Photo

Fareway Chicken Salad, sold in Iowa, Illinois, Minnesota, Nebraska and South Dakota, has sickened at least 115 victims with Salmonella Typhimurium since January 1, 2018 – the salad was produced between Dec. 15, 2017 and Feb. 13, 2018 and sold in plastic tubs While the majority of the cases have been identified in Iowa, there are also reports of illness in South Dakota, Nebraska, Illinois, and a Martin County resident in Minnesota.
The U.S. Department of Agriculture’s Food Safety and Inspection Service (FSIS) has confirmed the outbreak, in conjunction with state and local health agencies, but it was the Iowa Department of Public Health that initially brought in the FSIS to begin the investigation of Salmonella related illnesses. FSIS acknowledged it is working with the Iowa Department of Public Health and Department of Inspections and Appeals on this investigation.
While the product has now been recalled, the primary fear of the FSIS is that some of the Fareway Chicken Salad may still be in patrons’ refrigerators or freezers. Importantly, Salmonella is not eliminated through refrigeration or freezing.
The Des Moines Register reported that the tainted Fareway Chicken Salad was prepared by Triple T Specialty Meats in Ackley. Triple T Specialty Meats produced the Fareway Chicken Salad specifically and uniquely for Fareway stores. At least one Ackley spokesperson has noted that the company’s factory was not in operation at the present time. No further information was provided.
TO discuss a salmonella illness, or to talk to a salmonella lawyer, click here.
1 note
·
View note
Photo

Jimmy Johns is ONCE AGAIN in the cross-hairs of salmonella litigation due to selling contaminated sprouts on their sandwiches. Jimmy John’s has been in this situation many times before, and now a Jimmy John’s Salmonella lawsuit has been drafted for an Illinois woman. For more information, go to www.foodrecallsinamerica.com
0 notes
Photo

Two El Toro Restaurants were closed this month in Tacoma, Washington, including one in Westgate and one on Bridgeport Way. They were closed following an outbreak of norovirus that sickened at least 542 patrons, this according to health officials in Peirce County, Washington. Preliminary reports indicate that patrons ate at these locations between December 31st through the 8th. The owner, Ruben Arias, is reportedly working with health officials voluntarily. He also released a statement “The well-being of our guests has been our highest priority since our restaurant’s founding in 1979.” According to reports in the News Tribune, three other locations of the restaurant chain were cleaned and sanitized as a precaution.
Norovirus outbreaks are common this time of year, but rarely are this many people liked to a single establishment or string of establishments , as in the case here. For more information about the El Toro Norovirus outbreak or to talk to a norovirus attorney, click here or call 281-851-9343.
0 notes
Photo
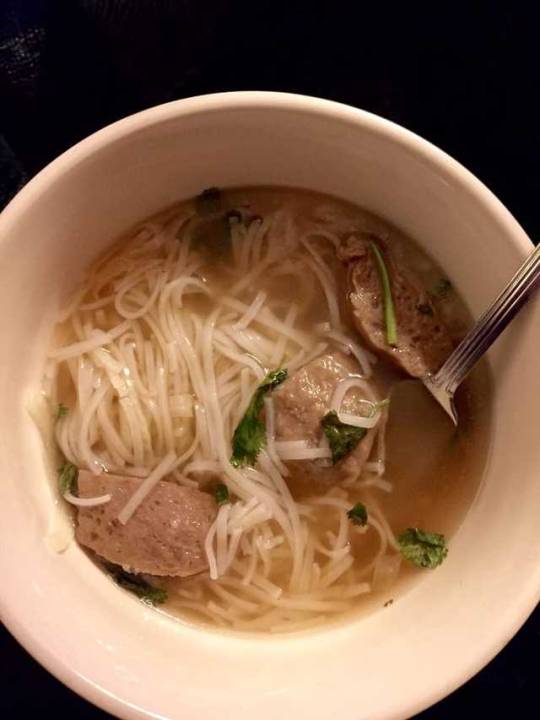
Seattle Washington restaurant closed after reports of food poisoning. The Pho Aroma, 5605 Delridge Way SW, Seattle, WA 98106, is closed while an investigation continues into a number of food poisoning reports potentially linked to food served patrons. The closure was ordered by King County Public Health on January 17, 2018. It remains unclear how many victims have been identified in this outbreak. Click here to speak to a food poisoning lawyer.
0 notes
Photo

French President Emmanuel Macron is now criticizing many of the retailers in France after Lactalis, one of his nation’s largest dairy product producers and providers of baby formula, issues a major recall for potential bacteria infected formula. In December, Lactalis ordered the recall of all the product from its Craon facility in NW France. Macron is just one of many to be critical of the recall, as reports continue to pour in that French retailers continued to offer the product for sale into January of this year. The French Agriculture Minister, Stephane Travert, stated that this represented a “major dysfunction in the withdrawal and recall” after news Lactalis products were still available for purchase at five major supermarkets. The company itself, Lactalis, is under criminal investigation and its Croan facility has been shuttered. The recall, which affects sales in 83 countries, currently includes a call for the return or destruction of about 12 million products. For more information about this large-scale recall, the impact globally and in France, or to talk to a food poisoning lawyer, call or text 281-851-9343.
0 notes
Photo

A major scare for consumers of salads: Often thought of as the most health options for a meal, recent E. coli outbreaks in Canada and the US, are reminding consumers that lettuce and other greens are only as safe as we make them. Consumers are encouraged to carefully wash all produce. Suppliers are also on the hook to make sure they follow proper GMPs and have proper HACCP in place - otherwise, they face the potential for large lawsuits and damage to their brand. One recent E. coli outbreak was linked to a popular grocery chain and resulted in significant litigation. And while the most recent E. coli outbreak liked to Romaine Lettuce was traced to a particular store or producer, it may yet be. Nearly 60 victims have been identified, including serous illnesses. For more information, call or contact a food poisoning lawyer hear.
0 notes
Photo

How Dangerous is Food Borne Illness? While most of the 48 million victims of food borne illness in the United States every year will recover without serious long-term impact, there is a small but consistently more recognized portion who are being diagnosed with post-infections IBS, IBD and Reactive Arthritis. Other studies are indicating post-infectious Crohn’s disease. The numbers still place the subgroup of victims at less than 5% of the total body of food poisoning vicinity, but this remains a significant number of people. Food Poisoning victims who develop thee conditions may do so for a year, decade, or even life. The cause remains under investigation, but may researchers have indicated that in some victims the immune and gastrointestinal systems that come under attack either recover very slowly or remain damaged for lengthy periods of time. For more information about long-term health implications, or to speak to a Food Poisoning lawyer, call or text 281-851-9343.
0 notes
Photo

Salmonella Lawyer Investigates Papaya Outbreak; Prepares Papaya Salmonella Lawsuit
One dead, 12 hospitalized, 47 victims identified in deadly Salmonella outbreak. Two strains of salmonella have been identified in the outbreak, though only one is confirmed to be part of the multi-state salmonella outbreak at present. The papaya salmonella outbreak is reminiscent of the listeria outbreak linked to cantaloupe a few years ago, this according to a salmonella lawyer who worked on the listeria cantaloupe cases, because the salmonella is on the husk, or peel, that is not eaten. The cutting process, however, infects the internal fruit and the salmonella is then ingested. After 12 to 72 hours (usually) the person becomes symptomatic with the signs of food poisoning, including vomiting (at times), diarrhea (always), nausea, head and body aches, an at times long-term illnesses such as IBS or reactive arthritis. Click here for more information about a salmonella lawyer or to file a salmonella lawsuit.
A papaya salmonella lawsuit is appropriate if you or a loved one was sickened after eating a papaya contaminated with salmonella. You can talk to a papaya salmonella lawyer at 713-306-3880.
1 note
·
View note
Photo

Nation-wide Outbreak of Salmonella linked to Papayas - once again a Mexico produce item is linked to a major outbreak. The Caribeña brand has been named as one of the brand implicated in the papaya salmonella outbreak - there may be others. So far, 12 states have felt the sting of contaminated Maradol Papayas - including Iowa, Kentucky, Louisiana, Massachusetts, Minnesota, New Jersey, New York (where one victim died), Pennsylvania, Texas, Utah, Virginia and Maryland (which reports at least 5 cases from one grocer). The one death was in New York. The victims are of all ages, including 1 years old to 97 years old, with more than a dozen being hospitalized. The Maradol Papayas originated in Mexico.
The primary stain in the papaya salmonella outbreak is Salmonella Kiambu -though another strain was also identified,
0 notes
Photo

Researchers from the University of Barcelona Enteric Viruses Group, led by scientists Rosa M. Pintó and Albert Bosch, have published findings in the Journal PloS Pathogens meant to understand and facilitate production of the Hepatitis A vaccination. The World Health Organization (WHO) has established that the Hepatitis A virus, or HAV, is the most prolific viral illness in the world, with about 1.4 million new cases annually.
This is amazing since HAV spreads through the traditional fecal-oral route and does not grow outside of the human body. Nonetheless, it is both difficult to detect and only a microscopic amount can begin the incubation process that will lead to illness onset 15 to 50 days post consumption.
According to Dr. Albert Bosch, because HAV does not grow easily outside the human body, and has a very low replication rate, vaccines are slow and expensive. But, explains Bosch, understanding the unique codon usage in HAV is key because HAV has a very unique pattern of behavior bonding only with tRNA, which occurs only rarely.
To challenge this behavior, researchers used actinomycin D to increase the available tRNA – a way of increasing HAV’s potential mating partners in the population.
With increased tRNA, however, the researchers saw a “Red Queen Effect” – the HAV simply re-adjusted to keep the low replication process. Some species/life forms have a built in mechanism of preventing their presence in a host to increase significantly. The mechanism for this is often a mystery. This “reaction” to actinomycin D seemed to defeat the process.
While the research of Drs. Pintó and Bosch to enhance HAV replication was unique and imaginative, HAV remains difficult to replicate.
For more information about HAV, click here.
1 note
·
View note
Photo

Food Poisoning in Fish: a New Study Summarizes Food Poisoning Outbreaks Linked to Fish Between 1998 and 2015
Of the six million food poisoning cases every year in the US, CDC believes more than a quarter million are linked to fish. During the 17 years of the study, at least 857 fish food poisoning outbreaks were identified, and these led to 4 fatalities, 359 hospitalizations, and nearly 5000 illnesses - and these are only the ones that are identified and counted, which is considered a very small portion of the overall numbers. Hawaii has has the highest number, accounting for a quarter of identified outbreaks, followed closely by Florida -together they account for half of all fish food poisoning outbreaks we know about. Of course this may be a result of the focus of health departments in those states or other unaccounted for factors. About a third of the “fish food poisoning” outbreaks were of scombrotoxin, followed by Salmonella and ciguatoxin. Vibrio was not counted among the fish food poisoning outbreaks, but figures highly among shellfish food poisoning outbreaks.
Tuna, mahi-mahi and grouper were the most commonly identified, with Salmonella linked to Tuna (there have been a number of high-profile salmonella sushi outbreaks), and scombrotoxin linked to both tuna and mahi-mahi.
The downside of this study is the difficulty in many outbreaks of identifying the actual source of the pathogen, beyond identification of the particular store, restaurant, or product. There may be many more cases where a pathogen is introduced into a location or product by fish but becomes synonymous only with the restaurant or finished product after cross contamination.
For more information about he study, click here.
0 notes
Photo

Vibrio is a potentially deadly bacteria that infect shell fish, especially oysters. Now, at least two dozen people have been infected in the Seattle Vibrio Outbreak of 2017, with people getting sick at restaurants such as Salted Sea; Wild Salmon Seafood Market; Chinooks; The White Swan Public House; Costco Wholesale #1225; Matt’s Rotisserie & Oyster lounge; and Elliott’s Oyster House. At least five of the victims in the Seattle Vibrio Outbreak of 2017 ate at the Salted Sea, while at least two of the victims of the Seattle Vibrio Outbreak of 2017 ate at the White Swan Public House. The exact location where the tainted oysters were harvested remains under investigation, though a number of them have been identified and subject to closure.
Among those beaches/areas where there have been closures for oysters since early June are growing areas in Grays Harbor, Poverty Bay, and Swinomish growing area. For a full list see here. May more locations are closed for scallops, which have often been linked to Vibrio.
The Washington State Department of Health (DOH) Shellfish Program is leading the trace-back investigation into the Seattle Vibrio Outbreak, which is proper protocol when an outbreak is linked to shellfish. All King COunty beaches are currently closed to clam harvesting.
As recently as March of 2015 the Washington State Board of Health (WSBH) adopted a new “Vibrio parahaemolyticus control plan” or rule WAC 246-282-006, to prevent the spread of Vibrio. The plan requires harvesters to have a Vibrio Control Plan and to follow very specific requirements in the harvesting and processing of the shellfish. For details, see here.
For more information about the Seattle Vibrio Outbreak of 2017, click here.
0 notes
Photo

Chipotle, Chipotle, Chipotle ... Norovirus, Salmonella, E. coli ... It appears this chain has had more food poisoning outbreaks than its next several rivals combined! In 2015, there were closures in Boston, Oregon, California (where a criminal investigation was opened in Simi Valley), and other locations. Now it is Virginia at the Tripleseven Road location in Sterling. Many of the problems seemed to stem from growing too fast and sourcing locally (small producers with, arguable, less stringent production standards). Chipotle has been criticized for failing to focus on HACCP/GMPs and has been accused of pressuring sick employees to come to work. Norovirus, which is suspected as the root of the recent closure, spreads easily but almost always through cross contamination, While Salmonella, E. coli or Listeria may be introduced into a food item, such as purchased tomatoes or flour,at multiple stages of harvest, production, transport or preparation, norovirus us traditionally injected into a food establishment by a sick person who touches items of surfaces, and then through cross contamination, the virus spreads throughout the establishment.
For more information on what to do if you get food poisoning, or to make a food poisoning claim, click here.
0 notes
Photo

Restaurant Cross Contamination is a Leading Cause of Food Poisoning in Localized Outbreaks
Here are the SIX BEST RULES for restaurant prevention of Cross-Contamination:
Emphasize Personal Hygiene - this includes having a no-sick policy where workers stay home when ill; regulation of clothing with clean aprons, smocks, and hair-nets; hand-washing and careful restroom policies; and use of disposable gloves.
Washing Hands. Not only when returning to work, but between tasks. A good worker will wash their hands every time they move from one preparation to the next. It also means using a DEDICATED hand sink, with soap, and adequate wash time - not just a quick rinse.
Avoid “Open Food Areas”: The use of condiment bars, buffets, and self-serve sis dangerous because a restaurant cannot control the traffic coming through their restaurant, or regulate the consumers’ behavior, effectively. Sick customers will frequent restaurants at times, and introduce pathogens. Using sneeze guards and other safeguards may help, but not having open food areas is always safer.
Separating Equipment. Food preparation should entail dedicated cutting boards, knives, and other equipment whenever possible. A key to preventing cross contamination is making sure equipment used for raw meat never touches or is used for preparation of vegetables, etc... A counter-top used to prepare raw poultry will be very unsafe and cleaning is often difficult - there are cracks, crevices, and spots that regular cleaning might miss. To the extent possible, a raw food preparation surface should only be used for foods that will be cooked.
Always Spend Time Cleaning and Sanitizing. This is vital because once bacteria or a virus get a foot hold, they can grow, spread, and become embedded. Too often these pathogens spread throughout en entire facility. Proper cleaning and sanitizing, done regularly, will help minimize and prevent the spread of food borne illness.
Using Prepared Foods. Using food that is processed is safer because there is less handling and less human contact required. Less human contact lessens the number of points at which pathogens can be introduced.
For more information about food poisoning outbreaks, call food poisoning lawyer Tony Coveny at 713-306-3880.
0 notes
Photo

The Smokehouse of New York, LLC, headquartered in Mamaroneck, New York, is subject to an order to cease selling its products. A U.S. federal judge in the Southern District of New York, the Honorable Joon H. Kim, issued the order after the U.S. Food and Drug Administration (FDA) identified listeria in its processing facility on multiple visits. The president of the company, Panagiota Soublis, was given the consent decree of permanent injunction on June 29, 2017. According to an Associate Commissioner for Regulatory Affairs at the FDA, Melinda K. Plaisie: “The Smokehouse of NY had several opportunities to come into compliance with the law. Through the use of modern technology, the FDA was able to establish that the company has resident strains of L. mono in its facility that it has consistently failed to eradicate. Conditions like these are unacceptable and the FDA took action to protect Americans.”
The initial finding was back in August of 2011 at the Mamaroneck facility. In a warning letter that followed, the FDA detailed significant violations of both Hazard Analysis Critical Control Point (HACCP) regulations and the Good Manufacturing Practice regulations in effect for seafood. Then, in 2013, the FDA again noted that the deficiencies at the Smokehouse were not being corrected. The problem then came to a head when, following an April 2017 inspection, investigators listeria throughout the facility in critical locations. The FDA observed poor sanitation, inadequate handwashing, improper disinfection practices, and “a failure to prevent cross-contamination between raw, in-process and finished products.”
No known illnesses were identified in the FDA report, but the listeria samples were subjected to PFGE typing to help the FDA identify illnesses should they be linked to the contaminated fish products.
0 notes
Photo

SAFELY SELECT AND PREPARE FRUITS AND VEGETABLES
Nature has provided numerous fruits and vegetables for us to consume as part of a balanced diet. They have been shown to provide resistance to some of the major killers – including heart disease, stroke, and even cancers (many contain anti-oxidants which are understood to fight cancer). They also provide alternatives to the processed and calorie-rich fast foods, processed foods, and quick /satisfying starches and carbs we can get on the run. But many of us struggle when trying to choose what vegetables, fruits, or nuts —we should be eating or serving.
Then there is the problem of food borne illness. A good dozen times a year we hear of another recall due to raw fruits, nuts, or vegetables containing Salmonella, E. coli, and Listeria, which can cause illnesses that often require hospitalization, long-tern illness, or keep us from work – all this in addition to feeling like we could die at any moment!.
To greatly improve your chances of eating only safe vegetables, nuts or fruits, always wash products that can be washed; refrigerate products that require refrigeration (even if they do not, cold temperatures reduce the spread/multiplication of pathogens on food); stay away for high-risk foods, like sprout which are notoriously hard to clean and often consumed raw; and clean utensils and knives (a few years back, a deadly listeria outbreak was linked cantaloupes - the listeria was on the shell, but introduced into the fruit through the cutting process.
In selecting which fruits or vegetables to buy – and how to prepare – follow these simple steps: (1) Inspect all fruits and vegetables for damage, such as a cut or bruise, as these can become contaminated. (2) Discard all fruits and vegetables that look spoiled or are subject to recall (its not worth the risk trying to clean them). (3) Wash all produce that is amenable to washing. (4) Wash your hands, counters, utensils, before, during and after handling produce. (5) Dry fruits and vegetables with a clean paper towel. (6) Do not store fruits and vegetables next to or below raw meat, seafood, or other foods that will need to be cooked. (7) Refrigerate all fruits and vegetables that have been cut or peeled, as these are more susceptible to contamination. (8) For fruits or vegetable dishes, refrigerate at 40°F or below after preparation.
While no guarantee, these steps will help prevent the spread of food borne illness among your family, friends, and co-workers.
0 notes
Photo

A Primer of Proper Cooking Temperatures for Meat, Dairy and Seafood
Often its hard to remember what temperatures, or hold times, are necessary to prevent illness when preparing meat for our friends and families. Here is primer on recommended temperatures for cooking:
(1) Red ground meats, such as beef, veal pork or lamb, should be cooked to 160 degrees. (2) Ground poultry should be cooked to 165 degrees. (3) Red meat steaks, roasts and chops can be cooked to 145 degrees if then also held for three minutes at rest. (4) Whole poultry needs to be cooked to 165. (5) All fresh pork and ham needs to be cooked to 145 degrees, unless it is rep-cooked, then 140 should suffice. ALWAYS allow a three minute “rest and hold” period for pork (6) Eggs should always be cooked to solid, or when used in dishes, reach an internal temperature of 160. (7) Fin fish to 145, or test for doneness when flaky/opaque. (8) Lobster, shrimp and crabs: until flesh is pearly and opaque. (9) for clams, oysters and mussels, make sure the shell is closed when introduced into cooking and opens during cooking. (10) For Scallops, until milky white. opaque, and firm.
These recommendations will not prevents all food borne illnesses, but they will help prevent them. To review the source of this information, click here.
0 notes