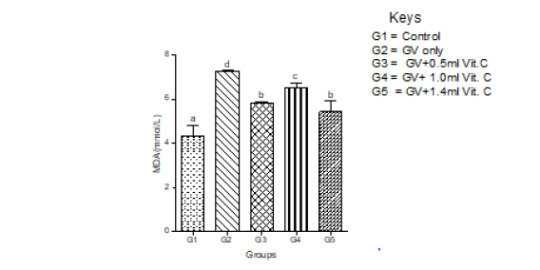
Antioxidant activity
Serum MDA increased significantly in GV alone group and decreased significantly (P<0.05) in a dose-independent manner in both male and female animals. In female animals, serum MDA significantly (P<0.05) increased in GV alone group, and significantly (P<0.05) decreased in GV plus low dose AA compared to the gasoline alone, group. Interestingly, serum CAT decreased significantly (P<0.05) in GV plus a medium and high dose of AA compared with the GV alone group (Figures 1-4).
Serum estradiol level
Means serum level of estradiol significantly (P<0.05) decreased in the GV-alone group compared with the control group. Estradiol significantly increased in GV plus low, medium, and high doses compared with the GV-alone group. The highest increment occurred in the group treated with low-dose of AA (Figure 5).
Serum follicle-stimulating hormones (FSH) level
Exposure of the female animals to GV-alone caused a significantly (P<0.05) decreased in serum FSH compared with normal control, whereas in male animals exposed to GV had a nonsignificant (P<0.05) changes in serum FSH compared with normal control. Also, the highest ameliorative effect of AA was obtained from the highest dose in female whereas, in the male animals, it was the medium dose that produced the highest ameliorative effect (Figure 6,7).
Serum luteinizing hormone (LH) level
In female animals, there was no significant (P>0.05) difference between the serum level of LH between the GV alone and the normal control. In the male animals, a significant (P<0.05) decrease in serum LH compared with the normal control was observed. In both sexes, medium doses of AA produced the highest protective effect on serum LH (Figure 8,9).
Serum progesterone level
Exposure to GV significantly (P<0.05) decreased in serum progesterone low dose of AA produced a significantly increased in serum progesterone level compared with normal control. Medium and high doses caused a significant (P<0.05) decrease in serum progesterone (Figure 10).
Serum testosterone level
Exposure to GV caused a non-significant decrease in serum testosterone levels compared to levels in the normal control group. The highest dose of AA produced the highest ameliorative effect on the GV-induced decrease in serum testosterone levels (Figure 11).
Figures 12 to 26 show the changes in the histomorphology of the ovaries (Figures 12-16), testis (Figures 17-21), and epididymis (Figures 22-25) following the exposure to GV, and concomitantly treated with AA. Similar to the changes in the biochemical markers of ovarian and testicular endpoints, a greater improvement in the ovarian histomorphology was found in the low dose AA-treated group, whereas the testicular and epididymal histomorphology showed greater improvement in the high dose AA-treated groups (Figure 12-26).
Discussion
The present study findings revealed that exposure to GV is associated with a significant alteration in OS status and reproductive system dysfunction in male and female rats. Accordingly, animals exposed to GV and concomitantly treated with different doses of AA showed dose-dependent beneficial or detrimental effects. For instance, serum levels of estrogen and progesterone in female animals were significantly higher in the group treated with low dose of AA. In contradistinction, male animals treated with the high dose of AA had the highest serum testosterone levels. Interestingly, the increase in serum progesterone and estrogen levels caused a corresponding decrease in serum levels of FSH and LH due to the negative feedback effect of the increased serum levels of the female sex hormones on the gonadotrophin-releasing hormone system. Also, improvement in the ovarian histomorphology following treatment with AA was more in the low-dose than the high-dose AA-treated female animals, and vice versa in the male group. Furthermore, serum CAT level increased, while serum MDA level decreased in the low dose AA-treated female animals. Whereas, male animals treated with a high dosage of AA had similar effects, demonstrating the gender-related heterogeneity in effects of AA. These findings are consistent with the results of a study conducted by Al-tib et al. [9], which showed that animals treated with a low dose of AA had a better ameliorative effect against potassium permanganate (KMno4)-induced ovarian dysfunction and OS including, improvement in the diameter of the ovary, corpus luteum, and graffian follicles as against the high dose AA-treated group with the least increment in the diameter of these structures. Besides the dose-dependent effect of AA against xenobiotic-induced ovarian dysfunction, the duration of treatment also showed an inverse relationship with the ovarian endpoints in previous studies. The acute treatment produced a higher protective effect on the ovary than chronic treatment. Accordingly, in a study to assess the action of AA on ovarian function of aging mice, Mohammad-Amin et al. [10] observed that acute treatment with AA produced a more beneficial effect on some reproductive endpoints than chronic treatment. Acute treatment of animals with AA (8 days) caused a better improvement in the volume of oocytes in the antral follicle, increased in the number of granulosa cells, primordial cells, secondary follicles, antral follicles, and primary follicles than those treated for 12 or 33 weeks. Also, a high dose of AA caused a decrease in serum superoxide dismutase (SOD) in granulosa cells. Similarly, Ismiyati et al. [11] studied the effect of combined AA and vitamin E against depot-medroxyprogesterone acetate (DMPA)-induced ovarian OS in rat and found that animals treated with the lowest dose of AA had a better ameliorative effect against DMPA-induced decrease in ovarian weight and SOD activity than the animals in the high dose AA treated group. Also, AA in its lowest dose significantly prevented DMPA-induced increase in MDA concentration in the ovarian tissue better than the group treated with the high dosage of AA. In the present study, female animals treated with a low dose of AA had the highest serum CAT and the least serum MDA, similar to males treated with the high dosage of AA. Furthermore, a study to assess the effect of AA on serum oestradiol in postmenopausal women reported that those who had the lowest plasma concentration of AA at baseline had the highest increment in plasma oestradiol level [12]. Also, one month of treatment with AA caused a significantly higher serum level of ovarian endpoints than three months of treatment. Convincing evidence indicates that the effect AA on plasma estrogen level was mediated by the synergistic antioxidant activities that provided a better antioxidant action than either of them alone, supporting the notion that antioxidants act as a cooperative network [13]. The contrary effects observed in the male group are similar to those of a plethora of research conducted to assess the action of AA on male reproductive performance in heterogeneous OS-related environments. Similarly, Sanghishetti et al. [14] found a better increase in indices of male reproductive function (testicular weight, seminiferous tubules weight, sperm count, and testosterone level) in the high dose AA-treated group than the low dose AA- treated group. Sperm concentration, sperm motility, and serum levels of testosterone and FSH were significantly higher in the high dose AA-treated group than the low dose AA treated and control groups in a study to assess the effect of AA on fertility parameters in male rats [15]. These findings are in good agreement with the bimodal characteristics of AA postulated by Schwartz [16]. A plausible explanation for the observed inverse correlation between the therapeutic dose and effect of AA on female reproductive endpoints may be because the female reproductive system naturally is endowed with efficient antioxidant systems. For instance, the ovaries have a rich and efficient antioxidant system made up of a non-enzymatic antioxidant (vitamin A, C, and E), and an enzymatic antioxidant (tripeptide glutathione, glutathione peroxidase (GPX), SOD, and CAT) [10, 17- 21], as well as estrogen the hormone of the female reproductive system has been shown to display an efficient antioxidant prowess. According to Bostanci et al. [13], there is a strong correlation between estrogen status and serum antioxidant capacity. These observations suggest that AA, when applied in low dosage, may provide a better protective effect against xenobiotic-induced reproductive dysfunction in females than the high dose treatment regimen. These could probably be because the low dosage of exogenous AA synergized with the rich ovarian antioxidant system to produce a synergistic/additive effect that plays a more antioxidant role than the high dosage of exogenous AA. Also, AA has a peak or maximum therapeutic serum/tissue concentration beyond which the efficacy declines. Earlier studies have observed that the ovary is the site of AA accumulation and turnover. The highest concentration of AA is present in the theca interna, granulosa, and corpus luteum. The follicular fluid has more AA than the serum, suggesting that the AA enters the follicular fluid against the concentration gradient by active transport [22,23]. Likely, the transport mechanism for AA is more effective at a low concentration of AA in the females and vice versa in the male animals. It is also a known fact that in a persistent OS as found in the present study, a critical serum concentration of ascorbate radicals is required to attend the highest effect, after which a steady decline ensues. This notion is in line with the theory of antioxidant paradox/or overuse that states that excessive use of antioxidants or an antioxidant combination may lead to reductive stress [24] that produces an effect similar to oxidative stress and is associated with some disease conditions including, cancer and cardiomyopathy [2]. Available evidence indicates that AA in very high concentrations can act as a pro-oxidant but behaves as an antioxidant in therapeutic doses [6]. Currently, there is a debate as to the best effective dose regimen of AA in terms of the amount and duration of intake for maintaining optimal health in humans. Accordingly, Chakraborthy et al. [6] studied the beneficial effects of AA in human health and disease and postulated that at high dosage, AA could behave as an antioxidant under physiological conditions, but switch over to a pro-oxidant under pathological condition, a view supported previously by Naidu [25].
Conclusion
Given the findings of the present study, it seems reasonable to opine that there is a gender difference in the effective dose of AA against xenobiotic-induced OS and reproductive toxicity. Therefore, gender-related dose adjustment is required when using AA to manage OS-related male or female reproductive disorders. This novel observation is of clinical and public health importance as the wrong dosage or prolongs therapy with AA can worsen a preexisting xenobiotic –induced OS and reproductive toxicity.
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information: https://irispublishers.com/aun/fulltext/gender-differences-in-the-effect-of-ascorbic-acid-against-petroleum-fume.ID.000537.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
1 note
·
View note
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
Traumatic Bulbar Urethral Stricture: Improvised Reconstruction with Muscle and Nerve Sparing Approach
Authored by: Mukesh Chandra Arya

Introduction
Bulbar urethra is the most common site of the stricture (46.9%). Meta-analysis of anterior urethral strictures showed etiology as iatrogenic (33%), idiopathic (33%) and, to a lesser extent, trauma (19%) and inflammation (15%). End-to-end anastomosis is the most valid treatment of choice for short bulbar traumatic urethral strictures, with cure rates close to 100% [1,2]. Bulbospongiosus muscle which covers bulbar urethra is primarily responsible for last few drops of urine and semen expulsion. Ejaculatory dysfunction (EjD) and post-void dribbling are common postoperative complications after muscle cutting bulbar urethroplasty in 23.3% and 29% patients, respectively. Here, we used a modified technique of sparing muscle and nerve to avoid these sequelae.
Material and Methodology
A retrospective analysis of 55 patients (January 2015 to January 2019) with traumatic bulbar stricture was done. Patients with post-inflammatory or with prior catheterization (without trauma) were excluded from the study group. In our department, retrograde urethrogram (RGU) is not done at the time of trauma. Based on the history of perineal trauma with blood at meatus, a presumptive diagnosis of bulbar urethral injury was made and trocar Suprapubic Cystostomy (SPC) was done. RGU and micturating cystourethrogram (MCU)were done at 3 months after injury. In cases with normal urethrogram, the trauma was presumed to be contusion. Such patients who voided well after clamping SPC were excluded. Those who had complete or near obliterative stricture were taken up for this study. Patients were asked about their complaints of post-operative EjD during their follow-up using 5 questions from MSHI (Male Sexual health questionnaire score) pertaining to ejaculation including frequency, volume, force and bother and compared with their pre-operative scores. Also, patients were asked “If they wet their undergarments after passing urine” to ascertain post-void dribble. Statistical analysis between these groups was done using IBM SPSS 25.0. From January 2015 to February 2017, all 30 patients were operated by standard muscle cutting technique (Group 1) and later on, 25 patients by modified muscle and nerve-sparing technique (Group 2). Surgical technique: Detailed history, blood investigations including complete blood count, serum creatinine and ultrasound abdomen was followed by RGU and MCU. Under anesthesia, antegrade and retrograde urethroscopy showed complete cut off at the level of the bulbar urethra. With the patient in the lithotomy position, midline perineal incision was given.
Standard technique: Bulbospongiosus muscle was divided in the midline. The bulbar urethra was mobilized up to the penoscrotal junction. Stricturous segment was identified and excised. A few interrupted 4/0 chromic catgut sutures were taken radially to tack the mucosa to the urethral wall and prevent retraction during the anastomosis. Proximal and distal urethral segment were spatulated at 6’o clock and 12’o clock respectively. End to end anastomosis was done over 14 Fr Silastic Foleys catheter using 4-0 polyglycolic acid(PGA) and drain was put before layered closure. The drain was removed on post-operative day 2 and Foleys catheter on day 21.
Modified technique: The perineal branch of the pudendal nerve is damaged during dissection of bulbospongiosus muscle which cannot be restored by suturing the muscle. So bulbospongiosus muscle was carefully separated from the corpus spongiosum by sharp dissection leaving the lateral margins of the muscle and central tendon of perineum intact. To expose the bulbar urethra, the muscle was pulled down using two small right-angle retractors (Figure 1).
The scarred urethra was excised and both ends were spatulated as in the standard technique. The proximal urethral segment was sutured to corpora at 11,12 and 1’O clock, followed by an end to end anastomosis. Ventrally thick corpus spongiosum was sutured in two layers from 3 – 9 o’clock with continuous 4-0 PGA suture over 14 F Silastic Foleys catheter (Figure 2).
This establishes early vascular continuity in corpus spongiosum and achieves better healing. The closure was done as in the standard technique. Prophylactic 3rd generation cephalosporin and amikacin were given for 3 days. Postoperative uroflowmetry was done at 6 weeks and RGU was done at 6 months (for documentation) in all patients. Patients were followed up for a period of one-year and were asked about their EjD and post-void dribble. Failure was considered if the patient had symptoms post-operatively or required an ancillary procedure. The patient was considered cured in the absence of symptoms and not needed any intervention.
Results
Age: ranged from 11 to 55 years with the mean age 31.12 years (Table 1).
Table 1:Age at operation.
Presentation: One patient (Group 1) presented with periurethral abscess following catheterization after trauma. SPC and drainage of the abscess was done. Rest of the patients were managed with immediate SPC followed by MCU and repair at three months.
Duration: The mean duration of surgery was 65 (54-74) minutes in Group 1 and 70 (58- 84) minutes in Group 2.
Length of stricture: Mean length of the stricture was 1.41 cm in our series. Length of the stricture was 1.47 and 1.36cm in Group 1 and 2 respectively.
Postoperative uroflow: Uroflow was done at 6 weeks and overall Mean Qmax was 23.036 ml/s (Table 2).
Results: Success rate (patient not needing post-operative intervention) was 100% in modified and 96.66% in standard urethroplasty group.
Post-operative EjD: EjD was evaluated by asking patients questions about frequency, volume, force and bother related to their ejaculation. Questions were framed from MSHQ (MSHQ5, MSHQ7, MSHQ8, MSHQ9, MSHQ12). Group 1 and Group 2 patients had a significant difference in their score pertaining to EjD and P-value was highly significant (Table 3, Figure 3).
Table 2:Post-operative Mean Qmax.
Post- void dribbling: Post-void dribble was seen in 10 patients (33.3%) in the standard group and 1 patient (4%) in the modified group (P-value 0.007).
Complications: None of the patients had a fistula. Only 1 patient (3.33%) with a prior history of catheterization and periurethral abscess had a stricture recurrence in the standard group. The success rate for our technique was 100% in this small series of patients operated by the modified technique. No patient had any intraoperative complications or required blood transfusion.
Wound infection: Three patients (10%) in Group 1 and two patients (8%) in Group 2 had wound infection respectively. All were managed conservatively with success. P-value (0.797) was not significant.
Discussion
Traumatic bulbar urethral strictures are usually of short length associated with intense spongiofibrosis. Therefore, such strictures are rationally managed with anastomotic urethroplasty rather than direct visual internal urethrotomy (DVIU) or augmentation. Immediate SPC, with delayed perineal anastomotic urethroplasty, remains the gold standard treatment. Bulbospongiosus is a paired muscle that covers the bulbar urethra. The rhythmic contractions of these muscles are responsible for the expulsion of semen and urine especially the last few drops. The perineal nerve (a branch of the pudendal nerve) innervates bulbospongiosus and ischiocavernosus muscles. Ejaculation may be disturbed by damage to the nerve and may result in a low volume of semen [10,11]. This nerve is damaged during dissection of bulbospongiosus muscles which can’t be restored by approximating the muscles in midline. The success of urethroplasty is not only related to stricture recurrence but also to the impact on the erectile and EjD in addition to postvoid dribbling. Muscle sparing urethroplasty technique was initially described by Barbagli et al as a modification of the standard technique to decrease the occurrence of these complications [12]. The bulbar urethra is elastic and can be mobilized from its attachment allowing to bridge a gap of 2 – 3 cm at the stricture site. Additionally, 1 cm of this length is lost in spatulation of proximal and distal urethral segments on either side. The bulbous urethra also offers other characteristics that make it particularly suitable for urethroplasty:(i) the mucosa is well-differentiated and more abundant than the spongiosa, so can be anastomosed on two planes, i.e. mucosa-mucosa and spongiosa-spongiosa; (ii) the spongiosa is thick and wellvascularized, with an adequate blood supply. This reduces the risk of ischemia and secondary fibrosis, limiting the likelihood of recurrent stricture [9,13]. Moreover, postvoid dribbling and semen sequestration will likely be post-operative complications following any bulbar urethroplasty. EjD was described as difficult, slow seminal ejaculation or poor semen volume observed by the patient. Unmarried patients experienced EjD during masturbation. EjD and postvoid dribbling are very annoying complaints requiring manual compression of the bulbar urethra and compromising their quality of life despite the success of urethroplasty. Modified Bulbar urethroplasty with muscle and nerve-sparing aims to preserve these functions in a significant number of cases. The three-suture technique keeps the anastomosis open and reduces the recurrence of stricture. Two-layered closure of ventral corpus spongiosum establishes better blood supply and hence, sound healing. Most astonishingly on post-operative RGU, we were not able to localize the site of anastomosis due to these modifications (Figure 4- 6).
Preservation of bulbospongiosus muscles and perineal nerves is advisable as they are involved in the expulsion of urine and semen from the bulb. The main limitation of end to end urethroplasty is the length of the stricture. If tried to bridge a longer gap, it may result in ventral curvature of the penis, and the anastomosis will be under tension with risk of failure [14]. In our series, stricture length ranged from 1 to 2 cm (mean-1.42 cm) and surgery outcomes were successful in 100% and 96.66% with Group 2 and 1 respectively. Similarly, Jun-Gyosuh et al. [15] found no recurrences in his series of 18 cases of end to end anastomoses. Elgammal MA [16] had 96% success rate in 24 out of 25 patients in post-traumatic bulbar urethral strictures. The age at presentation in this study ranged from 11 to 57 years with the mean age 31.4 years. the mean Qmax in our study was 23.04 ml/s while in the study by lumen et al. mean postoperative Qmax was 26.9 mL/s. Most of his patients were between 15 – 25 years. The results in our study confirm that patient age is not a factor in the success of the procedure and even old patients should not be denied surgery as observed by Barbagli et al. [17]. In our study, 2 patients had postvoid dribbling in Group 2 while no postvoid dribbling or semen sequestration was demonstrated in another study by Barbagli et al. [12]. Elkady E et al. [18]. also found that nine (36%) and 1 patient (4%) from muscle cutting and muscle-sparing group complained of postvoid dribbling with statistically significant difference between the two groups respectively (P=.01). EjD was evaluated by asking patients questions about frequency, volume, force and bother related to their ejaculation. Questions were framed from MSHQ (MSHQ5, MSHQ7, MSHQ8, MSHQ9, MSHQ12). Group 1 and Group 2 patients had a significant difference in their score pertaining to EjD and P-value was highly significant. Patients had a significant difference in each question of MSHQ related to ejaculation (frequency, volume, force and bother; p-value<0.005). Ariel Fredrick et al. [19] did a comparative study between muscle cutting and muscle-sparing urethroplasty (25 cases in each arm) for non-obliterative bulbar urethral stricture. They evaluated their results in terms of EjD and post-void dribble and found no significant difference. The plausible reason is that a significant number of their patients had preoperative EjD and post-void dribble in each arm due to stricture and these symptoms rather improved after surgery. Therefore, this study is not comparable to ours. We in our study did not come across any recurrence over a follow-up period of one year in the modified group, however1 patient had a recurrence in the standard group while in the study of Barbagli et al. [12], no patient had stricture recurrence. He had a history of catheterization after trauma and periurethral abscess. This resulted in long segment stricture and significant periurethral fibrosis. In such cases, muscle-sparing urethroplasty is not possible. Any attempt at catheterization in such patients can convert sterile hematoma into abscess and tissue loss. Prolonged catheterization may cause longer or even pan urethral stricture, making subsequent reconstruction difficult. This signifies the importance of urinary diversion rather than catheterization after urethral injury. This recurrent stricture was managed by redo-urethroplasty at 6 months. However, Elkady E. et al. found 3(12%) and 2(8%) recurrences in his study from muscle cutting and muscle-sparing group.
Conclusion
Standard anastomotic urethroplasty for traumatic bulbar stricture has a high success rate. However, a significant number of cases have bothersome post-void dribble and EjD despite successful urethroplasty. The three-suture technique with two-layered ventral spongiosal anastomosis resulted in indistinguishable suture line in post-operative RGU. Muscle and nerve-sparing technique showed statistically significant better results in terms of EjD and post-void dribble. This approach is, therefore, recommended in all cases of traumatic or inflammatory bulbar urethroplasties [17]. Patients with urethral injury are best served by a suprapubic diversion of urine and urethral rest rather than urethral catheterization.
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information: https://irispublishers.com/aun/fulltext/traumatic-bulbar-urethral-stricture-improvised-reconstruction.ID.000536.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
1 note
·
View note
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
Wishing You A Happy Thanksgiving Day!!!
It’s time to wish on the occasion of Thanksgiving Day for everyone on behalf of Journal Name . We Wish you Happy Thanksgiving Day to you and your family!!!

2 notes
·
View notes
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
Extra Scrotal Spermatocele – A Unique Case Presentation & Brief Review of literature
Authored by: Iqbal Singh
Abstract
Background: Spermatoceles are extra testicular lesions caused by cystic dilation of the efferent ductules filled with clear/milky fluid containing spermatozoa usually diagnosed incidentally either as a scrotal swelling or by ultrasonography. Suspecting and diagnosing spermatoceles presenting at extra scrotal positions is extremely rare and very few cases have been described in literature thus far. This article attempts to depict a patient presenting with one such spermatocele at an unusual location which adds to the scarce literature on the subject.
Case Presentation: A 60-year-old male presented with complaints of a gradually progressing left inguinal swelling for past 3 months with prior trivial scrotal trauma. Clinical evaluation and investigations revealed a 5 × 3 cm inguinal swelling extending up to the superior aspect of the left hemiscrotum that was confirmed as a spermatocele on pathological analysis at an unusual extra scrotal location.
Conclusion: Spermatoceles presenting at extra scrotal locations are extremely rare occurrences as is evident by the scant available published literature. This report adds to the scarce literature and also alerts the practicing urologist/surgeon towards insisting on a complete physical examination including simple but effective examination techniques like the transillumination technique as an aid to diagnosis of spermatoceles that may present uniquely at uncommon (extrascrotal) locations as in the present case.
Keywords: Extrascrotal; Inguinal; Spermatocele; case report
Abbreviations: FNAC: Fine Needle Aspiration Cytology; OPD: Outpatient Department
Introduction
Spermatoceles are usually asymptomatic and rarely cause clinical problems like disturbing pain and infertility. Self -examination and physical examination are the most common ways spermatoceles are detected. They are frequently seen on scrotal ultrasound as an incidental finding usually being located within scrotum cephalic and occasionally posterior to the testis [1]. Case reports of spermatoceles presenting at unusual locations are extremely rare with an extensive literature search revealing only 3 such cases which are depicted in Table 1 [2-4]. This case hence adds to the scarce literature on spermatocele with unusual presentations (Table 1).
Case Presentation
60-year-old male presented to surgical OPD with complaints of a gradually progressing painless left inguinal swelling for 3 months following history of trivial blunt scrotal trauma without any urinary/ sexual complaints. The patient was initially managed as a case of chronic epididymitis by a private practitioner with medications and reported to our clinic due to lack of improvement from the prior treatment. Physical examination revealed approximately 5 × 3 cm inguinal swelling extending up to the superior aspect of the left hemiscrotum (Figure 1). Bilateral testicular, scrotal, and abdominal examination was unremarkable. Ultrasonography suggested a hypoechoic lesion with low-level echogenicity and irregular walls abutting the left testis with superior extension into the inguinal region (Figure 2). FNAC of the cystic lesion revealed clear fluid with mature spermatozoa that confirmed the diagnosis of a spermatocele with predominant extra scrotal location (Figures 1,2).
Discussion
Spermatoceles are extra testicular lesions caused by cystic dilation of the efferent ductules filled with clear/milky fluid containing spermatozoa. They are generally found incidentally as single, unilateral, and mostly asymptomatic swellings [5]. The exact aetiology of spermatocele still remains obscure with the proposed hypothesis being shedding of senile seminiferous cells leading to obstruction and dilatation of the efferent ducts [6]. Spermatoceles are well characterized on ultrasonography, appearing as hypoechoic lesions with posterior acoustic enhancement and confirmed by Fine needle cytology which reveals cyst fluid-filled with mature spermatozoa [7]. Most spermatoceles are managed conservatively unless they are persistently symptomatic or when they trigger doubts of malignancy in which case they are managed by spermatocelectomy. Sclerotherapy using ethanolamine oleate forms another effective and safe therapeutic alternative to surgery with minimal side effects and low recurrence. Sclerotherapy in younger men is avoided owing to the danger of epididymitis and resulting infertility [8]. The patient was managed conservatively owing to a lack of distressing symptoms with FNAC proving partially therapeutic causing more than 50% reduction in swelling size and is currently on periodic clinical follow-ups.
Conclusion
Spermatoceles occurring at extra scrotal locations are extremely rare occurrences as is evident by the scant published literature. This report adds to the scarce literature and serves to alert the practicing urologist-surgeon to maintain a vigilant eye for abnormal presentations of a common disease by persistent usage of simple but effective physical examination techniques like the transillumination technique and scrotal ultrasonography which must be considered in the examination of all inguinal/ inguinoscrotal swellings keeping extra scrotal spermatoceles in the list of differential diagnosis.
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information:https://irispublishers.com/aun/fulltext/extra-scrotal-spermatocele-a-unique-case-presentation-brief-review-of-literature.ID.000535.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
1 note
·
View note
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
Surgical Options for Post-Prostatectomy Incontinence: A Review
Authored by: Alixandra Ryan
Abstract
Introduction: Post-prostatectomy incontinence affects anywhere from 1-40% of men after a radical prostatectomy, but treatment is often delayed and surgery is underperformed.1 Currently, the American Urological Association (AUA) and Society of Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction (SUFU) recommends post-prostatectomy patients are offered conservative therapies including pelvic floor muscle training in the immediate post-operative period, and surgical treatment may be offered to those who have confirmed stress incontinence (SUI) and fail to respond to conservative therapies. Surgical treatment options are based on the degree of stress urinary incontinence. The artificial urinary sphincter is typically recommended for moderate to severe SUI, while the male sling can be considered in those with mild to moderate SUI.2 However, the AUS is considered a more reliable treatment, particularly for severe SUI after prostatectomy.
Methods: The study was conducted using the PubMed database for recent papers between 2001 and 2020 with variations of phrases such as post-prostatectomy incontinence, treatment, AUS, male sling [1]. articles were selected for review. The AUA/SUFU guidelines for incontinence after prostate treatment were also referenced.
Results: The AUS is considered the gold standard of post-prostatectomy incontinence therapy. However, male slings are gaining popularity in the treatment of mild to moderate PPI. The overall consensus is a need for prospective research based upon standardized patient workup and outcomes reporting to better compare the surgical options for PPI.
Conclusion: Standardized workup and outcomes reporting would benefit the patient in determining which surgical option best treats postprostatectomy incontinence. As of right now, there is no standardized approach apart from history and physical exam of the patient. Cystoscopy and urodynamics could be a beneficial tool in evaluation patients pre- and post-operatively. Prospective randomized control trials could then utilize a standardized approach to better compare the surgical options for PPI.
Keywords: Post-prostatectomy incontinence, AUS, Male sling
Abbreviations: AUA: American urological association; SUFU: Society of urodynamics, female pelvic medicine and urogenital reconstruction; PPI: Post-prostatectomy incontinence; AUS: Artificial urethral sphincter; SUI: Stress urinary incontinence; ppd: Pads per day; RCT: Randomized control trial
Introduction
Post-prostatectomy incontinence affects anywhere from 1-40% of men after a radical prostatectomy, but treatment is often delayed, and surgery is underperformed [2]. It is estimated 10-20% of men experience severe SUI compared to the 6% who actually undergo a PPI surgery [3]. Current the AUA/SUFU guidelines recommend those who have bothersome SUI unresponsive to conservative therapies may be offered surgical therapy as early as 6 months if incontinence is not improving and should be offered this therapy by 12 months if not satisfied [4]. However, the mean time to surgery for SUI from radical prostatectomy is 2.8 years [3]. Patients undergoing prostatectomy should be informed that incontinence is typical in the short-term resolving by 12 months post-operatively in most cases but may persist in some men without further therapy [4]. Patients are recommended pelvic floor muscle exercises during the post-operative time period. Currently, the AUA/SUFU recommends evaluation with history, physical exam, and appropriate diagnostic modalities to determine the type and degree of incontinence [4]. The aim of this evaluation is to categorize the type of incontinence, determine the severity and bother of incontinence, and determine any complicating factors such as radiation therapy or persistent prostate cancer. Incontinence may be determined to be urgency, stress or mixed incontinence. Urgency incontinence is treated based on overactive bladder guidelines and will not be discussed here. Stress incontinence should be confirmed before surgical treatment options are offered. Stress incontinence may be confirmed using a combination of history and visual confirmation on physical exam, though some patients may require ancillary testing such as urodynamic evaluation (UDS) if additional storage or voiding dysfunction is suspected. The overarching opinion is that cystourethroscopy is to be performed as part of this confirmation to rule out bladder or urethral pathology [4]. Surgical treatment options are based on degree of stress urinary incontinence. An artificial urinary sphincter is typically recommended for moderate to severe SUI, while the male sling can be considered in those with mild to moderate SUI [2]. The AUS is considered a more predictable therapy than the male sling, but the requirements of a mechanical device must also be taken into consideration and discussed with patients.
Discussion
Methods
The study was conducted using the PubMed database for recent papers between 2001 and 2020 with variations of phrases including “post-prostatectomy incontinence”, “treatment”, “AUS”, “male sling”. The search yielded 108 results of which were filtered through based on title and/or abstract. Results not pertaining to patients who had undergone radical prostatectomy were filtered out. Other excluded results were studies focusing on cost-effectiveness, surgical technique, and poor-quality studies [5]. articles were selected for review. The AUA/SUFA guidelines were also referenced.
Result
Key points of articles were summarized in (Table 1).
Table 1:Article Summaries.
Discussion
Artificial urinary sphincter (AUS)
The AUS is considered the gold standard due to the extensive amount of published information on its use for the treatment of moderate to severe PPI [6]. Published reports on AUS data dating back to the 1990s consisted of the largest number of patients compared to other treatments. Not only is there extensive data on the device but the data have been consistent. According to Herschorn, the success of the AUS is between 59- 90%. The definition of success in this report was the use of 0-1 pads per day. However, the definition of continence does depend on the method of evaluation and success varies when using patient-administered questionnaires and pad-free rates. Despite the variation in continence, the patient satisfaction rate is high at 87-90% [6]. Considerations for an AUS placement include the patient’s ability to operate the device and the need for future reoperation due to loss of effectiveness over time. Patients with the AUS are more likely to have complications leading to revision [7,8]. The revision rate for the AUS due to mechanical failure, urethral atrophy, infection, or erosion varies, but Hershorn reports a 23% revision rate.4 A study by Tutolo et al. found a higher success rate in patients without previous incontinence surgery [9]. Previous pelvic radiation is not a contraindication for the AUS as with the male sling.4 However, based on a study by Walsh et al., the revision rate was reported as 41% in irradiated patients compared to 11% in those without irradiation [3] Despite the risk of needing a revision, the longterm durability is still considered superior. In addition, an AUS implantation after sling failure has comparable outcomes to first line AUS placement in mild to moderate incontinence patients [7].
Male sling
Although the AUS is considered the gold standard, the male sling has become a popular option for patients due to ease of surgery, improved outcomes, and low complications. A 21-month prospective, follow- up study found a cure rate of 62% defined by no pad usage.8 In this study, failure was associated with previous urethral stricture, incontinence surgery, or radiation therapy and pre-op 24-h pad weight of more than 200g/day. Another 34-month prospective follow-up study reported 73% of patients had complete resolution of symptoms and 60% of severe incontinence patients had resolution [10]. Additional prospective studies found a 66% success rate at 36-months and a 60% success rate at 39-months [11,12]. In a 52-month follow up, 51% of patients were reportedly using 0-1 ppd and 25% reported a 50 percent reduction in pad use [13]. Another prospective study found a success rate of 77%, 67%, and 63% at 3-month, 1-year, and 3-years respectively [14]. A retrospective study reported a decline in the success rate from 87.3% at initial follow-up to 62.5% at 2-years [15]. The most appealing factor of the male sling to patients compared to the AUS appears to be the absence of having to operate the device. In fact, one study found when given the choice, 92% of patients chose the male sling [16]. As many as 25% of patients are willing to go against surgeon recommendations of the AUS in favor of the male sling. However, the male sling fails to show similar robust results in patients who have a history of pelvic radiation history with only a 54% success rate [3]. The male sling also shows inferior outcomes in patients with a history of urethral stricture or bladder neck contracture. All the above-mentioned factors continue to be relative contraindications to use of a male sling. Based on numerous studies, the ideal candidate for a male sling has no history of radiation, previous stricture or contracture, as well as having only mild to moderate incontinence with a maximum of 200g on a 24-hour pad test and good urethral mobility [17,18].
AUS vs Sling
Success is usually defined by the use of 0-1 pad per day, although some studies define success as 50% improvement in pad use [18]. One study reported the AUS has an average success rate of 83% compared to the 71-75% success rate of male slings [3]. Another review found the average success rate was 65.7% for the AUS and between 48-64% for the male sling [18]. This study concluded that the success in AUS studies was better defined and likely gave the data on the AUS more of an advantage. Looking at mild to moderate incontinence, specifically, one retrospective study found no significant difference in continence rates, improvement rate, or patient satisfaction; however, the follow-up was at 42 months for the AUS and 24 months for the male sling [19]. The only significant difference found was the rate of more severe complications tended to be higher in the AUS population but that was likely due to the higher rates of co-morbidity scores and previous radiation. The AUS continues to be considered the preferred treatment for moderate to severe incontinence; however, there are fewer studies available on the newer male sling [20, 21]. A RCT study by Constable et al. is currently in progress to compare the AUS and male sling [22]. The study aims to use patient questionnaires, 3- day bladder diaries, and 24-h pad test to determine outcomes. Prospective, randomizedcontrol trials would greatly benefit the future of surgical options for post-prostatectomy incontinence.
Factors influencing patient selection and outcomes
The decision between the AUS or the male sling depends on a number of factors. Unfortunately, when stratifying patients preoperatively and measuring outcomes, a standard algorithm is lacking. The currently available studies fail to incorporate reliable pre- and post-operative prognostic factors [23]. Having a standard algorithm will help better select patients for the appropriate procedure. One report looked at urodynamic factors pre- and postoperatively for male sling surgery. Significant findings included changes in detrusor pressure at maximum flow and presence of detrusor overactivity compared to preoperative studies [24]. Another study found compliance and detrusor pressure were good predictors of outcome in patients with the AUS [25]. An additional study found bladder capacity, compliance, and presence of DO were a few urodynamic variables showing improvement post-AUS implantation [26]. Urodynamics could have a promising role in the standard evaluation; however, they currently are recommended to a lesser degree due to insufficient supporting evidence.
Conclusion
The overall consensus is that an algorithm for selecting patients for the AUS or the male sling would benefit from prospective research [1,5,20,27]. Standardizing the workup and outcome measurements would greatly improve patient selection and evaluating outcomes. Some studies have already begun to look at urodynamic data and QOL questionnaires for determining the success of postprostatectomy incontinence procedures. However, due to the lack of standardization, retrospective studies fail to identify pre- and postoperative factors. Urodynamics could offer great objective data in the workup of a patient for post- prostatectomy incontinence. Although more subjective, a standard QOL questionnaire could help quantify patient satisfaction rates. Prospective data is necessary to better compare the outcomes between surgical options for postprostatectomy incontinence.
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information: https://irispublishers.com/aun/fulltext/surgical-options-for-post-prostatectomy-incontinence-a-review.ID.000534.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
1 note
·
View note
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
Unexplained Recurrent Nocturnal Urethral Bleeding: An Unusual Presentation of Penile Fracture
Authored by: Mukesh Chandra Arya

Abstract
Introduction: Penile fracture is an emergency condition. Common presentation is classical history of trauma to erect penis followed by detumescence, penile swelling, ecchymosis and discoloration. Management is primarily surgical. We report our experience of such cases including a subgroup of patients with unexplained recurrent nocturnal urethral bleed without penile swelling and normal voiding.
Material and methods: This a retrospective study performed at our institution. Records of penile fracture cases managed over last 6 years were reviewed. Total of 63 patients were managed either by surgical (53 patients) or conservative (10 patients) approach. Sexual outcomes were measured with abbreviated International Index of Erectile Function (IIEF 5) questionnaire and compared with preoperative scores.
Results: Most common aetiology was coital trauma, seen in 88.9 % of patients. Mean age was 34.95 years. Urethral injury was present in 5 (9.4%) patients in the surgical group. Most common site of injury was ventrolateral {32 (60.4%)} over proximal shaft {49 (92.5%)}. Mean follow up was 19.27 months ranging from 6 to 41 months. Erectile function was preserved (no deterioration in IIEF 5 category) in 96.3 % and 100% of patients from surgical and conservative groups.
Conclusion: Unexplained recurrent nocturnal urethral bleed as a presentation of penile fracture, should be kept in mind. Such peculiar presentation, to our knowledge, has not been reported in literature. This subgroup of patients can be managed conservatively with good sexual and voiding functional outcome.
Keywords: Nocturnal urethral bleed; Penile fracture; Conservative management; Erectile dysfunction
Abbreviations: IIEF: International Index of Erectile Function; ED: Erectile Dysfunction
Introduction
Penile fracture is an emergency urological condition defined as rupture of tunica albuginea of corpora cavernosa because of trauma to erect penis as a result of sudden increase in intra-corporeal pressure. Typically it occurs during coitus when the phallus strikes against the pubis or perineum of partner producing a buckling injury [1]. It can also occur during self-manipulation, rolling over or falling onto erect penis or due to practice of “taqaandan” [2,3]. Patient usually describes a “cracking” or “popping” sound followed by detumescence, pain, swelling and discoloration of penile shaft. If the Buck’s fascia remains intact the hematoma is limited to shaft. If it is also disrupted the hematoma can reach to perineum and suprapubic area. Diagnosis is clinical and management is primarily surgical. We report our experience of managing penile fracture cases over last 6 years with especial impression upon a group of patients having an unusual clinical presentation with unexplained recurrent nocturnal urethral bleeding without penile swelling.
Materials and Methods
Introduction
This is a retrospective analytical study of cases of penile fracture treated at our institution from August 2014 to September 2019. Patients with penile fracture with diagnosis based on classical history of trauma on erect penis followed by sudden detumescence were included. They underwent routine hematology and biochemistry investigations. Pretrauma erectile function was documented using IIEF 5 questionnaire. They were managed either with surgery (N=53) or conservative treatment (N=10).Patients with minimum 6 months follow up were included. Patients with false penile fracture due to rupture of dorsal vein were excluded. Dorsal venous injury could be differentiated from penile fracture as the former does not lead to sudden detumescence, patient can cohabitate further and the site of hematoma being limited to dorsal surface of penis. Data was retrieved from institutional registry of penile fracture patients. Diagnosis of the condition was virtually clinical. Institutional protocol is of emergency repair of such cases without any delay. Conservative management was opted in a special subgroup of patients who presented with unexplained recurrent nocturnal urethral bleeding and either not diagnosed or misdiagnosed and treated for hematuria of unknown cause before being referred to us. This treatment plan was based on shared decision making. On enquiring further these patients had classical history of sexual trauma with “popping” sound and sudden detumescence but no penile swelling. The temporal association of proper history with their symptoms helped us to clinch the diagnosis. Classically all of them had no penile swelling and were voiding well. To document tunical rupture in this subgroup, imaging studies were performed. Ultrasound of penis in 8 /10 cases confirmed the diagnosis. MRI documented it in the remaining 2 cases. Conservative management included compressive dressing, Foley catheterization, antibiotics, anti-inflammatory and antierotic drugs (conjugated estrogen 0.625 mg PO twice daily for 1 week). Many of them refused admission and were managed on outpatient basis. The catheter was kept for 7 days. The surgical management included penile exploration under anaesthesia by a circumcoronal incision, penile degloving, inspection of corporeal tear, repair with delayed absorbable sutures (using PDS 3-0 with knots buried inside) followed by repair of Buck’s fascia over it and circumcision at conclusion of procedure. Circumcoronal incision allowed survey of whole penile shaft and also avoided overlying suture lines with sound healing. Delayed absorbable suture provides ample time for corporeal and tunical tissue to heal without abnormal feeling of knot post operatively. If Bucks fascia is intact and exploration is being performed, one can reach the site of tunic tear only after incising the fascia. Foley catheter was kept and compressive dressing applied. Concomitant urethral repair was undertaken if found injured except in one case in which the repair was staged. Apart from postoperative antibiotics (third generation Cephalosporin and aminoglycoside), anti-inflammatory drugs all patients were given conjugated estrogen 0.625 mg PO twice daily for 1week to prevent erections and advise was given to refrain from sexual activity for 6 weeks. Patients who had not undergone urethral repair were discharged on post-operative day 2nd after removal of dressing and Foley catheter. Catheter was kept for 2 weeks if urethral repair was contemplated. Follow up included history for any voiding or sexual symptoms and local physical examination. Erectile function was assessed at 6 months with IIEF 5 score [4].
Result
Total of 63 patients were included in the study. Mean age was 34.95 years ranging from 18 to 60 years. Most common mode of injury was coital trauma in 88.9 % of patients. Presentation was in different combinations of “popping” sound, sudden detumescence, penile swelling, ecchymosis, deviation and urethral bleed (Table 1)
Table 1:Patient characteristics and history.
Table 2:Intra operative findings, post-operative complications and follow up.
Table 3:Erectile function outcomes.
There was a peculiar group of 10 patients who had coital trauma followed by recurrent nocturnal urethral bleed without any symptom in daytime. They presented late to us and were treated elsewhere as UTI or hematuria but on enquiring into history all of them gave classical history of coital trauma. Ultrasound and/or MRI was done to confirm the diagnosis. The imaging revealed a tear of corpora cavernosa and overlying corpus spongiosum (Figure 1,2).
The proposed mechanism of such injury is a small corporal tear located just opposite to a spongiosal rent and intact Buck`s fascia. The intermittent nature of bleed was due to nocturnal erections opening the communication with corporal blood finding its way out through urethra. They found their undergarments full of blood in the morning when they woke up. As blood decompresses through urethra, penile swelling does not occur and they void clear urine during daytime. The operative findings, complications and follow up are presented in (Table 2).
Most common site of injury was ventrolateral {32 (60.4%)} and location on shaft was proximal {49 (92.5%)}. One patient presented late (>72 hours) with Foley catheter per urethra and local abscess. On exploration he had bilateral corporal tear, and complete urethral transection with pus formation (Figure 3).
He was managed with SPC and corporeal repair followed by delayed urethral repair at 6 weeks. Later on he developed urethrocutaneous fistula which healed spontaneously. Mean follow up was 19.27 months, ranging from 6 to 41 months. Erectile function at six months was preserved (No deterioration in IIEF 5 category) in 96.3 % and 100% of patients from surgery and conservative groups (Table 3).
One of the two patients who had deterioration in erectile function was the aforementioned patient with delayed presentation and abscess. The other one also had bilateral corporeal tear. A two patients from surgery group had new onset ED (one mild and 1 mild to moderate ED). These patients had complete transection of urethra with bilateral corporeal tear.
Discussion
Penile fracture is not very rare. It is a clinical diagnosis, with some workers performing ultrasound or MRI in equivocal cases and for documentation. Shukla et al investigated role of ultrasound in cases of penile fracture. In their series of 15 patients they could localize the site of injury, hematoma and urethral injury. Moreover they proposed a classification system for same [5]. Such classifications need test of time. Metzler et al published an interesting editorial of use of penile ultrasound in patients suspected to have penile fracture to differentiate it from penile ecchymosis only. They had patients on collagenase clostridium histolyticum (CCH) injection for Peyronies disease. Such patients with penile ecchymosis were subjected to ultrasound and spared of surgery in absence of any tunical tear [6]. Another masquerader that needs to be differentiated is dorsal vein injury. Koifman and colleagues used ultrasound in 24.6% of suspected cases of penile fracture. They didn’t find any tunica tear in patients who underwent ultrasound after low suspicion of penile fracture impressing the importance of clinical diagnosis [7]. We at our institution don’t do ultrasound for patients with classical history suggestive of penile fracture. This avoids delay without any change in management. There is no doubt that ultrasound is a readily available, simple, cost effective, non-invasive method of evaluation; operator dependence and at times, severe oedema obscuring the tunical tear limits its potential. Magnetic resonance Imaging has also been explored in this clinical condition. It can accurately demonstrate the integrity of tunica albuginea and any defect if present which manifests as discontinuity of tunica. It is especially useful in cases where ultrasound is inconclusive [8]. It is more sensitive than ultrasound, better able to differentiate a rupture of circumflex or dorsal vein of penis or when penile fracture is not associated with tear in overlying Buck’s fascia [9]. A systematic review with total 438 patients was analysed. The most commonly reported cause of penile fracture was sexual intercourse (80% of cases) and most common finding at examination was penile hematoma (97.5% of cases). Concomitant urethral injury was reported in 15% of cases [10]. Our study in concordance, also had coital trauma as most frequent cause (88.9%) with penile ecchymosis and deviation, being the most common examination findings (80.9% each). The incidence of urethral injury (in surgery group) in our study was 9.4%. The recommended management of the condition is emergency surgical repair and evacuation of hematoma and urethral repair if present concomitantly. Under spinal anaesthesia, the surgical approach most commonly used is circumcoronal incision, penile degloving with inspection of whole corpora and spongiosa to avoid any missed injury [10]. But with advent of imaging which can pinpoint the defect, targeted incision could be planned to avoid complete degloving [11]. Non absorbable suture is avoided for repair as it remains palpable post operatively. Several studies have shown better results for surgical approach as compared to nonsurgical approach [12,13]. A recent meta-analysis including 58 studies and 3213 patients concluded that early surgical interventions led to decreased complications as compared to delayed surgery or conservative management. Specifically the erectile functions were better preserved in patients who underwent surgical intervention as compared to conservative management. Surgical intervention resulted in less erectile dysfunction, curvature and painful erection (p<0.000001). No significant difference was seen in number of patient developing plaques or nodules (p=0.94). Clinical diagnosis by history and physical examination and prompt surgical management is the key to reduce complications [14]. In a recent prospective comparative study Patil et al found delay in surgery (>/=24hrs) as a significant predictor for worse surgical and erectile functional outcomes [15]. They had total of 18 patients and quite high (44%) ED rates at 6 months in their series. Muentener et al in their series of 29 patients with 17 managed conservatively concluded that immediate surgery had superior results as compared to non-operative management, however conservative therapy limited to selected uncomplicated cases could lead to equally good outcome [16]. In a recent series of 32 patients author didn’t find any major complications in either conservative or surgical group. Total of 44% of patients in this study were managed conservatively. However, five patients from conservative group underwent surgery later on [17]. Erectile function was preserved (no change in pre and post op IIEF 5 category) in 96.3% and 100% of patients in surgical group and conservative group respectively at 6 months. Only 2 patients had decline in erectile function as compared to their pre-operative status, both were from surgery group with bilateral corporeal tear. The limitation of our study is its retrospective nature and limited number of patients in conservative group. The strengths are better assessment of erectile function objectively as well as its comparison with pre-operative status which is very important in such cases. Our study also highlights an unusual presentation and successful management of penile fracture with recurrent nocturnal urethral bleeding without any penile swelling, which is not mentioned in the literature. Larger cohort of patients may further give some more insights into results of conservative approach.
Conclusion
Penile fracture is a clinical diagnosis but ultrasound could be a handy instrument in case of dilemma. MRI can also be used but has constraints of availability and cost in emergency settings. Management should be surgical and in case of doubt, shared decision making with low threshold for exploration. Bucks fascia incision may be required to unveil tunical rent. Bilateral corporeal injury +/- urethral injury and delayed presentation are associated with poor erectile functional outcomes. Unexplained recurrent nocturnal urethral bleeding may be the only presenting feature of penile fracture and should be kept in mind. Careful history is of utmost importance. Such peculiar presentation, to our knowledge has not been reported in literature. This subgroup of patients can be managed conservatively with fair sexual and functional outcome.
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information: https://irispublishers.com/aun/fulltext/unexplained-recurrent-nocturnal-urethral-bleeding-an-unusual-presentation.ID.000533.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
1 note
·
View note
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
Urethral Calculi: Presentation, Evaluation and Management
Authored by: Mukesh C Arya

Abstract
Introduction: Urethral calculi constitutes about 1-2% of all calculi in developing countries. Such calculi are more common in males in comparison to females owing to their longer urethra. Herein, we present a series of 264 such calculi.
Material and methods: This is a retrospective study of 264 cases of urethral calculi from July 2013 and February 2019. Detailed history, physical and local examination (palpation of penile urethra and perineum including Digital rectal /Per Vaginal examination) was done. Investigations included urine analysis, culture and sensitivity, ultrasonography (USG) whole abdomen with the perineal region and X-ray pelvis. A retrograde urethrogram was performed if associated urethral pathology was suspected. Cystourethroscopy confirmed the diagnosis in all cases. Patients were analysed about their age, sex, presentation, anatomical site of stone at the time of presentation, and their subsequent management. Composition of urethral calculi was studied using Fourier transform infrared spectroscopy (FTIR).
Results: A total of 264 patients with urethral calculi were analysed (250 males and 14 female). Most common age group was 21-40 years (46.8%). 203 (81.2%) of the calculi in the male patients were in the posterior urethra, 25 (10%) were in the penile/ bulbar urethra and 22(8.8%) in the fossa navicularis. The most common presenting symptom was dribbling & dysuria (70.45%). Radiological studies (X-ray pelvis and USG) showed stone in 85% of cases; Cystourethroscopy was diagnostic and discovered the stone in 15 % of additional cases. Size of stones varied from 1.2 to 2.5 cm. Most of the patients i.e. 190 (71.96 %) were treated with pushback cystolithotripsy (CLT).
Conclusion: Most urethral calculi in patients in developing countries originate from upper tract in contrast to the previous misconception that they originate in the bladder. Management of the urethral calculi varied according to the site, size and associated urethral pathology.
Keywords: Urethral calculus; anterior urethral calculi; pushback cystolithotripsy
Abbreviations: Cystolithotripsy (CLT); Ultrasonography (USG); Fourier transform infrared spectroscopy (FTIR)
Introduction
Urethral calculi are common in developing countries. There are only a few studies that have been conducted so far on these subsets of patients with very limited literature from developing countries. Urethral calculi are divided into primary which forms in urethra and secondary, which migrates from upper urinary tract. Primary urethral calculi are usually small and multiple, and secondary migratory calculi are usually large. Small calculus is commonly found in the anterior urethra and larger calculi usually occur in the posterior urethra. Primary urethral stones are generally composed of magnesium ammonium phosphate (struvite) or uric acid. Calcium oxalate and cystine stones originate from kidney. The causes of secondary stones are stricture, infection, and/or inflammation or within a poorly drained communicating cavity, with an obstruction, stagnation, acting as the predisposing factor.
Secondary or migratory stones are usually more common mainly comprising of calcium oxalate or citrate. Migratory stones are most often encountered in association with urethral stricture disease or other forms of urethral obstruction .The main symptoms are dribbling, dysuria, acute urinary retention, frequency, haematuria, interruption of the urinary stream, or a history of spontaneous passage of stone (such patients were excluded in our study). Retrograde manipulation into the urinary bladder followed by litholopaxy or lithotripsy is a suitable procedure for small urethral calculi. Anterior urethral calculi can be removed under local anaesthesia via endoscopy or ventral meatotomy.
Patients and Methods
This is a retrospective study of 264 patients presenting with urethral calculi from July 2013 and February 2019. A detailed urological history was taken along with physical and local examination including palpation of the urethra and digital rectal examination (DRE). Complete blood counts (CBC), serum biochemistry including serum urea and creatinine serum calcium, serum uric acid, serum parathyroid hormone (PTH), urine calcium creatinine ratio, urine analysis, urine culture and sensitivity, ultrasonography whole abdomen with perineal/scrotal region and x-ray pelvis were done. Intravenous urography (IVU) was done in cases with upper urinary tract calculi. A retrograde urethrogram was performed if associated urethral pathology was suspected. Cystourethroscopy was performed in all cases and confirmed the diagnosis. MRI (magnetic resonance imaging) was done in one female to depict relevant anatomy of the urethral diverticulum and associated stone. Urethral calculi were analysed about age, sex, presentation, the anatomical site at presentation, associated diseases, and management. Finally, the stone analysis was done using Fourier transform infrared spectroscopy (FTIR) to study the composition of urethral calculi.
Results
1. Age and sex: A total of 264 patients with urethral calculi were analysed (250 male and 14 female). Male to female ratio was 17.8: 1. Age ranged from 6 months to 86 years (Figure 1).
The maximum number of patient (46.6%) was in the 21-40 years of age group. Mean age was 52.7 years.
2. Presenting complaints: Most common presenting symptom was dribbling &dysuria (70.45 %) followed by penile& perineal pain (43.18%), decreased urinary stream & intermittency (36.36%), retention of urine and hematuria (12.87% each), fever (3.78%) and purulent discharge (2.27%) in these patients (Table 1).
Out of these, 81 stones (30.68%). were palpable; one female (age 31years) had procidentia with a palpable stone in the prolapsed bladder. Twenty-nine (10.98%) had associated diseases of the lower urinary tract, the commonest being urethral stricture (15 patients). Seventy-four patients (28.03%) had a prior history of urolithiasis or surgery for the same (Table 2).
Associated upper urinary tract calculi were found in 30 cases. Out of which, 2 were in the bladder, 20 in kidney and 18 in ureter (Table: 3).
3. Location of stones: In male patients, the most common location was in the posterior urethra 203 (81.2%), 13 (5.2%) in the bulbar urethra, 12 (4.8%) in penile urethra and 22(8.8%) in the fossa navicularis (Figure 2).
All-female patients and 7.57% of male patients presented with retention of urine (ROU). In these patients, catheterisation was done; while in 28 cases where the attempt of catheterisation was unsuccessful suprapubic catheterisation (SPC) was done.
4. Urine culture: In only 18 cases, urine culture was positive. Majority of them (15) were positive for E. coli, two for klebsiella and one showed growth of pseudomonas.
5. Management: One hundred fifty-one cases were operated under local anaesthesia, followed by 90 in spinal and 23 in general anaesthesia. Most of the patients i.e. 190 (71.96 %) were treated with pushback cystolithotripsy (CLT), 15 patients (5.68%) were treated with endoscopic retrieval, 12 patients (4.54%) were treated with meatotomy with the retrieval of stone. Larger stones impacted at meatus should be treated with meatotomy to prevent stricture. Holmium laser lithotripsy was done in nine patients of the pediatric age group using 6-7.5 F ureteroscope. Seven patients (2.64%) with urethral calculi and associated urethral strictures underwent visual internal urethrotomy or endoscopic dilatation initially; the stones were then pushed into the bladder and CLT was done. In the remaining eight patients (3.03%) urethrolithotomy & BMG onlay urethroplasty was done. Percutaneous cystolithotripsy (PCCL) done in 2 cases, perineal urethrostomy done in 1 case, CLT and bladder neck incision (BNI) done in 6 cases. Foley’s catheter was placed for 3-5 days after VIU/meatotomy, 3 weeks for onlay urethroplasty and for 2 weeks after diverticulectomy. Suprapubic cystolithotomy (SPCL) was done in 2 patients with neurogenic bladder and one patient with Exstrophy; these patients were put on CIC. One female had a diverticular stone which was treated with diverticulectomy and another female patient had associated uterine prolapse in whom sacral colpopexy was done (Table 4).
These patients were followed at 6 weeks and 3 months with symptomatology, uroflowmetry to detect stricture due to stone or transurethral surgery. Seven patients developed stricture in the bulbar urethra which was managed successfully with VIU. Twelve patients developed symptomatic urinary tract infection which was treated by culture-sensitive antibiotics.
6. Stone analysis: Stone analysis was performed in 100 cases using FTIR of which mostly (85 cases) were mixed stone with calcium oxalate monohydrate as a primary component, calcium phosphate in 10, struvite in 3 and uric acid stone in 2 patients (Table 5).
7. Metabolic evaluation: Metabolic evaluation could be done only in 33 patients. Among these, fifteen patients had hypercalciuria. One patient had hyperparathyroidism and 1 had hyperuricemia; they were referred to an endocrinologist for further management (Tables 6,7).
Discussion
Calculi in the urethra is not uncommon in developing countries. From developing countries, only a few studies were focused on such patients. In our study, patient age ranged from 6 months to 86 years with a mean of 52.7 years. Most of the patients (46.8%) were in the age group of 21-40 years. The difference in age prevalence may be due to the differences in lifestyle, nutritional habits and environmental conditions. Mean age in other studies was 43 – 46 years12,13. The proportion of females was 14 (5.3%) in our study and only one had associated diverticular disease. This was in contrast with other studies in which all of the females with urethral calculi had urethral diverticulae11,12. Dysuria remains to be the commonest symptom in the range of 33.33 % to 82.14 % in different studies 9,11,12,14. Retention of urine was commonest occurrence in 46% - 89% of patients1,4,9. The most common presenting symptom in our series was dribbling & dysuria (70.45 %) followed by penile & perineal pain (43.18%), decreased urinary stream & intermittency (36.36%). In our study, ROU was present in 12.87% of cases only. Associated upper tract calculi were present in 32 - 33% of the patients1,2. This emphasizes the importance of evaluation for the upper urinary tract in patients with urethral calculi. In our series, upper tract stones were present in 11.36% (20 in kidney and 18 in the ureter). Posterior urethral location is commonest for urethral calculi as presented in various studies 4,9,12,13,14. This was in concordance with our study in which 81% of stones were in posterior urethra. However, few authors have reported anterior urethra to be the most common site (50- 63%)1,10 (Figure 3).
In our series majority of stone, 237 (89.77 %) could be treated by different types of endoscopic procedures similar to study of Kamal etal4 in which 86% undergone endoscopic procedures. This was in contrast of study to Ameen and colleagues14. They reported spontaneous passage in the majority (70%). We however, excluded such patients. Stone analysis was reported in a few studies with mixed stones and calcium oxalate monohydrate as a principal constituent in a majority in around 70-80% % 4,11. Similar were the results in our series. Other constituents were calcium phosphate, struvite and uric acid. This confirms that most of these stones are dropped ones from an upper tract in contrast to common belief previously that these stones originated in the bladder. Correction of urethral stricture and control of infection is vital to prevent a recurrence. Chemical composition helps us to take preventive measures. Management of the urethral calculi varies according to the site, size and associated urethral pathology. Retrograde manipulation into the urinary bladder, followed by litholopaxy, is a safe procedure for posterior urethral calculi provided that the manipulation is done endoscopically or by saline irrigation under direct vision. Irrigation expands the urethra and facilitates the passage of stone to the bladder. A urethral stricture can be dealt by visual internal urethrotomy before manipulating the calculus into the urinary bladder. Impacted, large irregular calculi or those in a urethral diverticulum are best removed through open exploration, external urethrotomy followed by excision and repair of the diverticulum. Extraction through the external meatus is suitable only for small, smooth calculi in the region of fossa navicularis. It should be done with great caution to prevent urethral mucosal injury. In two cases of ureterocele with stones, endoscopic incision of ureterocele with CLT was done. In one female, CuT migrated into bladder and formed calculus, dealt with endoscopically.
Conclusion
Most urethral calculi in patients in developing countries originate from upper tract in contrast to previous misconception that they originate in the bladder. Furthermore, urethral anatomical pathology does not seem to be a necessary condition for most such stones. In all patients who presented with lower urinary tract symptoms especially in younger age group, urethral stone should be kept in mind as differential diagnosis and X-ray KUB with pelvis is advisable in these patients.
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information: https://irispublishers.com/aun/fulltext/urethral-calculi-presentation-evaluation-and-management.ID.000532.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
1 note
·
View note
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
External Iliac Vein Laceration-A Rare Complication of Tunneled Dialysis Catheter
Authored by: Hashmi MN

Abstract
Bleeding complication from Central dialysis catheter is rare. Usually it settles in short time after procedure. If patient is on antiplatelet therapy it can sometimes last for 24-48 hours and stops with pressure dressing. We report a rare case of ongoing (>96 hour post procedure) bleeding from dialysis catheter exit site and investigation revealed the cause was iliac vein laceration.
Introduction
Vascular access is life line of hemodialysis patients. Preferred choice is AVF but sometimes while awaiting maturation of AVF, a tunneled dialysis catheter is placed to fulfill need of renal replacement therapy. Dialysis catheter placement can sometimes result in complications and they are dealt accordingly.
Case
56-year-old female patient on Maintenance Hemodialysis underwent a new arteriovenous fistula (AVF) creation. She also underwent right tunneled femoral dialysis catheter insertion to cover dialysis till fistula is matured. She presented to OPD with bleeding at site of Catheter insertion during hemodialysis. This is common in newly inserted catheter especially if patient is on antiplatelet therapy. It usually stops in 24-48 hrs. Patient was examined and no obvious hematoma or bleeding cause identified at insertion site of femoral dialysis catheter. Exit site was clean (no evidence of infection) and all stitches were removed. Patient’s drug history was reviewed and she was not on any anticoagulation therapy. Laboratory parameters showed Normal coagulation profile, Hemoglobin 8.6g/dl and platelet count of 235x109/L. Patient later went for hemodialysis and on commencement of dialysis bleeding started from insertion site of dialysis catheter. This was unusual and in order to identify the cause we discussed case with radiology department and CT fluoroscopy was planned. Patient underwent CT to detect bleeding point. She had CT fluoroscopic angiogram (160 slice strength). Ultravist-300 Contrast medium of 100 ml was injected in femoral dialysis catheter. Imaging showed extra vasation of the contrast medium from external iliac vein at the level of femoral head. Laceration was 8 cm away from insertion point of catheter (Figure 1,2).
Discussion
Maintenance Hemodialysis patients lifeline is vascular access. Vascular access patency is another crucial step. AVF is preferred choice in patients who can tolerate surgery. Pre-emptive AVF is preferred choice [1]. A lot of patients had to undergo Permanent catheter insertion as initial access for bridging AVF maturation. Central Venous catheters (CVC) insertion complications include vascular injury (arterial puncture, pseudoaneurysm, air embolism, pneumothorax, and malposition). Indwelling complications are infection, thrombosis, catheter pinching/kinking, and fracture with possible embolization. Late complication is stenosis of veins that may occur over a period of time, after damage to the vein wall due to infection or mechanical stress. The risk of stenosis is reduced if the catheter lies in the center of a big vein with a high blood flow away from junctions with other veins [2]. Approximately one-third of hemodialysis patients who use tunneled dialysis catheter during 1 to 2 years’ experience complications [3]. Central venous stenosis has been reported in studies and usually occurs in small number of patients but more common in patients who undergo repeated CVC insertion or with long duration of catheter [4]. Our patient had bleeding secondary to iliac vein damage at level of femoral head anatomically which is rare. Patient had history of access issues and had multiple temporary lines insertion in past resulting in stenosis. In our case catheter placement was done by interventional radiologist and we suspect due to previous history of multiple dialysis lines placement there was stenosis present. On passing dilator the vein got damaged and resulted in iliac vein laceration. There is also possibility of vein damage from catheter tip which has been reported in case report [5]. Patient was referred to vascular surgery after confirmation of vein laceration and the injured vessel wall was treated surgically. Patient has been well since then and undergoing regular hemodialysis from AVF.
Conclusion
We wish to point rare complication of hemodialysis catheter which can happen during catheter placement. In such cases early investigation can reduce complications. Our patient was timely diagnosed and treated.
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information: https://irispublishers.com/aun/fulltext/external-lliac-vein-laceration-a-rare-complication.ID.000531.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
0 notes
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
Albuminuria in the Elderly More than a Marker of Renal or Cardiovascular Disease
Authored by: Joshua I Barzilay
Background
Albuminuria - the presence of more than 30 mg of alumin per one gram of creatinine in the urine - is highly prevalent in older adults. Based on data from the NHANES III study, more than 20% of adults over the age of 70 years have albuminuria, while among similarly aged adults with diabetes the prevalence reaches 40% [1,2]. To date, most studies have examined albuminuria as a risk factor for cardiovascular disease. We too have found albuminuria to be associated with a 70-80% increased prevalence of cardiovascular disease [3] and a doubling of mortality risk (mostly cardiovascular in nature) [4] as compared to older people without microalbuminuria.
More recently, we and others have shown that albuminuria is associated with other diseases of older age. The two most outstanding diseases of older age associated with albuminuria are hip fractures and dementia. In one study of ours [5], a doubling of albuminuria was significantly associated with hip fracture risk in women (hazard ratio, 1.12, 95 % CI, 1.001-1.25), but not in men. In two other studies, we found a borderline lower bone mineral density in association with albuminuria in men [5, 6]. We also reported that participants with baseline albuminuria had a significantly increased risk of hip fracture compared with participants without albuminuria (adjusted hazard ratio=1.36 [1.01, 1.84], P=0.05) [7]. Last, it is known that up to 40-50% of people with hip fractures have cognitive impairment (such as dementia or mild cognitive impairment [a possible precursor of dementia). In our analyses we found that the association of cognitive impairment with hip fracture risk was attenuated with adjustment for the presence of albuminuria [8]. Stated differently, albuminuria played a role in mediating the association of hip fracture risk with cognitive impairment. Given the above findings, it would appear that albuminuria is more than a disorder of the glomerulus or a cardio-renal risk factor.
Several studies have shown albuminuria to be related to other disorders of aging. These include reduced physical performance, as measured by gait speed and grip strength [9]; dementia [10]; reduced lung function, as measured by one second forced expiratory volume [11]; microvascular cardiomyopathy [12]; abnormal reactivity of small [13] and large blood vessels [14]; and abnormal retinal findings in people with diabetes [15]. Taken together, these findings suggest that albuminuria may be an indicator of enhanced physiological aging beyond its known association with cardiovascular risk, and a possible marker of a systemic functional disorder of the microvasculature [16].
Present Study
We reasoned that if albuminuria is indeed a marker of aging or of enhanced susceptibility to illness, then hospitalization rates would be higher in people with albuminuria as compared to people without albuminuria. In addition, we hypothesized that rates of hospitalization would be increased as well for a wide variety of disorders, especially in certain domains of aging—for example, heart failure, injury, cancer and infection. Finally, given the adverse association of diabetes on health, we hypothesized that people with albuminuria and diabetes would have a higher rate of hospitalization than people with albuminuria but without diabetes. To do such an analysis, we examined the Cardiovascular Health Study (CHS) data set. CHS is a follow up study of nearly 6000 Caucasian and African American adults (age >65 years at baseline) from four US research centers who have been passively followed for health outcomes over several decades. The cohort is well characterized and has served as a source for more than 1500 academic papers. Using incident hospitalization rates as a measure of outcome, we found albuminuria to have a pervasive and deleterious association on the health of older adults across a broad range of diagnoses. Hospitalization rates were 39% higher among people with albuminuria compared to people without albuminuria, even after adjustment for hypertension and diabetes (the main determinants of albuminuria), and adjustment for concomitant estimated glomerular filtration rate. The number of hospital days was increased by ~60% as well. Circulatory disorders (e.g., heart failure) accounted for the largest number of hospitalizations (~30%). Most hospitalizations, however, were not for circulatory disorders. Infectious, endocrine (e.g., diabetes), injury and respiratory (e.g., pneumonia) hospitalizations were increased 40- 90%. Cancer risks were also increased, but not significantly so. Genitourinary disorders, in particular, were increased by ~40% in men and ~75% in women. Diseases of the male genital organs (ICD 9 codes 600.0-608.0) were increased. Of interest, the presence of diabetes did not enhance the risk of being hospitalized for any of these disorders. From this latter finding it may be deduced that the effect of diabetes on hospitalization risk is mediated in large part through its association with albuminuria, not from diabetes per se. Also, of interest, was the fact that albuminuria did not significantly increase the risk of hospitalization for chronic kidney disease, though it did have a statistically significant association with acute kidney injury. For more specifics, the reader is referred to our article (see reference 1).
Conclusion
In conclusion, there are two take away messages from our study for the urologist and the nephrologist. One, albuminuria is most likely a manifestation of a systemic disorder that impacts the health of older adults. It is not just a renal microvascular disorder. Second, albuminuria is a risk factor for hospitalization. Additional attention to people with albuminuria, to optimize their health, may lead to cost savings.
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information: https://irispublishers.com/aun/fulltext/albuminuria-in-the-elderly-more-than-a-marker-of-renal-or-cardiovascular-disease.ID.000530.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
0 notes
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
Invasive Mole with Nephrotic Syndrome: A Case Report with Literature Review
Authored by: Yu Zhao
Abstract
Nephrotic syndrome(NS)associated with invasive mole (IM) is uncommon. In this report, we present a case of NS that developed from IM. A 22-year-old woman was admitted to our hospital because of left lower slightly abdominal pain with sparing vaginal bleeding and NS. Transabdominal ultrasound examination confirmed a regular shape, border clearance component with a typical honeycomb pattern in the left side of the uterus. The curettage was performed for her two times. A renal biopsy was performed and suggested minimal change disease (MCD). Interestingly, when the IM was removed, her NS was complete remission. We report the rare case to highlight the importance of considering that NS associated with IM should be kept in mind during management of a woman of childbearing age with renal involvement.
Keywords: Invasive mole; Nephrotic syndrome; Gestational trophoblastic neoplasia; hydatidiform mole
Introduction
Invasive mole (IM), a malignant tumor, is a form of gestational trophoblastic neoplasia (GTN), which are characterized by invasive hydatid tissue into the myometrium or distant metastasis [1]. The most common transfer locations for IM are the vagina, lungs and brain. The most common symptom of IM is irregular vaginal bleeding, but further symptoms caused by bleeding in the metastases may also be detected, such as hemoptysis and neurological symptoms [2]. Myometrial invasion, swollen villi and hyperplastic trophoblast are often considered to be the pathological features of IM. IM′s clinical diagnosis mainly depends on medical history, clinical symptoms, laboratory tests and examination using imaging. Pathological results are the most essential basis for diagnosis. Good prognosis based on timely and comprehensive chemotherapy [3]. In this report, we describe a patient presenting with NS in which the underlying diagnosis of IM was made by a combination of chance and a high level of clinical suspicion, and to improve patient care amongst internists by heightening awareness of this uncommon condition.
Case Report
A 22-year-old woman was admitted to our hospital because of slight left lower abdominal pain with sporadic vaginal bleeding. She reported amenorrhea for 37 days and had a positive urine β-hCG test. She had no obstetric history, with menarche at 13 years of age, regular menstruation and no pregnancy history. She was admitted to the department of nephrology because of NS and was treated with hydrochlorothiazide, but her oedema was aggravated. Her urine output decreased to 500 ml/day. She had no fever, erythema, joint pain or alopecia. Physical examination at admission revealed mucocutaneous pallor and generalized oedema. A soft elastic, non-tender palpable mass, approximately 10 cm in diameter, was identified in the lower left part of the abdomen. A vaginal examination showed a normal vulva and vagina. Laboratory examination showed the following: haemoglobin 93 g/L, total protein 50 g/L, albumin 28 g/L, serum β-hCG 15400 mIU/mL, urine β-hCG 34140 mIU/mL, and urine protein 3.5 g/24 h. Screening tests for hepatitis A, B, and C were negative. Testing for antinuclear antibodies, dsDNA antibodies, anticardiolipin antibodies and antineutrophil cytoplasmic antibodies were negative. Due to increased abdominal pain and oedema in the patient, haemoglobin was decreased to 81 g/L. Ectopic pregnancy was highly suspected and she was urgently transferred to the gynaecology department. A trans-abdominal ultrasound examination confirmed a regularshaped, clear-border mass with a typical honeycomb pattern on the left side of the uterus. An abdominopelvic computed tomography scan confirmed a substantial mass; ovarian cystadenocarcinoma and trophoblastic neoplasia of the uterus were considered. Suction curettage was performed twice. Gross suction curettage specimens showed placental tissue with different-sized vesicles that resembled a cluster of grapes, with the absence of a foetus. A light micrograph showed complete hydatidiform mole (III), and hydatidiform mole with myometrial invasion was confirmed by ultrasonography. A renal biopsy was performed. Light microscopy showed that the glomeruli were normal, without mesangial widening. The capillary loops were open and had normal in appearance. Immunofluorescence staining revealed that immunoglobulin G (IgG), IgA, IgM, C3, fibrinogen and C1q were all negative. Electron microscopy revealed that the thickness of the basement membrane was within the normal range, and diffuse foot process fusion was observed. The pathological findings suggested minimal change disease (MCD). After suction curettage, facial oedema and pretibial pitting oedema significantly subsided. Her urine output increased to 1000 ml/day, and she lost weight. Her abdominal pain was obviously eased, and the vaginal bleeding was clearly lessened. Serum β-hCG levels declined to 2068 mIU/mL. Blood chemistry tests revealed a total protein level of 54.3 g/L and albumin level of 32.6 g/L. 5-FU single chamber chemotherapy was administered. One month later, her serum β-hCG declined to 7.7 mIU/mL, her urine β-hCG decreased to 5 mIU/mL, her total protein was 57.7 g/L, her albumin was 41.9 g/L, and her urine protein was 0.56 g/24 h. She has been regularly followed for the last twenty-six months and has remained free of clinical symptoms.
Discussion
IM is responsible for the most cases of localized GTN1, which is one style of Gestational trophoblastic disease (GTD). IM occur in approximately 15% of patients with complete hydatidiform moles, while in other types of pregnancies it occurs less frequently [4]. In China, the incidence rate of IM following pregnancy is 0.94- 1.30% [5]. IM, sometimes, which are penetration of the peritoneum or adjacent parametria or the vaginal vault, are distinguished by excessive trophoblastic overgrowth and extensive penetration by trophoblastic elements, including whole villi, deep into the myometrium. As a result of the improved economy and the decline in overall birth rate, the prevalence of IM has declined over the past 30 years. However, IM has malignant tumor behavior and can undergo extensive metastasis. If not treated in time, it can be converted into choriocarcinoma with poor prognosis, which can lead to significant morbidity and mortality. The common causes of secondary adult female NS are systemic lupus erythematosus, hepatitis B, and Henoch-Schonlein purpura, etc. We report additionally the rare case about NS associated with IM in a 22-year-old unmarried woman. Myometrial invasion, swollen villi and hyperplastic trophoblasts are frequently considered to be pathological features of IM; however, the majority of IM cases are diagnosed clinically rather than pathologically [6]. Based on the clinical manifestation and correlation examination, we diagnosed NS associated with IM. From the treatment situation, with a nearly recover in laboratory test results after a week of the suction curettage. Our patient was consistent with the above references in clinical manifestation and prognosis. We thought the NS associated with IM, probably is the paraneoplastic phenomenon. Because when the suction curettage was administered, the NS secondary to the IM was general remission. It is not clear that the precise pathogenesis of relationship between the IM and NS. Rong YJ [7] showed that the pathogenesis may be due to maternal and trophoblast cells had abnormal immune response with immune complex deposition in glomeruli, causing increased permeability of the glomerular filtration membrane, which led to a series of pathophysiological changes. The placenta releases trophoblastic cells with cytotoxic characteristics and the capacity to cause secondary glomerular endothelial damage by Brown DW reported [8]. The NS associated with IM, probably is the paraneoplastic phenomenon. IM has malignant potential for local invasion and distant metastasis [8] and is probably capable of causing a paraneoplastic phenomenon, which is noted prior to the diagnosis of the malignancy. It is possible that the placenta releases trophoblastic cells with cytotoxic characteristics and the capacity to cause secondary glomerular endothelial damage. A review of the literature reveals that only 7 cases on NS accompanied by hydatidiform moles are shown in Table 1 [9-14].
Pathologic finding suggested respectively, pre-eclamptic nephropathy 9, 12, membrano proliferative glomerulonephritis10, focal segmental glomerulosclerosis [12] and MCD [13]. NS was the prominently manifestation, endothelial cell swelling or swollen epithelial cells with diffuse foot process fusion were the renal pathological presentation. Interestingly, when the IM was removed, the IM was complete remission. According the literatures, we did not find a tendency about pathology of NS associated with hydatidiform moles. Pathologic finding of our patient was MCD. We can actively infer that IM had a tendency to be associated with MCD. Recently, although MCD may occur in association with haematologic malignancies, lymphoma or leukaemias [15], rare cases of MCD associated with solid tumors have been reported. We report additionally the rare case to highlight the importance of considering that NS associated with GTD should be kept in mind during management of a woman of childbearing age with renal involvement, pregnancy history and menstrual history should be considered as an indispensable inquiry for the choice of correct treatment measures.
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information: https://irispublishers.com/aun/fulltext/invasive-mole-with-nephrotic-syndrome-a-case-report-with-literature-review.ID.000529.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
0 notes
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
New Treatment New Complication – Mini Review
Authored by: Ákos Géza Pethő
Abstract
Nephrotoxicity caused by medication could limit the treatment success. In multiple malignancies are playing crucial role the anti-cancer drugs which have well known nephrotoxicity. Using the conventional chemotherapies acute kidney injury could develop but not in all patients who are suffering cancers. In these patients will acute tubulointerstitial nephritis or rarely nephrotic syndrome occur. The onco-pharmacology is an intensively investigated field. In the recent decade’s novel therapies founded. The new treatments in oncology have more targeted affect on cancer cells. These drugs will be modifying the whole immune system with the fine balance between cancer surveillance and preserving self-tolerance. The immune checkpoint inhibitors have superior anti-cancer therapeutic affect but new, until unknown complication raised. In this mini review we will discuss the most acute kidney injuries during chemotherapy.
Keywords: Cancer; Chemotherapy; Immune system; Immune checkpoint inhibitors
Introduction
Nephrotoxicity caused by medication could limit the treatment success. In malignancies the conventional chemotherapeutic medications could cause acute or chronic kidney injury. The mechanism of the kidney injury is nontargeted cell killing with the possibility of the injure the renal microvasculature, glomerulus, tubular segments, and renal interstitial [1]. The clinical syndrome that caused by those conventional chemotherapeutic drugs could be various, e.g. acute kidney injury, proteinuria–hematuria, the nephrotic syndrome, isolated tubulopathies (with accompanying electrolyte and acid–base disturbances), hypertension, and chronic kidney disease [2]. Beyond these conventional chemotherapeutic medications novel cell specific immunotherapies were developed. Oncologists have used immunotherapies since the 1980s and 1990s. The first immunotherapies used were exogenous cytokines, such as IFN-α [3]. From this point intensively research was started, the anti-cancer therapies will have advanced further by intensifying the immune response [4]. The immunotherapies will fine balance between cancer surveillance and preserving self-tolerance. This novel immunotherapy known as immune checkpoints inhibitors. The modulation of the immune system is dependent on the complex interplay between multiple immune system components. In the pathway of the immune system respond playing rolecytotoxic, helper, and regulatory T cells; macrophages; natural killer cells; and myeloid-derived suppressor cells. By the respond of thy immune system is the most important point; the balance between a hyperactive immune response resulting in immune-mediated damage to healthy tissues and a hypoactive immune response resulting in infections and malignancies is achieved through a redundant and multilevel regulation of lymphocyte cytotoxic activity through immune checkpoint inhibition [5]. The novel immunotherapies have new side effects. Off-target inflammatory responses to checkpoint inhibitors are commonly referred to as immune-related adverse effects (irAEs).
Conventional Chemotherapies
Not all patients exposed to nephrotoxic chemotherapeutic agents develop kidney injury, suggesting the presence of severalc factors that enhance patient risk for nephrotoxicity. Most common is acute tubular injury or necrosis due to treatment with platinumcontaining regimens, ifosfamide, oledronic acid, pemetrexed, and numerous other chemotherapeutic agents [1]. But not only the renal tubulointerstitial and well known tubulopathy could occur. Some drugs could affect intraglomerular, causing focal and segmental glomerulosclerosis and minimal change disease, which promotes a form of drug-induced podocytopathy. ss such as pamidronate are widely used in the treatment of patients with lytic bony lesions secondary to breast cancer or multiple myeloma. Pamidronate causes a collapsing variety of FSGS [6]. Bisphosphonates have been associated with deterioration of renal function and histopathological changes in the kidney. Drug-related side effects are limiting factors to the use of bisphosphonates. Available data suggest that pamidronate and zolidronate, but not ibandronate, are associated with nephrotoxicity in the treatment of patients with malignant disease [7]. Other drug-induced forms of acute kidney injury include obstructive and inflammatory interstitial injury resulting from intratubular crystal precipitation induced by methotrexate and interstitial nephritis from various chemotherapeutic agents [8].
IFN-α Therapy
IFN-α was Food and Drug Administration (FDA) approved to treat CML in 1981 followed by hairy cell leukemia, AIDS-related Kaposi sarcoma, metastatic melanoma, and follicular non-Hodgkin lymphoma. IFN-α will enhances the effect or T cell–mediated responses, with cytokine release, e.g. IL-12 secretion, via several signaling events [9]. By IFN-α treatment could occur minimal change disease (MCD) or FSGS, which are manifestations of podocyte injury. Sometimes thrombotic microangiopathy (TMA) is the clinical symptom after administering of IFN-α, which reflects vascular endothelial damage [10].
Immune Checkpoint Inhibitors
The immune checkpoint inhibitors are more interesting field of anti-cancer drugs. Enhancing or suppressing T cell activation via costimulatory or coinhibitorymolecules modifies effector T cell response. Cytotoxic lymphocyte–associated antigen-4 (CTLA- 4) and programmed cell death protein-1 (PD-1) are two receptors that play an important role in negatively regulating T cell activation and function [11]. The most important effect of those receptors. that ligand binding to CTLA-4 and PD-1 receptors modifies the immune system response to antigens by inhibiting T cell activation. The inhibition of the T-cells allows the immunologic self-tolerance and prevents autoimmunity. Administration of immune checkpoint inhibitors could various of adverse autoimmune effects appear, e.g. dermatitis, colitis, pneumonitis, endocrinopathies. The incidence of IRAEs range from 15% to 90%, with severe IRAEsranging from 0.5% to 13% [12,13]. The mechanism of CPI-induced kidney injury is unknown, but CPI therapy in patients with kidney transplants could develop rejection. Because of this major side effect of CPI oncologist should consider the anti-cancer therapy in kidney transplanted patients [14]. The anti-CTLA4 drug (ipilimumab) in some cases caused minimal-change disease and interstitial nephritis. The ipilimumab has been described as causing acute kidney injury from interstitial nephritis as well as lupus nephritis, too [15]. Pathology revealed acute interstitial nephritis in most cases with varying degrees of foot process effacement. Most of the AKI occurred 6–12 weeks following the start of treatment, with the longest interval being 26 weeks [16]. Programmed cell death protein 1 (PD-1) play a crucial role in anti-cancer immunity, too. Monoclonal antibodies against PD-1 (nivolumab and pembrolizumab) andPD-L1 (atezolizumab) are currently used for the treatment of advanced stage cancers. Acute tubulointerstitial nephritis is an important manifestation of kidney injury associated with the use of anti-PD-1 drugs [17]. Nivolumab, a monoclonal anti-PD1 antibody can cause autoimmune glomerulonephritis as well as tubulointerstitial injury. The immune-related nephritis generally responded well to systemic corticosteroid treatment [18]. The oncologist almost uses combination therapy with ipilimumab and nivolumab. The combination therapy appears to increase the incidence and severity of adverse events as compared to the use of nivolumab alone [19].
Conclusion
The acute kidney injury is the most complication of the anticancer chemotherapy. The conventional anti-cancer drugs have dose effect and the possibility of the kidney injury raises with the decrease of the kidney function. In most cases after administrating the conventional chemotherapies acute tubulointerstitial nephritis will develop. The oncology treatment has novel drugs, which has more targeted anti-cancer effect. These new therapies are modifying the immune system. With the modification of the immune system will develop new symptoms and side effects. All potential causes of AKI (prerenal, ATN, obstruction) should be evaluated. If AKI is confirmed on a kidney biopsy as AIN or a podocytopathy. Strongly recommended the discontinuation of the check point inhibitors and a course of corticosteroids [20]. Empirical corticosteroid treatment may mask the progression of glomerular disease. However, biopsyconfirmed acute tubular necrosis does not require discontinuation of checkpoint inhibitor therapy, and while corticosteroid treatment appears to be harmless as far as oncologic outcomes are concerned, even a short-term course is associated with multiple systemic adverse effects [5]. The life expectancy of cancer patients is increasing, leading to a higher likelihood of developing some degree of kidney impairment and patients with kidney impairment are living longer, with an increased risk of developing concomitant cancer [21].
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information:https://irispublishers.com/aun/fulltext/new-treatment-new-complication-mini-review.ID.000528.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
0 notes
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
Successful Resuscitation of an Elderly Diabetic Patient Having Life Threatening Acute Severe Hyperkalemia
Authored by: Satyanand Sathi

Introduction
Among hospitalized patients, the prevalence of hyperkalemia has been approximated at 1% to 10% [1, 2]. Patients with diabetes mellitus, heart failure (HF), chronic kidney disease (CKD), and those using renin-angiotensin-aldosterone system inhibitors (RAASi) are at 2 to 3 times higher risk for hyperkalemia [3-5]. Hyperkalemia has become a more common concern as diabetic and HF patients usually take RAASi and mineral corticoid receptor antagonists (MRAs).The incidence of hyperkalemia is higher in diabetic patients as compare to the general population[6,7]. Normal ageing, particularly after the sixth decade, is associated with a decrease in renin production and may cause hyporeninemic hypoaldosteronism [8]. Shifting of potassium from the intracellular to the extracellular compartment can cause hyperkalemia and is called as shift hyperkalemia. The most common causative factor of chronic hyperkalemia in diabetics is the decreased tubular secretion of potassi um due to the syndrome of hyporeninemic hypoaldosteronism [9]. This syndrome is specified by mild to moderate renal insufficiency and patients usually present with asymptomatic hyperkalemia. Degree of severity of hyperkalemia is generally classified as mild (5.5- 6.5 mmol/l), moderate (6.5-7.5 mmol/l) and severe (>7.5 mmol/l) [10]. Hyperkalemia is further classified as acute or chronic [11]. Acute hyperkalemia occurs as a single event, over hours to days and usually requires emergency treatment. Chronic hyperkalemia develops over a period of weeks to months, may be persistent or develop periodically, and requires ongoing outpatient management [11].
Case Report
An 86-year-old female presented with a 2 day history of generalized weakness, fatigue, dizziness and inability to walk without any history of loss of consciousness, seizure, headache, sensory loss, or bowel and bladder involvement. She had 18 years history of diabetes mellitus, 4 years history of coronary artery disease (angioplasty 4 year before) and 4 years history of left ventricular dysfunction (left ventricular ejection fraction; 20 %) . She was on telmisartan 40 mg since last 4 years. There was no history of any intake of non steroidal anti inflammatory drugs (NSAIDS), beta blockers and indigenous medicine. On admission, she was awake. Physical examination showed that her body temperature was 97.6 degrees F, blood pressure was 80/60mmHg, pulse was feeble with rate146 beats/min, bilateral pitting type mild pedal edema was present. No remarkable findings were observed in her chest and abdomen. The patient’s laboratory profile was as follows: hemoglobin: 10.7 g/dl, total leukocyte count: 4900/mm3, platelet count: 1.8 × 105/ mm3, urinary protein: 2+, urinary sugar: 1+, urine microscopy: white blood cell count: 1–2/high-power field, red blood cell count: 0/high-power field, urinary pH: –6.5, 24-hour urinary protein: 2.2 g/day, serum albumin: 2.34 g/dl, HBsAg: negative, anti-HCV: negative, HIV I and II: negative, blood urea: 85mg/dl, serum creatinine: 1.9 mg/dl, estimated glomerular filtration rate (eGFR) by chronic kidney disease - improved prediction equations(CKD-EPI): 23.5 ml/min/1.73m2 ,random blood sugar: 224 mg/dl, serum sodium: 143 mEq/l, serum potassium: 9.34 mEq/l, serum chloride: 112 mEq/l, albumin corrected serum calcium:9.32 mg/dl, serum PO4: 4.2 mEq/l, arterial blood gas: pH 7.24, pCO2: 28 mm Hg, pO2: 104 mm Hg, HCO3: 12.9 mEq/l, anion gap: 18.1 mEq/l (normal range: 10–12). The electrocardiogram showed sine-wave pattern of severe hyperkalemia (fig.1). Ultrasonography abdomen showed bilateral normal size kidneys with increased bilateral renal cortical echogenicity. 2D-Echocardiography showed ischemic dilated cardiomyopathy with left ventricular ejection fraction (LVEF); 30 %. Fundus examination showed evidence of diabetic retinopathy. Thus, the diagnosis of type 2 diabetes mellitus with diabetic nephropathy with diabetic retinopathy with ischemic dilated cardiomyopathy with acute kidney injury with high anion gap metabolic acidosis with acute severe hyperkalemia was made.
Treatment
We initiated conservative medical treatment in the form of intravenous 4.65 mEq of calcium gluconate, intravenous bolus of 10 units of regular insulin with 25 grams of dextrose and nebulization with 20 mg albuterol (5mg/ml) but her electrocardiogram did not normalize. Patient was put on inotropic support to maintain normal blood pressure. Repeat serum potassium was 8.2 mEq/L. Hemodialysis was initiated in the view of severe hyperkalemia and metabolic acidosis. After 30 minutes of initiation of hemodialysis she developed ventricular tachycardia. Successful cardioversion was done by delivering 200 joules of direct current (DC) shock and hemodialysis was completed. After first session of hemodialysis, her potassium was 5.8 mEq/Land changes of severe hyperkalemia in electrocardiogram were normalized (fig. 2). Next day serum potassium was 6.8 mEq/L and arterial blood gas analysis showed metabolic acidosis. Second session of hemodialysis was done. After second hemodialysis, serum potassium was 5.7 mEq/L. Fludrocortisones .1 mg was added in the view of hyporeninemic hypoaldosteronism. On fourth day of admission her serum potassium was 4.8mEq/L and serum creatinine was 1.6mg%. After one month of follow up, her serum potassium was 3.8mEq/L and serum creatinine was 1.0 mg% .
Discussion
Hyperkalemia can be caused by either decreased renal excretion or excessive leakage of potassium from the intracellular space (cell shifts). Besides it acute and chronic renal failure, hypoaldosteronism and rhabdomyolysis, are typical examples leading to hyperkalemia [10]. In our case patient hyperkalemia was acute and severe with serum potassium level 9.3 mEq/L. In the setting of normal renal function adaptive response includes an intact cortical collecting duct, normal mineral corticoid levels and adequate distal delivery of sodium [12].Renal adaptive mechanisms allow the kidneys to maintain potassium homeostasis until the glomerular filtration rate (GFR) drops to less than 15 ml/min/1.73 m2 [10]. But in our case patient eGFR calculated by CKD-EPI was 23.5 ml/ min/1.73m2. Acute hyperkalemia in our case patient was out of proportion to fall in eGFR .In patients with diabetes, decreased mineral corticoid activity is often an early finding due to hyporeninemic hypoaldosteronism. This is the reason, hyperkalemia in diabetic patient usually develops even after mild or moderate decrease in the GFR. Elderly patients may have decreased renal function even without significant increase in serum creatinine levels (< 1.2 mg/ dL) [16]. It is studied that after the age of about 30 years, the glomerular filtration rate (GFR) begins to decline at an average rate of 1 ml per year [17].The older age (especially after sixth decade) is independent factor, responsible for high prevalence of hyperkalemia [8, 16]. It is due to age-related declines in plasma renin activity and aldosterone, as well as aldosterone resistance at the level of the renal tubule [8]. That’s why elderly subjects are at risk to develop hyperkalemia, when the patients are on drugs that block the renin-angiotensin-aldosterone axis or interfere with distal tubular potassium secretion. Our case patient was 86 years old female and had history of telmisartan intake that might be additional risk factor for hyperkalemia. As compare to acute kidney injury, in predialysis CKD patients, loss of nephron mass is equilibrated by compensatory increase in the secretory rate of potassium in remaining nephrons, such that fractional excretion of potassium is increased [13]. However, in heart failure, increased aldosterone causes increased absorption of sodium in proximal tubules, resulting in its decreased delivery to the distal nephrons, which in turn, results in decreased potassium excretion [14]. In heart failure patients with renal failure, the prevalence of hyperkalemia can be up to 20% and is associated with an increased risk of morbidity and cardiovascular mortality [14,15]. Our case patient had four years history of left ventricular dysfunction and on echocardiography her LVEF was 30%. Shift hyperkalemia can cause hyperkalemia with no net increase in total body potassium. Example of shift hyperkalemia in diabetes mellitus is metabolic acidosis [16]. For each 0.1 fall in pH , there is increase in potassium by approximately 0.4 mmol/L [16]. Arterial blood gas analysis of our case patient showed pH 7.24, pCO2: 28 mm Hg, HCO3: 12.9 mEq/l and anion gap was 18.1 mEq/l. Our case patient had high anion gap metabolic acidosis. 86 years of age, diabetes mellitus, high anion gap metabolic acidosis of renal failure, use of the renin-angiotensin-aldosterone axis blocker and heart failure were collectively responsible for acute severe hyperkalemia in our case patient. Chronic hyperkalemia is caused by impaired renal potassium excretion and not by the cell shift. The electrocardiogram in a hyperkalemic subject can progress from normal to ventricular tachycardia and asystole in a precipitous manner [18]. Serum creatinine of our case patient was 1.9 mg/dl at the time of admission and serum potassium was 9.3 mg/dl. The electrocardiogram showed classical sine-wave pattern of severe hyperkalemia. Medical management for hyperkalemia did not normalize the electrocardiogram in our case patient and patient developed ventricular tachycardia during hemodialysis. But after completion of first session of hemodialysis, electrocardiogram showed sinus rhythm.
Conclusion
Acute hyperkalemia occurs due to cell shifts and chronic hyperkalemia occurs due to decreased renal potassium excretion. Acute severe hyperkalemia in elderly diabetic patients may occur out of proportion to fall in eGFR. If electrocardiogram does not normalize with the conservative medical treatment, hemodialysis should be initiated immediately for hyperkalemia irrespective of serum creatinine level.
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information: https://irispublishers.com/aun/fulltext/successful-resuscitation-of-an-elderly-diabetic-patient.ID.000527.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
0 notes
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
The Effect of Pre-Incision Urethral Plate Width and Granular Width on the Outcome of Tabularized Incised Urethral Plate Repair Surgery in Distal Penile Hypospadias, A Prospective Study
Authored by: Diaa-Eldin Taha
Abstract
Objective: To determine the cosmetic and functional outcomes of hypospadias repair in relation to the width of the urethral plate in addition to granular width and configuration.
Materials and methods: The study was a prospective evaluation of patients operated for hypospadias. The urethral plate width (UPW) and glans width (GW) of the patients were measured preoperatively using standard calipers. The width of the urethral plate was correlated to the cosmetic outcome (using hypospadias objective penile evaluation [HOPE]) and functional outcome (using the urinary stream) of hypospadias repair. All patients were managed via the same technique using Snodgrass tabularized incised plate repair (TIP). All operations were performed by a single surgeon. All intaoperative data were recorded. All patients were followed up for 1 year. Success was defined as slit shaped meat us at the tip of the glans with no stenosis, fistula or diverticulum.
Results: All 38 patients were evaluated at 6 months and 1 year follows up. The mean age at surgery was 4.5 ± 2.1 years. Overall, the mean ± SD of UPW was 10.92 ± 1.24 mm. a 24 patients (61.5 %) (Group A) had a urethral plate width of less than 8 mm while 14 patients (35.9 %) (group B) had a urethral plate width greater or equal to 8 mm. the mean ± SD of GW was 9.52 ± 1.56 mm. Success was documented in 36/38 patients (94.3%). The only complication was Fistula in two patients (6.7 %), glans dehiscence in three patients (10%). Success rate was not statistically different in correlation of UPW and GW (p=0.5). The only statistically significant difference between all patients was a longer operative time in the patients with deficient urethral plate compared to others with adequate urethral plate (p= 0.005). The urinary stream was straight in 32 boys and sprayed in 6. Overall, mean ± SD HOPE score was 39.1 ± 8.83. A significant correlation found between the cosmetic outcome of the two groups and HOPE score (p = 0.06).
Conclusion: The pre-incision urethral plate width and granular width was not correlated with the TIP outcome. A better HOPE score is associated with wide urethral plate.
Keywords: Hypospadias; Urethral plate; Tabularized incised plate repair (TIP); Hypospadias objective penile evaluation
Introduction
Dating the final 2 decades, tabularized incised plate procedure (TIP) for repair of distal penile hypospadias is the foremost common method at numerous institutions. In any case, a few downsides counting metal and/or neourethral stenosis and the require for standard urethral dilatation have been recorded [1]. The preservation of the urethral plate and the increase in the surface area with healthy epithelium give better outcome [2] TIP is a procedure that is more dependent on urethral plate quality in comparison with other surgical procedures. The plate quality is generally regarded as one of the intrinsic risk factors influencing the outcomes of hypospadias repairs. However, there is currently no clear agreement on the evaluation of the urethral plate [3].The urethral plate width was classified based on an arbitrary 8-mm cutoff value, while groove depth was graded as deep, moderate and shallow. However, is the arbitrary value of 8 mm suitable for all penis sizes? [4]. Generally, urethral plate width increases with penis size, as the patient grows. It might be more appropriate to evaluate urethral plate quality with a parameter scaled with penis size. In recent years, Glans–Urethral Meat us–Shaft score was proposed to classify the severity of hypospadias, providing a concise method for evaluating urethral plate quality [4,5]. There is a debate regarding the effect of UPW and GW on the postoperative complications post TIP surgery. Some reports have found that urethral plate (UP) widths <8 mm before TIP incision increased urethroplasty complications [6]. While, The UP width before incision did not increase urethroplasty complications [7-9]. Glans size does not correlate with age in patients with hypospadias between 3 and 24 months old, supporting the decision to operate as early as 3 months in some centers [10]. Small glans size, defined as width <14 mm, is an independent risk factor for urethrocutanous fistula [8]. To address this void, we aimed to answer a question, Is the UPW and GW are a controlling factors for hypospadias outcome as regard the functional and cosmetic outcome?
Materials and Methods
After approval from Institutional Review Board, we conducted a prospective study that was carried out in Urology department in kafr el sheikh university, between November 2018 and November 2019. A total of 60 children diagnosed with distal penile hypospadias were included. Inclusion criteria were, distal penile hypospadias, primary, uncircumcised, and no or mild chordee (less than 30°), aged < 10 years, No associated syndromes and boys able and willing to comply with follow up schedule. We excluded boys who were recurrent, circumcised, with severe chordee. written consent with detailed description of the operation and expected complications was explained and signed from the parents. All operations were performed by single pediatric urologists. Preoperative IV antibiotic prophylaxis was given. A circumferential sub coronal incision is made proximal to the hypospadiac urethral meat us. The penis is degloved. A bilateral longitudinal incision was made along the urethral plate to prepare the granular wings. The flap was obtained from the inner dartos muscle and sutured overlying the incision line with 6/0 vicryl. The flap width and length were differing in every case according to the location of the meat us, urethral plate characteristics and depth of the midline incision. Urethroplasty was performed using 6/0 Vicryl continuous subcuticular then interrupted sutures and 2nd layer cover using dartos fascia flap. Granular approximation was done with 6/0 Vicryl. 8F stent was kept for 7-10 days. All patients were routinely followed up for cosmetic and functional results at 3 months intervals. By routine examination of the external genitalia, evaluation of the voiding symptoms, uroflowmetery study was performed if possible and it was repeated when the voided volume was insufficient or when the result was inconsistent with the physical examination and history. Overall acceptable cosmetic appearance of the penis was decided according to the slit like appearance of the neo-meat us, the straight position of the penis and this cosmetic aspect was judged by an independent blinded observer. Hypospadias Objective Penile Evaluation (HOPE) is considered a valuable tool for assessing the outcome [11].
Statistical Analysis
Statistical analysis was performed with IBM Statistical Package for Social Sciences. IBM SPSS Statistics for Windows (version 22.0. Armonk, NY) was used to evaluate multiple steps. Significance level was set to p < 0.05. Internal consistency reliability was tested using Cronbach’s α, and test-retest reliability was assessed with the Wilcox on signed rank test. For concurrent external validity, Spearman rank correlation was used. For values > 0.70, it was assumed that there was sufficient consistency and reliability.
Results
1. All 30 patients were evaluated at 1 year of follow up. Mean age at surgery was 4.5 ± 2.1 years.
2. Of the 30 patients who had their distal hypospadias repaired using TIP, seven patients (23.3 %) had glanular hypospadias, nine patients (30 %) had coronal hypospadias and 14 patients (46.7 %) had distal penile hypospadias (Table 1).
3. Overall, the mean ± SD of UPW was 10.92 ± 1.24 mm. a 24 patients (61.5 %) (group A) had a urethral plate width of less than 8 mm while 14 patients (35.9 %) (group B) had a urethral plate width greater or equal to 8 mm. the mean ± SD of GW was 9.52 ± 1.56 mm.
Functional outcome
1. The average urine flow rates (Qmax) of 38 patients was 7 ml/sec (5.3-10.3).
2. A 20 (83.3 %) patients in group A have good urinary stream while 12 patients ( 85.7%) in group B have good urinary stream.
3. There was a significant correlation between good urinary stream with the mean UPW of the 2 groups (p<0.05).
Post-operative complications
1. Two patients (6.3%) developed urethrocutanous fistula, three patients (10 %) developed granular dehiscence.
2. Five patients (14.3%) in group A developed complications while one patients (16.7%) in group B developed complications.
3. However, no statistical significance found in relation of the complications to the mean UPW or GW of the two groups of patients (p = 0.5).
Cosmetic outcome
1. The cosmetic outcome was assessed using Hypospadias Objective Penile Evaluation (HOPE), as shown in Table 2 (Table 2).
Table 2: Outcome in correlation to UPW.
2. Overall, mean ± SD hypospadias objective penile evaluation (HOPE) score was 39.1 ± 8.83. Group A patients had a mean HOPE score of 37.2 ± 6.4 SD while Group B patients had a mean HOPE score of 42.4 ± 6.1 SD.
3. A significant correlation found between the cosmetic outcome of the two groups and HOPE score (p = 0.06).
Discussion
Hypospadias is an extremely common anomaly. There are different procedures that have been described for the adjustment of hypospadias since of the presence of various hypospadias presentations. Be that as it may, no single technique had 100% satisfactory result [12]. The goals of hypospadias surgery include development of a urethra of sufficient caliber and length, orthotropic meat us at the tip of the glans permitting the patient to void in a straight stream without maddening spreading. Moreover, obtaining a conical glans and rearrangement of the dorsal skin provides a uniform ventral skin cover and correction of penile curvature just to achieve proper sexual intercourse and effectively inseminate [13]. Hypospadias surgery is continuously evolving, since its description by Galen in the first and second centuries AD, to improve a suboptimal functional and cosmetic results. The aim of hypospadias surgery is the creation of a straight penis with a slitlike meat us at the tip of the glans 7. In spite of the recognition of the urethral plate as the tissue distinct from the glans and penile skin that would have formed the urethra and as having a well vascularized connective tissue and its incorporation in hypospadias repair, an objective way of assessing the impact of urethral plate on outcome is yet to be established. Snodgrass in 1994 reported his own technique of tabularized incised plate urethroplasty (TIP) repair for distal hypospadias that gained a widespread use for its perceived simplicity and good cosmetic outcomes in the majority of cases [11]. However, unfortunately, when the urethral plate is narrow the rate of urethrocutaneous fistula, metal/neo-urethral stenosis is increased [12]. In the current study, we evaluated the effect of width of the urethral plate and granular width on outcome of hypospadias repair. Most of our patients had coronal and midpenile hypospadias (38.5 %%), the same findings by Part et al [14]. The reason for this is not clear but might be explained by the geographical location. Hypospadias Objective Penile Evaluation (HOPE) which assessed the cosmetic outcome, there was a statistical significance correlation (p = 0.06). This finding agrees with the result from some previous studies [15]. However, Aboutaleb et al [6] in their study We used 8 mm in the present study because urethral plate width 8mm or greater is essential for creation of adequate neourethra and successful hypospadias repair [16],while, Da Silva et al1 [15] in their study had 41.9% of their patients in the narrow urethral plate group and 58.1% in the wide urethral plate group. Comparing both studies, the slight difference in percentages may be explained by the fact that Da Silva used 10 mm as the dividing line between narrow and wide urethral plates while we used 8 mm in the current study. Nguyen et al [9] and Aboutaleb et al [6] in their studies also used 8 mm as the dividing line. Urethral plate of more than 8 mm is associated with good cosmetic outcome [16, 17] On the assessment of the functional outcome, 20 ( 83.3 %) patients in group A had good urinary stream while twenty patients 12 ( 85.7%) in group B had good urinary stream. Statistical analysis showed that there is a statistically significant difference between the 2 groups (p value of 0.05). This agrees with findings of some other studies that concluded that narrow urethral plate is associated with poor functional outcome such as poor urinary stream and complications such as metal stenosis and urethrocutanous fistula [17-19]. However, Nguyen et al and Da Silva et al [15] in their study concluded that width of urethral plate do not affect the functional outcome of hypospadias repair. This is related to the fact that there were confounding variables in their study such as penile size, glans shape and vascularity of the prepuce which were not separately analyzed. We did not assess penile size, glans shape and vascularity of the prepuce in the current study. There are a diversity in the complications following hypospadias repair. It ranges from 6-30% [20, 21]. The most common complication we recorded was urethrocutanous fistula. These differences in complication rates may be explained by the differences in surgical expertise due to low volume of hypospadias repairs done per year in our setting. The rate of urethrocutanous fistula in our study is not correlated with narrow urethral plate, a similar to [20]. While, Aboutaleb reported higher incidence in fistula in patients with narrow urethral plates when compared to those with wide urethral plate [6-21]. Though this study was a prospective study, it was limited by a small sample size that hindered the significant statistical difference detection in complications. Moreover, single surgeon series cannot be generalized as the outcome of repair, including complications, may be related to the skill of the surgeon.
Conclusion
The pre-incision urethral plate width and granular width was not correlated with the TIP outcome. A better HOPE score is associated with wide urethral plate. However, the width of the urethral plate and glanular width may predict the functional outcome (urinary stream).
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information:
https://irispublishers.com/aun/fulltext/the-effect-of-pre-incision-urethral-plate-width.ID.000526.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
0 notes
Text
Iris Publishers_ Annals of Urology & Nephrology (AUN)
Understanding the Time-Course of Nephrolithiasis Management
Authored by: Seth K Bechis
Abstract
Purpose: The growing incidence of acute nephrolithiasis has increased the burden on healthcare. We sought to assess the time-course of acute stone disease treatment from symptom onset to spontaneous passage or definitive treatment to better characterize the current state of management and identify areas for improvement. Methods: We performed a retrospective review of patients treated for acute nephrolithiasis from August 2016 until February 2017. Patients were included if they had symptomatic renal or ureteral stones, evaluation by urology, and documented resolution by spontaneous passage or surgery. Primary outcome was the time from initial presentation at the Emergency Department (ED) to procedure or passage. Secondary outcomes included time to outpatient evaluation by urology and delays to procedure scheduling greater than 14 days. Results: 61 patients (41% female) met selection criteria. Median time from initial presentation to procedure or stone passage was 45 or 26 days, respectively. Median time from ED to clinic visit was 12.5 days. Time from clinic visit to procedure or spontaneous passage was 29 or 16 days, respectively. 38 patients (62%) had documented causes for delay in treatment. Of this cohort, 22 (58%) were due to provider availability issues, 8 (21%) had contraindications to surgery, and 8 (21%) had patient-related delays.
Conclusion: Prolonged time to treatment of acute nephrolithiasis occurred in 30 (49%) of the cohort due to provider availability and patientspecific delays. Developing initiatives to expedite management through improved patient education and operating room availability may help reduce healthcare costs and patient discomfort.
Keywords: Kidney stones; Time-course; Urolithiasis; Ureteroscopy; SWL; PCNL
Abbreviations: ACU: acute care urology, AUA: American Urological Association, ED: Emergency Department, EHR: Electronic health record, IRB: Institutional Review Board, MET: Medical expulsive therapy, NHANES: National Health and Nutrition Examination Survey, UC: Urgent Care
Introduction
The incidence of kidney stones has been noted to be 8.4% in the United States as of 2010, a dramatic increase from 5.2% in 1994 based on analysis of NHANES data [1]. The rising incidence, morbidity and cost of kidney stone disease place a major burden on the U.S. healthcare system [2,3]. Reducing healthcare costs and ultimately improving quality of care first requires an evaluation of the current status of urolithiasis treatment as well as identification of obstacles to care. Current data show an average 3.4 urologists per 100,000 persons in the U.S., with a substantial shift toward metropolitan regions and an estimated 38 million Americans living in counties without a single urologist [4]. This lack of availability of timely urologic care leads to costly repeat emergency department visits [5,6]. Our study aimed to assess, at a single tertiary care center, the time-course of nephrolithiasis treatment, from onset of symptoms and initial presentation to resolution either by definitive treatment or spontaneous passage. We hypothesized that time to treatment or passage was greater than 30 days.
Methods
We conducted a retrospective review of patients treated for nephrolithiasis at a single, tertiary academic center from August 2016 to February 2017. Under an IRB-approved protocol (#170854), medical records were reviewed for patients at least 18 years of age seen at the UC San Diego Health Comprehensive Kidney Stone Center. Inclusion criteria were history of symptomatic renal or ureteral stones (i.e., causing colic), presentation at a San Diego Emergency Department (ED), Urgent Care (UC) or other clinic, subsequent evaluation at our urology clinic, and documented resolution of their stone(s) by either spontaneous passage or surgical procedure. Spontaneous passage was confirmed via a submitted sample of a passed stone or subsequent imaging results. The primary outcome of the study was the time from initial presentation at the ED, UC or clinic to surgical procedure or spontaneous passage. Secondary outcomes included time from first ED or UC presentation to evaluation by urology, time from initial presentation to spontaneous stone passage, and delays in procedure scheduling greater than 14 days following first urology clinic appointment (designated as “delay in treatment time”). Fourteen days was set by institution as a goal to achieve in order to optimize patient care. Patients with delays in treatment time were included in sub-group analyses only if reasons for delay were documented within the electronic health record. In order to capture the entire time-course of a stone episode, patients were excluded from the study if by the end of the review period they had not yet had surgery to remove their stone(s), had not yet passed their stone(s) spontaneously, or were unsure of stone passage. Descriptive statistical analyses were performed.
Results
During the study period, 61 patients met inclusion criteria (see Table 1).
Median time from initial presentation to surgery or spontaneous passage was 45 or 27 days, respectively. The median time between initial presentation and first Urology clinic visit was 12.5 days. In total, the median time from the first appointment with Urology until resolution via a procedure or spontaneous stone passage was 29 days or 16 days, respectively, with 28 days overall. Of the total cohort, 38 study subjects (62%) waited greater than 14 days between the first Urology appointment and surgery (Table 3).
Analyzing this subgroup, the majority (22 patients, 58%) of the delays were due to provider availability issues (including operating room, staff, and/or surgeon availability). Another 8 patients (21%) were delayed due to contraindications to surgery. These included a positive pre-operative urine culture (2 patients); urosepsis (2); recent abdominal aortic aneurysm surgery and on anticoagulation (1); admission for small bowel obstruction (1); epididymo-orchitis (1); and ureteral perforation during initial urgent ureteral stent placement (1). Definitive treatment for 8 patients was delayed due to patient-related issues including missed clinic or imaging appointments or lack of call back to schedule their surgery.
Discussion
Our study aimed to assess, at a single U.S. tertiary care center, the time-course of nephrolithiasis treatment, from onset of symptoms and initial presentation to definitive treatment and follow-up imaging. We found that patients waited an average of 45 days until surgical treatment of their stones. This timeframe is clinically concerning given the risks of ED revisits for renal colic and/or infection as well as long-term risks of chronic kidney disease and ureteral stricture after 6 weeks [6-8]. The American Urological Association (AUA) guidelines for surgical management of urolithiasis provides a moderate recommendation for definitive stone management within 6 weeks, based on a 1973 study noting irreversible upper tract damage after this time frame [9]. Our data is in line with other studies in the literature. One U.S. group found that the median time from ED visit and/or stent placement to definitive stone intervention was 31.5 days [10]. In Canada, the mean wait time in 2011 for elective ESWL procedures nationally was 59 days [11]. A retrospective review of a 6 month period in the United Kingdom found a median time from ED visit and stent placement to stone intervention of 119 days, with only 3% receiving definitive procedure within 30 days [12]. This contrasts sharply with the British Association of Urologic Surgeons (BAUS) proposed target time of 4 weeks for definitive intervention in patients with acute stone presentations [12]. The most common reason 62% of patients waited more than 14 days for surgery was due to lack of provider availability or inability to access sooner operating room time. At our institution, surgical scheduling is based on a rigid block schedule that discourages non-urgent add-on cases. For example, each surgeon performs urological surgery on scheduled days of the month and open time for elective cases in between these blocks rarely exists. This makes scheduling patients with semi-acute but non-urgent stones challenging. Other healthcare systems with more flexibility may have improved access to surgical treatment. A recent population- based cohort study by Brubaker et al of over 15,000 patients discharged from an ED in California with a stone diagnosis found a median time from ED to stone surgery of 28 days [13]. Interestingly, patients with Medicare, Medicaid or self-pay coverage as well as Black or Hispanic race experienced a wait of up to 12 to 36 days longer, bringing the time to definitive treatment to 6 to 9 weeks. Our study complements this large dataset as we verify findings at a single institution similar to Brubaker et al. In addition, our study provides clinical granularity about reasons for delay that is lacking in administrative datasets. Implementation of protocols to enhance follow-up and expedite treatment of acute stone episodes is in its infancy but already shows significant promise to improve healthcare- associated costs as well as patient morbidity [10, 14]. The formation of an acute care urology (ACU) service at one New York hospital to facilitate timely evaluation and treatment of patients presenting to the ED with acute stone disease was found to reduce ED return visits and hospital readmissions [10]. At our own institution, measured institution goals for access to care exist, and enhancing access to surgery is an ongoing goal. Our study is not without limitations. It is retrospective in nature and focused on a small cohort at a tertiary referral center. In addition, we did not capture data about payer status, race or medical comorbidities. Therefore, it is possible that the surgical stone cases at our institution may be more complex and require more specialized care than cases found in the community. In addition, as mentioned previously, our current surgical scheduling model does not easily accommodate expedited surgical cases. However, the predominance of ureteral stones and gender equality amongst our patients with acute renal colic is in line with that of the greater population. Future research will be focused on prospectively following patients to further identify obstacles in accessing care.
Conclusion
In our study of the time-course of acute nephrolithiasis, we found that the time from initial presentation to stone treatment was prolonged primarily due to provider availability, challenges in accessing expedited operating room time, and patient factors. These data suggest that improving provider availability, perhaps by incorporating a dedicated operating room to enable faster access for stone surgery cases, is critical to improving the overall morbidity and outcomes of acute stone management.
For More Open Access Journals in Iris Publishers Please Click on: https://irispublishers.com/
For More Information: https://irispublishers.com/aun/fulltext/understanding-the-time-course-of-nephrolithiasis.ID.000525.php
#Iris Publishers#Iris Publishers LLC#Open Access Journals of Urology#Open Access Journals of Nephrology
0 notes