Text
Earth Day 2018 Celebration at SUNY Downstate Medical Center

Global Earth Day 2018 focuses on ending plastic pollution
By Jeanine Botta
SUNY Downstate School of Public Health MPH Student
Earth Day was founded on April 22, 1970 as a means of protesting the effects of pollution on humans and wildlife. Earth Day allows us to set aside time to honor the earth and the ecosystem, and to teach the public about environmental stewardship. Today Earth Day is celebrated around the world, and we've seen the development of Earth Week and even Earth Month. Earth Day celebrations include large, festive gatherings with entertainment, food, and hundreds of vendors, as well as recycling events, and educational sessions that may involve panel discussions and opportunities to gain knowledge and practical expertise in dealing with environmental issues.
The campaign for Earth Day 2018 is End Plastic Pollution. Earth Day Network, the nonprofit environmental organization that leads Earth Day globally, has devised a strategy with goals for developing a regulatory framework to reduce and eliminate plastic waste, which has affected human, animal, and marine life, and contributed to the burden of waste products that are not capable of being recycled. The organization features a broad range of campaigns.
Earth Day, Week, and Month feature hundreds of events of every size and theme throughout New York’s tri-state area, and there will be a great many places to recycle all kinds of materials, including difficult to recycle items, such as textile scraps and torn clothing. Below is a collection of events involving lectures, panel discussions, films, and related links. If you are on campus on Friday, April 20th, be sure to visit the 10th Annual Earth Day Event at SUNY Downstate Medical Center. Details are below.

From Brooklyn to Puerto Rico: A Just Recovery
April 18 from 6:00 to 8:00 p.m. at The New School
The Auditorium, Room A106, 66 West 12th Street, New York, NY 10011
The Tishman Environment and Design Center at The New School celebrate Earth Day 2018 by standing in solidarity with Puerto Rico and other communities impacted by damages of the 2017 hurricane season, including hurricanes Sandy, Harvey, and Maria. Elizabeth Yeampierre, Executive Director of UPROSE, will discuss root causes of natural and man-made climate justice disasters and describe the Just Recovery model emerging in Puerto Rico and the United States.
Free and open to the public. RSVP requested.
SUNY Downstate Medical Center Green Initiative’s 10th Annual Earth Day Event
April 20 from 11:30 a.m. to 1:30 p.m. at SUNY Downstate Medical Center
Atrium, 450 Clarkson Avenue, Brooklyn, NY 11203
Join SUNY Downstate School of Public Health students and faculty at their table in the Atrium, which will feature information about dealing with electronics waste, current research related to exposure to the plasticizer bisphenol A (BPA), and other environmental topics. Learn more about the Environmental and Occupational Health Sciences program, the Planetary Health Club, and Downstate’s Global Public Health Club.
Assuring a Habitable Earth
April 21 from 11:00 a.m. to 4:30 p.m.
The Trustees Pavilion at Ramapo College of New Jersey
505 Ramapo Valley Road, Mahwah, NJ 07430
An Earth Day project of Ramapo Green and The Center for Sustainability features speakers discussing climate change, fossil fuels, and potential loss of our planet’s habitability
Earth Day Weekend at the Ranch and many other GreenThumb Events and Workshops
April 21 from 12:00 to 2:00 p.m. at Smiling Hogshead Ranch
25-30 Skillman Avenue, Long Island City, NY 11101
Participants can join the New York Restoration Project and deliver free trees to New Yorkers to plant in their yards and community gardens. Events and workshops are free. RSVP is requested.
Brooklyn Center Presents the 11th annual National Grid Earth Day Celebration
April 21 beginning at 2:00 p.m.
Weeksville Heritage Center, 158 Buffalo Avenue, Brooklyn, NY 11213
Brooklyn Center and the Weeksville Heritage Center host an Earth Day event in Crown Heights featuring activities and learning games to educate families on ways that we can care for the Earth and invest in a sustainable future. This is a free event and requires no tickets or registration. Recommended for children ages four and up.
EarthFest at the American Museum of Natural History
April 22 from 10:00 a.m. to 5:45 p.m.
Central Park West at 79th Street, New York, NY 10024
This event’s climate themed films will be shown at 11:00 a.m. and 1:00 and 4:00 p.m.
Celebrate Earth – NYC 2018
April 22 from 1:00 to 3:00 p.m.
Castle Clinton Plaza, Battery Park
This event will feature musical performances and speakers on topics that include climate, justice, concerns about Indian Point, intelligent energy and conservation, health and sustainable energy, and breaking free from plastic. This event is free. Registration is requested.
Green and Equitable: Brooklyn and the Zero Waste Challenge
April 25 from 6:00 to 8:30 p.m.
Brooklyn Borough Hall, 209 Joralemon Street, Brooklyn, NY 11201
A panel of experts, including the Brooklyn Solid Waste Advisory Board, the Brooklyn Borough President’s Office, community organizers, and city government and resource recovery experts, will discuss Brooklyn's approach to waste management, and review successes, challenges, and opportunities in accomplishing New York City’s goal of Zero Waste to Landfill by 2030.
Free registration is required. Light refreshments will be provided.
Art in a Dark Time
April 26 from 7:00 to 8:30 p.m.
Silver Center, Room 300 (enter at 32 Waverly Place)
Grey Art Gallery, 100 Washington Square East, New York, NY 10003
Moderator Dale Jamieson, and speakers Yanoula Athanassakis, Robert Hopkins, and Joel Sternfeld address the challenge of living consciously and ethically in a dark time. This event is cosponsored by New York University’s Departments of Art History, Environmental Studies, and Philosophy, Environmental Humanities Event Series at the Center for the Humanities, and Grey Art Gallery.
Plastic Pollution Seminar
April 27 from 1:00 to 2:00 p.m.
Dorot Center for Seniors, 171 West 85th Street, New York, NY 10024
Melissa Elstein and Judith Weis, Plastic Free Waters Partership steering committee members, will discuss the plastic pollution crisis, how it affects us, and steps we can take to reduce our use of plastic products in their talk How to Reduce Our Single-Use Plastic Consumption and Why It’s So Important. To RSVP call Shannon at (917) 441-4743
0 notes
Text
Fatalism as a Barrier to Colorectal Cancer Screening in a New York City Russian-speaking Immigrant Community
By Irina Dekhtyar, PT, DrPH, MPH
Department of Orthopedic Surgery/Rehabilitation Medicine
University Hospital of Brooklyn
SUNY-Downstate Medical Center
To me, my Grandma was always the epitome of strength, resilience, and survival. She survived revolutions, famine, the horrors of World War II, an era of “developed socialism” and Gorbachev's Perestroika, the collapse of the Soviet Union, the mafia-infested realities of the 1990’s, and, finally, immigration to the United States. As if these challenges of her life were not enough, there was yet another battle my Grandma had to face: colon cancer. It is quite hard to describe everything she went through: multiple surgeries, pains and fears of post-surgical recoveries, but one aspect of her post-cancer life is worth mentioning: though an agnostic, she believed that it was predetermined for her to get sick with cancer. She used to say: “It was written for me in my book of life, I just don’t know why.”
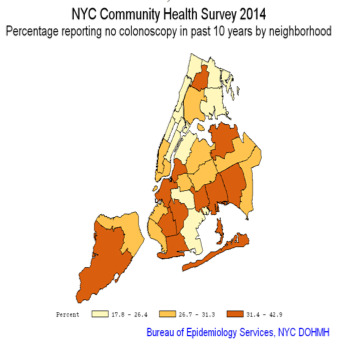
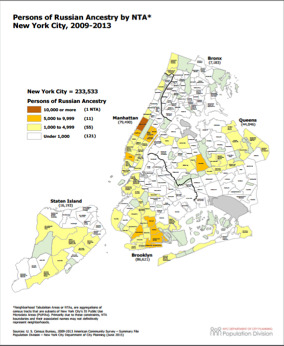
Colorectal Cancer (CRC) is the second most prevalent non-cutaneous malignancy in the US and one of the leading causes of death among both men and women. Two boroughs of New York City, Brooklyn and Staten Island, have the highest CRC - related mortality rates. The following maps illustrate the lowest rates of screening for CRC, particularly in southern Brooklyn and parts of Staten Island (left), and depict areas densely populated by Russian-speaking immigrants (right). The cluster of high mortality and low screening rates for CRC in the areas with large population of Russian-speaking immigrants may be indicative of high rates of undetected colon cancer in the Russian immigrant community since, when detected early, CRC is a preventable disease.
https://www.health.ny.gov/statistics/cancer/registry/pdf/volume1nycneighborhoods.pdf
There is a lack of information about screening preferences in the Russian-speaking immigrant community in the USA [1]. In 2015 -2016, I conducted a study to assess attitudes and beliefs about colorectal cancer (CRC), to discover factors affecting CRC screening behaviors among Russian – speaking immigrants living in NYC, and identify the most effective community-specific intervention methods to increase screening among this underserved population. I discovered several important factors affecting participation in CRC screening procedures in this population: lack of knowledge about CRC and screening modalities for CRC, mistrust toward the medical profession, and fatalism. In this blog, I would like to share my findings about the latter, the fatalism.
Fatalism is a complex concept but a familiar one in the public health research. As March was Colon Cancer Awareness Month, fatalism becomes particularly salient as it often one of the most frequent explanations for why adults delay or put off important screening tests. There is an extant body of research attributing low CRC screening rates in immigrants to the US to fatalism. The beliefs that there is no cure for cancer and that cancer is a “death sentence,” are found in many studies. A study in San Jose, Ca (2004), [2] described fatalistic attitudes and fear of cancer in the Latino and Vietnamese population [2]. Some Arab-American immigrants in New York reported the belief “that one’s prognosis was ultimately under God’s control and that God was the healer and source of solace and support.”[3]
In my NYC study, fatalism played a central role in the discussions of CRC screening among Russian-speaking immigrants in NYC. Fatalistic beliefs about cancer, such as the notion that the disease cannot be prevented and cured, were expressed by many participants, men and women alike. Several participants expressed that an individual gets sick with cancer because it is “predetermined” or “meant to be”. Many participants expressed their firm beliefs that there is no cure for cancer, that cancer is a “death sentence.” Throughout the discussions about screening for cancers in general and colorectal cancer in particular, time and again, fatalism appeared to be a significant factor affecting one’s decision to participate in screening activities. Many of the participants believed that cancer was a “punishment by God,” which was a very painful reminder of my late Grandma’s own conviction. The following are just a few verbatim quotes from some of the discussions:
“I think there is no cure. I mean, there are people who get chemotherapy, radiation therapy, but it just delays imminent deaths. There is no cure.” (male, 57)
We cannot change something that’s impossible to change.” (female, 54)
“I think if you are predetermined to get cancer, you will get it no matter what you do…Live your life and hope for the best” (female, 58)
“Cancer is a destiny for some people, so- to- say, it’s God’s punishment for sins. People have to pray to God. We all are in God’s hands. Everything happens for a reason…” (female, 52)
Interestingly, during the interviews, when required to say the word “cancer,” some of the participants changed their tone of voice to barely-heard whisper, while others tried their best to avoid saying “cancer” at all. Many of the participants, instead of saying the word “cancer,” said “It” or “swelling”. Several participants expressed feeling uncomfortable even talking about cancer. It was not a rare occurrence during the interviews when participants spit over their left shoulders exactly three times in fast succession and, in the same fast succession, knocked on the table they were sitting at (“wood”), when asked to talk about cancer-related issues.
The strong fatalistic attitudes toward cancer as well as the “taboo” meaning assigned to the word cancer suggests that a focused education campaign is necessary to dispel some of the misconceptions participants expressed about cancer and cancer screening. Even though the risks and benefits of the screening methods vary, there are compelling data supporting the notion that screening for colorectal cancer reduces the incidence of CRC by detecting and removing adenomatous polyps, precursors to CRC [4-6]. Early detection and removal of polyps leads to decreased morbidity of CRC in a population and decreased mortality from this disease. Inadequate use of screening modalities is a major contributing factor to CRC mortality [7]. Knowledge that CRC screening, if done early enough, can actually prevent and treat cancer (by removing polyps) would be an empowering step toward dispelling these long held beliefs.
My Grandma won the battle with colon cancer. She survived and lived a few more peaceful years until succumbing to advanced age and Alzheimer’s disease. Often, though, I think about the many people in the Russian-speaking community who die of colon cancer holding onto their false beliefs of predetermined and inevitable death from cancer, and those who refuse to undergo timely screening.
As my study revealed, besides fatalistic attitudes toward cancer in general and colon cancer in particular, lack of knowledge about the preventative nature of colon cancer, as well as lack of information about screening modalities, are the major barriers for screening. Through various educational activities, public health workers and experts in community outreach efforts need to devote their efforts to disseminate information in the Russian-speaking community regarding how to prevent colon cancer, and how to detect and treat it before it spreads.
Many lives can and should be saved through screening. Many people can thereby continue to be a part of a vibrant and diverse community of Russian-speaking immigrants while living healthy lives.
REFERENCES
1. Remennick, L.I., Preventive behavior among recent immigrants: Russian-speaking women and cancer screening in Israel. Soc Sci Med, 1999. 48(11): p. 1669-84.
2. Walsh, J.M., et al., Barriers to colorectal cancer screening in Latino and Vietnamese Americans. Compared with non-Latino white Americans. J Gen Intern Med, 2004. 19(2): p. 156-66.
3. Shah, S.M., et al., Arab American immigrants in New York: health care and cancer knowledge, attitudes, and beliefs. J Immigr Minor Health, 2008. 10(5): p. 429-36.
4. Winawer, S.J., et al., Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med, 1993. 329(27): p. 1977-81.
5. Bailey, C.E., et al., Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975-2010. JAMA Surg, 2015. 150(1): p. 17-22.
6. Winawer, S.J., et al., The National Polyp Study. Design, methods, and characteristics of patients with newly diagnosed polyps. The National Polyp Study Workgroup. Cancer, 1992. 70(5 Suppl): p. 1236-45.
7. Menon, U., et al., Beliefs associated with fecal occult blood test and colonoscopy use at a worksite colon cancer screening program. J Occup Environ Med, 2003. 45(8): p. 891-8.
0 notes
Text
Hypertension Health Crisis
More than 50% of Black Americans have High Blood Pressure
By Willie M. Abel, PhD, RN, FAHA
Assistant Professor of Nursing, The University of North Carolina at Charlotte
PRIDE-CVD Scholar Cohort 4
Heart disease is the leading cause of death for men and women in the United States with a higher death rate for Blacks (African Americans). The main risk factor for heart disease is hypertension, also called high blood pressure. Hypertension occurs when blood flows with a greater force through the blood vessels than normal causing them to constrict while creating a strain on the heart and damage to blood vessels. Uncontrolled high blood pressure not only damages the blood vessels (aneurysm), but it also damages the heart (myocardial infarction or heart attack, heart failure), brain (stroke, dementia), and kidneys (kidney failure).
Hypertension is particularly dangerous because it is considered a "silent killer" and develops slowly over time. Most people with hypertension do not know their blood pressure is high because they have no signs or symptoms and by the time they are diagnosed, their body is already damaged. Blacks in the United States have the highest prevalence of hypertension and tend to develop hypertension at younger ages than other racial/ethnic groups with higher blood pressures and worse disease severity. Thus, Blacks have higher rates of hypertension-related diseases such as heart attacks, heart failure, strokes, and kidney failure than Whites. The reasons for the elevated hypertension rates are not fully understood due to the disease state’s multifaceted nature, which is an interplay of genetics and physiology, cultural, psychosocial, socioeconomic, and environmental factors.
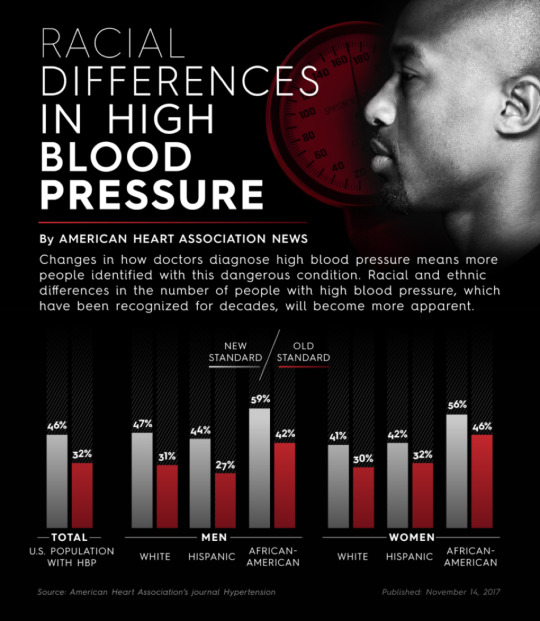
With the introduction of new high blood pressure guidelines, the already elevated prevalence of hypertension in Black men increases from 42% to 59%, and in Black women from 46% to 56% as compared to rates in the 40% range for Whites and Hispanics, indicating epidemic proportions (see American Heart Association chart on racial differences). Hypertension is widespread and not well controlled, which negatively affects health outcomes across our society.
Under the new guidelines, a diagnosis of hypertension is indicated if the blood pressure is equal to or greater than 130/80 mm Hg instead of the former guideline recommendation of 140/90 mm Hg (see blood pressure category below). As hypertension diagnoses escalate, the prescription of antihypertensive medications will increase for blood pressure control with aims to reduce cardiovascular disease and mortality.
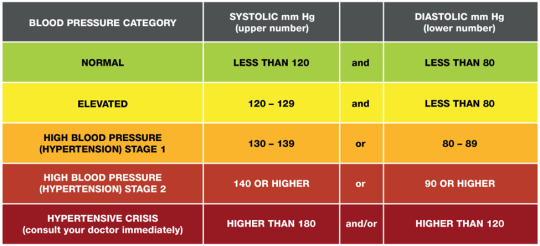
Knowing your blood pressure numbers is a must to determine if your blood pressure is normal or elevated, therefore it is best to have your blood pressure checked. If your blood pressure is elevated, lifestyle modifications (see chart below) should be implemented and your blood pressure monitored regularly to detect if the lifestyle changes you implement are working.
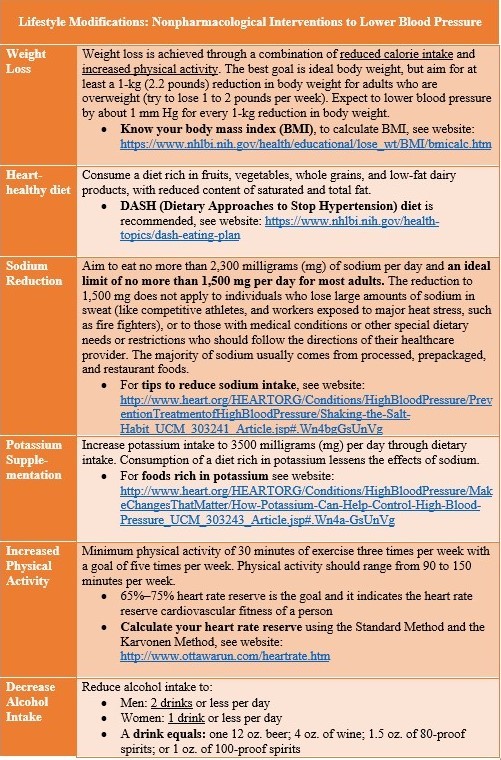
Body mass index (BMI) calculator website: https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm
DASH (Dietary Approaches to Stop Hypertension) diet website: https://www.nhlbi.nih.gov/health-topics/dash-eating-plan
Tips to reduce sodium intake website: http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/PreventionTreatmentofHighBloodPressure/Shaking-the-Salt-Habit_UCM_303241_Article.jsp#.Wn4bgGsUnVg
Foods rich in potassium website: http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/MakeChangesThatMatter/How-Potassium-Can-Help-Control-High-Blood-Pressure_UCM_303243_Article.jsp#.Wn4a-GsUnVg
Heart rate reserve calculator website:
http://www.ottawarun.com/heartrate.htm
If your blood pressure continues to Stage 1, and no cardiovascular disease risks (see chart below) exists, lifestyle modifications will continue. However, if your blood pressure is Stage 1 with cardiovascular risks, antihypertensive medication will be prescribed along with continued lifestyle modifications. For stage 2 hypertension, you will be treated with a combination of lifestyle modifications and two different types of antihypertensive medications. If your blood pressure is in the hypertensive crises range, you should see your health care provider immediately for prompt evaluation and treatment. For all states of hypertension, the blood pressure should be monitored by a health care provider monthly initially, to evaluate treatment response.
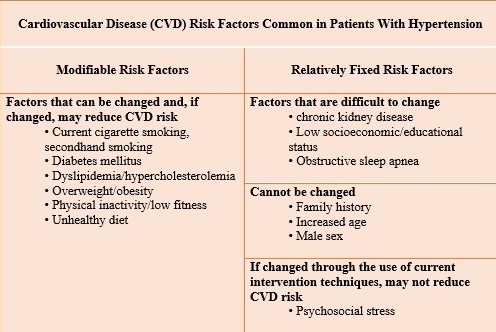
Hypertension cannot be cured, but it can be managed. Keeping the blood pressure at a normal level will reduce the risk of disabling diseases and death associated with uncontrolled blood pressure. Once started on antihypertensive medication, it is likely to be a lifelong course, in order to maintain blood pressure control. You should never stop or change your medication dosage or schedule without consulting your health care provider. Both lifestyle modifications and medication work better together than taking prescribed medication alone.
If you do not have hypertension, it is best to prevent it by engaging in healthy lifestyle behaviors. If you have been diagnosed with hypertension, then you need to work with your health care provider to manage your blood pressure. Become an active participant in your health care. Take time to learn about hypertension, the risks involved, how you contributed to the risk, and the role you need to play with risk reduction. Learn the name of your antihypertensive medication and how it works to lower your blood pressure. Actively engage in open communication with your health care provider to clear up any misperceptions about hypertension. Establish your role in the decision-making process as an informed participant. Together with your health care provider, address your individual needs, control your blood pressure, and improve your health status.
It is imperative that the hypertension epidemic is controlled before it escalates further. Frequent communication between the health care provider and the patient is key. Home blood pressure monitoring technology opens the door for better monitoring of the effects of antihypertensive medication and lifestyle modifications allowing a more rapid response to adherence issues and uncontrolled blood pressure. Real-time electronic monitoring of blood pressure, physical activity, weight measurements, etc. may provide valuable data to the health care provider. Monthly office visits with virtually no communication between visits does not allow for stringent blood pressure control. Technology has the potential to motivate both the health care provider and patient to become real partners in achieving blood pressure control and positive cardiovascular health outcomes.
References:
American Heart Associaiton News. (2017). More than half of all African-Americans have high blood pressure under new diagnostic guidelines Retrieved from https://news.heart.org/half-african-americans-high-blood-pressure-new-diagnostic-guidelines/
Pickering, T. G. (2001). Why are we doing so badly with the control of hypertension? Poor compliance is only part of the story. Journal of Clinical Hypertension, 3(3), 179-182. doi:10.1111/j.1524-6175.2001.00465.x
Whelton, P. K., Carey, R. M., Aronow, W. S., Casey, D. E., Jr. , Collins, K. J., Himmelfarb, C. D., . . . Wright, J. T., Jr. . (2017). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. Hypertension. doi:https://doi.org/10.1161/HYP.0000000000000065
1 note
·
View note
Text
Do We Dare Disturb the Universe?
By Jeanine Botta, School of Public Health MPH Student
Planetary Health comes to Downstate’s School of Public Health
Every February, the New York League of Conservation Voters releases its Environmental Scorecard, which tallies bill sponsorships and voting records of City Council members. If a Council member receives a perfect score, that means that he or she introduced legislation associated with the environment, or voted on every environmental legislative issue, or a combination of such measures.
In theory, if enough New Yorkers voted, this calculus could measure the environmental health of any given council district. But as recent election statistics show, most New Yorkers do not exercise their right to vote. Because of this, there is no environmental scorecard measuring variables like litter, noise, traffic congestion, and other factors that are needed to produce a robust environmental report that reflects objective data and residents’ views. Using the League’s tally as it currently exists, it is possible for a district to have a perfect score while their streetsare strewn with litter,teeming with traffic noise, and too congested to safely accommodate cyclists.The Environmental Scorecard also doesn’t reflect Council members’ receptivity to complaints from constituents about environmental issues.
How would Brooklyn residents in the areas surrounding Downstate rate their environment? How would they rate their quality of life? Do perceived environmental concerns and quality of life affect their decisions about outdoor activities and leisure time spent outside?
The recently formed Planetary Health Club is looking at these questions as its members develop an environmental quality of life survey. Intended for the neighborhoods surrounding SUNY Downstate Medical Center School of Public Health, the survey will focus on neighborhood residents’ subjective perception of their environment and how it impacts their quality of life and likelihood to participate in outdoor activities.
The Planetary Health Club was formed in July of 2017, and has the distinction of being the first such student club in the world. With the help of the Planetary Health Alliance, this club is beginning to connect with other Planetary Health initiatives across the globe.
What is Planetary Health?
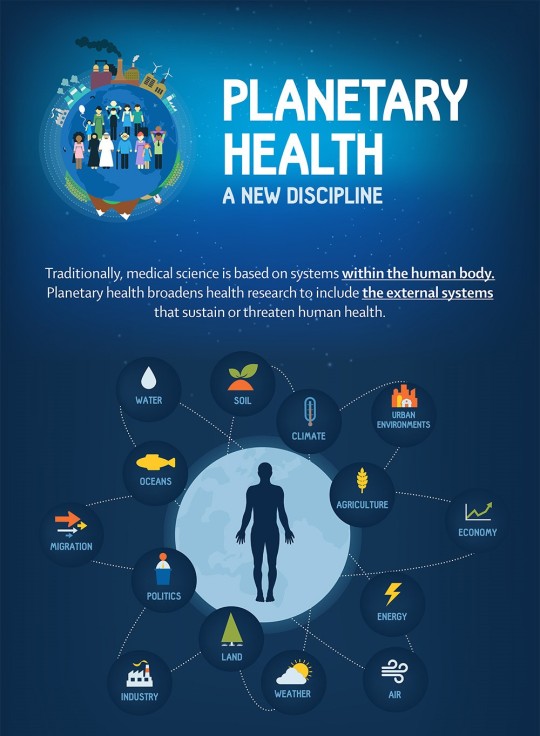
Image via The Lancet (expanded citation below)
This relatively new academic discipline takes an interdisciplinary approach to public health and environmental stewardship.
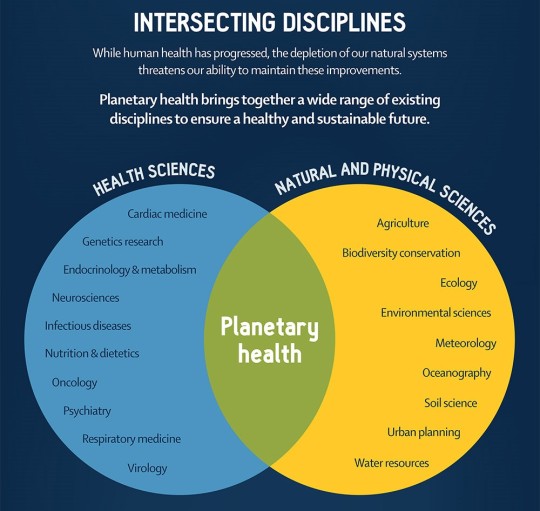
Image via The Lancet (expanded citation below)
To a public health student or practitioner, this might mean incorporating green cover within plans for a community garden to reduce exposure to mosquitoes, rather than relying on chemical repellants.
To a medical student or physician, this could mean advocating with city agencies to have more curb cuts incorporated within residential areas so that disabled people could more easily navigate the streets and enhance their independence.
To a nursing student or diabetes educator, this might involve developing a nutrition themed walking tour of local eateries with a focus on following a healthy diet while dining out.
To an architect, the planetary health perspective could mean hiring an acoustical consultant to analyze exterior sound elements before the design phase, and to advise about interior space before and during construction of a new healthcare facility.
On an individual or family level, the planetary health perspective could mean using a thermos rather than contributing to bottled water waste.

Image via The Lancet (expanded citation below)
Planetary health draws on a multitude of disciplines with a common goal of improving human health while taking responsibility for the effects of mankind’s activities on nature and ecosystems including marine life – indeed, the effects on all living creatures and all natural habitats.

Phoenix Community Garden is one of more than a hundred such green spaces developed in Brooklyn through the efforts of Open Space Greening. Community gardens exemplify the multidisciplinary approach of the planetary health perspective, as well as the cascade of benefits that can result from such an approach. The garden yields almost 2,000 pounds of vegetables, beans, and herbs, including enough to serve more than 500 people a day at a nearby soup kitchen. Many community gardens were built on vacant land, and their creation results in community involvement, educational opportunities, and provide the chance to interact with nature in a peaceful oasis in the middle of an urban setting.
In recent years, research on reduction in violent crime as a result of developing green space on formerly vacant lots has shown promising results.
Image via The Lancet (expanded citation below)
Downstate’s Planetary Health Club would love to add to its membership, and welcomes students from every discipline at the University. We understand hectic schedules, and plan our meetings accordingly.
Our next meeting will take place on campus, and is tentatively scheduled for the fourth week in January. If you’d like to attend a meeting to check it out and see if it could be for you, contact Kirsten Weisbeck at [email protected].
Related Links
www.nyenvironmentreport.com/conservation-group-releases-environmental-scorecard-for-city-council
https://council.nyc.gov/districts
http://www.ufoa.org/statistics/maps/brooklynSmall.jpg
https://www.reefill.com/single-post/2017/08/09/Bottled-Water-Waste
http://www.downstate.edu/bhr/reports/Community-Health-Report.pdf
https://www.rockefellerfoundation.org/blog/planetary-health-global-also-local
https://www.politico.com/agenda/story/2017/09/13/planetary-health-challenges-000514
https://planetaryhealthalliance.org/
1 note
·
View note
Text
AIDS Outreach Heads to the Barbershop
By Alan Dorsinville
Downstate SPH Student
The Barbershop Talk with Brothers (BTWB) program was born out of a necessity to address high rates of HIV transmission in Brooklyn, NY. In 2011, Black men had the highest rate of diagnosis for HIV among all ethnic groups. And within New York City, neighborhoods in Central Brooklyn including Bedford-Stuyvesant and Crown Heights had some of the highest rates of HIV in the city. In response to this growing public health issue, many programs over the years have developed interventions to target high risk groups such as injection drug users and men who have sex with men. However, there were few programs targeting heterosexual men, who at the time made up almost a quarter of HIV transmissions. It was out of this need Dr Tracey Wilson developed the Barbershop Talk with Brothers program as an HIV prevention program for heterosexual, non drug using Black males in Central Brooklyn.
Dr Tracey Wilson has an extensive research background in HIV/STD behavioral interventions and the social, cultural and psychological factors involved. Her goal with her research and this program was to understand the reasons behind this high rate of HIV transmission among Black heterosexual men and implement an intervention that would reduce these rates. While HIV prevention programs do exist, they often take place in STD clinics which only reach a small fraction of this population. In an effort to reach a greater number of males, she decided to bring the program to them in places that they already frequent. Barbershops are just the place as they play a central role in in African American communities, especially in Brooklyn. The relationship between barbers and their clients and the culture of open dialogue made barber shops and ideal place to provide HIV prevention and education to heterosexual men of all ages.
The program set up shop in East Flatbush, Flatbush, and Bedford-Stuyvesant, which are all neighborhoods with some of the highest incidence rates of HIV among Black males. Through evidence and community based interventions, this program sought to reduce individual risk and empower the community to support better health for its members. The barbershops were trained to bring up the program and motivate their clients to attend a three module program. These sessions covered health promotion and community health. By emphasizing HIV’s effect on the community as a whole, it helped participants understand HIV transmission as a public health and community issue and empower them to tackle this as a community. It also trained participants on how to share this information with others and practice safe behavior. In the end, BWB was a successful alternative to clinic-based HIV prevention for this population. By collaborating with barbershops and working within the community, it was able to disseminate information in communities that were at high risk of contraction. Specifically, the program improved participants’ attitudes and self-efficacy towards condom use, as well as reduce risky behavior. They were also successful in increasing perceptions of community empowerment. The Barbershop Talk with Brothers Program is one example of how SUNY Downstate is working with the community to tackle major health issues.

1 note
·
View note
Text
The Daunting Numbers Behind Pre-Diabetes
By Emeregildo Clark, Jr.
Downstate School of Public Health Alumnus
Diabetes is the seventh leading cause of death in the United States. To some that may not stand out as a staggering number, to diabetes and public health experts it is. It takes years of uncontrolled diabetes and mismanagement of the disease to lead to complications and death.
Unlike type 1 diabetes, which is called juvenile or early onset diabetes, type 2 diabetes is totally preventable. Type 2 diabetes is considered a lifestyle disease, therefore one can take note of their current lifestyle and see what the barriers to a healthier life are. But you can’t be a type 2 diabetic without first being a part of the 86 million pre-diabetics walking the country at this moment. I guess you have to start somewhere.
Now that should be a staggering number to anyone who looks at it. I just mentioned that diabetes is the seventh leading cause of death in the United States. What would happen if all of the 86 million pre-diabetics I just mentioned developed diabetes? That seven-spot on the charts might leap frog to six, five, or even 4.
I’ll give you an even more staggering number: 9 out of 10 of those 86 million pre-diabetics have no idea of her or his diagnosis. How might we combat this huge and growing public health issue? The National Diabetes Prevention Program (NDPP) developed by the Centers for Disease Control is one answer. Awareness of this program is growing, but to fight the prevalence of pre-diabetes, spreading the word about the DPP needs to be more aggressive.
The NDPP is a year-long program comprised of 16 weekly core sessions and 8 months of post-core sessions. During this time the participating pre-diabetic is given instruction on healthy eating, physical activity, and food tracking. An emphasis is placed on fat and the participants are taught and encouraged to count their fat grams.
To be eligible for the program the participant must have an A1c of a 5.7-6.4, which is considered within the pre-diabetic ranges. The goal of the program is for participants to lose 5-7% of their starting body weight. Accomplishing this will lead to the other goal of ultimately decreasing the participants A1c under the 5.7 starting point, which takes them out of the pre-diabetic stage.
In my experience as a pre-diabetic lifestyle coach, I have seen this happen numerous times. In my current Diabetes Prevention Program, I have participants that have already reached their 5 and 7% weight loss goals before the 16 weeks were up. Remember, NDPP is a year-long program, so that represents significant success. I also have a participant who lost 20 pounds before the 16 weeks were up and lowered his A1c substantially. He still has the post-core phase to complete and is already ahead of the curve. This is just a snapshot of how impactful the NDPP can be on the pre-diabetic population, the incidence of diabetes, and the overall healthcare cost burden in the United States.
To learn more about the National Diabetes Prevention Program (NDPP) you can go to the program’s website here, for all the information you need regarding this great lifestyle program. The NDPP works and the more providers, employers, states, that know about it, the farther the reach and impact the program will have.
3 notes
·
View notes
Text
Health and the New Urban Agenda
By Aimee Afable
Assistant Professor of Community Health Sciences
“Health as the pulse of the new urban agenda” was the theme of the 14th International Conference on Urban Health (ICUH) which took place in the town of Coimbra, Portugal September 26-29, 2017. The Conference was a continuation of the dialogue that began during the UN Conference on Housing and Sustainable Development in Quito, Ecuador in October 2016, which prioritized the UN Sustainable Development Goals 3 “Ensure healthy lives and promote well-being for all” and 11 “Make cities inclusive, safe, resilient and sustainable”. The 2017 ICUH was a global exchange of knowledge on how to integrate health into the practice of urban planning and design. The conference hosted 600+ stakeholders from 65 countries representing public health, economic development, industry, transportation, healthcare delivery, and many other sectors. This diversity was a testament to the urgency of creating multi-sectoral solutions to the challenges we face in our increasingly urban world.

The urban population has doubled in the last two decades. Today, 54% of the world lives in cities and by 2030, it is projected that 60% of the world will be living in cities. Because cities bring together large groups of diverse people in close proximity they can bring on profound environmental, economic and social change. However, that change may signal both progress and adversity, particular when change is rapid and unanticipated. Cities promise opportunities for upward mobility, innovation, but also unbridled consumerism, housing shortage, greater income inequality and shifts in lifestyle that may be detrimental to health – all trends that challenge the sustainability of modern cities. A worrying example of the latter is the recent growth in non-communicable disease worldwide.
Today obesity is considered by many as a 21st century epidemic and its growth worldwide has been attributed to rapid forms of urbanization. Continued rural to urban migration has led to a continuing convergence of lifestyle patterns around the world. Implicated in this process is what is known as the nutrition transition, first described by economist and nutrition researcher, Barry Popkins. Popkins documented greater consumption of processed foods, animal fats, simple sugars, and total energy intake and a shift to more sedentary occupations and forms of transportation. For the first time, we live in a world where there are more obese than underweight people. Obesity is a major driver of healthcare costs around the world as it associated with several diseases, including type 2 diabetes. Currently 415 million people worldwide have diabetes and two out of 3 of this total live in cities.
Not surprisingly, there has been increased scholarship in the development of an urban health theoretical framework to move toward a shared understanding of how populations are adapting to rapid urbanization. However, much of the discussion in urban health has overlooked the experience of cities in the US, particularly its largest city – NYC, a city of 8.5 million people. The presentations and plenary sessions at the 2017 ICUH in Coimbra reflected the experiences of cities in low and middle-income countries, which makes sense given that most of the rapid urban growth is happening in this part of the world. Of the world’s 31 megacities (that is, cities with 10 million inhabitants or more) in 2016, 24 are located in the less developed regions or the “global South”. China alone was home to six megacities in 2016, while India had five. However, how can the experience of older cities in the “global North” inform our understanding of the development and fate of the younger cities of today? Further, how are old and young cities different and how are they similar? What are the shared experiences and how can they contribute to common solutions?

The lived experiences of city residents will likely vary according to each city’s demography, geography and social diversity. Megacities, defined as cities with over 10 million residents, provide dramatically different experiences when compared to smaller cities of 1-2 million. Thus, NYC, a city of 8.5 million residents is moderate in size when compared to other cities worldwide. Also the rate of population growth must be considered. Between 2000-2016 NYC’s population remained nearly static whereas the Raleigh (NC) area more than doubled its population from 550,000 to 1.2 million in the same time period. Similarly, both Raleigh and NYC will have distinct experiences from Chongqing, China which went from mid-size to megacity in the same time period and Tokyo, the largest megacity in the world (over 38 million in 2016), but similar to NYC, had nearly static growth in the same time period. NYC has a reputation of being one of the wealthiest cities in the world (only second to Tokyo with regard to GDP), making assimilation and entry into the labor market more challenging. As a consequence, it is one of the most unequal cities of the world; the top 5% makes 88 times more than the bottom 20% in NYC. The city suffers from systemic differences in health status across different social groups. In NYC, Blacks and residents of high poverty areas die from diabetes at more than twice the rate of whites and more affluent residents. Finally, perhaps due to its unique geography bounded by water to the west, south and east, connected to mainland US only through its northern most borough, the Bronx, it does not experience the urban sprawl that characterizes many of the younger cities of the world.
Therefore, can NYC, as unique it may be, contribute to dialogue on sustainable urban development? What lessons, if any, can we offer to cities around the world? As students of public health living in NYC we cannot deny the central roles of place, race, and poverty in health and we recognize more and more that solutions to health inequities must consider the broad social determinants of health. The 2017 ICUH in Coimbra shifted the framework and passed the lens to urban planners, asking them to imagine how they would practice urban design differently if they considered health equity as a prerequisite for sustainable cities. How would you reimagine our city to achieve this same goal of health equity?
1 note
·
View note
Text
You Are What You Eat … Kinda
By Julia Mullins, Downstate School of Public Health DrPH (EOHS) Student

Christine Hurckes, a member of the OSI group, a large privately owned company offering aid and guidance to food facilities, said that “one scenario that is all too familiar is waiting for positive data to drive changes in design. That is attacking Listeria after it has crossed enemy lines … way too close for comfort. Don’t wait for positive data to start making changes. Don’t wait for the enemy to get that close.” As a food microbiologistworking for the United States Food and Drug Administration (1), I am confronted with the validity of this statement daily. I have witnessed firsthand the rollercoaster ride of the public when responding to a foodborne outbreak: the high anxiety of avoiding the types of food products as they climb the hill, the rush of panic as they realize they or their families may have consumed this product as they hang over the edge of that hill, and the relief once they feel the worst is over. They cycle through this ride over and over again. Picture this scenario that I am sure we have all experienced:
You return home from a nice dinner at the end of a long week and lay down on your couch to catch up on some TV. After binge watching the three episodes of Law and Order that you missed, you start to feel a grumble in your stomach. You ignore it for a bit, but after hearing that second famous Law and Order ‘chung-chung’ sound at the beginning of your fourth episode, you have to run to the bathroom like a hurdle jumping Olympian. This is the first of many visits you will be making to the bathroom that night and probably all the next day or so. But then, just as suddenly as it comes, it goes away, and you return to your already scheduled programming.
This is not an unlikely occurrence in our everyday lives unfortunately, but it is even more unfortunate that incidents like this go unreported. According to the FDA’s public website, there are an estimated 48 million cases of foodborne illness annually, which equates to about 1 in 6 individuals falling ill each year. These illnesses are then estimated to result in over 120,000 hospitalizations and about 3,000 deaths each year. That’s why, like the detectives on Law and Order, food microbiologists need to carefully investigate imported and domestic food products and facilities to identify the culprit.
The most likely cause of the under-reported food poisoning instances is Salmonella which typically only cause’s severe enough medical issues to seek medical treatment in immunocompromised individuals; however, bacteria such as Listeria and Enterohemorrhagic E.coli (EHEC) are much more dangerous to the general population. The names of these bacteria are probably familiar to you, but ask yourself – what you really know about them?
The FDA’s website is a great resource for recall and outbreak tracking, information about scientific advancements in food safety, laws and regulations, and anything else you would like to know in regards to food safety. You can even sign up for emails, text messages and alerts so you always have the most up-to-date information on what foods are being recalled at any particular time or get the most recent outbreak information here and here. The bottom line is that there is a ton of information out there to help you protect your family and communities food supply; you only need to know where to look.
According to the FDA’s website, and pretty much every single scientific textbook and website I have ever read, Salmonella is especially of concern for the young, elderly, and individuals with weakened immune systems. Healthy people who suffer from Salmonellosis, or an infection with Salmonella, suffer from classic food poisoning symptoms which usually self-resolve fairly quickly. However, if the bacterium finds its way into the blood stream because an individual’s immune system is too weak to fight it off, much more severe infections such as endocarditis may occur. These photos show a microscopic view of Salmonella and a visual culture of Salmonella on a special plate called Hektoen Enteric agar which causes most Salmonella to turn black.
In general, E.coli is a bacterium that is part of our normal flora, or normally lives in the intestinal tract of humans and animals. Most of these species of bacteria are harmless; however pathogenic, or disease causing E.coli such as EHEC (Enterohemorrhagic E.coli), can cause very severe and even fatal illness.Symptoms of this type of foodborne infection are the classic food poisoning symptoms, only much more sever and usually coupled with bloody diarrhea. One of the most famous examples of this type of fatal infection is the Jack in the Box outbreak of 1993 that was outlined in a New York Times article (4). This particular outbreak resulted in the tragic death of a two year old boy, whose father I had the honor of meeting at the North East Regional Retail Food Protection Seminar in 2015. After the death of his son, he decided to dedicate his life to keeping his son’s memory alive, sharing his story, stressing the importance of food safety and the laws that govern it. These photos show a microscopic view of E.coli on the and a visual culture of E.coli on a special plate called EMB agar that gives E.coli a distinctive green sheen to help identify it on the right:
Another very dangerous bacterium, and the one that I am most personally interested in studying and preventing, is Listeria. The most formidable species of Listeria is Listeria monocytogenes. It is very dangerous and extremely resilient, which causes it to be an even larger cause for concern in the food safety world. It is able to survive in refrigerated temperatures that will typically kill most other types of bacteria, and can be found in many other ‘ready-to-eat products’ such as poultry, seafood, meat and practically all dairy products. Pregnant women are one of the most susceptible groups to infection by this type of bacterium. Listeria is able to cross the placental barrier and may cause the fetus to spontaneously abort. That is the main reason pregnant women are told to avoid many types of food such as soft cheese and deli meats. These warnings should be taken very seriously. These photos show a microscopic view of Listeria and a visual culture of Listeria on a special plate called Chrome agar that gives Listeria a distinctive blue color to help identify it on the right:
Now that I have successfully scared you away from eating (for the next few hours at least), let me tell you want you can do to protect yourself and your family. First and foremost, educate yourself! Stay up to date on recalls and outbreaks and take all reports you may read about them very seriously. Also, learn the suggested temperatures for cooking and actually use a thermometer to ensure you are reaching those temperatures. See here for safe cooking guidelines from the Academy of Nutrition and Diabetics and www.foodsafety.gov.
Food microbiologists, no matter if they are working in a private or public industry, are all endeavoring to identify food that contain these nasty bacteria; however, the sad truth is that there is no best way to keep up with all the products that are imported into the country daily, that are grown or manufactured domestically, and the facilities that prepare, package or ship these products. That’s why identifying trends and targeting our search is so important. There are many methods that scientists all over the country are using to do this. The one that I am currently involved in is one of the most advanced pieces of technology, known as Whole Genome Sequencing, which is detailed on the FDA’s website as well.
Whole Genome Sequencing is a process that uses the DNA of bacteria, such as Salmonella and Listeria, to differentiate between different species of organism, as well as determine how closely two organisms of the same species are related to each other. The ultimate goal of using this technology is to build a database that can be used to more quickly identify organisms responsible for food borne illness, as well as better identify, track, stop and prevent outbreaks. By using a combined database, such as Genome Trakr, these bacteria found in foods even have the potential to be matched to clinical isolates also uploaded to the database by clinical microbiologists. Another goal of using this technology is to better public health by tracking these possible outbreaks geographically and using evolutionary biology to predict root sources of contamination for various food products; this way a harmful ingredient or condition can be stopped before the food product even enters the market.
The applications for the use of this technology in food supply protection are endless and new technologies and strategies are being developed constantly. Other potential applications include determining the effectiveness of a facilities cleaning and sanitization procedures, determining how organisms that could make us ill survive in the environment and the cooking process, or even using the technology to determine a pathogens antimicrobial or antibiotic resistance. We are extremely fortunate to live in a country where we have a general expectation of safety when it comes to the food we eat; however, there are definitely precautions we need to take to ensure our food supply stays that way. A US Senator from Nebraska, Mike Johanns, said it best, “Food safety involves everybody in the food chain.”
(1) All information and opinions stated are of my own and not reflective of the views of the agency. All information used can be found on the FDA’s public website, www.fda.gov.
1 note
·
View note