Text
New Interventional Orthopedics Atlas
Writing a textbook is an enormous undertaking. In creating a first of its kind, comprehensive textbook in Interventional Orthopedic Procedures, authors Williams, Sussman and Pitts have established a new benchmark in the field. Congratulations to its authors for their dedication, foresight and commitment to the advancement of Interventional Orthopedics.
What Is Interventional Orthopedics?
Interventional Orthopedics is a new medical specialty that utilizes the unlimited potential of PRP, bone marrow concentrate and other substrates in the treatment of common orthopedic conditions. To better understand the field and its importance please click below.
youtube
The New Groundbreaking Publication
Atlas of Interventional Orthopedics Procedure: Essential Guide for Fluoroscopy and Ultrasound Guided Procedures is the first comprehensive textbook that provides easy to follow, step by step guidance on spinal and peripheral joint injections. It provides practical content in one authoritative, user-friendly text. It is abundantly illustrated and easy to read. It reviews the basics of both ultrasound and x-ray imaging along with the different injectable therapeutic options such as PRP, bone marrow concentrate and adipose. There are dedicated chapters for the cervical, thoracic, and lumbar spine in additional to all the major peripheral joints. An advanced section covers important topics that include treatment of problematic calcified tendons, release of trigger finger, ultrasound guided excision of bone spurs and intraosseous injections.
The Authors
Dr. Christopher Williams
Dr. Williams is a United States Airforce veteran and graduate of Emory University School of Medicine. He completed his residency in Physical Medicine at Emory University along with a Fellowship in Interventional Orthopedics at the Centeno-Schultz Clinic. He is board certified in Physical Medicine.
Dr. John Pitts
Dr. Pitts graduated from Vanderbilt University School of Medicine and completed his residency in Physical Medicine at Emory University. He completed his fellowship in Interventional Orthopedics at the Centeno-Schultz Clinic. He joined the staff thereafter and has been the director of the fellowship program. He is a highly skilled, board-certified physician that has blessed our staff and community. If you are ever in our Broomfield clinic and hear a loud, deep laughter that makes you smile that is Dr. Pitts. This is his signature laugh. We, like the patients love it.
Dr. Walter Sussman
Dr. Sussman is a board-certified physician in physical medicine and rehabilitation with sports medicine fellowship. He is in private practice in Boston.
Gentleman,
Congratulations!
from Centeno-Schultz Clinic https://centenoschultz.com/new-interventional-orthopedics-atlas/
0 notes
Text
Shoulder Arthritis: All You Need To Know
The pain started as a small ache and now has progressed. You don’t recall any specific injury. Conservative care including rest, ice and heat have failed to provide any significant or sustained relief. Your doctor is concerned about shoulder arthritis. What is shoulder arthritis? What are the basic parts of the shoulder joint? What are the different types of shoulder arthritis? What are the most common symptoms of arthritis in the shoulder? What are the risk factors for shoulder arthritis? What are common treatment options for shoulder arthritis? When should you contact your doctor? How is shoulder arthritis diagnosed? What regenerative treatment options exist for shoulder arthritis? Let’s dig in.
Shoulder Arthritis
The shoulder is a truly remarkable joint. It allows you to reach out into virtually all directions: overhead, forward, and backwards. The shoulder joint allows us to reach overhead with heavy weight, grab the water out of the refrigerator, snake our belts through the pant loops, tuck our shirts in and perform pushups or burpees on demand. It is the unique structure of the shoulder joint that allows these motions. Unfortunately, like other joints in the body the shoulder is susceptible to irritation and injury. Osteoarthritis is the most common cause of disability in the United States, affecting up to 32.8% of patients over sixty years of age (1). Shoulder arthritis is a common condition estimated to be as high as 16-20% in the middle aged and elderly population (2). Shoulder arthritis can compromise range of motion, strength and be a source of debilitating pain. This blog will review the shoulder.
Shoulder Anatomy Basics
The shoulder is composed of the following:
Ball-Socket Joint: The head of the long bone of the arm (humerus) fits into a boney socket called the glenoid. It is a shallow joint which allows for the tremendous range of motion.
Secondary Smaller Joint: The collar bone joins the acromion to form the acromioclavicular joint (AC Joint). This is much smaller joint than the ball-socket joint discussed above. It is essential for scapular range of motion and function.
Ligaments: Ligaments are thick bands of connective tissue that connect bone to bone. The major shoulder ligaments are the superior, middle and inferior glenohumeral ligament and the coracohumeral ligament.
Tendons: Tendons are thick bands of connective tissue that connect muscle to bone. The rotator cuff is compromised of 4 tendons and is critical to the stability and the function of the shoulder.
Arthritis can cause injury to the ball socket or AC joint leading to joint damage, cartilage injury, restriction in range of motion and pain.
What Is Arthritis In The Shoulder?
Not all arthritis is the same. There are many different forms of arthritis. The most common include:
Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune disease. This means that immune system attacks its own healthy cells including the shoulder joint. It can also affect other tissues in the body causing problems in the lungs, heart and eyes. The most common symptoms are pain, swelling, tenderness and restriction in range of motion.
Osteoarthritis
Osteoarthritis is the most common form of arthritis. It is commonly referred to as “wear and tear” arthritis. Cartilage is thin, very strong connective tissue that covers the bones in a given joint. Cartilage allows for smooth, pain free motion of a joint. Osteoarthritis involves the breakdown of the cartilage resulting in pain, swelling and restriction in range of motion. Shoulder arthritis has been demonstrated to affect up to 32.8% of the patients over the age of sixty (3). The prevalence of shoulder osteoarthritis increases with age and women appear to be more susceptible than men.
Post-Traumatic Arthritis
Post-traumatic arthritis develops after an traumatic injury to the joint. As opposed to osteoarthritis which develops slowly over time, post traumatic osteoarthritis can develop months to years after the injury. It causes approximately 12% of all osteoarthritis cases and mainly affects younger adults (4).
Avascular Necrosis
Avascular necrosis also known as osteonecrosis is a severe medical condition in which the bone tissue dies. That is right, the bone dies. That was originally thought to be due to a lack of blood supply but other important factors are what contribute to this condition. It is most common in the hip but is also present in the shoulder joint. Risk factors for avascular necrosis include trauma, steroid use and excessive alcohol use.
Rotator Cuff Arthropathy
Rotator cuff arthropathy is a specific type of shoulder degeneration that develops over time after the rotator cuff is damaged. Arthropathy is a term that refers to any diseased condition in the joints. It can involve peripheral joints such as the shoulder as well the facet joints in the spine. Rotator cuff arthropathy affects females more than males and is common in the later decades of life. It is classified according to the severity of the damage ( Type 1 A-Type IIIB). The most common symptom is pain, restriction in range of motion and weakness. Diagnosis is made by physical examination and plain x-ray. The latter is significant for narrowing of the shoulder joint space and upward movement of the arm bone (humerus) in relation to the socket (glenoid)
Symptoms of Arthritis In the Shoulder
Shoulder arthritis typically is gradual in onset. Symptoms can vary from patient to patient depending upon the severity of the arthritis and other co-existing conditions. The most common symptoms of shoulder arthritis include:
Pain in The Shoulder Joint
Pain is the major sign of arthritis. It can be intermittent or constant.
Typically deep in the joint
Pain can also be located on the top of the shoulder in cases of AC joint arthritis.
Night pain is common
Pain may be aggravated by lifting, carrying heavy objects, overhead activities and exercise.
Limited Range of Motion
Normal shoulder range of motion may be restricted.
Difficulty raising arm over head
Difficulty with self-care (combing hair and dressing)
Swelling
Swelling is another sign of shoulder arthritis progression.
Loss of cartilage typically leads to inflammation and joint swelling
Swelling can increase after activity.
Tenderness
Shoulder and or AC joint may be tender to the touch
Tight or compression clothing may cause shoulder irritation
Tenderness and pain may limit use of shoulder
Crepitus (Grinding Sensation)
Popping, grinding or clicking is common
May or may not be painful
Shoulder may lock up due to loss of cartilage
Risk Factors for the Development of Shoulder Arthritis
There are a number of risk factors that have been identified for the development of shoulder arthritis. The most common include;
Advancing age
Shoulder arthritis prevalence rates increase with age from 1.8% in people in their 40’s to 27.5% in those in their 80’s (5).
Genetics
Unfortunately some of us carry that old family gene that predisposes us to degenerative conditions such a shoulder arthritis.
Obesity
This is in part explained by the increased load placed on the shoulder joint in patients with increased body weight.
Excessive Mechanical Loading
Powerlifting, training with heavy weights and repetitive shoulder motions required by some professions can lead to shoulder arthritis.
Shoulder Instability
Stability of the shoulder joint is imperative for optimal joint health and function. Shoulder instability due to ligament laxity or rotator cuff injuries can lead to shoulder instability. In such cases there is excessive motion of the arm bone (humerus) in relation to the socket leading to damage to the cartilage.
Fractures
Fractures can directly damage the cartilage leading to post traumatic osteoarthritis.
Rotator Cuff Injuries
The rotator cuff is compromised of four tendons that stabilize the shoulder, enable elevation and rotation of the shoulder and hold the arm bone (humerus) snuggly into the shoulder socket (glenoid). The four tendons are the supraspinatus, infraspinatus, subscapularis and teres minor. Injuries to the rotator cuff can compromise the stability of the shoulder leading to shoulder arthritis.
Inflammatory Arthritis
Inflammatory arthritis is a group of diseases caused by an overactive immune system. This is also called an autoimmune disorder in which the body attacks it own healthy cells. Examples include rheumatoid arthritis (RA), psoriatic arthritis, juvenile idiopathic and ankylosing spondylitis (AS) and gout.
Common Treatment for Arthritis of the Shoulder
Treatment options for shoulder arthritis depend upon the type and severity of the arthritis. When appropriate conservative care should always be the first step. The most common treatment options include:
Natural Treatments
Examples would include rest, activity modification, heat, ice, Tylenol and safe anti-inflammatory medications such as good quality fish oil and turmeric.
Traditional Non Surgical Treatments
Physical therapy. The Centeno-Schultz Clinic has a fantastic Physical Therapist with years of clinical experience.
Oral or injected steroids
Nonsteroidal Anti-inflammatory medications such as Ibuprofen
Surgical Procedures
When conservative therapy and rest fail to provide significant benefit patients are often referred for surgical consultation. There are a large number of orthopedic surgeries for shoulder arthritis. The specific surgery is dependent upon a number of different factors. The most common surgeries for shoulder arthritis include:
Arthroscopy
Arthroscopy is a minimally invasive surgical procedure in which a small camera is inserted into your shoulder joint to evaluate, diagnose and treat problems inside the joint. The procedure is typically performed in an outpatient setting and takes 30-60 minutes.
Hemiarthroplasty
A hemiarthroplasty is a partial shoulder replacement in which the ball portion of the arm bone (humerus) is replaced with an implant. This surgical procedure is indicated in severe cases of shoulder arthritis in which only the ball socket is damaged.
Shoulder Replacement (Arthroplasty)
Total shoulder replacement surgery involves surgically removing both the ball and socket portion of the joint and replacing it with artificial implants. The most common indication is severe shoulder arthritis in patients with compromised range of motion who have failed conservative therapy. The two most common types of replacements are the total shoulder replacement and the reverse shoulder replacement. Both are major surgeries associated with risks that include infection, failure, bleeding, persistent pain, nerve damage and implant fracture or displacement.
When Should You Consult Your Doctor?
Shoulder pain and limited range of motion can be debilitating. In many cases it can be due to overuse and typically gets better in several days. You know the weekend warrior events or over zealous workouts that trigger your shoulder pain. If however the pain and restriction persists, it is time to consult your doctor. Common symptoms that warrant a call to your doctor include:
Persistent redness
Persistent swelling
Severe Pain
Continued restriction in range of motion despite conservative care and rest
How to Diagnose Shoulder Arthritis?
Not all shoulder pain is due to shoulder arthritis. It is important to establish a correct diagnosis. The diagnosis of shoulder arthritis starts with a comprehensive evaluation with your doctor. The duration of the shoulder pain, its severity, aggravating and alleviating factors will be identified along with any events that may have triggered it. Past medical history is also important such as previous trauma, surgeries or co-existing problems such as diabetes.
Physical examination will include range of motion, shoulder strength and specific shoulder tests that evaluate the rotator cuff and labrum. The tests should include both shoulders in addition to a complete neurologic examination to ensure that shoulder weakness is not arising from an irritated or compressed nerve in the neck.
Radiographic studies will include an x-ray. Additional tests such as an MRI are often required. The MRI is a remarkable imaging study that can evaluate the rotator cuff tendons, labrum and cartilage surfaces.
At the Centeno-Schultz Clinic an in-office ultrasound is performed. Ultrasound is a powerful imaging modality that can provide immediate evaluation of the stability of the shoulder joint and integrity of the rotator cuff tendons, biceps and AC joint. No need to wait for lengthy pre-approval process required by insurance companies for an MRI or CT scan. Ultrasound in most cases can provide immediate information for the patient and the physician alike.
Regenerative Treatment Options for Shoulder Arthritis
The physicians at the Centeno-Schultz Clinic are experts in the evaluation and treatment of shoulder injuries and arthritis. We offer a comprehensive approach that is referred to as the SANS approach.
It stands for Stability, Articulation, Neurologic and Symmetry.
Stability is a very important, often overlooked issue that when compromised can lead to popping, cracking of the shoulder in addition to injury to the rotator cuff tendons and cartilage.
The shoulder is a shallow ball socket joint. It is held in position by the supporting ligaments and muscles. In some cases through trauma or loose ligaments, the ball portion of the shoulder can be dislocated or pulled out or socket. Why is this important? Once dislocated, the shoulder capsule can become stretched out or loose predisposing the shoulder to chronic instability. This is illustrated below.
Normal shoulder movement is illustrated on the left. Shoulder instability is illustrated on the right. Note there is excessive movement within the shallow shoulder socket that allows the ball portion of the joint to strike and injure the little gray triangle which is the labrum. Shoulder instability can lead to labrum injury and shoulder osteoarthritis.
Neurologic issues are also an important but often overlooked. At the Centeno-Schultz Clinic we always evaluate the patient as a whole a opposed to focusing only on the shoulder. The cervical spine is included in the examination as many cases of “shoulder pain” are actually pain being referred from an irritated or injured cervical facet or disc.
Treatment options vary depending upon the specific injury, its severity and presenting symptoms. Treatment options include PRP and bone marrow concentrate which is rich in stem cells. Both are powerhouses of healing.
The injections are demanding and require a thorough understanding of the shoulder anatomy. All injections are performed under ultrasound or x-ray guidance, or both. These injections can not be performed by your PCP or orthopedic surgeon. To watch one of my ultrasound guided shoulder injections please click on video below.
youtube
In Conclusion
Shoulder osteoarthritis is a common cause of pain and disability.
The shoulder is a shallow ball socket joint supported by ligaments and tendons. There is a second, larger joint called the AC joint.
There are many different forms of shoulder arthritis which include Rheumatoid, Osteoarthritis, Post-Traumatic, Avascular Necrosis and Rotator Cuff Arthropathy
The most common symptoms of shoulder arthritis include pain, limited range of motion, swelling, tenderness, and crepitus.
Risk factors for the development of shoulder arthritis include advancing age, genetics, obesity, excessive mechanical loading, shoulder instability, fracture, rotator cuff injuries, and inflammatory arthritis.
Common treatment options include conservative care, steroids, and surgery.
Symptoms that warrant a call to your doctor include persistent redness, swelling, pain and restricted range of motion that has not responded to rest and conservative care.
Diagnosis of shoulder arthritis starts with a thorough history and physical examination and radiographic studies such as an x-ray or MRI.
In-office ultrasound is a powerful, convenient imaging modality that can accurately access the integrity of the shoulder.
Regenerative treatment options include the use of PRP and bone marrow concentration that allows patients use their own cells to accelerate healing and forgo life changing shoulder surgeries.
If you or a loved one has ongoing shoulder pain that has not responded to conservative care please schedule a telemedicine consultation. A board certified, fellowship trained physician will review your history, imaging and discuss appropriate treatment options.
Persistent shoulder pain, swelling and restricted movement is a warning signal that you have a problem that warrants evaluation. If ignored, the injuries can progress often times causing permanent, irreversible changes. Avoid the pain and suffering and learn what the issues are and what regenerative options are available.
________________________________________________________________
1.Chillemi C, Franceschini V. Shoulder osteoarthritis. Arthritis. 2013;2013:370231. doi:10.1155/2013/370231
2.Ibounig T, Simons T, Launonen A, Paavola M. Glenohumeral osteoarthritis: an overview of etiology and diagnostics. Scand J Surg. 2021 Sep;110(3):441-451. doi: 10.1177/1457496920935018. Epub 2020 Jul 14. PMID: 32662351.
3.Chillemi C, Franceschini V. Shoulder osteoarthritis. Arthritis. 2013;2013:370231. doi:10.1155/2013/370231
4.Punzi L, Galozzi P, Luisetto R, et al. Post-traumatic arthritis: overview on pathogenic mechanisms and role of inflammation. RMD Open. 2016;2(2):e000279. Published 2016 Sep 6. doi:10.1136/rmdopen-2016-000279
5.Kobayashi T, Takagishi K, Shitara H, Ichinose T, Shimoyama D, Yamamoto A, Osawa T, Tajika T. Prevalence of and risk factors for shoulder osteoarthritis in Japanese middle-aged and elderly populations. J Shoulder Elbow Surg. 2014 May;23(5):613-9. doi: 10.1016/j.jse.2013.11.031. Epub 2014 Feb 20. PMID: 24561177.
from Centeno-Schultz Clinic https://centenoschultz.com/shoulder-arthritis-all-you-need-to-know/
0 notes
Text
ACL Tear Treatment Without Surgery: Our New Publication!
It all happened so suddenly. You were running down the field and made a quick cut. You heard an audible pop followed by searing knee pain and then collapsed to the ground. Your doctor thinks your tore your ACL and has referred you to a surgeon. What is the Anterior Cruciate Ligament? What is the function of the ACL? Are there different types of ACL injuries? What is ACL surgery? What are the risks associated with ACL surgery? Are there ACL tear treatments without surgery? What are their results and have they been published? Let’s dig in.
What Is the Anterior Cruciate Ligament (ACL)?
The knee has four major ligaments which are illustrated to the right. They include:
Anterior Cruciate Ligament (ACL)
Posterior Cruciate Ligament (PCL)
Medial Collateral Ligament (MCL)
Lateral Collateral Ligament (LCL)
The Anterior Cruciate Ligament (ACL) extends from the thigh bone (femur) to the shin bone (tibia) and limits forward and rotational movement of the knee. It is a key stabilizer in the knee. It is composed of two separate ligament bundles which include the Anterior Medial and the Posterior Lateral.
What Is the Function of the Anterior Cruciate Ligament?
The ACL is a major stabilizer of the knee that limits forward movement of the Femur on the Tibia (shin-bone)(1). It also restrains rotation of the Tibia.
Are there Different Types of ACL Injuries?
The ACL is the most commonly injured ligament in the body and occurs at an estimated incidence of 200,000 cases per year. However not all ACL tears are the same. It is important to know the specific type of tear. There are three principal types of ligament tears: partial thickness, complete thickness, and complete thickness with retractions
Partial Thickness Tear
This is where a portion of the ligament is torn.
Full Thickness, Non-Retracted Tear
This is a more severe injury. The tear extends across the entire surface of the ligament but the ligament is still held together by small remaining fibers.
Full-Thickness Retracted Tear
This is the worst-case scenario. The tear extends across the entire surface of the ligament and the ligament itself rips apart like a rubber band. The single ACL ligament is ripped apart with two ends that are no longer connected. A full-thickness, retracted ACL tear requires surgery.
What Is ACL Surgery?
ACL surgery is a major surgery that involves cutting out your torn ACL and replacing it with a GRAFT. What is a graft? It is a tissue taken from one site that is used in a different site in the body. The grafts themselves are not ligaments but rather are tendons taken from other areas of the body. There a 4 different types of grafts used in ACL surgery (3). They include:
Hamstring Tendon Graft
The Hamstring is the large muscle in the back of the thigh.
Patellar Tendon Graft:
The Patellar tendon is the large tendon in the front of the knee that connects the knee cap to the shin.
Quadriceps Tendon Graft
The Quadricep is the large muscle in the front of the thigh.
Cadaveric Tendon Graft
A cadaver is an individual that has died but has given permission to use their body tissues for medical use. They may be young or old, female or male.
Note that all the grafts used in ACL surgery are tendons and NOT ligaments.
What Are the Risks Associated with ACL Surgery?
ACL surgery is a major surgery that involves removing the damaged ligament and replacing with a patient’s tendon or cadaveric graft. There are significant risks associated with the surgery that include:
66% of teens who undergo ACL surgery will get Arthritis by age 30 (2).
Compromised positional sense and strength (3).
Increased risk of graft rupture for patients younger than 20 years of age (4).
Hamstring atrophy in patients who undergo a hamstring graft (5).
Knee instability
Diminished performance. Many professional athletes fail to return to their pre-surgery level of performance. Are there Alternatives to ACL Surgery?
ACL Tear Treatment Without Surgery ?
The Regenexx Percutaneous ACL Repair (Perc-ACLR) procedure is an advanced x-ray guided procedure where a patient’s own bone marrow concentrate which contains stem cells are injected into the damaged/torn ACL. It is a great ACL tear treatment without surgery option. Stem cells are your body’s own powerhouses of healing and can coordinate cells throughout the body to assist in the reorganization and healing of ligament injuries. We have published our results in two peer-reviewed journals (6)(7). MRI images of the ACL prior to and following bone marrow concentrate treatments have demonstrated profound healing. To review pre and post-procedure MRIs please click on the video below.
youtube
New Centeno-Schultz Clinic Publication
The Centeno-Schultz Clinic is excited about our newest peer reviewed publication. Publication is part of our commitment to advancing the field of Orthobiologics. We have a large number of publications which sets us apart from other clinics. To see the list of our publications please click here.
Our newest publication is a midterm analysis of patients with ACL tears that underwent x-ray guided injections of bone marrow concentrate and platelets into the ACL tears. Bone Marrow Concentrate is rich in stem cells. 50 patients were randomized into one of two groups: exercise therapy vs treatment group. Patients were 18-65 years of age with MRI evidence of ACL tear and pain or instability despite 3 months of conservative therapy. Pain and function were assessed at baseline and 1, 3, 6, 12 and 24 months. Results: Patients treated with Bone Marrow Concentrate injections had significant improvement in pain and function in comparison to the exercise group. In addition, they had significant improvement in their post treatment MRI scans consistent with healing.
Patients with ACL tears now have a non-surgical treatment option and can avoid the risks and extensive downtime associated with surgery and rehabilitation.
To learn more about non surgical treatment of ACL tears using your own cells, please click on the video below
youtube
In Summary
The Anterior Cruciate Ligament (ACL) is one of four major ligaments in the knee.
The ACL is a major stabilizer of the knee that limits forward movement of the Femur on the Tibia.
There are three principal types of ligament tears: partial thickness, complete thickness and complete thickness with retractions.
ACL surgery is a major surgery that involves cutting out your torn ACL and replacing it with a graft.
Major risks associated with ACL surgery include early onset knee Arthritis, compromised positional sense, graft rupture, Hamstring shrinkage and knee instability.
Regenexx Percutaneous ACL repair is an advanced x-ray guided procedure where a patient’s own bone marrow concentrate which contains stem cells are injected into the damaged/torn ACL.
Our newest peer reviewed publication demonstrated reduction in pain and improved function and post procedure MRI scans in patients treated with bone marrow concentrate in comparison to the controls.
Regenexx Percutaneous ACL repair is an alternative to ACL surgery and allows patient to avoid the risks associated with surgery.
If you or a loved one has sustained an ACL tear, please schedule a telemedicine consultation. Surgery is associated with long-term risks including graft rupture and then need for future surgeries. Learn from a board certified, fellowship trained physician your nonsurgical, regenerative treatment options.
1.Noyes FR. The function of the human anterior cruciate ligament and analysis of single- and double-bundle graft reconstructions. Sports Health. 2009;1(1):66-75. doi:10.1177/1941738108326980
2.Barenius B, Ponzer S, Shalabi A, Bujak R, Norlén L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014 May;42(5):1049-57. doi: 10.1177/0363546514526139. Epub 2014 Mar 18. PMID: 24644301.
3.Bączkowicz D, Skomudek A. Assessment of neuromuscular control in patients after anterior cruciate ligament reconstruction. Ortop Traumatol Rehabil. 2013 Jun 28;15(3):205-14. doi: 10.5604/15093492.1058410. PMID: 23897997.
4.Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014 Mar;42(3):641-7. doi: 10.1177/0363546513517540. Epub 2014 Jan 22. PMID: 24451111.
5. Snow BJ, Wilcox JJ, Burks RT, Greis PE. Evaluation of muscle size and fatty infiltration with MRI nine to eleven years following hamstring harvest for ACL reconstruction. J Bone Joint Surg Am. 2012 Jul 18;94(14):1274-82. doi: 10.2106/JBJS.K.00692. PMID: 22810397.
6. Centeno C, Markle J, Dodson E, et al. Symptomatic anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow concentrate and platelet products: a non-controlled registry study. J Transl Med. 2018;16(1):246. doi: 10.1186/s12967-018-1623-3.
7.Centeno CJ, Pitts J, Al-Sayegh H, Freeman MD. Anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow nucleated cells: a case series. J Pain Res. 2015;8:437-47. doi: 10.2147/JPR.S86244.
from Centeno-Schultz Clinic https://centenoschultz.com/acl-tear-treatment-without-surgery-our-new-publication/
0 notes
Text
Pain in Left Side of Neck: Causes and Treatment Options
It started as a low grade ache and has now progressed to a constant burn. Conservative care and medications have failed. Why is there pain in the left side of your Neck? How does the pain in the left side of Neck feel? What may be causing the Neck pain? What is the diagnostic process? What are the treatment options for pain in the left Neck? What are the Regenerative treatment options? Let’s dig in.
Understanding What’s Behind the Pain in Left Side of Neck
Almost everyone has experienced a sore or stiff Neck at some point. The overall prevalence of Neck pain ranges from 04. to 86.8% of the general population (1). Read more to learn the signs, symptoms, causes of treatment options for pain in the left side of Neck.
Why Is There Pain In The Left Side of Your Neck?
Neck pain can arise from a number of different conditions. Common causes of minor, intermittent Neck pain include fatigue, improper sleeping position, stress and overactivity. If neck pain persists it is a warning sign that you may have a problem that warrants investigation. Think of it as the red engine light on your car. It is warning that if left unchecked can progress to serious and expensive consequences.
What Does the Pain in the Left Side of the Neck Feel Like?
Neck pain can present in a number of different ways. Location and severity can very from patient to patient depending upon the injury and past medical history. Common examples include:
Neck stiffness
Sharp-shooting pain on the left side of the Neck
General soreness on the Neck area
Limited range of motion and flexibility
Headaches
Lightheadedness
Muscle tightness and spasm
Localized pain at the base of the skull
Possible Conditions Causing The Pain
Pain in the left side of the Neck can arise from many different sources. It is important to understand and identify where the pain is arising from. In doing so the best treatment plan can be started. Common causes of Neck pain include:
Cervical Disc Injury
Sandwiched between the boney building blocks in the Neck is a Disc. It functions as an important shock absorber and allows for motion between adjacent segments. It is susceptible to injury and degeneration. Common examples include Disc Protrusions, Annular Tears and Disc Herniations. Cervical Disc injury can cause pain in the left side of the Neck.
Muscle Tension
Muscles provide important stability and movement in the Neck. Muscles can be injured due to fatigue, trauma, repetitive activity, and poor ergonomics. Muscle tension can cause pain on either side of the Neck. When severe it limits your ability to move your Neck.
Cervical Facet Injury
A Facet joint is a paired joint located on the backside of the spine. Paired means that there is a right and left Facet joint. Facet joints are present at each level of spine and provide stability to the spine and limit movement. Like your knee or ankle joint, Facet joints are lined with cartilage which allows for smooth, pain free movement of the joint. Cervical Facet joints can become irritated or injured resulting in pain in the left side of the Neck.
Whiplash
Whiplash is a Neck injury due to forceful, rapid back-and-forth whipping motion of the head and Neck. Whiplash can also be described as “an acceleration-deceleration mechanism of energy to the Neck” (2). Whiplash is common with an estimated 1,000,000 cases per year in the United States (3). Whiplash type injuries can cause significant Neck pain and restriction in range of motion.
Ligament Injuries
Ligaments are thick pieces of connective tissue that connect bone to bone. Think of them as human duct tape. Ligaments provide stability to the Spine. Ligament injuries can compromise the stability of the Spine leading to dysfunction and pain in the left side of Neck. The great news is that many Grade 1 and 2 injuries can be treated with ultrasound and x-ray guided Regenerative treatments.
Cervical Radiculopathy
Cervical Radiculopathy is a painful medical condition that occurs as a result of irritation or compression of nerve in the Neck. Often times it is referred to as a ” pinched nerve” and can involve radiating arm pain, weakness and numbness. Pain is typically burning or electrical in character and unresponsive to Opioid therapy.
Cervical Fracture
Bones in the Spine are susceptible to fracture which can cause pain in left side of Neck. X-ray and CAT scans are useful in identifying fractures.
Infection
Infection of skin, muscles, tendons, bone and coverings of the Spinal Cord and Brain can cause pain in left side of Neck. Trauma is the most common cause. Treatment involves antibiotic treatment.
Torticollis
Torticollis is a painful medical condition in which the muscles in the Neck spasm and cause the head and neck to twist to one side. The exact cause of Torticollis is unknown. Symptoms include pain, inability to turn the head and muscle spasm.
Spinal Stenosis
Spinal Stenosis is a medical condition in which there is narrowing of the spaces within your Spine. This can put pressure on the nerves traveling within your Spine resulting in pain, dysfunction, weakness and numbness.
Spinal Tumor
Tumors in the Spine can occur causing pain, neurologic symptoms and restriction in range of motion. The good news is that some Spinal tumors are benign.
Diagnostic Process To Treat Symptoms
Neck pain is not a diagnosis but rather is a symptom. An accurate diagnosis is essential to best clinical outcomes. Masking pain with medications and injections is a disservice as it risks the underlying problem most likely getting worse. Establishing an accurate diagnosis starts with history of the current Neck pain, aggravating, alleviating factors and triggering event. Review of past medical, surgical history and traumas is important. Thereafter a physical examination will focus on range of motion, muscle symmetry and an intact neurologic system. Radiographic studies are often recommended and may include flexion, extension x-ray, CT scans and MRI. At the Centeno-Schultz Clinic an in office ultrasound examination is used to evaluate tendon, ligament and muscle integrity.
Treatment Options for Pain in Left Neck
Physical Therapy
Conservative care when appropriate should be the first line treatment. This would include Physical Therapy with emphasis on neutral Spine alignment, improved stability, range of motion and strength. The Centeno-Schultz Clinic has an outstanding Physical Therapist in house that can assist and guide patients in their care. To learn about Mark Reilly and treatment options more please click here.
Pain Relief Medications
The most common pain relief medications include:
NSAIDs
Persistent pain is often treated with NSAID’s which have significant side effects and risks. These medications are powerful anti-inflammatory agents that reduce inflammation. Common examples include Ibuprofen, Naproxen, and Diclofenac. Major risks include dependence, stroke, sudden-death, GI bleeding and depression of stem cell activity.
Narcotics
If pain persists and is not responsive to NSAID’s, some providers recommend oral Narcotics. This can be extremely dangerous as Narcotics have significant side side effects including dependence. Masking the pain with NSAID’s and Narcotics does not address or treat the underlying problem.
Oral Steroids
Steroids are powerful anti-inflammatory agents. Common examples include Prednisone, Methylprednisolone, Dexamethasone. Steroids have significant side effects that include increase risk of serious bone disease, depression of your stem cells and damage to tendons, ligament and cartilage. To learn more about the Steroid risks click here.
Corticosteroid Injections
When conservative care and medications fail some patients are referred to Steroid injections. While steroids are powerful anti-inflammatory agents they have significant risks which were discussed above. Steroid injections may actually make the pain worse long-term as Steroids can damage ligaments tendons and the cartilage of joints.
Surgery
Surgery is often recommended when pain persists despite conservative care, medication management and Steroid injections. There are many different types of surgeries and which will depend upon the underlying condition and its severity. Common risks associated with surgery include bleeding, infection, failure, escalation of pain, Adjacent Segment Disease and irreversible change in the biomechanics of the Cervical Spine. Surgery should be avoided if possible.
Home Strategies You Can Try For Pain in the Left Side of Neck
For acute pain that is mild in nature you may consider one of more of the following home treatments:
Rest: It’s best to stop the offending trigger or activity and give your body the chance to heal.
Heat: Heat improves the blood flow to a given area which can accelerate the healing process. Blood flow to an area of damage is like water in a garden. It promotes healing and recovery.
Good Posture: Extended periods of screen time on our phones and computers has compromised our posture and neutral spinal alignment. Good posture is essential of a healthy, happy and pain free Neck.
Good Sleeping Postures: Sleeping posture is strongly related to the quality of sleep (4). The two best positions are lying on your back or on your side. Sleeping on your back maintains normal spinal curvature (5)
Regenerative Treatment Options for Pain in Left Side of Neck
The Physicians at the Centeno-Schultz Clinic are experts in the treatment of Neck, Thoracic and Low Back Pain. Not all clinics or treatments are the same. Important differences between the Centeno-Schultz Clinic and others are:
Comprehensive Approach
The human body is a remarkable unit of nerves, muscles, tendons and bones that work together in a synchronistic way. Each body part works together and is reliant on other body parts. Remember the old Dem Bones song ” Shoulder bone is connected to the neck bone. Neck bone is connected to the head bone….” It is all interconnected. In evaluating a patient with Neck pain, the Shoulders, Thoracic and Low Back should also be examined. This is the SANS approach and stands for Stability, Articulation, Neurologic and Symmetry. To learn more about this unique approach click here.
Board Certification and Fellowship Trained Physicians
In medicine you get what you pay for. Years of study and experience are required for mastery in Orthopedics and Regenerative medicine. There are very few dedicated Fellowship programs solely focused on the use of PRP and using your body’s own healing agents like Bone Marrow Concentrate which contains your own stem cells for common Orthopedic conditions. Mid-levels such a PA’s and NP lack this expertise.
Extensive Publications
At the Centeno-Schultz Clinic were have a large number of peer reviewed publications. Collectively they represent over 40% of all the publications in the world on. To view the list click here.
Clinical Registry on Outcomes
Following clinical outcomes is critical to patient care as it allows both provider and patient to identify successes and areas that require additional improvement. Our registry track is easily accessed and tracks changes to pain, function and overall improvement. To see the registry please click here.
Clinical Experience
The Centeno-Schultz Clinic has 17 years of clinical experience in the treatment of common orthopedic conditions utilizing PRP and Bone Marrow Concentrate. There are no Botox injections , medication management or Radiofrequency Ablation procedures. Our exclusive focus is the advancement of Orthobiologics so that patients can avoid unnecessary and often times life changing orthopedic surgery. To learn more about Orthobiologics and how it can help you with your ongoing orthopedic pain, please watch the video below.
youtube
State of the Art Laboratory
At the Centeno-Schultz Clinic we have a university level laboratory staffed with Cell Biologists including a PhD. This allows us to use advanced, proprietary lab processing techniques to ensure we have the right concentrations of cells to treat your specific injury. In contrast most Regenerative clinics use one-size-fits-all bedside centrifuges which can lead to suboptimal clinical results. Each individual’s body and injury is unique and as such requires a tailored, customized PRP and or Bone Marrow Concentrate for optimal healing. Don’t cheat yourself.
Guidance on All Procedures
All injections are performed under X-ray or Ultrasound guidance to ensure that the cells are accurately injected into the targeted structures. Blind injections are below our standard of care and can limit patient’s success. The procedures are demanding as they require detailed understanding of the anatomy along with the ability to accurately place the needle into the targeted structure. These injections can not be performed by your PCP or Orthopedic surgeon. To watch a Cervical injection please click on the video below.
youtube
In Summary
Neck pain is common
Persistent Neck pain is a warning sign that warrants investigation.
Neck pain can present in a number of different ways which include stiffness, sharp shooting pain, soreness, and limited range of motion.
Possible causes of Neck pain include:
Cervical Disc injury
Muscle Tension
Cervical Facet Injury
Whiplash Injury
Cervical Radiculopathy
Cervical Fracture
Infection
Torticollis
Spinal Stenosis
Spinal Tumor
Treatment options for pain in Left neck include physical therapy, medications, steroid injections and surgery.
Regenerative treatment options exist that identify the cause of the pain and treat it using your own PRP and Bone Marrow Concentrate.
If you or a loved one have pain in Left neck that has not responded to conservative therapy, please schedule a Telemedicine consultation. Avoid the dependence of medications and periodic steroid injections. Stop the suffering and learn from a Board Certified, Fellowship trained Physician what your Regenerative treatment options are today.
1.Hoy DG, Protani M, De R, Buchbinder R. The epidemiology of neck pain. Best Pract Res Clin Rheumatol. 2010 Dec;24(6):783-92. doi: 10.1016/j.berh.2011.01.019. PMID: 21665126.
2.Pastakia K, Kumar S. Acute whiplash associated disorders (WAD). Open Access Emerg Med. 2011;3:29-32. Published 2011 Apr 27. doi:10.2147/OAEM.S17853.
3.Rosenfeld M, Seferiadis A, Gunnarsson R. Active involvement and intervention in patients exposed to whiplash trauma in automobile crashes reduces costs: a randomized, controlled clinical trial and health economic evaluation. Spine (Phila Pa 1976). 2006 Jul 15;31(16):1799-804. doi: 10.1097/01.brs.0000225975.12978.6c. Erratum in: Spine (Phila Pa 1976). 2012 Nov 15;37(24):E1537- 40. PMID: 16845354
4.Jeon MY, Jeong H, Lee S, Choi W, Park JH, Tak SJ, Choi DH, Yim J. Improving the quality of sleep with an optimal pillow: a randomized, comparative study. Tohoku J Exp Med. 2014 Jul;233(3):183-8. doi: 10.1620/tjem.233.183. PMID: 25008402.
5Lee WH, Ko MS. Effect of sleep posture on neck muscle activity. J Phys Ther Sci. 2017;29(6):1021-1024. doi:10.1589/jpts.29.1021.
from Centeno-Schultz Clinic https://centenoschultz.com/pain-in-left-side-of-neck-causes-and-treatment-options/
0 notes
Text
Occipital Cervical Fusion: Is There an Alternative?
The brain fog, dizziness and functional compromise continue to progress despite conservative care. Your doctor referred you for surgical consultation. The surgeon discussed treatment options. What is a Fusion? What is the Occiput? What is the Craniocervical Junction (CCJ)? What is an Occipital Cervical Fusion? What are the indications for an Occipital Cervical Fusion? What are the risks associated with Occipital Cervical Fusion? Are there alternatives to Occipital Cervical Fusion? What is the PICL procedure? Let’s dig in.
What Is a Fusion?
Fusion is a major surgery in which the spine is stabilized by a series of screws, bolts and plates. Fusion surgery can be performed in the neck, thoracic and lumbar spine.
What Is the Occiput?
The Occiput is the back of your skull. Otherwise known as your noggin. The skull resides on top the Cervical Spine. In fact the occiput forms a joint between the base of the skull and the top of the neck that is called the Craniocervical junction. To learn more about this important structure please click here.
What Is the Craniocervical Junction?
The base of the Occiput has a large opening called the Foramen Magnum. Important structures that pass from the skull through the Foramen Magnum include (1):
Spinal Cord
The Spinal Cord consists of neural tissue that starts at the base of the Brain and extends down into the low back. It is a cylindrical bundle of nerve fibers that control our voluntary and involuntary bodily functions. It carries signals between the brain and the rest of the body. As the Spinal Cord descends it is protected on all sides by Spinal bones. These bones provide boney armor to protect against injury. The Spinal Cord has an additional layer of protection afforded by the Spinal Fluid. The Spinal Fluid is also known as Cerebral Spinal fluid. It surrounds the Spinal Cord and extends the entire length of the Spine. The image to the right is a side view of the Spinal Cord as it exits the Brain. The Spinal Cord is black in color. The white that surrounds the Spinal Cord is the Spinal Fluid.
Cranial Nerves
As the Spinal Cord descends through the Foramen Magnum and Spine, important nerves branch off traveling to different parts of the body. There are a large number of nerves. These include the 12 Cranial nerves some of which control muscles whereas others are connected to internal organs such as the heart and lungs.
Arteries and Veins
Arteries and veins provide blood flow to and from important structures in the head, neck, and body. Without blood flow, the body cannot function.
Ligaments
Ligaments are the human duct tape that keeps everything in alignment and stable. The are many ligaments in the neck that provide stability. Two very important ligaments in the upper neck are the Alar and Transverse ligaments. To learn more about these ligaments please click here.
What Is an Occipital Cervical Fusion?
An Occipital Cervical Fusion also known as Occipitocervical Susion is a Major Surgery. It is not a routine operation and is a challenging procedure due to complex anatomy of the upper neck. The procedure involves rods, plates and screws that are placed into the Cervical Spine and Occiput. A plate secured by screws are placed at the base of the Occiput. Screws are also placed into one or more Cervical bones. Rods then connect the Occipital plate to the Cervical screws as shown below. The goal of Occipital Cervical Surgery is a boney fusion between the skull and neck and to relieve any abnormal pressure on the Brain Stem and Spinal Cord.
What Are the Indications for Occipital Cervical Fusion?
Occipital Cervical Fusion is used to treat various disorders of the Craniocervical Junction. The most common indication for Fusion is Craniocervical instability, and Brain Stem/Spinal Cord compression (2).
Craniocervical instability (CCI) is a medical condition where the strong ligaments that hold your head onto your neck are loose or lax (3). The major ligaments involved are the Alar, Transverse and Accessory ligaments. To learn more about CCI please click on the video below.
youtube
What Are the Risks Associated with Occipital Cervical Fusion?
The upper Cervical Spine is a very complex area rich in nerves, arteries, veins, ligaments, tendons, and muscles. The risks associated with Upper Neck Fusion are significant and include (4).
Infection
An infection can be localized to the skin or may penetrate deeper into the muscles or bone. Antibiotics are oftentimes required for skin infections. Bone infections require additional surgery.
Screw Loosening
The implanted screw can back out of the bone over time compromising the stability of the upper neck.
Rod/Screw Failure
The screws that are inserted into the Occiput or C1 or C2 as well as the connecting rods can fracture, bend or break. In most cases surgical revision is necessary.
Failed Fusion
Despite the implanted screws and hardware, the Occiput and Cervical Spine may not fuse together. This is called Pseudoarthrosis and compromises the spinal stability.
Cervical Facet injury
A Cervical Facet is a paired joint that resides at each level of the Spine. A poorly placed surgical screw can be advanced into the Facet joint thereby injuring the joint cartilage leading to arthritis, pain, and restriction in range of motion.
Hematoma
A collection of blood that can compress or injure nerves, arteries, and veins.
Nerve Injury
The Upper Cervical Spine is rich in nerves that are susceptible to injury due to traction, cutting of tissue or poorly placed surgical screws.
Continued Pain and Dysfunction
Despite Fusion some patients fail to obtain a reduction in pain and improvement in function.
Vertebral Artery Injury
The Vertebral Artery provides critical blood flow to the Spinal Cord and Brain. The artery can be compressed, irritated, or injured during the surgery.
Dural Leak: The Dura is a thin layer of connective tissue that covers the Brain and Spinal Cord. It can be injured during the surgery resulting in leakage of Spinal Fluid (5).
Limited Neck Range of Motion
Fusion of the Skull Base to the Upper Neck can severely restrict the range of motion in the neck.
Death
Adjacent Segment Disease (ASD): Fusion of the Spine significantly alters the biomechanics of the Spine. The fused segment is no longer able to absorb the forces of daily living. As such these forces are then transferred above and below the Fusion. This additional force can overload the Discs, Facet joints, muscle, and ligaments above and below the Fusion which start to break down. This is called Adjacent Segment Disease. To learn more about this please click on the video below.
youtube
Are there Alternatives to Occipital Cervical Fusion?
Yes!
n 2015 a nonsurgical treatment option for Cranial Cervical Instability was developed at the Centeno-Schultz Clinic. It involves the injection of a patient’s own Bone Marrow Concentrate into the damaged Alar and Transverse ligaments. The procedure is for mild to moderate cases of Craniocervical Instability that have not responded to conservative and Upper Cervical injection therapy. The procedure is very demanding and only performed at the Centeno-Schultz Clinic in Broomfield Colorado. The procedure is called Percutaneous Implantation of Cervical Ligaments (PICL) To learn more about this groundbreaking procedure please click on the video below.
youtube
In Summary
Fusion is a major surgery in which the Spine is stabilized by a series of screws, bolts and plates.
The Occiput is the back of your skull.
The Craniocervical Junction is where the Occiput and the Upper Neck bones come together to form a joint.
The Craniocervical Junction contains vital structures that include the Spinal Cord, Cranial Nerves, arteries, veins and ligaments.
An Occipital Cervical Fusion is a major surgery that involves screws, plates and rods that are placed into the Upper Cervical Spine and Occiput.
Occipital Cervical Fusion is used treat various disorders of the Craniocervical Junction. The most common indication is Craniocervical Instability (CCI) and Brainstem/Spinal Cord compression.
The risks associated with Occipitocervical Fusion are significant and include:
Infection
Screw Loosening
Rod/Screw Failure
Failed Fusion
Cervical Facet Injury
Hematoma
Continued Pain and Dysfunction
Vertebral Artery Injury
Dural Leak
Limited Range of Motion
Adjacent Segment Disease
Percutaneous Implantation of Cervical Ligaments (PICL) is an non surgical treatment option for mild to moderate cases of Craniocervical Instability that have not responded to conservative care.
If you or a loved one continue to suffer from headaches, dizziness, brain fog and chronic fatigue that has not responded to conservative therapy please schedule a telemedicine consultation. A board certified, fellowship trained Physician will review your history, imaging and discuss appropriate treatment options.
1.Flanagan MF. The Role of the Craniocervical Junction in Craniospinal Hydrodynamics and Neurodegenerative Conditions. Neurol Res Int. 2015;2015:794829. doi:10.1155/2015/794829
2.Deutsch H, Haid RW Jr, Rodts GE Jr, Mummaneni PV. Occipitocervical fixation: long-term results. Spine (Phila Pa 1976). 2005 Mar 1;30(5):530-5. doi: 10.1097/01.brs.0000154715.88911.ea. PMID: 15738785.
3.Offiah CE, Day E. The craniocervical junction: embryology, anatomy, biomechanics and imaging in blunt trauma. Insights Imaging. 2017;8(1):29–47. doi:10.1007/s13244-016-0530-5
4.Kukreja S, Ambekar S, Sin AH, Nanda A. Occipitocervical Fusion Surgery: Review of Operative Techniques and Results. J Neurol Surg B Skull Base. 2015;76(5):331-339. doi:10.1055/s-0034-1543967.
5.Upadhyaya M, Jain S, Kire N, Merchant Z, Kundnani V, Patel A. Surgical, clinical, and radiological outcomes of occipitocervical fusion using the plate-screw-rod system with allograft in craniocervical instability. J Craniovertebr Junction Spine. 2019;10(4):216-223. doi:10.4103/jcvjs.JCVJS_87_19
from Centeno-Schultz Clinic https://centenoschultz.com/occipital-cervical-fusion-is-there-an-alternative/
0 notes
Text
Ligaments of the Spine: Understanding Their Importance
It started as a dull ache and now has progressed. It feels like a knife in the back of your neck and is preventing you from daily activities. Medications, rest and conservative treatments have failed. Your doctor noticed on x-ray that the bones are out of alignment. He thinks you may have suffered a ligament injury. What is a ligament? What is the function of ligaments in the Spine? What are the 5 main ligaments of the Spine? Are there different types of ligament injuries? What can happen if Spinal ligaments are injured? Can ligaments heal on their own? What are the treatment options for ligaments of the Spine injuries? Let’s dig in.
What Is a Ligament?
A ligament a thick piece of connective tissue that connects bone to bone. Think of it as duct tape that holds bones together.
What Is the Function of Ligaments in the Spine?
Ligaments function to stabilizes the Spine, hold the Vertebral bodies together, limit Spinal motion and protect the Discs (1).
What Are the 5 Main Ligaments of the Spine?
Review of basic spinal anatomy will help you better appreciate the major ligaments of the Spine and their location. In this post I will be discussing the Cervical Spine: AKA the neck. All the ligaments discussed below are in the Cervical Spine but actually run the length of the Spine into the Sacrum.
The Spine is composed of boney building blocks that stack on upon another. These are called Vertebral bodies. In the Cervical Spine there are 7 boney building blocks which are numbered from 1 to 7. They are preceded by the letter “C” which refers to Cervical. Sandwiched between each of the building blocks is a spongey shock absorber called a Disc. At each level of the spine, Nerves exit through a boney doorway called the Neuroforamen.
There are a large number of both large and small ligaments in the Spine. The 5 main ligaments of the Spine include:
Anterior Longitudinal Ligament (ALL)
A one-inch thin ligament that is located on the front of the Spine. It starts at the base of the skull and extends into pelvis. To learn more about the Anterior Longitudinal Ligament please click here.
Posteror Longitudinal Ligament (PLL)
A one-inch thin ligament that is located on the backside of the boney building blocks of the spine (Vertebral bodies). Like the ALL, the PLL starts at the base of the skull and extends into the pelvis.
Supraspinous Ligament
On the backside of the Spine is a projecting bone that is easily felt. It is present at each level and is located in the midline. If you run your hand down someone’s neck these pointed bones are easily identified. These are the Spinous Processes. The Supraspinous ligament connects each of the Spinous Processes from C7 down to L4.
Interspinous Ligament
Like the Supraspinous Ligament, the Interspinous Ligament connects each of the Spinous Processes of the Spine. It is slightly deeper than Supraspinous Ligament. Its most supeficial fibers connect with the Supraspinous Ligament whereas the deeper fibers connect with the Ligamentum Flavum. Conceptually it is sandwiched between the Supraspinous Ligament and the Ligamentum Flavum
Ligamentum Flavum
The Ligamentum Flavum is a thick ligament that connects the Spinal bodies together. Specifically it connects the Lamina two adjacent Vertebral bodies. It is sandwiched between the Interspinous Ligament and the Dura. It starts in the C2 bone and extends down into the Pelvis. It is an important landmark for anesthesiologists when advancing their needle for epidural injections. The Ligamentum Flavum is thick and there can be significant change in the needle pressure when advancing into the Ligamentum Flavum. The technique is called Loss of Resistance (LOR). The Ligamentum Flavum can increase in thickness causing narrowing of the Spinal Canal, a condition known as Spinal Stenosis.
Can You Tear or Injure Ligaments in the Spine?
Ligaments in the Spine are susceptible to injury. Motor vehicle accidents, sports injuries, other traumatic events, and repetitive motion over time are the most frequent causes of ligament injury (2)
Are There Different Types of Ligament Injuries
Absolutely! Various types of trauma including motor vehicle accidents that can cause ligament injury. These injuries are classified into three grades.
Grade 1 sprain: Mild and includes slight stretching of the fibers and partial tear of the ligament.
Grade 2 sprain: More severe and involves a full thickness partial tear but the ligament is still intact.
Grade 3 sprain: Most severe and involves the entire ligament. The two edges of the ligament are pulled apart. This is otherwise known as a rupture.
What Happens if the Ligaments in the Spine Are Injured?
Spinal Ligaments provide important stability, limit motion, and protect the Spinal Discs. Injury to Spinal Ligaments is graded based upon the severity of the ligament injury. Injury of Spinal Ligaments can cause any of the following.
Slippage of vertebral body backwards in relation to the other spinal bones: retrolisthesis
Spinal Instability: The Spinal bones stack one upon another. They are supported by Spinal Ligaments. Injury to these ligaments can cause one or more of the Vertebral Bodies (boney building blocks) to move. This is referred to as Listhesis. If the bone is moved forward in relation to the adjacent bone it is called Anterolisthesis. Conversely if the bone is moved backwards in relation to the adjacent bone it is called Retrolisthesis.
Disc Injury: Movement of the Vertebral Bodies creates a shearing force on the Disc. This force can lead to Disc irritation, injury and degeneration. In addition, the loss of support provided by the ligament can cause Disc protrusions or Herniations.
Nerve Injury: Movement of one or more Vertebral Bodies can also irritate exiting nerve roots causing radiating extremity pain, numbness and tingling.
Spinal Stenosis: Movement of one or more Vertebral Bodies can narrow the Spinal Canal.
Facet Injury: Ligament instability in the Spine can lead to Facet overload, irritation, and injury which in turn can result in debilitating pain
Does an MRI Show Ligament Injury?
Yes! MRI is an effective radiographic study to evaluate injuries to the ligaments of the Spine (3). Common findings include blood or swelling adjacent to the ligament tear.
Can Ligaments of the Spine Heal?
Healing is dependent upon the severity of the injury. Ligament healing is an extensive 3 phase process that takes months. If a given ligament is allowed sufficient time to heal and is supported during the healing phase many Grade 1 injuries can heal. The problem with Spinal Ligament injuries is twofold:
Patients rarely allow sufficient time to heal which requires significant activity modification for months.
External bracing is not a practical option. Unlike a knee or ankle ligament injury where a knee or ankle brace can be applied, external Spinal braces are rarely used and poorly tolerated by most patients.
Treatment Options for Ligaments of the Spine Injuries
At the Centeno-Schultz Clinic treatment of Spinal Ligaments is a central portion of our philosophy and treatment protocol. We view the Spine as a collection of many parts working in a synchronized fashion. This approach is known as the Functional Spinal Unit (FSU) and is radically different from the approach used in most pain clinic which focus on one or more “Pain Generators”. To learn more about this approach please click here.
Spinal Ligament injuries can be treated by precise injections of PRP or Bone Marrow Concentrate under X-ray or ultrasound guidance. Blind injections are below our standard of care and place the patient at risk for Nerve, Disc and Vascular injuries. The injections are demanding and cannot be performed by your Orthopedic Surgeon or Family Physician. Below is a x-ray image of a Interspinous Ligament injection at C2. Below is an x-ray image of a Cervical Interspinous Ligament injection from my clinic. It was performed under x-ray guidance in a patient with Cervical Instability. .
Healing of ligaments following PRP or Bone Marrow Concentrate injections takes time. There are three distinct phases: inflammatory, proliferative and tissue remodeling. To learn more about ligament healing click on video below.
youtube
In Summary
A ligament a thick piece of connective tissue that connects bone to bone.
Ligaments function to stabilizes the spine, hold the Vertebral Bodies together, limit Spinal motion and protect the Discs.
There are 5 major ligaments of the Spine:
Anterior Longitudinal Ligament
Posterior Longitudinal Ligament
Supraspinous Ligament
Interspinous Ligament
Ligamentum Flavum
Ligaments of the Spine are susceptible to injury.
Ligament injury is graded based upon severity: grade 1, 2 and 3.
Injury to the Ligaments of the Spine can cause Spinal instability, Spinal Stenosis and injury to the Discs and Facets.
Grade 1 and some grade 2 ligaments can heal on their own if allowed sufficient time and bracing. Unfortunately, this is poorly tolerated by most patients.
Ligament injuries can be treated with precise x-ray and or ultrasound guided injections of PRP or Bone Marrow Concentrate allowing patients the opportunity to avoid surgery.
If you or a loved one has sustained trauma to the spine and has not responded to conservative therapy please schedule a Telemedicine consultation. Injury of the ligaments of the Spine are quite common and often times missed leading to Spinal Instability, and injury to the Spinal Discs, Facets and Nerves. Stop the suffering and learn what your Regenerative options are from a board certified, fellowship trained physician today.
1.Damm N, Rockenfeller R, Gruber K. Lumbar spinal ligament characteristics extracted from stepwise reduction experiments allow for preciser modeling than literature data. Biomech Model Mechanobiol. 2020;19(3):893-910. doi:10.1007/s10237-019-01259-6
2.Panjabi MM. A hypothesis of chronic back pain: ligament subfailure injuries lead to muscle control dysfunction. Eur Spine J. 2006;15(5):668-676. doi:10.1007/s00586-005-0925-3
3.Katzberg RW, Benedetti PF, Drake CM, Ivanovic M, Levine RA, Beatty CS, Nemzek WR, McFall RA, Ontell FK, Bishop DM, Poirier VC, Chong BW. Acute cervical spine injuries: prospective MR imaging assessment at a level 1 trauma center. Radiology. 1999 Oct;213(1):203-12. doi: 10.1148/radiology.213.1.r99oc40203. PMID: 10540663.
from Centeno-Schultz Clinic https://centenoschultz.com/ligaments-of-the-spine-understanding-their-importance/
0 notes
Text
Anterior Longitudinal Ligament: Could This Be Responsible for Your Ongoing Neck Pain?
The neck pain is unrelenting, and all started after being rear ended at a stoplight. Spine X-rays demonstrated some abnormal movement of the Spinal bones. Both conservative care and medications have failed. Your doctor thinks you have injured a Spinal ligament. What is the Anterior Longitudinal Ligament? What is the role of the Anterior Longitudinal Ligament? What ligaments are injured in a Whiplash type accident? Are there different types of ligament injuries? What happens if the Anterior Longitudinal Ligament is injured? Does MRI show ligament injuries? Can Spinal ligaments heal and what are the limitations? What are the treatment options for injuries to the Anterior Longitudinal Ligament? Let’s dig in.
What Is the Anterior Longitudinal Ligament (ALL)?
A ligament is a thick piece of connective tissue that connects bone to bone. Think of it as duct tape that holds bones together. The Anterior Longitudinal Ligament (ALL) is an important ligament located in the front of the neck. It starts at the base of the skull and extends down across the Cervical, Thoracic and Lumbar Spine ending at the Sacrum. It is approximately one inch is width and has three layers: superficial, intermediate and deep.
What Is the Role of the Anterior Longitudinal Ligament?
To understand the role of the role of the ALL it is important to review some spinal anatomy. The Spine is composed of boney building blocks that stack on upon another. In the Cervical Spine there are 7 boney building blocks. Sandwiched between each of the building blocks is a sponey shock absorber called a Disc. At each level of the Spine, Nerves exit through a boney doorway called the Neuroforamen. The Anterior Longitudinal Ligament covers the front portion of the Spine. It covers both the boney building block and the Disc.
The Anterior Longitudinal Ligament has 3 important roles:
Stabilizes the Spine
Limits motion
Confines, supports, and reinforces the anterior wall of the Disc
Which Ligaments Are Injured in Whiplash Type Accident?
Whiplash is a neck injury due to forceful, rapid back-and-forth whipping motion of the head and neck. Whiplash can also be described as “an acceleration-deceleration mechanism of energy to the neck” (1). The incidence of Whiplash injuries varies greatly between different parts of the world. For example, in Quebec Canada incidence is as high as 70 per 100,000 (2). It is estimated that there are 1,000,000 cases of Whiplash per year in the United States. Injuries can be significant and long lasting. Approximately 50% of Whiplash patients have reported chronic neck pain 15 years after the trauma (3).
Whiplash trauma can cause injury to multiple Spinal structures and ligaments, Facet joints, Discs, Muscles, Tendons and Nerves. The Anterior Longitudinal Ligament is particularly susceptible to injury due to the rapid back and forth whipping motion of the neck (4).
Are there Different Types of Anterior Longitudinal Ligament Tears?
Absolutely! Various types of trauma including motor vehicle accidents that can cause injury to the Anterior Longitudinal Ligament. Ligament injuries are classified into three grades.
Grade 1 sprain: Mild and includes slight stretching of the fibers and partial tear of the ligament..
Grad 2 sprain: More severe and involves a full thickness partial tear but the ligament is still intact.
Grade 3 sprain: Most severe and involves the entire ligament. The two edges of the ligament are pulled apart. This is otherwise known as a rupture.
What Happens if the Anterior Longitudinal Ligament is Injured?
The Anterior Longitudinal Ligament provides critical support to the Spine and Discs. Injury to the ALL can cause the following:
Spinal instability: Movement of one or more of the Vertebral Bodies (boney building blocks). This is referred to as Listhesis.
Loss of support and reinforcement of the Disc making the Disc vulnerable to injury including Disc Protrusion and Herniation.
Disc Injury: Movement of the Vertebral bodies creates a shearing force on the Disc creating irritation and injury
Nerve Injury: Movement of one or more Vertebral Bodies can also irritate exiting nerve roots causing radiating extremity pain.
Spinal Stenosis: Movement of one or more Vertebral Bodies can narrow the Spinal Canal
Injury to the ALL can cause irritation or injury to the Nerves within the Longitudinal Ligament resulting in pain and restriction in range of motion.
ALL Injury can also lead to bone formation within the ligament causing pain and dysfunction.
Does an MRI Show Ligament Injury?
Yes! MRI is an effective radiographic study to evaluate injuries to the Cervical ligaments which include the Anterior Longitudinal Ligament (5). Common findings include blood or swelling adjacent the ligament tear. In addition, there may be movement of the boney building blocks in the Spine such that one or more move backwards in relationship to the others. This is called Retrolisthesis.
Can Spinal Ligaments Heal?
Ligament healing is an extensive 3 phase process that takes months. If a given ligament is allowed sufficient time to heal and is supported during the healing phase many Grade 1 injuries can heal. The problem with Spinal ligament injuries is twofold:
Patients rarely allow sufficient time to heal which requires significant activity modification for months.
External bracing is not a practical option. Unlike a knee or ligament injury where a knee or ankle brace can be applied, external Spinal braces are rarely used and poorly tolerated by most patients.
Treatment Options for Anterior Longitudinal Ligament Injuries
At the Centeno-Schultz Clinic treatment of Spinal ligaments is a central portion of our philosophy and treatment protocol. We view the Spine as a collection of many parts working in a synchronized fashion. This approach is known as the Functional Spinal Unit (FSU) and is radically different from the approach used in most pain clinic which focus on one or more “Pain Generators”. To learn more about this approach please click here.
Anterior Longitudinal Ligament injuries have been successfully treated using precise ultrasound and x-ray guided injections. Blind injections, those without guidance are below the standard of care and put the patient at risk for Nerve, Disc and blood vessel injury.
Dr. John PItts was instrumental in developing this injection technique. An intimate working knowledge of the Spinal anatomy along with years of x-ray and ultrasound guided injections allowed for him to develop and refine this injection. We have all mastered this injection. It is a complex, highly skilled injection that you family doctor or orthopedic surgeon cannot perform. Below is x-ray image of my recent Anterior Longitudinal Ligament injection.
Healing of ligaments following PRP or Bone Marrow Concentrate injections which contain stem cells take time. There are three distinct phases: inflammatory, proliferative and tissue remodeling. To learn more about ligament healing click on video below.
youtube
In Summary
The Anterior Longitudinal Ligament is a small ligament in the front of your neck. It starts at the base of the Skull and extends into the Sacrum.
The Anterior Longitudinal Ligament has three important roles: stabilization, limits movement and supports the front wall of the discs.
Whiplash type traumas can cause injury to multiple structures in the spine including the Anterior Longitudinal Ligament.
Ligament injuries are graded based on the severity of the injury: Grade 1, Grade 2 and Grade 3.
Injury of the Anterior Longitudinal Ligament can result in Spinal Instability, Spinal Stenosis and injury to the Discs, Nerves and Facet joints.
MRI is an effective radiographic imaging technique to identify ligamental injury.
Most Grade 1 and some Grade 2 injuries can heal on their own if allowed to. Unfortunately, effective bracing of the spine of prolonged periods is rarely tolerated.
At the Centeno-Schultz Clinic we have pioneered a procedure where the Anterior Longitudinal Ligament injures can be treated with precisely guided injections of PRP or Bone Marrow Concentrate.
If you or a loved one has sustained trauma to the spine and has not responded to conservative therapy please schedule a telemedicine consultation. Ligament injuries are quite common and often times missed leading to Spinal Instability, and injury to the Discs, Facets and Nerves. Stop the suffering and learn from a board certified, fellowship trained physician what your Regenerative treatment options are today.
1.Pastakia K, Kumar S. Acute whiplash associated disorders (WAD). Open Access Emerg Med. 2011;3:29-32. Published 2011 Apr 27. doi:10.2147/OAEM.S17853.
2.Rosenfeld M, Seferiadis A, Gunnarsson R. Active involvement and intervention in patients exposed to whiplash trauma in automobile crashes reduces costs: a randomized, controlled clinical trial and health economic evaluation. Spine (Phila Pa 1976). 2006 Jul 15;31(16):1799-804. doi: 10.1097/01.brs.0000225975.12978.6c. Erratum in: Spine (Phila Pa 1976). 2012 Nov 15;37(24):E1537- 40. PMID: 16845354.
3.Squires B, Gargan MF, Bannister GC. Soft-tissue injuries of the cervical spine. 15-year follow-up. J Bone Joint Surg Br. 1996 Nov;78(6):955-7. doi: 10.1302/0301-620x78b6.1267. PMID: 8951014.
4.Stemper BD, Yoganandan N, Pintar FA, Rao RD. Anterior longitudinal ligament injuries in whiplash may lead to cervical instability. Med Eng Phys. 2006 Jul;28(6):515-24. doi: 10.1016/j.medengphy.2005.09.011. Epub 2005 Nov 10. PMID: 16289824.
5.Katzberg RW, Benedetti PF, Drake CM, Ivanovic M, Levine RA, Beatty CS, Nemzek WR, McFall RA, Ontell FK, Bishop DM, Poirier VC, Chong BW. Acute cervical spine injuries: prospective MR imaging assessment at a level 1 trauma center. Radiology. 1999 Oct;213(1):203-12. doi: 10.1148/radiology.213.1.r99oc40203. PMID: 10540663.
from Centeno-Schultz Clinic https://centenoschultz.com/anterior-longitudinal-ligament/
0 notes
Text
Anterior Longitudinal Ligament: Could This Be Responsible for Your Ongoing Neck Pain?
The neck pain is unrelenting, and all started after being rear ended at a stoplight. Spine X-rays demonstrated some abnormal movement of the Spinal bones. Both conservative care and medications have failed. Your doctor thinks you have injured a Spinal ligament. What is the Anterior Longitudinal Ligament? What is the role of the Anterior Longitudinal Ligament? What ligaments are injured in a Whiplash type accident? Are there different types of ligament injuries? What happens if the Anterior Longitudinal Ligament is injured? Does MRI show ligament injuries? Can Spinal ligaments heal and what are the limitations? What are the treatment options for injuries to the Anterior Longitudinal Ligament? Let’s dig in.
What Is the Anterior Longitudinal Ligament (ALL)?
A ligament is a thick piece of connective tissue that connects bone to bone. Think of it as duct tape that holds bones together. The Anterior Longitudinal Ligament (ALL) is an important ligament located in the front of the neck. It starts at the base of the skull and extends down across the Cervical, Thoracic and Lumbar Spine ending at the Sacrum. It is approximately one inch is width and has three layers: superficial, intermediate and deep.
What Is the Role of the Anterior Longitudinal Ligament?
To understand the role of the role of the ALL it is important to review some spinal anatomy. The Spine is composed of boney building blocks that stack on upon another. In the Cervical Spine there are 7 boney building blocks. Sandwiched between each of the building blocks is a sponey shock absorber called a Disc. At each level of the Spine, Nerves exit through a boney doorway called the Neuroforamen. The Anterior Longitudinal Ligament covers the front portion of the Spine. It covers both the boney building block and the Disc.
The Anterior Longitudinal Ligament has 3 important roles:
Stabilizes the Spine
Limits motion
Confines, supports, and reinforces the anterior wall of the Disc
Which Ligaments Are Injured in Whiplash Type Accident?
Whiplash is a neck injury due to forceful, rapid back-and-forth whipping motion of the head and neck. Whiplash can also be described as “an acceleration-deceleration mechanism of energy to the neck” (1). The incidence of Whiplash injuries varies greatly between different parts of the world. For example, in Quebec Canada incidence is as high as 70 per 100,000 (2). It is estimated that there are 1,000,000 cases of Whiplash per year in the United States. Injuries can be significant and long lasting. Approximately 50% of Whiplash patients have reported chronic neck pain 15 years after the trauma (3).
Whiplash trauma can cause injury to multiple Spinal structures and ligaments, Facet joints, Discs, Muscles, Tendons and Nerves. The Anterior Longitudinal Ligament is particularly susceptible to injury due to the rapid back and forth whipping motion of the neck (4).
Are there Different Types of Anterior Longitudinal Ligament Tears?
Absolutely! Various types of trauma including motor vehicle accidents that can cause injury to the Anterior Longitudinal Ligament. Ligament injuries are classified into three grades.
Grade 1 sprain: Mild and includes slight stretching of the fibers and partial tear of the ligament..
Grad 2 sprain: More severe and involves a full thickness partial tear but the ligament is still intact.
Grade 3 sprain: Most severe and involves the entire ligament. The two edges of the ligament are pulled apart. This is otherwise known as a rupture.
What Happens if the Anterior Longitudinal Ligament is Injured?
The Anterior Longitudinal Ligament provides critical support to the Spine and Discs. Injury to the ALL can cause the following:
Spinal instability: Movement of one or more of the Vertebral Bodies (boney building blocks). This is referred to as Listhesis.
Loss of support and reinforcement of the Disc making the Disc vulnerable to injury including Disc Protrusion and Herniation.
Disc Injury: Movement of the Vertebral bodies creates a shearing force on the Disc creating irritation and injury
Nerve Injury: Movement of one or more Vertebral Bodies can also irritate exiting nerve roots causing radiating extremity pain.
Spinal Stenosis: Movement of one or more Vertebral Bodies can narrow the Spinal Canal
Injury to the ALL can cause irritation or injury to the Nerves within the Longitudinal Ligament resulting in pain and restriction in range of motion.
ALL Injury can also lead to bone formation within the ligament causing pain and dysfunction.
Does an MRI Show Ligament Injury?
Yes! MRI is an effective radiographic study to evaluate injuries to the Cervical ligaments which include the Anterior Longitudinal Ligament (5). Common findings include blood or swelling adjacent the ligament tear. In addition, there may be movement of the boney building blocks in the Spine such that one or more move backwards in relationship to the others. This is called Retrolisthesis.
Can Spinal Ligaments Heal?
Ligament healing is an extensive 3 phase process that takes months. If a given ligament is allowed sufficient time to heal and is supported during the healing phase many Grade 1 injuries can heal. The problem with Spinal ligament injuries is twofold:
Patients rarely allow sufficient time to heal which requires significant activity modification for months.
External bracing is not a practical option. Unlike a knee or ligament injury where a knee or ankle brace can be applied, external Spinal braces are rarely used and poorly tolerated by most patients.
Treatment Options for Anterior Longitudinal Ligament Injuries
At the Centeno-Schultz Clinic treatment of Spinal ligaments is a central portion of our philosophy and treatment protocol. We view the Spine as a collection of many parts working in a synchronized fashion. This approach is known as the Functional Spinal Unit (FSU) and is radically different from the approach used in most pain clinic which focus on one or more “Pain Generators”. To learn more about this approach please click here.
Anterior Longitudinal Ligament injuries have been successfully treated using precise ultrasound and x-ray guided injections. Blind injections, those without guidance are below the standard of care and put the patient at risk for Nerve, Disc and blood vessel injury.
Dr. John PItts was instrumental in developing this injection technique. An intimate working knowledge of the Spinal anatomy along with years of x-ray and ultrasound guided injections allowed for him to develop and refine this injection. We have all mastered this injection. It is a complex, highly skilled injection that you family doctor or orthopedic surgeon cannot perform. Below is x-ray image of my recent Anterior Longitudinal Ligament injection.
Healing of ligaments following PRP or Bone Marrow Concentrate injections which contain stem cells take time. There are three distinct phases: inflammatory, proliferative and tissue remodeling. To learn more about ligament healing click on video below.
youtube
In Summary
The Anterior Longitudinal Ligament is a small ligament in the front of your neck. It starts at the base of the Skull and extends into the Sacrum.
The Anterior Longitudinal Ligament has three important roles: stabilization, limits movement and supports the front wall of the discs.
Whiplash type traumas can cause injury to multiple structures in the spine including the Anterior Longitudinal Ligament.
Ligament injuries are graded based on the severity of the injury: Grade 1, Grade 2 and Grade 3.
Injury of the Anterior Longitudinal Ligament can result in Spinal Instability, Spinal Stenosis and injury to the Discs, Nerves and Facet joints.
MRI is an effective radiographic imaging technique to identify ligamental injury.
Most Grade 1 and some Grade 2 injuries can heal on their own if allowed to. Unfortunately, effective bracing of the spine of prolonged periods is rarely tolerated.
At the Centeno-Schultz Clinic we have pioneered a procedure where the Anterior Longitudinal Ligament injures can be treated with precisely guided injections of PRP or Bone Marrow Concentrate.
If you or a loved one has sustained trauma to the spine and has not responded to conservative therapy please schedule a telemedicine consultation. Ligament injuries are quite common and often times missed leading to Spinal Instability, and injury to the Discs, Facets and Nerves. Stop the suffering and learn from a board certified, fellowship trained physician what your Regenerative treatment options are today.
1.Pastakia K, Kumar S. Acute whiplash associated disorders (WAD). Open Access Emerg Med. 2011;3:29-32. Published 2011 Apr 27. doi:10.2147/OAEM.S17853.
2.Rosenfeld M, Seferiadis A, Gunnarsson R. Active involvement and intervention in patients exposed to whiplash trauma in automobile crashes reduces costs: a randomized, controlled clinical trial and health economic evaluation. Spine (Phila Pa 1976). 2006 Jul 15;31(16):1799-804. doi: 10.1097/01.brs.0000225975.12978.6c. Erratum in: Spine (Phila Pa 1976). 2012 Nov 15;37(24):E1537- 40. PMID: 16845354.
3.Squires B, Gargan MF, Bannister GC. Soft-tissue injuries of the cervical spine. 15-year follow-up. J Bone Joint Surg Br. 1996 Nov;78(6):955-7. doi: 10.1302/0301-620x78b6.1267. PMID: 8951014.
4.Stemper BD, Yoganandan N, Pintar FA, Rao RD. Anterior longitudinal ligament injuries in whiplash may lead to cervical instability. Med Eng Phys. 2006 Jul;28(6):515-24. doi: 10.1016/j.medengphy.2005.09.011. Epub 2005 Nov 10. PMID: 16289824.
5.Katzberg RW, Benedetti PF, Drake CM, Ivanovic M, Levine RA, Beatty CS, Nemzek WR, McFall RA, Ontell FK, Bishop DM, Poirier VC, Chong BW. Acute cervical spine injuries: prospective MR imaging assessment at a level 1 trauma center. Radiology. 1999 Oct;213(1):203-12. doi: 10.1148/radiology.213.1.r99oc40203. PMID: 10540663.
from Centeno-Schultz Clinic https://centenoschultz.com/anterior-longitudinal-ligament-could-this-be-responsible-for-your-ongoing-neck-pain/
0 notes
Text
Cervical Fusion: The Truth That You Need to Know!
The neck pain started out gradually but continued despite conservative care and medications. Your doctor referred you for a surgical consultation. What is Cervical Fusion? Are there different types of Cervical Fusions? What happens during surgery? What are the indications for Neck Fusion surgery? What is the recovery from Neck Fusion? What are the complications associated with Cervical Fusion? What are the alternatives to Cervical Fusion? What regenerative alternatives exist?
Cervical Fusion: Introduction
Cervical Fusion is often recommended when chronic neck pain problems worsen over time. What exactly is it?
Cervical Fusion is a major surgery that involves joining one or more of the spinal bones together using screws, bolts, and plates (1). The hardware may be placed in the front (anterior) or the back( posterior) of the Cervical spine. The disc between the spinal bones is often times removed and replaced with a bone graft or a spacer.
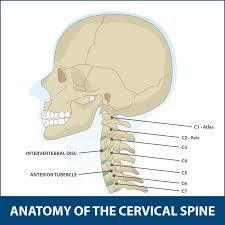
The neck of composed of 7 boney building blocks that are numbered from 1-7. The letter C is associated with the numbers to designate the Cervical Spine. Hence the bones in the neck are C1 through C7. Sandwiched between neck bones are important shock absorbers called Discs. A Cervical Fusion surgery removes this important shock absorber and joins the adjacent bones together with hardware.
Find out if Cervical Fusion is the right procedure for you. This post will cover the types of Cervical Fusion and indications.
Types of Cervical Fusion Procedures
There are several different types of Cervical Fusion procedures. The differences in part are due to their approach to the Cervical Spine. The two most common Cervical Fusions are an Anterior Cervical Discectomy (ACDF) and a Posterior Fusion. The goal is the treat symptomatic neck conditions that are progressive in nature and have not responded to conservative therapy. The Disc is removed in an effort to decrease the pain and relieve exiting nerve root or Spinal Cord compression. The principal difference between these two surgeries is the approach to the spine. One is from the front (anterior) whereas the other is from the back (posterior).
Side View X-ray of Anterior Cervical Discectomy (ACDF)
Anterior Cervical Discectomy and Fusion (ACDF) Interbody Fusion
This is one of the most common type of neck surgeries. One study cited an average of 137,000 ACDF surgeries performed annually in the United States (2). It involves removing the Disc through the front of the neck followed by the insertion of a plate with screws to stabilize the spine.
Posterior Fusion
A Posterior Fusion surgery involves removing the Disc from the backside of the neck. The surgical approach is from the posterior. Access to the Disc is more difficult through a posterior approach. Accordingly, there are significant postoperative complications with this approach that range from 8.6-49% (3)
What Happens During the Surgery?
Cervical Fusion is performed at a hospital or outpatient surgical center. It involves a general anesthetia in which you are put to sleep for the duration of the surgery.
Anterior Cervical Discectomy and Fusion has four principal steps.
Step 1: Anterior surgical approach
Anterior refers to the front of the neck. A horizontal skin incision is made in the front of the neck followed by separation of the different layers of muscle, tendons and fasica.
Step 2: Removal of Disc AKA Discectomy
After the correct Cervical Disc is identified using x-ray, it is surgically cut out. This removes the problematic Disc and allows evaluation of deeper structures in the Cervical Spine.
Step 3: Decompression of the Cervical Canal
Once the Disc in removed, the Posterior Longitudinal Ligament (PLL) is identified. This stabilizing ligament is frequently trimmed or cut out to allow for visualization of the central spinal canal. If an extruded Disc, Disc fragments or bone spurs are present within the Central Canal, and they are surgically removed. In addition, the boney doorway through which the spinal nerves exits is evaluated and roto-rootered out if bone spurs are compressing or irritating the spinal nerves.
Step 4: Cervical Fusion
A surgical cage or implant along with a bone graft is then inserted into the space previously occupied by the Cervical Disc. The goal is to maintain the disc space height and promote the two Cervical bones to mend together. A small plate is then attached in the front of the neck to the cervical bones. It provides stability and promotes fusion of the two bones.
Indications for Neck Fusion Surgery
There are several Cervical Spine conditions that may require surgery. The most common include:
Cervical Disc Degeneration/Injury
The Disc a important shock absorber that is sandwiched between the spinal bones in the neck. It is susceptible to injury and degeneration as result of trauma, and repetitive wear and tear. One or more Discs may become a source of severe neck pain. When conservative treatments fail some patients are referred for Cervical Fusion surgery.
Cervical Spinal Instability
The neck is composed of 7 bones stacked upon one another. They are held in place by ligaments, muscles, tendons, and fascia. If any of these structures are weakened or injured one of more of the stacked bones can slip forward. This is called Anterolisthesis. If the bone slips backwards in relation to the other bones, it is called Retrolisthesis. This movement can cause significant irritation and or injury to the Spinal Cord, exiting nerve roots, Facet joints and Cervical Discs. This in turn can cause debilitating neck and upper extremity pain. When it involves the ligaments that hold the head onto the neck patients can suffer significant neurologic symptoms including brain fog, fatigue, headaches, visual problems and vertigo. This condition is known as Craniocervical Instability (CCI). To learn more about Craniocervical Instability please click on the video below.
youtube
Nerve Compression
Nerves exit the Cervical Spine through a boney doorway called the Neural Foramen. The Foramen can be narrowed by Disc protrusion, Disc herniation, Facet joint overgrowth, ligament instability, Disc slippage or a cyst causing compression or injury to the nerve. This can cause radiating arm and hand pain, numbness and tingling and reduced muscle strength. When unresponsive to conservative care, some patients are referred for Neck Fusion evaluations.
Spinal Cord Compression
The Spinal Cord is the nerve network that controls most of your body’s function. It starts at the base of the brain and extends into the low back. It is encased in a protective layer of bone. It is surrounded and protected by an additional layer of fluid called the Cerebral Spinal Fluid. The Spinal Cord is fragile and susceptible to injury. Symptoms can be mild or severe depending on the extent of the damage. A tragic example is that of Christopher Reeves who sustained a traumatic Spinal Cord injury after a falling from a horse. He was paralyzed and required assistance with all bodily functions including breathing.
Trauma to Cervical Spine
Trauma to the spine can cause instability, compression of nerves and discs. Cervical Fusion is often recommended in severe cases to stabilize the spine and avoid Spinal Cord injury and paralysis.
Infection
The Cervical bones and Disc can become infected causing significant damage the neck. Neck Fusion is a treatment option when the infection is not controlled with antibiotic therapy.
Tumors
Cancer can occur anywhere in the body. When it occurs in the neck it can compromise the Spinal Cord, exiting Spinal nerves and the Discs. When the integrity of the Spine is compromised and conservative treatments fail, Cervical Fusion is often recommended.
Recovering From Neck Fusion Surgery
Recovery Time
Recovery time can vary widely from patient to patient. Factors affecting recovery time include severity of neck injury, activity level prior to the Neck Fusion and number of Cervical levels fused. Surgical pain typically improves in 1-3 weeks. Physical therapy is essential after the surgery and is typically started 3-4 hours after the surgery. The goal is provide strengthening and improve range of motion.
Eight Potential Complications Associated with Neck Fusion
There are inherent risks associated with any surgery. The most common complications from a Cervical Fusion include:
Difficulty Swallowing
Difficulty swallowing is called Dysphagia and can occur after Neck Fusion. The incidence of dysphagia after Cervical Fusion Surgery in one study was 12.7% (4). Difficulty swallowing can compromise calorie, fluid intake, and healing.
Failed Fusion
This is BAD news. Failure of the bones to fuse is called Non-union or Pseudoarthrosis. It means that despite the surgery, the inserted screws and plates, the extensive rehabilitation, and the pain the bones did not fuse together. The intended surgery has failed and now there is instability in the neck. The incidence of Non-union is striking and in one study was found to be 52% (5). The treatment for Non-union is terrible as it involves another surgery where the Fusion is revised and oftentimes the fusion is extended up or down an additional level.
Continued Neck Pain
Despite Neck Fusion surgery, many patients continue to have ongoing neck pain that requires oral narcotics. In a recent study 1 year after neck fusion only 39% of patients were able to return to work (6).
Spinal Fluid Leak (CSF)
The Dura is the outermost membrane that covers the Brain and Spinal Cord. This important membrane can be punctured during surgery causing a leak of Spinal Fluid. The incidence ranges from 1-17% (7). Severe headache is a common symptom of Spinal Fluid Leak. If left untreated, a Spinal Fluid Leak (CSF) can lead to infection, Brain abscess, and bleeding.
Nerve Injury
Nerves can be damaged during surgery and the incidence varies from 0.18% to 2.6% (8). Nerve injury can include exiting nerves as well as the spinal cord itself. After Cervical Fusion surgery patients may awaken after surgery with new onset left arm, face, or lower extremity pain.
Changes in Spinal Curve
The natural C curve in the neck is important for optimal function as it ensures proper alignment of all the bones, tendons, and ligaments in the neck. Cervical Fusion surgery not only alters the natural C curve in the neck but also adversely affects the curve in the low back. Ouch! A new study demonstrated that patients who underwent Cervical Fusion noted changes in both the neck, tailbone, and pelvis curves. This oftentimes leads to the onset of pain and injury (9).
Infection

Infection is a devastating complication and was found to occur in 16.6% of patients in a recent study. (10). Infection can involve the skin, muscle or bone. Treatment involves antibiotics, wound care, and 47% of patients in a recent study required additional surgery for wound care and skin grafting.
Adjacent Segment Disease
Adjacent Segment Disease (ASD) is a common complication of Neck Fusion with an incidence of 21% (11). It occurs as a direct result of the Fusion surgery. Why? The neck Discs are designed to absorb the forces of daily living. Fusing one or more discs together results in additional forces being placed on the Disc and Facet joints above and below the Fusion. This additional pressure results in wear and tear and degeneration often times requiring additional surgery. See our video below:
youtube
Alternatives to Cervical Fusion
There are several non-surgical treatment options for ongoing neck and arm pain. The appropriateness and success of these treatment options is based upon the severity of the injury, current symptoms and co-existing medication conditions. The most common treatments include:
Conservative Care
Conservative care when appropriate is the first line treatment for neck and arm pain. Treatment options include rest, stretching, physical therapy, and chiropractic care. The goal is to reduce ongoing pain and increase function.
Medications
Medication is often used in conjunction with conservative care. Examples include anti-inflammatory agents and muscle relaxants. Oral steroids are often recommended when pain persists but should be avoided due to the significant side effects including destroying cartilage, depressing stem cell activity and altering sugar levels. To learn more about the adverse effects of steroids please click here.
Traditional” Pain” Injections
When medication and conservative care fail, patients are often referred to a pain clinic for injections. These are STEROID injections and should be avoided. Steroids are powerful ant-inflammatory agents with many side effects detailed above. Furthermore, they can accelerate the underlying problems. Steroids cannot heal an injured Disc or Facet joint. Steroids can only decrease the inflammation associated with the injury. Healing of a neck injury requires a Regenerative option.
Regenerative Alternatives to Cervical Fusion
The Centeno-Schultz Clinic are experts in the treatment of neck pain. We are also experts in the use of PRP and Bone Marrow Concentrate in the spine. In 2005 we become the first clinic in the world to inject Bone Marrow-derived stem cells into the Disc. We are also leaders in the field of Regenerative Medicine and Interventional Orthopedics. We have published extensively in recognized, peer-reviewed journals. Our list of publications is available here.
Our approach is much different. Unlike the rushed, brief exam in most Orthopedic offices, we spend a dedicated amount of time reviewing your chief complaint, its duration, aggravating and alleviating factors, treatment to date, past medical history, medications, and events that led to the injury. We also review in detail all imaging. This includes x-ray, MRI, and CT scans.
Our approach is comprehensive in nature as we believe the body functions as a unit. For example examination of the shoulders is critical when evaluating patients with neck pain. This is because many patients with low Neck pain also have ongoing shoulder problems. The approach is referred to as SANS which stands for: Stability, Articulation, Neuro-Muscular and Symmetry. To learn more about our SANS approach please click here.
At the Centeno Schultz Clinic, there are an extensive number of Regenerative treatment options for patients with ongoing neck and or arm pain. The specific treatment will depend upon the underlying cause of the pain, its severity, and the patient’s symptoms. Treatment options include both PRP and Bone Marrow Concentrate which contains stem cells. We utilize customized PRP injections to ensure the best clinical results. It is important as middle aged and older patients require higher concentrations of PRP than younger patients. To learn more about the importance of PRP concentration please click here.
Both Bone Marrow Concentrate and PRP are precisely injected into the neck using x-ray and ultrasound guidance. The injections are challenging and cannot be performed by your surgeon, chiropractor, or physician assistant. To watch a Centeno-Schulz Clinic injection click on the video below.
youtube
In Conclusion
Cervical Fusion is a major surgery that involves joining one or more of the Spinal bones together using screws, bolts and plates.
The two most common Cervical Fusion procedures include the Anterior Cervical Discectomy and Fusion (ACDF) and Posterior Fusion.
ACDF involves four principal steps which are described above.
The most common indications for Neck Fusion are Disc degeneration, Cervical instability, nerve compression, Spinal Cord compression, trauma, infection and tumors
Recovery time from Neck Fusion surgery varies depending upon multiple factors
The eight potential complications associated with Cervical Fusion surgery include difficulty swallowing, failed fusion, continued neck pain, Spinal Fluid Leak, nerve injury, changes in spinal curve, infection, and Adjacent Segment Disease.
Alternatives to Cervical Fusion include when appropriate conservative care, medications and traditional pain injections.
Steroids are powerful ant-inflammatory agents that are associated with significant side effects and only treat the inflammation and NOT the underlying problem.
Regenerative treatment options identify and address the underlying problems utilizing a comprehensive approach and targeted injections using ultrasound and x-ray.
PRP and Bone Marrow Concentrate are powerful treatment options for neck and arm pain.
If you or a loved one continue to suffer from neck and or arm pain that has not responded to conservative therapy please schedule a telemedicine consultation. A board certified, fellowship trained physician will review your history, imaging and discuss appropriate treatment options.
1.Srikhande NN, Kumar VAK, Sai Kiran NA, et al. Clinical presentation and outcome after anterior cervical discectomy and fusion for degenerative cervical disc disease. J Craniovertebr Junction Spine. 2019;10(1):28-32. doi:10.4103/jcvjs.JCVJS_87_18
2.Epstein NE. A Review of Complication Rates for Anterior Cervical Diskectomy and Fusion (ACDF). Surg Neurol Int. 2019;10:100. Published 2019 Jun 7. doi:10.25259/SNI-191-2019
3.Badiee RK, Mayer R, Pennicooke B, Chou D, Mummaneni PV, Tan LA. Complications following posterior cervical decompression and fusion: a review of incidence, risk factors, and prevention strategies. J Spine Surg. 2020;6(1):323-333. doi:10.21037/jss.2019.11.01
4.De la Garza-Ramos R, Xu R, Ramhmdani S, Kosztowski T, Bydon M, Sciubba DM, Wolinsky JP, Witham TF, Gokaslan ZL, Bydon A. Long-term clinical outcomes following 3- and 4-level anterior cervical discectomy and fusion. J Neurosurg Spine. 2016 Jun;24(6):885-91. doi: 10.3171/2015.10.SPINE15795. Epub 2016 Feb 19. Erratum in: J Neurosurg Spine. 2016 Jun;24(6):996. PMID: 26895527.
5.https://medicalxpress.com/news/2018-10-pseudarthrosis-single-level-acdf-peek-interbody.html
6. Faour M, Anderson JT, Haas AR, et al. Return to Work Rates After Single-level Cervical Fusion for Degenerative Disc Disease Compared With Fusion for Radiculopathy in a Workers’ Compensation Setting. Spine. 2016;41(14):1160-6.DOI: 10.1097/BRS.0000000000001444.
7.Tosun B, Ilbay K, Kim MS, Selek O. Management of Persistent Cerebrospinal Fluid Leakage Following Thoraco-lumbar Surgery. Asian Spine J. 2012;6(3):157-62. doi: 10.4184/asj.2012.6.3.157.
8.Cheung JP, Luk KD. Complications of Anterior and Posterior Cervical Spine Surgery. Asian Spine J. 2016;10(2):385-400.doi: 10.4184/asj.2016.10.2.385
9.Cheung JP, Luk KD. Complications of Anterior and Posterior Cervical Spine Surgery. Asian Spine J. 2016;10(2):385-400.doi: 10.4184/asj.2016.10.2.385
10.Barnes M, Liew S. The incidence of infection after posterior cervical spine surgery: a 10 year review. Global Spine J. 2012;2(1):3-6.doi: 10.1055/s-0032-1307252.
11.Wu XD, Wang XW, Yuan W, et al. The effect of multilevel anterior cervical fusion on neck motion. Eur Spine J. 2012;21(7):1368-1373. doi:10.1007/s00586-012-2157-7
from Centeno-Schultz Clinic https://centenoschultz.com/cervical-fusion-the-truth-that-you-need-to-know/
0 notes
Text
What Is the Alar Ligament?
Introduction
Medicine is highly specialized now. Each specialty has a series of checkboxes that patient’s symptoms nicely fit into. For example, irregular heart rhythm with abnormal ECG is a cardiology problem. Shortness of breath with abnormal chest x-ray can be effectively evaluated and treated by a pulmonologist. Unfortunately, the symptoms and presentation of patients with upper cervical spine inatability do not fit nicely into any box. The irregular and often elevated heart rate is baffling to most cardiologists and most patients walk away with ” normal ” cardiac workup. So too with vertigo as the ENT specialist can find no explanation for their symptoms. Craniocervical instability is real and can present with a number of symptoms that do not conveniently fit into a one specialists box. At the Centeno-Schultz Clinic we are committed to advancing a better understanding of this debilitating condition.
Where Is the Alar Ligament Located?
The Alar ligaments are paired ligaments located at the upper cervical spine. A ligament is a thick band of connective tissue. Think of them as duct tape. As such the Alar ligament is duct tape that holds your head onto your neck. More specifically it is the thick band of connective tissue that connects the skull to the C2 bone. Anatomically speaking the Alar ligament joins the occipital condyles to the Dens (C2 bone). They lie on either side of the Apical ligament. They are thickest at the Occipital attachment. Their orientation can oblique or horizontal (1)
What Is the Function of the Alar Ligament?
The function of the Alar Ligament is to stabilize the upper cervical spine, limit rotation and contra-lateral lateral flexion. Lateral flexion is side bending of the neck. An example would be stretching your neck to the side in an attempt to touch your ear to your shoulder.
How Many Alar Ligaments are There?
Each of us have two Alar ligaments. A right and left Alar ligament that work together to provide stability for the upper cervical spine.
Injury to the Alar Ligaments
Upper cervical spine injuries are common and mainly caused by car and sport accidents or falls (2). Rotation of the neck and/ or hyperflexion is common in Alar ligament injuries (3). Dvorak demonstrated that Alar ligament was extended the most while the head is rotated and bent forward (flexed) (4). It is most vulnerable to injury in this position. Examples include:
A rear-end car crash, especially one where the head hits the back window (e.g., a pickup truck)
A sudden jolt to the neck/head
Something falling on the head
Placing axial loads on the head (e.g., one patient who performed a neck exercise by arching his back to place his whole weight on the head)
The Alar ligament can be also be injured with an overly aggressive chiropractic adjustment.
Other causes of Alar ligament injury include cogential disorders with hypermobility of the joints and spine. A classic example is Ehlers-Danlos Syndrome (EDS). To learn more about EDS and upper neck instabiity please click here.
What Is Craniocervical Instability (CCI)?
Injury to the Alar ligament can lead to upper cervical spine instability otherwise known as Craniocervical Instability (CCI). This is where there is excessive movement at the head neck junction. The upper neck facet joints (C0/C1, C1/2) become unstable and move around too much leading to injury and arthritis. This is turn recruits the muscles and tendons to work overtime to stablize the upper neck. Over time the muscles and tendons become overwhelmed and become injured and a source of pain and dysfunction.
Craniocervical Instability (CCI) is a medical condition characterized by injury and instability of the ligaments that hold your head onto the neck. The major ligaments involved are the Alar, Transverse and Accessory ligaments. It is a poorly understood condition that can be debilitating. Regretably it is often missed or misdiagnosed by medical providers. To learn more about CCI pleaseclick on the video below:
youtube
What Are the Symptoms of Alar Ligament Injury? (Feel Terrible)
Alar ligament injury can cause excessive movement between your head and neck. This in turn can cause movement and damage of upper cervical facet joints, discs, nerves, and blood vessels. Symptoms vary depending upon the severity of the ligament instability. In general the greater the instability the greater and more severe the symptoms. Common symptoms include.
1. Painful, Heavy Head
A constant to near-constant head pain that can be described as feeling like the head is too heavy for the neck to support. Many describe feeling like they have a “bobble-head”.
2. Headache
This is not your normal headache caused by your in-laws or excessive consumption of alcohol. This is a debilitating headache that is constant in duration and miserable. Headache is often caused by injury to the upper neck joints, muscles, and tendons due to ongoing instability.
3. Rapid Heart Rate
Elevated heart rate may occur as the Vagus nerve gets irritated by the extra motion in the upper neck. Another cause of elevated heart rate is Postural Orthostatic Tachycardia Syndrome (POTS). POTS is a medical condition that causes malfunction of the Autonomic nervous system. It is estimated to impact between 1,000,000 and 3,000,000 Americans. The Autonomic nervous system controls involuntary body functions such as heart rate and blood pressure. Malfunction of the Autonomic nervous system causes a number of symptoms which include rapid heart rate.
4. Brain Fog
Patients with CCI can struggle with memory, concentration, and ability to complete tasks. Every day can feel like your brain is stuffed full of cotton.
5. Neck Pain
Pain is typically localized at the base of the skull and aggravated bending forward and rotation. The pain can shoot up into the base of the skull, top of the head, forehead or behind the eyes.
6. Visual Problems
Visual disturbances can vary from mild to severe involving a number of different symptoms. Visual disturbances can happen because the upper neck supplies information to the brain to guide eye position and vice versa (5).
7. Dizziness
Balance problems can be a significant issue (6). Dizziness or imbalance is a feature related to the fact that the upper neck is a major contributor to balance (4). The upper neck provides position sense that has to be coordinated with balance information from the eyes and inner ear.
8. Chronic Fatigue
Excessive movement between the head and neck can cause irritation and dysfunction of the nervous system. The Autonomic nervous system is the most affected. A common symptom of autonomic dysfunction is chronic fatigue.
How Is an Alar Ligament Injury Diagnosed?
Regrettably, many clinics and providers focus on treating symptoms. Neck pain is not a diagnosis but rather is a symptom. At the Centeno-Schultz Clinic we are committed to understanding the underlying cause of your neck pain and dysfunction. An accurate diagnosis is critical. This will allow for a definitive treatment paln which in turn will allow for the best clinical outcomes. Diagnosing Craniocervical Instability (CCI) involves 7 main criteria which include:
Mechanism of Injury (How Did It Occur)
Understanding how and when the injury occurred is important. The two most common causes of CCI are trauma and medical conditions that cause people to have loose or compromised ligaments (8). Motor vehicle accidents, contact sports, and forceful manipulations by chiropractors are the most common examples of trauma. Ehlers Danlos Syndrome (EDS) is a group of inherited disorders that affect your ligaments and connective tissues (7).
Symptoms (Headache, Neck Pain and Neurologic Symptoms)
The symptoms associated with CCI can be extensive depending upon the severity of the instability. The most common symptoms include headache, upper neck pain, dizziness, visual disturbances, brain fog, fatigue, anxiety, visual challenges and elevated heart rate.
Physical Examination
In the age of managed care and 15-minute appointments, the art and practice of physical examination by a physician is almost gone. At the Centeno -Schultz Clinic all new patient evaluations undergo an extensive physical examination. Why? It is important to view the body as a whole and there are multiple potential physical findings in the neck, head, shoulder, and low back in patients with Cranial Cervical Instability.
Radiographic Studies for Cranial Instability ( Upper Neck MRI or DMX)
There are various types of radiographic studies which include x-ray, CT scan, and MRI. Unfortunately, traditional MRI and CT studies do not evaluate the upper cervical spine or alar and transverse ligaments. Special radiographic studies are required which include upper cervical MRI or rotatory CT scan. In addition, there are additional studies that involve the patient moving during the examination. These studies are useful to identify instability. Examples include upright MRI with upright flexion/extension. To see how this works please click on the video below.
Finally, a Digital Motion X-ray (DMX) is important in establishing the diagnosis of CCI. This is an x-ray examination that is recorded in which the patient is put through various movements including bending the neck forward, backward, and to the side. To learn more about DMX please click on the video below.
youtube
Response to Conservative Care
The common symptoms of CCI can also arise from different clinical conditions. For example, headaches with dizziness may arise from tight or contracted neck muscles. It is important that patients undergo conservative care such as rest, heat, stretching, physical therapy, massage, and chiropractic care. In some cases, symptoms improve with conservative therapy.
Response to Diagnostic Injections
A diagnostic injection is a precise injection into a specific structure asking the question of whether or not it resolved the pain. Often times this is very helpful in the evaluation of patients with CCI. All diagnostic injections are performed under ultrasound or x-ray guidance, or both. Examples of diagnostic injections include:
C0-1 and C1/2 Facet injections
Occipital nerve blocks
Superficial Cervical Plexus Blocks
Ligament injections
Level of Disability
Due to the severity of the symptoms, many patients are not able to complete their domestic or professional responsibilities. In severe cases of CCI, patients are confined to their homes and are socially isolated. The level of disability is important in evaluating and diagnosing Craniocervical Instability (CCI).
What Are the Treatment Options for Alar Ligament Injuries? (Conservative, Posterior Injections, Surgery)
There are three major types of treatment options. The specific type of treatment will depend upon the amount of instability and severity of symptoms.
Conservative
Patients with small amounts of instability can oftentimes be managed with conservative care. Conservative treatment options would include:
1. Upper cervical chiropractic care. Look for members of NUCCA (National Upper Cervical Chiropractic Association)
2. Physical Therapy
3. Bracing
4. Curve restoration. Look for chiropractors that specialize: Chiropractic BioPhysics.
Posterior Neck Injections
If conservative care fails to provide clinical improvement the next step is x-ray guided injections into the upper neck (8). Specifically, this would include injections into the Facet joints and Upper Cervical ligaments. An example would be the Supra and Interspinous ligaments that connect one vertebra to the next. Injections may utilize prolotherapy, PRP or Bone Marrow Concentrate. Not all injections are the same. There can be significant differences between clinics and practitioners. Accurate needle placement requires the use of x-ray and contrast. Contrast otherwise known as dye demonstrates where the needle it is. Equally important is it ensures that the needle is not in a blood vessel which can cause a serious complication. This is critical because if the needle is not in the targeted joint, the injected PRP or bone marrow concentrate will NOT magically get into the joint.
Surgery ( Fusion of Head to Neck)
If conservative care and injections fail many patients are referred for surgery.
There are many different types of surgical options all of which include Fusion. Fusion is a surgery that connects one or more segments of your spine together using screws, bolts, and plates. The goal is to provide stability. The most common is a Fusion of the head to the Cervical spine. This is illustrated in the picture to the right. It involves multiple screws and rods that are placed into the skull and neck. The procedure is major surgery with significant risks which include eventual arthritis above and below the Fusion, misplaced screws in nerves of Facet joints, and failure of the bones to fuse (non-union). Neck range of motion is permanently altered and, in most cases, severely restricted.
New Regenerative Treatment Option
In 2015 a nonsurgical treatment option for Cranial Cervical Instability was developed at the Centeno-Schultz Clinic. It involves the injection of a patient’s own bone marrow-derived stem cells into the damaged Alar, and Transverse ligaments. The procedure is very demanding and only performed at the Centeno-Schultz Clinic in Broomfield Colorado. The procedure is called Percutaneous Implantation of Cervical Ligaments (PICL) To learn more about this groundbreaking procedure please click on the video below.
youtube
In Summary
Medicine is highly compartmentalized with symptoms ideally fitting into checkboxes.
The symptoms and presentation of patients with Craniocervical Anstability do not fit the traditional checkboxes and therefore is often missed.
The Alar ligament is a paired ligament (a right and left) that is in the upper cervical spine.
The Alar ligaments function as duct tape to hold your head securely to your neck.
Injury of the Alar ligament can occur from trauma, overly aggressive chiropractic adjustments or due to congenital disorders.
Craniocervical Instability is medical condition characterized injury and instability of the ligaments that hold your head onto the neck. The major ligaments involved are the Alar, Transverse, and Accessory ligaments.
The symptoms of Craniocervical Instability are many and include headache, painful heavy head, brain fog, neck pain, vertigo, and fatigue.
There are 7 major criteria in diagnosing Craniocervical Instability.
Treatment options depend upon the severity of the instability and include when appropriate conservative care, injections, and surgery.
The PICL (Percutaneous Injection of Cervical Ligaments) is a breakthrough regenerative treatment option that allows appropriated identified patients to avoid surgery.
To learn more about the Alar ligament and Craniocervical Instability please download Dr. Centeno’s new book by clicking here.
If you or a loved one continue to suffer from headaches, dizziness, brain fog and chronic fatigue that has not responded to conservative therapy please schedule a telemedicine consultation. A board certified, fellowship trained physician will review your history, imaging and discuss appropriate treatment options.
—————————————————————————————————————————
1.Osmotherly PG, Rivett DA, Mercer SR. Revisiting the clinical anatomy of the alar ligaments. Eur Spine J. 2013;22(1):60-64. doi:10.1007/s00586-012-2496-4
2.Kaufmann RA, Marzi I, Vogl TJ. Delayed diagnosis of isolated alar ligament rupture: A case report. World J Radiol. 2015;7(10):357-360. doi:10.4329/wjr.v7.i10.357
3.Unal TC, Dolas I, Unal OF. Unilateral Alar Ligament Injury: Diagnostic, Clinical, and Biomechanical Features. World Neurosurg. 2019 Dec;132:e878-e884. doi: 10.1016/j.wneu.2019.07.198. Epub 2019 Aug 2. PMID: 31382064.
4.Panjabi M, Dvorak J, Crisco JJ 3rd, Oda T, Wang P, Grob D. Effects of alar ligament transection on upper cervical spine rotation. J Orthop Res. 1991 Jul;9(4):584-93. doi: 10.1002/jor.1100090415. PMID: 2045985.
5.Ischebeck BK, de Vries J, Van der Geest JN, et al. Eye movements in patients with Whiplash Associated Disorders: a systematic review. BMC Musculoskelet Disord. 2016;17(1):441. Published 2016 Oct 21. doi:10.1186/s12891-016-1284
6..Biesinger E. and Vertigo caused by disorders of the cervical vertebral column. Diagnosis and treatment. Adv Otorhinolaryngol. 1988; 39: 44– 51.
7.. Sobey G. Ehlers-Danlos syndrome – a commonly misunderstood group of conditions. Clin Med (Lond). 2014;14(4):432-436. doi:10.7861/clinmedicine.14-4-432
8.Centeno CJ1, Elliott J, Elkins WL, Freeman M. Fluoroscopically guided cervical prolotherapy for instability with blinded pre and post radiographic reading. Pain Physician. 2005 Jan;8(1):67-72. https://www.ncbi.nlm.nih.gov/pubmed/16850045
from Centeno-Schultz Clinic https://centenoschultz.com/what-is-the-alar-ligament/
0 notes
Text
Understanding Cervical Spine Instability Measurements
Cervical Spine Instability Measurements: How To Precisely Interpret Them
It was all a blur. You were waiting for the red light to change when a large truck slammed into your vehicle. You did not see the approaching vehicle but heard the skidding tires. The brain fog, dizziness and fatigue have not responeded to conservative therapy. Work and domestic responsibilites are overwhelming and difficult to complete. Isolation and sadness are constant companions. Your surgical consultation was overwhelming. They reviewed the x-rays and MRIs taking different measuresurements. You are so confused. What are cervical spine instability measurements? What are the basic structures in the cervical spine?
Introduction
Injuries to the upper cervical spine can cause a large number of poorly recognized or understood symptoms such as brain fog, dizziness and severe fatigue. As such many such injuries are misdiagnosed or missed altogether. Many patients are inappropriated labeled as psychologically unstable or hormonal. Cervical spine instability is real and can profoundly affect patients and their families alike. Cervical spine instability measurements are important to understand as they can lead to the accurate diagnosis of injuries to the upper cervical spine.
The Spinal Anatomy: An Overview
To understand Cervical Spine Instability Measurements, a basic review of neck anatomy is in order. The Cervcial Spine is composed of Discs, Facet joints, ligaments, nerves, tendons and tendons.
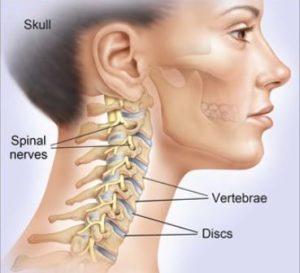
Bones
The bones in the neck are stacked upon one another. They are also known as vertebral bodies. These boney building blocks are numbered 1 through 7. The letter C precedes each number indicating that we are referencing the Cervical Spine. C=cervical. The top bone is the C1 and is also referred to as the Atlas. The lowest bone in the neck is the C7
Discs
The Disc is a fibrocartilage cushion that is sandwiched between each of the Vertebral Bodies. It is an important shock absorber. Its name is based on the bones it is sandwiched between. For example, the Disc between the C6 and C7 Vertebral Body is referred to as the C6/7 disc. It is susceptible to injury. Common examples of Disc injuries include Protrusions, Herniations, and Extrusions.
Facet Joints
The Facet Joints are small, paired joints on the backside of the neck. There is right and left Facet Joint at each spinal level. The Facet Joints provide important stability to the neck and limit movement. Like the knee and ankle joints, the Facet Joints are lined with cartilage which allows for smooth, pain-free motion. Unfortunately, Cervical Facets is susceptible to injury with the compromise of the joint cartilage and joint health. The result can be a limited range of motion in the neck and pain.
Ligaments
Ligaments are thick pieces of connective tissue that connect bone to bone. Essentially they are human Duck tape. They provide stability for the neck and head. There are a large number of ligaments in the Cervical Spine. The two most important ligaments are the Alar and Transverse ligaments. These ligaments essentially connect your head to your neck. Unfortunately, these ligaments are susceptible to injury.
Tendons
Tendons are connective tissue that connect muscle to bone. Muscles and tendons in the Cervical Spine provide important stability and enable movement. Tendons are susceptible to injury due to trauma, repetitive use, and degeneration. Injured tendons can jeopardize neck stability, health, and movement. The consequences can be nech pain, headaches, and a limited range of motion.
Spinal Cord
The Spinal Cord consists of neural tissue that starts at the base of the brain and extends down into the low back. It is a cylindrical bundle of nerve fibers that control our voluntary and involuntary bodily functions. It carries signals between the brain and the rest of the body. As the Spinal Cord descends from the skull and through the neck and rest of the body it is protected on all sides by spinal bones. These bones provide a boney armor to protect against injury. The Spinal Cord has an additional layer of protection afforded by the spinal fluid. The spinal fluid is also known as Cerebral Spinal Fluid. It surrounds the Spinal Cord and extends the entire length of the spine. The image to the right is a side view of the Spinal Cord as it exits the brain. The Spinal Cord is black in color. The white that surrounds it is the spinal fluid.
Cranial Nerves
As the Spinal Cord descends through the Foramen Magnum and spine, important nerves branch off traveling to different parts of the body. There are a large number of nerves. These include the 12 Cranial nerves some of which control muscles whereas others are connected to internal organs such as the heart and lungs.
Arteries and Veins
Arteries and veins provide blood flow to and from important structures in the head, neck, and body. Without blood flow, the body can not function.
What Is the Alar Ligament?
Ligaments are thick bands of connective tissue that connect one bone to another. The Alar ligament is a critical ligament in the upper neck as it connects your head to your neck. It connects the C2 bone (Dens) to the base of the skull. There is a right and left Alar ligament. Injury to the Alar ligament can lead to Craniocervical Instability. To learn more about this condition, its symptms and nonsurgical treatment options please click here.
What Is the Transverse Ligament?
The Transverse ligament is a thick band of connective tissue that snuggly holds the C2 bone in place. Like the Alar ligament it provides important stability in the upper neck. To learn more about the Transverse ligament please click here.
Cervical Spine Instability
Stability is important for optimal function. Take the wheels on your vehicle for example. Properly adjusted lug nuts allow your wheel/ tires to perform optimally. This in turns allows your car to travel at appropriate speeds in a wide range of conditions including rain and snow. If however the lug nuts are loose, the wheel is unstable which severely compromises your ability to travel at any speed, or any distance.
So too with Cervical Spine. Optimal neck function requires that the Cervical Discs, Facet Joints, and ligaments are stable and in proper alignment. Stability is dependent upon muscle strength and ligament integrity. Injury or laxity of the neck ligaments can lead to compromise Cervical Spine stability and optimal function. Instability puts the neck Discs, Facet joints and nerves are risk for injury resulting in pain, impaired function, and restriction in range of motion.
Types Of Cervical Spine Instability
There are many different types of Cervical Instability. Symptoms vary depending upon the severity of the instability. The two major types of Cervical Instability are:
Craniocervical Instability (CCI)
Craniocervical Instability involves the ligaments that hold your head onto your neck (1). The principal ligaments are the Alar and Transverse ligaments. When these ligaments become injured or loose there is excessive motion of the head on the neck. This in turn can cause a constellation of debilitating symptoms. To learn more about CCI and nonsurgical treatment options please click here.
Atlantoaxial Instability (AAI)
The Atlas is the C1 bone. The Axis is the C2 bone. The C1 and C2 bone come together and form a joint that is appropriately called the Atlantoaxial joint (AA). When supporting ligaments are injured or become loose the joint becomes unstable resulting in pain and functional decline (2). To learn more about the Atlantoaxial joint please click here.
Why Measurements Are Necessary
Cervical Spinal Instability Measurements are important as they can help establish the diagnosis of Cervical Instability. This diagnosis is poorly recognized or understood by most physicians. Symptoms can vary signficantly from patient to patient. Futhermore most Cervical Spine MRIs do not examine or report on the integreity of the Alar, Transverse ligament , C0/1, C1/2 joints. At the Centeno-Schultz Clinic we manually calculate a patient’s Cervical Spine Instability measurements.
How Is Cervical Instability Measured? (Static vs Dynamic Measurements)
One of the most confusing things for patients to appreciate is that Cervical Instability is a dynamic concept which by definition involves motion. In medicine, for something to be “unstable” means that is moves more than it was designed to. This excessive motion can cause signficant irritation, injury to key structures like the Spinal Cord, Spinal nerves and joints. Often this can give rise to a variety of symptoms like brain fog, memory problems, fatigue, dizziness and headachess.
Traditonal MRIs are taken with patient lying stationary in a tube. There is no movement so this is a static radiographic study. This unfortunatley is the standard of care of big university medical centers. What is necessary are dynamic tests that can evaluate the cervical spine during motion. Let’s take a deeper look into both static and dynamic measurements
Static Measurements
Grabb-Oakes
The Grabb-Oakes is radiographic measurement used to evaluate upper Cervical Spine conditions. Its measurement involves a two step process. First a line is drawn from the anterior aspect of the Foramen Magnum ( basion) that extends to the inferior backside of the C2 bone (Dens). A second line is then drawn that is peripendicular to this line that extends to the Dura. Given that the C2 bone is held snuggly by the Transverse ligament, a high Grabb-Oakes measurement can be due to a damaged or loose Transverse ligament. An abnormal measurement is often considered to be 9mm or more (3). With the advent of flexion-extension MRI, it’s easier to measure the G-O measurement when the patient moves, which provides more information. To learn more about Grabb-Oakes measurement please click on video below.
youtube
Clivo-Axial Angle
Clivo-Axial Angle
This is the angle between the Clivus and the backside of the C2 bone (Dens) . The problem being measured here is the skull is falling forward on the upper neck which can cause irritation of the front the Brainstem and upper Spinal Cord. This movement is controlled by strong ligaments in the back of the neck at the Nuchal, Supraspinous, and Interspinous ligaments. It’s also controlled by the posterior Atlantoaxial membrane (PAOM, a ligament at the back of the spinal canal) and to a lesser extent the Transverse ligament. Normal and abnormal values vary depending upon the author. Less than 150 degrees (4) was originally reported with others stating that normal is between 145° to 160° in the neutral position (5).
Powers Ratio
This is another measurement that determines if the head has moved forward on the upper neck. This one is more complex, requiring two lines (one between the basion and the back of the spinal canal at C1 and another between the Opisthion and the posterior aspect the front of the Atlas) and then some division is applied. If it’s less than 1, the ratio is normal, if it’s >1 then it’s abnormal. To learn more, see the video below:
youtube
Atlantodens Interval (ADI)
This is the distance between the backside of the C1 bone (Atlas) and the anterior aspect of the C2 bone (Dens). It measures the integrity of the Transverse ligament. Normal value is less than 3mm in adults (6). To learn more about Atlantodental Interval please click here
Movement -Based Measurements (DMX & Upright MRI)
For patients with Cervical Spine Instability it’s critical to understand the differences between static and moving studies. Since instability is a movement-based concept, images that capture what happens to the Craniocervical Junction when it moves will always be far superior to static images. However, because this field is newer, these measurements are less established and the data about what’s normal and abnormal is still being collected
DMX
DMX stands for Digital Motion X-ray, which is an x-ray that is recorded while the patient moves. The patient is put through various manuevers such as bending forward, backwards and to the right and left side. The alignment of the upper Cervical bones is analyzed as the patient is put through various manuevers. The doctor can see the relationship between the bones and when they get out of position with motion, the ligaments holding them are likely injured or stretched out.
The two measurements that upper Cervical Spine Instability patients should pay attention to here are C1-C2 overhang and the ADI. C1-C2 overhang is the amount of motion that happens side to side between the C1 and C2 bone when the patient bends their head to the side (7). This is controlled mostly by the Alar and Transverse ligaments. The ADI stands for Atlantodental Interval and is the distance between the backside of the C1 bone and the front of the C2 bone. In patients with Craniocervial Instability this measurement can increase when they bend forward. To learn more about both measurements, see the video below:
youtube
Upright MRI
Traditonal MRIs are static in nature as the patient is lying still on their back. This does not capture motion based problems such as Craniocervical and Atlantoaxial Instability. Upright MRIs however are dynamic in nature as the patient is upright and can be flexed forward or extended backwards. This is a very powerful tool in the evaluation of Cervical Instability. The Grabb-Oakes, Clivoaxial angle and Power’s ratio can be measured in the neutral, forward flexed and extended position. To better understand how this works please watch the video below.
youtube
How Proper Diagnosis Can Impact Treatments
Cervical Spine Instability measurements are powerful tools as they can help establish the diagnosis of Upper Cervical Instability. In addition, they can identify the specific ligament or ligaments that are injured or loose. This is critical as it will identify the exact targets that need to be injected under x-ray. The precise injections are with PRP or Bone Marrow Concentrate which contains stem cells.
For example, if a patient has an abnormal Grabb-Oakes measurement, it means that the Transverse Ligament is loose or injured. The Transverse ligament would then be one of the targeted structures in their treatment.
If the Clivio-Axial angle is abnormal the means that the ligaments in the back of the head are loose. Accordingly the Nuchal ligament, Supra and Infraspinous ligaments and PAOM would be targeted structures in their treatment.
If the C1/2 overhang on DMX is abnormal the targeted structures for treatment would be the Alar and Transverse ligament.
Diagnosing Cervical Spine Conditions Needs Precision
One of the most common problems we see in clinic is that patients do not have a formal diagnosis. Neck pain is not a diagnosis but rather is a symptom. It is only when an accurate diagnosis is established that an appropriate treatment plan can be discussed. Too many patients have undergone countless MRIs all of which are normal. This is because they are static imaging with the patient lying down. Dynamic studies such as upright MRI and DMX allow for the evaluation of instability. Cervical Spine Instability measurements are powerful tools that can help in the diagnosis of Upper Cervical Instability.
In Summary
Cervical Instability is real and regrettably often not appreciated or misdiagnosed.
Cervical Spinal Instability measurements are important as they can help establish the diagnosis of Cervical Instability.
The Cervical Spine is composed of bones, discs, facet joints, nerves, arteries, spinal cord and ligaments.
The Alar and Transverse ligament are the key stabilizer in the Upper Cervical Spine.
The two most common types of Cervical Spine Instability are Craniocervical Instability (CCI) and Atlantoaxial Instability (AAI).
Cervical Instability can be evaluated with both static and dynamic measurements.
Static measurements included the Grabb-Oakes, Clivo-Axial Angle and Atlantodental Interval (ADI).
Dynamic studies include Digital Motion X-Ray and Upright MRI.
Cervical Spine Instability measurements can identify specific ligament injuries that can targeted during treatment.
Neck pain is not a diagnosis. Patients need an accurate diagnosis. Cervical Spine Instability measurements can help in establishing a diagnosis.
If you or a loved one continues to suffer with ongoing brain fog, headaches and dizziness that has not responded to conservative care please schedule a telemedicine consultation. Learn why the countless MRIs have all been read as “normal”. Stop the suffering now.
——————————-
1.Young RM, Sherman JH, Wind JJ, Litvack Z, O’Brien J. Treatment of craniocervical instability using a posterior-only approach: report of 3 cases. J Neurosurg Spine. 2014 Aug;21(2):239-48. doi: 10.3171/2014.3.SPINE13684. Epub 2014 May 2. PMID: 24785968.
2.Yang SY, Boniello AJ, Poorman CE, Chang AL, Wang S, Passias PG. A review of the diagnosis and treatment of atlantoaxial dislocations. Global Spine J. 2014;4(3):197-210. doi:10.1055/s-0034-1376371
3.Grabb PA1, Mapstone TB, Oakes WJ. Ventral brain stem compression in pediatric and young adult patients with Chiari I malformations. Neurosurgery. 1999 Mar;44(3):520-7; discussion 527-8. https://www.ncbi.nlm.nih.gov/pubmed/10069589.
4. Khanna G, Sato Y. Imaging of the craniovertebral junction. Oper Tech Neurosurg. 2005;8(3):131–142. doi: 10.1053/j.otns.2005.10.004.
5.Henderson FC Sr, Henderson FC Jr, Wilson WA 4th, Mark AS, Koby M. Utility of the clivo-axial angle in assessing brainstem deformity: pilot study and literature review. Neurosurg Rev. 2018;41(1):149–163. doi:10.1007/s10143-017-0830-3.
6. ADI
7.Radcliff KE et al. Does C1 fracture displacement correlate with transverse ligament integrity? Orthop Surg 2013;5(2):94-9. https://www.ncbi.nlm.nih.gov/pubmed/23658043
from Centeno-Schultz Clinic https://centenoschultz.com/understanding-cervical-spine-instability-measurements/
0 notes
Text
Enter an optional heading…
Enter an optional heading…
from Centeno-Schultz Clinic https://centenoschultz.com/75608-2/
0 notes
Text
What Is the Atlantodens Interval? A QuickStart Guide
The headaches and dizziness became progressive in nature and responsive to conservative care. Chiropractic adjustments provided only transient relief as you could not maintain your adjustment. A surgeon reviewed your history, symptoms and radiographic studies. He mentioned different measurements that were abnormal. What is the Atlantodens Interval? What is the Atlas? What is the Axis bone? What is the Atlantoaxial Joint? What stabilizes the Atlantoaxial Joint? What are the unique problems associated with the Atlantoaxial Joint? What is Atlantoaxial Joint Instability? How is the Atlantodens Interval measured? What are the normal Atlantodens Interval measurements? What are the step by step instructions on how to measure the Atlantodens Interval? Let’s dig in.
Introduction
Problems with the head/neck stability can be devastating to both patients and their families. Unfortunately, most clinicians do not understand Craniocervical or Atlantoaxial Instability and often times dismiss patient complaints. Patients are misdiagnosed or labeled are psychologically unbalanced. We are committed to informing patients and providers alike on the importance of their two conditions.
What is the Atlantodens Interval (ADI)
The atlantodens interval is a radiographic measurement that is used in the evaluation of upper cervical spine conditions. It can also be referred to as the atlantodental interval. The atlandodens interval measurement is most commonly used in the evaluation of atlantoaxial instability (AAI).
Relevant Cervical Anatomy
Review of the upper neck anatomy will help with understanding this radiographic measurement and the assoicated clinical conditions. One of the most confusing aspects of cervical anatomy is due to the fact that the uppper neck bones which are numbered also have specific names. Deep breath.
What Is the Atlas? (C1 Bone)
Atlas AKA C1 Bone
The Atlas bone, also known as the C1 is the first bone in your neck (1). It is named after the Greek God Atlas who held up the world on his shoulders. The Atlas plays an important role as your head rests directly on this bone.
What Is the Axis Bone
Axis AKA C2 Bone
The Axis bone is the second bone in the neck and as such it is also referred to as C2 (2). It is an odd-looking bone as it has a boney peg that looks like the Washington Monument. This boney projection is called the Dens. The Dens extends upward to the Atlas bone. It provides a stable point upon which the Atlas bone can rotate.
What Is the Atlantoaxial (AA) Joint?
The AA joint is formed by the union of the C1 and C2 bones. Here is what the AA looks like from different angles.
Atlantoaxial Joint Stability (C1/2)
The stability of the Atlantoaxial joint is dependent upon ligaments and muscles of the upper neck. The Transverse ligament is the key stabilizer. It is a thick band that forms a tight seatbelt across the dens. More specifically it arches across the ring of the C1 bone and holds the Dens in tight contact with the C1 bone. It schematically illustrated in cross section below. The blue circle at the top represents the dens AKA C2 bone. The Transverse ligament snuggly holds the Dens in place much like a seatbelt.
Unique Problems with the Atlantoaxial Joint (C1/2 Joint)
The Atlantoaxial joint plays a very important function in the neck as it provides approximately 50% of rotation for the neck (2). Like all joints in the spine it lined with cartilage and has a joint capsule. What is unique and problematic about the AA joint is the shape of its internal joint surfaces. Most joints fit snuggly together as the joint surfaces fit together like a puzzle. It is the classic ball socket configuration. A common example includes the joint hip where the ball of the Femur fits snuggly into a socket. A convex surface fits snuggly into a concave surface as illustrated below. This configuration is stable.
Unfortunately the AA joint does have one joint surface fitting nicely into the other. Why? Because both surfaces of the joint are convex as illustrated below.
The convex/convex configuration makes for an inherently unstable joint as illustrated below.
Atlantoaxial Instability (AAI)
Atlantoaxial Instability is a medical condition where there is excessive movement betwen the C1 and C2 bone (3). The loss of stability of the AA joint can occur as a result traumatic, inflammatory and cogenital abnormalities (4). Examples of congenital conditions include Down’s syndrome and patients with hypermobility such a Ehlers-Danlos Syndrome. To learn more about the Ehlers-Danlos syndrome and Craniocervical Instability please click here.
How Is the Atlantodens Interval Measured?
The Atlantodens Interval is the distance between the backside of the C1 bone and the front of the C2 bone. It is measured in milimeters (mm). To accurately assess the presence of Atlantoaxial Instability it is important that the radiographic study includes both flexion and extension images. Why? Traditional radiographic studies are static as they have the patient lying still typically lying flat. Instability is best evaluateed during static tests with the patient upright and flexed forward and extended back.
What Are Normal Atlantodens Interval Measurements?
The Atlantodens Interval can be measured on x-rays, CT and MRI scans. The normal ADI for adults is less than 3 mm whereas it is less than 2mm for children.
Step by Step Instructions on How to Measure the Atlantodens Interval
Start with a good quality sagittal CT, x-ray or MRI image of the cervcial spine. AKA sideview
Identify the C2 bone AKA dens
Identify the front of the Atlas AKA C1 bone
4. Identify the backside of the C1 bone and draw a line. Next identify the front aspect of the C2 bone and draw a line.
5. The distance between the backside of the Atlas and the front portion of the C2 is the Atllantodens Interval. It is ilustrated by the double sided arrow. It is measured in mm.
In Summary
The Atlantodens Interval also known as the Atlantodental Interval (ADI) is a radiographic measurement used in the evaluation of upper cervical spine conditions.
The Atlantodens Interval is most commonly used in the evaluation of the Atlantoaxial Instability (AAI).
The Atlas also known as the C1 is bone is the top bone in the neck.
The Axis is the second bone in the neck and is also known as the C2.
The Atlantoaxial joint is the union of the C1 and C2 bone. It’s stability is dependent upon the ligaments and muscles of the upper neck.
The Transverse ligament is a key stabilizer and forms a seatbelt around the C2 bone.
Most joints are classic ball socket configuration. This convex/concave configuration is inherently stable.
The AA joint has a convex/convex configuration and is inherently unstable.
The Atlantodens Interval is the distance between the backside of the C1 bone and the front of the C2 bone. The distance between the two is the ADI and is measured in mm.
At the Centeno-Schultz Clinic we are experts in the managment of upper cervical conditions such as Craniocervical and Atlantocervical Instability. To learn more about Atlantoaxial Instability and Craniocervical instability please download our newest book: CCI 101 by clicking here.
If you or a loved one suffers from persistent headaches, neck pain and brain fog and has not responded to conservative therapy please schedule a New Patient Evaluation. A board certified, fellowship trained physician will compassionately review your history, symptoms and radiographic studies and discuss possible treatment options.
1.Mead LB 2nd, Millhouse PW, Krystal J, Vaccaro AR. C1 fractures: a review of diagnoses, management options, and outcomes. Curr Rev Musculoskelet Med. 2016;9(3):255-262. doi:10.1007/s12178-016-9356-5.
2.Klimo P Jr, Rao G, Brockmeyer D. Congenital anomalies of the cervical spine. Neurosurg Clin N Am. 2007 Jul;18(3):463-78. doi: 10.1016/j.nec.2007.04.005. PMID: 17678749.
3.Yang SY, Boniello AJ, Poorman CE, Chang AL, Wang S, Passias PG. A review of the diagnosis and treatment of atlantoaxial dislocations. Global Spine J. 2014;4(3):197-210. doi:10.1055/s-0034-1376371
4.Subin B, Liu JF, Marshall GJ, Huang HY, Ou JH, Xu GZ. Transoral anterior decompression and fusion of chronic irreducible atlantoaxial dislocation with spinal cord compression. Spine (Phila Pa 1976). 1995 Jun 1;20(11):1233-40. doi: 10.1097/00007632-199506000-00004. PMID: 7660230.
from Centeno-Schultz Clinic https://centenoschultz.com/what-is-the-atlantodens-interval-a-quickstart-guide/
0 notes
Text
Lower Back Pain When Sitting: Symptoms, Causes and Treatment Options
Introduction: Lower Back Pain When Sitting
After a long day on your feet sitting down is supposed to be way to relaxing. Unfortunately for some sitting for any length of time can be painful. Most people experience low back pain at some point in their life. The lifetime prevalence of low back pain is 85% (1). Let’s take a deeper look at the different types of pain and causes of low back pain when sitting.
Where in Your Back Does It Hurt?
The location of low back pain can vary signficantly from patient to patient. It is important to localize the pain. Common areas of low back pain include:
Upper Low Back Pain
This pain is in the upper portion of the back at the junction between the thoracic and lumbar spine.
Low Back Pain
This pain is localized in the low back below the level of the hips.
Midline Low Back Pain
This pain is localized right in the center of the low back.
Unilateral Low Back Pain
Low back pain can be localized exclusively on the right or left side of the back.
Buttock Pain
Some patients that complain of low back pain actually have buttock pain. It can be on either the right or left side or both. It can be superficial or deep.
Iliac Crest Pain
The Iliac Crest is top portion of the Ilium bone. It can also be referred to as the waist bone. You know, when you are scolding someone and put your hand on your waist, that is your iliac crest. The gluteal muscles attach to this bone and when inflammed or injured they can be a significant source of low back pain.
Tailbone Pain
The Sacrum bone is immediately below the Lumbar spine. The Coccyx is immediately below the Sacrum. Both the Sacrum and Coccyx can cause significant low back, and dysfunction.
Types of Lower Back Pain Only When Sitting
Pain can present in many different ways. It can be intermitent or constant. The quality of the low back pain can also vary depending upon the actual source of injury. Common examples include:
Sharp and Stabbing
Dull and Aching
Throbbing/ Pulsating
Pins and Needles
Burning
Electrical
Common Causes of Lower Back Pain When Sitting
Disc Protrusion or Herniation
The Lumbar spine is composed for 5 boney building blocks that are called Vertebral Bodies. Sandwiched between each of the Vertebral Bodies is a Disc. The Disc is an important shock absorber that is composed of a thick outer layer and a gelatinous inner core. The Disc is susceptible to injury and degeneration. Common disc injuries include Disc Protrusions, Disc Herniations and Disc Extrusions.
The outer layer of the Disc known as the Annulus is rich is nerve fibers. Why does this matter? An increase in Disc pressure can stimulate these nerve fibers resulting in signficant pain and dysfunction. Lying down reduces the pressure on the Disc. Conversely sitting increases the pressure on the disc. Lower back pain when sitting can be due to Disc protrusions or Herniations.
Facet Injury
The Facet joint is a paired joint on the backside of the spine. They guide and limit motion of the bones in the low back (2). Like your knee and hip joints, the Facet joints are lined with cartilage which allows the joints to move smoothly. Facet joints are susceptible to injury and degeneration. Facet joint injuries can be caused by trauma, heavy lifting, repetitive movements and car accidents. Lumbar Facet joints are a common source of pain accounting for between 15-45% of low back pain (3).
Ligament Instability
Ligaments are thick pieces of connective tissue that connect bone to bone. They provide important stability for the low back. Important ligaments in the low back include the Supra and Interspinous Ligaments. Ligament laxity due to injury or cogential laxity can cause low back pain when sitting.
Nerve Compression
Nerves exit at each level in the low back. They exit through a boney doorway which is called the Neural Foramen. The doorway may be narrowed by Disc Protrusions, Disc Herniation, Facet overgrowth, Bone Spurs or Ligamental Thickening. This can cause significant irritation and or compression of the exiting nerve resulting in low back pain and Sciatica. Sitting increased the pressure on the Disc which in turn may increase the nerve compression. Often times the result is an increase in low back pain when sitting.
Spinal Stenosis
Stenosis refers to a narrowing. In the Lumbar spine there are two principal types of Stenosis: Central Canal Stenosis and Foraminal stenosis.
Central Canal Stenosis occurs when there is narrowing of the central spinal column causing pressure on the spinal cord. Patients with moderate to advanced Central Canal Spinal Stenosis tend to walk in hunched forward posture. This is often times referred to as a ” shopping cart sign” as patients are bent forward in an attempt to open up the narrowed canal by flexing forward. Patients can also have severe leg pain with walking causing them to stop after several yards due to pain.
Foraminal Stenosis occurs when there is narrowing of the boney doorway through which the spinal nerves exit. This can occur on one side or both sides. Symptoms can include radiating leg pain, numbness, weakness and muscle shrinkage.
Sacroiliac Joint Dysfunction
The Sacroiliac Joint (SIJ is a major joint in the low back. It is composed of the Sacrum and the part of your pelvis called the Ilium. There is an right and left SI joint. Like your knees and hips, the SI joint is lined with cartilage. It is stabilized through an extensive network of ligaments. The SIJ can be injured through both traumatic and nontraumatic causes (4). Traumatic causes of SI joint injury include sudden and repetitive heaving lifting, rear end MVAs and hard falls onto the buttock. Non traumatic causes include Lumbar Fusion, pregnancy due to elevated hormone levels and Scoliosis. SI joint injury and instability is a common cause of unilateral low back pain when sitting.
Annular Tear
The Disc is composed of two principal parts: the Annulus Fibrous and the Nucleus Pulposus. The Nucleus is the gelatinous core that functions as a shock absorber. The Annulus Fibrous are outer fibers that surround and support the gelatious core. The Annulus is a strong radial tire-like structure that provides important stability for the Disc. The Annulus is susceptible in degeneration and injuries. A tear in the Annulus can occur with or without a Disc Protrusion or Herniation (5). The diagnosis of Annular tear is confirmed by MRI. On T2 imaging it is a bright small signal that looks a bright star in the evening sky. Annular tears are a common cause of low back pain when sitting.
Multifidus Muscle Atrophy
The stability of the Lumbar spine is dependent upon ligaments and muscles. The Multifidus is a small muscle that your doctor never talked to you. It is a critical to the stability of the Lumbar spine. Injury and weakness in the Multifidus can cause low back pain when sitting. To learn more please click on the video below.
youtube
Muscle Tightness
There a large number of muscles in the low back. They provide stability and allow us to rotate, bend forwards and backwards. They also have a protective role in that if there is an injury to the Lumbar Disc, Facet or tendon the muscles tighten. Persistent muscle tightness that does not respond to conservative treatment is a warning signal that you may have a low back injury. It warrants a deeper evaluation.
Spondylolisthesis
Spondylolisthesis is where one of the bones in the spine slips out of alignment. It can slip forward or backwards in relation to the other bones. This can cause injury to the Lumbar Discs, nerves and exiting nerves. Patients with Spondylolisthesis are unstable and can have lower back pain when sitting, bending or lifting.
Other Medical Conditions that Can Cause Lower Back Pain
Not all low back pain is due to injury of structures in the low back. Other important causes of low back pain include:
Kidney Stones
A Kidney Stone is a hard mass made from the chemicals in the urine. There are four types of Kidney Stones: Calcium Oxalate, Uric Acid, Struvite and Cystine. They can be small or large. They can localized irritation or block the flow or urine. Symptoms include severe one sided low back pain. Other symptoms include blood in the urine, fever and chills.
Gallbladder Disease
The Gallbladder is a part of your digestive system. Its main function is to store bile which helps break down fats. Inflammation of the Gallbladder or hardened deposits of bile called gallstones can cause Gallbladder disease and dysfunction. Symptoms include abdomen pain, fever, chills and low back pain. m
How You Can Prevent Lower Back Pain When You Sit (Overview)
The best way to avoid low back pain when sitting is to be proactive. Common strategies include:
Keep Moving
Movement is the best way to ward off back pain. Regular physical activity can make the back stronger to reduce future episodes of pain. Exercises should focus on increasing strength and improving range of motion.
Get Up from your Chair
Avoid prolonged sitting. If you sit at a desk in the office or at home all day, get up every 30 minutes and walk around. Consider a standing desk.
Posture
Optimize posture with neutral spinal alignment. Slouching compromises neutral spinal aligment and puts the Lumbar Discs, facets, ligaments and muscles at risk for injury and dysfunction.
Regular Exercise
Exercise has tremendous benefits both psychological and physical. Muscle mass and strength declines with age. Specifically, muscle mass decreases 3-8% per decade after the age of 30 and increases after the age of 60. Muscle strength is important for mobility and low back stability. Remember the adage: “Use it or lose it”
Stretching
Stretching has many important health benefits. Stretching can improve flexibility, range of motion, and posture which in turn can improve low back health and vitality.
Home Treatments to Ease Lower Back Pain
Mild low back pain after a long day or athletic event is not uncommon. When possible, it is best to resume normal or near normal activity as soon as possible. Conservative home treatment options include:
Intermittent Heat or Ice
Stretching
Gentle Massage
Safe oral anti-inflammatory medications such as fish oil and Turmeric. NSAIDs such as Motrin or Aleve have significant side effects and should be avoided. To learn more please click here.
Sleep with a pillow under your knees or on your side
When to Call Your Doctor
Pain tolerance can vary significantly from patient to patient. Low back pain that is tolerable for one patient may drive another one to the emergency room. You should consider seeing your doctor if you have:
Low back pain is persistent and not responsive to conservative care
Persistent leg numbness and tingling
Fever and chills
Loss of bowel or bladder function
How Important Is Getting A Solid Diagnosis?
Back pain is not a diagnosis. It is a symptom. For the very best clinical results it is critical that an accurate diagnosis is made. Specifically based upon medical history, physical examination and radiographic tests what structure or structures are causing your ongoing pain. This is the standard of care at the Centeno-Schultz Clinic.
Some pain clinics operate on the theory that a patient’s pain is arising from a single source. Many refer to this as identifying the “pain generator”. Accordingly, they will inject a specific part of the spine with diagnostic injections. For example, they may start with Lumbar Facet injections asking the question is the pain arising from the Facet Joints. If Facet Injections fail to provide benefit they move on and perform diagnostic Epidural injections. The problem with this model is that body is complex with many different, truly remarkable structures that all work in concert with one another.
At the Centeno-Schultz Clinic we understand the importance of viewing the body as a whole. We view the spine as a functional spinal unit (FSU). The Functional Spine Unit is composed of Discs, Facet Joints, bones, ligaments, tendons, and muscles. To learn more about what all these parts do, please click on the video as it will bring this whole topic together.
youtube
Treatment Options
At the Centeno-Schultz Clinic we bring a standard of care and expertise that is truly unique. We were the first clinic in the world to inject Bone Marrow Concentrate into the Lumbar Disc in 2005. Treatment of common orthopedic conditions with PRP and Bone Marrow Concentrate is our singular focus. We do not inject Botox, burn nerves using Radiofrequency, use high dose steroids or manage chronic narcotics. We are committed to highest standard of care which includes:
Establishing the correct diagnosis
Using ultrasound or x-ray guidance on all injections
Treating the spine as a Functional Unit (FSU))
Determining the most appropriate treatment option: Platelet Rich Plasma or Bone Marrow Concentrate or both.
Determining the appropriate PRP dose given the injury and your age. To learn more please click here.
Determining the type of Bone Marrow Concentrate: same day procedure or culture expanded ( Regenexx- SD or Regenexx-C)*
Identifying the appropriate rehabilitation to ensure best clinical outcome.
The Centeno-Schultz Clinic are experts in the evaluation and treatment of low back pain when sitting. Our goal is to avoid patient’s reliance on potentially addicting narcotics or life altering surgeries. To learn more about the complications associated with low back fusions please click here.
In Summary
Low back pain is common and most likley with affect you at some point in your life.
The location of low back pain varies but is important to localize if possible.
The quality of low back pain also varies. Common examples include sharp, stabbing, dull, aching and burning.
Common causes of low back pain when sitting are disc protrusion, facet injury, ligament instability, nerve compression, spinal stenosis, annular tear and sacroiliac joint dysfunction.
Other important causes of low back that need to considered are kidney stones and gallbladder disease.
Strategies to prevention low back pain when sitting include limited sitting, improved posture, regular exercise and stretching.
It is time to contact a doctor when your low back is persistent despite conservative care, persistent numbness and tingling, fever and chills or loss of bowel or bladder function.
Low back pain is not a diagnosis but rather is a symptom. Getting an accurate diagnosis is critical if you want the very best clinical outcomes.
At the Centeno-Schultz Clinic treatment options for low back pain when sitting may include x-ray or ultrasound guided injections of PRP or bone marrow concentrate.
If you or a loved one has low back pain when sitting that has not been responsive to conservative care, please schedule a telephone Candidacy discussion with a board-certified, fellowship-trained physician. From the comfort of your home or office, learn what treatment options are available for you. Call today and stop the pain, misery, and suffering.
*Regenexx-C is only avialble at a licensed site in the Cayman Islands.
1.Kiapour A, Joukar A, Elgafy H, Erbulut DU, Agarwal AK, Goel VK. Biomechanics of the Sacroiliac Joint: Anatomy, Function, Biomechanics, Sexual Dimorphism, and Causes of Pain. Int J Spine Surg. 2020 Feb 10;14(Suppl 1):3-13. doi: 10.14444/6077. PMID: 32123652; PMCID: PMC7041664.
2.Jaumard NV, Welch WC, Winkelstein BA. Spinal facet joint biomechanics and mechanotransduction in normal, injury and degenerative conditions. J Biomech Eng. 2011;133(7):071010. doi:10.1115/1.4004493
3.Perolat R, Kastler A, Nicot B, et al. Facet joint syndrome: from diagnosis to interventional management. Insights Imaging. 2018;9(5):773-789. doi:10.1007/s13244-018-0638-x
4.Chuang CW, Hung SK, Pan PT, Kao MC. Diagnosis and interventional pain management options for sacroiliac joint pain. Ci Ji Yi Xue Za Zhi. 2019 Sep 16;31(4):207-210. doi: 10.4103/tcmj.tcmj_54_19. PMID: 31867247; PMCID: PMC6905244.
5.Farshad-Amacker NA, Hughes AP, Aichmair A, Herzog RJ, Farshad M. Is an annular tear a predictor for accelerated disc degeneration? Eur Spine J. 2014 Sep;23(9):1825-9. doi: 10.1007/s00586-014-3260-8. Epub 2014 Mar 13. PMID: 24622958.
6.Volpi E, Nazemi R, Fujita S. Muscle tissue changes with aging. Curr Opin Clin Nutr Metab Care. 2004;7(4):405-410. doi:10.1097/01.mco.0000134362.76653.b2
from Centeno-Schultz Clinic https://centenoschultz.com/lower-back-pain-when-sitting-symptoms-causes-and-treatment-options/
0 notes
Text
6 Meniscus Tear Types – What They Are And How To Treat Them Properly
Even a small meniscus tear can make walking difficult for you. If you are experiencing any of these symptoms, you may want to seek medical help as soon as possible, depending on the type of tear you have. Needless to say, a lot depends on understanding the meniscus tear types there are and what each might mean for treatment options.
The meniscus is a fibrocartilage structure that sits on top of the tibia (lower leg bone). There is one on the medial (inside) aspect of the knee, one on the lateral (outside) aspect of the knee. It is shaped like a C and provides some cushion and support for the knee joint as it acts as a shock absorber.
A meniscus can be torn with a particular injury typically with sports, twisting, deep knee bending, rotating, or high-intensity type activities. Also, it can just gradually tear or wear out through degeneration throughout the years as we age.
Those degenerative tears can be found on most MRIs but are generally not of clinical relevance (1). There are 6 main types of meniscal tears: horizontal (longitudinal), radial (transverse), intrasubstance, bucket-handle, flap tear, and complex tear. For more information on the meniscus and knee problems read The Knee Owner’s Manual.
6 Meniscus Tear Types That You Need To Know About:
Types of Meniscus Tears
1. Horizontal tear (Longitudinal)
This is an up and down or front to back a tear in the meniscus. Many times these tears are in a portion of the meniscus that does get blood supply (red zone) so could potentially heal on their own. Physical therapy is a first-line treatment that often works. If they do not heal naturally or with physical therapy, then arthroscopic surgical repair can sometimes be tried to help. A surgical meniscectomy should NOT be done for these types of tears as they can make the knee worse. PRP (platelet-rich plasma) or bone marrow concentrate (BMAC) containing stem cells can heal these tears as an alternative to surgery. These are more natural, safer, and have easier recovery than surgery so these should be done prior to considering surgery in most cases. They can also be used in conjunction with surgery to improve surgical results.
2. Radial tear (transverse)
This is a left-to-right tear across the meniscus. These are the most common types of tears. Most commonly they are in what we call the white zone of the meniscus where it does not get much blood supply. Thus, they are hard to heal naturally. PT should still be the first line treatment but these may benefit more from PRP or bone marrow concentrate (BMAC). If you see a surgeon, they will likely try to cut this part out (meniscectomy) despite the evidence saying that a meniscectomy does not work and can make the knee worse, so this rarely should be done for these types of tears.
3. Intrasubstance tear (incomplete)
Usually, these are degenerative tears in the midportion of the meniscus. After age 30, these are very common findings of a meniscal tear on MRI, which is of little consequence. Physical therapy is the first-line treatment. Typically, if you have pain, it will be from other knee issues such as arthritis. For mild to moderate arthritis, PRP has excellent evidence it can help. If the arthritis is more moderate to severe then BMAC will be a better treatment option. Most surgeons will not even try to operate on these as surgery doesn’t help and meniscectomy can make the knee worse.
4. Bucket-handle tear
This is a tear where the meniscus is torn and flipped over like a bucket handle. These sometimes can cause some catching or alter the motion of the knee. If that is the case then those would be the rare type of tear that actually would need surgery if that is the case. Typically, a meniscectomy is done as these may not respond to repair. If this type of tear doesn’t have the mechanical symptoms or knee catching/locking, then it possibly can be helped with physical therapy, PRP, or BMAC.
5. Flap tear
This is where a small piece of the meniscus can be torn and flipped over. Sometimes this can cause some catching of the knee, sometimes it does not hurt. If there is no catching in the knee, then it would not warrant any surgery to remove that part of the meniscus. Physical therapy would be a first-line treatment, with PRP or BMAC being an option. If it is causing some catching or altering motion of the knee that might be another rare case where surgery is indicated for partial meniscectomy as these are difficult to repair.
6. Complex tear
The last of the types of meniscus tears is the complex tear, where you have a combination of different tears where it can be torn in multiple areas of the knee. Oftentimes when the surgeon sees these, they would attempt a meniscectomy again because most of the time these are difficult for them to try to repair.
Tear locations
On MRI and or with some degree with ultrasound, you can determine where the meniscus is torn. This is important to know for treatment and to determine if the tear matches with a patient’s pain.
Anterior horn: front part of the meniscus
Body: mid portion of the meniscus
Posterior horn: back part of the meniscus
Root: front or back deeper part wear the meniscus attaches to the tibia
Risk Factors for a Torn Meniscus
The meniscus can be torn with sports, high-intensity exercise, trauma. Risks would be being overweight, low physical activity levels, or doing too high of intense exercise without being in proper shape, or having incorrect form/biomechanics. Typically, movements like knee twisting, deep knee bending, rotating the knee can predispose to injury.
Natural Remedies For a Torn Meniscus
If you have knee pain and have been told you have a suspected meniscal tear either from an exam or from MRI, much of the time, this can heal on its own with 4-6 weeks of rest, doing some physical therapy that would focus on some range of motion and strengthening exercises and correcting maybe any biomechanical problems that may stem from the core, back, hips or the ankles. Nutritional support such as just working on a healthy diet, reducing inflammation in the body, taking some turmeric, fish oil, glucosamine, and chondroitin, can help knee pain and inflammation as well.
Revolutionary Treatments For A Meniscal Tear Without Surgery
If you go to most pain practices if you fail physical therapy and surgery is not yet recommended, they may recommend a steroid injection, which can help temporarily reduce inflammation in and around the knee and meniscus, but this is not advised as steroids as we know can cause damage to the joint cartilage, inhibit healing, and has a host of other negative side effects.
An injection of something called hyaluronic acid, which is a part of some of the lubricating fluid of the knee joint could be used for temporary pain relief. It does not help repair the area but may provide a few months of symptomatic benefit if there is not severe arthritis in the knee.
Meniscal surgery actually doesn’t have any evidence that it help meniscal tears and does have clear evidence that it can progress arthritis faster (2-8).
If you actually want to try and get the body heal that meniscus on its own where rest and physical therapy did not do the job, PRP has excellent evidence that helps with meniscal injuries as well as mild to moderate arthritis that can be associated with these. PRP when used in the right hands, should be injected precisely with ultrasound guidance into the torn parts of the meniscus, into any ligaments or tendons that may be injured or loose and into the knee joint itself for optimal results. Many practitioners just inject into the knee, which still can help quite a bit but not as much than if a more thorough approach is taken. There are more than 25 high level studies showing PRP helps with knee pain (Orthopedic Bone Marrow Stem Cell Historical Timeline (netdna-ssl.com)).
Bone marrow concentrate that contains stem cells within it can also be used for more severe meniscal tears or if there are meniscal tears with more moderate to severe arthritis. There are a few randomized control trials that show that this can be helpful for that as well (9-11). Again, you want to have a thorough skilled approach to make sure that image guidance is used, and all of the damage parts of the meniscus and associated areas of the knee such as tendons, ligaments, and joints are injected as well.
The latter two options are what we focus on at the Centeno-Schultz Clinic, promoting the body’s natural ability to heal itself with PRP and bone marrow concentrate has been shown to be very successful, has little risk, maintains the natural anatomy and structure of the joint, and has more evidence that is positive compared to meniscal surgeries, which evidence shows that we pretty much should not do the surgery except for the rare cases of types of meniscus tears with mechanical symptoms, such as flap or bucket-handle tears.
Keeping Your Meniscus Healthy
Knee your knee and meniscus healthy but eat healthily (see Nutrition 2.0), consider supplements such as glucosamine and chondroitin that can be good for arthritis or our stem cell support supplement), reduce excess inflammation by eating healthy, keeping a normal weight, exercising, and maybe taking a supplement such as turmeric. Keep the knee strong with some daily physical activity like elliptical, biking, walking, and some resistance/strength training 2x/week. For exercise make sure you warm up before and cool down after, have good technique, and stay within your functional limits. Physical therapists, Egoscue therapy, foundations training, muscle activation therapy (MAT), trainers, and other types of body therapists can help with form, posture, biomechanics, and treat minor problems to reduce the risk of injury.
Bottom Line
Meniscal tears are common findings in the knee, which many times are of little clinical significance. What matters is the type of meniscus tear.
If a tear is associated with pain, depending on the tear, most of these can be handled with nonsurgical treatment measures. When the traditional measures of rest, physical therapy, diet, and supplements fail, then PRP and bone marrow concentrate for more severe problems can be a great alternative to promote your body’s natural ability to heal, reducing pain, keeping the natural anatomy, and reducing the risk for future surgeries. Meniscal surgery, despite being the most common orthopedic surgery has little evidence to support it and actually good evidence to suggest that we should eliminate the majority of these types of surgeries. If you or anyone you know has a meniscal tear or knee pain and is interested to see if you are a candidate for treatment, please contact us. We are experts at boosting your body’s natural healing ability through precise image guided regenerative interventional orthopedic procedures.
References
(1) Risberg MA. Degenerative meniscus tears should be looked upon as wrinkles with age—and should be treated accordingly. British Journal of Sports Medicine 2014;48:741. http://dx.doi.org/10.1136/bjsports-2014-093568
(2) Katz JN, Brophy RH, Chaisson CE, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis [published correction appears in N Engl J Med. 2013 Aug 15;369(7):683]. N Engl J Med. 2013;368(18):1675–1684. doi:10.1056/NEJMoa1301408
(3) Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, Nurmi H, Kalske J, Järvinen TL; Finnish Degenerative Meniscal Lesion Study (FIDELITY) Group. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013 Dec 26;369(26):2515-24. doi: 10.1056/NEJMoa1305189.
(4) Sihvonen R, Englund M, Turkiewicz A, Järvinen TL; Finnish Degenerative Meniscal Lesion Study Group. Mechanical Symptoms and Arthroscopic Partial Meniscectomy in Patients With Degenerative Meniscus Tear: A Secondary Analysis of a Randomized Trial. Ann Intern Med. 2016 Apr 5;164(7):449-55. doi: 10.7326/M15-0899.
(5) Netravali NA, Giori NJ, Andriacchi TP. Partial medial meniscectomy and rotational differences at the knee during walking. J Biomech. 2010 Nov 16;43(15):2948-53. doi: 10.1016/j.jbiomech.2010.07.013.
(6) Cohen SB, Short CP, O’Hagan T, Wu HT, Morrison WB, Zoga AC. The effect of meniscal tears on cartilage loss of the knee: findings on serial MRIs. Phys Sportsmed. 2012 Sep;40(3):66-76. doi: 10.3810/psm.2012.09.1983.
(7) Longo UG, Ciuffreda M, Candela V, Rizzello G, D’Andrea V, Mannering N, Berton A, Salvatore G, Denaro V. Knee Osteoarthritis after Arthroscopic Partial Meniscectomy: Prevalence and Progression of Radiographic Changes after 5 to 12 Years Compared with Contralateral Knee. J Knee Surg. 2019 May;32(5):407-413. doi: 10.1055/s-0038-1646926.
(8) Katz JN, Shrestha S, Losina E, Jones MH, Marx RG, Mandl LA, Levy BA, MacFarlane LA, Spindler KP, Silva GS; MeTeOR Investigators, Collins JE. Five-year outcome of operative and non-operative management of meniscal tear in persons greater than 45 years old. Arthritis Rheumatol. 2019 Aug 20. doi: 10.1002/art.41082.
(9) Centeno C, Sheinkop M, Dodson E, Stemper I, Williams C, Hyzy M, Ichim T, Freeman M. A specific protocol of autologous bone marrow concentrate and platelet products versus exercise therapy for symptomatic knee osteoarthritis: a randomized controlled trial with 2 year follow-up. J Transl Med. 2018 Dec 13;16(1):355. doi: 10.1186/s12967-018-1736-8. PMID: 30545387; PMCID: PMC6293635.
(10) Hernigou P, Bouthors C, Bastard C, Flouzat Lachaniette CH, Rouard H, Dubory A. Subchondral bone or intra-articular injection of bone marrow concentrate mesenchymal stem cells in bilateral knee osteoarthritis: what better postpone knee arthroplasty at fifteen years? A randomized study. Int Orthop. 2020 Jul 2. doi: 10.1007/s00264-020-04687-7. Epub ahead of print. PMID: 32617651.
(11) Hernigou P, Delambre J, Quiennec S, Poignard A. Human bone marrow mesenchymal stem cell injection in subchondral lesions of knee osteoarthritis: a prospective randomized study versus contralateral arthroplasty at a mean fifteen year follow-up. Int Orthop. 2020 Apr 23. doi: 10.1007/s00264-020-04571-4. Epub ahead of print. PMID: 32322943.
from Centeno-Schultz Clinic https://centenoschultz.com/meniscus-tear-types/
0 notes
Text
Differences Between A Normal vs Abnormal Cervical Spine MRI
The neck pain was unrelenting and unresponsive to conservative care. Simple tasks and motions were impossible. At times there were sharp, shooting pains radiating down your arm with accompanying numbness and tingling. Your doctor ordered a Cervical MRI and you are awaiting the results. What is a Cervical MRI? How does an MRI work? Does MRI imaging use x-ray? What are the differenes between a normal vs abnormal Cervical Spine MRI? What are the advantages of MRI based diagnoses? What are the shortcomings of traditional MRI imaging? When should you get a Cervial Spine MRI? What does a normal Cervical Spine MRI look like? What are the most common abnormal findings? What are the consequences of misinterpreting a Cervical Spine MRI? What alternative exists? Lets dig in.
A Deeper Look into A Normal vs Abnormal Cervical Spine MRI
The internet has made medical information widely available. Many of our patients spend hours researching the results of their Cervical Spine MRIs. Self diagnosis is very common. Google is free whereas a medical education is many long years and hundreds of thousands of dollars. Reading your MRI report summary and researching the findings is not enough. There are important differences between a normal vs abnormal Cervical MRI which which will be discussed below.
What Is a Cervical Spine MRI?
MRI stands for Magnetic Resonance Imaging.
A Cervical MRI scan provides highly detailed pictures of your neck from different angles (1). The pictures are referred to as images and are numbered based upon the number of pictures taken. The different views include:
Axial: This is a cross section image. It divides the body into top and bottom halves. Image cutting the body in half with a top and bottom portion.
Coronal: This is a frontal view. it is a vertical plane that divides the body into front and back. I imagine a crown slicing downward creating a front and back.
Sagitial: This is a side view. Sagitial images start on the right side of the Cervical Spine and move to the left.
These different views allow physicians to accurately identify any and all abnormalities in your Cervical Spine MRI.
How Does an MRI Work?
MRI is an non-invasive technology that uses a powerful magnetic field and radio waves to produce detailed, 3-D pictures of your body (2). Our bodies contains millions of hydrogen atoms. Powerful magnets produce a strong magnetic field that forces the atoms in our body to align with that field. They all line up in the same direction. The radio waves the MRI produce disrupt this alignment. The radio waves are pulsed: turned on and then off. When they are turned off the MRI sensors are able to detect the energy released as the atoms realign with the magnetic field. This creates detailed images of our bodies.
An MRI scan uses a powerful magnetic field and radio waves to take detailed, 3-D pictures of your body.
Does a MRI Imaging Use x-ray?
No!
Advantages of MRI Based Diagnoses
MRI is a very powerful imaging modality that is being used with increased frequency. There are many advantages of being diagnosed with an MRI which include:
Detailed pictures of bones, cartilage, muscles, tendon and nerves. This is not possible with x-ray which only evaluates bone.
No radiation
Better resolution of soft tissues such as muscle, tendons and fat than CT scan
Detailed images from different views that allow better localization of a given structure. If you are evaluating a disc herniation for example you need to know exactly where it is, whether it is right or left sided and whether it irritates or compresses the exiting nerve root. An MRI can provide this specific information.
Shortcomings of Traditional MRI Based Diagnoses
Diagnosis Made in Isolation
Radiologists review MRI imaging and provide a formal report often times without any consideration of the patient’s medical history, limitations and current symptoms. Rarely are they aware of a patient’s entire medical history and findings on physical examination. Hence the diagnosis is made in isolation. Radiologists are obligated to report everything that they see. Hence the MRI report may mention different finding and abnormalities. Unfortunately all, some or none of the findings may explain a given patient’s symptoms.
Static vs Dynamic Studies
Traditional Cervical spine MRIs are performed with the patient lying still on their back. Movement in these type of MRI scans can compromise the quality of the images. These are known as static tests. Unfortunately these static tests can not evaluate the instability of the spine or the forces of gravity. Newer MRI technology now allows for patient to be upright as opposed to being flat. It also allows pateints to flex forward or extend backwards evaluating the presence or absence of instability. This is critical information that previously has not be available with static MRI imaging.
When Should You Get a Cervical Spine MRI? (Neck Pain)
There are many reasons why your doctor may order an MRI. The most common indication is severe neck pain or radiating arm pain that has not responded to physical therapy, rest, medications, chiropractic care.
Other reasons for a cervical spine MRI include
Trauma to the neck
Infection
Scoliosis (Curvature)
Headaches
Tingling and weakness in the arm
Birth defects of the spine
What Does a Normal Cervical MRI Look Like?
The Cervical Spine is composed of many different parts. Each is important and works in concert with all the other parts. The major parts of the Cervical Spine include:
Cervical Bones and Discs
The neck is composed of 7 boney building blocks that are called Vrtebral bodies. They are numbered from top to bottom starting with C1. The C denotes that we are discussing the cervical spine. Sandwiched between each of the bones is a a cushion also known as a Disc. The Disc is critical to the integrity and proper functioning of the neck as it absorbs the daily forces of living.
Cervical Facet Joints
A Facet Joint is a paired joint that resides in the back of the neck. They are cartilage lined joints that provide stability and limit range of motion. There is a right and left facet joint at each Cervical level. They are identified by the two vertebral bodies that they span. For example, the C5/6 facet joint is composed of the bones from both the C5 and C6 neck bones.
Central Canal
The Central Canal is a space that runs the entire length of the spine. It contains the spinal cord and spinal fluid. Narrowing of the Canal called stenosis and is graded based upon the severity of the narrowing. Central Canal Stenosis can cause several symptoms including neck pain, numbness of tingling in the arms and hands and problems with balance.
Neural Foramen
The Neural Foramen are the body’s doorways through which the spinal nerve roots exit the spinal column. There is a Neural Foramen at each level of the spine. There is also a right and left Neural Foramen. Narrowing of this boney doorway is called Neural Foramen Stenosis. This can cause irritation or pressure on the exiting nerve resulting in shooting pain down the arm, weakness and numbness.
Muscles
There is a large number of both large and small muscles in the neck. They play a critical role in the stability and mobility of the spine. Muscles can be injured, torn and atrophied (shrunken) and filled with adipose. This is especially important for the multifidus muscle which is a principal stabilizer in the spine. A previous blog discusses the importance of this small muscle in greater detail.
Tendons
Tendons are thick pieces of connective tissue that connect muscle to bone. Tendons are susceptible to inflammation, degeneration, partial thickness, and full thickness tears all of which can be visualized on a cervical spine MRI.
Common Abnormal Findings in Cervical Spine MRIs
The most common abnormal findings that you may come across in your Cervical Spine MRI report includes:
Cervical Spondylosis
This is a very broad term that is used to describe degenerative arthritis in the Cervical Spine. It is very common and typically gets worse with age.
Disc Injuries
The Disc is a gelatinous shock absorber that is sandwiched between each cervical vertebral bone. It absorbs the daily forces of life. It is susceptible to a number of different injuries which include Disc Protrusion, Herniation, and Extrusion.
Bone Spurs
A Bone Spur is a boney growth that develops on the edge of a bone. They can be small or large, smooth or irregular. They are typically the result of micro-instability. A Bone Spur is an attempt by your body to create stability. Bone Spurs in the cervical spine can compress nerves and narrow both the Neural Foramen and Central Canal creating Stenosis.
Facet Injuries
A Facet Joint is a paired joint that resides in the back of the neck. The joint is susceptible in injury and degeneration resulting in pain and restriction in range of motion. Trauma is the most common cause of injury.
Subluxation
The Cervical bones stack one upon another creating the Cervical Spine. The are all in alignment much like the drawers in your kitchen cabinets. Alignment allows for optimal performance and function. Unfortunately, trauma and wear and tear can compromise this alignment. Specifically, one vertebral bone can slip forward in relation to the other. This is called Anterolisthesis. “Listhesis” means slippage. Anterior means forward. A vertebral body can also slip backwards in relation to the other bones. This is called Retrolisthesis. Anterolisthesis and Retrolisthesis are both forms of Subluxation and can cause significant pain and dysfunction.
Central Canal Stenosis
The central canal is a space that runs the entire length of the spine. It contains the spinal cord and spinal fluid. Narrowing of the Canal space is called Stenosis and is graded depending on its severity. There are multiple causes of Central Canal Stenosis which include Disc Protrusions, Disc Herniations, Subluxations, Facet overgrowth and ligament thickening.
Foraminal Stenosis
Nerves exit the spinal cord through a boney doorway called the Neural Foramen. Foramen means opening or doorway. Stenosis means narrowing. Foraminal Stenosis is narrowing of the boney doorway through which the spinal nerves exit. When this occurs, the nerve can be irritated or compressed resulting is pain, numbness, tingling and weakness.
Consequences of Misinterpreting a Cervical Spine MRI
Most Cervical Spine MRIs are reviewed in isolation without access to a patient’s full medical history or findings on physical examination. Cervical Spine MRI reports vary in depth and detail. Not all physicians are looking with the same discerning eye. Because there are important differences between a normal vs abnormal Cervical Spine MRI at the Centeno-Schultz Clinic we personally review all MRIs and often times identify important finding that are not reported upon. We examine in detail the muscles, tendons and stability of the spine that is rarely discussed in formal reports. Why? Because it makes a difference in patients and their families lives. We are committed to making the correct diagnosis so that the correct treatment plan can implemented. Only then can optimal outcomes occur.
An Alternative to Traditional Cervical Spine MRIs
As discussed above traditional MRIs are performed with the patient lying still on their backs. This type of imaging cannot thoroughly evaluate the stability of the Spine or the impact of gravity on the Spine. Alternatives to traditional MRI imaging include:
Upright MRI
An upright MRI is performed with the patient standing or sitting and better evaluates the stability of the neck. It utilizes a front open design allowing patients to undergo scans in various positions. For example, patients can be bent forward or extended backward to determine if Cervical instability is present.
Digital Motion X-ray
Digital motion x-ray is a powerful tool utilized in the evaluation of the patients suspected of having Cranio-Cervical Instability. Under continuous x-ray, patients are put through various maneuvers that included flexion, extension, and side bending. To learn more please click on video below.
youtube
MRIs Do Not Represent the Entire Clinical Picture
In Conclusion
MRI stands for Magnetic Resonance Imaging
MRI imaging provides detailed pictures of the body from different views: axial, coronal and sagitial
MRI imaging uses a powerful magnetic field and radio waves.
NO radiation is used with MRI imaging
Advantages of MRI based diagnoses included detailed pictures of bone, cartilage, muscles, tendons and nerves
Traditional MRI based diagnoses are made in isolation without the entire clinical picture.
Indications for a Cervical MRI include neck pain, radiating arm pain unresponsive to conservative care.
Normal Cervical Spine MRI includes evaluation of the Cervical Discs, Facet joints, Central Canal, Neural Foramen, muscles and tendons
Abnormal Cervical Spine MRI may include Disc injuries, Degenerative Arthritis, Facet injuries, Subluxation, Central and Foraminal Stenosis.
Upright MRI and DMX are alternative imaging options that provide important clinical information.
There are important differences between a normal vs abnormal Cervical Spine MRI. These include the architecture and overall health of the Cervical Discs, Vertebrae, Facet Joints, muscles, nerves and ligaments.
At the Centeno-Schultz Clinic we understand the differences between a normal vs abnormal Cervical Spine MRI. These differences along with findings on physical examination and medical history are utilized to determine the best regenerative treatment plan. Stop spending hours researching the meaning of each medical term on your MRI formal report. Get a clearer picture of your Cervical Spine condition by booking an appointment with us today
1.Grover VP, Tognarelli JM, Crossey MM, Cox IJ, Taylor-Robinson SD, McPhail MJ. Magnetic Resonance Imaging: Principles and Techniques: Lessons for Clinicians. J Clin Exp Hepatol. 2015;5(3):246-255. doi:10.1016/j.jceh.2015.08.001
2.Berger A. Magnetic resonance imaging. BMJ. 2002;324(7328):35. doi:10.1136/bmj.324.7328.35
from Centeno-Schultz Clinic https://centenoschultz.com/differences-between-a-normal-vs-abnormal-cervical-spine-mri/
0 notes
Text
Stiff Neck: Causes, Related Conditions, Remedies, & Treatment
A stiff neck happens when muscles of the neck are strained or tense. It can sometimes be remedied at home, but when that fails, medical treatments are also available.
Stiff Neck
Conventional wisdom states that stiff neck symptoms can be treatable with nonsurgical remedies. However, not all stiff neck symptoms are benign, and leaving the stiff neck untreated can lead to a limited range of motion that can affect your overall health and quality of life. A stiff neck can cause pain, tightness, popping, and clicking noises and sensations and affect daily activities. A detailed examination of stiff neck symptoms can determine the exact condition affecting the stiffness of one’s neck.
Where Does the Neck Hurt?
Neck stiffness can occur at the base of the head, down to the shoulders. This can be associated with pain, crunching noises or popping sensations and may have some sharp pain associated with it.
Neck stiffness can cause pain extending down into the arms and may be associated with numbness, tingling or some weakness.
There can just be some focal localized points of pain anywhere along the neck column, back of the neck muscles, upper, lower and middle trap muscles between the shoulder blades or in the scalene muscles
Types of Neck Pain
Neck pain can be described as soreness or an aching sensation.
Someone can have spasms or sudden powerful tightening or twitching of the neck muscles.
You can develop dull headache-type pain or pain that radiates up around the base of the skull to the top of the head and sometimes to the front of the head.
May be a deep, sharp or stabbing sensation.
Severe pain with tingling sensations that may or may not radiate into the shoulders or down the arms or to the fingers.
Painful muscles and neck areas that are tender to the touch.
Common Causes Of Neck Pain
A thorough musculoskeletal physician will take symptoms, history of neck pain, stiffness, and associated symptoms and put them together to have a differential diagnosis to determine the exact cause of neck pain.
Poor Posture and Ergonomics
With the overuse of cell phones, tablets, and computers, there is an epidemic of poor posture and spinal misalignment. Posture is key to keeping healthy muscles, bones and joints, and discs for the spine. Prolonged looking down at digital devices can compromise muscles and normal spinal curves that can lead to problems. Also, poor ergonomic positions for certain occupations or activities where you are in a prolonged, awkward position can lead to wear and tear as well.
Teeth Grinding
Teeth grinding can be both a cause of neck pain and stiffness and a result of neck pain and stiffness. If one grinds one’s teeth, the facial muscles work harder and can tighten which can pull on the neck, causing head and neck and shoulder problems, Also, upper neck instability or misalignment can cause compensation of the jaw muscles that will lead to nerve irritation and teeth grinding.
Arthritis
Symptoms of arthritis include painful joints that can radiate pain in the upper, middle, or lower neck between the shoulder blades and upper neck areas. Arthritis develops with continued instability, poor posture, poor alignment, and wear and tear. The cartilage in the joints can become inflamed causing pain and stiffness and causing the joint to enlarge.
Cervical Disc Injury
The neck is composed of 7 building blocks called vertebral bodies and the surface between those building blocks are discs. The discs serve as important shock absorbers of the neck but these can be injured with continued wear and tear, poor posture, poor alignment and trauma. Injury to the disc can lead to pain directly in the disc that can radiate into the neck in between the shoulder blades or it can cause disk bulging, which can irritate the nearby nerves causing numbness, tingling, weakness down the shoulder and arm.
Cervical Nerve Injury
At each level of the neck, nerves exit the spine. They control movements of the neck, shoulders, arms, and fingers. Disc bulges and arthritis cause joints to increase in size. Ligament laxity, bulging facets getting enlarged or hypertrophied, disc bulges, etc. can cause less space around the nerves, which is referred to in medical terms as Stenosis.
Spinal Injuries
Spinal cord injuries can be serious and usually result from accidents, but trauma can come up insidiously like in the form of severe stenosis or less space around the nerves or a collection of fluid around the nerves, such as a syrinx. Typically, these result in severe significant weakness in the arms, even possibly the legs. If really severe, this can cause bowel or bladder issues, trouble breathing, or extreme pain. Additionally, other spinal injuries would be things such as fractures. They can occur from trauma or from osteoporosis, and these would need to be diagnosed and treated immediately.
Meningitis
Meningitis is a rare form of neck stiffness and pain. This is caused by infection, which can be viral, bacterial, fungal or parasitic. Bacterial meningitis is most common and is typically combated with vaccinations. If this is unrecognized, this can be fatal within a few days. Viral meningitis mostly resolves on its own, while fungal and parasitic infections can be severe, but they are much rarer. Symptoms usually include fever, stiff neck, headache, possible seizures, difficulty breathing, increased sleepiness, light sensitivity, and decreased appetite.
Home Remedies You Can Try
Relative rest can be tried to see if there is a muscle problem that goes away on its own.
Heat can be tried to relax the muscles and ease pain by using a heating pad or infrared heating pad.
Ice or cryotherapy may help soreness or swelling.
Doing some gentle stretching and light neck or upper back exercises may help.
Massage could potentially be beneficial to relax tight muscles.
Sometimes over-the-counter pain relievers such as Tylenol can be used.
Other pain relievers are nonsteroidal anti-inflammatory drugs or NSAIDs to reduce pain and inflammation.
How Stress Management Can Relieve Neck Pain
Stress can cause neck stiffness. Muscle tightness, which can pull on the neck and affect neck posture can cause headaches. Released stress hormones can make you more prone to inflammation and pain. So managing stress either with relaxation techniques, breathing techniques, or manual therapy such as massage can be very helpful.
When To See Your Doctor
It is best to see your doctor if some of your home remedies are not alleviating neck pain and it continues to persist or get worse. You should see your doctor if you are having pain, numbness, tingling, or weakness going down any extremity, if that is coming along very rapidly and not going away with any positions, maneuvers, or modalities, then you want to see your doctor right away.
Conventional Medical Advice On Stiff Neck
The traditional medicine approach to stiff neck symptoms might not be adequate for proper diagnosis and treatment. The traditional techniques include maybe doing a brief history, trying some medicines or home therapies. If that does not work, doing some specialized physical therapy may be helpful. All these are great, but if these things fail, the next typical steps may be steroid-type injections to help the pain, which can potentially help, but also can potentially make things worse and do not address the underlying issue.
Some nerve blocks and procedures can be done as both diagnostic tools and as a precursor to burn the nerves that can alleviate pain in the joint, but again have the sequelae of the consequences of burning nerves like making muscles weak. And then when these things fail, typically the only other solution offered is surgery — or just deal with it if no surgeon wants to operate.
However, there is a whole field of regenerative medicine or interventional orthopedics that can fill in the gaps for when physical therapy and home remedies are not enough and you do not quite need surgery. These techniques can include prolotherapy, PRP, or bone marrow concentrate containing stem cells, all of which are tools that can be injected precisely to stimulate your body’s own natural healing of certain areas.
Also, a proper diagnostic workup including a thorough history, thorough hands-on physical exam, perhaps ultrasound, perhaps MRI or imaging modality, perhaps several different diagnostic blocks with just local anesthetic to make sure you have made an adequate diagnosis.
How To Get A Proper Diagnosis
At the Centeno-Schultz Clinic, our diagnostic process consists of an hour-long evaluation in which we take a detailed history, a very thorough physical exam, ultrasound when appropriate, and reviewing of cervical x-rays that may include flexion/extension x-rays, a digital motion x-ray, and a cervical MRI. Most of the time with this information, we can have a firm diagnosis and develop a treatment plan. When the diagnosis is still not honed in, we can perhaps try some diagnostic blocks to further hone a diagnosis.
What Happens When Left Untreated
So when neck symptoms go untreated, these can lead to more serious problems, continued pain, worsening function for the patient. Sometimes things can progress overtime where the only solution may be surgery. If things go too far and then surgery was required but ignored, then it can cause some permanent deformity or permanent nerve-type injuries.
Latest Advances In Treating Stiff Neck
At the Centeno-Schultz Clinic, we have developed state-of-the-art treatments for chronic stiff neck. These include:
Prolotherapy injection, which is slightly irritating solution that can be injected into tendons and ligaments to help stimulate the body’s own repair mechanisms and has low risk and good evidence that they can help with neck instability.
PRP or platelet-rich plasma is a growth factor cocktail obtained from the blood. Blood can be taken, processed so that the platelets are isolated, concentrated for various formulations and can be injected into tendons, ligaments inside the joints, discs or around nerves with specialized platelet growth factors to help to repair those areas.
Bone marrow concentrate containing stem cells is the most powerful injection solution we can offer that is required for more severe cases, which can be injected into severely arthritic joints, disc tears, injured tendons, and ligaments with partial tears. The results of these techniques are tracked patients in the registry, which shows positive outcomes and pain, function and patient reported percentage improvement.
Do Not Miss What Your Body Is Telling You
If you have neck stiffness that is not going away with simple things or you are getting more concerning symptoms such as numbness, tingling, weakness, or radiation down the arm, then you need to get evaluated by a physician right away. The doctors at the Centeno-Schultz Clinic are experts in the diagnosis and treating musculoskeletal and orthopedic problems and in particular stiff neck, chronic stiff neck, and neck problems. We can offer a full diagnostic workup and develop a personalized specific treatment plan to help the pain by promoting your own body’s ability to heal itself without the use of drugs and surgeries so a more natural solution. You do not have to endure your neck pain for too long. Make an appointment with us today.
from Centeno-Schultz Clinic https://centenoschultz.com/stiff-neck/
0 notes